He has schizophrenia
Schizophrenia - Symptoms and causes
Overview
Schizophrenia is a serious mental disorder in which people interpret reality abnormally. Schizophrenia may result in some combination of hallucinations, delusions, and extremely disordered thinking and behavior that impairs daily functioning, and can be disabling.
People with schizophrenia require lifelong treatment. Early treatment may help get symptoms under control before serious complications develop and may help improve the long-term outlook.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
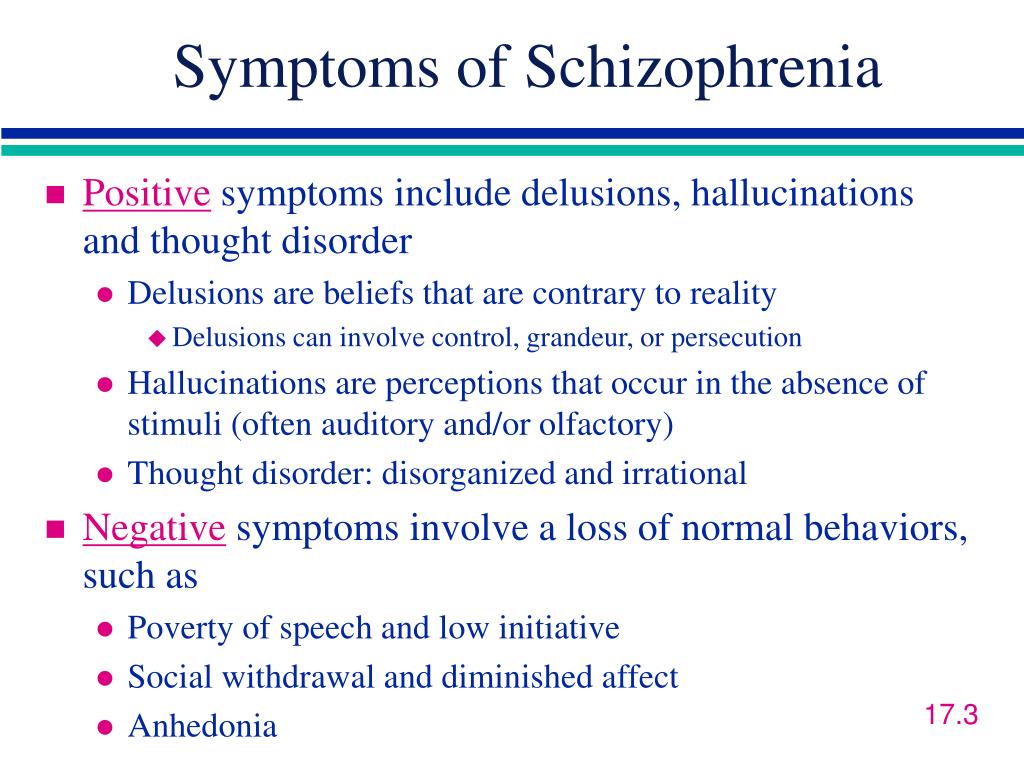
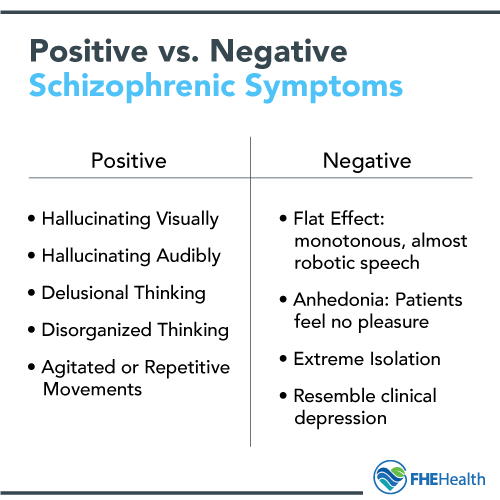
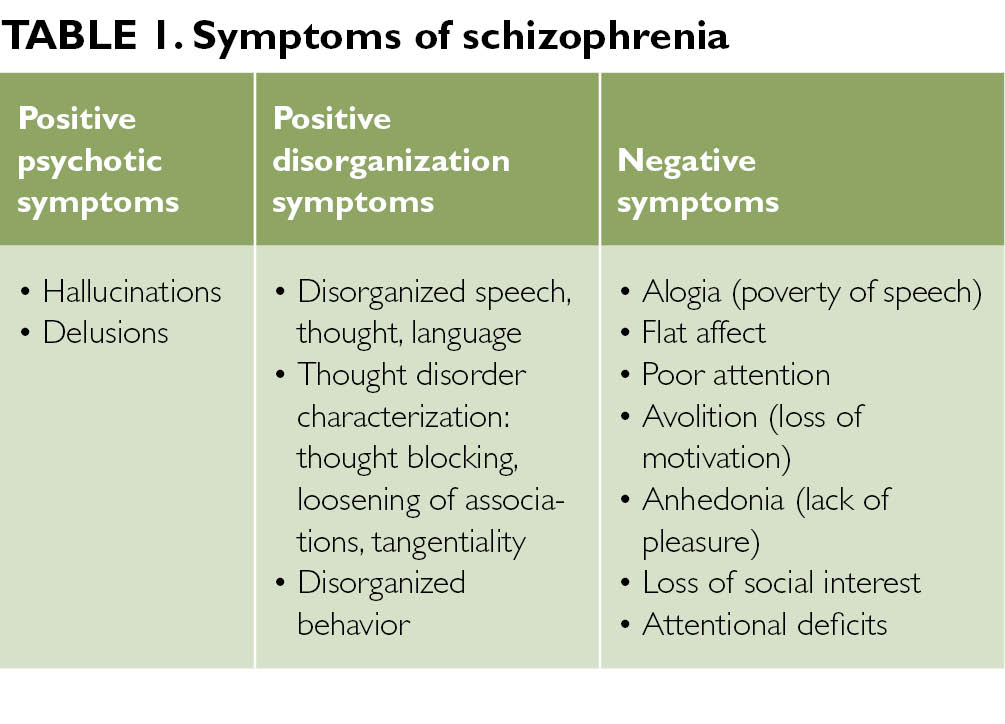
Schizophrenia involves a range of problems with thinking (cognition), behavior and emotions. Signs and symptoms may vary, but usually involve delusions, hallucinations or disorganized speech, and reflect an impaired ability to function. Symptoms may include:
- Delusions. These are false beliefs that are not based in reality.
For example, you think that you're being harmed or harassed; certain gestures or comments are directed at you; you have exceptional ability or fame; another person is in love with you; or a major catastrophe is about to occur. Delusions occur in most people with schizophrenia.
- Hallucinations. These usually involve seeing or hearing things that don't exist. Yet for the person with schizophrenia, they have the full force and impact of a normal experience. Hallucinations can be in any of the senses, but hearing voices is the most common hallucination.
- Disorganized thinking (speech). Disorganized thinking is inferred from disorganized speech. Effective communication can be impaired, and answers to questions may be partially or completely unrelated. Rarely, speech may include putting together meaningless words that can't be understood, sometimes known as word salad.
- Extremely disorganized or abnormal motor behavior.
 This may show in a number of ways, from childlike silliness to unpredictable agitation. Behavior isn't focused on a goal, so it's hard to do tasks. Behavior can include resistance to instructions, inappropriate or bizarre posture, a complete lack of response, or useless and excessive movement.
This may show in a number of ways, from childlike silliness to unpredictable agitation. Behavior isn't focused on a goal, so it's hard to do tasks. Behavior can include resistance to instructions, inappropriate or bizarre posture, a complete lack of response, or useless and excessive movement. - Negative symptoms. This refers to reduced or lack of ability to function normally. For example, the person may neglect personal hygiene or appear to lack emotion (doesn't make eye contact, doesn't change facial expressions or speaks in a monotone). Also, the person may lose interest in everyday activities, socially withdraw or lack the ability to experience pleasure.
Symptoms can vary in type and severity over time, with periods of worsening and remission of symptoms. Some symptoms may always be present.
In men, schizophrenia symptoms typically start in the early to mid-20s. In women, symptoms typically begin in the late 20s. It's uncommon for children to be diagnosed with schizophrenia and rare for those older than age 45.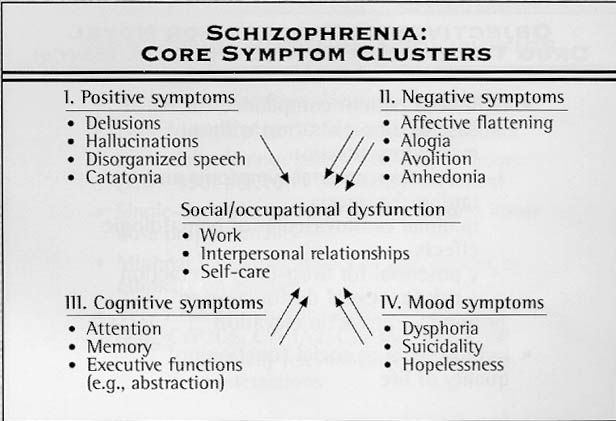
Symptoms in teenagers
Schizophrenia symptoms in teenagers are similar to those in adults, but the condition may be more difficult to recognize. This may be in part because some of the early symptoms of schizophrenia in teenagers are common for typical development during teen years, such as:
- Withdrawal from friends and family
- A drop in performance at school
- Trouble sleeping
- Irritability or depressed mood
- Lack of motivation
Also, recreational substance use, such as marijuana, methamphetamines or LSD, can sometimes cause similar signs and symptoms.
