What is the common cold of mental illness
Depression- A common cold of mental disorders
Introduction
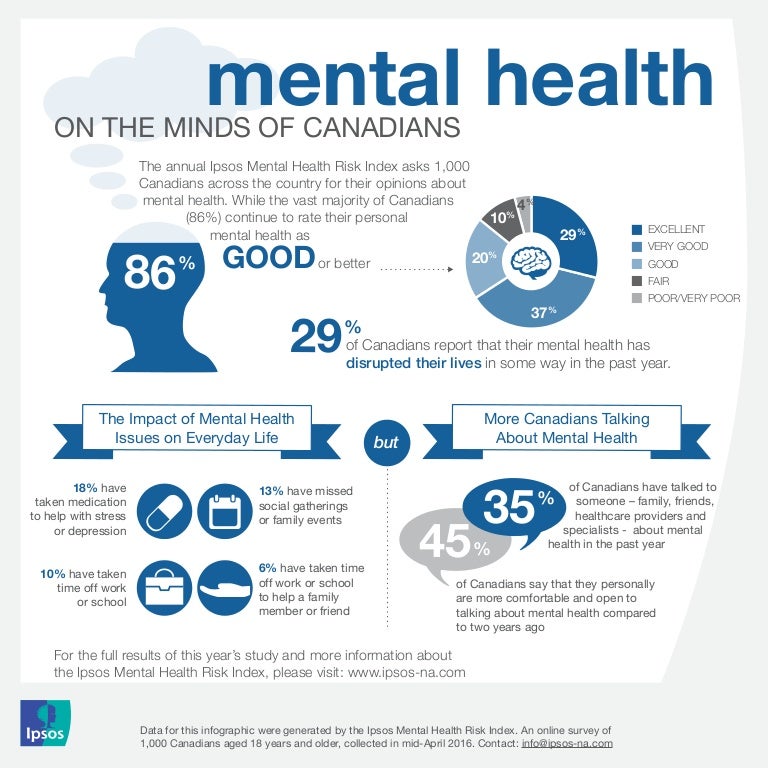
Depression isn't solely a state of being unhappy; it is an illness that conquers the flexibility to feel emotion, whether or not sensible or unhealthy, whatsoever. It not only involves the mind, it additionally involves the body and thoughts. In several cultures some complain of excessive headaches and extreme pain and this can be known as depression, moderate or otherwise. This illness is passed down through genes or will follow external events or may be caused by a chemical imbalance in the brain. Depression affects common fraction of all Americans, some while not even knowing it, at some time throughout their lives. Depression isn't an illness that solely influences males or youngsters of the age three to eleven [1]. Each individual is at risk of depression. Although women are three times additional seemingly to become depressed than men, men are 5 times additional seemingly to commit suicide when depressed than women [2].
There are differing types of depressions like major depression, persistent depressive disorder, bipolar disorder, seasonal effective disorder, psychotic depression, postpartum depression, premenstrual dysphoric disorder, situational depression, atypical depression [3]. Out of that the foremost severe case being the major depression. For some people major depression may end up in severe impairments that interfere with or limit one's ability to hold out major life activities. Though all age groups are open to depression, teenagers are the most common to be detected of being tormented by the sickness. This is often most likely as a result of peer pressure and also the changes in their life [4]. The aim this study was to understand the impact of clinical depression among the non-institutionalized adolescents and older population.
Causes and symptoms
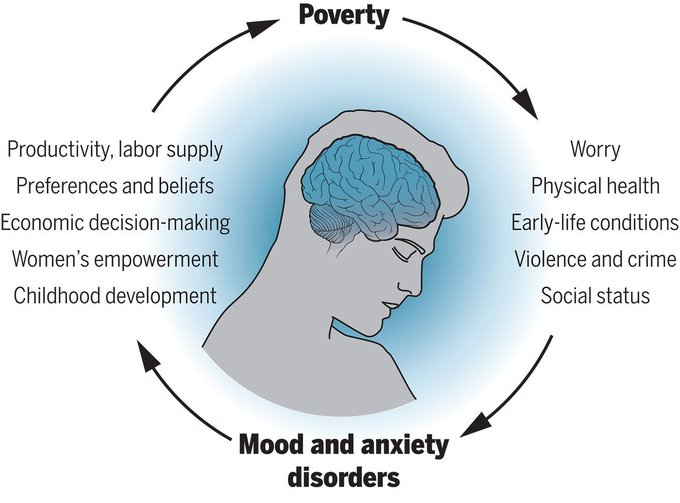
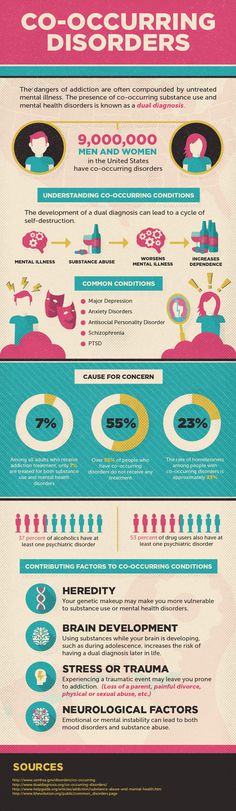
The exact reason for Major Depressive Disorder (MDD) isn't best known. However, there are many factors that may increase the chance of developing the condition. A combination of genes and stress will have an effect on brain chemistry and scale back the power to take care of mood stability. Changes in the balance of hormones would possibly continue to contribute to the event of MDD. This disorder might continuously be triggered by alcohol or substance abuse [5], sure medical conditions, like cancer or glandular disorder, specific sorts of medications including steroids. It may also include physical or mental abuse, conflict, death or loss, major life events, serious illness and other personal and professional problems [6].
A combination of genes and stress will have an effect on brain chemistry and scale back the power to take care of mood stability. Changes in the balance of hormones would possibly continue to contribute to the event of MDD. This disorder might continuously be triggered by alcohol or substance abuse [5], sure medical conditions, like cancer or glandular disorder, specific sorts of medications including steroids. It may also include physical or mental abuse, conflict, death or loss, major life events, serious illness and other personal and professional problems [6].
