Hearing voices ptsd
Post-Traumatic Stress Disorder (Symptoms) | Center for the Treatment and Study of Anxiety
- Symptoms
- Onset & Course
- What causes PTSD?
- More Information
Symptoms
Posttraumatic Stress Disorder (PTSD) is a pathological anxiety disorder resulting after exposure to a traumatic event. Current literature estimates that 8% of the U.S. population meets the criteria for PTSD and while PTSD cases commonly involve combat or assault experiences, there is a wide range of events capable of triggering PTSD symptoms. These events include car accidents, kidnappings, terrorist attacks, natural disasters, and any other traumatic experience where an individual experienced or witnessed an event that involved death or the threat of physical harm.
For example, should a car accident occur, PTSD could result in the drivers, the passengers, or a witness; yet, the development of PTSD in one individual does not imply the development of PTSD in others involved in the incident. How one responds to an event is dependent on a variety of factors that lie outside the traumatic experience itself.
Common Symptoms
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), PTSD is characterized by the following primary symptom areas (applies only for adults and children over age 6):
- Exposure to a traumatic event: Exposure to actual or threatened death, serious injury, or sexual violence in one or more ways, including:
- Directly experiencing the event
- Witnessing the event occur in person
- Learning that the event happened to a close family member or close friend
- Experiencing repeated or extreme exposure to distressing details of the event
- Intrusion or re-experiencing: Recurrent recollections of the event
- Dreams, intrusive memories, and discernable prolonged distress and physical reactions to cues that resemble the traumatic event
- Avoidance: Fear and avoidance behavior
- Avoidance of people, places, thoughts, feelings, or activities closely associated with the traumatic event
- Changes in Mood and Cognition: Negative alterations in emotions or thoughts
- Exaggerated negative beliefs and self-blame for the traumatic event, detachment from others, loss of interest, persistent negative emotional state, reduced ability to feel positive emotions
- Arousal and Hyper-reactivity: Agitation, state of constant wakefulness and alertness
- Hypervigilance, being easily startled, acting irritable or aggressive, recklessness, sleep disturbances, difficulty concentrating
Take, for example, somebody who witnesses a major car accident on a highway by their home. Over the following week, the individual begins to avoid driving on that highway and over the next month, avoids driving all together - either as a driver or a passenger. He/she may become irritable or angry while watching high-speed car chase scenes or avoid conversations about driving; yet, despite the apparent discomfort, the individual may refuse to discuss his/her fear. Moreover, although the witness is unwilling to discuss the fear or the traumatic event itself, he/she may still be haunted by the memory of the accident with segments of the event on “constant replay” in his/her mind.
Over the following week, the individual begins to avoid driving on that highway and over the next month, avoids driving all together - either as a driver or a passenger. He/she may become irritable or angry while watching high-speed car chase scenes or avoid conversations about driving; yet, despite the apparent discomfort, the individual may refuse to discuss his/her fear. Moreover, although the witness is unwilling to discuss the fear or the traumatic event itself, he/she may still be haunted by the memory of the accident with segments of the event on “constant replay” in his/her mind.
Young children do not experience the same reliving of the experience as adults. The progression of PTSD in young children may initially involve dreams about the traumatic event, however, these dreams frequently transform into more generalized nightmares about monsters or different threatening situations where they or another person is in danger. It is more difficult for children to express their sentiments verbally. Therefore, it is necessary for parents or teachers or other adult observers to recognize behavioral changes such as a decreased interest in activity or an altered sense of the future (i.e. the child now believing that he/she will no longer live to become an adult). Other signs of childhood PTSD may occur in the form of repetitive play if the child begins to recreate the incident with toys or may occur through the emergence of physical symptoms such as headaches or stomach aches.
Therefore, it is necessary for parents or teachers or other adult observers to recognize behavioral changes such as a decreased interest in activity or an altered sense of the future (i.e. the child now believing that he/she will no longer live to become an adult). Other signs of childhood PTSD may occur in the form of repetitive play if the child begins to recreate the incident with toys or may occur through the emergence of physical symptoms such as headaches or stomach aches.
An individual’s PTSD might include symptoms such as feelings of shame, or less commonly, compulsive or aggressive behaviors, or self-destructive behavior. These cases often interfere with an individual’s personal life and thus, they are also associated with certain social patterns. These patterns may include sexual dysfunction, marital conflicts, and job loss. There are also strong feelings of guilt and despair that lead to social withdrawal and substance abuse.
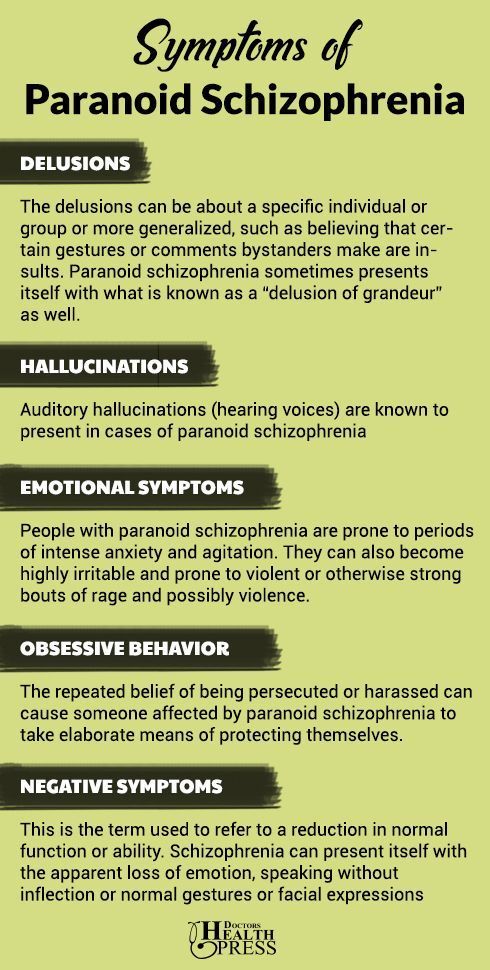
Rare cases of PTSD may involve auditory hallucinations and paranoid ideation. Individuals who experience auditory hallucinations may experience tinnitus, a constant ringing in one’s ears, or they may hear a voice or set of voices that are not physically present. Individuals who are experiencing paranoid ideation are highly guarded and constantly suspicious of being harmed and harassed by those around them. When the trauma involves violent death, symptoms of both complicated grief and PTSD may be present.
Individuals who experience auditory hallucinations may experience tinnitus, a constant ringing in one’s ears, or they may hear a voice or set of voices that are not physically present. Individuals who are experiencing paranoid ideation are highly guarded and constantly suspicious of being harmed and harassed by those around them. When the trauma involves violent death, symptoms of both complicated grief and PTSD may be present.
Back to Top
Onset & Course
The development of PTSD is somewhat unpredictable and can occur at any age. The severity and timing of PTSD symptoms differ with each individual; while symptoms usually begin within the first 3 months after the trauma, there can be a delay of months or even years before a person meets criteria to be diagnosed with PTSD.
PTSD typically develops immediately after the trauma. Nonetheless, in some cases symptoms may not emerge until years have passed since the event. Additionally, a traumatic incident may cause mild PTSD symptoms in one individual while chronically debilitating another. Duration of symptoms also varies, with some people recovering from trauma naturally in the first 3 months, and others experiencing symptoms for months or years.
Duration of symptoms also varies, with some people recovering from trauma naturally in the first 3 months, and others experiencing symptoms for months or years.
All PTSD sufferers usually experience a range of symptoms after a traumatic episode. These symptoms are maintained through avoidance behavior and treatment must be actively pursued in order for complete recovery. Particular variables surrounding the traumatic event may, however, influence the development of PTSD. Elements that are known to make PTSD more likely are the following:
- Perceived life threat
- Personal injury
- Interpersonal violence, particularly perpetrated by a caregiver
- Past and present vulnerability, including genetics, childhood trauma, insufficient emotional support, concurrent causes of stress
Example: Childhood abuse and rape
Symptoms of PTSD may emerge later in life. Example: “When I was child, I was abused by my uncle. I was scared by it at first but I eventually came to accept it. He stopped when I was twelve (I have not seen him since). I tried to forget him and blocked the memory from my mind. I had a healthy romantic life throughout high school and college. I dated numerous people and have been involved in two serious relationships. Last year, however, my best friend was raped by a co-worker. I consoled her and she recovered from the experience but since then, I have not been able to stop thinking about my uncle..."
I was scared by it at first but I eventually came to accept it. He stopped when I was twelve (I have not seen him since). I tried to forget him and blocked the memory from my mind. I had a healthy romantic life throughout high school and college. I dated numerous people and have been involved in two serious relationships. Last year, however, my best friend was raped by a co-worker. I consoled her and she recovered from the experience but since then, I have not been able to stop thinking about my uncle..."
Back to Top
What causes PTSD?
Why one person gets PTSD and not another is not completely understood. However, a traumatic experience is required for a diagnosis. Trauma events frequently associated with the development of PTSD include the following:
- Physical, emotional, or sexual abuse
- Combat experiences
- Terrorist attacks
- Natural disasters such as tornados, floods, earthquakes, or fires
- Life-threatening accidents, such as automobile accidents, airplane crashes, or boating accidents both experienced or witnessed
- Violent crimes, both experienced or witnessed
Epidemiological information
The prevalence of PTSD differs according to both gender and ethnicity. An estimated 8.7% of the U.S. adult population matches the criteria for PTSD with women more likely to develop symptoms than men. Compared with non-Latino European Americans within the U.S., elevated rates of PTSD have been reported mainly among U.S. Latinos, African Americans, and American Indians. Research also suggests that Asian-Americans have the lowest rates of PTSD within the country. These differences are attributed to a variety of cultural and socioeconomic phenomena.
An estimated 8.7% of the U.S. adult population matches the criteria for PTSD with women more likely to develop symptoms than men. Compared with non-Latino European Americans within the U.S., elevated rates of PTSD have been reported mainly among U.S. Latinos, African Americans, and American Indians. Research also suggests that Asian-Americans have the lowest rates of PTSD within the country. These differences are attributed to a variety of cultural and socioeconomic phenomena.
Lower estimates are seen in Europe and most Asian, Latin American, and African countries, ranging from around 0.5% to 1%. This follows the general finding that developed countries have significantly lower rates of PTSD than the developing world. The prevalence of PTSD in the developing world is, however, reasonable given the harsher political and economic climates.
Back to Top
More Information
National Institute of Mental Health (NIMH) - An organization with the National Institute of health dedicated to mental health research:
http://www. nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd/index.shtml
nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd/index.shtml
Army Behavioral Health - A PTSD informational website provided by the U.S. Army Medical Department for the support of Soldiers and their families:
http://armymedicine.mil/Pages/behavioralhealth.aspx
National Center for PTSD (NCPTSD) - A center established by the U.S. Department of Veteran Affairs to improve the well-being of U.S. veterans through PTSD research and education:
www.ncptsd.va.gov/
Prevalence of auditory pseudohallucinations in adult survivors of physical and sexual trauma with chronic post-traumatic stress disorder (PTSD)
- Journal List
- Elsevier Sponsored Documents
- PMC6259581
Behav Res Ther. 2018 Dec; 111: 113–118.
