Depression vitamins b12
Vitamin B12 Supplementation: Preventing Onset and Improving Prognosis of Depression
Cureus. 2020 Oct; 12(10): e11169.
Published online 2020 Oct 26. doi: 10.7759/cureus.11169
Monitoring Editor: Alexander Muacevic and John R Adler
,1,2,1,1 and 2
Author information Article notes Copyright and License information Disclaimer
Depression is a common mental health condition occurring across all ages, genders, and populations and is almost always multifaceted. It can manifest as a form of metabolic disorder, endocrine disorder, cardiovascular diseases, inflammatory disorders, deficiencies, or neurodegenerative disorders. Although there have been various treatment options available for the treatment of depression, it is still a sizable global health concern requiring more attention. This review article was produced by researching data and studies to prove a relationship between Vitamin B12 and depression.
Numerous studies were reviewed, and based on these studies, it was concluded that supplementation of Vitamin B12 early enough can delay the onset of depression and improve the effect of anti-depressants when used in conjunction with Vitamin B12. Although other vitamins like Vitamin B6 and folate are known to have an impact on depression, we have primarily focused on Vitamin B12 in an attempt to offer the providers a foundation to address this concern with their patients prone to depression or have had a major depressive episode in their life.
Keywords: serum vitamin b12, depression prevention, hyperhomocysteinemia, neuro-psychiatric
Over 264 million individuals suffer from depression across the world. Depression is one of the most commonly occurring mental health disorders occurring in adults and children [1]. The World Health Organization reported depression as one of the leading causes of disability worldwide [2].
The American Academy of Pediatrics' most recent guidelines states that depression screening is recommended to begin at as low as 12 years of age. It is a well-known fact that depression can become a serious medical condition, if long-lasting, and can affect the quality of life, reduce overall productivity, and lead to extreme thoughts known as suicidal ideation [1]. The most known causes of depression are external factors like abuse, death or loss, heredity, and medications. Over 17.3 million US adults, about 7.1% of the total population, have suffered from a minimum of one major depressive episode in their life. Figure shows the statistical data from 2017 outlining the prevalence of depression among adults in the United States.
It is a well-known fact that depression can become a serious medical condition, if long-lasting, and can affect the quality of life, reduce overall productivity, and lead to extreme thoughts known as suicidal ideation [1]. The most known causes of depression are external factors like abuse, death or loss, heredity, and medications. Over 17.3 million US adults, about 7.1% of the total population, have suffered from a minimum of one major depressive episode in their life. Figure shows the statistical data from 2017 outlining the prevalence of depression among adults in the United States.
Open in a separate window
Prevalence of Major Depressive Episodes Among US Adults
SAMHSA: Substance Abuse and Mental Health Services Administration; NH/OPI: Native Hawaiian/Other Pacific Islander; AI/AN: American Indian/Alaska Native
Depression is more prevalent in women and young adults aged 18-25 years of age [3], most likely reported due to emotional or psychological stress.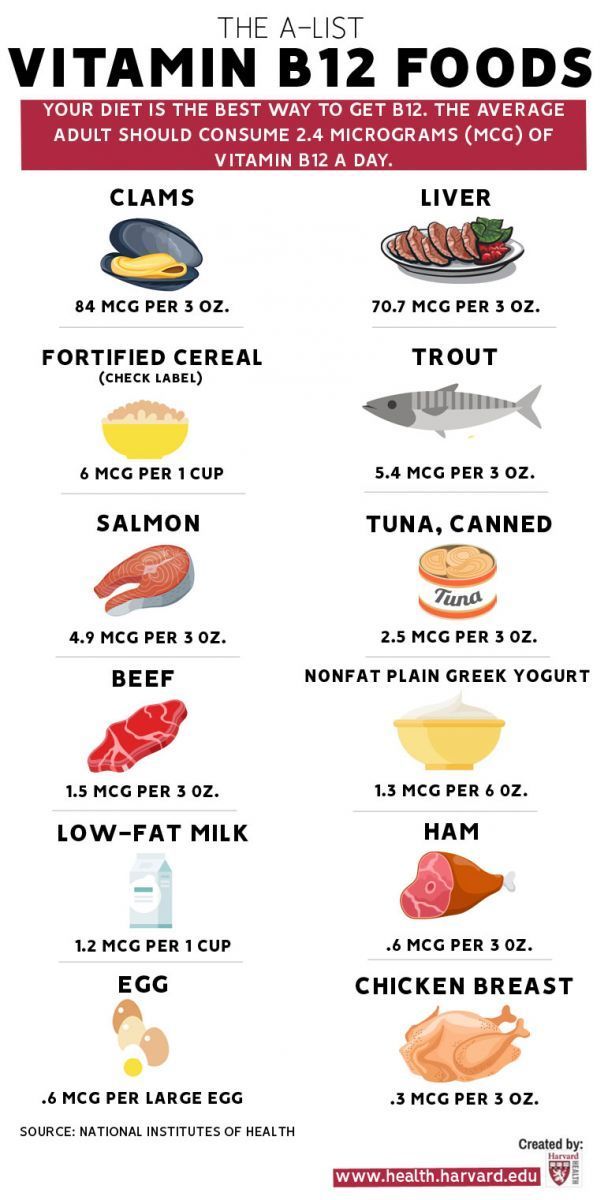 However, the completion of suicide attempts is more among men than women.
However, the completion of suicide attempts is more among men than women.
