How to know if i have bpd
Borderline Personality Disorder (BPD) - HelpGuide.org
personality disorders
If you have BPD, everything feels unstable: your relationships, moods, thinking, behavior—even your identity. But there is hope and this guide to symptoms, treatment, and recovery can help.
What is borderline personality disorder (BPD)?
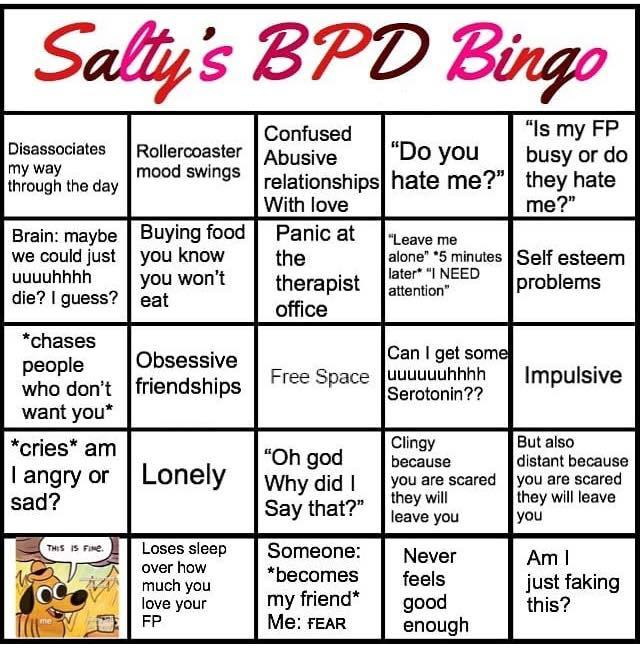
If you have borderline personality disorder (BPD), you probably feel like you're on a rollercoaster—and not just because of your unstable emotions or relationships, but also the wavering sense of who you are. Your self-image, goals, and even your likes and dislikes may change frequently in ways that feel confusing and unclear.
People with BPD tend to be extremely sensitive. Some describe it as like having an exposed nerve ending. Small things can trigger intense reactions. And once upset, you have trouble calming down. It's easy to understand how this emotional volatility and inability to self-soothe leads to relationship turmoil and impulsive—even reckless—behavior.
When you're in the throes of overwhelming emotions, you're unable to think straight or stay grounded. You may say hurtful things or act out in dangerous or inappropriate ways that make you feel guilty or ashamed afterwards. It's a painful cycle that can feel impossible to escape. But it's not. There are effective BPD treatments and coping skills that can help you feel better and back in control of your thoughts, feelings, and actions.
With over 25,000 licensed counselors, BetterHelp has a therapist that fits your needs. It's easy, affordable, and convenient.
GET 20% OFF
Online-Therapy.com is a complete toolbox of support, when you need it, on your schedule. It only takes a few minutes to sign up.
GET 20% OFF
Teen Counseling is an online therapy service for teens and young adults. Connect with your counselor by video, phone, or chat.
GET 20% OFF
BPD is treatable
In the past, many mental health professionals found it difficult to treat borderline personality disorder (BPD), so they came to the conclusion that there was little to be done. But we now know that BPD is treatable. In fact, the long-term prognosis for BPD is better than those for depression and bipolar disorder. However, it requires a specialized approach. The bottom line is that most people with BPD can and do get better—and they do so fairly rapidly with the right treatments and support.
But we now know that BPD is treatable. In fact, the long-term prognosis for BPD is better than those for depression and bipolar disorder. However, it requires a specialized approach. The bottom line is that most people with BPD can and do get better—and they do so fairly rapidly with the right treatments and support.
[Read: Helping Someone with Borderline Personality Disorder]
Healing is a matter of breaking the dysfunctional patterns of thinking, feeling, and behaving that are causing you distress. It's not easy to change lifelong habits. Choosing to pause, reflect, and then act in new ways will feel unnatural and uncomfortable at first. But with time you'll form new habits that help you maintain your emotional balance and stay in control.
Recognizing borderline personality disorder
Do you identify with the following statements?
- I often feel “empty.”
- My emotions shift very quickly, and I often experience extreme sadness, anger, and anxiety.
- I'm constantly afraid that the people I care about will abandon me or leave me.
- I would describe most of my romantic relationships as intense, but unstable.
- The way I feel about the people in my life can dramatically change from one moment to the next—and I don't always understand why.
- I often do things that I know are dangerous or unhealthy, such as driving recklessly, having unsafe sex, binge drinking, using drugs, or going on spending sprees.
- I've attempted to hurt myself, engaged in self-harm behaviors such as cutting, or threatened suicide.
- When I'm feeling insecure in a relationship, I tend to lash out or make impulsive gestures to keep the other person close.
If you identify with several of the statements, you may suffer from borderline personality disorder. Of course, you need a mental health professional to make an official diagnosis, as BPD can be easily confused with other issues.
[Read: Borderline Personality Disorder Test]
But even without a diagnosis, you may find the self-help tips in this article helpful for calming your inner emotional storm and learning to control self-damaging impulses.
Borderline personality disorder (BPD) manifests in many different ways, but for the purposes of diagnosis, mental health professionals group the symptoms into nine major categories. In order to be diagnosed with BPD, you must show signs of at least five of these symptoms. Furthermore, the symptoms must be long-standing (usually beginning in adolescence) and impact many areas of your life.
The 9 symptoms of BPD
- Fear of abandonment. People with BPD are often terrified of being abandoned or left alone. Even something as innocuous as a loved one arriving home late from work or going away for the weekend may trigger intense fear. This can prompt frantic efforts to keep the other person close. You may beg, cling, start fights, track your loved one's movements, or even physically block the person from leaving. Unfortunately, this behavior tends to have the opposite effect—driving others away.
- Unstable relationships. People with BPD tend to have relationships that are intense and short-lived.
 You may fall in love quickly, believing that each new person is the one who will make you feel whole, only to be quickly disappointed. Your relationships either seem perfect or horrible, without any middle ground. Your lovers, friends, or family members may feel like they have emotional whiplash as a result of your rapid swings from idealization to devaluation, anger, and hate.
You may fall in love quickly, believing that each new person is the one who will make you feel whole, only to be quickly disappointed. Your relationships either seem perfect or horrible, without any middle ground. Your lovers, friends, or family members may feel like they have emotional whiplash as a result of your rapid swings from idealization to devaluation, anger, and hate. - Unclear or shifting self-image. When you have BPD, your sense of self is typically unstable. Sometimes you may feel good about yourself, but other times you hate yourself, or even view yourself as evil. You probably don't have a clear idea of who you are or what you want in life. As a result, you may frequently change jobs, friends, lovers, religion, values, goals, or even sexual identity.
- Impulsive, self-destructive behaviors. If you have BPD, you may engage in harmful, sensation-seeking behaviors, especially when you're upset. You may impulsively spend money you can't afford, binge eat, drive recklessly, shoplift, engage in risky sex, or overdo it with drugs or alcohol.
 These risky behaviors may help you feel better in the moment, but they hurt you and those around you over the long-term.
These risky behaviors may help you feel better in the moment, but they hurt you and those around you over the long-term. - Self-harm. Suicidal behavior and deliberate self-harm is common in people with BPD. Suicidal behavior includes thinking about suicide, making suicidal gestures or threats, or actually carrying out a suicide attempt. Self-harm encompasses all other attempts to hurt yourself without suicidal intent. Common forms of self-harm include cutting and burning.
- Extreme emotional swings. Unstable emotions and moods are common with BPD. One moment, you may feel happy, and the next, despondent. Little things that other people brush off can send you into an emotional tailspin. These mood swings are intense, but they tend to pass fairly quickly (unlike the emotional swings of depression or bipolar disorder), usually lasting just a few minutes or hours.
- Chronic feelings of emptiness. People with BPD often talk about feeling empty, as if there's a hole or a void inside them.
 At the extreme, you may feel as if you're “nothing” or “nobody.” This feeling is uncomfortable, so you may try to fill the void with things like drugs, food, or sex. But nothing feels truly satisfying.
At the extreme, you may feel as if you're “nothing” or “nobody.” This feeling is uncomfortable, so you may try to fill the void with things like drugs, food, or sex. But nothing feels truly satisfying. - Explosive anger. If you have BPD, you may struggle with intense anger and a short temper. You may also have trouble controlling yourself once the fuse is lit—yelling, throwing things, or becoming completely consumed by rage. It's important to note that this anger isn't always directed outwards. You may spend a lot of time feeling angry at yourself.
- Feeling suspicious or out of touch with reality. People with BPD often struggle with paranoia or suspicious thoughts about others' motives. When under stress, you may even lose touch with reality—an experience known as dissociation. You may feel foggy, spaced out, or as if you're outside your own body.
