Hallucinations vs delusions examples
Hallucinations vs. Delusions: What’s the Difference?
Hallucinations vs. Delusions: What’s the Difference?Medically reviewed by Joslyn Jelinek, LCSW — By Jaime Herndon, MS, MPH, MFA on June 4, 2021
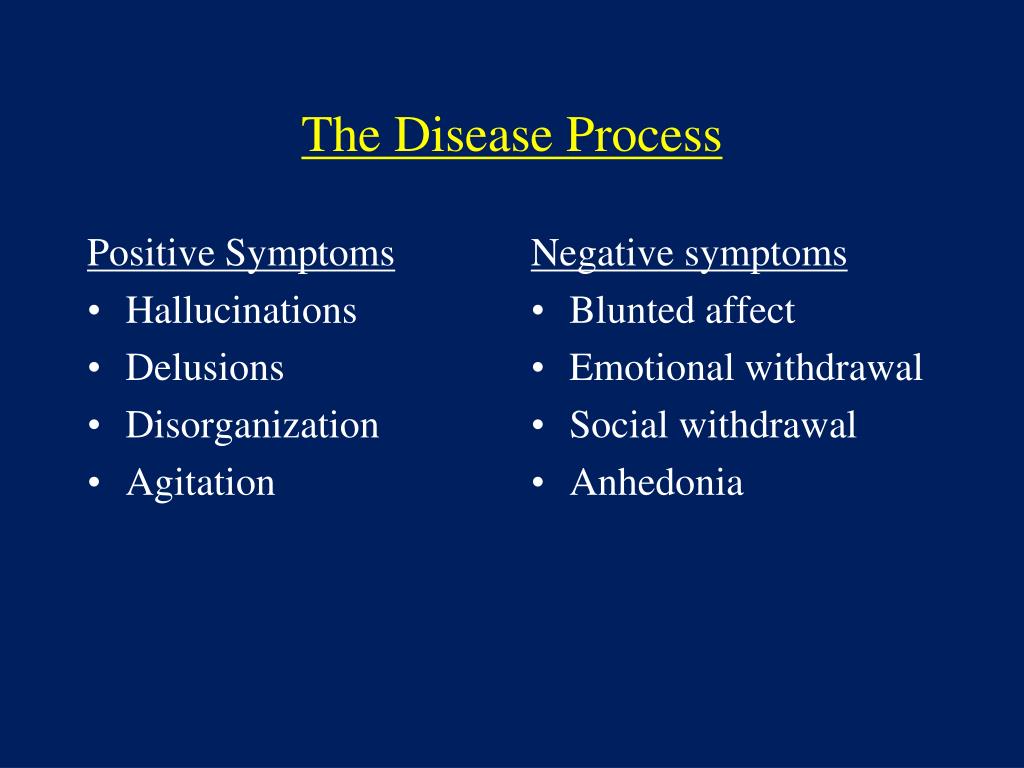
Symptoms of psychosis like hallucinations and delusions often overlap. This means it can be easy to get them mixed up. Although they’re both symptoms of psychosis and are part of an altered reality, the two symptoms have one major difference — one is sensory, and one is cognitive.
Knowing the difference between the two can help differentiate symptoms and get the appropriate treatment. In this article, we’ll compare hallucinations and delusions, including what causes them and how they’re treated.
Hallucinations and delusions are often grouped together when talking about various illnesses or conditions, but they’re not the same. While both of them are part of a false reality, a hallucination is a
sensory perception and a delusion is a false belief.
For instance, hallucinations can involve seeing someone who isn’t there or hearing people talking when there is no one around. Delusions, on the other hand, can involve someone thinking they are a celebrity when they’re not, for example.
Sometimes illnesses or medical conditions can cause hallucinations and/or delusions, or even psychosis. These illnesses can include:
- Parkinson’s disease
- Huntington’s disease
- brain tumors
- certain forms of dementia, like Alzheimer’s disease
- syphilis
- HIV
- some forms of epilepsy
- stroke
- substance use or withdrawal
Knowing the underlying causes of hallucinations and/or delusions is important, since an accurate diagnosis will help guide treatment.
Hallucinations are sensory experiences that one perceives as real when they’re actually not. They can be caused by medications, substance use, or certain medical or mental health conditions.
Hallucinations can be visual, olfactory (your sense of smell), gustatory (taste), auditory, or tactile.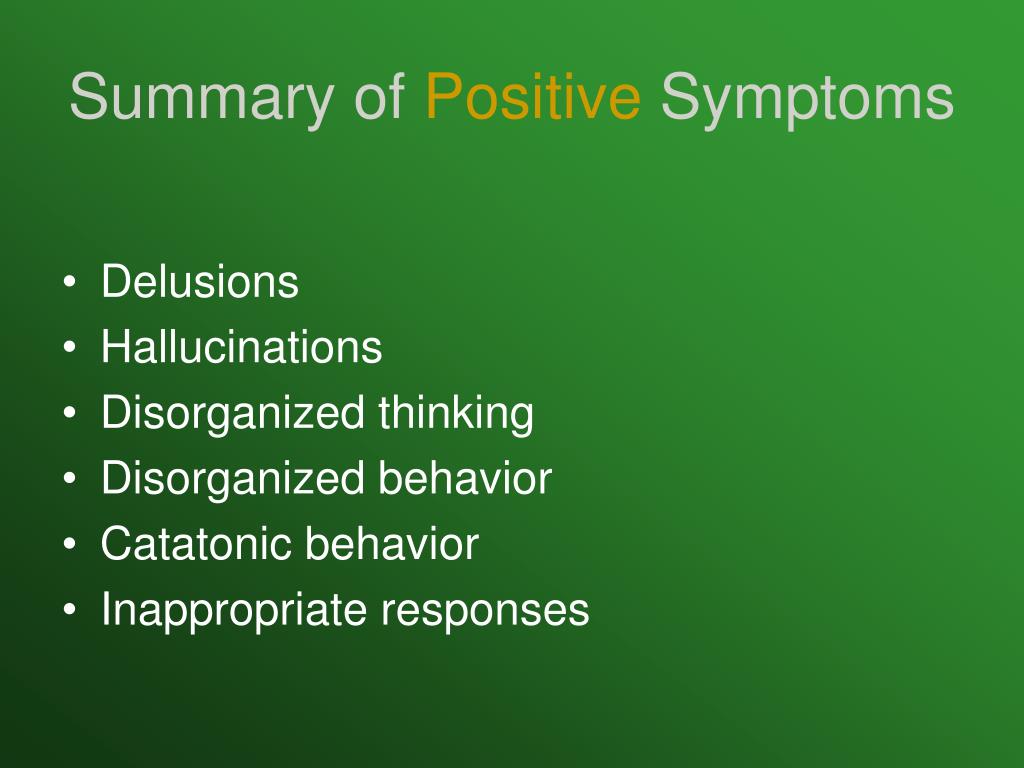 Someone might think they feel bugs on their skin, hear someone talking to them, see something that isn’t there, or even smell something that isn’t present.
Someone might think they feel bugs on their skin, hear someone talking to them, see something that isn’t there, or even smell something that isn’t present.
Medical conditions that can cause hallucinations can include:
- substance use
- mental illness
- lack of sleep
- medications
- migraine
- seizures
- social isolation
- deafness, blindness, or vision problems
- epilepsy
- high fevers
Delusions are beliefs that are obviously false. They’re symptoms of a disturbance in thinking.
The belief in a delusion isn’t accounted for by cultural or religious background. They also have nothing to do with the intelligence of the person who believes them. These beliefs are held even with evidence of the contrary and despite what almost everyone else thinks.
Delusions can be about almost anything, but common types of delusions include:
- delusion of persecution
- delusion of infidelity
- delusions of love
- delusions of grandeur
- religious delusions
- delusions of guilt or unworthiness
- nihilistic delusions
Conditions that may cause delusions can include:
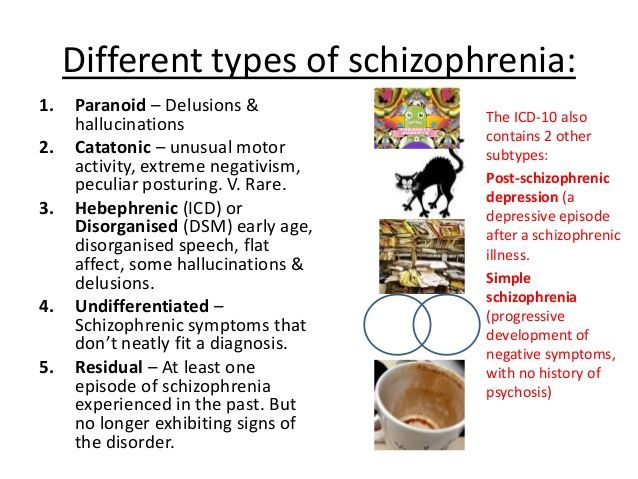
- schizophrenia
- affective psychosis, like in bipolar psychosis
- delusional disorder
Is hearing voices a hallucination or a delusion?
Hearing voices is a hallucination.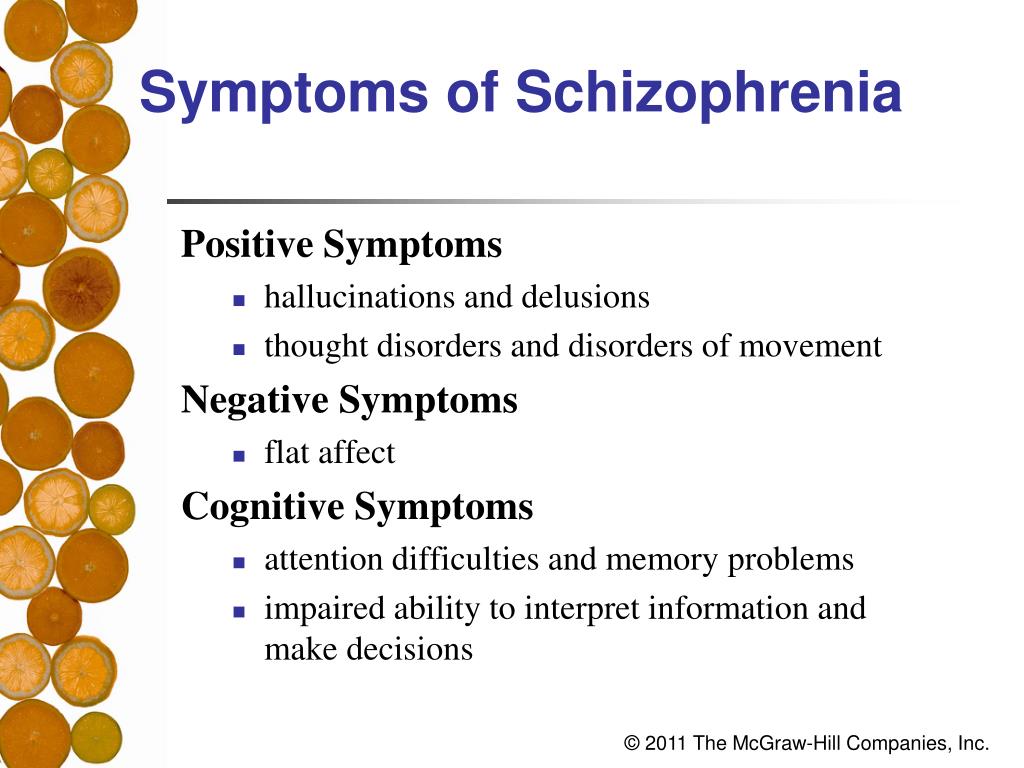 This is because hearing voices a sensory experience that isn’t real.
This is because hearing voices a sensory experience that isn’t real.
Delusions are beliefs, not experiences, so hearing voices would not be a delusion. A delusion would be someone believing that a person wants to hurt them, not simply hearing a voice.
