Excess dopamine schizophrenia
Dopamine in schizophrenia: a review and reconceptualization
Save citation to file
Format: Summary (text)PubMedPMIDAbstract (text)CSV
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Add to My Bibliography
- My Bibliography
Unable to load your delegates due to an error
Please try again
Your saved search
Name of saved search:
Search terms:
Test search terms
Email: (change)
Which day? The first SundayThe first MondayThe first TuesdayThe first WednesdayThe first ThursdayThe first FridayThe first SaturdayThe first dayThe first weekday
Which day? SundayMondayTuesdayWednesdayThursdayFridaySaturday
Report format: SummarySummary (text)AbstractAbstract (text)PubMed
Send at most: 1 item5 items10 items20 items50 items100 items200 items
Send even when there aren't any new results
Optional text in email:
Create a file for external citation management software
Full text links
Atypon
Full text links
Review
. 1991 Nov;148(11):1474-86.
doi: 10.1176/ajp.148.11.1474.
K L Davis 1 , R S Kahn, G Ko, M Davidson
Affiliations
Affiliation
- 1 Department of Psychiatry, Mount Sinai Hospital and School of Medicine, New York, NY 10029-6574.
- PMID: 1681750
- DOI: 10.1176/ajp.148.11.1474
Review
K L Davis et al. Am J Psychiatry. 1991 Nov.
. 1991 Nov;148(11):1474-86.
doi: 10.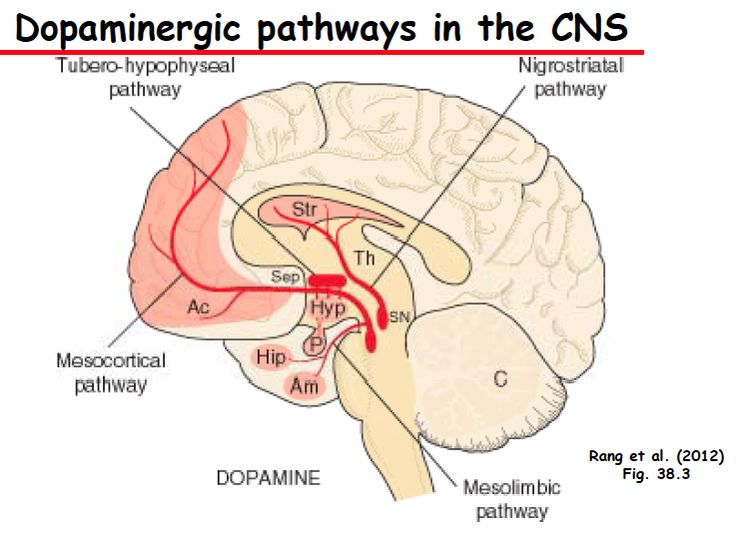 1176/ajp.148.11.1474.
1176/ajp.148.11.1474.
Authors
K L Davis 1 , R S Kahn, G Ko, M Davidson
Affiliation
- 1 Department of Psychiatry, Mount Sinai Hospital and School of Medicine, New York, NY 10029-6574.
- PMID: 1681750
- DOI: 10.1176/ajp.148.11.1474
Abstract
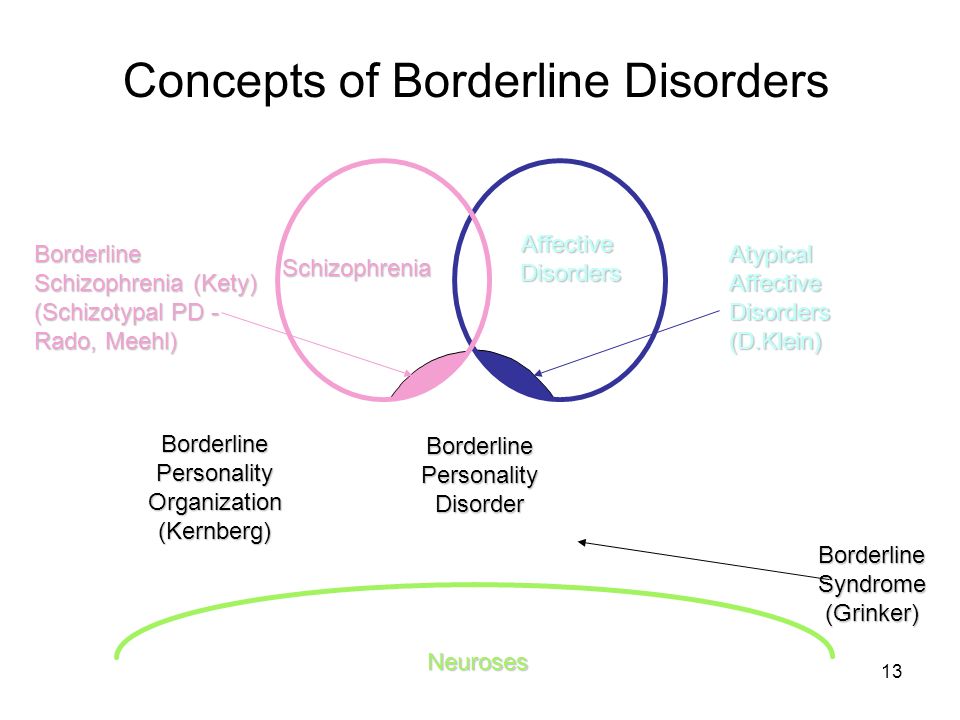
Objective: The initial hypothesis that schizophrenia is a manifestation of hyperdopaminergia has recently been faulted. However, several new findings suggest that abnormal, although not necessarily excessive, dopamine activity is an important factor in schizophrenia.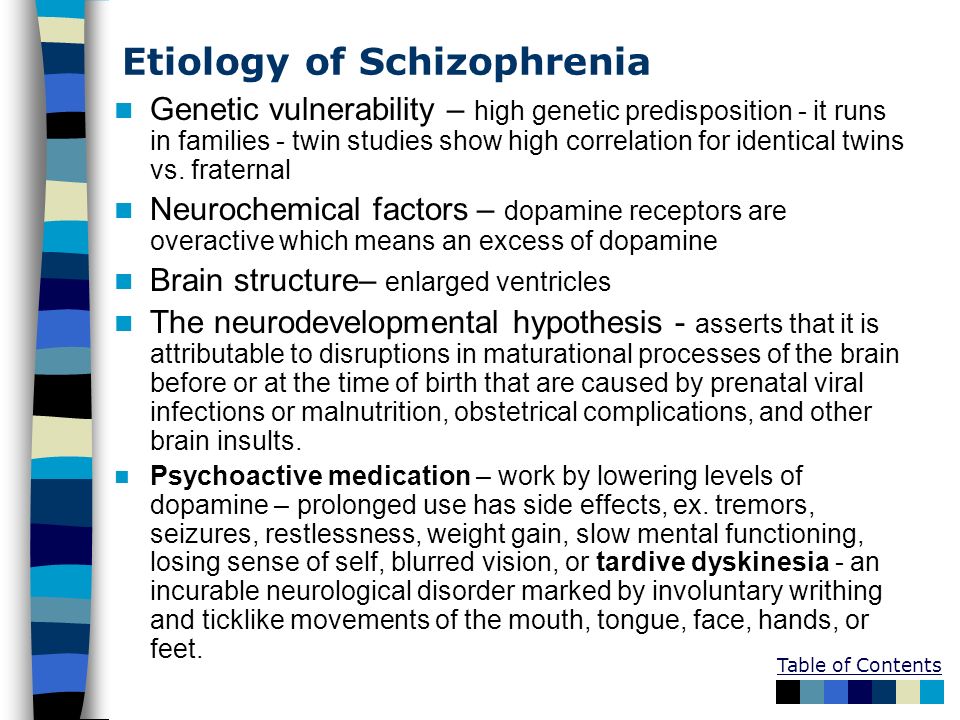 The authors discuss these findings and their implications.
The authors discuss these findings and their implications.
Method: All published studies regarding dopamine and schizophrenia and all studies on the role of dopamine in cognition were reviewed. Attention has focused on post-mortem studies, positron emission tomography, neuroleptic drug actions, plasma levels of the dopamine metabolite homovanillic acid (HVA), and cerebral blood flow.
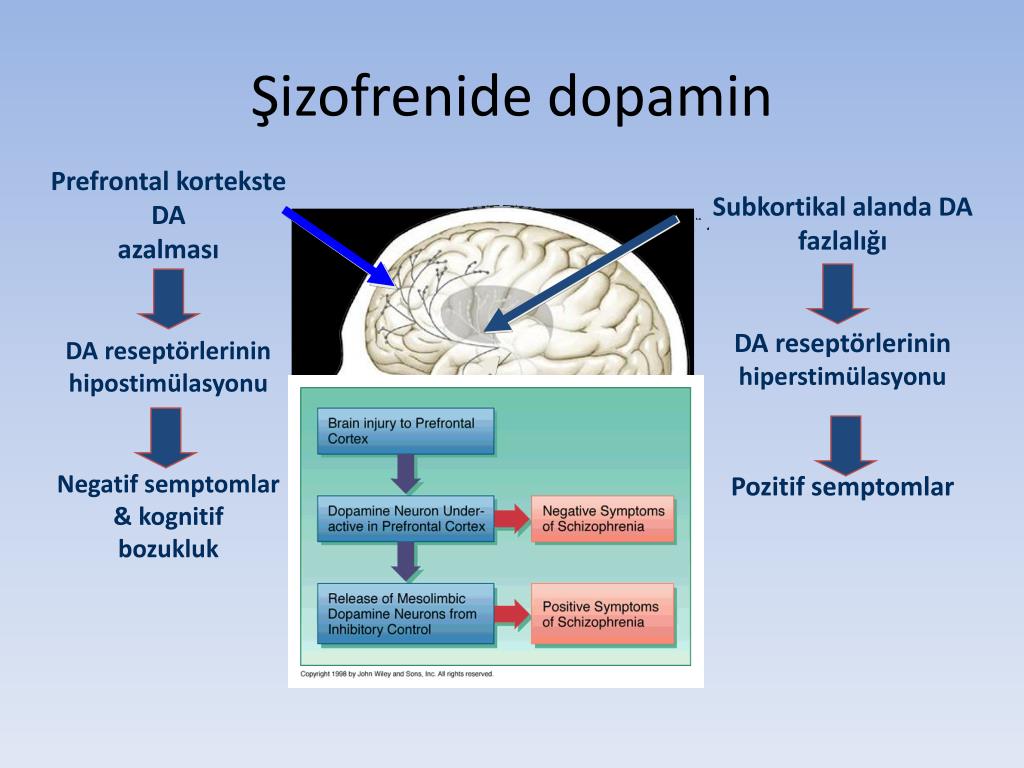
Results: Evidence, particularly from intracellular recording studies in animals and plasma HVA measurements, suggests that neuroleptics act by reducing dopamine activity in mesolimbic dopamine neurons. Post-mortem studies have shown high dopamine and HVA concentrations in various subcortical brain regions and greater than normal dopamine receptor densities in the brains of schizophrenic patients. On the other hand, the negative/deficit symptom complex of schizophrenia may be associated with low dopamine activity in the prefrontal cortex. Recent animal and human studies suggest that prefrontal dopamine neurons inhibit subcortical dopamine activity. The authors hypothesize that schizophrenia is characterized by abnormally low prefrontal dopamine activity (causing deficit symptoms) leading to excessive dopamine activity in mesolimbic dopamine neurons (causing positive symptoms).
