Going back on antidepressants
Why Aren’t My Antidepressants Working?
Reviewed By:
If you feel like your antidepressant has stopped working, you're not alone. It's common for a medication that once worked wonders to become ineffective, especially if you've been taking it for a long time. Symptoms return for up to 33% of people using antidepressants — it's called breakthrough depression.
"Usually an antidepressant that's worked for a patient will keep working," says Paul Nestadt, M.D., psychiatrist and co-director of the Jack and Mary McGlasson Anxiety Disorders Clinic at Johns Hopkins. "But sometimes, a new episode of depression might come up that's not as responsive to that medication, or the medication might just stop working altogether."
What causes depression medications to stop working?
Multiple factors can change the way your body responds to an antidepressant, including:
- Drug or alcohol use. Illicit drug use and alcohol can cause strong mood changes, which can make antidepressants ineffective.
- Pregnancy. Your body's weight and blood volume increase when you're pregnant. Talk to your doctor about taking antidepressants while pregnant, and about potentially adjusting your dosage to continue relieving symptoms.
- New stressors. A new stressful situation at home or work can result in a mood response for which the antidepressant can't compensate.
- Other medications. Interactions between antidepressants and medications for other health conditions can affect how well an antidepressant works.
Most often, though, antidepressants stop working for what seems to be no reason. "There's no good research that shows why a medication may stop working for someone," says Nestadt. "I think it's less an issue of building up tolerance and more likely constantly changing stressors and factors in the brain."
When to See a Doctor
If your depression symptoms return for more than a few days, it's time to see your doctor.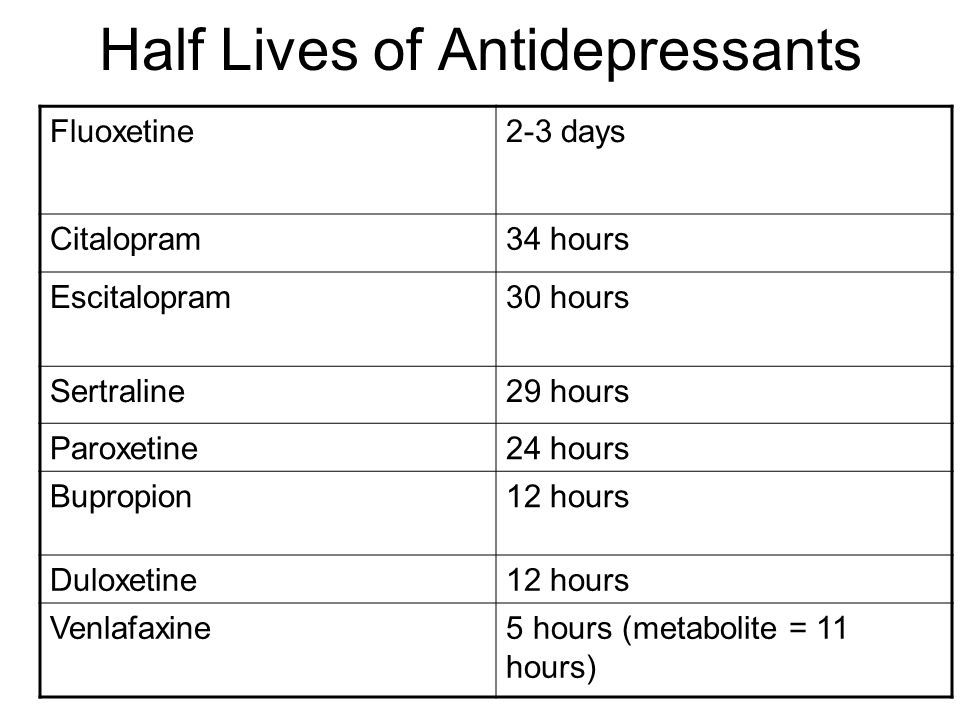 But even if you feel like your antidepressant isn't working, it's important to keep taking it until your doctor advises otherwise. You may need a dosage increase or a slow tapering off process. With many antidepressant medications, stopping their use too quickly can cause withdrawal effects such as:
But even if you feel like your antidepressant isn't working, it's important to keep taking it until your doctor advises otherwise. You may need a dosage increase or a slow tapering off process. With many antidepressant medications, stopping their use too quickly can cause withdrawal effects such as:
- Headaches
- Nausea
- Diarrhea or constipation
- Greater anxiety
- Suicidal thoughts
Early warning signs of breakthrough depression are the symptoms you typically experience when an episode of depression is coming on, says Nestadt. Depression symptoms vary from person to person, but signs include:
- Low mood
- Changes in sleep or appetite
- Decreased socializing
- Loss of interest in previously enjoyable activities
If your symptoms return, don't worry — adjusting the dose or switching to another antidepressant often solves the problem. (Note: If you have self-harm or suicidal thoughts, see your doctor immediately, call 911 or go to an emergency room.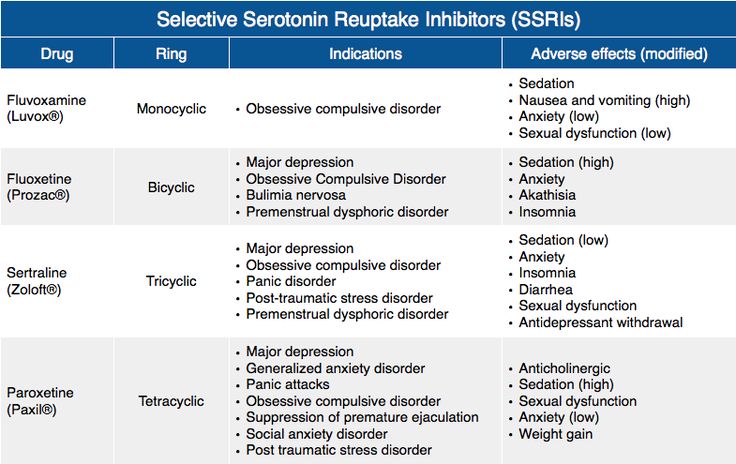 )
)
Changing Your Depression Medications
If you and your doctor have ruled out factors that could interfere with your current medication, your doctor may increase the dosage, switch you to another antidepressant or recommend you take an additional medication. Drug therapies that treat depression include:
Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRI drugs are the most commonly prescribed antidepressants and are often considered the first line of defense against depression. They increase your brain's level of a neurotransmitter (a chemical that transfers messages from brain cell to brain cell) called serotonin. This neurotransmitter is associated with feeling happy and content. SSRI side effects tend to be mild, and depression symptoms improve significantly for about 60% of people with moderate to severe depression.
