Dsm 5 adhd diagnostic code
| Disorder Class: Disorders Usually Diagnosed in Infancy, Childhood, and Adolescence | Disorder Class: Neurodevelopmental Disorders |
| A. Either (1) or (2): | A. A persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development, as characterized by (1) and/or (2): |
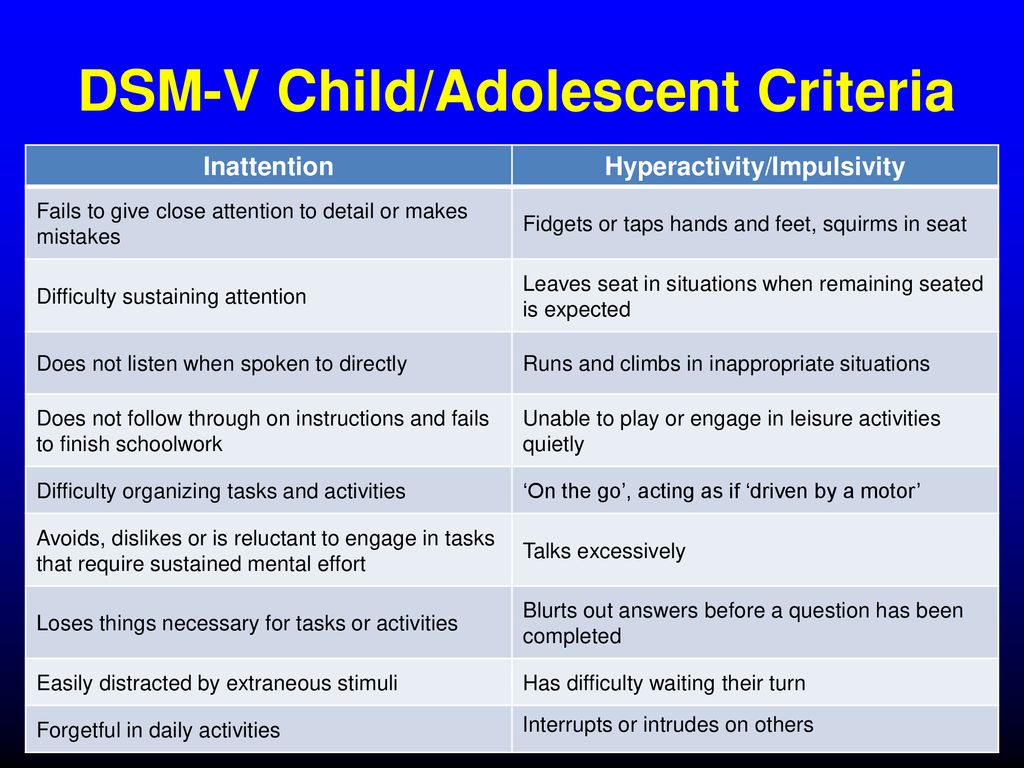
| 1. Six (or more) of the following symptoms of inattention have persisted for at least 6 months to a degree that is maladaptive and inconsistent with developmental level: | 1. Inattention: Six (or more) of the following symptoms have persisted for at least 6 months to a degree that is inconsistent with developmental level and that negatively impacts directly on social and academic/occupational activities: |
| Note: The symptoms are not solely a manifestation of oppositional behavior, defiance, hostility, or failure to understand tasks or instructions. For older adolescents and adults (age 17 or older), at least five symptoms are required. | |
| Inattention | |
| a. often fails to give close attention to details or makes careless mistakes in schoolwork, work, or other activities | a. Often fails to give close attention to details or makes careless mistakes in schoolwork, at work, or during other activities (e.g., overlooks or misses details, work is inaccurate). |
| b. often has difficulty sustaining attention in tasks or play activity | b. Often has difficulty sustaining attention in tasks or play activities (e.g., has difficulty remaining focused during lectures, conversations, or lengthy reading). |
| c. often does not seem to listen when spoken to directly | c. Often does not seem to listen when spoken to directly (e.g., mind seems elsewhere, even in the absence of any obvious distraction). |
| d. often does not follow through on instructions and fails to finish schoolwork, chores or duties in the workplace (not due to oppositional behavior or failure to understand instructions) | d. Often does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace (e.g., starts tasks but quickly loses focus and is easily sidetracked). |
| e. often has difficulty organizing tasks and activities | e. Often has difficulty organizing tasks and activities (e.g., difficulty managing sequential tasks; difficulty keeping materials and belongings in order; messy, disorganized work; has poor time management; fails to meet deadlines). |
| f. often avoids, dislikes, or is reluctant to engage in tasks that require sustained mental effort (such as schoolwork or homework) | f. Often avoids, dislikes, or is reluctant to engage in tasks that require sustained mental effort (e.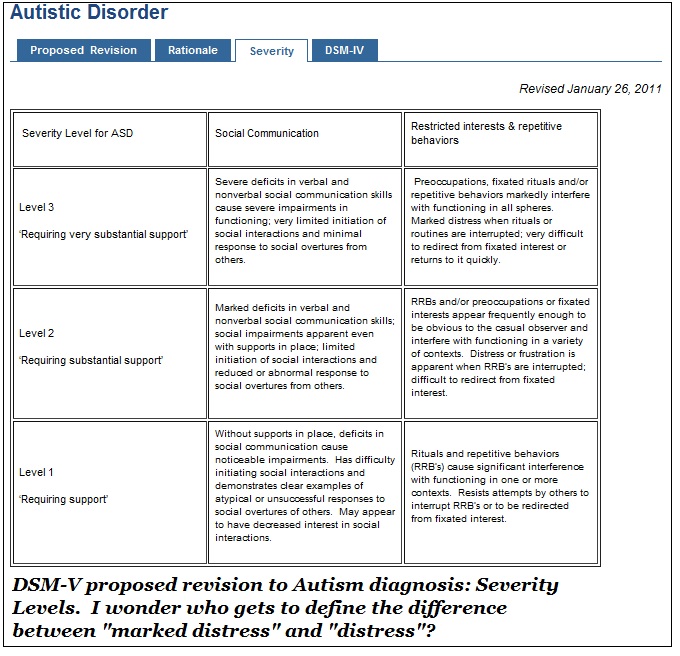 g., schoolwork or homework; for older adolescents and adults, preparing reports, completing forms, reviewing lengthy papers). g., schoolwork or homework; for older adolescents and adults, preparing reports, completing forms, reviewing lengthy papers). |
| g. often loses things necessary for tasks or activities (e.g., toys, school assignments, pencils, books or tools) | g. Often loses things necessary for tasks or activities (e.g., school materials, pencils, books, tools, wallets, keys, paperwork, eyeglasses, mobile telephones). |
| h. is often easily distracted by extraneous stimuli | h. Is often easily distracted by extraneous stimuli (for older adolescents and adults, may include unrelated thoughts). |
i.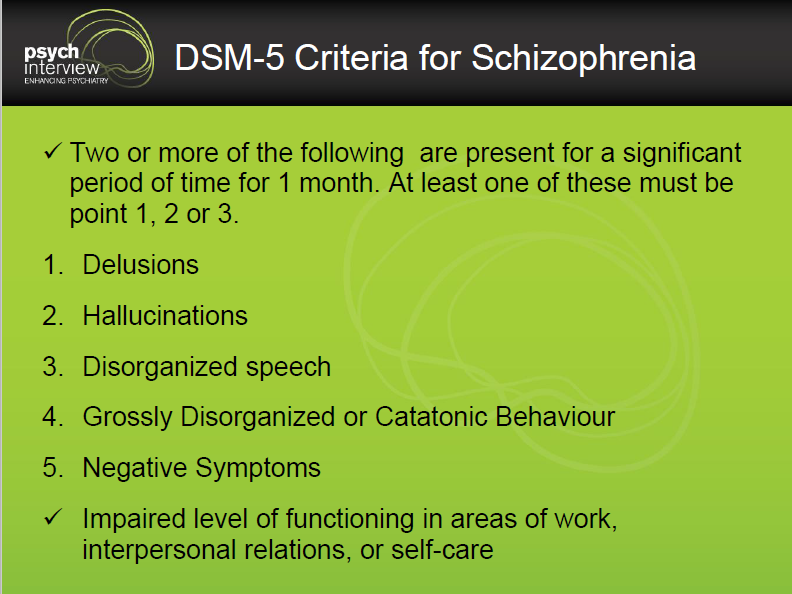 is often forgetful in daily activities is often forgetful in daily activities |
i. Is often forgetful in daily activities (e.g., doing chores, running errands; for older adolescents and adults, returning calls, paying bills, keeping appointments). |
