Emotional shut down depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse.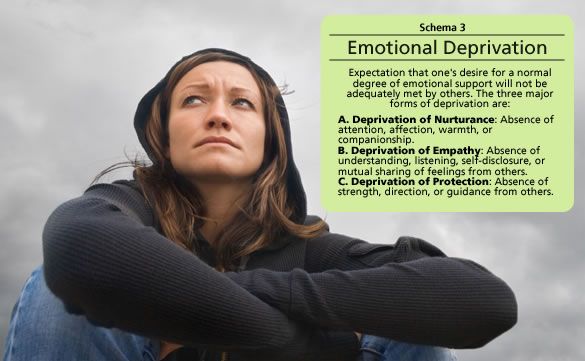 Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers. The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
- Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.
 4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk.
 They Hear You.
They Hear You. - Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
- Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses.
 The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States - The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month. The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
- Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.
 4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH) - Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 01/05/2023
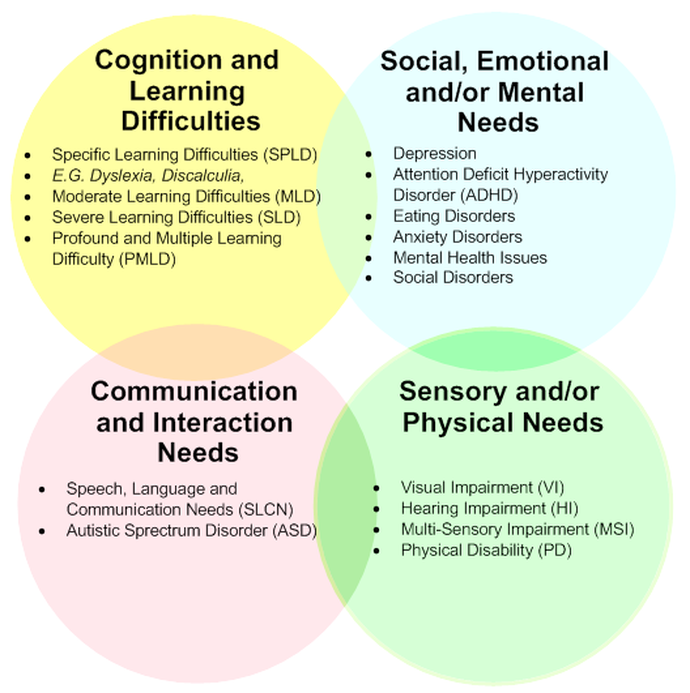
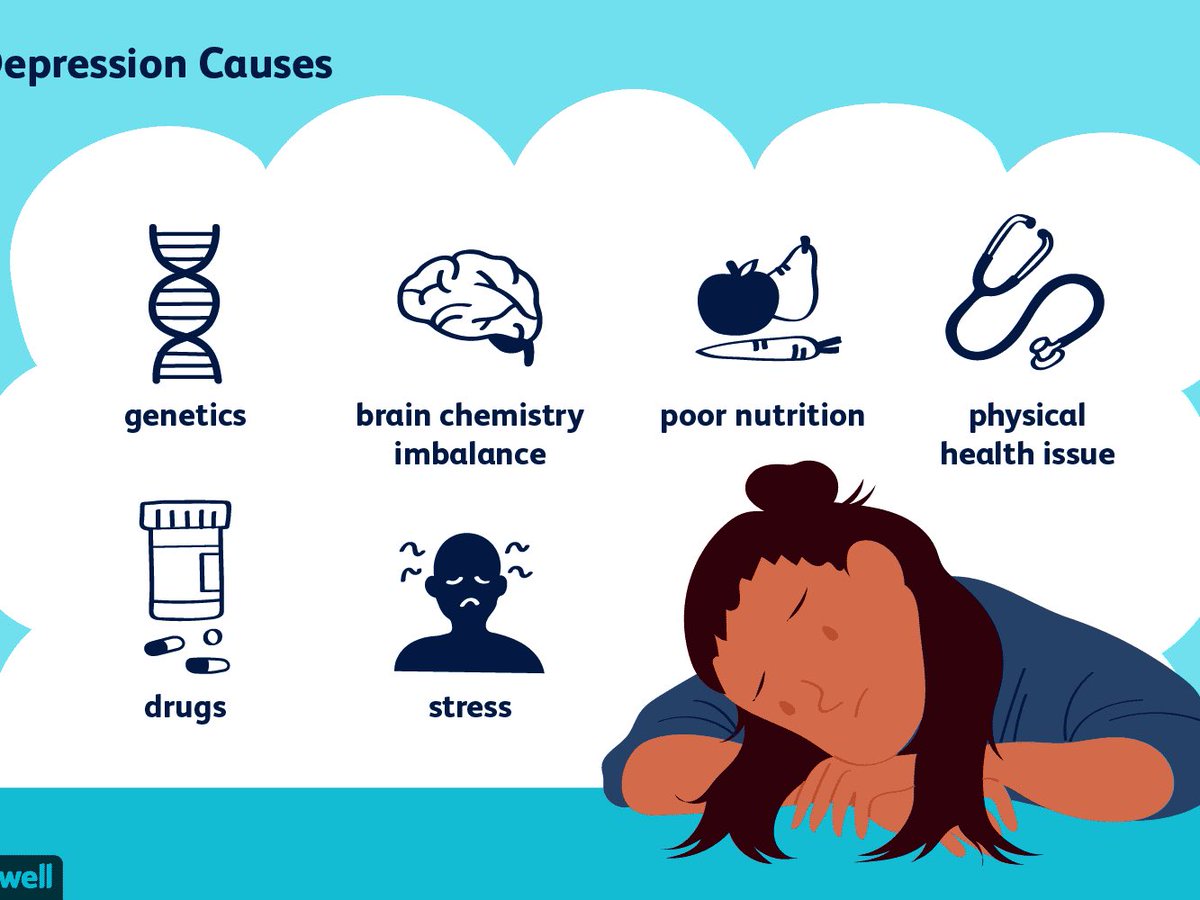
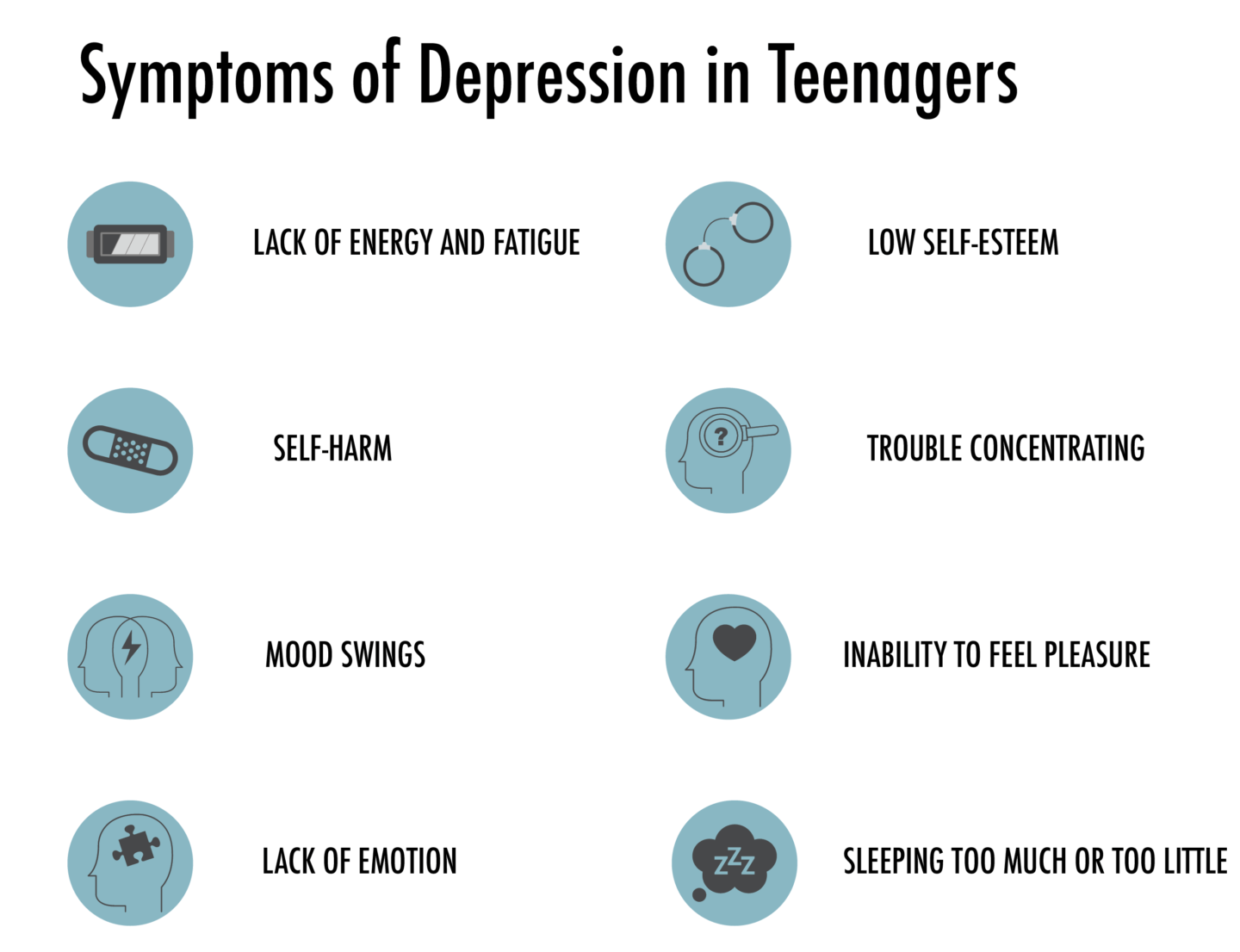
Depressive emotional disorders: diagnosis and treatment in a psychiatric center