Selective Serotonin Noradrenaline Reuptake Inhibitors (SSNRIs)
Both SSNRI and SSRI medications affect serotonin levels, but SSNRI drugs also impact the level of norepinephrine, another neurotransmitter that may affect mood. This type of medication is helpful for those who have extreme fatigue associated with depression, or who have had side effects or poor response to SSRI drugs.
This type of medication is helpful for those who have extreme fatigue associated with depression, or who have had side effects or poor response to SSRI drugs.
Tricyclic Antidepressants (TCAs)
TCA drugs increase serotonin and norepinephrine in the brain, but unlike other antidepressant types, they also block acetylcholine, a neurotransmitter associated with increased stress, anxiety and depression. You may experience more side effects with TCA medications than with SSRI or SSNRI drugs.
Monoamine Oxidase Inhibitors (MAOIs)
MAOI drugs inhibit the breakdown of dopamine, norepinephrine and serotonin, which increases their concentration in the brain. Low levels of these neurotransmitters are associated with depression and anxiety. MAOI drugs have a greater number of serious side effects. People taking them have to be mindful of the medication's interactions with certain foods and other drugs.
Bupropion
Bupropion acts on dopamine and norepinephrine.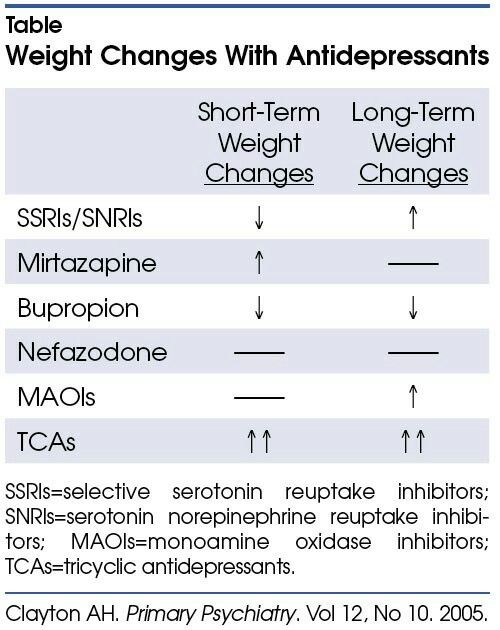 Its main advantage is that it doesn't cause troublesome side effects such as decreased libido and weight gain like other types of antidepressants do. However, it may be less helpful for depression with anxiety features.
Its main advantage is that it doesn't cause troublesome side effects such as decreased libido and weight gain like other types of antidepressants do. However, it may be less helpful for depression with anxiety features.
Esketamine
This newer drug provides relief from depression symptoms within hours by increasing levels of glutamate, the most abundant neurotransmitter in the brain. Esketamine comes in a nasal spray that must be administered in a clinic because it can cause hallucinations and other sensory side effects for up to two hours after treatment. It's an effective drug for those who haven't responded to other antidepressants.
If you're experiencing breakthrough depression, it's important to consult with your doctor so you can feel better again. "It's not unusual for medications to stop working," says Nestadt. "It happens with other sorts of medical treatments as well. Sometimes your blood pressure medicine is no longer effective and it has to be switched. It's just the nature of treating illness."
It's just the nature of treating illness."
Going Off Antidepressants - Harvard Health Publishing
Coming off your medication can cause antidepressant withdrawal – and could set you up for a relapse of depression.
Can going off your medication cause antidepressant withdrawal symptoms (antidepressant discontinuation syndrome)? About 10% of women ages 18 and over take antidepressants. As many of us know, these medications can be a godsend when depression has robbed life of its joy and made it hard to muster the energy and concentration to complete everyday tasks. But as you begin to feel better and want to move on, how long should you keep taking the pills?
If you're doing well on antidepressants and not complaining of too many side effects, many physicians will renew the prescription indefinitely — figuring that it offers a hedge against a relapse of depression. But side effects that you may have been willing to put up with initially — sexual side effects (decreased desire and difficulty having an orgasm), headache, insomnia, drowsiness, vivid dreaming, or just not feeling like yourself — can become less acceptable over time, especially if you think you no longer need the pills.
The decision to go off antidepressants should be considered thoughtfully and made with the support of your physician or therapist to make sure you're not stopping prematurely, risking a recurrence of depression. Once you decide to quit, you and your physician should take steps to minimize or avoid the discontinuation symptoms that can occur if such medications are withdrawn too quickly.
Why antidepressant withdrawal?
Antidepressants work by altering the levels of neurotransmitters — chemical messengers that attach to receptors on neurons (nerve cells) throughout the body and influence their activity. Neurons eventually adapt to the current level of neurotransmitters, and symptoms that range from mild to distressing may arise if the level changes too much too fast — for example, because you've suddenly stopped taking your antidepressant. They're generally not medically dangerous but may be uncomfortable.
Among the newer antidepressants, those that influence the serotonin system — selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) — are associated with a number of withdrawal symptoms, often called antidepressant or SSRI discontinuation syndrome. Stopping antidepressants such as bupropion (Wellbutrin) that do not affect serotonin systems — dopamine and norepinephrine reuptake inhibitors — seems less troublesome overall, although some patients develop extreme irritability.
