Does insurance pay for a therapist
Does Insurance Cover Therapy? When, How to Check, and More Tips
If you’re one of the millions of Americans who are considering therapy, health insurance coverage may be a concern. If you have health insurance, chances are good that your policy provides some level of coverage.
To address the importance of and demand for sustaining mental wellness, most insurance companies offer some coverage for mental health services. But there are large differences between the benefits health insurers provide and the out-of-pocket costs you might be required to pay.
If you have health insurance through your job, it may or may not include coverage for therapy. Even if you have coverage, it’s up to you to decide whether or not you wish to use it for mental healthcare. In some instances, people choose to pay out of pocket for therapeutic services rather than claim coverage through their insurer. Why?
Insurance companies only pay for medically necessary services. They require a mental health diagnosis before they will pay claims. Some people are not comfortable with this.
A mental health condition diagnosis may range from acute stress to insufficient sleep syndrome, various phobias, mental illnesses, or a number of other descriptors. When it comes to insurance, each of these would have a code number that would go with an insurance claim.
Employer-sponsored insurance in companies of 50+ employees
Companies of 50 or more full-time workers are legally mandated to provide health insurance. This mandate does not specify that mental health services be included as a benefit. Even so, most large companies, including those that are self-insured, do provide health insurance that includes some coverage of therapeutic services.
Employer-sponsored insurance in companies under 50 employees
Small companies that employ under 50 people are not legally required to provide health insurance to their employees. However, for those who do, mental health services and substance use disorder services must be included, no matter where or how the plan is purchased.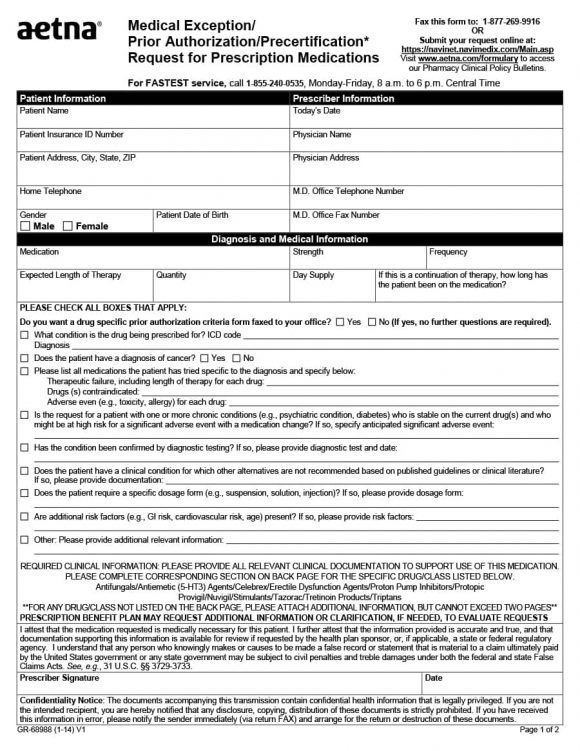
Health Insurance Marketplace plans
Under the Affordable Care Act, all plans purchased through the Health Insurance Marketplace must cover 10 essential health benefits. These include mental health services and substance use disorder services.
All Marketplace plans, whether they’re state or federally managed, include coverage for mental health. This pertains to individual plans, family plans, and small business plans.
Plans and their coverage vary by state. States also offer multiple plan options, which vary in terms of their coverage.
All Marketplace plans must include
- behavioral health treatments, such as psychotherapy and counseling
- mental and behavioral health inpatient services
- coverage for pre-existing conditions
- no yearly or lifetime dollar limits on mental health coverage
- parity protections so that the copays, coinsurance, and deductibles for mental health services are the same or similar to those for medical and surgical benefits
CHIP (Children’s Health Insurance Program)
CHIP provides federal funding to states so that they can provide low-cost health insurance for low-income households with children who aren’t eligible for Medicaid. CHIP coverage varies from state to state, but most provide a full array of mental health services, including:
CHIP coverage varies from state to state, but most provide a full array of mental health services, including:
- counseling
- therapy
- medication management
- social work services
- peer supports
- substance use disorder treatments
The Mental Health Parity and Addiction Equity Act (MHPAE) requires most CHIP programs to provide parity protections for mental health and substance use disorder services. This ensures that copays, coinsurance, and deductibles for therapy and other mental health services are the same or comparable to those for medical and surgical benefits.
Medicaid
All state-run Medicaid plans are required to cover essential health benefits, including mental health and substance use services. Medicaid plans vary by state to state, but are also subject to the MHPAE.
Medicare
Original Medicare covers inpatient behavioral health and substance use services under Part A. If you’re hospitalized, you may have a deductible per benefit period as well as coinsurance costs.
Outpatient mental health services, including an annual depression screening, are covered under Part B. You may incur out-of-pocket costs for therapeutic services, including the Part B deductible, copays, and coinsurance.
If you have a Medicare Advantage (Part C) plan, it’ll automatically cover therapeutic services at the same level or greater than original Medicare. Your costs may vary from those associated with original Medicare.
Register and log on to your insurance account online
Your health insurance plan’s website should contain information about your coverage and costs you can expect. Since insurers offer a variety of plans, make sure you’re logged on and viewing your specific insurance plan.
If you’re required to choose a therapist that’s in your plan’s network, a list of providers should be available online. You can also call and ask that a local list be given to you by phone or mail.
Call your insurance provider
If you need additional information, call the toll-free number on the back of your insurance card and ask questions about the types of therapeutic services you can expect coverage for, as well as any out-of-pocket costs you may incur. If you have a diagnostic code, that may help you get accurate information.
