Drinking on trintellix
Other medications, alcohol, and more
Trintellix (vortioxetine) is a brand-name prescription drug used to treat major depressive disorder in adults. As with other medications, Trintellix can interact with certain other drugs. It can also interact with some supplements. An interaction occurs when one substance causes another substance to have a different effect than expected.
For details about Trintellix’s interactions, keep reading. For additional information about Trintellix, including details about its uses, see this article.
In some cases, factors or conditions could prevent your doctor from prescribing Trintellix due to the risk of harm. These are known as contraindications. The contraindications of Trintellix include:
Taking a monoamine oxidase inhibitor (MAOI)
If you’ve recently taken a monoamine oxidase inhibitor (MAOI), talk with your doctor or pharmacist before taking Trintellix. Similar to Trintellix, MAOIs are used to treat depression.
Taking a combination of Trintellix and an MAOI can increase your risk of a serious side effect called serotonin syndrome. * (With serotonin syndrome, high levels of a chemical called serotonin build up in your body. This can lead to seizures and other life threatening complications.)
Due to this risk, doctors usually won’t prescribe Trintellix if you’re taking an MAOI or have taken one in the past 14 days. Also, your doctor likely won’t recommend starting treatment with an MAOI within 21 days of stopping Trintellix treatment.
Examples of MAOIs include:
- methylene blue (Provayblue)
- tranylcypromine (Parnate)
- phenelzine (Nardil)
- linezolid (Zyvox)
- selegiline (Emsam)
- isocarboxazid (Marplan)
If you take an MAOI, talk with your doctor. They can help determine when it’s safe for you to start Trintellix treatment.
* To learn about this side effect of Trintellix, see this article.
Having had an allergic reaction to Trintellix or any of its ingredients
If you’ve had an allergic reaction to Trintellix or any of its ingredients, your doctor will likely not prescribe Trintellix. Taking the drug could cause another allergic reaction. You can ask your doctor about other treatments that may be better choices for you.
Taking the drug could cause another allergic reaction. You can ask your doctor about other treatments that may be better choices for you.
Note: Before you start treatment with Trintellix, it’s important to tell your doctor if either of these contraindications applies to you. They can determine whether to prescribe Trintellix.
Trintellix is not known to interact with alcohol.
Your doctor may recommend avoiding alcohol when taking Trintellix. This is because alcohol may increase the risk of side effects* of Trintellix. For example, Trintellix may cause:
- nausea
- vomiting
- increased risk of bleeding
Since alcohol may also cause these side effects, the combination of alcohol and Trintellix may increase your risk even more.
If you’d like to drink alcohol while taking Trintellix, talk with your doctor about how much, if any, is safe for you.
* To learn about side effects of Trintellix, see this article.
Before you start treatment with Trintellix, tell your doctor and pharmacist which prescription, over-the-counter, and other medications you take. By sharing this information with them, you may help prevent possible interactions.
By sharing this information with them, you may help prevent possible interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Here’s a chart of drugs that can interact with Trintellix. Keep in mind that this chart doesn’t include all drugs that may interact with Trintellix. Some of these interactions are described in detail just below in “Drug interactions in depth.”
| Drug type or drug name | Drug examples | Interaction result with Trintellix |
| monoamine oxidase inhibitors (MAOIs) | • methylene blue (Provayblue) • tranylcypromine (Parnate) • phenelzine (Nardil) | can increase the risk of side effects from both Trintellix* and MAOIs† |
| selective serotonin reuptake inhibitors (SSRIs) | • sertraline (Zoloft) • escitalopram (Lexapro) • fluoxetine (Prozac) • paroxetine (Paxil) | can increase the risk of side effects from both Trintellix* and SSRIs |
| serotonin-norepinephrine reuptake inhibitors (SNRIs) | • duloxetine (Cymbalta) • desvenlafaxine (Pristiq) • venlafaxine (Effexor XR) | can increase the risk of side effects from both Trintellix* and SNRIs |
| triptans | • rizatriptan (Maxalt, Maxalt-MLT) • eletriptan (Relpax) • sumatriptan (Imitrex) | can increase the risk of side effects from both Trintellix* and triptans |
| tricyclic antidepressants (TCAs) | • amitriptyline • nortriptyline (Pamelor) • doxepin (Silenor) | can increase the risk of side effects from both Trintellix* and TCAs |
| nonsteroidal anti-inflammatory drugs (NSAIDs) | • ibuprofen (Advil, Motrin) • celecoxib (Celebrex) • naproxen (Aleve, Naprosyn) | can increase the risk of side effects from both Trintellix* and NSAIDs |
| certain pain medications | • fentanyl (Actiq, Fentora, others) • tramadol (ConZip) • oxycodone (Oxaydo, Roxicodone, others) | can increase the risk of side effects from both Trintellix* and certain pain medications |
| certain treatments for attention deficit hyperactivity disorder (ADHD) | • amphetamine salts (Adderall) • methylphenidate (Concerta, Ritalin, others) • lisdexamfetamine (Vyvanse) | can increase the risk of side effects from both Trintellix* and certain ADHD medications |
| CYP2D6 blockers | • bupropion (Wellbutrin SR, Wellbutrin XL) • fluoxetine (Prozac) • quinidine | can increase the risk of side effects from Trintellix* |
| CYP2D6 inducers | • rifampin (Rifadin, Rimactane) • carbamazepine (Carbatrol, Tegretol, others) • phenytoin (Dilantin, Phenytek) | can reduce the effectiveness of Trintellix |
| drugs that increase the risk of bleeding | • aspirin • clopidogrel (Plavix) • heparin • warfarin (Jantoven) | can increase the risk of side effects from both Trintellix* and drugs that increase the risk of bleeding |
| diuretics | • hydrochlorothiazide (Microzide) • spironolactone (Aldactone, CaroSpir) • furosemide (Lasix) | can increase the risk of side effects from both Trintellix* and diuretics |
| ergotamines | • dihydroergotamine (Migranal, Trudhesa) • ergotamine/caffeine (Migergot) • ergotamine tartrate (Ergomar) • methylergonovine (Methergine) | can increase the risk of side effects from both Trintellix* and ergotamines |
| lithium (Lithobid) | — | can increase the risk of side effects from both Trintellix* and lithium |
| buspirone | — | can increase the risk of side effects from both Trintellix* and buspirone |
| dextromethorphan (Delsym) | — | can increase the risk of side effects from both Trintellix* and dextromethorphan |
| phentermine (Adipex-P, Lomaira) | — | can increase the risk of side effects from both Trintellix* and phentermine |
* To learn about side effects of Trintellix, see this article.
† For more details, see the “When to avoid Trintellix” section above.
Here’s a closer look at certain drug interactions of Trintellix.
Selective serotonin reuptake inhibitors (SSRIs)
Selective serotonin reuptake inhibitors (SSRIs) are drugs that can be used to treat depression, panic disorder, and obsessive-compulsive disorder.
Interaction result. Taking Trintellix and an SSRIcan increase the risk of serotonin syndrome* and other side effects. (With serotonin syndrome, high levels of a chemical called serotonin build up in your body. This can lead to seizures and other life threatening complications.)
Interaction explained. Trintellix and SSRIs may work in similar ways to treat your depression. Both drugs are thought to increase the level of serotonin in your body. And taking multiple drugs that affect serotonin can increase your risk of serious side effects, such as serotonin syndrome.
