Heal schizophrenia naturally
8 Natural Treatments for Schizophrenia — Talkspace
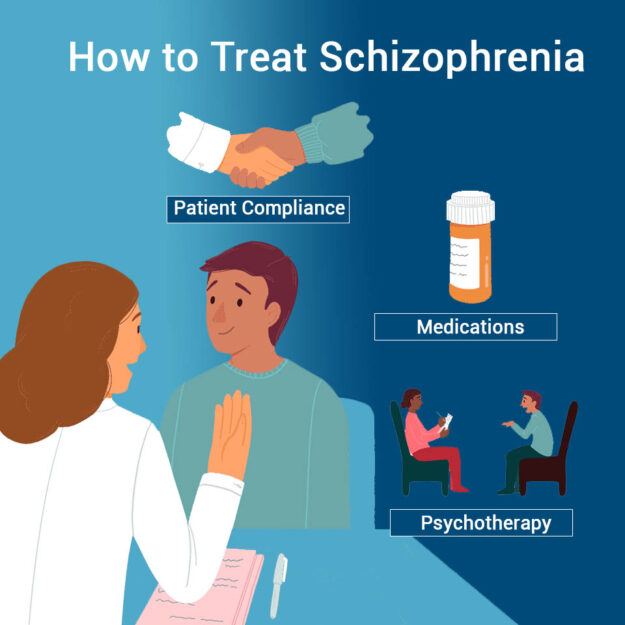
Medications like antipsychotics and therapy for schizophrenia are traditional treatment options for people living with schizophrenia. However, for about one-third of those diagnosed with it, schizophrenia is actually treatment-resistant. There is some good news, though. Several complementary natural ways to help manage symptoms of schizophrenia have been found helpful for many people.
Learn about additional, alternative methods that can help you deal with schizophrenia.
If you’re looking for a treatment for schizophrenia without medication, it’s important to note that prescribed medication is typically recommended. With that said, we’ve outlined how to combat schizophrenia naturally through several therapist-approved complementary methods. Each has proven effective or shown promise in one or more studies.
Please be aware: These holistic methods may not work the same way or be as effective as some more conventional methods of treatment. You should discuss any natural treatment you decide to try with your doctor or healthcare team. Sometimes natural methods can be most effective when coupled with more traditional forms of psychological treatment, like when used in combination with schizophrenia medication and/or talk therapy.
1. Vitamin B Supplements
One promising complementary natural treatment for schizophrenia involves the use of vitamin B supplements. Some research suggests that high doses of vitamin B might help to ease symptoms of different types of schizophrenia.
A 2017 study from the University of Manchester (UK), and other research, found that B vitamins might offer hope. The research shows that high doses of vitamins B6, B8, and B12, when taken with other forms of treatment, significantly reduced schizophrenia symptoms more than just using traditional methods alone did.
It’s important to note that this study combined the use of B vitamins with more traditional treatment methods.
“Vitamin supplements, CBD, and a low carb diet can help reduce the symptoms of schizophrenia. If these are used in conjunction with talk therapy and prescribed medications, the results are even better.”
Talkspace therapist Cynthia V. Catchings, LCSW-S
2. Diet
A variety of foods have been found to potentially decrease symptoms of several mental health conditions, including schizophrenia. In particular, an anti-inflammatory diet is believed to be extremely effective and valuable in reducing symptoms of schizophrenia.
This type of diet focuses on adding an abundance of fruits, vegetables, and whole grains while reducing consumption of dairy, red meat, and animal fats.
A 2020 study by researchers at the Department of Food and Nutrition, Seoul Women’s University in Korea, found that anti-inflammatory agents have the potential to help improve symptom severity of schizophrenia, while also working to decrease some of the risks that trigger the onset of episodes.
“A healthy diet rich in fruits, vegetables, and vitamin B is recommended to ease the symptoms, but cannot substitute your medication and therapy.”