| 2. Six (or more) of the following symptoms of hyperactivity-impulsivity have persisted for at least 6 months to a degree that is maladaptive and inconsistent with developmental level: | 2. Hyperactivity and impulsivity: Six (or more) of the following symptoms have persisted for at least 6 months to a degree that is inconsistent with developmental level and that negatively impacts directly on social and academic/occupational activities: |
Note: The symptoms are not solely a manifestation of oppositional behavior, defiance, hostility, or a failure to understand tasks or instructions.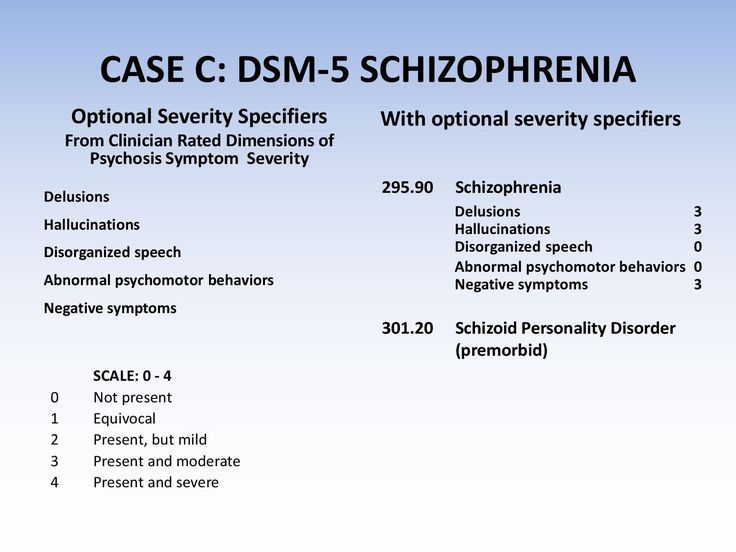 For older adolescents and adults (age 17 or older), at least five symptoms are required. For older adolescents and adults (age 17 or older), at least five symptoms are required. | |
| Hyperactivity | |
| a. Often fidgets with hands or feet or squirms in seat | a. Often fidgets with or taps hands or feet or squirms in seat. |
| b. Often leaves seat in classroom or in other situations in which remaining seated is expected | b. Often leaves seat in situations when remaining seated is expected (e.g., leaves his or her place in the classroom, in the office or other workplace, or in other situations that require remaining in place). |
| c. Often runs about or climbs excessively in situations in which it is inappropriate (in adolescents or adults, may be limited to subjective feelings of restlessness) | c. Often runs about or climbs in situations where it is inappropriate. (Note: In adolescents or adults, may be limited to feeling restless). |
| d. Often has difficulty playing or engaging in leisure activities quietly | d. Often unable to play or take part in leisure activities quietly. |
| e. Is often “on the go” or often acts as if “driven by a motor” | e. Is often “on the go” acting as if “driven by a motor” (e.g., is unable to be or uncomfortable being still for extended time, as in restaurants, meetings; may be experienced by others as being restless or difficult to keep up with).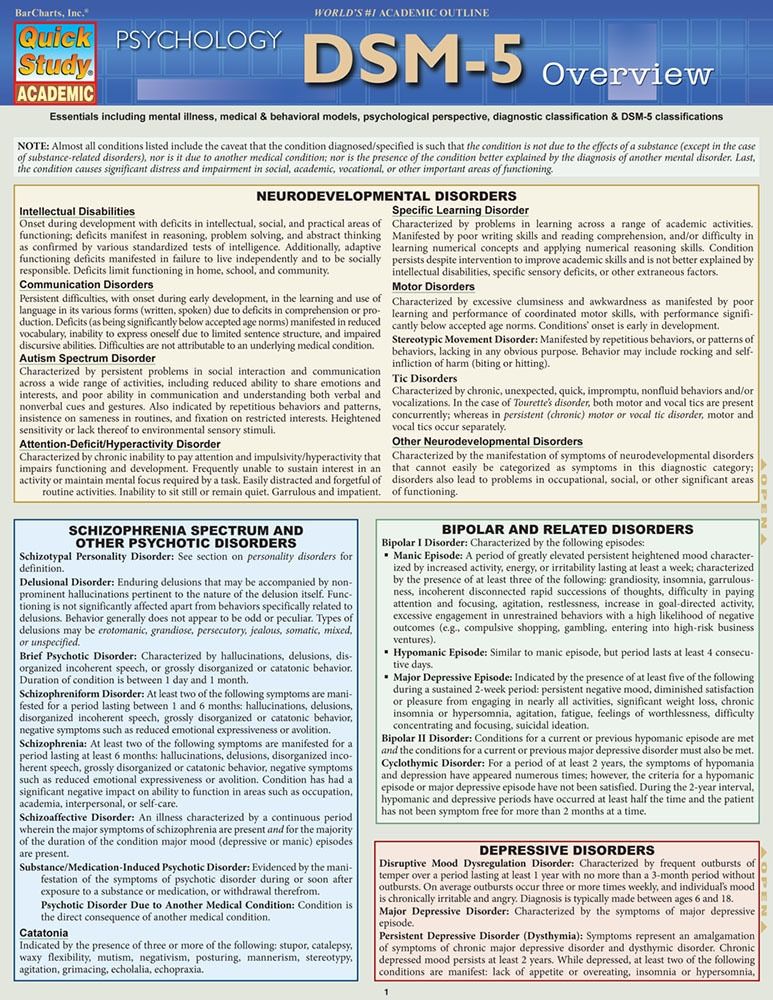 |
| f. Often talks excessively | f. Often talks excessively. |
| Impulsivity | |
| g. Often blurts out answers before questions have been completed | g. Often blurts out an answer before a question has been completed (e.g., completes people’s sentences; cannot wait for turn in conversation). |
| h. Often has difficulty awaiting turn | h. Often has trouble waiting his/her turn (e.g., while waiting in line).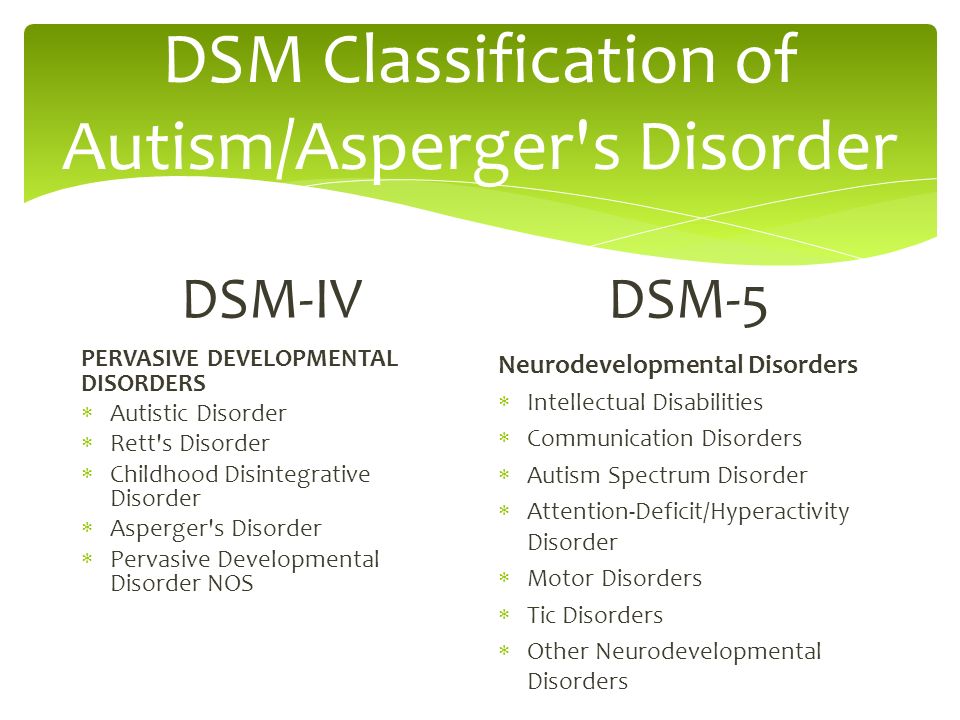 |
| i. Often interrupts or intrudes on others (e.g., butts into conversations or games) | i. Often interrupts or intrudes on others (e.g., butts into conversations, games, or activities; may start using other people’s things without asking or receiving permission; for adolescents and adults, may intrude into or take over what others are doing). |
| B. Some hyperactive-impulsive or inattentive symptoms must have been present before age 7 years. | B. Several inattentive or hyperactive-impulsive symptoms were present before age 12 years. |
| C. Some impairment from the symptoms is present in at least two settings (e.g., at school [or work] and at home). | C. Several inattentive or hyperactive-impulsive symptoms are present in two or more settings, (e.g., at home, school or work; with friends or relatives; in other activities). |
| D. There must be clear evidence of clinically significant impairment in social, academic or occupational functioning. | D. There is clear evidence that the symptoms interfere with, or reduce the quality of, social, school, or work functioning. |
