Can bpd turn into schizophrenia
Borderline Schizophrenia: What It Is and More
It’s rare for borderline personality disorder (BPD) and schizophrenia to occur together, but it is possible.
Mental health conditions aren’t usually cut-and-dry conditions. It’s common for some people to have multiple mental health conditions that might be connected, such as living with depression and anxiety, or post-traumatic stress disorder (PTSD) and substance use disorder (SUD).
The same is true for some people with schizophrenia and borderline personality disorder (BPD), which can occur together.
To understand what the co-occurring disorders of borderline personality disorder and schizophrenia might look like, it can be helpful to familiarize yourself with what each disorder looks like separately.
And despite the seriousness of each condition, managing symptoms is possible with the right treatment plan.
You won’t find the term “borderline schizophrenia” in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM 5). It hasn’t been a recognized disorder since 1980.
Borderline schizophrenia — or “pseudoneurotic schizophrenia” — is an outdated term once used interchangeably with “borderline psychosis.” Later on, this was split into the current classifications of schizotypal personality disorder and borderline personality disorder (BPD).
But there are some overlapping symptoms between BPD and schizophrenia.
Can you have BPD and schizophrenia together?
It is possible for someone to have both disorders at the same time, though it is rare. But more research is still needed on the comorbidity of BPD and schizophrenia.
While 2014 research indicates that people with borderline personality disorder often experience co-occurring psychiatric conditions, the exact rate of schizophrenia and BPD comorbidity specifically isn’t clear just yet.
A 2010 study found that 17.6% of people diagnosed with schizophrenia also met the criteria for BPD. But research from 2018 illustrated that schizophrenia was present in only 2% of females with BPD.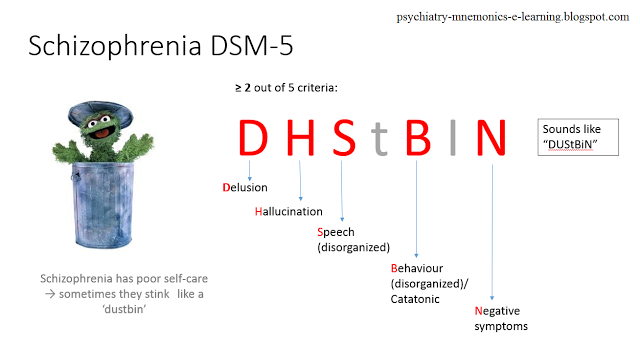
If you or a loved one has both BPD and schizophrenia, learning the similarities and differences of these conditions can be helpful in understanding how they may interact.
Borderline personality disorder (BPD)
BPD is classified in the DSM 5 as a personality disorder, which is generally characterized by:
- rigid thinking
- atypical behavior
- difficulty maintaining stable relationships
Research from 2008 found that up to 5.9% of people may experience BPD at some point in their lifetime. Onset typically occurs during adolescence or young adulthood.
Schizophrenia
Schizophrenia falls within the schizophrenia spectrum class of disorders in the DSM 5.
According to the National Institute of Mental Health (NIMH), schizophrenia affects less than 1% of the population, and is among the top 15 causes of disability worldwide, with symptoms indicating a diminished connection to reality.
Psychosis
Psychosis refers to a severe disconnection from reality.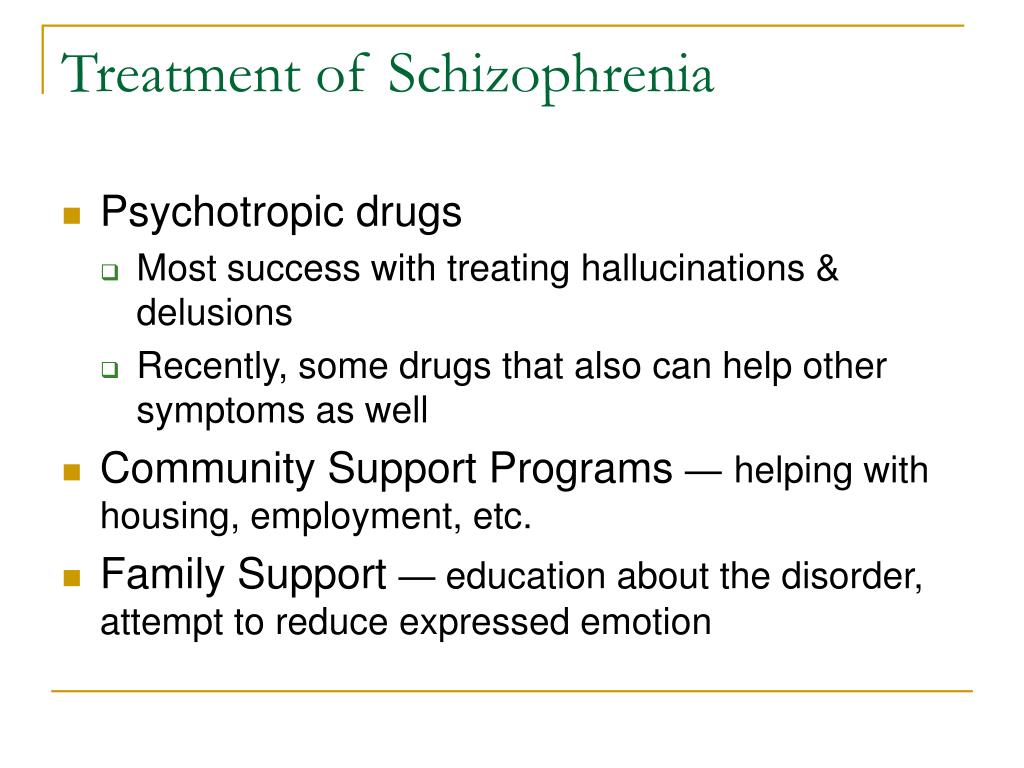 Psychotic episodes include hallucinations or delusions.
Psychotic episodes include hallucinations or delusions.
Psychosis can occur in both schizophrenia and borderline personality disorder, but psychotic episodes in BPD are, by definition, short, fleeting, and related to stress.
A significant but smaller percentage of people with BPD experience hallucinations than people with schizophrenia. According to research from 2021, an estimated 29% to 50% of people with BPD report hallucinations.
This is compared to an estimated 60% to 80% of people with schizophrenia who report experiencing these symptoms, based on a 2021 review.
And unlike schizophrenia, BPD psychotic episodes are generally not accompanied by negative symptoms or disorganization.
While it’s rare for BPD and schizophrenia to cooccur together, some symptoms may overlap.
Knowing the differences in how each condition’s symptoms can look and feel can be helpful.