The practicing physician or the psychological professional will create an MDD based on diagnosis of symptoms, feelings, and behavior patterns. The practitioner will raise certain queries or will provide with a questionnaire so that they will verify whether or not the individual got MDD [7]. In keeping with its criteria, you want to have five or a lot of the subsequent symptoms and experience them a minimum of once each day for a period of quite a pair of weeks.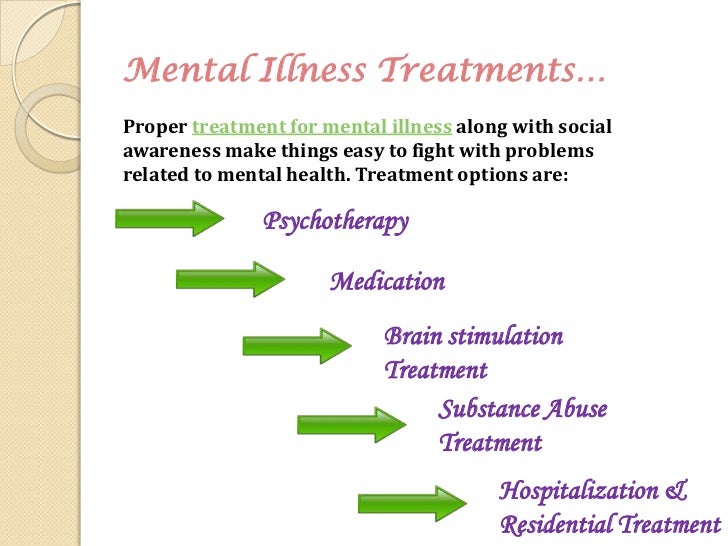 The symptoms includes: feeling unhappy or irritable most of the day, nearly every day; feeling less fascinated by most activities you once enjoyed; sudden loss or gain weight or have a modification in appetite; trouble falling asleep or wish to sleep over usual; expertise feelings of restlessness; feeling unusually tired and have an absence of energy; feeling unworthy or guilty; issues in concentrating, thinking, or making selections; thinking about harming yourself or committing suicide [8].
The symptoms includes: feeling unhappy or irritable most of the day, nearly every day; feeling less fascinated by most activities you once enjoyed; sudden loss or gain weight or have a modification in appetite; trouble falling asleep or wish to sleep over usual; expertise feelings of restlessness; feeling unusually tired and have an absence of energy; feeling unworthy or guilty; issues in concentrating, thinking, or making selections; thinking about harming yourself or committing suicide [8].
Methods
The prevalence information given here for major depressive episodes are from the 2016 National Survey on Drug Use and Health (NSDUH) [9]. The NSDUH study definition of major depressive episode is predicated primarily on the fourth edition of the Diagnostic and applied math Manual of Mental Disorders (DSM-IV):
- An amount of fortnight or longer throughout which there's either depressed mood or loss of interest or pleasure, and a minimum of four alternative symptoms that replicate a modification in functioning, like issues with sleep, eating, energy, concentration, self-image or repeated thoughts of death or suicide.
- For the NSDUH survey - in contrast to DSM-IV criteria - no exclusions were created for a serious depressive episode caused by medical sickness, sadness, or substance use disorders.
- Modules associated with major depressive episode derived from DSM-IV (1994) criteria for major depression were enclosed within the NSDUH questionnaire. The queries were custom-made from the depression module within the National Co-morbidity Survey Replication (NCS-R). Revisions to the queries within the modules were created primarily to cut back their length and to change the NCS-R queries that are interviewer-administered to the Audio Computer-Assisted Self-Interviewing (ACASI) format utilized in NSDUH. Additionally, some revisions, supported cognitive testing, were created to enhance comprehension. Moreover, although titles like those utilized in the NCS-R were used for the NSDUH modules, the results of those things might not be directly comparable. This is primarily because of differing modes of administration in every survey (ACASI in NSDUH vs.
 computer-assisted personal interviewing in NCS-R), revisions to phrasing necessary to take care of the logical processes of the ACASI surroundings, and potential context effects ensuing from deleting queries not expressly pertinent to major depression
computer-assisted personal interviewing in NCS-R), revisions to phrasing necessary to take care of the logical processes of the ACASI surroundings, and potential context effects ensuing from deleting queries not expressly pertinent to major depression - The Sheehan disability Scale (SDS) was accustomed assess the impact of major depressive episode on a person’s life. The SDS is a brief self-report tool with ratings from zero to ten (with ten being the highest) for the extent of impairment caused by the disorder in each of 4 role domains: home management, work, close relationships with others, and social life. A rating of ≥ 7 in a minimum of one domain is taken into account to be severe impairment. Respondents were excluded if SDS role impairment severity was unknown, or if specific activities listed within the SDS weren't applicable.
Population
The totality of NSDUH respondents for the major depressive episode estimates is that the civilian, non-institutionalized population aged 12-17 (adolescents) and 18 years old or older (adults) residing within the US.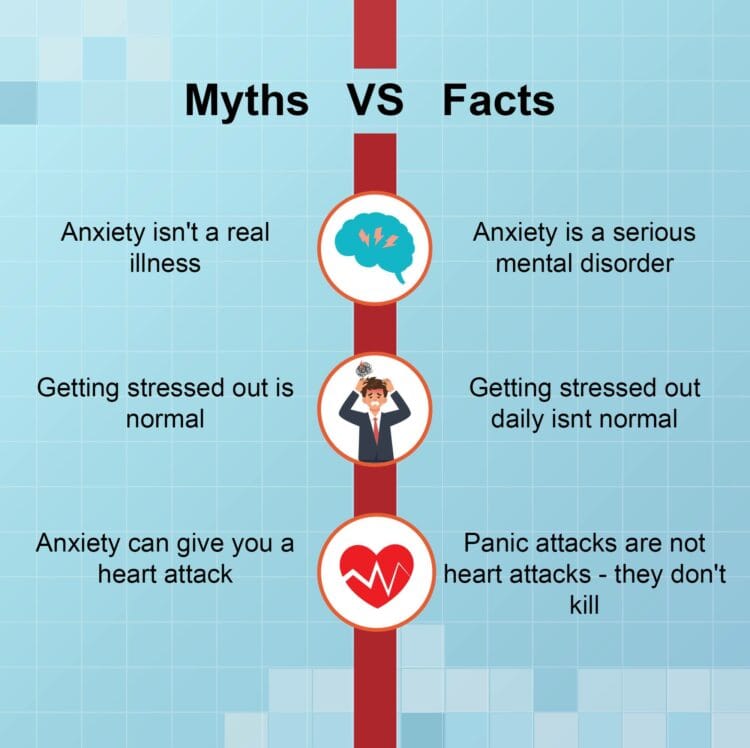 The survey covers residents of households, and persons in non-institutional cluster quarters (e.g., rooming/boarding homes, school dormitories, and migratory workers' camps). This survey doesn't include persons who, for the whole year, had no permanent address (e.g., homeless and/or travellers), who were on active military duty; or who resided in institutional cluster quarters (e.g., punitive facilities, nursing homes, mental institutions, long-run hospitals).
The survey covers residents of households, and persons in non-institutional cluster quarters (e.g., rooming/boarding homes, school dormitories, and migratory workers' camps). This survey doesn't include persons who, for the whole year, had no permanent address (e.g., homeless and/or travellers), who were on active military duty; or who resided in institutional cluster quarters (e.g., punitive facilities, nursing homes, mental institutions, long-run hospitals).
