Does weed increase serotonin
Serotonin Syndrome: Too Much of a Good Thing
Did you know that certain drug interactions can increase your chances of developing a potentially-lethal set of symptoms known as serotonin syndrome? Knowing which medications, over-the-counter remedies, supplements, and drugs of abuse put you at risk may just save your life.
First Things First—What is Serotonin?Serotonin is a neurotransmitter, which means it helps relay messages between different regions of the brain. It is closely associated with many different areas of physical and mental health, including:
- Mood
- Memory
- Sleep
- Sexual Desire/Function
- Learning
- Appetite
- Social Behavior
- Temperature Regulation
- Cardiovascular Function
- Muscle Performance
- Endocrine System
- Bowel Function
- Clotting
Up to 90% of the body’s serotonin is found in the gastrointestinal tract. Interestingly, although serotonin is manufactured in the both GI tract and the brain, it cannot pass through the blood-brain barrier. This means that the serotonin used by the brain must be produced there. This also means that while serotonin blood levels can be measured, there is no corresponding test to measure the amount of serotonin in a person’s brain. If there is any kind of imbalance, it is best detected through other signs and symptoms.
“Serotonin imbalance has long been linked to a variety of psychiatric disorders, including depression, bipolar disorder and schizophrenia…” ~ Dr. Tom Maniatis, Ph.D., Columbia University Serotonin is known as the “happy molecule” because of the role it plays in regulating positive moods and promoting active social engagement. Having the proper levels of serotonin is a key aspect of good overall brain health. But the opposite is also true – a serotonin deficiency can be linked to any or all of these serious mental illnesses, including:
- Depression—Of special relevance, women produce 52% less serotonin than men, and hormone levels fluctuate during menstruation.
 This helps explain why women are twice as likely as men to be diagnosed with depression.
This helps explain why women are twice as likely as men to be diagnosed with depression. - Anxiety—Both low AND high serotonin levels contribute to anxiety.
- Intermittent Explosive Disorder – Affecting the amygdala and characterized by extreme and uncontrollable outbursts of violence.
- Bipolar Disorder
- Schizophrenia
- Obsessive-Compulsive Disorder
- Autism—Up to 30% of autistic patients have low levels of serotonin.
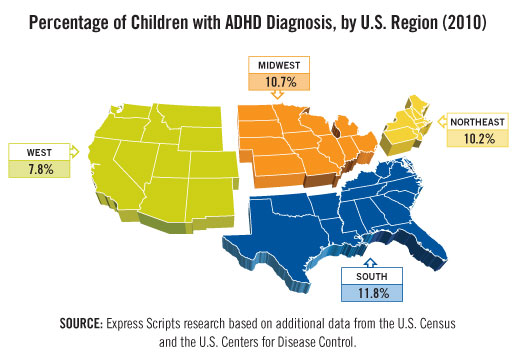
- ADHD—The children of mothers with serotonin deficiencies are up to 2.5 times more likely to be diagnosed with a hyperactivity disorder.
- Suicidal Ideation–reduced serotonin can “result in impaired inhibition and a greater propensity to act on powerful feelings such as suicidal or aggressive feelings”.
There are several reasons why someone might have low levels of serotonin in their brain.
- Alcohol
- Anger
- Aspartame
- Caffeine
- Diabetes or insulin resistance
- Diet Pills
- Digestion problems
- Ecstasy
- Genetics
- Hormone imbalances (adrenal, estrogen, thyroid)
- Hypoglycemia
- Inflammation
- Infections
- Lack of exposure to sunlight
- Malnutrition
- Medication
- Nutritional deficiencies
- Poor exercise
- Problems converting tryptophan to Serotonin
- Smoking
- Stress
“The higher the serotonin levels someone has, the less likely they will become addicted. ” ~ Dr. Sarah Bradbury, Ph.D., Victoria University of Wellington Serotonin levels play a complicated cyclical role in the development of an addictive disorder. There is a strong connection between mental illness and addiction. According to a study conducted among psychiatric patients:
” ~ Dr. Sarah Bradbury, Ph.D., Victoria University of Wellington Serotonin levels play a complicated cyclical role in the development of an addictive disorder. There is a strong connection between mental illness and addiction. According to a study conducted among psychiatric patients:
- 44% have a co-occurring Alcohol Use Disorder (AUD)
- 64% have a co-occurring Drug Use Disorder
And when you consider some of the specific psychiatric conditions linked to low serotonin levels, the connection between that deficiency and subsequent substance abuse becomes more apparent:
- AUD Patients—64% have depression
- Anxiety patients are twice as likely to be addicted/dependent on drugs.
- Cannabis use is a factor in 80% of schizophrenia cases.
- 56% of people with bipolar disorder abuse alcohol and/or drugs.
- More than 1 in 4 people with OCD meet the lifetime criteria for an addictive disorder.

- Adult alcoholics are up to 10 times more likely to have ADHD than non-drinkers.
There are three possible explanations for the comorbidity of low serotonin, mental illness, and addiction. FIRST, there may be a genetic link that predisposes someone to all three conditions—each would then play a part in the development of and the worsening of the others. SECOND, decreased serotonin activity can result in an impaired ability to plan, delay gratification, or control impulses. This means that a person with a serotonin is less biologically able to resist drug cravings. THIRD, when a person who is already genetically vulnerable to addiction also suffers from co-occurring serotonin deficiency and mental illness, they often attempt to self-medicate to alleviate the uncomfortable emotional symptoms of those conditions.
Serotonin Syndrome – Another Name for Neurotransmitter Toxicity And while using drugs or alcohol may make them feel better temporarily over the short-term, regular substance use progresses to substance abuse and addiction far too quickly and easily. Even worse, self-medicating when there is a serotonin imbalance can result in the rapidly-presenting and potentially-deadly symptoms of serotonin syndrome. Serotonin syndrome is a reaction to certain prescription medications, supplements, or illicit drugs that results in toxic levels of serotonin within the brain. In the case of legitimately-prescribed medications, the reaction can be triggered even when they are taken as directed. There is no laboratory test that can confirm serotonin syndrome. The condition is diagnosed based upon the patient’s history of drug/medication use, physical examination, and any presenting symptoms. This method is up to 97% accurate.
Even worse, self-medicating when there is a serotonin imbalance can result in the rapidly-presenting and potentially-deadly symptoms of serotonin syndrome. Serotonin syndrome is a reaction to certain prescription medications, supplements, or illicit drugs that results in toxic levels of serotonin within the brain. In the case of legitimately-prescribed medications, the reaction can be triggered even when they are taken as directed. There is no laboratory test that can confirm serotonin syndrome. The condition is diagnosed based upon the patient’s history of drug/medication use, physical examination, and any presenting symptoms. This method is up to 97% accurate.
Again, serotonin syndrome is a drug reaction, occurring after a new drug or a new dosage level is taken. Symptoms typically begin rapidly—6 to 24 hours after consumption.
- Agitation
- Confusion
- Restlessness, often to the point of feeling the need to be in constant motion
- Extreme aggressiveness
- Dilated pupils
- Jerky movement of the eyes
- Extremely sensitive reflexes
- Muscle spasms
- Uncontrollable twitches
- Tremors
- Full-body seizures
- Accelerated heartbeat
- High blood pressure
- Abnormally dry mouth
- Shivering
- Sweating
- High fever – over 104°
- Increased bowel sounds
- Diarrhea
- DEATH
The first step in treating serotonin syndrome is to discontinue use of the causal drug. If the triggering substance is discontinued, mild cases of serotonin poisoning will go away on its own within 1 to 3 days. However, in more serious cases of serotonin syndrome, hospitalization may be necessary. The next step is to administer a serotonin-inhibiting medication, such as:
If the triggering substance is discontinued, mild cases of serotonin poisoning will go away on its own within 1 to 3 days. However, in more serious cases of serotonin syndrome, hospitalization may be necessary. The next step is to administer a serotonin-inhibiting medication, such as:
- Alosetron
- Carbinoxamine
- Chlorpromazine
- Cilansetron
- Clozapine
- Cyproheptadine
- Dolasetron
- Fenclonine
- Feverfew
- Granisetron
- Hydroxyzine
- Ketanserin
- Metergoline
- Methdilazine
- Methysergide
- Mianserin
- Mitrazapine
- Nefazodone
- Ondansetron
- Oxatomide
- Oxetorone
- Palonosetron
- Pizotifen
- Promethazine
- Propranolol
- Quetiapine
- Reserpine
- Risperidone
- Ritanserin
- Spiperone
- Trazodone
- Tropisetron
The priority during treatment for serotonin is to regulate those symptoms that are life-threatening – hyperthermia, tachycardia, autonomic dysfunction, and seizures. Decontamination with activated charcoal may be necessary, as well as the administration of tranquilizers, sedatives, antihypertensive drugs, or even “flight-or-flight” hormones such as epinephrine or norepinephrine. Importantly, physical restraints are not recommended for serotonin poisoning patients who are severely agitated or delirious. Straining against those restraints forces muscle contractions that cause a dangerous buildup of lactic acid and increased body temperature. Patients using drugs with a long half-life or extended duration of action can experience symptoms up to two weeks, and muscle pain and weakness may persist for months.