E. The symptoms do not occur exclusively during the course of a pervasive developmental disorder, schizophrenia, or other psychotic disorders and is not better accounted for by another mental disorder (e.g., mood disorder, anxiety disorder, dissociative disorder, or a personality disorder). The symptoms do not occur exclusively during the course of a pervasive developmental disorder, schizophrenia, or other psychotic disorders and is not better accounted for by another mental disorder (e.g., mood disorder, anxiety disorder, dissociative disorder, or a personality disorder). | E. The symptoms do not occur exclusively during the course of schizophrenia or another psychotic disorder and are not better explained by another mental disorder (e.g., mood disorder, anxiety disorder, dissociative disorder, personality disorder, substance intoxication or withdrawal). |
Code based on type:
| Specify whether:
|
ADHD DSM-5® Criteria | Diagnostic Criteria for ADHD
ADHD DSM-5® Criteria | Diagnostic Criteria for ADHDThis site is for US healthcare professionals. If you’re an adult ADHD patient, please visit ADHDADULTHOOD.COM/AGAIN
ADHD is characterized by a persistent pattern of inattention and/or
hyperactivity/impulsivity that interferes with functioning or development.
 1
1
DSM-5
® DIAGNOSTIC CRITERIA FOR ADHD IN ADULTS1All criteria must be met for a diagnosis of ADHD in adults
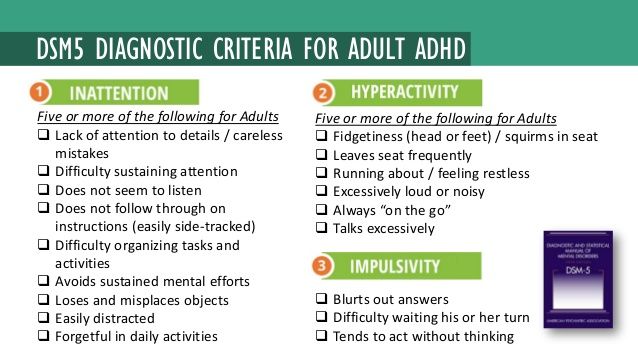
1:- Five or more symptoms of inattention and/or ≥5 symptoms of hyperactivity/impulsivity must have persisted for ≥6 months to a degree that is inconsistent with the developmental level and negatively impacts social and academic/occupational activities.
- Several symptoms (inattentive or hyperactive/impulsive) were present before the age of 12 years.
- Several symptoms (inattentive or hyperactive/impulsive) must be present in ≥2 settings (eg, at home, school, or work; with friends or relatives; in other activities).
-
There is clear evidence that the symptoms interfere with or reduce the quality of social, academic, or occupational functioning.

- Symptoms do not occur exclusively during the course of schizophrenia or another psychotic disorder, and are not better explained by another mental disorder (eg, mood disorder, anxiety disorder, dissociative disorder, personality disorder, substance intoxication, or withdrawal).
Diagnosis should be based on a complete history and evaluation of the patient.
Among other criteria that must be met for a diagnosis of ADHD, several symptoms (inattentive or hyperactive/impulsive) must be present in 2 or more settings (eg, at home, school, or work; with friends or relatives; in other activities).
ADHD Symptoms of
Inattention
- Makes careless mistakes/lacks attention to detail
- Difficulty sustaining attention
- Does not seem to listen when spoken to directly
- Fails to follow through on tasks and instructions
- Exhibits poor organization
- Avoids/dislikes tasks requiring sustained mental effort
- Loses things necessary for tasks/activities
- Easily distracted (including unrelated thoughts)
- Is forgetful in daily activities
ADHD Symptoms of
Hyperactivity/
Impulsivity
- Fidgets with or taps hands or feet, squirms in seat
- Leaves seat in situations when remaining seated is expected
- Experiences feelings of restlessness
- Has difficulty engaging in quiet, leisurely activities
- Is “on-the-go” or acts as if “driven by a motor”
- Talks excessively
- Blurts out answers
- Has difficulty waiting their turn
- Interrupts or intrudes on others
Symptoms must occur often
SCREENING AND DIAGNOSTIC SCALES
FOR USE WITH ADULTS
To aid physicians and psychologists in the diagnostic process, several validated behavior scales have been developed to help screen, diagnose, evaluate, and track symptoms of ADHD in adults.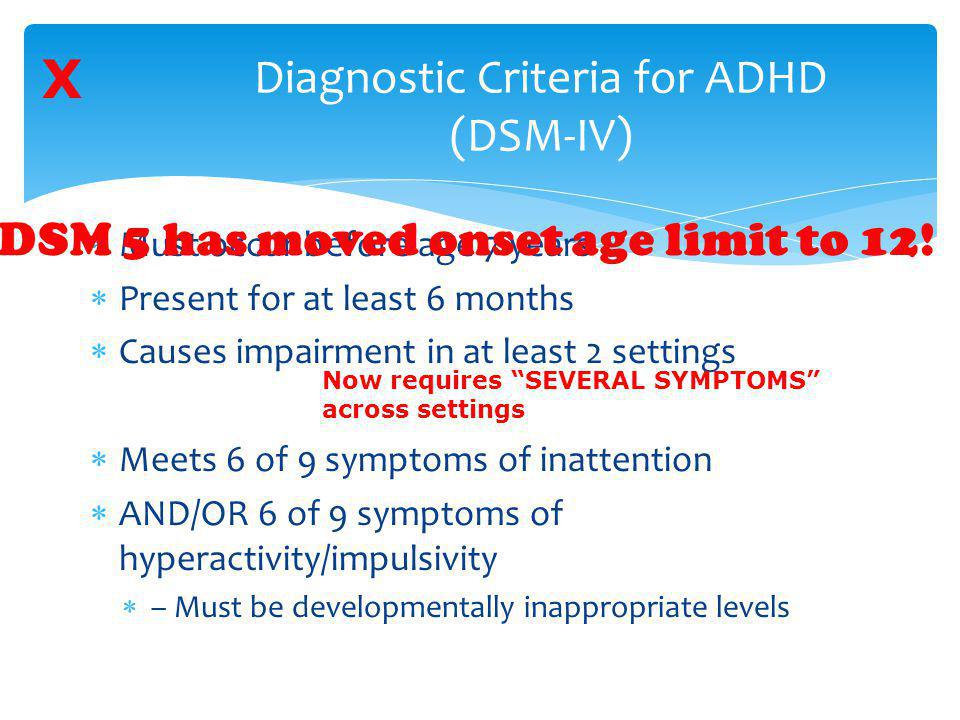
These scales are not to be used as sole diagnostic tools, nor should they replace the full clinical assessment based on the DSM-5® criteria; however, they may help review and quantify symptoms.2
Common behavior rating scales used in adults to assess ADHD and monitor ADHD symptoms.
