Schizoaffective disorder defined
Schizoaffective Disorder | NAMI: National Alliance on Mental Illness
- Overview
- Treatment
- Support
- Discuss
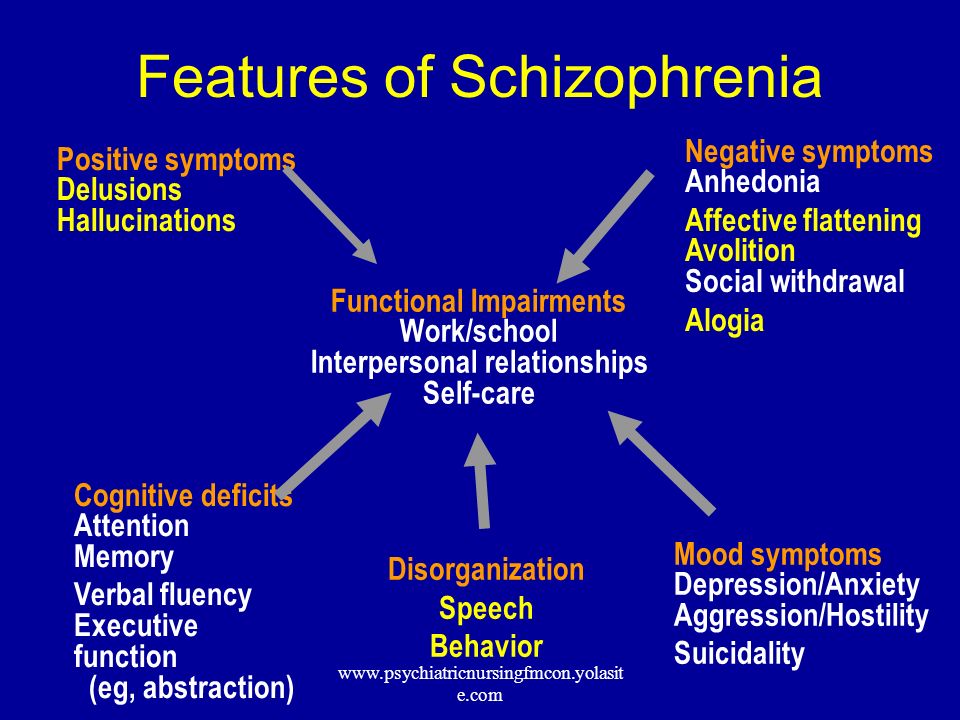
Schizoaffective disorder is a chronic mental health condition characterized primarily by symptoms of schizophrenia, such as hallucinations or delusions, and symptoms of a mood disorder, such as mania and depression.
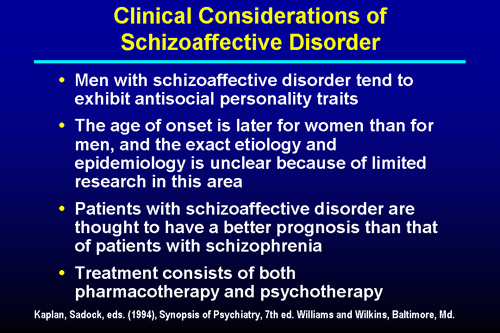
Many people with schizoaffective disorder are often incorrectly diagnosed at first with bipolar disorder or schizophrenia. Because schizoaffective disorder is less well-studied than the other two conditions, many interventions are borrowed from their treatment approaches.
Schizoaffective is relatively rare, with a lifetime prevalence of only 0.3%. Men and women experience schizoaffective disorder at the same rate, but men often develop the illness at an earlier age. Schizoaffective disorder can be managed effectively with medication and therapy. Co-occurring substance use disorders are a serious risk and require integrated treatment.
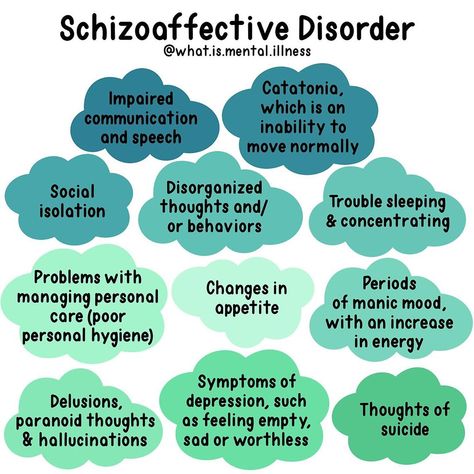
Symptoms
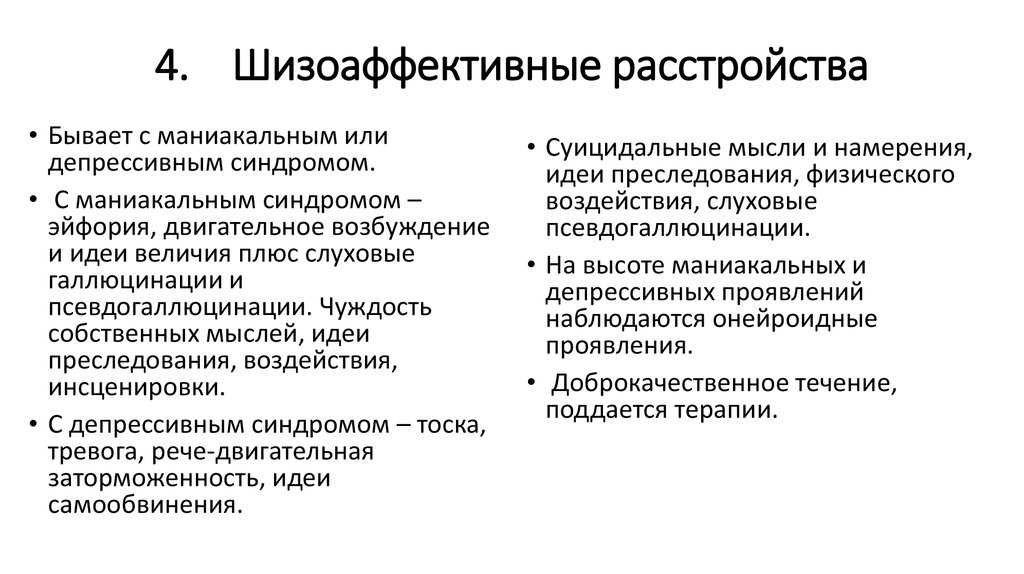
The symptoms of schizoaffective disorder can be severe and need to be monitored closely. Depending on the type of mood disorder diagnosed, depression or bipolar disorder, people will experience different symptoms:
- Hallucinations, which are seeing or hearing things that aren’t there.
- Delusions, which are false, fixed beliefs that are held regardless of contradictory evidence.
- Disorganized thinking. A person may switch very quickly from one topic to another or provide answers that are completely unrelated.
- Depressed mood. If a person has been diagnosed with schizoaffective disorder depressive type they will experience feelings of sadness, emptiness, feelings of worthlessness or other symptoms of depression.
- Manic behavior. If a person has been diagnosed with schizoaffective disorder: bipolar type they will experience feelings of euphoria, racing thoughts, increased risky behavior and other symptoms of mania.
Causes
The exact cause of schizoaffective disorder is unknown.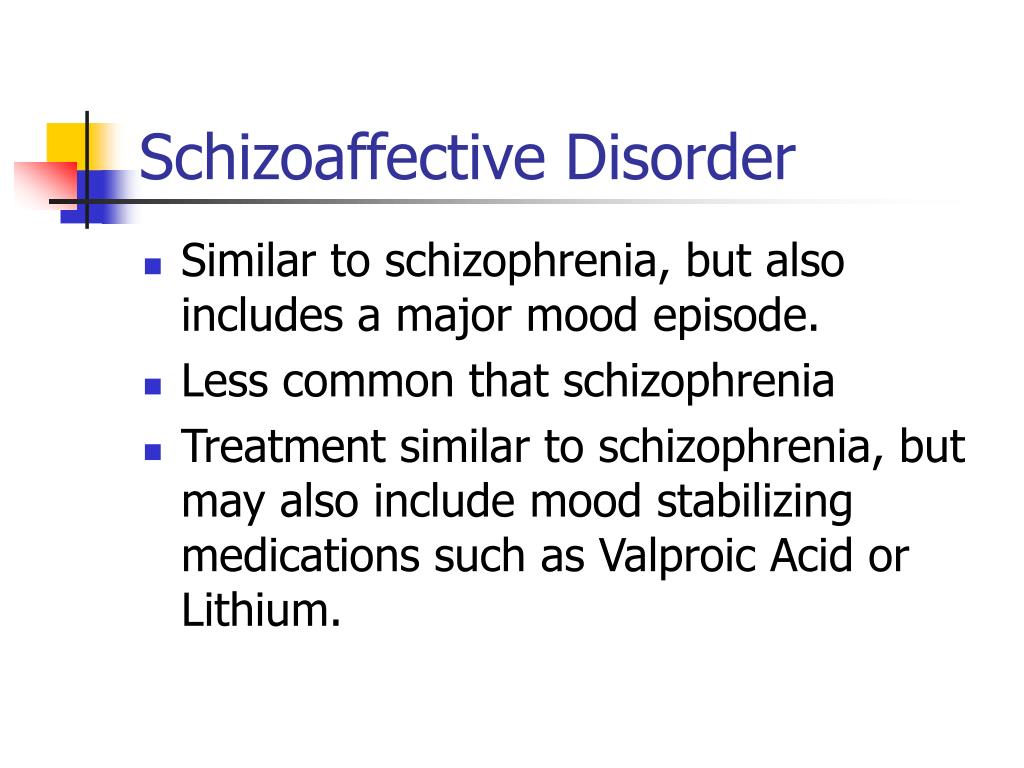 A combination of causes may contribute to the development of schizoaffective disorder.
A combination of causes may contribute to the development of schizoaffective disorder.
- Genetics. Schizoaffective disorder tends to run in families. This does not mean that if a relative has an illness, you will absolutely get it. But it does mean that there is a greater chance of you developing the illness.
- Brain chemistry and structure. Brain function and structure may be different in ways that science is only beginning to understand. Brain scans are helping to advance research in this area.
- Stress. Stressful events such as a death in the family, end of a marriage or loss of a job can trigger symptoms or an onset of the illness.
- Drug use. Psychoactive drugs such as LSD have been linked to the development of schizoaffective disorder.
