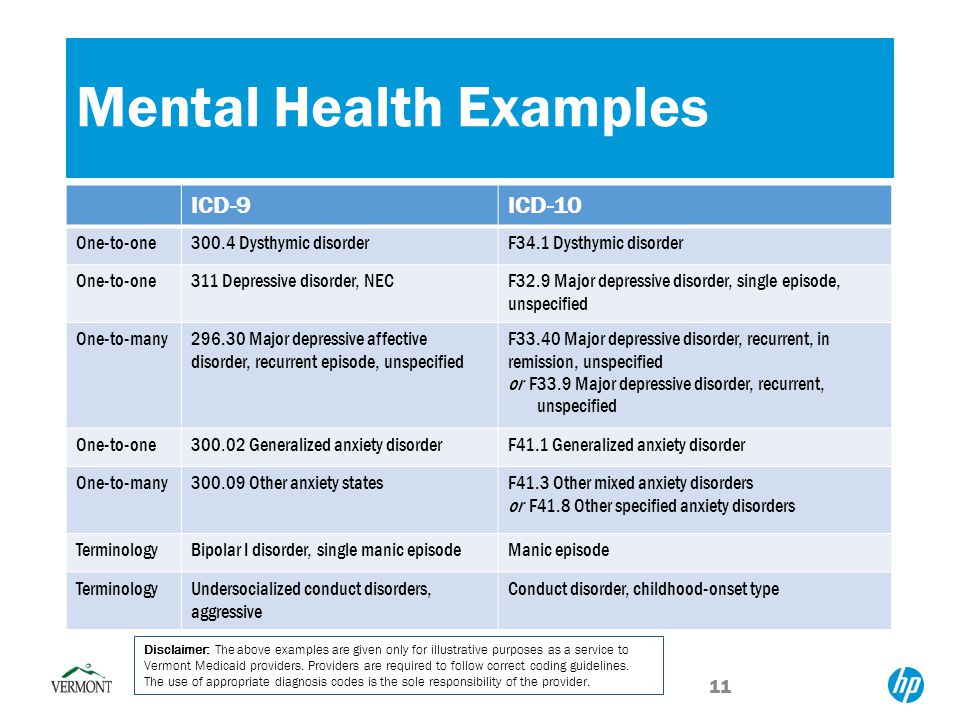
Example of major depressive disorder
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid.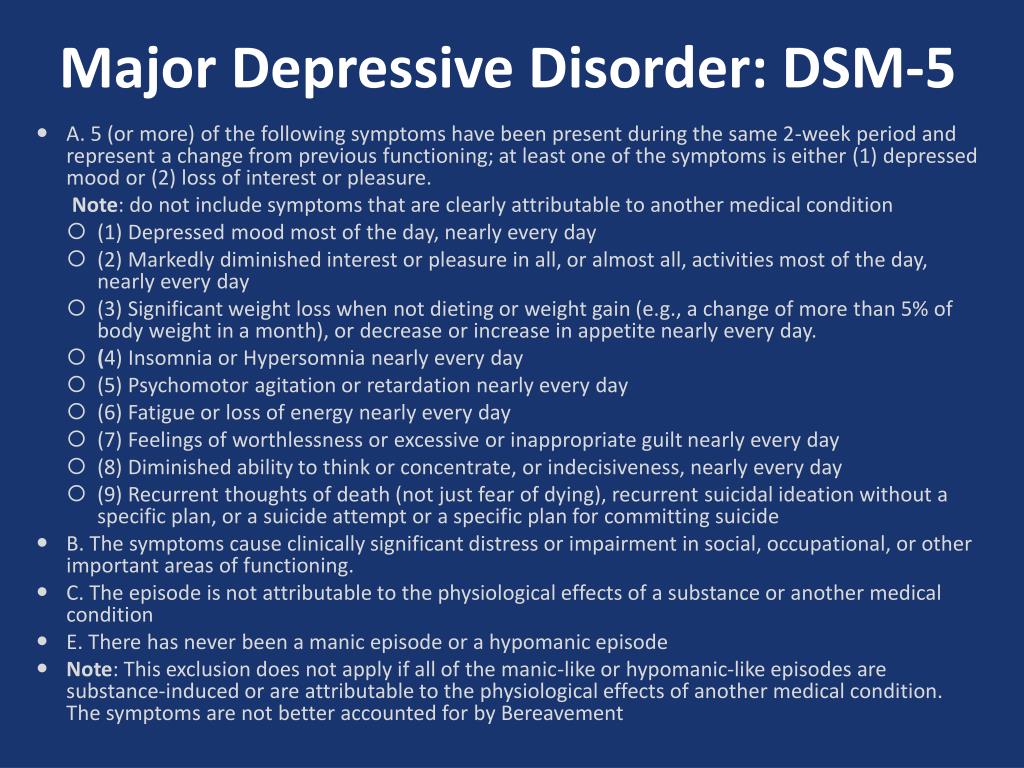 If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.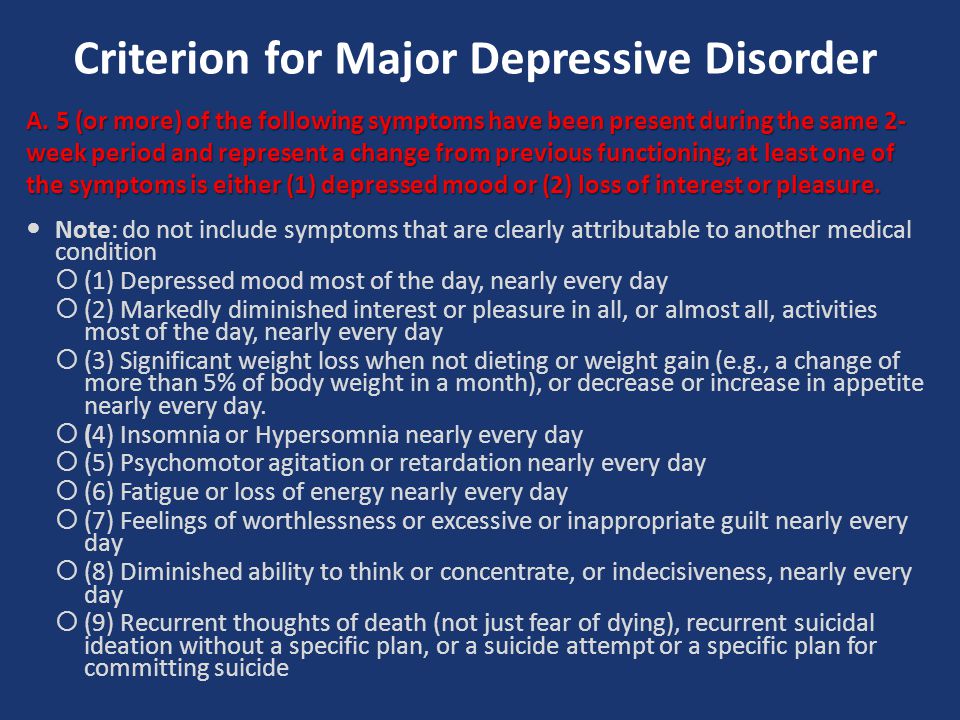
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.
-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly.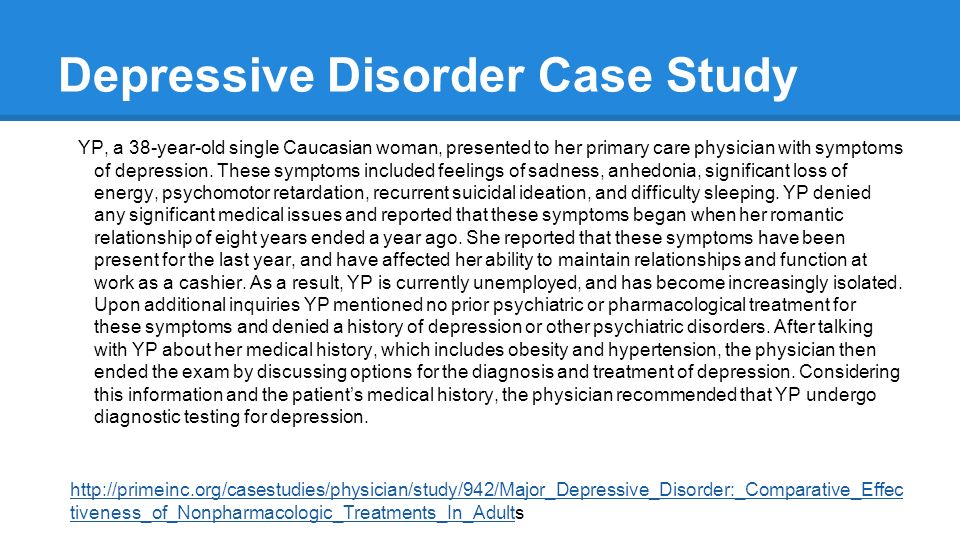 Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Types of depression - iFightDepression [EN]
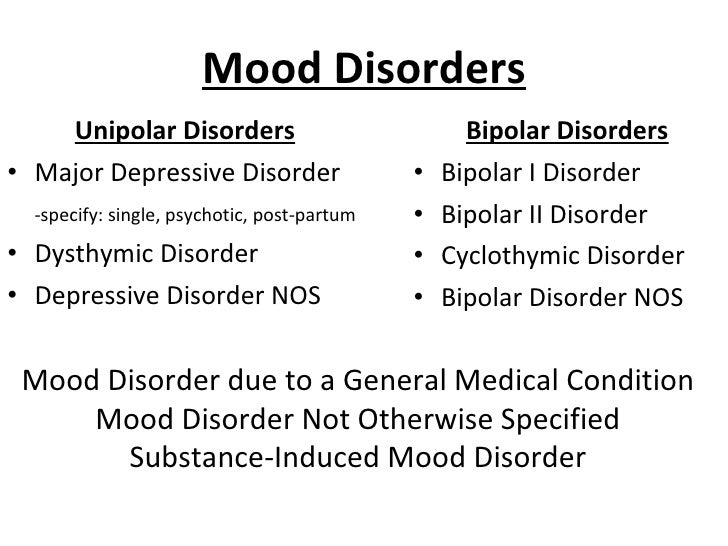
There are different types of depression, which are different.
