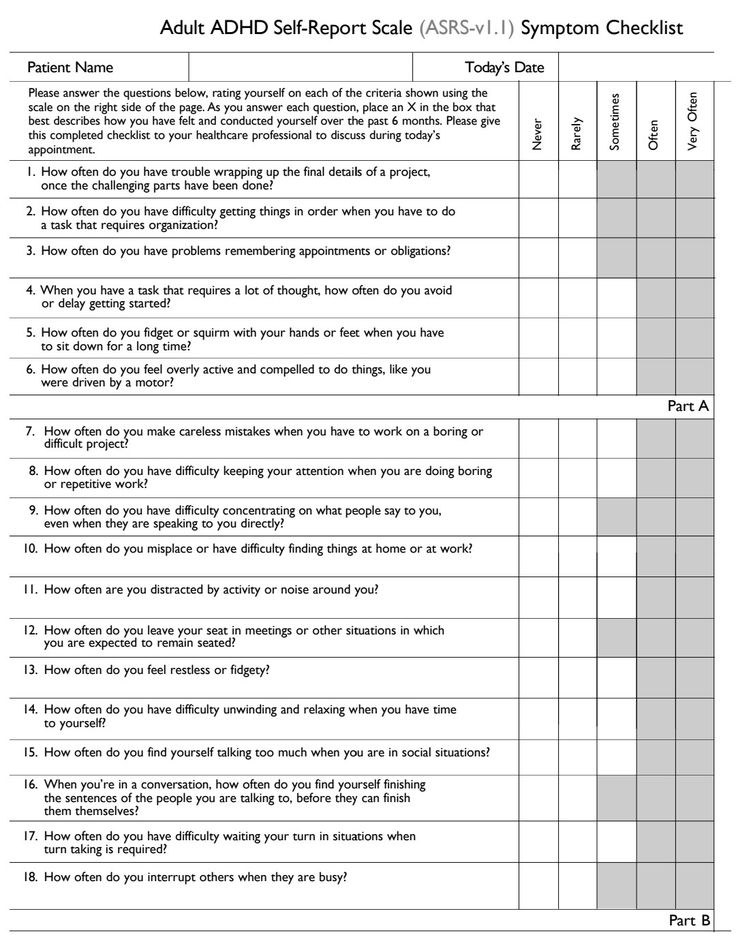
Adhd questionnaire uk
ADHD Test Online | Clinical Partners
Share this page
Question 1
I find it difficult finishing a task or project
- Never
- Rarely
- Sometimes
- Often
- Very often
Question 2
I find it difficult to organise myself or a task
- Never
- Rarely
- Sometimes
- Often
- Very often
Question 3
I find it difficult to remember appointments
- Never
- Rarely
- Sometimes
- Often
- Very often
Question 4
If a task or project requires a lot of thought I will often delay in getting it started
- Never
- Rarely
- Sometimes
- Often
- Very often
Question 5
I find it difficult to sit still and often fidget or squirm
- Never
- Rarely
- Sometimes
- Often
- Very often
Question 6
I would describe myself as being ‘on the go’ and feel compelled to do things, as if driven by a motor’
- Never
- Rarely
- Sometimes
- Often
- Very often
Question 7
I find it hard to remain focused in group settings
- Never
- Rarely
- Sometimes
- Often
- Very often
Question 8
My mind feels very cluttered and it is hard for me to concentrate on one thing at a time
- Never
- Rarely
- Sometimes
- Often
- Very often
Question 9
I make decisions quickly and fail to think through the consequences
- Never
- Rarely
- Sometimes
- Often
- Very often
Question 10
I am often irritable, with a short fuse
- Never
- Rarely
- Sometimes
- Often
- Very often
Question 11
I have mood swings, sometimes feeling quite high, other times low
- Never
- Rarely
- Sometimes
- Often
- Very often
Question 12
I often miss what is being said to me in conversations
- Never
- Rarely
- Sometimes
- Often
- Very often
Question 1 of 12
When answering the above questions please consider how they have applied to you in the 6 months or so.
This test will give an indication as to whether you are experiencing the most common symptoms of ADHD, but it cannot replace a full assessment nor should be used to self diagnose or decide upon a treatment plan.
This test was adapted from: Adapted from Mulhauser’s The Structured Adult ADHD Self-Test (SAAST)
Need to talk?
0203 326 9160 0203 326 9160
A free, confidential call could quickly help you get the support you need. Your call will be answered by an assistant psychologist who will listen to your concerns before explaining your options and suggesting the most appropriate treatment.
Take another test
View all tests
We have online mental health quizzes for many conditions including ADHD, autism, anxiety, depression, PTSD, and more. Each one should take no longer than five minutes.
Attention deficit hyperactivity disorder (ADHD) - Diagnosis
If you think you or your child may have attention deficit hyperactivity disorder (ADHD), speak to a GP.
If you're worried about your child, it may help to speak to their teachers, before seeing a GP, to find out if they have any concerns about your child's behaviour.
The GP cannot formally diagnose ADHD, but they can discuss your concerns with you and refer you for a specialist assessment, if necessary.
When you see a GP, they may ask you:
- about your symptoms or those of your child
- when these symptoms started
- where the symptoms occur – for example, at home, in school, college or university, or at work
- whether the symptoms affect your or your child's day-to-day life – for example, if they make socialising difficult
- if there have been any recent significant events in your or your child's life, such as a death or divorce in the family
- if there's a family history of ADHD
- about any other problems or symptoms of different health conditions you or your child may have
Next steps
Children and teenagers
If the GP thinks your child may have ADHD, they may first suggest a period of "watchful waiting" – lasting around 10 weeks – to see if your child's symptoms improve, stay the same or get worse.
They may also suggest starting a group-based, ADHD-focused parent training or education programme. Being offered a parent training and education programme does not mean you have been a bad parent – it aims to teach you ways of helping yourself and your child.
See treating ADHD for more information.
If your child's behaviour does not improve, and both you and the GP believe it's affecting their day-to-day life, the GP should refer you and your child to a specialist for a formal assessment.
Adults
For adults with possible ADHD, the GP will assess your symptoms and may refer you for an assessment if:
- you were not diagnosed with ADHD as a child, but your symptoms began during childhood and have been ongoing since
- your symptoms cannot be explained by a mental health condition
- your symptoms significantly affect your day-to-day life – for example, if you're underachieving at work or find intimate relationships difficult
You may also be referred to a specialist if you had ADHD as a child or young person and your symptoms are now causing moderate or severe functional impairment.
Assessment
You or your child may be referred to 1 of the following types of specialist for a formal assessment:
- a specialist child or adult psychiatrist
- a paediatrician – a specialist in children's health
- an appropriately qualified healthcare professional with training and expertise in the diagnosis of ADHD
Who you're referred to depends on your age and what's available in your local area.
There's no simple test to determine whether you or your child has ADHD, but your specialist can make an accurate diagnosis after a detailed assessment. The assessment may include:
- a physical examination, which can help rule out other possible causes for the symptoms
- a series of interviews with you or your child
- interviews or reports from other significant people, such as partners, parents and teachers
Diagnosis in children and teenagers
Diagnosing ADHD in children depends on a set of strict criteria. To be diagnosed with ADHD, your child must have 6 or more symptoms of inattentiveness, or 6 or more symptoms of hyperactivity and impulsiveness.
To be diagnosed with ADHD, your child must have 6 or more symptoms of inattentiveness, or 6 or more symptoms of hyperactivity and impulsiveness.
Read more about the symptoms of ADHD
To be diagnosed with ADHD, your child must also have:
- been displaying symptoms continuously for at least 6 months
- started to show symptoms before the age of 12
- been showing symptoms in at least 2 different settings – for example, at home and at school, to rule out the possibility that the behaviour is just a reaction to certain teachers or to parental control
- symptoms that make their lives considerably more difficult on a social, academic or occupational level
- symptoms that are not just part of a developmental disorder or difficult phase, and are not better accounted for by another condition
Diagnosis in adults
Diagnosing ADHD in adults is more difficult because there's some disagreement about whether the list of symptoms used to diagnose children and teenagers also applies to adults.
In some cases, an adult may be diagnosed with ADHD if they have 5 or more of the symptoms of inattentiveness, or 5 or more of hyperactivity and impulsiveness, listed in diagnostic criteria for children with ADHD.
As part of your assessment, the specialist will ask about your present symptoms. However, under current diagnostic guidelines, a diagnosis of ADHD in adults cannot be confirmed unless your symptoms have been present from childhood.
If you find it difficult to remember whether you had problems as a child, your specialist may wish to see your old school records, or talk to your parents, teachers or anyone else who knew you well when you were a child.
For an adult to be diagnosed with ADHD, their symptoms should also have a moderate effect on different areas of their life, such as:
- underachieving at work or in education
- driving dangerously
- difficulty making or keeping friends
- difficulty in relationships with partners
If your problems are recent and did not occur regularly in the past, you're not considered to have ADHD. This is because it's currently thought that ADHD cannot develop for the first time in adults.
This is because it's currently thought that ADHD cannot develop for the first time in adults.
Page last reviewed: 24 December 2021
Next review due: 24 December 2024
problem of parents or society? Principles of diagnosis, treatment and social adaptation of children with ADHD
03/27/2015
October 11-12, an open meeting of the working group was held in Kiev Ministry of Health of Ukraine on the development of requirements for program-targeted care for children with the most common forms mental disorders, during which topical issues were discussed diagnosis and treatment of hyperkinetic disorder, better known in society as Attention Deficit Hyperactivity Disorder (ADHD).
As part of the event for child psychiatrists and neurologists of Ukraine, the section of children's psychiatry of the Association of Psychiatrists of Ukraine together with the Department of Children's, Social and Forensic Psychiatry National Academy of Medicine postgraduate education. P.L. Shupyk and the Department of Social Problems of Therapy mental disorders of the Ukrainian Research Institute social and forensic psychiatry and narcology, an international seminar. The classes were conducted by well-known child psychiatrists from the Institute of Psychiatry and King's College London (Great Britain) - Professors Eric Taylor and Emily Simonov.
P.L. Shupyk and the Department of Social Problems of Therapy mental disorders of the Ukrainian Research Institute social and forensic psychiatry and narcology, an international seminar. The classes were conducted by well-known child psychiatrists from the Institute of Psychiatry and King's College London (Great Britain) - Professors Eric Taylor and Emily Simonov.
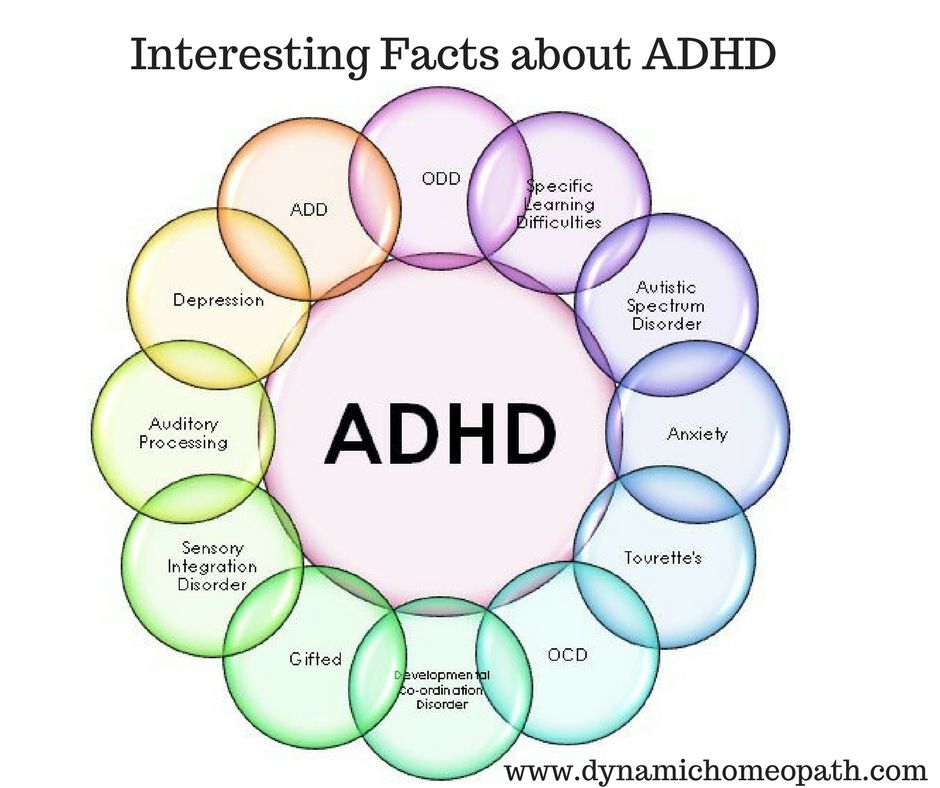
On the first day professor of child and adolescent psychiatry Emily Simonov gave a lecture on epidemiology, diagnostic criteria, typology, clinical and dynamic features and principles of ADHD classification. Attention Deficit Hyperactivity Disorder is a chronic mental neurodevelopmental disorder in children and characterized by a violation of the concentration function of attention, hyperactivity and impulsiveness. Serious complications of ADHD (Fig. 1) are insufficient the level of development of school skills, school maladaptation, behavioral disorders, formation of dependence on psychoactive substances.
Professor E. Simonov reported that when assessing the prevalence of ADHD, based on ICD-10 criteria, hyperkinetic disorder occurs in 1-2% of UK children. When diagnosing a disorder according to DSM-IV criteria for attention-deficit/hyperactivity disorder in 3-9% of children. The difference in scores is due to the fact that the disorder with attention deficit hyperactivity disorder while using the DSM-IV includes both more severe cases (hyperkinetic disorder in the understanding of ICD-10), and cases of attention deficit without hyperactivity.
According to the American Psychiatric Association, Attention Deficit Disorder and hyperactivity manifests in 4-12% of children aged between 6 and 12 years.
