Does lunesta cause weight gain
Managing weight gain from psychiatric medications
While psychiatric medications can be essential for improving mental health and well-being, they often come with unwanted side effects. One particular side effect of many psychiatric medications is weight gain. In this post we will explore how these medications cause weight gain, and what you can do to lessen the impact of this unwanted effect of many psychiatric medications.
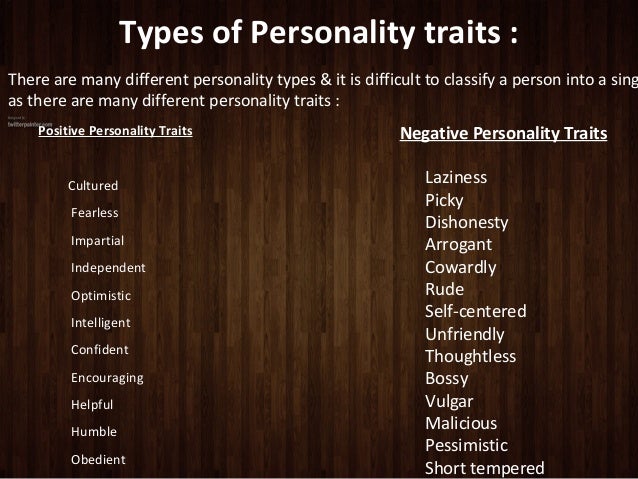
What are the different types of psychiatric medications?
There are five main types of psychiatric prescription medications: antidepressants, antipsychotics, anxiolytics (also known as anti-anxiety medications, which can include medications for sleep), mood stabilizers, and stimulants. Stimulants are not likely to cause weight gain. In fact, many of them reduce appetite and can cause weight loss as a side effect. These medications will not be discussed in this post.
Antidepressants can be divided into separate classes:
- SSRIs, or selective serotonin reuptake inhibitors, increase serotonin levels in the brain.
- SNRIs, or serotonin-norepinephrine reuptake inhibitors, increase both serotonin and norepinephrine in the brain.
- TCAs, or tricyclic antidepressants, increase serotonin, norepinephrine, and dopamine in the brain.
- MAOIs, or monoamine oxidase inhibitors, increase serotonin, dopamine, and norepinephrine in the brain.
Why do antidepressants cause weight changes?
All of these medications increase serotonin levels in the brain. Serotonin regulates mood and affects appetite, yet this can have varying results depending on length of treatment. Short-term use reduces impulsivity and increases satiety, which can reduce food intake and cause weight loss. However, long-term use (longer than a year) can cause downregulation of serotonin receptors, which subsequently causes cravings for carbohydrate-rich foods such as bread, pasta, and sweets that ultimately may lead to weight gain. The antidepressants with the highest risk of causing weight gain are amitriptyline, citalopram, mirtazapine, nortriptyline, trimipramine, paroxetine, and phenelzine.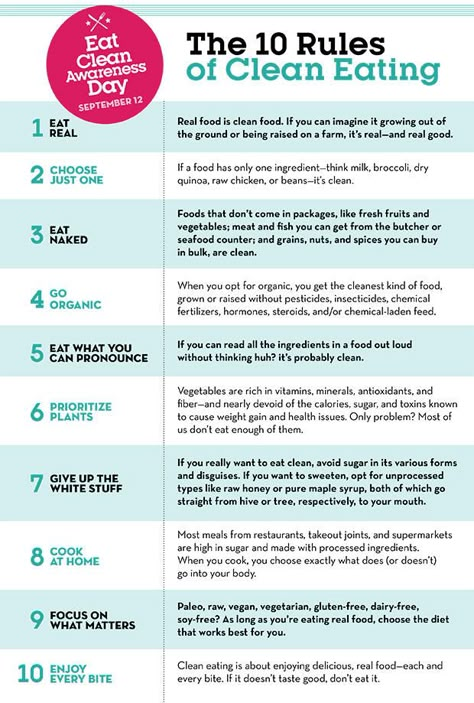
Why do antipsychotic medications worsen obesity-related diseases?
Antipsychotics can also be categorized into two classes: typical and atypical antipsychotics. Both classes can cause weight gain, but they differ in that atypical antipsychotics cause fewer movement disorder side effects. Like antidepressants, antipsychotics affect the chemical messengers in the brain associated with appetite control and energy metabolism, namely serotonin, dopamine, histamine, and muscarinic receptors. In addition to causing weight gain, antipsychotics can also impair glucose metabolism, increase cholesterol and triglyceride levels, and cause hypertension, all of which can lead to metabolic syndrome and worsen obesity-related diseases. The antipsychotics most likely to cause weight gain are olanzapine, risperidone, and quetiapine.
What about anti-anxiety medications and weight changes?
There is no clear link between traditional anti-anxiety medications such as benzodiazepines and weight gain. However, many antidepressants are also used for the treatment of anxiety, and may cause weight gain as discussed above.
However, many antidepressants are also used for the treatment of anxiety, and may cause weight gain as discussed above.
Similarly, not all medications for sleep cause weight gain; one that has been associated with weight gain is diphenhydramine (the active ingredient in Benadryl that is also used in many over-the-counter sleep aids). Diphenhydramine can contribute to weight gain by causing increased hunger and tiredness, which can make a person less active. Other sleep aids such as zolpidem (Ambien) or eszopiclone (Lunesta) have not been linked to weight gain.
Trazodone, a medication used for depression as well as insomnia, reduces excess serotonin at some sites, while increasing serotonin levels at other sites, thus affecting appetite as previously discussed.
Mood stabilizers are often used to treat bipolar disease, and can increase appetite or cause changes in metabolism. Although some antidepressants and antipsychotics are also used to treat bipolar disease, mood stabilizers such as lithium, valproic acid, divalproex sodium, carbamazepine, and lamotrigine are the mood stabilizers often used for treatment of bipolar disorder, and with the exception of lamotrigine, they are all known to increase the risk of weight gain.