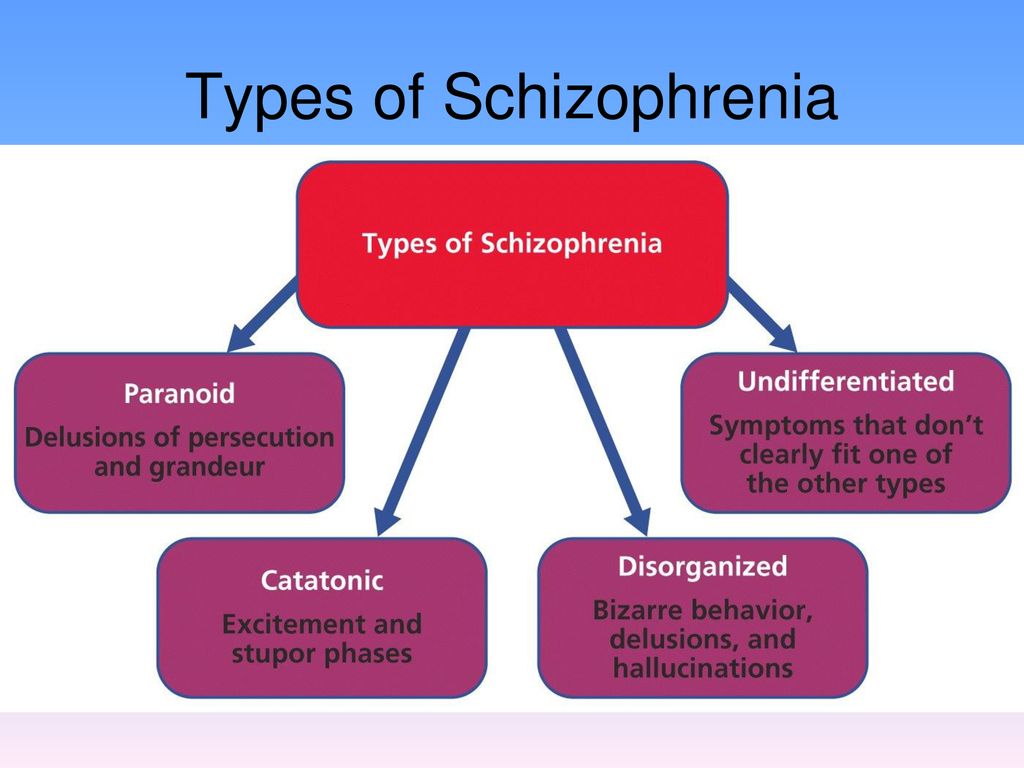
Schizophrenia symptoms
Schizophrenia symptoms generally fall under three categories:
- Positive symptoms: this includes psychosis (including hallucinations and delusions), disordered thinking and speech, altered sensations
- Negative symptoms: these symptoms include reduced motivation, difficulty planning, suppressed emotions, social withdrawal
- Cognitive symptoms: this can include trouble withattention or concentration, memory loss, difficulty absorbing information, trouble making decisions
BPD symptoms
Some of the most common symptoms of borderline personality disorder include:
- sweeping shifts in mood and behavior
- varying perceptions of self and others
- emotional instability, including episodes of anger
- depression and anxiety
- unstable relationships with friends, family, and romantic partners
- impulsivity
- feeling a lack of purpose or emptiness
- self-harm
- suicidal ideation
A significant but smaller percentage of people with BPD may also experience:
- dissociation
- hallucinations
- delusions
- paranoia
If you’re considering acting on suicidal thoughts, please seek professional support immediately.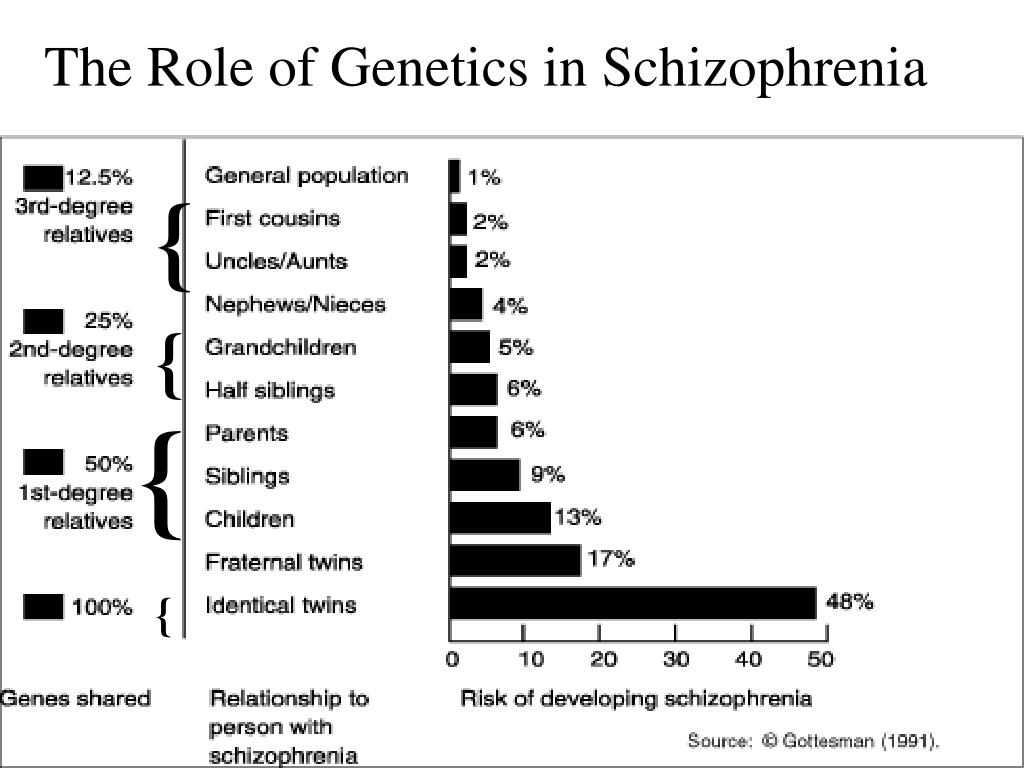
Calling or texting a crisis helpline will connect you with a trained counselor 24/7, any day of the year, completely free of charge:
- Call the National Suicide Prevention Lifeline at 988.
- Text HOME to 741741 to reach the Crisis Text Line.
The causes of both BPD and schizophrenia aren’t entirely clear to experts at this time, and more research is needed. It’s believed that genetics, physiology, and environment all play a role in the development of these conditions.
No single factor is likely to lead to the development of these disorders but rather a complex combination of multiple sources.
Genetics
Though no single gene has been identified as a cause of BPD or schizophrenia, it’s clear that family history may play a role in their development.
A 2017 review of twin studies found that if an identical twin develops schizophrenia, the other may have a higher chance of developing it, too.
