How can you help a depressed person
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.
-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
How to help a person in depression - Such cases
Every week, Takie Dela answers questions from readers. Today we will talk about depression, or rather, how to be a good friend for a person who finds himself in this state.
***
Approximately one in four has experienced depression at least once in their life. Although sometimes we, wringing our hands, call depression just an attack of bad mood. It is necessary to distinguish between blues, a mild depressive state (minor depression, subdepression) and a real clinical depression, which can drag on for several months.
Clinical depression is characterized by three main symptoms:
- Bad mood. But not the kind that usually happens after a hard day or week. With depression, a person loses the ability to rejoice, does not enjoy the usual things - food, communication with friends, sex, music, films. This condition is called anhedonia.
- Violation of thinking. It is difficult for a depressed person to think, it seems that thoughts are “like jelly”. Work is slower.
- Motor retardation. Depression is always accompanied by a constant feeling of fatigue. Forcing yourself to go somewhere in this state is extremely difficult.
If these symptoms are observed for more than a month, then this is a reason to see a doctor, but you can cope with mild depression on your own, with the help of relatives and psychotherapy. But relatives should remember a few simple rules - what to do, and what should never be said. That's what psychologists recommend.
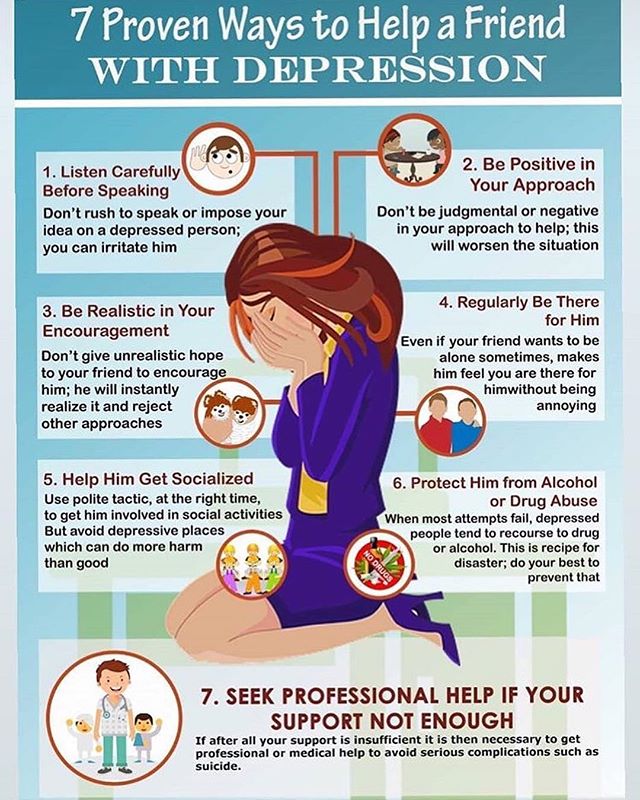
Let the person experience this state
Let's say your loved one experienced a failure, his expectations were not fulfilled, his plans were not realized. He is very upset, he is not happy with what he usually loves. Don't rush him. Say phrases: “Yes, stop thinking about it!” or “We need to move forward!” - it is forbidden. The state of sadness is not so bad for a person. Sadness allows you to relax a little after the race that was before, to come to your senses, to rethink, so that after that you can smoothly get out of this state.
He is very upset, he is not happy with what he usually loves. Don't rush him. Say phrases: “Yes, stop thinking about it!” or “We need to move forward!” - it is forbidden. The state of sadness is not so bad for a person. Sadness allows you to relax a little after the race that was before, to come to your senses, to rethink, so that after that you can smoothly get out of this state.
Be honest
“Yes, you failed to achieve the goal, but let's take a break and try again if you want, no - then try yourself in something else.”
Do not discount failure
Phrases: “Forget it”, “Stop it”, “Your failures mean nothing” will only make things worse. A person can and should learn from his failures a lesson. It just takes time.
Recognize the importance of this situation
“Yes, you tried, it didn't work, but it's important that you did it! The feelings you are experiencing right now are very important. Sadness, loss of strength - all this is natural, but I am there and will help you.
Sadness, loss of strength - all this is natural, but I am there and will help you.