Recent animal and human studies suggest that prefrontal dopamine neurons inhibit subcortical dopamine activity. The authors hypothesize that schizophrenia is characterized by abnormally low prefrontal dopamine activity (causing deficit symptoms) leading to excessive dopamine activity in mesolimbic dopamine neurons (causing positive symptoms).
Conclusions: The possible co-occurrence of high and low dopamine activity in schizophrenia has implications for the conceptualization of dopamine's role in schizophrenia. It would explain the concurrent presence of negative and positive symptoms. This hypothesis is testable and has important implications for treatment of schizophrenia and schizophrenia spectrum disorders.
Similar articles
-
Neuroleptics, dopamine, and schizophrenia.
Pickar D. Pickar D. Psychiatr Clin North Am. 1986 Mar;9(1):35-48. Psychiatr Clin North Am. 1986. PMID: 2870480
-
Effects of metabolic perturbation on plasma homovanillic acid in schizophrenia. Relationship to prefrontal cortex volume.
Breier A, Davis OR, Buchanan RW, Moricle LA, Munson RC. Breier A, et al. Arch Gen Psychiatry. 1993 Jul;50(7):541-50. doi: 10.1001/archpsyc.1993.01820190043005. Arch Gen Psychiatry. 1993. PMID: 8317948 Clinical Trial.
-
Down-regulation of central dopamine receptors in schizophrenia.
Zemlan FP, Hitzemann RJ, Hirschowitz J, Garver DL. Zemlan FP, et al. Am J Psychiatry. 1985 Nov;142(11):1334-7.
 doi: 10.1176/ajp.142.11.1334. Am J Psychiatry. 1985. PMID: 2865903
doi: 10.1176/ajp.142.11.1334. Am J Psychiatry. 1985. PMID: 2865903 -
Dopamine, the prefrontal cortex and schizophrenia.
Knable MB, Weinberger DR. Knable MB, et al. J Psychopharmacol. 1997;11(2):123-31. doi: 10.1177/026988119701100205. J Psychopharmacol. 1997. PMID: 9208376 Review.
-
Plasma homovanillic acid as an index of central dopaminergic activity: studies in schizophrenic patients.
Pickar D, Breier A, Kelsoe J. Pickar D, et al. Ann N Y Acad Sci. 1988;537:339-46. doi: 10.1111/j.1749-6632.1988.tb42118.x. Ann N Y Acad Sci. 1988. PMID: 2904783 Review.
See all similar articles
Cited by
-
The Hypothalamic-Pituitary-Gonadal Axis in Men with Schizophrenia.

Matuszewska A, Kowalski K, Jawień P, Tomkalski T, Gaweł-Dąbrowska D, Merwid-Ląd A, Szeląg E, Błaszczak K, Wiatrak B, Danielewski M, Piasny J, Szeląg A. Matuszewska A, et al. Int J Mol Sci. 2023 Mar 30;24(7):6492. doi: 10.3390/ijms24076492. Int J Mol Sci. 2023. PMID: 37047464 Free PMC article. Review.
-
Integrative Roles of Dopamine Pathway and Calcium Channels Reveal a Link between Schizophrenia and Opioid Use Disorder.
Thiagarajan SK, Mok SY, Ogawa S, Parhar IS, Tang PY. Thiagarajan SK, et al. Int J Mol Sci. 2023 Feb 17;24(4):4088. doi: 10.3390/ijms24044088. Int J Mol Sci. 2023. PMID: 36835497 Free PMC article.
-
Dual orexin/hypocretin receptor antagonism attenuates attentional impairments in an NMDA receptor hypofunction model of schizophrenia.

Maness EB, Blumenthal SA, Burk JA. Maness EB, et al. bioRxiv. 2023 Feb 5:2023.02.05.527043. doi: 10.1101/2023.02.05.527043. Preprint. bioRxiv. 2023. PMID: 36778441 Free PMC article.
-
Altered static and dynamic functional connectivity of habenula in first-episode, drug-naïve schizophrenia patients, and their association with symptoms including hallucination and anxiety.
Xue K, Chen J, Wei Y, Chen Y, Han S, Wang C, Zhang Y, Song X, Cheng J. Xue K, et al. Front Psychiatry. 2023 Jan 19;14:1078779. doi: 10.3389/fpsyt.2023.1078779. eCollection 2023. Front Psychiatry. 2023. PMID: 36741115 Free PMC article.
-
A Novel Microfluidic-Based OMC-PEDOT-PSS Composite Electrochemical Sensor for Continuous Dopamine Monitoring.

Nuh S, Numnuam A, Thavarungkul P, Phairatana T. Nuh S, et al. Biosensors (Basel). 2022 Dec 31;13(1):68. doi: 10.3390/bios13010068. Biosensors (Basel). 2022. PMID: 36671903 Free PMC article.
See all "Cited by" articles
Publication types
MeSH terms
Substances
Grant support
- MH-37922/MH/NIMH NIH HHS/United States
Full text links
Atypon
Cite
Format: AMA APA MLA NLM
Send To
Schizophrenia and Dopamine: Links and Connections
Schizophrenia is a severe type of mental illness that affects a person’s thoughts, perceptions, and behaviors. Researchers estimate up to 1 percent of adults worldwide have schizophrenia.
Researchers estimate up to 1 percent of adults worldwide have schizophrenia.
What exactly causes schizophrenia is still unclear. However, we do have some ideas about the various factors that may be involved. One of these is dopamine. It’s a type of brain chemical messenger called a neurotransmitter.
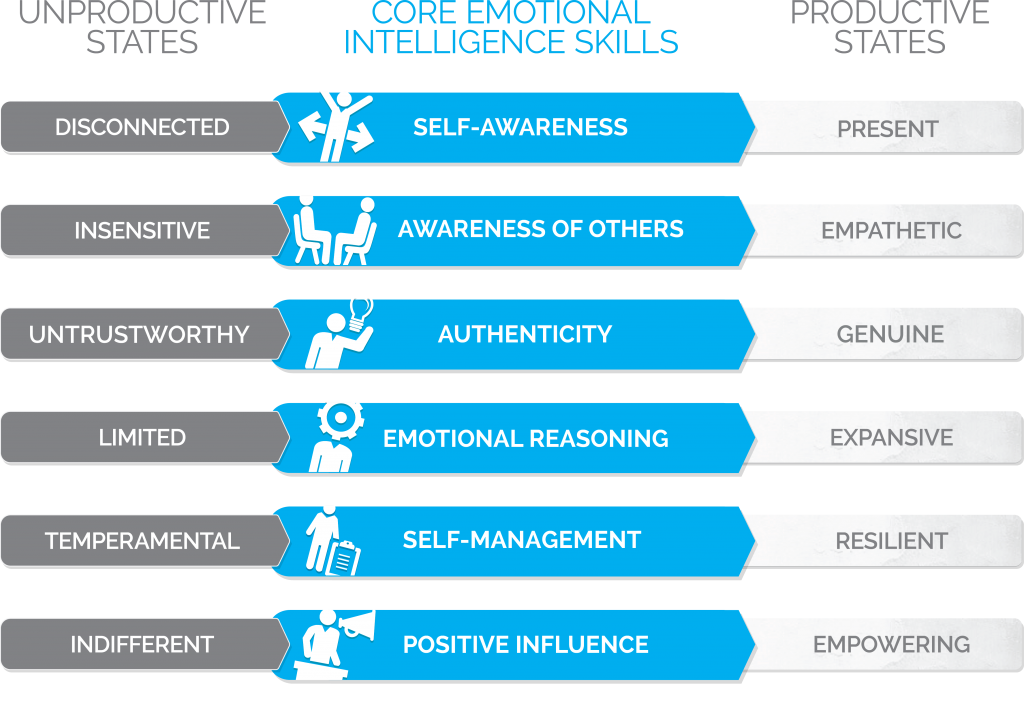
Experts believe that changes in dopamine activity may contribute to certain schizophrenia symptoms. This is called the dopamine hypothesis of schizophrenia. Keep reading below as we explore this concept in more detail.
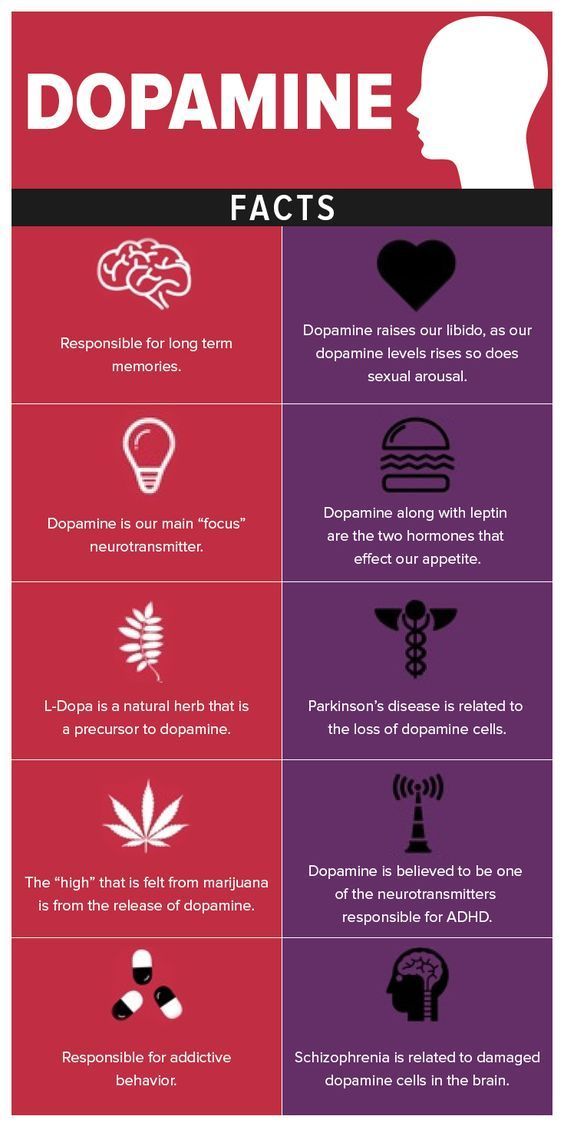
Dopamine is a type of neurotransmitter. Neurotransmitters are brain chemical messengers that help your nerve cells communicate with one another.