Diagnosis
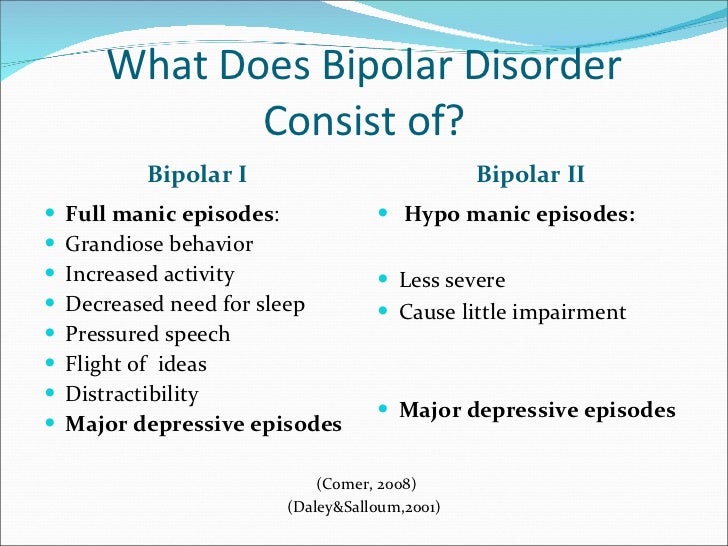
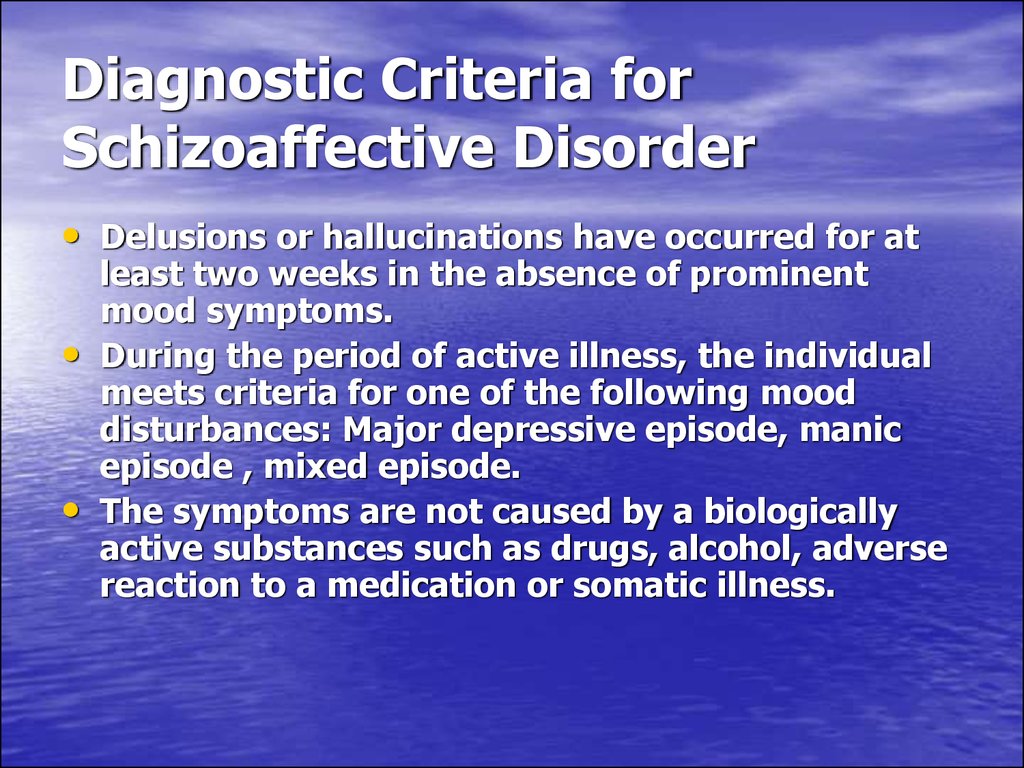
Schizoaffective disorder can be difficult to diagnose because it has symptoms of both schizophrenia and either depression or bipolar disorder.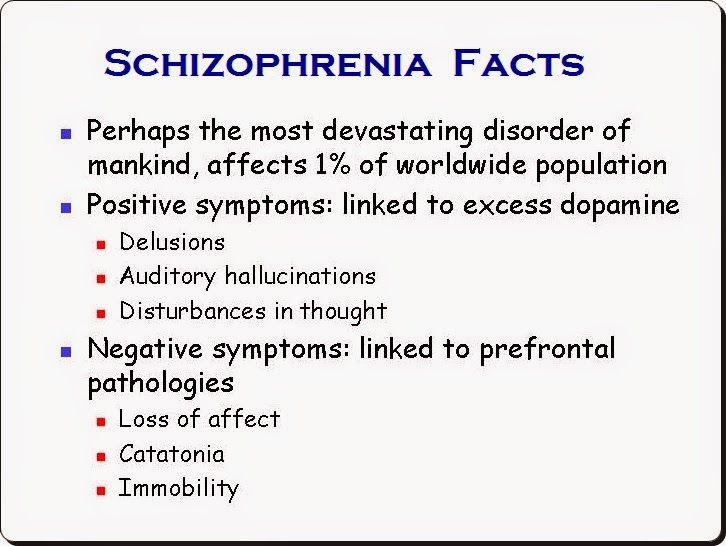 There are two major types of schizoaffective disorder: bipolar type and depressive type. To be diagnosed with schizoaffective disorder a person must have the following symptoms.
There are two major types of schizoaffective disorder: bipolar type and depressive type. To be diagnosed with schizoaffective disorder a person must have the following symptoms.
- A period during which there is a major mood disorder, either depression or mania, that occurs at the same time that symptoms of schizophrenia are present.
- Delusions or hallucinations for two or more weeks in the absence of a major mood episode.
- Symptoms that meet criteria for a major mood episode are present for the majority of the total duration of the illness.
- The abuse of drugs or a medication are not responsible for the symptoms.
Treatment
Schizoaffective disorder is treated and managed in several ways:
- Medications, including mood stabilizers, antipsychotic medications and antidepressants
- Psychotherapy, such as cognitive behavioral therapy or family-focused therapy
- Self-management strategies and education
Related Conditions
A person with schizoaffective disorder may have additional mental health conditions:
- Anxiety disorders
- Posttraumatic stress disorder (PTSD)
- Attention-deficit hyperactivity disorder (ADHD)
- Substance use disorders / Dual Diagnosis
Schizoaffective Disorder: Schizophrenia, Mood Disorder, Treatment
Overview
What is schizoaffective disorder?
Schizoaffective disorder is a serious mental health condition.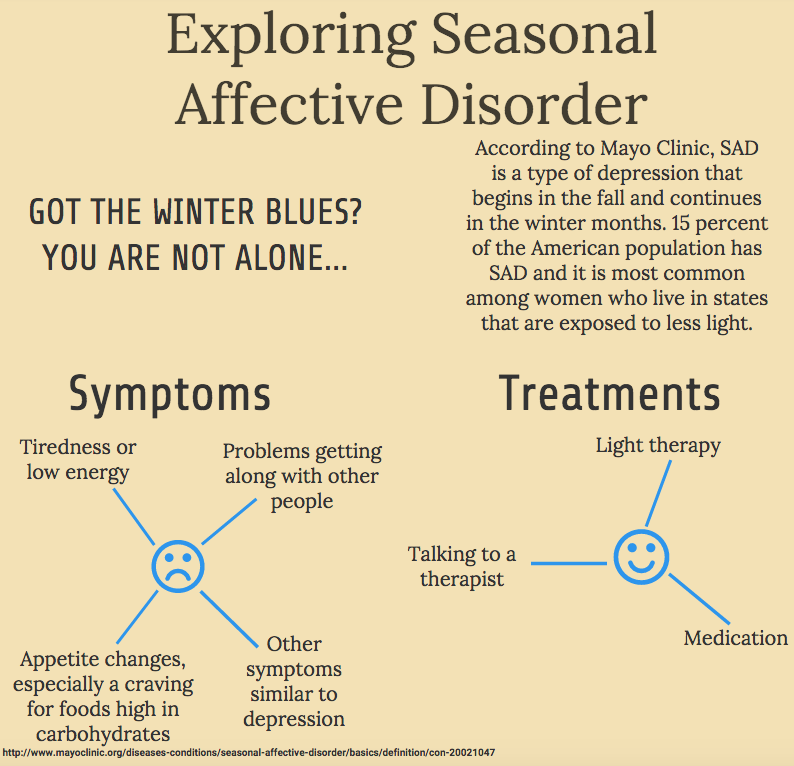 It has features of two different disorders:
It has features of two different disorders:
- “Schizo” means the psychotic symptoms of schizophrenia. This brain disorder changes how a person thinks, acts and expresses emotions. It also affects how someone perceives reality and relates to others.
- “Affective” refers to a mood disorder, or severe changes in a person’s mood, energy and behavior.
There’s no cure for schizoaffective disorder. But treatment can help people manage symptoms and improve their quality of life.
What are the types of schizoaffective disorder?
There are two types of schizoaffective disorder: bipolar schizoaffective disorder and depressive schizoaffective disorder. The two types are based on the associated mood disorder the person has:
- Bipolar disorder type: This condition features one or two types of different mood changes. People with bipolar disorder have severe highs (mania) alone or combined with lows (depression).
- Depressive type: People who have depression have feelings of sadness, worthlessness and hopelessness.
 They may have suicidal thoughts. They may also experience concentration and memory problems.
They may have suicidal thoughts. They may also experience concentration and memory problems.
How does schizoaffective disorder affect people?
This lifelong illness can affect all areas of a person’s life. A person with schizoaffective disorder can find it difficult to function at work or school. It also affects people’s relationships with family, friends and loved ones.Many people with schizoaffective disorder have periodic episodes. There are times when their symptoms surface and times when their symptoms might disappear for a while.
Who gets schizoaffective disorder?
The condition usually begins in the late teens or early adulthood, up to age 30. It rarely occurs in children. Studies suggest the disorder is more likely to occur in women than men.
How common is schizoaffective disorder?
Schizoaffective disorder is rare. Research estimates that 3 in every 1000 people (0.3%) will develop schizoaffective disorder in their lifetime.Still, it’s difficult to know exactly how many people have the condition because of the challenging diagnosis.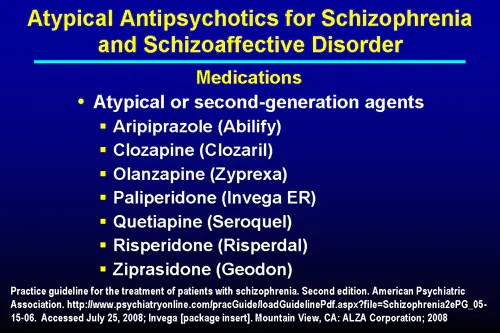 People with schizoaffective disorder have symptoms of two different mental health conditions. Some people might get misdiagnosed with schizophrenia. Others might get misdiagnosed with a mood disorder.
People with schizoaffective disorder have symptoms of two different mental health conditions. Some people might get misdiagnosed with schizophrenia. Others might get misdiagnosed with a mood disorder.
Symptoms and Causes
What causes schizoaffective disorder?
Researchers don’t know the exact cause of schizoaffective disorder. They believe several factors are involved:
- Genetics: Schizoaffective disorder might be hereditary. Parents may pass down the tendency to develop the condition to their children. Schizoaffective disorder can also occur in several members of an extended family.
- Brain chemistry: People with the disorder may have an imbalance of brain chemicals called neurotransmitters. These chemicals help nerve cells in the brain communicate with each other. An imbalance can throw off these connections, leading to symptoms.
- Brain structure: Abnormalities in the size or composition of different brain regions (such as the hippocampus, thalamus) may be associated with developing schizoaffective disorder.
- Environmental factors: Certain environmental factors may trigger schizoaffective disorder in people who inherited a higher risk. Factors may include highly stressful situations, emotional trauma or certain viral infections.
- Drug use: Using psychoactive drugs, such as marijuana, may lead to the development of schizoaffective disorder.
What are the symptoms of schizoaffective disorder?
Symptoms of schizoaffective disorder vary from one person to the next. They can range from mild to severe.
Someone with schizoaffective disorder experiences psychotic symptoms. They also experience severe mood changes, with symptoms of depression, mania or both. A person with schizoaffective disorder will have psychotic symptoms that occur alone and with mood changes.
Psychotic symptoms:
- Delusions (false beliefs with no basis in reality that the person won’t give up, even if given evidence to the contrary).
- Hallucinations (perceived sensations that aren’t real, such as hearing voices or seeing shadows).
- Inability to tell real from imaginary.
- Disorganized speech (difficulty producing clear and coherent sentences).
- Unclear thinking.
- Odd or unusual behavior.
- Paranoia.
- Lack of emotion in facial expression and speech.
- Poor motivation.
- Slow movements or inability to move.
Depression symptoms:
- Low or sad mood
- Thoughts of death or suicide.
- Feelings of worthlessness or hopelessness.
- Guilt or self-blame.
- Lack of energy and low mood
- Loss of interest in usual activities.
- Poor appetite.
- Changes in sleeping patterns (sleeping a little or a lot).
- Trouble thinking or concentrating.
- Weight loss or gain.
Mania symptoms:
- Agitation.
- Distractibility.
- Increased or rapid talking.
- Increased work, social and sexual activity.
- Inflated self-esteem.
- Not sleeping much.
- Rapid or racing thoughts.
- Self-destructive or dangerous behavior (spending sprees, reckless driving, unsafe sex).
Diagnosis and Tests
How is schizoaffective disorder diagnosed?
If someone is showing symptoms of schizophrenia and a mood disorder, see a healthcare provider. The provider will do a medical history and physical examination. There are no lab tests to diagnose schizoaffective disorder. But the provider may use X-rays and blood tests to rule out other illnesses that may be causing the symptoms.
If there is no physical cause for the symptoms, the provider may refer the person to a psychiatrist or psychologist. These professionals specialize in diagnosing and treating conditions tied to mental and behavioral health.
How does a psychiatrist or psychologist diagnose schizoaffective disorder?
Mental health professionals use specially designed interview and assessment tools to diagnose psychotic disorders. They listen to the person (or a loved one) describe the symptoms. They also watch the person’s speech, movement and behavior.