Emotional depression manifests itself in a decrease in interest in one's former hobbies, social contacts, and work. Attention and concentration of memory are disturbed, the patient experiences a deterioration in well-being. Diagnosis should be carried out by professional psychiatrists, while it is important to conduct a differential diagnosis - to determine whether the symptoms are a sign of depression or are they symptoms of experienced stress or nervous shock.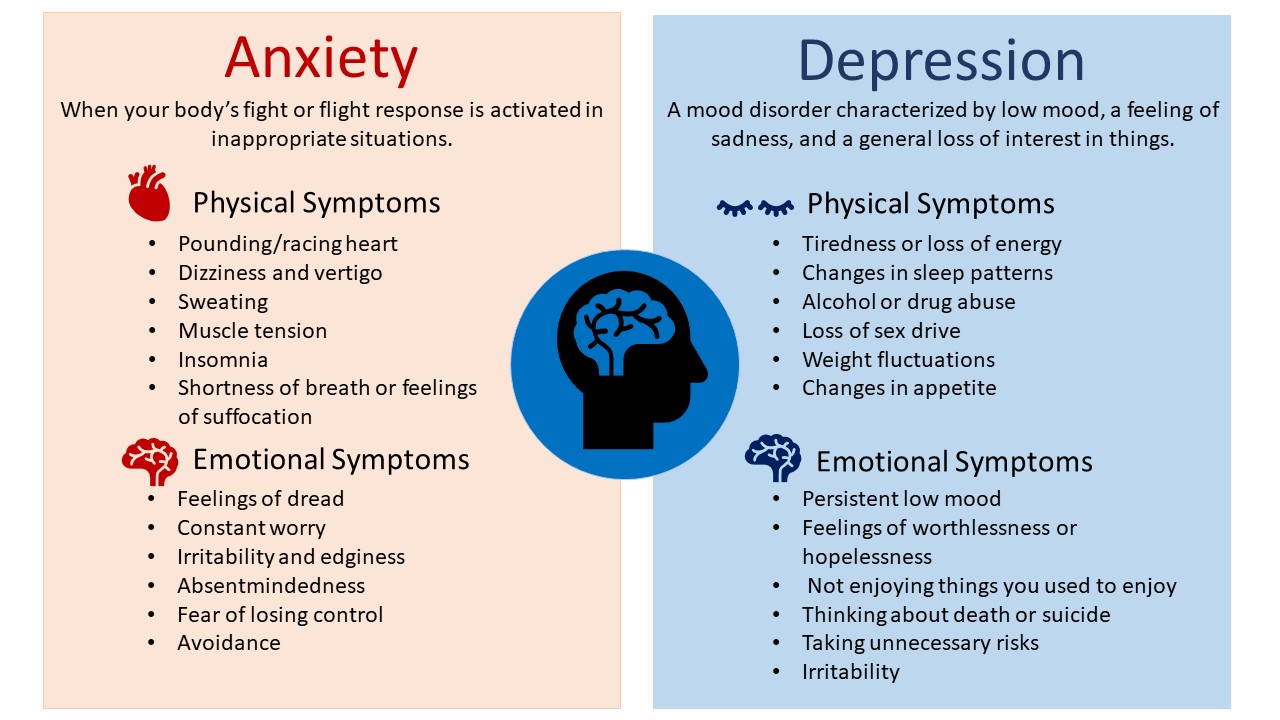
Submit an application for diagnosis and treatment
I confirm that I accept the terms of consent to the processing of personal data.
Emotional disorders are disorders characterized by a general decrease in functioning and activity. This is a large class of disorders, which include, for example, overwork, emotional burnout, depression. Depressive emotional disorders as a subspecies of this class of disorders are characterized by pronounced depressive symptoms: the patient experiences apathy, a feeling of hopelessness, unwillingness to do daily activities, loss of interest in life. The causes of depressive emotional disorder can be either endogenous (caused by internal causes) or exogenous (caused by external causes) in nature. Depressive emotional disorder can occur as a single episode (eg, postpartum depression, reaction to the death of a loved one, divorce) or as recurring depressive episodes. Thus, doctors distinguish the following types of depressive emotional disorder:
- Single depressive episode
- Recurrent depression
- Chronic depressive disorder
Features of the disorder
- Each type of affective disorder has characteristic manifestations.

- The main symptoms of depressive syndrome:
- lack of interest in the outside world;
- a state of prolonged sadness or melancholy;
- passivity, apathy;
- attention disorders;
- feeling of worthlessness;
- sleep disorders;
- decreased appetite;
- disability;
- recurrent suicidal thoughts;
- worsening of the general state of health, which is not explained by the examination.