Signs and symptoms vary in number, time, severity and frequency, but are generally very similar. Because different types of depression are treated differently, it is important to pinpoint the type of depression. Depending on gender, age and cultural characteristics, people have different symptoms and severity of depression.
Neurotic, reactive (minor) depression is treated with psychotherapy.
Somatic and psychotic - medication.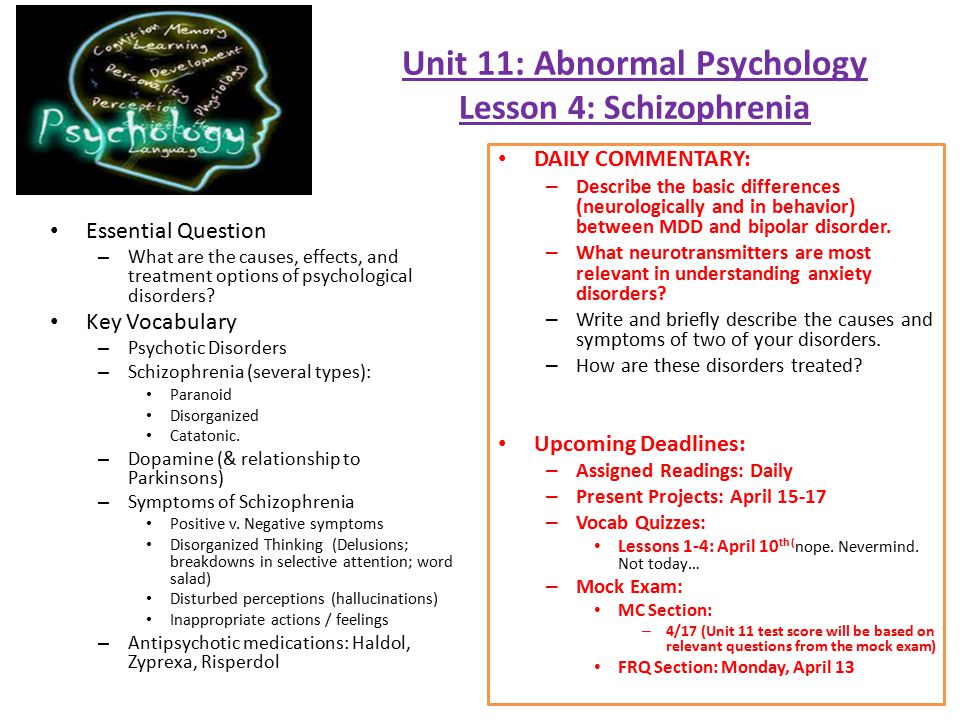 These terms are used by psychiatrists.
These terms are used by psychiatrists.
Studies have shown that depression has a phasic course. Periods of normal mood alternate with depressive episodes. Sometimes, instead of a depressive phase,
there may be a manic phase, which is manifested by irritability and high mood. If so, then it is not depression, but bipolar disorder (a more serious illness).
1. Depressive episode
The most common and typical form of depression is the depressive episode. An episode lasts from a few weeks to a year, but is always longer than 2 weeks. A single depressive episode is called a unipolar episode. Approximately one third of affected people experience only one episode, or "phase", during their lifetime. However, if a person does not receive appropriate treatment for depression, there is a risk of recurrent depressive episodes in the future. Depressive episodes always affect a person's performance to one degree or another.
2. Intermittent (recurrent) depressive disorder
When a depressive episode recurs, it is recurrent depressive disorder or major depressive disorder, which usually begins in adolescence or early adulthood.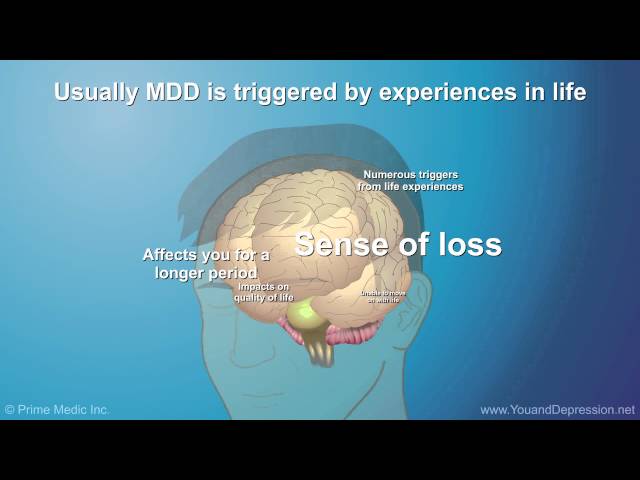 With this kind of depression, depressive phases, which can last from several months to several years, alternate with phases of normal mood. This type of depressive disorder can seriously affect performance and is unipolar in nature (no manic or hypomanic phase). This is the so-called "classic" or "clinical" depression.
With this kind of depression, depressive phases, which can last from several months to several years, alternate with phases of normal mood. This type of depressive disorder can seriously affect performance and is unipolar in nature (no manic or hypomanic phase). This is the so-called "classic" or "clinical" depression.
3. Dysthymia
Dysthymia presents with milder and less severe symptoms than a depressive episode or recurrent depression. However, the disorder is permanent, with symptoms lasting much longer, at least 2 years, sometimes decades, which is why it is called "chronic depression". This disorder is unipolar and also affects performance. This type of depression sometimes develops into a more severe form (major depressive episode) and if this happens it is called double depression.
4. Bipolar depression, type I
This is the type of depression in bipolar disorder, formerly called manic-depressive illness, and is less common than unipolar depression.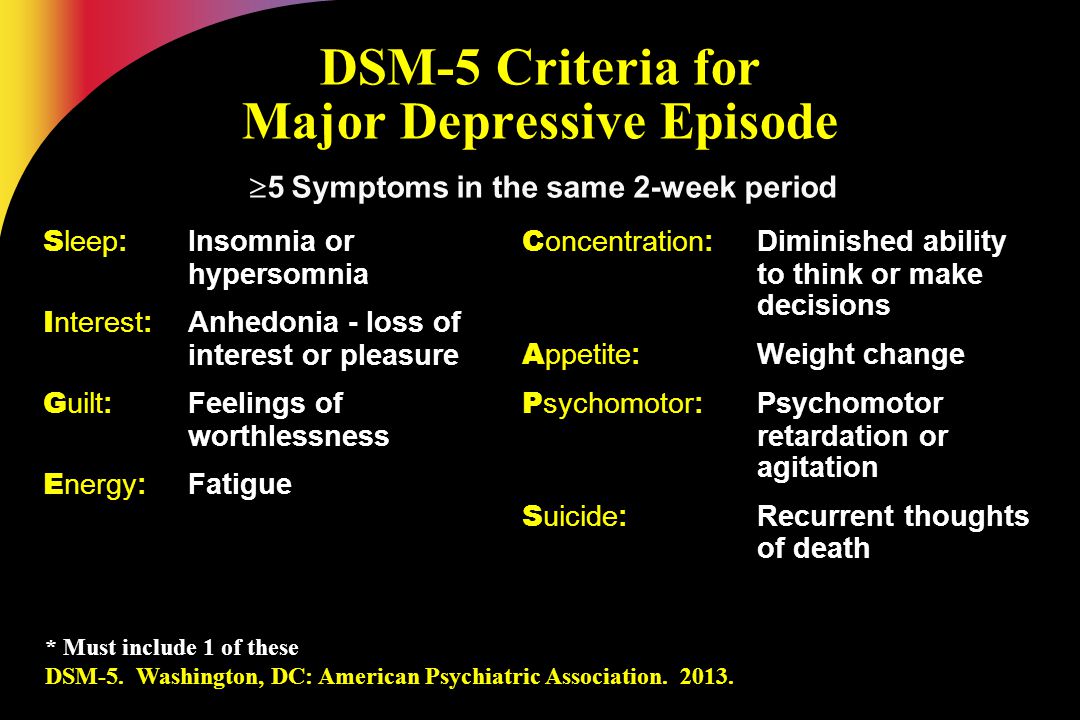 It consists of alternating depressive phases, phases of normal mood and so-called manic phases.
It consists of alternating depressive phases, phases of normal mood and so-called manic phases.
Manic phases are characterized by excessively high mood associated with hyperactivity, anxiety, and decreased need for sleep.
Mania affects thinking, judgment and social behavior causing serious problems and difficulties. When a person is in a manic phase, he makes frequent casual unsafe sex, makes unwise financial decisions. After a manic episode, such people often experience depression.
The best way to describe these "emotional upheavals" is "to be on top of the world and fall into the depths of despair".
Symptoms of the phases of depression in bipolar disorder are sometimes difficult to distinguish from unipolar depression.