Decontamination with activated charcoal may be necessary, as well as the administration of tranquilizers, sedatives, antihypertensive drugs, or even “flight-or-flight” hormones such as epinephrine or norepinephrine. Importantly, physical restraints are not recommended for serotonin poisoning patients who are severely agitated or delirious. Straining against those restraints forces muscle contractions that cause a dangerous buildup of lactic acid and increased body temperature. Patients using drugs with a long half-life or extended duration of action can experience symptoms up to two weeks, and muscle pain and weakness may persist for months.
Serotonin reuptake inhibitors (SSRIs) are a class of antidepressants that increase the serotonin levels by limiting reabsorption. Although primarily prescribed for major depression, SSRIs are also given for anxiety, OCD, PTSD, panic disorder, anorexia, bulimia, and chronic pain. They are the most-widely prescribed type of antidepressant.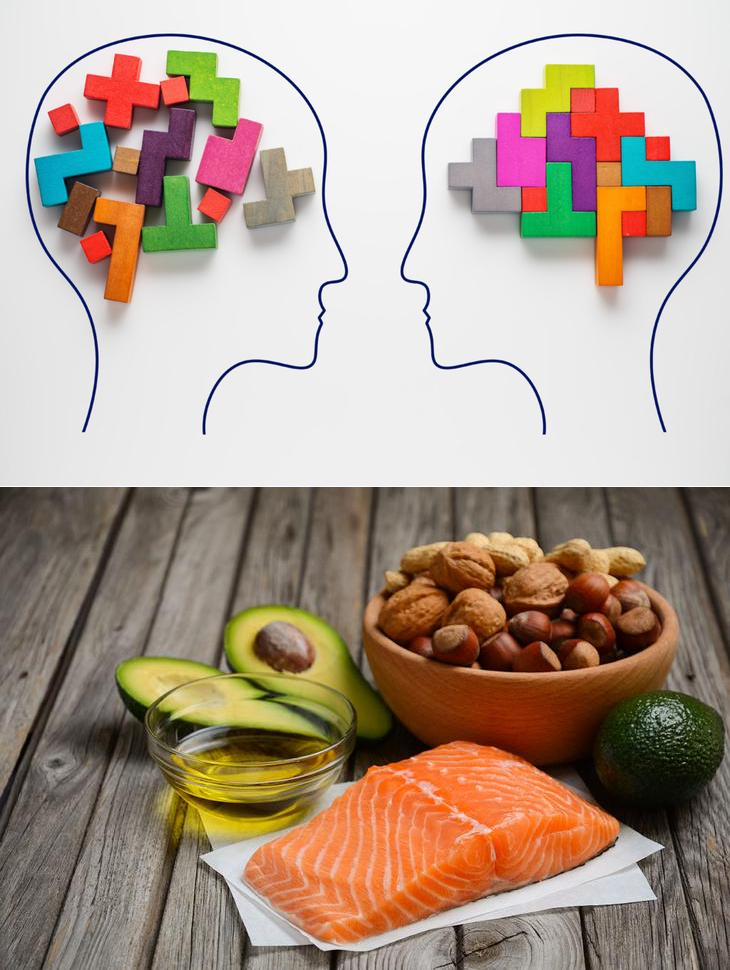 Serotonin syndrome occurs in approximately 15% of SSRI overdoses. Examples of SSRI medications include:
Serotonin syndrome occurs in approximately 15% of SSRI overdoses. Examples of SSRI medications include:
- Citalopram (Celexa)
- Dapoxetine (Priligy)
- Escitalopram (Lexapro)
- Fluoxetine (Prozac)
- Fluvoxamine (Luvox)
- Paroxetine (Paxil)
- Sertraline (Zoloft)
Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs), are a class of antidepressants that work by blocking the reabsorption of the neurotransmitters serotonin and norepinephrine, thereby increasing their levels. SNRIs can also be prescribed for anxiety, OCD, ADHD, fibromyalgia syndrome, chronic pain, and for the relief of severe menopausal symptoms. Abrupt discontinuation of SNRIs is not recommended because it can trigger withdrawal symptoms. Examples of SNRIs include:
- Atomoxetine (Strattera)
- Desvenlafaxine (Desfax, Ellefore, Pristiq)
- Duloxetine (Cymbalta)
- Levomilnacipran (Fetzima)
- Milnacipran (Dalcipran, Ixel, Savella, Toledomin)
- Tramadol (Ultram)
- Venlafaxine (Effexor) – the most-commonly-used SNRI
Some OTC pain relievers – aspirin, ibuprofen, and naproxen – interfere with the efficiency of these medications, and even worse, increase the risk of gastrointestinal bleeds. There are also a number of substances that, when used with SSRIs and SNRIs, may trigger serotonin syndrome. What is particularly concerning about this list is how many different conditions they treat:
There are also a number of substances that, when used with SSRIs and SNRIs, may trigger serotonin syndrome. What is particularly concerning about this list is how many different conditions they treat:
- Bupropion (Wellbutrin, Zyban) – anti-smoking medication
- Buspirone – prescribed for anti-anxiety
- Carbamazepine (Tegretol) – prescribed for migraines
- Cyclobenzaprine (Flexeril) – a muscle relaxant
- Dextromethorphan – an ingredient in many OTC cough suppressants, and an extremely-popular drug of abuse
- Droperidol (Inapsine) – for anti-nausea
- Ginseng – herbal supplement taken for memory, diabetes, fatigue, and menopause symptoms.
- Linezolid – prescribed for MRSA and other antibiotic-resistant infections
- Lithium – prescribed for bipolar disorder or major depression when other antidepressants don’t work
- MDMA (Ecstasy) –the illicit drug of choice the rave/party culture, abused for its stimulant and euphoriant effects
- Metoclopramide (Reglan) – for anti-nausea
- Mirtazapine – prescribed for both anxiety and depression
- Monoamine Oxidase Inhibitors (MAOIs) – often considered the “last line of defense” against depression, MAOIs are typically prescribed when other medications are ineffective
- Methylene Blue
- Moclobemide
- Phenelzine
- Selegiline
- Tranylcypromine
- Nutmeg – herbal supplement taken for brain health, blood pressure, and circulation
- Ondansetron (Zofran)—for anti-nausea
- Pethidine/Meperidine (Demerol) – a synthetic opioid pain medication
- Ritonavir (Norvir) – anti-retroviral medication given to treat HIV/AIDS
- Serotonin Norepinephrine Reuptake Inhibitors (SNRIs) – (more in the next section)
- St.
 John’s Wort – A medicinal herb popularly taken as an OTC supplement for depression
John’s Wort – A medicinal herb popularly taken as an OTC supplement for depression - Tramadol – a prescription opioid pain medication
- Tricyclic Antidepressants (TCAs) – an older generation of antidepressant/mood disorder medications
- Triptans (Amerge, Axert, Imitrex) – prescribed for migraines or cluster headaches
- Valproic Acid (Depakene) – given for migraines
- Yohimbe – a dietary supplement sold as an aphrodisiac
People with certain pre-existing conditions should avoid SSRIs and SNRIs:
- High blood pressure
- Chronic alcoholism
- Liver disease
- Coronary artery disease
- Anorexia
- Bulimia
- Glaucoma
These medications should NEVER be taken within 24 hours of another antidepressant, because it may result in a serotonin overdose.
Opioids and Serotonin Syndrome “Patients and practitioners should be aware that opioid analgesic use of longer than 30 days imposes risk of new-onset depression. ” ~Dr. Jeffrey Scherrer, Ph.D., Associate Professor for Family and Community Medicine, St. Louis University People who suffer pain lasting longer than 6 months have a more than quadrupled risk of depression than those not in chronic pain, according to the Journal of American Medicine. And, among opioid abusers who have switched to cheaper, easier-to-get heroin, the likelihood becomes even greater. Approximately 48% of heroin addicts also experience co-occurring depression. But when a person uses heroin or takes opioid painkillers like Vicodin, OxyContin, or codeine in combination with certain serotonergic medications, the risk of serotonin poisoning increases dramatically. There are two prevailing theories as to why the interaction between opioids and antidepressants increases the likelihood of serotonin syndrome. The first theory is that even alone, opioids act as inhibitors that prevent serotonin reabsorption. When combined with other inhibitors, the effect is magnified.