2-6- The scale has a question for each of the 18 symptom domains identified by the DSM-IV® criteria, with modifications to account for the adult presentation of ADHD symptoms
- Measures the frequency of how often symptoms occur based on a 0 to 4 rating scale (0=never, 1=rarely, 2=sometimes, 3=often, 4=very often)
- Can be used as an initial self-assessment tool to identify adults who may have ADHD but it is not diagnostic in and of itself
- The 6-question subset (Part A) of the ASRS Symptom Checklists comprised of questions that were found to be most predictive of ADHD symptoms
- Scoring is based on how often a symptom occurs
- The 18-item, clinician-based, semistructured interview employs adult-specific language to ensure adequate probing of adult manifestations of ADHD symptoms
- The 18 items in the scale correspond to the 18 symptoms in the DSM-IV® criteria
- Items represent 5 dimensions of symptoms: organizing work, sustaining attention and concentration, sustaining alertness and effort, managing frustration and other emotions, and using work memory
- The scale can be used as a self-report or as a clinician-administered scale
- Scoring is based on a 4-point frequency scale ranging from 0=never to 3=almost daily
- Contains 9 items assessing inattentive symptoms and 9 items assessing hyperactive/impulsive symptoms
- Scoring is based on a 4-point Likert-type severity scale ranging from 0=never to 3=very often
ADHD SCREENER
QandADHD FACT SHEET
Use the QandADHD Fact Sheet for a deeper look at how your patients’ ADHD symptoms extend beyond the workday.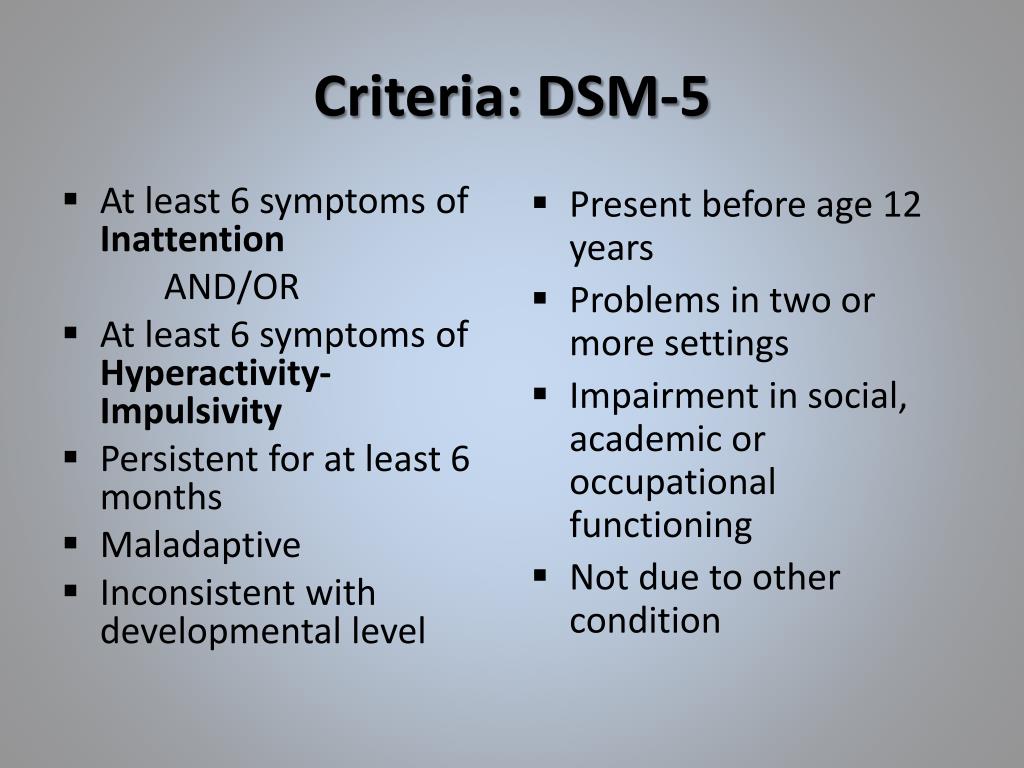
Get the Fact Sheet
References:
- American Psychiatric Association. Attention-deficit and disruptive behavior disorders. In: Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
- Murphy KR, Adler LA. Assessing attention-deficit/hyperactivity disorder in adults: focus on rating scales. J Clin Psychiat. 2004;65[suppl 3]:12-17.
- Adler L, Cohen BA. Diagnosis and evaluation of adults with attention-deficit/hyperactivity disorder. Psychiatr Clin N Am. 2004;27:187-201.
- Kessler RC, Adler L, Ames M, et al. The World Health Organization adult ADHD self-report scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35:245-256.
- Kessler RC, Green JG, Adler LA, et al.
 Structure and diagnosis of adult attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2010;67(11):1168-1178.
Structure and diagnosis of adult attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2010;67(11):1168-1178. - Goodman DW. ADHD in adults: update for clinicians on diagnosis and assessment. Prim Psychiatry. 2009;16(11):21-30.
DSM-5® is a registered trademark of the American Psychiatric Association.
You are about to
leave this website
Please be advised that Shire has no control over the content or presentation of the site you are about to view. Shire’s Privacy Policy does not apply to the website you are about to visit.
If you’d like to keep browsing, click Back.
Or, if you’d like to leave the site, click Continue.
Back Continue
You are about to leave QandADHD.
 com
com
If you’d like to keep browsing, click Back.
Or, if you’d like to leave the site, click Continue.
BACK CONTINUE
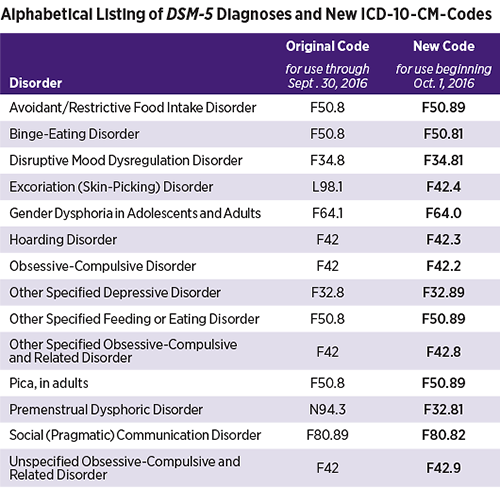
New American classification of mental disorders DSM-5 released to the world
Home > News > The new American classification of mental disorders DSM-5 is released to the world
| DSM-5 consists of three sections: it is (1) an introductory part with instructions for use and a warning about the forensic psychiatric use of the DSM-5; (2) diagnostic criteria and codes for routine clinical use; and (3) tools and techniques to inform clinical decision making. nine0003 Major changes:
The severity of the disorder is not determined by IQ, but by the level of adaptive functioning.
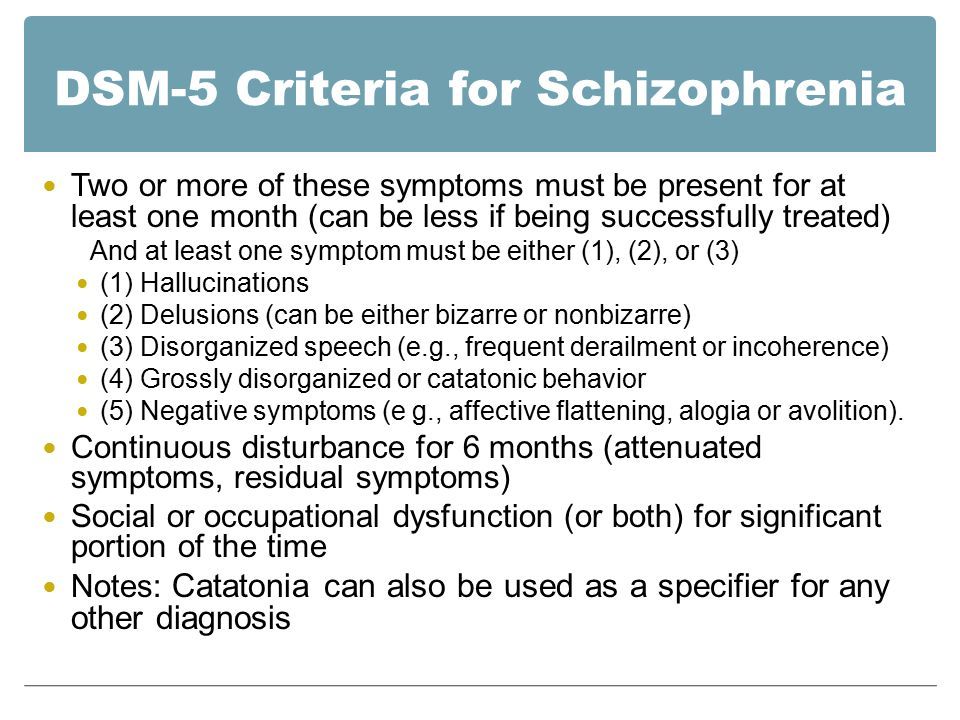
For the diagnosis of schizophrenia, symptoms of the first Schneider rank lose their special weight. One positive symptom is required for a diagnosis to be made. Subtypes are removed - in favor of the dimensional indicator of severity. For schizoaffective disorder, the mood aspect is emphasized, and for delusional disorder, frivolous content is no longer excluded – although it is evaluated separately.
