Feeling hopeless and depressed
Tips for Dealing with Hopelessness
Skip to content
When we experience an overwhelming loss or disruptive life change, or when we are dealing with chronic depression, it is common to feel like the situation is hopeless and will never change for the better. Hopelessness is a feeling of despair or lack of hope that life can feel better than it does. These feelings often lead to a lack of investment or interest in life—and, at its most extreme, can lead to suicidal thoughts. But with the right support and a change in mindset, hopelessness can be overcome.
If you or someone you know is looking for tips of for dealing with hopelessness, text “START” to 741-741 or call 1-800-273-TALK (8255)
Why We Need Hope
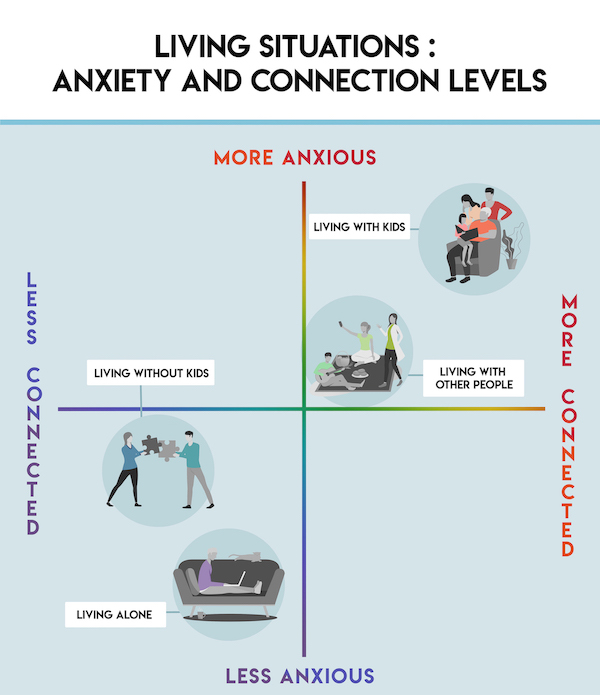
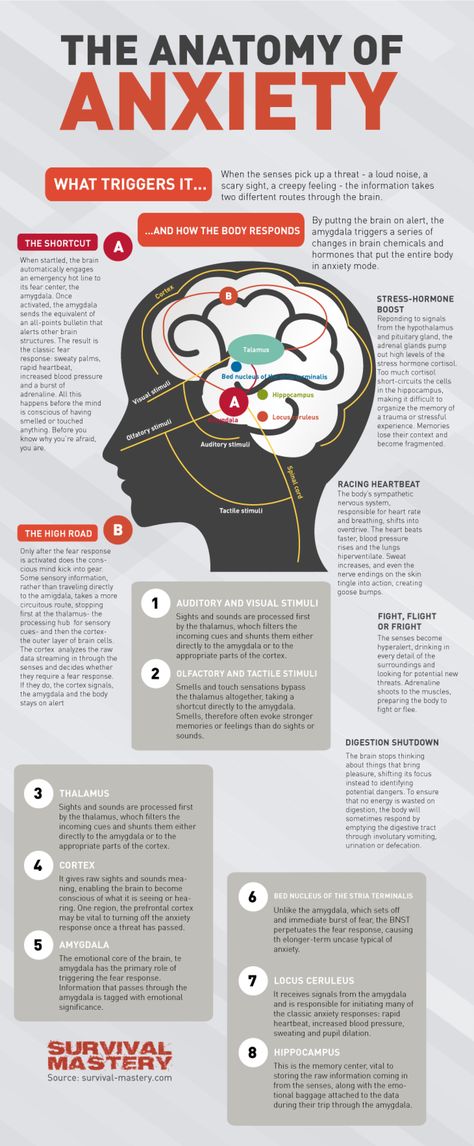
Hopelessness is most common in the wake of a significant loss or major life disruption, such as the death of a loved one, losing a job, confronting a major illness, or facing a financial crisis. It is especially common when someone is already struggling with other mental health challenges. Hopelessness may also be a sign of a broader mental health issue, such as depression or anxiety.