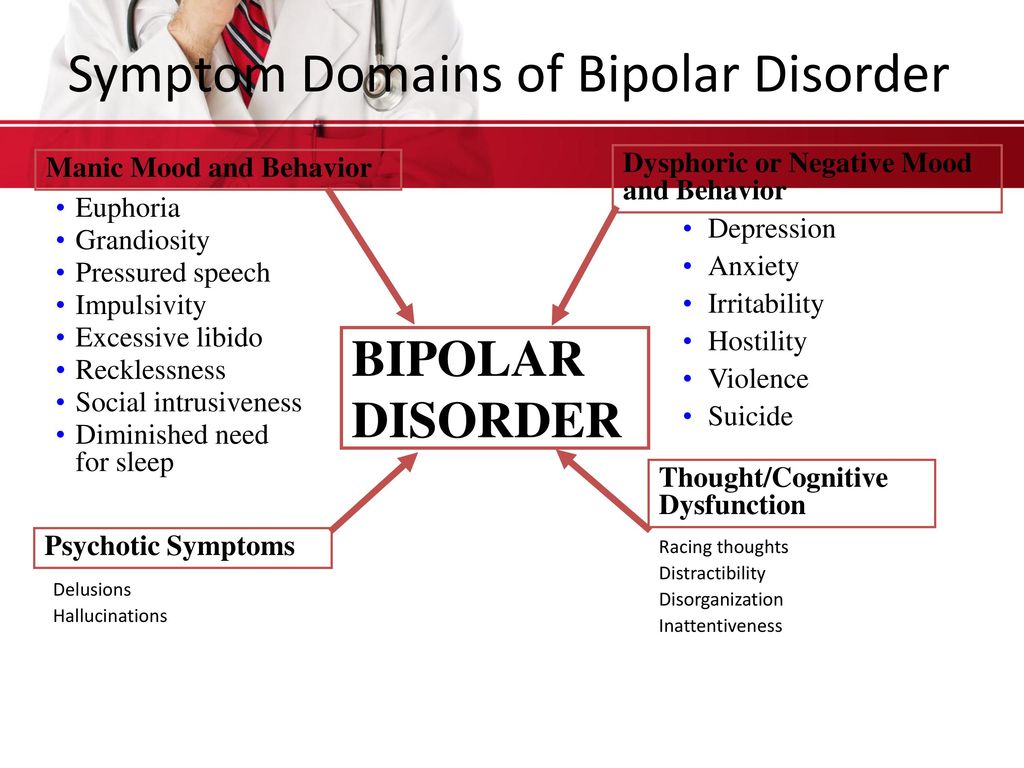
Bipolar disorder is characterized by
- alternating phases of depression and mania;
- depressed mood during the depressive phase;
- during a manic period - recklessness, irritability, aggression, hallucinations and/or delirium.
Manifestation of anxiety disorders
- severe, intrusive thoughts;
- sleep disorders;
- decreased appetite;
- constant feeling of anxiety or fear;
- shortness of breath;
- tachycardia;
- deterioration in concentration.

Forms of depressive disorders
Depressive disorder manifests itself in various forms. Depressive states differ in their depth, that is, in their severity. If, against the background of individual symptoms of depressed mood, you find the strength to force yourself to do daily activities, this is a mild degree of depression. If there are several depressive symptoms, and despite trying, you are still not able to do what you need to do, this is moderate depression. And severe depression, when almost all the symptoms of the disorder are present and it is extremely difficult for a person to cope with the usual daily tasks in everyday life.
Unipolar depression
The most common form of depressive disorder. The word monopolar means the presence of one extreme position - the "pole" - in the range of emotions, which is characterized, respectively, by only one - dreary, depressed - mood. As a rule, this is a persistent feeling of sadness or complete joylessness, insomnia, inability to concentrate, forgetfulness, loss of appetite, pain in different places, there is a heavy feeling of deep mental pain - longing.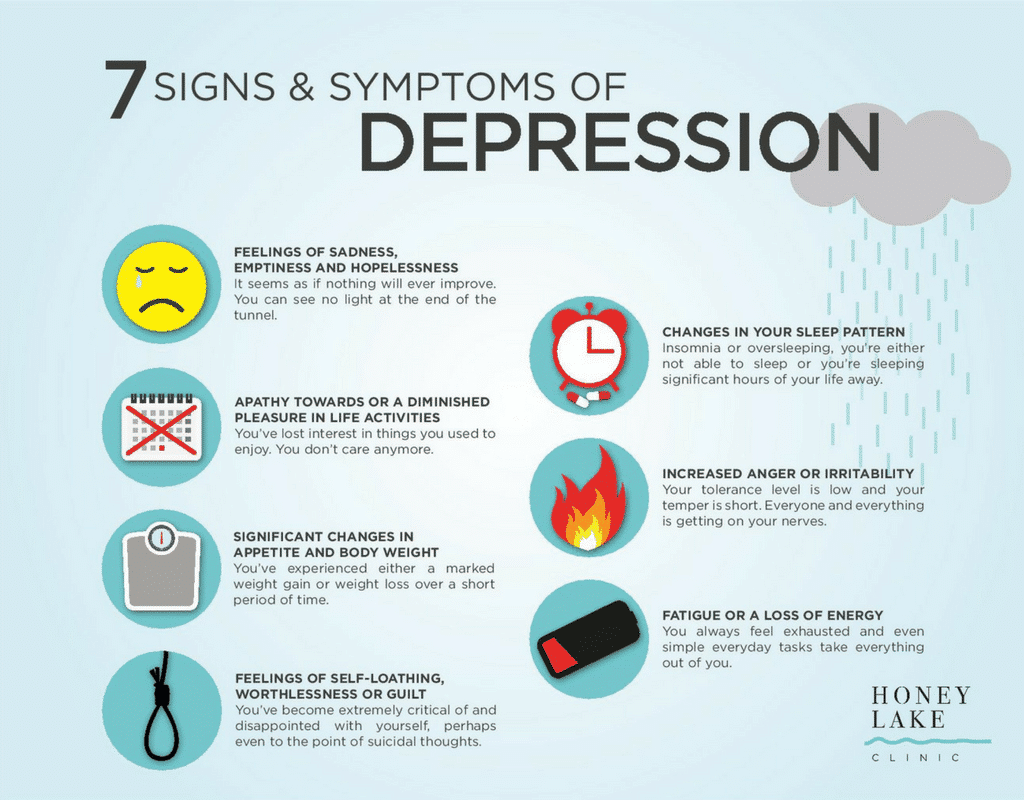 In this state, a person considers himself worthless, incapable of anything, and his position is hopeless. Self-esteem drops.