If you have a diagnostic code, that may help you get accurate information.
Check with your company’s HR department
If you’re insured through employment and need additional help, contact your human resources (HR) department, if you feel comfortable doing so.
Ask the therapist if they accept your insurance
Therapists and other providers often change the insurance plans they’re willing to accept and may have opted out of your plan.
First, you can’t be penalized for having a pre-existing condition or prior diagnosis of any type of mental illness. For that reason, you should be entitled to mental health services from day one of your plan’s start date.
Things that might affect when insurance coverage kicks in:
- After prior authorization. Some services may require pre-authorization before you can obtain coverage for them.
- After meeting a deductible. You may also have to meet an out-of-pocket deductible before your plan starts to cover therapy.
 Based on the type of plan you have, this amount may be significant.
Based on the type of plan you have, this amount may be significant. - After spending a minimum. In some instances, your plan may require that you pay a specified dollar amount on medical services before your coverage for therapy can start.
Some mental health services that may be covered by insurance include:
- psychiatric emergency services
- co-occurring medical and behavioral health conditions, such as coexisting addiction and depression. This is often referred to as a dual diagnosis.
- talking therapies, including psychotherapy and cognitive behavioral therapy
- unlimited outpatient sessions with a psychiatrist, clinical social worker, or clinical psychologist. In some instances, your insurer may cap the number of visits you’re allowed annually — unless your provider states in writing that they’re medically necessary for your care.
- telemedicine and online therapy
- inpatient behavioral health services received in a hospital or rehabilitative setting.
 Your plan may limit the length of your stay, or cap the dollar amount they’ll pay for your care per benefit period.
Your plan may limit the length of your stay, or cap the dollar amount they’ll pay for your care per benefit period. - addiction treatment
- medical detox services, including medications
Insurers only cover treatments that are considered medically necessary.
The breadth of coverage for specific therapeutic treatments, such as the length of rehab or hospital stays, also varies from plan to plan. So does the coverage and cost for medications you might be prescribed to treat your condition, both as an inpatient and as an outpatient.
Since insurers offer an array of plans, it’s not possible to give the specifics of each plan they cover. Here are some examples of coverage you may be able to get for therapy from specific insurers:
Does Blue Cross Blue Shield cover therapy?
The vast majority of Blue Cross Blue Shield insurance plans cover therapy.
If, however, your plan started before 2014 (when the Affordable Care Act was enacted) your plan may not cover therapy.
Blue Cross Blue Shield only covers evidence-based therapeutic services, such as psychoanalysis.
It doesn’t cover therapeutic services provided by a life coach or career coach.
It also doesn’t cover therapeutic services provided outside of a therapeutic setting, such as therapist-led systematic desensitization for phobias. These types of sessions may take place in a variety of locations, such as in a car if you have a phobia of driving, or on a plane if you have a phobia of flying.
Does Kaiser Permanente cover therapy?
Kaiser Permanente provides personalized treatment plans for mental health.
These plans typically cover one-on-one therapy with a professional such as a psychiatrist or nurse practitioner who specializes in mental health.
They also cover group therapy sessions and mental health classes.
Personalized stress management and addiction counseling are also included.
More insurers and examples
- about Aetna therapy coverage
- about United Healthcare therapy coverage
- about Cigna therapy coverage
There are many places to start your search for a therapist or counselor that you want to work with, from asking people you know to talking with your primary care physician.
Start with the in-network list
If your insurer has a network of providers, this may be a good place to start looking for a therapist. Each therapist listed should have some information about their practice and specialty areas. These may include pediatrics, geriatrics, conditions such as obsessive-compulsive disorder or bipolar disorder, and their approaches to care.
Review lists from organizations for your location
The American Psychiatric Association provides a list of psychiatrists who have opted in to the database by zip code.
The American Psychological Association provides a list of psychologists by zip code.
You can also look for a therapist through the Open Path Psychotherapy Collective. This nonprofit nationwide network offers inexpensive therapeutic options for individuals, couples, and children.
If you intend to pay for therapy out of pocket, know that psychiatrists may charge different rates per hour than other types of mental health professionals, such as psychologists or licensed clinical social workers. This may also affect the cost of your copay, if you use your insurance to pay for therapy.
This may also affect the cost of your copay, if you use your insurance to pay for therapy.
Paying for care
Understandably, the cost of therapy can be a big concern. Many therapists accept patients on a sliding scale. If you’re concerned about the cost of therapy, ask the therapist you’re considering if they’ll work with you on price or about any payment options they offer.
You can learn more about therapy at every budget level here.
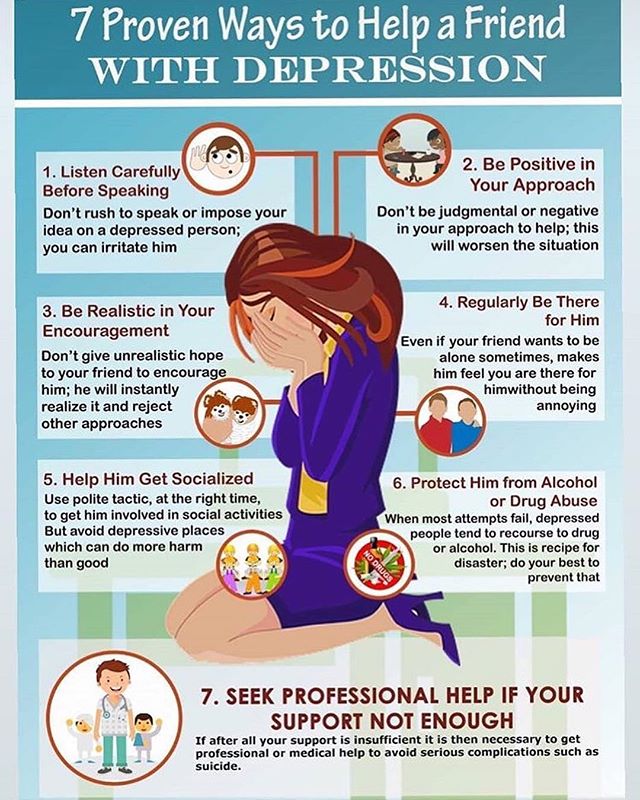
If mental health symptoms are getting very difficult to manage, reach out for professional support. A mental health professional can help you work through your symptoms and help you start treatment.