5. Bipolar depression type II
More like recurrent depressive disorder than bipolar disorder. In this disorder, multiple depressive phases alternate with phases of mania, but with less pronounced euphoria. During these phases, family and loved ones may even mistakenly assume that the person is doing well.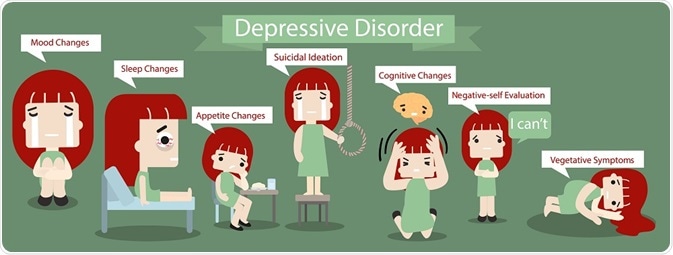
6. Mixed anxiety-depressive disorder
In anxiety-depressive disorder, the clinical picture is very similar to depression, however, in depression, depressive syndromes always come first. In this case, both anxious and depressive symptoms are evenly combined.
7. Depressive psychotic episode
A special form of depressive episode is psychotic or delusional depression. Psychosis is a condition in which people see or hear things that do not exist (hallucinations) and/or have false ideas or beliefs (delusions). There are various types of delusions such as self-accusation for no reason (delusion of guilt), financial ruin (delusions of poverty), feeling of an incomprehensible illness (hypochondriac delusions). People with delusional depression almost always require inpatient psychiatric treatment. Psychotic episodes can be either unipolar or bipolar.
8. Atypical depression
This type of depression is characterized by hypersensitivity and mood swings, overeating and drowsiness, panic attacks. This type of depression is mild and can be bipolar.
This type of depression is mild and can be bipolar.
9. Seasonal depressive disorder
This type of depression is similar to atypical depression and comes on seasonally with climate change, usually in autumn or winter. Usually, when the season ends, people return to normal functioning again.
10. Brief depressive disorder
This is a milder variant of depression that more often affects young people and is characterized by short depressive episodes lasting less than 2 weeks.
Major depressive disorders (clinical depression)
Depression is different from normal mood swings and short-term emotional responses to everyday problems. Prolonged moderate to severe depression can become a serious illness. This results in patients suffering greatly and doing poorly at work, at school and have problems in their families. At its worst, depression can lead to suicide.
Depression is a common illness worldwide, affecting more than 264 million people. Major depressive disorder is one of the most common forms of mental illness, affecting approximately one in six men and one in four women in their lives.
Major depressive disorder is one of the most common forms of mental illness, affecting approximately one in six men and one in four women in their lives.
Major depressive disorder (MDD) is a severe condition characterized by low mood, decreased interests, poor cognitive function, and autonomic symptoms such as disturbed sleep or eating. MDD can develop in one in six adults during their lifetime and affects about twice as many women as men.
Major symptoms of depressive disorder
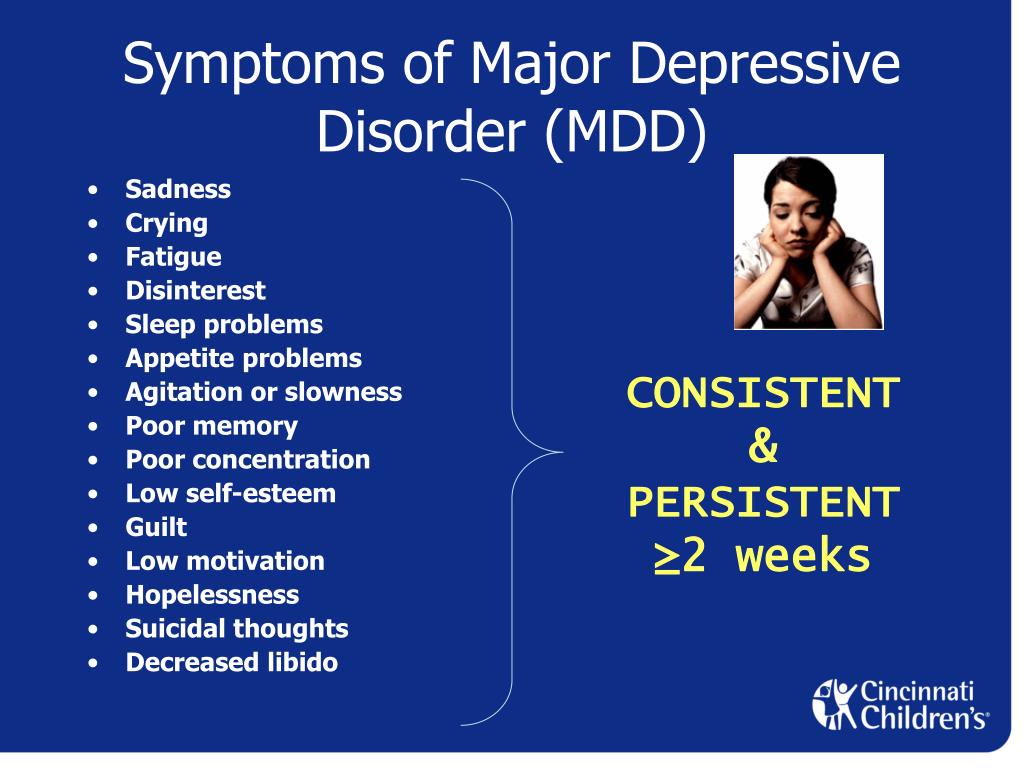
Symptoms of major depressive disorder (MDD) may include:
- depression almost every day
- loss of interest in activities you once enjoyed
- changes in appetite or weight
- sleep problems
- feeling of laziness or restlessness
- low energy
- feelings of hopelessness or worthlessness
- trouble concentrating
- frequent thoughts of death or suicide
Depressive relapses:
This is a highly relapsing condition: at least 50% of people recovering from a first episode of depression have at least one additional episode in their lifetime, and about 80% of people have a history of two recurring episodes.
Episodes typically recur within five years of the first episode, and the average person with a history of depression will have five to nine depressive episodes in their lifetime.
Symptoms of recurrent depression:
- difficulty concentrating
- disturbed sleep
- decreased energy level
- permanent light alarm
Major depression in adults:
Depression is a common adult disorder that often leads to poor quality of life and impaired role functioning. Depression is also associated with high rates of suicidal behavior and death. When depression occurs in the context of a medical illness, it is associated with increased healthcare costs, longer hospital stays, poor collaboration in treatment, etc.
Causes of depression in adults may be related to the difficulty of changing roles:
- low education and low income
- early pregnancy and childbirth
- divorces
- unstable operation
- highly competitive and hard work
Major symptoms of depression in adults include:
- Mostly sad or depressed mood
- Loss of interest or pleasure and avoidance of social gatherings
- Decreased energy and frequent fatigue
- Decreased concentration and attention
- Decreased self-esteem and self-confidence
- Thoughts on guilt and unworthiness
- A gloomy and pessimistic view of the future
- Thoughts or actions of harming oneself or suicidal thoughts
- Sleep disturbance or insomnia
- Pronounced or reduced appetite
DSM-5 Criteria for Major Depressive Disorder
According to the DSM-5, the following criteria must be met for a diagnosis of major depression:
At least five of the following symptoms must have been present for at least two weeks and reflect a change in previous functionality.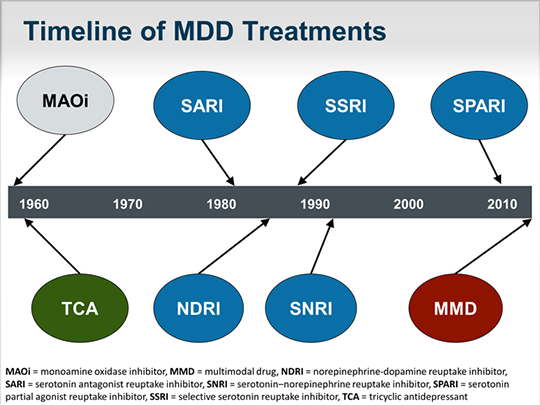 In addition, at least one of the symptoms is a low mood or loss of interest or pleasure.
In addition, at least one of the symptoms is a low mood or loss of interest or pleasure.
- The person is depressed most of the day, almost every day, as noted by himself or others.
- He or she is not interested in all or most activities most of the day, almost every day.
- Every day a person gains or loses a large amount of weight or has a decreased or increased appetite.
- Almost every day he or she suffers from insomnia or hypersomnia.
- Every day a person experiences psychomotor disturbances that are visible to others and can also be reported.
- Almost every day he or she feels exhausted or tired.
- Almost every day a person has thoughts of worthlessness or guilt.
- Every day a person's ability to think, concentrate, or make judgments deteriorates.
- He or she has recurrent suicidal thoughts, suicidal thoughts (without a definite plan), a suicide attempt, or a definite plan to commit suicide.
- The symptoms listed above cause clinical distress or interfere with daily activities.
- The episode of depression is not associated with the physiological effect of the drug or other disease.
- The onset of the episode is not better explained by specific or unspecified schizophrenia spectrum illness or other psychotic disorders.
- The person has never had a manic or hypomanic episode.