About 60% of children with ADHD experience problems with school adaptation, about 32% drop out of school. Children with Attention Deficit Disorder and hyperactivity, in adulthood have a lower professional level and often suffer from an inferiority complex. In their families 3-5 times higher divorce rate.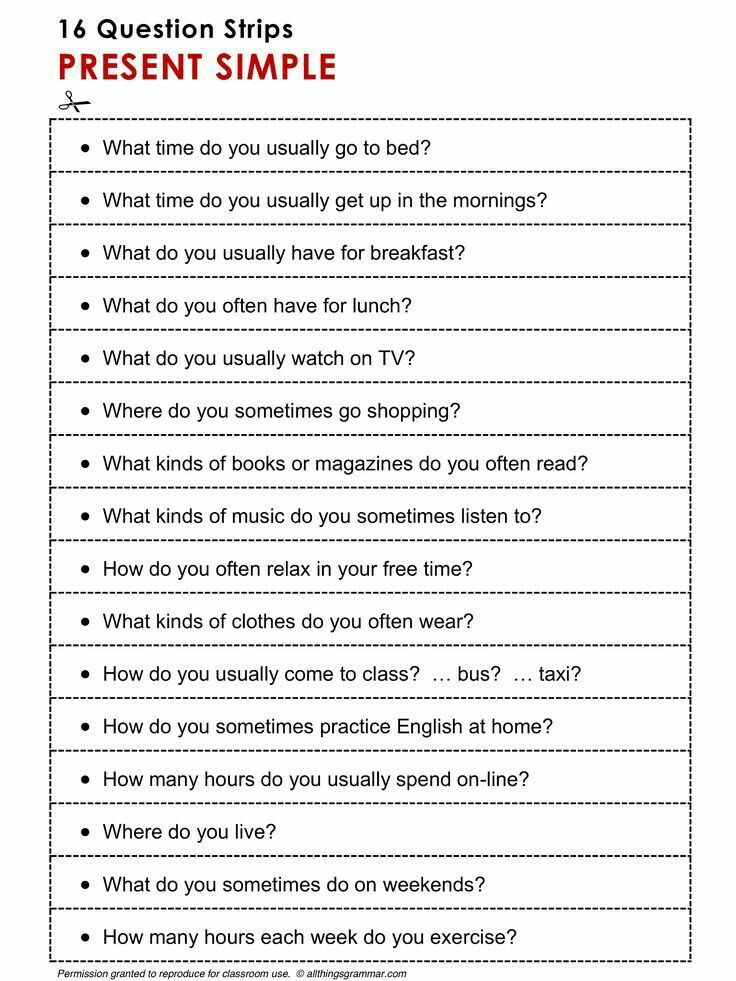 Among children with ADHD, a high percentage of adolescent pregnancy, 2 times the risk of developing alcohol dependence and psychoactive substances, a low probability of quitting smoking in adulthood, in 4 times higher risk of injury.
Among children with ADHD, a high percentage of adolescent pregnancy, 2 times the risk of developing alcohol dependence and psychoactive substances, a low probability of quitting smoking in adulthood, in 4 times higher risk of injury.
Clinical manifestations of ADHD are associated with structural and functional features brain, which may be due to the interaction of genetic, psychosocial factors and perinatal lesions of the central nervous system. Most children with ADHD have a genetic predisposition to development of this syndrome. Parents and relatives of hyperactive children similar violations of behavior are quite often noted.
There is now strong evidence that ADHD due to polymorphism and expression of genes with which they are associated insufficient activity of monoamine transporters, low sensitivity postsynaptic membrane receptors, regulation of release and reverse uptake of dopamine by the presynaptic membrane. Each of the listed genes increases the relative risk of developing attention deficit hyperactivity disorder slightly (at 1.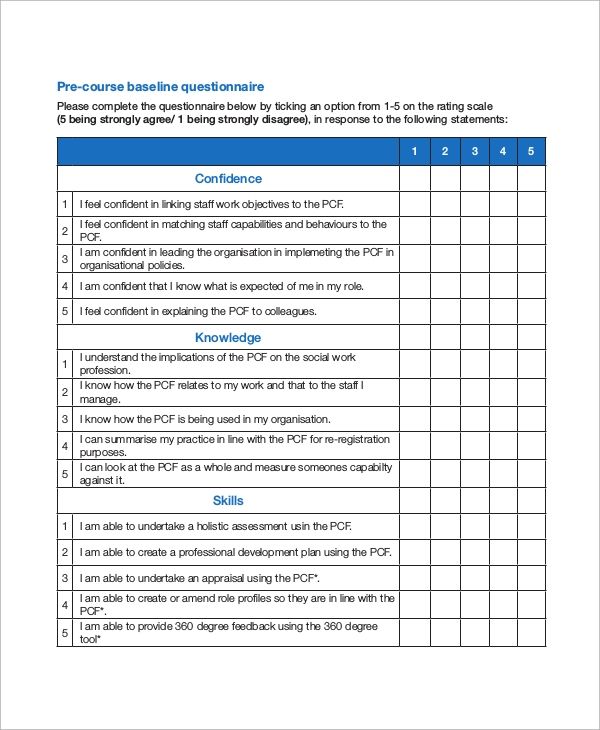 2-1.9times), which confirms the molecular genetic hypothesis that ADHD is caused by the interaction of many genomic factors, each of which has a weak independent influence. At the same time, several relatively rare genomic disorders (fragular X chromosome, genomic resistance to thyroid hormone), which have significant independent influence on the risk of developing the disease.
2-1.9times), which confirms the molecular genetic hypothesis that ADHD is caused by the interaction of many genomic factors, each of which has a weak independent influence. At the same time, several relatively rare genomic disorders (fragular X chromosome, genomic resistance to thyroid hormone), which have significant independent influence on the risk of developing the disease.
Recent studies have shown that children with ADHD have more slow maturation of the frontal lobe of the brain and the formation neuropsychological deficit. It is known that the anterior regions of the brain provide inhibitory effect on the ganglia of the brain stem - subcortical structures, providing automatic motor acts and non-purposeful motor activity. At the same time, this part of the brain is responsible for the connection between limbic system, brainstem ganglia, and cerebral cortex. Violation maturation of the anterior parts of the brain determines the formation of cognitive, emotional-volitional and psychomotor disorders.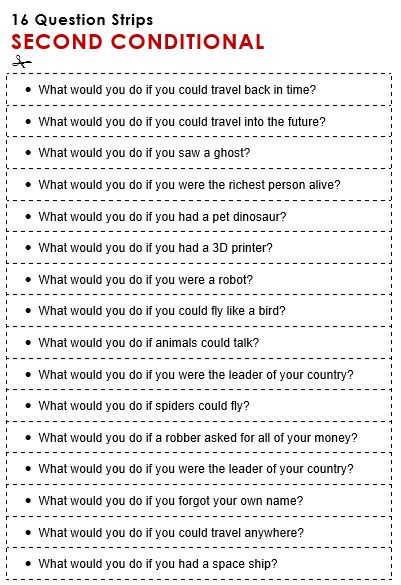
In patients with ADHD, there is an imbalance between the processes of arousal and braking. As a result, the main symptoms of ADHD are pronounced hyperactivity, impulsivity and impaired attention.
Symptoms of ADHD are usually clear once children reach 6 years of age. At the same time, parents complain about the child's lack of perseverance in completing tasks, requiring the involvement of cognitive functions, an overly rapid transition from one type of activity to another, the inability to complete many of the started cases. FROM some changes in the clinical picture of ADHD may occur with age due to changes in the ratio of symptoms: at a younger age more often predominates hyperactivity, in the older - inattention.
In addition to these symptoms, other disorders may be observed: cognitive disorders, specific delays in motor and speech development. Approximately at half of the cases in children with ADHD reveal impaired coordination. It could be clumsiness of movements, imbalance and visual-spatial coordination.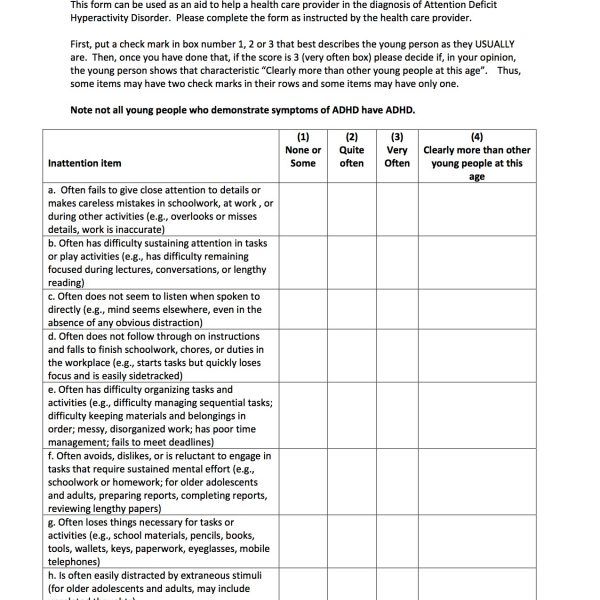
Emotional and volitional disorders are often observed in ADHD.
Many children with ADHD perform poorly in school, despite having a normal general score. mental development (IQ). Partial delays are common in ADHD development, including school skills (writing, counting, reading). Their main sign - the discrepancy between the actual performance and the one that can be expected based on IQ.
It must be remembered that ADHD is a disorder with a high index comorbidity, that is, it has a high frequency of concomitant mental disorders that also require timely detection and adequate therapy.
The correct qualification of comorbid disorders is essential for the correct planning therapeutic tactics for each individual child with ADHD.
Professor of Child and Adolescent Psychiatry Eric Taylor well known in the world as leader of the working group that prepared the European treatment protocols ADHD, in his lecture noted that, taking into account the system existing in Ukraine medical care and human resources, a preliminary diagnosis of ADHD could carried out by teachers and school psychologists by screening all children with behavioral problems.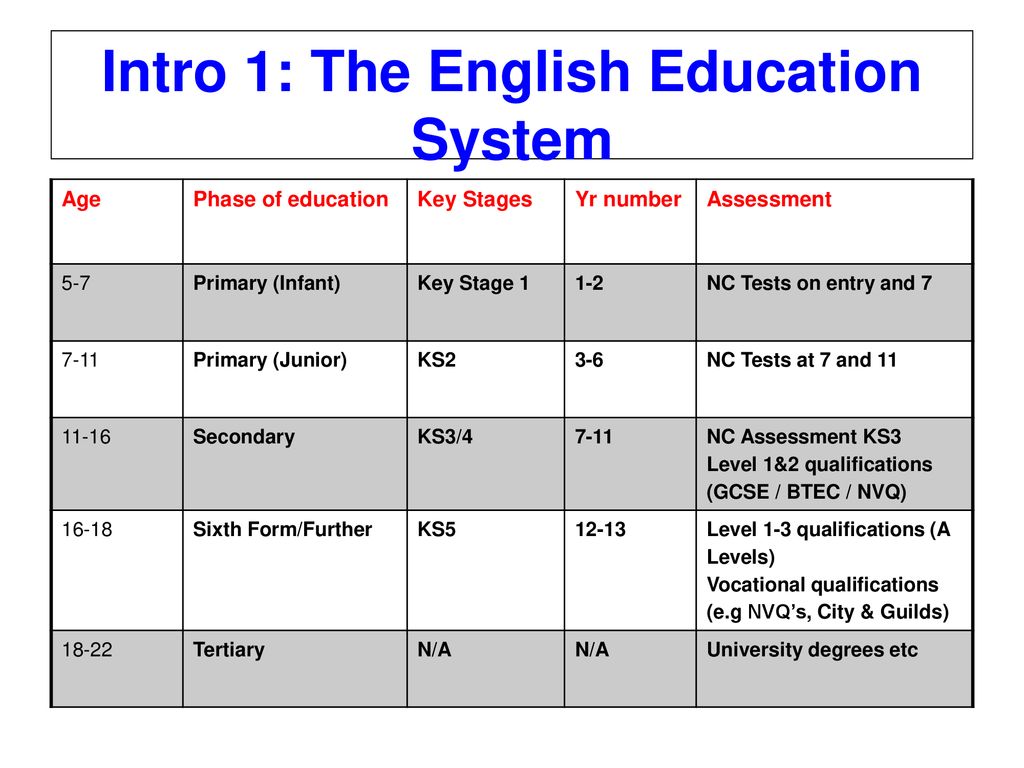 Professor proposed the final diagnosis of ADHD to lay on child psychiatrists and neurologists. Examination of a child with suspicion for ADHD should include conducting a structured interview and asking disorders of attention, activity and impulse control in various situations (at home, in school, among peers) at different times of the day. Screening on a scale Conners allows you to simplify the collection of formalized information from parents and child's teachers. As the main tool for diagnosing ADHD the professor suggested using a semi-structured interview developed a group of British researchers under his leadership. In agreement with authors in the sector of medical and social rehabilitation of children and adolescents with mental and behavioral disorders of the Ukrainian Research Institute of Social and forensic psychiatry, versions of the toolkit were prepared and tested on Ukrainian and Russian languages.
Professor proposed the final diagnosis of ADHD to lay on child psychiatrists and neurologists. Examination of a child with suspicion for ADHD should include conducting a structured interview and asking disorders of attention, activity and impulse control in various situations (at home, in school, among peers) at different times of the day. Screening on a scale Conners allows you to simplify the collection of formalized information from parents and child's teachers. As the main tool for diagnosing ADHD the professor suggested using a semi-structured interview developed a group of British researchers under his leadership. In agreement with authors in the sector of medical and social rehabilitation of children and adolescents with mental and behavioral disorders of the Ukrainian Research Institute of Social and forensic psychiatry, versions of the toolkit were prepared and tested on Ukrainian and Russian languages.
Abnormal levels are required for a diagnosis of ADHD inattention, hyperactivity and impulsivity, which are manifested in a wide range of diverse situations and persist over time. At it is necessary to exclude those cases that can be explained by stress situation in the family associated with its breakup, cruel attitude or sexual violence, other mental disorders such as mental health disorders autism spectrum, schizophrenia, mental retardation. Children with more intelligence higher than average may also experience problems with school adaptation due to inattention in the classroom, greater independence and impulsiveness in judgments and actions.
At it is necessary to exclude those cases that can be explained by stress situation in the family associated with its breakup, cruel attitude or sexual violence, other mental disorders such as mental health disorders autism spectrum, schizophrenia, mental retardation. Children with more intelligence higher than average may also experience problems with school adaptation due to inattention in the classroom, greater independence and impulsiveness in judgments and actions.
According to classification
DSM-IV identifies three forms of ADHD:
- combined;
- with a predominance of impaired attention;
- with dominant hyperactivity-impulsivity.
In ICD-10, attentional impairment is considered beyond hyperkinetic disorder.
ICD-10 for the diagnosis of ADHD provides for the use of the following list diagnostic criteria.
