High blood pressure stress anxiety
Managing Stress to Control High Blood Pressure
The importance of stress management
In today’s fast-paced world filled with increasing demands, stress management is a life skill and a lifesaver. It’s also important to note that while the link between stress and high blood pressure (HBP or hypertension) is still being studied, stress is known to contribute to risk factors like a poor diet and excessive alcohol consumption.
How stress affects your health
In addition to the emotional discomfort we feel when faced with a stressful situation, our bodies react by releasing stress hormones (adrenaline and cortisol) into the blood. These hormones prepare the body for the “fight or flight” response by making the heart beat faster and constricting blood vessels to get more blood to the core of the body instead of the extremities.
Constriction of blood vessels and increase in heart rate does raise blood pressure, but only temporarily — when the stress reaction goes away, blood pressure returns to its pre-stress level. This is called situational stress, and its effects are generally short-lived and disappear when the stressful event is over.
“Fight or flight” is a valuable response when we are faced with an imminent threat that we can handle by confronting or fleeing. However, our modern world contains many stressful events that we can’t handle with those options. Chronic (constant) stress causes our bodies to go into high gear on and off for days or weeks at a time. The links between chronic stress and blood pressure are not clear and are still being studied.
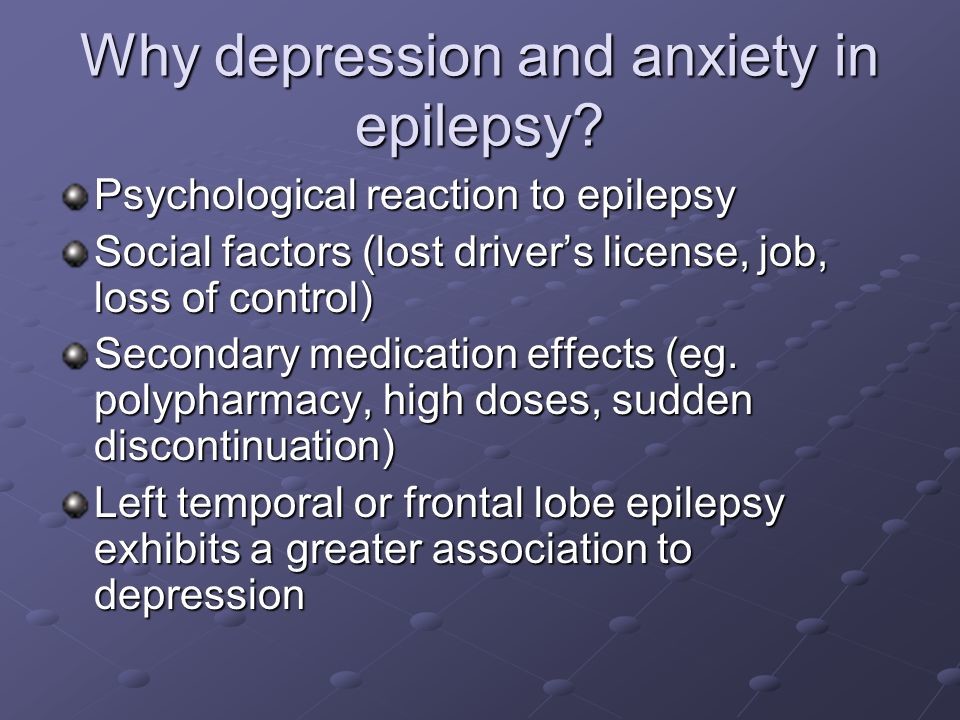
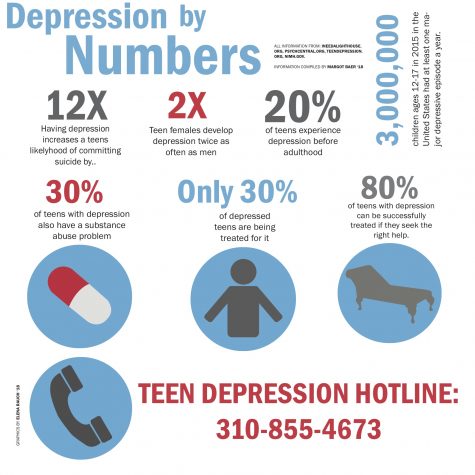
Stress versus anxiety
Stress is a lifestyle factor and, to a certain extent, a fact of life. Each of us also has a certain level of anxiety. On the other hand, chronic anxiety and anxiety disorders are medically diagnosed conditions, which can be impacted by stress.
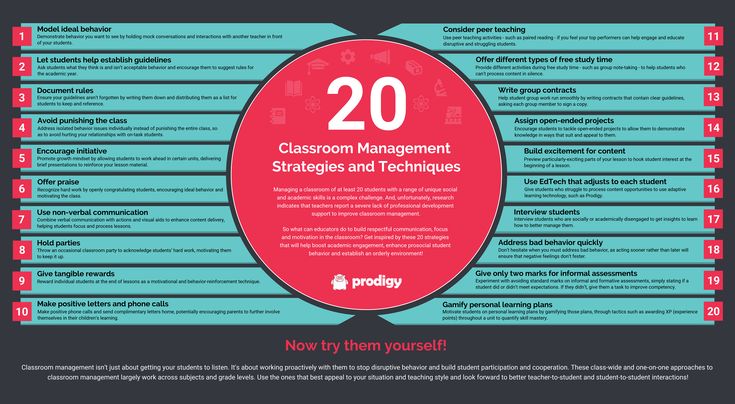
Fight stress with healthy habits
Learn to fight stress by making choices like talking with family and friends and making time for physical activity. These habits not only improve your health — they also rejuvenate your general well-being.
These habits not only improve your health — they also rejuvenate your general well-being.
Reduce stress by changing your expectations
Give yourself enough time to get things done.
Time management works wonders for reducing stress. Don’t try to pack too much into every moment.
Learn to say “no.” Don’t promise too much.
Reduce the amount of tension by having a shorter list of items that must be done. This may require you to reevaluate priorities and make difficult choices, but everyone must learn to live within manageable limits.
Reduce stress by recognizing where you have control
You can’t control all the outside events in your life.
However, you can change how you handle them emotionally and psychologically. Try to learn to accept things you can’t change. You don't have to solve all of life’s problems.
Think about problems under your control and make a plan to solve them.
You could talk to your boss about difficulties at work, talk with your neighbor if his dog bothers you or get help when you have too much to do.
Know your stress triggers.
Think ahead about what may upset you. Some things you can avoid. For example, spend less time with people who bother you or avoid driving in rush-hour traffic.