They listen to the person (or a loved one) describe the symptoms. They also watch the person’s speech, movement and behavior.
Providers figure out if these symptoms and behaviors match a specific disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). The American Psychiatric Association publishes the DSM-5. It’s considered the reference book for mental health conditions.
According to the DSM-5, a person has schizoaffective disorder if they have:
- Periods of uninterrupted mental illness, such as having symptoms of depression or another mood disorder for a long time.
- Episode of mania, major depression or both while also having symptoms of schizophrenia.
- At least two weeks of psychotic symptoms (such as delusions or hallucinations) without mood symptoms.
- No evidence of a substance use disorder or medications that may be causing the symptoms.
Management and Treatment
How is schizoaffective disorder treated?
Treatment for schizoaffective disorder involves medication combined with psychotherapy and skills training.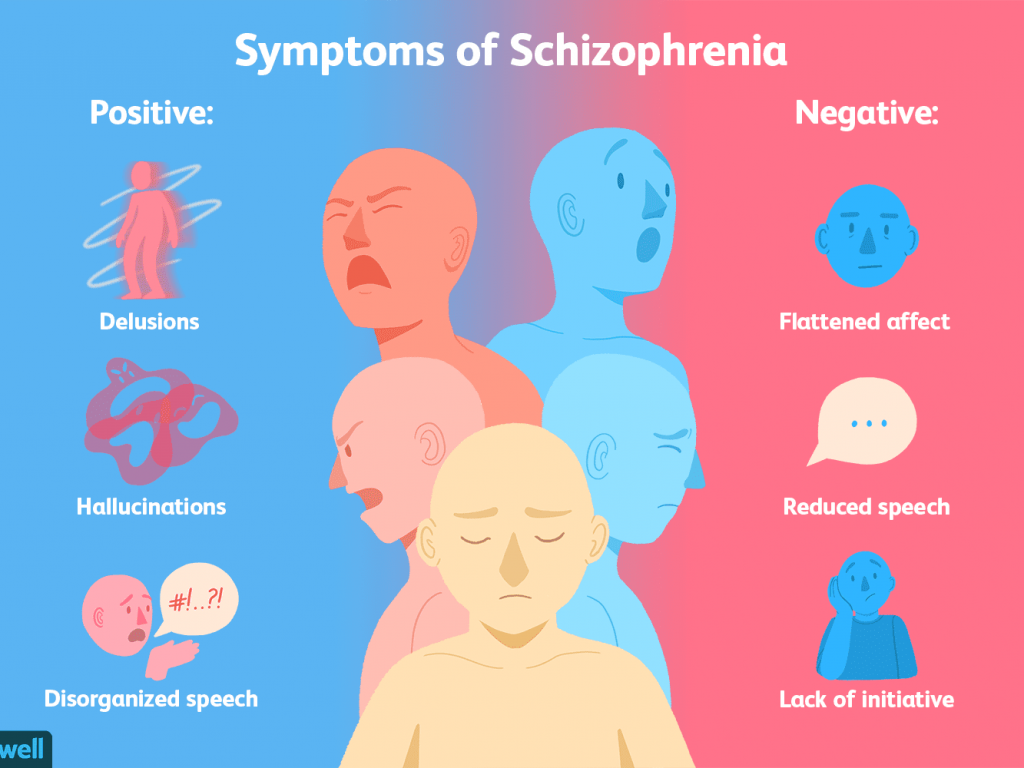 The medication helps stabilize the person’s mood and treats the psychotic symptoms. The therapy and skills training help improve their relationships and coping skills.
The medication helps stabilize the person’s mood and treats the psychotic symptoms. The therapy and skills training help improve their relationships and coping skills.
What medications treat schizoaffective disorder?
The provider will figure out the right medicine based on the type of mood disorder the person has:
- Antipsychotics: This is the primary medicine used to treat the psychotic symptoms that come with schizophrenia — for example, delusions, hallucinations and disordered thinking.
- Antidepressants: An antidepressant or mood stabilizer such as lithium can help treat mood-related symptoms. Sometimes, a person needs both an antidepressant and an antipsychotic.
How does psychotherapy treat schizoaffective disorder?
During therapy, the person talks to a trained mental health professional. The goal of psychotherapy is for the person to:
- Learn about the illness.
- Establish goals.
- Manage everyday problems related to the disorder.
Family therapy can also help. A therapist can help families learn how to cope with the illness and support their loved one. Family therapy helps improve symptoms and quality of life for the person with the disorder.
How does skills training help a person with schizoaffective disorder?
This type of counseling helps a person manage their everyday lives better. It often focuses on:
- Day-to-day activities, such as money and home management.
- Grooming and hygiene.
- Social skills.
- Work.
Does someone with schizoaffective disorder need to be hospitalized?
Most people with this disorder can get outpatient treatment. They go to a clinic or hospital for treatment during the day and then return home. Sometimes, people have severe symptoms, though, or they’re in danger of harming themselves or others. They may need to be hospitalized to stabilize their condition.
Are there side effects of schizoaffective treatment?
The medications may cause side effects.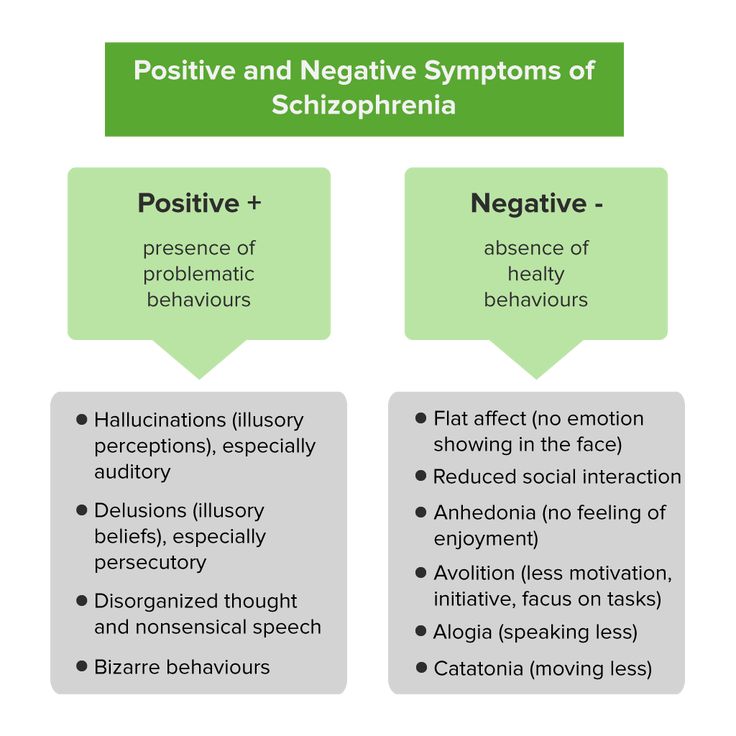
Side effects of lithium:
- Dizziness.
- Hand tremors.
- Loss of appetite.
- Low thyroid hormone.
- Mild diarrhea.
- Nausea.
Side effects of antidepressants (varies depending on the type of antidepressant):
- Constipation or diarrhea.
- Dry mouth.
- Headache.
- Sexual problems (including delayed orgasm or erectile dysfunction).
- Sleepiness or trouble sleeping.
- Sweating.
- Weight gain or loss.
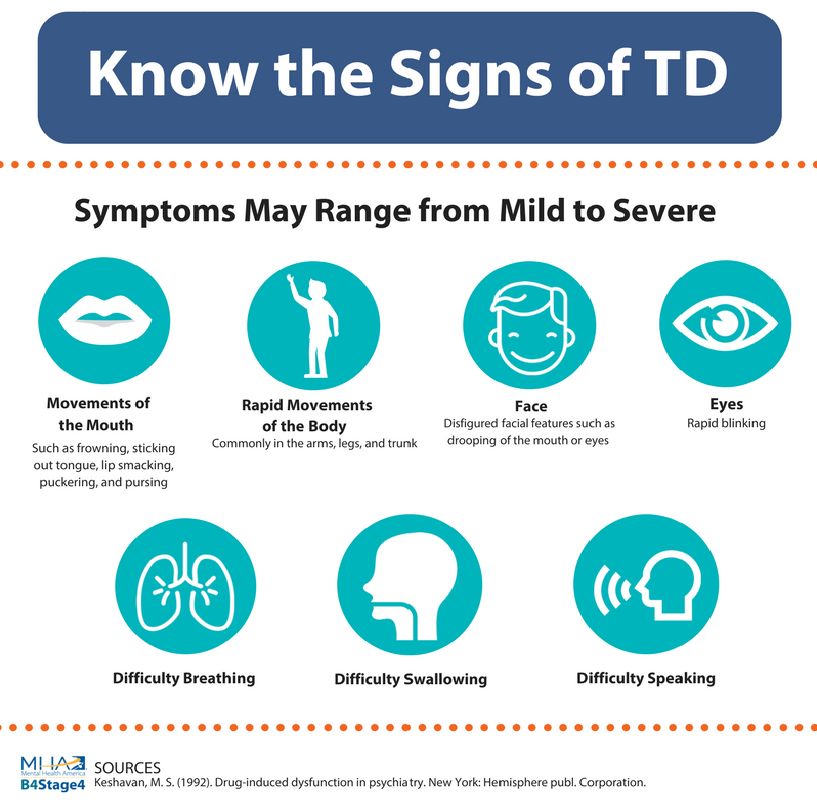
Side effects of antipsychotic medications:
- Drowsiness.
- Increased cholesterol and triglycerides.
- Increased risk of diabetes.
- Slow movements.
- Weight gain.
Prevention
Can schizoaffective disorder be prevented?
There’s no way to prevent schizoaffective disorder. But make sure to get an early diagnosis and treatment if you start noticing symptoms, either in yourself or a loved one. Prompt treatment helps avoid or reduce frequent relapses and hospitalizations. It can also decrease the disruption to the person’s life, family and relationships.
Prompt treatment helps avoid or reduce frequent relapses and hospitalizations. It can also decrease the disruption to the person’s life, family and relationships.
What other conditions might a person with schizoaffective disorder have?
A person with schizoaffective disorder may have other mental health conditions as well, including:
- Anxiety disorder.
- Substance use disorder.
- Attention-deficit hyperactivity disorder (ADHD).
- Post-traumatic stress disorder (PTSD).
Outlook / Prognosis
What’s the outlook for schizoaffective disorder?
There’s no cure for schizoaffective disorder. But treatment can help. The right combination of medication and therapy can:
- Help the person cope with the disorder.
- Improve social functioning.
- Lessen symptoms.
Living With
How should I take care of myself (or a loved one) when it comes to schizoaffective disorder?
Perhaps you’ve noticed signs of schizoaffective disorder in yourself or a loved one.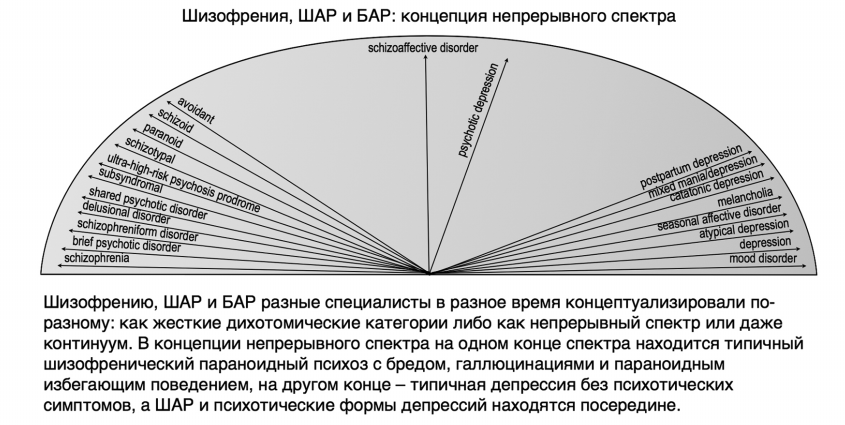 Those symptoms may include prolonged hallucinations, delusions, depression or manic episodes. The first step is to talk to a healthcare provider. Getting diagnosis and treatment as soon as possible helps improve symptoms and promote a good quality of life. Be sure to follow your provider’s treatment instructions:
Those symptoms may include prolonged hallucinations, delusions, depression or manic episodes. The first step is to talk to a healthcare provider. Getting diagnosis and treatment as soon as possible helps improve symptoms and promote a good quality of life. Be sure to follow your provider’s treatment instructions:
- Attend therapy sessions, including individual and family therapy.