2018 Dec; 111: 113–118.
doi: 10.1016/j.brat.2018.10.015
,a,∗,a,b and a
Author information Article notes Copyright and License information Disclaimer
Auditory Verbal Hallucinations (AVHs) are commonly associated with psychosis but are also reported in post-traumatic stress disorder (PTSD). Hearing voices after the experience of stress has been conceptualised as a dissociative experience. Brewin and Patel’s (2010) seminal study reported that hearing voices is relatively common in PTSD, as hearing voices was associated with PTSD in half and two thirds of military veterans and survivors of civilian trauma, respectively. The authors conceptualised these voices as “auditory pseudohallucinations.” To build upon this work, we administered Brewin and Patel's’ interview to adult survivors (n = 40) of physical and sexual trauma with chronic PTSD, and healthy controls (n = 39). In contrast to previous findings, only 5% (n = 2) of our PTSD sample reported recently hearing a voice that was consistent with an auditory pseudohallucination, with no reports in our control group.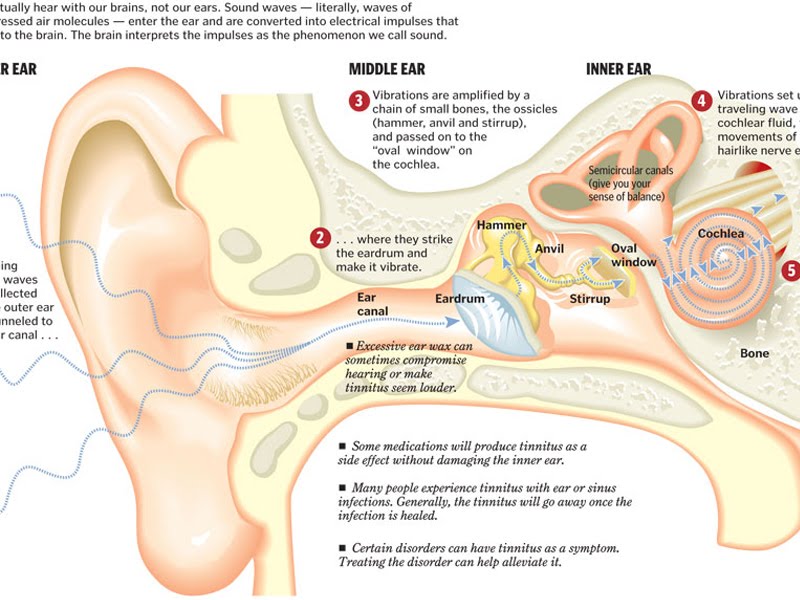 Thus, no support was provided for auditory pseudohallucinations as a significant symptom in this population.
Thus, no support was provided for auditory pseudohallucinations as a significant symptom in this population.
Keywords: Auditory verbal hallucinations, Pseudohallucinations, Hearing voices, PTSD, Dissociation
Auditory verbal hallucinations (AVHs) can be defined as the experience of hearing a voice in the absence of an appropriate external stimulus (Stanghellini & Cutting, 2003). However, the conceputalisation of AVHs and the extent to which hearing voices can be considered phenomenologically independent from other intrusive, unwanted and/or unintended cognitions, has been a matter of enduring academic and clinical debate (e.g., Aleman & Larøi, 2008; Slade & Bentall, 1988). AVHs are commonly associated with psychosis (American Psychiatric Association, 2013) and are recognised as a frequent source of distress and interference with functioning. As a result, AVHs are a major target of pharmacological interventions (Shergill, Murray, & McGuire, 1998) and psychological therapies (Thomas et al. , 2014) for psychosis. However AVHs have also been identified in other disorders (Pilton, Verese, Berry & Bucci, 2015), where the experience of voices can impede therapeutic efficacy. Consequently, there are recommendations for tailoring existing therapeutic interventions (such as cognitive behaviour therapy; CBT) specifically for the treatment of AVHs (e.g. Smailes, Alderson-Day, Fernyhough, McCarthy-Jones, & Dodgson, 2015). Although other types of (pseudo)hallucinatory experiences, such as visual and olfactory hallucinations have been described in individuals with severe PTSD (e.g. Hamner, 1997; Hamner, Frueh, Ulmer, & Arana, 1999), the focus of the current study was on the experience of hearing voices.
, 2014) for psychosis. However AVHs have also been identified in other disorders (Pilton, Verese, Berry & Bucci, 2015), where the experience of voices can impede therapeutic efficacy. Consequently, there are recommendations for tailoring existing therapeutic interventions (such as cognitive behaviour therapy; CBT) specifically for the treatment of AVHs (e.g. Smailes, Alderson-Day, Fernyhough, McCarthy-Jones, & Dodgson, 2015). Although other types of (pseudo)hallucinatory experiences, such as visual and olfactory hallucinations have been described in individuals with severe PTSD (e.g. Hamner, 1997; Hamner, Frueh, Ulmer, & Arana, 1999), the focus of the current study was on the experience of hearing voices.
In non-psychotic conditions, AVHs are most commonly reported in cases of combat-related Post Traumatic Stress Disorder (PTSD) (David, Kutcher, Jackson, & Mellman, 1999; Hamner et al., 1999; Seedat, Stein, Oosthuizen, Emsley, & Stein, 2003). Prevalence rates of AVHs in combat-related PTSD range from 20% to 58% (Brewin & Patel, 2010; David et al.![]() , 1999; Hamner et al., 1999; Ivezic, Bagariæ, Oruè, Mimica, & Ljubin, 2000; Seedat et al., 2003). Studies with civilian samples have been much less common. Anketell et al. (2010) evaluated a mixed sample of general psychiatric outpatients and those who had experienced conflict-related trauma and found that 50% of their sample with chronic PTSD reported AVHs. Similarly, Brewin and Patel (2010) suggested that AVHs are reported by a remarkable 67% of a civilian sample with PTSD.
, 1999; Hamner et al., 1999; Ivezic, Bagariæ, Oruè, Mimica, & Ljubin, 2000; Seedat et al., 2003). Studies with civilian samples have been much less common. Anketell et al. (2010) evaluated a mixed sample of general psychiatric outpatients and those who had experienced conflict-related trauma and found that 50% of their sample with chronic PTSD reported AVHs. Similarly, Brewin and Patel (2010) suggested that AVHs are reported by a remarkable 67% of a civilian sample with PTSD.
This suggested preponderance of AVHs in sufferers of PTSD runs counter to clinical descriptions of the disorder. AVHs are not included as a criterion in the DSM-5 (American Psychiatric Association [APA], 2013) criteria for PTSD, nor are they included as a key focus of treatment in any of the current evidence-based interventions for PTSD (i.e., eye movement desensitisation and reprocessing [EMDR], trauma-focused CBT, prolonged exposure, and cognitive processing therapy [CPT])). If AVHs are indeed a common and central component of the phenomenology of not only combat-related but civilian PTSD then this would have important nosogolical and therapeutic implications. Given this, the nature of AVHs in PTSD and the frequency of their experience in community PTSD samples is in need of further investigation and that is the focus of the present study.
Given this, the nature of AVHs in PTSD and the frequency of their experience in community PTSD samples is in need of further investigation and that is the focus of the present study.
A critical question is whether AVHs in PTSD are better conceptualised as pseudohallucinations linked to dissociative states, rather than as psychotic symptoms. Strong links between psychotic symptoms, including AVHs, and dissociative experiences have been demonstrated in a number of studies, in both clinical and non-clinical populations (see Moskowitz, Barker-Collo, & Ellson, 2004 for review). Allen, Coyne, and Console (1997) argued that dissociative detachment deprives individuals of “internal and external anchors”. The absence of anchors is proposed to increase an individual's sense of feeling disconnected from the world, interpersonal relationships, and within their intrapersonal self, resulting in a sense of confusion and disorientation, and critically, in an impairment in reality-testing. In this way, Moskowitz and Corstens (2007) proposed that for individuals hearing voices when exposed to high levels of stress, AVHs should be conceptualised as dissociative experiences. Similarly, Longden, Madill, and Waterman (2012) proposed that voices could be conceptualised as dissociated or ‘disowned components of the self’, arising from the failure to integrate adverse and traumatic sensory and psychological experiences into the context of the self. Hallucinatory experiences might therefore reflect directly or indirectly dissociated traumatic content (e.g., the voice of an abuser) impinging on conscious awareness (e.g. Anketell et al., 2010), rather than a psychotic symptom.
Similarly, Longden, Madill, and Waterman (2012) proposed that voices could be conceptualised as dissociated or ‘disowned components of the self’, arising from the failure to integrate adverse and traumatic sensory and psychological experiences into the context of the self. Hallucinatory experiences might therefore reflect directly or indirectly dissociated traumatic content (e.g., the voice of an abuser) impinging on conscious awareness (e.g. Anketell et al., 2010), rather than a psychotic symptom.
Indeed, prior research has demonstrated a strong correlation in veterans with PTSD between hearing voices and other dissociative experiences both in the present and at the time the traumatic event occurred (Brewin & Patel, 2010). Wearne, Curtis, Genetti, Samuel, and Sebastian (2017) also showed that dissociative experiences (including depersonalisation and derealisation) were a better predictor of AVHs than a diagnosis of PTSD. Both theory and prior research therefore suggest that the experience of AVHs in PTSD may be better understood as a dissociative experience and thus conceptualised as ‘pseudohallucinations’ and we shall use this term for the rest of the current article. A focus of the present study was therefore on the association between the experience of such pseudohallucinations and other dissociative symptoms.
A focus of the present study was therefore on the association between the experience of such pseudohallucinations and other dissociative symptoms.
For those experiencing civilian PTSD this raises the question of whether particular types of trauma exposure or trauma history are more or less likely to be associated with the experience of pseudo-hallucinations, as we know that dissociation is differentially associated with particular profiles of trauma exposure (Briere, 2006). The experience of childhood sexual abuse, has been established as a predictor of pseudohallucinations in samples both with and without psychosis (Hammersley & Fox, 2006; McCarthy-Jones, 2011; Read, McGregor, Coggan, & Thomas, 2006; Wearne et al., 2017), although the properties of the voices in these populations do not appear to differ between those with and without CSA (e.g. Offen, Waller, & Thomas, 2003). For this reason, the present study focused on a civilian sample presenting with PTSD following sexual assault, abuse or violence either in childhood or adulthood.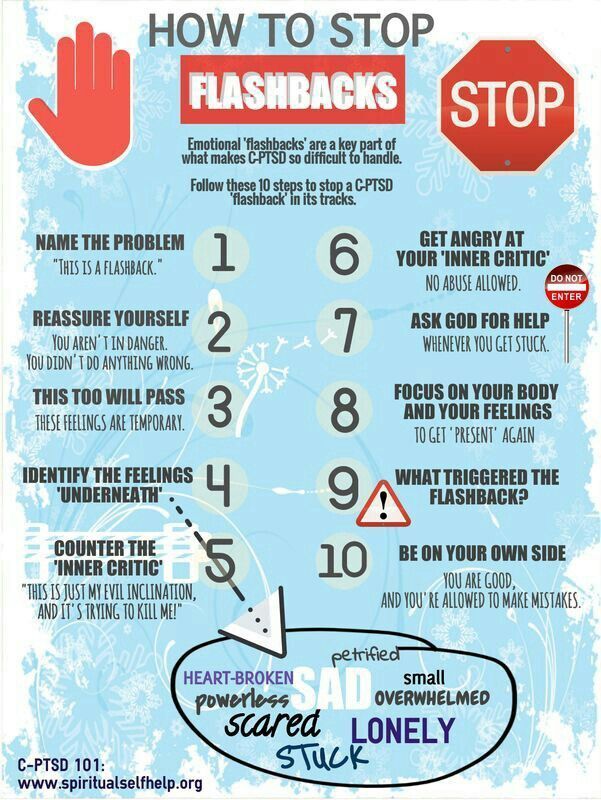 We reasoned that the predicted high incidence of dissociation in this population would mean that the clinical presentation should include pseudohallucinations if such experiences are indeed a prevalent symptom in civilian samples. This population also allowed us to elucidate putative associations between pseudohallucinations and trauma in childhood.