Reduce stress by taking care of your mood
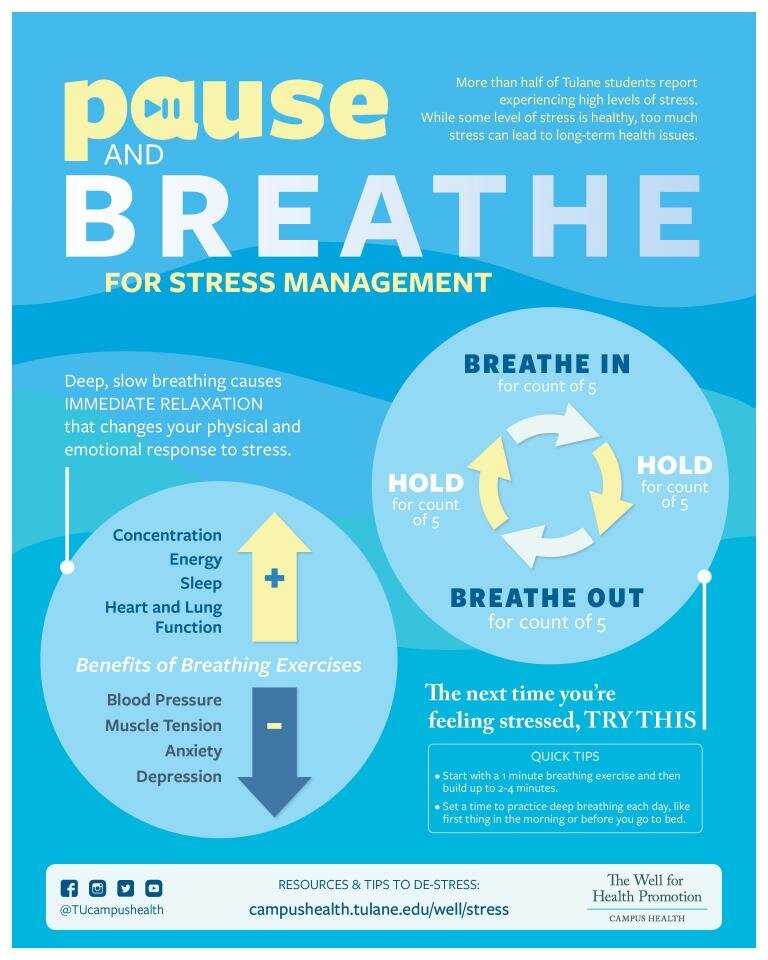
Relaxing is important.
Even if you are busy, take 15 to 20 minutes a day to sit quietly, breathe deeply and think of a peaceful picture.
Spend time developing supportive and nurturing relationships.
We all need supportive and encouraging relationships. Invest yourself in developing relationships that build character and foster growth.
Give yourself the gift of a healthy lifestyle.
Engage in physical activity regularly. Do what you enjoy; walk, swim, ride a bike or jog to get your muscles going. Letting go of the tension in your body will help you feel better.
Limit alcohol, don’t overeat and don’t smoke.
Relaxing for short periods during your workday, at night and on weekends may help lower your blood pressure.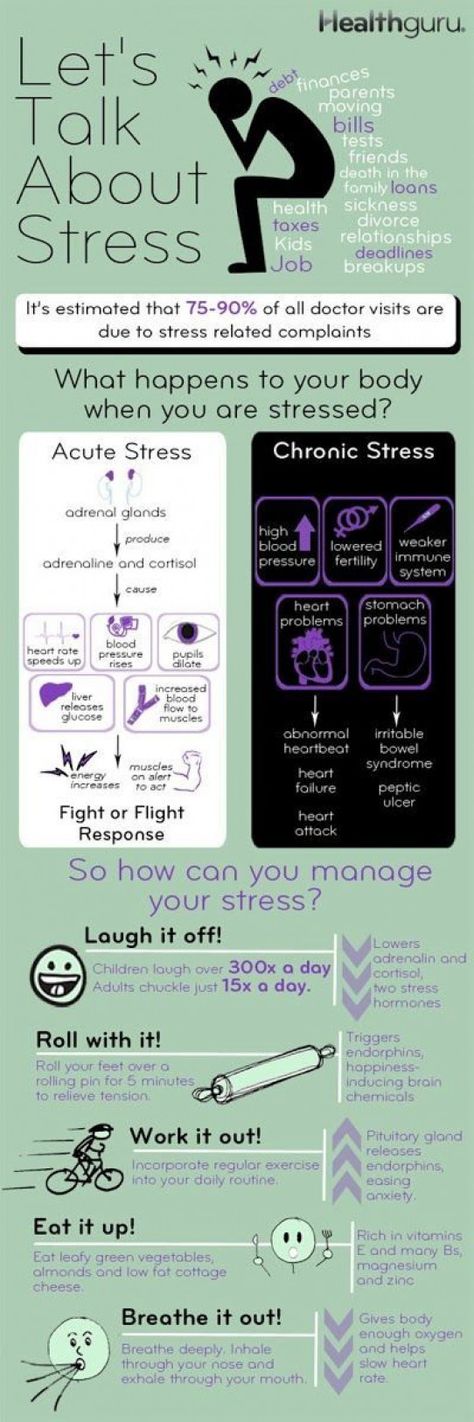 Another great stress-buster is to get regular physical activity.
Another great stress-buster is to get regular physical activity.
Reduce stress by practicing gratitude and joy
Practice gratitude.
Change how you respond to difficult situations, focusing on the positive, not the negative. Expressing gratitude to others can also boost your level of feeling good about life and reduce stressful thoughts.
Know what brings you pleasure and find ways to enjoy the experience.
Perhaps you enjoy volunteer opportunities or cooking your favorite foods. By taking time not only to participate in these activities but to intentionally enjoy them, you can build a satisfying life rather than hurry through your “relaxing activities” at a stressful pace.
Learn more
- Download a fact sheet on managing stress (PDF)
Written by American Heart Association editorial staff and reviewed by science and medicine advisers. See our editorial policies and staff.
Last Reviewed: Oct 31, 2016
Are They Connected? – Cleveland Clinic
You’re under a brutal deadline at work. You’re in the midst of an argument with your spouse. Your dog escapes from your yard, and you’re afraid he’ll be hit by a car as you try desperately to catch him.
You’re in the midst of an argument with your spouse. Your dog escapes from your yard, and you’re afraid he’ll be hit by a car as you try desperately to catch him.
In all of these examples, you may start to feel the physical symptoms of stress and anxiety — your pulse quickens and your mood takes a turn for the worse as your body begins to feel frayed. And common wisdom suggests that stress and anxiety send your blood pressure skyrocketing, too.
But what’s the real relationship between stress, anxiety and blood pressure? Do you need to worry about how short-term stress impacts your body, or is it only prolonged stress that’s problematic?
“Anxiety and stress themselves don’t necessarily elevate blood pressure in the long term,” says preventive cardiologist Luke Laffin, MD, “but they often have an impact on lifestyle factors, which can absolutely contribute to elevations in blood pressure.”