Hopelessness is a concerning feeling because, although we all experience loss, difficult times, or mental health challenges over the course of our lives, hope is a critical part of wellbeing. We need hope because it fosters positive feelings about situations out of our control and can help us keep going when we’re facing challenges. So if you are starting to feel hopeless, it’s important to understand what’s causing those feelings—and what you can do to reconnect with a sense of hope.
How to Deal with Hopelessness
We can’t always avoid situations that can make us feel hopeless, like the death of a loved one, the loss of a job, or financial stress. But we can learn to control how we react to stressors. Here are some helpful ways to deal with feelings of hopelessness when you’re faced with a difficult event or situation:
Reframe Hopeless Thoughts
One common thing that happens when you feel hopeless is catastrophizing, or imagining a worst case scenario. Catastrophizing may cause you to overestimate how bad a situation is or believe that a difficult situation is permanent.
Catastrophizing may cause you to overestimate how bad a situation is or believe that a difficult situation is permanent.
Because this mindset can reinforce feelings of hopelessness, one of the most powerful ways to deal with it is to learn to reframe hopeless thoughts. If you have trouble reframing, look at it this way:
- Accepting that while what you’ve experienced can’t be undone, the acute pain, shame, or grief that so often gives rise to hopelessness does lessen over time. Learning how to be gentle with yourself while it is intense can make a big difference.
- Understanding that, no matter how unfair or devastating this loss or change was, the future holds many more kind, soft, and happy moments than you can see right now —and it is better to be here for that future than not.
- Finding and focusing on the positives in life does not mean that you have to forget or invalidate the struggles you’ve experienced, it means that you do not have to suffer quite so acutely.

For example, let’s say you receive a rejection from the college of your choice. With a “worst case scenario” mindset, you may start to believe that you will never get into a good college and never be successful in your career. If you can open to other ways of framing it, you might allow yourself to imagine other options that also include all of the new experiences, people and opportunities ahead of you. You might, for example, end up taking a gap year and have totally new experiences as a result. It is helpful to keep in mind that there are often many routes to accomplishing your goals.
Practice Positive Coping Strategies
Hopelessness can also leave us feeling numb or empty, and it may be tempting to distract ourselves or find other ways of avoiding the feelings. It’s helpful to acknowledge that this impulse, while understandable, is not likely to help us feel better. Using unhealthy ways of coping, like drugs or alcohol, self-injury, or other risky behavior like reckless driving or unsafe sexual activity, is most likely to deepen the sense of hopelessness that we are hoping to avoid.
Instead, it is most useful to find and practice coping strategies that help you address any underlying feelings while also cultivating healthy coping strategies. Try creative ways of expressing your feelings, like journaling, drawing, singing. Move your body in ways that make you feel good. Practice self-care and positive self-talk, and practice gratitude for the things you have. Remember to show yourself compassion, even if you’re struggling to remain positive.
Lean on Your Support System
It’s natural to need support during a difficult time, but when we feel hopeless it can be hard to accept help or think that help from others will make a difference. If you’re having a hard time, try being honest with the people in your life about how you’re feeling. While hiding how we feel is understandable because we may worry about burdening others, it takes a lot of energy to hide and deprives us of support when we most need it. The people who care about us want to be there for us.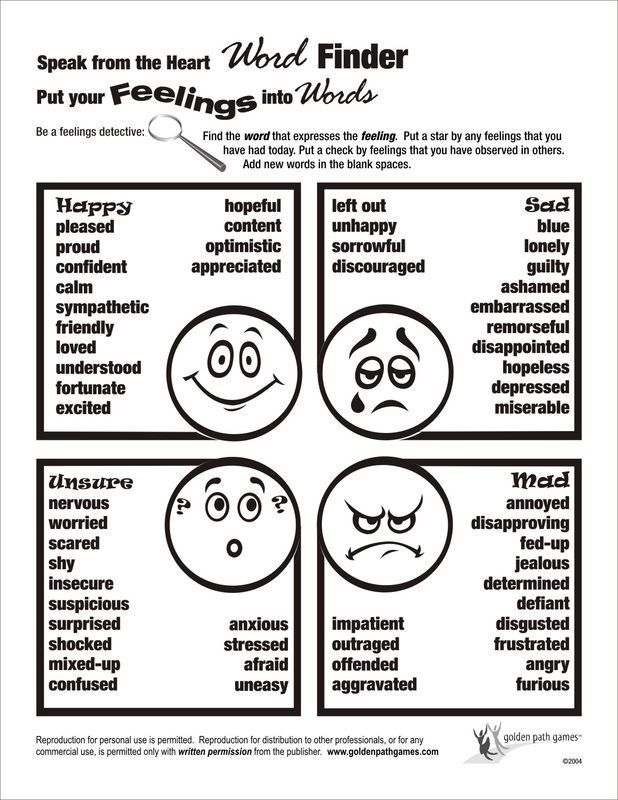 Plus, if we let them support us when we need it, we can inspire them to reach out for support from us and others when they need it.