Results
Prevalence of major depressive episode among adolescents
A calculable 3.1 million adolescents within the US had a minimum of one major depressive episode. This number depicted 12.8% of the US adolescents. The prevalence of major depressive episode was higher among adolescent females (19.4%) compared to males (6.4%). The prevalence of major depressive episode was highest among adolescents reported 2 or additional races (13.8%) (Figure 1).
Figure 1. Prevalence of major depressive episode among U. S. adolescents in 2016
S. adolescents in 2016
Treatment of major depressive episode among adolescents
Treatment varieties enclosed caregiver only, medication only, and combined caregiver and medicine. A calculable nineteen received care by a caregiver alone and another nineteen received combined care by a caregiver and medicine treatment. Treatment with medication alone was least common (2%). Approximately hour of adolescents with major depressive episode didn't receive treatment (Figure 2).
Figure 2. Treatment received among the past year by U.S. adolescents aged 12-17 with major depressive episode in 2016
Treatment
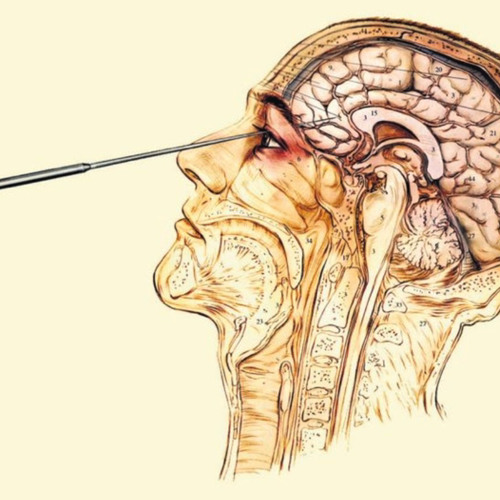
Major or Clinical Depression is a serious however treatable health problem. Depending on the severity of symptoms, your medical aid doctor or a specialist could suggest treatment. A large range of treatments are available for depression and new treatments (particularly medications) often appear. Continuing research implies that the proof for how well a treatment works is usually ever-changing too. Depressions that are a lot of biological in their origins of melancholic depression and psychotic depression has more probability to wish physical treatments like antidepressants and less probability to be resolved with psychological treatments alone. Non-melancholic depression that is linked to psychological factors, temperament characteristics and disagreeable life events, responds to each psychological treatments and physical treatments. May also recommend psychotherapy, or talk therapy, during which you address your emotional state.
Depressions that are a lot of biological in their origins of melancholic depression and psychotic depression has more probability to wish physical treatments like antidepressants and less probability to be resolved with psychological treatments alone. Non-melancholic depression that is linked to psychological factors, temperament characteristics and disagreeable life events, responds to each psychological treatments and physical treatments. May also recommend psychotherapy, or talk therapy, during which you address your emotional state.
Conclusion
2021 Copyright OAT. All rights reserv
Depression’s price to the US economy each year is estimated at 44 billion greenbacks [10]. This sickness is second only to cancer on the impact of our society. By itself depression will cause extreme disappointment, anxiety, insomnia and even thoughts of suicide. And yet, we don’t have an enormous organization to assist those that suffer from it. There's no “Association for Depressed.” Why is this? Why don’t the people of the US place one thing together to support and guide those that are suffering from depression?
There's no “Association for Depressed.” Why is this? Why don’t the people of the US place one thing together to support and guide those that are suffering from depression?
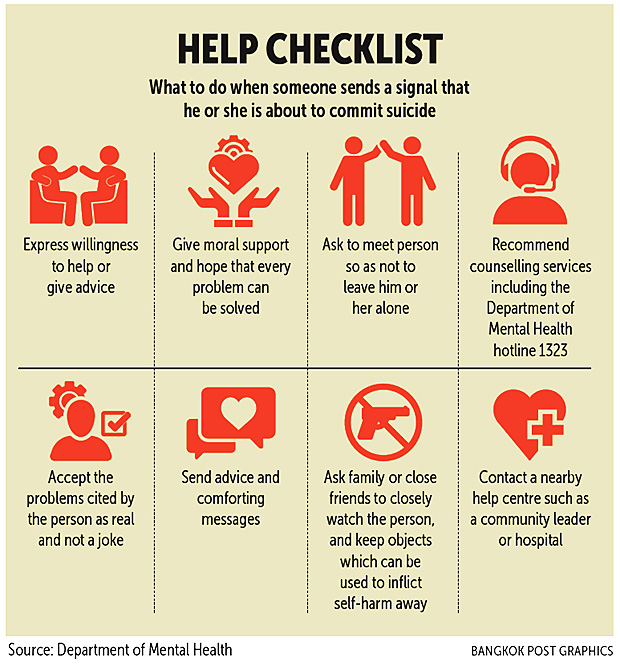
Depression isn't a matter to take thinly. It's not one thing to head off frequently, however to take to heart and realize help. Many individuals commit suicide on a daily basis due to depression. If you're or grasp somebody who is depressed get help. Don't hold it in forever, for you may be prone to the same issue. Lots of individuals get depression confused with extreme unhappiness. Depression isn't a term simply to be thrown around; it's a severe state of being.
References
- Schmidt CW (2007) Environmental connections: a deeper look into mental illness. Environ Health Perspect 115: A404-A410. [Crossref]
- Albert PR (2015) Why is depression more prevalent in women? J Psychiatry Neurosci 40: 219-221. [Crossref]
- Benazzi F (2006) Various forms of depression.
 Dialogues Clin Neurosci 8: 151-161. [Crossref]
Dialogues Clin Neurosci 8: 151-161. [Crossref] - Gayman MD, Turner RJ, Cui M (2008) Physical limitations and depressive symptoms: exploring the nature of the association. J Gerontol B Psychol Sci Soc Sci 63: S219-S28. [Crossref]
- Brook DW, Brook JS, Zhang C, Cohen P, Whiteman M (2002) Drug use and the risk of major depressive disorder, alcohol dependence, and substance use disorders. Arch Gen Psychiatry 59: 1039-1044. [Crossref]
- Paterniti S, Sterner I, Caldwell C, Bisserbe JC (2017) Childhood neglect predicts the course of major depression in a tertiary care sample: a follow-up study. BMC Psychiatry 17: 113. [Crossref]
- Kennedy SH (2008) Core symptoms of major depressive disorder: relevance to diagnosis and treatment. Dialogues Clin Neurosci 10: 271-277. [Crossref]
- Perlman K, Benrimoh D, Israel S, Rollins C, Brown E, et al.