Compared with schizophrenia symptoms in adults, teens may be:
- Less likely to have delusions
- More likely to have visual hallucinations
When to see a doctor
People with schizophrenia often lack awareness that their difficulties stem from a mental disorder that requires medical attention. So it often falls to family or friends to get them help.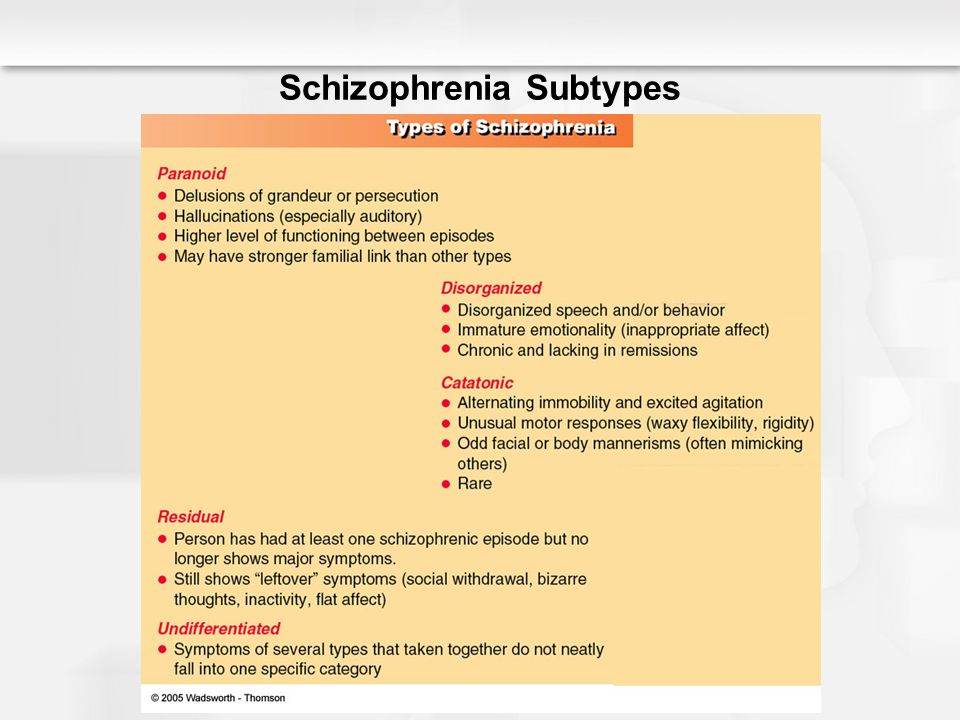
Helping someone who may have schizophrenia
If you think someone you know may have symptoms of schizophrenia, talk to him or her about your concerns. Although you can't force someone to seek professional help, you can offer encouragement and support and help your loved one find a qualified doctor or mental health professional.
If your loved one poses a danger to self or others or can't provide his or her own food, clothing, or shelter, you may need to call 911 or other emergency responders for help so that your loved one can be evaluated by a mental health professional.
In some cases, emergency hospitalization may be needed. Laws on involuntary commitment for mental health treatment vary by state. You can contact community mental health agencies or police departments in your area for details.
Suicidal thoughts and behavior
Suicidal thoughts and behavior are common among people with schizophrenia. If you have a loved one who is in danger of attempting suicide or has made a suicide attempt, make sure someone stays with that person. Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
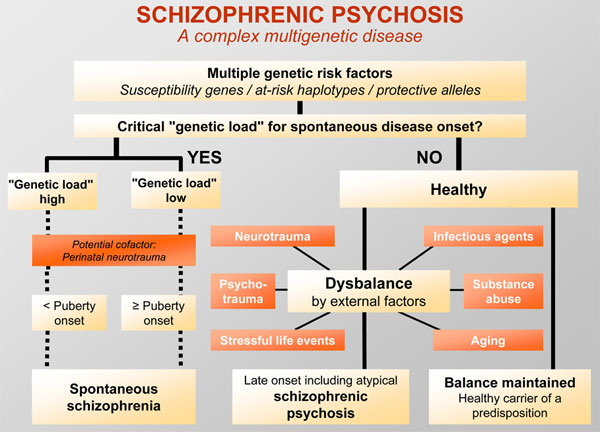
It's not known what causes schizophrenia, but researchers believe that a combination of genetics, brain chemistry and environment contributes to development of the disorder.
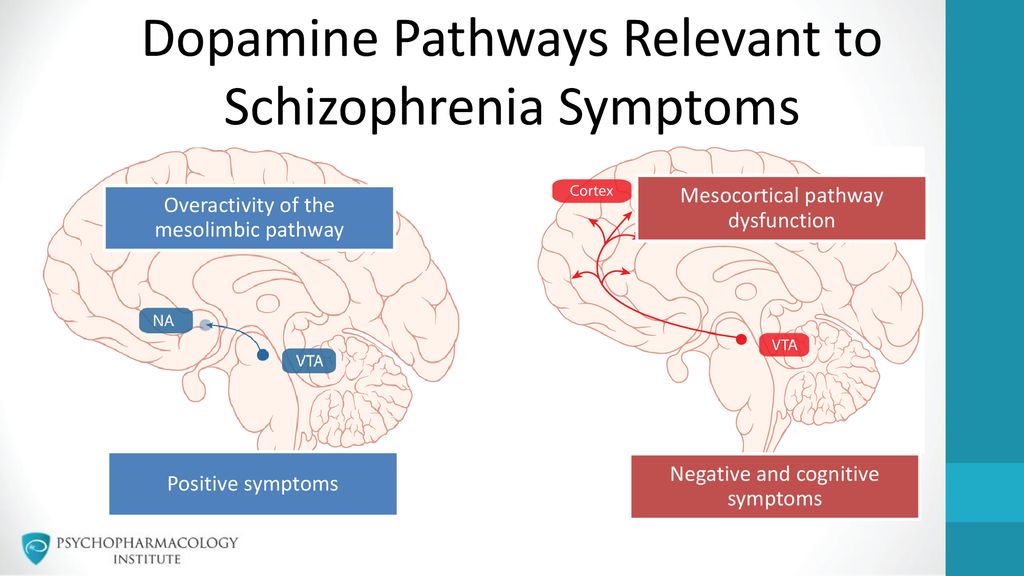
Problems with certain naturally occurring brain chemicals, including neurotransmitters called dopamine and glutamate, may contribute to schizophrenia. Neuroimaging studies show differences in the brain structure and central nervous system of people with schizophrenia. While researchers aren't certain about the significance of these changes, they indicate that schizophrenia is a brain disease.