Common co-occurring disorders
Borderline personality disorder is rarely diagnosed on its own. Common co-occurring disorders include:
Common co-occurring disorders include:
- depression or bipolar disorder
- substance abuse
- eating disorders
- anxiety disorders
When BPD is successfully treated, the other disorders often get improve, too. But the reverse isn't always true. For example, you may successfully treat symptoms of depression and still struggle with BPD.
Affiliate disclosure
Affordable online therapy for individuals and couples
Online-Therapy.com is the leading online provider of cognitive behavioral therapy (CBT). In addition to video, phone, and chat therapy sessions, they offer a complete online therapy toolbox with activity plans, worksheets, videos, and more.
Get instant access, wherever you are. It only takes a few minutes to sign up.
GET STARTED WITH 20% OFF
Causes—and hope
Most mental health professionals believe that borderline personality disorder (BPD) is caused by a combination of inherited or internal biological factors and external environmental factors, such as traumatic experiences in childhood.
Brain differences
There are many complex things happening in the BPD brain, and researchers are still untangling what it all means. But in essence, if you have BPD, your brain is on high alert. Things feel more scary and stressful to you than they do to other people. Your fight-or-flight switch is easily tripped, and once it's on, it hijacks your rational brain, triggering primitive survival instincts that aren't always appropriate to the situation at hand.
This may make it sound as if there's nothing you can do. After all, what can you do if your brain is different? But the truth is that you can change your brain. Every time you practice a new coping response or self-soothing technique you are creating new neural pathways. Some treatments, such as mindfulness meditation, can even grow your brain matter. And the more you practice, the stronger and more automatic these pathways will become. So don't give up! With time and dedication, you can change the way you think, feel, and act.
Personality disorders and stigma
When psychologists talk about “personality,” they're referring to the patterns of thinking, feeling, and behaving that make each of us unique. No one acts exactly the same all the time, but we do tend to interact and engage with the world in fairly consistent ways. This is why people are often described as “shy,” “outgoing,” “meticulous,” “fun-loving,” and so on. These are elements of personality.
Because personality is so intrinsically connected to identity, the term “personality disorder” might leave you feeling like there's something fundamentally wrong with who you are. But a personality disorder is not a character judgment. In clinical terms, “personality disorder” means that your pattern of relating to the world is significantly different from the norm. (In other words, you don't act in ways that most people expect). This causes consistent problems for you in many areas of your life, such as your relationships, career, and your feelings about yourself and others. But most importantly, these patterns can be changed!
But most importantly, these patterns can be changed!
Self-help tips: 3 keys to coping with BPD
- Calm the emotional storm
- Learn to control impulsivity and tolerate distress
- Improve your interpersonal skills
Self-help tip 1: Calm the emotional storm
As someone with BPD, you've probably spent a lot of time fighting your impulses and emotions, so acceptance can be a tough thing to wrap your mind around. But accepting your emotions doesn't mean approving of them or resigning yourself to suffering. All it means is that you stop trying to fight, avoid, suppress, or deny what you're feeling. Giving yourself permission to have these feelings can take away a lot of their power.
Try to simply experience your feelings without judgment or criticism. Let go of the past and the future and focus exclusively on the present moment. Mindfulness techniques can be very effective in this regard.
- Start by observing your emotions, as if from the outside.
- Watch as they come and go (it may help to think of them as waves).
- Focus on the physical sensations that accompany your emotions.
- Tell yourself that you accept what you're feeling right now.
- Remind yourself that just because you're feeling something doesn't mean it's reality.
[Listen: Eye of the Storm Meditation]
Do something that stimulates one or more of your senses
Engaging your sense is one of the quickest and easiest ways to quickly self-soothe. You will need to experiment to find out which sensory-based stimulation works best for you. You'll also need different strategies for different moods. What may help when you're angry or agitated is very different from what may help when you're numb or depressed. Here are some ideas to get started:
Touch. If you're not feeling enough, try running cold or hot (but not scalding hot) water over your hands; hold a piece of ice; or grip an object or the edge of a piece of furniture as tightly as you can. If you're feeling too much, and need to calm down, try taking a hot bath or shower; snuggling under the bed covers, or cuddling with a pet.
If you're feeling too much, and need to calm down, try taking a hot bath or shower; snuggling under the bed covers, or cuddling with a pet.
Taste. If you're feeling empty and numb, try sucking on strong-flavored mints or candies, or slowly eat something with an intense flavor, such as salt-and-vinegar chips. If you want to calm down, try something soothing such as hot tea or soup.
Smell. Light a candle, smell the flowers, try aromatherapy, spritz your favorite perfume, or whip up something in the kitchen that smells good. You may find that you respond best to strong smells, such as citrus, spices, and incense.
Sight. Focus on an image that captures your attention. This can be something in your immediate environment (a great view, a beautiful flower arrangement, a favorite painting or photo) or something in your imagination that you visualize.
Sound. Try listening to loud music, ringing a buzzer, or blowing a whistle when you need a jolt. To calm down, turn on soothing music or listen to the soothing sounds of nature, such as wind, birds, or the ocean. A sound machine works well if you can't hear the real thing.
To calm down, turn on soothing music or listen to the soothing sounds of nature, such as wind, birds, or the ocean. A sound machine works well if you can't hear the real thing.
Reduce your emotional vulnerability
You're more likely to experience negative emotions when you're run down and under stress. That's why it's very important to take care of your physical and mental well-being.
Take care of yourself by:
- Avoid mood-altering drugs
- Eating a balanced, nutritious diet
- Getting plenty of quality sleep
- Exercising regularly
- Minimizing stress
- Practicing relaxation techniques
Tip 2: Learn to control impulsivity and tolerate distress
The calming techniques discussed above can help you relax when you're starting to become derailed by stress. But what do you do when you're feeling overwhelmed by difficult feelings? This is where the impulsivity of borderline personality disorder (BPD) comes in. In the heat of the moment, you're so desperate for relief that you'll do anything, including things you know you shouldn't—such as cutting, reckless sex, dangerous driving, and binge drinking. It may even feel like you don't have a choice.
It may even feel like you don't have a choice.
Moving from being out of control of your behavior to being in control
It's important to recognize that these impulsive behaviors serve a purpose. They're coping mechanisms for dealing with distress. They make you feel better, even if just for a brief moment. But the long-term costs are extremely high.
Regaining control of your behavior starts with learning to tolerate distress. It's the key to changing the destructive patterns of BPD. The ability to tolerate distress will help you press pause when you have the urge to act out. Instead of reacting to difficult emotions with self-destructive behaviors, you will learn to ride them out while remaining in control of the experience.
For a step-by-step, self-guided program that will teach you how to ride the “wild horse” of overwhelming feelings, check out our free Emotional Intelligence Toolkit. The toolkit teaches you how to:
- get in touch with your emotions
- live with emotional intensity
- manage unpleasant or threatening feelings
- stay calm and focused even in upsetting situations
The toolkit will teach you how to tolerate distress, but it doesn't stop there. It will also teach you how to move from being emotionally shut down to experiencing your emotions fully. This allows you to experience the full range of positive emotions such as joy, peace, and fulfillment that are also cut off when you attempt to avoid negative feelings.
It will also teach you how to move from being emotionally shut down to experiencing your emotions fully. This allows you to experience the full range of positive emotions such as joy, peace, and fulfillment that are also cut off when you attempt to avoid negative feelings.
A grounding exercise to help you pause and regain control
Once the fight-or-flight response is triggered, there is no way to “think yourself” calm. Instead of focusing on your thoughts, focus on what you're feeling in your body. The following grounding exercise is a simple, quick way to put the brakes on impulsivity, calm down, and regain control. It can make a big difference in just a few short minutes.
Find a quiet spot and sit in a comfortable position.
Focus on what you're experiencing in your body. Feel the surface you're sitting on. Feel your feet on the floor. Feel your hands in your lap.
Concentrate on your breathing, taking slow, deep breaths. Breathe in slowly. Pause for a count of three. Then slowly breathe out, once more pausing for a count of three. Continue to do this for several minutes.
Breathe in slowly. Pause for a count of three. Then slowly breathe out, once more pausing for a count of three. Continue to do this for several minutes.
In case of emergency, distract yourself
If your attempts to calm down aren't working and you're starting to feel overwhelmed by destructive urges, distracting yourself may help. All you need is something to capture your focus long enough for the negative impulse to go away. Anything that draws your attention can work, but distraction is most effective when the activity is also soothing. In addition to the sensory-based strategies mentioned previously, here are some things you might try:
Watch TV. Choose something that's the opposite of what you're feeling: a comedy, if you're feeling sad, or something relaxing if you're angry or agitated.
Do something you enjoy that keeps you busy. This could be anything: gardening, painting, playing an instrument, knitting, reading a book, playing a computer game, or doing a Sudoku or word puzzle.
Throw yourself into work. You can also distract yourself with chores and errands: cleaning your house, doing yard work, going grocery shopping, grooming your pet, or doing the laundry.
Get active. Vigorous exercise is a healthy way to get your adrenaline pumping and let off steam. If you're feeling stressed, you may want to try more relaxing activities such as yoga or a walk around your neighborhood.