Different neurotransmitters attach (bind) to different receptors on nerve cells. When a neurotransmitter binds to the right receptor on a nerve cell, it triggers that cell to take a specific action. Think of it like a key in a lock.
Different neurotransmitters are associated with many physical and psychological processes in the body. For example, dopamine is involved in things like:
For example, dopamine is involved in things like:
- motivation and reward
- movement
- mood
- attention, learning, and memory
- sleep and dreaming
Neurotransmitters travel along neuronal pathways, which are basically long chains of nerve cells (neurons) that help different parts of the brain talk with one another.
Some pathways that appear to be associated with schizophrenia symptoms have been identified. These pathways use dopamine as their primary messenger, and include the mesolimbic pathway and the mesocortical pathway.
We’ll discuss the role these pathways may have in different schizophrenia symptoms a little later.
The dopamine hypothesis of schizophrenia has been around for a long time. In fact, it was first proposed in the 1960s.
During this time, doctors noticed that an antipsychotic drug called chlorpromazine, which reduces dopamine activity, effectively treated some types of schizophrenia symptoms.
Due to this observation, doctors and researchers theorized that increased levels of dopamine in the brain contributed to some symptoms of schizophrenia.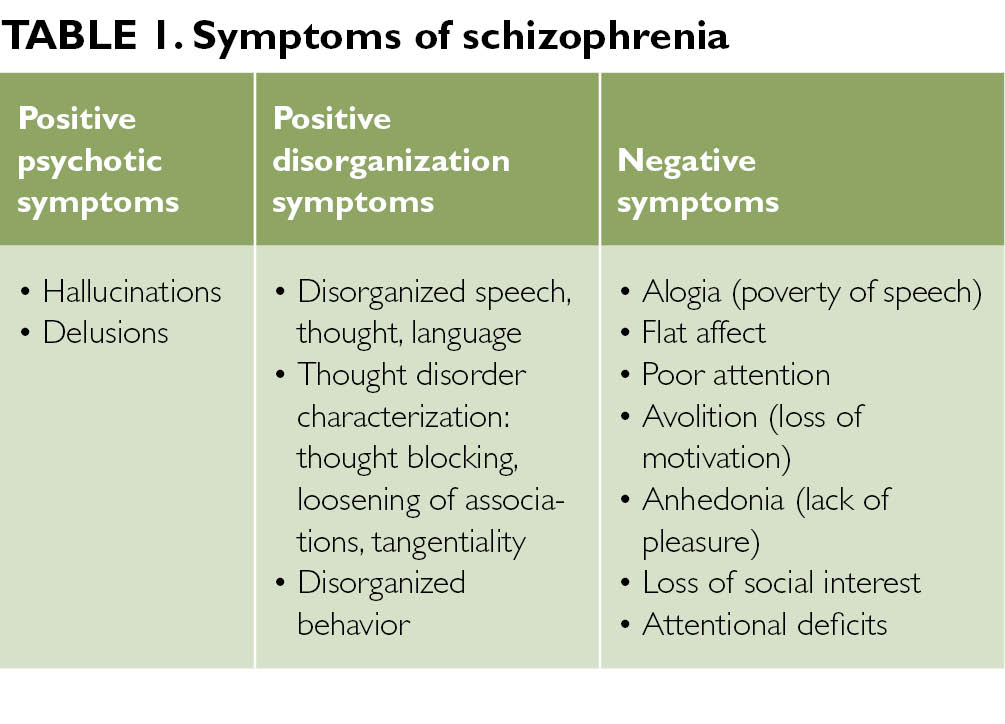 But it’s a little more complicated than that.
But it’s a little more complicated than that.
High levels of dopamine don’t cause schizophrenia symptoms. The role dopamine plays in schizophrenia is more complex than that and involves specific dopamine activity.
Over time, researchers have discovered evidence that isn’t in line with the original dopamine hypothesis of schizophrenia. For example, they found that some people with schizophrenia had typical levels of dopamine in their cerebrospinal fluid as opposed to elevated levels.
Further, researchers found that other antipsychotic drugs that do not block the effects of dopamine could still treat symptoms of schizophrenia.
Some schizophrenia symptoms may be triggered when certain areas of the brain have high levels of dopamine activity while others have lower levels of activity.
Other neurotransmitters and schizophrenia
Doctors and researchers have found that dopamine isn’t the only neurotransmitter involved in schizophrenia. Other neurotransmitters in the brain are also likely involved in some way.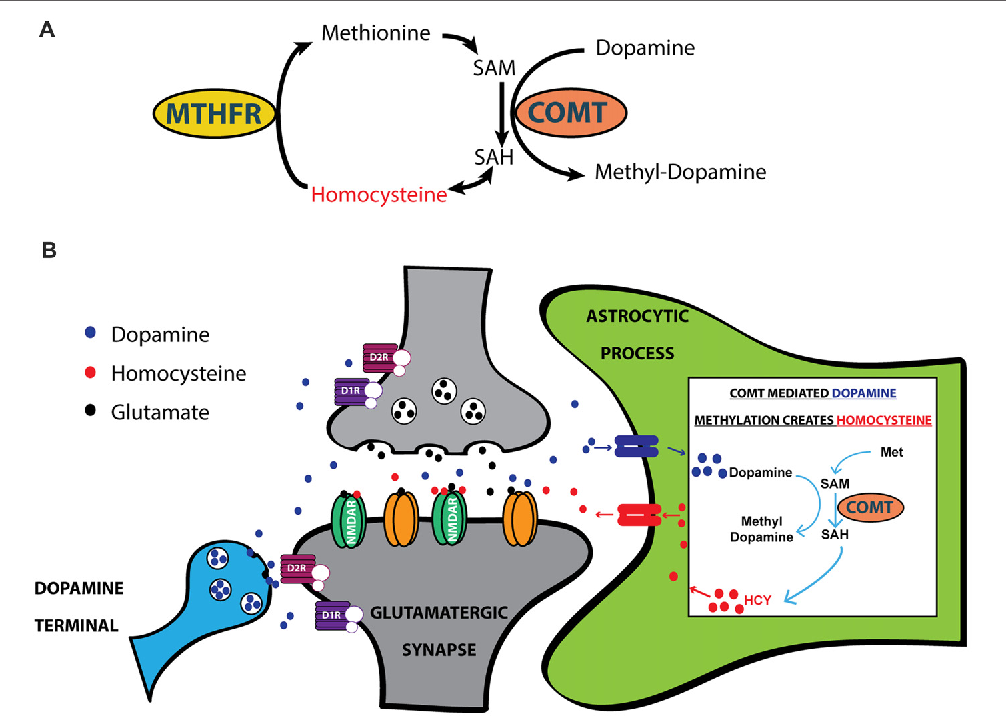
An example of this is glutamate. This neurotransmitter is important for things like learning, memory, and mood. Glutamate travels along a pathway that links several regions of the brain that may be important in schizophrenia.
Glutamate first came on the radar when it was found that inhibiting a certain type of glutamate receptor, called an NMDA receptor, led to schizophrenia-like symptoms.
Other neurotransmitters that may also be involved in schizophrenia include gamma-aminobutyric acid (GABA) and serotonin.
Schizophrenia causesIn addition to what we’ve discussed already, several other factors are believed to be involved in the development of schizophrenia:
- Genetics. Schizophrenia can run in families, although the exact genes involved are still unclear.
- Brain structure. Compared with people without schizophrenia, those with schizophrenia can have slight changes in their brain structure.

- Complications during pregnancy and birth. Some complications that happen during pregnancy and birth, such as low birth weight and maternal malnutrition, have been associated with increased schizophrenia risk.
- Environmental factors. It’s thought that factors like experiencing trauma or using certain types of drugs may help trigger schizophrenia in people who are at risk of the condition.
Overall, schizophrenia is a very complex condition. As such, it’s likely that an intricate combination of biological, genetic, and environmental factors play a role in causing it.
Was this helpful?
Doctors still don’t know exactly how dopamine relates to schizophrenia symptoms, but there are theories. Aberrant salience is another theory tied to schizophrenia and dopamine.
But what exactly is salience in the first place?
Generally speaking, salience is how your brain attaches importance to something. For example, when you’re crossing the street, cars are your most salient thought.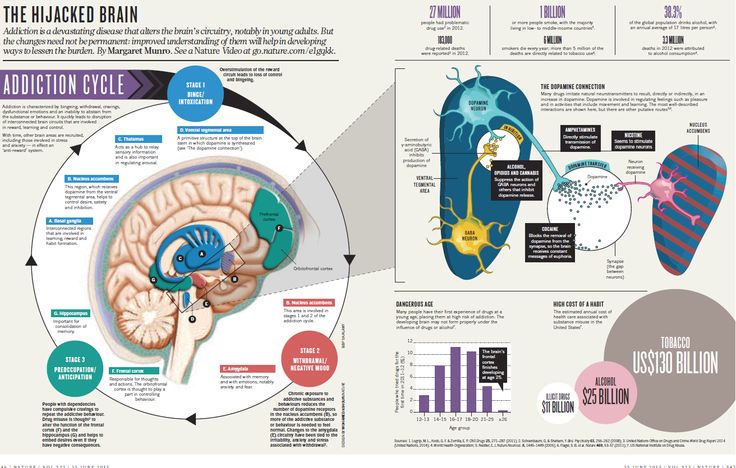
Researchers are investigating whether increased dopamine levels in the mesolimbic pathway may lead to problems with salience.
When salience is dysfunctional, someone crossing the street may pay little attention to cars because their brain is telling them it’s more important to pay attention to the birds flying overhead.
This theory can help explain some of the more noticeable symptoms of psychosis.
Below, we’ll explore the three categories of schizophrenia symptoms and discuss the potential of dopamine involvement.
Positive symptoms
Dopamine is most closely linked to positive symptoms of schizophrenia. Positive symptoms include:
- Hallucinations. This involves perceiving things that aren’t actually there. Hearing voices is the most common example.
- Delusions. These are strongly held beliefs that are untrue and may not seem logical to other people.
- Unusual speech patterns. This can include things like suddenly stopping in the middle of talking about something, moving quickly from topic to topic, or making up words.
- Atypical body movements. This may include things like repeating the same motion over and over again.
- Disordered thinking. This is a disordered way of thinking that can result in confusion and unusual behavior.
Remember the antipsychotic drugs we talked about earlier?
These actually work by blocking specific dopamine receptors. Blocking these receptors reduces positive schizophrenia symptoms but has little effect on other symptoms.
Positive symptoms have been linked to increased dopamine activity in the mesolimbic pathway. This is one of the major dopamine-related pathways in the brain.