Stopping antidepressants such as bupropion (Wellbutrin) that do not affect serotonin systems — dopamine and norepinephrine reuptake inhibitors — seems less troublesome overall, although some patients develop extreme irritability.
Having discontinuation symptoms doesn't mean you're addicted to your antidepressant. A person who is addicted craves the drug and often needs increasingly higher doses. Few people who take antidepressants develop a craving or feel a need to increase the dose. (Sometimes an SSRI will stop working — a phenomenon called "Prozac poop-out" — which may necessitate increasing the dose or adding another drug.)
Antidepressant withdrawal can look like depressionDiscontinuation symptoms can include anxiety and depression. Since these may be the reason you were prescribed antidepressants in the first place, their reappearance may suggest that you're having a relapse and need ongoing treatment.
If symptoms last more than a month and are worsening, it's worth considering whether you're having a relapse of depression. |
Antidepressant withdrawal symptoms
Neurotransmitters act throughout the body, and you may experience physical as well as mental effects when you stop taking antidepressants or lower the dose too fast. Common complaints include the following:
Common complaints include the following:
- Digestive. You may have nausea, vomiting, cramps, diarrhea, or loss of appetite.
- Blood vessel control. You may sweat excessively, flush, or find hot weather difficult to tolerate.
- Sleep changes. You may have trouble sleeping and unusual dreams or nightmares.
- Balance. You may become dizzy or lightheaded or feel like you don't quite have your "sea legs" when walking.
- Control of movements. You may experience tremors, restless legs, uneven gait, and difficulty coordinating speech and chewing movements.
- Unwanted feelings. You may have mood swings or feel agitated, anxious, manic, depressed, irritable, or confused — even paranoid or suicidal.
- Strange sensations. You may have pain or numbness; you may become hypersensitive to sound or sense a ringing in your ears; you may experience "brain-zaps" — a feeling that resembles an electric shock to your head — or a sensation that some people describe as "brain shivers.
 "
"
As dire as some of these symptoms may sound, you shouldn't let them discourage you if you want to go off your antidepressant. Many of the symptoms of SSRI discontinuation syndrome can be minimized or prevented by gradually lowering, or tapering, the dose over weeks to months, sometimes substituting longer-acting drugs such as fluoxetine (Prozac) for shorter-acting medications. The antidepressants most likely to cause troublesome symptoms are those that have a short half-life — that is, they break down and leave the body quickly. (See the chart "Antidepressant drugs and their half-lives.") Examples include venlafaxine (Effexor), sertraline (Zoloft), paroxetine (Paxil), and citalopram (Celexa). Extended-release versions of these drugs enter the body more slowly but leave it just as fast. Antidepressants with a longer half-life, chiefly fluoxetine, cause fewer problems on discontinuation.
Besides easing the transition, tapering the dose decreases the risk that depression will recur. In a Harvard Medical School study, nearly 400 patients (two-thirds of them women) were followed for more than a year after they stopped taking antidepressants prescribed for mood and anxiety disorders. Participants who discontinued rapidly (over one to seven days) were more likely to relapse within a few months than those who reduced the dose gradually over two or more weeks.
In a Harvard Medical School study, nearly 400 patients (two-thirds of them women) were followed for more than a year after they stopped taking antidepressants prescribed for mood and anxiety disorders. Participants who discontinued rapidly (over one to seven days) were more likely to relapse within a few months than those who reduced the dose gradually over two or more weeks.
Antidepressant drugs and their half-lives* | ||
| Drug | Half out of body in | 99% out of body in |
| Serotonin reuptake inhibitors | ||
| paroxetine (Paxil) | 24 hours | 4. |
| sertraline (Zoloft) | 26 hours | 5.4 days |
| escitalopram (Lexapro) | 27 to 32 hours | 6.1 days |
| citalopram (Celexa) | 36 hours | 7.3 days |
| fluoxetine (Prozac) | Four to six days | 25 days |
| Serotonin and norepinephrine reuptake inhibitors | ||
| venlafaxine (Effexor) | 5 hours | 1 day |
| duloxetine (Cymbalta) | 12 hours | 2. |
| desvenlafaxine (Pristiq) | 12 hours | 2.5 days |
| Dopamine and norepinephrine reuptake inhibitor | ||
| bupropion (Wellbutrin) | 21 hours | 4.4 days |
| *Discontinuation symptoms typically start when 90% or more of the drug has left your system. Source: Adapted from Joseph Glenmullen, M.D., The Antidepressant Solution: A Step-by-Step Guide to Safely Overcoming Antidepressant Withdrawal, Dependence, and "Addiction" (Free Press, 2006). | ||
How to go off antidepressants
If you're thinking about stopping antidepressants, you should go step-by-step, and consider the following:
Take your time. You may be tempted to stop taking antidepressants as soon as your symptoms ease, but depression can return if you quit too soon. Clinicians generally recommend staying on the medication for six to nine months before considering going off antidepressants. If you've had three or more recurrences of depression, make that at least two years.
Talk to your clinician about the benefits and risks of antidepressants in your particular situation, and work with her or him in deciding whether (and when) to stop using them. Before discontinuing, you should feel confident that you're functioning well, that your life circumstances are stable, and that you can cope with any negative thoughts that might emerge. Don't try to quit while you're under stress or undergoing a significant change in your life, such as a new job or an illness.
Make a plan. Going off an antidepressant usually involves reducing your dose in increments, allowing two to six weeks between dose reductions. Your clinician can instruct you in tapering your dose and prescribe the appropriate dosage pills for making the change. The schedule will depend on which antidepressant you're taking, how long you've been on it, your current dose, and any symptoms you had during previous medication changes. It's also a good idea to keep a "mood calendar" on which you record your mood (on a scale of one to 10) on a daily basis.