- Stay in contact with your provider, who can help manage and adjust your treatments as necessary.
- Take medications as directed. Talk to your provider to help manage side effects from the medications.
- Treat substance use disorders, if necessary.
When should I go to the emergency room?
If you or a loved one seems in danger of harming themselves or others, get help right away. Go to an emergency room, call 911, or call the National Suicide Prevention Lifeline at 800.273.8255. This national network of local crisis centers provides free, confidential emotional support to people in suicidal crisis or emotional distress.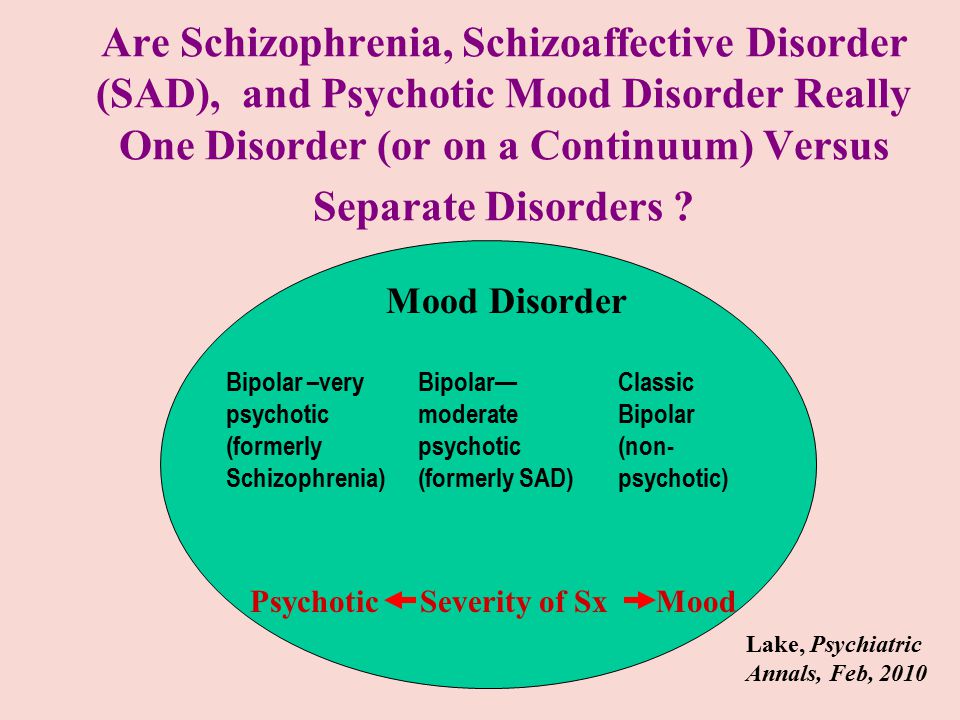 It’s available 24/7.
It’s available 24/7.
What else should I ask my healthcare provider?
If you or a loved one has schizoaffective disorder, ask your provider:
- What medication will help?
- What other therapy can help?
- Will this disorder ever go away?
- How long will treatment continue?
- Is there a higher risk for other conditions or disorders?
A note from Cleveland Clinic
Schizoaffective disorder is a serious mental health condition. It has features of both schizophrenia and a mood (affective) disorder. Schizoaffective symptoms may include symptoms of mania, depression and psychosis. It’s important to get treatment as soon as possible. If you notice symptoms of schizoaffective disorder, talk to a healthcare provider. Treatment for schizoaffective disorder includes medication and therapy. While there’s no cure for this disorder, treatment helps improve people’s symptoms and quality of life.
Features of schizoaffective seizures that developed after emotional stress
Until now, there is no consensus on the significance of psychogenic factors in the course and clinical manifestation of schizophrenia spectrum disorders.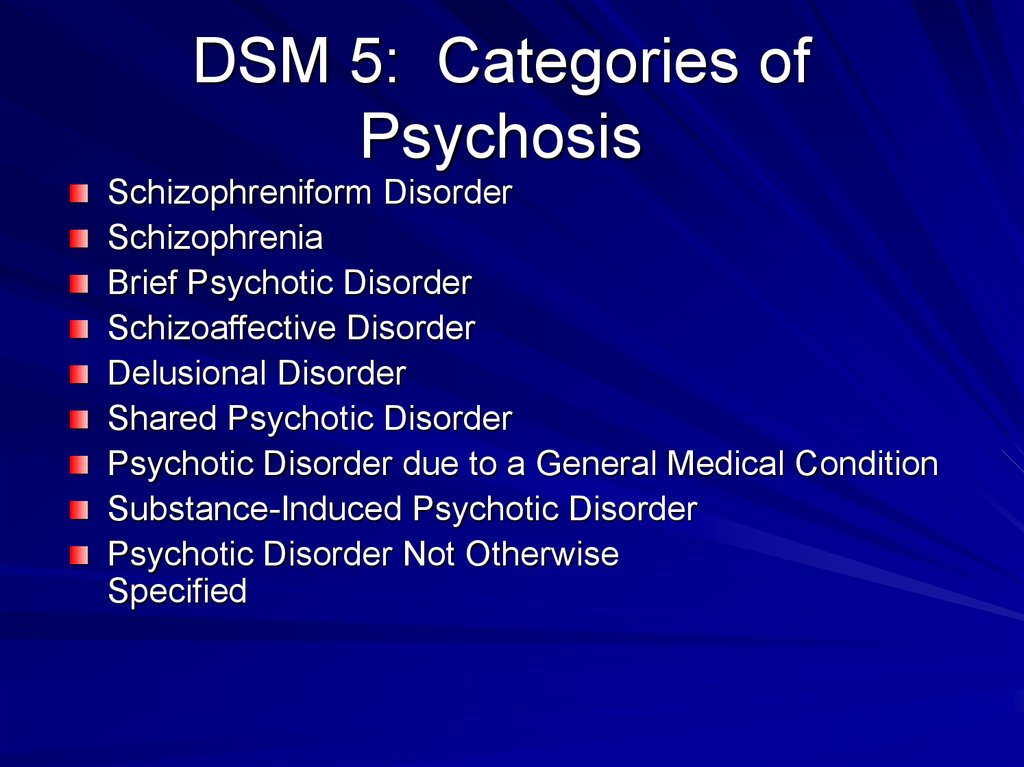 Since the time of E. Kraepelin (1898), this problem has occupied many researchers [2-7, 9, 12, 14, 16, 17].
Since the time of E. Kraepelin (1898), this problem has occupied many researchers [2-7, 9, 12, 14, 16, 17].
A variety of, often completely opposite, opinions were expressed - from the recognition of the direct etiological role of emotional stress in the development of schizophrenia [13, 15, 19] to the complete denial of any connection between mental trauma and this disease [8, 18]. And now there are a large number of works devoted to the relationship and mutual influence of schizophrenia spectrum disorders and psychogenic disorders, sometimes with mutually exclusive conclusions. At the same time, it should be noted that in the study of disorders of the schizophrenic circle in comparison with various variants of psychogeny, there are practically no references to schizoaffective disorder in modern literature. This is due to the fact that schizoaffective disorder was relatively recently singled out as an independent heading in the ICD-10.
The aim of this study was to determine the main clinical characteristics of schizoaffective seizures that developed after emotional stress. It is a continuation of the work that was published by us earlier [1].
It is a continuation of the work that was published by us earlier [1].
Material and methods
The studied sample was formed on the basis of a statement at the time of the examination of clinical signs of schizoaffective disorder and anamnestic information about the presence of one or more intense mental trauma immediately before the onset of psychosis or at the beginning of it.
In the main group of the surveyed there were 57 women and 17 men aged 27-60 (there were 21.6% of patients aged 49 to 60). The disease most often began at the age of 21-40 years.
In accordance with ICD-10, out of 74 patients of the main group, 62.2% were diagnosed with a depressive type of schizoaffective psychosis (F25.1), 25.7% - manic type (F25.0) and 12.1% - mixed type (F25.2).
The comparison group included 51 patients (42 women and 9 men) with autochthonous schizoaffective psychosis. Of these, 35.3% were diagnosed with a depressive type of schizoaffective disorder (F25.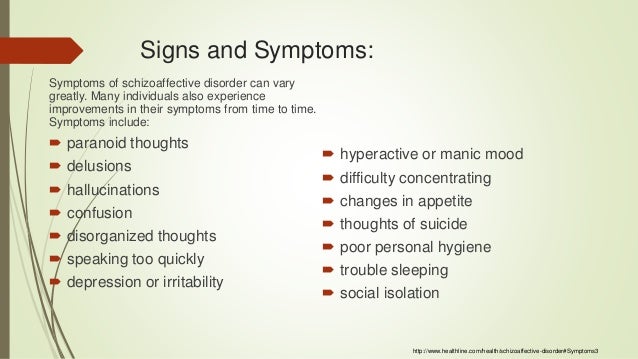 1), 45.1% had a manic type (F25.0), 19.6% mixed type (F25.2).
1), 45.1% had a manic type (F25.0), 19.6% mixed type (F25.2).
We used clinical-psychopathological, follow-up and experimental psychological research methods.
Statistical data processing was carried out by comparing average and relative values using χ 2 -test and Fisher's exact test.
Results and discussion
It is known that schizoaffective disorder occupies an intermediate position between schizophrenia and bipolar affective disorder, combining clinical manifestations of both diseases in various proportions. In accordance with this, schizodominant and affect dominant variants are distinguished [10]. The noted features are manifested by the polymorphism of the clinical picture, the variability of symptoms, the predominance of various psychopathological formations in the same patient at different periods of the development of a schizoaffective attack.
Schizoaffective disorder with previous emotional stress is an even more complex psychopathological formation, since along with typical endogenous mechanisms, psychogenic factors are involved in the formation of an affective-delusional psychotic state.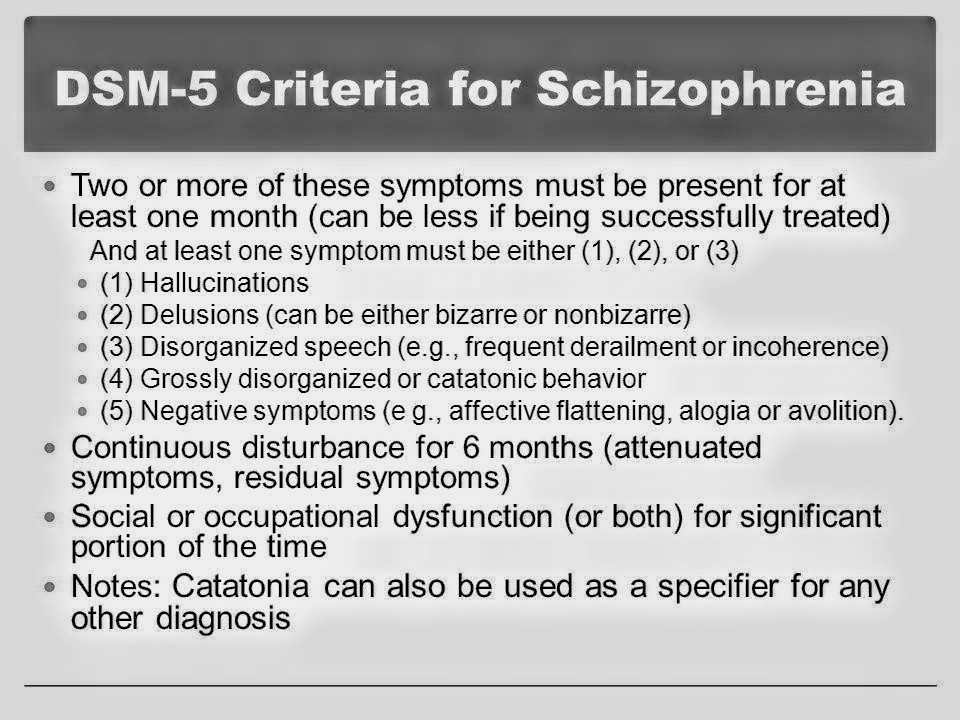 The picture of schizoaffective psychosis, already changeable and heterogeneous in its psychopathological structure, reflects the pathoplastic and pathokinetic influence of emotional stress. Psychogenic "refraction" of the manifestations of such psychosis often leads to diagnostic difficulties. For example, the presence of hysterical symptoms, the “sounding” of the plot of psychic trauma in psychotic experiences, and the “psychologically understandable” ideas of self-accusation suggest the acquired, psychogenic nature of the psychosis under study. At the same time, the presence of schizophrenic spectrum disorders (Kandinsky-Clerambault syndrome, acute sensory delusions of staging, intermetamorphosis, etc.) leaves no doubt about the endogenous origin of the psychotic state. Only a comprehensive analysis of the structure and development of schizoaffective psychosis with previous emotional stress, as well as the period preceding its manifestation, helps to resolve diagnostic difficulties, allowing you to establish certain patterns of pathodynamic relationships between endogenous and psychogenic disorders.