The diagnostic code for major depressive disorder is based on the frequency of recurrent episodes, the severity of the episodes, the presence of psychotic characteristics, and the state of remission. Below are the varieties of depression:
Severity of depression:
- Minor
- Moderate
- Heavy
- Psychotic
- In partial remission
- In complete remission
- Undefined
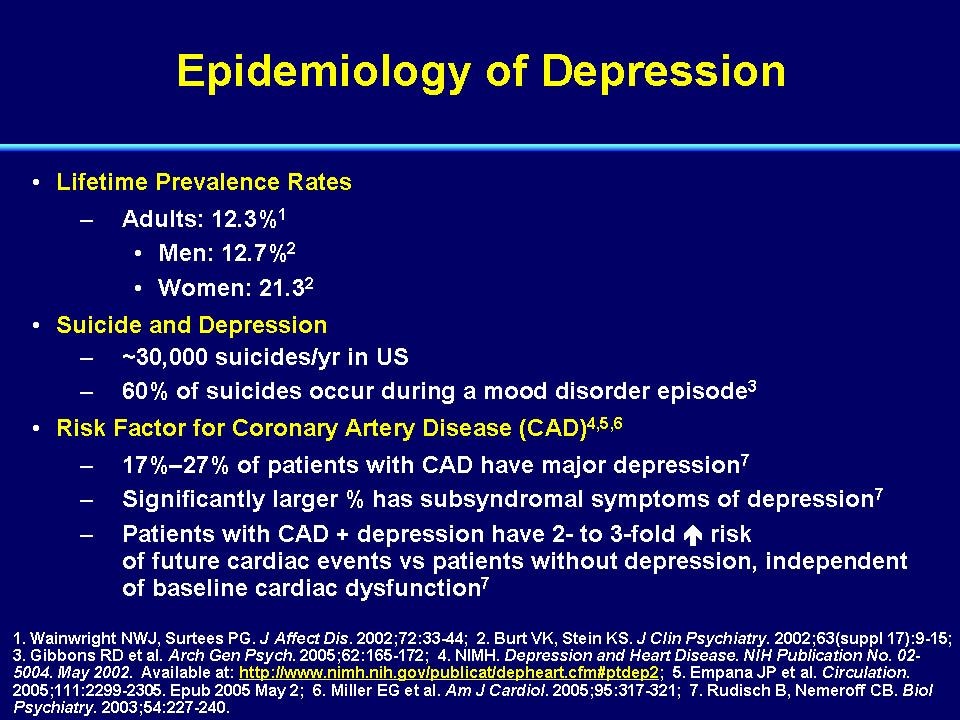
Epidemiology
Major depressive illness is a common mental illness. Its lifetime prevalence ranges from 5 to 17 percent.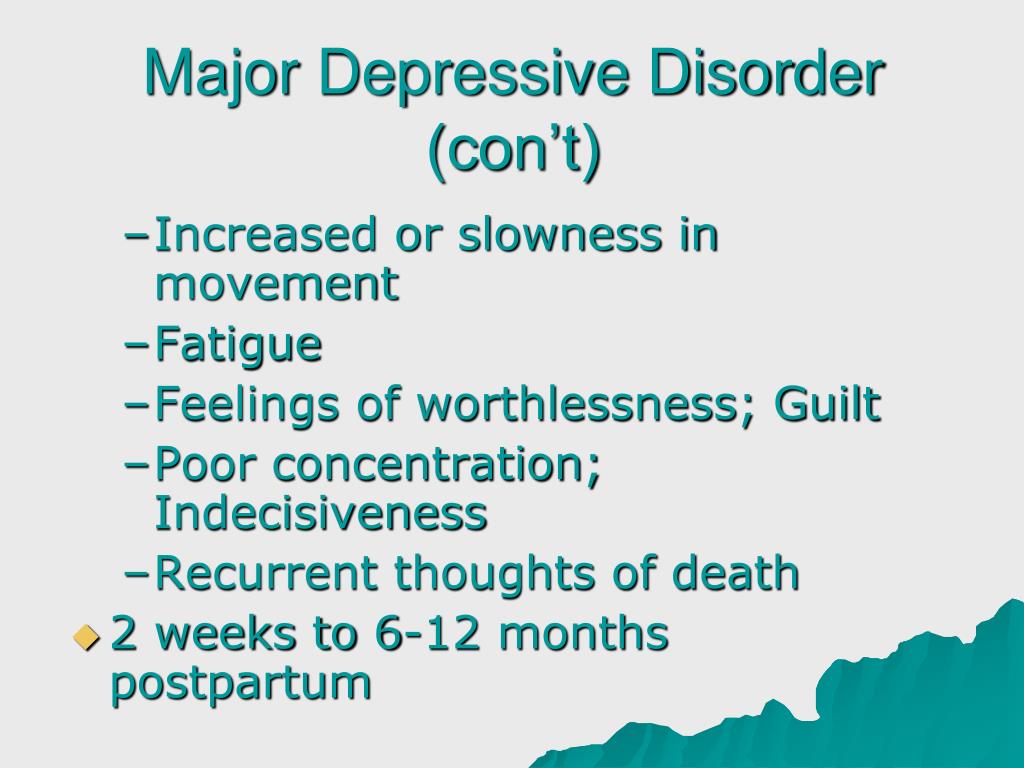 The incidence in women is about twice as high as in men. This is due to hormonal variations, the consequences of childbearing, different psychological pressures in men and women, and a behavioral model of learned helplessness. Although the median age of onset is around 40 years old, new studies show an increase in the incidence among younger populations due to the use of alcohol and other psychoactive substances.
The incidence in women is about twice as high as in men. This is due to hormonal variations, the consequences of childbearing, different psychological pressures in men and women, and a behavioral model of learned helplessness. Although the median age of onset is around 40 years old, new studies show an increase in the incidence among younger populations due to the use of alcohol and other psychoactive substances.
MDD is more common in divorced, separated, or bereaved individuals who do not have meaningful interpersonal interactions. There is no difference in the prevalence of MDD between races or socioeconomic status. People with MDD often have comorbidities such as substance abuse, panic disorder, social anxiety disorder, and obsessive-compulsive disorder.
The presence of these comorbidities in people with MDD increases the risk of suicide. Depression is more common in older people with underlying medical problems. Depression is more common in rural areas than in cities.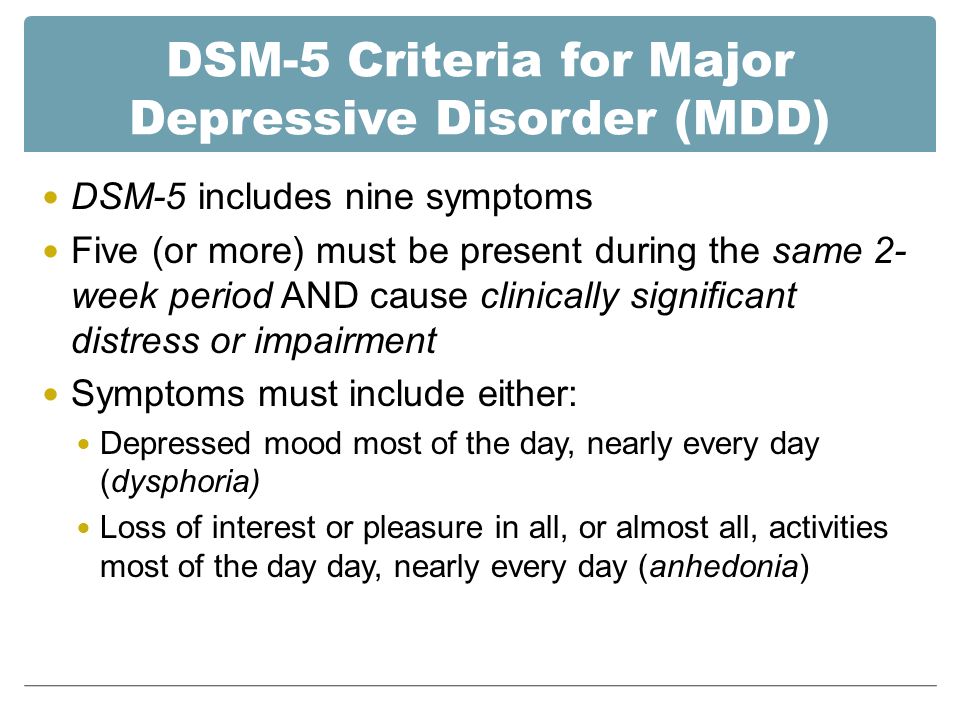
Pathophysiology of major depressive disorder
The genesis of major depressive disorder is believed to be multifaceted, with biological, genetic, environmental and psychological factors at play. It used to be thought that MDD was caused mainly by abnormalities in neurotransmitters, especially serotonin, norepinephrine, and dopamine.
This has been demonstrated by the use of several antidepressants in the treatment of depression, such as selective serotonin receptor inhibitors, serotonin-norepinephrine receptor inhibitors, and dopamine-norepinephrine receptor inhibitors. Serotonin metabolites have been found to decrease in people who have had suicidal thoughts. However, recent hypotheses suggest that this is largely due to more complex neuroregulatory systems and brain circuits, leading to subsequent disruption of the neurotransmitter systems.