Talkspace therapist Cynthia V. Catchings, LCSW-S
3. Deep Brain Stimulation
Deep brain stimulation (DBS) is yet another promising treatment for schizophrenia without medication. This procedure requires surgery to implant electrodes within your brain. These electrodes produce electric stimulation to areas in your brain to provide treatment. According to Johns Hopkins Medicine researchers, the treatment targets a specific region in the brain that’s known to be involved in the control of executive functions, learning, behaviors, and emotions. In even more promising news, it’s possible that DBS might work to alleviate symptoms that have otherwise been resistant to treatment.
4. CBD
One more potentially effective schizophrenia natural treatment is cannabidiol (CBD). While the prescription version of CBD is only approved by the FDA for a rare seizure disorder, some physicians have started recommending CBD off-label to help with schizophrenia symptoms (in states where CBD is legal).
Schizophrenia research done in 2011 by doctors at University Medical Centre Utrecht, Department of Psychiatry, The Netherlands, concluded that “high cannabidiol content cannabis was associated with significantly lower degrees of psychotic symptoms providing further support for the antipsychotic potential of cannabidiol.”
While this might offer hope for the use of CBD to treat schizophrenia psychosis, it’s also important to note that cannabis with a high THC content is associated with increased psychotic symptoms in some people. Much more research is needed before we can conclude how the relationship between CBD, THC, and schizophrenia truly works, and whether or not CBD is, in fact, a truly effective antipsychotic drug.
5. Antioxidants
Over time, schizophrenia can cause brain structure to change. In an effect known as oxidative stress, environmental chemicals can damage cells, but some antioxidants — like vitamin E, glutathione, and N-acetyl cysteine — might be helpful in treating symptoms of schizophrenia. These and other antioxidants are known to protect cells, and they also might help speed up response to other treatments and improve early intervention outcomes.
These and other antioxidants are known to protect cells, and they also might help speed up response to other treatments and improve early intervention outcomes.
While the evidence isn’t totally clear and more schizophrenia research must be done, preliminary studies do suggest that antioxidants, particularly when used in combination with medication, might be beneficial in treating positive symptoms of schizophrenia.
6. Amino Acids
If you’re wondering how to combat schizophrenia naturally, you might want to consider looking into amino acids like taurine. Science suggests that there’s likely some correlation between levels of certain amino acids in the brain and schizophrenia, but researchers remain unclear about the exact nature of this relationship. Our understanding will likely change in the future as more is learned about how amino acids interact with the brain.
For now, some research shows that people with schizophrenia who take taurine daily have benefited from improved symptoms in depression, psychosis, and occupational and social functioning.
7. Omega-3 Fatty Acids
Omega-3 fatty acids are another potential schizophrenia natural treatment. These essential fats, which the body can’t make on its own, are found in foods like salmon, sardines, and mackerel.
A 2020 study by researchers at I-Shou University in Taiwan found that Omega-3 fatty acid supplements can be effective at reducing the conversion rate to psychosis in adolescents with schizophrenia. The study also shows that Omega-3s might reduce the severity and improve positive symptoms and global functions in adolescents who have an ultra-high risk for psychosis.
8. Melatonin
Melatonin shows promise as a potentially effective treatment for schizophrenia. It’s a naturally occurring hormone that, among other things, helps to regulate sleep patterns. While sleep disturbances aren’t technically part of the criteria for a schizophrenia diagnosis, they are a consistently reported symptom in people diagnosed with the condition.
Researchers have found in some studies that the use of melatonin on a short-term basis might be effective for some people who experience sleep disturbance-related schizophrenia.
When to Seek Schizophrenia Treatment
“People displaying schizophrenia symptoms must seek treatment as soon as they start experiencing them; early detection can reduce the severity. The sooner you look for help, the better results you may have in reducing symptoms. Delaying treatment increases your risk of brain volume loss.”
Talkspace therapist Cynthia V. Catchings, LCSW-S
According to a study by Duke University Medical Center in North Carolina, untreated schizophrenia, or untimely psychological treatment for schizophrenia can result in a higher risk of adverse outcomes and brain volume loss. For most people with schizophrenia, the best schizophrenia treatment option combines both clinical and natural treatments.