 (2018) A systematic meta-review of predictors of antidepressant treatment outcome in major depressive disorder. J Affect Disord 243: 503-515. [Crossref]
(2018) A systematic meta-review of predictors of antidepressant treatment outcome in major depressive disorder. J Affect Disord 243: 503-515. [Crossref] - Park-Lee E, Lipari RN, Hedden SL, Kroutil LA, Porter JD (2016) Receipt of Services for Substance Use and Mental Health Issues Among Adults. CBHSQ Data Review, Rockville (MD). [Crossref]
- Chiu M, Lebenbaum M, Cheng J, de Oliveira C, Kurdyak P (2017) The direct healthcare costs associated with psychological distress and major depression: A population-based cohort study in Ontario, Canada. PloS one 12: e0184268. [Crossref]
Editorial Information
Editor-in-Chief
Article Type
Review Article
Publication history
Received: October 11, 2018
Accepted: October 22, 2018
Published: October 25, 2018
Copyright
©2018 Kandhakatla R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.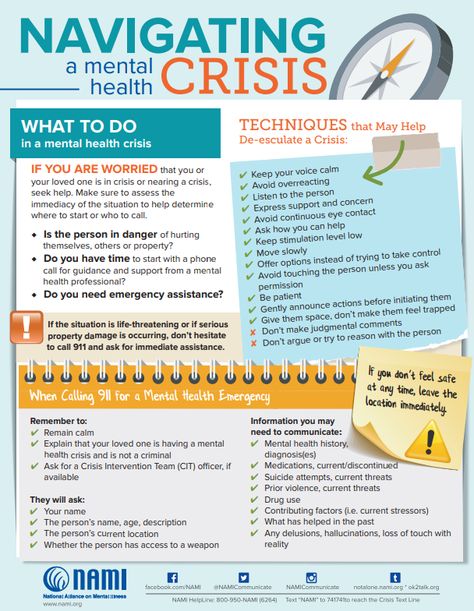
Citation
Kandhakatla R, Yarra R, Pallepati A, Patra S (2018) Depression- A common cold of mental disorders. Alzheimers Dement Cogn Neurol 2: DOI: 10.15761/ADCN.1000124.
Figure 1. Prevalence of major depressive episode among U.S. adolescents in 2016
Figure 2. Treatment received among the past year by U.S. adolescents aged 12-17 with major depressive episode in 2016
Anxiety & Depression the Common Colds of Mental Health
You may have heard depression and anxiety being referred to as the common colds of mental health. At first, it appears that this analogy has some truth. Colds are widespread and can affect anyone, of any age, at any time – like depression and anxiety. Just like general doctors see many patients due to cold symptoms, therapists see many patients due to the symptoms of anxiety and depression. However, this is where the similarities end and the analogy can become misleading. Depression and anxiety cannot be caught from another person, and you do not recover from them after a few days of rest. They may be common, but they will not go away on their own and need treatment. It is vital to highlight that just because depression and anxiety are frequently seen, it does not make them any less important. It is useful to understand the signs and symptoms of both of these mental health conditions so that you can seek help early for either yourself or a loved one.
They may be common, but they will not go away on their own and need treatment. It is vital to highlight that just because depression and anxiety are frequently seen, it does not make them any less important. It is useful to understand the signs and symptoms of both of these mental health conditions so that you can seek help early for either yourself or a loved one.
Depression
We all go through times in our life where we feel a bit down, but depression is much more than that. It persistently affects you for weeks or months causing feelings of unhappiness and hopelessness. You may lose interest in the activities you used to enjoy and feel tearful a lot of the time. Although it can lead to a range of different emotional and physical symptoms, here are a few of the common symptoms to look out for:
- Having a hopeless or helpless outlook on life
- Loss of interest in activities you used to enjoy
- Having a low mood, feeling sad, and experiencing uncontrollable emotions
- Sleep problems – sleeping too much or too little, and feeling fatigued
- Changes in appetite – eating too much or not enough.
 Weight gain or weight loss without actively trying to change weight
Weight gain or weight loss without actively trying to change weight - Symptoms of anxiety (see below for more details)
- Difficulty concentrating or making decisions
- Thoughts of worthlessness, death, or suicide
Depression can be a serious condition and has a significant impact on a person’s life. Symptoms range from mild to severe and affect every individual differently. If you are experiencing symptoms of depression, it is important to seek help. However big or small your worry may be, Sollars & Associates has 17 locations in Michigan that are here to support you.
Anxiety
Anxiety is a persistent feeling of fear, worry, or uneasiness that can be very intense. It’s normal to feel anxious in certain situations like attending a job interview or sitting an exam, but it is not normal if these feelings are constant and being to control your life. There are many different types of anxiety disorders that people can experience, such as phobias, post-traumatic stress disorder, panic disorder, or separation anxiety to name a few.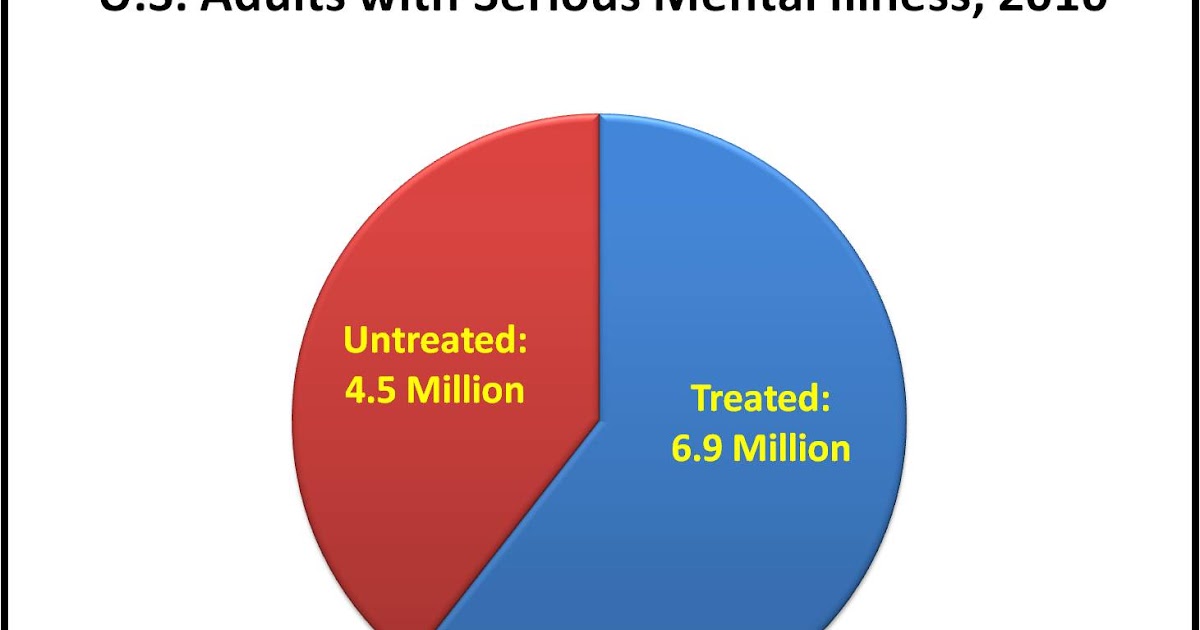 Similar to depression, anxiety can cause both emotional and physical symptoms that vary from person to person. Some of the common symptoms to look out for include:
Similar to depression, anxiety can cause both emotional and physical symptoms that vary from person to person. Some of the common symptoms to look out for include:
- Feeling worried, tense, nervous, or restless
- Problems sleeping due to worry or fear
- Physical symptoms such as a fast heart rate, sweating, shaking, dizziness, stomach problems, or rapid breathing
- Increased fatigue and weakness
- Difficulty concentrating and easily distracted by worry
- A feeling of impending doom or danger
- Experiencing nightmares and vivid dreams
Depression and anxiety are two different problems, but some people may experience both. It is important to try not to worry about labels. Both these conditions are common in fact, depression is the leading cause of disability worldwide. So, if you are experiencing symptoms of depression or anxiety – you are not alone. Most importantly, both conditions are treatable.