The picture of schizoaffective psychosis, already changeable and heterogeneous in its psychopathological structure, reflects the pathoplastic and pathokinetic influence of emotional stress. Psychogenic "refraction" of the manifestations of such psychosis often leads to diagnostic difficulties. For example, the presence of hysterical symptoms, the “sounding” of the plot of psychic trauma in psychotic experiences, and the “psychologically understandable” ideas of self-accusation suggest the acquired, psychogenic nature of the psychosis under study. At the same time, the presence of schizophrenic spectrum disorders (Kandinsky-Clerambault syndrome, acute sensory delusions of staging, intermetamorphosis, etc.) leaves no doubt about the endogenous origin of the psychotic state. Only a comprehensive analysis of the structure and development of schizoaffective psychosis with previous emotional stress, as well as the period preceding its manifestation, helps to resolve diagnostic difficulties, allowing you to establish certain patterns of pathodynamic relationships between endogenous and psychogenic disorders.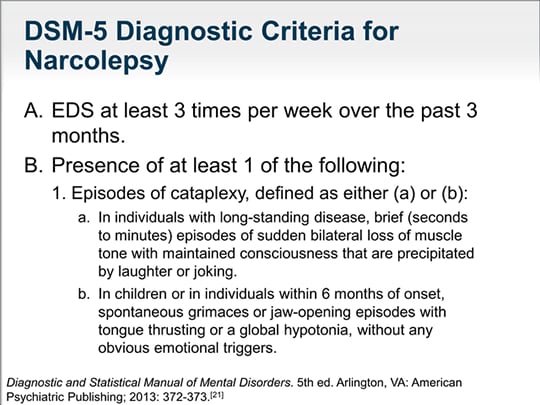
Structure and stages of development of schizoaffective disorder, which developed in connection with the impact of emotional stress . In these cases, various correlations of psychogenic and schizoaffective disorders were observed - from the development of an isolated classical schizoaffective disorder following psychogeny (provoking the effect of psychic trauma) to a complex affective-delusional state, with psychogenic and endogenous components that are difficult to differentiate.
The classic schizoaffective disorder, where the role of emotional stress was limited mainly to provocative influence, was observed in patients with a predominance of manic affect. In this case, the connection of an acute psychotic state with a mental trauma was exclusively temporary, and consisted in the psychogenic decompensation of the existing endogenous disease.
Syndromically complex "endogenous-psychogenic" formations arose due to the close "interlacing" of reactive and schizoaffective symptoms. There was a mutual influence and change, "superimposition" of disorders of different origin, their simultaneous existence. An example of the influence of psychogeny on schizoaffective disorder was its pathoplastic effect in the form of a reflection of the content of a traumatic event in psychotic experiences - affective, delusional and hallucinatory. The pathoplastic effect of psychic trauma in relation to affective disorders consisted in the predominance of depressive affect (the depressogenic effect of psychic trauma) with congruent delusional experiences that independently coexisted with psychotic incongruent disorders. During treatment, the symptoms unrelated to affect disappeared, the clinical picture was determined by psychotic depression with delusions of self-accusation, fully reflecting the content of mental trauma. Patients blamed themselves for the misfortune that had occurred, believed that they deserved severe punishment, public exposure, etc. The duration of depression did not depend on the intensity of treatment, but on the relevance of emotional stress, there was a disappearance of depressive symptoms when the psychotraumatic situation was resolved.
There was a mutual influence and change, "superimposition" of disorders of different origin, their simultaneous existence. An example of the influence of psychogeny on schizoaffective disorder was its pathoplastic effect in the form of a reflection of the content of a traumatic event in psychotic experiences - affective, delusional and hallucinatory. The pathoplastic effect of psychic trauma in relation to affective disorders consisted in the predominance of depressive affect (the depressogenic effect of psychic trauma) with congruent delusional experiences that independently coexisted with psychotic incongruent disorders. During treatment, the symptoms unrelated to affect disappeared, the clinical picture was determined by psychotic depression with delusions of self-accusation, fully reflecting the content of mental trauma. Patients blamed themselves for the misfortune that had occurred, believed that they deserved severe punishment, public exposure, etc. The duration of depression did not depend on the intensity of treatment, but on the relevance of emotional stress, there was a disappearance of depressive symptoms when the psychotraumatic situation was resolved. Depression with delusions of self-blame for a long time determined the mental state of patients, served as the reason for their long stay in the hospital, as well as persistent suicidal behavior with repeated suicidal attempts. In accordance with the traditional criteria for psychogenic illness, these disorders corresponded to reactive depression in the conventional sense. At the same time, depression with congruent delusions had the features of "endogenity" in the form of a typical and inverted circadian rhythm, the severity of all components of the depressive syndrome with ideational and motor retardation, vitality, as well as vegetative manifestations (sympathicotonia) common in endogenous depression. Thus, in the structure of schizoaffective disorder, accompanied by an unresolved traumatic situation, depression of the psychotic level was determined, endogenous in its origin and clinical manifestations and, at the same time, meeting Jaspers' criteria for psychogenic disorders. It is worth emphasizing that we are not talking about a new psychopathological formation or nosological unit, but about a kind of “imposition” of outwardly similar disorders [11], and their mutual aggravation.
Depression with delusions of self-blame for a long time determined the mental state of patients, served as the reason for their long stay in the hospital, as well as persistent suicidal behavior with repeated suicidal attempts. In accordance with the traditional criteria for psychogenic illness, these disorders corresponded to reactive depression in the conventional sense. At the same time, depression with congruent delusions had the features of "endogenity" in the form of a typical and inverted circadian rhythm, the severity of all components of the depressive syndrome with ideational and motor retardation, vitality, as well as vegetative manifestations (sympathicotonia) common in endogenous depression. Thus, in the structure of schizoaffective disorder, accompanied by an unresolved traumatic situation, depression of the psychotic level was determined, endogenous in its origin and clinical manifestations and, at the same time, meeting Jaspers' criteria for psychogenic disorders. It is worth emphasizing that we are not talking about a new psychopathological formation or nosological unit, but about a kind of “imposition” of outwardly similar disorders [11], and their mutual aggravation.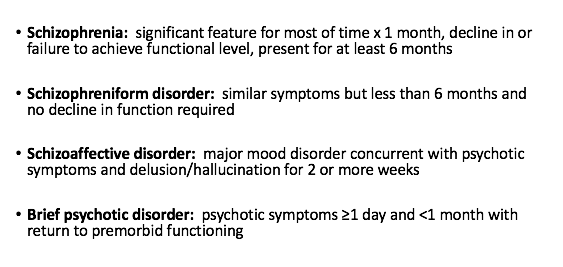
An example of the simultaneous coexistence of psychogenic and schizoaffective components is the development, against the background of fading incongruent affective symptoms, or together with it, hysterical disorders of both psychotic and non-psychotic levels, as well as phobias that are undoubtedly of psychogenic origin. The hysterical symptomatology was of a typical conditionally pleasant, desirable character, allowing the patients to get away from the psychotraumatic situation, or somehow "influence" it due to their manipulative orientation. Obsessive-phobic disorders arose in patients who survived the death of a relative from any severe and incurable somatic disease. For example, cancerophobia and thanatophobia were noted if death occurred as a result of cancer.
A pathoplastic effect on symptoms incongruent to affect was observed in schizodominant variants of schizoaffective disorder, where disorders incongruent to affect in the structure of psychosis were relatively systematized and syndromically formed (Kandinsky-Clerambault syndrome, etc. ). With affect-dominant variants, there was no pathoplastic influence of mental trauma, since acute sensory disorders (delusions of staging, twins, intermetamorphosis, Manichaean delusions, etc.) prevailed in the structure of the attack, which were little subjected to any change even with the most powerful psychogenic impact. The plot of acute sensual delirium was constantly changing, the affect was not constant, the attention of patients switched to the events taking place at the moment. The psychotraumatic situation was reflected in psychotic experiences only during the direct impact on the patient (for example, during a stay at a funeral, memorial service), then gave way to less significant or indifferent events (for example, what is happening in the hospital department). Thus, affect-dominant psychoses in most cases did not reflect the content of mental trauma, they were only in a temporary connection with it, and when separated from the traumatic event, this connection was lost.
). With affect-dominant variants, there was no pathoplastic influence of mental trauma, since acute sensory disorders (delusions of staging, twins, intermetamorphosis, Manichaean delusions, etc.) prevailed in the structure of the attack, which were little subjected to any change even with the most powerful psychogenic impact. The plot of acute sensual delirium was constantly changing, the affect was not constant, the attention of patients switched to the events taking place at the moment. The psychotraumatic situation was reflected in psychotic experiences only during the direct impact on the patient (for example, during a stay at a funeral, memorial service), then gave way to less significant or indifferent events (for example, what is happening in the hospital department). Thus, affect-dominant psychoses in most cases did not reflect the content of mental trauma, they were only in a temporary connection with it, and when separated from the traumatic event, this connection was lost.
Below are 2 examples of outwardly similar schizoaffective psychoses that arose after exposure to a mental trauma of the same content (death of a relative), with the development of attacks of delusional depersonalization, acute paraphrenia and oriented oneiroid at a height.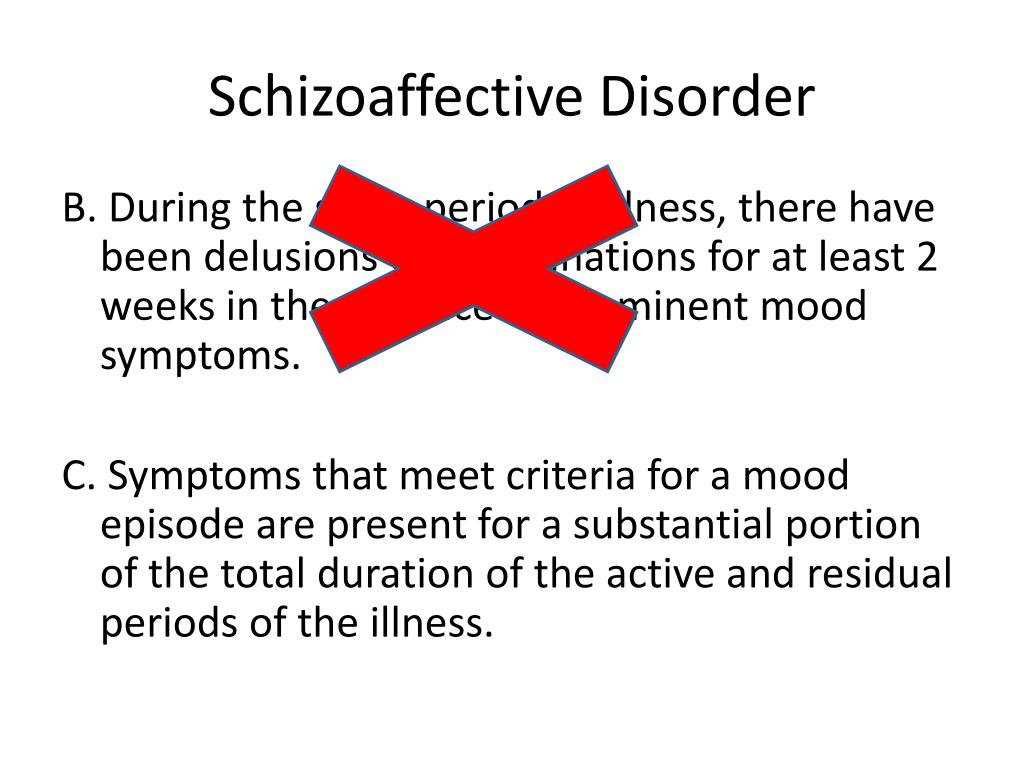 In the first case, the psychotic state of the affective-delusional structure with acute sensory delusions can be attributed to the affect-dominant variant of schizoaffective psychosis, in the second, due to the predominance of the Kandinsky-Clerambault hallucinatory-paranoid syndrome in the clinical picture, to the schizodominant variant.