Be careful with jokes
Do not joke rudely, scoff, ironically over the situation. Of course, it’s hard when a person close to you is in a bad mood, you want him to smile, and not go gloomy. It may seem that if you joke and make fun of the situation, then he will immediately cheer up and everything will immediately go smoothly. But it will most likely only get worse. Any rude intrusion, criticism will prevent you from getting out of a depressive state.
Do not force
It is strictly forbidden to forcefully drag a person to parties and walks in a depressed state. The mistake is that when we see a depressed person, we want to give him the energy of life. We say: "Look how great it all is!" But a person is simply not physically able to appreciate it. When he sees how people enjoy life, this only worsens his condition, he begins to wonder: "Why can't I do that?"
No aggression
Seeing that a person closes even more, in no case should one speak aggressively: “Why are you still in anguish?”, “Why are you sitting and being sad?”, “Pull yourself together, rag!” Such phrases are forbidden even as a joke.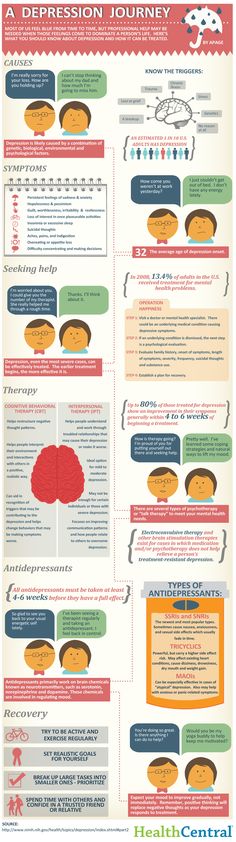
Be patient
Do not do anything excessive, be more restrained and calm. But if the condition of a person close to you does not improve within a month, this is a reason to contact a psychotherapist or psychiatrist. Perhaps we are talking about clinical depression, which must be treated with medication.
Help get rid of the fear of specialists
Many patients with clinical depression are afraid to go to a psychotherapist or psychiatrist. They think: “What if this is something worse than just depression, what if I’m going crazy” or “I can handle it myself”. Close people at this point should gently and carefully explain: “You know, it seems to be depression, and I read that it is completely cured. We will find a way out. Let's go to the specialist together. It seems to me that this will help you get out of this state.
Stay close
Stay close or nearby so your friend always knows that if they need help they will have someone to turn to.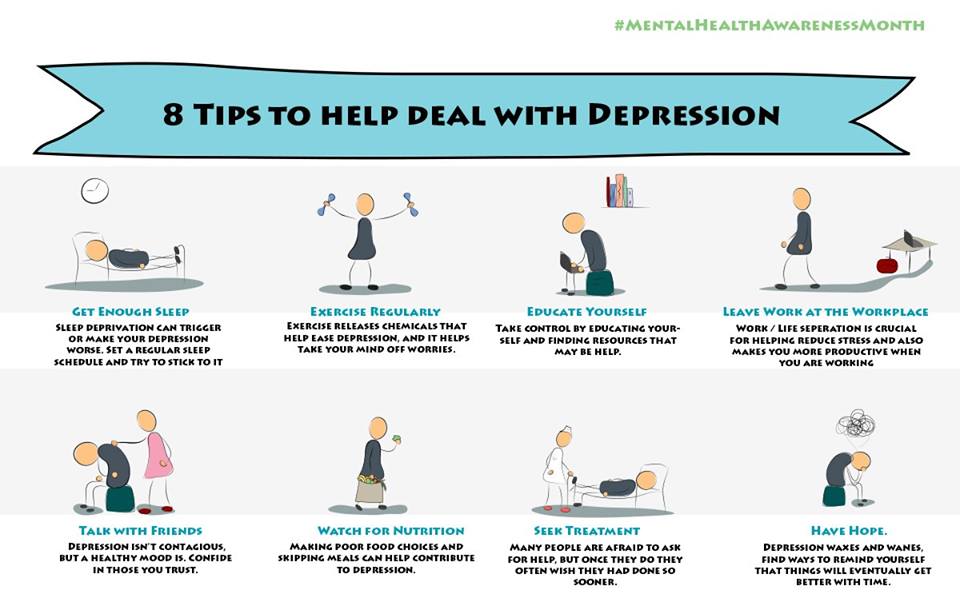
Do you want us to send you the best texts of "Such cases" to your e-mail? Subscribe to our weekly newsletter!