If you are looking for in-person or online counseling sessions in Michigan, then Sollars & Associates is here to help you.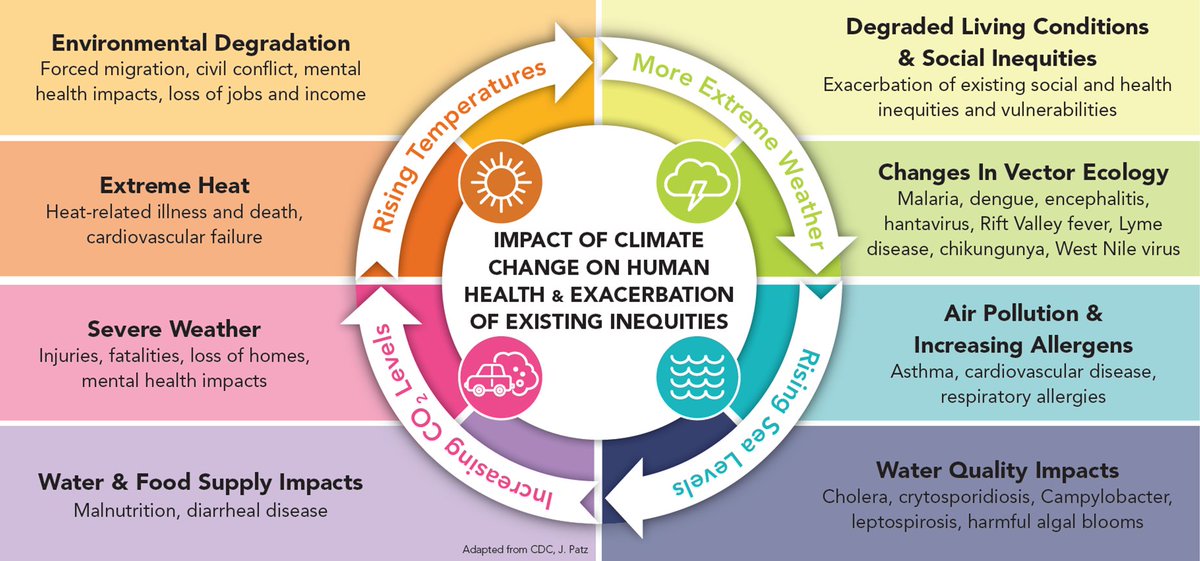 We have 17 locations all across Michigan, and it is easy to get in touch. Just fill out an online form or call us on (248) 787-0855 today. Our therapists are here to support your emotional and mental health needs.
We have 17 locations all across Michigan, and it is easy to get in touch. Just fill out an online form or call us on (248) 787-0855 today. Our therapists are here to support your emotional and mental health needs.
Psychosomatics of colds
The common cold is an acute infection of the upper respiratory tract, which usually occurs during the cold season. Cold, however, is not the cause of the disease - it facilitates the transmission of infection.
From the point of view of psychosomatics, our diseases are not only the result of viruses, bacteria, microorganisms, but also internal psycho-emotional states. For example, some people can get sick for only one day, lie down, and the very next day the illness, as it never happened. In others, the disease drags on, it is difficult to treat, and complications of the acute respiratory disease, SARS appear ... Some are constantly infected with viruses from their family members, colleagues, classmates . .. Others, for example, a mother caring for her child, on the contrary, do not get sick.
.. Others, for example, a mother caring for her child, on the contrary, do not get sick.
Morbidity statistics show the relationship between mental factors and the clinic of infectious diseases. Neurasthenics get upper respiratory tract infections 2-3 times more often and suffer from them longer than the general population on average. Experience shows that a person's susceptibility to respiratory viruses depends on his emotional state, and the personality itself, character traits, determines the specific picture of the disease and the course of the infectious disease. When we are waiting for someone at the station, we do not pay attention to hundreds of people passing by, because we are only interested in one, and the infection sees only the one who "needs" it.
Psychologists explain the reason for the development of the disease with the concept of “secondary benefit”. This term in psychology means that a person gains unconscious benefits during a cold. At the root of a cold, most often, there is overwork, an inability to solve and process the “little things” of everyday life and a desire to finally relax and get the attention of loved ones.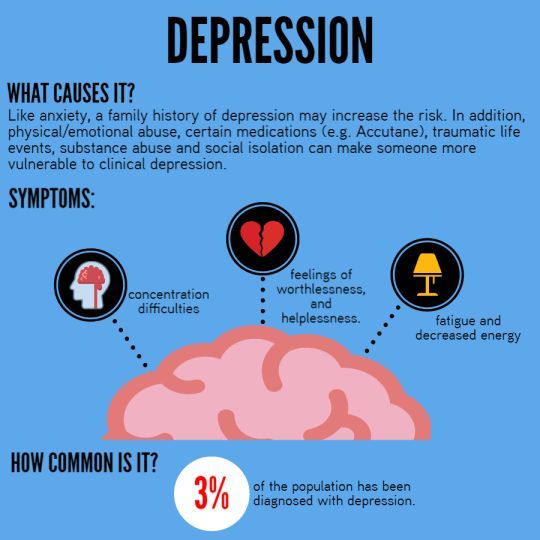
Somatization begins to act when it is not possible to find another way out.
In order to understand the problem of secondary benefits in relation to the disease, it is necessary to find the cause. But it happens that one negative emotion entails many consequences, which can be very difficult to understand and can take a long time to work with a psychologist. Fortunately, now there are diagnostic methods that can accurately and quickly, within an hour, determine the key reason - to specify an emotion, a psychological problem. Often the cause of a cold is completely unexpected reasons that lie deep in the subconscious.
Only by establishing the primary motivation and identifying the infection, the doctor can cure the patient.