GABA, an inhibitory neurotransmitter, as well as glutamate and glycine, important excitatory neurotransmitters, have been shown to play a role in the genesis of depression.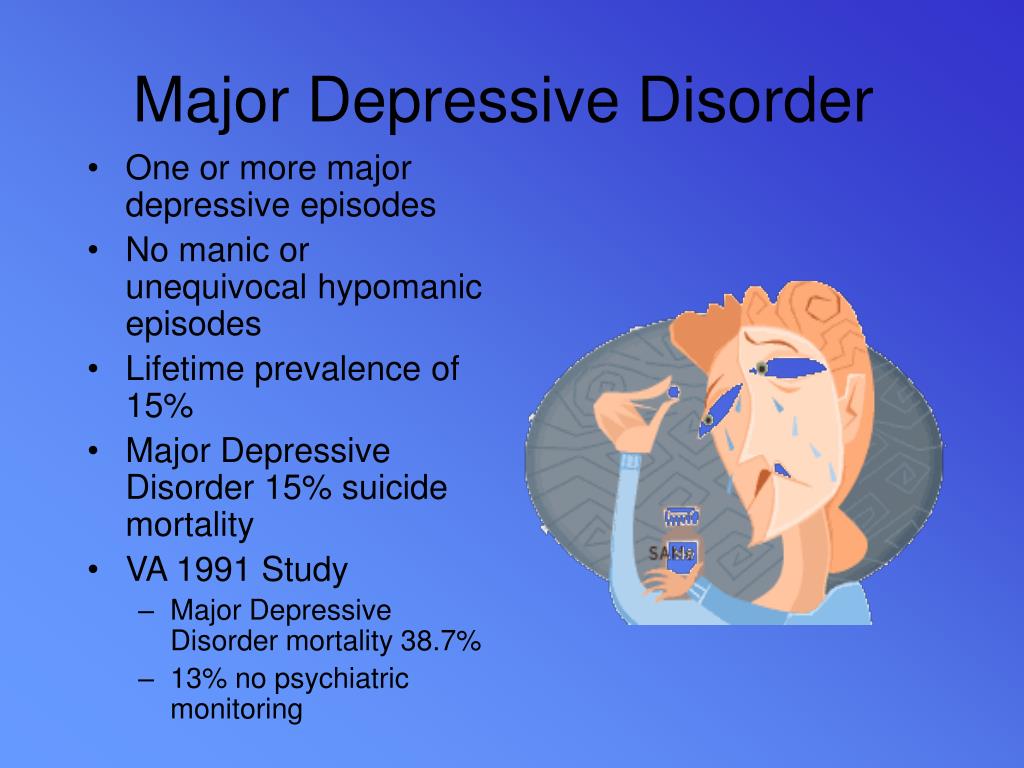 Depressed people have reduced plasma, cerebrospinal fluid, and brain levels of GABA. GABA is believed to act as an antidepressant by blocking the ascending monoamine pathways, including the mesocortical and mesolimbic systems.
Depressed people have reduced plasma, cerebrospinal fluid, and brain levels of GABA. GABA is believed to act as an antidepressant by blocking the ascending monoamine pathways, including the mesocortical and mesolimbic systems.
The antidepressant properties of drugs that oppose NMDA receptors have been investigated. Thyroid and growth hormone imbalances have also been linked to mood disorders. Numerous adversity and trauma in childhood have been linked to the development of depression later in life.
Severe early stress can cause dramatic changes in neuroendocrine and behavioral responses, leading to anatomical abnormalities in the cerebral cortex and severe depression later in life. Structural functional tomography of the brain in people with depression revealed greater hyperintensity in the subcortical regions and a decrease in the metabolism of the anterior brain regions on the left.
Family, adoption and twin studies have shown that genes play a role in the risk of depression. According to genetic studies, twins with MDD have a very high level of concordance, especially monozygotic twins. Life experience and personal qualities also have an impact.
According to genetic studies, twins with MDD have a very high level of concordance, especially monozygotic twins. Life experience and personal qualities also have an impact.
According to the theory of learned helplessness, the onset of depression is associated with the experience of uncontrollable events. Depression, according to cognitive theory, results from cognitive errors in those who are predisposed to depression.
Physical illnesses associated with depression
Physical sensations are especially common in depression and other mental illnesses. Although somatic symptoms are common in depressed individuals, they are of much lesser importance than major depressive symptoms in the diagnosis of depression.
The clinical stages of sad mood are characterized by both painful and non-painful bodily symptoms.
Major depressive disorder diagnosis
Major depressive disorder is a clinical diagnosis; this is mainly determined by the patient's medical history and assessment of mental status.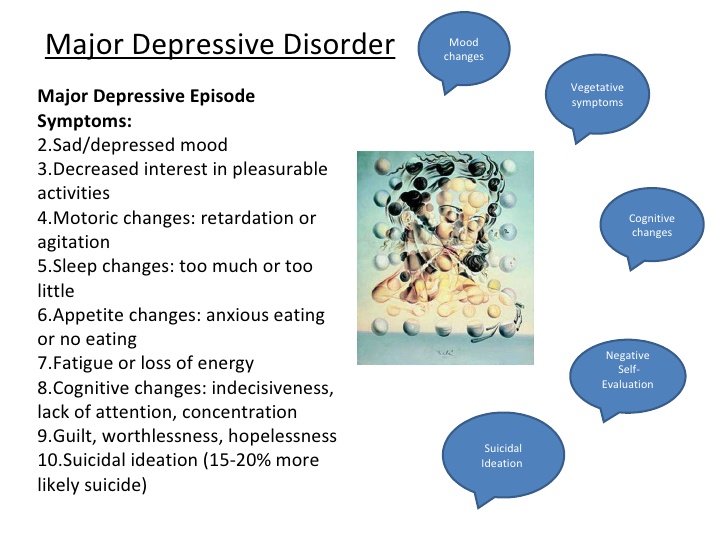 Along with symptomatology, the clinical interview should include medical history, family history, social history, and history of drug use. Related information from the patient's family/friends is an important component of the psychiatric evaluation.
Along with symptomatology, the clinical interview should include medical history, family history, social history, and history of drug use. Related information from the patient's family/friends is an important component of the psychiatric evaluation.
Although there are no objective tests to diagnose depression, routine laboratory tests such as CBC with a differential diagnosis, a comprehensive metabolic panel, thyroid-stimulating hormone, free T4, vitamin D, urinalysis, and toxicology screening are done to rule out organic or medical diseases. causes of depression.
People with depression often see their primary care physicians for medical problems related to their depression rather than seeking a mental health professional. In nearly half of the cases, patients deny experiencing depressive symptoms and are often referred to therapy by family members or sent by employers to be tested for social isolation and decreased activity. At each visit, it is critical to assess the patient for thoughts of suicide or murder.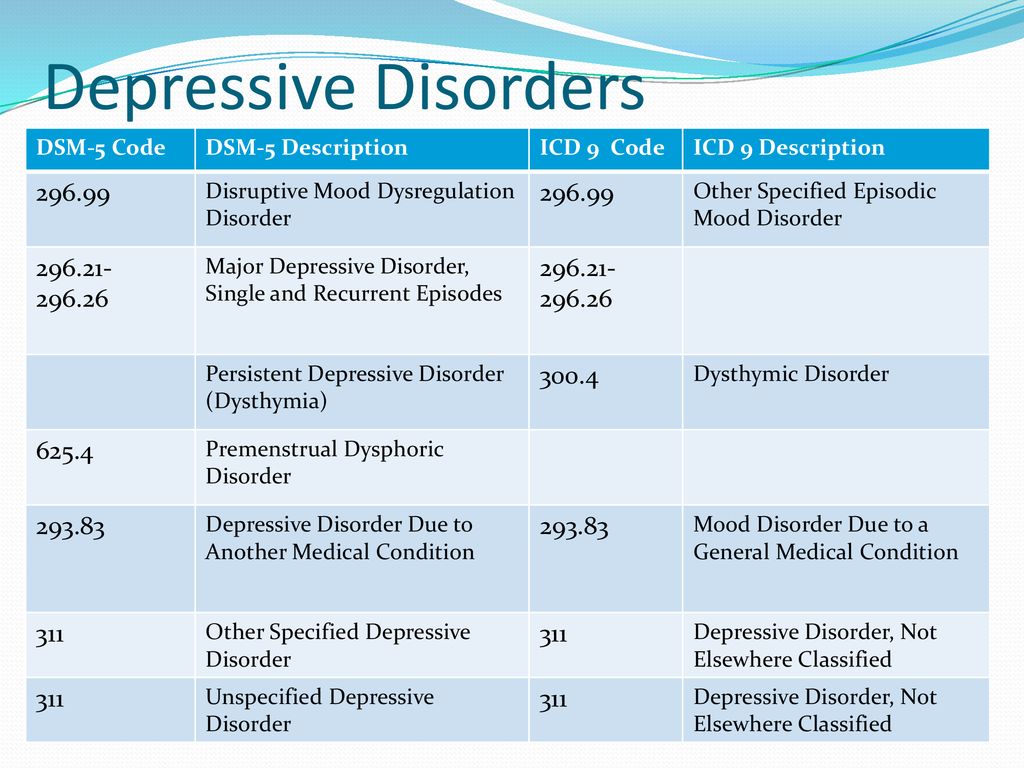
Being in a bad mood or feeling tense is common for all of us. When these feelings persist, you may suffer from depression or anxiety—or both. The self-assessment quizzes contain relevant questions to help you assess your current situation and develop a strategy to help you feel better sooner.
When you are going through a difficult moment, it is natural to feel depressed for a while; feelings like melancholy and loss help define who we are. However, if you feel sad or uncomfortable most of the time for an extended period of time, you may be suffering from depression.
Take a self-test to see if you are showing any warning signs of depression. This won't give you a diagnosis, but it will help you determine what to do next.
Major depressive disorder with psychotic features
Psychotic depression, also known as major depressive disorder with psychotic features, is a serious medical or mental illness that requires prompt treatment and constant monitoring by a physician or mental health professional.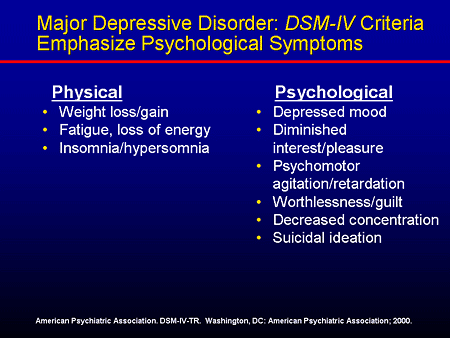
Major depression is a common mental condition that can have a detrimental effect on many aspects of a person's life. It affects mood and behavior as well as various bodily processes such as eating and sleeping. People who are severely depressed often lose interest in things they used to love and have difficulty doing daily activities. Sometimes they may even feel that life is not worth living.