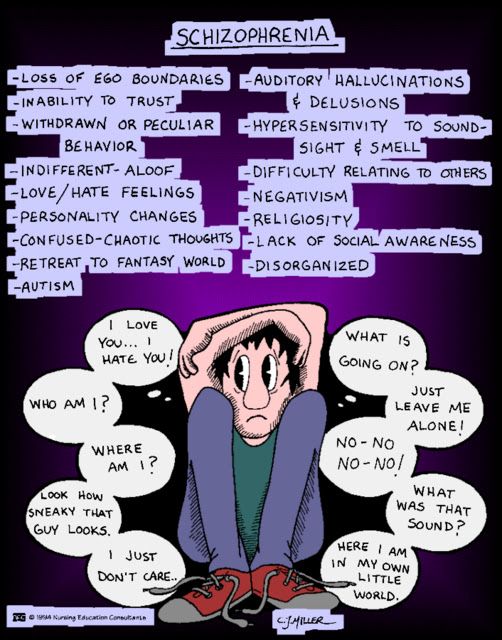
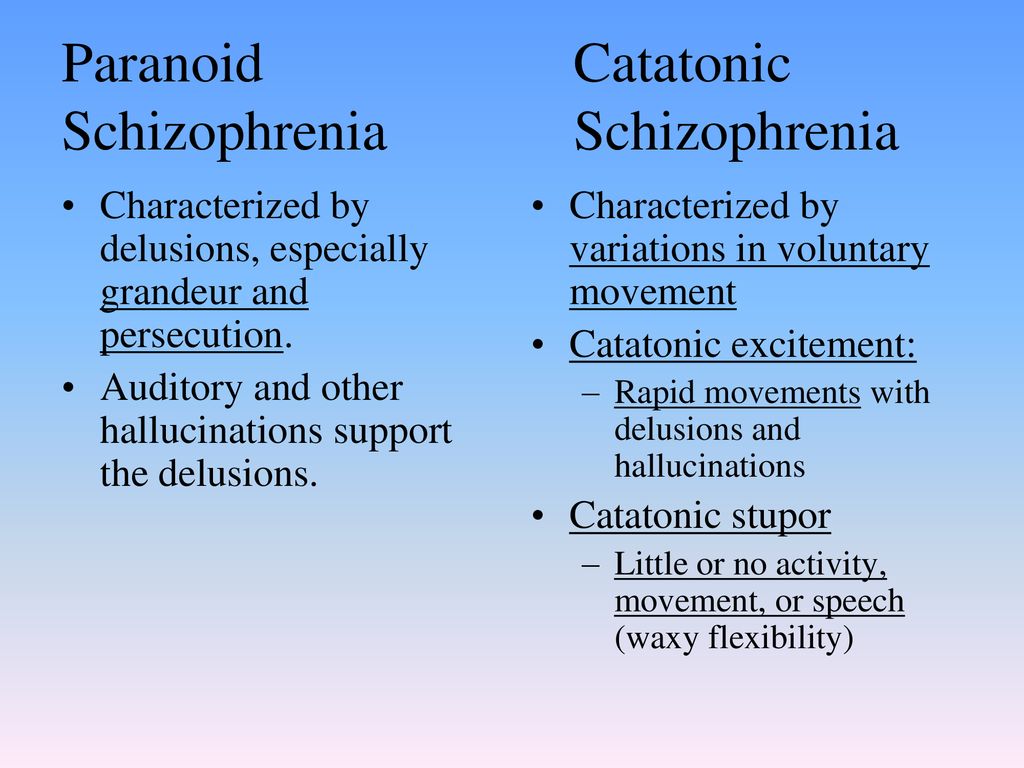
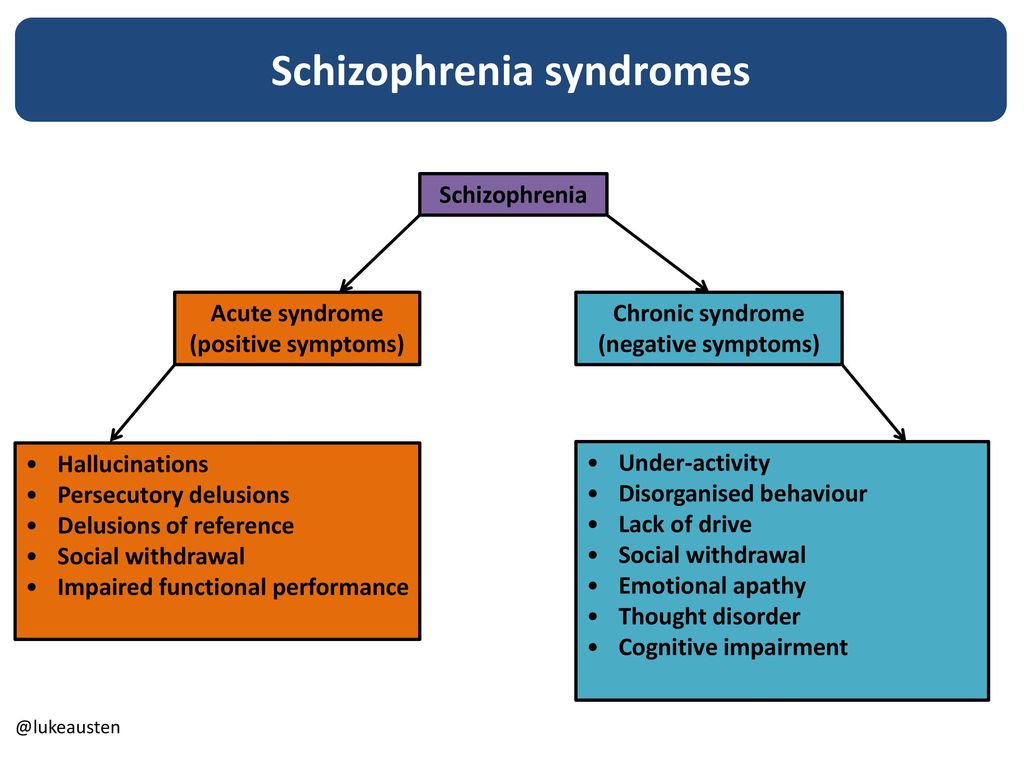
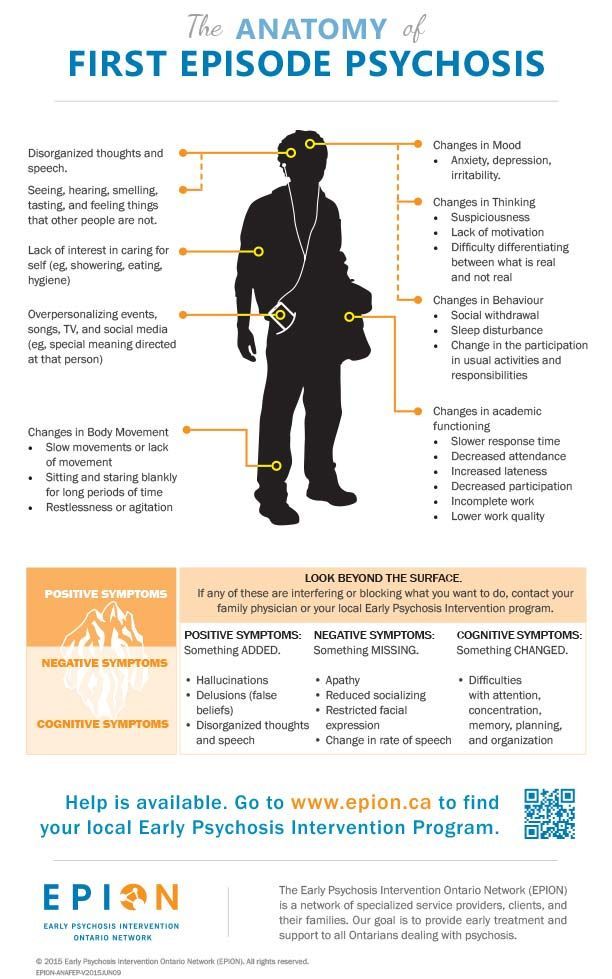
In schizophrenia, an individual appears to have lost touch with reality. It’s often diagnosed after a psychotic episode, which can include hallucinations and delusions.
While these are often symptoms of schizophrenia, hallucinations and delusions present with other symptoms like:
- flat affect
- difficulty with everyday functioning
- problems with thinking and memory
What is psychosis?
Psychosis is when a person has lost contact with reality. The person has disturbances in thinking and perception, and they may not know what’s real and what isn’t.
Hallucinations and delusions are often symptoms of psychosis. This is because they represent breaks with reality.
Treatment for hallucinations depends on what’s causing them.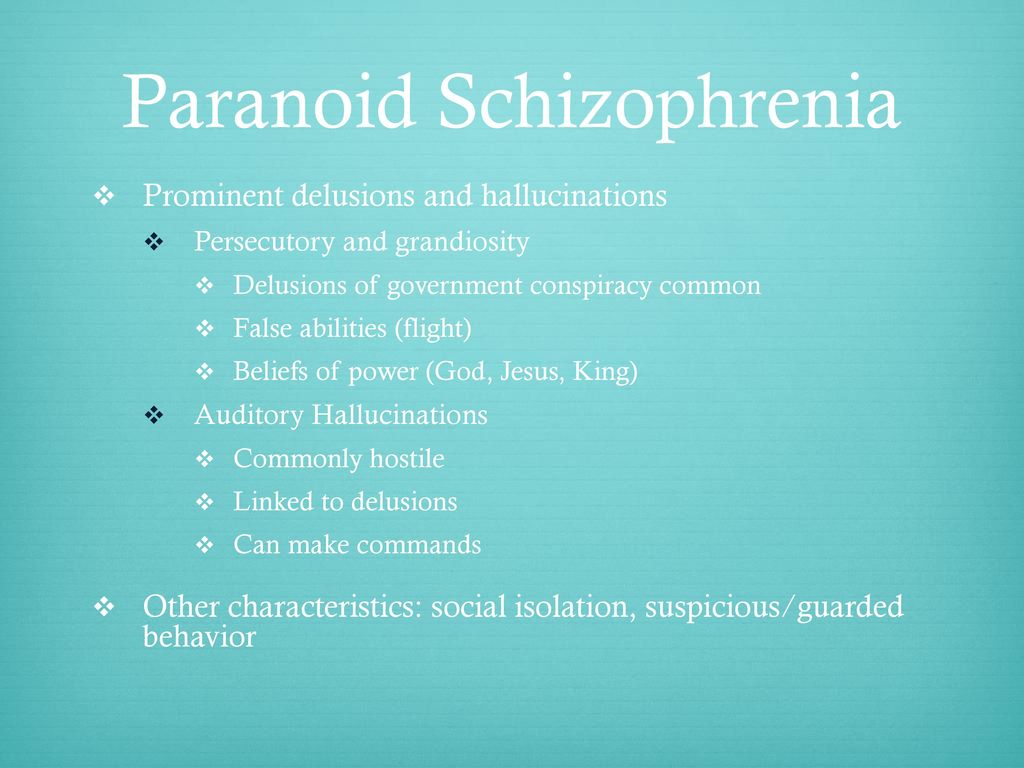 Medications may be used, along with counseling.
Medications may be used, along with counseling.
The specific medication that will be prescribed depends on what the hallucinations are a symptom of. Counseling can help you with insight into what you’re experiencing and work with you to develop coping strategies.
If the hallucinations are because of a medication, your doctor may reduce the dosage of that medication or discontinue it.
Cognitive-behavioral therapy (CBT) is an effective way to treat delusions. CBT therapy is a process that involves building a relationship with a mental health professional, recognizing how delusions are affecting you, and implementing CBT strategies.
If the delusions are part of psychosis, CBT is often used together with antipsychotic drugs.
It can be easy to confuse hallucinations and delusions. Both are symptoms of psychosis, and indicate a break from reality. They also often occur together.
But though the two are related, hallucinations and delusions each have their own unique symptoms.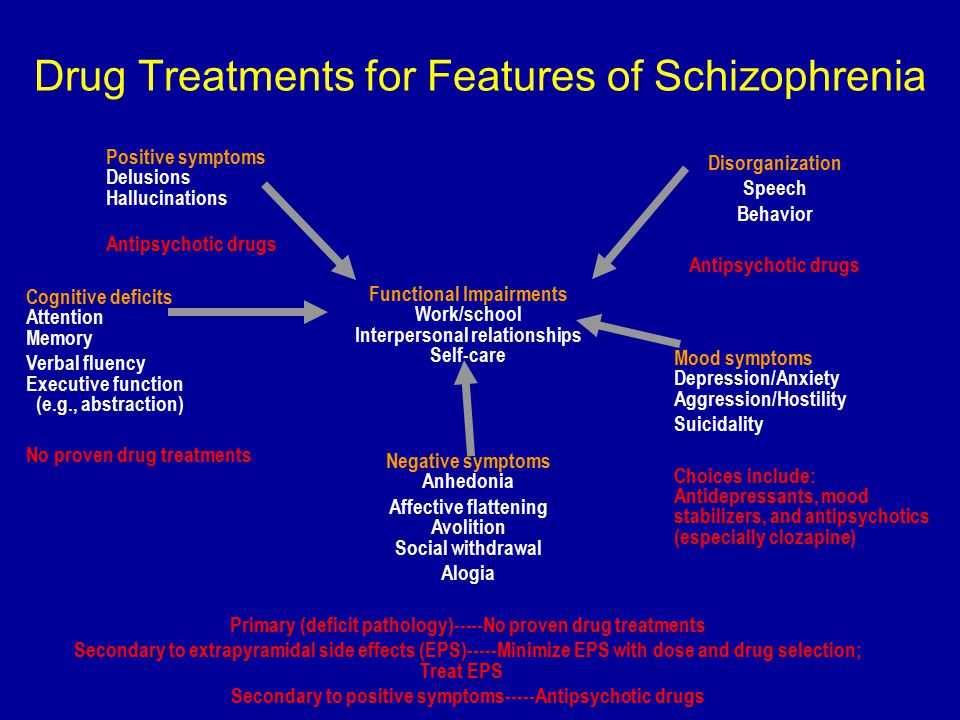 Hallucinations indicate more of a sensory experience, and delusions are a false belief.