Negative and cognitive symptoms
The negative symptoms of schizophrenia can include:
- apathy or disinterest in daily activities
- limited emotional expression
- avoiding social interactions
- trouble with planning or following through with plans
- low energy levels
People with schizophrenia can also have cognitive symptoms, which can include issues with things like:
- learning and memory
- concentration
- attention
- decision making
Decreases in dopamine activity in certain areas of the brain may lead to the negative and cognitive symptoms of schizophrenia.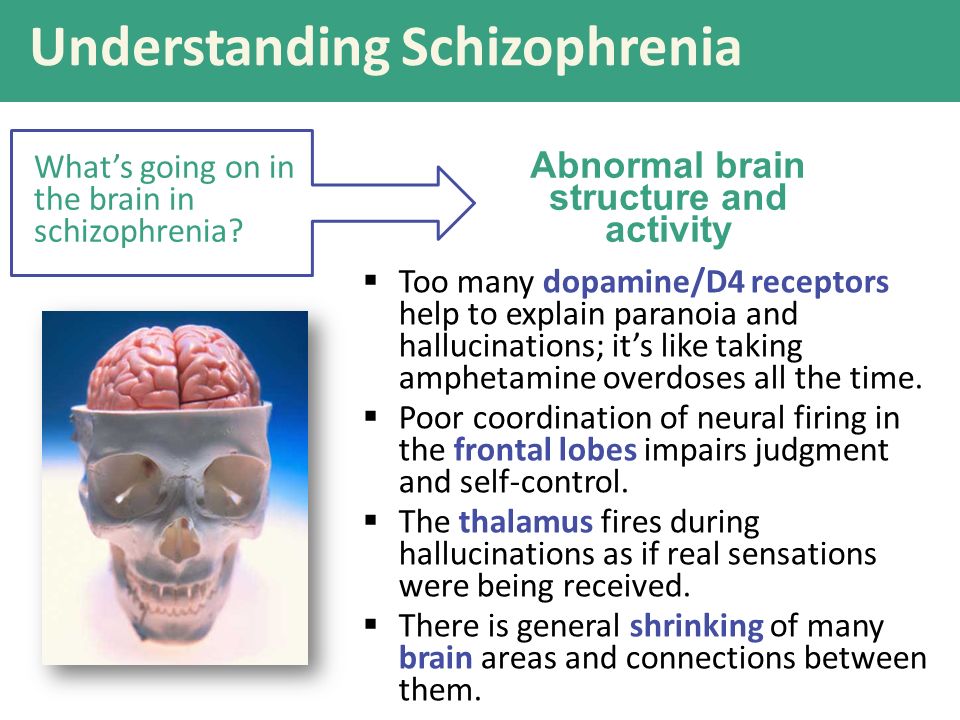 The pathway thought to be affected by this is called the mesocortical pathway.
The pathway thought to be affected by this is called the mesocortical pathway.
The mesocortical pathway is another one of the major dopamine-related pathways in the brain. Messages sent along this pathway go to the prefrontal cortex. This is an area of the brain associated with processes like:
- decision making
- memory
- attention
- motivation
- emotional control
Note that the processes above are those that are largely affected by negative and cognitive symptoms of schizophrenia. As such, it makes sense that reduced dopamine activity along this pathway may contribute to these symptoms.
Dopamine plays an important role in the treatment of schizophrenia. Antipsychotic drugs block dopamine activity and are used to manage the positive symptoms of schizophrenia.
However, people taking antipsychotic drugs often experience side effects. These can include:
- drowsiness
- weight gain
- dry mouth
- constipation
- difficulty thinking or concentrating
- feeling restless
- tremors
- involuntary muscle contractions (dystonia)
- low blood pressure when standing up (orthostatic hypotension)
- an increased risk of diabetes
- tardive dyskinesia, which causes involuntary movements, often in the face, tongue, and jaw
The exact side effects a person may experience can vary based on the specific antipsychotic drug that’s used. Often, lowering the dose or switching to a different drug can reduce side effects.
Often, lowering the dose or switching to a different drug can reduce side effects.
Another downside is that antipsychotic drugs don’t help nearly as much with negative and cognitive symptoms. These types of symptoms are typically managed with one or a combination of the following psychosocial treatments:
- cognitive behavioral therapy
- family therapy
- behavioral and social skills training
- supported employment
There’s currently no cure for schizophrenia, but it can be successfully managed. It’s a chronic (long lasting) condition that requires treatment over the course of a person’s lifetime.
Researchers continue to investigate the role of dopamine in schizophrenia. This is not only important in further understanding the causes of schizophrenia itself, but also in improving treatment.
Current antipsychotic drugs are mostly effective for positive symptoms. Even then, some cases of schizophrenia can be resistant to these drugs. Further, antipsychotic drugs can come with significant side effects, particularly when they’re used long term.
Understanding how dopamine and other neurotransmitters affect schizophrenia can help researchers develop newer treatments that:
- are more effective overall
- target neurotransmitters other than dopamine
- help address negative and cognitive symptoms
- have fewer side effects
Increases in dopamine activity in certain parts of the brain can contribute to the positive symptoms of schizophrenia. Meanwhile, reduced dopamine activity in other parts of the brain may affect negative and cognitive symptoms.
Dopamine is just one of many factors involved in schizophrenia symptoms. Other neurotransmitters and various physical, genetic, and environmental factors are also important.
The antipsychotic drugs currently in use primarily target dopamine and can help manage positive symptoms of schizophrenia, but not others.
Dopamine
The dopaminergic theory of the pathogenesis of schizophrenia has been popular throughout the last quarter of the 20th century.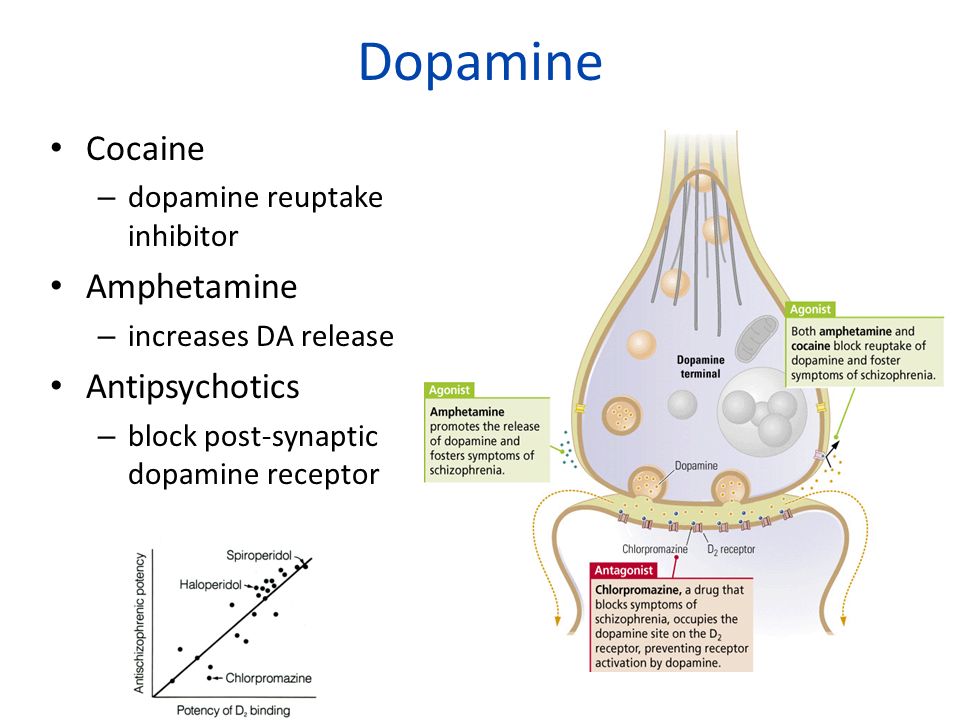 It seems significant to acquaint the reader with the main provisions of the modern doctrine of dopamine.
It seems significant to acquaint the reader with the main provisions of the modern doctrine of dopamine.
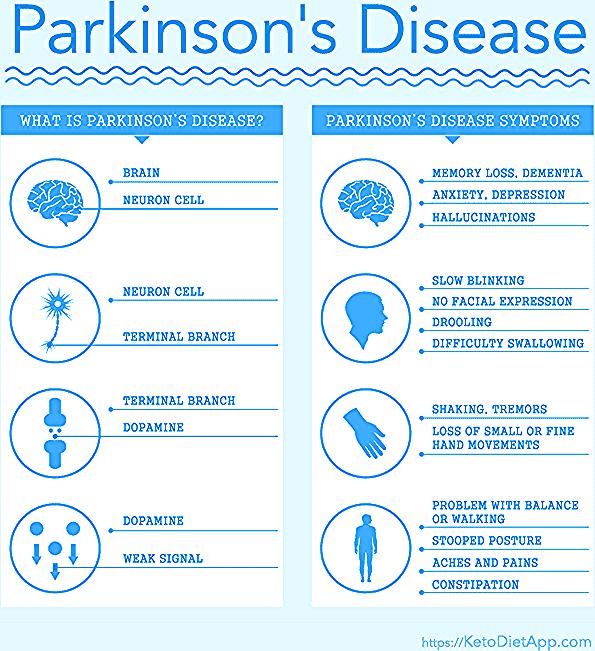
Dopamine is not only a precursor of norepinephrine, but also acts as a transmitter itself. The localization of dopamine in the nervous system differs from the localization of other catecholamines: norepinephrine and adrenaline.
A rich network of dopamine-sensitive receptors has been found in many structures of the central nervous system.
The entire vast area of the median eminence is occupied by dopaminergic terminals, and only a few nerve cell endings in this area are sensitive to norepinephrine.
Dopamine-sensitive neurons are mainly concentrated in the following structures: substantia nigra, ventral tegmentum, striatum, olfactory bulb, hypothalamus (arcuate nucleus), around the medulla oblongata ventricles (periventricular area) and retina.
Axons of dopamine-sensitive neurons project to the frontal cortex (ends of dopamine-sensitive receptors in the cerebral cortex are quite rare), the limbic system, the neostriatum, and the median eminence.
The basal ganglia consist of the caudate nucleus and putamen (neostriatum), the inner and outer segments of the globus pallidus, the reticular and compact parts of the substantia nigra, and the subthalamic nucleus.