Call a friend. Talking to someone you trust can be a quick and highly effective way to distract yourself, feel better, and gain some perspective.
Tip 3: Improve your interpersonal skills
If you have borderline personality disorder, you've probably struggled with maintaining stable, satisfying relationships with lovers, co-workers, and friends. This is because you have trouble stepping back and seeing things from other people's perspective. You tend to misread the thoughts and feelings of others, misunderstand how others see you, and overlook how they're affected by your behavior. It's not that you don't care, but when it comes to other people, you have a big blind spot. Recognizing your interpersonal blind spot is the first step. When you stop blaming others, you can start taking steps to improve your relationships and your social skills.
It's not that you don't care, but when it comes to other people, you have a big blind spot. Recognizing your interpersonal blind spot is the first step. When you stop blaming others, you can start taking steps to improve your relationships and your social skills.
Check your assumptions
When you're derailed by stress and negativity, as people with BPD often are, it's easy to misread the intentions of others. If you're aware of this tendency, check your assumptions. Remember, you're not a mind reader! Instead of jumping to (usually negative) conclusions, consider alternative motivations. As an example, let's say that your partner was abrupt with you on the phone and now you're feeling insecure and afraid they've lost interest in you. Before you act on those feelings:
Stop to consider the different possibilities. Maybe your partner is under pressure at work. Maybe he's having a stressful day. Maybe he hasn't had his coffee yet. There are many alternative explanations for his behavior.
Ask the person to clarify their intentions. One of the simplest ways to check your assumptions is to ask the other person what they're thinking or feeling. Double check what they meant by their words or actions. Instead of asking in an accusatory manner, try a softer approach: “I could be wrong, but it feels like…” or “Maybe I'm being overly sensitive, but I get the sense that…“
Put a stop to projection
Do you have a tendency to take your negative feelings and project them on to other people? Do you lash out at others when you're feeling bad about yourself? Does feedback or constructive criticism feel like a personal attack? If so, you may have a problem with projection.
To fight projection, you'll need to learn to apply the brakes—just like you did to curb your impulsive behaviors. Tune in to your emotions and the physical sensations in your body. Take note of signs of stress, such as rapid heart rate, muscle tension, sweating, nausea, or light-headedness. When you're feeling this way, you're likely to go on the attack and say something you'll regret later. Pause and take a few slow deep breaths. Then ask yourself the following three questions:
- Am I upset with myself?
- Am I feeling ashamed or afraid?
- Am I worried about being abandoned?
If the answer is yes, take a conversation break. Tell the other person that you're feeling emotional and would like some time to think before discussing things further.
Take responsibility for your role
Finally, it's important to take responsibility for the role you play in your relationships. Ask yourself how your actions might contribute to problems. How do your words and behaviors make your loved ones feel? Are you falling into the trap of seeing the other person as either all good or all bad? As you make an effort to put yourself in other people's shoes, give them the benefit of the doubt, and reduce your defensiveness, you'll start to notice a difference in the quality of your relationships.
BPD treatment
If you think that you or a loved one may be suffering from BPD, it's best to seek professional help, ideally from someone with experience diagnosing and treating BPD.
The importance of finding the right therapist
The support and guidance of a qualified therapist can make a huge difference in BPD treatment and recovery. Therapy may serve as a safe space where you can start working through your relationship and trust issues and “try on” new coping techniques.
An experienced professional will be familiar with BPD therapies such as dialectical behavior therapy (DBT) and schema-focused therapy. But while these therapies have proven to be helpful, it's not always necessary to follow a specific treatment approach. Many experts believe that weekly therapy involving education about the disorder, family support, and social and emotional skills training can treat most BPD cases.
It's important to take the time to find a therapist you feel safe with—someone who seems to get you and makes you feel accepted and understood. Take your time finding the right person. But once you do, make a commitment to therapy. You may start out thinking that your therapist is going to be your savior, only to become disillusioned and feel like they have nothing to offer. Remember that these swings from idealization to demonization are a symptom of BPD. Try to stick it out with your therapist and allow the relationship to grow. And keep in mind that change, by its very nature, is uncomfortable. If you don't ever feel uncomfortable in therapy, you're probably not progressing.
Don't count on a medication cure
Although many people with BPD take medication, the fact is that there is very little research showing that it is helpful. What's more, in the U.S., the Food and Drug Administration (FDA) has not approved any medications for the treatment of BPD. This doesn't mean that medication is never helpful—especially if you suffer from co-occurring problems such as depression or anxiety—but it is not a cure for BPD itself.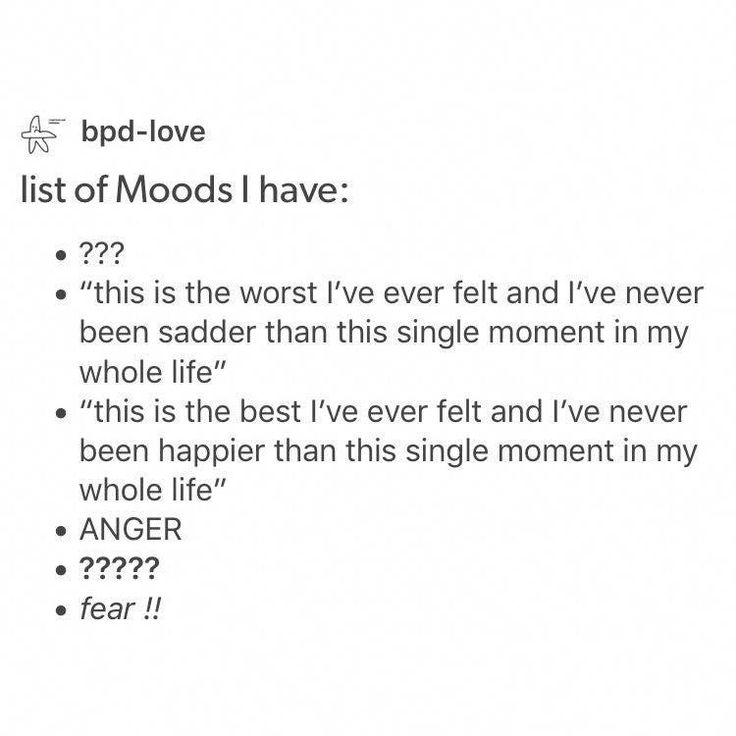
When it comes to BPD, therapy is much more effective. You just have to give it time. However, your doctor may consider medication if:
- You have been diagnosed with both BPD and depression or bipolar disorder.
- You suffer from panic attacks or severe anxiety.
- You begin hallucinating or having bizarre, paranoid thoughts.
- You are feeling suicidal or at risk of hurting yourself or others.
Authors: Melinda Smith, M.A. and Jeanne Segal, Ph.D.
- References
Personality Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425787.x18_Personality_Disorders
Choi-Kain, Lois W.
 , Ellen F. Finch, Sara R. Masland, James A. Jenkins, and Brandon T. Unruh. “What Works in the Treatment of Borderline Personality Disorder.” Current Behavioral Neuroscience Reports 4, no. 1 (March 1, 2017): 21–30. https://doi.org/10.1007/s40473-017-0103-z
, Ellen F. Finch, Sara R. Masland, James A. Jenkins, and Brandon T. Unruh. “What Works in the Treatment of Borderline Personality Disorder.” Current Behavioral Neuroscience Reports 4, no. 1 (March 1, 2017): 21–30. https://doi.org/10.1007/s40473-017-0103-zStoffers-Winterling, Jutta M., Birgit A. Völlm, Gerta Rücker, Antje Timmer, Nick Huband, and Klaus Lieb. “Psychological Therapies for People with Borderline Personality Disorder.” Cochrane Database of Systematic Reviews, no. 8 (2012). https://doi.org/10.1002/14651858.CD005652.pub2
Kulacaoglu, Filiz, and Samet Kose. “Borderline Personality Disorder (BPD): In the Midst of Vulnerability, Chaos, and Awe.” Brain Sciences 8, no. 11 (November 18, 2018): 201. https://doi.org/10.3390/brainsci8110201
Bozzatello, Paola, Silvio Bellino, Marco Bosia, and Paola Rocca. “Early Detection and Outcome in Borderline Personality Disorder.” Frontiers in Psychiatry 10 (2019): 710. https://doi.org/10.3389/fpsyt.