Therapy is especially important if your symptoms are negatively affecting your daily life.
However, you don’t need a diagnosis to talk with a therapist or psychiatrist. They can also help when you’re dealing with feelings of stress or overwhelm.
Other reasons people go to therapy include:
- going through a major life transition
- experiencing grief
- managing relationship difficulties
Can insurance be used for therapy?
Yes, insurance can be used for therapy. Health insurance typically covers therapist visits and group therapy.
Health insurance typically covers therapist visits and group therapy.
The level of coverage will vary based on your insurance provider and plan.
Additionally, since insurance only covers “medically necessary” services, some insurance companies may require a mental health diagnosis before they will pay claims.
How much does therapy cost?
The cost of therapy can vary widely depending on your location, your therapist, the type of your visit (in-person vs. remote), and other factors.
Generally, many therapists charge between $65 and $200 per session.
What does insurance cover for mental health?
Some mental health services typically covered by health insurance plans include:
- therapy
- group therapy
- addiction treatment
- inpatient behavioral services
- emergency mental health services
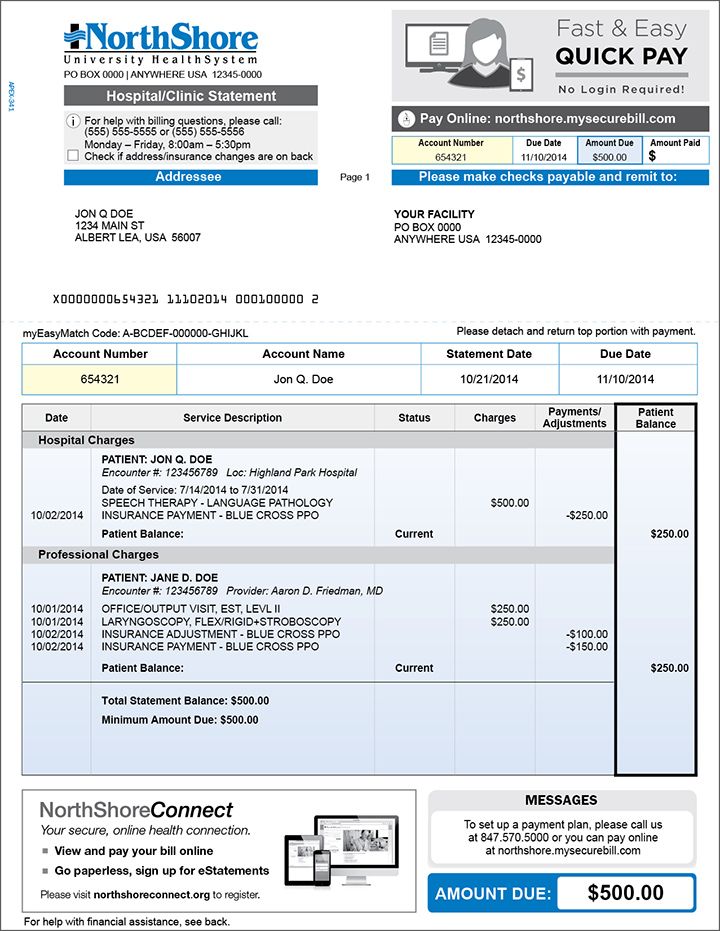
How does my therapist bill my insurance provider?
Most therapists will bill your insurance company for you. Your therapist will contact your insurance provider with the needed information, such as their name and address, your diagnosis, and the type of services you received.
Your therapist will contact your insurance provider with the needed information, such as their name and address, your diagnosis, and the type of services you received.
Sometimes, you might pay a copay upfront. In other cases, you may need to pay the full price of your session and be reimbursed later.
Does insurance cover couples counseling?
If you’re planning on using insurance to pay for couples counseling, the rule requiring a mental health diagnosis will continue to apply in most cases: One partner must receive a diagnosis for insurance to cover it. Some people feel this has the potential to skew their therapeutic experience.
As with any diagnosis you receive, a mental health condition diagnosis may remain in your permanent record. In some instances, it may be accessed by background checking systems.