How to help a person with depression
Among relatives and friends of any person, people suffering from depression can meet. The help and support that a healthy person can provide to another person tormented by a depressive disorder is invaluable; the main thing is to do it as efficiently as possible and at the same time avoid common mistakes.
Contents
- 10 tips for helping a loved one with depression
- What not to do
- When intervention is needed
- Crisis support
According to the National Institute of Mental Health, more than 300,000,000 adults and children worldwide are living with depression worldwide. But not everyone experiences depression in the same way, and symptoms can vary from person to person.
If your friend or relative has a true depressive disorder, they may have specific symptoms, such as:
- the person becomes sad, he tends to cry;
- people with depression seem to be more pessimistic than usual, or who have lost all hope about the future;
- the patient often begins to talk about his feelings of guilt, spiritual emptiness or his own worthlessness;
- people with depression lose interest in communicating with others, begin to seek loneliness;
- such patients are easily distressed or become extremely irritable;
- their general tone decreases, patients move slowly or seem to be generally limp;
- they lose interest in their appearance or neglect basic hygiene, such as regular showering and brushing their teeth; 90,013 depressed patients have trouble sleeping or sleep much more than usual;
- patients care much less about their usual activities and interests;
- they become forgetful, have trouble concentrating or problem solving;
- depressed patients often eat more or less than usual;
- often talk about death or suicide.
Below are 10 tips for helping a loved one with depression, as well as a few tips on what to avoid when dealing with someone with depression.
1. The importance of listening to others
Tell a friend or loved one that you would like to help him or her in some way. You can start a conversation by sharing your own concerns and asking a specific question. For example: “You seem to be having a hard time lately. What happened that worries you? Keep in mind that your friend may really want to talk about how he feels, but at the same time, he may not want advice from others. A simple tactic of talking with the patient will help to better understand his condition, his mental problems:
- Ask questions to get more information, instead of "thinking out" what the patient's messages mean.
- Make it clear to the interlocutor that you are dealing with his problems. You might say, “It really does sound like you have a problem. I'm sorry to hear this".

- Show empathy and concern with your body language, that is, with appropriate movements and gestures. Your friend may not feel like being open about their problems right away, so it's worth continuing to talk to them about your concerns and desire to help from time to time. Keep asking open-ended questions (without being too pushy) and express your concerns. Try to keep conversations exclusively in private, tête-à-tête, whenever possible. If you live in different regions, try video chatting.
2. Help the person find qualified support
Your friend or relative may not know they are dealing with depression or may not be sure where or how to seek help. Even if he understands that therapy can help him solve problems, he may hesitate to start looking for a doctor and visit him for a long time. If your friend is interested in counseling, offer to help them find potential therapists. You can help your friends or loved ones make a list of questions to discuss with the doctor and identify the most pressing issues that they should definitely remember during the first visit. Encouraging and supporting the patient in finding a doctor and scheduling a date/time visit to his office is of great importance for the success of the treatment, especially when the patient does not dare to do it on his own.
Encouraging and supporting the patient in finding a doctor and scheduling a date/time visit to his office is of great importance for the success of the treatment, especially when the patient does not dare to do it on his own.
3. About supporting the patient during the course of therapy
On a particularly difficult day, your friend may not even feel like leaving the house. Depression can drain energy and increase the desire to self-isolate. If a friend or loved one starts saying things like, "I don't think I'll be going to psychotherapy anymore," start encouraging them to keep going.
You might say, “Last week you said that the treatment session was really productive, and after that you felt much better. What if today's session also significantly improves your condition?