” ~Dr. Jeffrey Scherrer, Ph.D., Associate Professor for Family and Community Medicine, St. Louis University People who suffer pain lasting longer than 6 months have a more than quadrupled risk of depression than those not in chronic pain, according to the Journal of American Medicine. And, among opioid abusers who have switched to cheaper, easier-to-get heroin, the likelihood becomes even greater. Approximately 48% of heroin addicts also experience co-occurring depression. But when a person uses heroin or takes opioid painkillers like Vicodin, OxyContin, or codeine in combination with certain serotonergic medications, the risk of serotonin poisoning increases dramatically. There are two prevailing theories as to why the interaction between opioids and antidepressants increases the likelihood of serotonin syndrome. The first theory is that even alone, opioids act as inhibitors that prevent serotonin reabsorption. When combined with other inhibitors, the effect is magnified. Secondly, opioids impact the production of GABA, another neurotransmitter, and as a result, access serotonin is released. In addition, while some opioids – specifically, buprenorphine, hydromorphone, oxycodone, and oxymorphone – are not reuptake inhibitors, they still increase serotonin levels by some as-yet-undiscovered mechanism. Among all opioids, fentanyl has been linked to serotonin syndrome most often, followed by oxycodone and methadone. In 2016, the potentially-dangerous interaction between opioids and serotonergic substances caused the FDA to require drug manufacturers to make changes to the warning labels on opioid medications.
Secondly, opioids impact the production of GABA, another neurotransmitter, and as a result, access serotonin is released. In addition, while some opioids – specifically, buprenorphine, hydromorphone, oxycodone, and oxymorphone – are not reuptake inhibitors, they still increase serotonin levels by some as-yet-undiscovered mechanism. Among all opioids, fentanyl has been linked to serotonin syndrome most often, followed by oxycodone and methadone. In 2016, the potentially-dangerous interaction between opioids and serotonergic substances caused the FDA to require drug manufacturers to make changes to the warning labels on opioid medications.
ADHD medications treat hyperactivity by balancing out serotonin and dopamine levels within the brain. However, when taken in combination with SSRIs, SNRIs, or other serotonergic drugs, those levels can become toxic. Prescription ADHD drugs include:
- Adderall
- Ritalin
- Vyvanse
- Concerta
The abuse of illegal drugs can also have a significant impact on the serotonin levels within the brain. Besides the aforementioned heroin, other drugs that can contribute to serotonin syndrome include:
Besides the aforementioned heroin, other drugs that can contribute to serotonin syndrome include:
- Cocaine –Fatalities have been reported
- Ecstasy – Can cause multi-organ failure
- LSD – This potent hallucinogen disrupts the serotonin system
- Methamphetamines – Especially at high doses
- Marijuana—At low doses, marijuana increases serotonin levels. Paradoxically, at high doses, it causes a major serotonin depletion, making it more likely the user will need antidepressants. It is also important to note that when marijuana is smoked it is difficult to accurately measure the dosage.
- Alcohol—Drinking alcohol temporarily raises serotonin levels—raising the odds of serotonin syndrome—but chronic alcoholism causes a deficiency that can dramatically worsen depression.
The first takeaway is that serotonin syndrome is a serious, potentially life-threatening condition that should not be ignored. When symptoms manifest, serotonin syndrome can rapidly turn into an emergency, so medical help should be sought immediately. Serotonin syndrome is almost completely avoidable, and communication is the best tool you have at your disposal. ALWAYS be completely open and honest with your doctor about any medications, supplements, OTC remedies, and drugs you are taking – legal or not. Your doctor is not there to judge you, and omitting anything could jeopardize your health. At the same time, depression is also not to be taken lightly, especially if it co-occurs with a substance abuse disorder. To find just the right balance of medication, therapy, and lifestyle changes that will help you successfully manage both conditions, you need the help of an experienced staff of professional specialists.
When symptoms manifest, serotonin syndrome can rapidly turn into an emergency, so medical help should be sought immediately. Serotonin syndrome is almost completely avoidable, and communication is the best tool you have at your disposal. ALWAYS be completely open and honest with your doctor about any medications, supplements, OTC remedies, and drugs you are taking – legal or not. Your doctor is not there to judge you, and omitting anything could jeopardize your health. At the same time, depression is also not to be taken lightly, especially if it co-occurs with a substance abuse disorder. To find just the right balance of medication, therapy, and lifestyle changes that will help you successfully manage both conditions, you need the help of an experienced staff of professional specialists.
Give it a Rating!
Full Infographic:
Tagged drug interactions that may be hurting you, symptoms of serotonin syndrome, what causes serotonin deficiency, what is serotonin syndrome
Does Marijuana Affect Serotonin? | Jointly
Did you know that cannabis affects serotonin levels? New research suggests that marijuana use may cause some changes in serotonin functioning.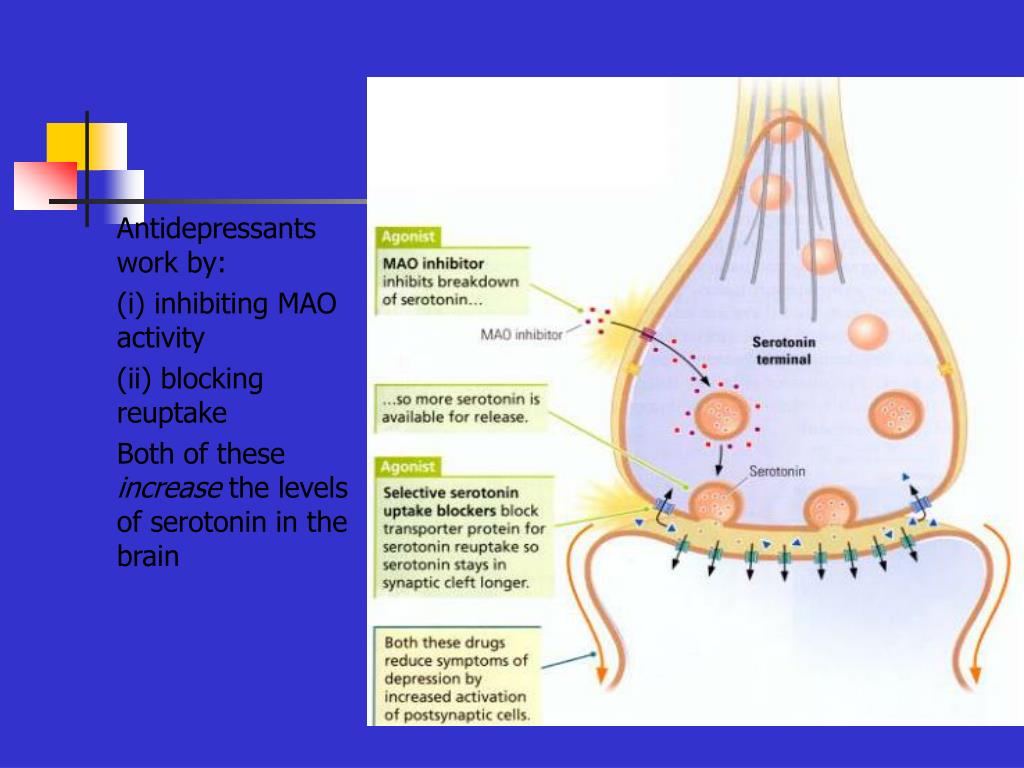 Read on to learn more about the link between marijuana and serotonin, and how this relationship could impact your mood.
Read on to learn more about the link between marijuana and serotonin, and how this relationship could impact your mood.
What is serotonin?
Serotonin, or 5-Hydroxytryptamine (5-HT), is a monoamine neurotransmitter with a complex and multi-faceted function. Serotonin is involved in mood, learning, memory, as well as physiological processes like vasoconstriction or vomiting.
Over 90% of all serotonin in the body is located within the gastrointestinal tract, where it is used to regulate intestinal movements.
However, serotonin is much more well-known for its role in the brain. Serotonin is often called the "happiness hormone" due to its role in modulating impact mood, appetite, and sleep. Several classes of antidepressants such as selective serotonin reuptake inhibitors (SSRIs) target the serotonergic system.