Bipolar Disorder (BD)
Depression in patients with bipolar disorder (BD) is a significant clinical problem. Since schizophrenia dominates even in the treatment of BD, depression is associated not only with schizophrenia, but also with BD and comorbid medical disorders with a high risk of suicide.
Diagnosis of bipolar disorder (BD) and risk factors:
Approximately 12-17% of cases of bipolar disorder are not recognized until the mood "transforms" into hypomania or mania, either spontaneously or under the influence of substances uplifting mood.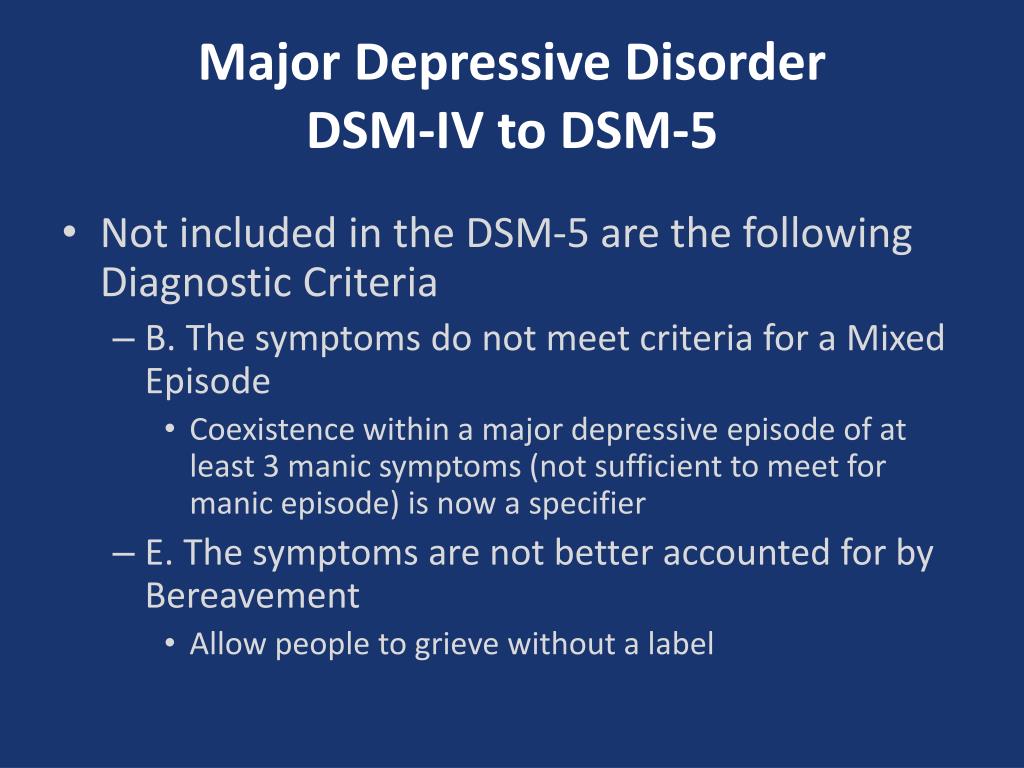
Factors suggesting a diagnosis of BD:
- Family mania, psychosis, "nervous breakdown" or psychiatric hospitalization
- Early onset, often with depressive symptoms
- Cyclothymic mood
- Multiple relapses (eg, 4 episodes of depression in 10 years)
- Depression with characteristic agitation, anger, insomnia, irritability, talkativeness.
- Other features are "mixed" or hypomanic or psychotic symptoms.
- Clinically "worsens", especially with mixed properties, during antidepressant treatment.
- Suicidal thoughts and actions
- Alcohol or drug abuse
Major depressive disorder in children and adolescents:
Major depressive disorder (MDD) can have a significant impact, occurring during childhood and adolescence. Associated with this are poor school performance, interpersonal problems later in life, early parenthood, and an increased risk of other psychiatric and substance use disorders.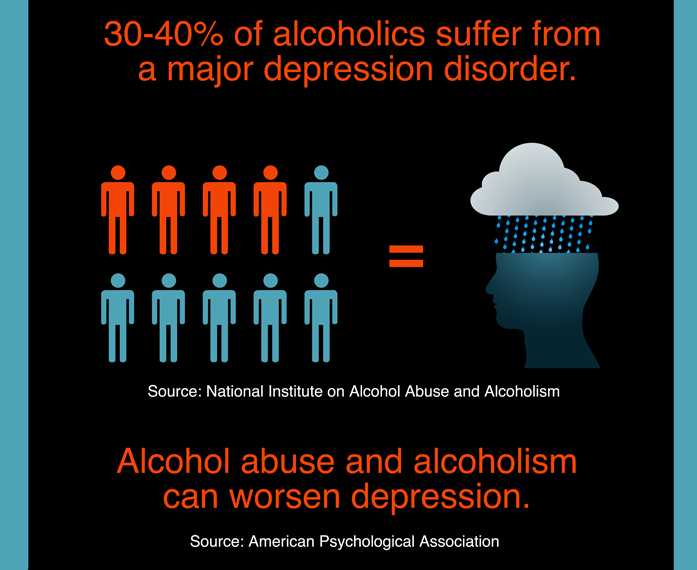 Diagnosing MDD in childhood is difficult. Children with MDD are often underdiagnosed and undertreated, and only 50% of adolescents are diagnosed before reaching adulthood.
Diagnosing MDD in childhood is difficult. Children with MDD are often underdiagnosed and undertreated, and only 50% of adolescents are diagnosed before reaching adulthood.
Symptoms of depression in children aged 3-8 years include:
- unsubstantiated claims.
- irritability
- less signs of depression
- anxiety
- behavioral changes
As the child becomes a teenager and adult, the presentation of symptoms meets the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria:
- Irritability.
- Expected weight gain.
- Lethargy or inner restlessness.
- May be delusional and not limited to feelings of guilt.
Postpartum depression
Postpartum depression affects one in seven women (PPD). While most women recover quickly from childhood blues, PPD lasts much longer and has a significant impact on women's ability to return to normal activities.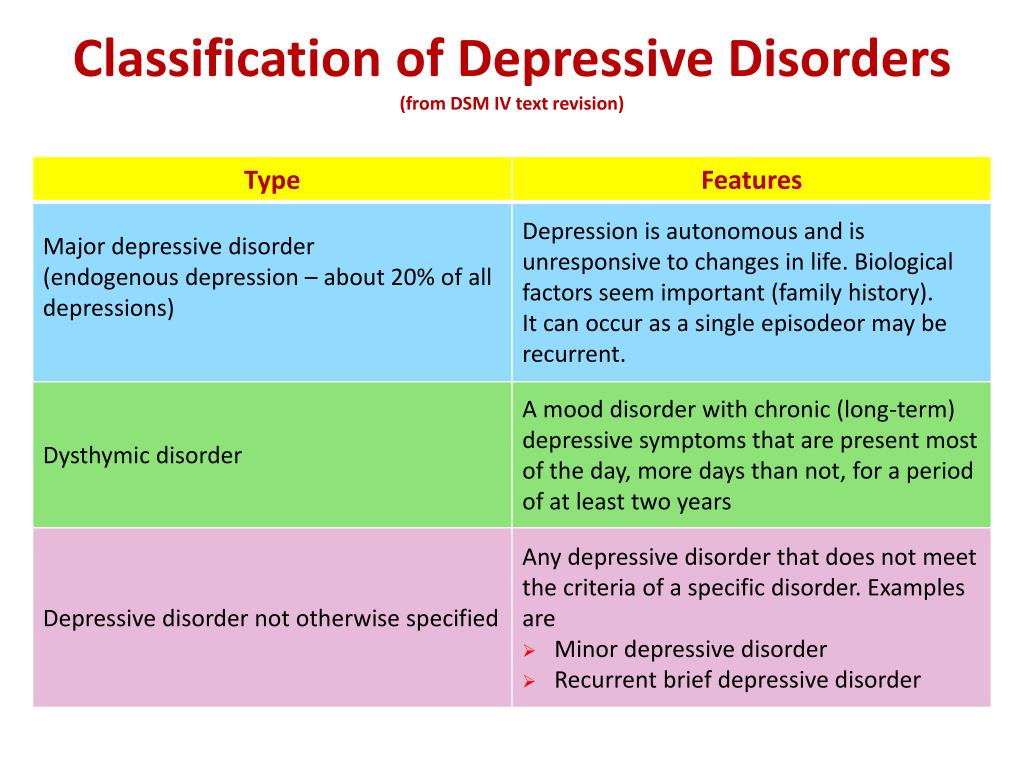
PDD affects the mother and her relationship with the child. PRD impairs maternal brain response and behavior. Postpartum depression most often occurs within 6 weeks after delivery. PDD affects 6.5 to 20% of women. It is more common in teenage girls, mothers who have given birth prematurely, and women living in cities.
In one study, African American and Hispanic mothers reported onset of symptoms within 2 weeks of birth, while white mothers reported onset of symptoms later.