We reasoned that the predicted high incidence of dissociation in this population would mean that the clinical presentation should include pseudohallucinations if such experiences are indeed a prevalent symptom in civilian samples. This population also allowed us to elucidate putative associations between pseudohallucinations and trauma in childhood.
Hamner and colleagues (Hamner, 1997; Hamner et al., 1999) have also suggested that pseudohallucinations in PTSD might be best accounted for as a function of comorbid depression. Since depression is not typically associated with high levels of dissociation, Brewin and Patel (2010) proposed that finding high levels of pseudohallucinations in a depressed sample would argue against their being a dissociative phenomenon. In their study of civilians with PTSD, Brewin and Patel (2010) collected an additional depressed sample without a primary diagnosis of PTSD. They found that 10% of the depressed sample reported the experience of pseudohallucinations and that these individuals scored in the low range on dissociative measures.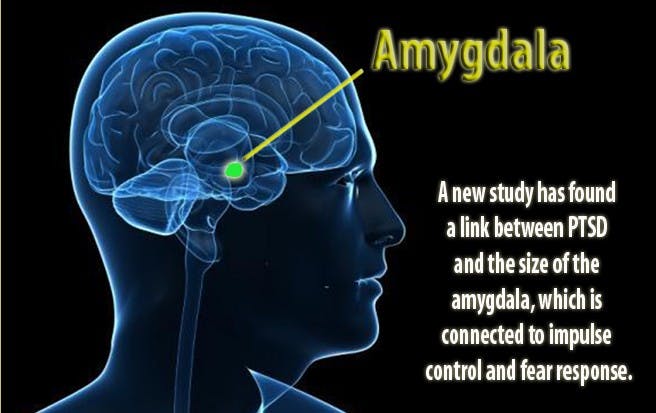 1 From this, Brewin and Patel (2010) concluded that pseudohallucinations were not a function of comorbid depression but likely to be an aspect of dissociation. However, showing that pseudohallucinations do not characterize individuals with depression is not the same as investigating the role of comorbid depression in those with PTSD. In the present study, we therefore evaluated the relationship between depression comorbidity and pseudohallucinations in our community PTSD sample.
1 From this, Brewin and Patel (2010) concluded that pseudohallucinations were not a function of comorbid depression but likely to be an aspect of dissociation. However, showing that pseudohallucinations do not characterize individuals with depression is not the same as investigating the role of comorbid depression in those with PTSD. In the present study, we therefore evaluated the relationship between depression comorbidity and pseudohallucinations in our community PTSD sample.
In sum, using both a self-report measure of dissociative experiences and a semi-structured interview to assess pseudohallucinations in trauma survivors (Brewin & Patel, 2010), we sought to determine if the prevalence of pseudohallucinations in a British sample of adult survivors of repeated physical and sexual trauma was as high as reported in the two previous studies with civilian samples (Anketell et al., 2010; Brewin & Patel, 2010). We also aimed to determine whether the frequency of pseudohallucinations was associated with the experience of childhood versus adult trauma.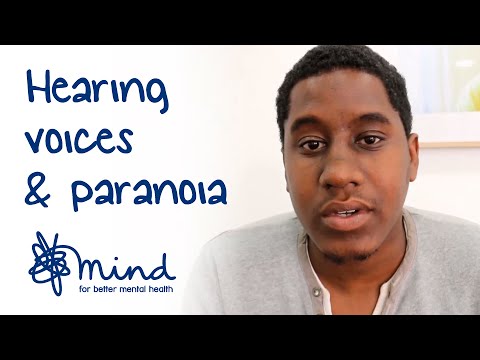 Finally, we aimed to explore the nature of pseudohallucinations by determining if their experience was associated with other dissociative symptomatology and with the experience of comorbid depression.
Finally, we aimed to explore the nature of pseudohallucinations by determining if their experience was associated with other dissociative symptomatology and with the experience of comorbid depression.
2.1. Participants
Ethics approval was obtained from the NHS National Research Ethics Service (reference 11/H0305/1). We recruited adults (aged 18–62) with a current diagnosis of chronic2 PTSD (n = 40) according to the DSM-IV (APA, 2013), following a history of sexual, physical and/or emotional abuse (as Criterion A events), and a healthy control group with no history of disordered mental health (n = 40), as determined using the Structured Clinical Interview for the DSM-IV (SCID-I; First, Spitzer, Gibbon, Williams, & Janet, 1996). Fifteen of the PTSD participants were recruited from the Haven – A Sexual Assault Referral Centre (SARC) in Paddington. They were invited to take part following attendance at the Haven follow-up clinic or during an assessment for counseling or psychological therapy. Twenty-five of the PTSD participants and all of the control participants were recruited from the MRC Cognition and Brain Sciences Unit Volunteer Panels –databases of some 2000 community volunteers who have agreed to help with psychological research. Volunteers were recruited to the panels via advertisements in local newspapers.
Twenty-five of the PTSD participants and all of the control participants were recruited from the MRC Cognition and Brain Sciences Unit Volunteer Panels –databases of some 2000 community volunteers who have agreed to help with psychological research. Volunteers were recruited to the panels via advertisements in local newspapers.
According to the SCID-I, 35 (88%) of the PTSD group were exposed to between two and ‘too many to count’ past traumatic experiences (‘Criterion A traumas’). Nineteen (47.5%) reported that they experienced trauma prior to the age of 18, with the remaining 52% having only experienced trauma during adulthood (allowing us to compare AVHs between those with and without childhood trauma histories). Thirty eight percent of the total sample had experienced sexual assault during adulthood. All participants met DSM-IV criteria for chronic PTSD occurring as a result of these traumatic experiences. Sixteen (40%) had a comorbid diagnosis of Major Depressive Disorder (MDD), as determined by the SCID-I. One control participant met criteria for Obsessive Compulsive Disorder and was excluded.
One control participant met criteria for Obsessive Compulsive Disorder and was excluded.
2.2. Procedure and measures
Participants completed the measures in a single session, individually and face-to-face with the experimenter, in a quiet testing room. All participants completed the SCID-I, to derive diagnoses of PTSD and other Axis I disorders and to determine that criteria for Schizophrenia Spectrum and Other Psychotic Disorders were not met. In addition, participants completed the Beck Depression Inventory (BDI-I; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961 3) to assess current depression symptomatology, along with two measures of hearing voices – the Dissociative Experiences Scale II (DES-II; Item 27 focuses on hearing voices), and a semi-structured interview to assess hearing voices (Brewin & Patel, 2010).
Dissociative Experiences Scale-II (DES-II; Carlson & Putnam, 1993). The Dissociative Experiences Scale (DES-II) is a 28-item self-report instrument and widely used clinical tool to measure dissociation. The DES-II has good validity and reliability, and good psychometric properties (Carlson et al., 1993; Carlson & Putnam, 1993). Hearing voices is included as Item 27 on the DES-II: “Some people sometimes find they hear voices inside their head that tell them to do things or comment on things they are doing. Circle a number (0–100) to show what percentage of time this happens to you.” This item is part of a subset of DES-II items (the Dissociative Experiences Scale-II Taxon; DES-T; comprising items 3, 5, 7, 8, 12, 13, 22 and 27) that differentiate individuals with pathological dissociation from those showing normal variation in dissociative experiences (Waller, Putnam, & Carlson, 1996).
The DES-II has good validity and reliability, and good psychometric properties (Carlson et al., 1993; Carlson & Putnam, 1993). Hearing voices is included as Item 27 on the DES-II: “Some people sometimes find they hear voices inside their head that tell them to do things or comment on things they are doing. Circle a number (0–100) to show what percentage of time this happens to you.” This item is part of a subset of DES-II items (the Dissociative Experiences Scale-II Taxon; DES-T; comprising items 3, 5, 7, 8, 12, 13, 22 and 27) that differentiate individuals with pathological dissociation from those showing normal variation in dissociative experiences (Waller, Putnam, & Carlson, 1996).
Auditory Pseudohallucinations Interview (Brewin & Patel, 2010). The Auditory Pseudohallucinations Interview was administered to all PTSD and control participants. This measure was taken from prior evaluations of pseudohallucinations (Brewin & Patel, 2010). To our knowledge, this measure has not been used in any other published studies. We administered the semi-structure interview in its entirety, as used by Brewin and Patel (2010).
We administered the semi-structure interview in its entirety, as used by Brewin and Patel (2010).
The interview asked "Have you been aware in the past week of a stream of thoughts that repeats a very similar message over and over again inside your head? Sometimes the thoughts may just comment, or give instructions, or say if something is good or bad”. If participants responded yes, they were asked "Do you experience this as a voice or as a stream of thoughts?4″ If identified as a voice, details of up to three separate voices were recorded, including gender, whether it was a voice they recognised, how the voice referred to them, how often they currently heard the voice, when they had first noticed the voice, whether the voice related in any way to a past traumatic experience and the extent to which the voice seemed real (i.e., like someone was actually speaking to them). Participants described what the voice typically said and rated the effect of hearing the voice on a five-point scale for the extent to which they a) believed the content, b) could disagree with the voice, and c) could control the voice.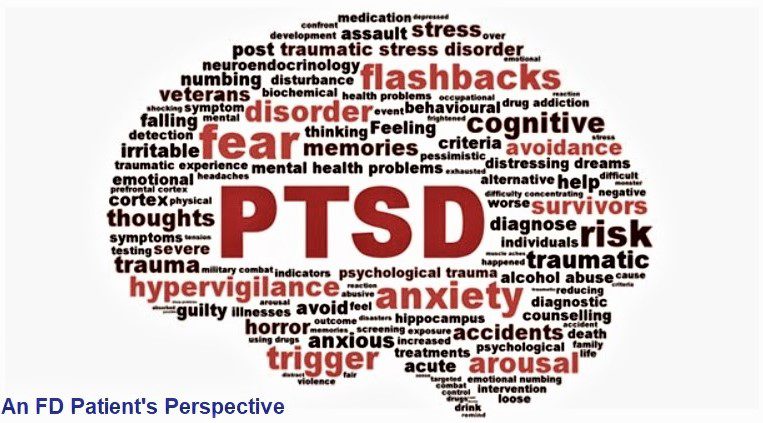 Finally, again using five-point scales, they were asked to rate the extent to which encouraging, critical, happy, angry, rational, intimidating, supportive, and strong described each voice.
Finally, again using five-point scales, they were asked to rate the extent to which encouraging, critical, happy, angry, rational, intimidating, supportive, and strong described each voice.
Demographic and symptom data are presented in . We observed the expected between-group difference in BDI-I scores. The control group were younger and more educated than the PTSD group, thus these variables were covaried in analyses. All results remained the same when the participants who had only experienced one trauma (n = 5) were removed from analyses, and data were re-analysed including only those who had experienced repeated traumas. The relationship between the number of experienced traumatic events and the key outcome measures is presented in .