Carelessness. For at least 6 months, they are persistently present at least 6 signs of inattention from among the following (with symptoms are so pronounced that they are maladaptive and do not correspond to the level child development).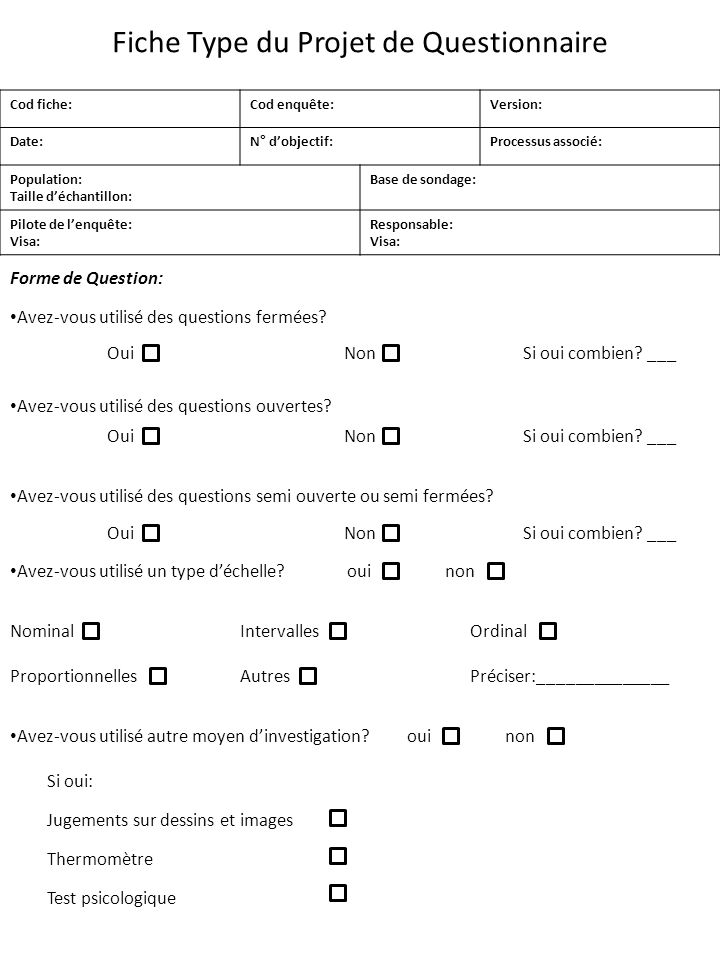
1. Often fails to pay close attention to details or allows (clearly not negligent) mistakes in schoolwork or other activities.
2. Often unable to hold attention for a long time in the process of performing tasks or play activities.
3. It is often noticeable that he does not listen to what he is told.
4. Often doesn't follow instructions given or doesn't follow through. school tasks or other responsibilities.
5. Often there is a violation of the ability to rational organization completing tasks.
6. Avoids activities that require constant mental stress.
7. Often loses things needed to complete certain tasks.
8. Easily distracted by external stimuli.
9. Often forgetful during daily activities.
Hyperactivity. For at least 6 months there are at least 3 signs of hyperactivity (moreover, the symptoms are so pronounced that they are maladaptive and do not correspond to the level of development of the child).
1. Often uneasily moves arms or legs, fidgets in a chair.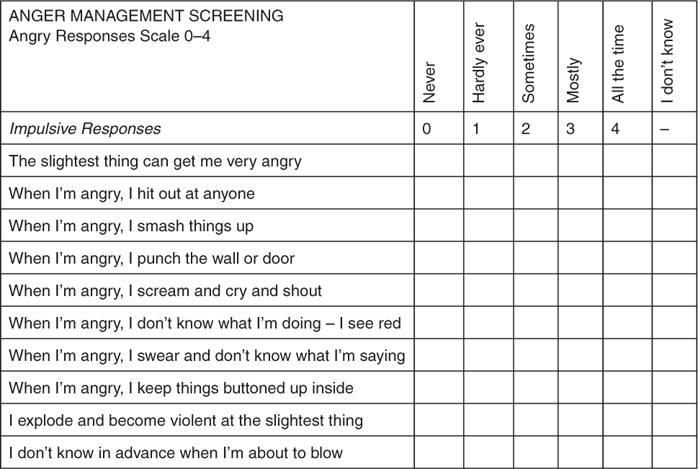
2. Leaves his seat at his desk or behaves in a similar way in a situation when you need to sit.
3. Often starts running or climbing in situations where this inappropriate.
4. Often makes excessive noise while playing or has trouble if you need to spend your leisure time in some quiet activity.
5. Demonstrates a consistent, persistent set of signs of overactivity, which is not significantly influenced by the social context or requirements adults.
Impulsiveness. For at least 6 months, one and more signs (moreover, the symptoms are so pronounced that they are maladaptive and do not correspond to the level of development of the child).
1. Often yells out an answer before the question being asked is final. formulated.
2. Unable to stand in lines, wait patiently for their turn at games, or group situations.
3. Frequently interrupts the lessons or speech of others or intervenes in various situations.
4. Often talks too much in the absence of an adequate response to attempts to regulate such behavior.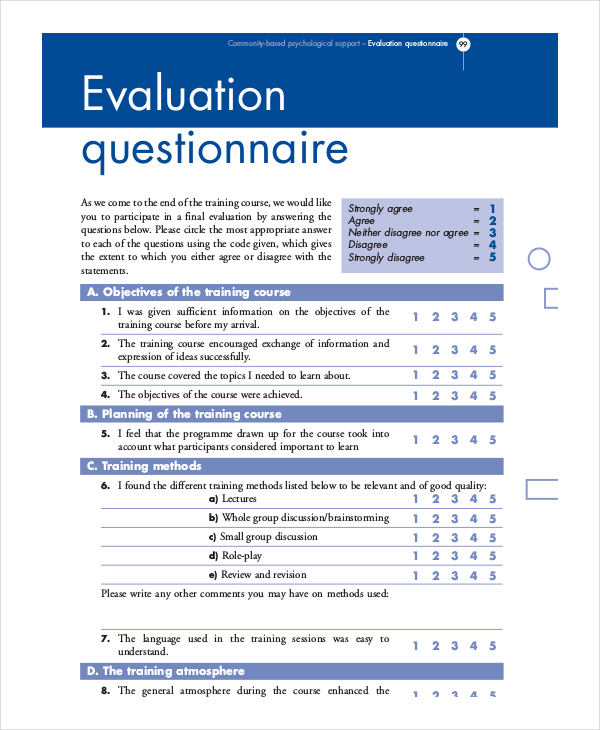
At the same time, all the symptoms are maladaptive in nature and do not correspond to the level child development.
The second seminar was devoted to the complex treatment of ADHD. Professor Eric Taylor gave a lecture on the general principles of psychological and social treatment children with ADHD and talked about how the main therapeutic interventions for ADHD are psychoeducation, behavioral therapy and psychopharmacotherapy. Therapeutic interventions should be aimed at the child, his parents, pedagogical environment. The most effective non-pharmacological methods are psychoeducation and training of parents and teachers in methods that increase the effectiveness of managing the behavior of the child. Behavioral therapy provides influence on the child by creating motivation for him to change his behavior. Cognitive psychotherapy and training also have positive results. social skills in children.
According to the European guidelines for the treatment of ADHD, the treatment of preschool children and also school-aged children with mild ADHD should start with behavioral therapy. Pharmacological treatment is added when behavioral therapy is ineffective therapy and in severe forms of the disorder.
Pharmacological treatment is added when behavioral therapy is ineffective therapy and in severe forms of the disorder.
According to the latest major study by the National US Institute of Mental Health (MTA Cooperative Group, 1999, 2004), in which compared the effectiveness of behavioral, drug and combination therapy for ADHD, isolated use of pharmacotherapy according to compared with the use of behavioral therapy is much more effective. In the study, combination therapy (combination of pharmacotherapy with behavioral) had little benefit compared to isolated pharmacological treatment. However, combination therapy according to the same research is more effective in terms of improving the situation in family, as well as influence on comorbid disorders.
in a lecture on the principles of pharmacological treatment of ADHD, Professor Emily Simonov spoke about the fact that the evidence base regarding the effectiveness in the treatment ADHD has drugs that regulate the activity of the neurotransmitters norepinephrine and dopamine. According to modern European recommendations, drugs of the first of choice in the treatment of ADHD are psychostimulants.
According to modern European recommendations, drugs of the first of choice in the treatment of ADHD are psychostimulants.
Psychostimulants have been successfully used for several decades in worldwide for the treatment of ADHD as the most effective drugs for these disorders (Fig. 2).
The mechanism of action of psychostimulants is to block the reuptake catecholamines by presynaptic nerve endings and their breakdown monoamine oxidase. As a result, the concentration in the presynaptic gaps of monoamines (dopamine and / or norepinephrine).
One of the problems associated with psychostimulant treatment is the need to provide the child with sufficient concentration function of attention in the morning (to eliminate behavioral disorders in the family before school), at school, after schools (due to the need to ensure the effectiveness of homework tasks), in the evening (to eliminate behavioral disorders when communicating with peers and family members). Refuse the complex selection of doses and their timing admission, avoid the need to involve teachers in ensuring control over taking the drug during the child's stay at school allows the introduction of clinical practice of long-acting psychostimulants, in particular methylphenidate (Concerta).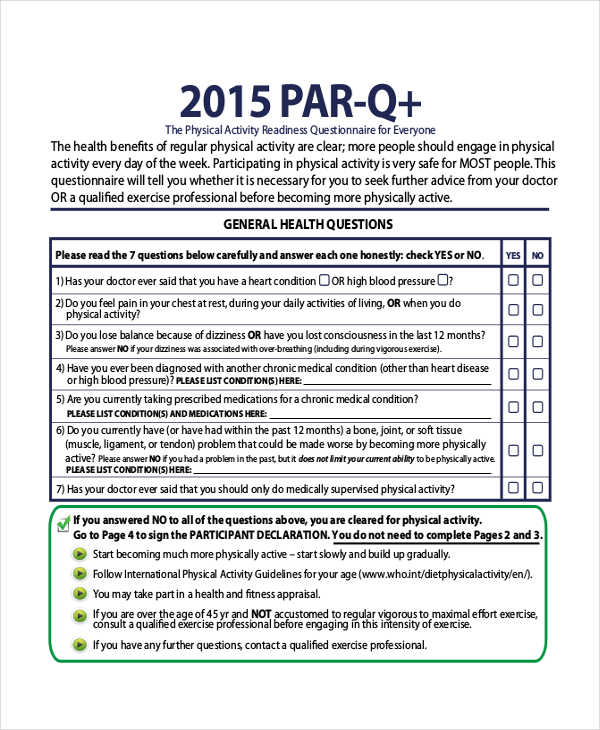 Concerta's drug, which has a mechanism of slow release of the active substance, provides a uniform concentration methylphenidate in plasma for 12 hours. This allows you to control ADHD symptoms both during school and at home. Taking the drug long action avoids sharp fluctuations in concentration methylphenidate in plasma and, accordingly, fluctuations in ADHD symptoms over day. In addition, the slow release of the substance provides better drug tolerance, compliance and reduced child stigma at school.
Concerta's drug, which has a mechanism of slow release of the active substance, provides a uniform concentration methylphenidate in plasma for 12 hours. This allows you to control ADHD symptoms both during school and at home. Taking the drug long action avoids sharp fluctuations in concentration methylphenidate in plasma and, accordingly, fluctuations in ADHD symptoms over day. In addition, the slow release of the substance provides better drug tolerance, compliance and reduced child stigma at school.
It should be noted that the practice of prescribing antipsychotics to children with ADHD is currently time is not supported by current protocols for the treatment of this disorder, which due to the lack of evidence base on their effectiveness - on the one hand, and a high risk of side effects on the other. The professor emphasized that the basis for prescribing neuroleptics (exclusively atypical) for ADHD may be be only the presence of oppositional-provocative and aggressive forms of behavior, and not hyperactivity.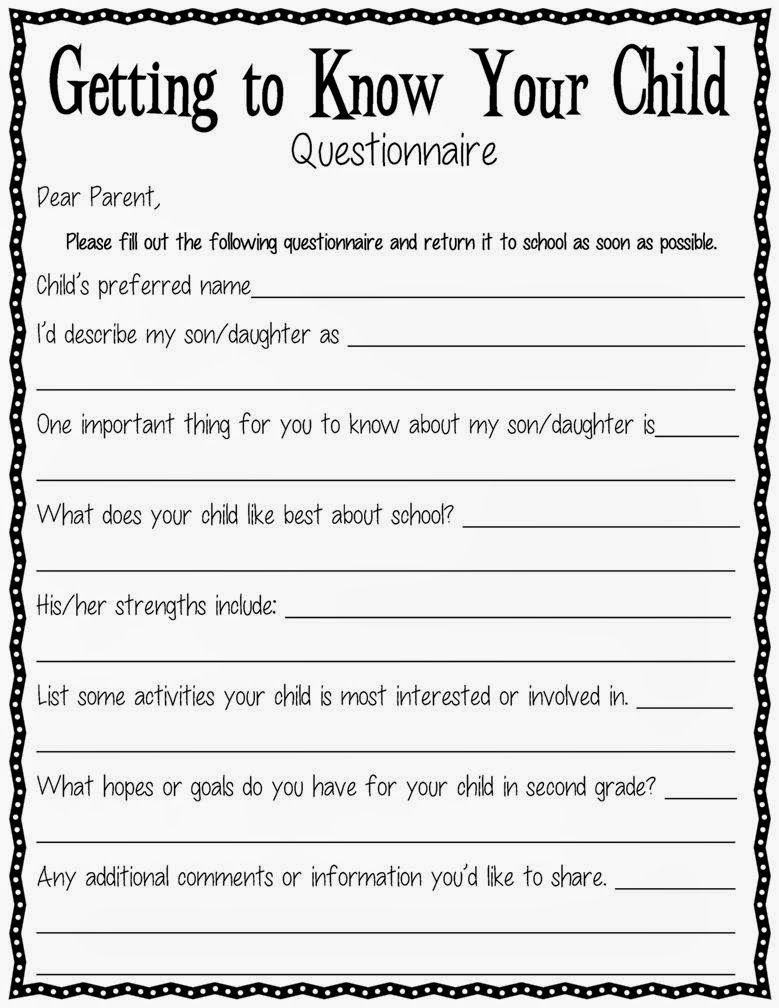 The ADHD treatment protocol, in addition to psychostimulants, allows the use of clonidine, antidepressants and atomoxetine, but states them less effective and more risk of side effects.
The ADHD treatment protocol, in addition to psychostimulants, allows the use of clonidine, antidepressants and atomoxetine, but states them less effective and more risk of side effects.
The professor also noted that in the group of patients with ADHD who were treated psychostimulants, fewer problems associated with addictions (smoking, alcoholism, non-medical use of psychoactive substances), compared with patients with ADHD who were not treated with psychostimulants. The mechanisms of this protective effects of psychostimulants are to reduce the symptoms of ADHD, especially in impulsivity, as well as in the reduction of aggressive disorders and late personality disorders, in the possibility of academic success and career achievement or in improving social and family relationships.