Risk factors
Although the precise cause of schizophrenia isn't known, certain factors seem to increase the risk of developing or triggering schizophrenia, including:
- Having a family history of schizophrenia
- Some pregnancy and birth complications, such as malnutrition or exposure to toxins or viruses that may impact brain development
- Taking mind-altering (psychoactive or psychotropic) drugs during teen years and young adulthood
Complications
Left untreated, schizophrenia can result in severe problems that affect every area of life.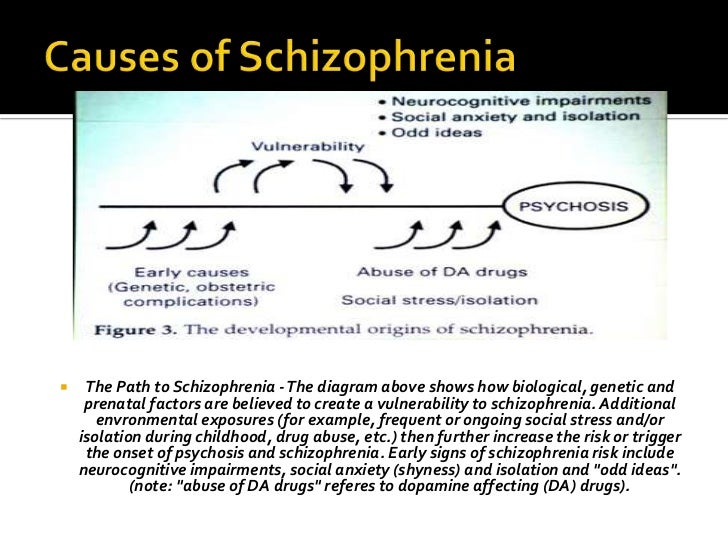 Complications that schizophrenia may cause or be associated with include:
Complications that schizophrenia may cause or be associated with include:
- Suicide, suicide attempts and thoughts of suicide
- Anxiety disorders and obsessive-compulsive disorder (OCD)
- Depression
- Abuse of alcohol or other drugs, including nicotine
- Inability to work or attend school
- Financial problems and homelessness
- Social isolation
- Health and medical problems
- Being victimized
- Aggressive behavior, although it's uncommon
Prevention
There's no sure way to prevent schizophrenia, but sticking with the treatment plan can help prevent relapses or worsening of symptoms. In addition, researchers hope that learning more about risk factors for schizophrenia may lead to earlier diagnosis and treatment.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
NIMH » Schizophrenia
Overview
Schizophrenia is a serious mental illness that affects how a person thinks, feels, and behaves.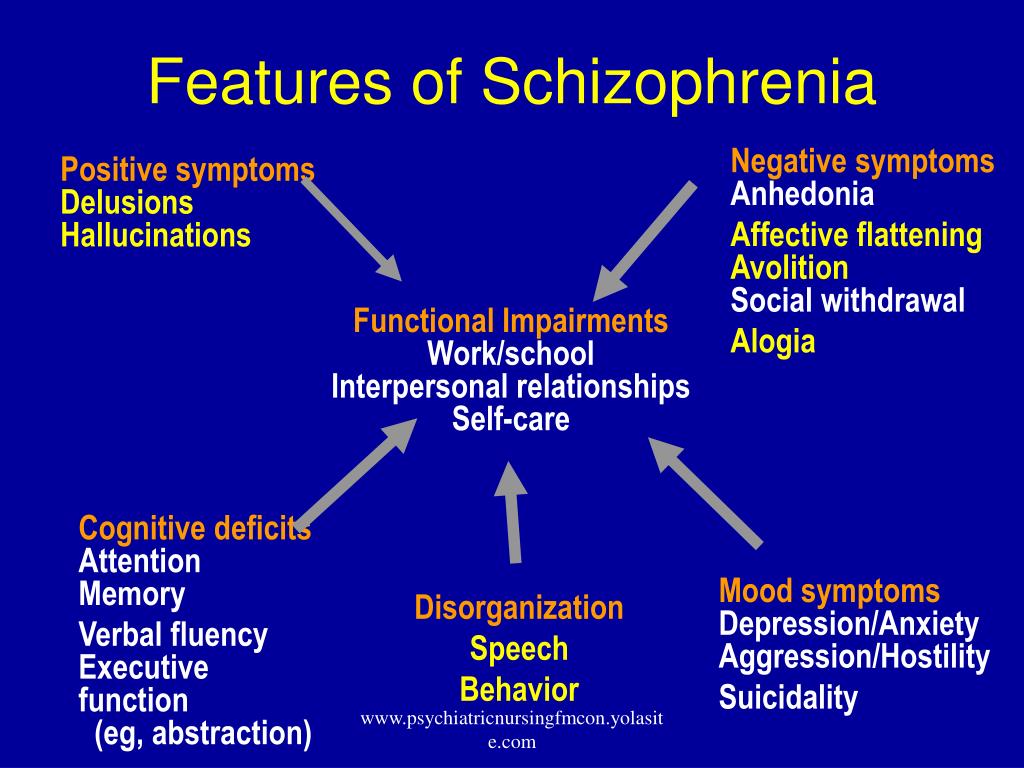 People with schizophrenia may seem like they have lost touch with reality, which can be distressing for them and for their family and friends. The symptoms of schizophrenia can make it difficult to participate in usual, everyday activities, but effective treatments are available. Many people who receive treatment can engage in school or work, achieve independence, and enjoy personal relationships.
People with schizophrenia may seem like they have lost touch with reality, which can be distressing for them and for their family and friends. The symptoms of schizophrenia can make it difficult to participate in usual, everyday activities, but effective treatments are available. Many people who receive treatment can engage in school or work, achieve independence, and enjoy personal relationships.
Onset and Symptoms
The Centers for Disease Control and Prevention (CDC) has recognized that having certain mental disorders, including depression and schizophrenia, can make people more likely to get severely ill from COVID-19. Learn more about getting help and finding a health care provider on NIMH's Help for Mental Illnesses webpage.
It’s important to recognize the symptoms of schizophrenia and seek help as early as possible. People with schizophrenia are usually diagnosed between the ages of 16 and 30, after the first episode of psychosis. Starting treatment as soon as possible following the first episode of psychosis is an important step toward recovery. However, research shows that gradual changes in thinking, mood, and social functioning often appear before the first episode of psychosis. Schizophrenia is rare in younger children.
However, research shows that gradual changes in thinking, mood, and social functioning often appear before the first episode of psychosis. Schizophrenia is rare in younger children.
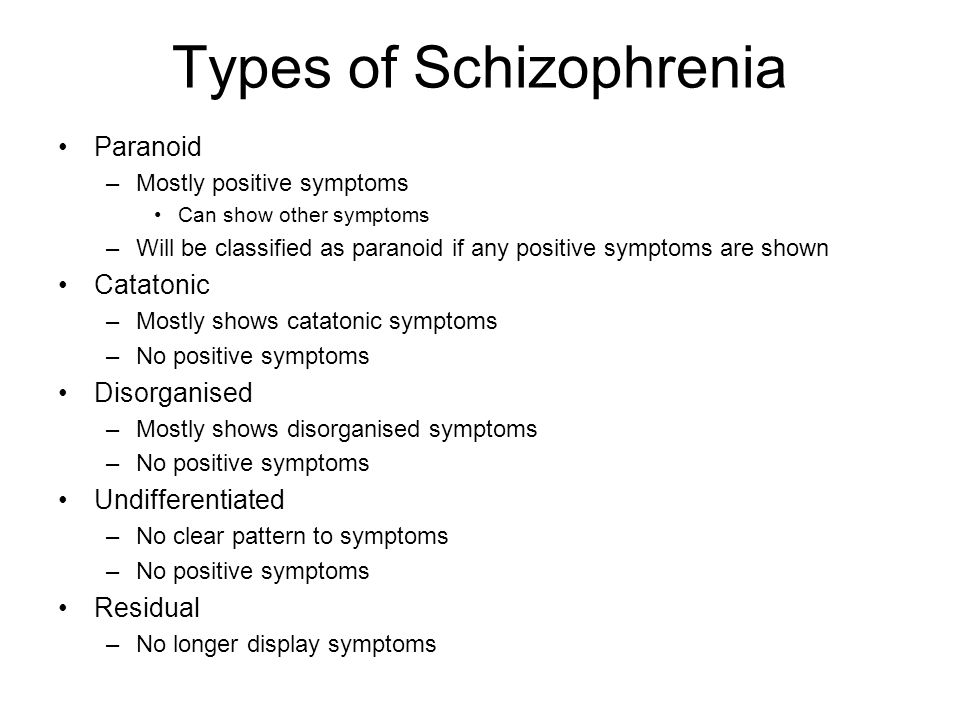
Schizophrenia symptoms can differ from person to person, but they generally fall into three main categories: psychotic, negative, and cognitive.
Psychotic symptoms include changes in the way a person thinks, acts, and experiences the world. People with psychotic symptoms may lose a shared sense of reality with others and experience the world in a distorted way. For some people, these symptoms come and go. For others, the symptoms become stable over time. Psychotic symptoms include:
- Hallucinations: When a person sees, hears, smells, tastes, or feels things that are not actually there. Hearing voices is common for people with schizophrenia. People who hear voices may hear them for a long time before family or friends notice a problem.
- Delusions: When a person has strong beliefs that are not true and may seem irrational to others.
 For example, individuals experiencing delusions may believe that people on the radio and television are sending special messages that require a certain response, or they may believe that they are in danger or that others are trying to hurt them.
For example, individuals experiencing delusions may believe that people on the radio and television are sending special messages that require a certain response, or they may believe that they are in danger or that others are trying to hurt them. - Thought disorder: When a person has ways of thinking that are unusual or illogical. People with thought disorder may have trouble organizing their thoughts and speech. Sometimes a person will stop talking in the middle of a thought, jump from topic to topic, or make up words that have no meaning.
- Movement disorder : When a person exhibits abnormal body movements. People with movement disorder may repeat certain motions over and over.
Negative symptoms include loss of motivation, loss of interest or enjoyment in daily activities, withdrawal from social life, difficulty showing emotions, and difficulty functioning normally. Negative symptoms include:
- Having trouble planning and sticking with activities, such as grocery shopping
- Having trouble anticipating and feeling pleasure in everyday life
- Talking in a dull voice and showing limited facial expression
- Avoiding social interaction or interacting in socially awkward ways
- Having very low energy and spending a lot of time in passive activities.
 In extreme cases, a person might stop moving or talking for a while, which is a rare condition called catatonia.
In extreme cases, a person might stop moving or talking for a while, which is a rare condition called catatonia.
These symptoms are sometimes mistaken for symptoms of depression or other mental illnesses.