In the first case, the psychotic state of the affective-delusional structure with acute sensory delusions can be attributed to the affect-dominant variant of schizoaffective psychosis, in the second, due to the predominance of the Kandinsky-Clerambault hallucinatory-paranoid syndrome in the clinical picture, to the schizodominant variant.
Patient R. , 29 years old. She took care of her dying father for 2 months. Within a week of his death, schizoaffective disorder manifested. During her stay in the department for patients with an acute psychotic state, she noticed that everyone around her was playing. For some reason, they played games forgotten from childhood, for example, words or something else. They communicated by hints, eye movements, changes in posture. The patient was included in the proposed game, as she considered it a prerequisite for everyone in the hospital. I saw an unusual transformation of the people around me. In a strange way, the patients, passing by, instantly reincarnated into a completely different person, as a rule, into a patient of the same department.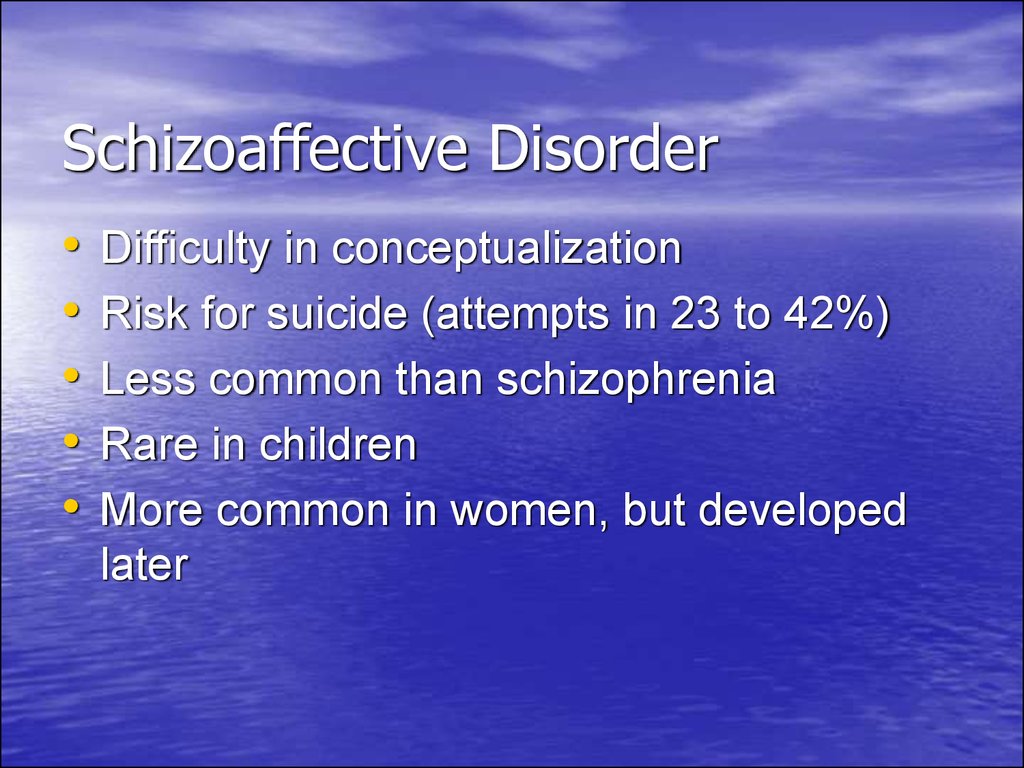 Along with this, some special inner gaze appeared, the patient clearly saw an hourglass inside the body, counting down her last minutes. A metronome worked in the chest, with each passage of the zero mark by the arrow, everything around changed - the situation, some people turned into other people, etc. The rhythm of the metronome was also constantly changing, and therefore the rhythm of life around was not constant. At the same time I saw a cannonball in my chest, a charge similar to a grenade with a lit wick. Gradually, this charge grew, expanded, filled the whole body of the patient from the inside, rested his legs and arms against the surrounding objects - the bed, the back of the chair. In the end, it exploded and shattered into small pieces on the sides. Further, “rising as an ascending stream of cumulus clouds to the top of the pyramid”, I saw flashes, individual faces, heard fragments of phrases. From above she looked at the department, which was the base of the pyramid, saw the sick, doctors and herself lying on the bed with her eyes closed.
Along with this, some special inner gaze appeared, the patient clearly saw an hourglass inside the body, counting down her last minutes. A metronome worked in the chest, with each passage of the zero mark by the arrow, everything around changed - the situation, some people turned into other people, etc. The rhythm of the metronome was also constantly changing, and therefore the rhythm of life around was not constant. At the same time I saw a cannonball in my chest, a charge similar to a grenade with a lit wick. Gradually, this charge grew, expanded, filled the whole body of the patient from the inside, rested his legs and arms against the surrounding objects - the bed, the back of the chair. In the end, it exploded and shattered into small pieces on the sides. Further, “rising as an ascending stream of cumulus clouds to the top of the pyramid”, I saw flashes, individual faces, heard fragments of phrases. From above she looked at the department, which was the base of the pyramid, saw the sick, doctors and herself lying on the bed with her eyes closed.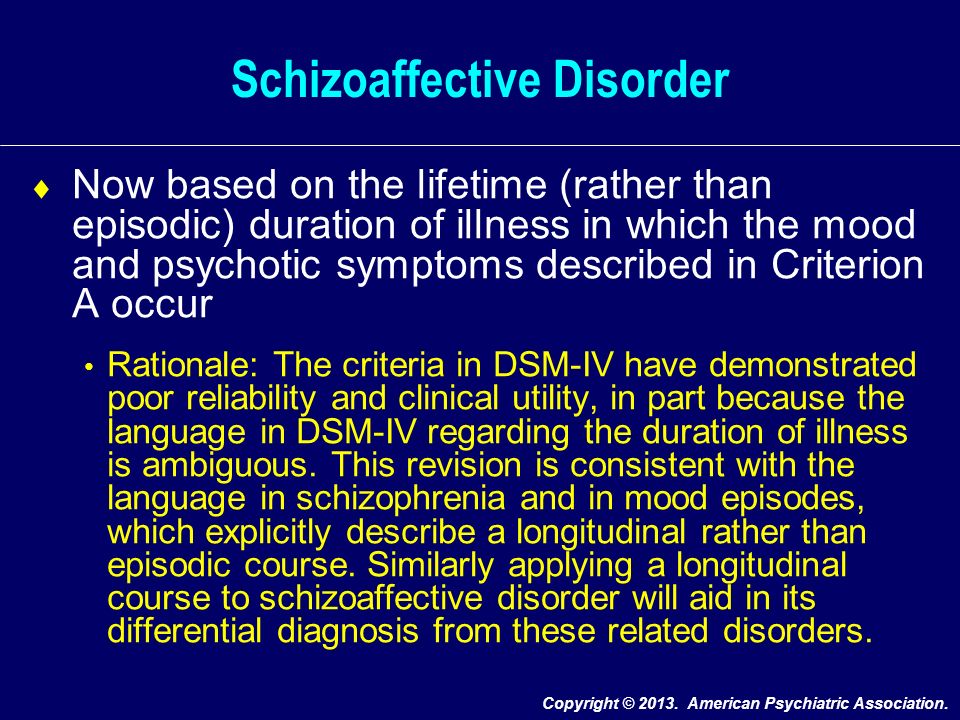 I felt absolutely weightless, I did not feel my body at all. At that moment, she was her own soul, leaving the body and rushing upward. She herself “like a cross turned upside down, like the nose of a concorde aircraft and at the same time like the tip of a blue flame of a candle” hung on the top of the pyramid and watched everything that happened, controlled the performance below with the power of thought and the movement of her fingers. All the people in sight obeyed her every wish.
I felt absolutely weightless, I did not feel my body at all. At that moment, she was her own soul, leaving the body and rushing upward. She herself “like a cross turned upside down, like the nose of a concorde aircraft and at the same time like the tip of a blue flame of a candle” hung on the top of the pyramid and watched everything that happened, controlled the performance below with the power of thought and the movement of her fingers. All the people in sight obeyed her every wish.
In this case, an affect-dominant variant of schizoaffective disorder developed after emotional stress. Mental trauma was preceded by a long mental and physical stress associated with caring for a dying father. It can be assumed that exhaustion and a psychogenic depressed mood created the "ground" for the development of an acute psychotic state with scene-like hallucinatory disorders, oneiroid-oriented, constantly changing picture of delusional disorders without including the plot of a mental trauma in them.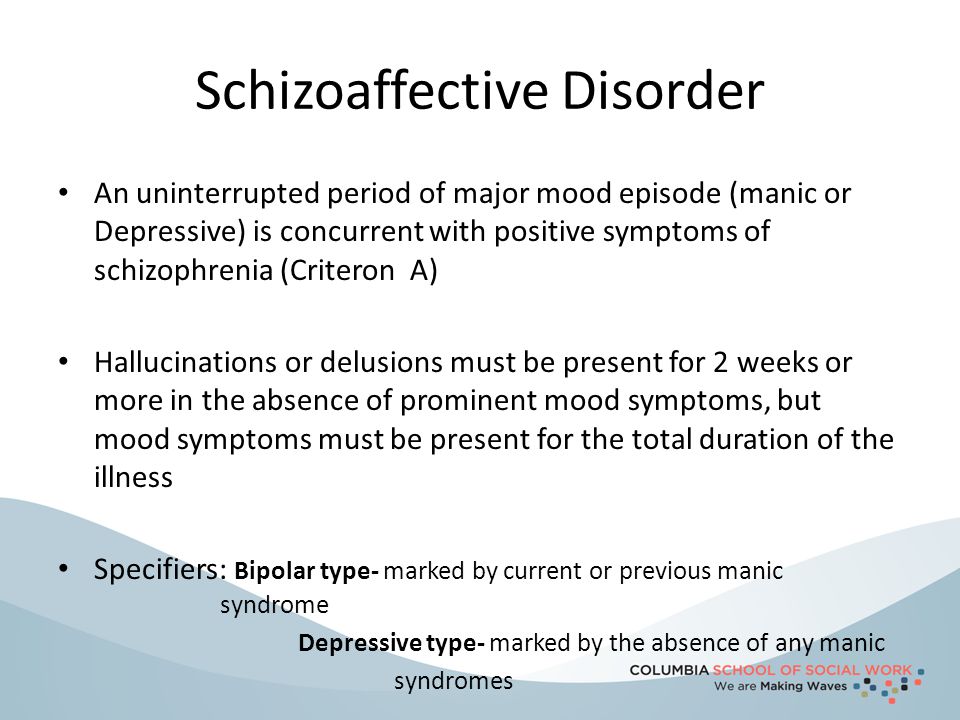
Patient M. , 31 years old. After the news of her brother’s death, she was “in a rather strange state” - she could not speak, she wanted to cry, but there were no tears, she felt a “heavy mental burden”, “grave anguish” in her chest, did not sleep for several days, but could not force herself to get out of bed. A week later, I noticed that someone, with the help of magical energy, takes away the last strength, puts disgusting thoughts into my head. Gradually, the thoughts became loud, turned into the voices of her husband's relatives, who read prayers and tried to separate them with the help of witchcraft. The voice of the deceased brother repeated: "You must die too, go down from heaven to hell." Indeed, looking closely at what was happening, I realized that she died and her soul was transferred to heaven, while the body remained in the same place. The patient, lying in her room, could not get up and look out the window, but this did not prevent her from seeing the terrible events that took place there through her fault.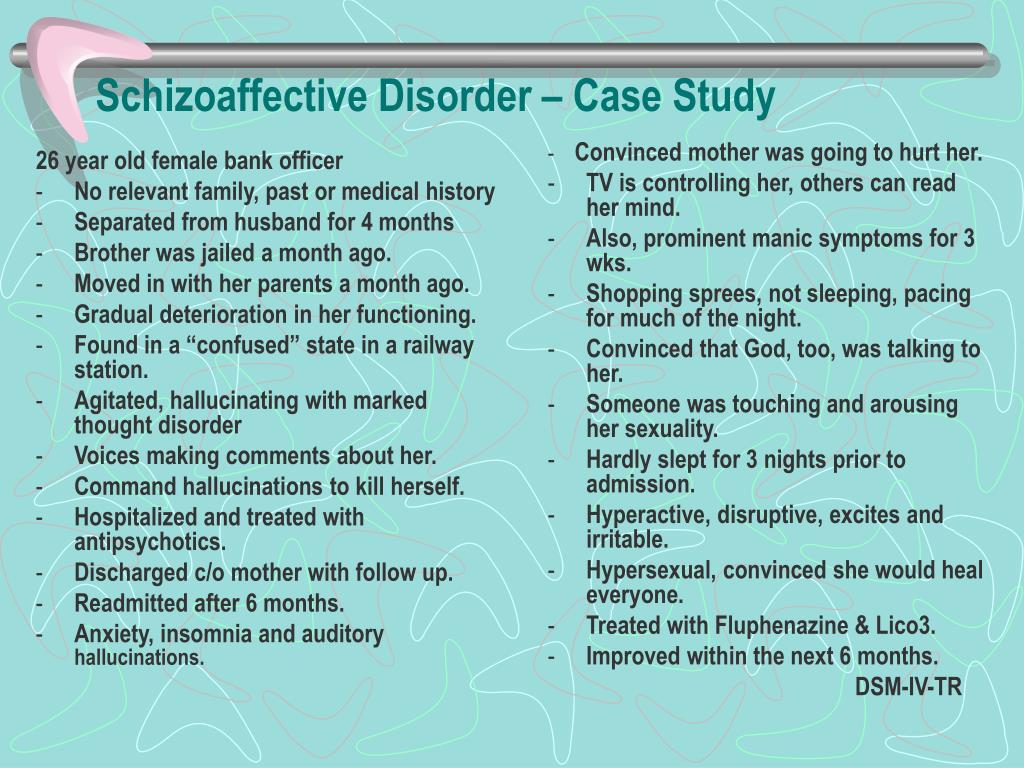 She herself was the foliage of a tree that grew under the windows, from there she clearly watched the street. She lay like a quiet and motionless tree, and did not make a single sound. Only occasionally, with a gust of wind, did a rustling wave run over her leafy fingers. The birds got tangled in its crown and fell dead down. Nearby, a brother hung on a handle in the form of the same leaf. The voices of relatives ordered: "Drop it down, cut off the branch." Unable to disobey the sinister sorcery, the patient tensed the muscles of the back of her head, and, with giant scissors put on her head, as far as she could, cut off her brother from the branch on which he was holding. The brother remained to hold on, and the severed leg fell down, where already lay mountains of decapitated corpses. From time to time, a tram passed through them with a roar and a ringing. The patient understood with horror that all these people died because of her, that her beloved brother must also go to hell. The brother shouted: "What are you doing, don't listen to them.