Consider psychotherapy. Fewer than 20% of people on antidepressants undergo psychotherapy, although it's often important in recovering from depression and avoiding recurrence. In a meta-analysis of controlled studies, investigators at Harvard Medical School and other universities found that people who undergo psychotherapy while discontinuing an antidepressant are less likely to have a relapse.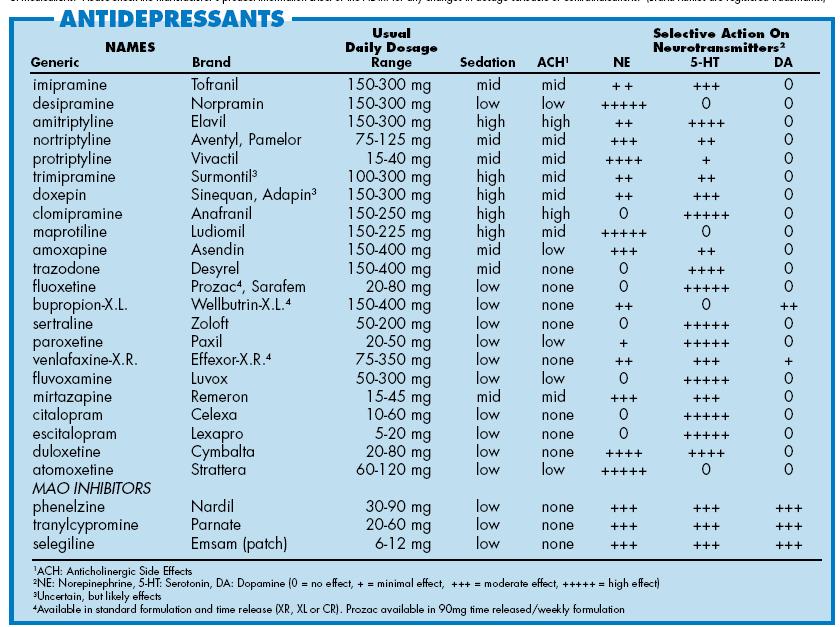
Stay active. Bolster your internal resources with good nutrition, stress-reduction techniques, regular sleep — and especially physical activity. Exercise has a powerful antidepressant effect. It's been shown that people are far less likely to relapse after recovering from depression if they exercise three times a week or more. Exercise makes serotonin more available for binding to receptor sites on nerve cells, so it can compensate for changes in serotonin levels as you taper off SSRIs and other medications that target the serotonin system.
Seek support. Stay in touch with your clinician as you go through the process. Let her or him know about any physical or emotional symptoms that could be related to discontinuation. If the symptoms are mild, you'll probably be reassured that they're just temporary, the result of the medication clearing your system. (A short course of a non-antidepressant medication such as an antihistamine, anti-anxiety medication, or sleeping aid can sometimes ease these symptoms.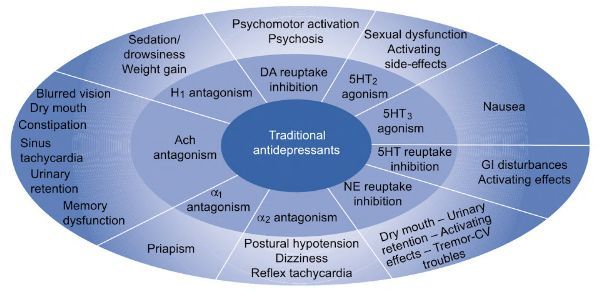 ) If symptoms are severe, you might need to go back to a previous dose and reduce the levels more slowly. If you're taking an SSRI with a short half-life, switching to a longer-acting drug, like fluoxetine, may help.
) If symptoms are severe, you might need to go back to a previous dose and reduce the levels more slowly. If you're taking an SSRI with a short half-life, switching to a longer-acting drug, like fluoxetine, may help.
You may want to involve a relative or close friend in your planning. If people around you realize that you're discontinuing antidepressants and may occasionally be irritable or tearful, they'll be less likely to take it personally. A close friend or family member may also be able to recognize signs of recurring depression that you might not perceive.
Complete the taper. By the time you stop taking the medication, your dose will be tiny. (You may already have been cutting your pills in half or using a liquid formula to achieve progressively smaller doses.) Some psychiatrists prescribe a single 20-milligram tablet of fluoxetine the day after the last dose of a shorter-acting antidepressant in order to ease its final washout from the body, although this approach hasn't been tested in a clinical trial.
Check in with your clinician one month after you've stopped the medication altogether. At this follow-up appointment, she or he will check to make sure discontinuation symptoms have eased and there are no signs of returning depression. Ongoing monthly check-ins may be advised.
Image: AlinaTraut/Getty Images
What are antidepressants? | Colta.ru
What are antidepressants? | Colta.ruOctober 24, 2013 Colta Specials Educational program
119
Burial of a doll Short course: free music How to reform healthcare in Russia? Short course: free jazz Viktor Shenderovich. A short praise of ironyHow to write "Tetris"How search engines workAnatoly Naiman: life without a prescriptionWhat is a post-Soviet person? What is culture?
COLTA. RU revives the project "Likbez" , in which well-known experts will present their views on the fundamental concepts and phenomena of culture and life . In the next series of children's psychiatrist, suicidologist and psychotherapist Elena Vrono tells how to deal with fears with the help of medicines.
RU revives the project "Likbez" , in which well-known experts will present their views on the fundamental concepts and phenomena of culture and life . In the next series of children's psychiatrist, suicidologist and psychotherapist Elena Vrono tells how to deal with fears with the help of medicines.