Most health insurance plans cover some level of therapeutic services. The amount of coverage you can expect will vary from plan to plan. In many instances, you’ll have a deductible to pay before your services are covered.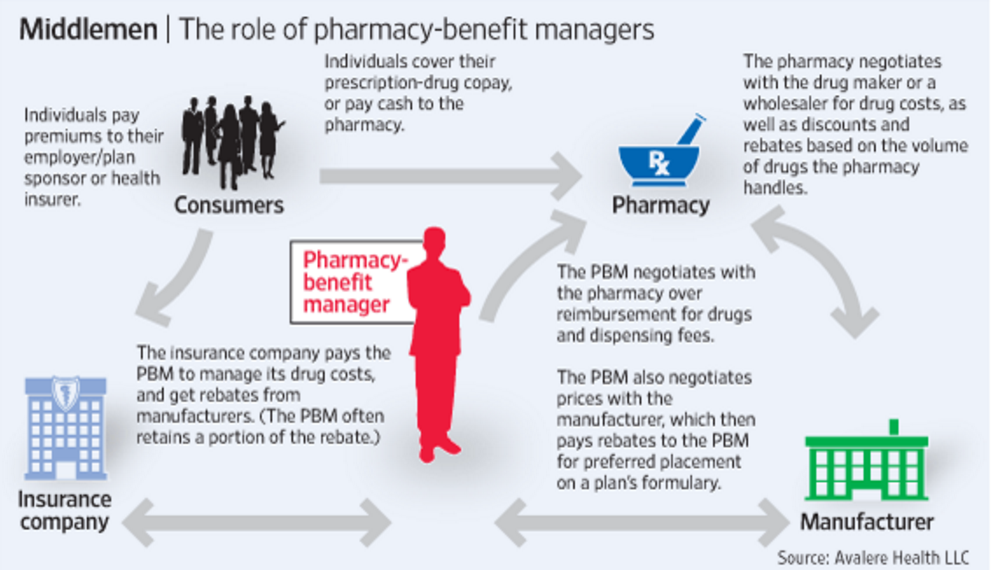 Copays and coinsurance may also apply.
Copays and coinsurance may also apply.
Services such as therapist visits, group therapy, and emergency mental healthcare are typically covered by health insurance plans. Rehabilitative services for addiction are also included.
Therapy can be expensive, with or without insurance. There are low-cost options that can help, such as therapists who take sliding scale payments and psychotherapeutic collectives that offer steeply reduced sessions.
If you need therapy but can’t afford it, talk to your doctor or another professional you trust, such as a clergy member or school guidance counselor. There are many ways that the financial barriers between you and the therapeutic care you need can be removed.
4 Key Reasons Using Insurance For Therapy is a Bad Idea
Although having mental health benefits gives many more people access to therapy, it comes at a price. Given changes happening in health care law, it’s essential to know the long term costs of using insurance to pay for therapy.
When someone is set on staying in-network
Many people call my office and immediately ask, “do you take my insurance?” If we say no, we often hear, “I’ll keep calling around until I find someone that does.”
I’m really baffled when someone says, “wow! You guys are exactly what I’ve been looking for! But I’m going to call around until I find someone in-network.”
What?
When someone is set on using insurance, there’s little we can say to change their minds.
Most of us pay a ton for health insurance and want to use it as often as possible. I definitely do.
Lots of people lump therapy in with health care. If health insurance is for health care, then they should be able to use insurance to pay for therapy.
If only it were that easy.
Using insurance for therapy comes with strings attached
Many people don’t realize that there are real, long-term costs when using insurance to pay for therapy. Unfortunately, we don’t get this information when we sign up for our plans.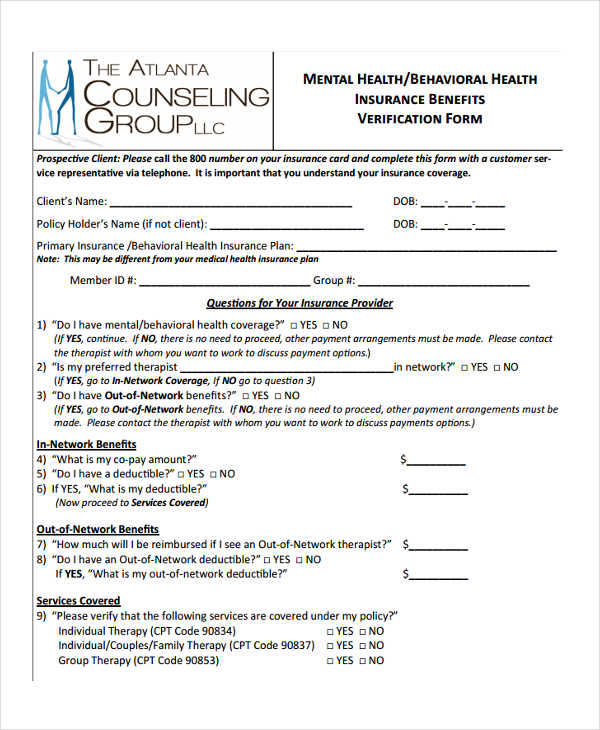
It’s not like this is top-secret. It’s in the public domain. You can Google it. When you read what’s up, it’s no wonder insurance companies and employers don’t highlight it in your benefits package.
Fewer therapists are taking insurance. Among therapists who still accept insurance, more are letting patients know about the risks of using health insurance to pay for therapy.
This isn’t a scare tactic. It’s part of informed consent.
If you’re going to use insurance to pay for therapy, you should know the risks.
Once you learn what these risks are, you have to ask, “is using my insurance worth it?”
The real costs of using insurance for therapy
- You will have a pre-existing condition on your insurance record:
In order to bill your insurance company, a therapist needs to diagnose you with a mental illness. This means that your insurance record will forever contain that information.
Given expected changes in health care laws, this will make buying health, disability, and life insurance harder and more expensive for you and your family. You will only qualify for limited, high deductible plans with high co-pays. The first phase of these restrictions is already in place.
You will only qualify for limited, high deductible plans with high co-pays. The first phase of these restrictions is already in place.
You may be thinking, “who cares? Everything is a pre-existing condition now.” Mental health diagnoses can be treated differently. If you don’t believe that, just ask someone who is considered uninsurable due to a diagnosis they received after psychological testing. I have patients who’ve been devastated by that.