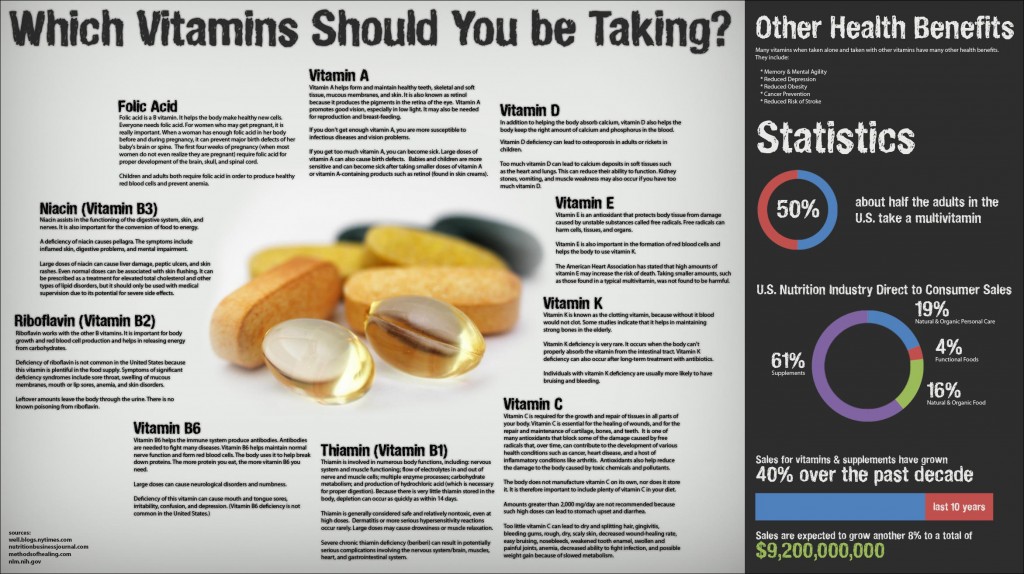
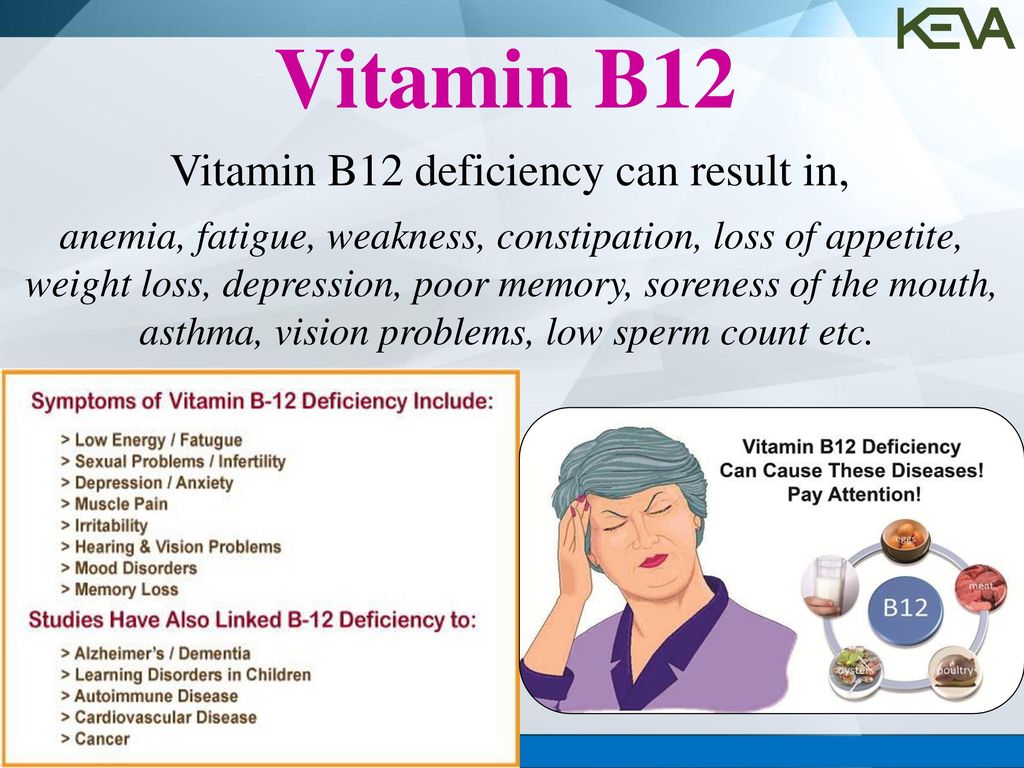
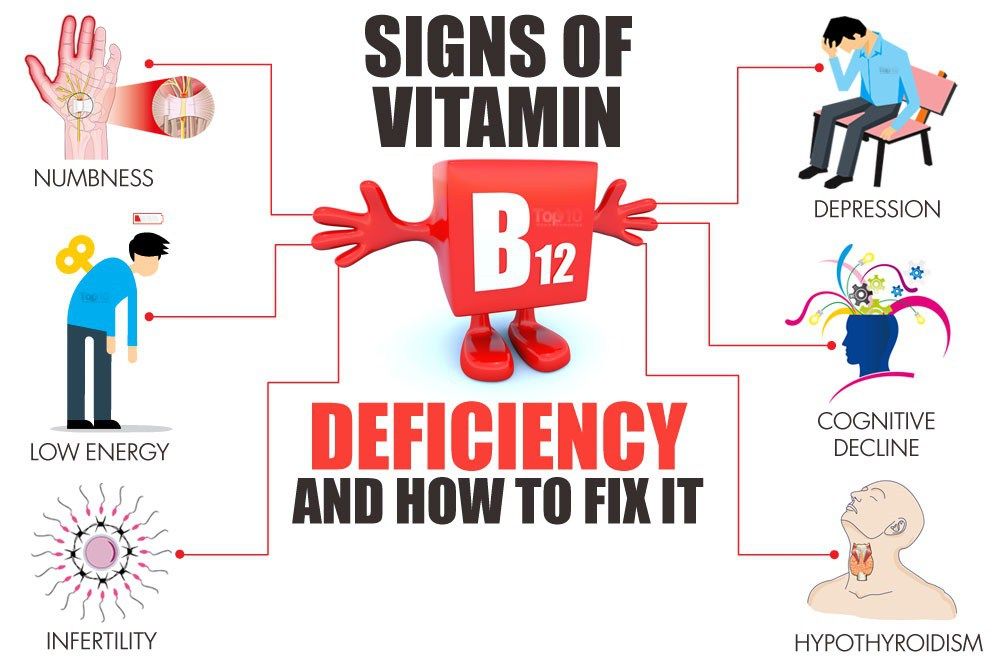
Vitamin B12 is a water-soluble vitamin synthesized by the bacteria present in the human body. It is predominantly acquired by the intake of meat products, and thus individuals with a vegetarian or vegan diet tend to be naturally deficient. Deficiency of this particular vitamin can lead to fatigue, weakness, constipation, balance issues, mental fogginess, peripheral tingling, depression, and cognitive issues [4,5].
Numerous studies are being performed to determine the relationship between Vitamin B12 and depression, and if supplementation of Vitamin B12 can slow the progression of depression or prevent it. So far, there has not been concrete evidence that shows the positive effects of Vitamin B12 supplementation in patients with or prone to depression. However, some studies have shown positive effects on patients with depression when supplementation of Vitamin B12 is implemented. Some clinical studies have shown that higher Vitamin B12 levels in the body resulted in better outcomes in patients suffering from depressive and other mental health disorders [6], whereas some studies have also stated that adolescents with borderline levels of serum Vitamin B12 levels develop cognitive changes requiring treatment [7].
Depression is a lifelong battle for the majority of the population across the world. Especially with the current situation in the world and the COVID-19 pandemic associated with lockdowns, loss of jobs, housing, and immigration statuses, the incidence of depression and other mental health disorders has significantly increased among children, adolescents, and adults, not being limited to a specific age group. This paper aims to find the effects of Vitamin B12 on depression with the help of other reviewed articles, in an attempt to allow providers to make evidence-based decisions to prevent and manage depression by merely supplementing individuals with Vitamin B12.
Our review focuses on the effects of Vitamin B12 supplementation at the onset or during the prognosis of depression. A total of 35 studies and articles were reviewed for this review [1-35]. We used PubMed and Google Scholar as our main databases to identify, screen, and choose the relevant articles. We chose the studies that were relevant to the topic and were published in English. We did not include gray literature or unpublished studies.