 2019.00710
2019.00710Ripoll, Luis H. “Psychopharmacologic Treatment of Borderline Personality Disorder.” Dialogues in Clinical Neuroscience 15, no. 2 (June 2013): 213–24. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3811092/
Angstman, Kurt, and Norman H. Rasmussen. “Personality Disorders: Review and Clinical Application in Daily Practice.” American Family Physician 84, no. 11 (December 1, 2011): 1253–60. https://www.aafp.org/afp/2011/1201/p1253.html
Borderline Personality Disorder – Overview of symptoms, causes, and treatment. (National Institute of Mental Health)
Borderline Personality Disorder (BPD) –Explains borderline personality disorder (BPD) including possible causes, how you can access treatment and support, and tips for helping yourself. (Mind)
What is Dialectical Behavior Therapy (DBT)? – A comprehensive article with ten short videos. (Behavioral Tech)
Helplines and support
In the U.S.: Call the NAMI HelpLine at 1-800-950-6264
UK: Call the the Mind infoline at 0300 123 3393
Australia: Call the Sane Helpline at 1800 187 263
Canada: Find Your CMHA for a helpline near you
India: Call the Vandrevala Foundation Helpline at 1860 2662 345 or 1800 2333 330
Last updated: December 15, 2022
Helping Someone with Borderline Personality Disorder
personality disorders
Have a loved one who's been diagnosed with BPD? While you can’t force them to seek treatment, you can take steps to improve communication, set healthy boundaries, and stabilize your relationship.
BPD and relationships
People with borderline personality disorder (BPD) tend to have major difficulties with relationships, especially with those closest to them. Their wild mood swings, angry outbursts, chronic abandonment fears, and impulsive and irrational behaviors can leave loved ones feeling helpless, abused, and off balance. Partners and family members of people with BPD often describe the relationship as an emotional roller coaster with no end in sight. You may feel like you're at the mercy of your loved one's BPD symptoms—trapped unless you leave the relationship or the person takes steps to get treatment. But you have more power than you think.
You can change the relationship by managing your own reactions, establishing firm limits, and improving communication between you and your loved one. There's no magic cure but with the right treatment and support, many people with BPD can and do get better and their relationships can become more stable and rewarding. In fact, patients with the most support and stability at home tend to show improvements sooner than those whose relationships are more chaotic and insecure.
In fact, patients with the most support and stability at home tend to show improvements sooner than those whose relationships are more chaotic and insecure.
Whether it's your partner, parent, child, sibling, friend, or other loved one with BPD, you can improve both the relationship and your own quality of life, even if the person with BPD isn't ready to acknowledge the problem or seek treatment.
Learning all you can
If your loved one has borderline personality disorder, it's important to recognize that he or she is suffering. The destructive and hurtful behaviors are a reaction to deep emotional pain. In other words, they're not about you. When your loved one does or says something hurtful towards you, understand that the behavior is motivated by the desire to stop the pain they are experiencing; it's rarely deliberate.
Learning about BPD won't automatically solve your relationship problems, but it will help you understand what you're dealing with and handle difficulties in more constructive ways.
With over 25,000 licensed counselors, BetterHelp has a therapist that fits your needs. It's easy, affordable, and convenient.
GET 20% OFF
Online-Therapy.com is a complete toolbox of support, when you need it, on your schedule. It only takes a few minutes to sign up.
GET 20% OFF
Teen Counseling is an online therapy service for teens and young adults. Connect with your counselor by video, phone, or chat.
GET 20% OFF
Recognizing the signs and symptoms of borderline personality disorder is not always easy. BPD is rarely diagnosed on its own, but often in conjunction with co-occurring disorders such as depression, bipolar disorder, anxiety, an eating disorder, or substance abuse. Your family member or loved one with BPD may be extremely sensitive, so small things can often trigger intense reactions.
Once upset, borderline people are often unable to think straight or calm themselves in a healthy way. They may say hurtful things or act out in dangerous or inappropriate ways.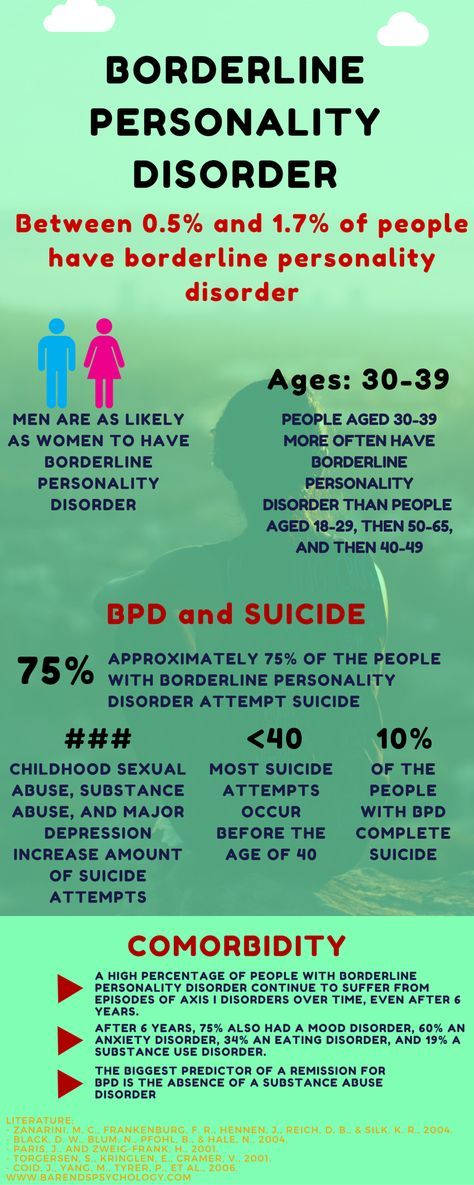 This emotional volatility can cause turmoil in their relationships and stress for family members, partners, and friends.
This emotional volatility can cause turmoil in their relationships and stress for family members, partners, and friends.
Many people in a close relationship with someone who suffers from BPD often know that there’s something wrong with their loved one, but have no idea what it is or if there is even a name for it. Learning a diagnosis of borderline personality disorder can come as a source of both relief and hope.
Does your loved one have borderline personality disorder?
In your relationship:
- Do you feel like you have to tiptoe around your loved one, watching every little thing you say or do for fear of setting them off? Do you often hide what you think or feel in order to avoid fights and hurt feelings?
- Does your loved one shift almost instantaneously between emotional extremes? For example, are they calm one moment, raging the next, then suddenly despondent? Are these rapid mood swings unpredictable and seemingly irrational?
- Does your loved one tend to view you as all good or bad, with no middle ground? For example, either you're “perfect,” and the only one they can count on, or you're “selfish” and “unfeeling” and never truly loved them.
- Do you feel like you can't win: that anything you say or do will be twisted and used against you? Does it feel as if your loved one's expectations are constantly changing, so you're never sure how to keep the peace?
- Is everything always your fault? Do you feel constantly criticized and blamed for things that don't even make sense? Does the person accuse you of doing and saying things you never did? Do you feel misunderstood whenever you try to explain or reassure your partner?
- Do you feel manipulated by fear, guilt, or outrageous behavior? Does your loved one make threats, fly into violent rages, make dramatic declarations, or do dangerous things when they think you're unhappy or may leave?
If you answer “yes” to most of these questions, your partner or family member might have borderline personality disorder.
[Read: Borderline Personality Disorder Test]
To help someone with BPD, first take care of yourself
When a family member or partner has borderline personality disorder, it's all too easy to get caught up in heroic efforts to please and appease him or her. You may find yourself putting most of your energy into the person with BPD at the expense of your own emotional needs. But this is a recipe for resentment, depression, burnout, and even physical illness.
You may find yourself putting most of your energy into the person with BPD at the expense of your own emotional needs. But this is a recipe for resentment, depression, burnout, and even physical illness.
You can't help someone else or enjoy sustainable, satisfying relationships when you're run down and overwhelmed by stress. As in the event of an in-flight emergency, you must “put on your own oxygen mask first.”
Avoid the temptation to isolate. Make it a priority to stay in touch with family and friends who make you feel good. You need the support of people who will listen to you, make you feel cared for, and offer reality checks when needed.
You're allowed (and encouraged) to have a life! Give yourself permission to have a life outside of your relationship with the person with BPD. It's not selfish to carve out time for yourself to relax and have fun. In fact, when you return to your BPD relationship, you'll both benefit from your improved perspective.
Join a support group for BPD family members. Meeting with others who understand what you're going through can go a long way. If you can't find an in-person support group in your area, you may want to consider joining an online BPD community.
Don't neglect your physical health. Eating healthfully, exercising, and getting quality sleep can easily fall by the wayside when you're caught up in relationship drama. Try to avoid this pitfall. When you're healthy and well rested, you're better able to handle stress and control your own emotions and behaviors.
Learn to manage stress. Getting anxious or upset in response to problem behavior will only increase your loved one's anger or agitation. By practicing with sensory input, you can learn to relieve stress as it's happening and stay calm and relaxed when the pressure builds.
Remember the 3 C's rule
Many friends or family members often feel guilty and blame themselves for the destructive behavior of the borderline person. You may question what you did to make the person so angry, think you somehow deserve the abuse, or feel responsible for any failure or relapse in treatment.
You may question what you did to make the person so angry, think you somehow deserve the abuse, or feel responsible for any failure or relapse in treatment.
But it's important to remember that you're not responsible for another person. The person with BPD is responsible for their own actions and behaviors.
The 3 C's are:
- I didn't cause it.