Examples of SSRI drugs. Here are some SSRIs that may interact with Trintellix:
Here are some SSRIs that may interact with Trintellix:
- sertraline (Zoloft)
- escitalopram (Lexapro)
- fluoxetine (Prozac)
- paroxetine (Paxil)
Steps you or your doctor may take. Before starting Trintellix treatment, tell your doctor if you take any SSRIs. They may recommend that you avoid taking SSRIs along with Trintellix. Your doctor will recommend the best treatment plan for your depression.
However, if your doctor prescribes Trintellix with an SSRI, they may monitor you more often for symptoms of serotonin syndrome. You can also watch for these symptoms. They may include anxiety, hallucinations, sweating, and muscle spasms. If you have any of these symptoms, contact your doctor or seek emergency help right away.
* To learn about this side effect of Trintellix, see this article.
CYP2D6 inducers
CYP2D6 inducers are drugs that can be used for different conditions, including seizures and infections.
Interaction result. Taking Trintellix and a CYP2D6 inducer together can decrease the effectiveness of Trintellix.
Interaction explained. Trintellix is broken down in your body by an enzyme (a type of protein) called CYP2D6. Some drugs may cause CYP2D6 to work faster than usual. These are known as CYP2D6 inducers.
If you take Trintellix and a CYP2D6 inducer, the inducer may cause the CYP2D6 enzyme to break down Trintellix more quickly. This means you’ll have less Trintellix in your body than usual. So, the drug likely won’t be as effective as it should be.
Examples of CYP2D6 inducers. Here are some CYP2D6 inducers that may interact with Trintellix:
- rifampin (Rifadin, Rimactane)
- carbamazepine (Carbatrol, Tegretol, others)
- phenytoin (Dilantin, Phenytek)
Steps you or your doctor may take. Before starting treatment with Trintellix, tell your doctor about any medications that you take. Your doctor or pharmacist can look through your current medications to see if you take any CYP2D6 inducers. In some cases, if you’re taking a CYP2D6 inducer, your doctor may prescribe a higher dose of Trintellix. (To learn about the dosages of Trintellix, see this article.)
Your doctor or pharmacist can look through your current medications to see if you take any CYP2D6 inducers. In some cases, if you’re taking a CYP2D6 inducer, your doctor may prescribe a higher dose of Trintellix. (To learn about the dosages of Trintellix, see this article.)
Tricyclic antidepressants (TCAs)
Tricyclic antidepressants (TCAs) are often used to treat depression.
Interaction result. Taking Trintellix with TCAscan increase the risk of serotonin syndrome.
Interaction explained. Trintellix can increase the levels of a chemical in your body called serotonin. TCAs can also increase your serotonin levels. So, taking this combination of medications may increase the risk further. When serotonin levels become too high, a serious side effect called serotonin syndrome can occur.
Examples of TCA drugs. Here are some TCAs that may interact with Trintellix:
- amitriptyline
- nortriptyline (Pamelor)
- doxepin (Silenor)
Steps you or your doctor may take.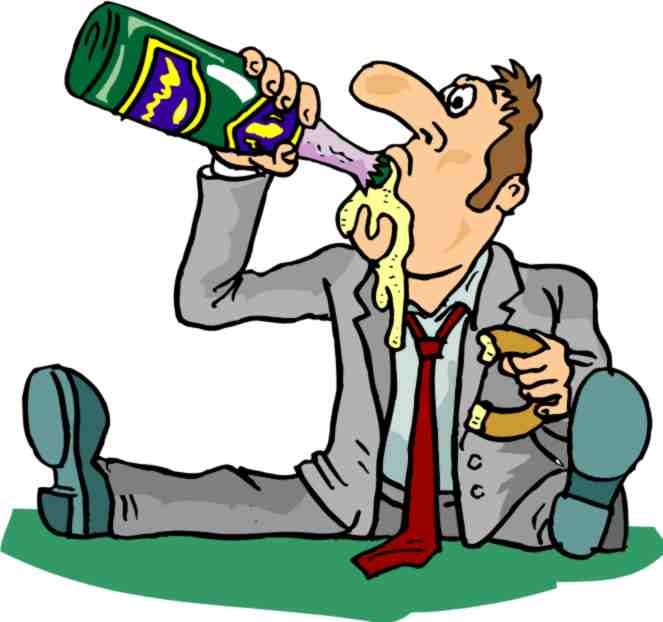 Before starting Trintellix treatment, tell your doctor if you take any TCAs. Your doctor can look through your current medications and help identify if any are TCAs.They’ll likely recommend that you avoid these medications during Trintellix treatment. Your doctor will recommend the best treatment plan for your condition.
Before starting Trintellix treatment, tell your doctor if you take any TCAs. Your doctor can look through your current medications and help identify if any are TCAs.They’ll likely recommend that you avoid these medications during Trintellix treatment. Your doctor will recommend the best treatment plan for your condition.
If your doctor prescribes Trintellix with a TCA, they may monitor you more often for symptoms of serotonin syndrome. You can also watch for these symptoms, which may include anxiety, hallucinations, sweating, and muscle spasms. If you have any of these symptoms, contact your doctor or seek emergency help right away.
Trintellix may have other interactions, such as with supplements, foods, vaccines, or even lab tests. You’ll find details below. Keep in mind that the following information does not include all other possible interactions with Trintellix.
Trintellix interactions with supplements
Before you start treatment with Trintellix, tell your doctor and pharmacist which supplements, herbs, and vitamins you take. By sharing this information with them, you may help prevent possible interactions.
By sharing this information with them, you may help prevent possible interactions.
It’s possible for certain supplements to increase your serotonin levels. (Serotonin is a chemical in your body.) Trintellix can also raise serotonin levels. So, taking certain supplements with Trintellix may increase serotonin levels further.
If serotonin levels become too high, serotonin syndrome could occur. This can lead to seizures and other life threatening complications.
Examples of these supplements may include:
- tryptophan
- 5-hydroxytryptophan
If you have questions about the above supplements or any drug interactions that may affect you, ask your doctor or pharmacist.
Trintellix interactions with herbs
Certain herbs, such as St. John’s wort, can increase your serotonin levels. Similar to Trintellix, St. John’s wort can increase serotonin levels. So, taking certain this herb with Trintellix may increase serotonin levels even more. This could lead to serotonin syndrome, which could cause seizures and other life threatening complications.
If you have questions about what herbs you can take with Trintellix, talk with your doctor or pharmacist.
Trintellix and vitamins
There are no specific reports of vitamins interacting with Trintellix. However, it’s possible that interactions with vitamins could be recognized in the future. Because of this, you should talk with your doctor or pharmacist before taking any vitamin product with Trintellix.
Trintellix and food
There were no reports of food interactions with Trintellix. The drug isn’t known to interact with any foods. And Trintellix shouldn’t affect your appetite. If you’d like to learn more about eating certain foods during treatment with Trintellix, talk with your doctor.
Trintellix and vaccines
There aren’t any known interactions between Trintellix and vaccines. However, if you need to get any vaccines during your treatment with Trintellix, talk with your doctor or pharmacist. They can help make sure that none of your other medications interact with the vaccines.
