Guilt anxiety depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid.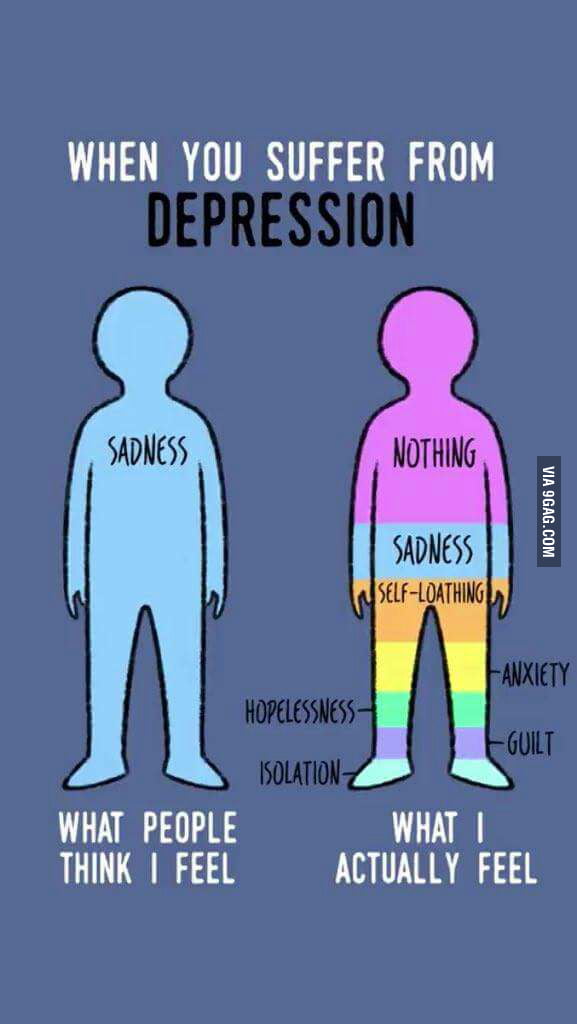 If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.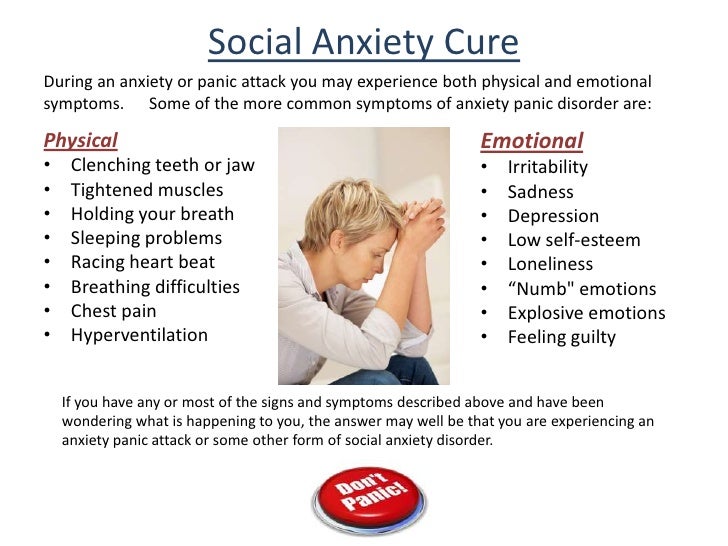
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers.
 The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH) - Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
- The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.
4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.
7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
- Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month.
The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
- Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
- Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
- The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
- Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 01/05/2023
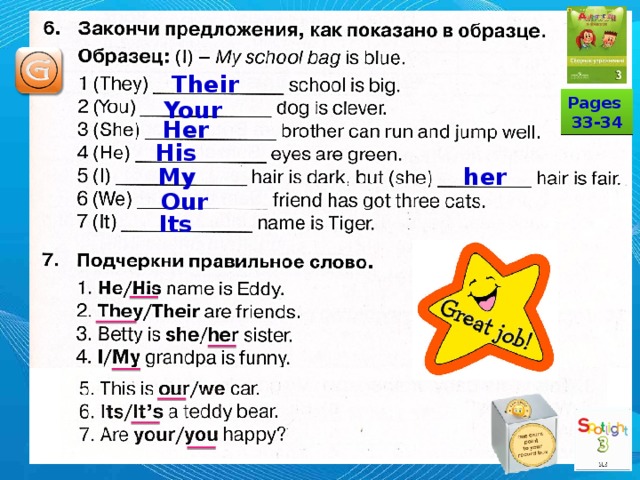
What do we know about anxiety and depression?
Evgeniy Gennadievich Ilchenko, psychotherapist of the Department for the Treatment of Borderline Mental Disorders and Psychotherapy of the National Research Center for Psychiatry and Neurology. V.M. Bekhterev.
Anxiety, depression are conditions that are characteristic of disturbances in the state of the emotional sphere. Today, about 110 million people in the world suffer from depression. According to the World Health Organization, one in five women and one in fifteen men suffer from depression in major cities around the world. It is believed that by 2020 depression will take one of the first places among all diseases. Approximately 70% of depressed patients show suicidal tendencies, and depressed patients older than 75 have the highest rate of suicide.