We did not include gray literature or unpublished studies.
Vitamin B12 and hyperhomocysteinemia
Micronutrients are known to affect the normal structure and functions of the brain. For this paper, we will be focusing on one specific micronutrient - Vitamin B12. Cyanocobalamin, also known as Vitamin B12, is one of the most important water-soluble vitamins. The primary functions of Vitamin B12 are appropriate red blood cell formation, neurological functioning, and DNA synthesis [8]. Deficiency of Vitamin B12 can result in hematological changes, neurological and psychiatric problems, which can manifest as irritability, changes in personality, depression, and memory loss [9]. It is also known to worsen depression by excitotoxic reactions caused by the accumulation of homocysteine [10].
Vitamin B12 deficiency is reportedly known to cause mental disturbances in numerous individuals. However, there is little evidence to show the correlation between psychosis and Vitamin B12. Cobalamin is one of the essential elements for monoamine neurotransmitter synthesis in the brain. A study published in 2011 in the Academy of Psychosomatic Medicine included supplementation of Vitamin B12 and folate, which resulted in improved cognitive functioning among patients participating in the study. A borderline Vitamin B12 level of 75-95 pg/mL, as well as up to a normal level of 307 pg/mL, is known to cause neuropsychiatric symptoms in patients, and such symptoms may start manifesting even with such borderline deficiencies or low normal levels of Vitamin B12. The study does dispute if the effects were of the Vitamin B12 supplementation or anti-depressant medications; however, it concludes that supplementation did increase the overall response to the anti-depressants [11].
A study published in 2011 in the Academy of Psychosomatic Medicine included supplementation of Vitamin B12 and folate, which resulted in improved cognitive functioning among patients participating in the study. A borderline Vitamin B12 level of 75-95 pg/mL, as well as up to a normal level of 307 pg/mL, is known to cause neuropsychiatric symptoms in patients, and such symptoms may start manifesting even with such borderline deficiencies or low normal levels of Vitamin B12. The study does dispute if the effects were of the Vitamin B12 supplementation or anti-depressant medications; however, it concludes that supplementation did increase the overall response to the anti-depressants [11].