Trintellix and lab tests
There aren’t any known interactions between Trintellix and lab tests. However, if you need to have any lab tests done, talk with your doctor about any medications that you take. They can help make sure that none of your other medications will interact with your lab tests.
TRINTELLIX INTERACTION WITH CANNABIS OR CBDCannabis (often called marijuana) and cannabis products, such as cannabidiol (CBD), have not been specifically reported to interact with Trintellix. However, as with any drug or supplement, talk with your doctor before using cannabis in combination with Trintellix. The impact of cannabis may affect how well you stick to your Trintellix treatment plan.
Note: Cannabis is illegal at a federal level but is legal in many U.S. states to varying degrees.
Certain medical conditions and other factors may increase the risk of interactions with Trintellix. Before you take this drug, be sure to talk with your doctor about your health history. Trintellix may not be the right treatment option if you have certain medical conditions or other factors affecting your health.
Trintellix may not be the right treatment option if you have certain medical conditions or other factors affecting your health.
Health conditions or factors that might interact with Trintellix include:
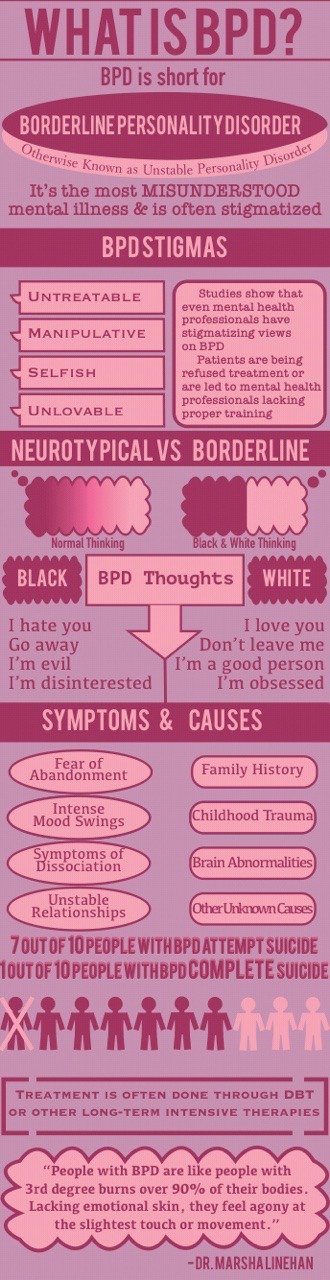
Suicidal thoughts and behaviors. Before taking Trintellix, tell your doctor if you’ve ever had mood problems, such as suicidal thoughts or behaviors. The drug has a boxed warning about the risk of suicidal thoughts and behaviors in certain people. A boxed warning is a serious warning from the Food and Drug Administration (FDA). For details, refer to “Boxed warning” at the top of this article.
Seizures or seizure disorders. Tell your doctor if you’ve ever had any seizures or if you currently have a seizure disorder. In rare cases, it’s possible for Trintellix to increase your risk of seizures. So if you’ve ever had these conditions, you may have an increased risk of this side effect with the drug.
You may also have an increased risk of seizures if you stop taking Trintellix suddenly. Talk with your doctor to see whether Trintellix may be a safe treatment option for you.
Talk with your doctor to see whether Trintellix may be a safe treatment option for you.
Personal or family history of mood problems. If you have or have had any mood problems other than depression, tell your doctor before starting Trintellix treatment. Also tell them if anyone in your family has or has had a mood problem, including bipolar disorder. Trintellix can increase your risk of mood problems. Your doctor can help determine whether this medication is safe for you.
Glaucoma. It’s possible for Trintellix to cause or worsen glaucoma. If you already have glaucoma, taking Trintellix may worsen your condition. In this case, your doctor can help determine whether Trintellix is right for you.
Low sodium levels in your blood. It’s possible for Trintellix to lower sodium levels in your blood. And, if you already have low blood sodium levels, taking Trintellix may worsen your condition.
If your blood sodium levels become too low, you may have increased risk of serious problems. These include memory problems, confusion, hallucinations, breathing problems, and seizures. Due to this risk, your doctor will likely treat your low sodium levels before you take Trintellix.
These include memory problems, confusion, hallucinations, breathing problems, and seizures. Due to this risk, your doctor will likely treat your low sodium levels before you take Trintellix.
Bleeding problems. If you have any bleeding problems or bleeding disorders, such as hemophilia, tell your doctor before starting Trintellix treatment. This medication may increase your risk of bleeding, including serious bleeding in your digestive system. If you already have a bleeding disorder, you may have an increased risk of this side effect. Your doctor can help determine whether Trintellix is safe for you.
Pregnancy. It’s not known if it’s safe to take Trintellix during pregnancy. If you’re pregnant or planning to become pregnant, talk with your doctor to see whether it may be safe for you to take Trintellix.(For details about Trintellix and pregnancy, see this article.)
Breastfeeding. It’s unknown if it’s safe to take Trintellix while breastfeeding. Currently, it’s not known if the drug passes into breast milk or what effects it may have on a breastfed child. If you’re breastfeeding, talk with your doctor before taking Trintellix.
Currently, it’s not known if the drug passes into breast milk or what effects it may have on a breastfed child. If you’re breastfeeding, talk with your doctor before taking Trintellix.
Allergic reaction. If you’ve had an allergic reaction to Trintellix or any of its ingredients, your doctor will likely not prescribe Trintellix. To learn more, see “When to avoid Trintellix” above.
Suicide prevention
If you know someone at immediate risk of self-harm, suicide, or hurting another person:
- Ask the tough question: “Are you considering suicide?”
- Listen to the person without judgment.
- Call 911 or the local emergency number, or text TALK to 741741 to communicate with a trained crisis counselor.
- Stay with the person until professional help arrives.
- Try to remove any weapons, medications, or other potentially harmful objects.
If you or someone you know is having thoughts of suicide, a prevention hotline can help. The 988 Suicide and Crisis Lifeline is available 24 hours a day at 988. During a crisis, people who are hard of hearing can use their preferred relay service or dial 711 then 988.
The 988 Suicide and Crisis Lifeline is available 24 hours a day at 988. During a crisis, people who are hard of hearing can use their preferred relay service or dial 711 then 988.
Click here for more links and local resources.
Was this helpful?
Here are some frequently asked questions about Trintellix and possible interactions.
Does Trintellix interfere with sleep medications?
No, Trintellix shouldn’t interfere with sleep medications. So, if you take a sleep medication, it’s likely safe to continue taking it during Trintellix treatment.
Examples of sleep medications that are likely safe to take with Trintellix include:
- zolpidem (Ambien)
- eszopiclone (Lunesta)
- ramelteon (Rozerem)
It’s important to note that Trintellix may cause sleeping problems in rare cases. These problems may occur if you experience manic episodes (periods of high energy or excitement) or develop worsening depression or mood changes from Trintellix treatment.
If you notice changes in your sleep pattern when starting Trintellix treatment, talk with your doctor. They can help determine what may be causing them and suggest possible treatments.
Are there any interactions between Trintellix and Viagra?
No, there aren’t any known interactions between Trintellix and sildenafil (Viagra). However, Trintellix may affect you sexually and increase your risk of developing sexual side effects. These can include:
- delayed ejaculation
- decreased libido (sex drive)
- problems having or maintaining an erection
So, if you develop sexual side effects while taking Trintellix, your doctor may prescribe Viagra if you’re male.* Talk with your doctor if you have questions about sexual side effects from Trintellix or how to best treat them.