Premenstrual dysphoric disorder
Premenstrual symptoms are a group of psychological, behavioral and physical symptoms that cyclically occur before menstruation and subsequently resolve after menstruation in women of reproductive age. Most women experience relatively mild pain and the symptoms do not interfere with their personal, social, or professional lives; however, 5% to 8% of women experience moderate or severe symptoms that can cause significant distress and functional impairment.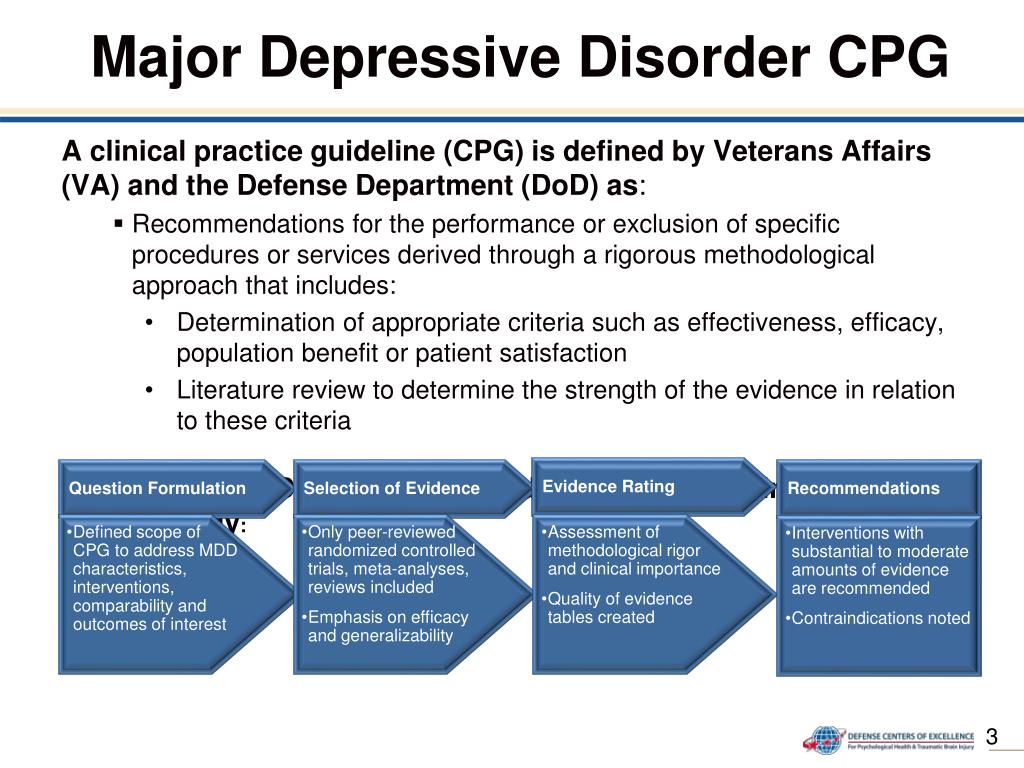
All women of reproductive age, from menarche to menopause, may have premenstrual symptoms. Premenstrual symptoms are a common problem for women of reproductive age. In the United States, 70 to 90 percent of women of reproductive age report at least some premenstrual pain.
Approximately one third of these women have symptoms severe enough to warrant a diagnosis of PMS. PMDD, the most severe type of premenstrual symptom complex, occurs in 3-8% of these women.
Treatment of major depressive disorder
Treatment of major depressive disorder (MDD) in adults:
Treatment options for major depressive disorder include medication, psychological, interventional and lifestyle changes. Medications and/or psychotherapy are used initially to treat MDD.
Combination treatment, including both drugs and psychotherapy, has been shown to be more effective than either treatment alone. Electroconvulsive therapy has been shown to be more effective than any other treatment for severe major depression.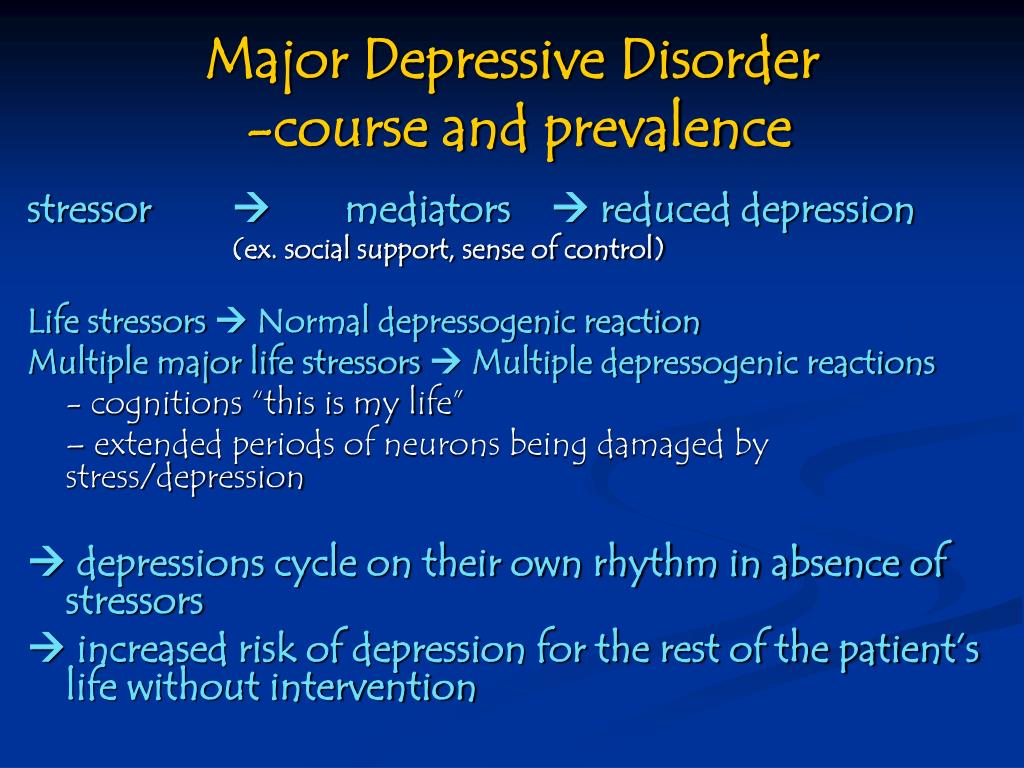
Patient psychotherapy:
Depression education and treatment can be provided to all patients. When appropriate, education may be provided to eligible family members.
Information about available treatment options will help patients make informed decisions, anticipate side effects, and follow prescribed treatment. Another important aspect of education was informing patients and concerned family members about the delayed duration of antidepressant onset of action.
Pharmacotherapy and acute treatment:
Antidepressants may be used as the primary treatment for patients with moderate or severe depression.
Clinical features that may indicate that the drug is a preferred therapeutic agent include a history of previous positive response to antidepressants, severity of symptoms, significant sleep disturbance and appetite disturbance.
Patients with severe depression with psychotic features will require antidepressant and antipsychotic and/or electroconvulsive therapy (ECT).
All antidepressants are effective, although their side effects vary. The following drugs have been approved by the FDA for the treatment of MDD:
- Fluoxetine, sertraline, citalopram, escitalopram, paroxetine, and fluvoxamine are examples of selective serotonin reuptake inhibitors (SSRIs). They are commonly used as first line therapy and are the most commonly prescribed antidepressants.
- Venlafaxine, duloxetine, desvenlafaxine, levomilnacipran and milnacipran are examples of serotonin and norepinephrine reuptake inhibitors (SNRIs). They are often used to treat depressed people who also have pain problems.
- Trazodone, vilazodone and vortioxetine are serotonin modulators.
- Bupropion and mirtazapine are examples of atypical antidepressants. When patients experience sexual side effects from SSRIs or SNRIs, they are often recommended as monotherapy or as adjunctive drugs.
- Amitriptyline, imipramine, clomipramine, doxepin, nortriptyline and desipramine are tricyclic antidepressants (TCAs).
- Tranylcypromine, phenelzine, selegiline, and isocarboxazid are examples of monoamine oxidase inhibitors (MAOIs). Due to the high prevalence of side effects and death in overdose, MAOIs and TCAs are not commonly used.
- Other drugs that can be used to improve the effectiveness of antidepressants include mood stabilizers and antipsychotics.
The role of yoga and meditation in managing depression:
Originating in ancient India, yoga is recognized as a form of alternative medicine using mind-body practice. Yoga philosophy is based on 8 elements that are best described as the ethical principles of a meaningful and purposeful life. Yoga can help with depression through the following mechanisms:
- Muscle relaxation resulting in less pain
- Creating Balanced Energy
- Decreased breathing and heart rate
- Lowering blood pressure and cortisol levels
- Increase blood flow
- Reducing stress and anxiety through calmness
- Improve pre-existing ailments such as arthritis, cancer, mental illness and more.
Treatment of major depressive disorder (MDD) in children and adolescents
Psychotherapy is important for both patients and their families, so everyone is aware of the plan and goals of treatment. When the patient receives information, the severity of symptoms decreases. Mental education may include knowledge about the signs and symptoms of depression, the clinical course of the illness, the risk of exacerbation, treatment options, and parental advice on how to interact with depressed young people.
According to research by Sandra Mullen, psychotherapy, along with medication, is often recommended for the treatment of major depressive disorder (MDD) in children and adolescents diagnosed with depression, suicidal ideation, and transient hypomania/mania.
Treatment of bipolar depression
Bipolar depression remains a clinical problem. Treatment options are limited, especially in the treatment of the acute phase of bipolar depression. There are currently only three approved drugs: OFC, quetiapine (immediate or extended release) and lurasidone (lithium monotherapy or adjuvant therapy or valproate). All three agents have similar efficacy profiles. They differ in duration.
There are currently only three approved drugs: OFC, quetiapine (immediate or extended release) and lurasidone (lithium monotherapy or adjuvant therapy or valproate). All three agents have similar efficacy profiles. They differ in duration.
Non-approved agents and treatments
Non-pharmacological drugs such as lamotrigine, antidepressants, modafinil, pramipexole, ketamine, and electroconvulsive therapy (ECT) are often prescribed for the treatment of acute bipolar depression.