- I can't cure it.
- I can't control it.
Source: Out of the Fog
Communicating with someone who has BPD
Communication is a key part of any relationship but communicating with a borderline person can be especially challenging. People in a close relationship with a borderline adult often liken talking with their loved one to arguing with a small child. People with BPD have trouble reading body language or understanding the nonverbal content of a conversation. They may say things that are cruel, unfair, or irrational. Their fear of abandonment can cause them to overreact to any perceived slight, no matter how small, and their aggression can result in impulsive fits of rage, verbal abuse, or even violence.
The problem for people with BPD is that the disorder distorts both the messages they hear and those they try to express. BPD expert and author, Randi Kreger, likens it to “having ‘aural dyslexia,' in which they hear words and sentences backwards, inside out, sideways, and devoid of context.”
Listening to your loved one and acknowledging their feelings is one of the best ways to help someone with BPD calm down. When you appreciate how a borderline person hears you and adjust how you communicate with them, you can help diffuse the attacks and rages and build a stronger, closer relationship.
Communication tips
It's important to recognize when it's safe to start a conversation. If your loved one is raging, verbally abusive, or making physical threats, now is not the time to talk. Better to calmly postpone the conversation by saying something like, “Let's talk later when we're both calm. I want to give you my full attention but that's too hard for me to do right now. ”
”
When things are calmer:
Listen actively and be sympathetic. Avoid distractions such as the TV, computer, or cell phone. Try not to interrupt or redirect the conversation to your concerns. Set aside your judgment, withhold blame and criticism, and show your interest in what's being said by nodding occasionally or making small verbal comments like “yes” or “uh huh.” You don't have to agree with what the person is saying to make it clear that you're listening and sympathetic.
Focus on the emotions, not the words. The feelings of the person with BPD communicate much more than what the words he or she is using. People with BPD need validation and acknowledgement of the pain they're struggling with. Listen to the emotion your loved one is trying to communicate without getting bogged down in attempting to reconcile the words being used.
Try to make the person with BPD feel heard. Don't point out how you feel that they're wrong, try to win the argument, or invalidate their feelings, even when what they're saying is totally irrational.
Do your best to stay calm, even when the person with BPD is acting out. Avoid getting defensive in the face of accusations and criticisms, no matter how unfair you feel they are. Defending yourself will only make your loved one angrier. Walk away if you need to give yourself time and space to cool down.
Seek to distract your loved one when emotions rise. Anything that draws your loved one's attention can work, but distraction is most effective when the activity is also soothing. Try exercising, sipping hot tea, listening to music, grooming a pet, painting, gardening, or completing household chores.
Talk about things other than the disorder. You and your loved one's lives aren't solely defined by the disorder, so make the time to explore and discuss other interests. Discussions about light subjects can help to diffuse the conflict between you and may encourage your loved one to discover new interests or resume old hobbies.
Don't ignore self-destructive behaviors and suicidal threats
If you believe your loved one is at an immediate risk for suicide Do NOT leave the person alone. Call your loved one's therapist or:
- In the U.S., dial 911 or call the National Suicide Prevention Lifeline at 1-800-273-TALK.
- In other countries, call your country's emergency services number or visit IASP to find a suicide prevention helpline.
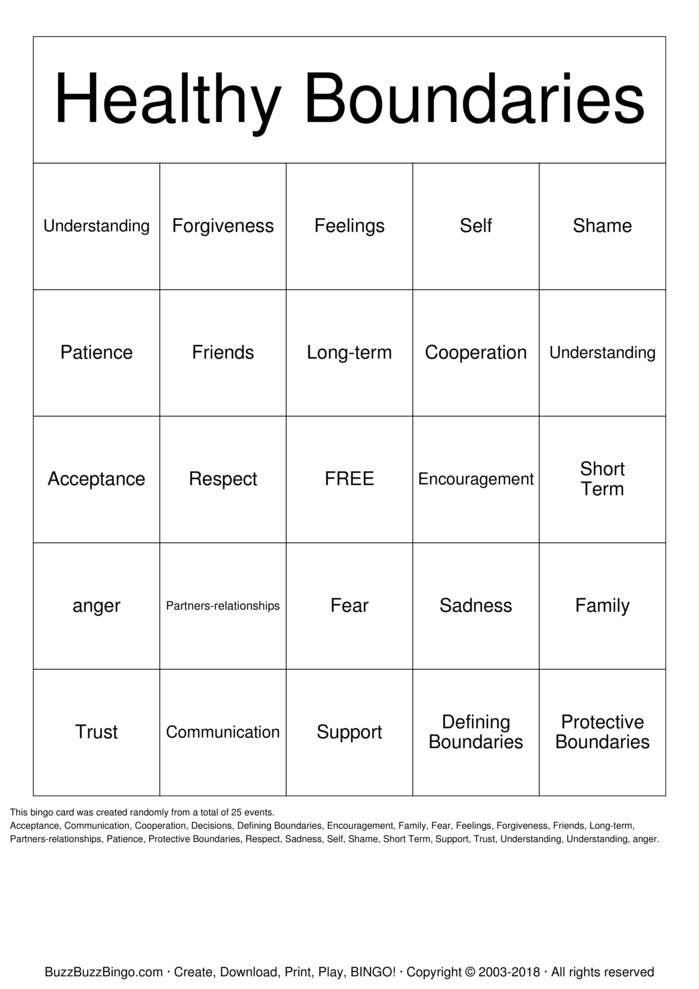
Setting healthy boundaries with a borderline loved one
One of the most effective ways to help a loved one with BPD gain control over their behavior is to set and enforce healthy limits or boundaries. Setting limits can help your loved one better handle the demands of the outside world, where schools, work, and the legal system, for example, all set and enforce strict limits on what constitutes acceptable behavior.
Establishing boundaries in your relationship can replace the chaos and instability of your current situation with an important sense of structure and provide you with more choices about how to react when confronted by negative behavior. When both parties honor the boundaries, you'll be able to build a sense of trust and respect between you, which are key ingredients for any meaningful relationship.
When both parties honor the boundaries, you'll be able to build a sense of trust and respect between you, which are key ingredients for any meaningful relationship.
Setting boundaries is not a magic fix for a relationship, though. In fact, things may initially get worse before they get better. The person with BPD fears rejection and is sensitive to any perceived slight. This means that if you've never set boundaries in your relationship before, your loved one is likely to react badly when you start. If you back down in the face of your loved one's rage or abuse, you'll only be reinforcing their negative behavior and the cycle will continue. But, remaining firm and standing by your decisions can be empowering to you, benefit your loved one, and ultimately transform your relationship.
How to set and reinforce healthy boundaries
Talk to your loved one about boundaries at a time when you're both calm, not in the heat of an argument. Decide what behavior you will and will not tolerate from the person and make those expectations clear. For example, you may tell your loved one, “If you can't talk to me without screaming abuse at me, I will walk out.”
For example, you may tell your loved one, “If you can't talk to me without screaming abuse at me, I will walk out.”
Do…
- Calmly reassure the person with BPD when setting limits. Say something like, “I love you and I want our relationship to work, but I can't handle the stress caused by your behavior. I need you to make this change for me.”
- Make sure everyone in the family agrees on the boundaries—and how to enforce the consequences if they're ignored.
- Think of setting boundaries as a process rather than a single event. Instead of hitting your loved one with a long list of boundaries all at once, introduce them gradually, one or two at a time.
Don't…
- Make threats and ultimatums that you can't carry out. As is human nature, your loved one will inevitably test the limits you set. If you relent and don't enforce the consequences, your loved one will know the boundary is meaningless and the negative behavior will continue.
 Ultimatums are a last resort (and again, you must be prepared to follow through).
Ultimatums are a last resort (and again, you must be prepared to follow through). - Tolerate abusive behavior. No one should have to put up with verbal abuse or physical violence. Just because your loved one's behavior is the result of a personality disorder, it doesn't make the behavior any less real or any less damaging to you or other family members.
- Enable the person with BPD by protecting them from the consequences of their actions. If your loved one won't respect your boundaries and continues to make you feel unsafe, then you may need to leave. It doesn't mean you don't love them, but your self-care should always take priority.
Supporting your loved one's BPD treatment
Borderline personality disorder is highly treatable, yet it's common for people with BPD to avoid treatment or deny that they have a problem. Even if this is the case with your loved one, you can still offer support, improve communication, and set boundaries while continuing to encourage your friend or family member to seek professional help.
While medication options are limited, the guidance of a qualified therapist can make a huge difference to your loved one's recovery. BPD therapies, such as Dialectical Behavior Therapy (DBT) and schema-focused therapy, can help your loved one work through their relationship and trust issues and explore new coping techniques. In therapy, they can learn how to calm the emotional storm and self-soothe in healthy ways.
How to support treatment
If your loved one won't acknowledge that they have a problem with BPD, you may want to consider couple's therapy. Here, the focus is on the relationship and promoting better communication, rather than on your loved one's disorder. Your partner may more readily agree to this and eventually consider pursuing BPD therapy in the future.