In this state, a person considers himself worthless, incapable of anything, and his position is hopeless. Self-esteem drops.
Dysthymia
A long-term form of depressive disorder characterized by persistent feelings of despondency. In a state of dysthymia, a person is gloomy - always or almost always. Thoughts are dominated by anxiety, guilt, a person in himself, inhibited, any events and circumstances of life are perceived only as failures, condemnation of oneself and others. The course of dysthymia is long - for years. The gloomy mood inherent in dysthymia leads to tension in the family, in marital relationships, in the professional sphere.
Seasonal affective disorder
A form of depression that occurs at a specific time of the year. Most of those suffering from this disease feel depressed and lethargic in winter, while in summer their mood is normal and even joyful. As a rule, depression occurs in October-November, and ends in March-April. Some people suffer from seasonal affective disorder during other months of the year. Accompanied by a breakdown, fatigue, the need to sleep more, increased appetite, inability to concentrate on work and do anything around the house after work, the mood is dominated by depression, anxiety, avoidance of communication, increased irritability.
Some people suffer from seasonal affective disorder during other months of the year. Accompanied by a breakdown, fatigue, the need to sleep more, increased appetite, inability to concentrate on work and do anything around the house after work, the mood is dominated by depression, anxiety, avoidance of communication, increased irritability.
Bipolar depression
A form of depression in which a person's mood makes transitions between extreme positions or poles: between sad mood (depression) and joyful mood (mania). On average, in the intermediate position, the mood is normal. During the depressive phase of the disorder, the same symptoms appear as in major depression, as the mood changes, a state of mild mania (hypomania) may occur, which is characterized by increased activity, increased activity, emotional alertness and self-confidence. In the phase of mania, the mood is abnormally elevated, excessive sociability, irritability and anger are pronounced.
Violation of expressiveness and strength of emotions
- Sensitivity. It is characterized by excessive sensitivity to an emotional event and vulnerability. For example, a person may burst into tears if an apple falls out of his hands. Sensitivity may be innate or accompany a personality disorder.
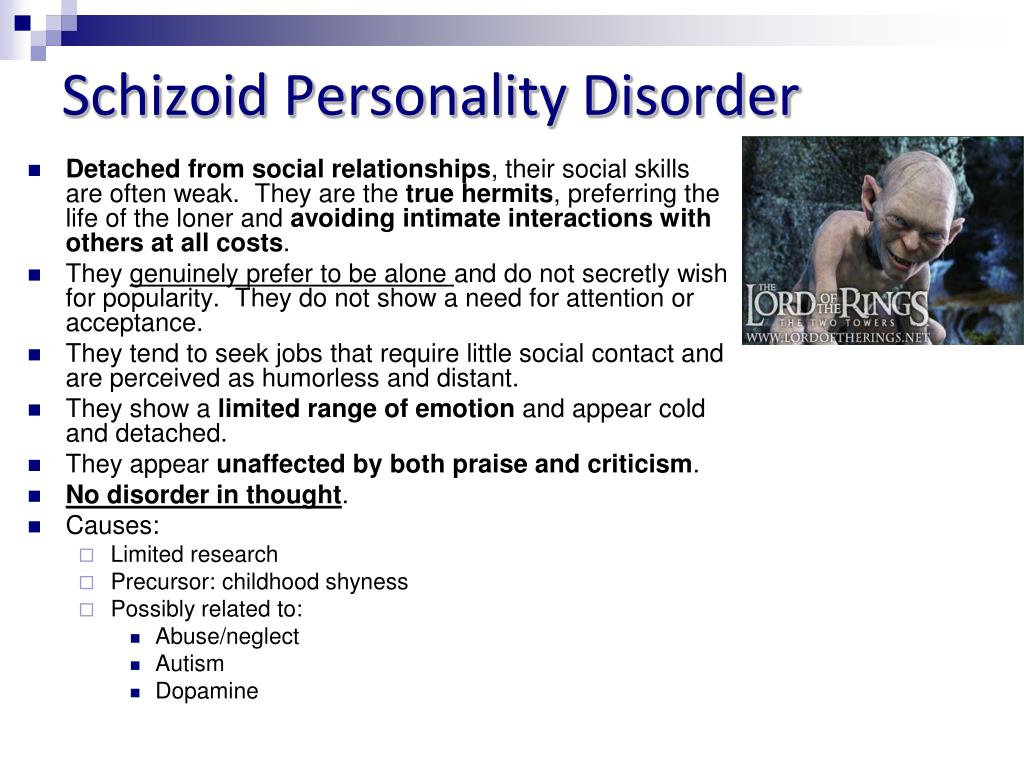
- Emotional coldness. It is characterized by blunting of emotions. Events do not cause an adequate reaction. Phenomena and objects are met with a cold attitude, regardless of their significance. For example, the death of a loved one does not cause sadness or sadness in a person. It usually occurs in schizophrenia and schizoid personality disorder.