Treatment of recurrent depression:
Some patients may experience recurrent episodes of depression throughout their lives unless supportive care is used to prevent relapse. Treatment should include psychotherapy and pharmacotherapy, and the dose should generally not be reduced after remission has been achieved.
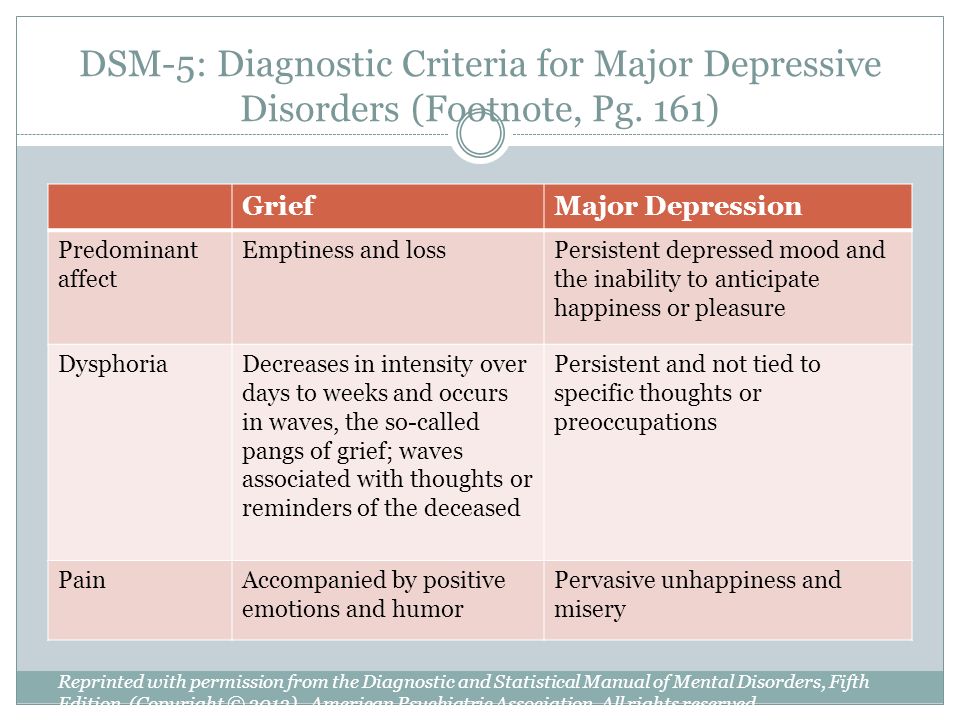
Differential
Critical to rule out depressive disorder due to another medical condition, depressive disorder due to psychoactive substances/drugs, dysthymia, cyclothymia, bereavement, adjustment disorder with depressed mood, bipolar disorder, schizoaffective disorder, schizophrenia, anxiety disorders and eating disorders when assessed for DMD.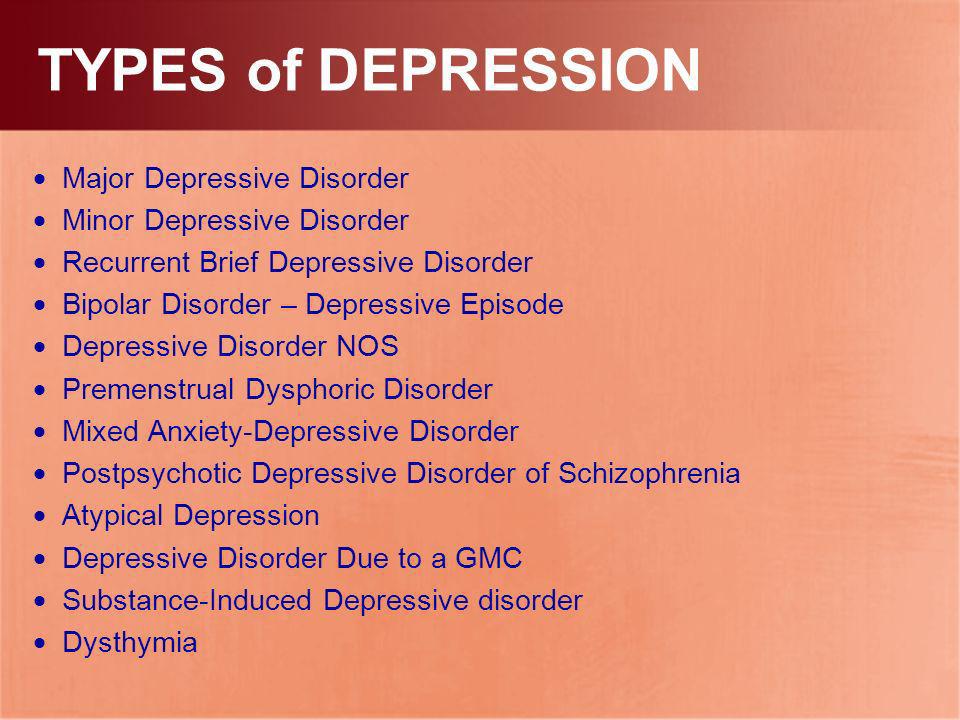 Depressive symptoms can develop as a result of the following factors:
Depressive symptoms can develop as a result of the following factors:
- Neurological causes such as cerebrovascular accident, multiple sclerosis, epilepsy, Parkinson's disease and Alzheimer's disease.
- Endocrine diseases such as diabetes, thyroid disease and adrenal disease.
- Metabolic disorders such as hypercalcemia, hyponatremia
- Drugs/substances causing dependence: steroids, antihypertensives, anticonvulsants, antibiotics, sedatives, sleeping pills, alcohol, stimulant withdrawal.
- Nutrient deficiencies such as vitamin D, B12, B6, iron or folate deficiency
- Infectious diseases such as HIV and syphilis
- Malignant neoplasms
Prognosis
Episodes of depression in untreated major depressive disorder may last 6 to 12 months. Approximately two-thirds of people with MDD think about suicide, and 10 to 15% commit suicide. MDD is a chronic relapsing disease; the recurrence rate after the first episode is about 50%, 70% after the second episode and 90% after the third episode.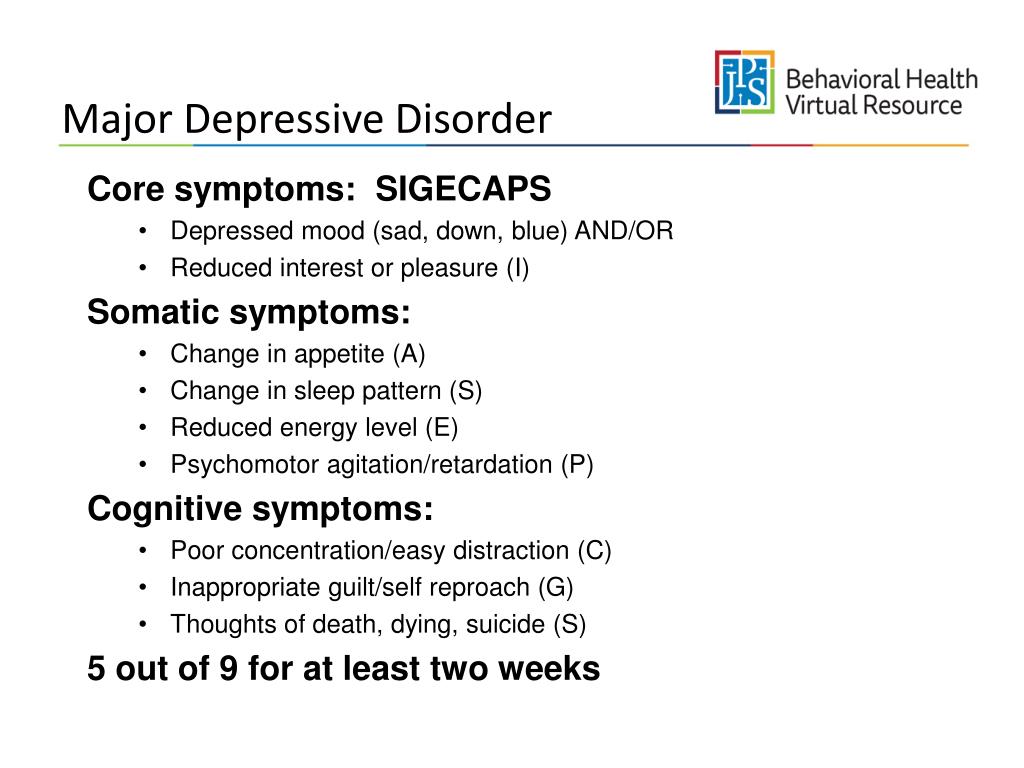 Approximately 5-10% of people with MDD develop bipolar disorder.
Approximately 5-10% of people with MDD develop bipolar disorder.
Patients with mild episodes, no psychotic symptoms, improved adherence, a reliable support system, and adequate premorbid functioning have a positive prognosis for MDD. In the presence of a concomitant mental disorder, personality disorder, multiple hospitalizations and advanced age, the prognosis is poor.
Complications
MDD is one of the leading causes of disability in the world. This not only causes severe functional impairment, but also negatively affects interpersonal relationships, reducing the quality of life. Individuals with MDD are at significant risk of developing comorbid anxiety and drug use disorders, which increase the risk of suicide.
Diabetes, hypertension, chronic obstructive pulmonary disease and coronary heart disease may be aggravated by depression. People who are depressed are more likely to engage in self-destructive behavior as a coping method. Left untreated, MDD can be quite debilitating.