Cognitive symptoms include problems in attention, concentration, and memory. These symptoms can make it hard to follow a conversation, learn new things, or remember appointments. A person’s level of cognitive functioning is one of the best predictors of their day-to-day functioning. Cognitive functioning is evaluated using specific tests. Cognitive symptoms include:
- Having trouble processing information to make decisions
- Having trouble using information immediately after learning it
- Having trouble focusing or paying attention
Risk of Violence
Most people with schizophrenia are not violent. Overall, people with schizophrenia are more likely than those without the illness to be harmed by others.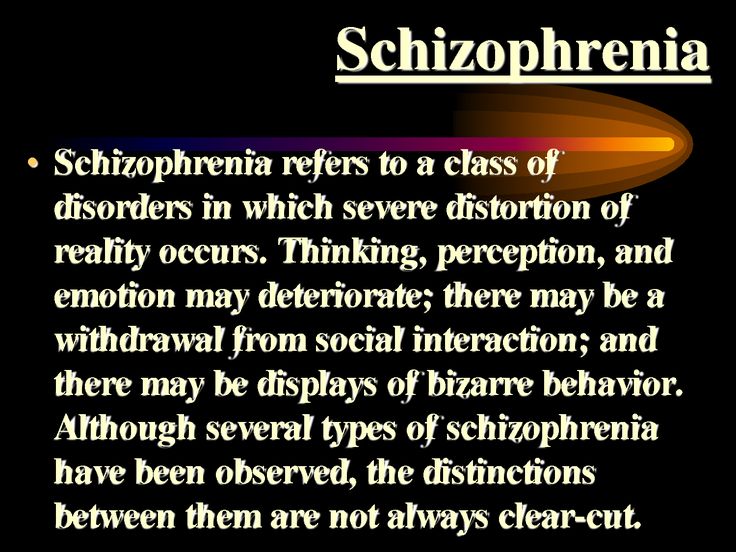 For people with schizophrenia, the risk of self-harm and of violence to others is greatest when the illness is untreated. It is important to help people who are showing symptoms to get treatment as quickly as possible.
For people with schizophrenia, the risk of self-harm and of violence to others is greatest when the illness is untreated. It is important to help people who are showing symptoms to get treatment as quickly as possible.
Schizophrenia vs. Dissociative Identity Disorder
Although some of the signs may seem similar on the surface, schizophrenia is not dissociative identity disorder (which used to be called multiple personality disorder or split personality). People with dissociative identity disorder have two or more distinct identities that are present and that alternately take control of them.
Risk Factors
Several factors may contribute to a person’s risk of developing schizophrenia, including:
Genetics: Schizophrenia sometimes runs in families. However, just because one family member has schizophrenia, it does not mean that other members of the family also will have it. Studies suggest that many different genes may increase a person’s chances of developing schizophrenia, but that no single gene causes the disorder by itself.
Environment: Research suggests that a combination of genetic factors and aspects of a person’s environment and life experiences may play a role in the development of schizophrenia. These environmental factors that may include living in poverty, stressful or dangerous surroundings, and exposure to viruses or nutritional problems before birth.
Brain structure and function: Research shows that people with schizophrenia may be more likely to have differences in the size of certain brain areas and in connections between brain areas. Some of these brain differences may develop before birth. Researchers are working to better understand how brain structure and function may relate to schizophrenia.
Treatments and Therapies
Current treatments for schizophrenia focus on helping individuals manage their symptoms, improve day-to-day functioning, and achieve personal life goals, such as completing education, pursuing a career, and having fulfilling relationships.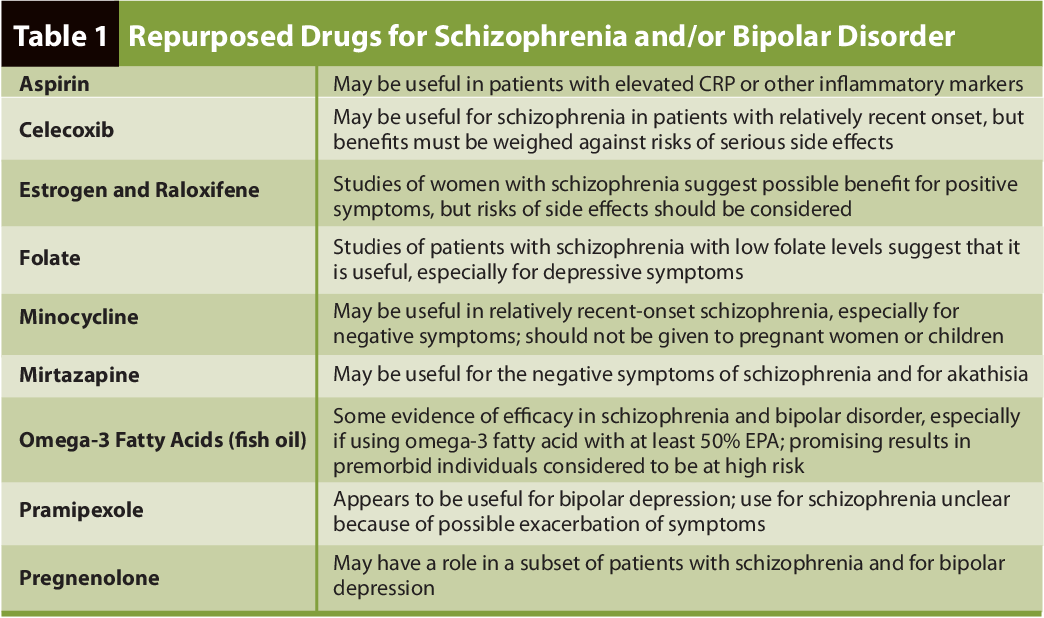
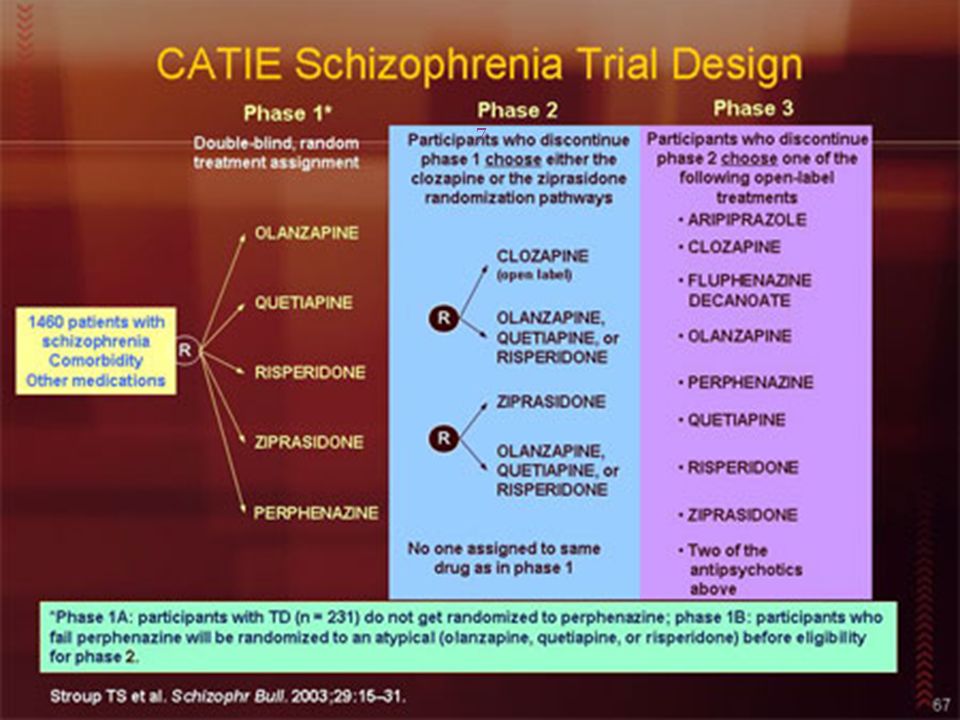
Antipsychotic Medications
Antipsychotic medications can help make psychotic symptoms less intense and less frequent. These medications are usually taken every day in a pill or liquid forms. Some antipsychotic medications are given as injections once or twice a month.
If a person’s symptoms do not improve with usual antipsychotic medications, they may be prescribed clozapine. People who take clozapine must have regular blood tests to check for a potentially dangerous side effect that occurs in 1-2% of patients.
People respond to antipsychotic medications in different ways. It is important to report any side effects to a health care provider. Many people taking antipsychotic medications experience side effects such as weight gain, dry mouth, restlessness, and drowsiness when they start taking these medications. Some of these side effects may go away over time, while others may last.