Family members of those with BPD also have a higher chance of developing the condition, according to research from 2021.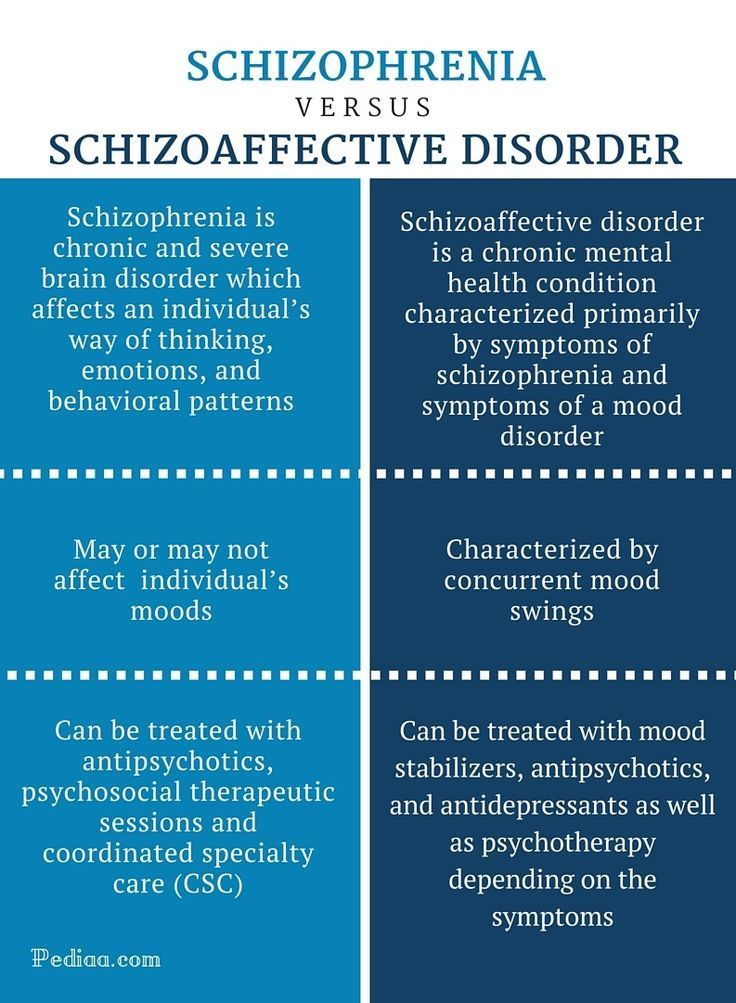
But this doesn’t mean that having a family member with one of these conditions guarantees that you will develop it, too.
Environment
Experiencing trauma early in life can be a contributing factor to developing BPD.
A 2021 review indicates that up to 90% of people living with BPD experienced childhood trauma, including:
- physical, verbal, or sexual abuse
- neglect
- bullying
A different 2021 review suggests that environmental sources may account for between 15% to 40% of the chance of developing schizophrenia, but those sources are believed to be more diverse than those that contribute to BPD.
This may include:
- complications at birth
- certain infections during pregnancy
- season of birth
- social factors, such as migration and living in cities
- adverse childhood experiences (ACEs), like abuse and neglect
- drug use, especially cannabis
Physiology
Differences in neurotransmitter levels — especially serotonin and dopamine — may impact the development of both schizophrenia and BPD.
And, it’s not just your brain chemicals. Regions of the brain in charge of emotion regulation and impulse control — including the amygdala and hippocampus — may look and function differently in people with BPD.
Neuroimaging research from 2018 of people with schizophrenia showed significant differences in the size and activity of the frontal and temporal lobes, which play a large role in:
- memory
- emotion
- language functioning
Both BPD and schizophrenia require professional treatment to manage. These conditions can be more difficult to address if you haven’t received an accurate diagnosis.
Working with a doctor or therapist on designing an effective treatment plan can help you manage symptoms.
Treatment plans for both conditions may consist of a combination of:
- psychotherapy
- medication
- self-care or lifestyle changes
Finding the best treatment plan for your symptoms can take time. You may have to try multiple strategies before finding what works for you.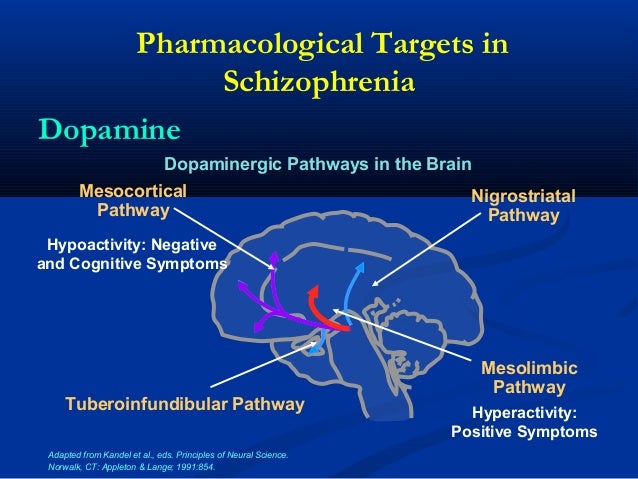
Therapy
Psychotherapy is considered a first-line treatment for BPD and is often used to treat schizophrenia in combination with medication.
Specific types of therapy used for BPD include:
- dialectical behavioral therapy (DBT)
- cognitive behavioral therapy (CBT)
- transference-focused therapy
Though research on how well transference-focused therapy performs is mixed.
For those with schizophrenia, therapy may focus more heavily on developing skills for managing everyday life.