Hallucinations indicate more of a sensory experience, and delusions are a false belief.
There are ways to help treat and manage hallucinations and delusions. With medication and therapy, an individual can manage their symptoms appropriately.
If you or a loved one are living with hallucinations or delusions, talk with your doctor. They can help you with next steps to get help, or refer you to a mental health professional who has more specialization and can provide the support you need.
Last medically reviewed on June 4, 2021
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Bell V, et al. (2021). Derationalizing delusions.
ncbi.nlm.nih.gov/pmc/articles/PMC7820571/ - Health Quality Ontario.
 (2018). Cognitive behavioural therapy for psychosis: A health technology assessment.
(2018). Cognitive behavioural therapy for psychosis: A health technology assessment.
ncbi.nlm.nih.gov/pmc/articles/PMC6235075/ - Lancellotta E, et al. (2019). Are clinical delusions adaptive?
ncbi.nlm.nih.gov/pmc/articles/PMC6899558/ - Schizophrenia. (2020).
nimh.nih.gov/health/topics/schizophrenia/ - Steps for working with delusions. (2021).
bcss.org/support/how-do-i-get-help-for-my-loved-one/steps-working-delusions/ - What is psychosis? (n.d.).
nimh.nih.gov/health/topics/schizophrenia/raise/what-is-psychosis
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Jun 4, 2021
Written By
Jaime R. Herndon, MS, MPH, MFA
Edited By
Debbie Nurmi
Medically Reviewed By
Joslyn Jelinek, LCSW, CYT
Copy Edited By
Connor Rice
Share this article
Medically reviewed by Joslyn Jelinek, LCSW — By Jaime Herndon, MS, MPH, MFA on June 4, 2021
Read this next
Everything You Need to Know About Hallucinations
Medically reviewed by Timothy J.
 Legg, PhD, PsyD
Legg, PhD, PsyDHallucinations are sensations that appear real but are created by your mind. They can affect all of your senses. Learn about the types, causes, and…
READ MORE
All About Closed-Eye Hallucinations
Medically reviewed by Ann Marie Griff, O.D.
Closed-eye hallucinations are the shapes and colors you may see when you shut your eyes. They're typically harmless and not a cause for concern…
READ MORE
Psychosis
Medically reviewed by Karin Gepp, PsyD
Psychosis is a serious mental disorder characterized by a disconnect from reality. We’ll explain the symptoms and causes as well as risk factors.
READ MORE
Does Bipolar Disorder Cause Hallucinations?
Medically reviewed by Timothy J. Legg, PhD, PsyD
Hallucinations tend to be associated with mental conditions, like schizophrenia.
 But people with bipolar disorder can have them too.
But people with bipolar disorder can have them too.READ MORE
What Is Hallucinogen Persisting Perception Disorder (HPPD)?
Medically reviewed by Nicole Washington, DO, MPH
Although rare, some people who've taken hallucinogens develop hallucinogen persisting perception disorder (HPPD), a sensory disorder. Learn more.
READ MORE
OCD and Kids: Video Games, Screen Time Linked to Compulsive Behavior
New research suggests there may be a link between the number of hours a child spends playing video games and their risk of developing…
READ MORE
Holiday Stress: Why Now May be the Best Time to Treat Yourself
New research finds that self-gifting (or treating yourself) can help reduce stress and increase your happiness.
READ MORE
What Is Nonverbal Learning Disorder?
Medically reviewed by Nicole Washington, DO, MPH
If you suspect you or your child has NVLD, consider speaking with a mental health professional.
READ MORE
Understanding the Link Between Suicide and Chronic Pain
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Studies have shown that suicidal thoughts can be connected to living with chronic pain. Let's look at why and what resources can support you.
READ MORE
How Silly Distractions at Work Can Boost Your Happiness and Focus
A new study finds that taking a positive work break, like watching a funny video on your computer, can recharge your mood and improve your focus.
READ MORE
What’s the Difference Between a Delusion and a Hallucination? – BrightQuest Treatment Centers
Hallucinations and delusions are similar in that they are both false but seem very real to the person experiencing them.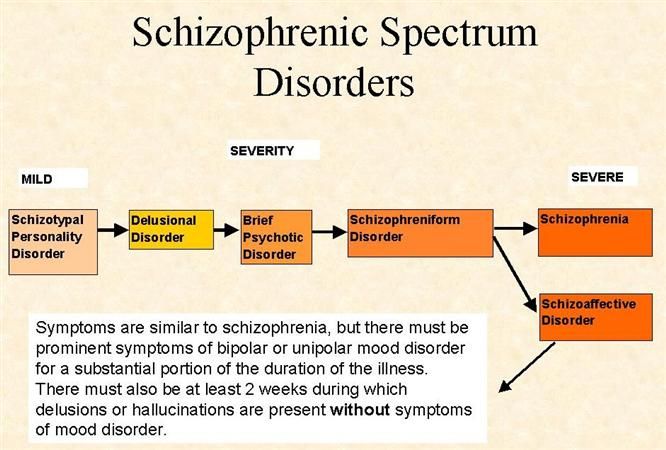 Both are caused by certain mental illnesses but can also be triggered by medical conditions, injuries, or by no known cause at all. A hallucination involves the senses and feels real but is not. A delusion is a false belief that persists in spite of evidence. Neither is always cause for concern, but when experienced should lead to medical and mental health evaluations.
Both are caused by certain mental illnesses but can also be triggered by medical conditions, injuries, or by no known cause at all. A hallucination involves the senses and feels real but is not. A delusion is a false belief that persists in spite of evidence. Neither is always cause for concern, but when experienced should lead to medical and mental health evaluations.
Delusions and hallucinations are similar but also have some significant differences. Both are often caused by the same mental illnesses, like schizophrenia or bipolar disorder; both involve distortions in reality; and both can occur even in the absence of mental illness.
The differences are that hallucinations are things that are sensed but not real, while delusions are beliefs that are not real or correct.
Hallucinations vs. Delusions
Both hallucinations and delusions are characteristic symptoms of psychosis and mental illnesses that can trigger psychotic episodes, such as schizophrenia.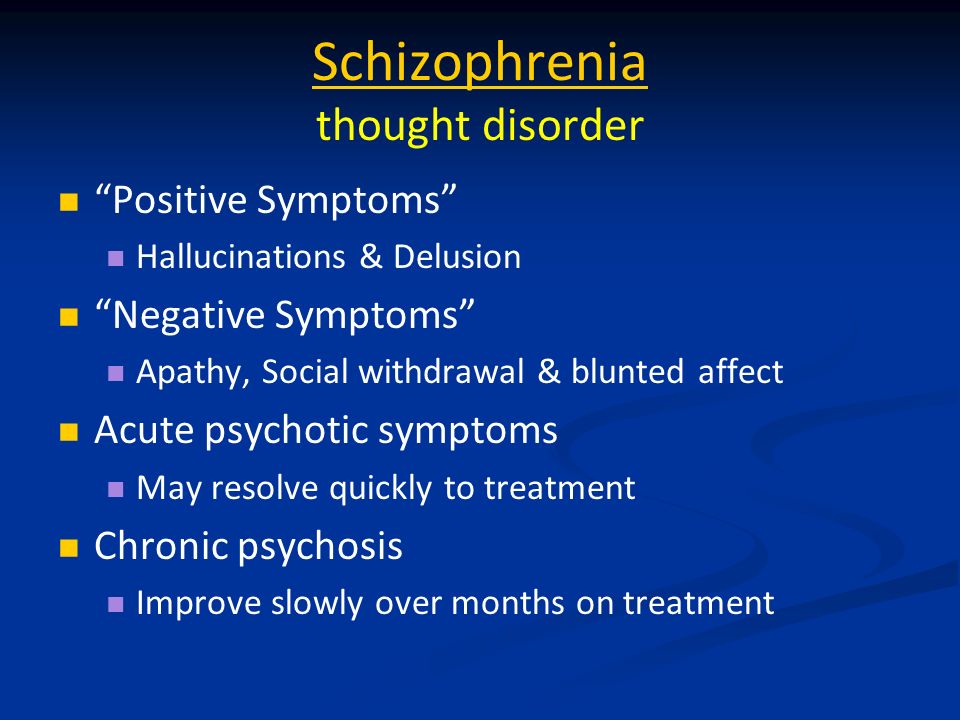 However, there are also other causes and triggers, including physical medical conditions. While one episode of a delusion or a single hallucination may not indicate any serious underlying condition, either one should be checked out and evaluated by a medical doctor or mental health professional.
However, there are also other causes and triggers, including physical medical conditions. While one episode of a delusion or a single hallucination may not indicate any serious underlying condition, either one should be checked out and evaluated by a medical doctor or mental health professional.
A hallucination is anything that is sensed—heard, seen, felt, or even smelled—that is not real. The person experiencing a hallucination may believe that it is real, and everything about the vision, sound, voice, or other sensation seems very real.
The definition of delusion is a little different, although it also involves the experience of something that feels real but isn’t. A delusion is a belief that is obviously false, and yet the individual experiencing it thinks it is absolutely true. A delusion is not a belief that is false because of a person’s intelligence, education, culture, religion, or other similar factor; instead, it is false because it of some abnormality in the individual’s thinking.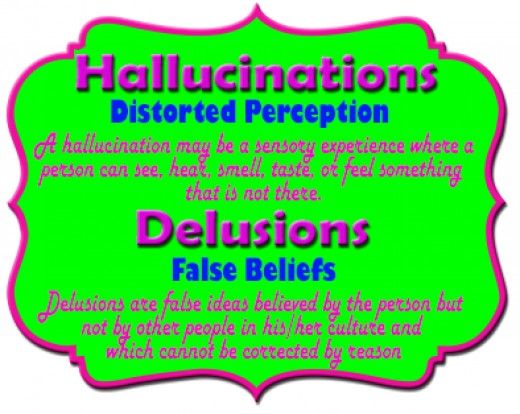 That person will firmly believe in the delusion even when repeatedly shown evidence to the contrary.
That person will firmly believe in the delusion even when repeatedly shown evidence to the contrary.
Both hallucinations and delusions are disturbances in reality. They are experiences that seem real to the observer but are not real. One difference is that a person experiencing a hallucination may realize it is not true—for instance, when a migraine causes an aura or lines in the vision. When caused by a mental illness, hallucinations and delusions often occur together.
Recent research has determined that as many as one in 20 people have hallucinations that are not caused by drug use, alcohol, dreams, or psychotic disorders. The study also found that about six percent of people have experienced hallucinations or delusions and that hallucinations are much more common.
Examples of Hallucinations
A hallucination can literally be anything related to the senses, and different people with the same condition can experience something totally unique. There are some common types of hallucinations, though, including:
- A crawling feeling on the skin
- Hearing ordinary sounds that aren’t there, like doors closing or footsteps
- Hearing voices, including those that command a person to do something
- Seeing lights or patterns
- A sensation of floating or being outside one’s body
- Smelling an odor for which there is no explanation; this is rare
Begin Your Recovery Journey Today.
 619-466-0547
619-466-0547 Examples of Delusions
Any persistent and false belief may be a delusion, but as with hallucinations there are some common types and categories of delusions, most often triggered by a mental illness or psychotic episode:
- Persecutory. These are delusions in which a person believes someone is out to get them or is mistreating them.
- Grandiose. A grandiose delusion is any belief relating to having special powers, relationships with someone important or famous, or having exceptional talents or abilities.
- Jealous. Delusions of jealousy involve believing a partner is being unfaithful.
- Somatic. A false belief that one is sick or physically disabled is somatic.
- Bizarre. Delusions are often non-bizarre, meaning they could be true but aren’t. Bizarre delusions are those that could not be true, such as believing someone is controlling one’s mind.
Getting Help for Hallucinations or Delusions
There is evidence that perfectly healthy people sometimes experience hallucinations and less commonly delusions. However, if you have other symptoms, or these sensations or false beliefs persist, it is important to seek medical or mental health care. A doctor can rule out any medical conditions, while a mental health professional can screen for and diagnose an underlying mental illness. If there is a mental illness causing the symptoms, a thorough treatment plan that may involve medications and therapy can help.
We are here to listen compassionately. Our free, confidential telephone consultation will help you find treatment that will work for you, whether it is with us or a different program.
We can guide you in approaching a loved one who needs treatment.
We're here to listen
Call us today at
619-466-0547
FGBNU NTsPZ.