The neostriatum is considered the main part of the basal ganglia, receiving information from the entire cortex in accordance with the somatotopic projection, as well as from the intralaminar nuclei of the thalamus. Information enters from the basal ganglia through the internal segment of the globus pallidus and reticular substantia nigra, passes through the nuclei of the thalamus (anteroventral and ventrolateral), which are projected to the premotor cortex, supplementary motor cortex and prefrontal cortex. The projection also extends to the spinal cord, especially the pedunculopontine nucleus, which takes part in locomotor acts, as well as to the superior colliculus of the quadrigemina, which takes part in the regulation of eye movements. The basal ganglia form several circles of neural networks.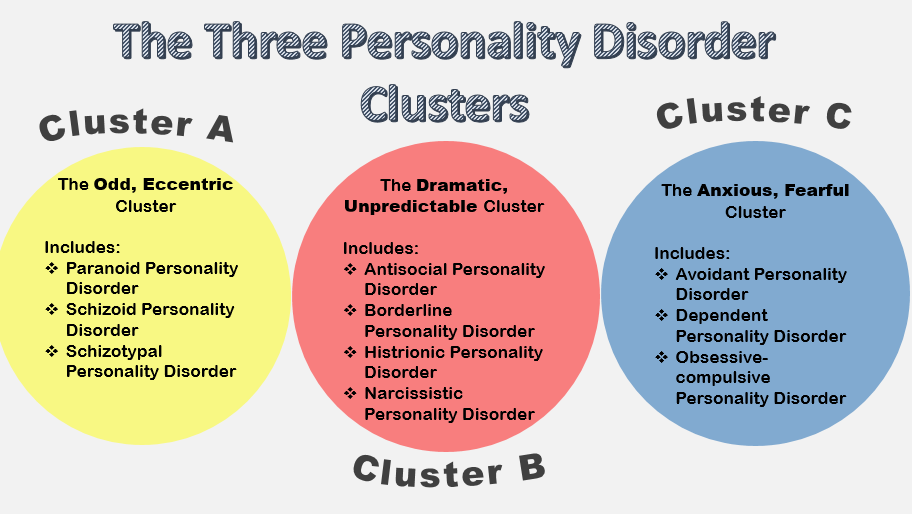 In the strianigrostriatal circle, the last link is dopaminergic. The neostriatum is composed of bands and striosomes that contain small amounts of acetylcholinesterase (AchE).
In the strianigrostriatal circle, the last link is dopaminergic. The neostriatum is composed of bands and striosomes that contain small amounts of acetylcholinesterase (AchE).
The bulk of postsynaptic dopamine receptors, as noted above, is concentrated in the striatum, in the region of the globus pallidus and the caudate nucleus. The fibers of the cells of the substantia nigra approach the neurons of these nuclei, while the axons of the globus pallidus and the caudate nucleus go in the opposite direction, forming the nigrostriatal system, which plays an important role in the regulation of mental and motor reactions.
Dopamine is deposited in large vesicles of the synapse. After being released (exocytosis) into the synaptic cleft, it interacts with various types of receptors. Then it is inactivated in the extracellular space or in glial cells and, like other catecholamines, is destroyed by two enzymes - monoamine oxidase (MAO) and catechol-o-methyltransferase (COMT). Two types of monoamine oxidases (MAO-A and MAO-B) have been described.
Unlike the striatum, the prefrontal cortex does not have carriers, dopamine, the latter are protein compounds that carry out reuptake. In addition, in their structure they resemble protein compounds that represent serotonin receptors. Reuptake proteins can be blocked, as in the case of serotonin reuptake inhibitors, or absent altogether, as in the case of schizophrenia in the prefrontal cortex. In all these cases, enzymes (COMT) that break down neurotransmitters begin to play an extremely important role. Thus, the effect of COMT on dopamine activity in the prefrontal cortex is beyond doubt.
Animal studies have shown that COMT is involved in the breakdown of more than 60% of dopamine located in the prefrontal cortex. We emphasize that the dopamine of the prefrontal cortex is involved in cognitive processes. Increased dopamine activity in the prefrontal cortex, according to studies conducted on patients suffering from Parkinson's disease, improves cognitive functions. It turns out that dopamine allows, as it were, to concentrate most of the energy in those areas of the brain that are involved in information processing.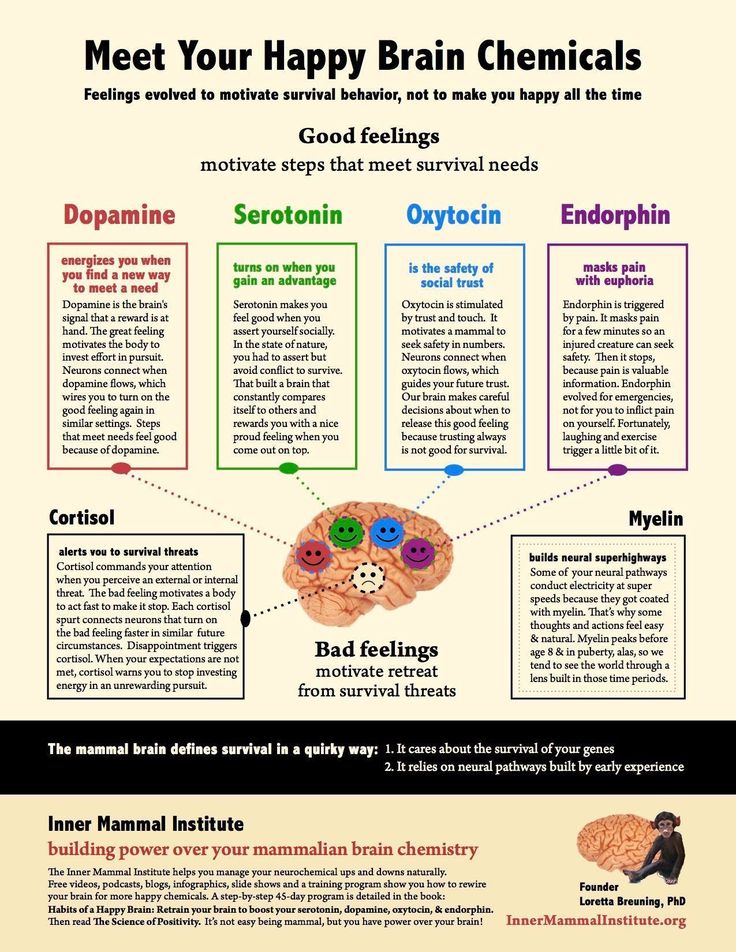 Disruption of dopamine transmission leads to attention deficit.
Disruption of dopamine transmission leads to attention deficit.
MAO-B dominates in catecholaminergic neurons and their axons. A part of the undestroyed mediator is transferred back to the end of the receptor (intraneuronal metabolism) with the help of capture by a special transport system and can be reused.
Dopamine responsive receptors are slow metabotropic receptors. A long polypeptide chain crosses the membrane seven times, the glycosylated N-terminus faces the extracellular space, and the C-terminus is located in the cytoplasm. Dopamine receptors are coupled to adenylate cyclase via G-proteins.
Dopamine receptors can be localized both post- and pre-synaptically, in particular, on noradrenergic and dopaminergic nerve endings, thus controlling the release of mediators. So, for example, presynaptic D3 receptors can regulate the release of dopamine.
The first nigrostriatal pathway starts from substantia nigra neurons, A9 nucleus (depending on rostrocaudal localization, catecholamine neurons are classified from A1 to A15).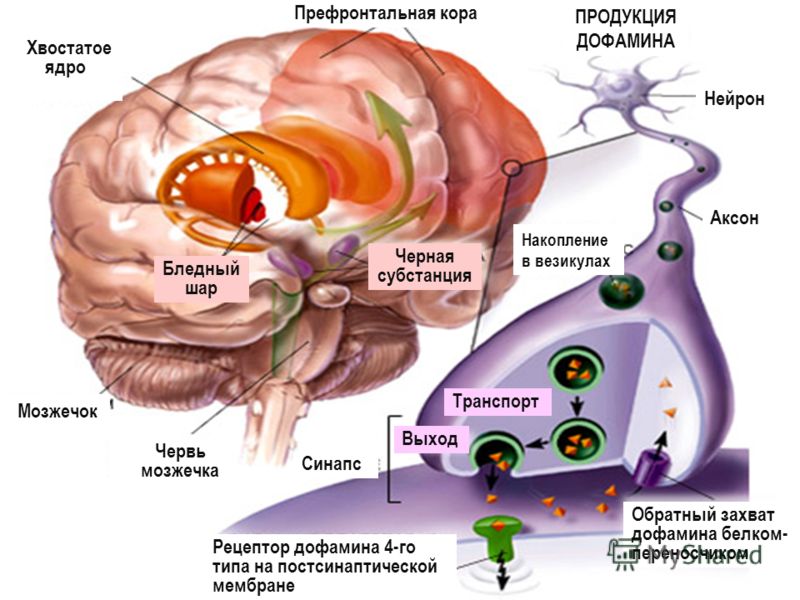 The axons of neurons located in the substantia nigra extend to the dorsal part of the body of the striatum (corpus striatum). The nigrostriatal pathway is related to the regulation (coordination) of the motor (sensory-motor) functions of the body, cognitive integration, the formation of stereotyped actions and the initiation of motor acts, and the blockade of dopamine transmission in this tract by neuroleptics is manifested by symptoms of parkinsonism.
The axons of neurons located in the substantia nigra extend to the dorsal part of the body of the striatum (corpus striatum). The nigrostriatal pathway is related to the regulation (coordination) of the motor (sensory-motor) functions of the body, cognitive integration, the formation of stereotyped actions and the initiation of motor acts, and the blockade of dopamine transmission in this tract by neuroleptics is manifested by symptoms of parkinsonism.
The second dopaminergic pathway - mesolimbic - is formed from the neurons of the ventral tegmental field (A10) and goes to the structures of the limbic region: the nucleus accumbens, olfactory bulbs, amygdala, periform cortex.
Third - mesocortical also starts from A10, but goes to the prefrontal cortex.
According to one of the hypotheses of the pathogenesis of schizophrenia, the onset of the disease is due to a decrease in the activity of the dopaminergic mesocortical system, while the productive symptoms of psychosis arise in connection with an increase in the activity of the dopaminergic mesolimbic system (possibly also the corticolimbic system)
Table 10 summarizes the role of dopaminergic tracts in the pathogenesis of some clinical symptoms of schizophrenia.
| No. | Dopaminergic tract | Symptoms |
| 1 | Nigrostriatal | Changes in motor activity, |
| 2 | Mesolimbic | Positive symptoms |
| 3 | Mesocortical | Negative symptomatology |
| 4 | Tuberoinfundibular | Neuroendocrine disorders (prolactinemia) |
Dopaminergic neurons of the periventricular and arcuate nuclei of the mediobasal hypothalamus (A14 and A12) transport dopamine to the pituitary gland.