The same applies to drugs. If your friend wants to stop taking medication because of unpleasant side effects, encourage him not to break his prescribed medication regimen, but at the same time start encouraging him to talk to his psychiatrist about switching to another antidepressant or stopping the drugs completely.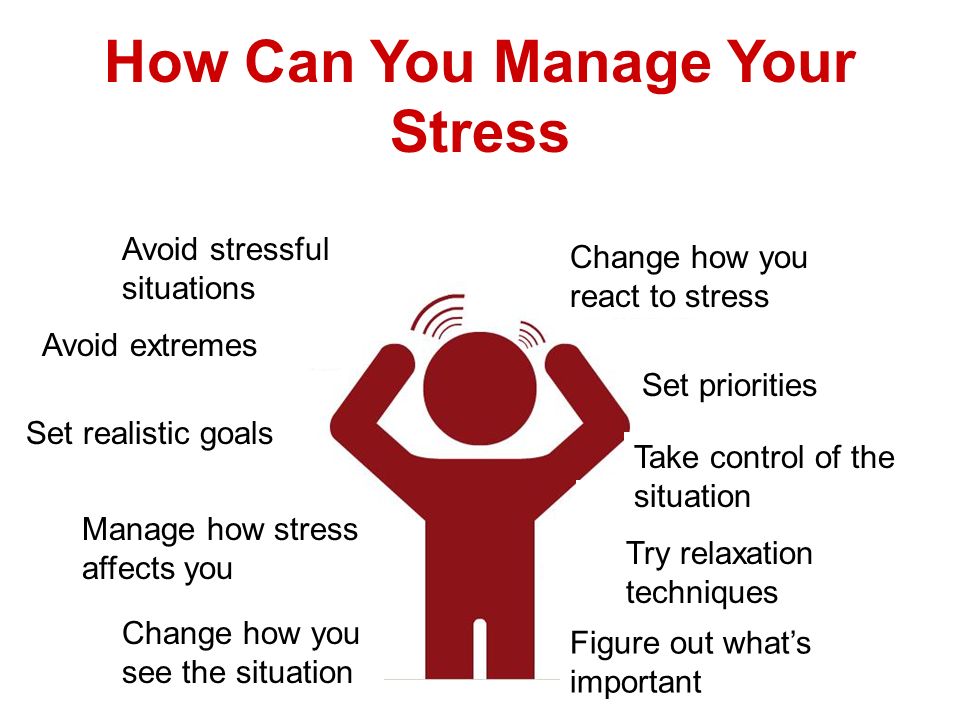 Abruptly stopping antidepressants without permission/supervision from a healthcare professional can have serious consequences.
Abruptly stopping antidepressants without permission/supervision from a healthcare professional can have serious consequences.
4. Don't forget to take care of yourself
When you're caring for someone living with depression, it's tempting to drop everything to be close to the depressed person and provide them with all kinds of support. If you want to help a friend, it's a noble gesture, but it's also important to take care of your own needs. If you begin to give all your energy to support a friend or loved one, you will have very little self-care left. And if later you start to feel "burnt out" or exhausted, this will not help your friend much.
Benefits of setting boundaries in communication
Setting boundaries can help you maintain your strength. For example, you can tell your friend that you can talk to him when you get home from work, but not before. If you're worried that a loved one or friend will worry about not being able to contact you, offer to help them come up with a contingency plan should they need to communicate with you during the work day.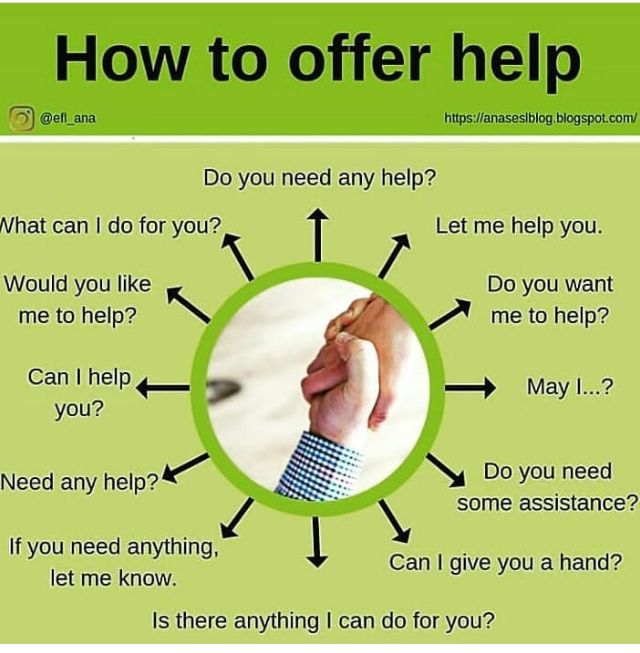 This may include looking up a hotline number they can call or a code word they can send you in a text message if they have a moment of crisis. You can suggest to the patient that you will visit him every other day or have lunch or dinner with him twice a week, instead of trying to help daily. Inviting other friends can help build a great support network.
This may include looking up a hotline number they can call or a code word they can send you in a text message if they have a moment of crisis. You can suggest to the patient that you will visit him every other day or have lunch or dinner with him twice a week, instead of trying to help daily. Inviting other friends can help build a great support network.