How stress and anxiety impact blood pressure
Dr. Laffin confirms that there is indeed a relationship between stress, anxiety, high blood pressure and the risk of other heart-related health issues — but it might not be what you think.
“While stress and anxiety can definitely cause elevated blood pressure, they don’t necessarily cause sustained elevations in blood pressure,” he says.
To understand this, it’s important to know about the two categories of stress we experience: acute stress and chronic stress. While both can cause your blood pressure to go up, they have different long-term effects.
Acute stress and blood pressure
Acute stress is temporary stress caused by a specific event, like the ones mentioned above. Bouts of anxiety, like having a panic attack, can also cause acute stress that raises your blood pressure.
“If we’re in a stressful situation, the normal physiologic response is to increase blood pressure,” Dr. Laffin explains. “Acute stress can increase your heart rate and rev up your sympathetic nervous system, which, in turn, raises your blood pressure.”
Advertising Policy
In these cases, your symptoms dissipate once your stressor is gone. You complete your deadline, you make up with your spouse, you catch your dog, you come down from your panic attack — and soon, your blood pressure returns to normal, too.
It’s normal to experience changes in blood pressure throughout the day, and your body is typically skilled at managing them. “The body can handle acute changes in blood pressure pretty well,” Dr. Laffin says. “What we’re really worried about is chronically elevated blood pressure.”
Chronic stress and blood pressure
Researchers don’t know as much about the ways chronic stress affects blood pressure, Dr. Laffin notes. But what they do know is that stress can impact your lifestyle habits and increase your risk of health concerns.
“Stress can manifest as unhealthy lifestyle habits that can ultimately impact your cardiovascular risk,” Dr. Laffin explains. When you’re chronically stressed, you may:
- Sleep less or more poorly.
- Not exercise as much.
- Make unhealthy dietary choices.
- Smoke, drink or abuse drugs.
All of these habits can lead to higher blood pressure and increase your risk of stroke or other heart issues.
When does acute stress become chronic stress?
Because we all handle stress in different ways, it can be hard to see the signs of acute stress turning into chronic stress. Stressors that last for weeks on end turn into chronic stressors that need to be addressed for the sake of your heart health (not to mention your mental health!)
Stressors that last for weeks on end turn into chronic stressors that need to be addressed for the sake of your heart health (not to mention your mental health!)
“If a couple of weeks turn into a couple of months, and a couple of months turn into a couple of years, it can be very difficult to turn those patterns around,” Dr. Laffin warns. “It also becomes harder to get rid of some extra belly fat, which ends up rising blood pressure, blood sugar, blood cholesterol and more.”
How can you lower stress, anxiety and blood pressure?
We all have to deal with a certain amount of stress and anxiety, and the way we do so impacts our health.
Advertising Policy
“It really can come down to how someone perceives stress,” Dr. Laffin says. “Two people can be in the exact same situation, but it can be much more stressful to one than the other. Some people just deal better with stress and have healthier coping strategies or support systems.”
He shares some of the ways you can lower your stress levels and get a handle on your anxiety, which can, in turn, lower your blood pressure.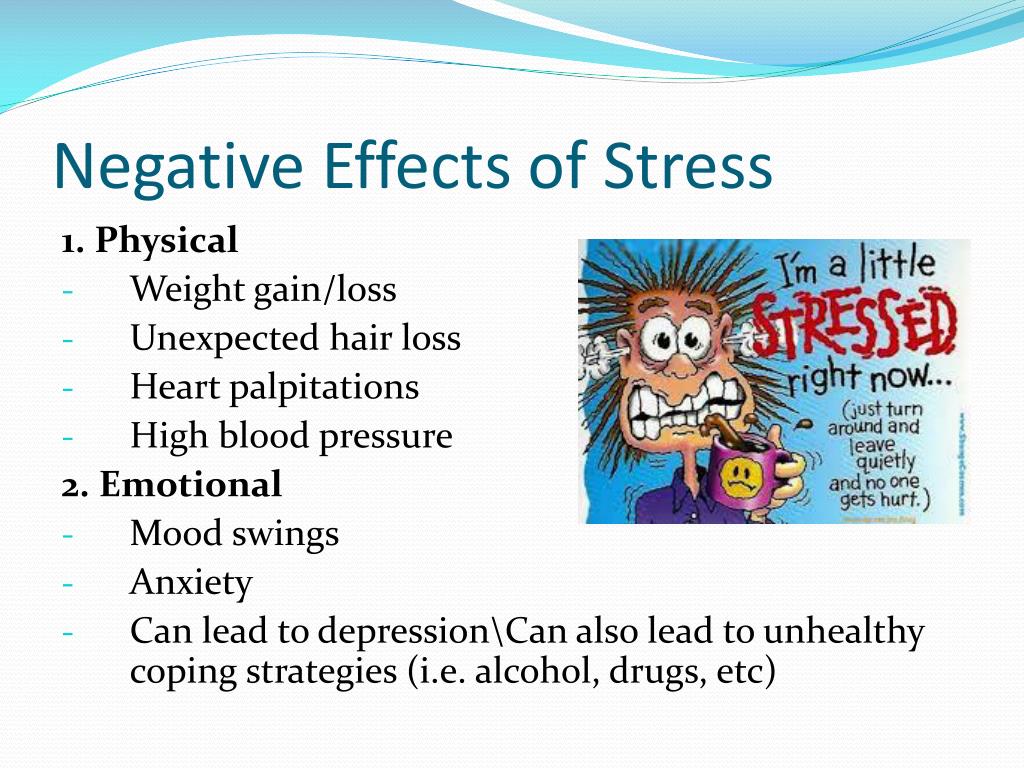
- Work it out: “Regular exercise is a great way to make people feel better, decrease stress levels and help them adapt to stressful situations,” Dr. Laffin says. The positive effects on your heart health are also important for your blood pressure.
- Get enough high-quality sleep: Focus on both the quantity and the quality of your sleep, aiming for six to eight hours of uninterrupted sleep per night. “For stable blood pressures, you need to get about six to eight hours of uninterrupted sleep at night.”
- Remove stressors, when you can: To reduce your stress, it’s critical to try to remove some of the things that cause it. Of course, that’s easier said than done when your main stressor is your job or a family member. In these cases, additional steps, like therapy, may help you deal with your stress.
- Maintain a heart-healthy diet: Foods high in salt and fat can increase your blood pressure even before you add stress and anxiety to the mix.
 To keep blood pressure down, try to scale way back on those foods while adding in heart-healthy, antioxidant-rich foods.
To keep blood pressure down, try to scale way back on those foods while adding in heart-healthy, antioxidant-rich foods. - Try meditation: Various forms of meditation can help you cope with both acute and chronic stress. And one study showed that mindfulness meditation programs may improve anxiety, too.