Encourage your loved one to explore healthy ways of handling stress and emotions by practicing mindfulness and employing relaxation techniques such as yoga, deep breathing, or meditation. Sensory-based stimulation can also help them to relieve stress in the moment. Again, you can participate in any of these therapies with your loved one, which can strengthen your bond and may encourage them to pursue other avenues of treatment as well.
Again, you can participate in any of these therapies with your loved one, which can strengthen your bond and may encourage them to pursue other avenues of treatment as well.
By developing an ability to tolerate distress, your loved one can learn how to press pause when the urge to act out or behave impulsively strikes. HelpGuide's free Emotional Intelligence Toolkit offers a step-by-step, self-guided program to teach your loved one how to ride the “wild horse” of overwhelming feelings while staying calm and focused.
Setting goals for BPD recovery: Go slowly
When supporting your loved one's recovery, it's important to be patient and set realistic goals. Change can and does happen but, as with reversing any kind of behavior pattern, it takes time.
- Take baby steps rather than aiming for huge, unattainable goals that set you and your loved one up for failure and discouragement. By lowering expectations and setting small goals to be achieved step by step, you and your loved one have a greater chance of success.

- Supporting your loved one's recovery can be both extremely challenging and rewarding. You need to take care of yourself, but the process can help you grow as an individual and strengthen the relationship between you.
Authors: Melinda Smith, M.A, Lawrence Robinson, and Jeanne Segal, Ph.D.
- References
Personality Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425787.x18_Personality_Disorders
Choi-Kain, Lois W., Ellen F. Finch, Sara R. Masland, James A. Jenkins, and Brandon T. Unruh. “What Works in the Treatment of Borderline Personality Disorder.” Current Behavioral Neuroscience Reports 4, no.
 1 (March 1, 2017): 21–30. https://doi.org/10.1007/s40473-017-0103-z
1 (March 1, 2017): 21–30. https://doi.org/10.1007/s40473-017-0103-zStoffers-Winterling, Jutta M., Birgit A. Völlm, Gerta Rücker, Antje Timmer, Nick Huband, and Klaus Lieb. “Psychological Therapies for People with Borderline Personality Disorder.” Cochrane Database of Systematic Reviews, no. 8 (2012). https://doi.org/10.1002/14651858.CD005652.pub2
Kulacaoglu, Filiz, and Samet Kose. “Borderline Personality Disorder (BPD): In the Midst of Vulnerability, Chaos, and Awe.” Brain Sciences 8, no. 11 (November 18, 2018): 201. https://doi.org/10.3390/brainsci8110201
Bozzatello, Paola, Silvio Bellino, Marco Bosia, and Paola Rocca. “Early Detection and Outcome in Borderline Personality Disorder.” Frontiers in Psychiatry 10 (2019): 710. https://doi.org/10.3389/fpsyt.2019.00710
Ripoll, Luis H. “Psychopharmacologic Treatment of Borderline Personality Disorder.” Dialogues in Clinical Neuroscience 15, no. 2 (June 2013): 213–24. https://www.ncbi.
 nlm.nih.gov/pmc/articles/PMC3811092/
nlm.nih.gov/pmc/articles/PMC3811092/Ng, Fiona Y. Y., Marianne E. Bourke, and Brin F. S. Grenyer. “Recovery from Borderline Personality Disorder: A Systematic Review of the Perspectives of Consumers, Clinicians, Family and Carers.” PLOS ONE 11, no. 8 (August 9, 2016): e0160515. https://doi.org/10.1371/journal.pone.0160515
Sutherland, Ruth, John Baker, and Sharon Prince. “Support, Interventions and Outcomes for Families/Carers of People with Borderline Personality Disorder: A Systematic Review.” Personality and Mental Health 14, no. 2 (2020): 199–214. https://doi.org/10.1002/pmh.1473
Angstman, Kurt, and Norman H. Rasmussen. “Personality Disorders: Review and Clinical Application in Daily Practice.” American Family Physician 84, no. 11 (December 1, 2011): 1253–60. https://www.aafp.org/afp/2011/1201/p1253.html
Borderline Personality Disorder – Overview of symptoms, causes, and treatment. (National Institute of Mental Health)
Borderline Personality Disorder (BPD) –Explains borderline personality disorder (BPD) including possible causes, how you can access treatment and support, and tips for helping yourself. (Mind)
(Mind)
What is Dialectical Behavior Therapy (DBT)? – A comprehensive article with ten shot videos. (Behavioral Tech)
Helplines and support
In the U.S.: Call the NAMI HelpLine at 1-800-950-6264
UK: Call the the Mind infoline at 0300 123 3393
Australia: Call the Sane Helpline at 1800 187 263
Canada: Find Your CMHA for a helpline near you
India: Call the Vandrevala Foundation Helpline at 1860 2662 345 or 1800 2333 330
Last updated: December 15, 2022
Borderline Personality Disorder Symptom Test
Borderline Personality Disorder includes many different symptoms that in one way or another indicate the presence of this mental disorder. However, the severity of the disease and its symptoms can vary greatly.
This test incorporates the results of previous studies to ensure the validity and reliability of results for borderline personality disorder symptoms.
Do you have symptoms of borderline disorder? For each following statement, indicate how much you agree with it.
The Borderline Personality Disorder Test (IDR-BPDST) is owned by IDRlabs. It builds on the work of Dr. M. Zanarini and her colleagues who created the Mental Disorder Symptom Inventory (MSI-BPD). This test is not affiliated with any particular researcher or organization in the field of psychopathology.
The Borderline Personality Disorder Test is based on material that has been published in the following sources: Zanarini, Mary & Vujanovic, A & Parachini, Elizabeth & Villatte, Jennifer & Frankenburg, Frances & Hennen, John. (2003). A screening measure for BPD: The McLean screening instrument for Borderline Personality Disorder (MSI-BPD). Journal of personality disorders. 17.568-73. 10.1521/pedi.17.6.568.25355. Keng SL, Lee Y, Drabu S, Hong RY, Chee CYI, Ho CSH, Ho RCM. Construct Validity of the McLean Screening Instrument for Borderline Personality Disorder in Two Singaporean Samples. J Pers Discord. 2019Aug; 33(4): 450-469. Epub 2018 Jun 27 PMID: 29949444. Kröger C, Huget F, Roepke S. Diagnostische Effizienz des McLean Screening Instrument für Borderline-Persönlichkeitsstörung in einer Stichprobe, die eine stationäre, störungsspezifische Behandlung in Anspruch nehmen möchte [Diagnostic Instrument for Diagnostic accuracy of the McLean borderline personality disorder in an inpatient sample who seek a disorder-specific treatment]. Psychother Psychosom Med Psychol. Nov 2011; 61(11):481-6. German. Epub 2011 Nov 11 PMID: 22081467.
J Pers Discord. 2019Aug; 33(4): 450-469. Epub 2018 Jun 27 PMID: 29949444. Kröger C, Huget F, Roepke S. Diagnostische Effizienz des McLean Screening Instrument für Borderline-Persönlichkeitsstörung in einer Stichprobe, die eine stationäre, störungsspezifische Behandlung in Anspruch nehmen möchte [Diagnostic Instrument for Diagnostic accuracy of the McLean borderline personality disorder in an inpatient sample who seek a disorder-specific treatment]. Psychother Psychosom Med Psychol. Nov 2011; 61(11):481-6. German. Epub 2011 Nov 11 PMID: 22081467.
The work of Dr. Zanarini and her colleagues looks at the main symptoms that are characteristic of borderline personality disorder. This paper also describes certain diagnostic criteria that have been used in the studies. This test provides information for educational purposes only. IDRlabs and this test are in no way affiliated with the above researchers, organizations or institutions.
The borderline personality disorder symptom test relies on known research on the condition and other psychiatric disorders. However, all free online tests like this one are only introductory materials that will not be able to determine your inherent qualities with absolute accuracy and reliability. Therefore, our test provides information for educational purposes only. Detailed information about your mental state can only be provided by a certified specialist.
However, all free online tests like this one are only introductory materials that will not be able to determine your inherent qualities with absolute accuracy and reliability. Therefore, our test provides information for educational purposes only. Detailed information about your mental state can only be provided by a certified specialist.
As the authors of this free online borderline personality disorder symptom ratio test, we have made every effort to ensure that this test is reliable and valid through numerous tests and statistical data controls. However, free online tests like this provide information "as is" and should not be construed as providing professional or certified advice of any kind. For more information about our online tests, please see our Terms of Service.
Borderline personality disorder: symptoms, treatment, communication tips
- What is it
- Test
- Symptoms
- Causes and risk factors
- Is it being treated
- How to communicate with a person with BPD
- Expert commentary
What is borderline personality disorder
Borderline personality disorder (BPD) inevitably affects how a person thinks and feels, how he interacts with others [1]. The diagnosis is recorded in the ICD-10 and is considered a subspecies of an emotionally unstable personality disorder. The disorder manifests itself in problems with self-esteem, the management of emotions and behavior, high anxiety and desocialization, and leads to unstable relationships with others. With borderline personality disorder, a person experiences a fear of being alone or abandoned. Misplaced anger, impulsiveness, frequent mood swings can alienate potential partners.