People are mortally afraid of going to psychiatrists, and going to a psychotherapist seems to be not so scary for them anymore. A psychotherapist is a doctor who does not resort to medication support. This, of course, is a legacy of the totalitarian past, which will make itself felt for a very long time. Until quite recently, psychiatry was a fearsome weapon in the hands of the state. And to admit oneself mentally ill was simply dangerous for oneself and loved ones. However, psychiatrists are arranged differently: some are ready to talk with the patient and consider it a very important component of treatment, while others believe that they have a technical tool in the form of a medicine. They write out a prescription and, without further ado, firmly shake the patient's hand.
They write out a prescription and, without further ado, firmly shake the patient's hand.
I mainly meet people along the way who, although they suffer from mental disorders (panic attacks, depression, insomnia, neurotic disorders, tics, obsessions), nevertheless overcome them without stopping the flow of their usual life. Although such a life cannot be fully considered normal, because a person who, for example, experiences constant anxiety and fear, becomes very tense and irritable. Outwardly, this often looks like aggressiveness. The quality of his life and the life of his loved ones is deteriorating. Family ties suffer, his career success suffers, because his efficiency decreases.
I am often asked the question - is it necessary to resort to medicines? It won't just go away? I answer: probably, it will pass, only it will take a lifetime. It will take a long time. The main criterion for me when to give up is when you see that the symptoms that you find in yourself (depressed mood, anhedonia, fears, anxiety states, panic attacks) are ruining your life.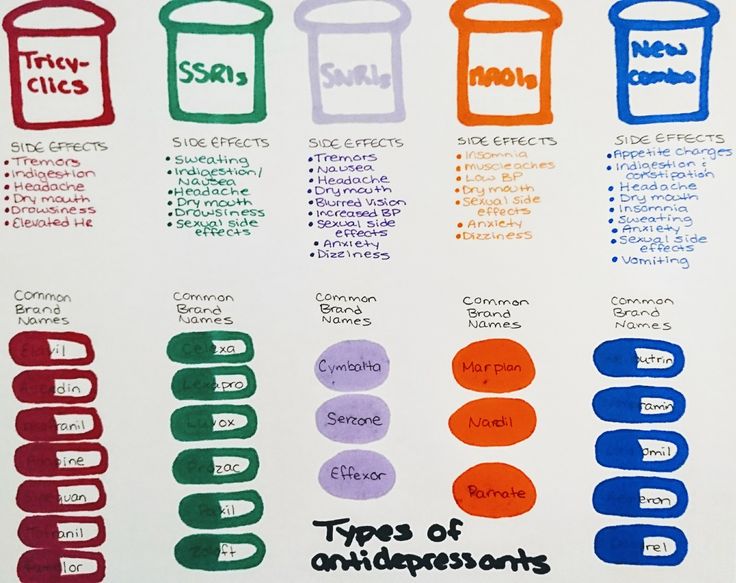 For example, you have troubling fears, in connection with which you check many times whether you turned off the kettle when you left or not. Coming back from the elevator. I even almost reached the subway, and ... "no, let me go check it out." It is uncomfortable, unpleasant, painful. As long as you get it right - get it right. But then the moment comes that you couldn’t leave the house because of the teapot. The time has passed for which you had an important meeting, but you canceled it, imagining that you were ill. And this is not the first time - the situation repeats itself. When you see that fears that seemed nonsense and innocent prevent you from living, you need to go to a psychiatrist.
For example, you have troubling fears, in connection with which you check many times whether you turned off the kettle when you left or not. Coming back from the elevator. I even almost reached the subway, and ... "no, let me go check it out." It is uncomfortable, unpleasant, painful. As long as you get it right - get it right. But then the moment comes that you couldn’t leave the house because of the teapot. The time has passed for which you had an important meeting, but you canceled it, imagining that you were ill. And this is not the first time - the situation repeats itself. When you see that fears that seemed nonsense and innocent prevent you from living, you need to go to a psychiatrist.
Modern antidepressants are designed not to reduce, but only to improve the quality of life.
Modern antidepressants make it possible to deal with such disorders. And for this you do not need to take a vacation or go to the hospital. This has been possible since the latest generation of antidepressants appeared, which interfere with very subtle biochemistry and affect the functioning of the systems that command the transmission of nerve impulses (the neurotransmitter system). They target different receptors, mainly serotonergic . The drugs of the previous generation were often much more effective than the current ones, that is, they had a more immediate effect, but at the same time they had severe side effects - almost always there was, for example, lightheadedness or dry mouth, and a sharp increase in body weight. When you deal in outpatient practice with people who "remain in life", you understand that these are all very serious things. It is necessary to choose drugs so that there are as few side effects as possible. Side effects are various somatic discomfort that you have to endure. It's a matter of price. Are you ready to endure it? Are your loved ones ready to endure? So, for example, in the treatment of many serotonergic drugs, various kinds of sexual dysfunctions are observed. They are temporary and dose dependent. The patient must be warned about this (this is called "obtaining informed consent"), as well as his partner, because he can take it personally and the relationship will suffer from this.
They target different receptors, mainly serotonergic . The drugs of the previous generation were often much more effective than the current ones, that is, they had a more immediate effect, but at the same time they had severe side effects - almost always there was, for example, lightheadedness or dry mouth, and a sharp increase in body weight. When you deal in outpatient practice with people who "remain in life", you understand that these are all very serious things. It is necessary to choose drugs so that there are as few side effects as possible. Side effects are various somatic discomfort that you have to endure. It's a matter of price. Are you ready to endure it? Are your loved ones ready to endure? So, for example, in the treatment of many serotonergic drugs, various kinds of sexual dysfunctions are observed. They are temporary and dose dependent. The patient must be warned about this (this is called "obtaining informed consent"), as well as his partner, because he can take it personally and the relationship will suffer from this.