* Sex and gender exist on spectrums. Use of the term “male” in this article refers to sex assigned at birth.
What antidepressant works well with Trintellix?
Your doctor can help determine whether another antidepressant may work well with Trintellix.
However, other antidepressants aren’t typically prescribed with Trintellix due to possible interactions. These include selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), and tricyclic antidepressants (TCAs). (To learn more, see the “Trintellix interactions with other medications” section above.)
Instead of antidepressants, your doctor may prescribe other drugs along with Trintellix to treat your depression. For example, your doctor may recommend taking Trintellix with antipsychotic drugs that are approved to treat depression. These include lurasidone (Latuda), brexpiprazole (Rexulti), and aripiprazole (Abilify). These drugs are not known to interact with Trintellix.
To learn about which drugs you can safely take with Trintellix, be sure to talk with your doctor or pharmacist.
Does Trintellix affect dopamine?
No, Trintellix shouldn’t affect dopamine levels in your body. Dopamine is a chemical messenger that helps regulate certain moods and emotions.
Instead, Trintellix works to treat depression by affecting the levels of another chemical called serotonin. Other antidepressants, such as bupropion (Wellbutrin SR, Wellbutrin XL), work by affecting the levels of dopamine and another chemical called norepinephrine.
If you have questions or concerns about how Trintellix works differently than other antidepressants, talk with your doctor or pharmacist.
You can take certain steps to help prevent interactions with Trintellix. Your doctor and pharmacist are key resources, so reach out to them before starting treatment. For example, you should plan to do the following:
- Let them know if you drink alcohol or use cannabis.
- Tell them about any other medications you take, as well as any supplements, herbs, and vitamins.
- Create a medication list, which your doctor and pharmacist can help you fill out.
It’s also important to read the Trintellix label and other paperwork that may come with the drug. The label may have colored stickers that mention an interaction. And the paperwork, sometimes called the medication guide or patient package insert, may contain details about interactions. (If Trintellix doesn’t come with paperwork, you can ask your pharmacist to print a copy.) If you have questions about this information, ask your doctor or pharmacist.
The label may have colored stickers that mention an interaction. And the paperwork, sometimes called the medication guide or patient package insert, may contain details about interactions. (If Trintellix doesn’t come with paperwork, you can ask your pharmacist to print a copy.) If you have questions about this information, ask your doctor or pharmacist.
You can also help prevent interactions with Trintellix by taking it exactly as your doctor prescribes.
Besides learning about interactions, you may want to find out more about Trintellix. These resources might help:
- Overview of Trintellix. For a general overview of Trintellix, see this article.
- Side effects. If you’re interested in the side effects of Trintellix, see this article. Another option is to refer to the Trintellix prescribing information.
- Dosage specifics. To learn about the dosage of Trintellix, see this article.
- Drug comparison.
 For information about how Trintellix compares with Zoloft, Wellbutrin, Lexapro, and more, read this article.
For information about how Trintellix compares with Zoloft, Wellbutrin, Lexapro, and more, read this article. - Facts about depression. To learn more about your condition, see our depression hub.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.
What happens when you mix Trintellix and alcohol?
Here’s what you should know about drinking while taking this SSRI depression medication
Improving your symptoms of depression has been important to you and you’ve recently started on Trintellix to see if it makes you feel better. Now, you have an invitation from a friend to come over for a glass of wine that evening to catch up.
You’re wondering, is it safe to mix Trintellix and alcohol?
What is Trintellix?
Trintellix (vortioxetine) is in a class of medications known as selective serotonin reuptake inhibitors (SSRIs). Unlike some other SSRIs such as Prozac, Trintellix hasn’t been on the market long. It received its FDA approval for use in the United States in 2013. It’s a type of antidepressant used to treat major depressive disorder (MDD).
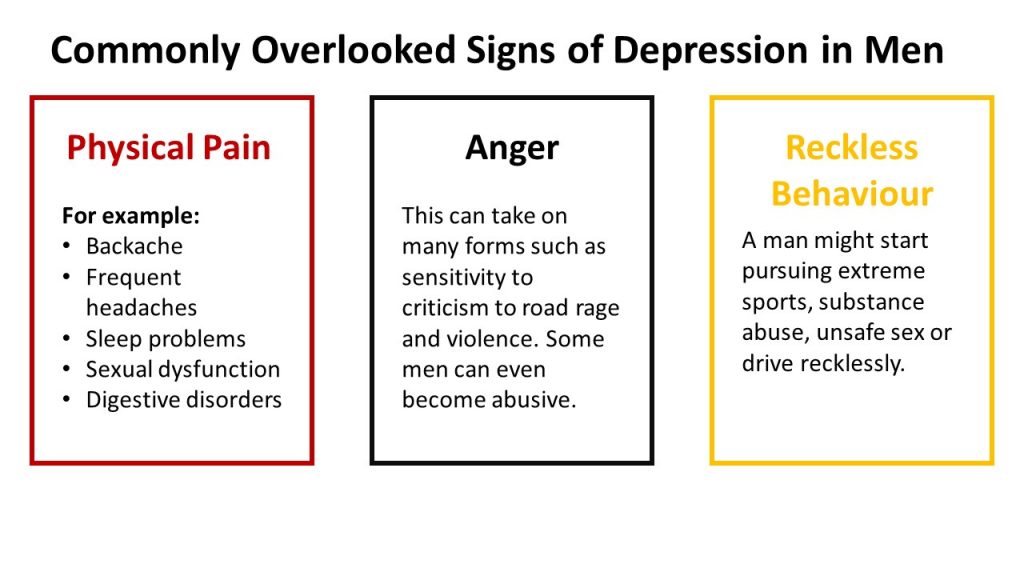
MDD is also known as depression and can include symptoms such as:
- Feelings of hopelessness
- Loss of interest in previously enjoyable activities
- Reduced energy
- Trouble sleeping
- Difficulty concentrating
If you have MDD, these symptoms affect you almost daily for at least two weeks at a time.
It’s not clear exactly how Trintellix works in the body, but it’s thought to increase serotonin, an important neurotransmitter in the brain. Low levels of serotonin may be linked to symptoms of depression.
Is it safe to mix alcohol with Trintellix?
The short answer is no, it’s not recommended to drink alcohol while you’re taking Trintellix. But it’s not black and white when it comes to avoiding alcohol completely while on Trintellix.
Trintellix’s prescribing information doesn’t list alcohol as a contraindication or warning. Also, the effects of Trintellix on the liver appear to be minimal, says John Mendelson, MD, the chief medical officer at Ria Health. There’s a chance you could experience abnormal liver enzyme levels, but elevations of these enzymes are rare. Over time, as you continue to take Trintellix, those levels would go back down to normal. Also, with the available data, there haven’t been instances of sudden liver damage or jaundice.