Hyperhomocysteinemia
Higher homocysteine levels are associated with a phenomenon called "methionine loading." A deficiency of Vitamin B12 along with B6 and folate usually prevents the conversion of homocysteine to methionine, increasing the levels of homocysteine. Hyperhomocysteinemia can also occur in patients with renal disorders or genetic alterations of methyl-tetrahydro-folate reductase or cystathionine beta-synthetase, which are required for the metabolism of homocysteine [12,13]. Higher levels of homocysteine affect the DNA formation and overall turnover of red blood cells (RBCs), causing the development of megaloblastic or pernicious anemia, ultimately affecting the cognitive ability and mood of the patient [14-17]. Figure gives an overview of the various neurochemical pathways affected by Vitamin B12 levels, which ultimately leads to some form of depressive disorder or episode.
Higher levels of homocysteine affect the DNA formation and overall turnover of red blood cells (RBCs), causing the development of megaloblastic or pernicious anemia, ultimately affecting the cognitive ability and mood of the patient [14-17]. Figure gives an overview of the various neurochemical pathways affected by Vitamin B12 levels, which ultimately leads to some form of depressive disorder or episode.
Open in a separate window
Neurochemical Pathways Affected by Vitamin B12 Levels
Vitamin B12 is interdependent with other micronutrients, mainly Vitamin B6 and folate. This interdependence affects multiple neuronal pathways that are not directly controlled by Vitamin B12. Neurotransmitters are required to conduct the signals from one neuron to another, with the help of pre- and post-synaptic junctions. The malfunctioning of any of these pathways can lead to depression [4]. Lower Vitamin B12 levels are also known to increase the risk of cognitive decline, Alzheimer's disease, and dementia. According to Vogiatzoglou et al., higher Vitamin B12 levels have proven to protect patients against brain atrophy [18].
According to Vogiatzoglou et al., higher Vitamin B12 levels have proven to protect patients against brain atrophy [18].
Pathophysiology of depression
Over a decade ago, depression was commonly seen in adult and elderly patients but had become far more common among the younger population. According to the Journal of Psychological Medicine, the rates of depression have increased drastically among children as young as 12 years and older.
Depression, once diagnosed, is clinically treated with anti-depressants and cognitive behavioral therapy (CBT). In patients where the anti-depressant regimen is not eliciting a response, an additional drug from a different pharmaceutical group has proved to have a significant effect [19,20]. However, long-term and extensive pharmacotherapy are almost always associated with the extent of undesirable effects on the patient like the risk of major adverse cardiovascular events, decline in cognitive functioning over time, behavioral changes including but not limited to sexual problems, and feeling of "emotional numbness. " The B vitamins are crucial particulates of the 1-carbon metabolism wherein 5-methyltetrahydrofolate and methylcobalamin help convert homocysteine to methionine, which in turn forms S-adenosylmethionine (SAM), which is the essential methyl donor required for the production of monoamine neurotransmitters, phospholipids, and nucleotides [21].
" The B vitamins are crucial particulates of the 1-carbon metabolism wherein 5-methyltetrahydrofolate and methylcobalamin help convert homocysteine to methionine, which in turn forms S-adenosylmethionine (SAM), which is the essential methyl donor required for the production of monoamine neurotransmitters, phospholipids, and nucleotides [21].
A study performed in 2010 by Skarupski et al. included a sample US population of 35,053 older adults, and the results of this study stated that higher intakes of Vitamin B12 and B6 were associated with a lower risk of developing depressive symptoms by an average of 7.2 years [23]. According to Hutto, cobalamin and folate are components of the synthesis of monoamine neurotransmitters, which may lead to psychotic behavior by a rise in Bh5 (tetrahydrobiopterin) production [24]. Moorthy et al. published an article in the Journal of Nutrition in 2010, which discussed the C677T polymorphism of the methylenetetrahydrofolate reductase (MTHFR) gene in various ethnic groups.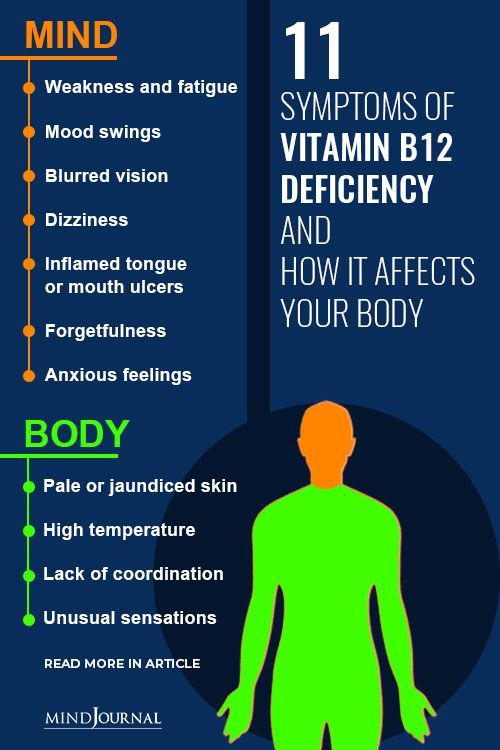 The study showed lesser scores on the Mini-Mental Status Exam (MMSE) and higher depression scores among patients with lower plasma levels of Vitamin B12 [25].
The study showed lesser scores on the Mini-Mental Status Exam (MMSE) and higher depression scores among patients with lower plasma levels of Vitamin B12 [25].