When seeking clinical treatments, online therapy can help, and that’s where Talkspace comes in. Talkspace allows you to connect with a licensed therapist from the palm of your hand, and experience the most convenient, affordable way to improve your mental health.
Talkspace allows you to connect with a licensed therapist from the palm of your hand, and experience the most convenient, affordable way to improve your mental health.
See references
- Taylor & Francis. 2022. Treatment-Resistant Schizophrenia – The Role of Clozapine.
- B vitamins reduce schizophrenia symptoms, study finds.
- Firth J, Stubbs B, Sarris J et al. The effects of vitamin and mineral supplementation on symptoms of schizophrenia: a systematic review and meta-analysis.
- Cha H, Yang S. Anti-Inflammatory Diets and Schizophrenia.
- Cascella N, Butala A, Mills K et al. Deep Brain Stimulation of the Substantia Nigra Pars Reticulata for Treatment-Resistant Schizophrenia:
- Schubart C, Sommer I, van Gastel W, Goetgebuer R, Kahn R, Boks M. Cannabis with high cannabidiol content is associated with fewer psychotic experiences.

- Tharoor H, Mara S, Gopal S. Role of Novel Dietary Supplement N-acetyl Cysteine in Treating Negative Symptoms in Schizophrenia:
- De Luca V, Viggiano E, Messina G et al. Peripheral Amino Acid Levels in Schizophrenia and Antipsychotic Treatment.
- O’Donnell C, Allott K, Murphy B et al. Adjunctive Taurine in First-Episode Psychosis. J Clin Psychiatry. 2016;77(12):e1610-e1617.
- Hsu M, Huang Y, Ouyang W. Beneficial effects of omega-3 fatty acid supplementation in schizophrenia: possible mechanisms.
- Kaskie R, Graziano B, Ferrarelli F. Schizophrenia and sleep disorders: links, risks, and management challenges.
- Kumar P, Andrade C, Bhakta S, Singh N. Melatonin in Schizophrenic Outpatients With Insomnia.
- McEvoy J. The importance of early treatment of schizophrenia.
Alternative Treatments for Schizophrenia
Schizophrenia is a lifelong mental health condition that affects the way a person may see or perceive the world around them.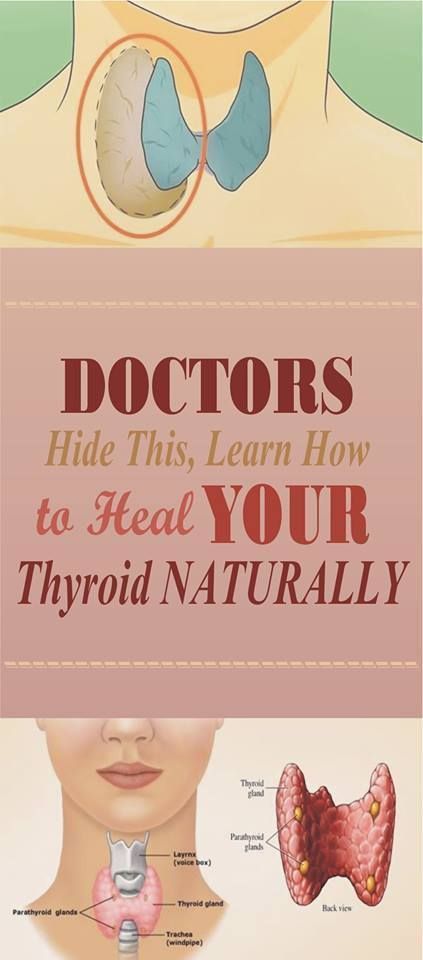 It requires treatment from a licensed healthcare professional, which usually combines medication and therapy.
It requires treatment from a licensed healthcare professional, which usually combines medication and therapy.
It’s estimated that 0.25 and 0.64 percent of people in the United States live with schizophrenia.
If you have this condition, it’s important that you follow your doctor’s order for treatment and use complementary treatments only in addition to prescribed treatment.