Medications to manage stress and anxiety
“Managing hypertension (stress) is really 70% lifestyle and 30% medications,” Dr. Laffin says.
To start, expect your doctor to ask questions about your lifestyle and habits, including your sleep. “I always talk to patients about the impact of sleep on heart health, and how stress impacts sleep,” he adds.
You may also need to rely on medication to bring down your anxiety. But just like the ability to handle stress, what medication will work best varies from person to person and requires consultation with your healthcare provider.
“If stress and anxiety are leading to a lot of blood pressure elevation, we can try medications called beta-blockers,” Dr. Laffin says. “They’re not the first line of treatment for blood pressure in most people, but they can be helpful for people with significant stress and anxiety because they decrease your sympathetic nervous system activity and slow down your heart rate in stressful situations.”
Laffin says. “They’re not the first line of treatment for blood pressure in most people, but they can be helpful for people with significant stress and anxiety because they decrease your sympathetic nervous system activity and slow down your heart rate in stressful situations.”
Other medications for bringing down blood pressure include calcium channel blockers and angiotensin receptor blockers. But it’s not all about medication. Remember: There’s no cure-all medication that will ensure a healthy heart, so it’s up to you to embrace a lifestyle that will help keep your ticker in tip-top shape.
To hear more from Dr. Laffin on this topic, listen to the Health Essentials Podcast episode “Combating High Blood Pressure.” New episodes of the Health Essentials Podcast publish every Wednesday.
Pressure and stress / bwell-swiss.ru
- What is stress?
- Pressure increase in response to stress as an adaptation
- Increased blood pressure due to chronic stress or adaptation failure
- How to correctly assess the level of your pressure during stress?
What is stress?
According to the classical definition, stress in medicine is called a non-specific reaction of the body that occurs as a response to the action of various physical factors and strong emotions (stressors) that threaten to disrupt the stable state of the body, and leading to characteristic changes in the nervous and endocrine systems.
It is widely believed that stress is always bad for a person. But in fact, stress performs the most important protective and adaptive function, launches processes that allow you to survive a stressful situation with the least losses, to emerge victorious from it. The only real danger is repetitive, chronic stress [1].
This difference is clearly visible if we consider the effect of stress on blood pressure as an example.
Increasing pressure in response to stress as an adaptation
Consider the classic situation where a person needs to publicly present and then discuss a project with colleagues.
Feeling of excitement, emotional tension grows, the body reacts to this by releasing many hormones. Adrenaline, norepinephrine and cortisol lead to an increase in heart rate, increased pressure, increased blood flow, and an increase in blood glucose levels. Such changes lead to an improvement in the blood supply to the brain, it absorbs an increased amount of glucose and oxygen from the blood, increases concentration, concentration, increases the speed of reaction, which means that a person becomes maximally collected and ready to answer any question [2].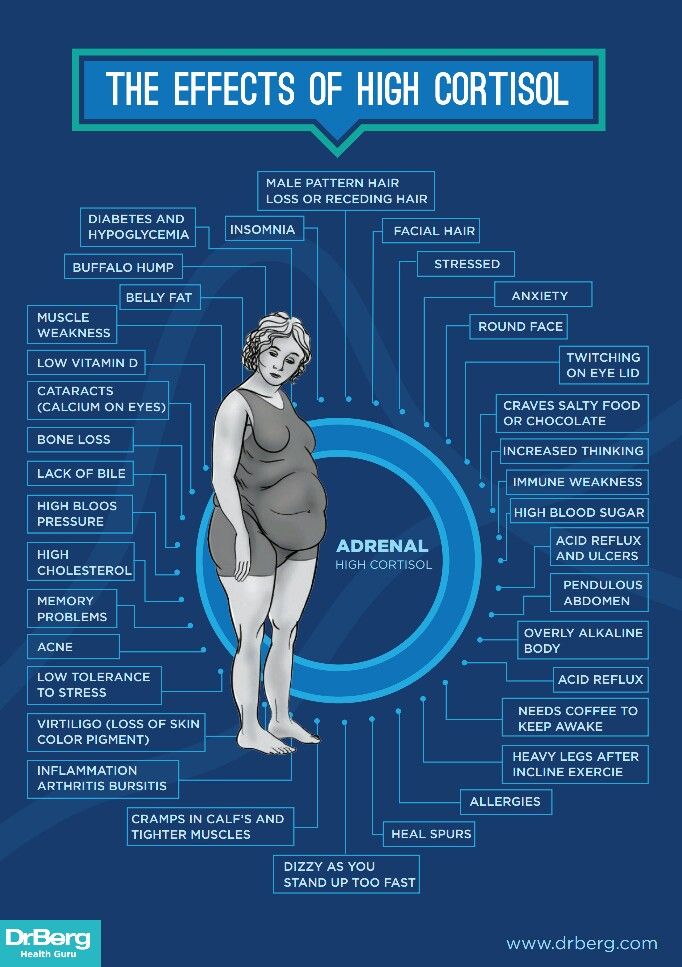 At the same time, in a healthy person, the pressure will be within acceptable limits, not higher than 140/90.
At the same time, in a healthy person, the pressure will be within acceptable limits, not higher than 140/90.
After some time, the discussion of the project ends, the stress factor disappears and the body returns to its original state. In a few hours, the heart rate decreases, blood pressure normalizes [3]. Thus, with the help of stress, the body successfully adapted to the situation, and then returned to a stable state (homeostasis).
Such a short-term increase in pressure can be harmful only if the person suffers from hypertension or other chronic diseases.
Increased blood pressure due to chronic stress or failure of adaptation
Suppose that the same person has a "black" streak in his life. First, the child messed up at school, and had to go to the director, then an icicle fell on the car and broke through the roof, and then the neighbors also flooded the apartment. Because of this, the next day he was late for work, having received a scolding from his superiors. A day later, his previously approved project was curtailed due to lack of funding, and he was transferred to remote work due to the pandemic, depriving him of the opportunity to see his beloved colleagues live.
A day later, his previously approved project was curtailed due to lack of funding, and he was transferred to remote work due to the pandemic, depriving him of the opportunity to see his beloved colleagues live.
Such a series of stressful effects did not allow the body to fully recover, which led to a chronic increase in the level of cortisol, corticosterone and mineralocorticoid hormones in the blood, and these hormones, in turn, contributed to maintaining high blood pressure for a long time [5, 7]. As a result, there was a breakdown in adaptation, the body began to consider constantly elevated pressure as the norm, and baroceptors responsible for regulating pressure and various body systems responsible for homeostasis adapted to this level [4]. A step was taken towards the development of hypertension.