There are effective strategies to minimize weight gain
For people taking psychiatric medications for mental health, there are strategies to minimize weight gain. Optimizing lifestyle and daily habits is important. This includes eating a healthy diet with whole foods and limiting processed foods and added sugars; staying physically active; minimizing stress; and ensuring adequate restful sleep. Physical activity, in particular, can have a double effect of both improving mental health and minimizing weight gain that might otherwise occur. Cognitive and behavioral strategies under the guidance of a psychologist may be useful for avoiding giving in to any increased cravings for sweets and carbohydrates.
Another strategy to minimize weight gain is to work with your healthcare provider to determine if there might be an appropriate alternate medication option with a lower risk of weight gain. In addition, the anti-diabetes medication metformin has been shown to be effective in treating and preventing psychotropic-induced weight gain. Other medications prescribed for weight loss may also be appropriate to help counteract the weight gain experienced by psychotropic medications.
Other medications prescribed for weight loss may also be appropriate to help counteract the weight gain experienced by psychotropic medications.
Be aware that almost all medications have a risk of causing side effects, and it is important to ensure that the benefits of taking any medications will outweigh the risks. Speaking to your primary care provider, psychiatrist, or obesity medicine specialist can be useful in determining which options may work best for you.
Lunesta Side Effects: Adverse Reactions And Complications
Lunesta, the brand name for generic drug eszopiclone, is non-benzodiazepine acting as sedatives-hypnotics to treat acute and chronic insomnia. It interacts with the GABA receptors in the brain which regulate the sleeping pattern to produce a calming effect. It helps in getting better and longer sleep at night. Although taking it can help with conditions like insomnia still, like other sedative-hypnotics, there are several Lunesta side effects. It is a type IV-controlled substance that may lead to physical and psychological dependence. That is why its misuse and dependency need to be regularly monitored. In this article, detailed information about side effects, dangers of its long-term use, and liability of dependence on the drug will be provided to cover any queries.
It is a type IV-controlled substance that may lead to physical and psychological dependence. That is why its misuse and dependency need to be regularly monitored. In this article, detailed information about side effects, dangers of its long-term use, and liability of dependence on the drug will be provided to cover any queries.
Common Lunesta Side Effects
Lunesta (eszopiclone) is used in the treatment of sleeping problems. It is an approved medication for sleep improvement, maintenance, increase in quality and quantity of sleep as well as the improvement of next day function. It can help with transient and chronic insomnia and disturbed sleep schedules. While it is considered safe, it also has some undesirable effects.
Common Side Effects of Lunesta Include:
- headache
- dizziness
- anxiety
- metallic after taste
- daytime somnolence
More Severe Side Effects of Lunesta Can Range From:
- short-term memory impairment
- change in behavior
- aggression
- hallucinations
- self-harming thoughts
While headache dizziness and metallic taste are short-term side effects, others are especially manifested if one is taking its treatment for several months. These Lunesta Side Effects occur in less than 2% of individuals but taking more than the recommended dose can increase the frequency of these side effects. These effects can be physical as well as psychological and must be consulted with the doctor.
These Lunesta Side Effects occur in less than 2% of individuals but taking more than the recommended dose can increase the frequency of these side effects. These effects can be physical as well as psychological and must be consulted with the doctor.
Physical Lunesta Side Effects
The most common side effects of lunesta reported on treatment with eszopiclone are dry mouth, metallic taste, and headache. Metallic aftertaste or bitter taste on tip of the tongue is reported by the majority of people taking it even with the first dose compared to the other side effects which are usually presented after long term use.
Other Physical Lunesta Side Effects Experienced by People Taking It Aside From the Ones Mentioned Above Are:
- Itchy rash on the skin
- Cough
- Stomach-ache
- Loss of appetite
- Daytime somnolence
- Hangover feeling
- Dizziness
- Constipation
Allergic reaction to this drug is rare, however, severe dizziness, rash itch, difficulty in breathing, swollen tongue are red flags for an allergic reaction that one should look out for. It can maintain its calming effects even after a full night’s sleep. This can result in daytime sleepiness and drowsiness. There should be at least 8 hours of sleep after taking medication to combat the daytime somnolence. It is also important not to exceed the recommended 2-3mg dosage. Exceeded amounts result in severe and long-lasting physical effects. Prevalence for these side effects is less than 2% of the medication is taken properly, in the recommended dosage, and without any other interacting substances.
It can maintain its calming effects even after a full night’s sleep. This can result in daytime sleepiness and drowsiness. There should be at least 8 hours of sleep after taking medication to combat the daytime somnolence. It is also important not to exceed the recommended 2-3mg dosage. Exceeded amounts result in severe and long-lasting physical effects. Prevalence for these side effects is less than 2% of the medication is taken properly, in the recommended dosage, and without any other interacting substances.
Psychological Lunesta Side Effects
Eszopiclone works by interacting with GABA receptors in the brain. Where this interaction produces a calming effect for a sound overnight sleep, overuse of this drug can cause other psychological side effects. Most Common Psychological Lunesta Side Effects Include:
- Anxiety
- Mood swings
- Drug dependence
- Hallucination
One can Experience Severe Psychological Symptoms If The Use Of Medicine Is Dosage. These Are:
These Are:
- Memory loss or amnesia
- Confused thoughts
- Aggressive behavior
- Abnormal self-harming thoughts
- Auditory and visual hallucination
- Agitation
- Jitters
- Worsening of depression
Another psychological complication experienced by less than 1% of people is somnambulism or sleepwalking. A person can have a conversation, eat, drive, go to places or even engage in sexual activity while still being asleep. Most people don’t have a memory of these events and this can impose serious effects on their social functioning. These symptoms are usually presented by patients who either take a high dose or take it with other recreational substances like alcohol or illegal drugs.
The Dangers Of Lunesta Long-Term Use
The medication is used as a short term treatment of insomnia. It is a type IV controlled substance which means its long-term use can lead to physical and psychological dependence. It not only has a potential addicting effect but can also cause severe adverse reactions on long-term use such as mood swings, drug tolerance, memory loss, depression, and in extreme cases it can even cause organ failure.