So while Trintellix rarely causes extensive damage to the liver, there are reasons you should be cautious when taking this medication with alcohol.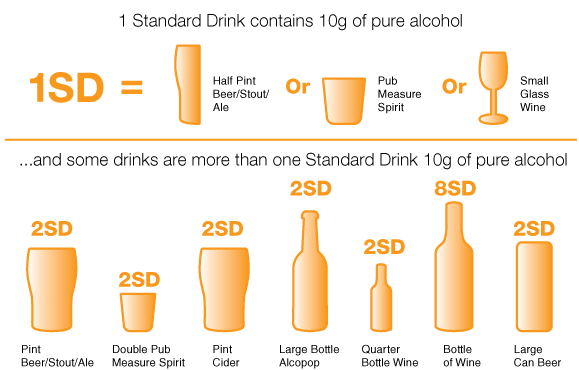
Drinking that glass of wine can increase the side effects you might experience while taking Trintellix. These side effects can include feeling dizzy, feeling sleepy, and having trouble focusing. If you experience these side effects, you may feel them even more if you drink alcohol.
“No amount of alcohol is safe,” explains Seema Bonney, MD, the founder and medical director of the Anti-Aging & Longevity Center of Philadelphia. “Alcohol and Trintellix shouldn’t be consumed together as [the combination] may cause dizziness and vomiting.”
Can you drink alcohol while taking other antidepressants?
The Food and Drug Administration (FDA) states Trintellix doesn’t “increase the impairment of mental and motor skills caused by alcohol.” This doesn’t mean there’s no risk, though.
Alcohol itself is a central nervous system depressant. It can cause you to become drowsy, feel uncoordinated, and have slurred speech. The problem is, antidepressants can cause the same effects.
According to Dr. Bonney, since alcohol is a depressant it could actually worsen your symptoms of depression over time. Chronic alcohol use has been linked to lower serotonin levels. Since the goal of taking Trintellix is to increase your serotonin levels, the alcohol you drink can undo all the work your antidepressant is trying to do.
According to the National Institute on Alcohol Abuse and Alcoholism, alcohol shouldn’t be used with medications to treat depression. Some of these medications include:
- Abilify (aripiprazole)
- Cymbalta (duloxetine)
- Effexor (venlafaxine)
- Invega (paliperidone)
- Lexapro (escitalopram)
- Paxil (paroxetine)
- Prozac (fluoxetine)
- Zoloft (sertraline)
Monoamine oxidase inhibitors (MAOIs), a type of medication used to treat depression, can cause dangerously high blood pressure when mixed with alcohol. MAOIs can prevent the breakdown of tyramine, a substance found in certain foods and alcoholic drinks that can cause high blood pressure in large amounts.
MAOIs can prevent the breakdown of tyramine, a substance found in certain foods and alcoholic drinks that can cause high blood pressure in large amounts.
Wellbutrin (bupropion) can lower your tolerance for alcohol. This means it can take less alcohol than you would usually drink in order to feel its effects.
RELATED: Zoloft and alcohol
Does alcohol make depression worse?
Drinking alcohol can make your depression symptoms worse. For some people, alcohol is used to self-treat depression. Alcohol can make you feel relaxed and less anxious in the short term, but it can also cause you to feel more depressed in the long term.
“One big concern with drinking alcohol is that it actually undermines the primary medical purpose of taking an antidepressant,” explains Dr. Bonney. “It makes you more likely to have worsening depression or anxiety.”
According to Dr. Bonney, drinking alcohol while on antidepressants can also cause:
- Suicidal thoughts and ideas
- Dizziness and nausea
- Severe anxiety
- Headaches
- Impaired coordination
- Digestive problems
- Slurred speech
- Impaired judgment and motor skills
Everyone has their own unique situation and comfort level with drinking alcohol. If you have questions about taking Trintellix for depression, its side effects, or whether you can combine Trintellix and alcohol, talk with your healthcare provider for personalized advice.
If you have questions about taking Trintellix for depression, its side effects, or whether you can combine Trintellix and alcohol, talk with your healthcare provider for personalized advice.
Antidepressant discontinuation syndrome: diagnosis, prevention and treatment
04/18/2017
UP TO ZMISTU NUMBER
Withdrawal symptoms may occur after discontinuation of any class of antidepressants. The largest number of publications is devoted to selective serotonin reuptake inhibitors (SSRIs), apparently due to the fact that drugs of this class are most often prescribed for the treatment of depressive disorders. Usually these symptoms are mild and disappear on their own after a while. However, some patients may need to resume pharmacotherapy. This review briefly discusses the main clinical aspects of the antidepressant discontinuation syndrome.
This review briefly discusses the main clinical aspects of the antidepressant discontinuation syndrome.
This condition is also called antidepressant withdrawal syndrome, although this is not entirely correct. The appearance of symptoms after stopping therapy does not mean that the drug is addictive. Antidepressants do not have addictive potential and do not cause addiction. This is an important positive point that should be communicated to patients, since most people will stop taking the prescribed treatment as soon as possible in case of fear of becoming dependent on the drug.
Why is it important to recognize antidepressant withdrawal syndrome?
There are three reasons: discomfort for the patient, diagnostic problem and possible compliance problems. Although withdrawal symptoms are rarely life-threatening, they are always associated with discomfort and some degree of psychosocial maladjustment. Hence the second problem: having experienced a withdrawal syndrome, the patient hardly agrees to any psychopharmacotherapy in the future. And finally, symptoms that occur in connection with the cessation of the action of an antidepressant can be mistaken for an exacerbation of a depressive disorder, another mental disorder, or a physical illness.
And finally, symptoms that occur in connection with the cessation of the action of an antidepressant can be mistaken for an exacerbation of a depressive disorder, another mental disorder, or a physical illness.
For example, consider two typical scenarios. Convinced of achieving remission of major depressive disorder, the doctor hurries to please the patient that the antidepressant can be stopped, but forgets to tell how to do it correctly. The patient takes everything literally and the next day forgets about the medicine. A week later, he develops withdrawal symptoms, and he addresses his complaints to a) the same psychiatrist who forgets to ask how the antidepressant was withdrawn and perceives the symptoms as a relapse of depression; b) to another specialist, for example, a neurologist, to whom he prefers not to report about treatment with a psychiatrist. And the neurologist interprets these non-specific symptoms according to his competence. As a result, unnecessary examinations and possibly even treatment.
In addition, symptoms can be confused with side effects of a newly prescribed drug after discontinuation of an antidepressant, especially when switching between antidepressants with different mechanisms of action, for example, from paroxetine (SSRI) to bupropion (a dopamine and norepinephrine reuptake inhibitor). This can lead to the erroneous conclusion that the patient does not tolerate the new drug well. Symptoms of discontinuation of therapy may also be perceived as failure of therapy, especially irritability and anxiety.
Symptoms of discontinuation of antidepressant therapy can be divided into six categories: sensory symptoms, balance disorders, general somatic, affective, gastrointestinal symptoms, and sleep disorders (Fig.).
At first, information about the listed manifestations was accumulated from reports of clinical cases. Then this problem was studied in prospective double-blind clinical trials in which patients were specifically randomized to the abolition of antidepressant therapy.
In English literature, a mnemonic device is used to memorize the spectrum of antidepressant withdrawal syndrome: the main symptoms are encrypted in the word FINISH.
F - from "flu-like" - flu-like symptoms;
I - insomnia;
N - from "nausea" - nausea;
I - from "imbalance" - imbalance;
S - sensory symptoms;
H - from "hyperarousal" - increased excitability, which reflects affective disorders.