Schizophrenia is a chronic brain disorder. It can cause many symptoms, including:
- hallucinations
- paranoia
- breaking from reality
- flat affect, or a reduced ability to express emotions
Treatment usually includes antipsychotic medications. It may also include:
- group or individual therapy
- psychoeducation
- rehabilitation
Complementary and alternative medicine (CAM) treatments are another option that people like to explore.
The terms “complementary” and “alternative” are often used interchangeably. But these words actually describe two different types of treatment.
The term “complementary” refers to nonmainstream treatments used along with conventional treatments. The term “alternative” refers to situations when nonmainstream approaches are used instead of conventional treatments.
Keep in mind
Medication is important in managing schizophrenia. CAM treatments should not replace the care of a doctor or prescribed medication. They should only be used in addition to traditional treatment.
Talk with your doctor before using any CAM treatment to see whether it’s safe for you. They can also help come up with a CAM treatment that fits your specific needs.
Vitamin treatment
A 2014 research review notes that B vitamins, including vitamins B12 and B6, may be helpful in treating schizophrenia. Several studies have used a combination of these vitamins.
The researchers also looked at a few small studies suggesting that vitamins C and E may be beneficial. But the review concluded that more research is needed.
Some studies in this review have linked vitamin D deficiency, especially early in life, with schizophrenia. It isn’t clear whether people who have already received a schizophrenia diagnosis would benefit from taking the vitamin.
It isn’t clear whether people who have already received a schizophrenia diagnosis would benefit from taking the vitamin.
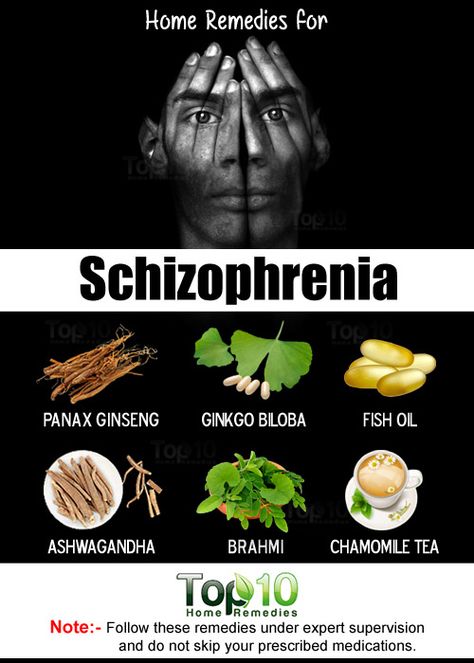
Fish oil supplements
Fish oil is a rich source of omega-3 fatty acids. These nutrients are known to reduce inflammation in your body. Inflammation may play a role in many mental health conditions, including schizophrenia.
In a 2015 study involving 81 young people at high risk of schizophrenia, those who took fish oil supplements were less likely to develop the condition. The results are promising, but more research is needed.
It isn’t clear whether fish oil supplements improve symptoms in people who have already received a schizophrenia diagnosis. But there may be other benefits, such as improved heart health.
For example, 2009 research notes that people with schizophrenia are at higher risk of metabolic syndrome. This, in turn, increases the risk of heart disease. So, some people with schizophrenia may decide to try omega-3 fatty acids for the heart health benefits alone.
Diet management
Research from 2019 on ketogenic diets has also shown promising results in treating schizophrenia.
A ketogenic diet is a high fat, low carbohydrate diet that also includes high protein foods. But diet changes do not always make a difference for people with schizophrenia.
More research is needed to determine whether there’s a relationship between diet and schizophrenia.
Always talk with your doctor before making major changes to your diet. A diet change should not be used to replace medication.