- Emotional dullness. This is absolute emotional coldness. Any event, regardless of emotional significance, does not cause a reaction. Emotional dullness occurs with a schizophrenic defect, the end state of schizophrenia.
- Apathy. It is characterized by indifference and indifference to the events of the outside world.
 They do not arouse interest or motivation.
They do not arouse interest or motivation.
Violation of the adequacy of emotions
- Ambivalence. A person has two opposite emotions at the same time: love and hate, joy and sadness, disgust and interest. This is a sign of schizophrenia.
- Inadequacy. The patient has an emotion that does not correspond to the event. For example, at the funeral of a loved one, the patient may laugh and have fun. Usually accompanies schizophrenia.
Violation of stability of emotions
- Lability. Emotions often change, regardless of the reason. Usually occurs with neurasthenia, autonomic dysfunction syndrome, asthenia, intoxication, hypoxia, organic brain damage. For example, an emotionally labile disorder. It occurs after a difficult birth, with brain tumors and traumatic brain injuries.
- Explosiveness. The threshold of sensitivity decreases. The patient has an outburst of rage, aggression and anger, despite the fact that objectively the situation should not cause such emotions.
 Occurs in epilepsy, epileptoid (excitable, explosive) personality disorder, after organic brain damage.
Occurs in epilepsy, epileptoid (excitable, explosive) personality disorder, after organic brain damage. - Weakness. It is characterized by a fluctuation of emotions from one extreme to another for a small reason. For example, a grandmother cries at the sight of her grandson. Weakness is characteristic of elderly patients, manifested in atherosclerosis of the arteries of the brain, with asthenic neurosis.
Diagnosis and treatment
If depressive emotional disorders are suspected, diagnosis is carried out in a specialized clinic by an experienced psychiatrist. To make a diagnosis, a so-called psychiatric inteq is carried out, during which the patient is asked questions about his current condition, a detailed history is collected, and, if necessary, a conversation is held with the patient's relatives. As a rule, with a depressive emotional disorder, the following factors attract attention:
- Decreased mood
- Apathy
- Decreased concentration and attention
- Loss of interest in previously beloved activities
- Limitation of social contacts
- Sometimes - psychosomatic manifestations (pain of various localization)
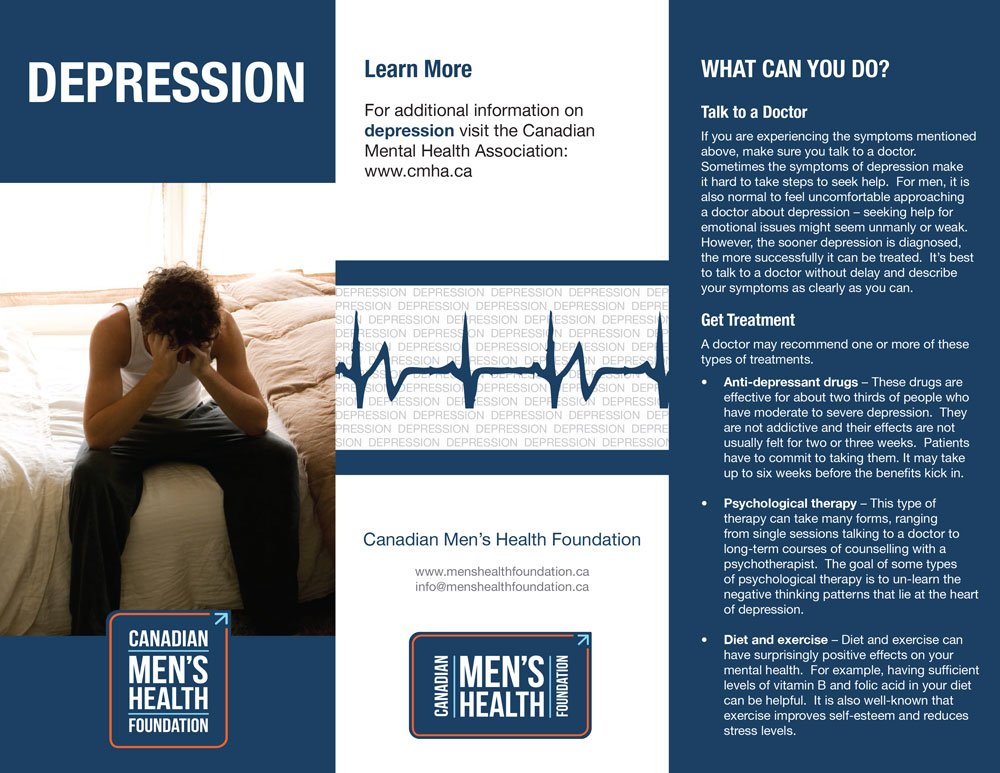
- Stage 1. Relief of acute symptoms. It is achieved through the use of pharmacotherapy.
- Stage 2. Stabilization therapy. Taking medications in a maintenance dosage and a course of psychotherapy.
- Stage 3. Prevention of depressive emotional disorders. Achieved through supportive psychotherapy and psychoeducational conversations.
, drugs, chemicals) In the course of a clinical interview, the doctor also determines whether it is a first-time symptom or a recurring episode of the disease, since in depressive emotional disorders, diagnosis aims to determine not only the causes, but also the nature of the course of the disorder.