Daily supplementation of oral Vitamin B12 (100 mcg) and folic acid (400 mcg) has been shown to increase cognitive function in a randomized controlled trial performed by Walker et al. in 2012 [26]. They proposed two theories by which this could occur: reduced homocysteine levels and lowered vascular and metabolic risk factors occurring due to supplementation with Vitamin B12 and folic acid [26]. Another study performed in 2012, specifically among the Iranian population with major depressive disorders, also indicated lower plasma concentrations of Vitamin B12 among the Tabrizian patients who had depressive symptoms [27].
Melancholic depressive symptoms were more relatively associated with lower plasma Vitamin B12 levels. One such study reviewed concluded that Vitamin B12 deficiency played an important role in the pathogenesis of depressive symptoms [28]. A randomized controlled trial performed in 2013 among the Pakistani population attempted to identify the coexistence of depression and Vitamin B12 deficiency. This study reported that 22% of the sample depressed population had associated low Vitamin B12 levels to constitute a deficiency, 36% had low normal Vitamin B12 levels, and 42% of the sample population had normal serum B12 levels [29]. Vitamin B12, in combination with folic acid, is known to reduce the levels of homocysteine, thereby reducing the toxic effects and thus improving the effect of anti-depressants by increasing the effectiveness of anti-depressants S-adenosylmethionine (SAMe) [30]. A study performed among the Indian population in 2017 demonstrated that Vitamin B12-deficient individuals, mostly vegetarians, were more prone to developing neurological problems [31]. Figure illustrates the effects of Vitamin B12 deficiency on depression.
A randomized controlled trial performed in 2013 among the Pakistani population attempted to identify the coexistence of depression and Vitamin B12 deficiency. This study reported that 22% of the sample depressed population had associated low Vitamin B12 levels to constitute a deficiency, 36% had low normal Vitamin B12 levels, and 42% of the sample population had normal serum B12 levels [29]. Vitamin B12, in combination with folic acid, is known to reduce the levels of homocysteine, thereby reducing the toxic effects and thus improving the effect of anti-depressants by increasing the effectiveness of anti-depressants S-adenosylmethionine (SAMe) [30]. A study performed among the Indian population in 2017 demonstrated that Vitamin B12-deficient individuals, mostly vegetarians, were more prone to developing neurological problems [31]. Figure illustrates the effects of Vitamin B12 deficiency on depression.
Open in a separate window
Pathophysiology of Depression
The total cyanocobalamin and methylcobalamin levels in patients with autism and schizophrenia were reported to be lower as compared to the age-matched control subjects.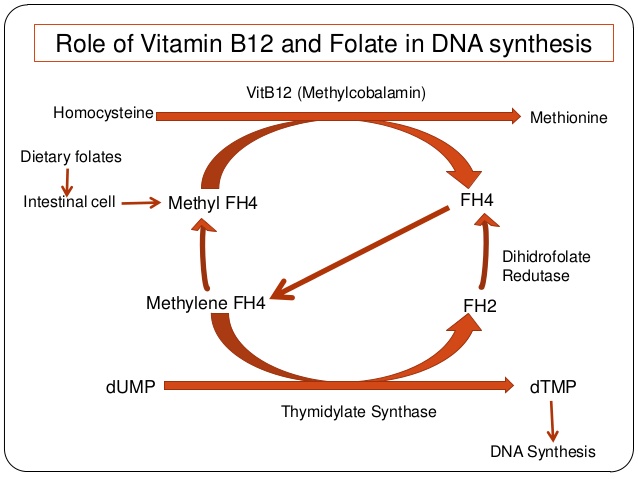 Although the association with the levels and depression was not performed, the study analyzed brain samples [22]. It concluded Vitamin B12-dependent methylation reactions in the brain played a crucial role in the presentation of neurological symptoms and disorders [22]. A cross-sectional study was performed in 2018 to understand the association between vitamins and depression to gather data more based explicitly on sex-specific criteria; evidently, females were identified to be more at risk as compared to men and had coinciding lower serum Vitamin B12 levels [32]. Low normal serum Vitamin B12 is also posing a risk to pregnant women and makes them more prone to develop depressive symptoms. According to a secondary analysis of the National Health and Nutrition Examination Survey and a reported Patient Health Questionnaire-9 (PHQ-9) score of 10 or more among the subjects, pregnant women were reported to be 3.82 times more predisposed to developing depression [33].
Although the association with the levels and depression was not performed, the study analyzed brain samples [22]. It concluded Vitamin B12-dependent methylation reactions in the brain played a crucial role in the presentation of neurological symptoms and disorders [22]. A cross-sectional study was performed in 2018 to understand the association between vitamins and depression to gather data more based explicitly on sex-specific criteria; evidently, females were identified to be more at risk as compared to men and had coinciding lower serum Vitamin B12 levels [32]. Low normal serum Vitamin B12 is also posing a risk to pregnant women and makes them more prone to develop depressive symptoms. According to a secondary analysis of the National Health and Nutrition Examination Survey and a reported Patient Health Questionnaire-9 (PHQ-9) score of 10 or more among the subjects, pregnant women were reported to be 3.82 times more predisposed to developing depression [33].
One-carbon metabolism has been extensively linked with psychiatric disorders among numerous studies. One such recent study published in 2020 comprised of 89 patients, mainly children and adolescents, and included a patient group that was already diagnosed with depression and a control group. They were subsequently tested for serum levels of Vitamin B12, homocysteine, and Vitamin D. The study utilized correlation analysis and showed a negative relationship between the severity of depressive symptoms and Vitamin B12, and associated hyperhomocysteinemia, concluding that low normal levels or deficiency of Vitamin B12 can become a significant contributing factor toward depression [34]. Case-control studies performed have yielded similar results; however, the sample population has been limited, which necessitates studies comprising larger population groups. Patients diagnosed with depression are highly likely to be non-compliant, thus suggesting better ways of managing and overcoming the non-compliant behavior, which also goes hand in hand with improper dietary intake of essential nutrients.