Relaxation and stress management
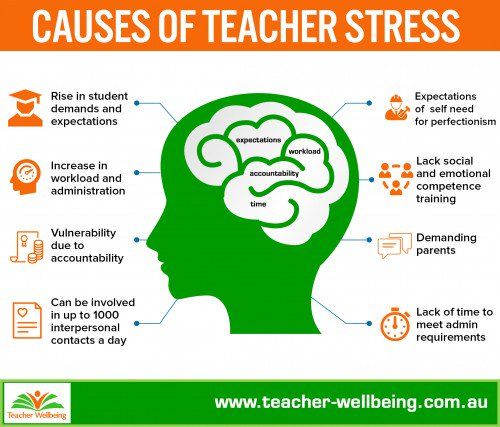
Most people experience stress. However, if you have schizophrenia, stress can increase symptoms of hallucinations and delusions, according to the National Alliance on Mental Illness.
Some ways to reduce stress include making lifestyle changes, such as:
- recognizing stress triggers
- creating a daily schedule or routine
- exercising
- meditating
- doing breathing exercises
- practicing yoga
- eating a balanced diet
- engaging in therapy
- avoiding drugs and alcohol
- following a sleeping schedule
Be sure to talk with your doctor before making any significant lifestyle changes. They will be able to help you come up with a treatment plan that works for you.
They will be able to help you come up with a treatment plan that works for you.
CBD
CBD is a newer alternative treatment for schizophrenia. Not only is there limited research on its effectiveness, but the research is also conflicting.
One small 2021 study showed that CBD may help improve cognitive function with low side effects. However, a 2021 review does not support CBD use in treating schizophrenia.
Always check with your doctor before using CBD products, especially if you take medication for your schizophrenia. CBD can interfere with some medications.
Melatonin
Melatonin is a hormone that is naturally present in your body. According to a 2012 research review, if you have schizophrenia, your melatonin levels might be lower.
This may cause side effects such as dyskinesia (when your body moves without your control) or insomnia. Taking melatonin supplements may help treat some of these symptoms.
Make sure you talk with your doctor before taking any melatonin supplements. Melatonin supplements should not be used in place of conventional schizophrenia medication.
Melatonin supplements should not be used in place of conventional schizophrenia medication.
If you have schizophrenia, CAM treatments may be an option for you. But it’s important to speak with your doctor before trying any new treatments.
Vitamins and natural supplements can interfere with some medications. Some alternative treatments are not based on solid evidence. They may also be dangerous.
Be sure to ask your doctor about the safety of any new treatment you are considering.
Schizophrenia
Schizophrenia- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find Country »
- A
- B
- C
- D
- E
- e
- ё 9000
- x
- C
- h
- Sh
9000 WHO in countries » - Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Schizophrenia
Key Facts
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.
- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations.
- Globally, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective care options for patients with schizophrenia that can lead to a complete recovery of at least one in three patients.
Symptoms
Schizophrenia is characterized by significant disturbances in perception of reality and behavioral changes such as:
- persistent delusions: the patient has a persistent belief in the truth of certain things, despite evidence to the contrary;
- persistent hallucinations: the patient hears, sees, touches non-existent things and smells non-existent smells;
- sensation of external influence, control or passivity: the presence in the patient of the sensation that his feelings, impulses, actions or thoughts are dictated from outside, put in or disappear from consciousness by someone else's will, or that his thoughts are broadcast to others;
- disorganized thinking, often expressed in incoherent or pointless speech;
- Significant disorganization of behavior, which manifests itself, for example, in the performance by the patient of actions that may seem strange or meaningless, or in an unpredictable or inappropriate emotional reaction that does not give the patient the opportunity to organization of their behavior;
- "negative symptoms" such as extreme poverty of speech, smoothness of emotional reactions, inability to feel interest or pleasure, social autism; and/or
- Extreme agitation or, on the contrary, slowness of movements, freezing in unusual postures.

People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms.
Scope and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease.
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
Individuals with schizophrenia are 2-3 times more likely to die early than the population average (2). It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment.