The nucleus accumbens and some other subcortical structures of the limbic system are also related to some manifestations of schizophrenia, and the connection between the neurons of the ventral tegmental field of the midbrain with the basal ganglia probably plays a certain role here.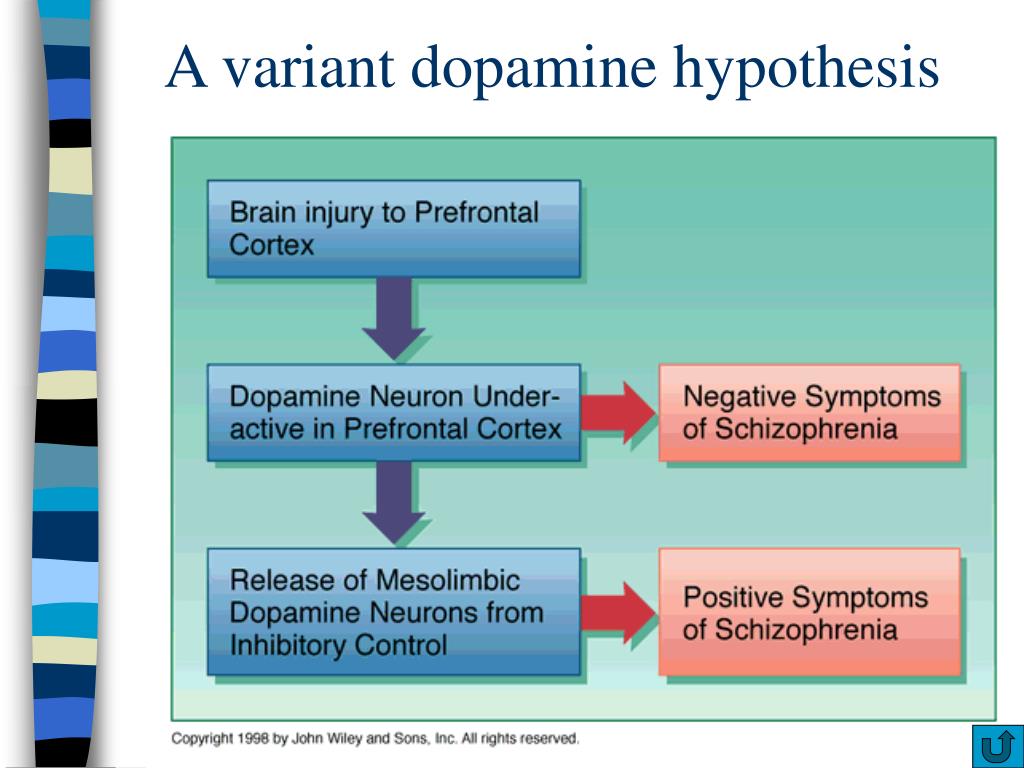
Dopamine receptor heterogeneity is known. Currently, 5 subtypes of dopamine receptors (D1-D5) have been isolated, cloned and characterized using molecular biological, biochemical and pharmacological methods, differing in binding characteristics to various agonists and antagonists, as well as in the signal transduction system.
All dopamine receptor subtypes are grouped into two families: D1-like (D1 and D5) and D2-like (D2, D3, D4).
Classification of dopamine receptors
D1-like
- D1 (neurons of the nigrostriatal and mesocorticolimbic systems, tonsils)
- D5 (peripheral parts of the nervous system)
D2-like
- D2 (striatum, limbic structures of the brain: substantia nigra, ventral tegmental area, hippocampus)
- D3 (striatum including nucleus accumbens)
- D4
More studied are D1 and D2 dopamine receptors, which, however, like other dopamine receptors, are single-chain polypeptides comprising from 387 to 475 amino acid residues.
D1 and D2 dopamine receptors are expressed and have more selective agonists and antagonists than other dopamine receptor subtypes.
It has been established that Gs-coupled D1-type receptors activate adenylate cyclase. Activation of D1-D5 receptors leads to an increase in the level of intracellular cAMP.
The genomic structure of dopamine receptors depends on belonging to one or another receptor family. The D1 subtype genes do not have introns, while the D2, D3, D4 genes have 6, 5 and 3 introns, respectively. The presence of introns allows the formation of various isoforms using alternative plasing.
Dopamine D1 receptors (stimulated by adenylate cyclase) are localized mainly in the neurons of the nigrostriatal and mesocorticolimbic systems, the amygdala. However, they are less common in the brain of a normal person than D2.
D1 receptors are inhibited only by relatively high (micromolar) concentrations of antagonists, such as the antipsychotic haloperidol.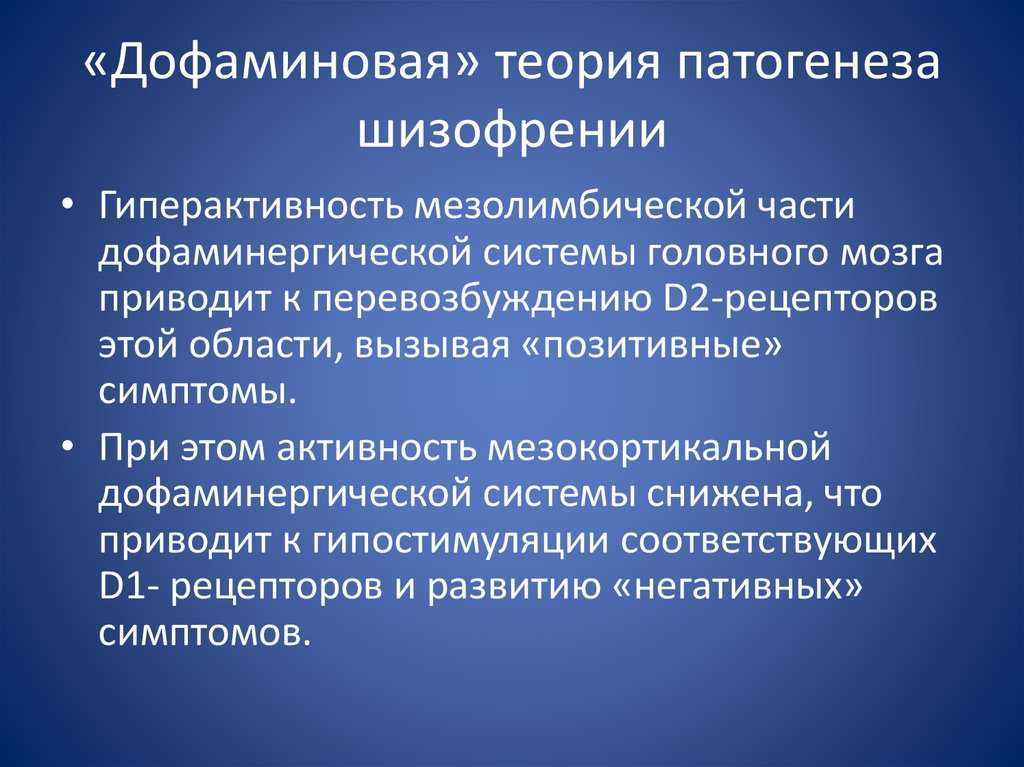
The D2 dopamine receptor, which is predominant in the brain of a healthy person, compared to other dopamine-sensitive receptors, exhibits the highest affinity for many antipsychotics. According to some studies conducted using positron emission tomography, it has the highest density in the striatum and limbic structures of the brain.
A high concentration of receptors of this type is found in the substantia nigra, ventral tegmental areas, and hippocampus.
When examining the prefrontal cortex, no significant differences in the density of D2 receptors were found.
Activation of D2 receptors leads to a decrease in the level of intracellular cAMP (cyclic adenosine monophosphate).
The density of D1 and D2-type receptors is noticeably higher than that of D3 and D4; in addition, the former types of receptors have been identified in more brain structures.
Dopamine D3 and D4 receptors have a more limited distribution in the human brain, with the D3 receptor being the most extensively studied.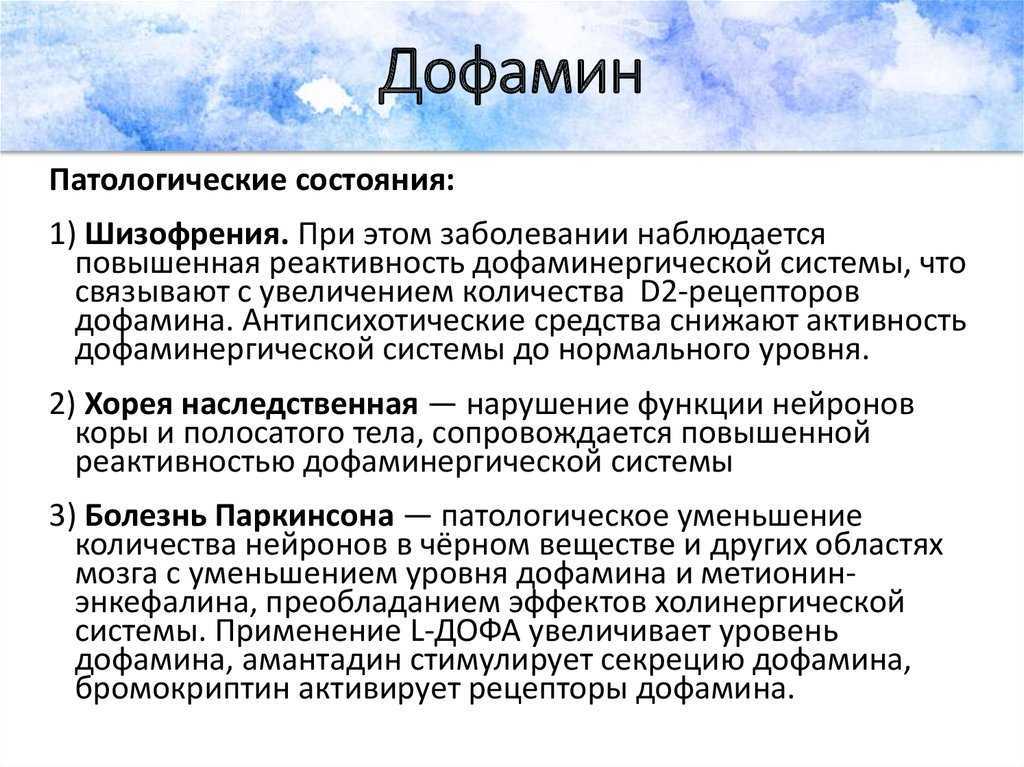 Expression of D3 receptors is characteristic of the ventricular striatum, including the nucleus accumbens. In patients with schizophrenia, an increase in the density of D3 type receptors was found here with a relative accumulation of "truncated forms" of the receptor protein, which are formed during abnormal plicing. D3, D4 receptors depend on the cAMP signaling system.
Expression of D3 receptors is characteristic of the ventricular striatum, including the nucleus accumbens. In patients with schizophrenia, an increase in the density of D3 type receptors was found here with a relative accumulation of "truncated forms" of the receptor protein, which are formed during abnormal plicing. D3, D4 receptors depend on the cAMP signaling system.
D5-type receptors are found mainly in the peripheral parts of the nervous system.