I am suffering, I am afraid…
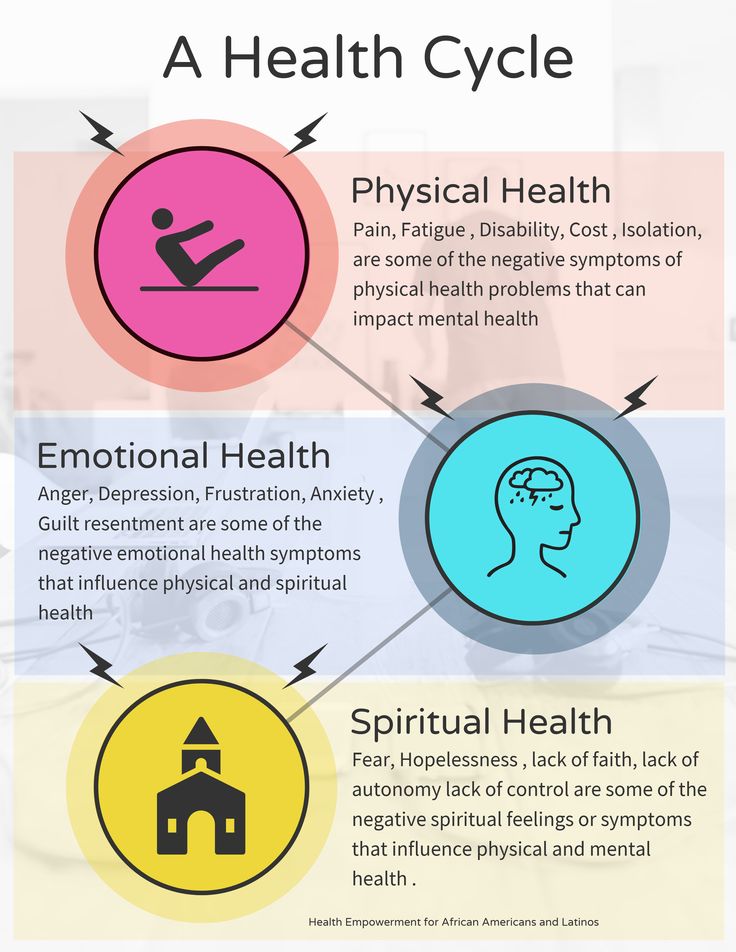
What is depression? Depression is a disease that can throw a person out of emotional balance for a long time and significantly impair the quality of his life. It can be difficult for you to concentrate, nothing is interesting, nothing pleases, doubts and fears are constantly overcome. Depression usually comes after a psychological trauma or negative event. Often it develops as if for no apparent reason. It can be caused by constant stress, accumulating fatigue, fears. Depression is more than just low mood. In this case, the work of the whole organism changes, as a person suffers from insomnia or early awakenings, he loses his appetite or begins to seize his anxiety, which leads to obesity and the development of metabolic syndrome, there is a hormonal imbalance. A person changes his attitude towards others and himself.
Longing, apathy, anxiety…
How does depression manifest itself? The first symptoms include weakness, fatigue, unwillingness to do anything, strain once again, contact and communicate with people, go to work. Later, bodily symptoms may join these complaints - palpitations, sweating, trembling in the body, hot or cold flashes.
Three areas are involved in depression - emotional, mental and physical. At the emotional level, depression, melancholy, apathy, and anxiety are observed. On the mental level - thoughts about one's guilt, self-accusations, a negative vision of the future, a feeling of hopelessness, that "no one will help me." On the physical level - chronic pain, muscle tension, constipation, dizziness, heaviness in the head. And all these symptoms can constantly change: “Today my head hurts, and yesterday my joints hurt, the day before yesterday my heart hurt.”
Maybe it's psychosomatics?
It is worth noting that there are different types of depression. According to the classification, depressions are diverse: major, minor, neurotic, autumnal, endogenous, psychogenic, reactive, etc. There is depression associated with the reproductive function of a woman, this is prenatal and postnatal. There is age-related depression associated with the physiological restructuring of the body, there is an obvious one that occurs with a sharply reduced mood, melancholy, and depression. There is a masked depression that hides under the guise of another disease. For example, chronic pain syndrome - pain in different parts of the body. There is depression, which is masked by gastrointestinal symptoms - diarrhea, constipation, stomach pain. Patients go to doctors for a long time and unsuccessfully, are treated by different specialists. But there is no improvement. At this stage, it is important to recognize psychosomatic disorders. It is worth looking, but what gives a person a disease? How is she good for him? It is quite possible that in this way a person attracts attention to himself, seeks location, manipulates loved ones and relatives.
How can I help?