It is a type IV controlled substance which means its long-term use can lead to physical and psychological dependence. It not only has a potential addicting effect but can also cause severe adverse reactions on long-term use such as mood swings, drug tolerance, memory loss, depression, and in extreme cases it can even cause organ failure.
Drug Tolerance
Using eszopiclone is beneficial for the short-term treatment of insomnia but If the medicine is continued for a long time, drug tolerance can develop with Lunesta long term use. It will take more and more dosages of medicine to produce the same effect. This drug tolerance can potentially lead to overdose and a disturbed sleep cycle. Therefore, while it is safe for short-term treatment of insomnia, it is not recommended for long-term use.
Memory Loss
Memory loss is another one of Lunesta side effects that can occur after Lunesta long term use. It is used in the treatment of insomnia because it acts as a central nervous system depressant. It depresses nerve fiber firing in the central nervous system to reduce the stress response. Long-term CNS depression can lead to memory impairment and amnesia. This can be corrected by gradually decreasing the dosage and withdrawing the medication.
It depresses nerve fiber firing in the central nervous system to reduce the stress response. Long-term CNS depression can lead to memory impairment and amnesia. This can be corrected by gradually decreasing the dosage and withdrawing the medication.
Depression
Side effects of Lunesta include worsening of existing depression symptoms and even causing depression in some patients. Low moods, suicidal thoughts, and irrational decisions are some other depression-related manifestations of using eszopiclone. If changes in one’s behavior are observed, a medical practitioner should be consulted immediately.
Organ Dysfunction
Our body has its drugs detoxification system. Disrupting the normal function of these organs is another complication of eszopiclone. Medicines are metabolized in the kidneys and liver. Taking a high dose of this medication for a long time causes stress on these organs and can lead to dysfunction. At the start, it can be reversed by simply withdrawing the medication slowly but as it progresses, it can enter an irreversible phase which can progress to end-stage organ failure. Therefore, it is important to take no more than the recommended medical dose and the recommended period.
Therefore, it is important to take no more than the recommended medical dose and the recommended period.
Lunesta And Weight
Weight changes are rare and are reported by less than 1% of Lunesta (eszopiclone) users. It can cause weight fluctuation owing to its effect on the central nervous system and body metabolism. There are not many studies that focus on weight changes with eszopiclone use or provide information about its association but many patients reported noticing weight changes. Although Eszopiclone mechanism of action doesn’t directly affect weight still, its effect on the central nervous system and mild effect on metabolism can be indirectly linked to weight and body mass fluctuation in some people.
Lunesta And Weight Gain
Does Lunesta Cause Weight Gain?. This is the most common medical concern for people who are just starting on this medicine by their doctor. Although weight gain is not a severe side effect of Lunesta. People who are on Lunesta sometimes report feelings of hunger while they are on drugs. Its use can increase the appetite and cause weight gain. It can be carefully ministered by using dietary restrictions and having proper sleep.
Its use can increase the appetite and cause weight gain. It can be carefully ministered by using dietary restrictions and having proper sleep.
Lunesta And Weight Loss
Weight loss is a very rare effect of Lunesta. Some people report unintentional weight loss with the use of this drug, which can be linked to its unpleasant or bitter after taste and dry mouth which can lead to loss of appetite. Loss of appetite may remain unnoticed by people but can cause weight loss due to lack of proper nutrition. The studies still have to provide information about their direct association with each other.
Lunesta In Pregnancy
The use of the drug in pregnancy is still under debate and information about its use in pregnancy is lacking. There are no controlled human trials proving its effect on pregnancy, this is why one should take extra caution while using it during pregnancy. It is labeled as FDA category C, which means it should only be prescribed with consideration. A pregnant woman should use it only under the doctor’s recommendation. There are not many studies that identify its risk factors and interaction in pregnant women and nursing mothers.
There are not many studies that identify its risk factors and interaction in pregnant women and nursing mothers.
It can only be prescribed if the beneficial medical effects outweigh the potential risk to the health of the fetus.
Preventing Lunesta Side Effects
This medication is a relatively safe drug, and if taken properly, less than 2% of people experience these side effects. Management of these side effects is important for the patient’s comfort and medical needs. These side effects can be reduced by taking only the recommended dosage. Having a window period of 8 hours to sleep can help with dizziness. For the common side effects, waiting for our body to adjust to the drugs is often the best option. Limiting the use of drugs like CNS depressants or alcohol can help with drug interactions. If these symptoms become severe, switching to another medicine under the doctor’s advice can be considered. It is important to have the proper information and these decisions should only be taken under the guidance of a doctor and consultation of a healthcare professional.
Hope Without Commitment
Find the best treatment options. Call our free and confidential helpline
(888)-772-4219
Most private insurances accepted
Marketing fee may apply
Page Sources
- Greenblatt, D. J., & Zammit, G. K. (2012). Pharmacokinetic evaluation of eszopiclone: Clinical and therapeutic implications. Expert Opinion on Drug Metabolism and Toxicology, 8(12). https://doi.org/10.1517/17425255.2012.741588
- Halas, C. J. (2006). Eszopiclone. American Journal of Health-System Pharmacy : AJHP : Official Journal of the American Society of Health-System Pharmacists, 63(1). https://doi.org/10.2146/ajhp050357
- K., M., A., A., & N., H. (2014). Evaluation of the efficacy and adverse effect (unpleasant taste) of eszopiclone in Japanese patients. International Journal of Neuropsychopharmacology, 17(SUPPL. 1).
- Monti, J. M., & Pandi-Perumal, S. R. (2007). Eszopiclone: Its use in the treatment of insomnia.
 Neuropsychiatric Disease and Treatment, 3(4).