According to the dopamine hypothesis of the development of schizophrenia, many symptoms of this disease arise due to increased activity of dopaminergic pathways of information transmission, increased activity of dopamine, especially in mesolimbic structures, or increased sensitivity of receptors for this mediator.
As a result of the activation of the dopaminergic system, structural and functional disorders appear in those areas of the brain that are innervated by this system, and the disorganization of the functioning of the prefrontal cortex is of particular importance (Tamminga C.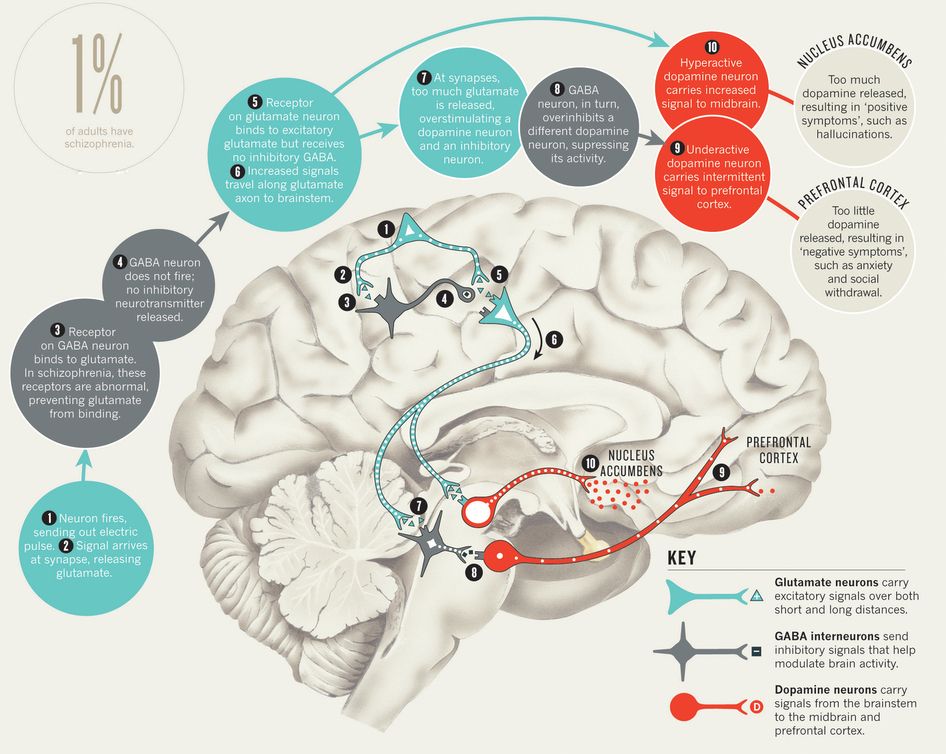 , 2006).
, 2006).
This hypothesis is supported by experimental psychoses, amphetamine psychosis, the results of studies on antipsychotics, the discovery of a large number of dopamine receptors in some post-mortem studies of the brain of patients with schizophrenia.
The dopamine analogue, the plant alkaloid mescaline, can cause hallucinations similar to those seen in schizophrenia. The dopamine precursor dihydroxyphenylalanine, which is used in Parkinson's disease, can also cause symptoms similar to those of schizophrenia.
In schizophrenia, there is an increase in activity (excess) of dopamine in mesolimbic brain structures (presumably responsible for positive symptoms, such as hallucinations) and its decrease (deficiency) in mesocortical structures, the prefrontal cortex (possibly responsible for negative symptoms and cognitive disorders).
The prefrontal cortex, and especially the dorsal lateral part of it, is probably directly related to the manifestations of schizophrenia.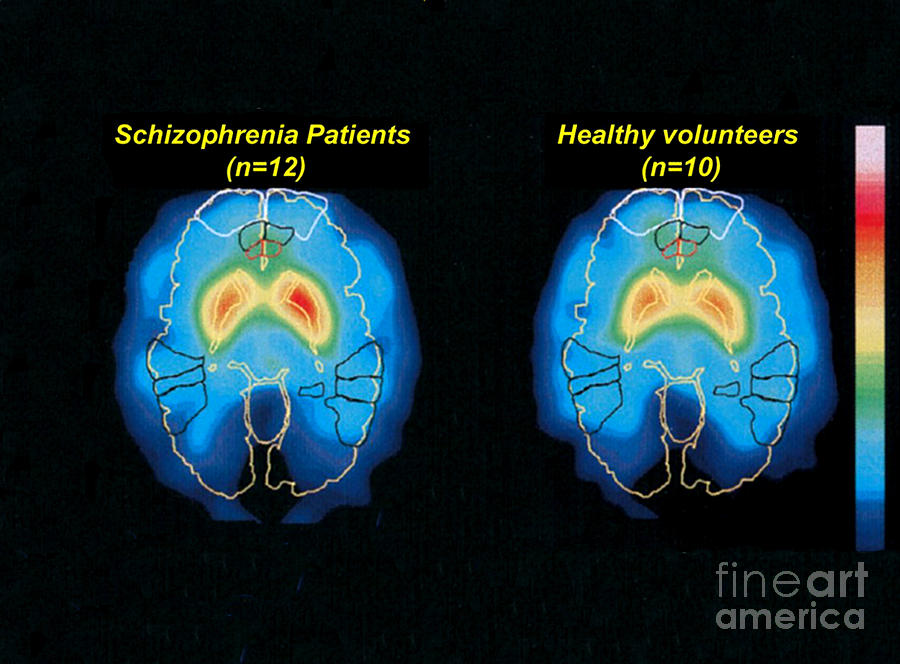 The defeat of this area leads to functional manifestations similar to the negative symptoms of schizophrenia.
The defeat of this area leads to functional manifestations similar to the negative symptoms of schizophrenia.
The evolution of the dopaminergic theory of the pathogenesis of schizophrenia has shifted the focus from the mediator to the receptor component of the dopamine system.
With the improvement of neuroimaging methods, it became possible to directly determine the binding parameters of receptors and receptor targets of psychopharmacological drugs.
An informative approach to assessing the activity of the dopaminergic system in schizophrenia is based on the use of ligands that selectively interact with D2 receptors and make it possible to determine their ability to bind.
By comparing the number of occupied receptors before and after drug administration, it is possible to estimate the ratio of dopamine release and reuptake (Ann S., Coyle J., 2007). It turned out that D2 receptors, after interacting with the ligand, inhibit adenylate cyclase, mediating their action through Gi proteins.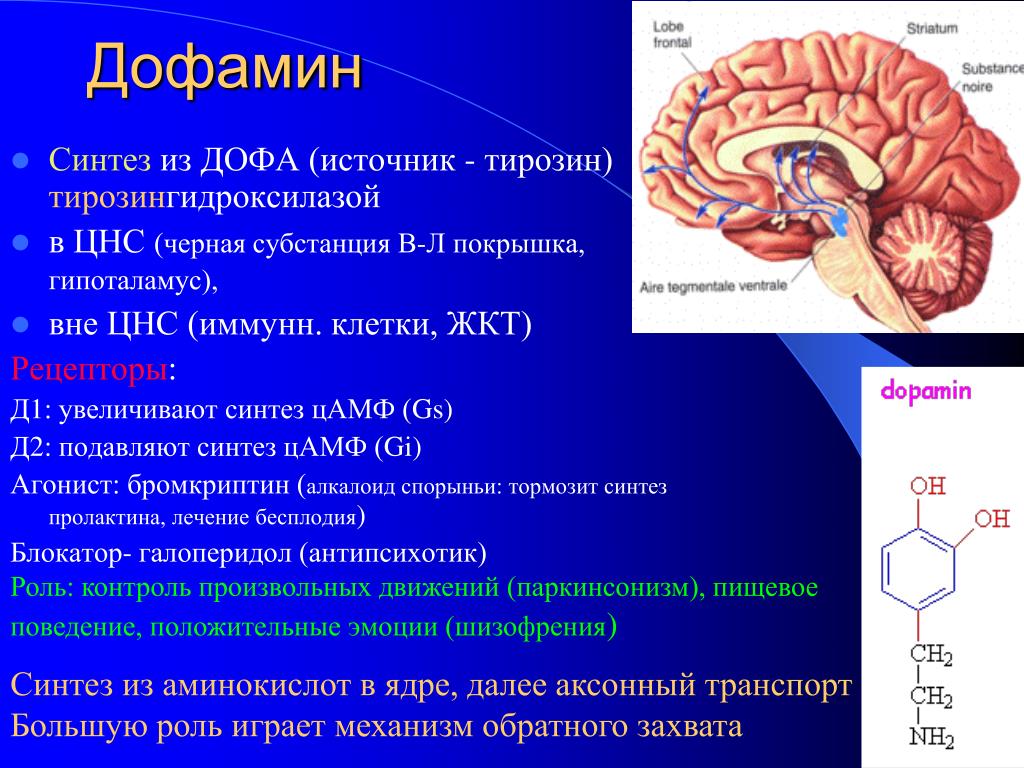 D2 receptors are suppressed by low concentrations of antagonists, and a functional decrease in dopamine activity occurs.
D2 receptors are suppressed by low concentrations of antagonists, and a functional decrease in dopamine activity occurs.
In modern works on the pathogenesis of schizophrenia, much attention is paid to the analysis of the density and ratio of different types of dopaminergic receptors.
Many researchers believe that a change in the ratio between different types of dopamine receptors underlies the pathogenesis of schizophrenia. Suppression of the functions of D1 and D2 receptors leads to a violation of various forms of stereotyped motor activity. An unbalanced increase in the functions of dopamine-sensitive receptors (mainly D2-type) probably also plays a large role in the pathogenesis of schizophrenia.
The dorsolateral prefrontal cortex, in particular responsible for working memory and executive functions, is dominated by D1-type dopamine receptors. It should be noted that the activity of the cerebral cortex affects the release of dopamine in the striatum, and, on the contrary, an increase in dopaminergic irradiation to the cortex from the subcortical structures leads to an exacerbation of the productive symptoms of schizophrenia.
The literature on the role of D1 receptors in schizophrenia is extremely contradictory.
According to most researchers, D 1-receptors are not damaged in schizophrenia , however, in some studies, a decrease in their density (possibly also D2) in the cortex of the frontal lobes was noted These changes are especially noticeable with severe negative symptoms. In the context of the above, let us recall the decrease in dopaminergic activity between the mesocortical region and the prefrontal cortex. From this we can conclude that the appointment of neuroleptics such as haloperidol, due to the blockade of D1 receptors, leads to an increase in negative symptoms and, possibly, cognitive deficits. 9 D 1 - receptors in the prefrontal cortex of the brain, there is a deterioration in working memory .