What should be kept in mind? First of all, there are no magical remedies in the world that would only heal and not cause any toxic effects. If someone says “yes” to you, they are lying to you. Can not be! The question is how to find a balance between the benefits of a drug and the harm it causes, because any chemical you use has toxic effects. In addition, a balance must be struck between the dangers of using drugs and those of not taking treatment. How destructive the disease itself will be. This is what needs to be weighed.
Modern drugs - if they are prescribed by a specialist - do not bring irreversible harm. Moreover, antidepressants are a group of drugs that are not addictive. Many of them even allow the use of alcohol in small quantities. They are designed not to reduce, but only to improve the quality of life. But there is an unconditional, necessary requirement - to withstand the terms of treatment that are declared by the developers. These periods are usually very, very large.
The myth that nerve cells do not regenerate is refuted.
It is completely useless to talk empty talk about these being marketing ploys. Indeed, the pharmaceutical business is a very capital-intensive business. There are huge funds going around. But at the same time, there is no reason to believe that all drug efficacy researchers are bought by pharmaceutical companies. This is such a conspiracy toy, which is also beneficial to someone. First of all, those who are thinking about how to move this drug off the market in order to replace it with some other one. In order not to be trapped, it is necessary to act consciously, consult a doctor and trust him. Only a specialist will be able to determine the balance of harm and benefit of the drug, because he understands the mechanism of its action.
Antidepressants work like this. There are very important proteins, the function of which is that they carry nerve impulses on themselves. Serotonin, which is on everyone's lips, is one of them. The trick is that, on the one hand, it is produced by a nerve cell and is thrown into the intercellular space in order to fulfill its function. But in order for the nerve cell to function, it must swallow some of this substance back as food. It's called a "pump". When, under the influence of various stresses, the “pump” fails, then, for example, too little serotonin remains in the intercellular space, and the nerve impulse is not transmitted as well as it should. The drug helps to stop the reuptake. He is hindered. Therefore, the drug here plays the role of not a prosthesis for the leg, but a crutch. And while there is a crutch, gradually this pump regains its ability to be full. This takes a lot of time.
Serotonin, which is on everyone's lips, is one of them. The trick is that, on the one hand, it is produced by a nerve cell and is thrown into the intercellular space in order to fulfill its function. But in order for the nerve cell to function, it must swallow some of this substance back as food. It's called a "pump". When, under the influence of various stresses, the “pump” fails, then, for example, too little serotonin remains in the intercellular space, and the nerve impulse is not transmitted as well as it should. The drug helps to stop the reuptake. He is hindered. Therefore, the drug here plays the role of not a prosthesis for the leg, but a crutch. And while there is a crutch, gradually this pump regains its ability to be full. This takes a lot of time.
Patience is key when taking antidepressants. There will be no immediate effect, because the action of these drugs is due to the fact that they adjust to a very tricky biochemistry that regulates mood changes, an increase or decrease in the level of anxiety, all sorts of somatic signals that have no organic soil under them, look like a somatic disease , but in fact are a mask of depression or anxiety. On the other hand, it is absolutely necessary to resist the temptation to stop treatment as soon as you feel better. To do this, you need to see a doctor, regularly share your feelings with him, and provide him with feedback. When you feel better, it doesn't cost anything to lose the motivation to swallow pills. I don’t feel like it, it’s a pity for the money (these drugs are not cheap), and besides, there is a self-confidence that you haven’t experienced for a long time, and you think: “Next, I myself!” But when this “next” comes, the person himself cannot evaluate. It is absolutely necessary to meet the deadlines, because achieving the effect is not a trick (well, this drug will not work, we will choose another one), it is important not to disrupt this effect. And wait for the moment when we will carefully cancel the drug, and the effect will remain in place. This can only be achieved by being patient and meeting deadlines.
On the other hand, it is absolutely necessary to resist the temptation to stop treatment as soon as you feel better. To do this, you need to see a doctor, regularly share your feelings with him, and provide him with feedback. When you feel better, it doesn't cost anything to lose the motivation to swallow pills. I don’t feel like it, it’s a pity for the money (these drugs are not cheap), and besides, there is a self-confidence that you haven’t experienced for a long time, and you think: “Next, I myself!” But when this “next” comes, the person himself cannot evaluate. It is absolutely necessary to meet the deadlines, because achieving the effect is not a trick (well, this drug will not work, we will choose another one), it is important not to disrupt this effect. And wait for the moment when we will carefully cancel the drug, and the effect will remain in place. This can only be achieved by being patient and meeting deadlines.
The head is an unpaired organ, and it is unlikely that it will be possible to replace it with a donor one.

Susceptibility to depression depends on how the genes lay down. Experience shows that those people who suffer from depression also find sufferers among their relatives more often than those who have never had depression. It should be clarified that there is no fatal predisposition. A mother who suffers from depression will not necessarily have the same child. Indeed, this cunning biochemistry, which determines the level of optimism, the level of anxiety, everything that is superstructural, unsteady and intangible, is not very stress-resistant. It is impossible to imagine life without stress.
To say “Am I depressed?” and get together for a consultation with a doctor, you need to make sure that its symptoms are found constantly for a certain time, do not allow you to fully function, turning into a system, and cannot be dictated by any other reasons. And the reasons can be very different. For example, when the thyroid gland is not functioning properly, symptoms of true severe depression occur.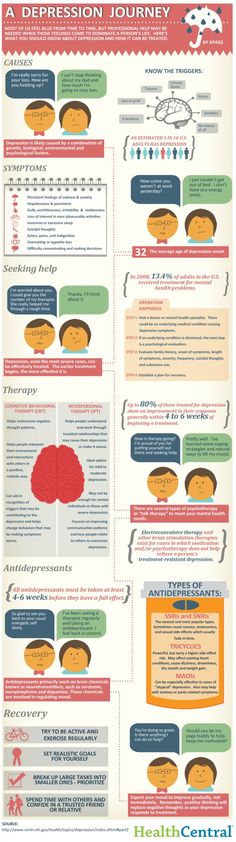 It often happens that people turn to a psychiatrist with this, who prescribes antidepressants, but they do not cause an effect. The patient finally thinks about the examination with which to begin. A lot of somatic diseases occur under the guise of depression. There are frequent diseases (for example, angina pectoris), which at the beginning of an attack cause a real panic attack. And there is only one thing you can do about it - consult a doctor. Self-employment is dangerous here.