Neuropsychiatric Disease and Treatment, 3(4). - Rösner, S., Englbrecht, C., Wehrle, R., Hajak, G., & Soyka, M. (2018). Eszopiclone for insomnia. In Cochrane Database of Systematic Reviews (Vol. 2018, Issue 10). https://doi.org/10.1002/14651858.CD010703.pub2
Published on: October 20th, 2016
Updated on: December 15th, 2021
About Author
Olivier George, Ph.D.
Olivier George is a medical writer and head manager of the rehab center in California. He spends a lot of time in collecting and analyzing the traditional approaches for substance abuse treatment and assessing their efficiency.
Medically Reviewed by
Michael Espelin APRN
8 years of nursing experience in wide variety of behavioral and addition settings that include adult inpatient and outpatient mental health services with substance use disorders, and geriatric long-term care and hospice care. He has a particular interest in psychopharmacology, nutritional psychiatry, and alternative treatment options involving particular vitamins, dietary supplements, and administering auricular acupuncture.
Have something to say?
Share your story in our Addiction Treatment Communities
Medicines that can make you gain weight
Taking medicines that your doctor prescribes for you for a particular reason may be accompanied by side effects that are not always desirable. Unfortunately, doctors do not always warn about what medications can lead to, and many would like to know what to expect from a course of medications.
Website editor
Tags:
The fight against excess weight
Medications
Migraine
hypertension
Getty Images
One of the most common drug side effects is weight gain. Let's make a reservation right away - this does not happen for everyone and not always, but you can be one of those "lucky ones" who really put on weight.
We talk about drugs that can cause weight gain. We are sure that it is better to know and take some steps in advance so as not to gain weight than to accidentally discover an extra 3-5, or even 10 kg, gained over several weeks of taking the drug.
In general, it would be absolutely useful to discuss with the doctor all the possible "side effects" that the prescribed medicine can cause in order to take timely action. This, however, applies to any side effects, and not just those associated with weight. In some cases, undesirable effects are inevitable, but there are situations when their occurrence can be completely avoided or at least made less pronounced.
Steroids
Steroid preparations can be prescribed for various diseases. They make it quite easy to achieve an improvement in the condition, but the treatment is often accompanied by an undesirable effect, including insomnia, increased appetite and swelling.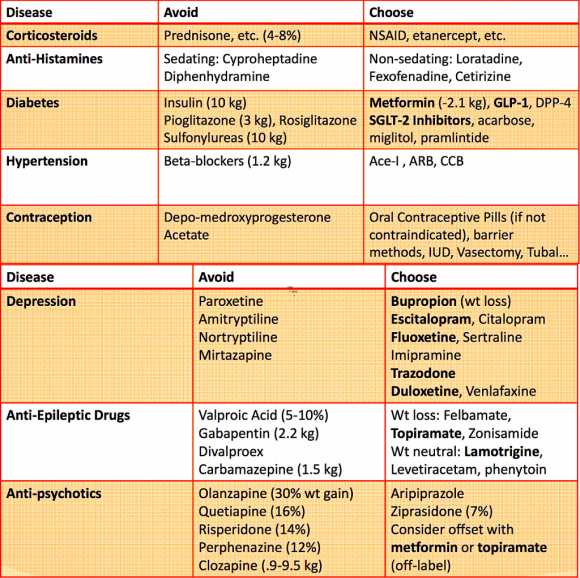 All this is the perfect combo for those extra pounds to literally stick in strategic places. It is important that steroids are available in different forms - these can be ointments and creams, sprays, as well as tablets. The latter just cause weight gain the most. You can reduce your chances of gaining weight by choosing the lowest possible dose for you, as well as adjusting your diet and choosing the ideal sleep pattern for you.
All this is the perfect combo for those extra pounds to literally stick in strategic places. It is important that steroids are available in different forms - these can be ointments and creams, sprays, as well as tablets. The latter just cause weight gain the most. You can reduce your chances of gaining weight by choosing the lowest possible dose for you, as well as adjusting your diet and choosing the ideal sleep pattern for you.
Antidepressants
Many people say that you can gain weight on antidepressants. Fortunately, not everyone is gaining it, although this, of course, is quite real. Selective serotonin reuptake inhibitors pose the greatest danger in this regard, so if you are taking drugs whose active ingredient belongs to this class of substances, be careful.
The fact is that such drugs not only improve your mood and help you feel less depressed, but also increase your appetite. And here the connection is quite obvious: you want to eat more - you eat more - your weight increases.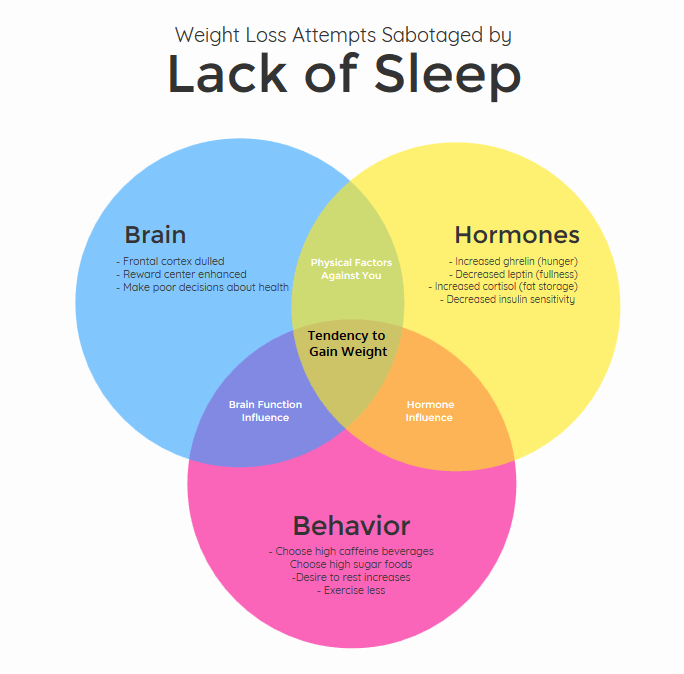
If you are prone to weight gain, then discuss with your doctor in advance that you are worried about the fact that he will become more - it is likely that he will be able to choose another suitable drug for you.