It should be noted that the symptoms presented in the figure are mainly associated with discontinuation of SSRIs and serotonin and norepinephrine reuptake inhibitors. The spectrum of symptoms during withdrawal of monoamine oxidase inhibitors (MAOIs) and tricyclic antidepressants has its own specifics. Thus, in the event of discontinuation of tricyclic antidepressants, sensory symptoms and balance disorders, as a rule, are not observed. With the abolition of MAO inhibitors, symptoms may be more pronounced than after the abolition of SSRIs. Patients may experience a worsening of depressive and anxiety symptoms, an acute impairment of consciousness up to catatonia.
When do withdrawal symptoms appear and how long do they last?
They usually appear within the first week after stopping the antidepressant; according to studies, on average on the second day. Spontaneous resolution occurs at different times - from 1 day to 3 weeks, on average, patients continue to experience symptoms for 10 days.
What causes withdrawal syndrome?
The syndrome occurs when all classes of antidepressants are discontinued. The largest number of reports was recorded for paroxetine. The half-life of the drug from blood plasma is the indicator that correlates more than others with the risk of developing a withdrawal syndrome. In other words, the shorter the residual effect of the drug after the last dose, the higher the likelihood of symptoms.
For example, fluoxetine has a half-life of 7 days, so this SSRI has the lowest risk of withdrawal. Paroxetine has an average half-life of 24 hours, hence the high risk of withdrawal syndrome, especially when the therapeutic dose is abruptly stopped.
Can antidepressant discontinuation syndrome be distinguished from depression relapse?
Common symptoms include dysphoria, decreased appetite, sleep disturbances and fatigue. But there are also distinctive features—symptoms that are rarely seen in depression, such as sensory phenomena (paresthesias) as well as dizziness, headache, and nausea. In addition, in the case of withdrawal syndrome, a rapid (within 1 day) improvement can be observed when the drug is resumed, while recurrent depression does not respond so quickly to therapy.
Who is at risk for developing antidepressant withdrawal syndrome?
Typically, these are patients who begin to feel better after a few weeks of taking an antidepressant and are not sufficiently informed about the need for long-term maintenance therapy. Women who find out they are pregnant during treatment may also abruptly stop taking the antidepressant for safety reasons.
How to stop antidepressants to minimize the risk of withdrawal?
Patients should be explained in an accessible form the features of the action of the prescribed antidepressant, the rules for increasing and gradually reducing the dose, and warn about a possible deterioration in well-being with an abrupt cessation of therapy. But at the same time, the words "withdrawal syndrome", "addiction", "addiction" should be avoided, since they can be perceived negatively and cause early termination of therapy. Sooner or later, that happy moment comes when it becomes clear that antidepressants can be abandoned. However, the withdrawal process, as a rule, takes several weeks, but in some cases even longer, especially if the patient's health worsens at the first steps of dose reduction. When prescribing fluoxetine, it is possible to cancel the drug without a gradual dose reduction, although it has not been specifically studied in studies.
If possible, you should also discuss with the patient's relatives the creation of the most favorable conditions for the period of antidepressant withdrawal. Patients with major depressive disorder, as a rule, do not work and are at home, therefore they are not subjected to external psycho-emotional stress. It is optimal if the patient's close environment tries to create a positive atmosphere and tries to involve a family member in some kind of activity in order to distract from the perception of possible withdrawal symptoms.
How to help patients who complain of feeling worse after stopping antidepressants?
If this does happen, explain to the patient that the symptoms are not life-threatening and usually resolve within a few days. If the patient continues to experience symptoms and they reduce quality of life, it is common practice to restart the therapeutic dose of the antidepressant. In the future, you can again try to stop the drug through a very gradual dose reduction. If this does not help, then it is possible to transfer the patient to fluoxetine-SSRI with the lowest risk of withdrawal syndrome, and then cancel it.
Literature
1. Haddad P.M., AndersonI.M. (2007). Recognizing and managing antidepressant discontinuation symptoms. Advances in Psychiatric treatment, 13(6): 447-457.
2. Warner C.H., Bobo W., Warner C., Reid S., Rachal J. (2006). Antidepressant discontinuation syndrome. American Family Physician, 74(3): 449-456.
3. Renoir T. (2013). Selective serotonin reuptake inhibitor antidepressant treatment discontinuation syndrome: a review of the clinical evidence and the possible mechanisms involved. Frontiers in Pharmacology, 4.
Prepared by Dmitry Molchanov
- Number:
- Thematic issue "Neurology, Psychiatry, Psychotherapy" No. 1 (40), March 2017
03/24/2023 Psychiatry Therapy and family medicine Buspirone in neuropsychiatry: a review of the literature
Buspirone is a new anxiolytic drug with additive mild antidepressant and antipsychotic effects (introduced to the Ukrainian pharmaceutical market by the drug Spitomin® of the company "Egis"). A distinctly single representative of the class of serotonergic anxiolytics-azapirons. ...
03/24/2023 PsychiatryComplex PTSD, analysis of psychotraumatic factors and consequences for military servicemen 9for the population of Ukraine, look at the nutrition of medical and psychological rehabilitation, based on the latest recommendations of international hospitals, the results of monitoring clinical studies. ...
03/01/2023 PsychiatryTherapy and family medicineEscitalopram - a new generation antidepressant: from scientific data to practical research
The truth is good for our skin, that the treasures of life and health are the most precious treasures, while physical and psychological become - however, vagomi warehouses of deep health and well-being. One of the most important problems of protecting health is that suspense in the form of depression - illness, which is characterized by a permanent humiliation, the second interest to be-like activity, which sounds to bring satisfaction, and also nezdatenistyu vikozhuvaty 2 more protracted It is important that depression can be blamed on whether people are independent of the state, economically or equal to enlightenment [1-3]. In our world, according to fakhivtsiv estimates, ≈280 million people suffer from depression, or 3.8% of the population [4]. It is one of the most widespread mental pathologies and the main cause of disability in the whole world [5]. ...
What you should know about antidepressants
Ekaterina Kushnir
treats anxiety disorder
I have generalized anxiety disorder.
For a long time I coped without pills and other help, but one day I got tired of constant anxiety and began to interfere with my normal life. As a result, I turned to a private psychiatrist.
The doctor prescribed an antidepressant from the SSRI group - these are selective serotonin reuptake inhibitors. Such drugs are the first thing prescribed in the treatment of depression and a number of other conditions, including my disease.
The doctor immediately warned me about some peculiarities associated with taking the drug. Some of them I then felt on myself. I think everyone who plans to be treated with antidepressants should know about them.
At the same time, it should be taken into account that most of the negative effects of therapy are temporary and not dangerous, and if they do not go away, one medicine can be replaced with another. Antidepressants help many people with mental disorders and other illnesses get rid of their symptoms and return to a full life, so you definitely should not be afraid of them. The main thing is to take such drugs when they are really needed: as prescribed by a competent doctor and under his control.
See a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
Fact No. 1
Antidepressants may make symptoms worse at firstAntidepressants can increase anxiety in anxiety disorders, as well as cause irritability and agitation - the so-called causeless motor agitation, the inability to sit still. It's not dangerous, but rather unpleasant. This condition is sometimes referred to as initial anxiety, that is, the anxiety of starting therapy. Up to 65% of people face it.