Table 1
Mean (standard deviation) clinical Characteristics of PTSD Participants and Controls.
| PTSD Group (n = 40) | Control Group (n = 39) | Statistical Test | Effect Size (d) | |
|---|---|---|---|---|
| Years in Education | 14. 15 (2.54) 15 (2.54) | 17.03 (1.90) | t(70.37) = 5.78, p < .001 | |
| Age (in years) | 34.40 (12.35) | 28.95 (8.22) | t(67.39) = 2.33, p = .02 | |
| Beck Depression Inventory score | 27.10 (12.59) | 3.46 (6.16) | t(55.39) = 10.42, p < .001 | |
| Dissociative Experiences Scalea (DES-II) score | 26.80 (18.95) | 5.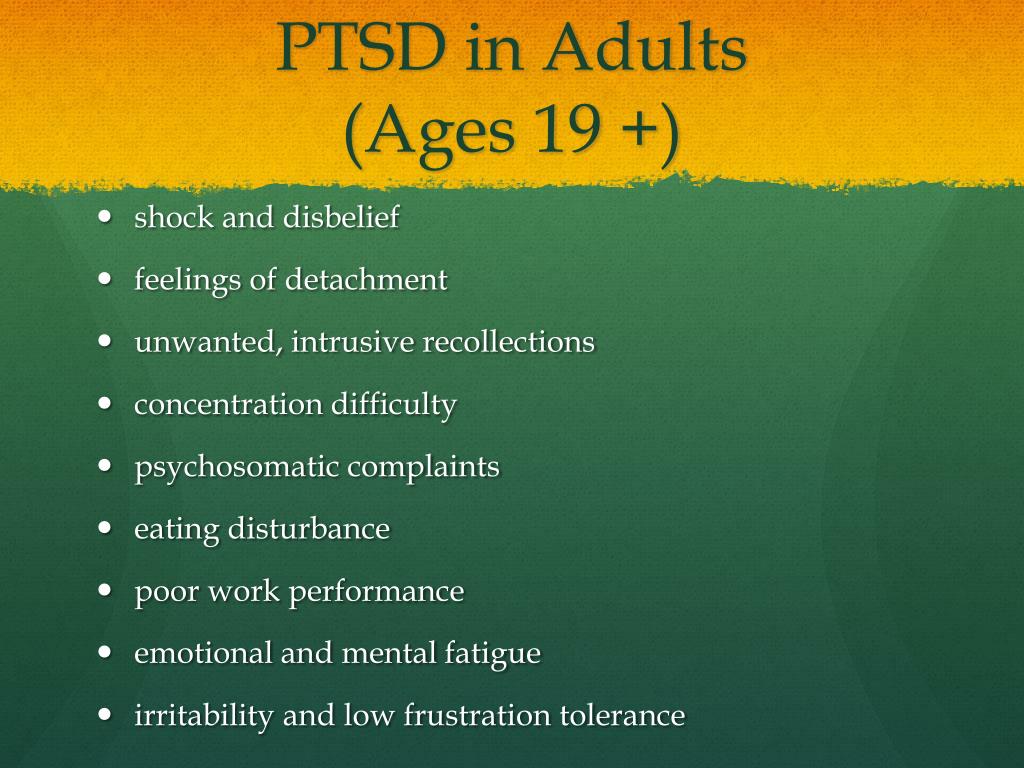 41 (6.04) 41 (6.04) | F(1, 75) = 22.03, p < .001 | 0.54 |
| DES-II Item 27 (hearing voices) score | 13.00 (25.34) | 0.00 (0.00) | F(1, 75) = 6.36, p = .01 | 0.29 |
| DES-T score | 21.44 (19.36) | 1.85 (3.33) | F(1, 75) = 19.57, p < .001 | 0.51 |
Open in a separate window
aDES-II analyses covaried age and education.
Open in a separate window
a) Relationship between the Number of Experienced Traumatic Events and the Complex Trauma Symptoms Questionnaire (CTSQ) Total Score for the PTSD Group (n=40). b) Relationship between the Number of Experienced Traumatic Events and the Dissociative Experiences Scale (DES-II) Total Score for the PTSD Group (n=40). c). Relationship between the Number of Experienced Traumatic Events and the Dissociative Experiences Scale Taxon (DES-T) for the PTSD Group (n=40).
b) Relationship between the Number of Experienced Traumatic Events and the Dissociative Experiences Scale (DES-II) Total Score for the PTSD Group (n=40). c). Relationship between the Number of Experienced Traumatic Events and the Dissociative Experiences Scale Taxon (DES-T) for the PTSD Group (n=40).
DES-II data. DES scores across groups are also displayed in . As can be seen from the table, ANCOVAs including age and education as covariates comparing the PTSD and control groups revealed significant group differences on the DES-II, DES-T and DES Item 27, with the PTSD group scoring significantly higher on all indices. Scores on Item 27 were strongly correlated with the sum of the remaining DES-T items, r (38) = 0.68, p < .001.
Within the PTSD sample, 13/40 (32.5%) answered positively (reported hearing voices >10% of the time) to Item 27. This contrasts with 48.4% of Brewin and Patel's (2010) veteran sample. None of the controls endorsed this item.
Those within the PTSD group reporting childhood trauma (n = 19) scored significantly higher on the DES-II (M = 33.31, SD = 22.52), t(36) = 2.32, p = .03, and on the DES-T (M = 27.04, SD = 23.33), t(36) = 2.08, p=.05, than those reporting trauma only in adulthood (n = 21; DES-II: M = 19.55, SD = 12.57; DES-T: M = 14.47, SD = 12.22). However, critically, there was no support for a difference between groups on Item 27 (childhood: M = 11.58, SD = 25.44; adulthood: M = 11.05, SD = 22.08), t(36) = 0.07, p = .95, d = 0.02, where the effect size was trivial (Cohen, 1992.
There were positive significant correlations between the DES-T scores and the total score on the CTSQ, r(38) = 0.64, n = 40, p < .001and the BDI, r(38) = 0.45, n = 40, p = .004) for the PTSD group.
Sixteen (40%) participants with PTSD also had a diagnosis of MDD. Scores on the DES-II did not significantly differ between those with (DES-II: M = 28. 48, SD = 17.20; DES-T:M = 23.52, SD = 17.97; Item 27: M = 11.25, SD = 26.05) and without (DES-II: M = 25.67, SD = 20.31; DES-T: M = 20.05, SD = 20.50; Item 27: M = 14.17, SD = 25.35) comorbid MDD on the DES-II, t(38) = 0.46, p = .65, DES-T, t(38) = 0.55, p > .05, or Item 27, t(38) = -0.35, p = .73 and effect sizes were trivial (0.11 for DES-II, 0.12 for DES-T and 0.10 for Item 27)(Cohen, 1992).
48, SD = 17.20; DES-T:M = 23.52, SD = 17.97; Item 27: M = 11.25, SD = 26.05) and without (DES-II: M = 25.67, SD = 20.31; DES-T: M = 20.05, SD = 20.50; Item 27: M = 14.17, SD = 25.35) comorbid MDD on the DES-II, t(38) = 0.46, p = .65, DES-T, t(38) = 0.55, p > .05, or Item 27, t(38) = -0.35, p = .73 and effect sizes were trivial (0.11 for DES-II, 0.12 for DES-T and 0.10 for Item 27)(Cohen, 1992).
Semi-structured interview. In response to the interview, 18/40 (45%) participants with PTSD reported having experienced a stream of thoughts in the past week. Of these, 11 (61.1%) had an MDD diagnosis and eight (44.4%) reported experiencing childhood trauma. However, only two (11.11%) of those participants reported hearing repetitive thoughts in the form of a voice speaking to them. Each had PTSD following childhood trauma (one had experienced sexual and one physical childhood abuse). This contrasts starkly with Brewin and Patel's (2010) finding of 67% of a heterogeneous civilian PTSD sample reporting voices on the same interview measure.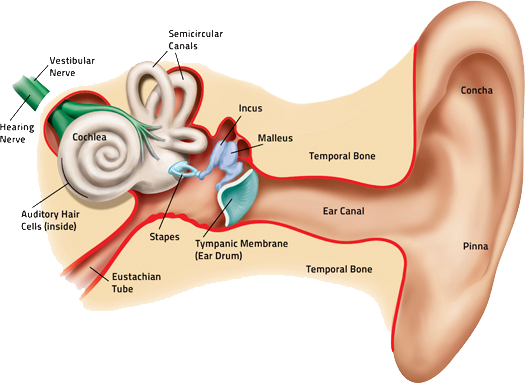 Both participants here regarded the voice as a manifestation of their own thoughts (a “pseudohallucination”, Brewin & Patel, 2010). Each reported hearing one voice, which they recognised. One participant identified the voice as her father, who referred to her by name, and the other was identified as the female participant's own voice, which referred to them as ‘stupid bitch’ and was described as ‘talking to me like someone else would’. In both cases, the voice was heard ‘many times a day’. The effect of the voice was described as positive in one case (own voice) and negative in the other (father's voice). Both participants described the voice as having been present since childhood.
Both participants here regarded the voice as a manifestation of their own thoughts (a “pseudohallucination”, Brewin & Patel, 2010). Each reported hearing one voice, which they recognised. One participant identified the voice as her father, who referred to her by name, and the other was identified as the female participant's own voice, which referred to them as ‘stupid bitch’ and was described as ‘talking to me like someone else would’. In both cases, the voice was heard ‘many times a day’. The effect of the voice was described as positive in one case (own voice) and negative in the other (father's voice). Both participants described the voice as having been present since childhood.
In the control group, 3/39 (8%) participants reported having experienced a stream of thoughts, but none identified these as a voice.
In this study, we sought to determine if the prevalence of auditory pseudohallucinations in a British sample of adult survivors of physical and sexual trauma with chronic PTSD was as high as reported in the two previous studies with civilian samples (Anketell et al. , 2010; Brewin & Patel, 2010). We also aimed to determine whether the frequency of auditory pseudohallucinations was associated with the experience of childhood versus adult trauma. Finally, we aimed to explore the nature of auditory pseudohallucinations by determining if their experience was associated with other dissociative symptomatology and with the experience of comorbid depression.
, 2010; Brewin & Patel, 2010). We also aimed to determine whether the frequency of auditory pseudohallucinations was associated with the experience of childhood versus adult trauma. Finally, we aimed to explore the nature of auditory pseudohallucinations by determining if their experience was associated with other dissociative symptomatology and with the experience of comorbid depression.
In our PTSD sample, 32.5% answered positively (reported hearing voices >10% of the time) to Item 27 of the DES-II. When this question was presented within a semi structured interview, 45% of the PTSD group endorsed such experiences. However, when probed as to whether they experienced this “as a voice or a stream of thoughts”, only 2/40 (5%) of our sample of survivors of physical and sexual trauma reported recently hearing “a voice” that was consistent with an auditory pseudohallucination. This is significantly lower than the 67% of Brewin and Patel's (2010) PTSD sample, using the same semi-structured interview approach, and than the 50% reported by Anketell et al. (2010). None of our healthy control participants endorsed hearing voices on the interview measure nor on item 27 of the DES-II.
(2010). None of our healthy control participants endorsed hearing voices on the interview measure nor on item 27 of the DES-II.
We also sought to evaluate the relationship of the experience of childhood trauma and of comorbid depression with the experience of hearing voices. However, as only two participants endorsed hearing voices, meaningful analyses were not possible. Of note, however, we found no support for differential endorsement of the relevant items on the DES for those with PTSD as a function of childhood trauma, or for those with PTSD and comorbid depression.
There are a number of factors which may have contributed to the discrepancy in endorsement of voices on the DES-II relative to the interview. A key difference between these measures is that during the interview the individual is required to explicitly distinguish between the endorsed experience being either a) a voice talking to them or b) a stream of thoughts, and the majority (all bar two) of the participants reported that it was a stream of thoughts. It is possible that the DES-II may capture rumination and internal self-talk, and thus the more fine-grained evaluation provided by the interview question may account for why the incident reduced from that reported in the DES-T. Of course, there is also the possibility that participants did not want to discuss the voice face-to-face with a clinician for fear of negative evaluation or discomfort, and thus more readily reported hearing voices in the self-report format but we feel this is unlikely given that participants had consented to take part in the study knowing that this was a focus. These issues will need to be addressed in future studies.