Birth control pills
Oral contraceptives have many side effects, some of which are quite pleasant and desirable. But, let's not hide, weight gain is not included in this list for everyone.
It works like this: progesterone, which is part of birth control pills, increases appetite, which causes women to eat more and gain weight. Another possible mechanism is that while taking contraceptives, the body begins to more actively retain water, and the weight also goes up because of this.
Antihistamines
Popular antihistamine-based allergy medications are most often not available by prescription. They can be prescribed by a doctor, but many people buy these drugs on their own initiative and choose the dosage on their own.
In addition to the fact that the selection of drugs still has to be handled by a specialist, there is another danger. All the same kilograms that you can gain. Taking allergy medications frequently can lead to weight gain. This happens more often in women than in men. If you notice that you are really gaining weight on the background of a course of antihistamines, but at least try to change the dosage form: the spray in this case will be much less dangerous than tablets.
Blood pressure medications
Medicines prescribed for hypertension, such as beta-blockers and angiotensin receptor blockers, also affect weight. Unfortunately, in the case of such drugs, the choice is not too rich. There is nothing to replace them and cancel, most likely, the doctor will not allow. And this means that in order to prevent gaining extra pounds, you will have to carefully monitor your lifestyle, adjust your diet and try to introduce at least a minimum of physical activity into your daily routine.
Migraine Medicines
Migraine pain is terrible and excruciating, so finding that one medicine or another really helps with these nightmarish headaches is priceless. People who suffer from migraines are often ready to go to great lengths to improve their condition, and they may not even notice such "little things" as weight gain while taking medication.
However, in any case, for those who suffer from migraines, it is important to monitor their condition, minimize or completely eliminate the influence of triggers that can provoke a migraine attack.
Drug-induced esophagitis
The first case of drug-induced esophagitis was described in 1970 by J. Pemberton [1]: ulcers of the esophageal mucosa were found in a patient taking potassium chloride [2]. Since that publication, a number of articles have appeared with reports of the development of drug-induced esophagitis against the background of the use of many drugs (drugs) from different pharmacological groups, they are summarized in table . In total, about 100 drugs have been identified that may be the cause of the development of drug-induced esophagitis [3]. Esophagitis associated with the use of antibiotics, antiretroviral and antitumor drugs, non-steroidal anti-inflammatory drugs (NSAIDs) is the best studied [4]. Drug-induced lesions of the esophagus occur as a result of the direct toxic effect of drugs and their effect on the nervous system (lower pressure in the lower esophageal sphincter, difficulty in emptying the stomach, etc.) [2, 4]. Drugs can also cause or exacerbate the course of gastroesophageal reflux disease (GERD) and, as a result, esophagitis [2, 4]. Drug-induced lesions of the esophagus significantly reduce the patient's quality of life.
Table . Medicines, the intake of which is associated with the development of drug-induced esophagitis [1-6, 9, 11, 12, 15–21, 23–29]
| Group of medicines | Drug | Mechanism | Level of evidence |
Evidence level: A - one or more randomized, controlled clinical trials; B - non-randomized clinical trials, prospective observational studies, cohort studies, retrospective studies, case-control studies, meta-analyses and/or post-marketing surveillance; C - the presence of one or more published cases or a series of cases.
Epidemiology
The incidence of drug-induced esophagitis is not completely known, but there are separate regional studies. For example, in Sweden, the incidence of drug-induced esophagitis is 4 cases per 100,000 population per year. Drug-induced esophagitis is more common in women aged 18–70 years, as well as in the elderly [4].
Classification and pathogenetic mechanisms
Drugs, the use of which is associated with the development of drug-induced esophagitis, can be divided into three groups according to their effect on the mucosa of the esophagus [4, 5]. The drugs of the first group cause temporary damage to the mucous membrane due to the low pH when dissolved in water. Localized discrete ulcers appear, which, after discontinuation of the drug, heal on their own without the formation of esophageal strictures. This group of drugs includes doxycycline, tetracycline, clindamycin, emepronium bromide, ascorbic acid and ferrous sulfate (II). Drugs of the second group cause permanent damage to the mucous membrane of the esophagus. These include quinidine, potassium chloride, and bisphosphonates. Drugs of the third group, causing permanent damage to the mucosa of the esophagus with strictures, include NSAIDs [4, 5]. According to one of the studies, the number of cases of esophagitis caused by the drugs of the first group is 65.8%, the drugs of the second group - 12.4%, the third group - 21.8% [5].
Drug-induced esophagitis occurs as a result of a combination of three main components of pathogenetic mechanisms: the action of drugs, the characteristics of the esophagus and exogenous factors [4, 6]. Drugs can cause esophagitis by direct or indirect effects on the mucosa of the esophagus [4]. The direct effect is the formation of caustic compounds (acids, alkalis, etc.), the indirect effect is the induction of a systemic reaction that can damage the mucosa (for example, the induction of acid reflux by calcium channel antagonists) [4]. In addition, the following characteristics of the drug are important: drug coating, duration of contact with the esophagus, release rate, size and shape.
In addition, the following characteristics of the drug are important: drug coating, duration of contact with the esophagus, release rate, size and shape.
Morphological and functional disorders such as esophageal achalasia, strictures, reflux, diverticula and hernias of the esophagus, cardiomegaly may increase the risk of drug-induced esophagitis due to a concomitant decrease in pressure in the distal esophagus. However, drug-induced esophagitis can also occur against the background of the normal state of the esophagus [4]. Exogenous factors that depend on the patient include body position when taking drugs, the amount of water taken with the drug, the time of taking the drug and the amount of saliva [6].
Pathophysiological mechanisms of development of drug-induced esophagitis against the background of individual drugs are presented in table .