She herself was the foliage of a tree that grew under the windows, from there she clearly watched the street. She lay like a quiet and motionless tree, and did not make a single sound. Only occasionally, with a gust of wind, did a rustling wave run over her leafy fingers. The birds got tangled in its crown and fell dead down. Nearby, a brother hung on a handle in the form of the same leaf. The voices of relatives ordered: "Drop it down, cut off the branch." Unable to disobey the sinister sorcery, the patient tensed the muscles of the back of her head, and, with giant scissors put on her head, as far as she could, cut off her brother from the branch on which he was holding. The brother remained to hold on, and the severed leg fell down, where already lay mountains of decapitated corpses. From time to time, a tram passed through them with a roar and a ringing. The patient understood with horror that all these people died because of her, that her beloved brother must also go to hell. The brother shouted: "What are you doing, don't listen to them.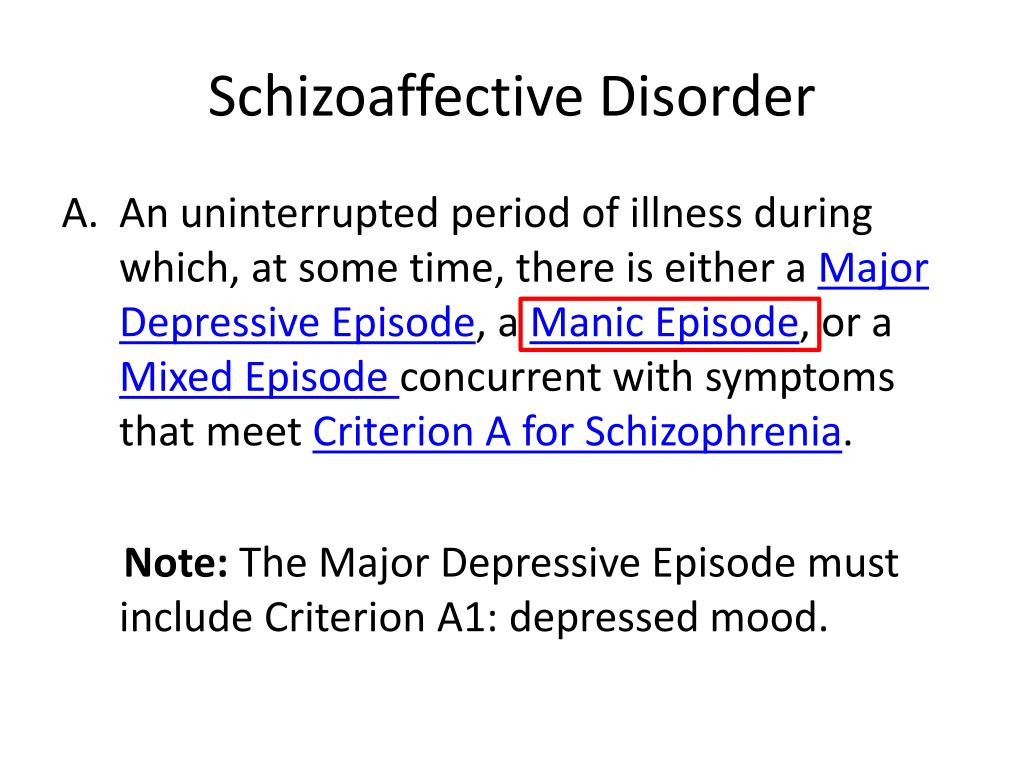 " Another order came, the patient finally cut the branch, and the brother fell down. He said that now he was in hell, and the sick woman should also follow him. Indeed, she saw that her husband had turned into a strange red creature, spewing flames. He only remotely resembled a real husband. Under the windows I saw freshly dug earth, I realized that my husband had died, and under his appearance the devil was in the room. She remembers well how the doctors came for her, she believed that they were taking her lifeless body to the morgue. After hospitalization, she clearly understood that she was in the hospital, for 2 weeks she heard the same terrible voices that scolded the patient and gave "terrifying" orders.
" Another order came, the patient finally cut the branch, and the brother fell down. He said that now he was in hell, and the sick woman should also follow him. Indeed, she saw that her husband had turned into a strange red creature, spewing flames. He only remotely resembled a real husband. Under the windows I saw freshly dug earth, I realized that my husband had died, and under his appearance the devil was in the room. She remembers well how the doctors came for her, she believed that they were taking her lifeless body to the morgue. After hospitalization, she clearly understood that she was in the hospital, for 2 weeks she heard the same terrible voices that scolded the patient and gave "terrifying" orders.
In this observation, after the tragic death of his brother, a schizoaffective disorder of the depressive type developed, referring to the schizodominant variant due to the predominance of the Kandinsky-Clerambault syndrome. At the same time, at the height of the attack, the development of depressive paraphrenia (delusion of evil power), delusional depersonalization and oriented oneiroid was noted.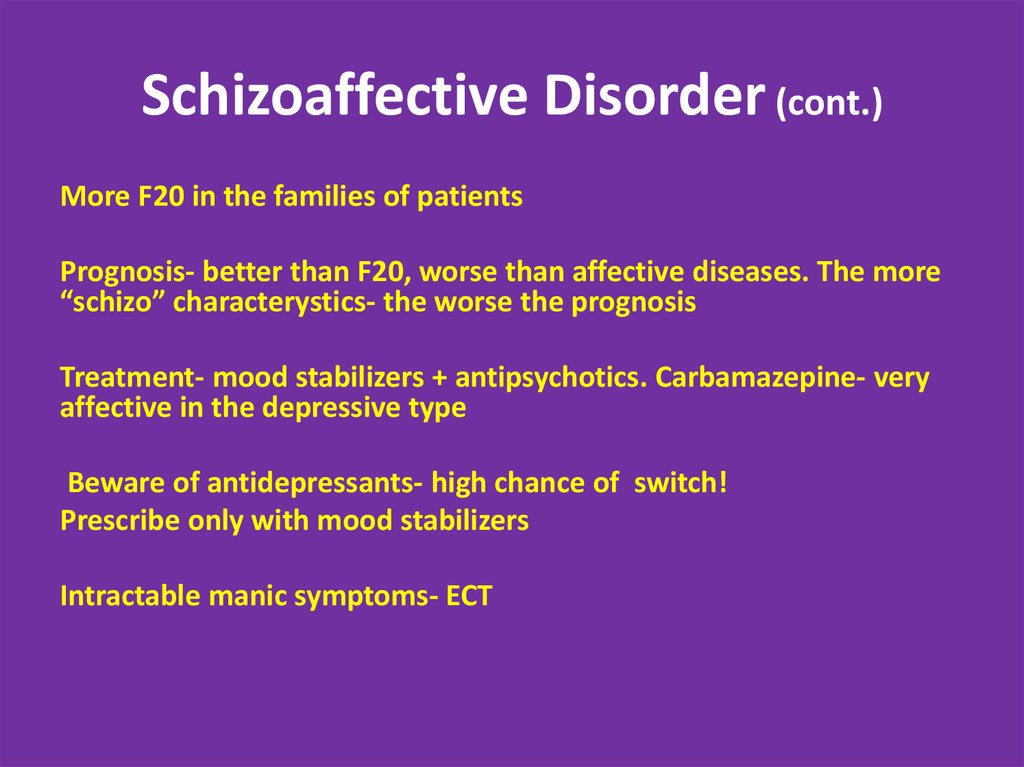 Psychic trauma in this observation had a pathoplastic effect on disorders incongruent to affect, psychotic experiences reflected the content of the experienced psychotraumatic event.
Psychic trauma in this observation had a pathoplastic effect on disorders incongruent to affect, psychotic experiences reflected the content of the experienced psychotraumatic event.
Schizoaffective disorder after emotional stress, despite its complexity and polymorphism, was not a static condition, but changed over time. First, the typical staging of the development of a schizoaffective seizure persisted, where, despite the close relationship with psychogenic disorders, affective, congruent, and affect-incongruent disorders predominated at different stages. Secondly, schizoaffective disorder underwent a change upon repeated exposure to mental trauma due to the pathokinetic effect of emotional stress with deterioration within the existing syndrome, transition to a deeper register of mental pathology, breakage of psychosis with affect inversion, paradoxical improvement in the mental state, development of a schizoaffective seizure of the type "last drop" [1]. It should be noted that changes in the structure of a schizoaffective seizure after emotional stress were noted only within the known limits of the listed reactions and did not go beyond the "endogenous possibilities" of schizoaffective disorder.
Thus, the psychotic state of the affective-delusional structure that developed in connection with emotional stress, depending on the syndromic affiliation (affect-dominant or schizodominant variants), was subjected to the pathoplastic and pathokinetic effects of mental trauma within the "boundaries" of schizoaffective disorder. At the same time, there was a simultaneous coexistence of disorders of endogenous and psychogenic origin, as well as their mutual aggravation. Patients with an unresolved or insoluble traumatic situation require increased attention. In this case, a thorough clinical analysis of the psychotic state with a differentiated therapeutic approach to its schizoaffective and psychogenic components is necessary. Along with the use of neuroleptics, mood stabilizers, antidepressants, it is required to use individual psychotherapeutic techniques aimed at reducing fixation on a traumatic situation and its deactivation, as well as finding ways to overcome resistance to treatment (shock treatment methods, one-time breaks in therapy, the use of maximum tolerated doses, combinations of drugs of various groups and mechanisms of action).