Method for the treatment of frequent colds. A 34-year-old patient came to us with complaints of chronic colds lasting for months, persistent cough and heart pain. General recommendations - to treat duties easier, not to take everything to heart, brought a slight retreat of the disease.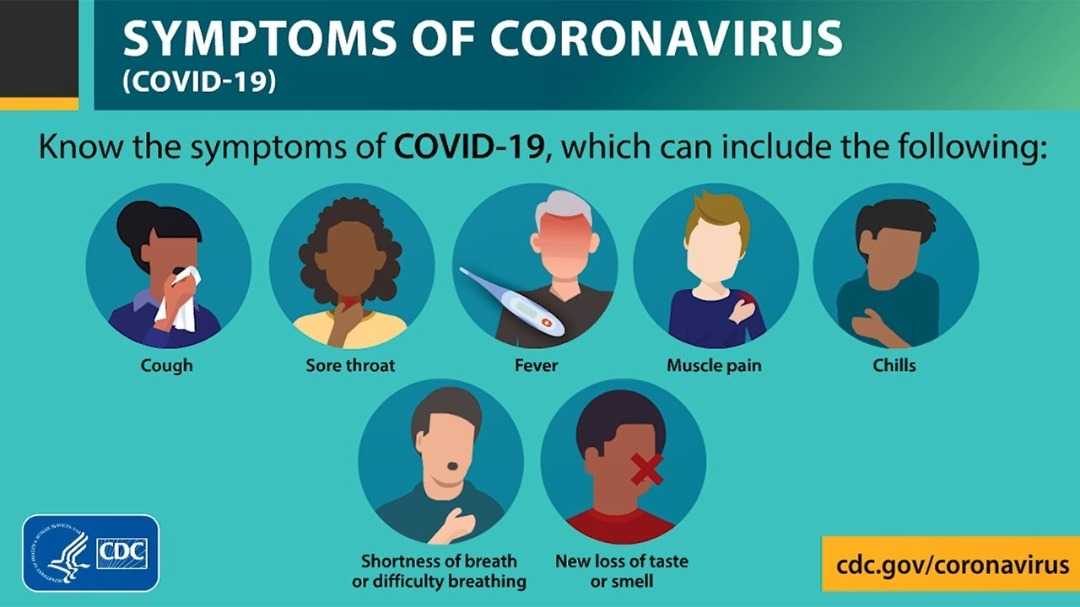
In the process of diagnosing the psycho-emotional state, relatively persistent cough, it turned out that the patient is experiencing difficulties with the distribution of funds. It turned out that the reason for the depression of the body was the fact that the patient has been working in a low-paid position for many years, which upsets her very much, but she is simply afraid to change jobs.
What we did in her case was to select an individual psychosomatic drug that changes her attitude to financial expenses. Surprisingly, you will say, but the patient noticeably improved with this approach to the treatment of her problem. Two months later, the fears receded and she became interested in a hobby that began to bring her additional income.
Over the past couple of years, she no longer complained of colds.
If you are tired of debilitating "colds" or your child constantly "catches the virus", then remember that you always have the opportunity to contact our specialists who will determine the exact psycho-emotional component and the true cause of your disease and, most importantly, they will resolve it in the safest and most comfortable way.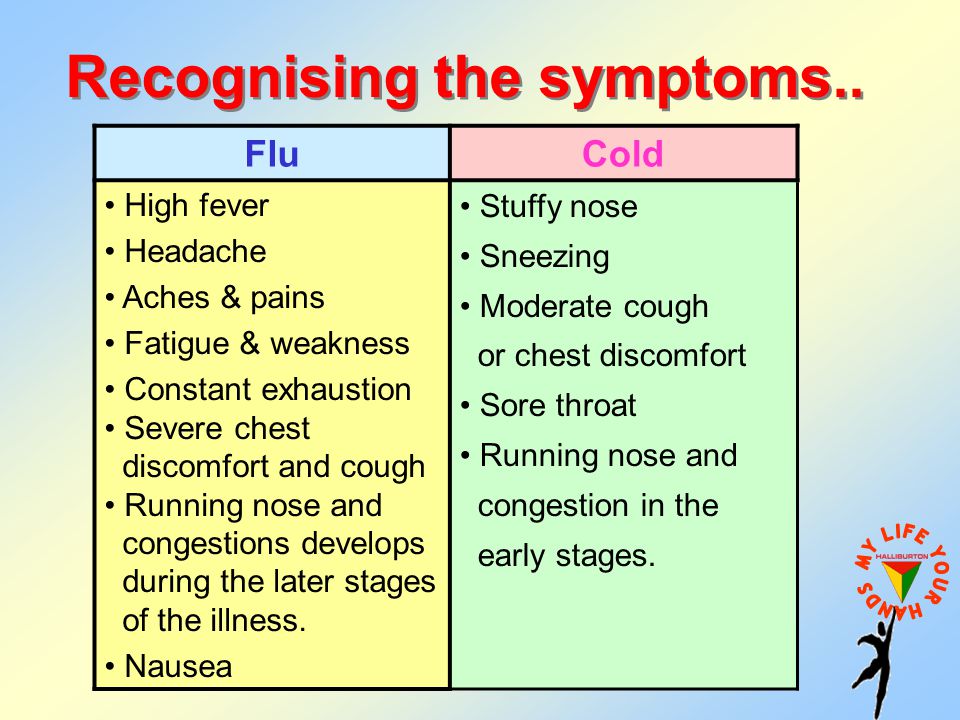
Be healthy!
Doctor Zhanna Zoltanovna Kopas
Georgy Kostyuk: Viruses can become a trigger for many diseases0003
04/12/2020 18:14
Heading:
Society And many, as it turned out, are completely unprepared for such a turn. Scandals, psychoses… How to deal with stress within four walls? How to protect yourself and your loved ones from nervous breakdowns? The RG columnist talks about this with the chief psychiatrist of Moscow, Doctor of Medical Sciences, Professor Georgy Kostyuk.
Alexander Korolkov / RG
Georgy Petrovich, is there an increase in mental illness during a pandemic and self-isolation?
Georgy Kostyuk: Yes, this is the first time this has happened... And we have yet to find out what psychological consequences this phenomenon conceals. The information that we have now indicates an aggravation of the problems that already exist in a person in the family.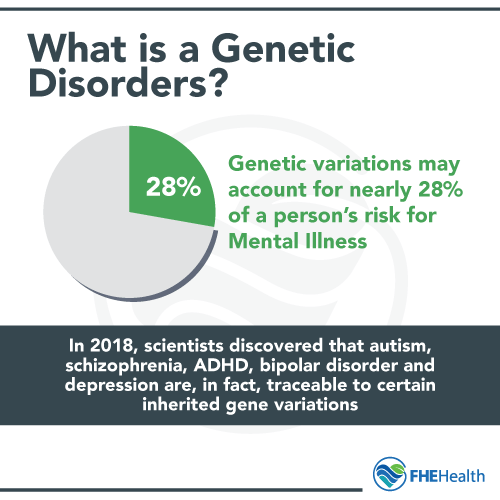 For example, the increase in cases of domestic violence.
For example, the increase in cases of domestic violence.