Risk factors
Risk factors for the development of drug-induced esophagitis include lying on the back during and within 30 minutes after taking the drug, insufficient water when using drugs, the use of large tablets of drugs and / or in a gelatin capsule, as well as the presence of concomitant pathology of the esophagus, characterized by a decrease in pressure in the lower esophageal sphincter [4].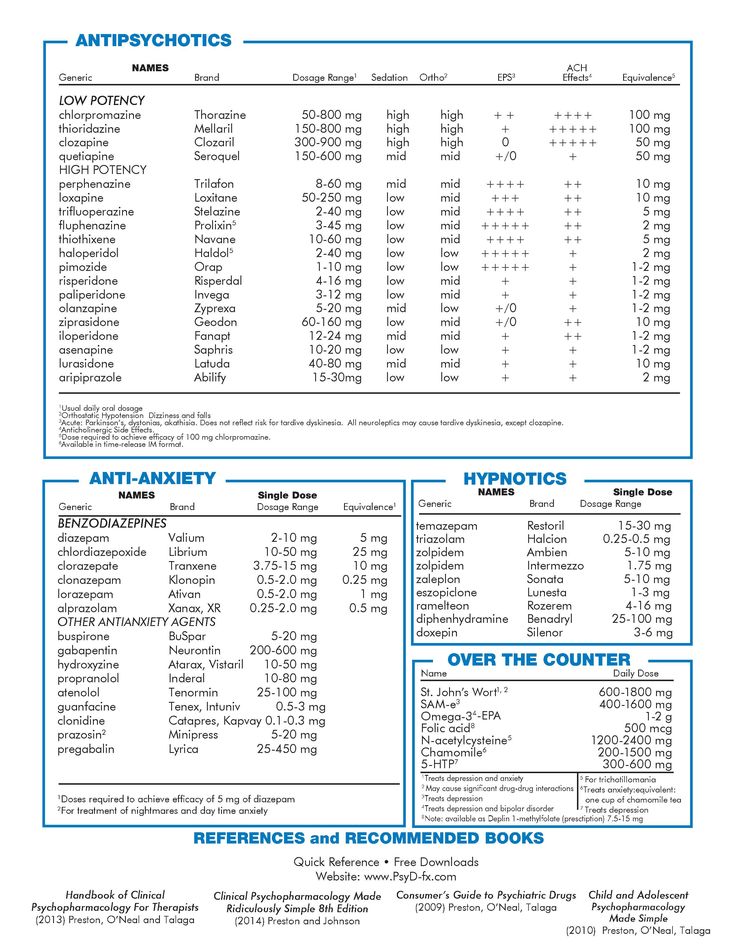
Clinical picture, diagnosis and differential diagnosis
Clinical symptoms of drug-induced esophagitis do not differ from esophagitis of other etiologies [4]. The occurrence of retrosternal pain, odynophagia, dysphagia, nausea and vomiting is noted [4, 7]. Severe cases of drug-induced esophagitis may be accompanied by weight loss and/or gastrointestinal bleeding. The occurrence of these symptoms correlates with the fact and / or time of taking drugs that can cause esophagitis, the time interval ranges from several hours to 10 days. In addition, during the history taking, it is necessary to pay attention to the position of the body in which the patient takes these drugs [4].
Some signs of esophageal pathology are found in 99% of patients with drug-induced esophagitis [6]. During endoscopy, various pathological changes can be detected: superficial erythema, mucosal erosion, esophageal ulcers (up to the formation of “kissing” ulcers in 43. 6% of cases [8]), strictures, esophago-respiratory fistulas, esophageal perforation. Lesions of the esophagus are more common in its middle third (in one study, lesions of the middle third of the esophagus amounted to 78.2% [8]), since in this place the esophagus experiences external pressure from the aortic arch and left atrium, although in some cases they can be localized in distal or proximal. Endoscopic examination can detect fragments of drugs [7]. The use of esophagoscopy is especially recommended in cases where the patient does not respond to therapy or the drug cannot be withdrawn [4].
6% of cases [8]), strictures, esophago-respiratory fistulas, esophageal perforation. Lesions of the esophagus are more common in its middle third (in one study, lesions of the middle third of the esophagus amounted to 78.2% [8]), since in this place the esophagus experiences external pressure from the aortic arch and left atrium, although in some cases they can be localized in distal or proximal. Endoscopic examination can detect fragments of drugs [7]. The use of esophagoscopy is especially recommended in cases where the patient does not respond to therapy or the drug cannot be withdrawn [4].
Double contrast is recommended for esophagography, as single contrast examination may show normal results. During the procedure, strictures, esophageal ulcers, external compression of the esophagus, and mobility abnormalities are detected [4, 6]. Histological examination of the biopsy of the esophageal mucosa does not reveal the etiology of drug-induced esophagitis. Usually the result is benign ulcers and acute inflammatory changes, however, histological evaluation is necessary for differential diagnosis with infectious pathology and malignant neoplasms of the esophagus [4].
Drug-induced esophagitis must be differentiated from esophagitis of another etiology and other pathology of the esophagus: these are herpetic esophagitis, eosinophilic esophagitis, candidal esophagitis, Crohn's disease, reflux esophagitis, giant ulcer of the esophagus.
Complications
Complications of drug-induced esophagitis include: gastrointestinal bleeding, esophageal stenosis and stricture, esophageal perforation, intramural esophageal hematoma, mediastinitis, etc. [2].
Treatment
For the treatment of drug-induced esophagitis, it is recommended to stop taking the drug that caused this condition and carry out symptomatic therapy with such drugs [2, 6, 7, 9] as lidocaine (local pain relief), proton pump inhibitors (PPIs) ), h3-receptor antagonists, antacids. Daily intake of PPIs in the morning in most patients can quickly relieve heartburn and cure esophagitis within a few weeks [2, 6]. Patients who do not respond well to a standard single daily dose of PPI should be given PPI twice a day [6]. A number of studies recommend the use of sucralfate in combination with PPIs to create a protective mucosal barrier [10, 11]. It should be noted that special studies on the treatment of exactly drug-induced esophagitis have not been conducted. In severe cases (strictures of the esophagus, bleeding from an ulcer, accumulation of drugs in the affected esophagus, etc.), endoscopic treatment is indicated [4].