Types of therapy commonly used include:
- cognitive behavioral therapy (CBT)
- social skills training
- assertive community treatment
- acceptance and commitment therapy
Medication
Currently, there are no FDA-approved medications available to specifically treat BPD. But some people with BPD may have overlapping mental health conditions and may be prescribed medications for those conditions, such as:
- antidepressants
- antipsychotics
- mood stabilizers
For people with schizophrenia, antipsychotic medication is commonly prescribed to help manage hallucinations and delusions, including:
- haloperidol (Haldol)
- aripiprazole (Abilify)
- clozapine (Clozaril)
- quetiapine (Seroquel)
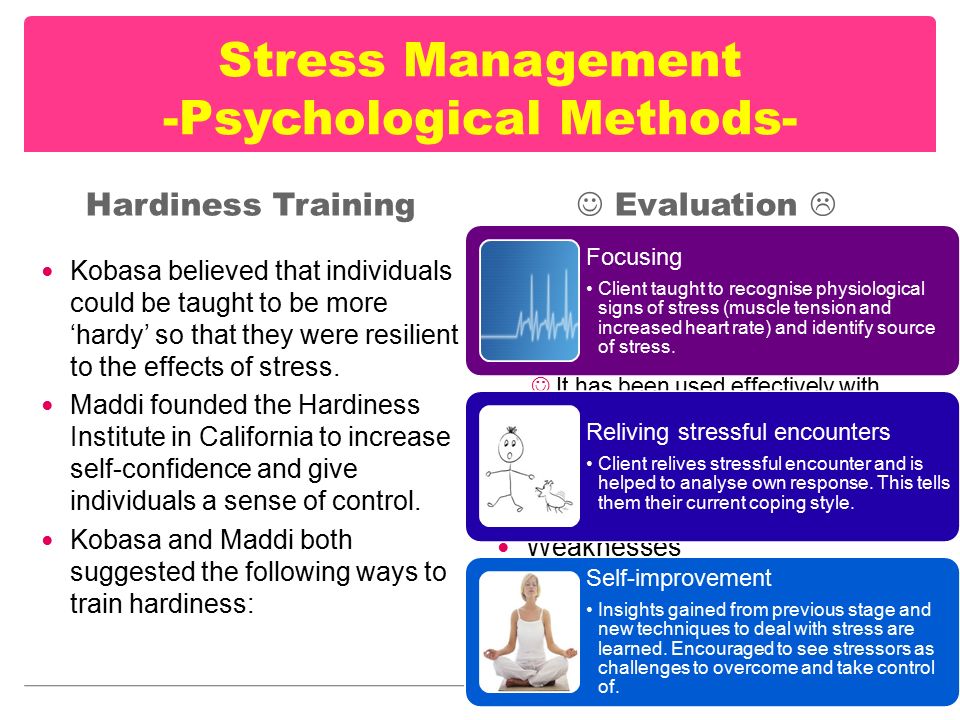
Self-care
Stress can impact both BPD and schizophrenia, and lifestyle changes centered on self-care can be essential for managing symptoms of these conditions.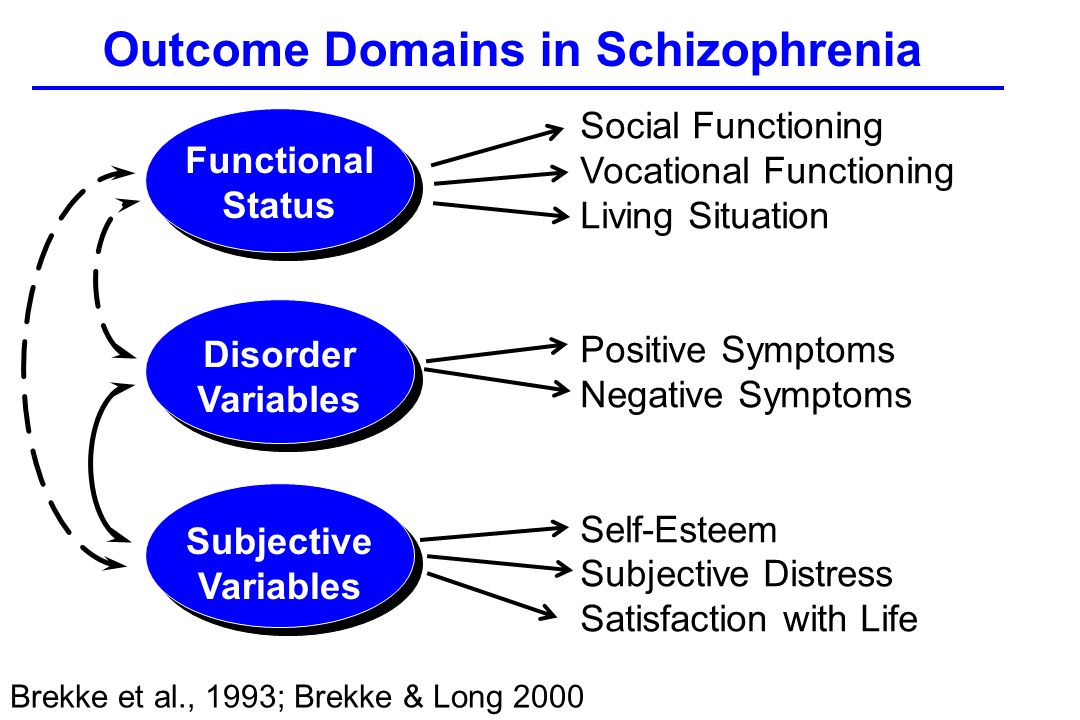
Some examples of self-care strategies include:
- exercising regularly
- eating nutritious foods
- maintaining a consistent sleep routine
- meditation and mindfulness practices
- journaling
- making time for hobbies and activities you love
- creating a support network
- joining support groups
If you or someone you know is experiencing symptoms of BPD and schizophrenia, you’re not alone. It’s possible to manage the symptoms of these conditions with the right treatment plan.
Consider talking with your doctor or therapist as a first step. Being curious and educating yourself on what these two conditions can look like — as well as possible treatment options — can be a helpful place to start your mental health journey.
If you’re ready to get help but don’t know where to begin, you can check out Psych Central’s hub for finding mental health support.
A Look at the Unoffical Diagnosis
Schizophrenia
A closer look at borderline schizophrenia – the unofficial diagnosis linking the shared symptoms of schizophrenia and borderline personality disorder (BPD).
Katie Hurley, LCSW
Medical ReviewerFarah Fazel, PsyS
What is Borderline Schizophrenia?
The term “borderline schizophrenia” does not refer to an established diagnosis in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). It is sometimes used, however, to refer to an individual who meets some, but not all, of the criterion for schizophrenia or to refer to parallel symptoms of borderline personality disorder and schizophrenia.
Symptoms of Borderline Schizophrenia
Given that “borderline schizophrenia” is not a formal diagnosis, it’s difficult to establish specific symptoms. It does help to understand the symptoms of schizophrenia, as the term can refer to an individual who shows some symptoms of the disease.
Two or more of the following symptoms are present for a significant portion of time during a one-month period.1
Level of functioning in work, interpersonal connection, or self-care is impaired by the symptoms for a significant portion of time.
 Change in functioning is significant compared to previous level of functioning.
Change in functioning is significant compared to previous level of functioning.Continuous signs of the disturbance for a six-month period. This period can include at least one month of active symptoms followed by residual periods or periods marked by negative symptoms.
Schizoaffective disorder and depressive or bipolar disorder with psychotic features have been ruled out.
The disturbance is not attributed to drug use or another medical condition.
If there is a history of autism spectrum disorder or a childhood communication disorder, a diagnosis of schizophrenia is only made if there are prominent delusions or hallucinations.
Schizophrenia and Borderline Personality Disorder (BPD)
Schizophrenia and borderline personality disorder (BPD) can share symptoms.