And if we talk about the consequences of the pandemic, we still cannot say exactly what they will be for the coronavirus pandemic, but we can remember the history. We have survived pandemics of swine, bird flu, SARS, which were quite recent, 10-20 years ago. These pandemics have not affected Russia as much as some other countries. However, we can find out the results of studies conducted in countries where the pandemic has been. Now they often remember the Spanish flu epidemic, which happened exactly 100 years ago.
There are scientific publications that analyze the impact of the pandemic on mental health. The research considers three aspects: immediate psychological reactions during a pandemic, mental disorders in those who are ill with a viral infection, and long-term consequences for the nervous system and psyche.
If we talk about the first aspect, about psychological reactions, we can cite as an example a study conducted during the swine flu epidemic among residents of the UK. The survey showed that about 40 percent of people have significantly changed their lifestyle. Formally, they followed all the recommendations of experts: they left the house less often, washed their hands more often, and disinfected surfaces. However, they also experienced high levels of anxiety. And some of them perceived the usual cold symptoms as manifestations of swine flu.
The survey showed that about 40 percent of people have significantly changed their lifestyle. Formally, they followed all the recommendations of experts: they left the house less often, washed their hands more often, and disinfected surfaces. However, they also experienced high levels of anxiety. And some of them perceived the usual cold symptoms as manifestations of swine flu.
If we talk about more serious mental disorders, then we can recall the American psychiatrist Carl Menninger, who made an interesting observation during the Spanish flu epidemic a century ago .
George Kostyuk : Yes. The clinic where he worked began to receive a large number of patients with influenza, which was accompanied by psychotic symptoms. At the same time, the symptoms of psychosis disappeared as soon as patients recovered from the flu.
From the point of view of long-term consequences, the influence of viral infections on the occurrence of severe mental disorders is considered.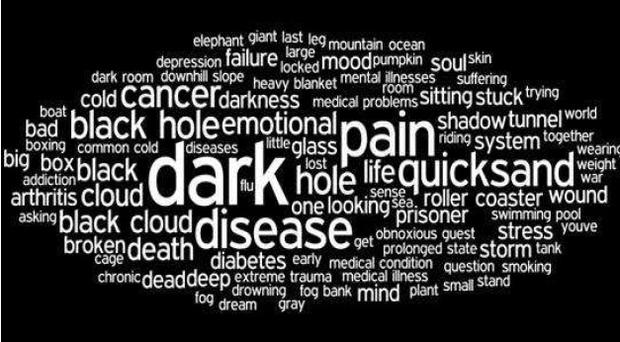 Such as schizophrenia, dementia, mental retardation. It has been observed that children who are born during the winter months, i.e. the months of spikes in seasonal illnesses, are more likely to suffer from schizophrenia. There are also risks during pregnancy: if a woman suffered a viral disease during pregnancy, then the risk of developing disorders of the nervous system increases in the child born.
Such as schizophrenia, dementia, mental retardation. It has been observed that children who are born during the winter months, i.e. the months of spikes in seasonal illnesses, are more likely to suffer from schizophrenia. There are also risks during pregnancy: if a woman suffered a viral disease during pregnancy, then the risk of developing disorders of the nervous system increases in the child born.
Viral infections may increase the risk of delirium, Parkinson's disease and Alzheimer's disease in the elderly. At the same time, it is impossible to clearly predict that some changes in the psyche may occur in a particular person together with a viral infection. Nevertheless, viruses can act as a trigger not only for mental illness, but also somatic ones. We must not forget about the vulnerability of each individual and the genetic predisposition to the development of changes in the psyche.
Today we know that the influence of viruses on the nervous system and psyche is possible, but we do not find direct correlations. Most likely, as with any complex phenomena, there is a combination of factors: genetic predisposition, vulnerability of the organism and the influence of external circumstances.
Most likely, as with any complex phenomena, there is a combination of factors: genetic predisposition, vulnerability of the organism and the influence of external circumstances.
Is self-isolation fraught with long-term consequences?
Georgy Kostyuk: So far, we cannot give a clear answer to the question of whether self-isolation will have long-term consequences for each of us. Naturally, everything depends on the conditions and circumstances in which a person is isolated. One story, if this is a conscious choice of a person who has a constant income, good housing, and prosperous family relationships. If none of his loved ones was affected by the virus, if there are interests that allow you not to get bored during isolation. It is a completely different story if at least some of the life circumstances from this list are not so prosperous. But even in this case, much will depend on the initial mental characteristics of a person, on his adaptability. After all, it is known that even under the most terrible circumstances, during catastrophes, wars, not all people begin to suffer from mental disorders.
After all, it is known that even under the most terrible circumstances, during catastrophes, wars, not all people begin to suffer from mental disorders.
How can people who live in cramped conditions cope with isolation? People with children who find it difficult to explain that you can’t go out?
Georgy Kostyuk: Indeed, for many this can be a problem. But it cannot be said that this problem will be completely new; rather, it will be exacerbated. In the case of children, everything initially depends on how the parents used to build their relationship with them. If the relationship is understanding, loving, if parents are interested in spending time with children, then joint isolation is unlikely to be a torment. Children, on the other hand, easily turn unusual life circumstances into a game. They have a developed imagination, so you can and should use these properties of the child's psyche to overcome the stress of isolation. Play more, communicate, learn something new together.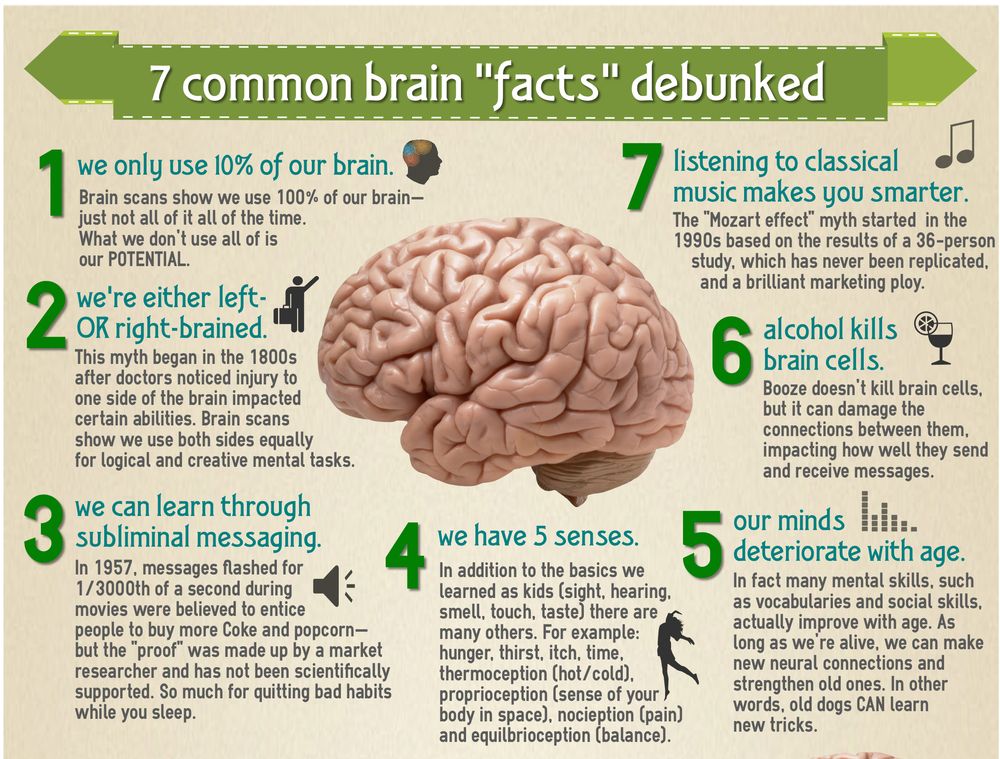 Exercise together. You need to allow children to sometimes rage, throw out their energy. Communication with parents is most often a basic need for children. Much more than the need for walking. If this is provided, then it is unlikely that the child will miss the street very much.