It is possible that the DES-II may capture rumination and internal self-talk, and thus the more fine-grained evaluation provided by the interview question may account for why the incident reduced from that reported in the DES-T. Of course, there is also the possibility that participants did not want to discuss the voice face-to-face with a clinician for fear of negative evaluation or discomfort, and thus more readily reported hearing voices in the self-report format but we feel this is unlikely given that participants had consented to take part in the study knowing that this was a focus. These issues will need to be addressed in future studies.
In our sample of adults with a history of repeated physical and sexual trauma, we therefore found no evidence to support the previously reported high prevalence rates of auditory pseudohallucinations in other PTSD samples assessed using similar interview measures. The question of course is raised as to why there should be such a discrepancy between our findings and previous work. One possibility is that auditory pseudohallucinations are not a feature, specifically, of PTSD populations who have experienced repeated sexual or physical interpersonal trauma. However, given the previous literature linking such trauma exposure to higher levels of dissociation (Briere, 2006) and to the experience of auditory pseudohallucinations in individuals with and without psychosis (Hammersley & Fox, 2006; McCarthy-Jones, 2011; Read, van Os, Morrison, & Ross, 2015; Wearne & Genetti, 2015), one would have predicted a priori a higher prevalence of AVHs in the present sample relative to a heterogeneous community sample of the kind evaluated by Brewin and Patel (2010). Another possibility is although auditory pseudohallucinations have been conceptualised in the literature as a distinct psychological symptom, they should instead be considered as an artefact of recurrent intrusive memories and the auditory re-experiencing of traumatic events. We found that 18/40 of our PTSD group reported having experienced a stream of thoughts but only two reported this was a voice speaking to them when probed by a clinician with extensive experience of working with complex PTSD populations.
One possibility is that auditory pseudohallucinations are not a feature, specifically, of PTSD populations who have experienced repeated sexual or physical interpersonal trauma. However, given the previous literature linking such trauma exposure to higher levels of dissociation (Briere, 2006) and to the experience of auditory pseudohallucinations in individuals with and without psychosis (Hammersley & Fox, 2006; McCarthy-Jones, 2011; Read, van Os, Morrison, & Ross, 2015; Wearne & Genetti, 2015), one would have predicted a priori a higher prevalence of AVHs in the present sample relative to a heterogeneous community sample of the kind evaluated by Brewin and Patel (2010). Another possibility is although auditory pseudohallucinations have been conceptualised in the literature as a distinct psychological symptom, they should instead be considered as an artefact of recurrent intrusive memories and the auditory re-experiencing of traumatic events. We found that 18/40 of our PTSD group reported having experienced a stream of thoughts but only two reported this was a voice speaking to them when probed by a clinician with extensive experience of working with complex PTSD populations. Perhaps only these two participants had found the metaphor of “hearing voices” to be a helpful way of explaining a recurrent intrusion.
Perhaps only these two participants had found the metaphor of “hearing voices” to be a helpful way of explaining a recurrent intrusion.
A recent review (Steel, 2015) explored the relationship between hallucinations (including AVHs) and stressful or traumatic life events, with the reviewed studies indicating that there was a 12–40% overlap in the content of pseudohallucinations and traumatic memories The largest phenomenological survey of AVHs to date involved interviewing 199 voice hearers (McCarthy-Jones et al., 2014). Of these, 12% reported that they heard voices, which were identical replays of memories of previous conversations, whilst 31% reported that the relationship was similar but not identical. Similarly, studies reviewed by Steel (2015) suggested the presence of thematic links between prior trauma and the content of hallucinations. Steel (2015) concluded that the relationship between hallucinations and past traumatic experiences remains elusive, and thus is in need of further investigation. If AVHs are the auditory re-experiencing of past traumatic events then this has important implications for treatment; for example, the content of AVHs may represent hotpots that require rescripting in trauma-focused CBT and other similar interventions.
If AVHs are the auditory re-experiencing of past traumatic events then this has important implications for treatment; for example, the content of AVHs may represent hotpots that require rescripting in trauma-focused CBT and other similar interventions.
Limitations of this study include the specific focus on individuals with a chronic history of multiple incidences of sexual, physical and/or emotional abuse, rather than a broader inclusion of other, non-interpersonal traumatic experiences. As is common when working with survivors of repeated traumas, it was difficult to distinctly separate out different trauma types and their timing, especially with those who had experienced childhood trauma, and this therefore represents a methodological limitation. Our control and PTSD groups were also not matched for age and education level, although this turned out to be moot as there was minimal difference in our core construct of interest – endorsement of hearing voices in a semi-structured clinical interview. An additional limitation of the study was not including a formal measure of PTSD severity, such as the Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995), although all participants did meet criteria for the Chronic PTSD specifier on the SCID.
An additional limitation of the study was not including a formal measure of PTSD severity, such as the Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995), although all participants did meet criteria for the Chronic PTSD specifier on the SCID.
In summary, in contrast to our predictions we found no support for a significant presence of auditory pseudohallucinations in a civilian sample of adults with chronic PTSD following sexual and/or physical interpersonal trauma. Our results suggest that prior reports of high prevalence of auditory pseudohallucinations in civilian samples are in need of further replication.
This work was supported by the UK Medical Research Council (MRC; grant number SUAG/006/RG91365).
1Below 30 on the Dissociative Experiences Scale-II (DES-II; Carlson & Putnam, 1993).
2duration of symptoms is 3 months or more (APA, 2013).
3The first version of the BDI was used for legacy reasons to do with the Department volunteer panels.
4The wording of this question was changed from ‘Do you experience this as a voice or just as a stream of thoughts’ by removing the word ‘just’ as we were concerned that keeping it in implied that one was more important than the other.
Aleman A., Larøi F. American Psychological Association; Washington, DC: 2008. Hallucinations: The science of idiosyncratic perception. [Google Scholar]
Allen J.G., Coyne L., Console D.A. Dissociative detachment contributes to psychoticism and personality decompensation. Comprehensive Psychiatry. 1997;38:327–334. [PubMed] [Google Scholar]
American Psychiatric Association . 5th ed. American Psychiatric Publishing; Arlington, VA: 2013. Diagnostic and statistical manual of mental disorders. [Google Scholar]
Anketell C., Dorahy M.J., Shannon M., Elder R., Hamilton G., Corry M. An exploratory analysis of voice hearing in chronic PTSD: Potential associated mechanisms. Journal of Trauma & Dissociation.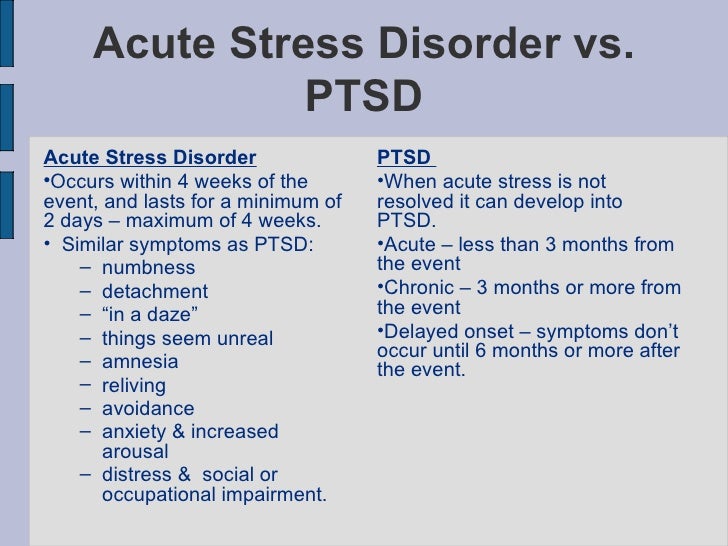 2010;11:93–107. [PubMed] [Google Scholar]
2010;11:93–107. [PubMed] [Google Scholar]
Beck A.T., Ward C.H., Mendelson M., Mock J., Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. [PubMed] [Google Scholar]
Blake D.D., Weathers F.W., Nagy L.M., Kaloupek D.G., Gusman F.D., Charney D.S. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. [PubMed] [Google Scholar]
Brewin C.R., Patel T. Auditory pseudohallucinations in United Kingdom war veterans and civilians with posttraumatic stress disorder. Journal of Clinical Psychiatry. 2010;71:419–425. [PubMed] [Google Scholar]