Dr. Dennis Ugrin (King's College London Institute of Psychiatry) conducted practical classes on the diagnosis of ADHD. Students gained experience with structured interview, parent and teacher questionnaire Conners.
October 13, a press conference was held in UNIAN "Hyperactive children: a test for maturity of Ukrainian society”. Questions were raised about the special needs of children with attention deficit hyperactivity disorder, improving their school and family adaptation.
As the WHO national program coordinator noted in his speech "Mental health" Igor Anatolevich Martsenkovsky , mental health and psychological well-being are fundamental components of life child, allowing him to reveal his life potential, to become socially active citizens. Attention deficit hyperactivity disorder is one of the main problems of child psychiatry in Europe and the world, the success of solving which largely determines the state of mental health of children and adolescents populations. Since the 60s, in the countries of the European Union and the USA, a to date, a harmonious integrated system of medical, psychological and pedagogical assistance to children with ADHD. This system is built on principles of evidence-based medicine, deep respect for the rights and special needs of such children and is aimed at their full social, including school reintegration.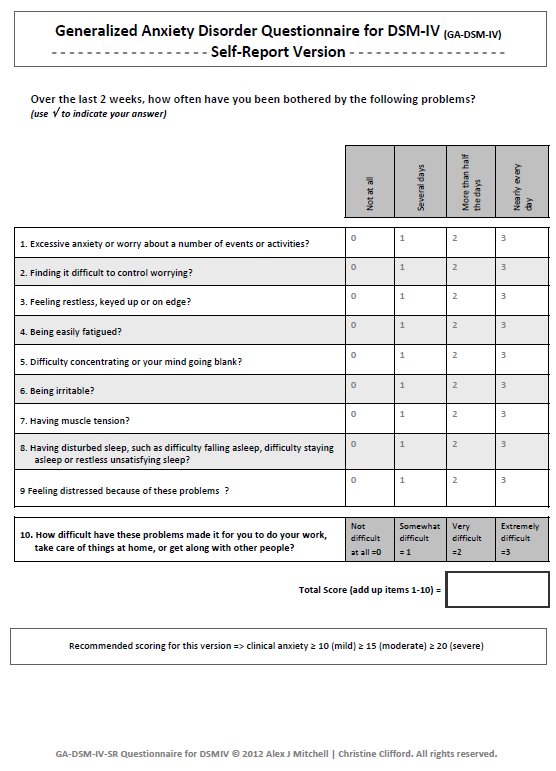
Further, Doctor of Medical Sciences I.A. Martsenkovsky spoke about the difficulties related to the schooling of children with ADHD and the organization of medical care them.
– Until recently, the existence of a problem was not recognized in Ukraine, special the needs of such children, primarily related to schooling, were ignored. Official statistics of the Ministry of Health of Ukraine causes confusion. It seems that Ukrainian children, in contrast to their peers in Europe, attention deficit disorder and hyperactivity almost never occurs. Ukrainian schools demonstrate inability to create the necessary conditions for the education of such children. many schoolchildren suffering from ADHD are transferred to an individual form of education. Difficult recognize the normal situation in which outside the walls of a mass school are children with intact intelligence.
The organization of medical care for children with ADHD in Ukraine looks enough archaic, the established therapeutic practice does not correspond to modern scientific achievements. In our country, there is no specialization of doctors in the field child psychotherapy, there are no specialists trained in the field of cognitive behavioral therapy. Only recently, after Department of Child Psychiatry, National Academy of Postgraduate Education. P.L. Shupyk was headed by Professor Vyacheslav Danilovich Mishiev, the situation with the training of the necessary specialists was recognized as relevant and began change for the better. Another problem: there are no programs in Ukraine psychological correction of behavioral disorders at the place of residence or study children with behavioral disorders. Such programs are very effective in correction of behavioral disorders associated with ADHD.
In our country, there is no specialization of doctors in the field child psychotherapy, there are no specialists trained in the field of cognitive behavioral therapy. Only recently, after Department of Child Psychiatry, National Academy of Postgraduate Education. P.L. Shupyk was headed by Professor Vyacheslav Danilovich Mishiev, the situation with the training of the necessary specialists was recognized as relevant and began change for the better. Another problem: there are no programs in Ukraine psychological correction of behavioral disorders at the place of residence or study children with behavioral disorders. Such programs are very effective in correction of behavioral disorders associated with ADHD.
Many children have been on high doses of antipsychotics and antiepileptics for years. drugs. The efficacy and safety of such treatment raises fair doubts in most countries of the world. S. Goldstein and Anna Teeter Ellison in their fundamental monograph on attention deficit disorder and hyperactivity, back in 1988 it was stated that the risk associated with use of antipsychotics for the treatment of ADHD in children is far superior likely benefit.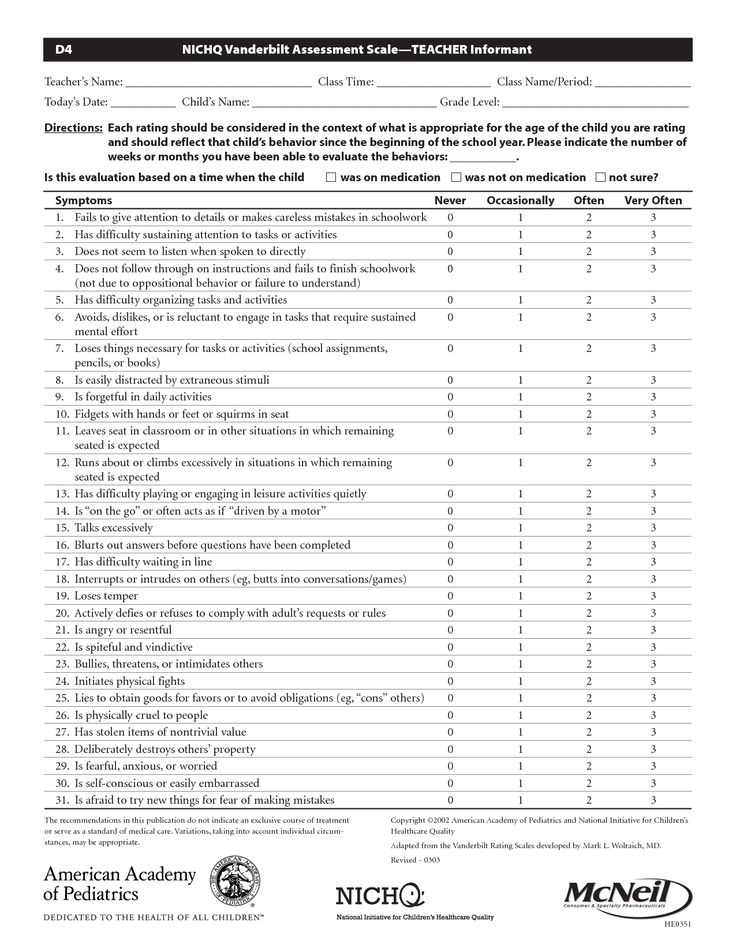 Another therapeutic tactic common in Ukraine is associated with the theoretical ideas of some Russian colleagues and involves the appointment of children with ADHD a variety of neurometabolic drugs. The rationale for their appointment is the alleged presence of a certain residual organics, which is the goal of such therapy. results Numerous controlled studies conducted in European countries Union and the United States allow to argue that such therapy is contrary to the principles evidence-based medicine (especially dangerous is the use of neurometabolic drugs in young children). There is a point of view that it can increase probability of expression of certain gene mutations and act as a factor predispositions of disorders from the autism spectrum. At the same time, the Ukrainian specialists lack experience in the use of drugs that are the first line of therapy for ADHD in most countries of the world (except for some former republics USSR). First of all, we are talking about methylphenidate.
Another therapeutic tactic common in Ukraine is associated with the theoretical ideas of some Russian colleagues and involves the appointment of children with ADHD a variety of neurometabolic drugs. The rationale for their appointment is the alleged presence of a certain residual organics, which is the goal of such therapy. results Numerous controlled studies conducted in European countries Union and the United States allow to argue that such therapy is contrary to the principles evidence-based medicine (especially dangerous is the use of neurometabolic drugs in young children). There is a point of view that it can increase probability of expression of certain gene mutations and act as a factor predispositions of disorders from the autism spectrum. At the same time, the Ukrainian specialists lack experience in the use of drugs that are the first line of therapy for ADHD in most countries of the world (except for some former republics USSR). First of all, we are talking about methylphenidate.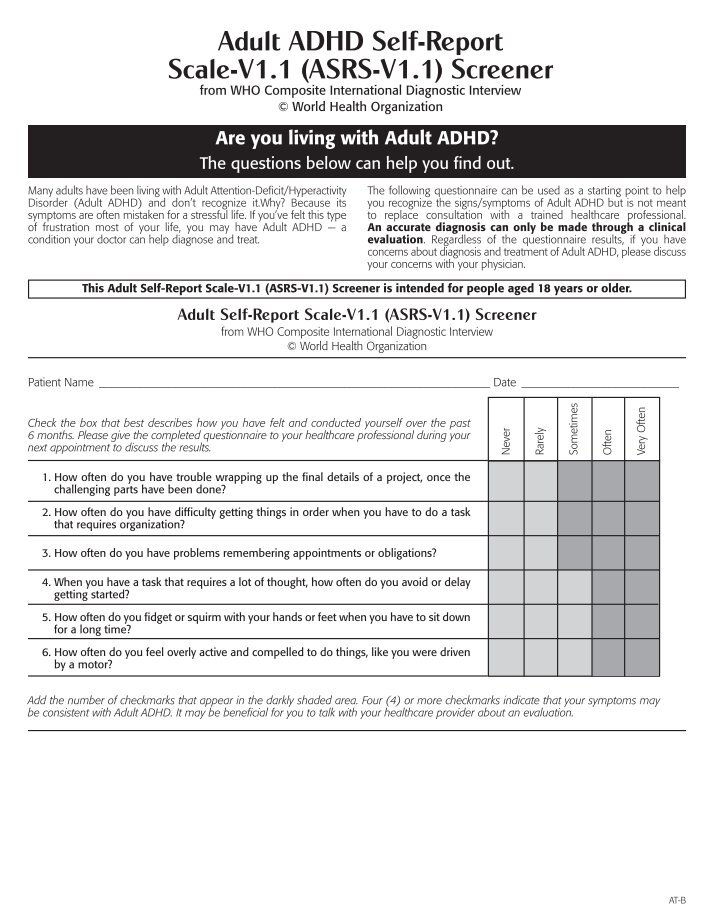 It's no better with the use of other drugs that have proven clinical efficacy. AT as the first line of drug therapy, psychostimulants appear in NICE recommendations (Great Britain), European recommendations, recommendations SIGN (Scotland), AAP guidelines (American Academy of Pediatrics), AACAP (American Academy of Child and Adolescent Psychiatry) guidelines. How to explain these facts? Ukrainian children, unlike European peers suffer from other mental disorders? Their ADHD proceeds differently and requires another treatment? Of course not! There are no children even with severe forms of ADHD in Ukraine. treat or treat ignoring the principles of evidence-based medicine.
It's no better with the use of other drugs that have proven clinical efficacy. AT as the first line of drug therapy, psychostimulants appear in NICE recommendations (Great Britain), European recommendations, recommendations SIGN (Scotland), AAP guidelines (American Academy of Pediatrics), AACAP (American Academy of Child and Adolescent Psychiatry) guidelines. How to explain these facts? Ukrainian children, unlike European peers suffer from other mental disorders? Their ADHD proceeds differently and requires another treatment? Of course not! There are no children even with severe forms of ADHD in Ukraine. treat or treat ignoring the principles of evidence-based medicine.
Such treatment causes a significantly more severe course of ADHD in Ukrainians. children and creates serious difficulties for both children with these disorders and and for their environment. To change the situation, it is necessary to carry out comprehensive reforms. The Ministry of Health cannot solve the problem on its own mental health care for children with ADHD. Impossible to effectively help children with ADHD without taking into account their special educational needs. These children are not should be transferred to individual forms of education, but should be integrated into school teams. During the reforms the Ministry of Education of Ukraine must go his part of the way. In many cases, qualified school interventions are sufficient, and resorting to drug treatment is not account for. We need to solve the problem of psychological and psychotherapeutic assistance to parents and children with ADHD. Without school psychologists this problem is difficult to solve.
Impossible to effectively help children with ADHD without taking into account their special educational needs. These children are not should be transferred to individual forms of education, but should be integrated into school teams. During the reforms the Ministry of Education of Ukraine must go his part of the way. In many cases, qualified school interventions are sufficient, and resorting to drug treatment is not account for. We need to solve the problem of psychological and psychotherapeutic assistance to parents and children with ADHD. Without school psychologists this problem is difficult to solve.
But the main goal of reforming the system of care for children with deficiency disorder attention and hyperactivity should be a change in attitude towards these children with from educators, peers and parents. We need social advertising aimed at protecting the mental health of children. We need to connect to education of parents of children in the field of mental health of family doctors, pediatricians, pediatric neurologists.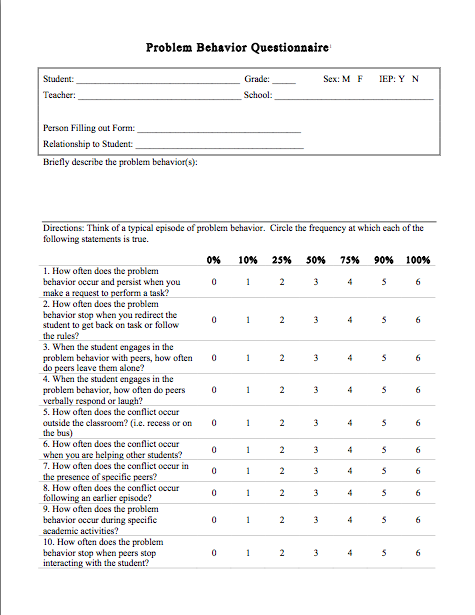 Ukraine needs to organize a system for providing psychiatric care in primary care, at the place of residence and study of the child. This should be primarily primary and secondary prevention, screening with purpose of early diagnosis. I believe that Ukrainian society has the strength to change health care system for children with ADHD.
Ukraine needs to organize a system for providing psychiatric care in primary care, at the place of residence and study of the child. This should be primarily primary and secondary prevention, screening with purpose of early diagnosis. I believe that Ukrainian society has the strength to change health care system for children with ADHD.