Exercise together. You need to allow children to sometimes rage, throw out their energy. Communication with parents is most often a basic need for children. Much more than the need for walking. If this is provided, then it is unlikely that the child will miss the street very much.
As a rule, in conditions of self-isolation, the problems that already exist in a person in the family become aggravated
Is our psychiatric service ready to provide assistance in the current conditions?
Georgy Kostyuk: Medical institutions are now being urgently redesigned to combat the coronavirus. And psychiatric hospitals will be ready to provide their resources if necessary.
Currently, the work of the psychiatric service is aimed at providing the maximum possible psychological and psychotherapeutic support. On the basis of the Moscow psychiatric hospitals named after Alekseev, named after Gannushkin, there are telephone psychological assistance services for the population of Moscow.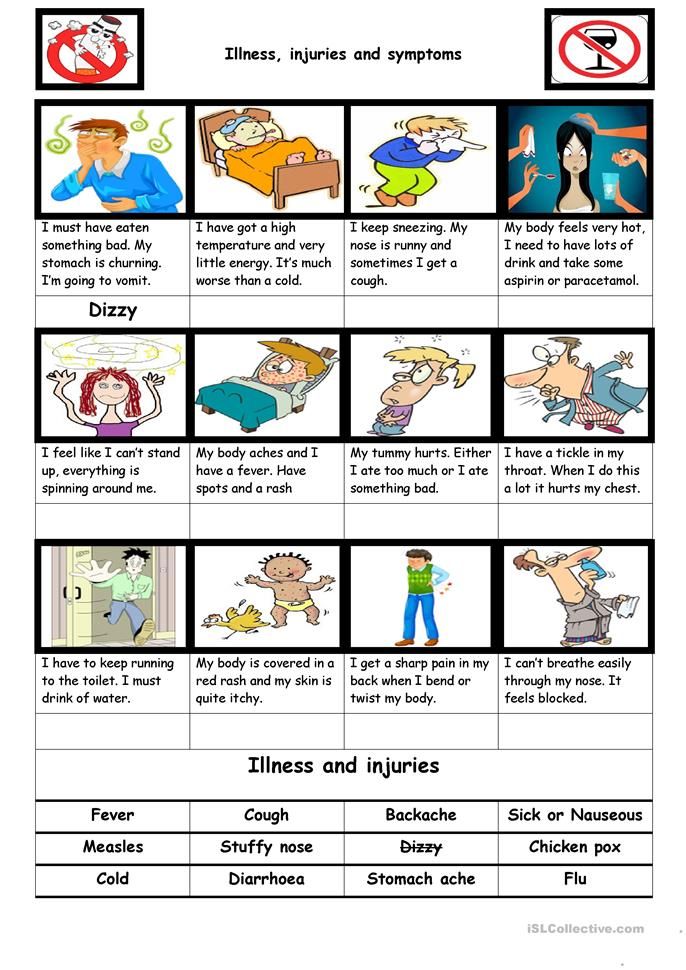 In the Alekseev hospital, in a specially equipped room, in compliance with all prescribed measures aimed at preventing the spread of a new virus, video communication between patients and their relatives was organized. And so, despite the quarantine, loved ones can see each other and talk to each other. In the format of video communication, conversations of relatives of patients with attending physicians are also taking place.
In the Alekseev hospital, in a specially equipped room, in compliance with all prescribed measures aimed at preventing the spread of a new virus, video communication between patients and their relatives was organized. And so, despite the quarantine, loved ones can see each other and talk to each other. In the format of video communication, conversations of relatives of patients with attending physicians are also taking place.
Hospitals are operating as normal and providing patient care, outreach teams and home care. The service is ready to respond flexibly to the needs of the population.
Mental illness is not contagious. They are not an infection. But in general they are much more dangerous. Or?..
Georgy Kostyuk: Mental illness is most often associated with the quality of life and how a person functions in society, rather than with an immediate threat to life. But the indirect consequences can be very serious: with these disorders, a person can lose the opportunity to work normally, live independently, and enjoy life. Yes, there are those ailments that are associated with issues of life and death - suicidal behavior, eating disorders, psychomotor agitation and others. Mental disorders are a big burden on society. They lead to indirect long-term consequences. And the features of these consequences are different from infectious diseases. It is no coincidence that WHO considers the consequences of infectious and non-communicable diseases separately. If we single out the proportion of mental illnesses among noncommunicable diseases, they consistently appear in the top ten.
Yes, there are those ailments that are associated with issues of life and death - suicidal behavior, eating disorders, psychomotor agitation and others. Mental disorders are a big burden on society. They lead to indirect long-term consequences. And the features of these consequences are different from infectious diseases. It is no coincidence that WHO considers the consequences of infectious and non-communicable diseases separately. If we single out the proportion of mental illnesses among noncommunicable diseases, they consistently appear in the top ten.
In general, people with mental disorders are much less of a threat to society than people without obvious signs of such disorders.
Children should be allowed to run wild sometimes, throw out their energy. Communication with parents is most often the main need of a child.
Georgy Kostyuk: Most of us are now focused on the dangers of the coronavirus situation and the general negativity. But there are also positive moments. We can feel the importance of human life, the reality of mutual help and support, we can reconsider our value system.
But there are also positive moments. We can feel the importance of human life, the reality of mutual help and support, we can reconsider our value system.
For physicians, the good side of this situation is that now, instead of the usual theoretical talk about the importance of the medical field, there is a real advancement of medicine and science to the fore. Medical workers are perceived as heroes, they break applause every day in many countries of the world. It is unlikely that they have ever received such a standing ovation before! And those who receive medical care now can make sure that health workers are ready to leave home to do their job.
A unique moment for culture is that museums, theatres, cinemas, bookstores offer free virtual access to their treasures. Universities open access to their educational resources. Could we have thought that venerable specialists would conduct virtual lessons for schoolchildren?
The usual way of life with constant fuss, excessive consumption, entertainment is now impossible for many.