One study found that both patients with schizophrenia and patients with BPD experience hearing voices. The difference between the two being that paranoid delusions occurred in less than one-third of patients with BPD, compared with two-thirds in schizophrenia.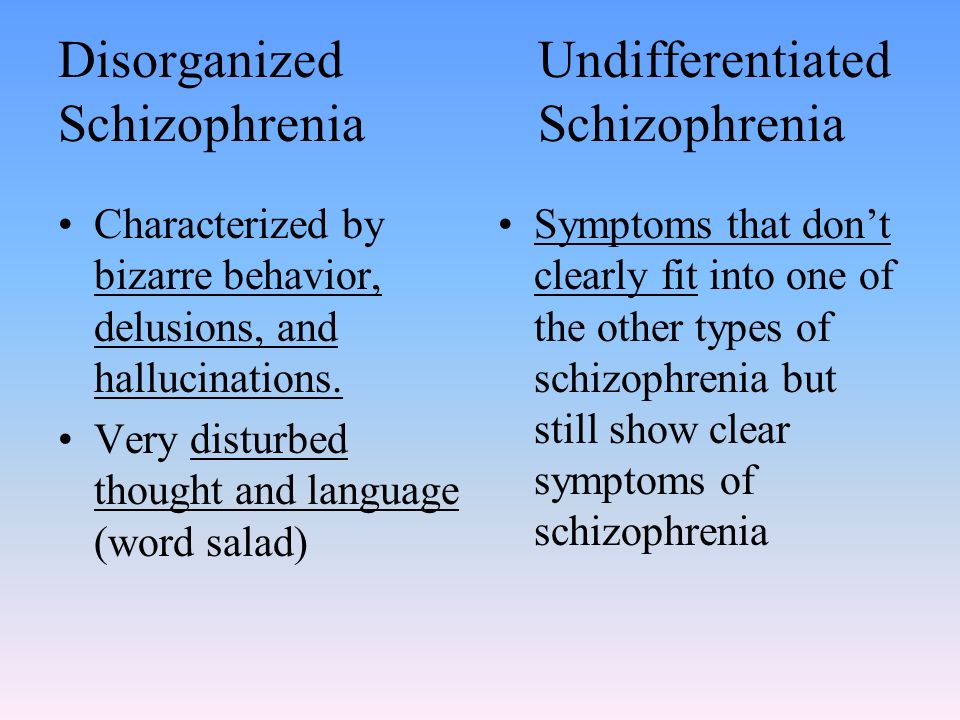 The study also found that auditory hallucinations are common in both populations.
The study also found that auditory hallucinations are common in both populations.
According to the results of this study, schizophrenia and BPD frequently co-exist. Accurate diagnosis of either or both conditions plays an important role in establishing an effective treatment plan.
Symptoms of Borderline Personality Disorder (BPD)
Given the comorbidity between schizophrenia and BPD, it can be useful to understand the symptoms of BPD.
BPD includes a pervasive pattern of instability of interpersonal relationships, self-image, and affects, marked impulsivity, beginning in early adulthood as indicated by at least five (or more) of the following symptoms:
Frantic efforts to avoid real or imagined abandonment
A pattern of unstable and intense relationships characterized by alternating extremes of idealization and devaluation
Identity disturbance characterized by persistently unstable self-image or sense of self
Impulsivity in at least two areas that are self-damaging: spending, sex, substance abuse, reckless driving, binge eating)
Affective instability due to reactivity of mood (intense episodic dysphoria, irritability, or anxiety)
Chronic feelings of emptiness
Inappropriate, intense anger or difficulty controlling anger
Transient, stress-related paranoid ideation or severe dissociative symptoms
During periods of extreme stress, paranoid ideation or dissociative symptoms can occur.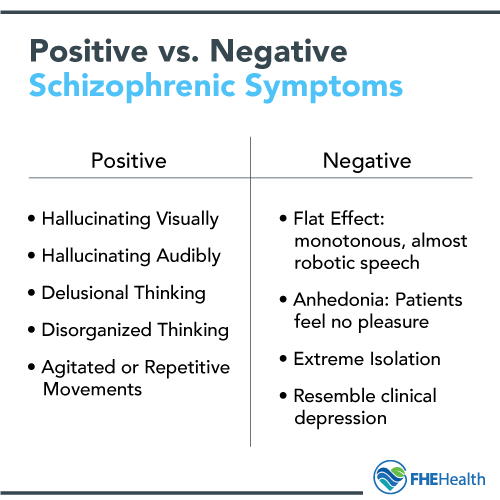 While these symptoms are generally insufficient to require an additional diagnosis, they can parallel some active symptoms of schizophrenia.
While these symptoms are generally insufficient to require an additional diagnosis, they can parallel some active symptoms of schizophrenia.
Seek Clarification
BPD is a very different diagnosis than schizophrenia, though the two can co-exist. While BPD is characterized by a pattern of instability in interpersonal relationships; schizophrenia is characterized by a range of cognitive, behavioral, and emotional dysfunctions.
If you, or someone you know, are described as having “borderline schizophrenia”, it could point toward mild symptoms, unclear symptoms, or a combination of symptoms. The best thing you can do is to seek clarification from a licensed professional.
The best way to find a treatment plan that works for you is to understand your symptoms. A second opinion or a follow-up visit to ask specific questions is always a good idea.
- American Psychological Association, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, American Psychiatric Publishing, Washington, D.
 C., 2013.
C., 2013. - Kingdon, David, et al., “Schizophrenia and Borderline Personality Disorder Similarities and Differences in the Experience of Auditory Hallucinations, Paranoia, and Childhood Trauma,” The Journal of Nervous and Mental Disease, 198(6), June 2010: 399-403.
Notes: This article was originally published December 13, 2017 and most recently updated October 25, 2022.
Borderline Schizophrenia - Phoenix Center
Borderline Schizophrenia is an unofficial diagnosis linking common symptoms of schizophrenia and borderline personality disorder.
What is borderline schizophrenia?
The term "borderline schizophrenia" does not refer to an established diagnosis in ICD-10. However, it is sometimes used to refer to a diagnosis of a patient who exhibits some but not all of the symptoms of schizophrenia, or to refer to the parallel symptoms of borderline personality disorder and schizophrenia.
Symptoms of borderline schizophrenia
If a person has the following symptoms for a month or more, this may be a manifestation of schizophrenia and a psychiatrist should be consulted:
- Delusions
- Brad
- Confusion
- Hallucinations
- Disorganized speech
- Extremely disorganized or catatonic behavior
- Negative symptoms (i.
 e. decreased emotional expression)
e. decreased emotional expression)
There are changes in the habitual way of life. The level of working capacity decreases, it is difficult for a person to contact with others, the performance of habitual activities becomes difficult. Such changes are noticeable and complicate a person's life.
Symptoms within 6 months. This period may include at least one month of positive symptoms followed by residual or negative symptom periods of schizophrenia.
Diagnoses such as schizoaffective disorder and depressive or bipolar disorder with psychotic features were excluded.
The disorder is not related to drug use or another medical condition.
If there is a history of autism spectrum disorder or communication disorder in childhood, a diagnosis of schizophrenia is made only if significant delusions or hallucinations are present.
Borderline personality disorder symptoms
Borderline personality disorder symptoms include a common pattern of interpersonal instability, unstable self-image, marked impulsivity beginning in early adulthood as evidenced by at least five (or more) of the following:
- Desperate efforts to avoid reality.

- A model of unstable and tense relations characterized by alternating extremes of idealization and devaluation.