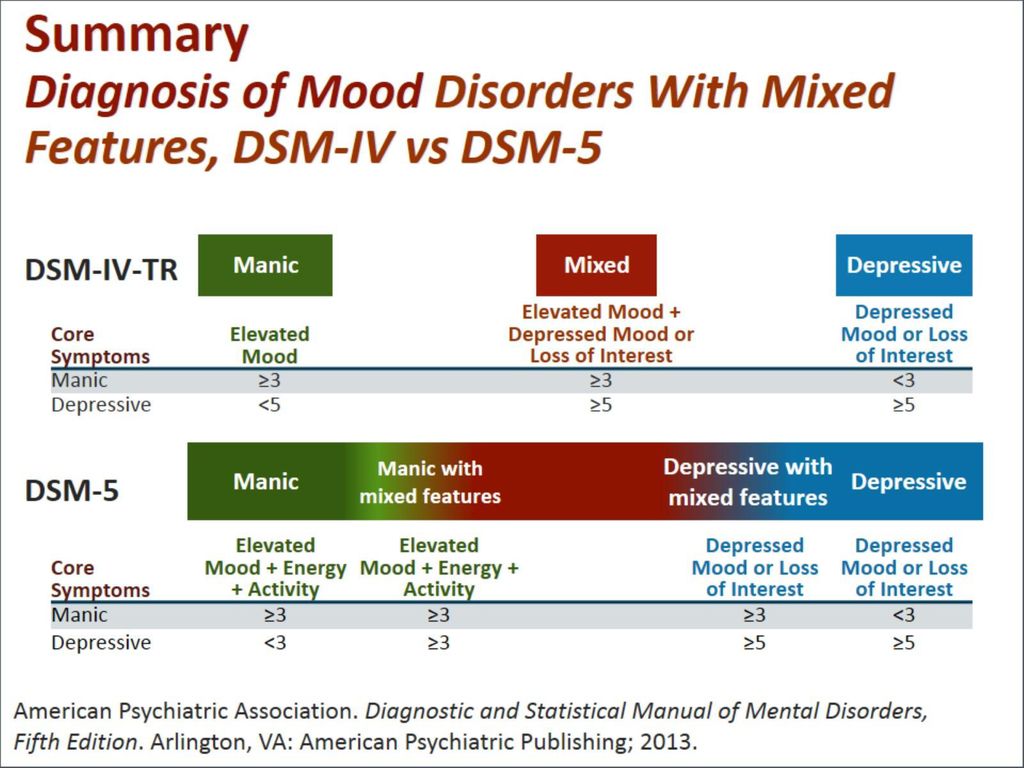
Bipolar and related disorders are now separated from depressive disorders and placed in a separate category. A clearer definition of mania is given and refinements for mixed episodes are introduced, which lowers the threshold for disorder. Added a residual subcategory ""other"" and a qualifying score for anxiety symptoms.
Disruptive mood dysregulation disorder and premenstrual dysphoric disorder added. Chronic depression and dysthymia are combined into one diagnosis, now it is ""persistent depressive disorder (dysthymia)"" with a number of clarifying indicators. Major depressive disorder remained virtually unchanged, however, for "subthreshold" symptoms, a clarifying indicator ""mixed manifestations"" was introduced.
|
ISSN 2588-0519 (Print)
ISSN 2618-8473 (Online)
ADHD (attention deficit hyperactivity disorder): m_d_n — LiveJournal
International Classification of Diseases of the World Health Organization, 10th revision90, and the Diagnostic and Statistical Manual of Mental Disorders IV revision in the new text edition, adopted by the American Psychiatric Association in 2000 (English designations ICD-10 and DSM-IV-TR, respectively), give way to new classifiers. ICD-11 will be officially implemented in 2015, DSM-V will be officially implemented in 2013, http://www.dsm5.org/Pages/Default.aspx mentioned in the new edition. English original http://www.dsm5.org/Documents/ADHD%20Fact%20Sheet.pdf, Russian translation:The Diagnostic and Statistical Manual of Mental Disorders (DSM-V) 5th edition definition of attention deficit/hyperactivity disorder (ADHD) has been updated to better characterize the experiences of adults with ADHD.
 This revision is based on over twenty years of scientific research that shows that ADHD, although it starts in childhood, can last into adulthood for some. Previous editions of the DSM provided no guidance to clinicians regarding the diagnosis of adults with this condition. To ensure that children can receive treatment as adults, if needed, the criteria for ADHD have been reformulated. nine0003
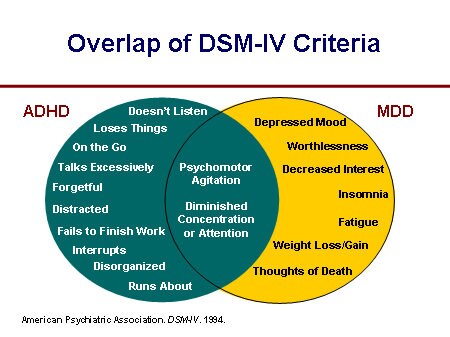
This revision is based on over twenty years of scientific research that shows that ADHD, although it starts in childhood, can last into adulthood for some. Previous editions of the DSM provided no guidance to clinicians regarding the diagnosis of adults with this condition. To ensure that children can receive treatment as adults, if needed, the criteria for ADHD have been reformulated. nine0003 ADHD can be characterized as a behavioral pattern that manifests itself in several areas of activity (eg, school AND home), which affects the executive (functional) level in social, educational and work areas. As in the DSM-IV, the symptoms of the disorder are classified into two categories, inattention and hyperactivity with impulsivity, which includes behaviors such as "not noticing details", "difficulty organizing" a task or activity, "talkative", "fiddling with hands" , "turns around in a chair" rather than sitting on it in appropriate situations. nine0003
Diagnosis of children (under 17 years of age) requires the presence of 6 symptoms (out of 8) from each (or both) of the proposed lists for the criterion "inattention", and for the criterion "hyperactivity and impulsivity". For young people and adults (over 17 years old), the presence of 5 is mandatory. Since the criteria themselves have not changed in content compared to DSM-IV, childhood, adolescence and adulthood can be illustrated with examples of the type of behavior. The descriptions will help clinicians better recognize the typical symptoms of ADHD at each stage of a patient's life. Guided by DSM-5, other symptoms must first appear before the age of 12 years. In a previous revision of the guidelines, the first onset of a symptom was required before the age of 7 years. This change is based on research conducted since 1994-year-olds who found that the clinical presentation and course, severity, recovery and response to treatment in children diagnosed before the age of 7 compared to children diagnosed later did not differ.
For young people and adults (over 17 years old), the presence of 5 is mandatory. Since the criteria themselves have not changed in content compared to DSM-IV, childhood, adolescence and adulthood can be illustrated with examples of the type of behavior. The descriptions will help clinicians better recognize the typical symptoms of ADHD at each stage of a patient's life. Guided by DSM-5, other symptoms must first appear before the age of 12 years. In a previous revision of the guidelines, the first onset of a symptom was required before the age of 7 years. This change is based on research conducted since 1994-year-olds who found that the clinical presentation and course, severity, recovery and response to treatment in children diagnosed before the age of 7 compared to children diagnosed later did not differ.