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, lead to isolation and disruption of health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective treatment for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia.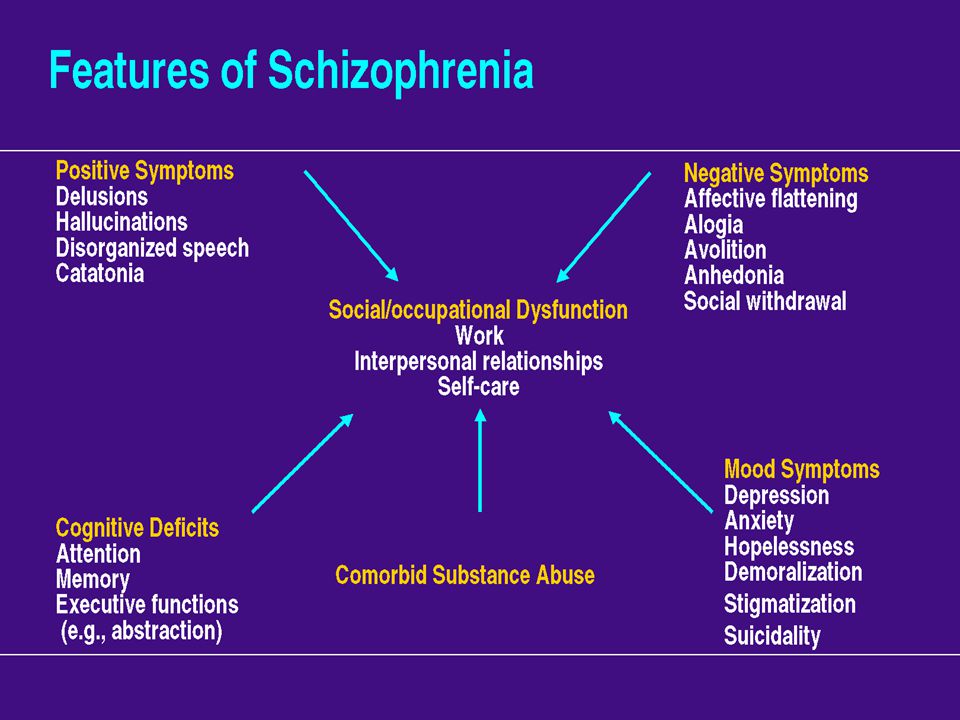 Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities.
Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities.
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg life skills education). The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
WHO activities
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care.
The WHO Mental Health Gap Action Program (mhGAP) is working to develop evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings. The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities.
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J.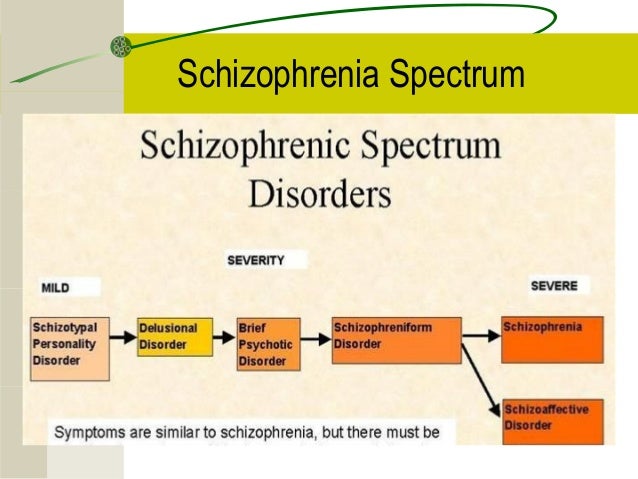 Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
(2) Institute of Health Metrics and Evaluation (IHME). Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/27a7644e8ad28e739382d31e77589dd7 (accessed 25 September 2021)
(3) LaursenTM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology , 2014;10, 425-438.
(4) WHO. Mental health systems in selected low- and middle-income countries: a WHO-AIMS cross-national analysis. WHO: Geneva, 2009
(5) Jaeschke K et al. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017 Glob Ment Health 2021;8:e27.