Take care of your own emotions
Spending a lot of time with a loved one who is depressed can cause emotional loss. Determine your limits on experiencing difficult emotions and make sure you have the time and opportunity to regenerate your soul. If you need to let your friend know that you will be unavailable for a short period of time, you can say something like, “I can't talk on the phone at certain times. But then I will definitely call you.
5. Raise your own awareness of depression
Imagine having to educate every person in your life about your mental or physical health problems - explaining it over and over again.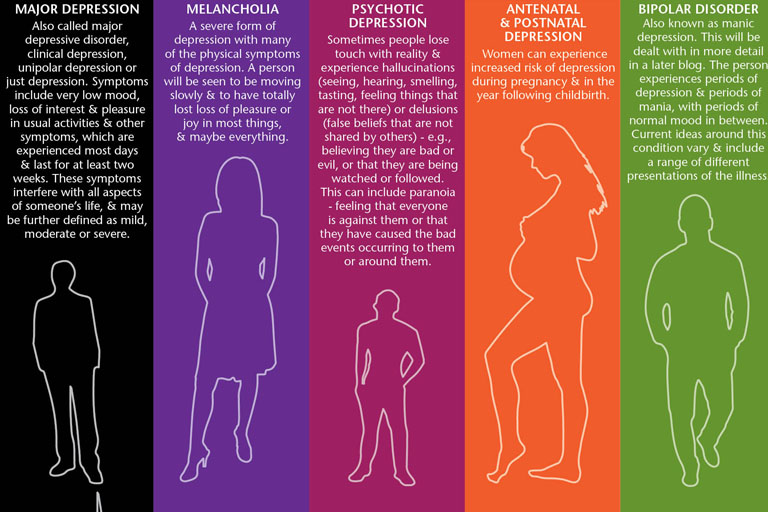 It would become too exhausting for you. You can talk to your friend about his specific symptoms or how he is feeling, but avoid asking him to tell you about depression in general. Read on your own about depression symptoms, causes, diagnostic criteria, and treatments.
It would become too exhausting for you. You can talk to your friend about his specific symptoms or how he is feeling, but avoid asking him to tell you about depression in general. Read on your own about depression symptoms, causes, diagnostic criteria, and treatments.
Although people experience depression differently, becoming familiar with common symptoms and terminology can help you have deeper conversations with your friend.
6. Offer help with daily living
Depression can make daily tasks seem overwhelming. Really simple things like doing laundry, grocery shopping, or paying bills can get left undone and start to pile up, and it ends up making it really, really hard to decide where to start. Your friend may appreciate the offer of help, but at the same time, it is also possible that he will not be able to clearly say what exactly he needs help with. So instead of telling the patient, "Let me know if I can do something," you should ask him, "What exactly do you need help with most today?" If you notice his fridge is empty, say, "Can we go shopping together, or will I buy what you need if you write me a list?" A perfectly acceptable option is: "Let's go grocery shopping and cook dinner together. "
"
If your friend has stopped washing the dishes, if they have a lot of dirty laundry or other unfinished household chores, call them, turn on the music and do the work together. Your presence and assistance will make it easier for him to do the job and it will not be given to him by an impossible task.
7. Inviting guests can improve the mood of the patient
People living with depression may find it difficult to maintain relationships with friends and make plans for the future or stick to them. But canceling plans can contribute to the feelings of guilt that are common in those who suffer from depression. Refusal of invitations can lead to a decrease in their number, and this can increase the patient's self-isolation. This in turn can worsen the symptoms of depression. You can help put your friend at ease by continuing to send out invitations to visit, even if you know for sure that he's unlikely to have to. Tell him that you understand that he may not follow through when he is especially depressed and there is no pressure on your part for him to come over until he is in the mood to do so.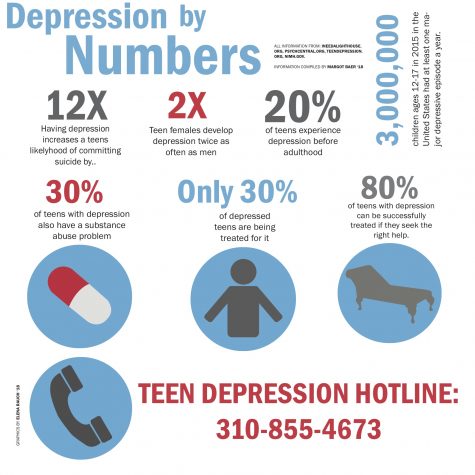 Just remind a friend or relative that you are always happy to see them whenever they feel like it.