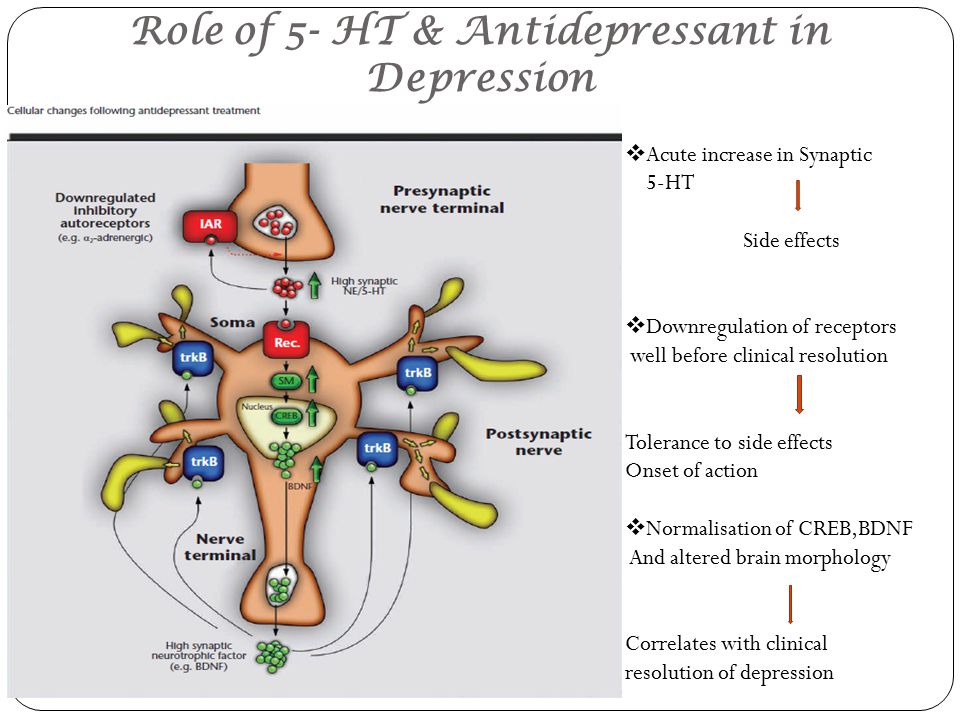
Serotonin levels usually are low in people who suffer from depression. Several supporting studies have been published, most notably a 2015 study by Philip J. Cowen and Michael Browning published in the Journal of World Psychiatry, which associated serotonin with depression. Recent research indicates that other factors may be involved in depression, such as brain-derived neurotrophic factor (BDNF).
Cowen and Michael Browning published in the Journal of World Psychiatry, which associated serotonin with depression. Recent research indicates that other factors may be involved in depression, such as brain-derived neurotrophic factor (BDNF).
Does cannabis increase serotonin?
Does cannabis increase serotonin? There isn’t a simple answer to this question. The endocannabinoid system and the serotonin system have a complex relationship. For example, both systems are involved in appetite, sleep, and emotional processes. Additionally, cannabis contains many different chemicals including cannabinoids, terpenes, and flavonoids—many of which may exert biological effects.
However, animal studies indicate that a low dose of a CB1 receptor agonists like THC acutely increases serotonin, but a high dose produces the opposite effect: decreasing serotonin neurotransmission.
Many people want to know, “does THC release serotonin?”
Does THC release serotonin?THC has been shown to inhibit serotonin re-uptake—which is how SSRIs work.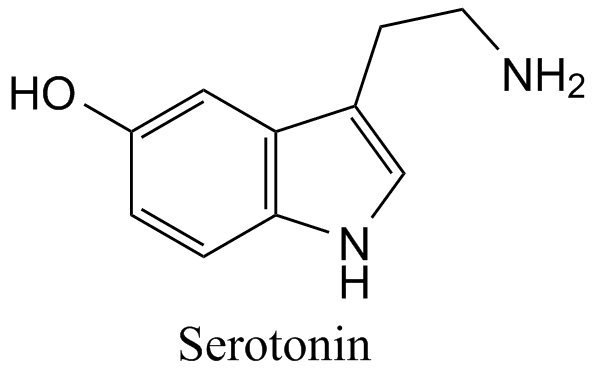 In short, THC doesn’t “release serotonin,” but low dose THC may increase the level of serotonin neurotransmission. However, long-term (chronic) cannabis use produces a different effect on the serotonin system.
In short, THC doesn’t “release serotonin,” but low dose THC may increase the level of serotonin neurotransmission. However, long-term (chronic) cannabis use produces a different effect on the serotonin system.
For example, long-term cannabinoid administration alters 5-HT receptor signaling by upregulating 5-HT2A gene activity and downregulating 5-HT1A gene activity. These results are noteworthy, as a similar finding has been observed in depression. These two receptors appear to “elicit opposing behavior” with 5-HT1A activation inducing anxiolysis (decreased anxiety) and 5-HT2A activation inducing anxiety.
Because cannabis does affect serotonin, cannabis overdoses can mimic the symptoms of serotonin syndrome.
Serotonin syndrome symptoms: what are they?Serotonin syndrome is a potentially fatal adverse drug reaction caused by excessive serotonergic activity in the central nervous system and periphery.
This condition usually occurs when you star taking a new drug or increase your dose of antidepressants. Symptoms can include:
Symptoms can include:
● High blood pressure
● Agitation
● Accelerated heartbeat
● Abnormally dry mouth
● Confusion
● Extreme aggressiveness
● Jerky movement of the eyes
● Dilated pupils
● Restlessness, characterized by a sense that one needs to be constantly moving
● Extremely sensitive reflexes
● Muscle spasms
● Uncontrollable twitches
● Tremors
● Full-body seizures
● Sweating
● Shivering
● High fever – over 104°
● Increased bowel sounds
● Diarrhea
● Death
Can marijuana cause serotonin syndrome?
Does marijuana increase serotonin? At low doses, marijuana increases serotonin levels, leading to feelings of pleasure and well-being. On the other hand, higher doses of THC have the opposite effect. But if cannabis can increase serotonin, can you get serotonin syndrome from weed?
While there are anecdotal reports of cannabis-induced serotonin syndrome, there are no peer-reviewed case studies linking serotonin syndrome to cannabis.
However, acute cannabis toxicity (a weed overdose) can resemble serotonin syndrome. A
So just how does weed deplete serotonin? When marijuana intake is high, THC inhibits serotonin reuptake, which may lead to depression as potent cannabinoid receptor agonists activate the brain's serotonin receptors.
As more states legalize marijuana, the potential for high-potency marijuana abuse could lead to an increase in the number of emergency department (ED) visits. For example, a 2020 case study describes a pair of teenage patients who presented to the emergency department with dilated pupils, stiffness in both legs, and convulsions in both feet following inhalation of a cannabis concentrate.
Serotonin syndrome was initially considered, but the patients were both eventually diagnosed with cannabis toxicity. For that reason, it's helpful to remember that both serotonin syndrome and cannabis toxicity should be considered in cases where serotonin syndrome is suspected.
Can CBD cause serotonin syndrome?
In 2014, an animal study showed that CBD interacts with serotonin and may have mild antidepressant and sedative properties. If you are only taking CBD, CBD can’t cause serotonin syndrome.
If you are only taking CBD, CBD can’t cause serotonin syndrome.
However, CBD interacts with drug-metabolizing enzymes and has been shown to interact with various antidepressants. CBD combined with antidepressants could potentially cause serotonin syndrome. If you are taking an SSRI, talk to your doctor before adding cannabis or CBD into your routine.
Get Started on Your Cannabis Wellness Journey
Have you started your cannabis wellness journey? Jointly is a new cannabis wellness app that helps you discover purposeful cannabis consumption so you can achieve your wellness goals with cannabis and CBD. On the Jointly app, you can find new cannabis products, rate products based on how well they helped you achieve your goals, and track and optimize 15 factors that can impact your cannabis experience. These 15 factors include your dose, the environment in which you consume cannabis, who you are with when you ingest, how hydrated you are, the quality of your diet, how much sleep you got last night, and more. Download the Jointly app on the App Store or the Google Play Store to get started on your cannabis wellness journey.
Download the Jointly app on the App Store or the Google Play Store to get started on your cannabis wellness journey.
Anti-Depressant Products or Foods to Improve Mood
Ours mood and emotions depend not only on external circumstances and health, but also from the function of the endocrine glands - the hypothalamus and the epiphysis. The hormones that produced by them, regulate our sleep, the state of the immune system, emotional mood and the degree of protection of the body in stressful situations.
Special replaced by neurotransmitters, chemicals in the brain transmitting information from one neuron to another. They are synthesized by amino acids and for their formation, a constant supply of certain nutrients is necessary. substances. The most well-known neurotransmitters that affect neuropsychic state of a person, are serotonin, norepinephrine, dopamine (dopamine), acetylcholine and GABA (gamma-aminobutyric acid).
Which substances regulate our mood?
From of these substances, dopamine most significantly affects our mood (dopamine) and serotonin.
Dopamine causes a feeling of pleasure when we do something that we like (for example, eat, listening to music, playing sports). Thanks to him, we can show activity, be motivated and feel satisfied. By the way, drugs such as cocaine, nicotine, opiates, heroin and alcohol increase dopamine levels. Therefore, many researchers believe that the tendency of some people to smoke, use drugs and alcohol, gambling and overeating are costed by a dopamine deficiency in the brain brain. Decreased dopamine levels lead to impaired memory and concentration attention, decrease in vital energy (the so-called "vital activity"), a person ceases to enjoy life and becomes subject to bad habits and obsessive states. a lack of dopamine in the corresponding areas of the brain leads to a loss of initiative (to "sitting and daydreaming"), a more serious deficit - the complete inability to make an active action.