- An identity disorder characterized by persistently unstable self-image, unstable self-perception and self-esteem.
- Impulsivity in at least two self-destructive areas: finances, sex life, substance abuse, reckless driving, overeating.
- Affective instability due to mood reactivity (intense episodic dysphoria, irritability or restlessness).
- Chronic feeling of emptiness.
- Inappropriate, intense anger or difficulty controlling anger.
- Transient, stress-related paranoid ideas or severe dissociative symptoms.
Paranoid thoughts or dissociative symptoms may occur during periods of high stress.
PROTECT YOUR HEALTH AND THE HEALTH OF YOUR LOVED ONES!
PLEASE CONTACT A PSYCHIATRIST IN TIME!
Causes, Symptoms and Treatments
Borderline Personality Disorder (abbreviated as BPD ) is increasingly common among children today.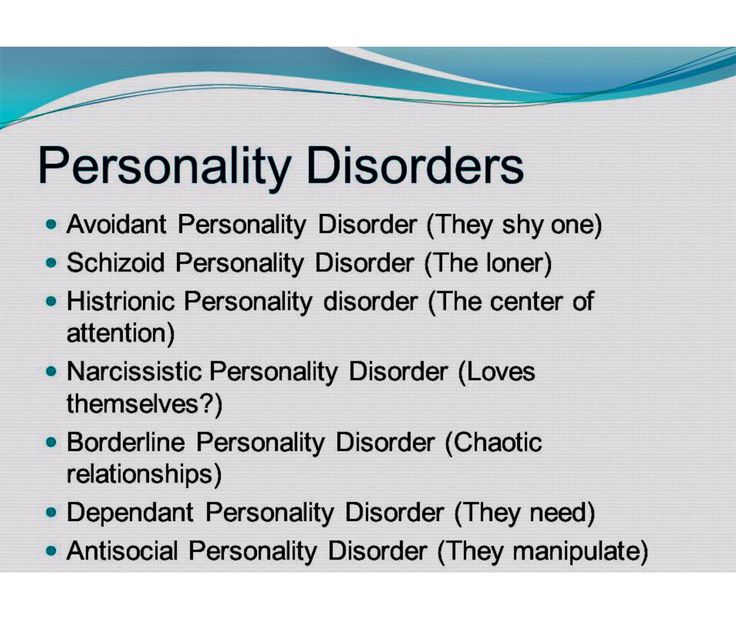 The pathogenesis of this type of psychopathy is usually accompanied by a complex of unfavorable factors.
The pathogenesis of this type of psychopathy is usually accompanied by a complex of unfavorable factors.
It is quite difficult to recognize this type of disease in everyday life. Often, it is confused with narcissism or simply the bad character of the individual, since the behavior of the "border guards" can be characterized by an extreme degree of unpredictability and hysteria, as well as a tendency to manipulation. For example, they confess their love to a partner, and after a couple of hours they leave “forever”, they can sincerely sympathize with someone, and then hit. It is also very common for patients of this type to constantly violate the boundaries of other people, shifting their problems onto them, and avoiding responsibility. Consider the symptoms of borderline in more detail.
Symptoms of borderline personality disorder (BPD)
The main symptomatic difference of this type of disorder is prolonged abnormal behavior of the patient .
While in many other psychopathy periods of instability alternate with remission, in the case of BPD the patient behaves destructively over a long period of time. In the field of psychological anomalies are such manifestations as:
In the field of psychological anomalies are such manifestations as:
- aggressive behavior leading to problems in relationships,
- unstable emotional background and inadequate self-image,
- high anxiety,
- total fear of loneliness and permanent feeling of boredom,
- dichotomous thinking and changeable mood, dividing the world only into "black and white" (today I love, but tomorrow I hate).
Also among the main symptoms can be noted: sociopathy and fear of society associated with low self-esteem and, as a result, separation anxiety (it is experienced by a person when separated from home or loved ones). Patients often exhibit reckless irresponsible "risky" behavior, the extreme form of which may be self-harm or suicide attempt.
Types of spontaneous actions that accompany mental borderline personality disorders
Due to difficulties in self-identification, lack of one's own opinion and a tendency to polarity, spontaneous destructive actions are characteristic of BPD sufferers.
The panic fear of loneliness and the lack of an inner core pushes them into contact with sociopathic personalities who are characterized by destructive behavior: gambling, theft, vandalism, promiscuous relationships, drug addiction. This also includes self-harm, which was mentioned above.
One of the reasons for this uncontrolled behavior is the problem with holding the inner impulse. The level of impulsivity is so high that a person is not able to control it.
Andrey Nikolaevich Cherednichenko
Chief physician of the Korsakov Medical Center network, psychiatrist-narcologist
- Experience for more than 12 years
Consultation
Records for reception
Emotionally unstable personality disorder in the ICD of the 10th revision personality disorder is defined as "Emotionally unstable personality disorder (F60.3)". In the clinical community on the territory of the Russian Federation, this name is used quite often and is used due to the fact that the main symptom, as described above, manifests itself in the form of an emotionally unstable mental state of a person.
BPD pathogenesis
In the pathogenesis of the disease lies an incorrectly or incompletely formed intrapersonal self-awareness, in other words, “self-identification”. Border guards hardly realize how they relate to the main areas of life. They have problems with the concept of their opinions, interests, hobbies, and their character as well. Hence the more common definition of the disorder - "borderline". In this aspect, it means maneuvering on the verge between psychopathy and a stable state. The word "borderline" in a particular case means a precarious state between the norm and deviation, as if a person lives on the verge between "mental illness" (psychosis) and "mental health". That is why, the slang name for patients of this type is “borderliners” (from the English expression “border line”, which literally translates as “border”).
In classical psychiatry, borderline personality disorder is also classified as an ego syntonic disorder. Ego syntonicity implies that the patient does not assess his condition as painful, is not critical of him and calmly accepts deviations in behavior, not believing that they harm him in any way.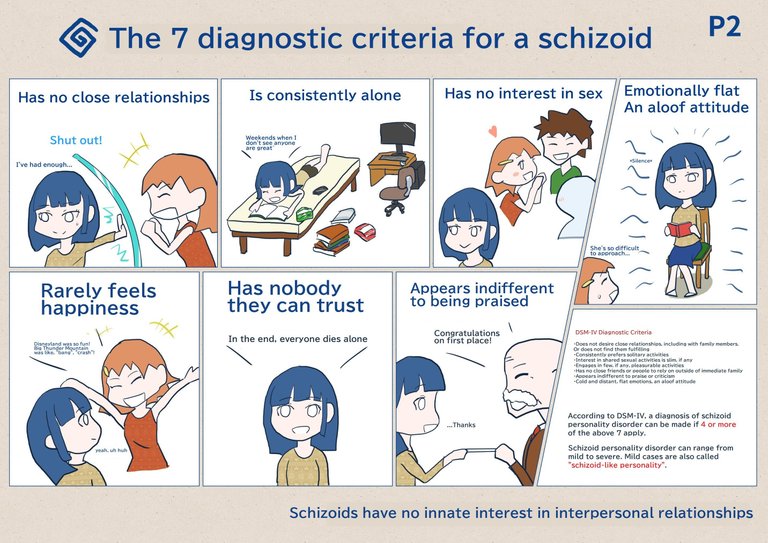 Moreover, the patient, as it were, “defends” his symptom, preventing his own cure due to the difficulty in identifying his own “I”.