It is these people who often turn to therapists with complaints such as “pressure jumps from nerves” or “constant headache at work”. After all, any additional stress factor will cause a further increase in the already elevated level of blood pressure, leading to the development of unpleasant symptoms and the risk of a hypertensive crisis [9].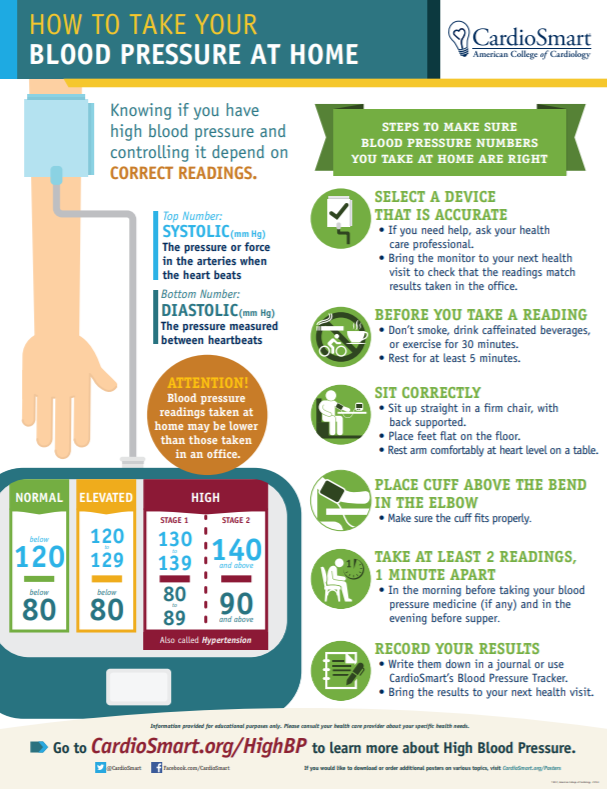
How to correctly assess the level of your pressure during stress?
It is best to measure pressure with an accurate automatic blood pressure monitor in a sitting position, after resting for 10-15 minutes.
During a stressful event and 2-4 hours after it, elevated blood pressure can be recorded [9]. However, if a person does not experience severe discomfort, and the numbers do not exceed 140-150 units of systolic (“upper”) pressure and 100 units of diastolic (“lower”) pressure, then this condition can be attributed to the normal variant during adaptation to stress.
If the pressure remains high for more than 6 hours, symptoms such as headache, dizziness, tinnitus, blurred vision, nausea are observed, it makes sense to call an ambulance or see a doctor. Also, the reason for going to the doctor can be constantly high blood pressure for several days or the appearance of similar symptoms during any emotional experiences [8].
The best way to control your condition is with the help of an observation diary, briefly describing what exactly led to the increase in pressure, to what level it rose and what were the symptoms. Such a diary will greatly help the specialist to choose and prescribe the right treatment. It is most convenient to keep such a diary when the tonometer has a memory function and remembers the results of the last measurements.
Such a diary will greatly help the specialist to choose and prescribe the right treatment. It is most convenient to keep such a diary when the tonometer has a memory function and remembers the results of the last measurements.
1. Bobkov A.I., Reshetnyak D.V., Nikushkin E.V. On compensated and decompensated hormonal and biochemical disorders in clinical stress. Klin. lab. diag. – 2009. No. 9, pp. 42–43
2. Buijs, R. M., & Van Eden, C. G. (2000). The integration of stress by the hypothalamus, amygdala and prefrontal cortex: balance between the autonomic nervous system and the neuroendocrine system. Cognition, Emotion and
3. Autonomic Responses: The Integrative Role of the Prefrontal Cortex and Limbic Structures, 117–132.
4. Yaribeygi, H., Panahi, Y., Sahraei, H., Johnston, T. P., & Sahebkar, A. (2017). The impact of stress on body function: A review.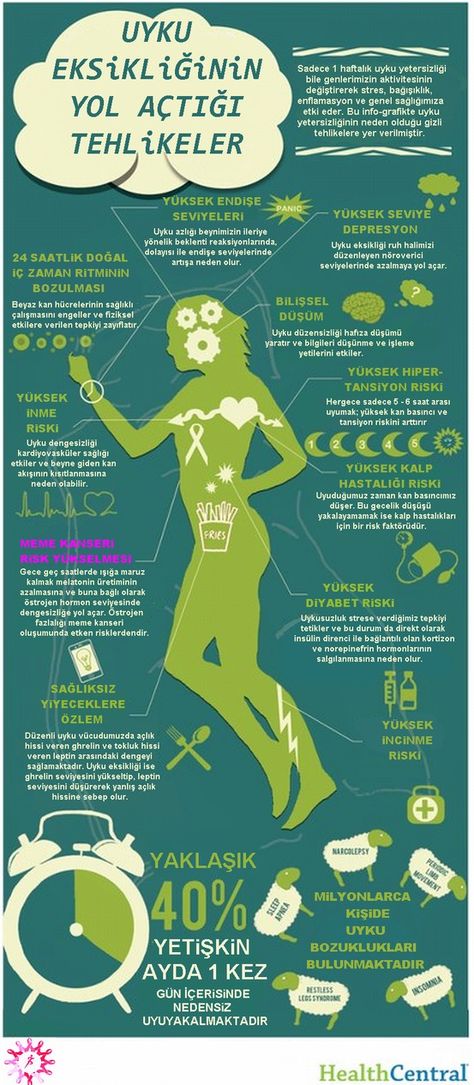 EXCLI journal, 16, 1057–1072.
EXCLI journal, 16, 1057–1072.
5. McEwen B.S. (2006). Protective and damaging effects of stress mediators: central role of the brain. Dialogues in clinical neuroscience, 8(4), 367–381.
6. Ostroumova, O. D., & Kochetkov, A. I. (2018). Worksite hypertension as a model of stress-induced arterial hypertension. Terapevticheskii arkhiv, 90(9), 123–132.
7. Strizhakov, L. A., Babanov, S. A., Lebedeva, M. V., Moiseev, S. V., & Fomin, V. V. (2018). Arterial hypertension at the workplace: risk factors and the population value. Terapevticheskii archiv, 90(9), 138–143.
8. Antonov, E. V., Markel', A. L., & Yakobson, G. S. (2011). Aldosterone and stress-dependent arterial hypertension. Bulletin of experimental biology and medicine, 152(2), 188–191.
9. Akagi, S., Matsubara, H., Nakamura, K., & Ito, H. (2018). Modern treatment to reduce pulmonary arterial pressure in pulmonary arterial hypertension. Journal of cardiology, 72(6), 466–472.
Journal of cardiology, 72(6), 466–472.