However must be remembered that excess of this substance contributes to the behavior associated with the "search for pleasure" (hedonic behaviour).
Serotonin is synthesized in our body from the amino acid tryptophan, which comes from food. It is involved in the regulation of mood, suppresses feelings of anxiety, affects libido and appetite. With its deficiency, social disorders can be observed, phobias, sleep and memory disorders, as well as disorders of the cardiovascular and endocrine functions. Low serotonin levels can lead to depression mood, anxiety, decreased energy, migraines, sleep disorders, obsessive or manic states, feelings of tension and irritation, there is a craving for sweets or, conversely, loss of appetite, memory impairment and concentration, angry and aggressive behavior, slow muscle movements and slow speech. By the way, serotonin deficiency contributes to alcoholism (alcohol temporarily raises serotonin levels, but lowers it in the long run).
How is the bad autumn serotonin deficient mood?
The role of the serotonin system of the brain in such pathological conditions, like seasonal depression and premenstrual syndrome.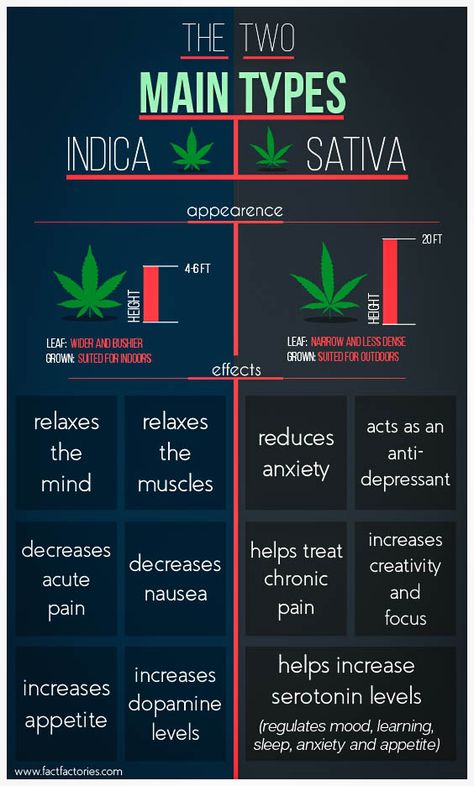 In both cases, the symptoms diseases include depression, anxiety, often some degree of weakening behavior control. With seasonal disorders, these phenomena occur in autumn-winter period, accompanied by lengthening of sleep and depressed mood. PMS occurs in the last days of the menstrual cycle, and the change in hormonal background during this period also affects the level of serotonin in the brain.
In both cases, the symptoms diseases include depression, anxiety, often some degree of weakening behavior control. With seasonal disorders, these phenomena occur in autumn-winter period, accompanied by lengthening of sleep and depressed mood. PMS occurs in the last days of the menstrual cycle, and the change in hormonal background during this period also affects the level of serotonin in the brain.
If the amount of serotonin going off scale?..
Must note that an excessive amount of serotonin causes sedation, a decrease in sexual arousal, a sense of well-being, bliss. However, if the level serotonin becomes too high, this can lead to the development serotonin syndrome.
Serotonin syndrome: excess worse than a disadvantage?
Extreme high levels of serotonin can be toxic, however reaching these levels food is impossible. Such a state can only occur with the abuse of antidepressants. Serotonin syndrome causes severe trembling, profuse sweating, insomnia, nausea, dental trembling, chills, shivering from cold, aggressiveness, self-confidence, agitation and increased body temperature.
How to use nutrition to increase the level substances that regulate mood?
Increasing serotonin levels naturally comes from a diet rich in tryptophan, vitamins, zinc and poor "empty" carbohydrates. And of course this the misconception that serotonin in its finished form is already contained in products. Serotonin is produced in the brain from the essential amino acid tryptophan.
Research in Oxford University's Department of Psychiatry show that when patients with depression in remission are deprived of tryptophan, their depression returns. Women who once had depression were divided into two groups and fed some food containing tryptophan, others food not containing it. AT at the end of the experiment, ten of the fourteen women who did not receive tryptophan, were in a mild depression, while none of women who received tryptophan did not have mood problems.
Tryptophan, which is used in the synthesis serotonin, found in meat, eggs, cheese, bananas, milk, yogurt. However without enough vitamins B 3 , B 6 , omega-3 fatty tryptophan acids can be processed according to a different chemical formula and turn into a substance that does not affect the mood. Therefore, it is important to use products-sources of these irreplaceable substances.
However without enough vitamins B 3 , B 6 , omega-3 fatty tryptophan acids can be processed according to a different chemical formula and turn into a substance that does not affect the mood. Therefore, it is important to use products-sources of these irreplaceable substances.
For increasing the amount of dopamine in the body, which affects mood and motivation, the content of the preceding amino acids tyrosine should be increased in the diet and phenylalanine. These amino acids are converted into dopamine with the help of vitamin co-factors such as vitamin B 6 and folic acid. big the amount of dopamine precursors found in beets, soy, meat, almonds, cereals and eggs.
Folic acid and iron are also important for participation in the production of substances that regulate mood. Study at King's College Hospital in London found that 33% of patients with psychiatric disorders, including depression, were deficient in folate acids and iron.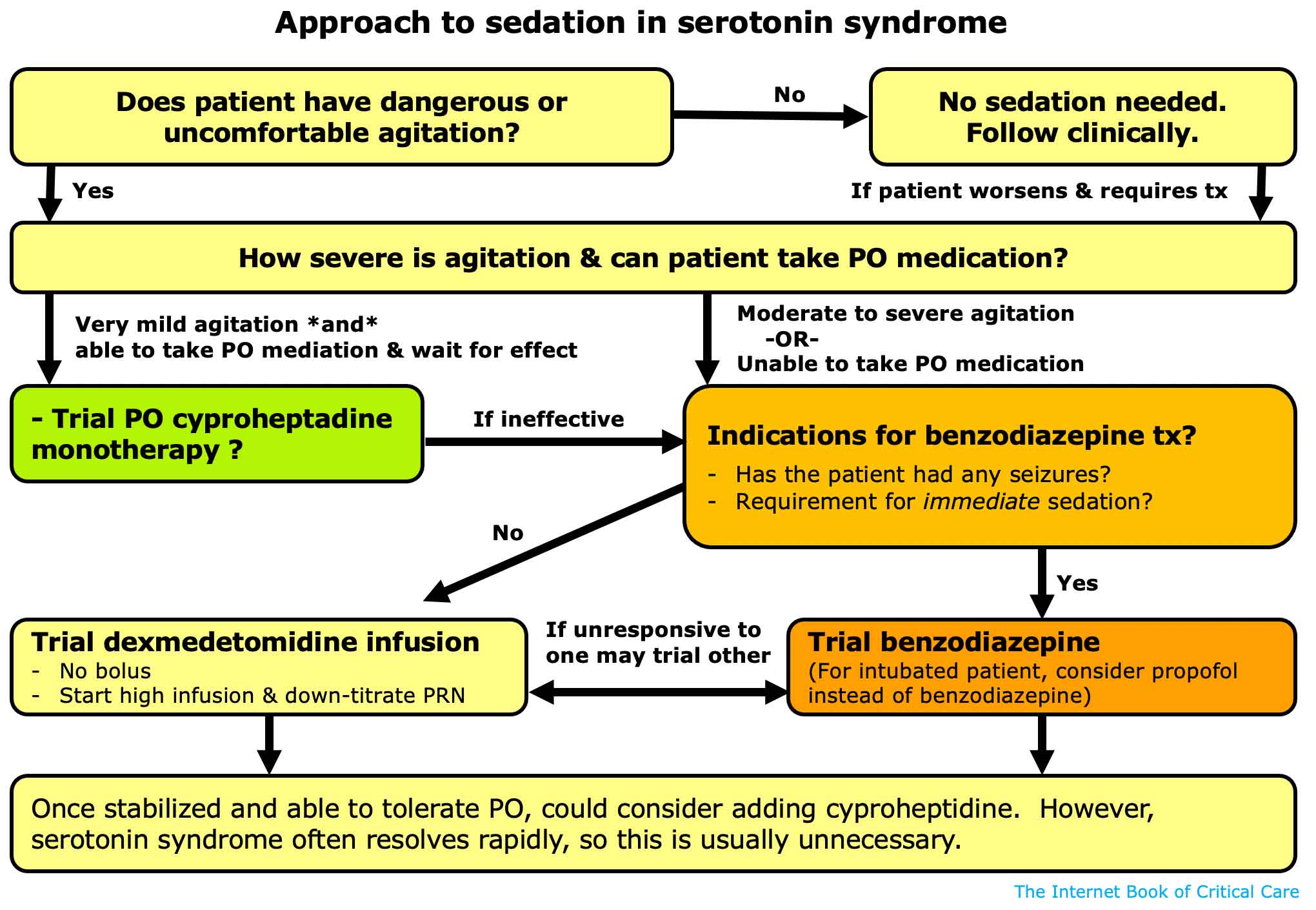
What other than food affects serotonin content in the body?