Antidepressant-induced anxiety syndrome - a systematic review in the British Journal of Psychiatry
There is also evidence that some classes of antidepressants, including SSRIs, may increase suicidal ideation in depression in young people aged 18 to 24 years. These data are not very reliable, and in older people, the risk of suicide no longer increases and even decreases.
Without treatment, depression is more likely to lead to suicidal thoughts, and in case of anxiety, you just need to prepare for such an effect, then it will be easier to survive the attacks.
The doctor told me that in the first two or three weeks there may be an increase in anxiety, but I did not take it too seriously.
Everything was fine for the first week. After about seven days, I became nervous and irritable. And then I woke up at night and after a while I felt an incomprehensible fear. My heartbeat increased, my head was spinning, my throat was constricted. Because of this, I felt a real panic - I spent the rest of the night fighting terrible thoughts, in the morning I got up completely broken.
/list/antidepressant-myths/
8 myths about antidepressants
I have never had such panic attacks before medication - my anxiety was background, general. I got scared and wrote to the doctor, who reassured me and said that it was not dangerous and would pass soon.
After that, I already expected these panic attacks, immediately tried to relax, calm down, remember that this was just a temporary effect of the drugs. And they ended faster, and then they completely disappeared.
My letter to a psychiatrist. I was scared: I expected an increase in background anxiety, but not panic attacks. I even thought about giving up the medicineFact No. 2
The effect of antidepressant treatment will not be immediateIncrease the dose of antidepressants gradually to reduce side effects. They usually start with the minimum, and then bring it up to the working one. For example, for SSRIs with the active ingredient "sertraline", the working dose is from 100 mg per day. I started taking such a drug with 25 mg, and then gradually, in several steps, under the supervision of a doctor, raised the dose to 100 mg.
SSRI dosage - NHS
What doses of antidepressants will be optimal - an article in The Lancet
The process of reaching a working dose can take from two weeks to a month or more. It depends on the drug and its tolerance. I turned out to be sensitive to the medicine, it was hard for me to survive every increase in dosage: anxiety increased again, there were other side effects that then stopped. However, this is not the case for everyone, sometimes the process goes faster.
The full therapeutic effect, that is, the disappearance or a strong improvement in the symptoms of the disease, occurs some time after reaching the working dosage. As a rule, this is a week or two, although some positive changes may be earlier. For some people, this process stretches for a longer period: 6-12 weeks. Minimum initial doses of drugs usually do not work.
It is better to prepare right away for the fact that the symptoms of the disease will not disappear in the first weeks of treatment. And remember - this does not always mean that the drug needs to be changed, sometimes you just need to wait or further increase the dosage under the supervision of a doctor.
Fact No. 3
Another way to mitigate the side effects of antidepressants is to prescribe an additional drug along with them: for example, from the group of tranquilizers. Such drugs may have their own side effects, they should not be taken for a long time. Unlike antidepressants, some of them can be addictive. They are usually appointed for a month, but this period may be shorter or longer.
Antidepressants together with benzodiazepines work better for depression - BMJ magazine
My doctor prescribed a rather mild drug for me. However, he did not suit me. At first, it caused increased drowsiness: during the period of increased anxiety, it went away for a while, but then returned - even with half a pill I turned off and could sleep all day. And if I drank at night, I woke up with difficulty in the morning. The psychiatrist prescribed another medicine, but I could not buy it: the drug was not available in any pharmacy nearby.
As a result, I simply endured all the side effects of therapy - they were unpleasant, but tolerable. When discussing with the doctor, she called this option acceptable if the side effects of the second medicine only worsen the situation.
My prescriptions for drugs. I never used one, because there was no such medicine in pharmaciesFact No. 4
Side effects are not always, but they areModern antidepressants, including SSRIs, are mild and have almost no side effects. Older drugs - tricyclic antidepressants and monoamine oxidase inhibitors - cause more side effects. Doctors usually use them when milder first-line drugs don't work or when they can't be prescribed.
Side effects of antidepressants - the National Health Service of Great Britain
Side effects of various antidepressants - Uptodate
Side effects of antidepressants and their impact on the treatment of large depressive disorder - the journal NATURE
STOCE OF READING OF STROTOLINONA 9000 - UPTODATEDTED 9000 effects of antidepressants - advice from the staff of the Mayo Clinic
The choice of an SSRI drug does not guarantee the absence of side effects - many people tolerate treatment easily, but sometimes a change of drug may be necessary.
For the first couple of weeks of taking it, there is a risk that you will not feel well - it's worth thinking about. It may be worth scheduling the start of therapy on vacation.
I work remotely, and it was easier for me: the first pill was taken on Saturday, I slept through the weekend. Then she continued to work, but refused any additional loads: housework, part-time jobs, training and everything else.
It was hard to work: I wanted to sleep, then I began to worry and get distracted. I also had diarrhea, nausea, headaches, tremors, i.e. hand trembling, hot flashes, sweating, palpitations. At night, panic attacks began, in the morning I had difficulty getting up because I was in pain and dizzy.
There are mixed data on how common side effects of antidepressants are. If we summarize them, then the numbers look something like this:
- nausea - about 25% feel it;
- diarrhea - it happens in 15% of people, and 5%, on the contrary, will have constipation;
- about 20% of people experience sweating and feeling hot;
- sexual dysfunction, decreased libido may occur in 80% of cases;
- insomnia - in 11% of cases;
- headache and dizziness - in about 10-11% of cases;
- weight gain - not all drugs give this effect.
Some, on the contrary, can reduce weight. On my medicine, I lost 2 kilograms in the first month, despite the fact that I quit training due to poor health. True, then they returned back.
It can be seen that most side effects occur in less than half of the cases. In addition, in most cases they pass in the first weeks and are not dangerous.
Side effects not listed above are very rare. I was "lucky", and I faced one such - a decrease in visual acuity. Once in the morning I noticed that I see worse without glasses. A little later, I realized that something was wrong with the glasses.
I wrote to the doctor, she replied that this happens, as a rule, is not dangerous and passes, but it is better to visit an ophthalmologist. I went to the ophthalmologist, everything was fine with my eyes, there was nothing terrible, but my vision really worsened - it was not a subjective feeling. On the right eye, it was -0.5 diopters, it became -0.75, and on the left eye it was -1. 5, and it became -3.5.
I was offered to try changing the drug, but I decided to wait. Vision was then restored. I have not yet gone to the doctor to have it measured, but according to subjective feelings, it is at the same level as before: I am comfortable again in my glasses.
Side effects should not be tolerated - if something greatly worries, scares or interferes with life, it is better to tell the doctor right away. The psychiatrist will be able to determine whether the side effect of the drug is dangerous and whether it is worth continuing to take it. There are several antidepressants of the SSRI group, in addition, there are groups of drugs with a slightly different mechanism of action. As a rule, doctors manage to find a medicine that gives a good effect without side effects.
If there is no danger, the doctor can adjust the dose or increase it more gradually - this often helps to cope with unpleasant effects.
I wrote to the doctor again when my visual acuity decreased Fact No. 5
Antidepressants are not drugs that you can stop drinking as soon as you get better. They are taken for a long time: usually from several months, less often several years.