 This is fundamentally important, because the choice and duration of therapy depends on the exact diagnosis. For depressive emotional disorders, treatment usually consists of the selection of medication and psychotherapy. Preparations are selected individually in each case. In Israel, the psychiatric clinic "IsraClinic" uses the latest generation of drugs with a minimum number of side effects and maximum efficiency. As a rule, if a patient has depressive emotional disorders, treatment takes place in three stages:
This is fundamentally important, because the choice and duration of therapy depends on the exact diagnosis. For depressive emotional disorders, treatment usually consists of the selection of medication and psychotherapy. Preparations are selected individually in each case. In Israel, the psychiatric clinic "IsraClinic" uses the latest generation of drugs with a minimum number of side effects and maximum efficiency. As a rule, if a patient has depressive emotional disorders, treatment takes place in three stages: It is a very important task for physicians involved in therapy to prevent the recurrence of the disease after treatment. This is especially true for patients with recurrent and chronic depressive disorder. Also, the issue of prevention of depressive emotional disorders is also relevant for thousands of ordinary people who are constantly faced with stressful situations at work or at home, for people with an anxious and overly emotional psychotype, for those who have experienced a very strong emotional shock. Any disease is easier to prevent than to treat, so the clinic "IsraClinic" offers its assistance not only to patients with diagnosed disorders and diseases, but also to people who find themselves in a difficult life situation and feel "on the verge".
This is especially true for patients with recurrent and chronic depressive disorder. Also, the issue of prevention of depressive emotional disorders is also relevant for thousands of ordinary people who are constantly faced with stressful situations at work or at home, for people with an anxious and overly emotional psychotype, for those who have experienced a very strong emotional shock. Any disease is easier to prevent than to treat, so the clinic "IsraClinic" offers its assistance not only to patients with diagnosed disorders and diseases, but also to people who find themselves in a difficult life situation and feel "on the verge".
Depression and depressive conditions. Help with treatment.
Be satisfied with what you have in life. Be grateful also for what does not belong to you, for it relieves you of many unnecessary worries. But try to get what you really need and make the best use of every minute of your life.
Imayat Khan
One of the most common diseases on earth is depression. Thus, according to the WHO, more than 150 million people worldwide suffer from depression. According to Russian health care, about 15 million people suffer from depression in Russia. According to American psychologists, women suffer from depression twice as much as men. In adolescent boys and young men, depression is often accompanied by breakdowns, and in girls and young women it is accompanied by eating disorders (anorexia and bulimia).
Thus, according to the WHO, more than 150 million people worldwide suffer from depression. According to Russian health care, about 15 million people suffer from depression in Russia. According to American psychologists, women suffer from depression twice as much as men. In adolescent boys and young men, depression is often accompanied by breakdowns, and in girls and young women it is accompanied by eating disorders (anorexia and bulimia).
Depression is an affective state characterized by a negative emotional background, with changes in the sphere of motivational, cognitive representations and general passivity of behavior.
Churchill, who suffered from bouts of depression, called this illness "black dog". Other famous people who suffered from manic-depressive states gave different names to this disease: "Edge of the abyss", "Endless darkness in reality", "All-devouring flame of the soul".
Here is what Curtiss A., author of Depression, writes about depression. “For 30 long years I was depressed and melancholy. Due to chronic severe depression, my life was empty and my marriage slightly collapsed. … Living in depression is like being in a torture chamber. But you can learn to get out of there ... However, over the past 15 years, I have been so rarely inclined to consider a depressive state that now I am inclined to consider depression not as a pathology of the psyche, but as a strict spiritual mentor.
Due to chronic severe depression, my life was empty and my marriage slightly collapsed. … Living in depression is like being in a torture chamber. But you can learn to get out of there ... However, over the past 15 years, I have been so rarely inclined to consider a depressive state that now I am inclined to consider depression not as a pathology of the psyche, but as a strict spiritual mentor.
As Izard KE points out, most psychoanalysts agree that the most important components of depression are the loss of self-esteem, self-confidence and self-esteem.
The experience of depression includes the following fundamental emotions: sadness (key emotion), disgust, contempt, anger, fear, guilt, and embarrassment. According to Izard K.E. anger, disgust, contempt are manifested by a person both in relation to himself and in relation to other people.
When depressed, a person experiences negative emotions: depression, melancholy, despair. Volitional activity is sharply reduced. Decreased self-esteem. A person may feel guilty for the events of the past, those unpleasant events that occurred through the fault of a person.
Decreased self-esteem. A person may feel guilty for the events of the past, those unpleasant events that occurred through the fault of a person.
During the period of depression, slowness, lack of initiative, and rapid fatigue are characteristic, which leads to a sharp decrease in productivity in one activity or another.
In case of prolonged depression, suicide attempts are possible.
In healthy people, depression can occur in the event of a difficult life situation, including due to the loss of loved ones, divorce, infidelity, infertility (inability to become a mother or father), due to unfulfilled hopes and other circumstances.
In addition, there is pathological depression as one of the main psychiatric syndromes.
Depression classification:
- Biological factors (organic and endogenous, i.e. innate nature). With biological factors, medications are most often used in the treatment.
- Psychosocial factors (of a psychological nature). With the predominance of psychosocial factors, various methods of psychotherapy are used.