There are no mutually exclusive criteria in the DSM-5 for Attention Deficit Hyperactivity Disorder and Autism Spectrum Disorder, as the symptoms of both coexist. However, the symptoms of ADHD should not be observed during schizophrenia or other psychotic disorder, and should not be better explained in terms of the clinical picture of another illness, such as depressive or bipolar disorder, anxiety disorder, dissociative disorder, personality disorder, substance intoxication, or withdrawal to intoxication.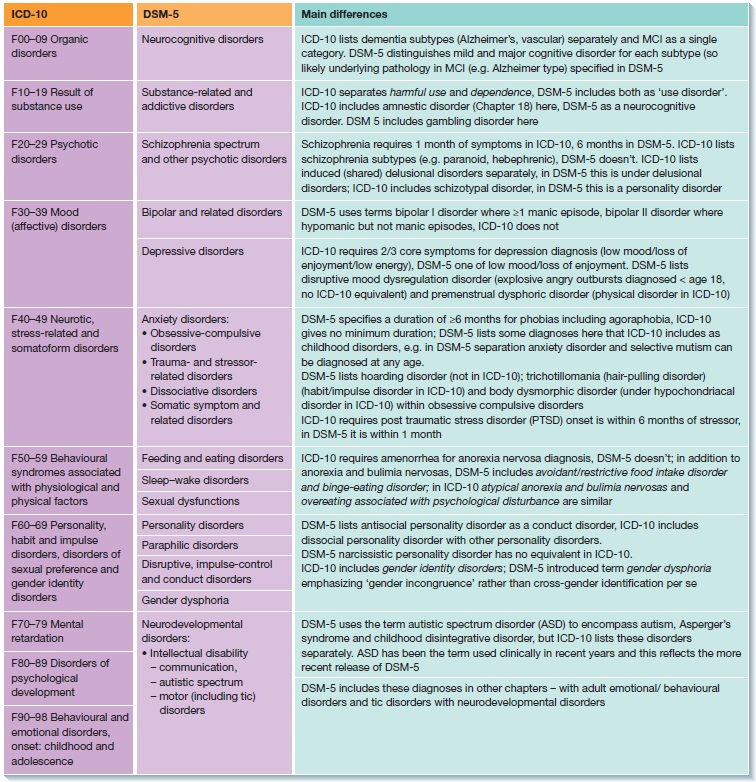
 01 Attention-Deficit/Hyperactivity Disorder, Predominantly Hyperactive-Impulsive Type: if Criterion A2 is met but Criterion A1 is not met for the past 6 months
01 Attention-Deficit/Hyperactivity Disorder, Predominantly Hyperactive-Impulsive Type: if Criterion A2 is met but Criterion A1 is not met for the past 6 months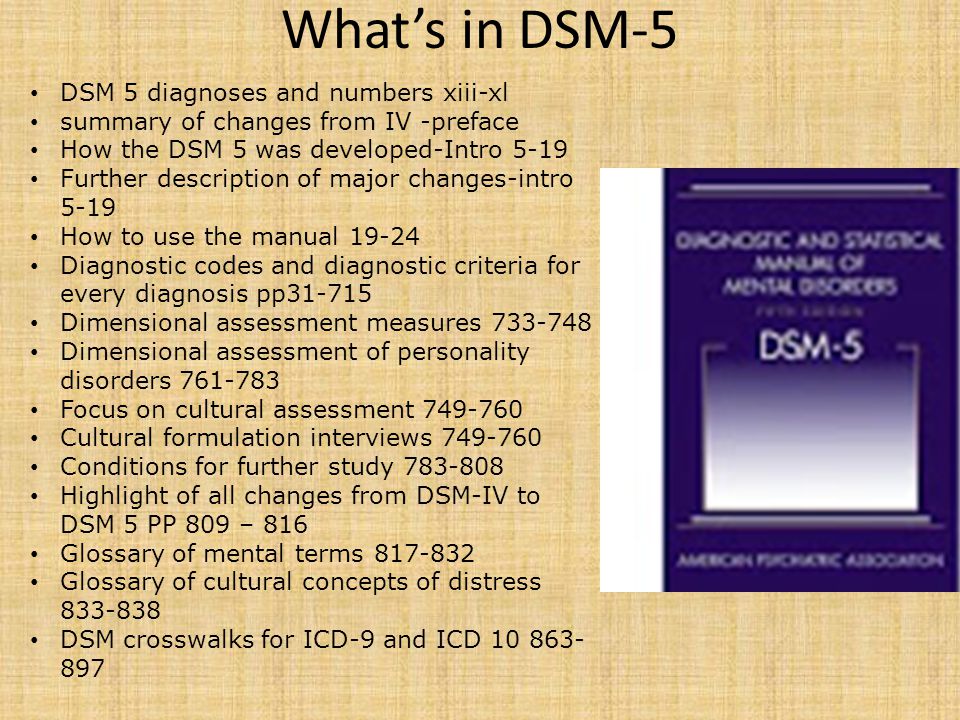
 Speech disorders have entered the new category "social communication disorder", in which some of the syndromes coincide with "autism spectrum disorder". The category "Autism Spectrum Disorders" replaces the DSM-4 diagnoses of autism, Asperger's syndrome, childhood disintegrative disorder, and an unspecified general developmental disorder, all of which cease to exist as separate diagnoses. ADHD can start later (before 12) and is treated differently in different areas. Learning disorders and movement disorders are organized differently in this chapter and somewhat combined. nine0003
Speech disorders have entered the new category "social communication disorder", in which some of the syndromes coincide with "autism spectrum disorder". The category "Autism Spectrum Disorders" replaces the DSM-4 diagnoses of autism, Asperger's syndrome, childhood disintegrative disorder, and an unspecified general developmental disorder, all of which cease to exist as separate diagnoses. ADHD can start later (before 12) and is treated differently in different areas. Learning disorders and movement disorders are organized differently in this chapter and somewhat combined. nine0003 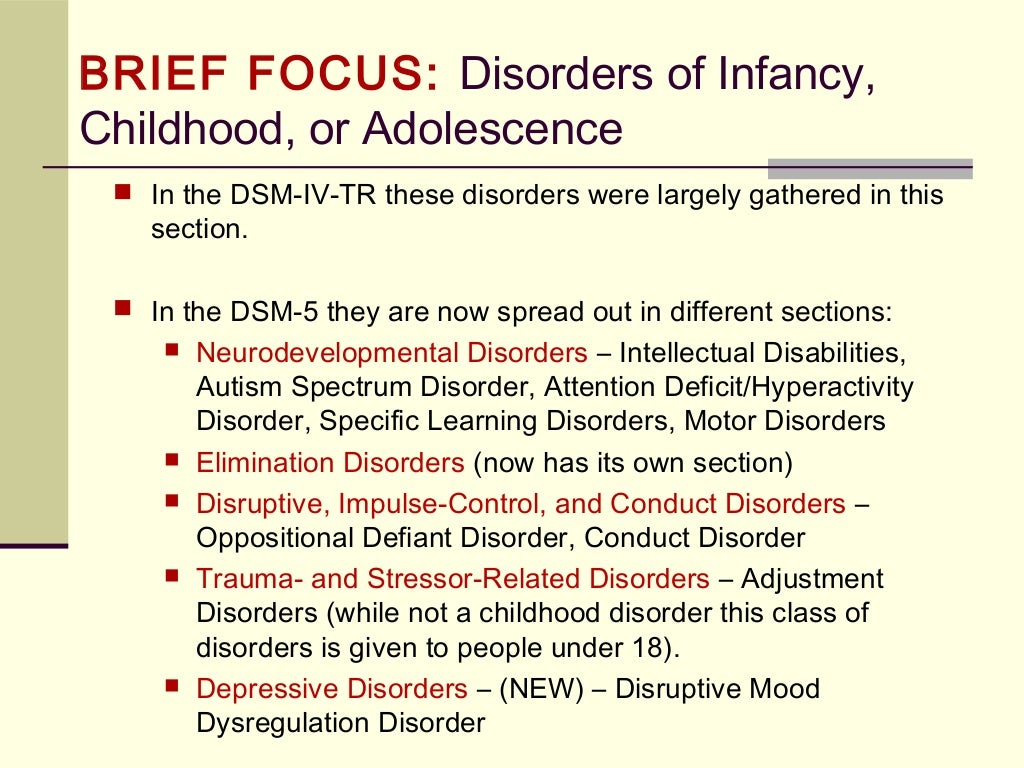 The "catatonia" section has been expanded: this code can now be entered as an adjacent diagnosis (specifying indicator) for depressive, bipolar and psychotic disorders. nine0003