Plus, if we let them support us when we need it, we can inspire them to reach out for support from us and others when they need it.
When to Seek Help for Feelings of Hopelessness
If you have just experienced a significant loss or life change, feelings of hopelessness may be both natural and temporary. It is helpful to allow yourself time to grieve, practice self-compassion and self-care, and find the support you need.
But sometimes a sense of hopelessness stays longer than is healthy, and without an easy explanation. You may still be experiencing memories, feelings, or other associations brought up by whatever triggered feelings of hopelessness in the first place, or struggling with other mental and emotional challenges. If you or someone you know is struggling with hopelessness, here are some warning signs to watch out for:
- Intense feelings of hopelessness lasts for two weeks or longer
- There is no apparent cause or trigger for the hopelessness
- Feeling fatigue, a lack of motivation, or no longer enjoying things that used to bring joy
- Cycling between feelings of hopelessness or depression and euphoria or feeling “high”
- Sudden changes in sleep patterns, eating habits, or hygiene
- Isolating or withdrawing from friends and family
- Symptoms are negatively impacting relationships, performance at work or school, or everyday life
- Feeling the urge to self-injure or harm others
- Using hopeless or defeated language like “What’s the point?” or “Life doesn’t matter.
 ”
” - Having suicidal thoughts. Even passing suicidal thoughts, such as “it would be better if I died,” should be taken seriously.
- Engaging in reckless or suicidal behavior, like increased drug use or risky sexual activity
If you notice any of these changes in yourself or a loved one, it is likely time to seek help from a trained mental health professional. Sometimes, even short-term professional support can make a really big difference.
How to Help Someone Who Feels Hopeless
If you notice these signs in a friend or a loved one, there are ways to support them and help relieve their hopelessness:
- Approach with open-hearted curiosity. Ask questions in a way that lets your friend know you care. Be open to listening to them, and respect that there may not be things they want to tell you or things you don’t need to know. While you may want to know more, prying may cause the person to withdraw, and will make sharing harder for them down the line.

- Be patient. Understand that talking about their feelings may be difficult, scary, or overwhelming for your friend. Be respectful of what they feel ready to share with you. Show them that you are a safe space for them to share their feelings at their own pace.
- Show empathy. Do not try to rationalize, debate, try to “fix” their situation, make them see the “bright side” of things, or shame them for feeling hopeless. Instead, listen to them with the intention of feeling what they feel, even if briefly, so that can better authentically understand and reflect this back to them. This validates what they’ve experienced and shows concern for their situation.
- Offer your support in ways that are respectful to your friend and manageable for you. Offer to support your friend in ways that won’t harm or exhaust you. Support can range from just being there to listen to more hands-on help, like helping them find professional support.
- Encourage them to seek professional support. There is a limit to what kinds of support friends can provide. Encourage your friend to reach out to a trained mental health professional, like a school counselor or a therapist.
- Share your own experiences. If you have ever struggled with hopelessness, sharing your experience and what brought you hope can make your friend feel less alone.
- Keep inviting them to activities. Sometimes people who feel hopeless will withdraw from friends or activities they enjoy. Inviting them to spend time with you may help them feel less isolated and give them new positive experiences to look forward to.
- Take it seriously if they mention self-injury or suicide. Do not keep this a secret, even if they ask you to. Contact the National Suicide Prevention Lifeline at 800-273-8255. If you believe your friend is in immediate danger, call 9-1-1.