With the predominance of psychosocial factors, various methods of psychotherapy are used.
There are two types of depression:
- Psychogenic depression;
- Endogenous depression.
The consequences of depression are:
decrease in labor activity, alcohol and drug use, frequent divorces, death due to suicide.
Alexander Lowen in his book "Depression and the Body" writes that "the depressive reaction immobilizes a person. He finds himself unable to muster the strength to carry on with his usual activities. He feels defeated, hopeless, and as long as the state of depression persists, he sees no point in making any effort. … A depressive reaction can often have no obvious cause. In many cases, it occurs when a person is approaching the realization of his goal or has achieved it.
Depressive syndrome According to Zharikov N.M., Tyulpin Yu.G. The main symptom of depression is a decrease in mood, slowing down of thinking, and motor retardation. A person complains of longing, depression, sadness. A person does not show a reaction to either a joyful event or a sad one. Feelings can be of varying intensity - from slight pessimism and sadness to the feeling of a "stone in the heart."
A person complains of longing, depression, sadness. A person does not show a reaction to either a joyful event or a sad one. Feelings can be of varying intensity - from slight pessimism and sadness to the feeling of a "stone in the heart."
Slowing down of thinking is expressed by slow monosyllabic speech, long thinking of the answer. In a more complex case, the person is silent, spontaneous speech is absent.
Motor retardation is revealed in stiffness, slowness, slowness. In severe depression, depressive stupor is possible.
Depressed people have low self-esteem, they consider themselves insignificant people. They are pessimistic about not only their present, but also their past and future. In severe depression, delusions of self-blame and self-destruction are often formed.
Appetite sharply decreases, sometimes on the contrary there are bouts of overeating.
No interest in the opposite sex.
Women stop doing housework, cannot take care of young children, do not pay attention to their appearance.
Men can't cope with their favorite work, unable to get out of bed in the morning, get ready and go to work, they can lie all day without sleep. Patients do not enjoy anything.
Patients sleep poorly at night and cannot rest during the day. Waking up in the early morning hours is especially characteristic, after which the person can no longer fall asleep. How to get out of depression?
Tips for reducing depression
To improve mood, it is recommended to move more, increase the duration of sleep, take a warm shower before bed, but do not wipe the skin dry. For the treatment of seasonal depression, phototherapy (staying in a solarium) is effective. Go skiing in winter.
It is desirable to use light wallpaper and furniture in the interior of the apartment. Nowadays, some people have a tendency to use dark colors in the apartment.
Depressed patients are encouraged to photograph clouds, especially in sunny weather. Be more often in nature.
Keeping diaries helps a lot, where it is recommended to reflect all the good things that happened during the day.
Swimming, jogging, walking in the park, cycling, roller skating helps a lot.
Dance classes are good for women, for example, in the fitness club there are various dance programs.
Listening to music is good for regulating your emotional state. There is a whole list of these works, but it is better to listen to your inner voice and listen to what you want at a given time and exactly as much as you want in order to enjoy this process.
Yoga will help you find peace of mind.
Hobbies: knitting, embroidery, drawing, photography, making various crafts from natural materials, designing various models of aircraft, sailboats, tanks, etc. It helps well in expressing one's feelings, one's condition, writing stories or poems.
Medical treatment It is prescribed for patients with mild, moderate and severe manifestations of depression. A necessary condition for the effectiveness of treatment is cooperation with the doctor: strict adherence to the prescribed therapy regimen, regular visits to the doctor, a detailed, frank account of one's condition and life's difficulties.
A necessary condition for the effectiveness of treatment is cooperation with the doctor: strict adherence to the prescribed therapy regimen, regular visits to the doctor, a detailed, frank account of one's condition and life's difficulties.
Antidepressants.
Proper therapy allows in most cases to completely get rid of the symptoms of depression. Depression requires specialist treatment. The main class of drugs for the treatment of depression are antidepressants. Currently, there are various drugs in this group, of which tricyclic antidepressants (amitriptyline, melipramine) have been used since the late 50s. In recent years, the number of antidepressants has increased significantly.
The main advantages of new generation antidepressants are improved tolerability, reduced side effects, reduced toxicity and high safety in case of overdose. Antidepressants are a safe class of psychotropic medications when used properly and as directed by a physician. The dose of the drug is determined individually for each patient. You need to know that the therapeutic effect of antidepressants can appear slowly and gradually, so it is important to tune in positively and wait for it to appear.
You need to know that the therapeutic effect of antidepressants can appear slowly and gradually, so it is important to tune in positively and wait for it to appear.
Help from loved ones is also important in overcoming depression
The support of loved ones, even when the patient does not express interest in it, is very important in overcoming depression.
In this regard, the following advice can be given to relatives of patients:
- remember that depression is a disease in which sympathy is needed, but in no case should you plunge into the disease along with the patient, sharing his pessimism and despair. You need to be able to maintain a certain emotional distance, all the time reminding yourself and the patient that depression is a transient emotional state
- studies have shown that depression is especially unfavorable in those families where many critical remarks are made to the patient. Try to make it clear to the patient that his condition is not his fault, but a misfortune, that he needs help and treatment
- try not to focus on the illness of a loved one and bring positive emotions into your life and into the life of your family.