Anxiety Therapy - UpToDate
For example, for generalized anxiety disorder, the duration of treatment is at least a year. Moreover, the date is not counted from the very beginning, but from the moment when a lasting effect appeared from the pills. In fact, they will have to be drunk for about 1.5 years - it depends on how long it takes to reach the working dosage of the medicine.
The cost of a package of the most famous antidepressant Zoloft is about 700 R, enough for about a month. That is, a course of therapy will cost about 10,000 R - maybe more or less, depending on which drug is selected.
Psychotherapy review - UpToDate
Another drug of the same group already costs more than 2000 R per pack. Source: rigla.ru The cost of an appointment with a good psychiatrist in Moscow is 3000-5000 R. At first, you will need to visit him about once every 1-1.5 months, then less often.
You can apply to the psycho-neurological dispensary at the place of residence under compulsory medical insurance - it's free. At the same time, they will not put you on psychiatric registration: it was canceled in 1993. People with disorders that do not threaten their lives or those around them are on consultative and diagnostic care. If you stop going to the doctor, he will not find out what happened: a person seeks help at will.
Psychotherapy, usually cognitive-behavioral, is also commonly prescribed to enhance and sustain the effect of antidepressants. In many cases, it improves the effectiveness of drugs, including depression and generalized anxiety disorder. An appointment with a psychotherapist in Moscow costs an average of 5000 R. For treatment, you will need about 10 sessions or more.
/psychotherapy/
How psychotherapy works
Fact No. 6
Antidepressants do not develop dependence. However, if you abruptly stop drinking them, there will be a withdrawal syndrome. This is felt as electric current discharges while moving or turning the head, headaches, dizziness, insomnia. Many people experience symptoms similar to the flu or an intestinal virus: low fever, diarrhea, general malaise, chills. Often there is anxiety, there are intrusive images.
Withdrawal symptoms after taking serotonin reuptake inhibitors - Journal of Clinical Psychiatry
How difficult it is to stop taking antidepressants - American Psychological Association
Stopping antidepressants in adults - UpToDate
treatment, they should be canceled only under the supervision of a doctor.
Antidepressant withdrawal occurs as gradually as the start of treatment. The dosage is slowly reduced, usually at this time again a cover-up drug is prescribed to alleviate side effects. As a rule, this is the same medicine that was at the beginning of the intake.
Withdrawal is usually harmless and resolves within the first weeks of stopping the drug. Sometimes even within a few days - it still depends on which medicine was prescribed. If severely disturbing symptoms appear during the withdrawal period, you should consult a doctor.
Fact No. 7
If you need to change the drug, everything will start overIt is far from always possible to immediately find the right antidepressant - sometimes the side effects do not go away and you need to take a new one.
Changing antidepressants in adults - UpToDate
Serotonin syndrome - MSD
Most often, it is started again with a small dosage, this delays the process of obtaining the effect of treatment. The new drug may also have side effects - the same or different. We will have to wait again until they pass.
You won't be able to change the drug on your own, since all antidepressants are sold only by prescription - and that's good. Switching from one drug to another can be dangerous if you do not know the characteristics of different groups of drugs.
For example, taking SSRIs is possible only some time after the withdrawal of antidepressants from the group of monoamine oxidase inhibitors - due to the risk of developing serotonin syndrome. This is a potentially fatal condition, accompanied by a change in mental state, high fever, increased muscle tone and other symptoms.
If the drug is changed correctly, there will be no dangerous negative effects, so consultation with a doctor is required.
/psychotherapy-search/
How to choose a psychotherapist
Fact No. 8
Among antidepressants there are original drugs and generics Preparations may be original or generic. Originals are medicines first released by some pharmaceutical company that have passed all clinical trials and checks. Generics are drugs with the same active ingredient from another pharmaceutical company, that is, copied from the original drug.
Theoretically, the effect of generic drugs should not differ from the effect of original drugs. However, this is possible, since generics may contain other additional substances or the manufacturer may use other raw materials.
Due to my anxiety, I did not read anything in detail about specific drugs before I bought my first antidepressant in a pharmacy, so as not to be scared and not think about taking it. I also didn’t think to ask the doctor about this question.
/list/covid-depression/
Psychoneurological complications after covid: memory problems and depression
As a result, I first bought a generic because it was in stock. Then it turned out that, after all, according to the experience of my psychiatrist, the original drug often gives fewer side effects and is better tolerated. As a result, I changed the generic to the original drug - and, indeed, the side effects softened.
In my subjective opinion, which is supported by some data, in the case of antidepressants and other psychotropic drugs, you should always choose the original medicine. Moreover, the cost of originals and generics is not always very different.
Originals and generics of some SSRIs
| Active ingredient | Original | Original price | Generics | Cost of generics |
|---|---|---|---|---|
| Sertraline | Zoloft | About 700 R, 100 mg tablets | Serenata, Sirlift | 500-600 R 100 mg tablets |
| Escitalopram | Cipralex | 3000 R 10 mg tablets | "Selektra", "Elycea" | 500-1300 R 10 mg tablets |
| Fluoxetine | Prozac | About 350 R, 20 mg tablets | Profluzak, Fluoxetine | 100-200 R, 20 mg tablets |
CERTRIN
Original
Zoloft
The cost of the original
about 700 r, tablets 100 mg
generies
Serenata
Cost of
9000 500-600 r. , tablets 100 mgEscitalopram
Original
Cipralex
Original cost
3000 r, tablets 10 mg
Generiki
“Chektra”, “Elice”
The cost of generics
500-1300 r, tablets 10 mg
Fluxetin
“Prozak”
9000 original
About 350 R, tablets 20 mg
Generics
Profluzak, Fluoxetine
Cost of generics
100—200 R, tablets 20 mg
one remained unclaimed Fact No. 9
Drinking alcohol while taking antidepressants may exacerbate unpleasant side effects. Also, alcohol is a depressant, that is, it has the opposite effect, and its intake can adversely affect the results of treatment.
Why you shouldn't mix antidepressants and alcohol - Mayo Clinic
Alcohol is strictly forbidden to drink with some groups of antidepressants, for example, tricyclic antidepressants and monoamine oxidase inhibitors: combination with the latter, for example, can lead to an uncontrolled increase in pressure. MAO inhibitors in general require a special diet - it is unlikely that a doctor will prescribe such drugs as the first antidepressants, but if necessary, he will issue a list of what is allowed and prohibited.
With other antidepressants, moderate use may not be dangerous and even pass without consequences, but doctors still recommend abstaining so as not to increase side effects and improve treatment outcome.
The main thing is not to temporarily stop taking the drug in order to drink. This can lead to the development of a withdrawal syndrome.
/trevoga/
How I Treated Generalized Anxiety Disorder under CHI
Fact No. 10
Antidepressants are incompatible with certain drugs and have contraindicationsIt is important to tell your doctor what medications you are taking and what chronic illnesses you have. For example, SSRIs may not be suitable for epilepsy and bleeding disorders, and tricyclic antidepressants are usually not prescribed for those who have recently had a heart attack, suffer from glaucoma, or porphyria.
Antidepressant Warnings - NHS
Drug Compatibility Test - Drugs.com
It is also important to be careful if you are about to take any over-the-counter medicine. For example, ibuprofen, which people often take on their own to relieve pain and reduce fever. It should not be taken with SSRIs as it increases the risk of gastrointestinal side effects.