The "catatonia" section has been expanded: this code can now be entered as an adjacent diagnosis (specifying indicator) for depressive, bipolar and psychotic disorders. nine0003 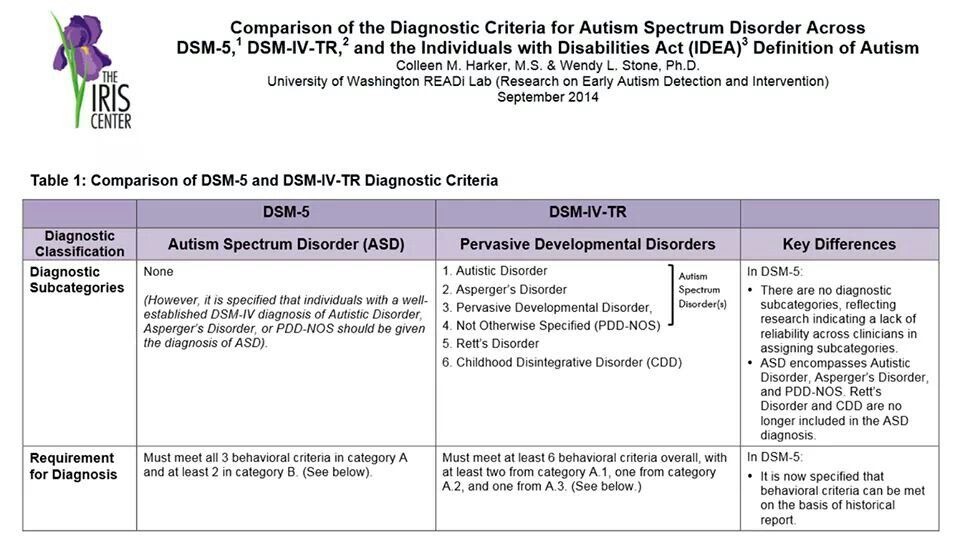 A clarifying indicator for anxious distress has also been introduced. Removed grounds for exclusion for grief. nine(see below) Various phobia criteria are slightly adapted, and agoraphobia and panic are decoupled. Panic attacks can act as a clarifying indicator for other diagnoses. The diagnoses of separation anxiety disorder and selective mutism are no longer specific "childhood" diagnoses. nine0003
A clarifying indicator for anxious distress has also been introduced. Removed grounds for exclusion for grief. nine(see below) Various phobia criteria are slightly adapted, and agoraphobia and panic are decoupled. Panic attacks can act as a clarifying indicator for other diagnoses. The diagnoses of separation anxiety disorder and selective mutism are no longer specific "childhood" diagnoses. nine0003  Also ruled out is the requirement to directly experience fear, horror, or feelings of helplessness. Avoidance and emotional flattening are separated, and at the same time, emotional flattening is added, incl. persistent depressed mood. Recklessness, (auto) destructive behavior, irritability and aggression are added to the already known symptoms of arousal. For children and adolescents in puberty, lower diagnostic thresholds are used. The adjustment disorder remained unchanged. Reactive attachment disorder has been moved to this chapter. nine0003
Also ruled out is the requirement to directly experience fear, horror, or feelings of helplessness. Avoidance and emotional flattening are separated, and at the same time, emotional flattening is added, incl. persistent depressed mood. Recklessness, (auto) destructive behavior, irritability and aggression are added to the already known symptoms of arousal. For children and adolescents in puberty, lower diagnostic thresholds are used. The adjustment disorder remained unchanged. Reactive attachment disorder has been moved to this chapter. nine0003 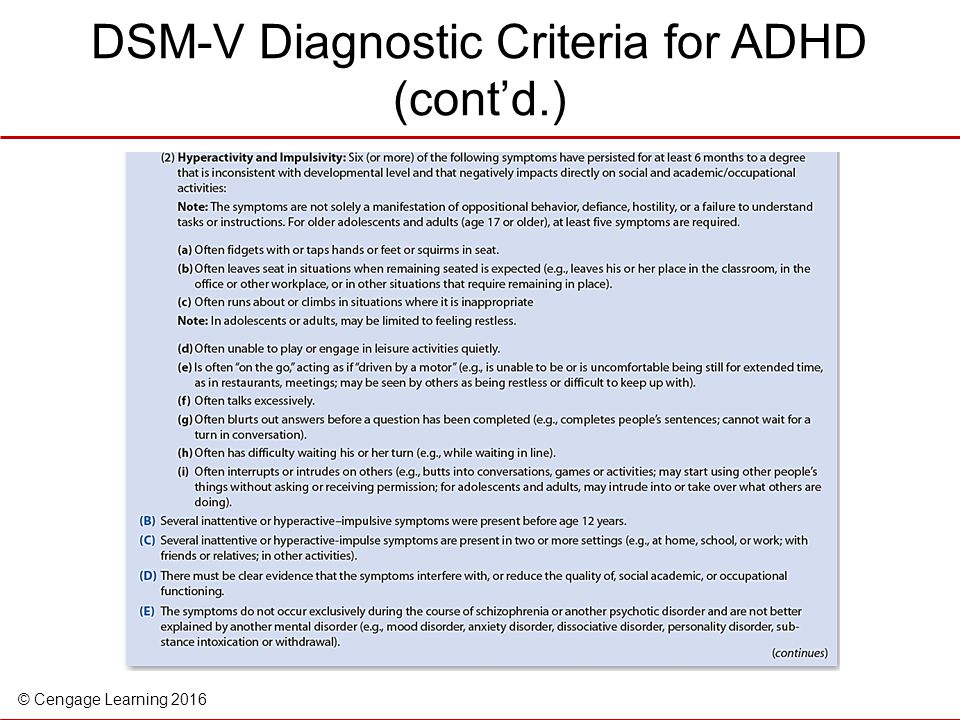 Removed somatization disorder, hypochondriasis, pain disorder, and unspecified somatoform disorder from DSM. A diagnosis of a "disorder with somatic symptoms" can be made on par with a diagnosis from another medical specialty only if the somatic symptoms are associated with abnormal thoughts, feelings, and behaviors. Unexplained medical symptoms play a decisive role only in false pregnancy and conversion (i.e. functional disorder with neurological symptoms). In other cases, positive symptoms should be sought in this group. nine0003