Director for International Cooperation of the Association of Psychiatrists of Ukraine Tina Beradze emphasized that the problem of children with ADHD is not only medical, but also social character - most of them retain some of the symptoms and during adulthood. In general, patients with ADHD have a lower ability to social adaptation, lower level of education and greater the frequency of development of states of dependence on psychotropic drugs compared with the general population. Therefore, early diagnosis and timely treatment of ADHD are relevant to our society, which is facing severe social consequences of insufficient attention to this problem.
Professor Emily Simonov reported that in 2004 the World Association of Children and of Adolescent Psychiatry and Allied Professions recognized ADHD as the #1 problem in the field children's healthcare. According to the results of international studies, initiated by WHO, the prevalence of ADHD in different countries is 3-20%.
The problem of ADHD requires a wider discussion around the world, especially in those countries where, until recently, it has received little attention. The primary task of specialists in the field of child and adolescent psychiatry in any state is to initiate a discussion of ADHD problems on appropriate level and intensify efforts to identify children with disorders.
Professor Eric Taylor noted that in recent years a large the number of studies on the problem of ADHD, the results of which significantly replenished the knowledge base in the field of etiology, pathogenesis and clinical manifestations of this disease. Scientific data have been obtained to form accurate understanding of the nature of hyperactivity in children and understand the essence of the problem.
One of the tasks of the medical community is the constant work with school teachers and parents, on whom the creation of optimal conditions for children with ADHD, the success of their treatment and adaptation in society. The intervention of educators and parent education are sufficient effective forms of assistance. The professor emphasized the importance of cooperation medical experts and parents whose children have hyperactive disorders, in creating a system for assessing such children and recommendations for their treatment.
Some children with Attention Deficit Hyperactivity Disorder, however, need medical treatment. Psychostimulant therapy is the safest and most effective form of such treatment.
Experience with European approaches to helping children with ADHD told the head of the training and rehabilitation center "Dzherelo" Oleg Romanchuk (Lviv) .
It was interesting to learn that over the past three years, specialists The Center is implementing a program for the early detection of children with ADHD and providing them with needed help. A lot of educational work is being done with teachers elementary grades in schools and educators of preschool institutions. Support is provided for families with children with ADHD.
A lot of educational work is being done with teachers elementary grades in schools and educators of preschool institutions. Support is provided for families with children with ADHD.
The results of the ongoing work show the enormous potential of such children, which can be realized only if timely detection disorder, its treatment and creation of comfortable conditions for the development abilities of children with ADHD, the speaker noted.
The ways of solving the problems associated with ADHD in Ukraine were reported in her speech Head of the Department of Maternal and Childhood Protection of the Ministry of Health of Ukraine Raisa Alexandrovna Moiseenko .
She stressed that the priority task is to develop the Ministry of Health of Ukraine together with the Ministry of Education and Science and the Ministry of Labor and Social policy protocol for the treatment of children with ADHD. The second step towards a solution this problem should be the creation of centers for training specialists - teachers, medical and social workers, which will contribute to formation of an intersectoral approach in helping children with ADHD.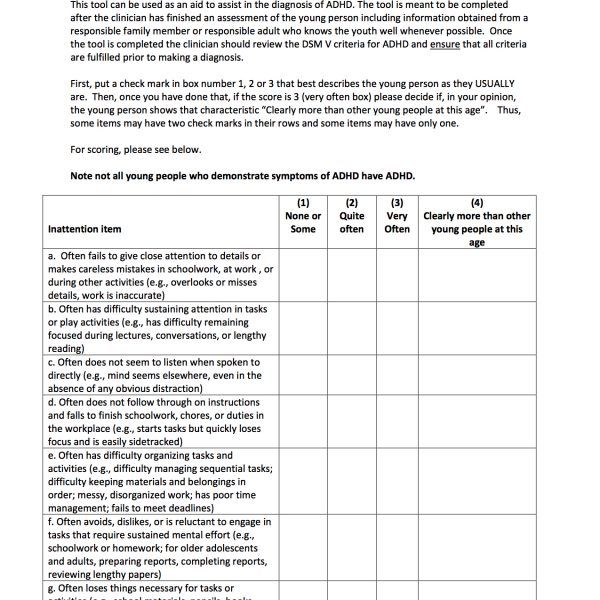 AT At present, the Ministry of Health has prepared methodological recommendations on program-targeted services for such children, providing for creation of a system of coordinated medical, psychological, pedagogical, corrective and social measures aimed at improving the quality help for hyperactive children.
AT At present, the Ministry of Health has prepared methodological recommendations on program-targeted services for such children, providing for creation of a system of coordinated medical, psychological, pedagogical, corrective and social measures aimed at improving the quality help for hyperactive children.
Head of the Department of Child, Social and Forensic Psychiatry, National medical academy of postgraduate education. P.L. Shupika, doctor of Medical Sciences, Professor Vyacheslav Danilovich Mishiev drew attention to significant differences in treatment approaches used in pediatric and adult psychiatry. Child psychiatry is the field of behavioral disorders, problems, associated with hyperactivity, emotional-volitional incontinence. At present time, domestic specialists in the field of child and adolescent psychiatry with the support of foreign specialists carry out the development of programs for more in-depth study of the problem of ADHD, early detection of this disorder and training of relevant specialists.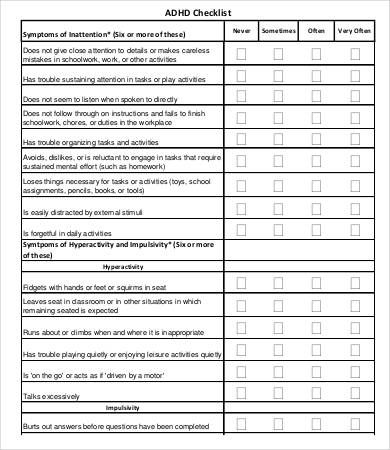
The participants of the press conference expressed their hope that the joint work representatives of state structures of health care, science, practical doctors and teachers with the support of the state will contribute to a significant improving the level of medical and social care provided to children with ADHD in Ukraine.
Prepared by Natalia Ocheretyanaya
- Number:
- No. 23/1 December - Neurology. Psychiatry. Psychotherapy
09.12.2022 Therapy and family medicine ELOM‑080 (Respero Myrtol / Respero Myrtol forte): what are the benefits of protecting herbal medicine against rhinosinusitis?
10th Spring near the metro station Hamburg (Nimechchina) an international symposium "Reduction of mucociliary clearance: lessons from infections of the upper respiratory pathways to COVID-19", organized by the German pharmaceutical company Bosch GmbH & Cohlsk Gamp. kg. Її dosvid of the development of innovative solutions for the investigation of the pathology of the dichal system for 50 years. In just one hour, a lot of two medicinal products have been created and put into practice, among them ELOM-080 - standardizations of myrtol, which are presented by the Berlin-Chemie Menarini company under the trade name Gelomyrtol in Europe Respero Myrtol / Respero Myrtol forte in Ukraine. One of the spheres of ELOM-080 treatment, and the treatment of rhinosinusitis itself, was actively observed in the framework of the call as from the position of clinicians, so from the point of view of scientific research ....
kg. Її dosvid of the development of innovative solutions for the investigation of the pathology of the dichal system for 50 years. In just one hour, a lot of two medicinal products have been created and put into practice, among them ELOM-080 - standardizations of myrtol, which are presented by the Berlin-Chemie Menarini company under the trade name Gelomyrtol in Europe Respero Myrtol / Respero Myrtol forte in Ukraine. One of the spheres of ELOM-080 treatment, and the treatment of rhinosinusitis itself, was actively observed in the framework of the call as from the position of clinicians, so from the point of view of scientific research ....
09.12.2022 Amtolmetin guacil is a non-steroidal antiseptic drug with gastroprotective power The gastrotoxicity of NSAIDs does not lessen the predilection of patients to cure, and may cause fatal ductal bleeding [1]. Amtolmetin guacyl (AMG) is a non-acidic ester precursor of tolmetin, which acts as an anti-inflammatory, pain-reducing and antipyretic agent as a member of the NSAID class, but also as a representative of non-selective molecules of this group of gastroprotective powers. Mechanisms and clinical effects of AMG reviewed in this way....
Amtolmetin guacyl (AMG) is a non-acidic ester precursor of tolmetin, which acts as an anti-inflammatory, pain-reducing and antipyretic agent as a member of the NSAID class, but also as a representative of non-selective molecules of this group of gastroprotective powers. Mechanisms and clinical effects of AMG reviewed in this way....
09.12.2022 Therapy and family medicine Current nutraceutical complexes in ophthalmology
A significant role in the pathogenesis of low eye diseases and oxidative stress. Apparently, oxidative stress is blamed on the result of damage to the balance between active forms of sour (peroxides and free radicals) and the antioxidant system of bacteria. Disruption of oxide-oxidative processes leading to the rise of active forms of sour, resulting in the oxidation of proteins, lipids and DNA of the clitin.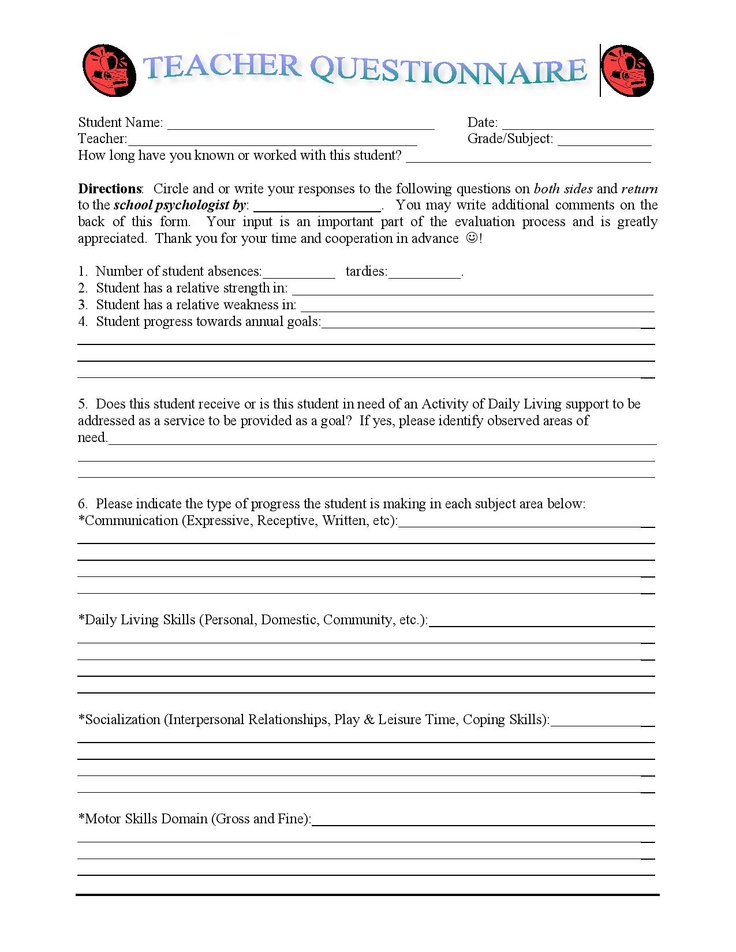 Oxidative stress can lead to the death of cells. The basis of the disruption of the balance between active forms of acidity and the antioxidant system of sourness of cells is the disruption of the antioxidant system of sourness due to the deficiency of storable ....
Oxidative stress can lead to the death of cells. The basis of the disruption of the balance between active forms of acidity and the antioxidant system of sourness of cells is the disruption of the antioxidant system of sourness due to the deficiency of storable ....
Higher education BSPU
Lecture on the training course "Pedagogical support for children with ADHD", topic 1 "Concept, clinical principles and manifestations of ADHD"
Concept, clinical signs and manifestations of ADHD
Questions:
1. The concept and signs of the disease
A hyperactive child is always on the move, does not complete a single task, does not respond to comments. He "starts" the class and got everyone already: teachers, parents, and children! However, the main symptom of the disease is distracted attention: the child cannot concentrate on anything, whether it is a game, study or watching a TV show.
He "starts" the class and got everyone already: teachers, parents, and children! However, the main symptom of the disease is distracted attention: the child cannot concentrate on anything, whether it is a game, study or watching a TV show.
Has everyone seen such children and used an unkind word to commemorate their parents who raised them poorly? In fact, these children are sick.
PORTRAIT OF FIDGET PHIL
For the first time a child with a similar pathology was described by the German neuropsychiatrist Heinrich Hoffmann and gave him the nickname Fidget Phil ; since then, doctors have called children with this syndrome.
At the age of 7, Phil, as a rule, is not yet ready for school, his higher brain functions have not fully matured. He is often distracted in class and makes many mistakes. It can be difficult for him to master reading, writing and counting, but not because of a weak intellect, but because of a violation of perception.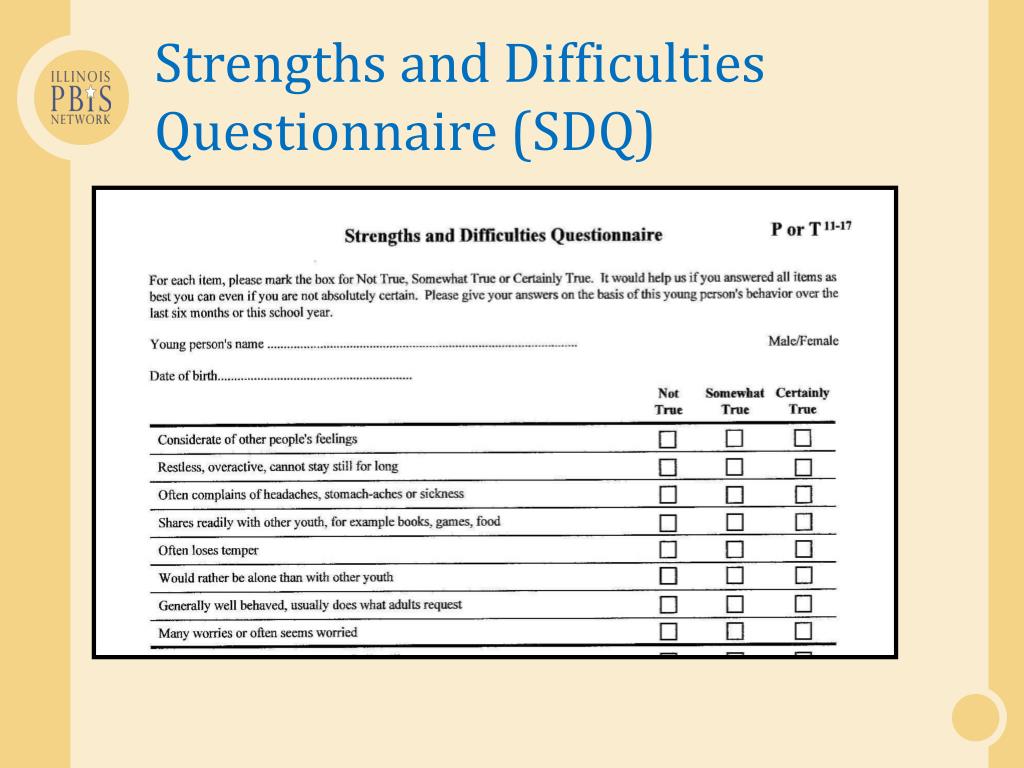 He can work productively for no more than 5-15 minutes - then his brain "turns off" for 3-7 minutes, accumulating energy for the next work cycle. At this time, Phil is engaged in extraneous matters and does not react to the words of the teacher.