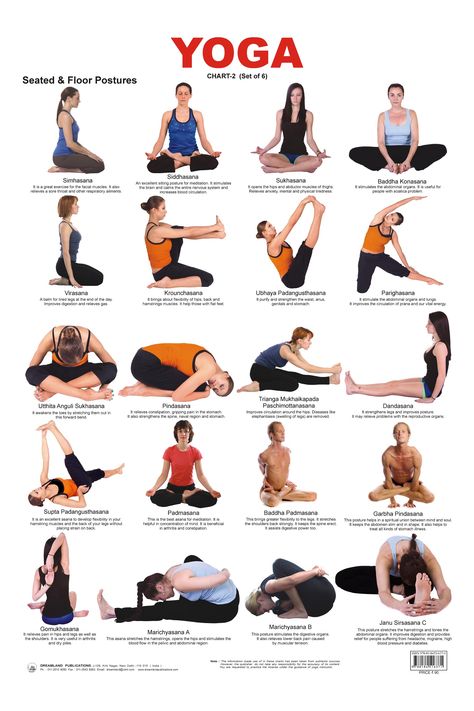
Sometimes depressed patients try to alleviate their mental state through physical pain, inflicting injuries and injuries on themselves. This is definitely not an option. How can others help such patients? First of all, do not ignore or forbid complaining, do not try to cheer up the patient, do not appeal to conscience and faith, do not demand the adoption of any important decisions, but simply be there and listen patiently. As for direct treatment, there is no “magic” remedy for depression. Various methods are used here: psychotherapy, pharmacotherapy, electroconvulsive therapy, physiotherapy, aroma and color therapy, physical activity. If we talk about the prevention of depression, then this is a healthy lifestyle and a positive attitude, communication with nature.
Experiences about the future
Depression is a negative experience of past life events that we cannot change, and anxiety is an experience for the future, this is a vague, unpleasant emotional state characterized by the expectation of an unfavorable development of events, the presence of bad forebodings, tension and anxiety. It is directed to the future, it is the expectation of something indefinite. The state of anxiety is pointless, but anxiety is a personality trait of a person prone to experiencing anxiety, and constantly experiencing it. Most often, a person's anxiety is associated with the expectation of the social consequences of his success or failure.
Risk factors for the development of anxiety include childhood trauma, stress, personality traits, genetic predisposition, alcohol and psychoactive substances. Anxiety can be normal or excessive. In pathological cases, anxiety becomes constant and harmful, appearing not only in stressful situations, but also for no apparent reason, and then anxiety not only does not help a person, but begins to interfere with his daily activities.
Panic attacks
The largest category of anxiety disorders are phobias, with about a hundred variants. Anxiety disorders include post-traumatic stress disorder, social anxiety, panic attacks, and separation anxiety. Speaking of anxiety, it is worth mentioning panic attacks separately. How do they appear? Unexpected internal tension, pointless fear, timidity, stiffness, feeling of danger, unreality of what is happening, "lump in the throat", chills, sweating, heart palpitations, suffocation, nausea, diarrhea, dizziness, goosebumps, restlessness. What to do in such cases? It is necessary to focus on the real situation, to calm down, to be distracted, to understand that there is no real threat. Auto-training, progressive muscle relaxation, breathing techniques work great. But this must be learned. The state of a panic attack can be constantly repeated and the fear each time feels real. It is necessary to learn to understand and catch yourself in a state of “pre-panic”, not to let yourself breathe heavily and rapidly, try to say “I” on the inhale, and “calm” on the exhale.
Anxiety, guilt and depression | Defectology Prof.
In the two preceding chapters I have dealt with the general nature of anxiety and its relation to fright and shock, two emotions that are certainly similar to it in physical manifestations and in that which are as often observed in animals as in person. This chapter will deal with the relationship of anxiety to guilt and depression, two other feelings that are more psychologically complex and, in all likelihood, unique to humans}'. Someone will surely say that a dog sometimes looks guilty or depressed, but I doubt that there will be those who will say this with the same confidence as one can say that the animal is frightened or shocked, or with which he will say about himself, that feels guilty or oppressed.
In addition, in this chapter we will deal exclusively with human psychology and psychopathology, as well as those states of the soul that we know only through self-observation and empathy. Therefore, I cannot quote physiological descriptions of guilt and depression in the same way that I quoted Pavlov and Wittehorn when talking about vigilance. This would be inappropriate, since severe depression is undoubtedly accompanied by physiological changes, but animals do not experience the same feelings as normal depression. Attempts have already been made to present human depression as analogous to the hibernation of animals, but despite the fact that hibernation includes a general depression of vital activity, it is more like sleep than depression. Animal hibernation is a calm and apparently painless state, while human depression is a painful, agitated and anxious state of mind and body, usually accompanied by insomnia. The anguish of isolated or captive animals cannot really be regarded as identical with human depression; rather, depression is like unhappiness and despair. The reasons why I want to consider the relation of anxiety to guilt and depression are practical and clinical. In both healthy and diseased states, anxiety, guilt, and depression are experienced simultaneously. Those who seek psychological help very often complain about the feeling of two or three of these feelings, which makes them think of them as an interconnected triad.
This is reflected in psychological and psychoanalytic theories, which tend to interpret and delineate the feelings that make up this triad by mutually using their names. The hidden connection of these three emotions is also surprising, since anxiety, at first glance, is incompatible with guilt and depression, as it is directed to the future, while guilt in most cases refers to the past; again, anxiety increases, and depression reduces vitality
All information is taken from open sources.