Just remind a friend or relative that you are always happy to see them whenever they feel like it.
8. Be patient
Depression usually improves with treatment, but it can be a slow process that usually involves trial and error. Your friend and doctor may need to try several different approaches to counseling or medication before they find the best option. Even successful treatment does not always mean that depression is completely gone. Your friend may still have symptoms from time to time. Because of this, he will have good days and bad days - that is, days with a more or less normal or depressed mood. Avoid assuming that a good day means the friend is "completely cured" and try not to get frustrated if a series of bad days gives the impression that your friend's condition will never get better. Depression has no clear recovery timeline. Expecting your friend to return to their normal self after a few weeks of therapy is not a realistic approach to this illness.
9.
 Stay in touch
Stay in touch Reminding your friend that you care about them can help improve outcomes. Even if you can't spend a lot of time with your friend on a regular basis, keep in touch with them regularly via text, phone, or short visits to their home. Just by sending a short text with the message: “I think of you and care about you”, you can significantly improve your mood. People who live with depression may become more withdrawn and avoid socializing, so you may find that the situation requires you to make more efforts to maintain friendships. But the fact that you continue to be present in your friend's life as a positive character can go a long way towards improving his condition. Remind yourself regularly to your friend during his treatment for depression.
10. Depression can come in many forms
Depression often involves sadness or low mood, but it has other, less well-known symptoms. For example, many people do not realize that depression can have the following manifestations:
- temper tantrums and irritability;
- confusion, problems with memory or concentration;
- excessive fatigue or trouble sleeping;
- physical symptoms such as indigestion, frequent headaches, or pain in the back and other muscles.
Your friend may often be in a bad mood or feel exhausted for a long time. Try to understand that what he is feeling is still part of the depression, even if the symptoms do not fit into the stereotypical manifestations of this illness. Even if you don't know how to help your friend feel better, just tell them, “I'm sorry you're feeling bad. I'm here to help you if there's anything I can do" and maybe that will help.
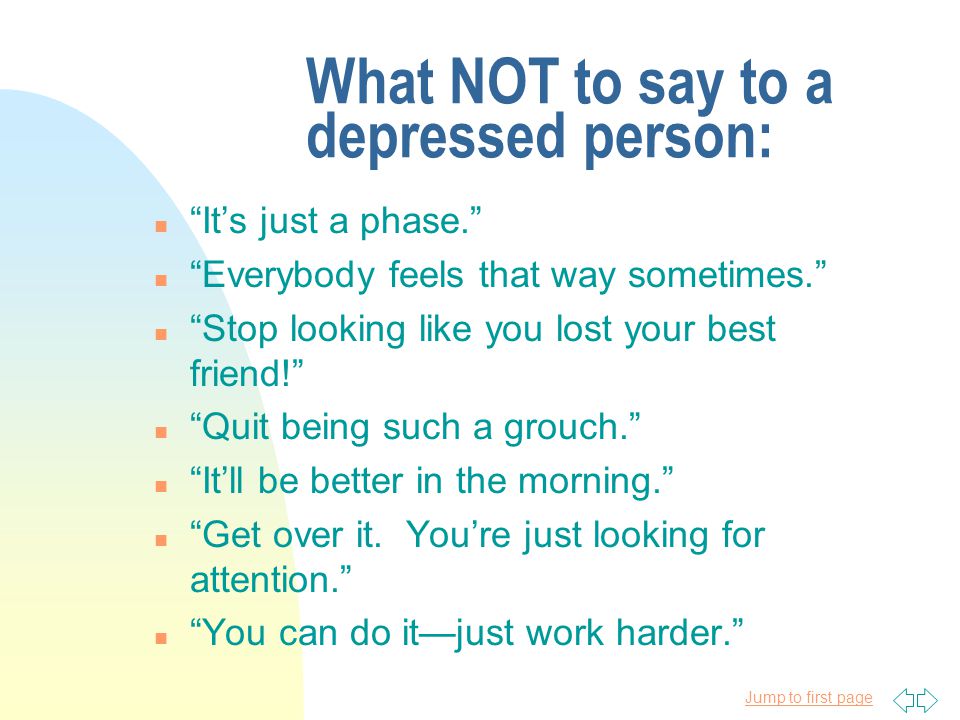
What not to do
1. Don't take things too personally
Your friend's depression is not your fault, nor is it his fault. Try not to let it affect you if he seems to lunge at you in anger or frustration, keeps canceling plans (or forgets to follow up), or avoids a lot of work. You may need to take a break from your friend at some point. It's okay if you're feeling emotionally drained, but it's also important to avoid blaming your friend or saying things that might contribute to negative feelings. Instead, consider talking to a therapist or other person about how you feel.