< Paranoid syndrome.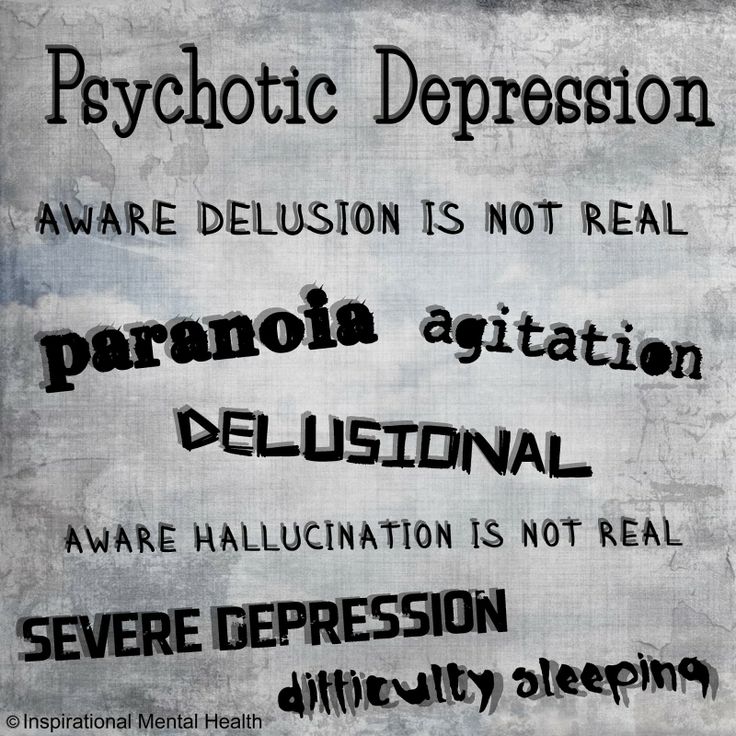 Primary systematized delusions of interpretation of various content (jealousy, inventions, persecution, reformism, etc.), often existing as a monosymptom in the complete absence of other productive disorders. If the latter arise, then they are located on the periphery of the paranoid structure and subject to it in plot. Paralogical structure of thinking ("crooked thinking"), delusional detailing are characteristic. The ability to make correct judgments and inferences on issues that do not affect delusional beliefs is not noticeably impaired, which indicates catathymic (that is, associated with an unconscious complex of affectively colored representations, and not a general change in mood) mechanisms of delusional formation. There may be memory impairments in the form of delusional confabulations (“memory hallucinations”). There are, in addition, hallucinations of the imagination, the content of which is associated with dominant experiences. As the delusion expands, an ever wider range of phenomena becomes the object of pathological interpretations.
Primary systematized delusions of interpretation of various content (jealousy, inventions, persecution, reformism, etc.), often existing as a monosymptom in the complete absence of other productive disorders. If the latter arise, then they are located on the periphery of the paranoid structure and subject to it in plot. Paralogical structure of thinking ("crooked thinking"), delusional detailing are characteristic. The ability to make correct judgments and inferences on issues that do not affect delusional beliefs is not noticeably impaired, which indicates catathymic (that is, associated with an unconscious complex of affectively colored representations, and not a general change in mood) mechanisms of delusional formation. There may be memory impairments in the form of delusional confabulations (“memory hallucinations”). There are, in addition, hallucinations of the imagination, the content of which is associated with dominant experiences. As the delusion expands, an ever wider range of phenomena becomes the object of pathological interpretations.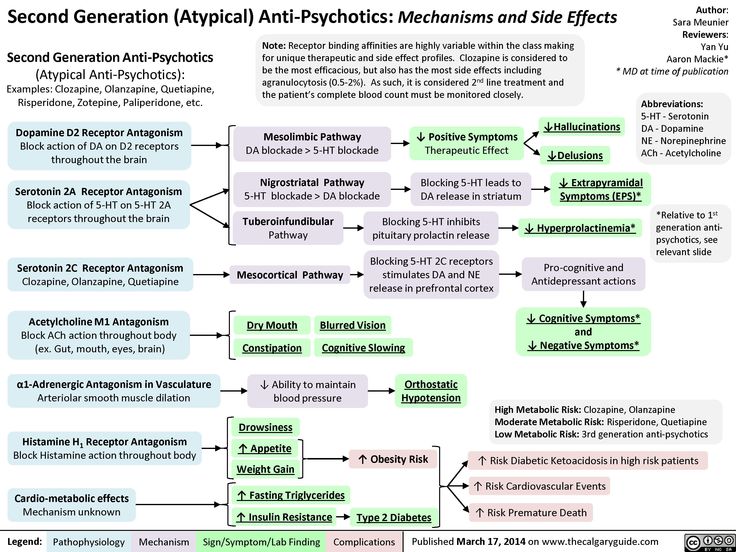 There is also a delusional interpretation of past events. Paranoid syndrome usually occurs against the background of a slightly elevated mood (expansive delusions) or subdepression (sensitive, hypochondriacal delusions). The content of delirium at the remote stages of development may acquire a megalomaniac character. Unlike paraphrenia, delirium continues to be interpretive and, in terms of its scope, does not go beyond what is fundamentally possible in reality (“prophets, outstanding discoverers, brilliant scientists and writers, great reformers,” etc.). There are chronic, existing for a number and even decades, and acute variants of the paranoid syndrome. Chronic paranoid delusions are most often observed with relatively slowly developing delusional schizophrenia. Delusions in such cases are usually monothematic. The possibility that there is an independent form of the disease, paranoia, is not excluded. Acute, usually less systematized paranoid states occur in the structure of attacks of fur-like schizophrenia.
There is also a delusional interpretation of past events. Paranoid syndrome usually occurs against the background of a slightly elevated mood (expansive delusions) or subdepression (sensitive, hypochondriacal delusions). The content of delirium at the remote stages of development may acquire a megalomaniac character. Unlike paraphrenia, delirium continues to be interpretive and, in terms of its scope, does not go beyond what is fundamentally possible in reality (“prophets, outstanding discoverers, brilliant scientists and writers, great reformers,” etc.). There are chronic, existing for a number and even decades, and acute variants of the paranoid syndrome. Chronic paranoid delusions are most often observed with relatively slowly developing delusional schizophrenia. Delusions in such cases are usually monothematic. The possibility that there is an independent form of the disease, paranoia, is not excluded. Acute, usually less systematized paranoid states occur in the structure of attacks of fur-like schizophrenia. At the same time, the delusional concept is loose, unstable and may have several different themes or centers of crystallization of false judgments. nine0005
At the same time, the delusional concept is loose, unstable and may have several different themes or centers of crystallization of false judgments. nine0005
Some authors consider it justified to distinguish between paranoid and paranoid syndromes (Zavilyansky et al., 1989). Paranoid refers to chronic systematized overvalued delusions (starting with overvalued ideas), arising under the influence of a key traumatic situation for the patient. Paranoid and epileptoid features of a premorbid personality of constitutional, post-procedural or organic genesis have the development of delirium. The mechanisms of delusional formation are associated with psychological rather than biological disorders "psychogenic-reactive" delusional formation. Paranoid syndrome in this interpretation is appropriate to consider in the framework of the pathological development of personality. nine0005
Paranoid or hallucinatory-paranoid syndrome. Includes delusional ideas of persecutory content, hallucinations, pseudohallucinations and other phenomena of mental automatism, affective disorders.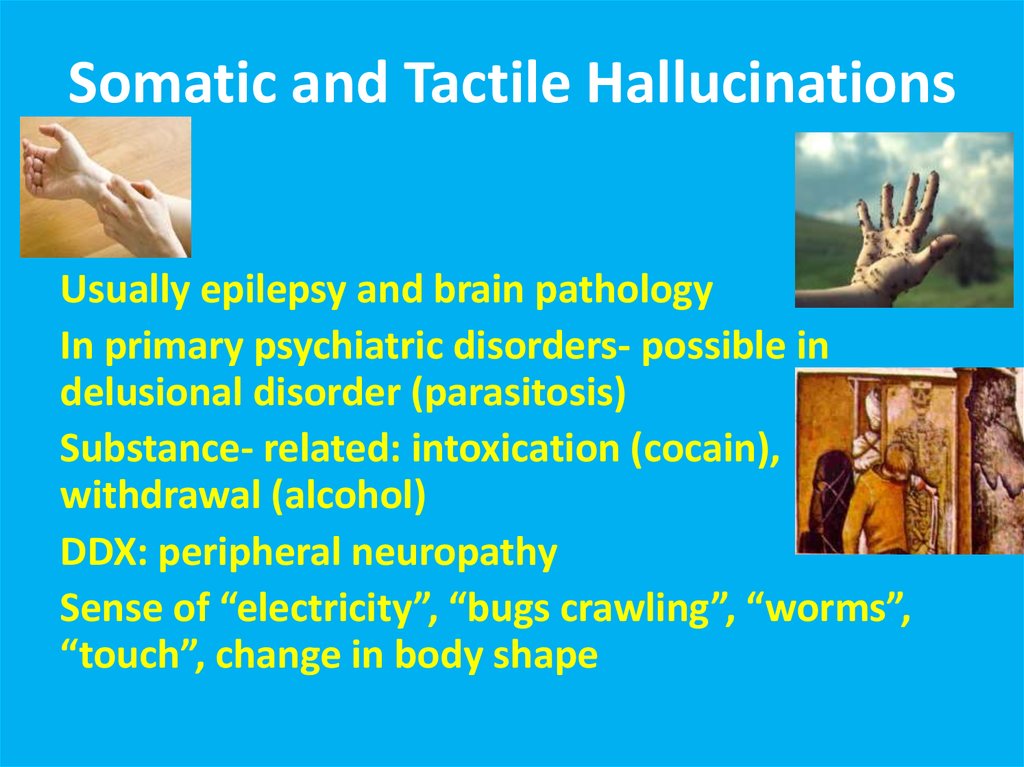 There are acute and chronic hallucinatory-paranoid syndromes.
There are acute and chronic hallucinatory-paranoid syndromes.
Acute paranoid acute sensory delusions of persecution (in the form of delusions of perception) of a specific direction, accompanied by verbal illusions, hallucinations, fear, anxiety, confusion, incorrect behavior, reflecting the content of delusional ideas. It is observed in schizophrenia, intoxication, epileptic psychoses. Acute paranoid states can also occur in special situations (long journeys associated with insomnia, alcohol intoxication, emotional stress, somatogeny) road or situational paranoids described by S. G. Zhislin. nine0005
Acute hallucinatory-paranoid syndrome is an acute sensory delusion of persecutory content that occurs against the background of fear, confusion and is combined with pseudohallucinations and other phenomena of mental automatism. It is more common in the structure of attacks of fur-like schizophrenia, with atypical alcoholic psychoses.
Chronic hallucinatory-paranoid syndrome (synonyms: Kandinsky-Clerambault syndrome, other eponyms, mental automatism syndrome, intrusion syndrome, deposition syndrome, xenopathic syndrome, parasitism syndrome, influence syndrome, external influence syndrome, alienation syndrome, mastery syndrome, polyphrenia, nuclear syndrome) the difference in the names reflects the dissimilarity in the opinions of their authors regarding what violations should be considered determining the structure of the syndrome: mental automatisms, self-awareness disorders, the experience of openness or delusional ideas of physical and mental influence.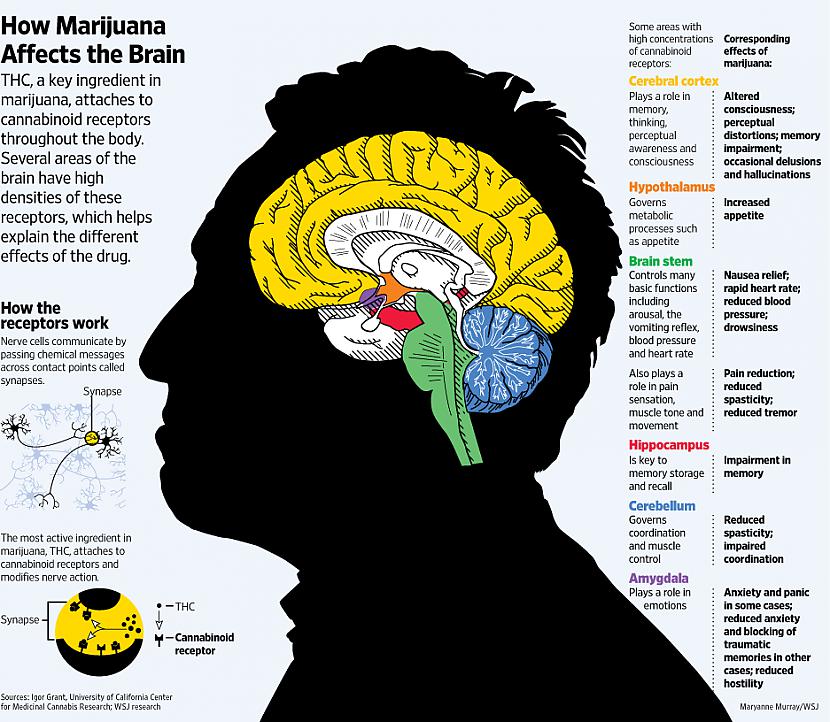 nine0005
nine0005
Psychic automatisms in their completed form represent the experience of violence, intrusion, doneness of one's own mental processes, behavior, physiological acts. There are the following types of mental automatisms.