Moreover, the patient, as it were, “defends” his symptom, preventing his own cure due to the difficulty in identifying his own “I”.
Causes of BPD
The underlying causes of BPD are currently not clearly defined, however, like most other disorders, BPD is caused by a group of factors.
Hereditary (genetic determinism), physiological (disturbances in the brain) and social factors (low stress resistance and psychological traumatic factor).
Unfavorable social environment
According to statistics, groups of people exposed to an unfavorable social environment, for example, in the family, are more susceptible to the disease. These include:
- difficult childhood,
- abuse,
- tyranny,
- physical or emotional domestic violence,
- early loss of parents.
It is worth noting that "borderliness" occurs 3 times more often among women than among men.
Post-traumatic stress disorder (PTSD) , as a variation of an unfavorable social factor, can act not only as a cause, but also as a concomitant individual disease that is in a pathogenetic relationship with the diagnosis in question.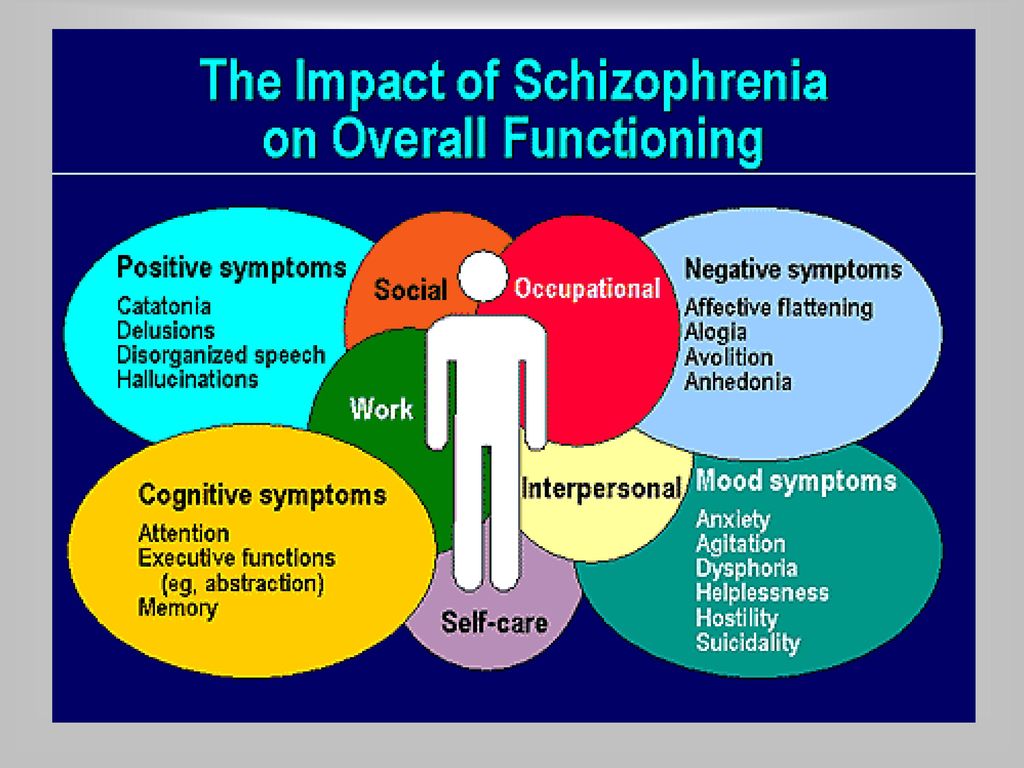
Childhood chronic emotional trauma can contribute to the development of BPD, but in rare cases it is the only cause. Personal qualities that are responsible for the ability to cope with a stressful situation in this aspect also play a big role. Here it is worth noting that, according to statistics, an injury received in childhood (especially before the age of 10) can lead to a subsequent disorder much more likely than an injury received at an older age. Also, scientists note that situations not associated with direct violence, such as natural disasters or catastrophes, are less likely to lead to the development of post-traumatic syndrome.
Physiology
Another group of factors considers a possible cause of the development of the disease - disturbances in the functioning of neural brain connections, namely the destruction of the functioning of the frontal-limbic neurons
Heredity
diagnosis. It is quite difficult to achieve clear indicators in this vein, however, according to European studies, BPD is located in 3rd place out of 10 in terms of the genetic determinant among personality disorders.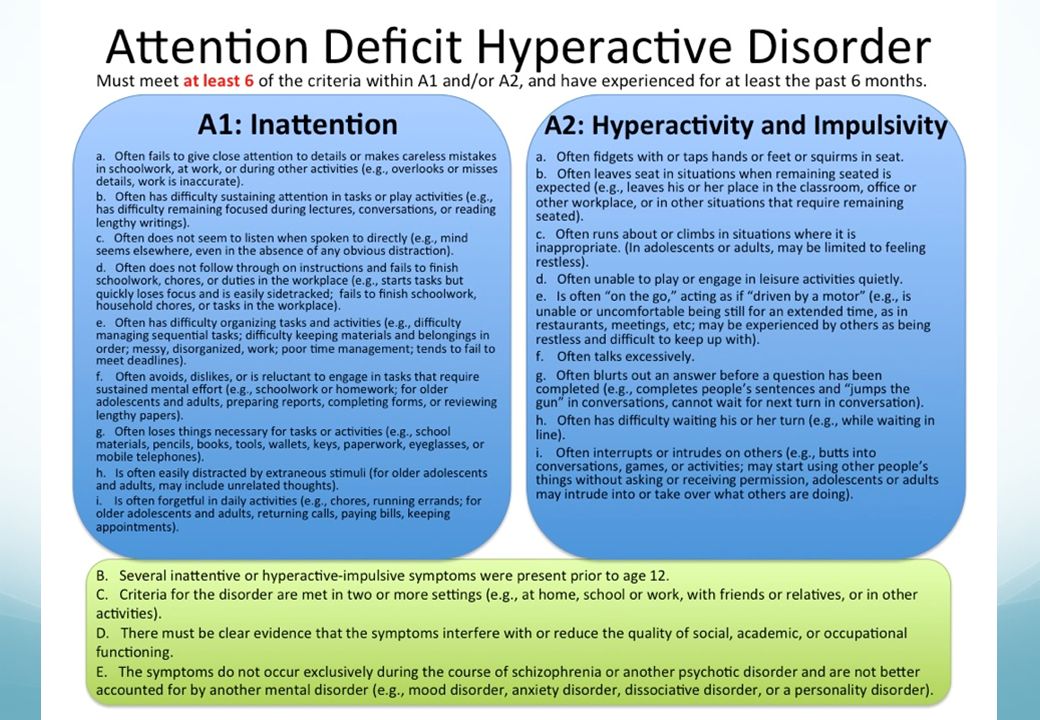 It is logical to note that deviations in the work of certain parts of the brain can be inherited and lead to a number of psychological problems, the development of which is aggravated by the social factor. Most studies show that most often borderlineness is transmitted from the mother.