- You might have to wait months for an appointment:
The average wait time for an appointment at an insurance practice is 2-4 months. By the time you can see someone, you’ll have lost the momentum that pushed you to call in the first place, and/or you’ll be worse than before. You may even require an intensive treatment program instead of weekly sessions by that point.
- You lose control over the confidentiality of your information:
A mental health diagnosis goes on your permanent insurance record. This record can be accessed by any insurance company or government agency during background checks.
This record can be accessed by any insurance company or government agency during background checks.
If you need security clearance for work, want to join the military, are applying for jobs that require a criminal background check, or are involved in a Workman’s Comp case, all your mental health information can be accessed.
Finally, if you’re ever sued, the opposing party can subpoena your medical and mental health records to build a case against you. This becomes a disaster quickly in divorce cases.
- You’re less likely to be committed to the process:
Paying $100-$150 for a therapy session, sometimes weekly for months or years, can make you nauseous. However, there’s a lot of research showing that people value what they pay for. The more you pay, the more invested you are in making sure you get something out of it.
Here’s a basic example. If you’re about to pay $150 for a meal, you’re more likely to research the restaurant, get dressed up, ask the server questions, and savor each bite. How often do you do this when you pay $15 for a meal?
How often do you do this when you pay $15 for a meal?
Therapists see the same thing all of the time. In general, people who pay out of pocket tend to be more invested in the process, are more likely to complete challenges, and are more likely to reach their clinical goals.
It’s not personal. It’s basic human behavior.
Are there exceptions? You bet. Based on what I’ve seen, it’s when people have to save and sacrifice to pay a high weekly co-pay. Again, real skin in the game equals progress.
Yes, there are exceptions
If your finances are so limited that using insurance is the only way you’ll get the therapy you need, then please do it.
If your co-pay is too high, please contact community mental health centers or university training clinics that offer discounted therapy.
Getting treatment is always the priority.
Is therapy worth the cost?
I’ve seen people take out loans to pay for therapy with a top expert because they knew it’s what they needed.
I’ve also seen people who drive luxury cars quit therapy because their co-pay went up by $20.
How we spend our money depends on how we determine value.
If you’re set on using insurance even though you have other options, like using out-of-network benefits or money you would rather spend on other purchases, then please do so.
However, if you have out-of-network benefits or the means to pay out of pocket, I strongly recommend you do so, at least for therapy and other specialists.
The unfortunate trend in the US is that fewer specialists across health care are accepting insurance.
We’re also seeing this in countries with socialized medicine like the UK and Canada.
Another reality is that deductibles and co-pays will continue to rise.
There are patients in the practice who pay an $80 co-pay to see a therapist who would otherwise charge them $95. If you can manage it, is saving $15 worth the risk?
We’re already seeing that, if you want good treatment for yourself or a loved one, you’ll have to pay for it.
Next steps
We’re in unknown waters when it comes to health care. As insurance laws continue to change, we’ll have to figure out our own health care and pay for it.
Using out of network benefits to pay for therapy will still result in a diagnosis on your record, but you’ll have so much more control over what else is there. You can protect your privacy.
Whenever possible, go with the provider that’s the best fit for your personality and needs.
This is especially important in therapy where treatment by someone who isn’t a specialist and/or a good fit for your personality could make you worse and prolong your suffering.
If how you think is one of the biggest predictors of how long you live, isn’t it worth the investment?
When you’re ready to invest in your health and mindset to get the happiness, success, and quality of life you want, please call us to schedule an appointment.
Please contact us to set up an appointment.
We can help give you information, a map for next steps, and hope that you can have the life you want.
Wishing you the best,
Dr. Levy
Director
Bucks County Anxiety Center
Dr. Ronit Levy is a clinical psychologist and director of Bucks County Anxiety Center in Newtown, PA. She specializes in treating teens and adults struggling with anxiety due to Anxiety Disorders, OCD, chronic illness, and life events. Dr. Levy trains and supervises other therapists and presents on mental health in the community.
When you do not need to pay for treatment and where to complain if they demand money - news
In Russia there is the concept of free medicine. This means that citizens do not have to pay anything from their wallet for some services. These treatment costs are paid by the state and insurance companies. All this is regulated by laws and programs that cannot be fully studied and understood by an ordinary person. Therefore, sometimes people pay for what they can get for free, wait longer than expected, or do not ask for help at all, although the budget allocates money for this.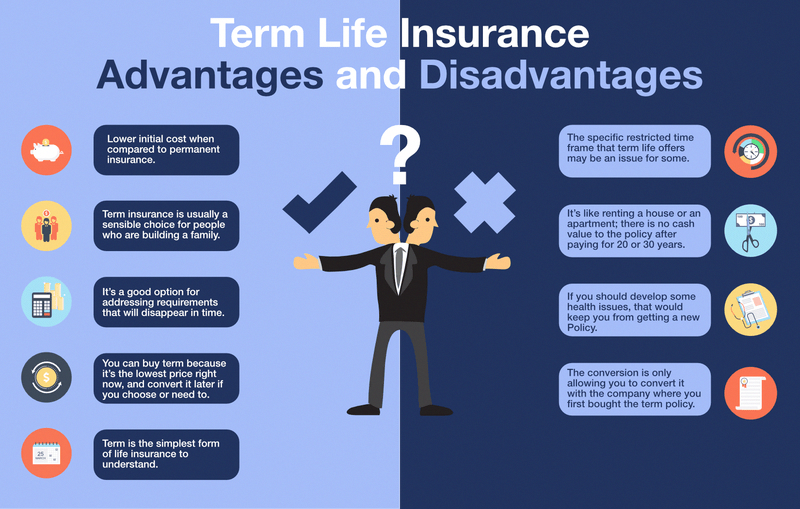 nine0003
nine0003
Source:
Ministry of Health leaflet
The Ministry of Health has issued a leaflet containing all the important things people need to know about treatment, money and protecting rights. The memo, although smaller than the law, is still large and not very clear. And there is not everything that is desirable to know. In ten years they will learn to speak human, but for now we will perform the rite of translation.