Associative or ideational automatism disorders of mental activity, memory, perception, affective sphere, proceeding with the experience of alienation and violence: influxes of thoughts, non-stop flow of thoughts, states of blockade of mental activity, symptoms of insertion, reading thoughts, a symptom of unwinding memories, pseudo-hallucinatory pseudo-memories, sudden delays in memories, phenomena of figurative mentism, etc. Manifestations of ideational automatism include, in addition, auditory and visual pseudo-hallucinations, as well as a number of affective disorders: “made” mood, “induced” fear, anger, ecstasy, “caused” sadness or indifference and others. "Done" dreams adjoin this group of automatisms. The inclusion of auditory verbal and visual pseudo-hallucinations in the group of ideational automatisms is due to their close connection with the processes of thinking verbal pseudo-hallucinations with verbal, and visual with figurative forms of thinking. nine0005
nine0005
Senestopathic or sensory automatism - a variety of senestopathic sensations, the appearance of which patients associate with the influence of external forces. In addition, this includes olfactory, gustatory, tactile and endosomatic pseudohallucinations. Sensory automatism includes various changes in appetite, taste, smell, sexual desire and physiological needs, as well as sleep disturbances, vegetative disorders (tachycardia, excessive sweating, vomiting, diarrhea, etc.), "caused", according to patients, from outside . nine0005
Kinesthetic or motor automatism urges to activity, individual movements, actions, deeds, expressive acts, hyperkinesis arising from the experience of violence. Receptive processes can also proceed with the phenomena of doneness: “They make you look, listen, smell, look with my eyes”, etc.
Speech-motor automatism phenomena of forced speaking, writing, as well as kinesthetic, verbal and graphic hallucinations.
The formation of psychic automatisms takes place in a certain sequence.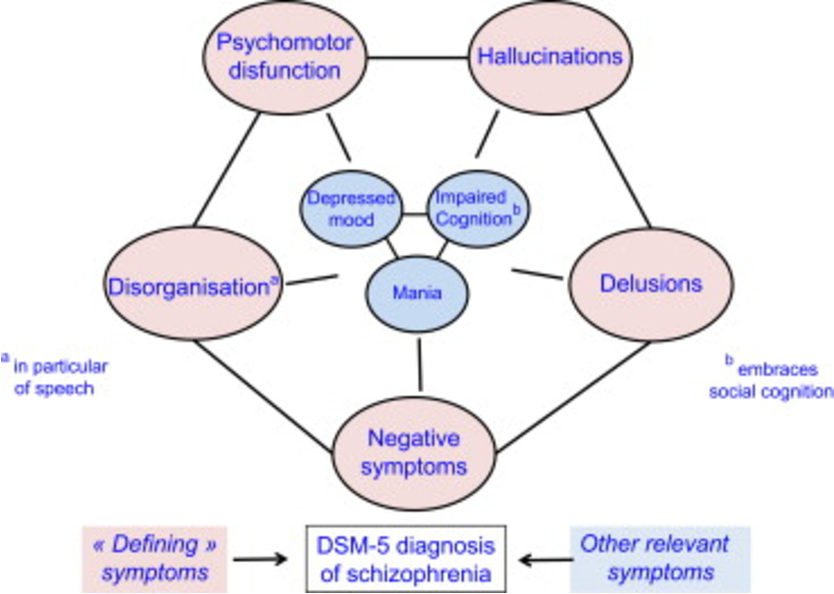 At the first stage of the development of ideator automatism, “strange, unexpected, wild, parallel, intersecting” thoughts appear, alien in content to the entire personality structure: “I never think like that”. At the same time, sudden interruptions of necessary thoughts may occur. Alienation concerns the content of thoughts, but not the process of thinking itself (“thoughts are mine, only very strange ones”). Then the feeling of one's own activity of thinking is lost: “Thoughts float, go on their own, flow non-stop” or there are states of blockade of mental activity. In the future, alienation becomes total the feeling of belonging to one’s own thoughts is completely lost: “The thoughts are not mine, someone thinks in me, in the head the thoughts of other people ”. Finally, there is a feeling that the thoughts “Come from outside, are introduced into the head, invested”. There are "telepathic" contacts with other people, the ability to directly read the thoughts of others, mentally communicate with others.
At the first stage of the development of ideator automatism, “strange, unexpected, wild, parallel, intersecting” thoughts appear, alien in content to the entire personality structure: “I never think like that”. At the same time, sudden interruptions of necessary thoughts may occur. Alienation concerns the content of thoughts, but not the process of thinking itself (“thoughts are mine, only very strange ones”). Then the feeling of one's own activity of thinking is lost: “Thoughts float, go on their own, flow non-stop” or there are states of blockade of mental activity. In the future, alienation becomes total the feeling of belonging to one’s own thoughts is completely lost: “The thoughts are not mine, someone thinks in me, in the head the thoughts of other people ”. Finally, there is a feeling that the thoughts “Come from outside, are introduced into the head, invested”. There are "telepathic" contacts with other people, the ability to directly read the thoughts of others, mentally communicate with others. At the same time, patients may claim that at times they are deprived of the ability to think or "pull out thoughts", "steal". nine0005
At the same time, patients may claim that at times they are deprived of the ability to think or "pull out thoughts", "steal". nine0005
Verbal pseudo-hallucinations may develop in the following way. At first, the phenomenon of sounding one’s own thoughts arises: “Thoughts rustle, sound in the head.” Then your own voice begins to be heard in your head, repeating the thoughts. This could be called hallucinations of inner speech. The content of statements is gradually expanding (statings, comments, advice, orders, etc.), while the voice "doubles, multiplies". Further, "alien voices" are heard in the head. The content of their statements is becoming more and more diverse, divorced from reality and the personality of patients. In other words, the alienation of the process of internal speaking also grows in a certain sequence. Finally, the phenomenon of "made, induced voices" arises. At the same time, the voices speak on a variety of topics, often abstracted from personal experiences, sometimes they convey absurd and fantastic information: “The voices behind the ears speak on local topics, and in the head on state ones.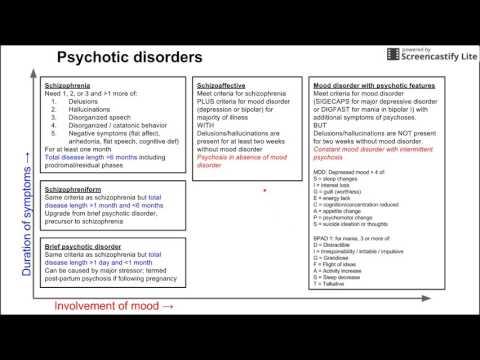 ” The degree of alienation of what is said by voices can therefore be different. nine0005
” The degree of alienation of what is said by voices can therefore be different. nine0005
The dynamics of kinesthetic automatism generally corresponds to those described above. Initially, previously unusual impulses for action, impulsive inclinations appear, strange and unexpected actions and deeds are committed for the patients themselves. Subjectively, they are perceived as belonging to one's own personality, although they are unusual in content. There may be short action stops. Subsequently, actions and deeds are performed without a sense of one's own activity, involuntarily: "I do it without noticing it, and when I notice it, it's hard to stop." There are states of blockade or "paralysis" of impulses to action. At the next stage, activity proceeds with a distinct experience of alienation of one’s own activity and violence: “Something is pushing from the inside, prompting, not a voice, but some kind of internal force”. Interruption episodes are also experienced with a touch of violence. At the final stage of the development of motor automatisms, there is a feeling that motor acts are done from the outside: “My body is controlled Someone controls my hands One hand belongs to my wife, the other to my stepfather, my legs mine Looks through my eyes”. With the feeling of external influence, the states of blockade of impulses to action proceed. nine0005
At the final stage of the development of motor automatisms, there is a feeling that motor acts are done from the outside: “My body is controlled Someone controls my hands One hand belongs to my wife, the other to my stepfather, my legs mine Looks through my eyes”. With the feeling of external influence, the states of blockade of impulses to action proceed. nine0005
The sequence of development of speech-motor automatisms can be similar. At first, separate words or phrases are broken that are alien to the direction of the patient's thoughts, absurd in content. Often, individual words are suddenly forgotten or the formulation of thoughts is disturbed. Then the feeling of one’s own activity that accompanies speech is lost: “The language speaks by itself, I will say, and then the meaning of what was said Sometimes I start talking”, Or for a short time, the “language” stops, does not obey. Further, a feeling of alienation and violence arises in relation to one's own speech: “It is as if it is not I who speak, but something in me.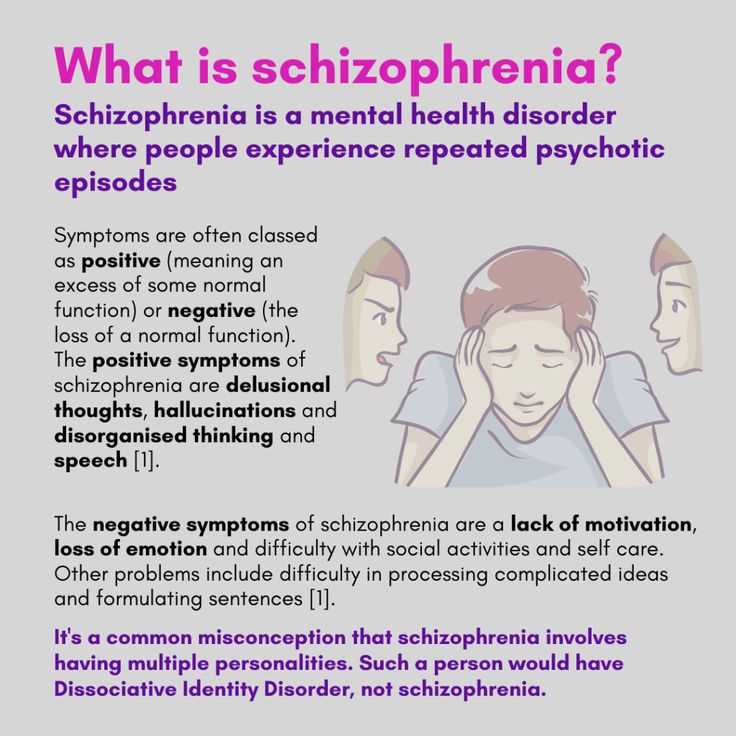 My doppelgänger uses language and I can't stop talking." Episodes of mutism are experienced as violent. Finally, there is a feeling of external mastery of speech: “Outsiders speak my language They give lectures on international topics in my language, and at that time I don’t think about anything at all.” States of loss of spontaneous speech are also associated with external phenomena. The development of speech-motor automatisms can begin with the appearance of kinesthetic verbal hallucinations: there is a sensation of movement of the articulatory apparatus, corresponding to speech, and ideas about the involuntary mental pronunciation of words. Subsequently, the internal monologue acquires a verbal-acoustic tone, a slight movement of the tongue and lips appears. At the final stage, true articulatory movements occur with the actual pronunciation of words aloud. nine0005