How to diagnose schizoaffective disorder according to ICD-11 or DSM-5?
In this section
Panellists, live at the 29th European Psychiatric Association (EPA) Virtual Congress 2021, discussed in detail whether schizoaffective disorder should now be diagnosed ( ICD-11) instead of diagnosing in dynamics (DSM-5). Professor Peter Falkai argued in favor of this approach, while Professor Ingrid Melle spoke out against it. The discussion was led by Professor of the Department of Psychiatry of the Campania University. Luigi Vanvitelli Silvana Galderisi.
In a survey conducted at the beginning of the debate, 64% of participants indicated that schizoaffective disorder should be diagnosed in the dynamics, while 21% of specialists supported the diagnosis at the moment, and 14% answered that they were not sure.
Diagnosis of schizoaffective disorder should be carried out at the current moment (ICD-11), and not in dynamics (DSM-5) Prof.
 Peter Falkay supported this approach.
Peter Falkay supported this approach. He began his speech by describing the diagnostic criteria for schizoaffective disorder; According to the provisions of the International Classification of Diseases, 11th Revision (ICD-11), a diagnosis can only be established if the symptoms of schizophrenia and a moderate or severe affective episode are observed simultaneously or with an interval of several days 1 . Moreover, the total duration of the symptoms of schizophrenia and the affective episode must be one month 1 .
In contrast, according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), confirmation of schizoaffective disorder requires a continuous period of illness with an apparent affective episode and symptoms of schizophrenia that meet criterion A, which include delusions, hallucinations, and negative symptoms 2 . In the absence of overt affective episodes, positive symptoms must be observed for two or more weeks during the entire duration of the illness, and these symptoms must not be associated with the use of any substances or other diseases 2 .
Professor Falcay noted that the main difference between the diagnostic criteria for schizoaffective disorder according to ICD-11 and DSM-5 is how the episodes are considered - at the same time the relevant symptoms are detected or during the entire duration of the disease 1.2 . This is important because some patients with schizophrenia may have only one episode, while others have multiple episodes with asymptomatic intervals of several decades 2 .
Prof. Falcay went on to highlight the significant differences between the ICD-11 and the DSM-5 in the conceptualization of schizoaffective disorder. According to the ICD-11, diagnostic criteria must be met simultaneously for affective episodes lasting one month and psychotic symptoms occurring at about the same time 1 . This definition focuses on the presence of symptoms during a single episode rather than a lifetime. In contrast, the DSM-5 criteria require a retrospective assessment of the relationship of psychotic and affective symptoms throughout the duration of the disease, and it is much more difficult to restore an accurate clinical picture in this case 2 .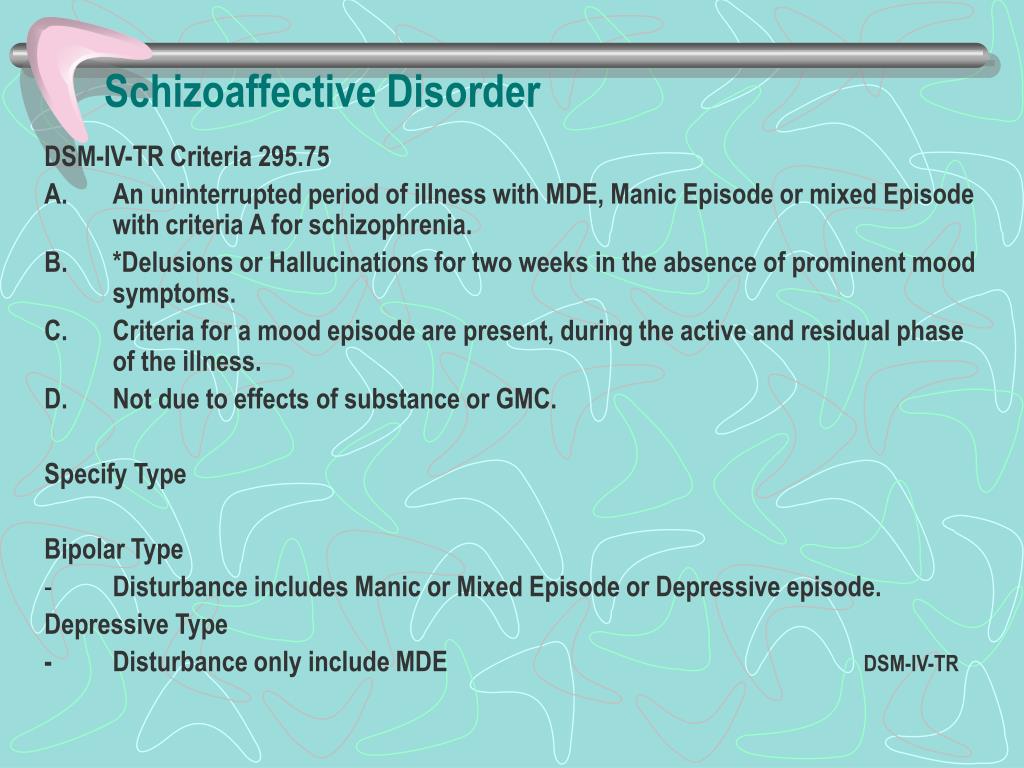
According to Prof. Falkay, these differences in diagnostic approaches partly reflect trade-offs between stability and diagnostic feasibility, which greatly affect reliability. Because the DSM-5 diagnostic criteria involve evaluation of symptoms throughout the duration of the illness, they are relatively stable. However, the high diagnostic reliability of this approach can be called into question. Indeed, Prof. Falcay stressed that the issue of reliability has long been noted in the diagnosis of schizoaffective disorder according to the DSM criteria. On the other hand, the approach proposed in the ICD-11 reflects the changing nature of the clinical picture of many psychotic disorders over time.
The results of studies conducted in clinical practice may support this argument. Professor Falcay noted that they proved the high reliability of the ICD-11 diagnostic criteria for schizoaffective disorder, along with ease of use and clarity. For example, data from a meta-analysis of 42 studies indicated high prospective stability in the diagnosis of schizophrenic and affective spectrum psychoses, as well as the absence of statistically significant differences when using ICD and DSM 9 criteria. 0023 3 .
0023 3 .
In addition, it has become apparent that schizoaffective disorder has long had various definitions, ranging from the position that it is a separate nosological form, to the assertion that schizophrenia and a mood disorder coexist. However, it has been recognized that there are strong clinical reasons for maintaining such a diagnosis, and the DSM-5 criteria have clear limitations, both theoretical and practical, and therefore should be simplified.
Prof. Falcay concluded by stating that he supported the current method of diagnosing schizoaffective disorder as described in ICD-11. This is mainly due to the fact that this method is more applicable in clinical practice than the dynamic assessment recommended in DSM-5. Moreover, considering diagnostic stability for at least 4.5 years 3 , ICD-11 provides a rational way to define and diagnose this elusive disorder.
Diagnosis of schizoaffective disorder should be carried out not at the current moment (ICD-11), but in dynamics (DSM-5)
of Medicine at the University of Oslo defended the opposite view, according to which schizoaffective disorder should be diagnosed not as of the current moment, but in dynamics, as proposed in the DSM-5.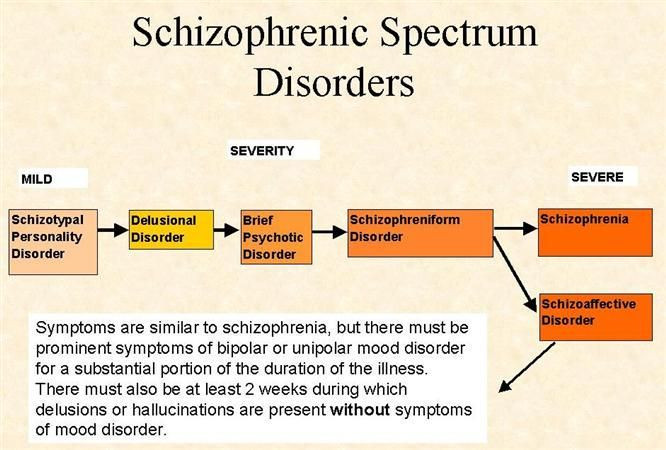
Professor Melle began her presentation by mentioning a series of clinical cases. In 1939, Kasanin first described a number of "rather atypical" cases, the clinical picture of which could indicate both schizophrenia spectrum disorders and affective disorders. This led to a whole series of questions about whether schizoaffective disorder is schizophrenia, manic-depressive psychosis, something in between, or a separate illness.
According to Professor Melle, schizoaffective disorder may include more asymptomatic periods than schizophrenia, and therefore the diagnosis of schizoaffective disorder is considered a viable concept, as it allows better prediction of patient outcomes and increases the likelihood of correct and timely treatment.
However, schizoaffective disorder should not be considered as a separate disorder, but rather as part of a broad spectrum of psychotic and affective disorders that are intermediate between schizophrenia and bipolar disorder. From the time the DSM was first drafted in 1952 to the present, clinical views on schizoaffective disorder have changed, and in reality there was not much in common between the DSM-IV and the ICD-10.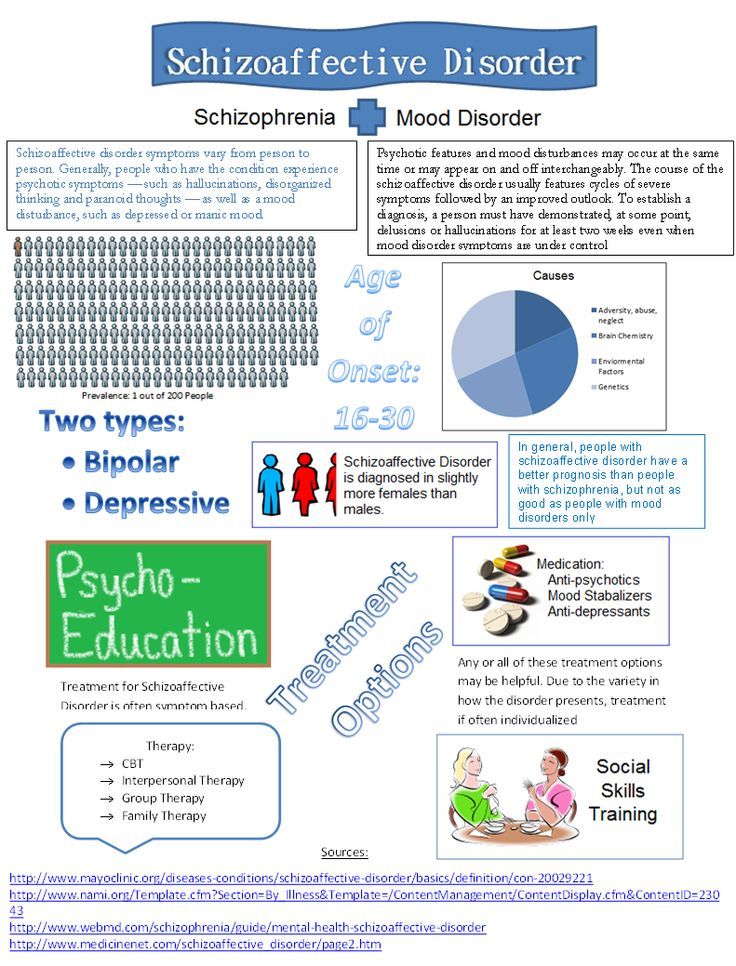
Today, DSM-5 diagnostic criteria require a continuous period of illness during which there is an apparent affective episode and symptoms of schizophrenia that meet criterion A2. However, the ICD-11 defines schizoaffective disorder as having all the symptoms of schizophrenia that occur around the same time as affective episode 9.0023 1 .
Significantly, the DSM-5 recommends that affective symptoms be assessed throughout the duration of a psychotic illness, while the ICD-11 suggests that they be analyzed only at the time of the current episode. Professor Melle further emphasized that the results of empirical studies indicated differences in clinical symptoms between episodes, therefore, within the framework of ICD-11, the diagnosis can change from one episode to another. This significantly affects the reliability of the diagnosis. When using the time course recommended in DSM-5, the entire medical history is considered as a whole, which reduces the risk of making a diagnosis based on an atypical episode.