He can work productively for no more than 5-15 minutes - then his brain "turns off" for 3-7 minutes, accumulating energy for the next work cycle. At this time, Phil is engaged in extraneous matters and does not react to the words of the teacher.
Phil is always in a hurry, fussing, aimlessly grabbing objects, opening drawers... He is long-winded, jumping from one to another in conversation. May suffer from tics, grimace, make obsessive movements. He often bumps into corners, cannot stand on one leg, and sometimes suffers from fine and gross motor impairments. In 68% of such livestock, sleep disturbances are noted, in 40% - bedwetting.
Phil is impulsive, excitable and aggressive. He is internally tense all the time, his mood instantly changes, often there is a feeling of fear, anxiety and anxiety. Phil finds it difficult to get along with his peers. He lags behind them in mental development, but seeks to command and lead, so he has few friends. Relationships with adults are also difficult: punishments do not work on him, and praises do not stimulate him. The reward must be very strong in order for Phil to behave better.
The reward must be very strong in order for Phil to behave better.
Previously, this pathology was called as soon as: "mild brain dysfunction", "hyperkinetic syndrome", "motor disinhibition"... In recent years, doctors have settled on the name "attention deficit hyperactivity disorder".
ADHD is one of the manifestations of minimal brain dysfunction (MMD), that is, very mild brain insufficiency, which manifests itself in a deficit of certain structures and impaired maturation of higher levels of brain activity. MMD is classified as a functional disorder that is reversible and normalizes as the brain grows and matures. MMD is not a medical diagnosis in the truest sense of the word; rather, it is only a statement of the fact of the presence of mild disorders in the brain, the cause and essence of which have yet to be clarified in order to begin treatment. Children with a reactive type of MMD and are called differently hyperactive .
Attention deficit/hyperactivity disorder - dysfunction of the central nervous system (mainly the reticular formation of the brain), manifested by difficulties in concentrating and maintaining attention, learning and memory disorders, as well as difficulties in processing exogenous and endogenous information and stimuli.
Prevalence.
According to statistics, about 5-10% of school-age children suffer from Attention Deficit Hyperactivity Disorder. Approximately 20%-60% of the syndrome persists into adulthood. By adolescence, motor hyperactivity usually subsides, but learning disabilities, lack of attention, and inability to concentrate persist in most children.
Now this diagnosis is heard more and more often. Statistics (Zavadenko N.N.) shows that in Russia there are 4 - 18% of such children, in the USA - 4 - 20%, in the UK - 1 - 3%, in Italy - 3 - 10%, in China - 1 - 13 %, in Australia - 7 - 10%.
On average, there are at least 1-2 children in each class who need treatment for this condition. Most often, it manifests itself at the age of 6-12, when the "zhivchik" goes to school and it turns out that he himself cannot study, and interferes with others.
Most often, it manifests itself at the age of 6-12, when the "zhivchik" goes to school and it turns out that he himself cannot study, and interferes with others.
And then the problem turns from a medical one into a social one: not achieving success in studies, receiving criticism for their behavior, such children behave worse and worse. World statistics confirms that among juvenile delinquents there are many patients with attention deficit hyperactivity disorder.
Gender differences
All researchers emphasize the higher prevalence of the disease among boys compared to girls.
According to the authors and literature, among boys aged 7-12 years, signs of the syndrome are diagnosed 2-3 times more often than among girls. Among adolescents, this ratio is 1:1, and among 20-25-year-olds it is 1:2, with a predominance of girls. In the clinic, the ratio of boys and girls varies from 6:1 to 9:1.
The predominance of boys is not only a consequence of the subjective opinion of the respondents answering the questionnaire. Although teachers most often see violators of the order in boys. The high frequency of symptoms of the disease in boys may be due to the influence of hereditary factors, as well as the higher vulnerability of the male fetus to pathogenetic effects during pregnancy and childbirth. In girls, the large hemispheres of the brain are less specialized, so they have a greater reserve of compensatory functions compared to boys with damage to the central nervous system.
Although teachers most often see violators of the order in boys. The high frequency of symptoms of the disease in boys may be due to the influence of hereditary factors, as well as the higher vulnerability of the male fetus to pathogenetic effects during pregnancy and childbirth. In girls, the large hemispheres of the brain are less specialized, so they have a greater reserve of compensatory functions compared to boys with damage to the central nervous system.
In addition, there are gender differences in the structure and dynamics of behavioral disorders. In boys, symptoms of hyperactivity and other behavioral disorders appear from the age of 3-4, which forces parents to consult a doctor even before the child enters school.
Among girls, hyperactivity is less common, the disease in them often manifests itself in the form of attention disorders. In girls, behavioral deviations manifest themselves more latently and therefore are not detected during one or two follow-ups, therefore they are not treated and have a more unfavorable prognosis. To a much greater extent, compared with boys, they have social maladaptation, learning difficulties, and personality disorders.
To a much greater extent, compared with boys, they have social maladaptation, learning difficulties, and personality disorders.
Status and race
There is no clear evidence that either socioeconomic status (SES) or race affects the prevalence of ADHD. Although some studies indicate a higher percentage of ADHD among children with low SES and African American children, these data may be due to the increase in this set of conditions of aggression and behavior problems, and not ADHD itself (see Barkley, 1996).
2. Clinical manifestations and types of ADHD
Psychological portrait of a hyperactive child
You cannot hold such a child in your arms, he is like a spinning top. To say of him that he is restless is to say nothing. It's like mercury. They did not keep track - and he is somewhere upstairs, from where he can be removed only with the help of a fire escape. Penetrating into all the cracks, falling into all the pits, climbing all the nooks and crannies, exploring all the attics and basements, touching everything and overturning everything, filling himself with bruises and bumps, he rushes day and day around the apartment, around the yard, and without proper supervision and through the streets.
It is , the hypermobile , who most often escapes from the kindergarten, but not intentionally, but because he discovers an accidentally open gate or gap in the fence. It is he who most often finds himself on the carriageway of the street, arranges a short circuit in the electrical network or overturns a pot of boiling water on himself. If at least one sewer manhole is not covered by negligence in the city, the super-mobile one will climb in there without thinking how he will get out of it. It is he who finds and blows up the cartridges and grenades left over from the war. Naturally, the lion's share of accidents happens to him.
His hands are in constant motion: they are wrinkling, tearing, turning buttons, peeling the paint on the wall. He can't sit still. He even stands, shifting from foot to foot, and it seems that in another moment - and he will take off, rush to the ends of the world. He eats either standing, or literally bouncing on a chair. He will dodge all over, even playing, listening to a fairy tale, looking at the TV screen. Sometimes it seems that he never learned to sit, and it is hard to believe that he did not run for over a year.
Sometimes it seems that he never learned to sit, and it is hard to believe that he did not run for over a year.
Some of the overactive are especially unbearable in the morning, others in the evening, and then they cannot be put to sleep. They play tricks in bed, fall asleep, standing on their knees and elbows, and when they fall asleep, they knock the sheet into a ball, because they are restless even in a dream. Those who are restless in the morning fall asleep instantly and sleep like the dead. But both about the first and the second they say: "It's good when he sleeps." And parents take a breath, feel calm, only after laying down such a child and making sure that he finally calmed down.
Clothes and shoes literally "burn" on the super mobile. He constantly loses his hat, scarf, mittens, and then his school bag, and you can’t get enough of it.
The Overactive is impulsive, and no one dares to predict what he will do in the next moment. And he doesn't know it either. He has everything on a short circuit: he saw - he grabbed - he ran. He acts without thinking about the consequences, although he does not plan bad things and he himself is sincerely upset by the incident, the fault of which he becomes. However, more often he believes that he did nothing wrong, because he did not want it. And if an overactive child broke a vase, then, in his opinion, it fell by itself, because it did not stand well.
He has everything on a short circuit: he saw - he grabbed - he ran. He acts without thinking about the consequences, although he does not plan bad things and he himself is sincerely upset by the incident, the fault of which he becomes. However, more often he believes that he did nothing wrong, because he did not want it. And if an overactive child broke a vase, then, in his opinion, it fell by itself, because it did not stand well.
He takes punishment easily, because traditional slaps, reproaches, refusals of requests do not upset him. An overactive person does not remember resentment, does not hold a grudge, and, although he quarrels every minute, he immediately reconciles. True, sometimes he is excessively quick-tempered, aggressive, pugnacious, and not harmless and good-natured, but evil and even cruel, but in such cases we are talking about a more severe brain lesion and certainly with increased convulsive readiness of it, which is found during electroencephalographic examination.
Due to an excess of feelings, the overactive person is not able to speak calmly, but shouts, proving, making excuses, arguing. This is the noisiest child of all. Naturally, he chooses only noisy and active games, in which everything reduces to running around. He's always in the middle of a boyish dump. Not a single "heap is small" can do without it. Extracted from its very thick, rumpled, but happy - this is it, super-mobile. Sweat doesn't dry out. From constant overexcitation, his hair stands on end, his eyes shine and just do not pop out of their sockets. He has many friends, because he is sociable, ready recklessly for any leprosy, does not whine when hurt, and never lose heart.
The biggest trouble of the super mobile is distractibility. His head is like a weather vane in the wind: now turning in one direction, where something briefly attracted attention, then in the other. Having become interested in something, he forgets about the previous one, does not bring a single thing to the end.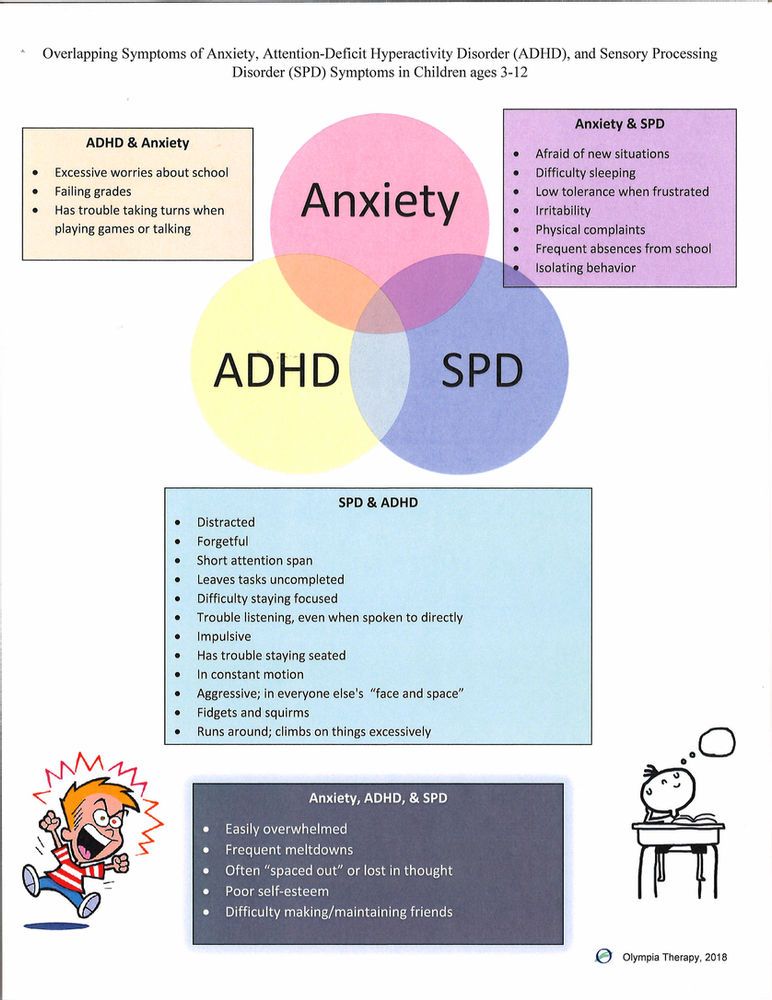 New impressions lead him from one passion to another. If he ended up at the opposite end of the city, then not knowing how, not remembering the way, for he went first to an unusual car near the parapet, then to a bright shop window, then to the crowd that had gathered on the occasion and as a result found himself in a police station picket, from where every minute sounds of radio: "Attention, who lost the boy?".
New impressions lead him from one passion to another. If he ended up at the opposite end of the city, then not knowing how, not remembering the way, for he went first to an unusual car near the parapet, then to a bright shop window, then to the crowd that had gathered on the occasion and as a result found himself in a police station picket, from where every minute sounds of radio: "Attention, who lost the boy?".
Everything attracts his attention, but it does not linger on anything, it slides from one to another: here he is watching a television program, immediately shifts his gaze to a fly on the ceiling, so that after another second he is distracted by a conversation between his mother and grandmother. He can't concentrate in class at school. He looks at the blackboard in fits and starts, and the teacher does not attract his attention. He does not hear her explanations, never knows what is given at home. When writing, the overactive skips letters, does not complete words and sentences. In the simplest examples, he makes ridiculous mistakes, but not because of a lack of ability, but due to damage to the areas of the brain that are in charge of writing ( dysgraphia ).
In the simplest examples, he makes ridiculous mistakes, but not because of a lack of ability, but due to damage to the areas of the brain that are in charge of writing ( dysgraphia ).
The Overactive is curious, but not inquisitive. He looks at everything, but as a result he sees nothing. If you do not engage in his upbringing, he will remain so: not stupid, but not really smart either. Superficial will be his knowledge, reasoning, conclusions, because in his thoughts he runs, not stopping at anything. Chaos in the head of a hypermobile is akin to chaos in his pockets, where there are a lot of random and scattered things.