Shared decision making between doctors and patients is the recommended strategy for determining the best type of medication or medication combination and the right dose.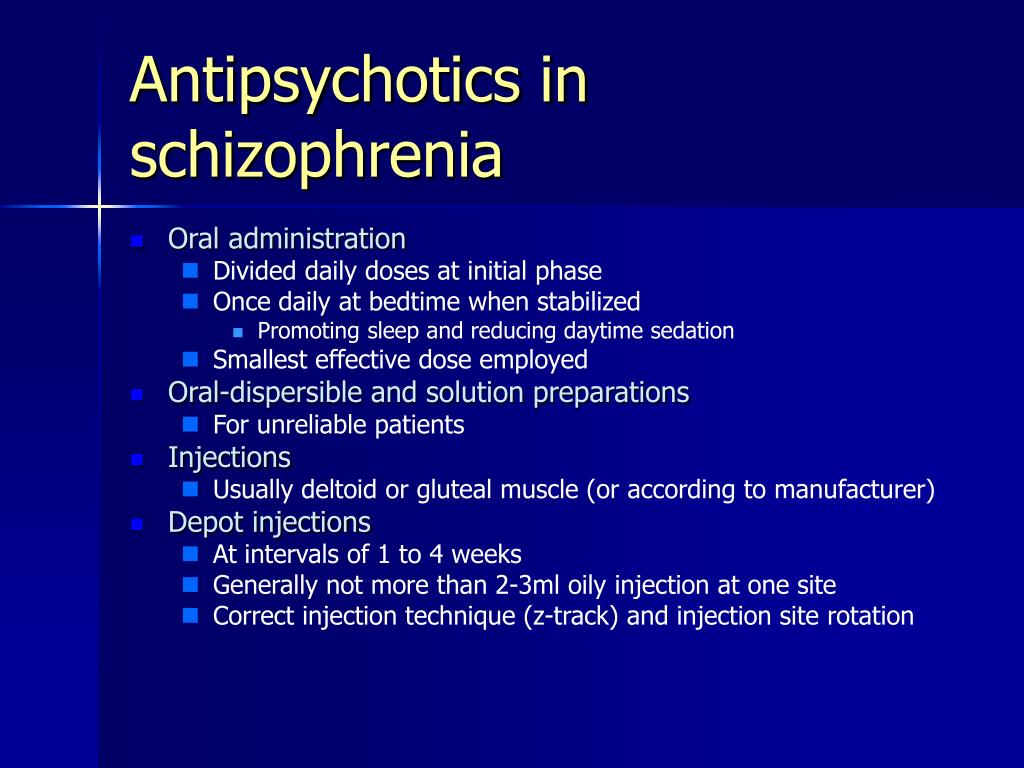 You can find the latest information on warnings, patient medication guides, or newly approved medications on the U.S. Food and Drug Administration (FDA) website.
You can find the latest information on warnings, patient medication guides, or newly approved medications on the U.S. Food and Drug Administration (FDA) website.
Psychosocial Treatments
Psychosocial treatments help people find solutions to everyday challenges and manage symptoms while attending school, working, and forming relationships. These treatments are often used together with antipsychotic medication. People who participate in regular psychosocial treatment are less likely to have symptoms reoccur or to be hospitalized.
Examples of this kind of treatment include cognitive behavioral therapy, behavioral skills training, supported employment, and cognitive remediation interventions.
You can find information about psychosocial treatments on the National Institute of Mental Health (NIMH) psychotherapies webpage.
Family Education and Support
Educational programs can help family and friends learn about symptoms of schizophrenia, treatment options, and strategies for helping loved ones with the illness. These programs can help friends and family manage their distress, boost their own coping skills, and strengthen their ability to provide support. For more information about family-based services in your area, you can visit the family education and support groups page on the National Alliance on Mental Illness website.
These programs can help friends and family manage their distress, boost their own coping skills, and strengthen their ability to provide support. For more information about family-based services in your area, you can visit the family education and support groups page on the National Alliance on Mental Illness website.
Coordinated Specialty Care
Coordinated specialty care (CSC) programs are recovery-focused programs for people with first episode psychosis, an early stage of schizophrenia. Health professionals and specialists work together as a team to provide CSC, which includes psychotherapy, medication, case management, employment and education support, and family education and support. The treatment team works collaboratively with the individual to make treatment decisions, involving family members as much as possible.
Compared with typical care, CSC is more effective at reducing symptoms, improving quality of life, and increasing involvement in work or school. Check here for more information about CSC programs.
Assertive Community Treatment
Assertive Community Treatment (ACT) is designed especially for individuals with schizophrenia who are likely to experience multiple hospitalizations or homelessness. ACT is usually delivered by a team of health professionals who work together to provide care to patients in the community. Check here for more information about ACT programs.
Treatment for Drug and Alcohol Misuse
It is common for people with schizophrenia to have problems with drugs and alcohol. A treatment program that includes treatment for both schizophrenia and substance use is important for recovery because substance use can interfere with treatment for schizophrenia.
How can I help a friend or relative with schizophrenia?
It can be difficult to know how to help someone who is experiencing psychosis.
Here are some things you can do:
- Help them get treatment and encourage them to stay in treatment.
- Remember that their beliefs or hallucinations seem very real to them.

- Be respectful, supportive, and kind without tolerating dangerous or inappropriate behavior.
- Look for support groups and family education programs, such as those offered by the National Alliance on Mental Illness.
If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide & Crisis Lifeline at 988 or chat at 988lifeline.org. In life-threatening situations, call 911.
Finding Help
If you’re not sure where to get help, your health care provider is a good place to start. Your health care provider can refer you to a qualified mental health professional, such as a psychiatrist or psychologist who has experience treating schizophrenia. You can learn more about getting help on NIMH's Help for Mental Illness webpage.
The Substance Abuse and Mental Health Services Administration (SAMHSA) provides the Behavioral Health Treatment Services Locator, an online tool to help you find mental health services in your area. You can find information about treatment facilities that offer coordinated specialty care by using SAMHSA’s Early Serious Mental Illness Treatment Locator.
You can find information about treatment facilities that offer coordinated specialty care by using SAMHSA’s Early Serious Mental Illness Treatment Locator.
For tips on talking with your health care provider about your mental health and getting the most out of your visit, read NIMH’s fact sheet, Taking Control of Your Mental Health: Tips for Talking With Your Health Care Provider.
Join a Study
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage: Information about participating in clinical trials
- Clinicaltrials.gov: Current Studies on Schizophrenia: List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
- Join a Study: Schizophrenia: List of studies being conducted on the NIH Campus in Bethesda, MD
Learn More
Free Brochures and Shareable Resources
- Schizophrenia: A brief brochure on schizophrenia that offers basic information on signs and symptoms, treatment, and finding help. Also available en español.
- Understanding Psychosis: A fact sheet that presents information on psychosis, including causes, signs and symptoms, treatment, and resources for help.
 Also available en español.
Also available en español. - Shareable Resources on Schizophrenia: Help support schizophrenia awareness and education in your community. Use these digital resources, including graphics and messages, to spread the word about schizophrenia.
Research and Statistics
- Accelerating Medicines Partnership® Program - Schizophrenia (AMP® SCZ): This AMP public-private collaborative effort aims to promote the development of effective, targeted treatments for those at risk of developing schizophrenia. More information about the program is also available on the AMP SCZ website.
- Early Psychosis Intervention Network (EPINET): This broad research initiative aims to develop models for the effective delivery of coordinated specialty care (CSC) services for early psychosis.
- Journal Articles: This webpage provides information on references and abstracts from MEDLINE/PubMed (National Library of Medicine).
- Psychotic Disorders Research Program: This program supports research into the origins, onset, course, and outcome of schizophrenia spectrum disorders and other psychotic illnesses.
- Recovery After an Initial Schizophrenia Episode (RAISE): The NIMH RAISE research initiative included two studies examining different aspects of coordinated specialty care treatments for people who were experiencing early psychosis.
- Schizophrenia Statistics: This webpage provides information on the best statistics currently available on the prevalence and treatment of schizophrenia in the U.S.
Last Reviewed: May 2022
Unless otherwise specified, NIMH information and publications are in the public domain and available for use free of charge. Citation of NIMH is appreciated. Please see our Citing NIMH Information and Publications page for more information.
Schizophrenia
Schizophrenia- Healthcare issues »
- A
- B
- B
- G
- D
- E
- and
- 9000 About
- P
- P
- With
- T
- U
- F
- x
- S
- B
- E
- S
- I
005
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find country »
- A
- B
- C
- g
- D
- E
- and
- th
- K
- L
- 9000 N
- 9000
- in
- f
- x
- C
- hours
- Sh
- Sh.
- 9000 WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Events
- Photo reports
- case studies
- Questions and answers
- Speeches
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Schizophrenia
Key Facts
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.
- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations.
- Worldwide, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective options for helping patients with schizophrenia, which can lead to a complete recovery of at least one in three patients.
Symptoms
Schizophrenia is characterized by significant disturbances in the perception of reality and behavioral changes, such as:
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms.
Scope and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease.