10. Heine, H., & Weiss, M. (1987). Life stress and hypertension. European heart journal, 8 Suppl B, 45–55.
Author
Kasabov K.A.,
Lecturer at the First Moscow State Medical University named after I.M. Sechenov, Researcher, Research Institute of Pharmacology named after A.I. V.V.Zakusova.
blood pressurehuman pressure increasedstrong stressreduce pressurestress causeanxiety feelinghuman stress
Share this article with friends
The role of anxiety disorders in hypertension and the possibility of their correction | #03/07
In recent years, more and more evidence has been accumulating that anxiety and some other psychopathological conditions are independent risk factors for the development of arterial hypertension (AH) and should be considered in conjunction with recognized risk factors [7]. These pathologies increase morbidity and mortality from hypertension and coronary heart disease (CHD) [2].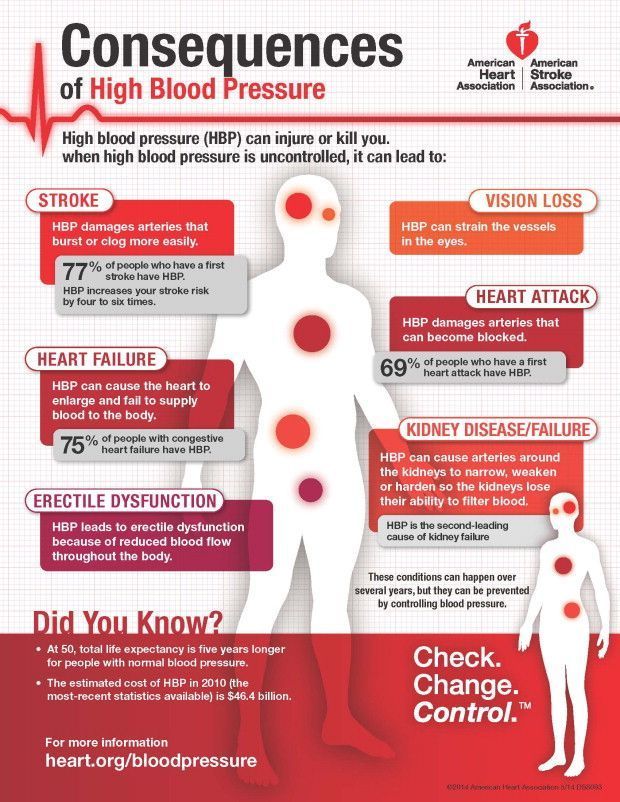 Anxiety disorder should be detected and treated in a timely manner, as it worsens the prognosis of somatic pathology [1]. The importance of anxiety disorder in cardiology is confirmed by the results of a prospective 32-year study conducted in the United States by the Centers for Disease Control and Prevention [7], which showed that with increased anxiety, the probability of fatal myocardial infarction increases by 1.9times, sudden death - 4.5 times. At the same time, social epidemiological studies using objective methods conducted at the State Research Center for Preventive Medicine showed that the population experienced an increase in the level of psychological stress. It was found that about 70% of the country's population lives in conditions of chronic high- and medium-level psychosocial stress [3].
Anxiety disorder should be detected and treated in a timely manner, as it worsens the prognosis of somatic pathology [1]. The importance of anxiety disorder in cardiology is confirmed by the results of a prospective 32-year study conducted in the United States by the Centers for Disease Control and Prevention [7], which showed that with increased anxiety, the probability of fatal myocardial infarction increases by 1.9times, sudden death - 4.5 times. At the same time, social epidemiological studies using objective methods conducted at the State Research Center for Preventive Medicine showed that the population experienced an increase in the level of psychological stress. It was found that about 70% of the country's population lives in conditions of chronic high- and medium-level psychosocial stress [3].
In this regard, special attention is paid to the study of the role of anxiety in the development of hypertension, one of the main risk factors for coronary artery disease. It is known that hypertension is one of the most common cardiovascular diseases affecting, in particular, 25–35% of the Russian population.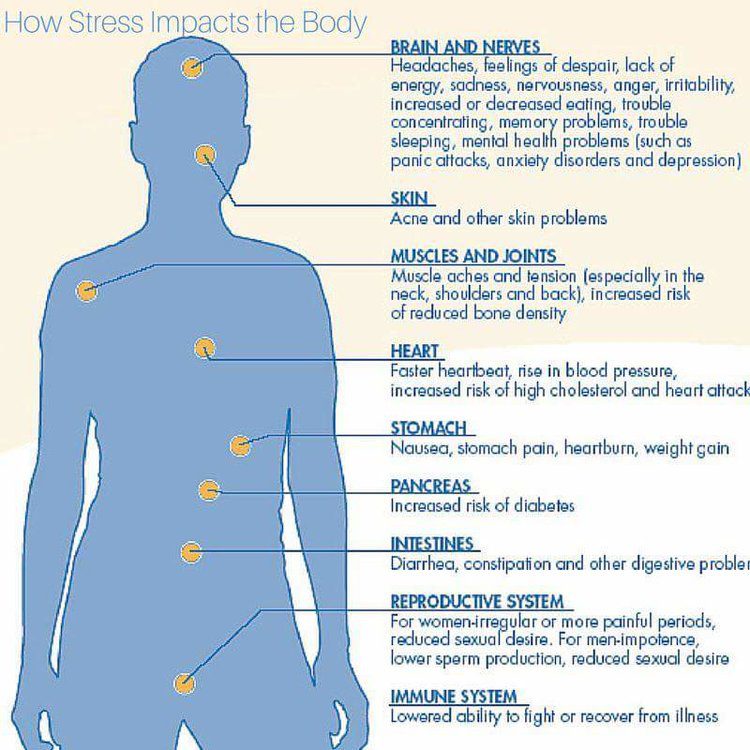 Assumptions that affective disorders, most often anxiety and depression, occupy an important place in the development and course of hypertension, were expressed at the beginning of the last century. Currently, work on the study of the relationship between hypertension and affective disorders is carried out in two directions.
Assumptions that affective disorders, most often anxiety and depression, occupy an important place in the development and course of hypertension, were expressed at the beginning of the last century. Currently, work on the study of the relationship between hypertension and affective disorders is carried out in two directions.
On the one hand, the results of large studies have been published demonstrating the relationship between symptoms of anxiety or depression and the development of hypertension, on the other hand, hypertension is considered as a psychosomatic disease, in the treatment of which psychotropic drugs play a very important role [4].