Patients who do not respond well to a standard single daily dose of PPI should be given PPI twice a day [6]. A number of studies recommend the use of sucralfate in combination with PPIs to create a protective mucosal barrier [10, 11]. It should be noted that special studies on the treatment of exactly drug-induced esophagitis have not been conducted. In severe cases (strictures of the esophagus, bleeding from an ulcer, accumulation of drugs in the affected esophagus, etc.), endoscopic treatment is indicated [4].
Prevention
For the prevention of drug-induced esophagitis, it is recommended not to take drugs at bedtime and in the supine position, and to take one tablet at a time with 200-250 ml of liquid to increase the amplitude and duration of esophageal peristalsis [4 ]. In elderly patients and patients with esophageal dysmotility, it is preferable to take drugs in liquid form, if possible, large gelatin-coated drugs are excluded [4].
Prognosis
The prognosis of patients with timely diagnosed drug-induced esophagitis is usually favorable [2]. As a rule, a week after stopping the drug and starting symptomatic therapy, the esophageal mucosa is restored. Follow-up endoscopy is usually not required [2].
As a rule, a week after stopping the drug and starting symptomatic therapy, the esophageal mucosa is restored. Follow-up endoscopy is usually not required [2].
Certain drugs associated with the development of drug-induced esophagitis and gastroesophageal reflux disease
Antibiotics. Drug-induced esophagitis can be caused by some antibiotics [6]. After dissolution in saliva, the pH of tetracycline and its derivatives changes to the acid side. There are several reports of the occurrence of severe esophagitis after taking tetracycline with insufficient water and just before bedtime [5, 6]. There are also descriptions of clinical cases of doxycycline-induced esophagitis in patients with malaria [12]. These patients complained of hiccups, and during endoscopy they found erosions and ulcers of the esophagus [6]. In one study, doxycycline-induced esophagitis was found in 24 out of 25 patients [10]. The average age of patients with antibiotic-induced esophagitis is about 30 years [11].
Antiretroviral drugs . Zidovudine, which inhibits human immunodeficiency virus replication, can also cause drug-induced esophagitis, with both multiple and large single ulcers being found [6]. In one study, a patient with a history of zidovudine-induced esophagitis also had episodes of drug use in the supine position and without drinking water [6]. Drug-induced esophagitis can also be caused by antiretroviral drugs such as nelfinavir and zalcitabine [4].
Glucocorticoids. One study showed the ability of dexamethasone to reduce pressure in the lower esophageal sphincter [13]. In addition, there is evidence that taking prednisolone increases the contact time of hydrochloric acid with the mucosa of the esophagus by more than 2 times and thereby increases the likelihood of esophagitis [5].
NSAIDs . NSAID-induced esophageal injury remains an important public health problem. For example, taking low doses of acetylsalicylic acid can approximately 2-fold increase the likelihood of developing peptic esophagitis [9]. Among the pathogenetic mechanisms for the development of NSAID-induced esophagitis, there is an increase in gastric secretion and a decrease in pH, a direct contact effect of drugs, a decrease in bicarbonate production and a change in the properties of mucus, inhibition of gastric motility and provoking gastroesophageal reflux [9]. There is a high probability of extraesophageal symptoms (cough, choking, morning hoarseness, halitosis, etc.). There are the following risk factors for the occurrence of NSAID-induced lesions of the esophagus [9]: older age, male gender, concomitant use of glucocorticoids, alendronate, low doses of acetylsalicylic acid. Erosive esophagitis is more often found in patients with gastric and duodenal ulcers, as well as in the presence of hiatal hernia [9]. The incidence of esophageal strictures in NSAID-induced esophagitis reaches 40–50% [11]. In one of the retrospective longitudinal controlled studies, it was found that taking NSAIDs increases the risk of GERD by 2.
Among the pathogenetic mechanisms for the development of NSAID-induced esophagitis, there is an increase in gastric secretion and a decrease in pH, a direct contact effect of drugs, a decrease in bicarbonate production and a change in the properties of mucus, inhibition of gastric motility and provoking gastroesophageal reflux [9]. There is a high probability of extraesophageal symptoms (cough, choking, morning hoarseness, halitosis, etc.). There are the following risk factors for the occurrence of NSAID-induced lesions of the esophagus [9]: older age, male gender, concomitant use of glucocorticoids, alendronate, low doses of acetylsalicylic acid. Erosive esophagitis is more often found in patients with gastric and duodenal ulcers, as well as in the presence of hiatal hernia [9]. The incidence of esophageal strictures in NSAID-induced esophagitis reaches 40–50% [11]. In one of the retrospective longitudinal controlled studies, it was found that taking NSAIDs increases the risk of GERD by 2. 11 times [5].
11 times [5].
Chemotherapeutic drugs. Injuries to the esophagus when taking chemotherapeutic drugs are mainly caused by their direct action on the mucous membrane [5]. Cases of esophagitis induced by taking bleomycin, cytarabine, dactinomycin, daunorubicin, fluorouracil, metrotrexate, vincristine have been described [7, 14].
Hormones and their derivatives. There is evidence of an increased risk of developing and more severe course of GERD in patients taking conjugated estrogens for a year or more, as well as receiving estrogen therapy alone or progesterone therapy alone [15, 16]. However, when using combined hormone replacement therapy, an increase in the risk of developing GERD was not found [5].
Antiarrhythmic drugs. An association has been established between the occurrence of esophagitis and oral administration of the antiarrhythmic drug quinidine [5, 11]. According to one study, the average age of patients with quinidine-induced esophagitis was 60 years [11].