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
People with schizophrenia are 2-3 times more likely to die early than the population average (2).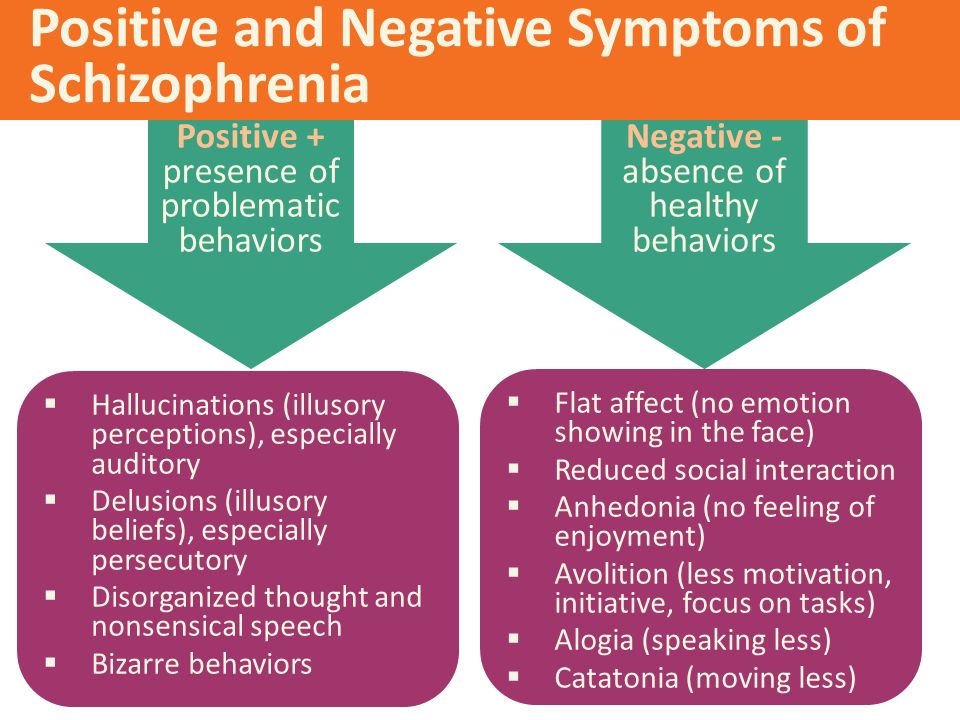 It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment.
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, lead to isolation and disruption of health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.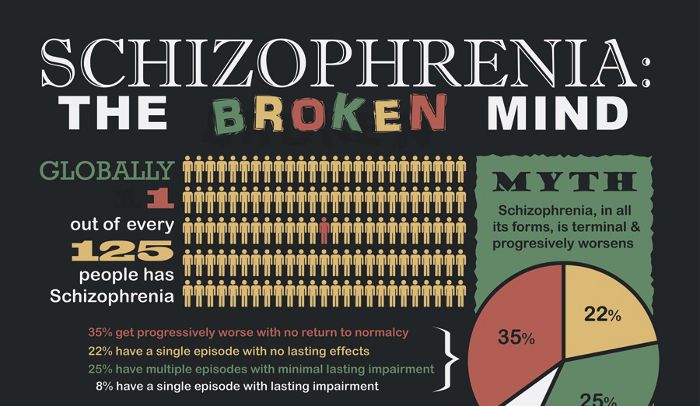
Causes of schizophrenia
Science has not established any single cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective way of providing care for mental disorders and is regularly associated with the violation of the fundamental rights of patients with schizophrenia. Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities.
Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities.
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education). The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
WHO action
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care.
The WHO Mental Health Gap Action Program (mhGAP) is working to develop evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings.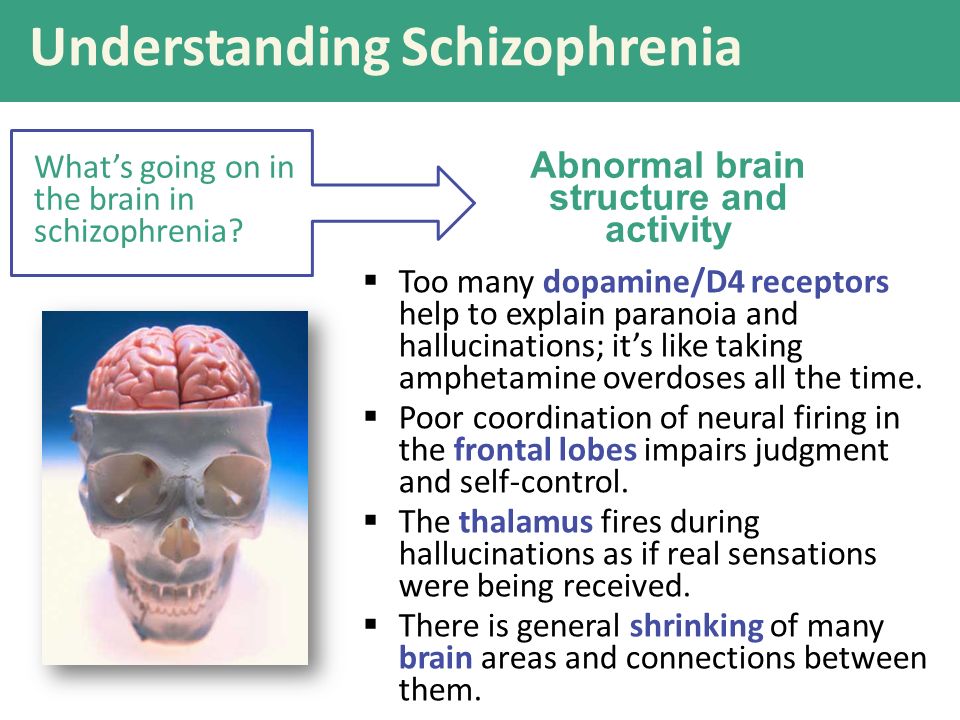 The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities.
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J.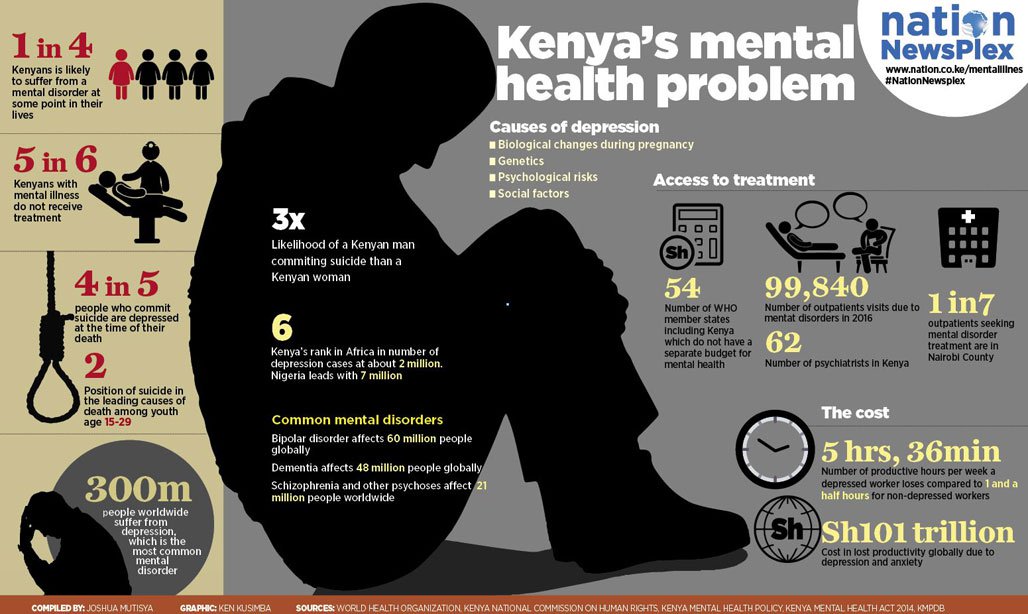 Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
(2) Institute of Health Metrics and Evaluation (IHME). Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/27a7644e8ad28e739382d31e77589dd7 (accessed 25 September 2021)
(3) LaursenTM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology , 2014;10, 425-438.
(4) WHO. Mental health systems in selected low- and middle-income countries: a WHO-AIMS cross-national analysis. WHO: Geneva, 2009
(5) Jaeschke K et al. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017 Glob Ment Health 2021;8:e27.
The brain of a person suffering from schizophrenia: how the disease manifests itself and how scientists fight it
The brain of a person suffering from schizophrenia: how the disease manifests itself and how scientists fight it
Even if there are no people suffering from schizophrenia among your acquaintances, most likely, you have an idea about its symptoms.
The disorder can manifest as hallucinations, delusions, and paranoia, as well as difficulty concentrating, organizing thoughts, and performing basic daily tasks.
For many years doctors knew little about this disease, except for the symptoms reported by the patients themselves. The causes of schizophrenia and how it affects the brain have for the most part remained a mystery due to the extreme difficulty scientists have had in trying to understand the most complex—and least accessible—organ in the human body.
But today, thanks to new technologies, the veil of secrecy is beginning to be covered.
“Over the past few years, we have seen tremendous advances in the understanding and treatment of schizophrenia,” says MD Husseini Manji, MD, Global Head of Neurology Therapeutics at Janssen. “This area of medicine is going through an exciting period.”