Treatment of schizophrenia in the elderly. Treatment of senile schizophrenia
Treatment of schizophrenia in the elderly is becoming increasingly important for our country.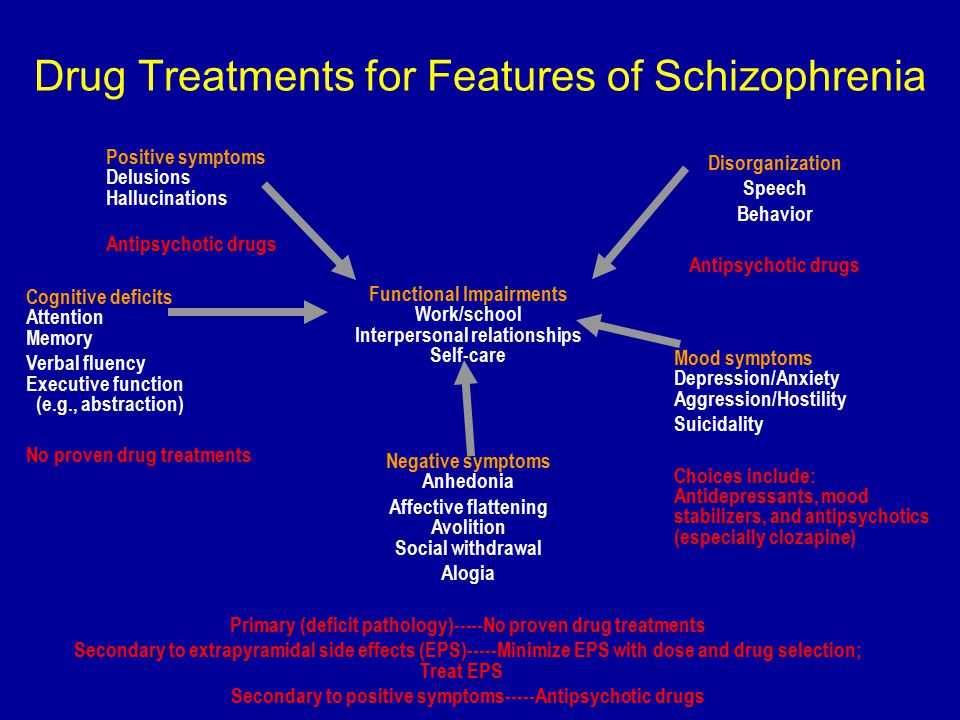 After all, old age is a period in life when a person changes not only physiologically, but also psychologically. At the same time, according to statistics, only 25% of the first symptoms appeared after 65 years, and in 75% the disease began to manifest itself earlier.
After all, old age is a period in life when a person changes not only physiologically, but also psychologically. At the same time, according to statistics, only 25% of the first symptoms appeared after 65 years, and in 75% the disease began to manifest itself earlier.
ELDERLY SCHIZOPHRENIA TREATMENT AVAILABLE AT 9 BRANCHES0220
Treatment of schizophrenia in the elderly in the Primorsky district
Address: St. Petersburg , Primorsky district, st. Repishcheva, 13
Treatment of schizophrenia in the elderly in the Petrogradsky district
Address: St. Petersburg , Petrogradsky district, st. Lenina, 5
Treatment of schizophrenia in the elderly in the Krasnogvardeisky district
Address: St. Petersburg , Krasnogvardeisky district, Novocherkassky pr., 33 building 3
Treatment of schizophrenia in the elderly in Vsevolozhsk
Address: Vsevolozhsk , Oktyabrsky Ave, 96
Schizophrenia in the elderly: types and symptoms
Before prescribing treatment for schizophrenia in the elderly, a correct diagnosis should be made, because it depends on what kind of treatment tactics should be used. There are two types of the disease:
There are two types of the disease:
- early onset schizophrenia;
- disease acquired in old age.
In this case, the second type is divided into two more subtypes:
- with late (after 40 years) onset;
- with a very late (after 60 years) onset.
Based on the type of disease, one or another therapy is prescribed, which makes the treatment of schizophrenia in old age the most effective. However, all types have similar points, namely:
- problems with psychosocial adjustment;
- using the method of neuroimaging, an insignificant pathology of the brain is detected;
- there is a genetic predisposition;
- severe productive symptoms are present.