Without educative influence, he will confine himself to questions: "Who is this?" and "what is it?", "where?", "where?" and where?" "Why?" will sound, but the hypermobile will be satisfied with the simplest answers, but "what will happen?" may not arise, because it does not interest him. As a result, his orientation will be reduced to superficial ideas about objects and people, to a simplified and concretely grounded knowledge of life, limited to the near space and narrowed environment of communication with those who are like himself. He is not interested in tomorrow and even what will happen tonight.
He is not interested in tomorrow and even what will happen tonight.
Peak manifestations of hyperdynamic syndrome or hypermobility syndrome - 6-7 years with reverse development in favorable cases by 14-15 years. However, obvious already in the first year of life, with improper upbringing, it crushingly manifests itself just from the age of 13 and older, in this case determining the fate of an adult.
In no other case does a child's difficulty, expressed in such blatant disinhibition and distractibility, cause so many censures and complaints from parents, kindergarten teachers and teachers, as in this one. The super mobile is most threatened by rejection. He is able to bring out of patience the most calm and familiar adults. No one is reproached, shamed, reprimanded, punished as much as someone who is super mobile. In the end, he himself is convinced that there is no more difficult and stupid child in the whole wide world. As a result, most of the super-mobile protesters become embittered.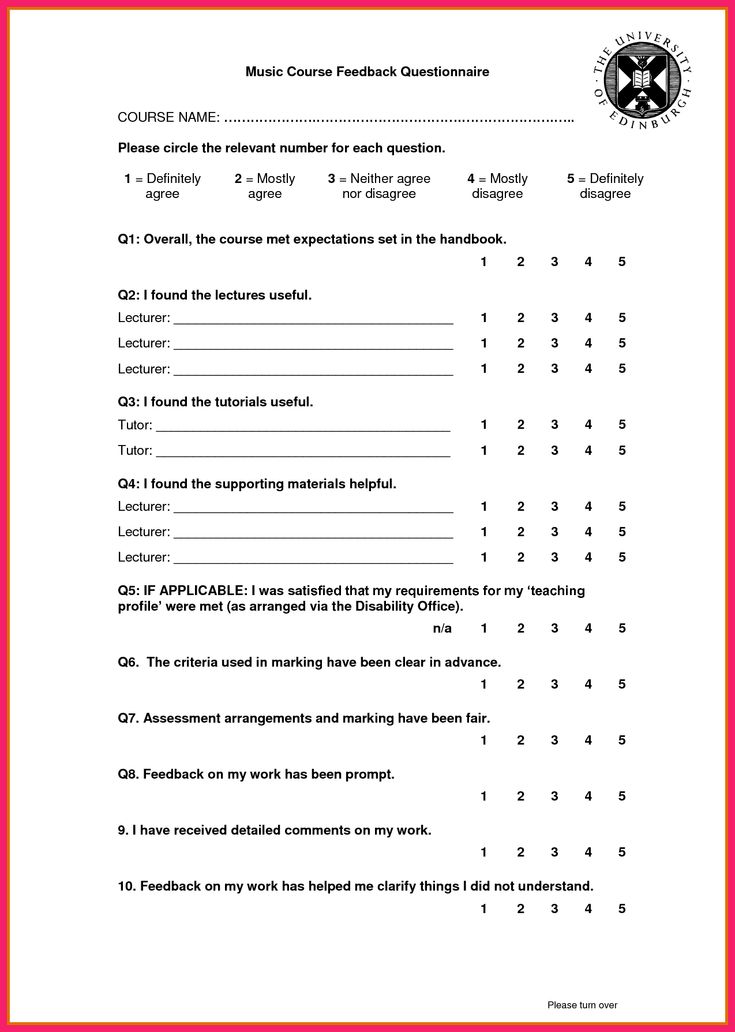 After all, they have, albeit slightly, but the nervous system is damaged: it is highly excitable. And such children tend to react aggressively to incessant pulling and suppression of their activity.
After all, they have, albeit slightly, but the nervous system is damaged: it is highly excitable. And such children tend to react aggressively to incessant pulling and suppression of their activity.
If the restraint and suppression is constant and the child is finally convinced that he is "the worst", the hyperactive becomes the leader of the protest difficult teenagers, demonstratively deviating in behavior, ignoring school studies or may become unstable, which he carries like a chip in river, from trouble to trouble. The hypermobile then blindly follows any group of teenagers in their idle pastime. In this variant, the superficiality of interests and relationships with other adolescents, which follows from distractibility, comes to the fore. Some of the over-active, if they are nevertheless scorched with censures and punishments, if they are endlessly pursued by failures, fall into a hysterical neurosis.
Also hyperactivity children have poor motor coordination, characterized by awkward erratic movements. They are characterized by constant external chatter, which happens when the internal speech that controls social behavior is unformed.
They are characterized by constant external chatter, which happens when the internal speech that controls social behavior is unformed.
Among these children there may be gifted children with extraordinary abilities. Hyperactive children may have good general intelligence , but developmental disabilities prevent its full development. The uncompensated discrepancy between the level of development and intellect is manifested on the one hand in the somatic sphere, on the other hand in the characteristics of behavior. Since the fixed patterns of such deviant behavior (due to the imperfection of the restraining centers) lead to the fact that these children retain them in adulthood, although they cease to be disinhibited and can already concentrate their attention.
One of the three main components of the syndrome is impulsivity, which is determined by a deficiency of a deterrent. The child shows impulsive motor and verbal activity, he acts as if thoughtlessly, moves from one activity to another, chats without thinking (“speech is ahead of thought”).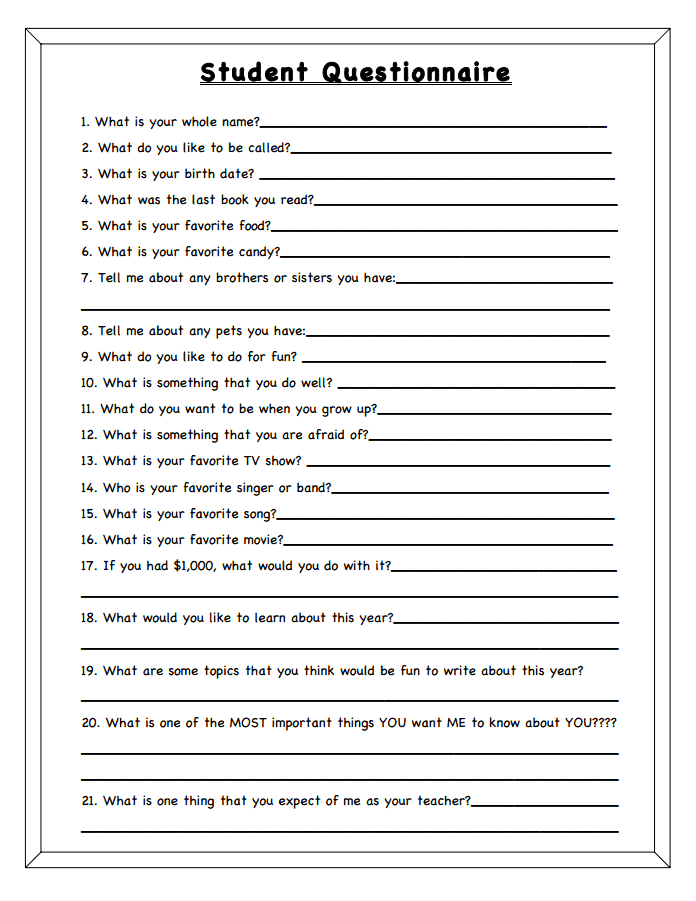 He often does not get along with his peers, in games he becomes a "target".
He often does not get along with his peers, in games he becomes a "target".
Annoying and distracting environmental factors in situations such as being at a party or in a store, at a party, in a crowd, etc., change the child's behavior for the worse. An outburst of anger or a shout is accompanied by trivial insults.
The social-behavioral aspects of these children are important not only because of their widespread negative influence on their peers, but also because these children serve as a kind of social catalyst that influences the behavior of others and often in an undesirable direction.
The child has difficulties in relationships not only with peers, but also with adults. In relation to the first, they are aggressive and demanding. School-age children are very sensitive to the behavior of such classmates and reject their friendship. Parents often complain that their children do not have friends and that their peers refuse to study or play with them.
In sociometric studies, these children often receive negative characteristics from their comrades. They note that these children are "a cause for concern", "annoying other children".
Deviant behavior is manifested in the fact that children are aggressive, explosive, impulsive. Impulsivity remains a pervasive feature. Such children are prone to delinquency, to various forms of grouping, since it is easier to imitate bad behavior than good. And since the will, higher emotions and higher needs have not matured, life develops in such a way that personal problems are already on the way.
Children with ADHD may experience difficulties in relationships, including peer loneliness, mood disorders, anxiety, and even substance abuse. Adolescents with ADHD are more likely to be involved in traffic accidents and are twice as likely to receive notices and fines from traffic inspectors.
Types of ADHD in children.
The following types of ADHD can be classified according to the manifestation of symptoms:
Combined type (inattentive/hyperactive/impulsive).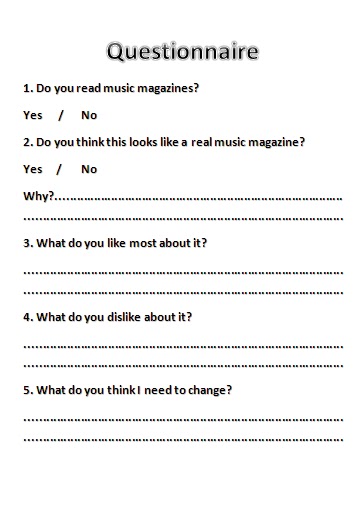 A syndrome that combines attention deficit hyperactivity disorder.
A syndrome that combines attention deficit hyperactivity disorder.
Children with this type of ADHD show all three symptoms. This is the most common form of the syndrome.
It is difficult for them to concentrate on one subject for a long time. In addition, they are impulsive, very mobile - they are "jumping" (hyperactive), which can be very annoying during a lesson in the classroom.
Children with this type of disorder are more visible and easier to diagnose.
Hyperactive/impulsive typ. Attention Deficit Hyperactivity Disorder. In this type of ADHD, children show both hyperactivity and impulsivity, but are able to focus.
They are fussy and talkative, feel restless, cannot sit in one place for a long time (for example, during lunch, doing homework, etc.). These children may be traumatized, that is, because of their activity, they are more likely to be injured than children who do not have ADHD. Young children may be overly active and have problems with their impulsiveness (they may interrupt others when talking, grab objects with their hands, behave inappropriately).
Inattentive type . Attention Deficit Disorder Without Hyperactivity This type of ADHD used to be called Attention Deficit Disorder. Children with this type do not show excessive activity. They do not interfere with school lessons and other activities, so their symptoms may not even be paid attention to.
Children with inattention are not able to maintain attention at the appropriate level for their age. Parents and teachers may complain that children are unable to concentrate, are distracted, jump from one activity to another, disorganized, forgetful, and prone to daydreaming.
This type of disorder is more difficult to identify and diagnose. These are the dreamers. They seem to be listening, but in fact they are thinking about something else, easily distracted. They are calm, not very mobile, and the teacher does not pay attention to them. Parents also do not always understand why a quiet, calm child has problems in school, and consider laziness to be the reason.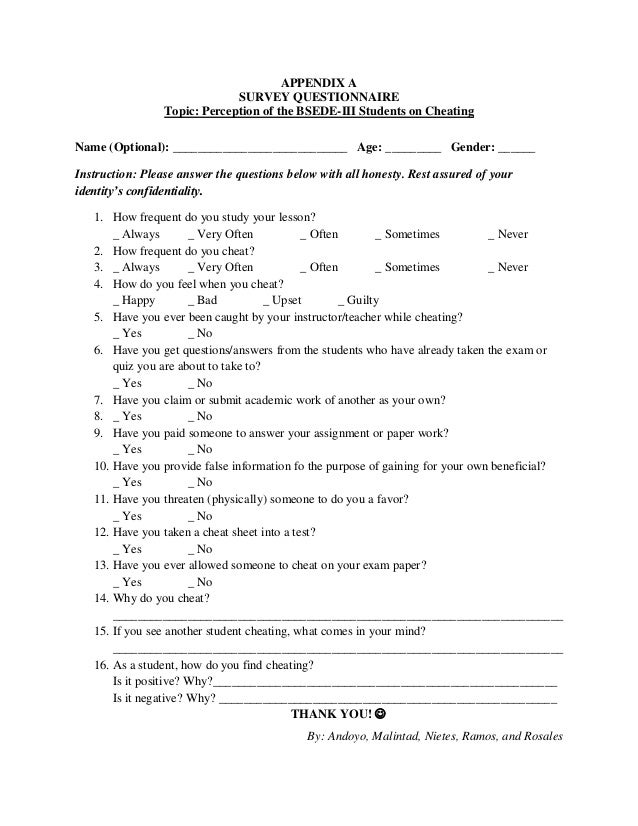
Attention deficit without hyperactivity is more common in girls.
3. A historical outline of the study of ADHD
The syndrome itself appeared suddenly and very recently. Only in 1980, in the third edition of the American Diagnostic and Statistical Handbook (DSM-III), did a mention of ADHD appear, and until that time no one knew anything about it at all.
In general, the evolution of DSM causes fair bewilderment for many. The first edition of this handbook (1952) provided data on 112 mental illnesses and disorders. In subsequent editions, their number has steadily increased, reaching 374 in the modern, fourth edition!
Dr. Carol Travis, author of the best-selling Misdiagnosis, was given the opportunity to make her own sarcastic diagnosis to the manual's authors: "compulsive diagnostic word-creation."
The existence of such a psychological disorder as ADHD was "proven" by a simple vote of experts from the American Psychiatric Association.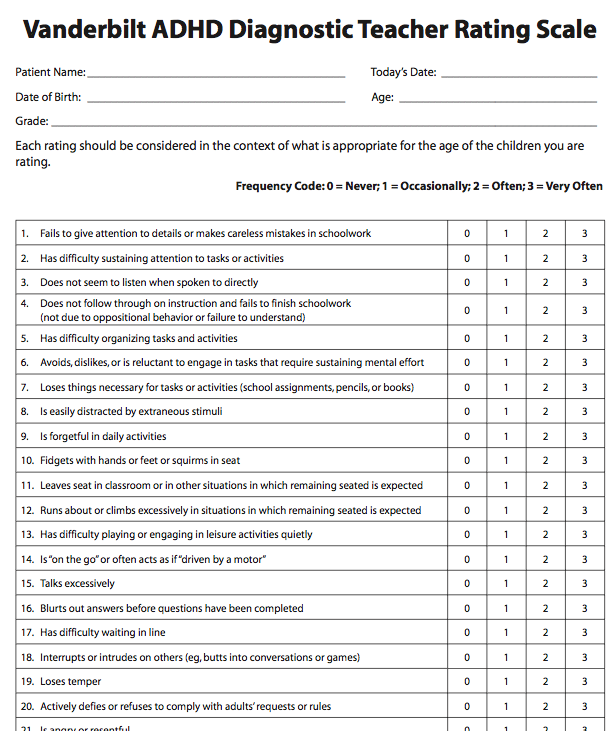 On the other hand, latent homosexuality was excluded from the list of psychological disorders (where it existed quite reasonably and for many years) under the pressure of politically engaged individuals.