My doppelgänger uses language and I can't stop talking." Episodes of mutism are experienced as violent. Finally, there is a feeling of external mastery of speech: “Outsiders speak my language They give lectures on international topics in my language, and at that time I don’t think about anything at all.” States of loss of spontaneous speech are also associated with external phenomena. The development of speech-motor automatisms can begin with the appearance of kinesthetic verbal hallucinations: there is a sensation of movement of the articulatory apparatus, corresponding to speech, and ideas about the involuntary mental pronunciation of words. Subsequently, the internal monologue acquires a verbal-acoustic tone, a slight movement of the tongue and lips appears. At the final stage, true articulatory movements occur with the actual pronunciation of words aloud. nine0005
Senestopathic automatism usually develops immediately, bypassing certain intermediate stages. Only in some cases, before its appearance, can one state the phenomenon of alienation of senestopathic sensations: “Terrible headaches, and at the same time it seems that this is happening not with me, but with someone else”.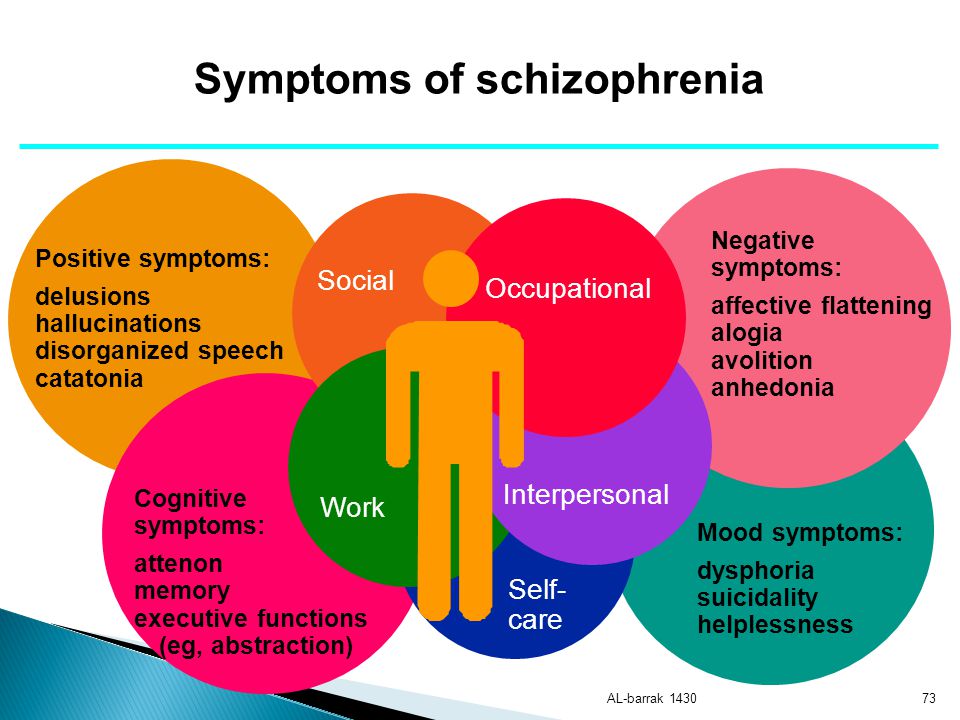
In the structure of psychic automatisms, Clerambault distinguished two types of polar phenomena: positive and negative. The content of the first is the pathological activity of a functional system, the second is the suspension or blockade of the activity of the corresponding system. Positive automatisms in the sphere of ideational disorders are the violent flow of thoughts, the symptom of investing thoughts, the symptom of unwinding memories, made emotions, induced dreams, verbal and visual pseudo-hallucinations, etc. Their antipode, that is, negative automatisms, can be states of blockage of mental activity, a symptom of withdrawal , pulling out thoughts, sudden loss of memory, emotional reactions, negative auditory and visual hallucinations that occur with a sense of being done, forcible deprivation of dreams, etc. In the sphere of senestopathic automatism, these will be respectively made sensations and loss of sensitivity caused from the outside, in kinesthetic automatism violent actions and states of delay in motor reactions, loss of the ability to make decisions, blockade of motives for activity.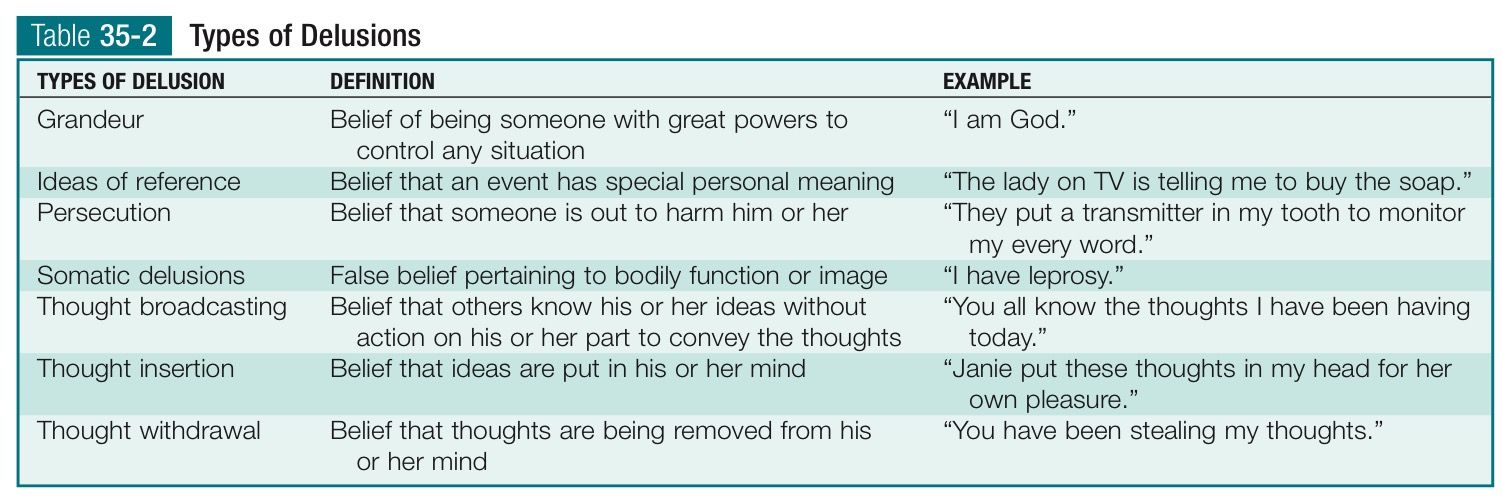 In speech-motor automatism, the polar phenomena will be forced speaking and sudden delays in speech. According to Clerambo, schizophrenia is more characteristic of negative phenomena, especially if the disease begins at a young age. In fact, positive and negative automatisms can be combined. So, forced speaking is usually accompanied by a state of blockade of mental activity: “The tongue speaks, but at this time I don’t think about anything, there are no thoughts.” nine0005
In speech-motor automatism, the polar phenomena will be forced speaking and sudden delays in speech. According to Clerambo, schizophrenia is more characteristic of negative phenomena, especially if the disease begins at a young age. In fact, positive and negative automatisms can be combined. So, forced speaking is usually accompanied by a state of blockade of mental activity: “The tongue speaks, but at this time I don’t think about anything, there are no thoughts.” nine0005
Disorders of self-consciousness arising from the syndrome of mental automatism are expressed by the phenomena of alienation of one's own mental processes, the experience of the violence of their course, a split personality and the consciousness of an internal antagonistic double, and later a feeling of mastery of external forces. Despite the seemingly obvious nature of the disorder, patients usually do not have a critical attitude towards the disease, which in turn can also indicate a gross pathology of self-awareness. Simultaneously with the growth of the phenomena of alienation, the devastation of the sphere of the personal "I" is progressing. Some patients even "forget" what it is. Mental acts emanating from the name of one's "I" do not remain at all, alienation has spread to all sides of the "I". At the same time, thanks to appropriation, a person can "acquire" new abilities and features that were not previously inherent in it. Sometimes the phenomenon of transitivism is observed not only the patient, but also others (or mostly others) are the object of external influence and all sorts of violent manipulations, their own feelings are projected onto others. nine0005
Simultaneously with the growth of the phenomena of alienation, the devastation of the sphere of the personal "I" is progressing. Some patients even "forget" what it is. Mental acts emanating from the name of one's "I" do not remain at all, alienation has spread to all sides of the "I". At the same time, thanks to appropriation, a person can "acquire" new abilities and features that were not previously inherent in it. Sometimes the phenomenon of transitivism is observed not only the patient, but also others (or mostly others) are the object of external influence and all sorts of violent manipulations, their own feelings are projected onto others. nine0005
The experience of openness comes with a variety of echo symptoms. A symptom of echo-thoughts surrounding, according to the patient, repeat aloud what he just thought. Hallucinatory echo voices repeat, "duplicate" the thoughts of the patient. A symptom of the sound of one's own thoughts thoughts "rustle, sound in the head, others hear them.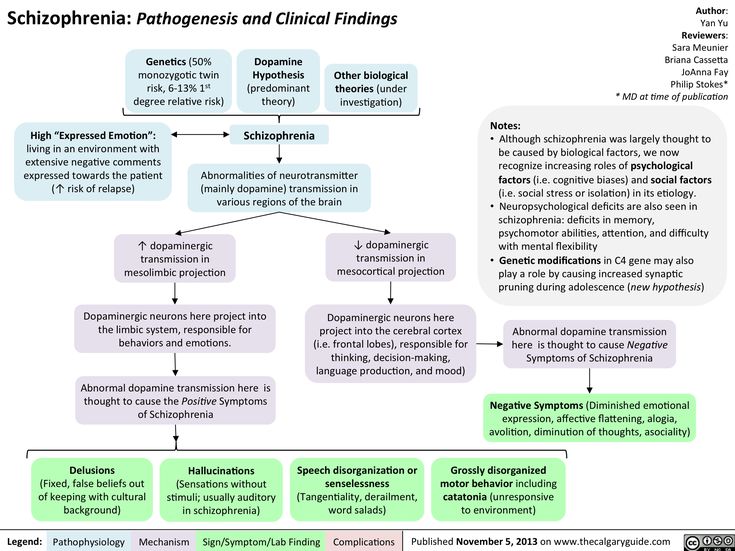 " Anticipatory echo voices warn the patient about what he will hear, see, feel or do after some time. Echo of actions voices state the actions, intentions of the patient: “I am photographed, my actions are recorded”. nine0005
" Anticipatory echo voices warn the patient about what he will hear, see, feel or do after some time. Echo of actions voices state the actions, intentions of the patient: “I am photographed, my actions are recorded”. nine0005
Voices can repeat and comment on impulses and behavior, give it this or that assessment, which is also accompanied by an experience of openness: “Everyone knows about me, nothing is kept to oneself.” Echo letters voices repeat; what the patient writes. Reading echo voices repeat what the patient reads to himself. Echoes of speech voices repeat everything said by the patient to someone aloud. Sometimes the voices make the patient repeat for them what he told others, or, on the contrary, mentally or aloud once again say what he heard from someone. The above echo phenomena can be iterative in the form of multiple repetitions. So, a patient (he is 11 years old) has episodes of two, three hours, when what other people say three, five times in a strange voice is repeated “in the head”.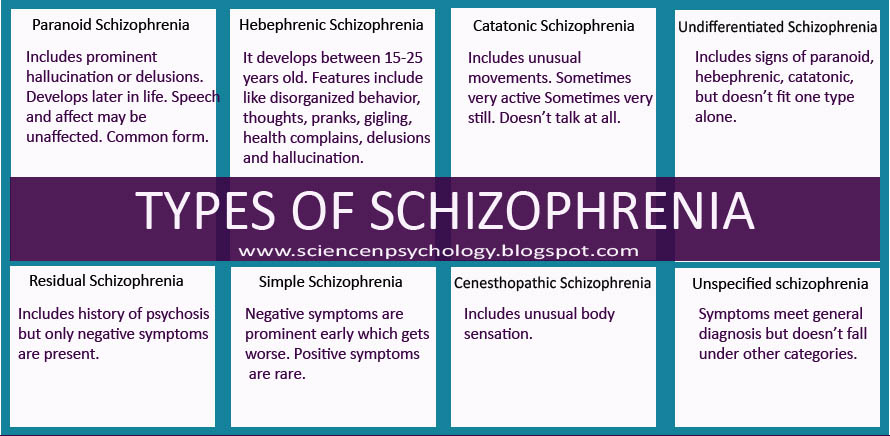 More often one word is repeated. During repetitions, he perceives what is happening worse, cannot watch TV. Other echo phenomena occur. So, the speech of others can be repeated by voices from the outside or sounding in the head. Voices with external projection are sometimes duplicated by internal ones. The experience of openness can be observed even in the absence of echo symptoms, it can arise in the most direct way: “I feel that my thoughts are known to everyone There was a feeling that God knows everything about me I am in front of him like an open book The voices are silent, which means they are eavesdropping on what I think ". nine0005
More often one word is repeated. During repetitions, he perceives what is happening worse, cannot watch TV. Other echo phenomena occur. So, the speech of others can be repeated by voices from the outside or sounding in the head. Voices with external projection are sometimes duplicated by internal ones. The experience of openness can be observed even in the absence of echo symptoms, it can arise in the most direct way: “I feel that my thoughts are known to everyone There was a feeling that God knows everything about me I am in front of him like an open book The voices are silent, which means they are eavesdropping on what I think ". nine0005
Delusion of physical and mental influence belief in the impact on the body, somatic and mental processes of various external forces: hypnosis, witchcraft, rays, biofields, etc.