Late-onset schizophrenia has a milder course: fewer negative symptoms, good response to antipsychotic drugs, more effective recovery of neuropsychological functions. This type responds well to modern drugs, and the treatment of very late-onset senile schizophrenia gives good results.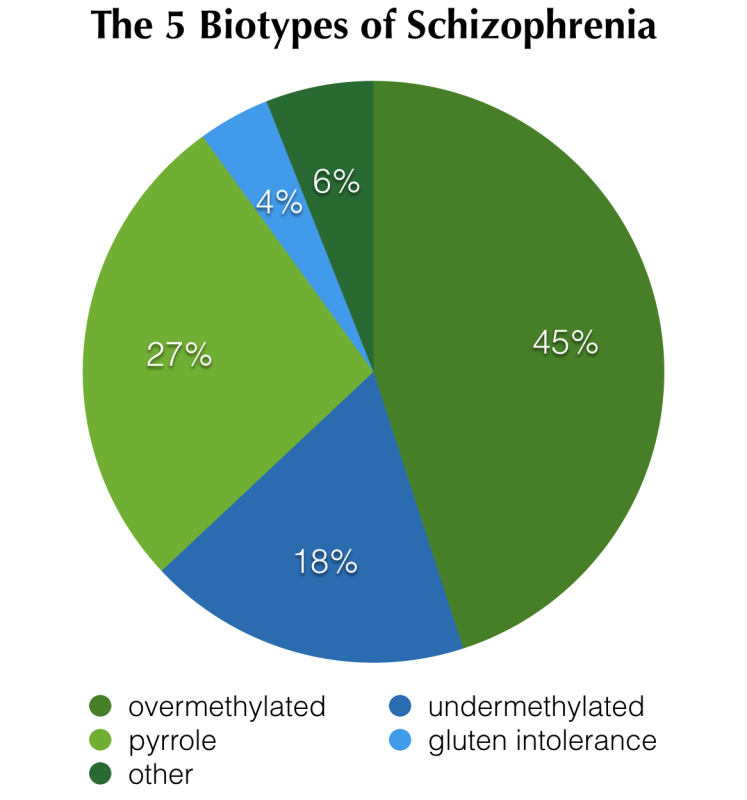 After all, there are often no formal thought disorders, and the probability of a family history is close to zero.
After all, there are often no formal thought disorders, and the probability of a family history is close to zero.
At the same time, a disease with a very late onset has a number of characteristic features:
- possible hallucinations;
- higher risk in women;
- sensory disturbances occur;
- high probability of developing dyskinesia;
- the patient is isolated from society solely at his own request.
Early signs of disease
Treatment of senile schizophrenia is prescribed by a doctor when the first symptoms appear. The initial period of the disease can manifest itself in the form of the following obsessive states:
- compulsions - obsessive actions;
- obsessions - obsessive thoughts;
- phobias - obsessive fears.
These conditions are subtle at first, but become more pronounced with time, resulting in the following symptoms:
- unreasonable outbursts of aggression;
- auditory, in some cases visual hallucinations;
- loss of interest in hobbies that the patient has been doing for a long time;
- obsessions, fears.
When the first signs of illness appear, you should promptly contact a specialist.
Our advantages
Treatment of schizophrenia in the elderly in St. Petersburg in the medical center "Dynasty" is carried out taking into account the advanced modern methods adopted by the world psychiatric practice. Our clinic is one of the few private clinics in the region that provides effective treatment for the entire spectrum of psychiatric pathology. This is possible thanks to:
- excellent material base - hospital, equipment;
- experienced professionals. More than 40 qualified psychiatrists;
- privacy policy and tactful approach to patients;
- close cooperation with government clinics and research institutes.
Clinics "Dynasty" are conveniently located in three districts of St. Petersburg, in addition, we treat schizophrenia in the elderly in Vsevolozhsk
Reception is conducted by doctors:
Select the Dynasty branch on Novocherkassky avenue, Krasnogvardeisky districtDynasty on Lenina, Petrogradsky districtDynasty on Repishcheva, Primorsky districtDynasty in VsevolozhskVisiting service
Children's specialists
Consults online