It often happens that people turn to a psychiatrist with this, who prescribes antidepressants, but they do not cause an effect. The patient finally thinks about the examination with which to begin. A lot of somatic diseases occur under the guise of depression. There are frequent diseases (for example, angina pectoris), which at the beginning of an attack cause a real panic attack. And there is only one thing you can do about it - consult a doctor. Self-employment is dangerous here.
Over-the-counter products - vitamins and phytocomplexes - can be used for prevention. The exception is herbal medicines that try to pass themselves off as antidepressants, for example, from St. John's wort. Although they are sold without prescriptions, this is quite a risky thing. Phytopreparations are more physiological. They act while spinning in the blood. And you can count on the fact that even if you missed the drug, it will not bring serious destruction.
Can nootropics be used to prevent disorders? Almost all nootropics are designed in such a way that their molecules allow themselves to be ridden by an oxygen molecule and then penetrate the membrane into the nerve cell, supplying it with excess oxygen. This improves metabolism. There is a danger here - almost all nootropics, due to their activating effect, also activate mental activity. If you struggle with anxiety or fear, the anxiety will rise and the fear will rise too.
This improves metabolism. There is a danger here - almost all nootropics, due to their activating effect, also activate mental activity. If you struggle with anxiety or fear, the anxiety will rise and the fear will rise too.
Susceptibility to depression depends on how the genes lay down.
The attitude to taking antidepressants as a manifestation of spinelessness is the Soviet way of looking at things. Escape from reality is when you improve your mood with alcohol or cocaine. Neither alcohol, nor cocaine, nor other drugs can improve your performance. And you don’t set such a goal for yourself either - you achieve euphoria. And the right person - the one who knows how to survive in difficult conditions, pulls himself together. Medications are completely different: firstly, you control what you do, and secondly, they are aimed at ensuring that your activity remains the way you need it for a fulfilling life. It's not an escape at all.
The most important thing is to give up pride. Man, of course, is god-like, but at the same time he is a subject of nature, a biological subject. Everything that happens to us is all metaphysics, all love, hatred, all the subtlest intellectual activity, and so on. - is a product of the functioning of the neuropsychic sphere. You need to allow yourself a slightly more even biological, rather than a biological, view of what is happening to you. Then you will not be terrified that some pill affects your immortal soul. No, it's not. You intervene in a painful process that develops as a result of a disorder in the functioning of the neuropsychic sphere. Just like you take bronchodilators if you're having an asthma attack. To approach the fact that what is happening to you is dictated by a biological device means to try to give up pride. It is very difficult because it is not real.
Man, of course, is god-like, but at the same time he is a subject of nature, a biological subject. Everything that happens to us is all metaphysics, all love, hatred, all the subtlest intellectual activity, and so on. - is a product of the functioning of the neuropsychic sphere. You need to allow yourself a slightly more even biological, rather than a biological, view of what is happening to you. Then you will not be terrified that some pill affects your immortal soul. No, it's not. You intervene in a painful process that develops as a result of a disorder in the functioning of the neuropsychic sphere. Just like you take bronchodilators if you're having an asthma attack. To approach the fact that what is happening to you is dictated by a biological device means to try to give up pride. It is very difficult because it is not real.
With the development of high technology in medicine, the most perfect miracles have become possible. For example, the myth that nerve cells do not regenerate is refuted. This is wrong! The nerve cell is very intricately arranged and differs from any other, in particular, in that it has many processes (dendrites), which allow the cells to approach each other very smoothly. Previously, it was possible to work with a nerve cell only on sectional material, that is, when a person had already died. Sections were taken and viewed with very powerful microscopes, and they saw that in those who suffered from a depressive disorder, the cell configuration changed very much. Now it can be done in vivo - live. And it is clear that when a person suffers from depression, his nerve cell changes, its processes become smoother and they do not fit well with other cells. That is, a person first of all loses what makes him the king of nature - his mental plasticity, his ability to adapt to the most incredible conditions. His adaptability is decreasing. But then we see with the same microscope that when the antidepressant treatment begins, these processes take their former shape - they grow again.
This is wrong! The nerve cell is very intricately arranged and differs from any other, in particular, in that it has many processes (dendrites), which allow the cells to approach each other very smoothly. Previously, it was possible to work with a nerve cell only on sectional material, that is, when a person had already died. Sections were taken and viewed with very powerful microscopes, and they saw that in those who suffered from a depressive disorder, the cell configuration changed very much. Now it can be done in vivo - live. And it is clear that when a person suffers from depression, his nerve cell changes, its processes become smoother and they do not fit well with other cells. That is, a person first of all loses what makes him the king of nature - his mental plasticity, his ability to adapt to the most incredible conditions. His adaptability is decreasing. But then we see with the same microscope that when the antidepressant treatment begins, these processes take their former shape - they grow again.
Psychiatric science cannot rely on the possibility of organ transplantation instead of drug treatment. The head is an unpaired organ, and it is unlikely that it will be possible to replace it with a donor one. So, it is necessary to move along the path of improving the biochemical impact. Each next drug should be more effective than the previous one and have fewer side effects. Creating an ideal medicine that would only heal and do no harm is an unattainable dream.
Recorded by Yulia Ryzhenko
Like the material? Help the site!