National Suicide Prevention Lifeline
You’re Not Alone
Back to landing page
Search Resource Center
Type your search term below
Get Help Now
If you or someone you know needs to talk to someone right now, text HOME to 741-741 or call 1-800-273-TALK (8255) for a free confidential conversation with a trained counselor 24/7.
If you are experiencing a mental health crisis, text or call 988.
If this is a medical emergency or if there is immediate danger of harm, call 911 and explain that you need support for a mental health crisis.
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.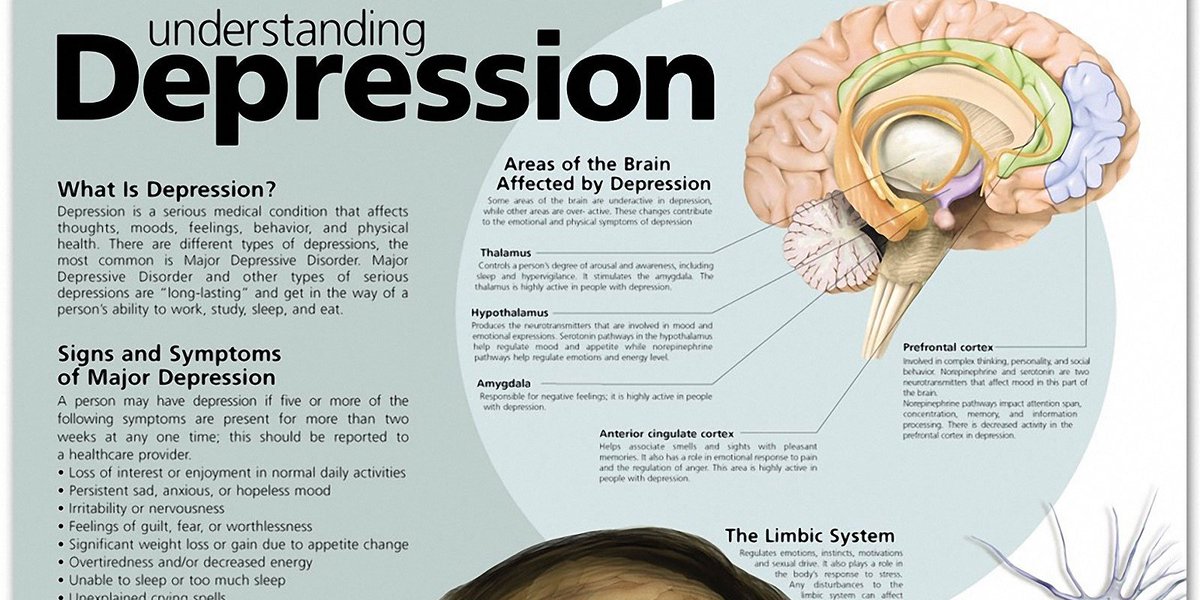
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.
Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
What is a feeling of despair in a person, an explanation of the state of despair
According to studies, despair begins to be felt especially often and sharply when people enter the period of early adulthood - 30-40 years. This harmful feeling causes problems with mental and somatic health.
The state of despair can be seen as a symptom of mental disorders, or it can be a situational emotion that occurs in response to negative life events. An oppressive sense of hopelessness is found in diseases such as depression, anxiety disorders, bipolar disorder, eating disorders, post-traumatic stress disorder, various types of addictions, and more. Despair is not always associated with a psychiatric diagnosis, but, regardless of the cause, this feeling has a devastating effect on life and health. Negative emotions threaten not only the well-being and mental stability of a person. They can also rob you of the motivation you need to complete daily tasks, connect with people, or even seek help.
An oppressive sense of hopelessness is found in diseases such as depression, anxiety disorders, bipolar disorder, eating disorders, post-traumatic stress disorder, various types of addictions, and more. Despair is not always associated with a psychiatric diagnosis, but, regardless of the cause, this feeling has a devastating effect on life and health. Negative emotions threaten not only the well-being and mental stability of a person. They can also rob you of the motivation you need to complete daily tasks, connect with people, or even seek help.
People often experience feelings of despair after tragic events. This is usually the main emotion that arises in response to a sudden traumatic event. In this case, this is a normal and understandable reaction, but it can lead to rash decisions in critical situations, or it can drag on and poison life for a long time. Fortunately, it is in our power to dispel this pernicious feeling. We can learn to cope with any loss, move on, change and continue our lives if we do not ignore the problematic situation and turn for help.