Removed somatization disorder, hypochondriasis, pain disorder, and unspecified somatoform disorder from DSM. A diagnosis of a "disorder with somatic symptoms" can be made on par with a diagnosis from another medical specialty only if the somatic symptoms are associated with abnormal thoughts, feelings, and behaviors. Unexplained medical symptoms play a decisive role only in false pregnancy and conversion (i.e. functional disorder with neurological symptoms). In other cases, positive symptoms should be sought in this group. nine0003  The chapter presents a large number of sleep disorders described in terms of physical characteristics in relation to circadian rhythms and respiratory disorders. This group includes Restless legs syndrome and REM Sleep Behavior Disorder. A large diagnostic choice predisposes to move away from the use of "unspecified" diagnoses. nine0003
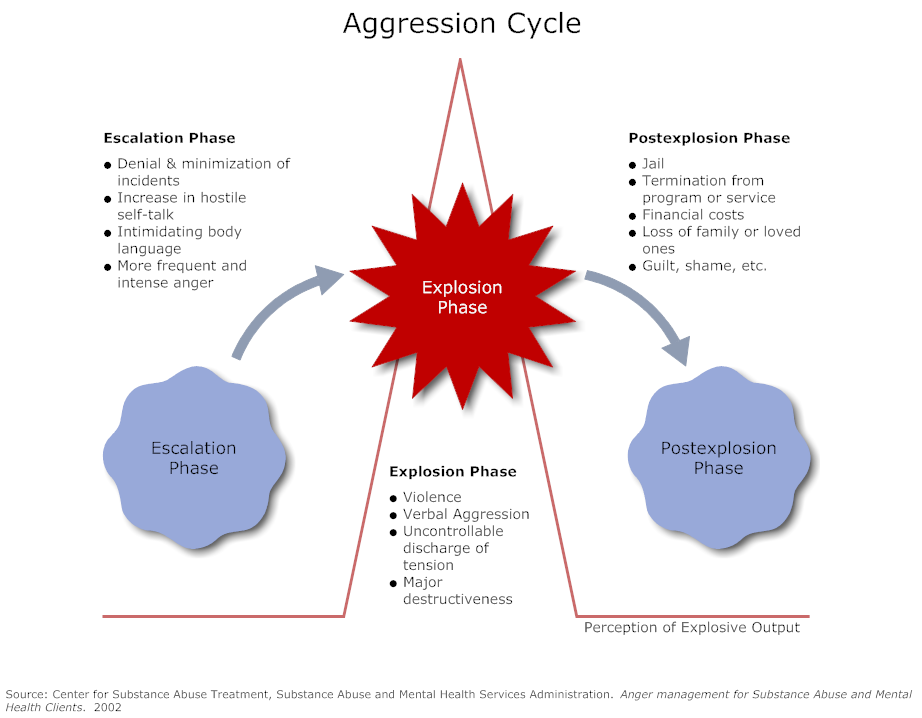
The chapter presents a large number of sleep disorders described in terms of physical characteristics in relation to circadian rhythms and respiratory disorders. This group includes Restless legs syndrome and REM Sleep Behavior Disorder. A large diagnostic choice predisposes to move away from the use of "unspecified" diagnoses. nine0003 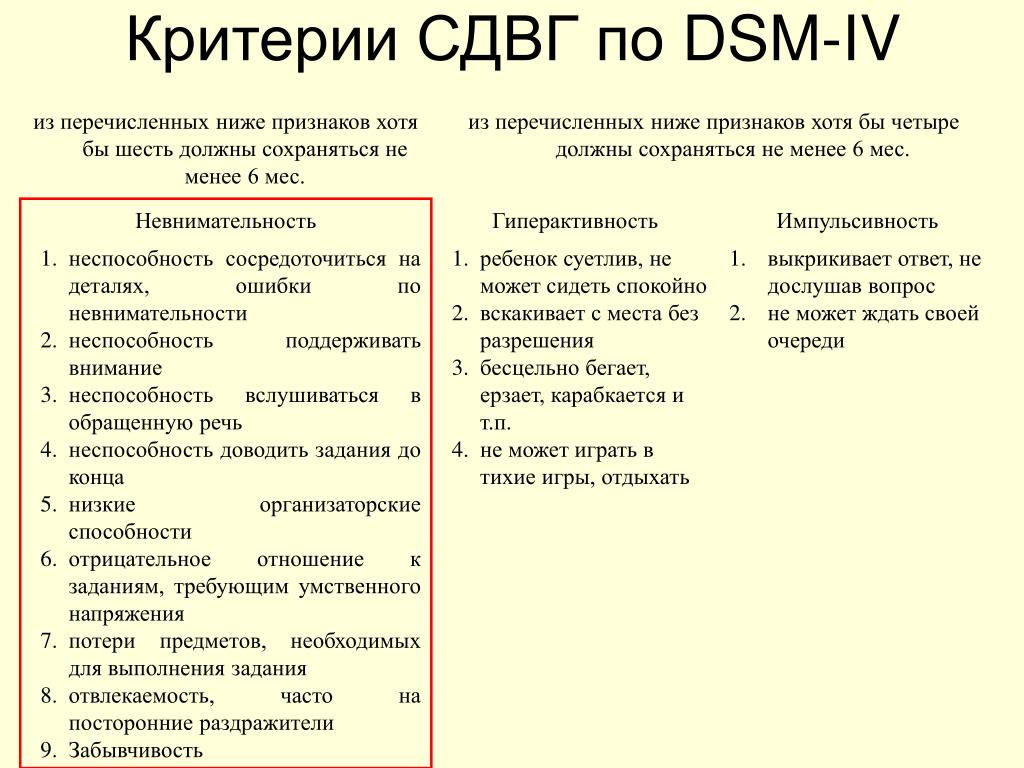 In addition to a variety of impulse control disorders, antisocial personality disorder, dubbed from the chapter on personality disorders, also got here. The criteria for oppositional defiant disorder have been revised and weighted. In conduct disorder (Conduct Disorder), the grounds for excluding the diagnosis have been removed, but the clarifying indicator “callous-unemotional” has been added. Intermittent Explosive Disorder can now be verbal, and the rest of the criteria for this disorder are much more refined. nine0003
In addition to a variety of impulse control disorders, antisocial personality disorder, dubbed from the chapter on personality disorders, also got here. The criteria for oppositional defiant disorder have been revised and weighted. In conduct disorder (Conduct Disorder), the grounds for excluding the diagnosis have been removed, but the clarifying indicator “callous-unemotional” has been added. Intermittent Explosive Disorder can now be verbal, and the rest of the criteria for this disorder are much more refined. nine0003 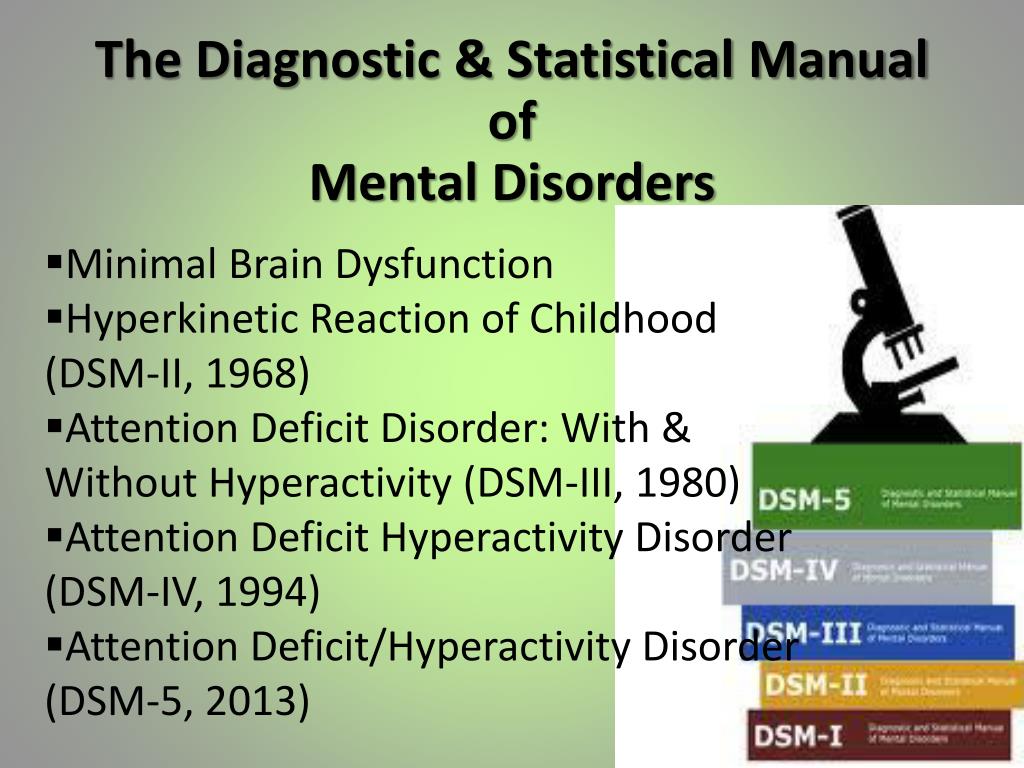 nine0003
nine0003