Briere J. Dissociative symptoms and trauma exposure: Specificity, affect dysregulation, and posttraumatic stress. The Journal of Nervous and Mental Disease. 2006;194:78–82. [PubMed] [Google Scholar]
Carlson E.B., Putnam F.W. An update on the dissociative experiences scale. Dissociation. 1993;6:16–27. [Google Scholar]
Carlson E.B., Putnam F. W., Ross C.A., Torem M., Coons P., Dill D.L. Validity of the dissociative experiences scale in screening for multiple personality disorder: A multicenter study. American Journal of Psychiatry. 1993;150:1030–1036. [PubMed] [Google Scholar]
W., Ross C.A., Torem M., Coons P., Dill D.L. Validity of the dissociative experiences scale in screening for multiple personality disorder: A multicenter study. American Journal of Psychiatry. 1993;150:1030–1036. [PubMed] [Google Scholar]
Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037/0033-2909.112.1.155. [PubMed] [CrossRef] [Google Scholar]
David D., Kutcher G.S., Jackson E.I., Mellman T.A. Psychotic symptoms in combat-related posttraumatic stress disorder. Journal of Clinical Psychiatry. 1999;60:29–32. doi: 10.4088/JCP.v60n0106. [PubMed] [CrossRef] [Google Scholar]
First M.B., Spitzer R.L., Gibbon M., Williams J.B., Janet B.W. American Psychiatric Press, Inc; Washington, D.C.: 1996. Structured clinical interview for DSM-IV Axis I disorders, clinician version (SCID -CV) [Google Scholar]
Hammersley P., Fox R. Childhood trauma and psychosis in the major mood disorders. In: Larkins W., Morrison A., editors. Trauma and psychosis: New directions for theory and therapy. Routledge; New York: 2006. [Google Scholar]
Routledge; New York: 2006. [Google Scholar]
Hamner M.B. Psychotic features and combat‐associated PTSD. Depression and Anxiety. 1997;5:34–38. doi:10.1002/(SICI)1520-6394(1997)5:1<34::AID-DA6>3.0.CO;2-5. [PubMed] [Google Scholar]
Hamner M.B., Frueh B.C., Ulmer H.G., Arana G.W. Psychotic features and illness severity in combat veterans with chronic post-traumatic stress disorder. Biological Psychiatry. 1999;45:846–852. doi: 10.1016/S0006-3223(98)00301-1. [PubMed] [CrossRef] [Google Scholar]
Ivezic S., Bagariæ A., Oruè L., Mimica N., Ljubin T. Psychotic symptoms and comorbid psychiatric disorders in Croatian combat related post-traumatic stress disorder patients. Croatian Medical Journal. 2000;41:179–183. [PubMed] [Google Scholar]
Longden E., Madill A., Waterman M.G. Dissociation, trauma, and the role of lived experience: Toward a new conceptualization of voice hearing. Psychological Bulletin. 2012;138:28–76. [PubMed] [Google Scholar]
McCarthy-Jones S. Voices from the storm: A critical review of quantitative studies of auditory verbal hallucinations and childhood sexual abuse.![]() Clinical Psychology Review. 2011;31:983–992. doi: 10.1016/j.cpr.2011.05.004. [PubMed] [CrossRef] [Google Scholar]
Clinical Psychology Review. 2011;31:983–992. doi: 10.1016/j.cpr.2011.05.004. [PubMed] [CrossRef] [Google Scholar]
McCarthy-Jones S., Trauer T., Mackinnon A., Sims E., Thomas N., Copolov D. A new phenomenological survey of auditory hallucinations: Evidence for subtypes and implications for theory and practice. Schizophrenia Bulletin. 2014;40:231–235. [PMC free article] [PubMed] [Google Scholar]
Moskowitz A., Barker-Collo S., Ellson L. Replication of dissociation-psychoticism link in New Zealand students and inmates. The Journal of Nervous and Mental Disease. 2004;193:722–727. [PubMed] [Google Scholar]
Moskowitz A., Corstens D. Auditory hallucinations: Psychotic symptom or dissociative experience? Journal of Psychological Trauma. 2007;6:35–63. doi: 10.1300/J513v06n02_04. [CrossRef] [Google Scholar]
Offen L., Waller G., Thomas G. Is reported childhood sexual abuse associated with the psychopathological characteristics of patients who experience auditory hallucinations? Child Abuse & Neglect. 2003;27:919–927. doi: 10.1016/S0145-2134(03)00139-X. [PubMed] [CrossRef] [Google Scholar]
2003;27:919–927. doi: 10.1016/S0145-2134(03)00139-X. [PubMed] [CrossRef] [Google Scholar]
Pilton M., Varese F., Berry K., Bucci S. The relationship between dissociation and voices: A systematic literature review and meta-analysis. Clinical Psychology Review. 2015;40:138–155. [PubMed] [Google Scholar]
Read J., McGregor K., Coggan C., Thomas D.R. Mental health services and sexual abuse: The need for staff training. Journal of Trauma & Dissociation. 2006;7:33–50. [PubMed] [Google Scholar]
Read J., van Os J., Morrison A.P., Ross C.A. Childhood trauma, psychosis and schizophrenia: A literature review with theoretical and clinical implications. Acta Psychiatrica Scandinavica. 2005;112:330–350. [PubMed] [Google Scholar]
Seedat S., Stein M.B., Oosthuizen P.P., Emsley R.A., Stein D.J. Linking posttraumatic stress disorder and psychosis: A look at epidemiology, phenomenology, and treatment. The Journal of Nervous and Mental Disease. 2003;191:675–681. [PubMed] [Google Scholar]
Shergill S.![]() S., Murray R.M., McGuire P.K. Auditory hallucinations: A review of psychological treatments. Schizophrenia Research. 1998;32:137–150. [PubMed] [Google Scholar]
S., Murray R.M., McGuire P.K. Auditory hallucinations: A review of psychological treatments. Schizophrenia Research. 1998;32:137–150. [PubMed] [Google Scholar]
Slade P., Bentall R.P. 1988. Sensory deception: A scientific analysis of hallucination. (London: Croom Helm) [Google Scholar]
Smailes D., Alderson-Day B., Fernyhough C., McCarthy-Jones S., Dodgson G. Tailoring cognitive behavioural therapy to subtypes of voice-hearing. Frontiers in Psychology. 2015;6:1933. [PMC free article] [PubMed] [Google Scholar]
Stanghellini G., Cutting J. Auditory verbal hallucinations — breaking the silence of inner dialogue. Psychopathology. 2003;36:120–128. [PubMed] [Google Scholar]
Steel C. Hallucinations as a trauma based memory: Implications for psychological interventions. Frontiers in Psychology. 2015;6:1262. doi: 10.3389/fpsyg.2015.01262. ISSN 16641078. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Thomas N., Hayward M., Peters E., van der Gaag M., Bentall R.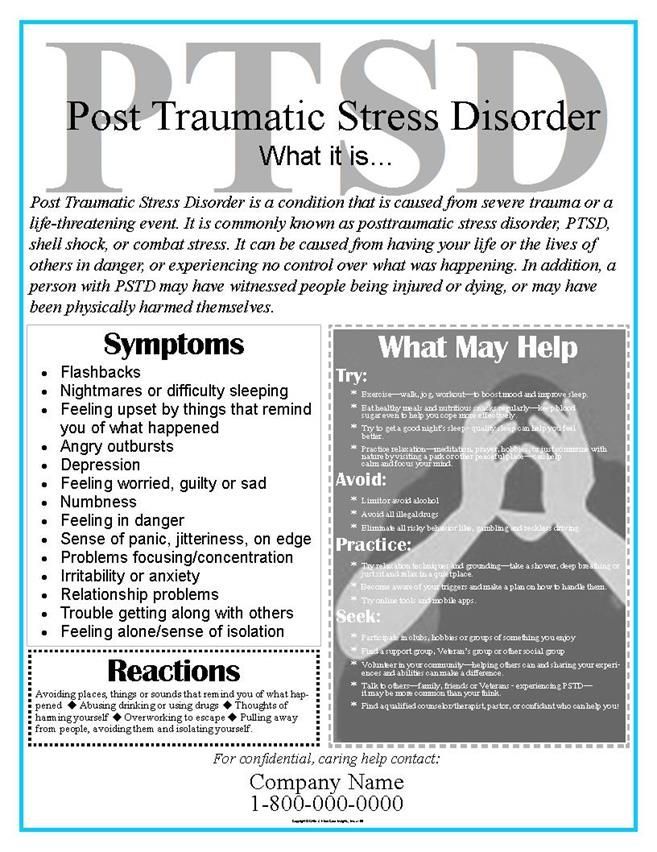 P., Jenner J. Psychological therapies for auditory hallucinations (voices): Current status and key directions for future research. Schizophrenia Bulletin. 2014;40:202–212. [PMC free article] [PubMed] [Google Scholar]
P., Jenner J. Psychological therapies for auditory hallucinations (voices): Current status and key directions for future research. Schizophrenia Bulletin. 2014;40:202–212. [PMC free article] [PubMed] [Google Scholar]
Waller N.G., Putnam F.W., Carlson E.B. Types of dissociation and dissociative types: A taxometric analysis of dissociative experiences. Psychological Methods. 1996;1:300–321. doi: 10.1037/1082-989X.1.3.300. [CrossRef] [Google Scholar]
Wearne D., Genetti A. Pseudohallucinations versus hallucinations: Wherein lies the difference? Australasian Psychiatry. 2015;23(3):254–257. doi: 10.1177/1039856215586150. [PubMed] [CrossRef] [Google Scholar]
Wearne D., Curtis G.J., Genetti A., Samuel M., Sebastian J. Where pseudo- hallucinations meet dissociation: A cluster analysis. Australasian Psychiatry. 2017;4:364–368. [PubMed] [Google Scholar]
Treatment of voices in the head in St. Petersburg
- Main
- Psychiatry
- Treatment of hallucinations
- Voices in the head
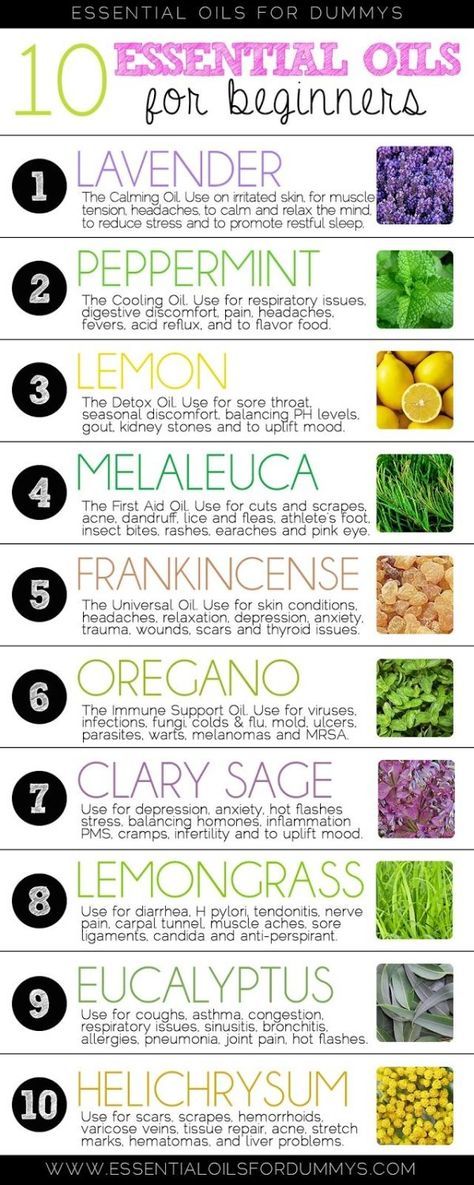
Voices in the head (R44.0 according to ICD-10) can be a symptom of various mental and somatic diseases. At the same time, about 10% of healthy people around the world from time to time may encounter this deception of auditory perception, caused, for example, by severe overwork or external mechanical noise. nine0013
Voices in the head can be caused not only by severe mental illness or organic damage to the brain. Auditory perception deceptions often occur against the background of severe stress, neurotic disorders, alcohol abuse or improper medication.
If the voices in your head appear regularly and cause discomfort, you should make an appointment with a psychiatrist. The doctor will listen to complaints, conduct an examination and, depending on the result of the preliminary examination, prescribe medication for the voices in the head or refer you for additional diagnostics in order to clarify the cause. nine0013
Treatment of voices in the head in our clinic is carried out by psychiatrists with extensive clinical experience. If criticism of one's own condition persists, outpatient treatment may be prescribed; in other cases, when the voices in the head are unconditionally commanding and threatening, it is necessary to undergo treatment in the hospital.
Doctor's consultation on the treatment of voices in the head:
+7 (812) 407-18-00
Thank you for your trust!