Anticoagulants. Dabigatran etexilate is an oral anticoagulant that is now increasingly used due to its good tolerability, efficacy and lack of the need to control the blood coagulation system. However, in the last decade there are more and more reports of side effects from the gastrointestinal tract when taking the drug dabigatran etexilate [17-19]. Y. Toya et al. [20] report the occurrence of dabigatran-induced esophagitis in 20% of study participants, according to endoscopic examination data [20]. There is no study that has identified the prevalence of dabigatran-induced esophagitis, but one retrospective review of 91 case histories of patients treated with dabigatran etexilate noted that 19 (20.9%) patients on upper gastrointestinal endoscopy endoscopic signs of esophagitis were found in the intestinal tract [18, 21].
In its structure, dabigatran etexilate contains tartaric acid, which, when released in the esophagus, damages the mucous membrane. Dabigatran-induced esophagitis can either manifest itself with typical symptoms (retrosternal pain, odynophagia, dysphagia, etc.) or be asymptomatic [17, 18]. The asymptomatic course of dabigatran-induced esophagitis may go unnoticed for a long time in patients who do not undergo endoscopy [21]. Most often, patients with esophagitis associated with taking the drug dabigatran etexilate took it during ventricular fibrillation at a dose of 110 mg 2 times a day [19]. Usually, discontinuation of this drug in combination with PPI therapy for 1 week is sufficient to relieve the symptoms of dabigatran-induced esophagitis [18].
Dabigatran-induced esophagitis can either manifest itself with typical symptoms (retrosternal pain, odynophagia, dysphagia, etc.) or be asymptomatic [17, 18]. The asymptomatic course of dabigatran-induced esophagitis may go unnoticed for a long time in patients who do not undergo endoscopy [21]. Most often, patients with esophagitis associated with taking the drug dabigatran etexilate took it during ventricular fibrillation at a dose of 110 mg 2 times a day [19]. Usually, discontinuation of this drug in combination with PPI therapy for 1 week is sufficient to relieve the symptoms of dabigatran-induced esophagitis [18].
Calcium channel blockers. According to one study, the use of calcium channel blockers for 6 years induced the development of GERD in 16.5% of patients [22]. More often, manifestation or exacerbation of GERD occurs when taking nifedipine (21.5%), amlodipine (23.8%) and felodipine (21.5%) [5].
Nitrates. Nitrates reduce pressure in the lower esophageal sphincter, and can also have a direct damaging effect on the mucosa of the esophagus, inducing the development of GERD and esophagitis [5]. There are results from a double-blind, placebo-controlled study showing that isosorbide dinitrate significantly reduces pressure in the esophageal sphincter [23]. Even foods high in nitrates can increase the risk of GERD by 3 times [5].
There are results from a double-blind, placebo-controlled study showing that isosorbide dinitrate significantly reduces pressure in the esophageal sphincter [23]. Even foods high in nitrates can increase the risk of GERD by 3 times [5].
Adenosinergic drugs. There are data from randomized controlled trials proving the induction of GERD and increased reflux by theophylline drugs due to a decrease in pressure in the lower esophageal sphincter [5, 24].
Anticholinergic drugs. Emepronium bromide is an anticholinergic drug used to reduce the frequency of urination. More often it is prescribed to women, in connection with this, women predominate among patients with esophagitis induced by taking emepronium bromide [11]. However, there is a report of the occurrence of esophagitis in children taking this drug [25].
Antihyperglycemic drugs. There is evidence of the ability of the hypoglycemic drug glimepiride to cause damage to the esophagus, but the mechanism of its occurrence remains unknown [2, 5].
Bisphosphonates. Alendronate, a selective osteoclast inhibitor, prevents bone resorption and is used to prevent and treat postmenopausal osteoporosis. However, the daily use of alendronate at a dose of 40 mg increases the incidence of complications from the gastrointestinal tract due to the direct effect on the mucous membrane [6]. There is a description of a clinical case of the development of alendronate-induced esophagitis in a patient with postmenopausal osteoporosis while taking alendronate for three months at a dose of 10 mg/day [3].
Another bisphosphonate, risedronate, is less toxic. In a pooled study of 9 clinical trials, which included more than 10,000 patients, there was no statistically significant difference between the incidence of esophageal side effects in patients taking risedronate and patients taking placebo [11].
Antidepressants. Long-term use of tricyclic antidepressants can induce the development of GERD due to their anticholinergic action, which causes a decrease in pressure in the lower esophageal sphincter. The highest risk of developing GERD is observed in patients taking amitriptyline. In addition, the occurrence of lesions of the esophagus correlates with the use of dotypine, lofepramine, clomipramine [5].
The highest risk of developing GERD is observed in patients taking amitriptyline. In addition, the occurrence of lesions of the esophagus correlates with the use of dotypine, lofepramine, clomipramine [5].
Anxiolytics. In one study, approximately 30% of patients treated with alprazolam experienced GERD symptoms predominantly at night due to the inhibitory effect of the drug on the central nervous system [5].
Benzodiazepines. There is evidence that benzodiazepine drugs reduce the pressure in the lower esophageal sphincter, increasing the duration of reflux in both healthy people and patients with GERD [5]. For example, the appointment of diazepam at a dose of 5 mg / day reduces the level of pressure in the lower esophageal sphincter by 18.9%, and at a dose of 10 mg/day — by 37.8% [5].
Antiepileptic drugs . A clinical case report of esophageal ulceration resulting from the use of phenytoin in an elderly patient has been published [26].
Vitamins. Ascorbic acid, due to its damaging effect on the mucous membrane of the esophagus, can cause esophagitis and increase reflux [5, 27].
Macro and microelements. There are reports that potassium chloride-associated esophagitis is more common in women with rheumatic heart disease [11]. In addition, there is a possibility of developing damage to the esophagus induced by the intake of iron sulfate [11].
Other drugs. In addition to these, some other drugs can cause damage to the esophagus, such as pinaverium bromide, tiropramide [2].
Medication-associated lesions of the esophagus remain an urgent problem, as they are accompanied by clinical symptoms that significantly impair the quality of life of patients, and can also cause severe complications. Timely diagnosis, treatment and prevention of drug-induced diseases of the esophagus are important tasks for the practitioner.