Ekaterina Miroshkina
economist
Author profile
There will be no yellow plate today
Read the entire article to be aware of your rights. As they say, the devil is in the details.
What kind of medical care is provided free of charge
Russia guarantees that it will provide you with some medical services free of charge. In fact, they are not free, but not people pay for them, but the budget and the health insurance fund.
To receive these services, you need to have a CHI policy: it confirms that you are insured and the state allocates money for your treatment. Sometimes a policy is not needed, but help will still be provided to everyone and for free. nine0003
Sometimes a policy is not needed, but help will still be provided to everyone and for free. nine0003
/oms/
How the CHI policy works
According to the law, you do not need to pay for these types of assistance:
- Consultations of general practitioners, pediatricians, general practitioners and narrow specialists.
- Prevention, diagnosis and treatment in hospital.
- Pregnancy and childbirth management, even if complex technologies are needed, IVF.
- High-tech medical care with unique treatments, cell technologies and robots.
- Ambulance for diseases, poisoning, injuries, accidents and acute conditions. nine0037 If necessary, medical evacuation is also free.
- Pain relief and relief from incurable diseases - outpatient and inpatient.
- Scheduled medical examinations and prophylaxis for adults and children, including tests.
- Medical rehabilitation.

- Chemotherapy, dialysis.
- Vaccinations according to the national calendar.
- Prescription and use of drugs in a hospital - but only from a special list.
- Auxiliary materials and therapeutic nutrition, if necessary for indications. nine0033
- Accommodation in a separate box, if necessary due to a diagnosis or epidemic.
- Meals and accommodation for parents if a child under 4 years old is admitted to the hospital. If the child is older, then it is free only if indicated - when the child cannot lie alone.
- Transportation of a patient accompanied by a health worker, if you need to go somewhere for treatment or diagnosis.
Never have to pay for emergency care. Even a private medical organization is obliged to provide it free of charge and without a policy. nine0038 If there is a threat to life, you can contact any medical institution - paid or free, at the place of registration or in another city. For refusing to save a person or if money is required for this - criminal liability.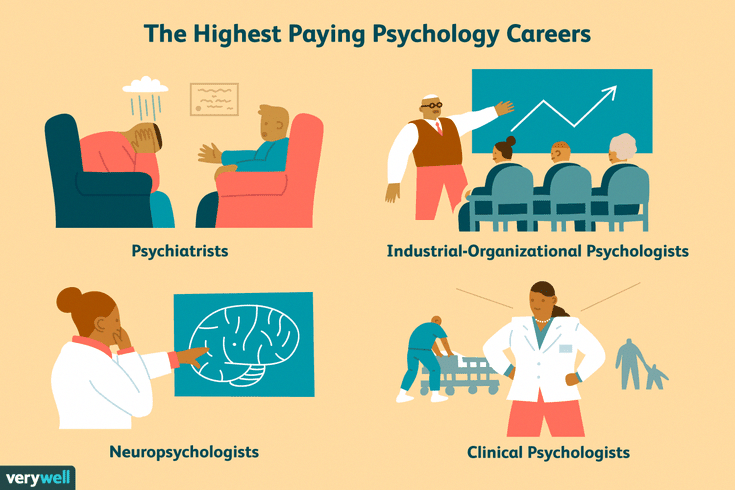
/kvota/
How to get a quota for an operation
Who is entitled to free medicines
In addition to consultations, treatment, diagnostics, screenings and surgeries, in some cases free medicines are entitled. But medicines are not issued in general upon any appeal, but, for example, only in a hospital, when an ambulance is called, or for specific diseases. If you apply for outpatient treatment, free medicines are provided for certain diagnoses, certain categories of patients, or you can buy them at a 50% discount. nine0003
Rules for prescribing drugs free of charge or at a discount
For example, children from large families, patients with tuberculosis, HIV, and police officers can receive free prescription drugs. There are also regional incentives.
How long do you have to wait until you get help
According to the urgency, medical care is divided into three types:
- Planned is prevention or treatment when nothing threatens life.
 For example, a medical examination or a preventive appointment with a dentist or an ophthalmologist. If a chronic disease worsens, this can also be planned assistance. nine0033
For example, a medical examination or a preventive appointment with a dentist or an ophthalmologist. If a chronic disease worsens, this can also be planned assistance. nine0033 - Emergency - a sudden exacerbation or acute condition, but still not life-threatening. For example, high fever, poisoning, high blood pressure, or an attack of pancreatitis.
- Emergency - if there is a threat to life. A person has a suspected heart attack, a stab wound, or a child does not get fever and convulsions.
/plastika-oms/
How to make an expensive CHI operation
Each type has its own waiting time. The maximum terms are set not by a polyclinic and not by a specific doctor, but by the law. If an ambulance travels for three hours during a heart attack, this is a violation. But you can wait for a tomography for two weeks - everything is according to the law. nine0111
planned 0
Poskovka, pediatrician or therapist
day after circulation
Narrow specialists
2 weeks
Diagnostics in the polyclinic: X -ray, mammography, ultrasound, ultrasound 9000 2 weeks 2 weeks 2 weeks 2 weeks for all - a month, for oncology - 2 weeks after the appointment
Complex operations, except for high-tech
for all - a month, for oncology - 2 weeks after diagnosis
Emergency
The patient turned to the clinic or hospital
2 hours after the circulation of
Emergency
caused an ambulance, there is a threat to
20 minutes, sometimes longer, taking into account the plugs, climate and features of the region
01010109 When to pay for treatment
Although medicine is free, sometimes you have to pay for help and treatment.