On the other hand, latent homosexuality was excluded from the list of psychological disorders (where it existed quite reasonably and for many years) under the pressure of politically engaged individuals.
The term "attention deficit disorder" has been separated from the broader concept of "minimal brain dysfunction".
The history of the study of minimal brain dysfunction is associated with the studies of E. Kahn et al. (1934), although separate studies have been carried out earlier. Observing school-age children with such behavioral disorders as motor disinhibition, distractibility, impulsive behavior, the authors suggested that the cause of these changes is brain damage of unknown etiology, and proposed the term "minimal brain damage". Later, learning disorders (difficulties and specific impairments in learning writing, reading, counting skills; disorders of perception and speech) were included in the concept of "minimal brain damage".
In 1962 the Oxford International Research Group in Child Neurology held a symposium on the problem of minimal brain damage. It decided that a more appropriate term for this disorder is "minimal brain dysfunction".
It decided that a more appropriate term for this disorder is "minimal brain dysfunction".
It was assumed that while with "minimal brain damage" there are structural changes in the central nervous system, then with "mild brain dysfunction" there is no localized brain damage, but there is neurochemical and neurophysiological dysfunction.
Various authors attributed at least 100 clinical manifestations to "mild brain dysfunction", including, in addition to increased motor activity and insufficient concentration of attention, aggressiveness, dyslexia, dysgraphia, dyscalculia, visual-perceptual disturbances, etc.
According to Clements, "mild brain dysfunction" is a disorder in children of average or near average (in some above average) intelligence, with mild to severe behavioral disturbances associated with minimal abnormalities in the central nervous system, which may be characterized by various combinations disorders of perception, speech, memory, attention control, motor functions.
B 1975 . B.D. Schmitt opposed the name of the disease "mild brain dysfunction", justifying this by the fact that such a name is usually associated with brain damage, causing parents to fear for the future of the child, his intellectual development. This "label" follows the child from class to class, from school to school. In addition, according to the author, there is no reliable scientific evidence in favor of this term.
The author substantiates this by the following facts: despite the high prevalence of this pathology in various countries of the world, in some of them, for example in the UK, it is quite rare (0.4%).
In 1980, the American Psychiatric Association developed a working classification - DSM-IV (4th edition of the Diagnostic and Statistical Manual of Mental Disorders) - the term "attention deficit" was first introduced, which replaced the term "mild brain dysfunction ", "hyperactivity". Cases previously described as minimal brain dysfunction are proposed to be considered as attention deficit hyperactivity disorder. The underlying premise was that the most common and significant clinical symptoms of minimal brain dysfunction included impaired attention and hyperactivity.
The underlying premise was that the most common and significant clinical symptoms of minimal brain dysfunction included impaired attention and hyperactivity.
In the ICD-10, the syndrome is covered under "Emotional and behavioral disorders with onset usually in childhood and adolescence" under "Disturbance of activity and attention" (F90.0) and "Hyperkinetic conduct disorder" (F90.1).
ICD-10 - International Classification of Diseases 10th revision. As of January 2007, this is the generally accepted classification for coding medical diagnoses, developed by the World Health Organization. ICD-10 consists of 21 sections, each of which contains subsections with codes for diseases and conditions.
The basic symptom of the syndrome was the symptom of "impaired attention". This was justified by the fact that attention disorder occurs in all patients with this pathology, and increased motor activity is not always. In addition to the violation of attention, the emphasis is on the inappropriate behavior of the child.
Later S.E. Schawith et al. divided the syndrome into 3 types: attention deficit hyperactivity disorder, attention deficit hyperactivity disorder without hyperactivity, and the so-called residual type syndrome, a term used to describe adolescents and young adults who had attention deficit hyperactivity disorder at an early age.
4. Prognosis of development
The prognosis of the disease depends on the severity of symptoms, timely diagnosis and appropriate treatment. With early therapeutic intervention, the prognosis for these children is favorable. However, they need constant supervision until graduation.
Experts note the variability of the course of the syndrome: disorders can continue during adolescence and into adulthood. Excessive activity is usually the first symptom that begins remission - alleviating the course of the disease. The peak manifestation of motor disinhibition occurs at 6–7 years of age, with a reverse development by 14–15 years, impulsivity decreases by the end of school, attention deficit, as a rule, remains to one degree or another throughout life. Remissions are not usually observed before the age of 12 years.
Remissions are not usually observed before the age of 12 years.
R.A. Barkley notes that 25 to 50% of hyperactive children outgrow the syndrome. However, in 6-8% of patients, according to O.V. Khaletskaya and V.M. Troshin, the symptoms of the disorder lead to mental retardation, and at an older age they contribute to the emergence of serious psychopathological disorders and asocial conditions.
For the rest, symptoms of varying severity persist and lead to problems in daily life. Such people are often accompanied by a feeling of "impatient and restless", impulsiveness, social inadequacy, a feeling of low self-esteem throughout life. They are disorganized and have little control over their activities.
In adolescence, hyperactive children develop early cravings for alcohol and drugs. For them, to a greater extent than for healthy peers, a tendency to delinquency is characteristic. Only a small percentage (15% versus 50% in controls) of them graduate from school.
What is the prognosis for children with attention deficit hyperactivity disorder?
1.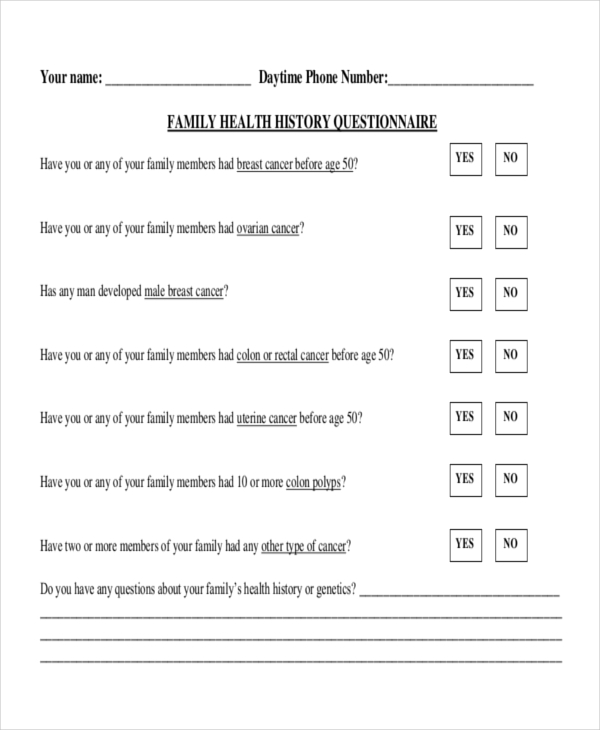 Over time, symptoms disappear and children become adolescents, adults without abnormalities. Analysis of the results of most studies suggests that 25 to 50% of children "outgrow" this syndrome.
Over time, symptoms disappear and children become adolescents, adults without abnormalities. Analysis of the results of most studies suggests that 25 to 50% of children "outgrow" this syndrome.
2. Symptoms in varying degrees of severity persist, but without signs of psychopathology. Such children are the majority (from 50% or more). They have problems in their daily life. According to the survey, they are constantly accompanied by a feeling of "impatient and restless", impulsiveness, social inadequacy, a feeling of low self-esteem throughout their lives. There are reports of a higher frequency of accidents, divorces, job changes among this group of people.
3. Severe complications develop in adults in the form of personality or antisocial changes, alcoholism and even psychotic conditions.
Antisocial behavior is manifested by a wide range of violations, up to serious crime.
Unfavorable prognosis factors for the syndrome are its combination with mental illness, the presence of psychopathology in the mother, as well as symptoms of impulsivity in the patient himself.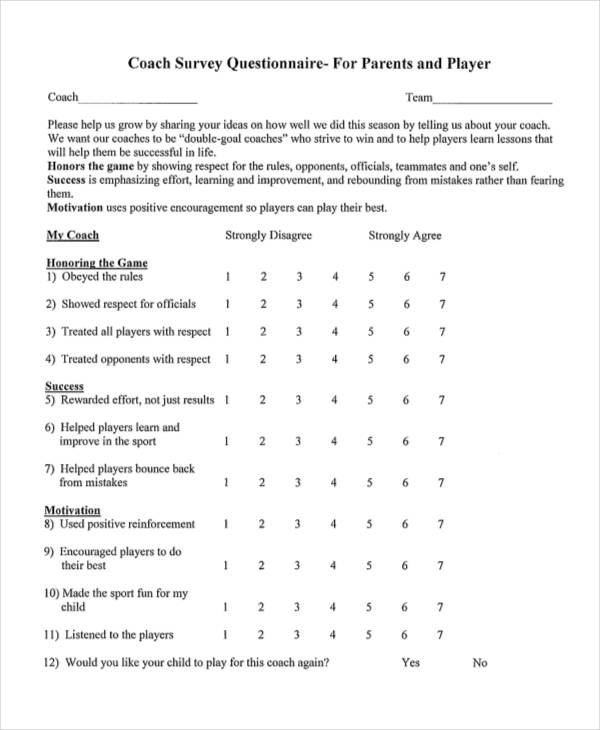
Thus, the prognosis for children with attention deficit hyperactivity disorder is alarming, and the prospects are rather bleak. In such a situation, one cannot hope that children will "outgrow" their condition. Therefore, there is a need for further development of diagnostic methods adapted to our conditions.
5. Typical problems of a child with ADHD
ADHD + conduct disorder (CD). There is a strong association between ADHD and disruptive behavior disorders. By 7 years of age, 35-60% of children with ADHD who are referred to a clinic are also diagnosed with oppositional defiant disorder (ODD), and in mid-childhood and adolescence, 30-50% are also diagnosed with RP. The combination of ADHD + RP occurs earlier than ADHD alone, and the ratio of boys to girls is higher in this case. In general, this is a more severe impairment that negatively affects a wide range of variables related to the children themselves, their relationships with their parents and school performance.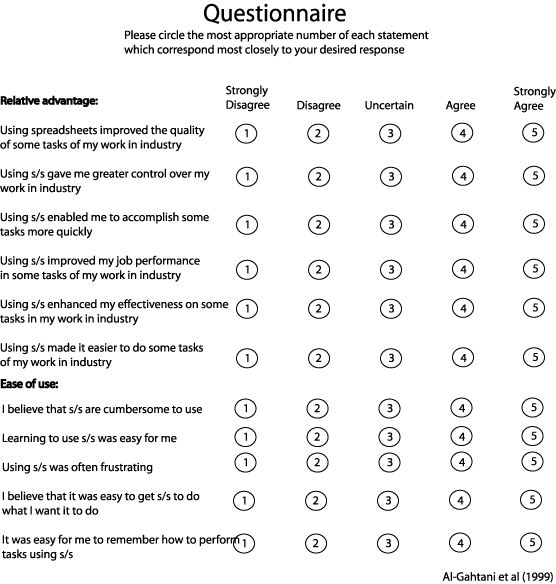
ADHD + anxiety disorder ( TP ). ADHD overlaps with anxiety disorders in 25-40% of the clinical population. The presence of an anxiety disorder, unlike conduct disorder, usually ameliorates rather than exacerbates the disorder. In particular, in children with ADHD + TP, there is a decrease in externalized manifestations in general and impulsivity in particular.
ADHD + learning disability (LL). From 19up to 26% of children with ADHD also have some form of learning disability.
Family relations . The DSM-IV characterizes ADHD as a "disturbing (disruptive) behavior disorder" because its symptoms of aggression, opposition, pushiness, and disorganization undermine the compromise inherent in normal social communication. As you might expect, these symptoms have a negative impact on family relationships.
Mothers are less responsive or less likely to reward their children with ADHD, more negative and domineering in their reactions.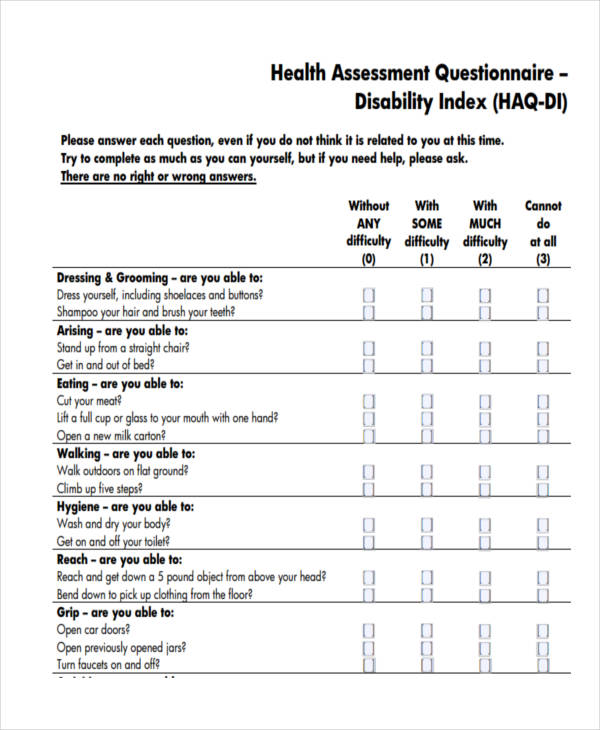 Although the relationship of children to fathers is somewhat less problematic, there is also an increase in father-child conflicts.
Although the relationship of children to fathers is somewhat less problematic, there is also an increase in father-child conflicts.
Peer relationships. Annoying, intrusive, and insensitive behavior in children with ADHD markedly increases the likelihood of peer rejection and social isolation. In addition, the time it takes for peers to notice and react negatively to new kids with ADHD is frighteningly short, estimated at minutes and hours. Parental behavior also plays a role in the status of children with ADHD among their peers. Hinshaw and colleagues (Hinshaw et al., 1997) found that authoritative parenting, with its inherent combination of firmly established boundaries, adequate confrontation, reasoning, warmth, and support, markedly promoted social competence in children with ADHD.
Academic problems . Most children with ADHD who are referred to clinics do poorly in school, and about a quarter of them are characterized by more aggressive manifestations.