On the amount of serotonin in our body affects the level of female sex hormones (estrogen). In this regard, some women in the premenstrual period, and also in menopause there are problems with mood. In addition, one must remember that stress reduces the amount of serotonin as the body uses it reserves for peace of mind.
Physical exercise and good lighting help stimulate serotonin synthesis and increase its quantity. Antidepressants also help the brain restore serotonin stores.
Mood enhancing products
It should be noted that the recommended antidepressant products do not contain these neurotransmitters. Both serotonin and dopamine are produced only the human body when eating food rich in already known to you precursor substances (carbohydrates, tryptophan, tyrosine, etc.), from which they are synthesized.
Fish
Oily fish (herring, sardines, mackerel, salmon, cod, salmon) are rich in omega-3 fatty acids acids that regulate serotonin.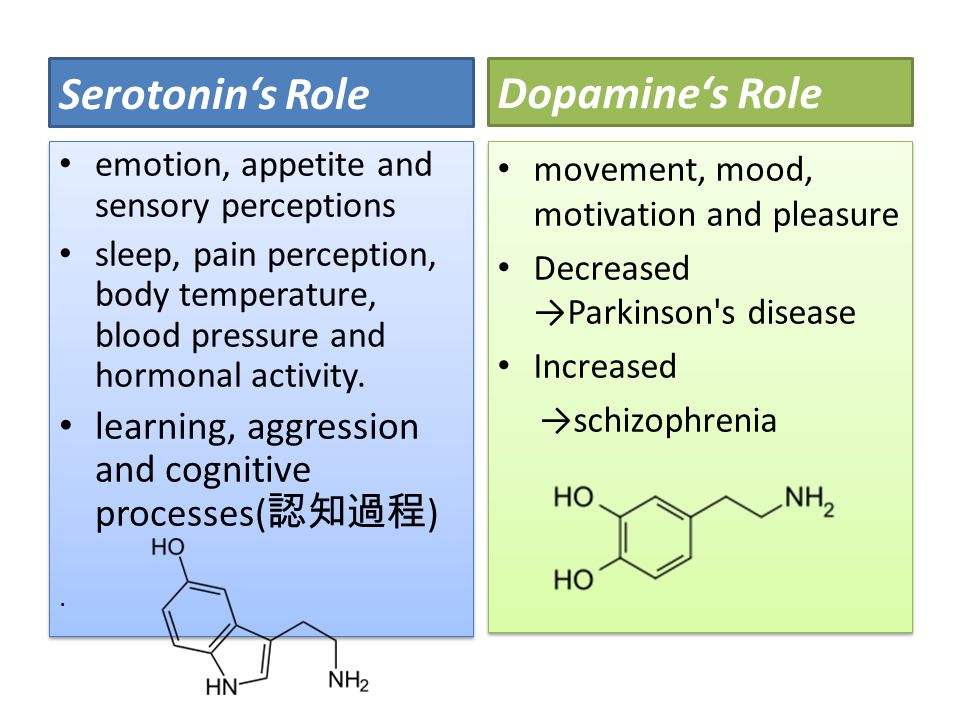 To foods rich in fatty acids Omega-3s, in addition to fish, include nuts, seeds, avocados, unrefined vegetable oil. Including oily fish twice a week amount of at least 200 g (per week), you will provide your body with necessary amount of omega-3 fatty acids. Held in Kyoto (Japan) studies have shown that students who took three months of daily from 1.5 to 1.8 g of fish oil (as part of oily fish), not showed an increase in social aggressiveness during the exams, characterized by significant mental stress.
To foods rich in fatty acids Omega-3s, in addition to fish, include nuts, seeds, avocados, unrefined vegetable oil. Including oily fish twice a week amount of at least 200 g (per week), you will provide your body with necessary amount of omega-3 fatty acids. Held in Kyoto (Japan) studies have shown that students who took three months of daily from 1.5 to 1.8 g of fish oil (as part of oily fish), not showed an increase in social aggressiveness during the exams, characterized by significant mental stress.
Chicken, turkey, lean pork and beef, egg white, lean dairy products
listed foods are leading sources of the amino acids tyrosine and tryptophan and vitamins of group B, necessary for the synthesis of "pleasure hormones". AT In particular, meat contains pantothenic acid, which is involved in production of the amino acid phenylalanine, which is a precursor to dopamine a hormone that improves mood and prevents the development of depression.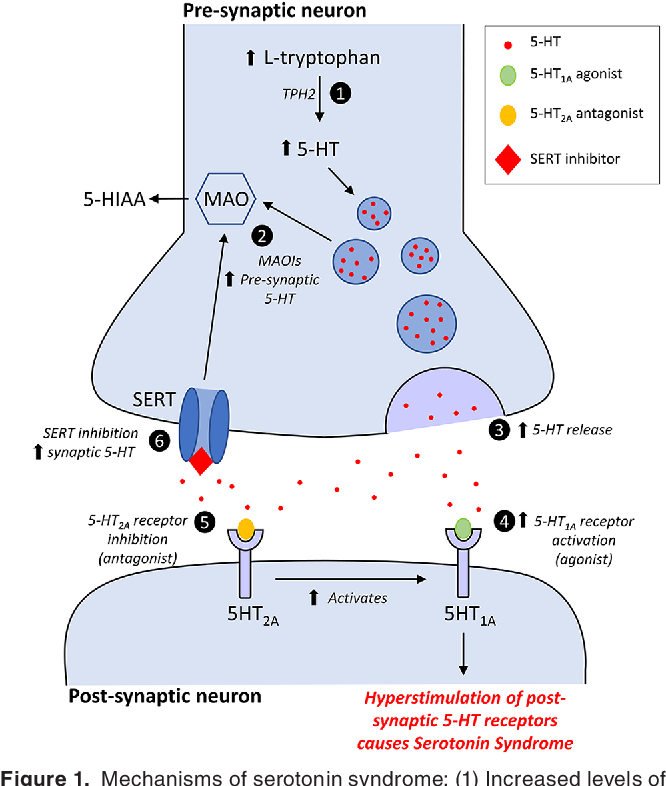
Cabbage Marine
Marine cabbage is rich in B vitamins that regulate the work of the adrenal glands and, accordingly, the production of the hormone adrenaline, the lack of which is capable of cause chronic fatigue. Also a leading source organic iodine and other trace elements that normalize the work thyroid gland, on the activity of which our mood depends.
Marine it is better to buy cabbage not pickled, but dried, and then by yourself at home cook or grind in a coffee grinder and use as a condiment and as a salt substitute.
Fruit, especially bananas
B bananas, in addition to tryptophan, contain vitamin B 6 , which, as already was said to be necessary for the synthesis of serotonin - the main regulator moods. In addition, bananas are rich in the alkaloid harman, the basis which is the "drug of happiness" - mescaline, which can cause a feeling of euphoria. To maintain strength, it is recommended to eat 1 banana, mashed and poured with boiling water (in the form of mashed potatoes).
Gorky chocolate
Cocoa beans, from which chocolate is obtained, contain phenylethylamine, which contributes to the production of endorphins in the body - substances that increase mood. Besides, cocoa beans contain magnesium, which can relieve stress.
Oat and buckwheat dishes
Same as meat, oatmeal and buckwheat contain a precursor of serotonin - the amino acid tryptophan. Also, these products contain complex carbohydrates, which, slowly absorbed, normalize blood sugar levels. Consequently, regulate insulin levels. And insulin, in turn, performs the function transporting tryptophan to the brain, where it is already processed into serotonin.
Vegetables (leafy greens, tomatoes, chili peppers, beets, garlic, broccoli, celery and cauliflower)
All of these are sources of essential micronutrients (vitamins A, C, E, B 1 , B 2 , B 9 , PP, minerals: potassium, calcium, iron, sodium, phosphorus, magnesium, copper, manganese, iodine, chromium, boron), which are necessary for formation of major neurotransmitters.
Tomatoes also contain the compound lycopene, which is a powerful antioxidant that regulates metabolic processes in the brain, which helps deal with depression. In addition, tomatoes contain other "mood enhancers" such as folic acid and magnesium, and also iron and vitamin B 6 which are important for the brain to produce mood regulating neurotransmitters such as serotonin, dopamine and norepinephrine.
In beets contains another active substance - betaine. Vitamin-like compound which affects the hormonal status of a woman, thereby contributing to normalization of mood in premenstrual and menopausal periods.