- Anonymous consultation with a psychiatrist
- Prevention of relapses
- Accurate diagnosis of the causes of hallucinations
| Service | Price | |
|---|---|---|
| Psychiatric appointment nine0049 | 5 000 ₽ | |
| Psychotherapist appointment | 5 000 ₽ | nine0045|
| Hypnotherapy | 8 000 ₽ | |
| Calling a doctor at home | 6 000 ₽ | |
| Treatment in a hospital | 8 Hallucinations - https://www. Update date: 08/26/2022
Make an appointment Date and time: (not set) Make an appointment with a psychiatrist Make an appointment with a psychiatrist Select the date and time of reception Tomorrow January 15 Monday January 16 Tuesday January 17 Wednesday January 18 Thursday January 19 Friday January 20 Saturday January 21 Sunday January 22 Monday January 23 Tuesday January 24 Wednesday January 25 Thursday January 26 Friday January 27 Saturday January 28 Sunday January 29 Monday January 30 Tuesday 31 January The voices in the head are being treated Bocharov Alexey Psychiatrist, psychotherapist Psychiatrist, psychotherapist, sexologist, child psychiatrist Work experience 42 years Sinenchenko Andrey Psychiatrist, psychotherapist Psychiatrist, psychotherapist, narcologist Work experience 23 years Zun Sergey Psychiatrist, narcologist Psychiatrist, narcologist, psychotherapist Work experience 34 years Lisitsyna Elena Psychiatrist Psychiatrist Work experience 34 years nine0012 Buchelnikova VictoriaViktorovna Psychiatrist Psychiatrist Work experience 16 years Voronina Elvira Psychiatrist Psychiatrist Work experience 28 years Efimova Evgenia Second category Work experience 20 years Psychiatrist Experience 20 years Gorobets Elena Psychiatrist Psychiatrist Work experience 17 years Travnikova Oksana Psychiatrist Psychiatrist Work experience 22 years Kurochkina Nadezhda Psychiatrist Psychiatrist Work experience 20 years Suslennikova Elena Psychiatrist, psychotherapist Psychiatrist, psychotherapist Work experience 26 years nine0012 Chuban OlgaIvanovna Psychiatrist, psychotherapist Psychiatrist, psychotherapist, psychologist Work experience 14 years Popov Andrey Psychiatrist Psychiatrist Work experience 36 years Stetsiv Lyudmila Psychiatrist, psychotherapist Psychiatrist, psychotherapist Work experience 32 years Prokhorchev Konstantin Psychiatrist, psychotherapist Psychiatrist, psychotherapist Work experience 13 years Gulevsky Roman Psychiatrist, narcologist Psychiatrist, narcologist Work experience 26 years Konoplin Dmitry Narcologist, psychiatrist Narcologist, psychiatrist Work experience 25 years Stavitskaya Svetlana Psychiatrist Psychiatrist Work experience 25 years Pylskaya Anna Psychiatrist Psychiatrist Work experience 8 years nine0012 Trofimova AlexandraOlegovna Psychiatrist, child psychiatrist Psychiatrist, child psychiatrist Work experience 29 years Zholobetskaya Maria Psychiatrist, psychotherapist Psychiatrist, psychotherapist Work experience 23 years Endrzheevskaya Diana Psychiatrist, psychotherapist Psychiatrist, child psychiatrist, psychotherapist Work experience 15 years Usov Grigory MD Work experience 25 years Psychiatrist, psychotherapist Work experience 25 years Ivanov Alexander Psychiatrist, narcologist Psychiatrist, narcologist Work experience 21 years Semenov Andrey Psychiatrist, narcologist Psychiatrist, narcologist, transfusiologist Work experience 24 years Leave a request for a call: +7 (812) 407-18-00 "A very powerful feeling of guilt for having survived. " What to do with PTSD " What to do with PTSD © Illustration by Diana Dnepr 25 Oct 2022, 13:00 nine0013 Three out of four combatants on the front lines of the Vietnam War developed post-traumatic stress disorder (PTSD). Now Russian society is threatened by the return to civilian life of tens of thousands of injured people. What this can lead to and what to do with their loved ones, psychologist Evgenia Dashkova told Taiga.info.Taiga.info: What is PTSD, how does it manifest itself? - Post-traumatic stress disorder - now this is the official name, but in Russian it is more often called "trauma". In short: PTSD (post-traumatic stress disorder) is the consequences of a traumatic event on the psyche. nine0013 The key to PTSD is that the person experiences or witnesses an extremely traumatic or extremely powerful negative event. Usually with a threat to life, health, for himself, or he can watch how a threat to the life of his loved ones or other people in general appears. The second side of PTSD is the consequences for the psyche. The psyche, under the influence of a traumatic event, does not withstand, and, by and large, it collapses, all aspects of its functioning are violated. On the one hand, without trauma, without a traumatic event, there can be no PTSD. It may be that there is a traumatic event, but PTSD did not happen. That is, there must also be an impact on the psyche. What is it? There are three main consequences for the psyche. The first is the so-called intrusion. As if the psyche experiences this [event] again and again and again. These are memories of what happened. When people say that it is "as if standing in front of their eyes. The second is the opposite tendency, avoidance. A person tries with all his might not to feel it, not to think about it, somehow distract himself. Then avoid anything that contains memories. Since this is also reminded by one's own feelings, one's own experiences, a person begins to move away from experiences. He tries not to feel fear, not to feel affection. Because, for example, you lost someone you loved, and then attachment reminds you of that pain. The third is overstimulation. The nervous system becomes overexcited at the moments of a traumatic event, especially if there were several of them or if it is a childhood trauma. At the moment of a threat to life, the nervous system is excited to make efforts to somehow cope with this, but nothing happens. Taiga.info: What does this mean? - Firstly, very strong sensitivity to everything, great anxiety. Especially in women who have experienced mistreatment, the nervous system is constantly looking for threats everywhere, you are constantly on your guard. You are constantly "cutting the clearing". In children who have experienced violence, this usually manifests itself in the fact that all adults around can be dangerous. In people who were prone to aggression before the injury, this manifests itself in outbursts of anger - they can be beaten for any reason, explode, flare up, throw things, anything. It's almost always a bad dream. Because the nervous system almost never calms down. Nightmares, some kind of tremors, jumps, and due to constant overexcitation, the body literally cannot stop, and in order to start resting and recovering, you need to calm down, but the nervous system cannot do this. |
 webmd.com
webmd.com  department
department  This very event is key. It may be an accident, some kind of natural disaster, but this is not as scary for the people themselves as the events that people themselves commit. The most traumatic events are what people do to other people. These are any manifestations of violence, rape, murder. nine0013
This very event is key. It may be an accident, some kind of natural disaster, but this is not as scary for the people themselves as the events that people themselves commit. The most traumatic events are what people do to other people. These are any manifestations of violence, rape, murder. nine0013 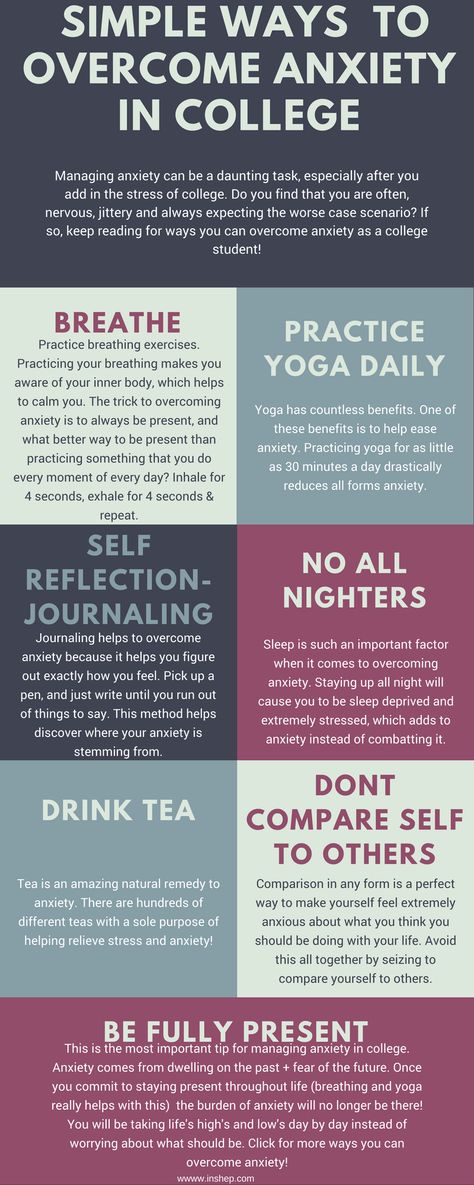 " What is called "flashbacks", it can be in the form of dreams, nightmares, some causeless feelings of fear. A person may not see it, not remember it, but you are in a panic for no reason. For no reason, horrified. All of a sudden, blood pressure starts to scale, literally a hypertensive crisis. It can also be memories at the level of words. When you hear any words, voices. This happens especially strongly in the first months, hours, years after a traumatic event. This is such a groundhog day, only the most terrible in life. nine0013
" What is called "flashbacks", it can be in the form of dreams, nightmares, some causeless feelings of fear. A person may not see it, not remember it, but you are in a panic for no reason. For no reason, horrified. All of a sudden, blood pressure starts to scale, literally a hypertensive crisis. It can also be memories at the level of words. When you hear any words, voices. This happens especially strongly in the first months, hours, years after a traumatic event. This is such a groundhog day, only the most terrible in life. nine0013  And the person avoids. He can avoid it in different ways. Purely behavioral - don't go somewhere, don't do something, and so on, don't talk about it. You can hear from so many people that grandfathers and great-grandfathers never talked about military operations. They were silent, remained silent, left, did not speak. This is the most typical everyday case of avoidance. Among those people who have experienced violence in everyday life - this is manifested in the refusal to speak, the refusal to even remember about this [traumatic event]. Through silence, a person tries to get rid of this, and there can be a variety of ways to avoid it - alcohol, drugs, sticking to social networks, extreme sports. nine0013