Decreased density of D1 receptors in the cortex of the frontal lobes
- Negative symptoms
- Cognitive impairment
Increased density of D2 receptors in the limbic system
- Positive symptoms
The results of some studies suggest that the density of D2 receptors in patients with schizophrenia is increased by almost 10% compared with the control group.
Autoradiography (positron emission tomography - PET) revealed differences in the expression of D2 receptors in the supragranular and granular layers of the temporal cortex of the brain of patients with schizophrenia, an increase in the number of dopaminergic neurons in the limbic system. However, other studies have not confirmed this fact.
Hyperactivity of D2 receptors or increased dopaminergic activity in the subcortical structures of the brain, more precisely in the mesolimbic system, according to most researchers, is one of the main links in the pathogenesis of positive symptoms in schizophrenia. Blockade of D2 receptors leads to a weakening of the latter.
Examination of the brain of patients with schizophrenia after their death revealed an increase in the density of receptors D 2- types in various structures, with the most pronounced changes found in the left amygdala , part of the limbic system, and temporal lobe . However, due to the fact that neurons decay after death, the true concentration of dopamine in brain tissues is almost impossible to determine.
Lifetime neuroimaging (PET, SPECT) methods aimed at studying dopaminergic processes occurring in schizophrenia in the striatum demonstrated that the focus of research should be shifted from postsynaptic D2 receptors to presynaptic ones. It is on these receptors that most researchers have found significant changes (Karlsson A., Lekrubier I., 2004).
In schizophrenia, an increase in the number of dopamine receptors in the caudate nucleus was found, and in the striatum, the number and density of receptors of the type D 4 , which is normally found only in small quantities, increases 4-5 times.
The D4 dopamine receptor has the highest density in the limbic cortex of the brain and has an increased affinity for clozapine (the D4 receptor is controlled by a gene located on the 11th chromosome - p15.5 polymorphic region). Based on the foregoing, it can be assumed that minor types of dopamine receptors are activated in schizophrenia.
For a long time it was not clear what causes an increase in the number of dopamine receptors in schizophrenia. Whether this fact is due to the process of the disease itself or is it the result of treatment with psychotropic drugs. Recently, quite convincing data have been obtained indicating that an increase in the number of dopamine receptors in schizophrenia is not a consequence of pharmacotherapy with psychotropic drugs.
A high activity of the system sensitive to dopamine to hormonal influences has been established. Modification of postsynaptic dopamine receptors by female sex hormones (estrogens and progesterone) has been shown. The lack of these hormones reduces, and the excess, on the contrary, enhances the response of dopamine receptors to interaction with the ligand.
Dopaminergic hyperactivity largely explains the development of positive symptoms, while some researchers associate the occurrence of negative symptoms with hypofunction of the dopamine system. (Carpenter W., Buchanan R., 1994).
Dopamine receptor agonists that activate the dopaminergic system include: apomorphine , pergolide, bromocriptine , quinagolide, cabergoline, aminotetralin -tetrahydronaphthalene (ADTH), amphetamine, methylphenidate, cocaine . Abuse of these substances can provoke psychosis, in the clinical picture of which productive symptoms are expressed, in particular, paranoid syndrome. In addition, the use of psychostimulants can cause a relapse of schizophrenia.
Dopamine receptor agonists
- Apomorphine
- Bromocriptine
- Cabergoline
- Amphetamine
- Methylphenidate
- Cocaine
- L-dopa
In the literature on the dopamine theory of the pathogenesis of schizophrenia, one can find statements that the use of amphetamine provokes a significantly greater release of dopamine in patients with schizophrenia than in healthy people. The "amphetamine effect" manifests itself more clearly during an exacerbation of productive psychotic symptoms.
Some investigators have found an association between certain manifestations of negative symptoms (affective flattening) and a decrease in dopaminergic transmission in the striatum. However, it should be noted that such signs of negative symptoms as aboulia-anhedonia and cognitive disorders such as impaired attention do not correlate with the D2 receptor density index.
The relationship between the activity of the dopaminergic system of the brain and the productive and negative symptoms of schizophrenia is shown in Table 11.
Some researchers believe that dopamine receptors are hypersensitive (overactive) in schizophrenia, but the level of dopamine in the brain tissues is not increased.
Table 11. Correlation of positive and negative symptoms of schizophrenia with the level of activity of the dopaminergic system of the brain0051 Positive symptoms Negative symptoms Increased activity of dopaminergic neurons in the limbic structures of the brain Decreased activity of dopaminergic neurons in the prefrontal cortex Increased activity of dopaminergic neurons in Broca's area, in the superior temporal gyrus (auditory hallucinations) Decreased dopaminergic activity in the anterior cingular gyrus (attention deficit, thinking disorder) Increase in the number of dopamine receptors D2 and D4 Normal or reduced dopamine D2 receptors Low platelet MAO activity High platelet MAO activity Increased activity of hippocampal neurons Decreased activity of hippocampal neurons Changes at the neurochemical level are more pronounced than at the structural level Structural rather than functional (neurochemical) changes Administration of the dopamine precursor DOPA or the substances noted above that enhance the release of the mediator from presynaptic endings (amphetamine), i. At first, psychomotor agitation develops, and then monotonous stereotypical movements are observed. The plant analogue of dopamine, mescaline (trimethoxyphenylalanine), causes hallucinations that resemble hallucinations in schizophrenia. It is known that currently no pharmacological agents have been found that react specifically with respect to various isoforms of D2 receptors. It is interesting to note that a number of dopamine receptor agonists are able to reduce the severity of negative symptoms in schizophrenia, while antagonists, on the contrary, increase it. This fact may indicate the opposite direction of the links in the pathogenesis of positive and negative symptoms of schizophrenia. However, it is possible that in schizophrenia, an increase in the activity of the dopaminergic system in the anterior cingulate cortex and other limbic structures of the brain leads to the occurrence of positive symptoms, while negative symptoms appear as a result of a decrease in the activity of dopaminergic neurons in the prefrontal cortex of the brain. Psychotropic substances with the ability to inhibit dopaminergic receptors are widely used in the treatment of schizophrenia. Many antipsychotics are structurally similar to the dopamine molecule, so they affect postsynaptic receptors for this neurotransmitter and can block them. The most well-known dopamine D2 receptor antagonists include: haloperidol, spiroperidol, phenothiazine derivatives (chlorpromazine, perphenazine), clozapine, sulpiride. These substances can cause extrapyramidal disorders, the genesis of which is associated with the blockade of dopamine receptors, i.e. a decrease in their activity, similar to the effect in Parkinson's disease, the symptoms of which include extrapyramidal disorders and where death or weakening of the activity of dopaminergic neurons is noted. Note that as a result of taking atypical antipsychotics, D2 receptors are blocked differentially. Some drugs, for example, clozapine, blockade of D2 receptors in the temporal cortex (amygdala, hippocampus), while moderate affinity is found here. Risperidone shows a higher affinity for D2 receptors located in the limbic system. In the brain of patients with schizophrenia, there is a pronounced decrease in the activity of MAO , the main enzyme that oxidizes catecholamines, which, in turn, may be the cause of the accumulation of mediators, in particular dopamine. If four isoforms of MAO are described in a healthy person (1, 11 - alpha, 11 - beta, 111), then in schizophrenia, form 111 was not found and other forms were significantly modified. Along with a general decrease in MAO activity in schizophrenia, a significant increase in the metabolism of catecholamines along the minor quinoid pathway was found (normally, no more than 5% of catecholamines are oxidized along the quinoid pathway). Despite numerous data indicating the important role of dopamine in the genesis of schizophrenia, a number of facts cast doubt on the validity of this hypothesis. We present here only a few of them. The improvement in the condition of patients with schizophrenia begins much later than the blockade of dopamine receptors, i.e. the clinical effect is at odds with the pharmacological mechanism of drug action. Antipsychotics do not always have an effect on the symptoms of schizophrenia, even with significant (over 90%) blockade of dopamine receptors and can reduce it with a slight blockade, as, for example, in the case of clozapine, which blocks only 20-60% of D2 receptors. According to some psychiatrists, the action of antipsychotics is due to the blockade of D2 receptors, but this effect indirectly triggers a change in other neurotransmitter systems. It is known that dopamine-sensitive neurons modulate the activity of other neurotransmitters, for example, the GABAergic activity of the prefrontal cortex, on the other hand, serotonin-sensitive neurons affect the activity of dopamine-sensitive neurons of the mesolimbic system. Note that the clinical efficacy of some modern antipsychotics is more associated with the effect on serotonin receptors than dopamine. In schizophrenia, it was not possible to detect a primary defect in dopaminergic transmission, due to the fact that the functional assessment of the dopaminergic system, the researchers received different results. Attempts to determine in vivo levels of dopamine and its metabolite, homovanillic acid, in blood plasma, urine, and cerebrospinal fluid have also yielded conflicting results, probably due to the large volume of biological media leveling those changes that may be a reflection of dysfunction of the dopaminergic system in schizophrenia. There is information in the literature that refutes the presence of an increase in dopamine metabolism in schizophrenia. It is noted that at present there is no convincing evidence of a general hyperactivity of the dopaminergic system in schizophrenia. This is also indicated by the fact that dyskinesia, which may reflect an increase in dopaminergic activity, is rare in schizophrenia. Back to Table of Contents 02/19/2022 Dopamine is a substance found in most living beings and is responsible for the feeling of reward. This is one of the so-called hormones happiness. The fact that there is a fair amount of this substance is of decisive importance for a person. Both its excess and defect can cause serious harm to those who suffer from it, and therefore its regulation is of paramount importance. In addition to reward circuits, dopamine is involved, among others, in the functions of attention, motivation, memory, pleasure and motor control . Dopamine is a neurotransmitter in the central nervous system . Let's see why dopamine can be more than is considered normal: If you have excess dopamine, you may observe the following symptoms: There are some changes associated with excess dopamine: Dopamine regulates very important functions such as memory, sleep or mood. That's why it's so important to regulate dopamine levels. There are different ways to reduce this excess dopamine: Medications Antipsychotics are drugs that lower dopamine levels. e. that increase the level of the neurotransmitter can cause a state close to the clinical picture of schizophrenia.
Therefore, drugs for the treatment of schizophrenia should increase the activity of the dopaminergic system in the prefrontal cortex of the brain, but weaken its activity in the limbic structures.
It is interesting to note that these reactions are characteristic of muscle tissue, and not of brain tissue. After indolization and several redox reactions, a number of biologically active compounds are formed, the effects of which differ from the effects of conventional mediators. Thus, in particular, adrenochrome (“substance of fear”) is formed, the accumulation of which in the brain tissues causes a feeling of fear and adrenolutin, which removes these sensations.
Too much dopamine
Causes of excess dopamine
Symptoms of excess dopamine
Diseases caused by excess dopamine
In fact, his treatment is levodopa, a drug that is responsible for lowering dopamine levels.
How to regulate dopamine levels?