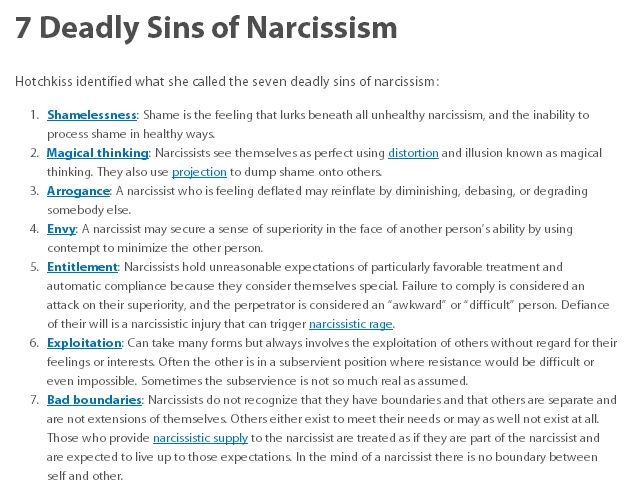
2. Do not try to correct the patient's behavior
Depression is a serious mental health disorder that requires professional treatment. It is difficult for a person who has never had depression to understand exactly what the patient feels. Clinical depression is not just a mood swing that can be improved with phrases like "you should be grateful for the good things in your life" or "just stop thinking about the sad things." If you don't want to say something vulnerable to someone who is living with a severe physical illness like diabetes or cancer, you probably shouldn't say that kind of thing to your friend with depression either. Positive support can let your friend know that they really matter to you.
3. Don't give unsolicited advice
While certain lifestyle changes often improve symptoms of depression, making these changes is difficult in the midst of a depressive episode. You may want to help a friend by offering advice, such as exercising more or eating healthier foods.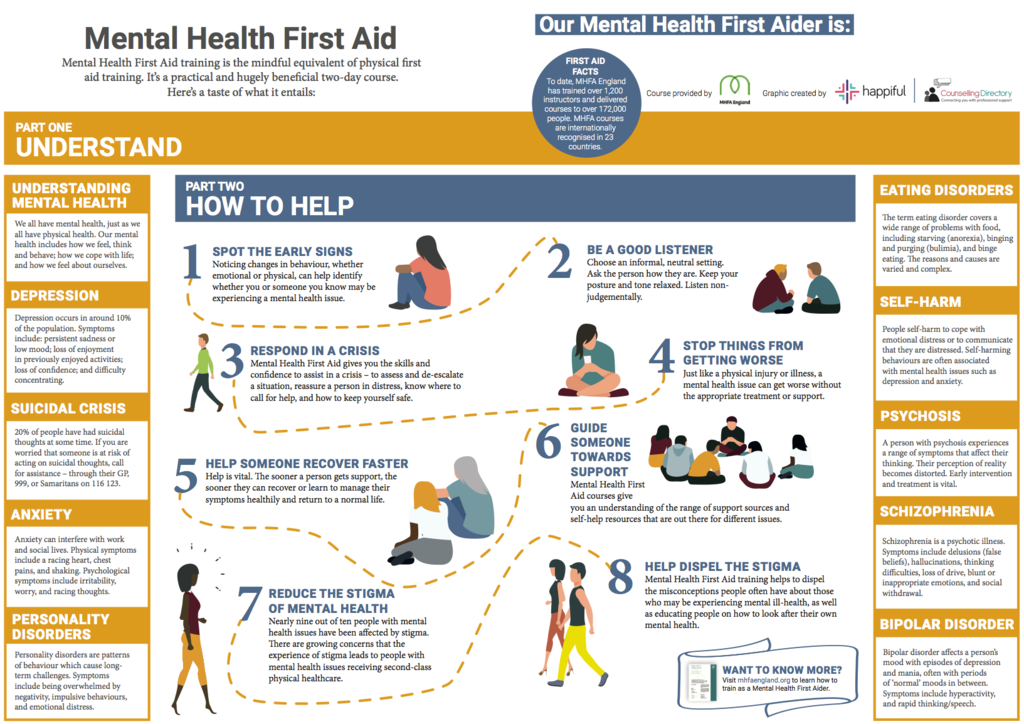 But, even if it's good advice, your friend may not want to listen to it at the moment. There may come a day when your friend wants to find out what foods can help with depression or how exercise can relieve symptoms. However, by this time, it may be best to stick to empathic listening and avoid offering advice unless he asks for it. Encourage positive change by taking a depressed friend out for a walk or cooking delicious meals together.