/teeth-cure-for-free/
How to treat your teeth in a private clinic for free
Optional. Because the budget doesn't pay for it or you want it faster. For example, you can come to a free clinic, get an appointment with a therapist or an endocrinologist at the expense of the budget, and take tests for a fee: so that at a convenient time, and not on a working day.
I would like to be treated for a fee. That is, going not to an ophthalmologist in your clinic, but to an advanced medical center with laser technology. And a child’s tooth is removed not by a coupon, but for a fee with anesthesia, toys and music. nine0003
Need better service. Services for money can be not only medical. For example, after a free operation or childbirth, you can ask for a paid ward.
This is not how the state treats. There is an order in the laws - how to provide medical care. With such a disease, they treat it like this, such procedures, these materials. If a patient wants to receive medical services in a different order, they can be offered for a fee. For example, you have to wait two weeks for a coupon to see an endocrinologist. If you pay, they can take faster. There is no violation here. Breaking the rules - for money. nine0003
Anonymous treatment. In order for the state to pay for an appointment, operation or medication, you need to know who applied for them. Hospitals report on each person and their treatment. If you want to keep your identity a secret from the state, you can pay. It is not possible to receive anonymous assistance under compulsory medical insurance, but you can encrypt personal data with a digital code.
No policy or citizenship. You must be insured to receive free assistance. A policy can also be issued without citizenship, but you can’t just come to a therapist at a clinic to check your eyesight. Without a policy, they will be accepted free of charge only in emergency cases. Policies are issued even to the unemployed, children and entrepreneurs. You don’t always have to pay fees for this, but the document itself needs to be drawn up. nine0003
Without a policy, they will be accepted free of charge only in emergency cases. Policies are issued even to the unemployed, children and entrepreneurs. You don’t always have to pay fees for this, but the document itself needs to be drawn up. nine0003
Visiting another clinic or hospital. Each person is assigned to some medical institution by registration or by personal choice. You can choose no more than once a year. But you can come to another clinic or not to your doctor at any time - for money.
Rules for paid medical services
What if doctors impose paid services?
Offering paid services, materials and examinations is not in itself a violation. By law, you can offer the patient to pay for expensive suture material if it heals better with it and does not need to be removed later. They will use Russian for free, and German for money. nine0003
But in this case, the patient must be given the whole scenario: he must understand that he will still not be left without stitches and anesthesia for free.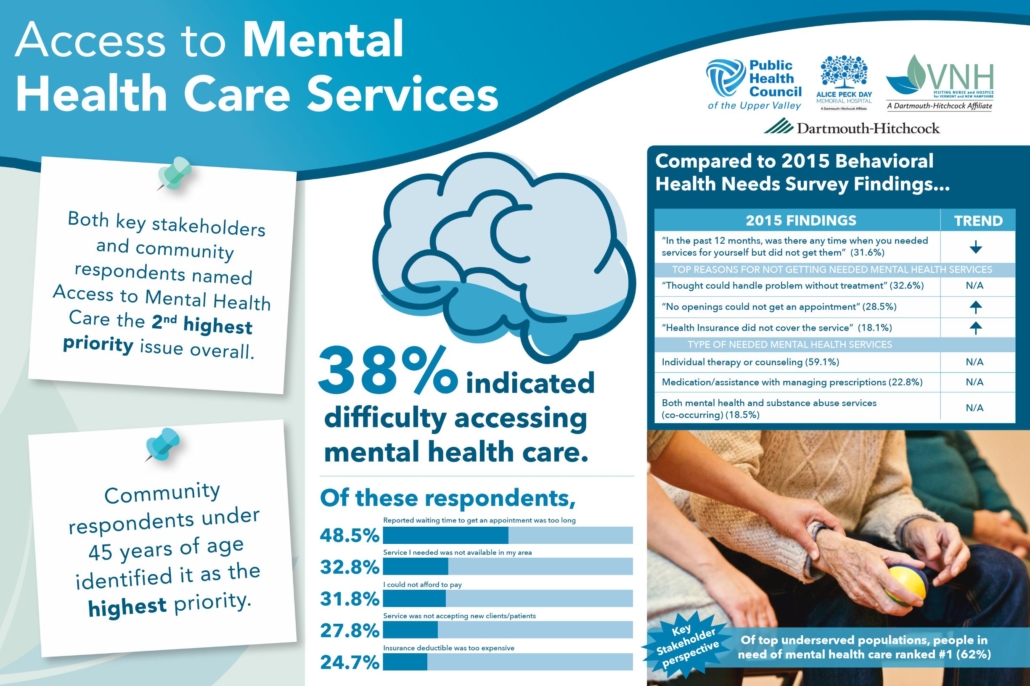 A doctor can offer something better, but not make you pay for the mere fact of treatment if it can be free by law. You can always refuse an offer to pay extra.
A doctor can offer something better, but not make you pay for the mere fact of treatment if it can be free by law. You can always refuse an offer to pay extra.
If the doctor is just charging services for money and hinting at poor treatment or delayed examinations without additional payment, you need to complain.
/patient-can/
What does the law say about doctors
Where to complain if they demand money?