It is logical to note that deviations in the work of certain parts of the brain can be inherited and lead to a number of psychological problems, the development of which is aggravated by the social factor. Most studies show that most often borderlineness is transmitted from the mother.
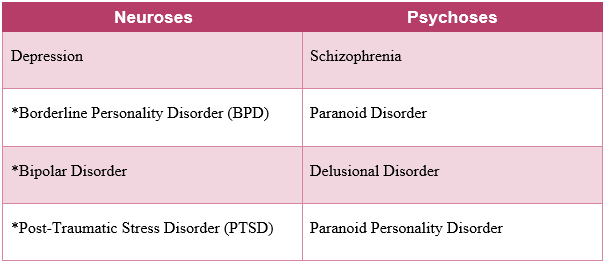
Borderline state of the psyche in psychiatry and the severity of personality disorders
In clinical psychiatry, three levels of mental disorder are traditionally distinguished:
- Neurotic . These include neuroses of a different nature, implying reversible temporary conditions that can be treated.
- Psychopathic level . In its plane lie personality disorders, which include anomalies in the nature of various pathogenesis or painful changes in its features, with which nothing can be done, since they relate to the personality structure of the individual.
- Finally, the deepest lesion of the psyche manifests itself at the psychotic level .
 This includes such manifestations as delirium, hallucinations, twilight consciousness.
This includes such manifestations as delirium, hallucinations, twilight consciousness.
Modern psychoanalysis distinguishes 4 levels of deviations. Between the state of psychosis and neurosis, it is conditionally located just “ borderline level”, also called borderline state . A borderline state can mean both the disorder itself and the designation of the level of mental damage.
How to reliably identify borderline personality disorder (BPD)
Borderline personality disorder is extremely difficult to diagnose and differentiate, as it has a high level of comorbidity, in other words, it is combined with a large number of comorbid disorders. For example, panic anxiety, eating disorders, bipolar affective disorder, attention deficit disorder, sociopathy, and so on. In connection with the above, the patient has to undergo a long diagnostic process and special tests.
Borderline personality disorder BPD test
One of the fairly popular tools for detecting the presence of psychopathy are tests, which are, in fact, a personality questionnaire.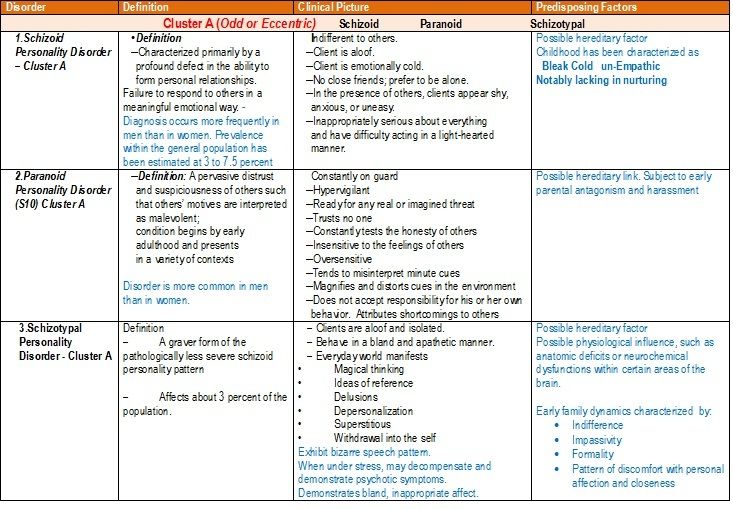 Used in modern clinical psychology, a test for screening for the bright signs of BPD was developed in 2012 by a group of scientists. In their work, the authors relied on the basic criteria for differentiating borderline disorder.
Used in modern clinical psychology, a test for screening for the bright signs of BPD was developed in 2012 by a group of scientists. In their work, the authors relied on the basic criteria for differentiating borderline disorder.
The questionnaire edited by them is a fairly effective tool for diagnostic verification and confirmation of symptoms. It is used both in psychiatric and general clinical, and in other practices that are not directly related to medicine.
The test itself consists of 20 questions and asks the subject to answer only yes or no. For each answer, the system counts a certain number of points. The probability of diagnosing BPD appears if the respondent scored more than 25 points.
Treatment of borderline personality disorder (BPD)
Cherednichenko Andrey Nikolaevich
Chief physician of the network of medical centers "Korsakov", psychiatrist-narcologist
- Experience over 12 years
Consultation
Appointment
Like most other mental disorders, borderline disorder is not treated at home and requires complex occupational therapy, including both medication (taking antidepressants and antipsychotics) and psychotherapy. And only a psychiatrist, often in tandem with a clinical psychologist, can competently develop an effective course of treatment.
And only a psychiatrist, often in tandem with a clinical psychologist, can competently develop an effective course of treatment.
The drug course is developed in accordance with the individual characteristics of the patient's body and includes the following drug groups:
- Selective inhibitors of are aimed at preventing depressive episodes and reducing anxiety/panic/borderline states.
- Mood stabilizers .
One of the most popular remedies is Lamotrigine. It is also used to neutralize depression, mood lability and impulsivity.
- Atypical antipsychotics .
Now the 2nd generation of drugs of this cluster has already been developed, which have proven themselves well in neutralizing the symptoms of the cognitive sphere, such as: aggression, distortion of perception of reality, paranoia, dichotomy of thinking and disorganization.
As for the group of benzodiazepines and stimulants, they are used in modern therapy extremely rarely due to the high risk of dependence and, accordingly, overdose.

Thus, the main task of drug therapy in borderline personality disorder is to reduce the brightness of symptoms and alleviate the general condition of the patient.
It is worth noting that BPD is the most difficult to treat due to the patient's ego syntony, which we discussed above. It is the patient with BPD who is the most difficult to respond to any therapy due to the rigidity of the psyche and the clear conviction that everything is generally normal with them.
However, when it comes to Selective Inhibitors, Dialectical Behavioral Therapy (DBT), one of the varieties of Cognitive Behavioral Therapy (CBT), is considered the most effective method in the modern clinical community. As part of the treatment, the patient is taught to look at the problem from different points of view and evaluate the causal relationship in different ways. Due to satisfaction with their symptoms and rigidity, "border guards" are difficult to treat, so the psychotherapeutic process can be lengthy.