One such recent study published in 2020 comprised of 89 patients, mainly children and adolescents, and included a patient group that was already diagnosed with depression and a control group. They were subsequently tested for serum levels of Vitamin B12, homocysteine, and Vitamin D. The study utilized correlation analysis and showed a negative relationship between the severity of depressive symptoms and Vitamin B12, and associated hyperhomocysteinemia, concluding that low normal levels or deficiency of Vitamin B12 can become a significant contributing factor toward depression [34]. Case-control studies performed have yielded similar results; however, the sample population has been limited, which necessitates studies comprising larger population groups. Patients diagnosed with depression are highly likely to be non-compliant, thus suggesting better ways of managing and overcoming the non-compliant behavior, which also goes hand in hand with improper dietary intake of essential nutrients. Khosravi et al. performed a case-control study to identify the correlation between increased and decreased intake of Vitamin B12 and folate with depression and its severity. An inversely proportional relationship was established between Vitamin B12 and folate levels and depression [35]. Table gives a snapshot of the studies reviewed for this article along with their results.
Khosravi et al. performed a case-control study to identify the correlation between increased and decreased intake of Vitamin B12 and folate with depression and its severity. An inversely proportional relationship was established between Vitamin B12 and folate levels and depression [35]. Table gives a snapshot of the studies reviewed for this article along with their results.
Table 1
Effects of Vitamin B12 on Depressive Symptoms
SSRI: Selective serotonin reuptake inhibitor
| Author | Year of Publication | Purpose of the Study | Results/Conclusion |
| Skarupski et al. [23] | 2010 | To determine if Vitamin B12 or B6 intake affected the onset of depressive symptoms | Higher intakes of both Vitamins B12 and B6 reduced depressive symptoms over time. |
| Walker et al. [26] | 2012 | To identify if folic acid and Vitamin B12 supplementation prevented cognitive decline | Long-term supplementation improved cognitive functioning |
| Gargari et al. [27] | 2012 | To assess nutritional status in patients with major depressive disorders | Vitamin B12 and folate levels were markedly lower among identified patients |
| Seppälä et al. [28] | 2013 | To identify a relationship between Vitamin B12 levels and depressive symptoms | Vitamin B12 levels were reported to be correlated with melancholic depressive symptoms more than non-melancholic. |
Syed et al.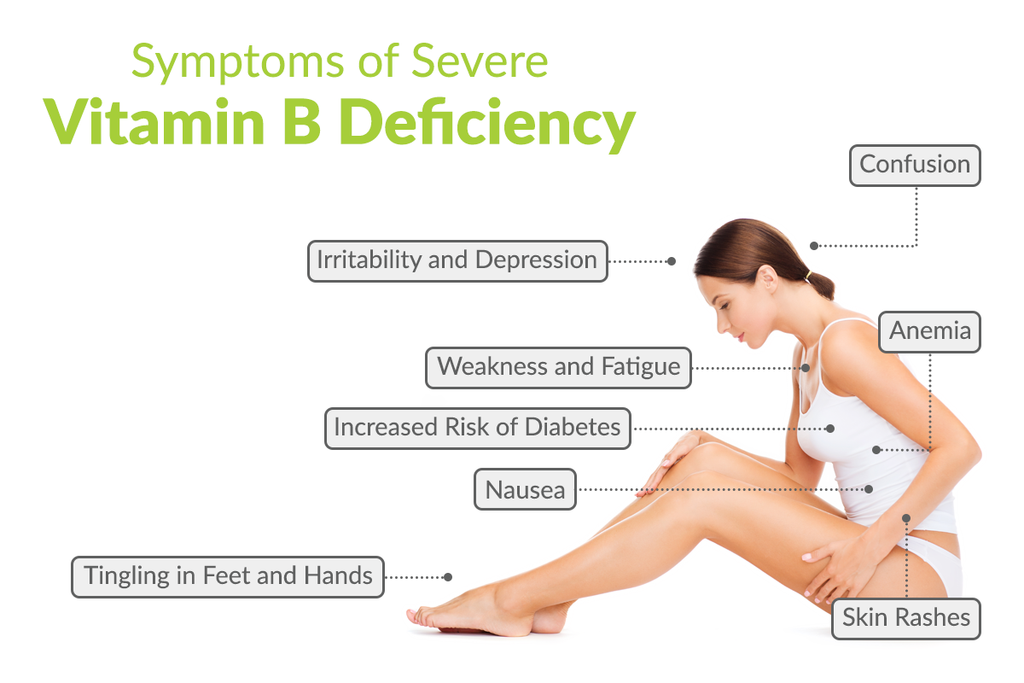 [29] [29] | 2013 | To compare the response of SSRI monotherapy vs. B12 augmentation in patients with depression | Supplementation of Vitamin B12 along with anti-depressant therapy greatly improved depressive symptoms. |
| Peppard et al. [33] | 2019 | To identify the risk of depression in pregnant women | The study stated that women during the antenatal period with low normal Vitamin B12 levels were 3.82 times more prone to develop depression. |
Open in a separate window
Among the numerous articles reviewed for this topic, the majority of them proposed that Vitamin B12 levels are related to the severity of depression. Although this topic lacks tangible and sizable data to prove the same, healthcare providers need to take into consideration the studies reviewed in this paper and utilize them to test the effects of Vitamin B12 supplementation in patients with neuropsychiatric disorders.