Thanks capsaicin of chili peppers, dishes acquire not only spiciness, but are also healing for our mood. The fact is that in response to the use of this irritating substance, our brain produces endorphins - natural compounds, which have a calming effect.
What As for garlic, it contains a large amount of chromium, which affects on the regulation of the formation of serotonin - the "happy" chemical.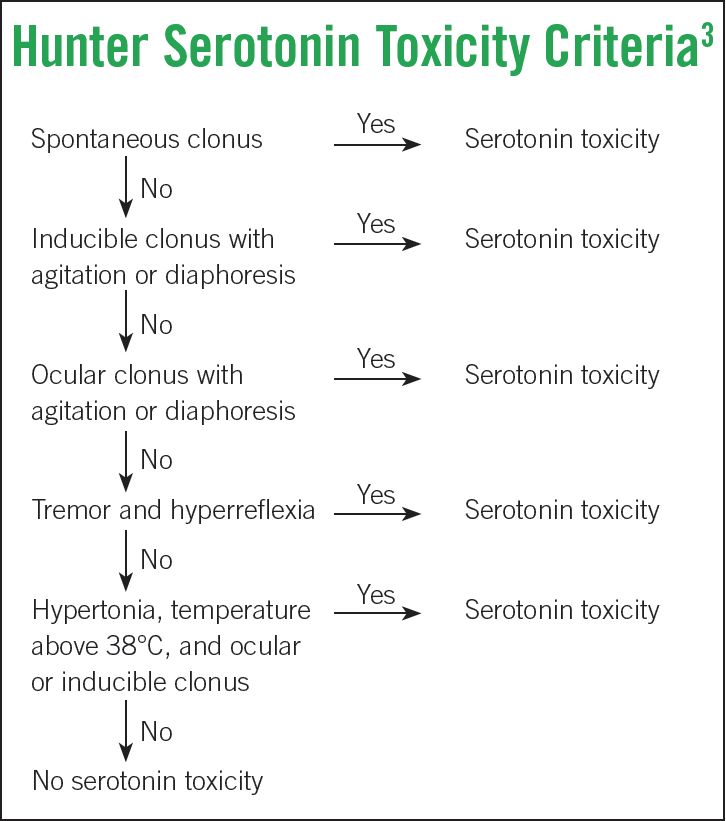
Honey
B unlike useless refined sugar, honey contains B vitamins, folic acid, iron, manganese, chromium plus about 180 biologically active compounds such as quercetin and caffeic acid, which increase the production "mood hormones" and energy in the brain.
Menu anti-stress diet
Breakfast
2 tsp. sprouted and washed grains with sprouts 1.5–3 mm long, oat muesli with dried apricots, raisins and nuts, a cup of cocoa, 2 pieces toasted rye bread, banana.
Second breakfast
Orange, 2-3 cubes of dark chocolate and a cup of green tea, rye or oatmeal bread.
Lunch
Vegetable soup, side dish of brown rice or buckwheat, a piece of chicken or fish, salad tomatoes and sweet peppers with vegetable oil and chili peppers, rye bread, green tea or mineral water.
Snack
Yoghurt and chocolate chip cookies, raisins, dates, nuts.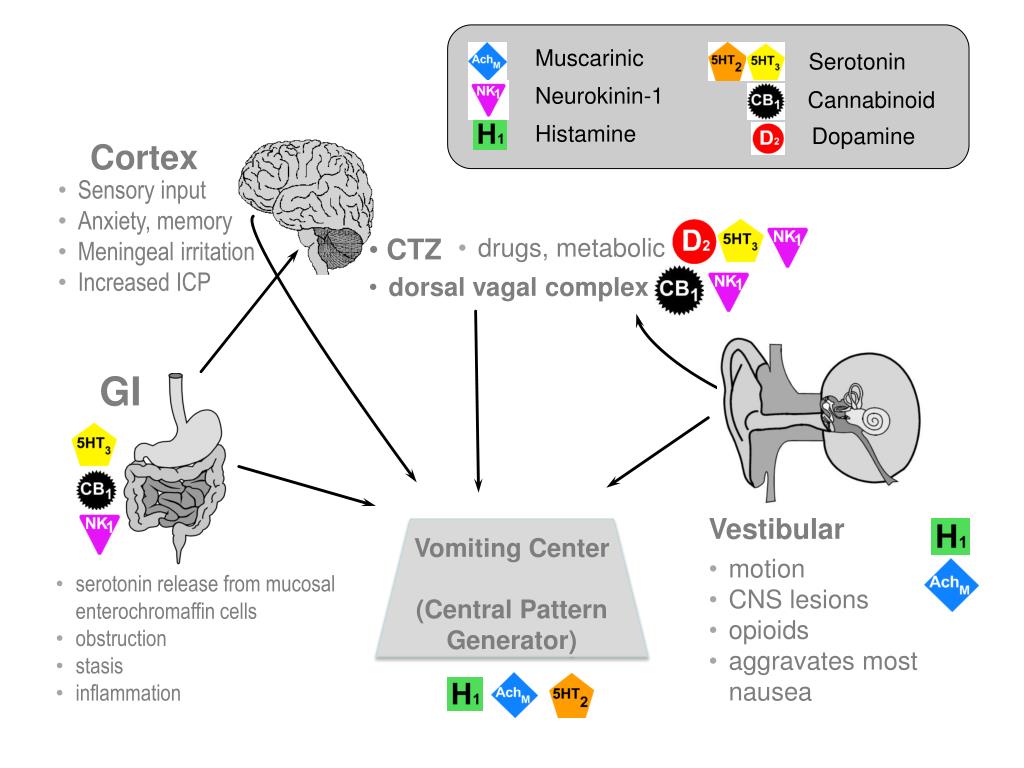
Dinner
Vegetable stew (stewed asparagus, peppers, kohlrabi, celery root and greens, tomatoes), cheese or cheese. Juice or biokefir.
Before bedtime
Hot milk or a cup of cocoa with milk and honey or an infusion of a phytocollection-regulator mood + brewer's yeast tablet.
Mood-regulating herbal teas medicinal herbs that have a sedative effect will help reduce emotional stress during stress, the root and leaves of valerian, oregano, lemon balm, St. John's wort and hops.
At stress, depression, apathy, it is useful to brew tea from St. John's wort, rose hips, raspberry or strawberry leaves, oregano and mint. Better to use a thermos: a handful rose hips, 1 tbsp. l. herbs pour a liter of boiling water and leave for at least 2 hours. You can not filter, but add boiling water during the day. Prepare a new one in the morning infusion. This soothing tea can be drunk for 5-7 days.
Also An infusion of St. John's wort and valerian root will be effective: 1 tbsp. l. St. John's wort, 1 tsp. valerian root. Prepare and receive in the same way as previous collection.
Try for a week, brew instead of regular or green tea such soothing herbal tea. You will feel your improvement emotional state.
Infusion from hop cones and mint acts similarly to synthetic tranquilizers, but has no side effects and is safe for health. The infusion is prepared as follows: 1 tsp hop cones and mint steamed with a glass of boiling water. insist 30 minutes, strain and drink in 2 doses, adding a slice of lemon and a teaspoon of honey.
For in order to normalize sleep and reduce the psychological stress of the body you can prepare sachets from the collection of herbs: hop cones, lavender, oregano, lemon balm. With such a collection, it is necessary to fill a small pillow sewn from cotton fabric or linen and put under the pillow at the head.
Except In addition, aromatic essential oils will help improve mood: lavender soothe, ylang-ylang will relax and reduce tension, cedar will help to cope with anxiety and fear. Other aroma oils will help during the day: orange oil tones, reduces mental fatigue, spruce and pine oil tones and stimulates physical and mental performance.
Other aroma oils will help during the day: orange oil tones, reduces mental fatigue, spruce and pine oil tones and stimulates physical and mental performance.
Natalya Batsukova,
candidate of Medical Sciences, Associate Professor, Head of the Department of General Hygiene of the Belarusian State Medical University
← Bioavailability of nutrients, or How to get the most out of food |
How to speed up the synthesis of serotonin and improve mood?
Serotonin is a neurotransmitter that can affect mood. Foods containing the essential amino acid known as tryptophan are known to promote serotonin synthesis. Such products that help to naturally increase the level of biologically active substances include salmon, eggs, spinach, etc.