But, even if it's good advice, your friend may not want to listen to it at the moment. There may come a day when your friend wants to find out what foods can help with depression or how exercise can relieve symptoms. However, by this time, it may be best to stick to empathic listening and avoid offering advice unless he asks for it. Encourage positive change by taking a depressed friend out for a walk or cooking delicious meals together.
4. Don't belittle the patient's symptoms
If your friend is talking about depression, you can say something like, "I understand" or "We've all been through it." But if you've never dealt with depression, it can reduce your empathy to a minimum. Depression goes beyond just feeling sad or depressed. Sadness usually goes away fairly quickly, while depression can linger and affect mood, relationships, work, school, and every other aspect of life for months or even years. Comparing what a depressed person is going through to other people's troubles, or saying things like, "But it could have been a lot worse," usually doesn't help. Your friend's heartache is what is real to him. Say something like, “I can't imagine how hard it is to deal with this. I know I can't make you feel better, but remember that you are not alone."
Your friend's heartache is what is real to him. Say something like, “I can't imagine how hard it is to deal with this. I know I can't make you feel better, but remember that you are not alone."
5. Do not comment on prescription medications
Medicines can be very helpful for depression, but they are not for everyone. Some people have a very difficult time with the side effects of antidepressants and prefer to treat their depression with psychotherapy or natural products. Even if you think your friend should be taking an antidepressant, remember that medication choice is a personal decision. Also, if you personally do not believe in medicines, avoid discussing this when talking to the sick. For some people, medication is the only way to start the steps towards recovery. In the end, whether or not to take antidepressants is a very personal decision for the patient, which he usually has to make on his own after a detailed conversation with the doctor.
When Intervention Is Needed
Depression can increase a person's risk of suicide or self-harm, so it's good to know how to recognize the signs of this danger.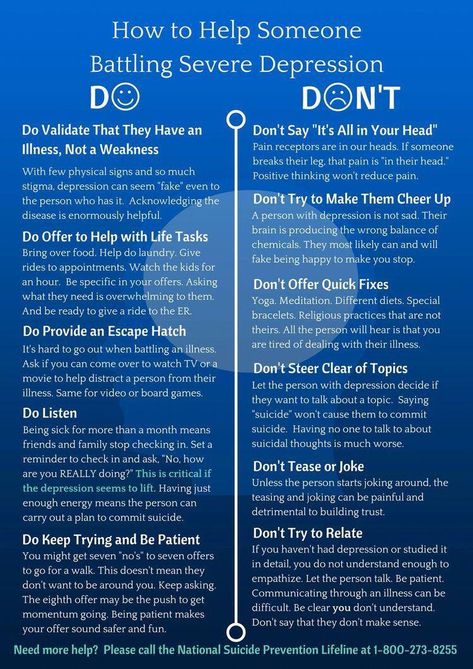 Below is a list of some of the signs that may indicate the presence of suicidal thoughts:
Below is a list of some of the signs that may indicate the presence of suicidal thoughts:
- frequent mood or personality changes;
- talk or death;
- acquisition of weapons;
- increase in alcohol consumption or initiation of drug use;
- risky or dangerous behaviour;
- disposal of own belongings or distribution of property;
- talking about feelings of being trapped or wanting to end all problems at once;
- self-isolation;
- too expressive farewell after each meeting.
If you think your friend is thinking about suicide, ask him to call his GP while you are with him, or ask your friend for permission to call his doctor instead.
Crisis Support
You can also take your friend to a mental health emergency room. If possible, stay with him until he has no more suicidal thoughts. Make sure he can't access weapons or drugs. If you're worried about your friend's mental state, you might start to worry that mentioning it might make them think about suicide.