The diagnosis is recorded in the ICD-10 and is considered a subspecies of an emotionally unstable personality disorder. The disorder manifests itself in problems with self-esteem, the management of emotions and behavior, high anxiety and desocialization, and leads to unstable relationships with others. With borderline personality disorder, a person experiences a fear of being alone or abandoned. Misplaced anger, impulsiveness, frequent mood swings can alienate potential partners.
Advertising on RBC www.adv.rbc.ru
Deviations are usually recorded in young people and may worsen with age. However, many patients diagnosed with BPD are able to live a full life, having worked through the main problems.
Borderline Personality Disorder Test
Some of the symptoms may point directly to BPD, but only the attending physician will give exact information. If you suspect you have a disorder, answer a few questions:
- Do you have a fear of being alone that makes you act inappropriately? For example, constantly call a partner, try to be always near him.

- Have you ever had to change your mind towards your partner, move from love to hate for no particular reason?
- Have you ever felt that you do not have a clear idea of yourself, that you are not sure of your self-worth?
- Have you committed impulsive dangerous acts? For example, have you taken drugs, spent large sums of money recklessly, or had unprotected sex?
- Have you harmed yourself, threatened suicide in the presence of loved ones?
- Do you experience severe mood swings, from anxiety and irritability to days of depression and apathy?
- Do you find it difficult to control your anger?
- When you find yourself in a stressful situation, do you feel as if you are disconnected from reality and your own body, do not control your thoughts and behavior?
If you answered "yes" to more questions, it makes sense to talk to a psychotherapist. Symptoms do not always point to borderline personality disorder and may be due to other health problems. Only a specialist can make a correct diagnosis and give competent advice.
Only a specialist can make a correct diagnosis and give competent advice.
© Yuris Alhumaydy/Unsplash
Symptoms of borderline personality disorder
BPD affects how a person relates to himself and others, how he behaves in society. Signs and symptoms vary, there may be several, or just a couple from the list [2]:
- Strong fear of being abandoned. A person is ready to go to extreme measures to avoid the real or imagined withdrawal or rejection of a partner.
- Tendency to unstable relationships. For example, a person idealizes a partner, but at some point suddenly decides that the latter is cruel and unfair.
- Rapid changes in self-identification and self-esteem. Goals and values switch disproportionately to the circumstances - abruptly and for no particular reason. A person tends to consider himself bad, he needs impulses from the outside in order to feel alive and needed.
- Stress related paranoia. Loss of contact with reality lasting from several minutes to several hours.

- Impulsive behavior, propensity to take risks. Gambling, reckless driving, unsafe sex, alcohol abuse, overeating, drugs.
- Success sabotage. Sudden unreasonable rejection of positive relationships, good work.
- Self-mutilation, suicidal tendencies. Often occur in response to separation anxiety or partner rejection.
- Sudden mood swings lasting from several hours to several days. Bright, hypertrophied emotions: happiness, anxiety, shame and irritability.
- Constantly accompanying feeling of emptiness, lack of interest in what is happening.
- Aggression - strong anger, cruel sarcastic remarks to interlocutors, fights.
Causes and risk factors
As with other mental health problems, the causes of borderline personality disorder are not fully understood. In addition to circumstances such as childhood abuse or neglect, borderline personality disorder may be associated with the following factors.
- Genetics.
 Studies involving twins and their relatives suggest that BPD may be inherited and be part of a mental health complex [3].
Studies involving twins and their relatives suggest that BPD may be inherited and be part of a mental health complex [3]. - Anomalies of the brain. Several studies have confirmed changes in certain parts of the brain involved in the regulation of emotions, especially impulsivity and aggression [4]. Patients with BPD may have malfunctions in the regulation of chemicals, such as the production of serotonin, which affects mood.
Is there a cure for borderline personality disorder
BPD is difficult to treat. But with the help of modern, evidence-based therapies, people with the disorder can be helped to manage their symptoms and improve their quality of life. It is good if the treatment is carried out by a licensed doctor who specializes in this disease. Sometimes the patient will need to interact not only with a psychiatrist, but also with a social worker who will help to adapt in the absence of loved ones.
The doctor usually conducts an interview and discusses the person's symptoms. Then there is a thorough medical examination and testing, which allows you to exclude other diseases. Comorbid disorders can make BPD difficult to diagnose and treat, especially if their symptoms overlap. For example, a person may show signs of depression, bipolar disorder, anxiety, substance use problems, or eating disorders. If a patient with borderline personality disorder does not receive proper treatment, they are more likely to develop chronic illnesses. And not only mentally, but also physically - patients with BPD tend to make choices in favor of an unhealthy lifestyle and self-harm.
Then there is a thorough medical examination and testing, which allows you to exclude other diseases. Comorbid disorders can make BPD difficult to diagnose and treat, especially if their symptoms overlap. For example, a person may show signs of depression, bipolar disorder, anxiety, substance use problems, or eating disorders. If a patient with borderline personality disorder does not receive proper treatment, they are more likely to develop chronic illnesses. And not only mentally, but also physically - patients with BPD tend to make choices in favor of an unhealthy lifestyle and self-harm.
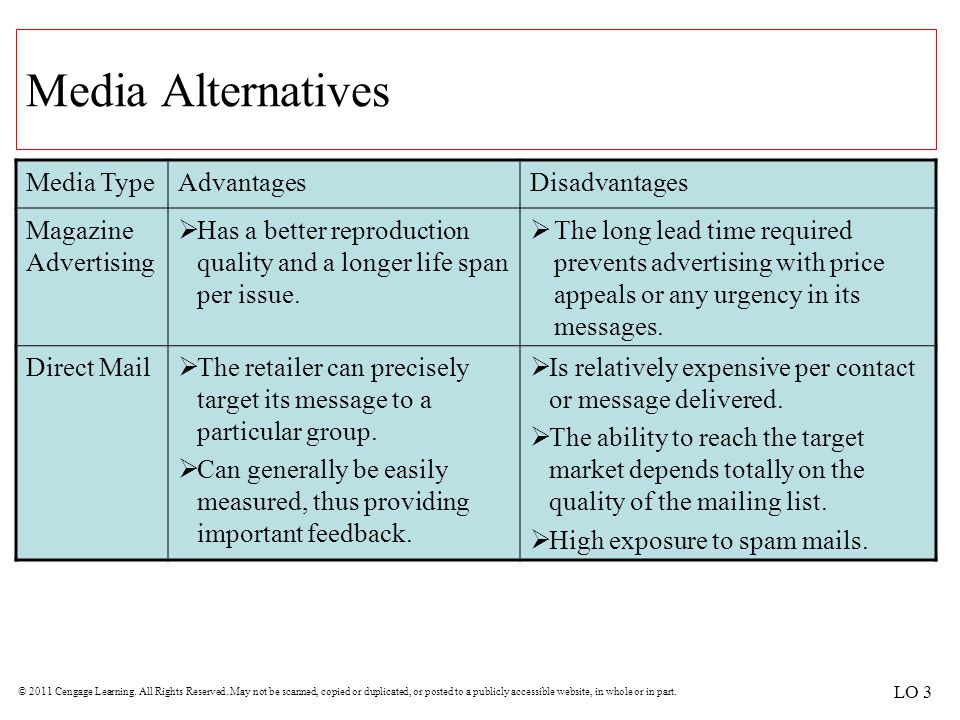
Psychotherapy is the first line of treatment for a person with BPD. It can take place both individually and in a group. The second option helps the patient to interact with other people and express himself in society. Most often, the doctor uses one of two therapy options, or combines them:
- Dialectical Behavioral Therapy (DBT). It uses the concepts of awareness and acceptance of the current situation and emotional state.
 DBT also teaches skills to control and reduce self-destructive behavior.
DBT also teaches skills to control and reduce self-destructive behavior. - Cognitive behavioral therapy (CBT). This type of assistance allows you to identify and change the core beliefs that underlie inaccurate acceptance of yourself and others, as well as problems associated with communication.
Because their benefits are unclear, medications are not commonly used as the primary treatment for borderline personality disorder. However, in some cases, a psychiatrist may recommend medications to treat certain symptoms, such as controlling mood swings and depression. The psychotherapist should specialize in borderline personality disorder, that is, receive additional education in this area.
How to communicate with a person with BPD
People with BPD are often very suspicious and vulnerable. They need support, and it is important for them to realize that they have someone to turn to in case of exacerbations. Eliza Gordezki, a writer, artist and queer feminist with BPD, has developed a manual for interacting with people who have been diagnosed with BPD [5]. Here are the main recommendations.
Here are the main recommendations.