Serotonin is present in the brain, blood, intestines and connective tissue. He takes part in the processes of contraction of blood vessels, transmission of nerve impulses and maintaining the normal state of the brain.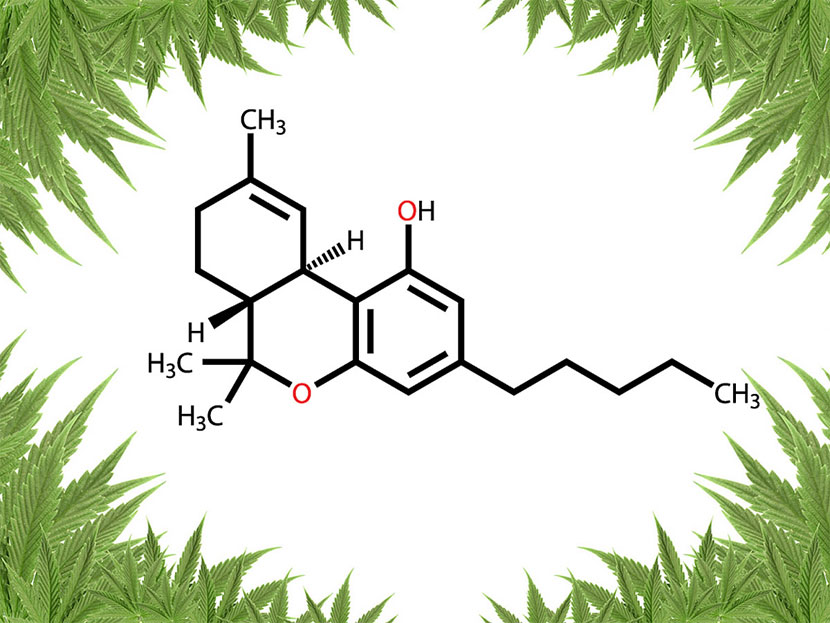 Serotonin is essential for overall health and a sense of well-being, and the very name of this neurotransmitter is often associated with a good mood. Currently, the biological mechanisms of serotonin in the brain remain not fully understood, however, in the course of previous studies, scientists have concluded that low levels of serotonin are associated with mood disorders, and it may play a role in the development of depression. A decrease in the level of serotonin in the brain can cause memory impairment and bad mood. In addition, it has a more negative impact on the health of people who have previously been diagnosed with depression.
Serotonin is essential for overall health and a sense of well-being, and the very name of this neurotransmitter is often associated with a good mood. Currently, the biological mechanisms of serotonin in the brain remain not fully understood, however, in the course of previous studies, scientists have concluded that low levels of serotonin are associated with mood disorders, and it may play a role in the development of depression. A decrease in the level of serotonin in the brain can cause memory impairment and bad mood. In addition, it has a more negative impact on the health of people who have previously been diagnosed with depression.
Serotonin and tryptophan
Tryptophan is an amino acid, without which the synthesis of serotonin is impossible. In addition, it plays an important role in maintaining the normal state of the brain and healthy sleep. Tryptophan is not synthesized in the human body; it must be obtained from food. Fortunately, this amino acid, unlike serotonin, is found in various foods.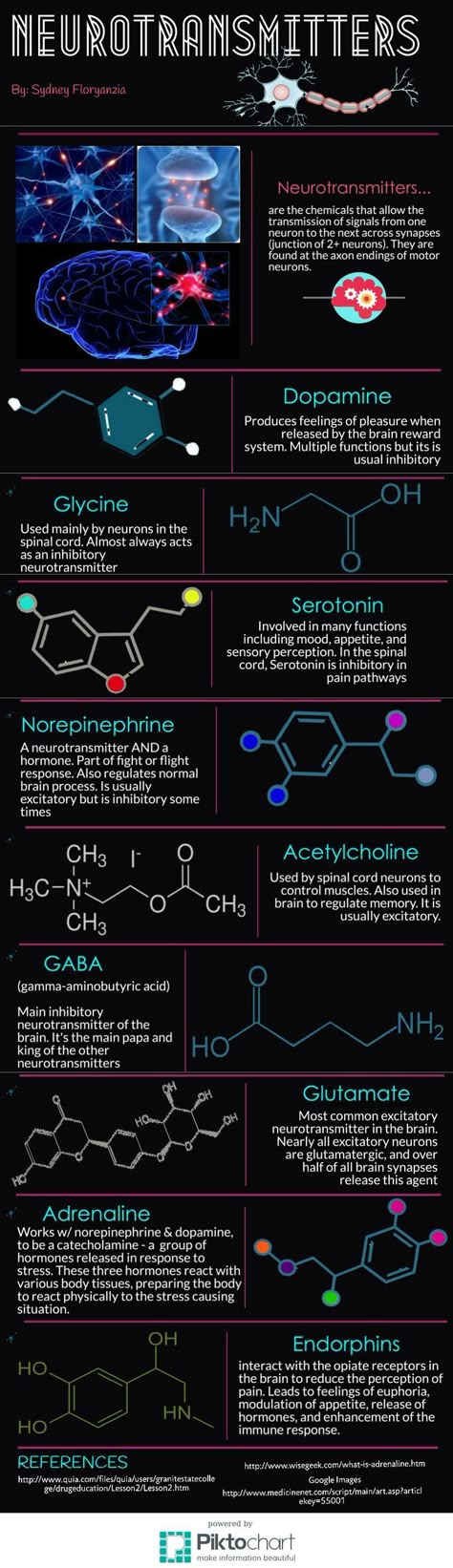 Including these foods in your diet has a positive effect on a person’s energy, mood and sleep quality, and is also an important step in maintaining mental and physical health.
Including these foods in your diet has a positive effect on a person’s energy, mood and sleep quality, and is also an important step in maintaining mental and physical health.
Foods that increase serotonin production
Tryptophan, which is necessary for the synthesis of serotonin, is usually found in foods containing protein. While meat is often the main source of protein for many people, there are many vegetarian and vegan sources of amino acids.
Foods rich in tryptophan include:
1. Salmon. This oily fish is also a source of omega-3 fatty acids and vitamin D, which are important for maintaining health, in particular for improving the condition of the musculoskeletal system, skin and eyes. Eating two servings of fish a week can provide enough tryptophan.
2. Bird. Poultry meat (chicken, turkey and goose) is usually high in protein along with low fat content.
3. Eggs. Some ways of cooking eggs are healthier than others. When frying eggs, a lot of fat is often used, which reduces their usefulness.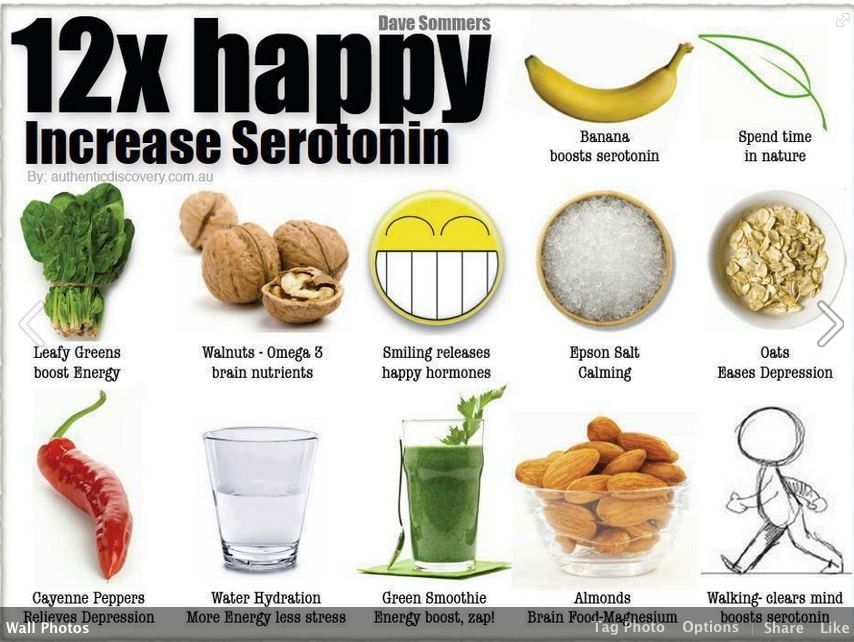 An omelet with salad or boiled eggs can be a good option, since they do not add any fat during cooking.
An omelet with salad or boiled eggs can be a good option, since they do not add any fat during cooking.
4. Spinach. Dark green leafy vegetables like spinach are a good source of tryptophan. Spinach is also a good source of iron, which is essential for red blood cell synthesis. An iron deficiency in the diet can lead to anemia, fatigue, or difficulty breathing.
5. Grains and seeds. These foods do not contain as much tryptophan as fatty fish, poultry, or eggs. However, they are a good source of amino acids and protein for vegetarians and vegans. Some easy ways to eat more grains include adding them to salads, porridges, and yogurts, and opting for whole grain breads.
6. Milk. It is also a good source of calcium, which is essential for maintaining healthy bones and teeth.
7. Soy products. Foods containing soy, such as tofu, soy milk, or soy sauce, are sources of tryptophan. They can be a good option for vegetarians and vegans.
8. Nuts. Nuts are a good source of protein, unsaturated fatty acids and fiber.