The possibility of developing new treatments for people with schizophrenia was one of the reasons that attracted Dr.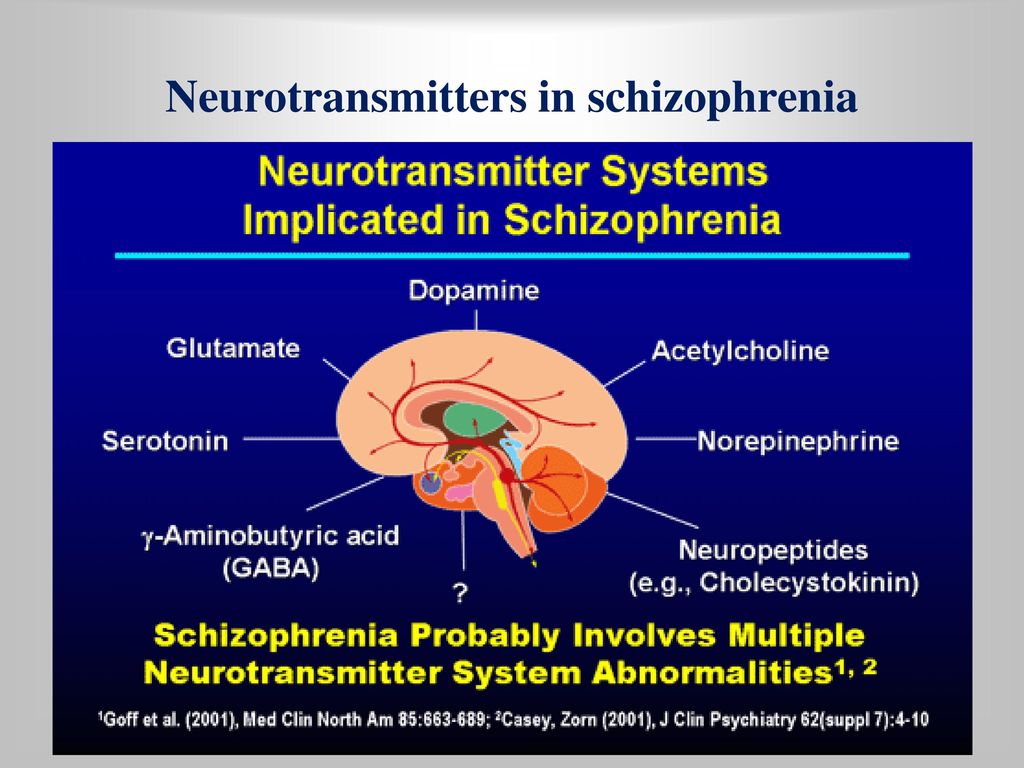 Manji to the company. Then, in 2008, he was director of the National Institute of Mental Health and director of the Mood and Anxiety Disorders Program.
Manji to the company. Then, in 2008, he was director of the National Institute of Mental Health and director of the Mood and Anxiety Disorders Program.
“Several drug companies tried to convince me to join them, but at Johnson & Johnson they were focusing on neuroscience just as many were moving away from the field,” he explains. “The science of mental illness has reached a point of maturity where existing knowledge can be translated into advanced treatments for illnesses like schizophrenia.”
The nearly 2.5 million people with schizophrenia—one percent of the US adult population—are looking forward to progress in understanding and treating this complex disease.
Dr. Husseini Manji,
Head of Global Therapeutics Neurology at Janssen
Schizophrenia is one of the most severe mental illnesses. It usually manifests itself in late adolescence or after 20 years of age. Its consequences can be catastrophic: people with schizophrenia are at increased risk of becoming unemployed, homeless and incarcerated.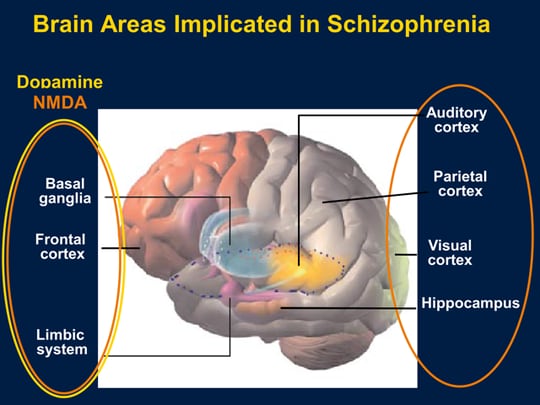 About a third of patients attempt to commit suicide, and about one in ten eventually succeeds.
About a third of patients attempt to commit suicide, and about one in ten eventually succeeds.
Researchers know that schizophrenia is largely hereditary, but they know less about the biological basis of the disease. However, thanks to advanced brain imaging technologies, scientists such as Dr. Manji are beginning to gain a clearer picture of the changes taking place in the brain of a person with schizophrenia. It turns out that these changes occur even before the onset of clinical symptoms.
Study of the brain of a patient with schizophrenia
Over the past decade, several brain imaging studies have provided evidence that structural abnormalities are present in the brains of patients with schizophrenia. This gave scientists clues to the biological causes of the disease and how it progresses.
In one 15-year study funded in part by Janssen and described in the American Psychiatric Journal ( American Journal of Psychiatry ), it was found that during the first attack of psychosis, patients had less brain tissue than healthy people. Although losses stabilized over time, long-term relapses of psychosis were associated with additional volume reductions.
Although losses stabilized over time, long-term relapses of psychosis were associated with additional volume reductions.
"We knew from earlier post-mortem studies on the brains of schizophrenic patients that they have fewer synapses and neural branches that allow neurons to communicate," explains MD Scott W. Woods, Professor of Psychiatry and Director of the Research Clinic prodromal period of psychosis PRIME at Yale University. “We think this explains the reduction in brain tissue seen on the scans.”
During adolescence, everyone experiences a normal loss of a certain amount of gray matter, which contains neurons and their short processes, but experts believe that in people at high risk of developing schizophrenia, this process may proceed too quickly or actively, causing psychosis.
Imaging studies indicate a lack of gray and white matter in the brains of people with schizophrenia. In adolescence, everyone experiences a normal loss of a certain amount of gray matter, which contains neurons and their short processes, but experts believe that in people at high risk of developing schizophrenia, this process may proceed too quickly or actively, causing psychosis.
The abnormal development of the white matter, which contains long, myelinated nerve fibers that connect the four lobes of the brain, can also be a tipping point for some people who are predisposed to this condition. The authors of the study, published in the journal Clinical Neuroimaging ( NeuroImage: Clinical ), suggest that this may be related to cognitive symptoms in patients with schizophrenia, including cognitive and memory impairments, apathy, and low motivation.
What causes these losses is still unknown, but a common theory is that inflammation contributes to the progression of many diseases. Two years ago, British researchers discovered increased activity of immune cells in the brains of schizophrenic patients and people at risk. It is not clear what exactly can serve as a stimulus for the onset of the inflammatory process, but in the course of previous studies it was possible to establish a link between infections at an early age and cases of schizophrenia.
"Inflammation is one of the mechanisms leading to the destruction of synapses and neuronal branches in the brain, so severe inflammation could explain the loss," says Dr. Woods.
Advanced Brain Protection
By learning about these brain abnormalities, Janssen scientists understand the importance of treating people at the earliest stage of schizophrenia and discovering new ways to minimize the damage caused by multiple relapses.
One of Janssen's important areas of research is finding ways to improve treatment adherence. This problem is faced by any doctor who treats chronic diseases, but it is especially difficult when working with patients suffering from schizophrenia. Only about half of patients are taking prescribed medications. Failure to adhere to the regimen sets off a cycle of relapse and return of symptoms that is difficult to break and weakens the response to treatment.
“Unfortunately, the nature of schizophrenia limits patients' understanding of the disease,” says Dr. Manji. “In many cases, when they feel a little better, they stop taking the medication. However, unlike, for example, patients with diabetes, who feel the effects of missing a dose of insulin after only a few hours, patients with schizophrenia who stop taking antipsychotic drugs may not experience symptoms of relapse for several weeks.
Manji. “In many cases, when they feel a little better, they stop taking the medication. However, unlike, for example, patients with diabetes, who feel the effects of missing a dose of insulin after only a few hours, patients with schizophrenia who stop taking antipsychotic drugs may not experience symptoms of relapse for several weeks.
Janssen scientists have attempted to help reverse this severe cycle of relapse by developing long-acting injectable antipsychotics that are given to patients less frequently than other drugs.
To further protect patients from the damaging effects of multiple relapses, Janssen is exploring ways to identify patients at high risk of relapse using data collected from smartphones, medical trackers and body sensors.
Long-acting injectables are administered by physicians, so if a patient misses a dose, the attending physician will know and take action.