What is despair
Everyone experiences despair at difficult times in their lives. We may despair from time to time about our work, marriage, sex life, finances, world events, and more. But usually this despair dissipates over time, and life goes on. At least until the next crisis.
But sometimes despair does not go away, but, on the contrary, deepens and begins to significantly affect behavior, flowing into a chronic problem. When this feeling reduces the quality of life, prevents you from moving towards goals, dreams and desires, then it becomes pathological or clinical despair.
Despair is characterized by a lack of hope, optimism, and passion for life. This feeling can be described as a mixture of mental anguish, despondency and disappointment, which lead to the loss of the meaning of one's existence. Therefore, in despair, the explanation that life goes on and all problems can be solved may not have the desired effect if there was no preliminary psychotherapeutic preparation.
Despair is a strong emotion that negatively affects how a person perceives himself, other people, personal circumstances and the world in general. Often, hopelessness guides a person's behavior, because of it there is a negative attitude towards the future and the loss of any motivation. To despair means to stop appreciating even those things and events that were once very important. Emotions are often associated with a lack of inspiration, as well as feelings of powerlessness, helplessness, abandonment, oppression, and social isolation.
People who know what despair is can say the following about themselves:
- My situation will never get better
- I have no future
- Nobody and nothing can help me
- I feel like I've given up
- It's too late to change anything
- I have no hope for a bright future
- I will never be happy again
Unfortunately, it is not always possible to contact a specialist immediately after a traumatic event. But if a person feels that time is running out, and the feeling of despair does not go away, then it is necessary to seek professional help. The therapist will not only help you find the cause of despair and eliminate the feeling of hopelessness, but also teach you how to cope with life's difficulties and think rationally in critical situations. This will help to avoid rash actions that will negatively affect life for many years to come. There is no need to visit a psychotherapist whenever there is a feeling of hopelessness. A competent specialist will teach you how to be persistent and independently cope with these situations in the future. Therapy will make it clear that no matter how hopeless things seem now, there is always hope and meaning to move on.
But if a person feels that time is running out, and the feeling of despair does not go away, then it is necessary to seek professional help. The therapist will not only help you find the cause of despair and eliminate the feeling of hopelessness, but also teach you how to cope with life's difficulties and think rationally in critical situations. This will help to avoid rash actions that will negatively affect life for many years to come. There is no need to visit a psychotherapist whenever there is a feeling of hopelessness. A competent specialist will teach you how to be persistent and independently cope with these situations in the future. Therapy will make it clear that no matter how hopeless things seem now, there is always hope and meaning to move on.
Suppressed motivation, lack of interest, negative thoughts about the future, and low self-esteem are all common issues that accompany feelings of desperation and that must be dealt with in the therapist's office.
One of the effective psychotherapeutic approaches that are used for this problem is cognitive therapy. It is aimed at working out the negative thoughts and attitudes of the patient. Because the cognitive approach requires people undergoing treatment to carefully consider the validity of their assumptions, a person who is discouraged may initially be resistant to this approach. However, an experienced specialist removes these psychological barriers, helping the patient to look at life from a different angle.
Numerous studies show that psychotherapy often helps people who have fallen into despair find hope and achieve lasting mental health.
If necessary, drug therapy can be carried out, which includes modern antidepressants, mild sleeping pills and other drugs, the choice of which depends on the situation.
What despair means for children
Despair and depression can occur at any age: not only in adulthood or old age, but also in adolescence or even early childhood. The psyche of children is extremely unstable and vulnerable. As such, children and teens are usually more susceptible to trauma than adults, but with the right support and reassurance, they can also recover faster.
The psyche of children is extremely unstable and vulnerable. As such, children and teens are usually more susceptible to trauma than adults, but with the right support and reassurance, they can also recover faster.
The strong, confusing, and frightening emotions that follow traumatic events undermine a child's sense of security, causing them to feel helpless and vulnerable.