In addition to the above-described phenomena of alienation, in the syndrome of mental automatism, opposite phenomena can occur - appropriation phenomena that make up the active or inverted version of the Kandinsky-Clerambault syndrome.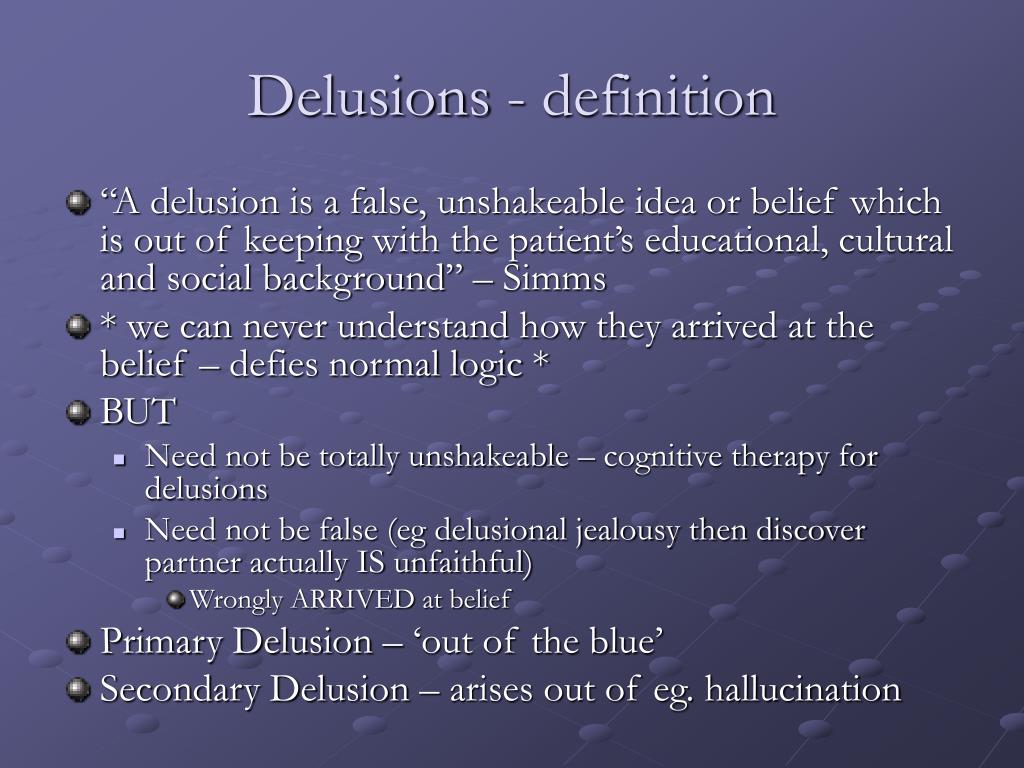 In this case, patients express the belief that they themselves have a hypnotic effect on others, control their behavior, are able to read the thoughts of other people, the latter have become an instrument of their power, behave like puppets, puppets, parsley, etc. A combination of alienation phenomena and appropriation of V. I. Akkerman (1936) considered it a symptom characteristic of schizophrenia.
In this case, patients express the belief that they themselves have a hypnotic effect on others, control their behavior, are able to read the thoughts of other people, the latter have become an instrument of their power, behave like puppets, puppets, parsley, etc. A combination of alienation phenomena and appropriation of V. I. Akkerman (1936) considered it a symptom characteristic of schizophrenia.
There are hallucinatory and delusional variants of the syndrome of mental automatism. In the first of them, various pseudohallucinations predominate, which is observed mainly during acute hallucinatory-delusional states in schizophrenia, in the second - delusional phenomena that dominate in chronically current paranoid schizophrenia. In chronic schizophrenic delusions of the interpretative type, associative automatisms come to the fore over time. Senestopathic automatisms may predominate in the structure of attacks of fur-like schizophrenia. In lucid-catatonic states, a significant place is occupied by kinesthetic automatisms.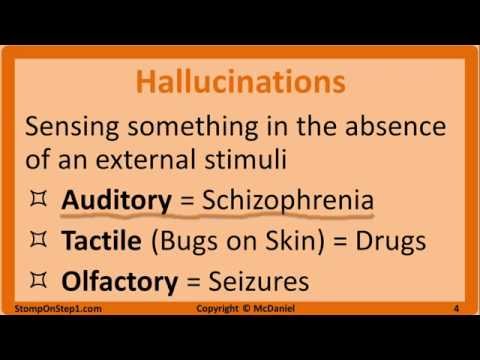 In addition to schizophrenia, the phenomena of mental automatism can occur with exogenous organic, acute and chronic epileptic psychoses. nine0005
In addition to schizophrenia, the phenomena of mental automatism can occur with exogenous organic, acute and chronic epileptic psychoses. nine0005
Paraphrenic syndrome. Combination of systematized or fragmented delusions of persecution and influence, phenomena of psychic automatism with figurative megalomaniac delusions of grandiose content, incredibly absurd and completely divorced from reality (power, grandeur, wealth, etc.), with expansive confabulosis, delusional depersonalization and often somewhat elevated mood. Paraphrenic delusions can be quite coherent systematized paraphrenia. A slender, detailed paraphrenic structure is created by combining a succession of delusional insights and testifies to the known intellectual safety of patients a sign that brings it closer to a paranoid syndrome. By analogy with paranoia, the existence of an independent painful form, paraphrenia, is assumed. Paraphrenic syndrome can arise on the basis of whimsically changeable delusions of the imagination fantastic paraphrenia and fantastic confabulations confabulatory paraphrenia, hallucinations of megalomaniacal content hallucinatory paraphrenia.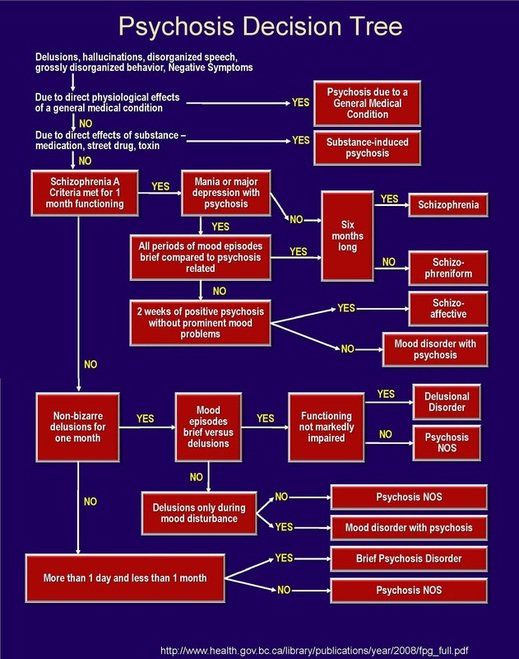 There are hallucinatory and delusional variants of paraphrenic syndrome. The predominance of hallucinatory disorders over delusional ones generally indicates a deeper disorder of mental activity than their inverse ratio. In addition, there are acute and chronic variants of paraphrenic syndrome. At the height of acute paraphrenia with Manichaean, metabolic delirium, delusions of special significance and intermetamorphosis, which usually occurs against the background of severe affective disorders, oneiroid stupefaction may develop. Paraphrenic states that appear against the background of a manic mood are called expansive paraphrenia, and against the background of depression, depressive paraphrenia. Cotard's syndrome is considered a variant of the latter. nine0005
There are hallucinatory and delusional variants of paraphrenic syndrome. The predominance of hallucinatory disorders over delusional ones generally indicates a deeper disorder of mental activity than their inverse ratio. In addition, there are acute and chronic variants of paraphrenic syndrome. At the height of acute paraphrenia with Manichaean, metabolic delirium, delusions of special significance and intermetamorphosis, which usually occurs against the background of severe affective disorders, oneiroid stupefaction may develop. Paraphrenic states that appear against the background of a manic mood are called expansive paraphrenia, and against the background of depression, depressive paraphrenia. Cotard's syndrome is considered a variant of the latter. nine0005
Systematized and expansive forms of paraphrenia are believed to be more characteristic of schizophrenia (remote stages of the course of paranoid schizophrenia, affective-delusional attacks of fur-like schizophrenia), confabulatory and fantastic paraphrenia - organic processes and late-age psychoses (senile paraphrenia).
Cotard's syndrome (melancholic paraphrenia). Fantastic nonsense of nihilistic and hypochondriacal content, which is formed against the background of an anxious-depressive state and agitation (“everything is lost, all people are dead, life, civilization, the planet, the whole Universe is dead”). Often includes delusional ideas of immortality. Patients claim that they are doomed to endless wanderings and eternal torment - a symptom of Ahasuerus. Cotard's syndrome refers to the manifestations of involutional melancholy. nine0005
Hallucinatory syndromes. Hallucinosis a condition characterized by a predominance of hallucinations in the absence of formal signs of clouding of consciousness. The most common are verbal hallucinations, less often - visual, tactile and olfactory. Usually one kind of hallucinations dominates, their combinations are much more rare. There are acute and chronic variants of the hallucinatory syndrome (any of those listed below).
Acute verbal hallucinosis syndrome.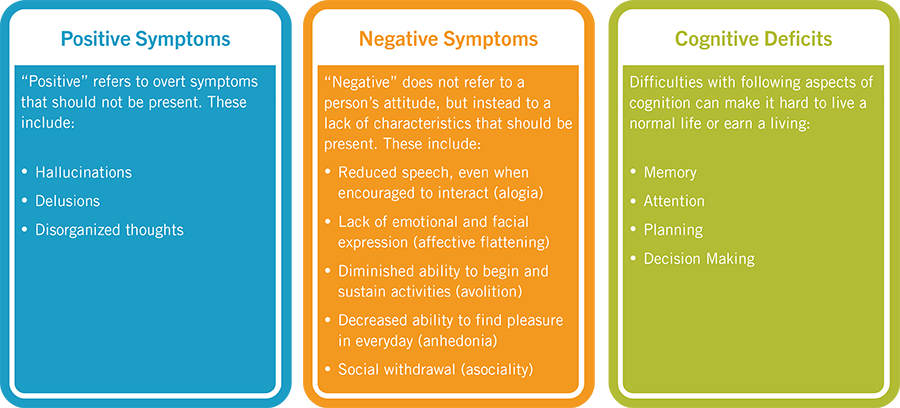 nine0004 Manifested by numerous auditory, often scene-like hallucinations, sometimes related to such an extent that there may be an erroneous impression of the presence of visual illusions of perception. There are also hallucinatory delusions (delusions that have been dissolved in the content of auditory deceptions, or manifested by a delusional assessment of the latter; for example, voices threaten to kill or are assessed by the patient as “rigged”, “special experiment”), fear, confusion, behavioral disturbances. Occurs in schizophrenia, intoxication, infectious psychoses. nine0005
nine0004 Manifested by numerous auditory, often scene-like hallucinations, sometimes related to such an extent that there may be an erroneous impression of the presence of visual illusions of perception. There are also hallucinatory delusions (delusions that have been dissolved in the content of auditory deceptions, or manifested by a delusional assessment of the latter; for example, voices threaten to kill or are assessed by the patient as “rigged”, “special experiment”), fear, confusion, behavioral disturbances. Occurs in schizophrenia, intoxication, infectious psychoses. nine0005
Syndrome of chronic verbal hallucinosis. Often develops after acute. In fact, auditory delusions often turn out to be a mixed phenomenon, with signs of true (bright sensoriality, external projection) and false (made, intimate connection with the mental "I", delusions of influence) hallucinations. Hallucinations and pseudo-hallucinations can coexist at the same time. Patients "get used" to hallucinatory characters, complex relationships develop between them: conflicts, consent, subordination, trust.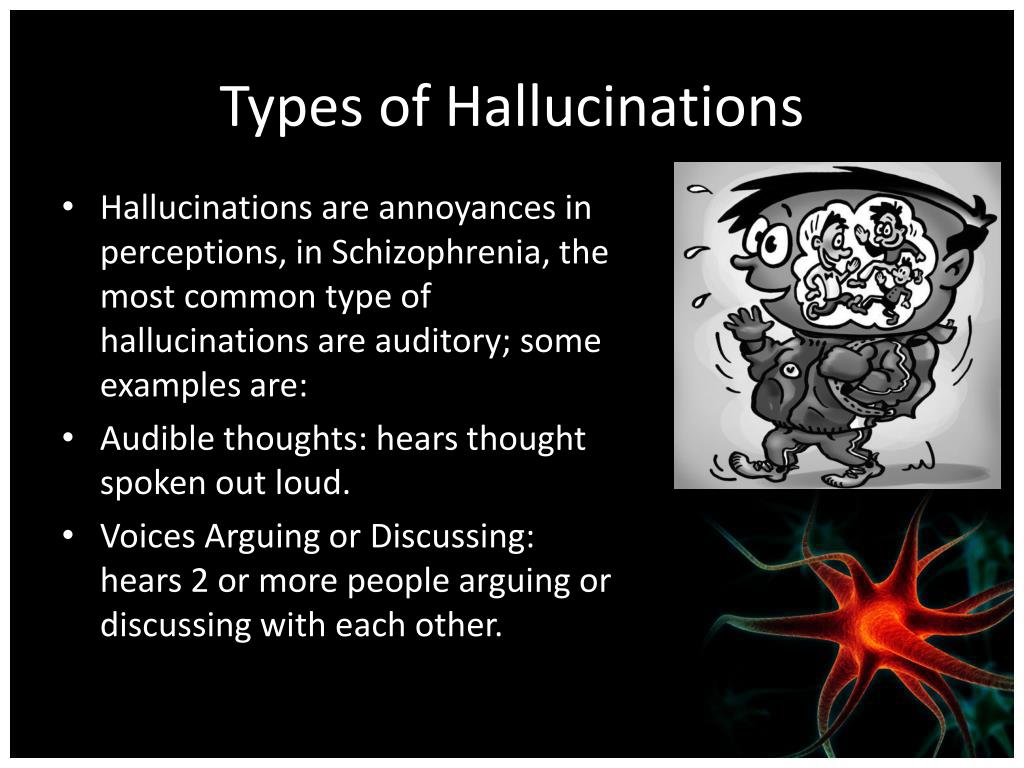 More often these relationships are antagonistic, and the patient usually finds himself in a dependent position. There are several votes. So, the patient has three voices, they call themselves "A", "B" and "C". Voices love to philosophize, argue, teach. At one time they were fond of the topic of love, so that the patient had to read them books only about this. They constantly provoke the patient to do strange things. “I know why they give me money to be considered crazy,” she explains herself. The mood of the voices changes: sometimes they are hostile, sometimes benevolent, sometimes sad. The behavior of chronically hallucinating patients is generally more ordered than in acute hallucinosis. More often, the attitude towards voices is ambivalent, and a critical attitude to the deceptions of perception may appear. The voices themselves can say that they are a manifestation of the disease, and that they need to be treated, they even say something, for example, "haloperidol". Chronic verbal hallucinosis occurs in the hallucinatory variant of hallucinatory-paranoid schizophrenia, chronic alcoholic psychosis, organic diseases of the brain.