To further protect patients from the damaging effects of multiple relapses, Janssen is exploring ways to identify patients at high risk of relapse using data collected from smartphones, medical trackers and body sensors.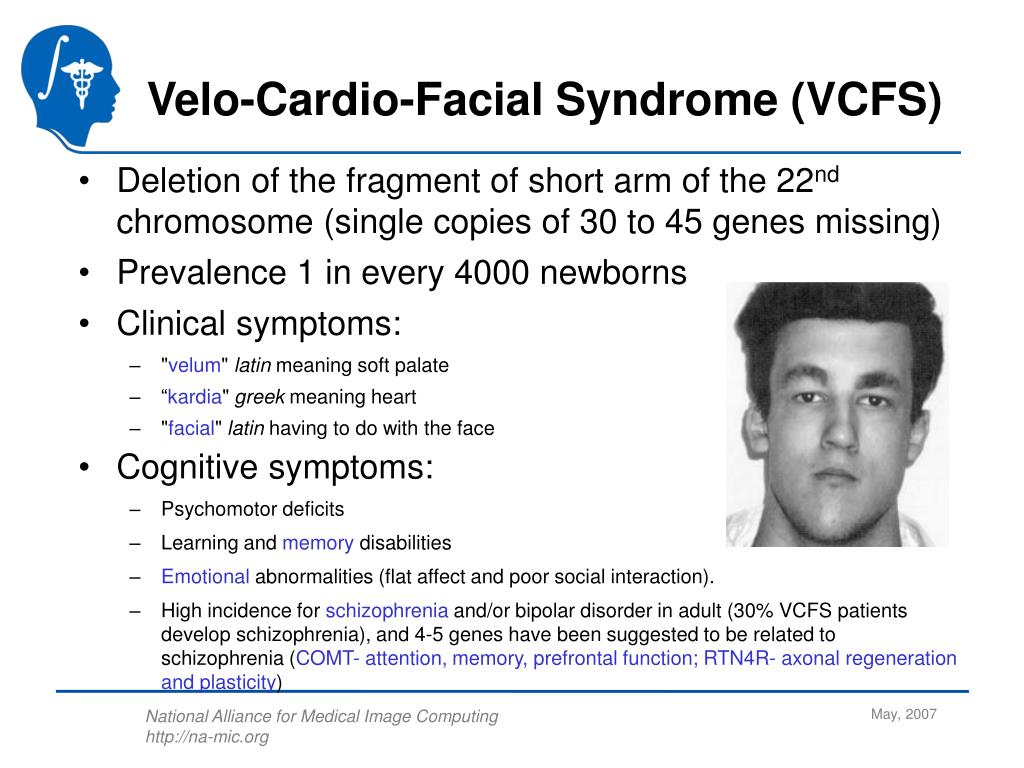
“We want to know if by tracking factors such as sleep, activity levels, interactions with other people and other biomarkers, we can provide doctors with early information about an impending relapse,” explains Dr. Manji. “This would give them the ability to identify patients who are deteriorating and get in touch with them, instead of waiting for them to come to the appointment themselves.”
Among other things, incorporating medical technology into a patient's treatment plan would help clinicians gain more objective data on how a person is actually feeling. Practice shows that when patients are asked about their well-being for several weeks, they remember only the last day or two. With more long-term, measurable data, clinicians could not only have a relatively clear picture of how a patient is feeling, but also be more constructive in their appointments.
“If patients are stable and you don't have to spend so much time just dealing with psychotic symptoms, you can focus on finding constructive ways to help them get back to normal,” says Dr.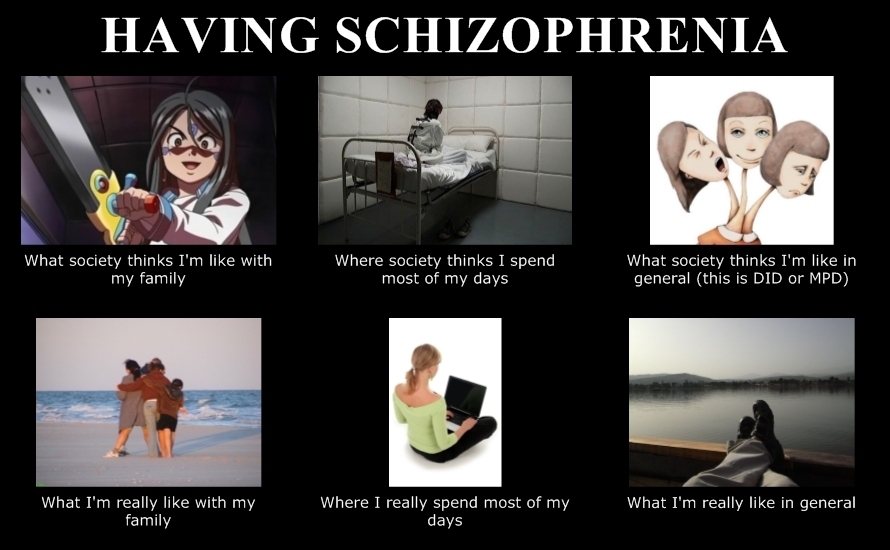 Manji.
Manji.
More than just symptom relief, it's a comprehensive treatment
To truly improve the lives of people with schizophrenia, scientists are not only developing new drugs, but also advancing the principles of integrative care. Dr. Manji said he was drawn to work at Johnson & Johnson because the company shares his belief that medicine must go beyond pills to provide the best possible outcome for patients with schizophrenia.
“We want people to understand that the best way to treat schizophrenia in the long term is through a more holistic, integrated model of care,” he explains. Mental illness has a big impact on every aspect of a person's life: their physical health, behavior and relationships. Patients require several types of correction, and not just medication.”
One of Janssen's research focuses on the vital role of carers and the challenges they face in treating and caring for people with schizophrenia. Patients are currently being recruited for a one-year clinical trial called Family Intervention in Recent Onset Schizophrenia Treatment (FIRST). The scientists plan to evaluate the overall impact that caregivers can have on patients by participating in a program of psychological education and training for caregivers. Perhaps such programs will help reduce the number of treatment failures, such as psychiatric hospitalization and suicide or attempted suicide.
The scientists plan to evaluate the overall impact that caregivers can have on patients by participating in a program of psychological education and training for caregivers. Perhaps such programs will help reduce the number of treatment failures, such as psychiatric hospitalization and suicide or attempted suicide.
The company's sincere commitment to improving the lives of patients is reflected in its projects in partnership with academia, government and the biotechnology industry. “This disease is so complex that we need to come together to make progress in research,” says Dr. Manji.
In 2015, Janssen Research & Development launched the Open Translational Science in Schizophrenia (OPTICS) project, a forum for collaborative analysis of Janssen clinical trial data and publicly available information on schizophrenia provided by the National Institutes of Health.
In addition, the company is an industry partner in a recently formed consortium led by the Johns Hopkins University School of Medicine and the Salk Institute for Biological Research.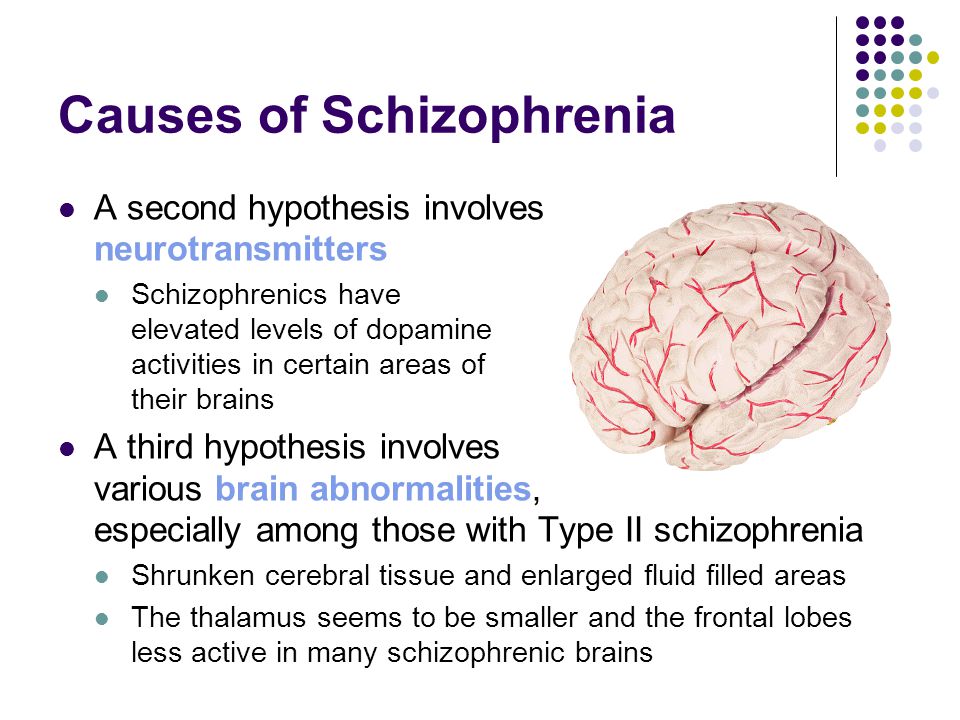 The consortium aims to improve the quality of induced pluripotent stem cell technology, a tool that allows scientists to harvest skin cells from mentally ill patients and convert them into neurons. By building a neural model of schizophrenia using patient cells, scientists hope to gain new insights into the underlying mechanisms of the disease in order to develop more targeted treatments.
The consortium aims to improve the quality of induced pluripotent stem cell technology, a tool that allows scientists to harvest skin cells from mentally ill patients and convert them into neurons. By building a neural model of schizophrenia using patient cells, scientists hope to gain new insights into the underlying mechanisms of the disease in order to develop more targeted treatments.
Dr. Manji believes that such innovative projects will not only lead to new treatments for schizophrenia, but also approaches to delay and possibly even prevent the disease.
“We now know that schizophrenia, like many other diseases, does not strike people overnight,” he explains. “It matures before a person develops full-blown psychosis, and the sooner treatment is started, the better the long-term prognosis will be.
If we learn to identify people at high risk of developing schizophrenia and learn what happens to them at the earliest stages, then in the long run we can change the entire trajectory of the disease.