Tell loved ones that you will take care of them
People with BPD tend to think that if they don't hear this confirmation, then others around them are indifferent. Suitable phrases:
- "Just writing to you to tell you I care about you."
- "I wanted you to know that I'm thinking of you right now."
- "I love having you in my life and I wanted to make sure you knew that."
Take an interest in well-being and affairs
For people with BPD, this is a vicious circle: they are afraid of being rejected, so they do not share their experiences in order to eliminate the risks of negative reactions from others. Asking how you are doing is a good strategy for making contact.
- “Hi, how are you?”
- “I saw you posted a sad post on Facebook. I wanted to make sure you were okay."
Soften bad news with support and sympathy
When you tell your loved one some unpleasant information, try to remind him that he is important to you and that you will support him in any case. A person with BPD needs to be aware that his feelings are taken into account and not perceived as something feigned.
A person with BPD needs to be aware that his feelings are taken into account and not perceived as something feigned.
- "It's not easy for me to support you in this crisis, but I need to know what to do to make it easier for you to deal with it."
Match words
Marsha Linehan, who developed the Dialectical Behavior Model (one of the most common treatments for people with BPD), uses specific vocabulary in her manuals [6]. Rather than characterize a person or their actions with judgmental words, she prefers adjectives such as "efficient, skillful, and wise" (or the reverse, "inefficient, inept, and unwise"). These words separate a person from his behavior, they name qualities that can be changed. If someone is being violent, negative, or insulting, you can say something like:
- “I can see you're upset. I understand why you are upset, but these actions are very inefficient and will not bring you the desired results. Let's think together how we can achieve greater sense and achieve the desired prospects.

Compare this phrase with those that many are used to using in similar situations: “It's not normal if you react like that!”, “It's impossible to communicate with you, there is too much drama”, “Why are you overreacting? You are always so sensitive!”
© Pavel Danilyuk/Pexels
Be attentive to triggers
The only way to determine what is bothering a loved one is to ask and observe. Among people with BPD, two triggers are common (eng. trigger - a reason, a trigger; in psychology - an irritant that causes a certain reaction) - to be thrown and to be rejected. Simple situations that most people are used to can cause a strong negative reaction with borderline personality disorder. For example, if you reschedule a meeting or began to devote more time to other things, did not respond to a message for a long time, or forgot to call. Of course, changing plans is normal, but when communicating with a person with BPD, it is worth taking a little time to explain your actions to him:
- “I remember that we planned to meet on Friday and have dinner together, and I'm sorry, but I have to cancel this meeting.
 I was assigned to make an urgent report, and I will be at work all evening. It will be great if, along with the cancellation of plans, you offer a quick alternative: “But I really want to spend time with you! Maybe we can meet on Saturday for lunch?
I was assigned to make an urgent report, and I will be at work all evening. It will be great if, along with the cancellation of plans, you offer a quick alternative: “But I really want to spend time with you! Maybe we can meet on Saturday for lunch?
Repeat and confirm
People with BPD need to be reminded of your positive attitude. Frequent reinforcement and support is an important part of their well-being and confidence in the world. Be patient and focus on good moments, convince your loved one if he breaks into negative emotions, even if it seems to you that they are unreasonable. For example, your friend is upset that they don't reply to a message. At this point, he may seriously believe that the interlocutor hates him. Inform that this is not the case, most likely, the person is just busy, he will definitely write or call as soon as he has time.
What works well for one person may not work for another, so it's always best to talk to your loved ones and ask what they need.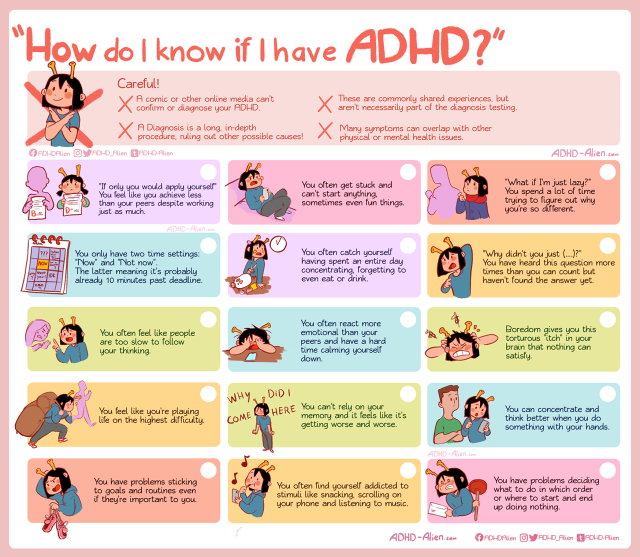
Expert comment
Andrey Yudin, psychologist, Gestalt therapist, co-founder of Stemning Gestalt Center
It is not always possible to build relationships with a person with BPD [7]. But if it's not a destructive abusive relationship and it's important for you to keep the relationship going, you need to put in a lot of effort. First of all, set boundaries - when you can come or call, whether you can shout. Sometimes it can take years to rebuild, especially when it comes to older relatives. It will take a lot of labor and therapeutic support.
Borderline personality disorder is one of the three basic personality disorders in modern psychotherapy, the other two being schizoid and narcissistic. BPD is the most well studied and isolated, it is in the public eye due to its clinical manifestations. The disorder is included in the ICD-10, but the difficulty lies in the lack of uniform criteria for the diagnosis. There are three obvious signs of borderline personality disorder:
- The person does not take care of himself.
 For example, he does not visit doctors, while experiencing guilt and shame for his choice. This factor applies to both hygiene and personal relationships.
For example, he does not visit doctors, while experiencing guilt and shame for his choice. This factor applies to both hygiene and personal relationships. - Approach speed. People with BPD tend to quickly make contacts and just as quickly become disillusioned with new acquaintances, friends, and romantic relationships.
- Extreme fear of rejection. If a person is afraid of being abandoned, being rejected by relatives, friends or partners, then this is a clear sign of BPD.
With BPD, there is a clear lack of self-activation - urging oneself to some kind of action. At the same time, it is difficult for a person to explain to himself why he cannot do this. Trying to rouse himself to action, he begins to worry. Borderline personality disorder begins in childhood, between 16 and 24 months. It is often the result of severe abuse, physical, emotional or sexual abuse, or a parent's negative response to a child's need for emotional closeness. In the case of premature separation, a mental structure is formed from two separate parts, which normally should be integrated into each other, but in BPD these are two separate modules.
BPD is often associated with drug addiction. Suffering, feelings of frustration, dissatisfaction encourage a person to chemically regulate his emotional state. This is alcohol, and drugs, and self-damaging behavior, and not only in relation to the body. For example, a person can spend all the money on payday.
With regard to BPD during adolescence, for this stage of human development, many of the "symptoms" are actually normal behavior. Severe emotional experiences, dulling the sense of self-preservation, experiments with substances and partners. But from the age of 16-18, when the transitional stage has been passed, the persistence of these signs may be a reason to contact a specialist.
Those close to people with BPD face, first of all, their emotional instability. The biggest difficulty is the chaotic influence on the lives of others. If a person with a narcissistic disorder extends his suspiciousness to the assessments of others, then with BPD people tend to have a different focus - love / not love, rejection / acceptance. A person may try to return the location of the partner or play ahead of the curve - break off the relationship, if he assumes that he may be abandoned. People with BPD may become abusers because of the unbearable emotional experiences they are trying to change in this way.
A person may try to return the location of the partner or play ahead of the curve - break off the relationship, if he assumes that he may be abandoned. People with BPD may become abusers because of the unbearable emotional experiences they are trying to change in this way.
In the professional field, BPD can be suspected, for example, in rock stars. Moreover, the presence of such a feature for people in this profession will even be a plus. There will be a lot of life and pain in their work, it is very sincere and can be healing for other people.
If you encounter a person with BPD at work—a boss, a colleague, a subordinate—they are likely to have fairly loose boundaries because they find it difficult to set and maintain them. This may be a person who perfidiously treats other people's borders or, conversely, distances himself and avoids communication. People with BPD are very successful. Such bosses have reactive behavior, chaos in the department, and many will be uncomfortable. But there are qualities in BPD that are good for management: empathy, intuition, even being aggressive can be an asset for career advancement.
But there are qualities in BPD that are good for management: empathy, intuition, even being aggressive can be an asset for career advancement.
The diagnosis and treatment of borderline personality disorder requires a specific set of skills that are not taught in psychology departments, at least not in basic education programs. Most psychologists do not have such qualifications; a maximum of 10% of practicing specialists have it. Therefore, educational work is especially important so that people can find the understanding and support that are so needed. The peculiarity of therapy for BPD will be directed to the very two modules of consciousness (patterns) of the patient. A person with BPD may go to the doctor from their positive childhood pattern and talk about how well the treatment is working. He does this because he is used to being held in relationships in this way, he has learned that he must give positive emotional nourishment "so as not to be abandoned." The therapist must frustrate this pattern, help to go beyond it.