According to the literature, the prevalence of neurotic and somatoform disorders with anxiety symptoms in patients with hypertension can reach 51.3% [2, 5]. However, the number of studies is limited, and there are no clear recommendations for the management of these patients. It is known that comorbid anxiety-depressive disorders, like hypertension, in themselves lead to a significant decrease in working capacity, while they aggravate the course of a somatic disease, contribute to the formation of a hypochondriacal type of internal disease [7].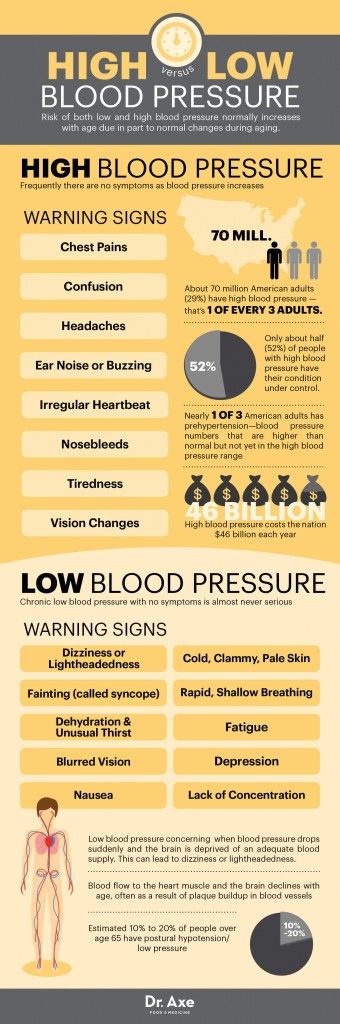 In this regard, it seems very interesting and important to determine the possibility of the effect of complex therapy with antihypertensive drugs and a “daytime” anxiolytic on the course of hypertension in patients with anxiety.
In this regard, it seems very interesting and important to determine the possibility of the effect of complex therapy with antihypertensive drugs and a “daytime” anxiolytic on the course of hypertension in patients with anxiety.
Anxiolytic therapy significantly improves the quality of life of patients with cardiovascular diseases, contributes to their better compensation in the process of somatotropic therapy, and further adaptation to the disease. Tranquilizers are the most adequate, effective and safe drugs for the relief of adaptation disorders in cardiac patients [2, 3]. However, patients often avoid taking benzodiazepines, fearing the development of addiction symptoms, unpleasant side effects in the form of lethargy, muscle weakness, and impaired attention. Elderly patients often fear the development of coordination disorders in them due to the fear of falling, the appearance of instability.
Taking into account the noted problems, in recent years there has been an increasing need for drugs with a tranquilizing effect of the non-benzodiazepine series.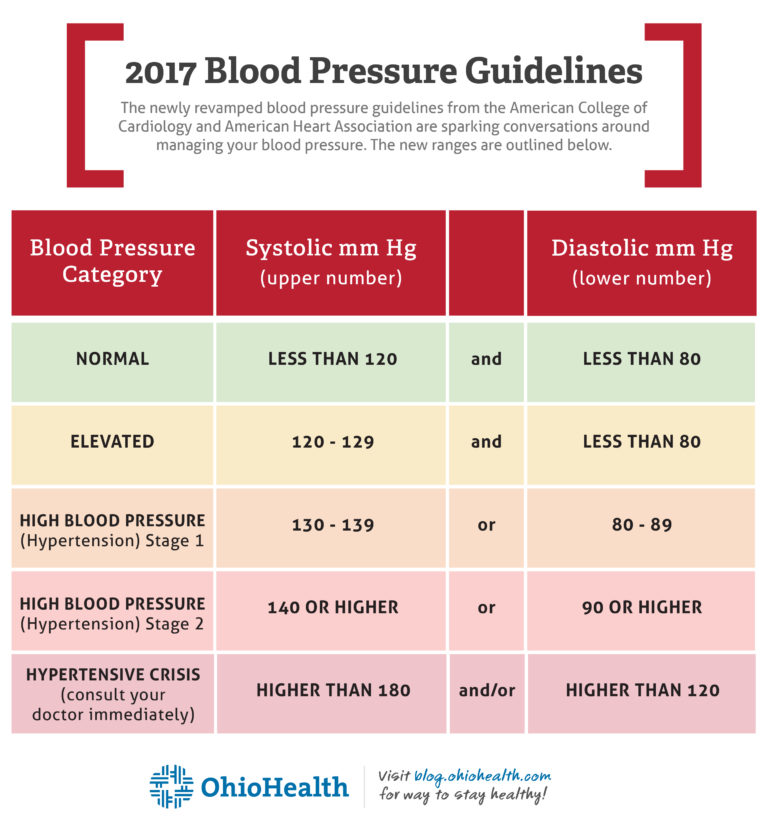 These drugs include Tenoten.
These drugs include Tenoten.
The drug Tenoten is an ultra-low dose (ULD) to the brain-specific protein S100. The mechanisms of action of anti-S100 SMD in anxiety states are probably associated with a modification of the functional activity of the endogenous S100 protein and its ligands. As a result, its GABA-mimetic effect is realized, restoration of GABAergic neurotransmission. The clinical effect in this case is manifested by facilitating falling asleep, reducing behavioral manifestations of anxiety, improving memory, and reducing asthenia.
The aim of the study was to evaluate the efficacy and tolerability of combined treatment with antihypertensive drugs and the anti-anxiety drug Tenoten in patients with hypertension. The duration of the study is 4 weeks.
The study involved 60 patients with hypertension aged 61.41 ± 6.91 years (from 38 to 77 years). Patients were divided randomly into two groups (main and control) of 30 people. There were 18 men and 12 women in the main group, 19 in the comparison group.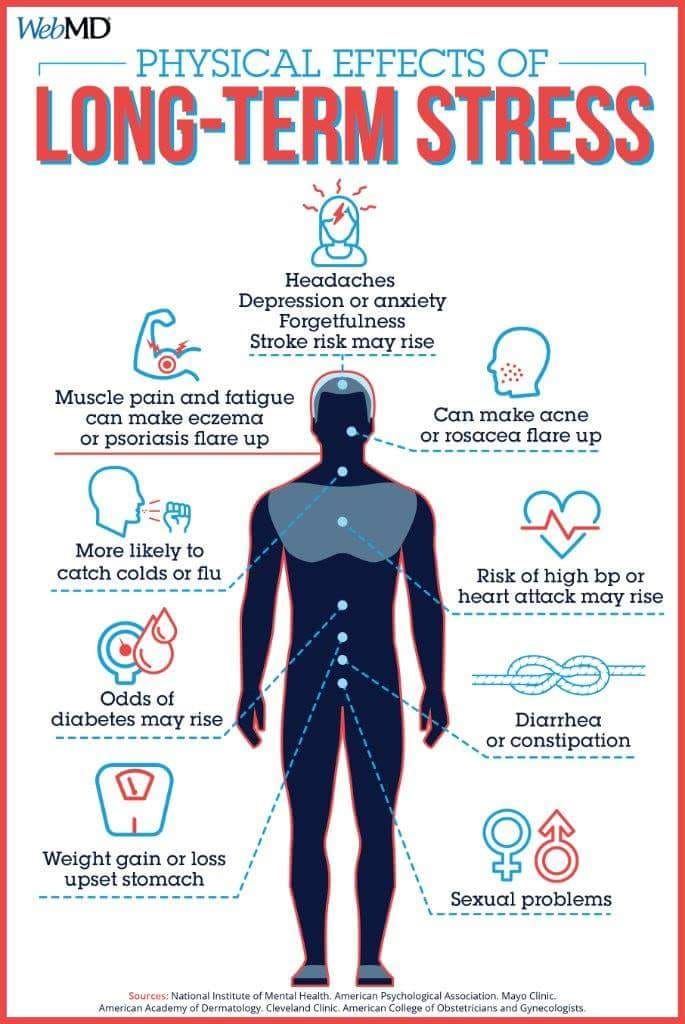 men and 11 women.
men and 11 women.