If in a polyclinic or hospital they demand money from you for something they should do for free, write complaints:
- to the head of the department or the head physician;
- to the insurance company that issued the policy;
- to the health insurance fund or Roszdravnadzor;
- to the Ministry of Health;
- to court.
If you did not want to pay and because of this you were treated poorly, did not have the necessary tests, or were discharged from the hospital ahead of time, complain to Rospotrebnadzor. A public hospital patient is just as much a consumer of services as a client of a hairdresser, dry cleaner or language school. Your rights are protected by law. Compensation can be demanded for poor treatment from the hospital. But first, write a complaint to the hospital itself, that's the order. nine0003
A public hospital patient is just as much a consumer of services as a client of a hairdresser, dry cleaner or language school. Your rights are protected by law. Compensation can be demanded for poor treatment from the hospital. But first, write a complaint to the hospital itself, that's the order. nine0003
An amazing story 01.08.17
How one hospital failed to cure a child and paid the price
Who are insurance representatives and why are they needed?
If you have a policy, you are insured with a specific insurance company. She gets paid for it. And hospitals and clinics receive money from her.
Specially trained people should monitor how their clients are being treated, whether their rights are violated and whether they are demanding extra money from them. If something is not clear about treatment and payments, you can call the insurance company and sort it out. Sometimes representatives of insurance companies sit right in clinics.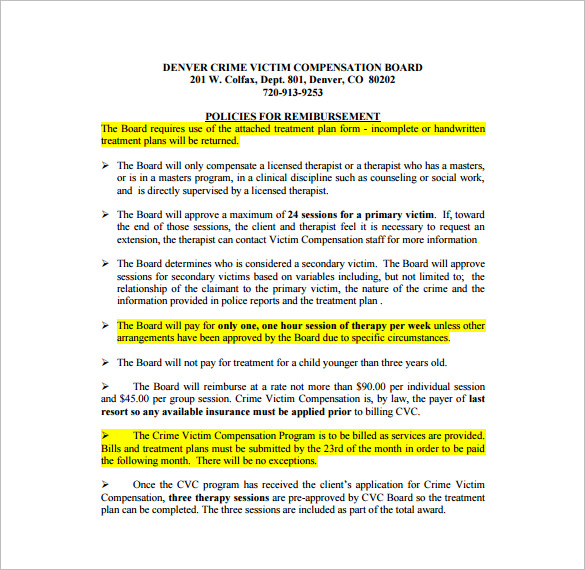 nine0003
nine0003
Here are some problems that an insurance representative can help you solve:
- You need to replace your policy.
- Want to join another polyclinic.
- Confused about the laws regarding medicine.
- There are complaints against doctors and the hospital.
- You want to have a medical examination, but don't know how.
- Complicated quota operation needed.
- You were treated badly or demanded money.
- They do not make an appointment with a narrow specialist, although there is a referral. nine0033
- You have to wait a long time for examinations, tests or surgery.
- They do not give out free medicines, although they are required to.
The telephone number of the insurance company is indicated on the policy. In any unclear situation, call them. You can directly from the doctor's office.
/analiz/
You are entitled to free tests under compulsory medical insurance
How to get an appointment with a doctor under the VHI policy?
Basics of insurance
If the insured has purchased a VHI policy, this does not mean that all issues related to obtaining medical care, which is provided for by insurance, are automatically resolved. After all, you still need to get to the doctor, and we will tell you how to do this in the article. nine0003
After all, you still need to get to the doctor, and we will tell you how to do this in the article. nine0003
07/26/19
2074
Share
What should I do if I need to see a doctor?
If the owner of the VHI policy has a need for medical care, then he should clearly understand why this can be done and where to go to pay for the service. The contract specifies:
- insured events;
- list of medical services; nine0033
- list of service medical institutions;
- procedure for the policyholder in the event of an insured event.
If the policyholder does not fully understand whether the case is insured, where, to whom and how he can apply, then it would be right to call the dispatcher of the insurance company for clarification.
A conscientious insurer will not fight back from the client, but will provide comprehensive information.
If the case falls into the category of insurance, the dispatcher will recommend the course of action necessary in order to get an appointment with a specialist in a medical institution. nine0003
Thus, before contacting a doctor, the owner of the VHI policy must be clearly aware of the following circumstances:
- insurance case;
- you can apply to such and such institutions;
- what is the procedure for making an appointment;
- how to pay for the service.
How to make an appointment?
You can make an appointment with a doctor through the registry of a medical institution or an online service, similar to how it is done under compulsory medical insurance. In this case, the patient must clarify that he wants to get an appointment under the VHI policy. If there are problems with the registry, then you need to contact the insurance company so that it settles the misunderstanding. nine0003
Another option is also possible - make an appointment with a doctor through an insurance company. In some cases, this can also be done online. Such an opportunity is provided, for example, on the RESO-Garantia website. The client indicates personal and contact data, VHI policy number, diagnosis (symptoms of the disease), information about the service he wants to receive, and the desired date of admission.
In some cases, this can also be done online. Such an opportunity is provided, for example, on the RESO-Garantia website. The client indicates personal and contact data, VHI policy number, diagnosis (symptoms of the disease), information about the service he wants to receive, and the desired date of admission.
What should I bring with me and what questions may arise at the appointment?
When contacting a medical institution, the patient must have a passport and a VHI policy. If the appeal is primary, then it is better to come in advance, since it will take time for the registry to issue a medical card. It must be taken with you to the doctor, as well as other medical documents. This may be a card of another medical institution, certificates, extracts from the medical history and other documents related to the subject of the appeal. nine0003
If during the appointment the doctor will offer the patient to pay for services and procedures, citing the fact that they are not included in the VHI policy, you should contact the insurance company.