Limitations
The limitations of this topic are that the studies that have been reviewed for this paper have had relatively smaller sample population sizes. There is still a need for more research with a larger sample size to find more concrete evidence of the positive effects of Vitamin B12 on depression.
In this article, we reviewed over 30 to 40 published articles and studies to understand the correlation between the supplementation of Vitamin B12 and the prognosis of depression. Based on the reviewed studies, it was found that although there is no concrete evidence showing positive effects of Vitamin B12 on depression or depressive symptoms, the lower levels of Vitamin B12 in the body are associated with a higher risk of developing depression. Routine testing for plasma Vitamin B12 levels can be recommended for patients across the board beginning at the adolescent age to prevent the population from developing depression or other forms of cognitive under-functioning, which may lead to depression.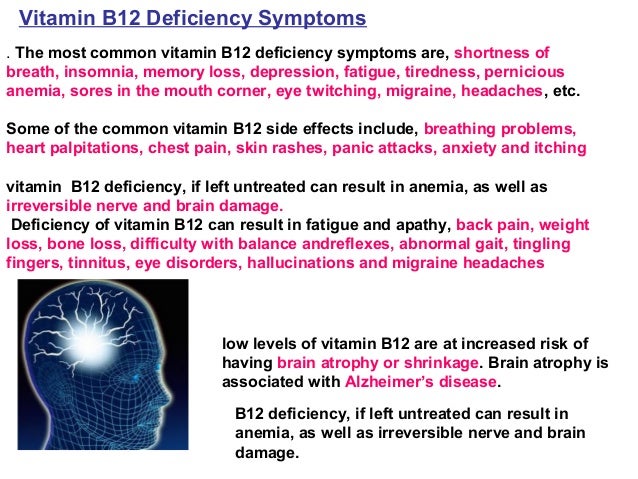 Low normal levels of Vitamin B12 should be recommended to be evaluated for symptoms of Vitamin B12 deficiency, including any neurological manifestations, as these symptoms can present even when the levels are within a normal range. However, additional studies with larger population groups should be done to formulate an evidence-based criterion for providers to adapt across the world.
Low normal levels of Vitamin B12 should be recommended to be evaluated for symptoms of Vitamin B12 deficiency, including any neurological manifestations, as these symptoms can present even when the levels are within a normal range. However, additional studies with larger population groups should be done to formulate an evidence-based criterion for providers to adapt across the world.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.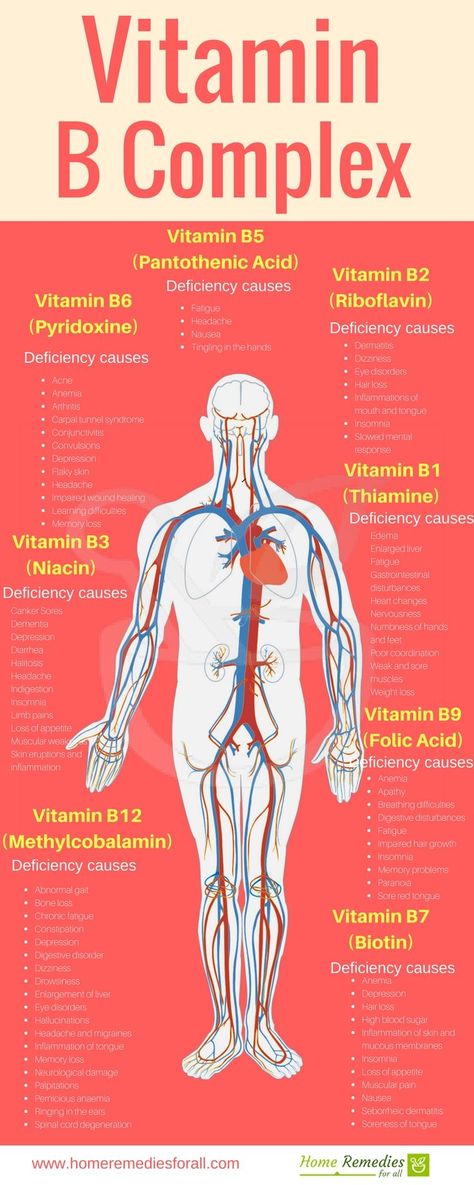
1. Depression. [Sep;2020 ];https://www.who.int/news-room/fact-sheets/detail/depression 2020
2. Depression in the United States household population, 2005-2006. [Sep;2020 ];Pratt L, Brody D. https://www.cdc.gov/nchs/data/databriefs/db07.pdf 2008
3. Major depression. [Sep;2020 ];https://www.nimh.nih.gov/health/statistics/major-depression.shtml 2017
4. The effects of vitamin B in depression. Mikkelsen K, Stojanovska L, Apostolopoulos V. Curr Med Chem. 2016;23:4317–4337. [PubMed] [Google Scholar]
5. The prevalence of cobalamin deficiency among vegetarians assessed by serum vitamin B12: a review of literature. Pawlak R, Lester SE, Babatunde T. Eur J Clin Nutr. 2014;68:541–548. [PubMed] [Google Scholar]