And the person avoids. He can avoid it in different ways. Purely behavioral - don't go somewhere, don't do something, and so on, don't talk about it. You can hear from so many people that grandfathers and great-grandfathers never talked about military operations. They were silent, remained silent, left, did not speak. This is the most typical everyday case of avoidance. Among those people who have experienced violence in everyday life - this is manifested in the refusal to speak, the refusal to even remember about this [traumatic event]. Through silence, a person tries to get rid of this, and there can be a variety of ways to avoid it - alcohol, drugs, sticking to social networks, extreme sports. nine0013  A person still remains in trouble, still remains in a situation of threat. And this state of overexcitation does not end. A person in trauma seems to be in that overexcitation all the time that never ends. nine0013
A person still remains in trouble, still remains in a situation of threat. And this state of overexcitation does not end. A person in trauma seems to be in that overexcitation all the time that never ends. nine0013 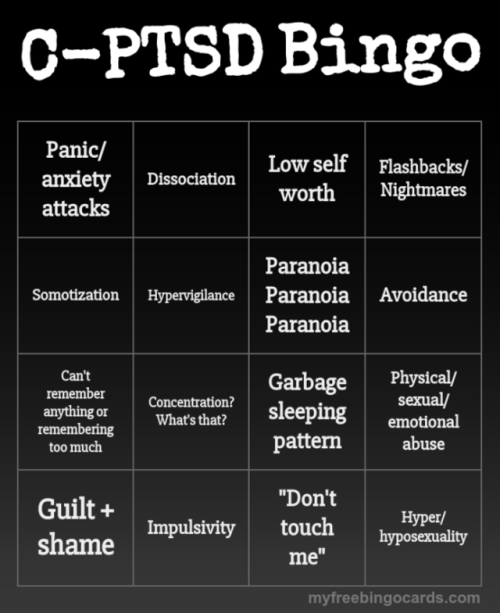 A person becomes one who is constantly in a situation of danger. nine0514
A person becomes one who is constantly in a situation of danger. nine0514  " Usually it is a very powerful feeling of guilt for having survived. Or it is a feeling of shame because you allowed something to be done to you. Faith in people is completely destroyed, in general, faith in humanity in such a global world. And faith in God, in some higher powers, in the fact that the world is worthy to live in it, to give birth to children. It's all just falling apart. We get the ruins of personality and a completely destroyed nervous system. nine0013
" Usually it is a very powerful feeling of guilt for having survived. Or it is a feeling of shame because you allowed something to be done to you. Faith in people is completely destroyed, in general, faith in humanity in such a global world. And faith in God, in some higher powers, in the fact that the world is worthy to live in it, to give birth to children. It's all just falling apart. We get the ruins of personality and a completely destroyed nervous system. nine0013  But it can also be adaptive if you find yourself in volunteering, activism, helping others. And this helps to bring meaning to life and bring faith in people to life. nine0013
But it can also be adaptive if you find yourself in volunteering, activism, helping others. And this helps to bring meaning to life and bring faith in people to life. nine0013  nine0013
nine0013 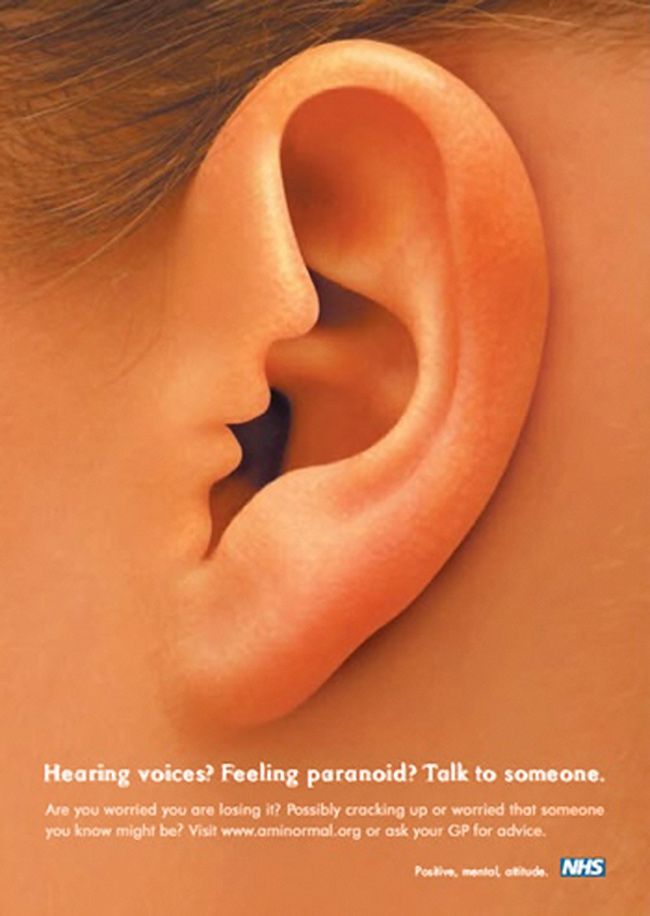 Here among them, in my opinion, only about 9% of PTSD. That is, the key is the events themselves, how dangerous, painful they were, where you were. nine0013
Here among them, in my opinion, only about 9% of PTSD. That is, the key is the events themselves, how dangerous, painful they were, where you were. nine0013 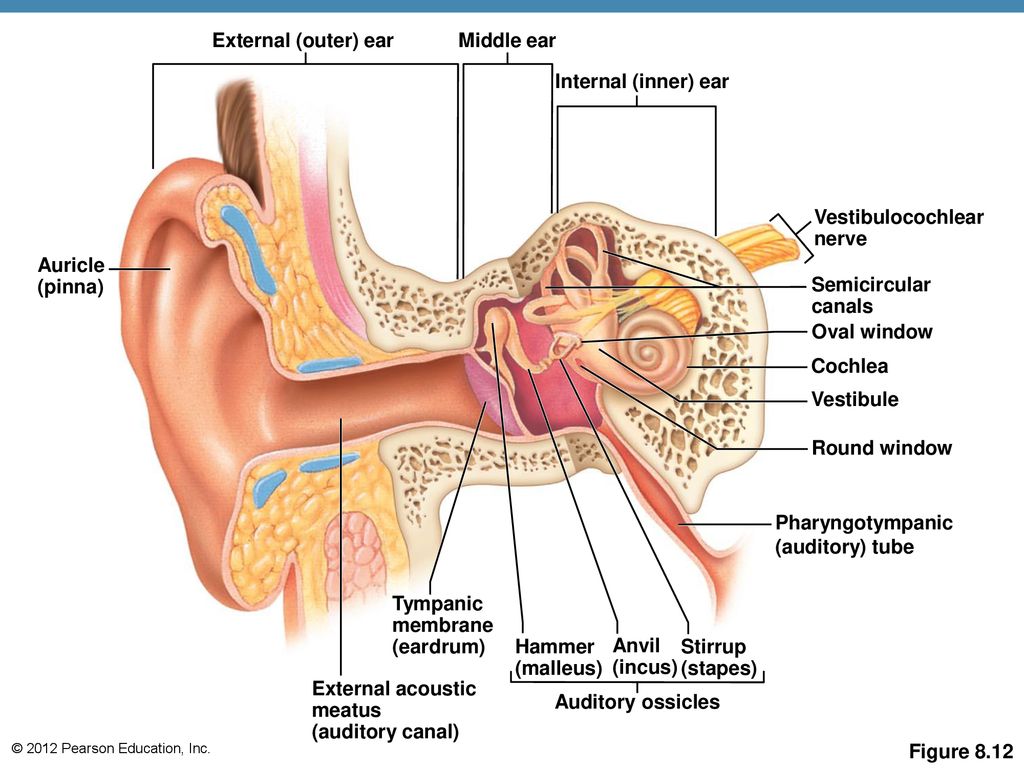 The data from there is as follows: if a soldier stayed on the front line for 200 days, not a single one left unbroken. There are conditions that no one can stand.
The data from there is as follows: if a soldier stayed on the front line for 200 days, not a single one left unbroken. There are conditions that no one can stand.  Accordingly, at the level of the body, it has not been so strongly imprinted, so it will be easier to work with it. More prone to vicarious trauma are journalists, the same volunteers, activists, psychologists, all those who often see violence. The simplest thing in the prevention of vicarious trauma is to minimize the similarity of the picture to real life. Mute the sound, if possible, turn the screen to black and white. If possible, do not watch the video, but read the texts. Make the situation as unlike reality as possible. nine0013
Accordingly, at the level of the body, it has not been so strongly imprinted, so it will be easier to work with it. More prone to vicarious trauma are journalists, the same volunteers, activists, psychologists, all those who often see violence. The simplest thing in the prevention of vicarious trauma is to minimize the similarity of the picture to real life. Mute the sound, if possible, turn the screen to black and white. If possible, do not watch the video, but read the texts. Make the situation as unlike reality as possible. nine0013 
 Secondly, it is to secure yourself financially, if your husband came and he has depression or hard drinking, you will have to somehow get out. After all, close people with PTSD have little strength, everything is bad, there are many difficulties in life, and if we throw all our strength into helping another person, we ourselves can remain stranded after a while. Therefore, the first thing is to protect yourself by any means. nine0013
Secondly, it is to secure yourself financially, if your husband came and he has depression or hard drinking, you will have to somehow get out. After all, close people with PTSD have little strength, everything is bad, there are many difficulties in life, and if we throw all our strength into helping another person, we ourselves can remain stranded after a while. Therefore, the first thing is to protect yourself by any means. nine0013  nine0013
nine0013  During nightmares, during falling into a stupor, you need to constantly repeat "you are safe, I am with you, everything is fine." Tactility helps. Touch this blanket, touch this, bring any warm drink. Let him not even drink, just give it to his hands. You know, like in American films - they cover the victims of some disasters with a blanket, they cover with a blanket with a head and something warm in their hands - this gives a feeling of security. This can be done at home, it helps a person to see that he has returned from the places of violence, from the street where she was caught and raped, that the person is no longer at home with the father who beat him, that he is safe here and now. nine0013
During nightmares, during falling into a stupor, you need to constantly repeat "you are safe, I am with you, everything is fine." Tactility helps. Touch this blanket, touch this, bring any warm drink. Let him not even drink, just give it to his hands. You know, like in American films - they cover the victims of some disasters with a blanket, they cover with a blanket with a head and something warm in their hands - this gives a feeling of security. This can be done at home, it helps a person to see that he has returned from the places of violence, from the street where she was caught and raped, that the person is no longer at home with the father who beat him, that he is safe here and now. nine0013  To summarize: the first is to take care of yourself, the second is to ensure the safety of the person, help him understand that he is safe, the third is the psychiatrist.
To summarize: the first is to take care of yourself, the second is to ensure the safety of the person, help him understand that he is safe, the third is the psychiatrist. 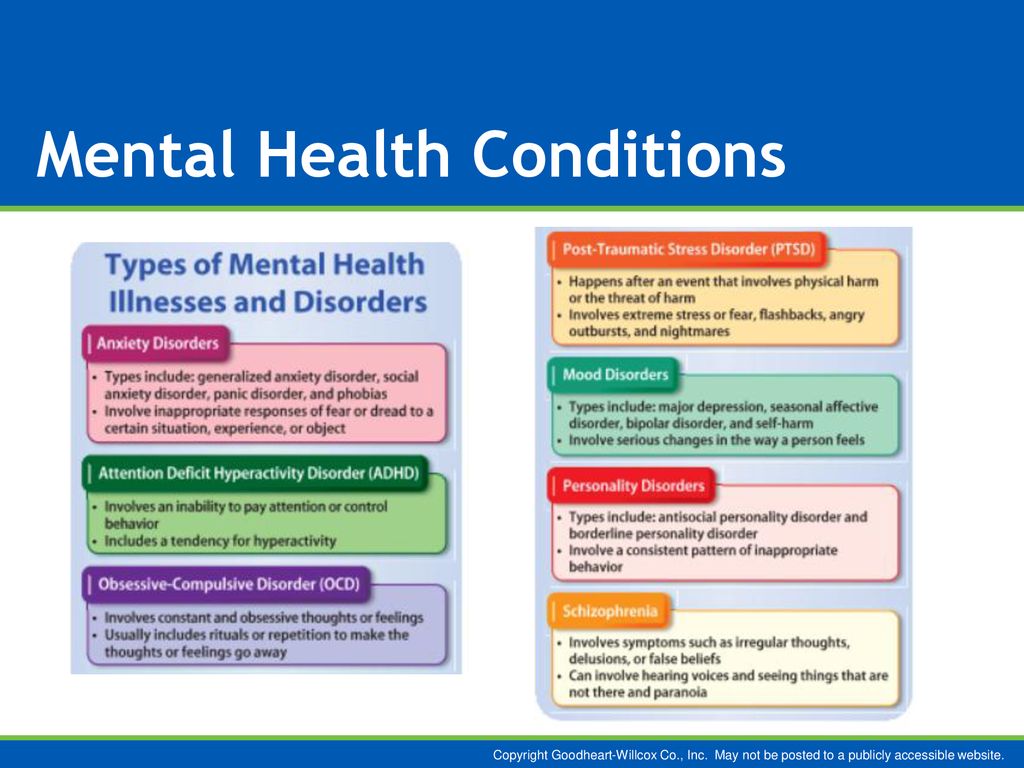 Yes, they will be completely different.
Yes, they will be completely different.  Why help with something that is already good.
Why help with something that is already good. 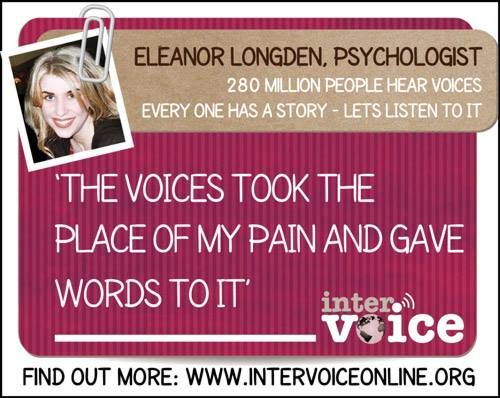 To serve in the army now, many go just from lack of money in order to somehow earn money on the contract. Therefore, I think that this is a completely lost situation. I think that people who have returned now will just drink too much. There are two options. If a person before the injury had a tendency to illegal behavior, then these will be outbursts of aggression and trauma to everyone around him. If a person, let's say, of high moral qualities, then it will most likely be depression, some kind of quiet alcoholism and a lot of suicide attempts. nine0013
To serve in the army now, many go just from lack of money in order to somehow earn money on the contract. Therefore, I think that this is a completely lost situation. I think that people who have returned now will just drink too much. There are two options. If a person before the injury had a tendency to illegal behavior, then these will be outbursts of aggression and trauma to everyone around him. If a person, let's say, of high moral qualities, then it will most likely be depression, some kind of quiet alcoholism and a lot of suicide attempts. nine0013