AH in the main group with a moderate course (II degree) was observed in 60% of patients, with a severe course (III degree) - in 40%; in the comparison group, there were 66.6% of patients with a moderate course, and 33.4% with a severe course. The average duration of AH disease was 10.61 ± 4.1 years (from 3 to 20 years).
Of great importance in the course of hypertension is a family history, lifestyle, risk factors and comorbidities.
Persons with symptomatic hypertension and complicated forms of hypertension were excluded from the study.
In the comparison group, patients received only antihypertensive therapy - ACE inhibitors, β-blockers, diuretics (Enap, Hypothiazid, Acridilol, Arifon). Patients of the main group received combined treatment with antihypertensive drugs in combination with Tenoten, which was prescribed according to the scheme: 6 tablets per day for the first 2 weeks, and then 1 tablet 3 times a day.
Treatment was prescribed for a month. Monitoring in dynamics was carried out at the beginning of the study, after 2 and 4 weeks of therapy.
Monitoring in dynamics was carried out at the beginning of the study, after 2 and 4 weeks of therapy.
The personal anxiety scale (J. Teylor) was used to assess the mental status, which is designed to measure the level of anxiety (adapted by T. A. Nemchininov).
The questionnaire consists of 50 statements. Evaluation of the results of the study is carried out by counting the number of responses of the subject, indicating anxiety; the total score is:
40-50 points - an indicator of a very high level of anxiety;
20-40 points - high level of anxiety;
15-20 points - average level of anxiety with a tendency to high;
5-15 points - average level of anxiety with a tendency to low;
0-5 points - low level of anxiety.
A study of the mental status of patients in both groups revealed anxiety symptoms of varying severity in a significant proportion of patients. The number of patients with an initial high level of anxiety was 40% in the main group and 43% in the comparison group. The number of patients with an initial average level of anxiety with a tendency to high was 60% in the main group and 56.6% in the comparison group.
The number of patients with an initial average level of anxiety with a tendency to high was 60% in the main group and 56.6% in the comparison group.
Research results
By the end of the study, the high level of anxiety decreased in the main group by 39.39% and reached the average level of anxiety with a tendency to low, and in the comparison group, the level of anxiety decreased only by 3.6%.
In patients of the main group who took Tenoten, a clear decrease in the level of anxiety was noted already after 2 weeks and by the end of the month it reached significance in comparison with the group of patients who received standard antihypertensive therapy. The relief of affective disorders was accompanied by a decrease in complaints of anxiety, feelings of helplessness, self-doubt, a sense of threatening danger, poor sleep ( tab. 1).
The demonstrated differences in the dynamics of anxiety indicators in the studied groups of patients confirmed the possibility of effective correction of these disorders in patients with AH with Tenoten. However, it was extremely interesting to assess whether this therapy and the severity of associated anxiety disorders affect the effectiveness of antihypertensive therapy in general.
However, it was extremely interesting to assess whether this therapy and the severity of associated anxiety disorders affect the effectiveness of antihypertensive therapy in general.
A decrease in the values of maximum systolic and diastolic pressure occurred in both studied groups. By the end of the month of treatment, the decrease in blood pressure (BP) reached a statistically significant significance. In the main group of patients who additionally took Tenoten, systolic blood pressure (BP) decreased by 24.28% - almost to the age norm, in the comparison group there was a decrease by 16.48%, i.e. there was some excess of normal values. The decrease in diastolic pressure by the end of the 4th week in the main group (by 17.7%) and in the comparison group (by 5.9%) was also significant ( tab. 2 , 3 ).
The addition of Tenoten to the complex therapy in patients with high and moderate levels of anxiety made it possible to achieve a much more pronounced improvement in blood pressure. Against the background of therapy with Tenoten, a more rapid effect of antihypertensive drugs is observed - after 2 weeks of combined administration of the drug in patients of the main group, blood pressure decreased to the target level, in contrast to the comparison group, where it remained above the target.
Against the background of therapy with Tenoten, a more rapid effect of antihypertensive drugs is observed - after 2 weeks of combined administration of the drug in patients of the main group, blood pressure decreased to the target level, in contrast to the comparison group, where it remained above the target.
Conclusion
The results of our study show that all patients with hypertension have anxiety symptoms of varying severity, which aggravate the course of the disease, contributing to higher levels of both systolic and diastolic blood pressure. The inclusion of the modern "daytime" anxiolytic Tenoten in the complex therapy of patients with hypertension increases the effectiveness of the treatment, reduces the level of anxiety, which contributes to a more rapid onset of the hypotensive effect. Tenoten is well tolerated by patients, does not cause orthostatic hypotension and any other undesirable side effects.
Literature
- Avedisova AS Anxiety disorders // Yu.
 A. Alexandrovsky. Mental disorders in general medical practice and their treatment. M.: GEOTAR-MED, 2004. S. 66–73.
A. Alexandrovsky. Mental disorders in general medical practice and their treatment. M.: GEOTAR-MED, 2004. S. 66–73. - Kopina O. S., Suslova S. F., Zaikin E. R. Population studies of psychosocial stress as a risk factor for cardiovascular diseases// Cardiology. 1996. No. 36 (3). pp. 53–56.
- Sudakov KV Emotional stress and arterial hypertension. M.: VNIIMI, 1976.
- Chazov EI Ischemic heart disease and the possibility of improving the effectiveness of its treatment// Clinical trials of drugs in Russia. 2001. No. 1. S. 2–4.
- Kawachi I., Sparrow D., Vokonas P. S., Wess S. T. Symptoms of anxiety and risk of coronary heart disease. The Normative Aging Study. circulation. 1994; 90, 5: 2225–2229.
- Lavie C., Milani R. Prevalence of anxiety in coronary patients with improvement following cardiac rehabilitation and exercise training. Am J Cardiol. 2004; 93:336–339.
- Sonas B. S., Franks P., Ingram D. D. Are symptoms of anxiety and depression risk factor for hyprtension? Longitudinal evidence from the National Health and Nutrition Examination Survey I Epidemiologic Follow-up Study.