Trauma and despair - what does it mean for children and how to recognize them? Manifestations depend on the situation and the age of the child. Among them:
- Unfounded fears
- Frequent crying and screaming
- A large number of aimless movements or, conversely, reduced motor activity
- Return to behaviors that are characteristic of an earlier age, such as thumb sucking or bedwetting
- Loss of interest in friends, family and former hobbies
- Sleep problems
- Irritability
- Poor school performance
- Complaints of physical ailment
- Feelings of depression, apathy or guilt
Ignoring the problem can lead to irreversible consequences: the child will stop living a full life, may start studying, lose friends and interest in life for many years. Deep despair often degenerates into acts of violence: either against oneself or against others. In the worst cases, mental illness develops, various types of addictions and even suicidal behavior occur.
Deep despair often degenerates into acts of violence: either against oneself or against others. In the worst cases, mental illness develops, various types of addictions and even suicidal behavior occur.
If a child has fallen into despair so much that this feeling for a long time prevents him from functioning at school or at home, this means that it is no longer possible to postpone the appeal to a psychotherapist.
Signs to watch out for parents:
- Despair persists for 6 weeks or more
- Academic and performance problems
- The child often complains of headaches, nausea, abdominal pain or sleep disturbance
- Child finds it increasingly difficult to communicate with friends and family
- Child or adolescent expresses suicidal thoughts
- The child became withdrawn, anxious
- Outbursts of rage and aggression that never happened before
- Bad mood, sadness, tearfulness
The more parents know about the causes, symptoms, and treatment options for their child's depression, the faster their recovery will be. It must be remembered that a child of any age needs not only love, but also respect and trust with at least one of the adult family members. Sometimes the participation of a professional is necessary to normalize intra-family relations. Any major change takes time. But with the support of parents and the help of a competent specialist, anxious thoughts and despair will begin to fade away, and the child's life will return to normal in a few weeks.
It must be remembered that a child of any age needs not only love, but also respect and trust with at least one of the adult family members. Sometimes the participation of a professional is necessary to normalize intra-family relations. Any major change takes time. But with the support of parents and the help of a competent specialist, anxious thoughts and despair will begin to fade away, and the child's life will return to normal in a few weeks.
Manifestation of depression | SKKSPS No. 1
Although at least 350 million people worldwide suffer from depression (World Health Organization estimate), many often do not want to admit that they are sick. Depression is still accompanied by feelings of shame and personal inferiority. A person may view their depression as a just punishment for being "bad" and feel guilty about it.
Depression hits hard on the ability to work. People either suffer silently at work, unable to fully fulfill their duties, or go on sick leave, sometimes for a long time. This causes unnecessary suffering for the patients themselves, a high burden on the shoulders of their loved ones, and a high cost to society due to loss of productivity.
This causes unnecessary suffering for the patients themselves, a high burden on the shoulders of their loved ones, and a high cost to society due to loss of productivity.
Depression is curable, but still about 50% of major depressive conditions remain untreated. We encourage people who think they may have depression to seek help from a psychologist or psychiatrist.
Because of guilt, people suffering from depression often do not want to see a specialist. Nevertheless, effective treatments for depressive disorders are available today.
In general terms, depression is a common mental disorder characterized by sadness, loss of interest or joy, guilt and low self-esteem, sleep or appetite disturbances, lethargy and poor concentration. The disease can become chronic or periodically fade and resume. Depression has a significant impact on a person's ability to cope with the problems of everyday life. In its most severe form, depression can lead to irreversible consequences, to the belief that life is meaningless and the desire to part with it.
Most cases of depression are successfully treated with medication and psychotherapy.
Manifestations of depression
Symptoms of depression can be very different. Depressive states are manifested by a violation of almost all aspects of mental life: mood, memory, will, activity, which is expressed in the appearance of sadness, sadness, mental and muscular retardation, lasting continuously for at least two weeks. Depressed mood in depression can be felt as a slight sadness, sadness, and boundless despair. Often it is accompanied by a feeling of melancholy, unbearable heaviness in the soul, with excruciating pain behind the sternum, a feeling of hopelessness, deep depression, hopelessness, helplessness, despair and self-doubt. At the same time, a person suffering from depression is completely immersed in his gloomy experiences, and external events, even the most joyful ones, do not affect him, do not affect his mood, and sometimes even worsen it.
In the next article, we will talk in more detail about the symptoms of depression and methods of helping those who suffer from this disease.