Test
Angels and Ghosts of "Other Space"
Do you know the heroes of the main Russian festival of new music?
news
March 11, 2022
14:52 COLTA.RU blocked in Russia
March 3, 2022
17:48 "Rain" temporarily stops broadcasting
17:18 The Union of Journalists of Karelia complained about Roskomnadzor to the Prosecutor General's Office
16:32 Sergey Abashin left the Association of Ethnologists and Anthropologists of Russia
15:36 The Prosecutor General's Office called participation in anti-war rallies extremism
All news
New in Colta Specials Most Read
Be Russian, Resist Death
11338
No future
14890
With a broken trough
9967
There will be no future
11637
Vulnerable future
10259
Editorial COLTA
73326
Culture during "war operations"
47488
Polyphonic witnesses of the end and beginning. Essays by Ganna Komar
Essays by Ganna Komar
8615
Branches
1249
The arrival of father Alexander Men and the late Soviet intelligentsia
466
Letter to dad
615
Olivia Plender. "History of the Kingdom of Beasts"
340
Today online
Around the horizontalMaria Rachmaninova: “The state is not an undoubted blessing”
Arnold Khachaturov and Sergey Mashukov talked with anarchist historian about the fate of the horizontal idea in the last two centuries
February 21, 20232347
Around the horizontalCo-living as a model for activism
Sociologist Lyubov Chernysheva studied St. Petersburg communal apartments. Maria Muskevich learned what achievements and mistakes can be found in this experience for activist initiatives
Petersburg communal apartments. Maria Muskevich learned what achievements and mistakes can be found in this experience for activist initiatives
February 13, 20234348
Around the horizontal"Conflicts are normal." About the pitfalls of horizontal
Horizontal associations are not only roses, very often they are quite tangible thorns. And you better be ready for them.
February 10, 20235409
Around the horizontalWhat prevents the anti-war movement from uniting?
Aleksey Sidorenko, head of the Greenhouse of Social Technologies, analyzes the difficulties of the anti-war movement and makes a proposal
January 24, 202310531
Colta SpecialsBe Russian, Resist Death
The future depends on survival practices, says Kirill Medvedev
January 24, 202311338
Colta SpecialsNo Future
Alexander Morozov on possible ways out of the 2022 disaster
January 24, 202314890
Colta SpecialsWith a broken trough
Olga Romanova about the best option from terrible
January 24, 20239967
Colta SpecialsNo Future
Lina Bulakhova and Oksana Timofeeva cancel the government and themselves
January 24, 202311637
Colta SpecialsVulnerable Future
Elena Fanailova deals with the present
January 24, 202310259
Around the horizontalHow communities can work safely and together
A small guide to the essentials for your peace of mind and productivity - from new digital services to practices of the 19th century
December 26, 202224458
Around the horizontal lineIlya Budraitskis: “It was important in the experience of dissidents to take other people's ideas seriously”
A conversation about the useful lessons of Soviet dissidence, about the conflict between the ethics of persuasion and the ethics of responsibility, and why people who support SVO should not be treated like robots or zombies
December 14, 202229041
Around the horizontalSvetlana Barsukova: "The stupidity of the law is often extinguished by the wisdom of practical actions"
A well-known sociologist about the huge repertoire of informal practices in Russia (from the system of bribes to neighborly mutual assistance), about the collective reaction to times of crisis and why even in the most ethically dangerous areas one can find common sense and benefit
December 5, 202227530
Long-term use of antidepressants is associated with an increased risk of coronary artery disease, cerebrovascular disease, cardiovascular and overall mortality, but a reduced risk of hypertension and diabetes mellitus: a large observational study
is 6 months, with a continuing risk of recurrence - 2 years. Very often, patients continue to take drugs for years.
Very often, patients continue to take drugs for years. It is known that depression is associated with an increase in the frequency of CVD risk factors (smoking, obesity, physical inactivity) and so on. In this situation, it is very difficult in an observational study to assess the safety profile of antidepressants in terms of cardiovascular complications and overall mortality: it is not entirely clear which will have an adverse effect - antidepressants or depression itself. Therefore, the bulk of research on this topic, as a rule, causes a lot of comments.
The British Journal of Psychiatry Open published the results of an analysis of the UK Biobank registry, the design of which claims to account for the maximum number of associated risk factors, including behavioral and socioeconomic. This is supposed to help separate the effects of antidepressants and depression itself. The study included patients who initially did not suffer from CVD, did not take cardiometabolic drugs, and did not use antidepressants during the last 12 months before inclusion. Of the 222,121 participants included, 8% were taking antidepressants at 5 years and 6% at 10 years. Serotonin reuptake inhibitors and other antidepressants were analyzed separately (amitriptyline was excluded from the analysis as low doses are often prescribed in older patients for insomnia).
Of the 222,121 participants included, 8% were taking antidepressants at 5 years and 6% at 10 years. Serotonin reuptake inhibitors and other antidepressants were analyzed separately (amitriptyline was excluded from the analysis as low doses are often prescribed in older patients for insomnia).
Multivariate analysis taking into account a large number of risk factors showed that long-term use of serotonin reuptake inhibitors is associated with an increased risk of cerebrovascular disease (OR 1.34, 95% CI 1.02–1.77), cardiovascular mortality (OR 1.87, 95% CI 1.38–2.53) and death from all causes (OR 1.73, 1.48–2.03) after 10 years. For other antidepressants, similar patterns are revealed, but the odds ratios are higher: the OR for CHD is 1.99 (1.31–3.01), for cardiovascular death - 1.86 (1.10–3.15), for death from all causes - 2.2 (1.71–2.84). A relationship was found between doses of drugs and the risk of complications. Whether there is a causal relationship between antidepressants and increased mortality remains unclear.
 Here's how to distinguish discontinuation symptoms from relapse:
Here's how to distinguish discontinuation symptoms from relapse: 4 days
4 days 5 days
5 days