More often these relationships are antagonistic, and the patient usually finds himself in a dependent position. There are several votes. So, the patient has three voices, they call themselves "A", "B" and "C". Voices love to philosophize, argue, teach. At one time they were fond of the topic of love, so that the patient had to read them books only about this. They constantly provoke the patient to do strange things. “I know why they give me money to be considered crazy,” she explains herself. The mood of the voices changes: sometimes they are hostile, sometimes benevolent, sometimes sad. The behavior of chronically hallucinating patients is generally more ordered than in acute hallucinosis. More often, the attitude towards voices is ambivalent, and a critical attitude to the deceptions of perception may appear. The voices themselves can say that they are a manifestation of the disease, and that they need to be treated, they even say something, for example, "haloperidol". Chronic verbal hallucinosis occurs in the hallucinatory variant of hallucinatory-paranoid schizophrenia, chronic alcoholic psychosis, organic diseases of the brain. nine0005
nine0005
Visual hallucinosis. Occurs with complete or significant loss of vision (H. Bonnet hallucinations), lesions of the brain stem, Van Bogart encephalitis, intoxication, in extreme old age. Characterized by optical illusions in the form of small (midget) visions of animals, birds, people, colored and mobile. Patients are distant from them, but at night, with the appearance of confusion and excitement, the critical attitude may be lost.
Tactile hallucinosis. nine0004 Characterized by profuse tactile hallucinations, hallucinatory delusions of obsession with skin parasites (Ekbom's dermatozoic delusions, external zoopathy). Algohallucinosis - continuous phantom pain radiating to the missing part of the limb. Gabeck's olfactory hallucinosis. Persistent olfactory hallucinations, often projected onto one's own body or internal organs. At the same time, hypochondriacal and nihilistic delusions are observed, as well as sensitive ideas of relation. When extraprojecting olfactory hallucinations, delusional ideas of poisoning join.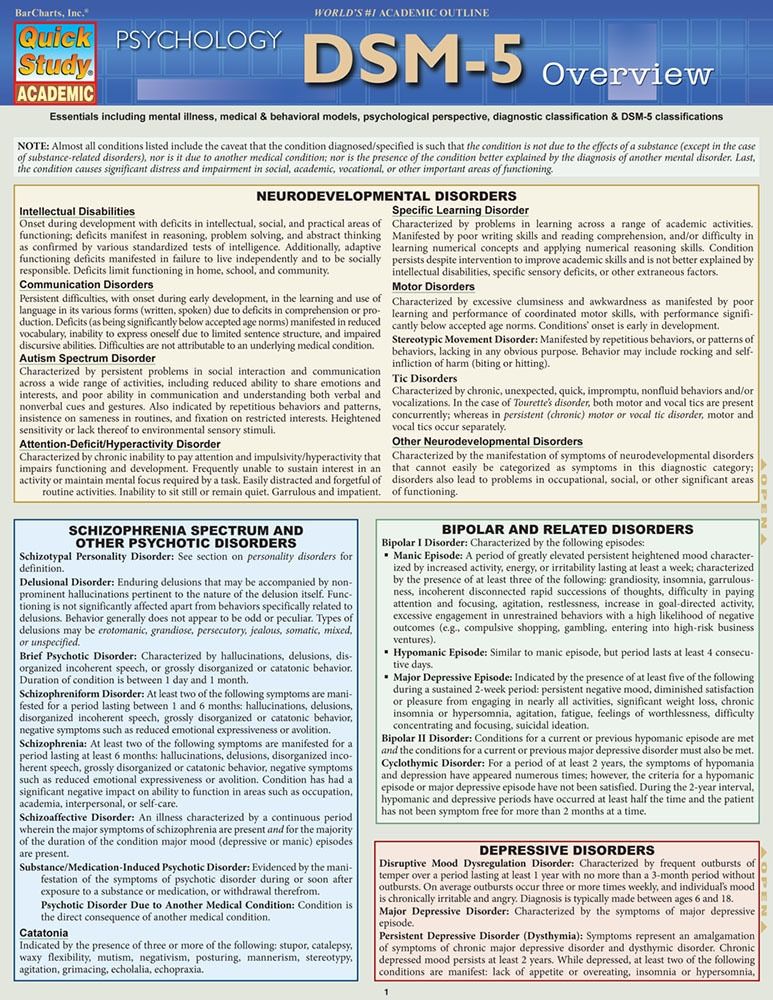 nine0005
nine0005 "I hid my psychosis for ten years." The story of a man with hallucinations
Subscribe to our newsletter "Context": it will help you understand the events.
Photo copyright, Luke Watkin
Photo caption,Luke Watkin first experienced hallucinations at the age of 12.
Luke Watkin was in high school when it happened. He was walking along an empty school corridor and suddenly heard a strange sound. nine0004
"It seemed to me that there was a screech of train brakes, and then a metallic clang. For me it was a complete surprise, I just did not understand what happened. And then I got scared," he says.
This was his first encounter with mental illness. He was then 12 years old.
- "We were taught not to whine": how to accept and overcome depression
- Euthanasia due to mental illness.
 Was there an alternative?
Was there an alternative? - Skunk cannabis increases the risk of psychosis
The auditory hallucinations were growing - he heard single words, his own name, and at the end - whole phrases, as if someone was trying to talk to him.
This is one of the main signs of psychosis - hallucinations and delusions, and they can be caused by a specific disease - schizophrenia, bipolar disorder or acute depression.
Stress, trauma, drugs, alcohol, drug exposure, or a brain tumor can also cause these phenomena. nine0005
The invisible enemy
Psychosis is not as common as depression - it affects less than one person in a hundred. Experts say that for the successful treatment of psychosis, it is important to recognize and diagnose it as soon as possible.
Psychotic people are much more likely to commit suicide or cause physical injury to themselves.
According to psychiatrists, more than half of the sick admit that it was difficult for them to notice the initial symptoms of psychosis.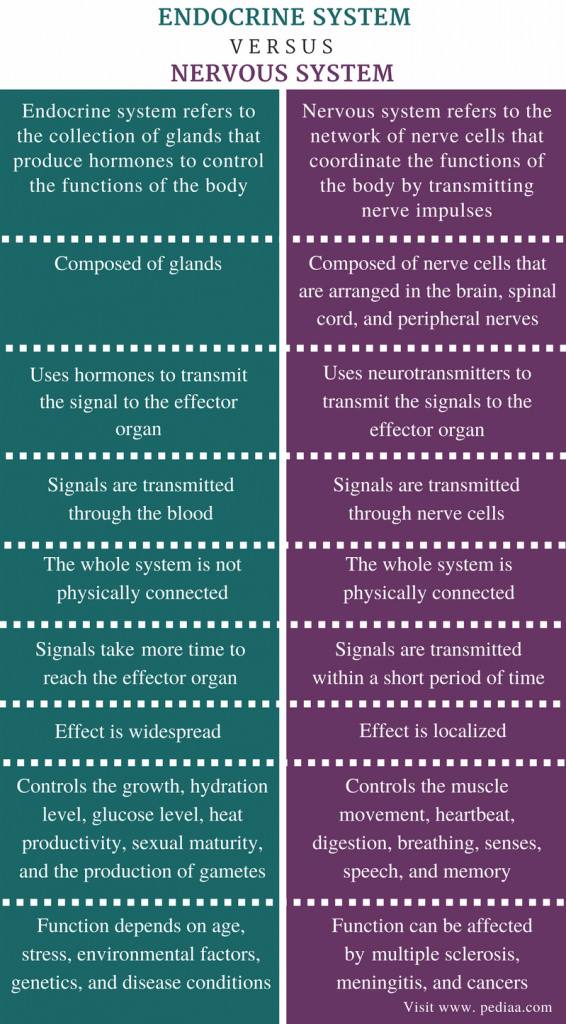 nine0005
nine0005
Most often, such symptoms appear in the age group of 18-24 years, and psychiatrists believe that a lack of knowledge in this area leads to the fact that young people do not receive timely help.
There are more hidden signs that indicate mental distress and the approach of a psychotic state - growing self-isolation, a tendency to strange views and ideas, sharp mood swings and confusion in thoughts.
Symptoms of psychosis:
- Hallucinations, when it seems to a person that he sees, hears, feels something that does not exist in reality
- Rapid continuous speech
- Confused speech - for example, a quick transition from one topic to another in one phrase prevails
- 0104
- Sudden loss of train of thought, resulting in a sudden pause in conversation
Luke tried to talk about anxiety symptoms with the teacher, but, he said, he was given to understand that this should not be shared with everyone.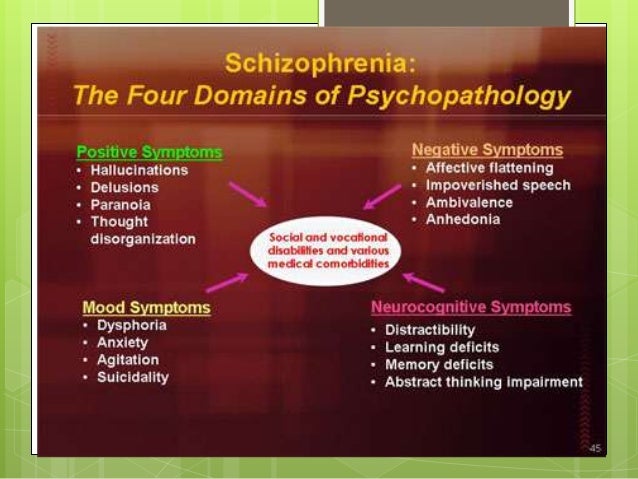
So he decided to be firm and keep the secret to himself. Luke kept quiet about his illness until he had to drop out of his third year at university.
He admits now that even members of his family would find it difficult to notice that something was wrong with him. nine0005
"They thought I was quiet because that's how I dealt with problems. I rarely left my room and preferred not to talk to anyone. And my parents used to think of me as a quiet and calm child," says Luke.
But when he became a student, it was difficult for him - it turned out to be impossible to hide his psychosis in the conditions of student life.
He dropped out of school without telling his parents, who didn't suspect a thing.
image copyrightFamily photo
Photo image caption,When Luke's father Steve found out about his son's illness, he was understanding and caring.
"When my illness got to the point, I just disappeared," says Luke.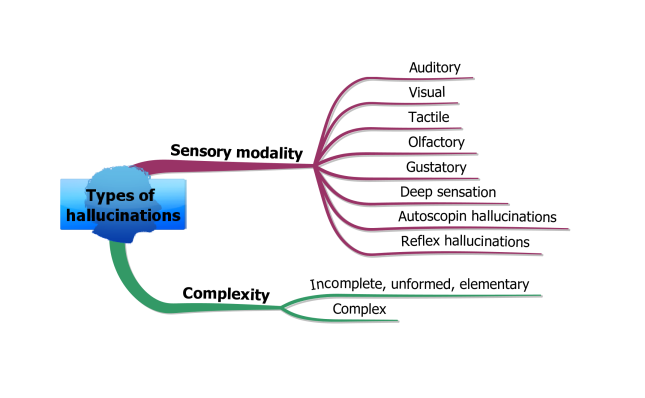 "I stopped keeping in touch with my parents."
"I stopped keeping in touch with my parents."
"When the university told them that I had dropped out, they realized that something was happening to me, and this was the first step towards a cure. They showed complete understanding and care."
In Britain, psychiatrists advise anyone who shows signs of psychosis to immediately contact their doctor. nine0005
Psychosis is usually treated with a combination of medication, psychotherapy, and social and family support.
Attitudes of society are changing
Luke was treated - he was prescribed antipsychotic medication and was connected to the early intervention service.
"Now, when I remember my past, it seems incredible to me. I refused to complain about my condition - the very thought of it did not occur to me. Now I complain constantly, but then I was simply afraid to think about my illness without talking about talking about it with the doctor," recalls Luke.