6. High vitamin B12 level and good treatment outcome may be associated in major depressive disorder. Hintikka J, Tolmunen T, Tanskanen A, Viinamäki H. BMC Psychiatry. 2003;3:17. [PMC free article] [PubMed] [Google Scholar]
7. Signs of impaired cognitive function in adolescents with marginal cobalamin status.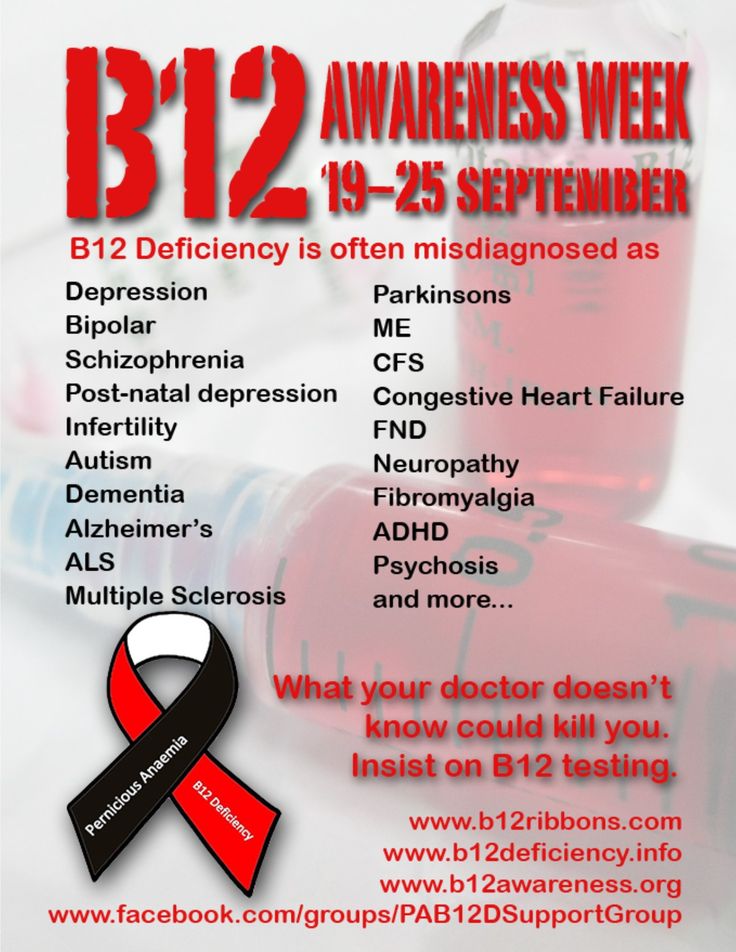 Louwman MW, van Dusseldorp M, van de Vijver FJ, et al. Am J Clin Nutr. 2000;72:762–769. [PubMed] [Google Scholar]
Louwman MW, van Dusseldorp M, van de Vijver FJ, et al. Am J Clin Nutr. 2000;72:762–769. [PubMed] [Google Scholar]
8. Folate and vitamin B-12 status in relation to anemia, macrocytosis, and cognitive impairment in older Americans in the age of folic acid fortification. Morris MS, Jacques PF, Rosenberg IH, Selhub J. Am J Clin Nutr. 2007;85:193–200. [PMC free article] [PubMed] [Google Scholar]
9. Vitamin B12 deficiency. Oh R, Brown DL. https://pubmed.ncbi.nlm.nih.gov/12643357/ Am Fam Physician. 2003;67:979–986. [PubMed] [Google Scholar]
10. Clinical spectrum and diagnosis of cobalamin deficiency. Stabler SP, Allen RH, Savage DG, Lindenbaum J. https://pubmed.ncbi.nlm.nih.gov/2393714/ Blood. 1990;76:871–881. [PubMed] [Google Scholar]
11. Acute psychotic depression as a sole manifestation of vitamin B12 deficiency. Bar-Shai M, Gott D, Marmor S. Psychosomatics. 2011;52:384–386. [PubMed] [Google Scholar]
12. Homocysteine, renal function, and risk of cardiovascular disease. Clarke R, Lewington S, Landray M. Kidney Int Suppl. 2003;63:131. [PubMed] [Google Scholar]
Clarke R, Lewington S, Landray M. Kidney Int Suppl. 2003;63:131. [PubMed] [Google Scholar]
13. The kidney and homocysteine metabolism. Friedman AN, Bostom AG, Selhub J, Levey AS, Rosenberg IH. https://pubmed.ncbi.nlm.nih.gov/11562419/ J Am Soc Nephrol. 2001;12:2181–2189. [PubMed] [Google Scholar]
14. Folic acid with or without vitamin B12 for cognition and dementia. Malouf M, Grimley EJ, Areosa SA. Cochrane Database Syst Rev. 2003 [PubMed] [Google Scholar]
15. Folate, vitamin B12 and vitamin B6 and one carbon metabolism. Selhub J. https://pubmed.ncbi.nlm.nih.gov/11813080/ J Nutr Health Aging. 2002;6:39–42. [PubMed] [Google Scholar]
16. Vitamin B6, B12, and folic acid supplementation and cognitive function: a systematic review of randomized trials. Balk EM, Raman G, Tatsioni A, Chung M, Lau J, Rosenberg IH. Arch Intern Med. 2007;167:21–30. [PubMed] [Google Scholar]
17. Homocysteine and folate metabolism in depression. Bottiglieri T. Prog Neuropsychopharmacol Biol Psychiatry.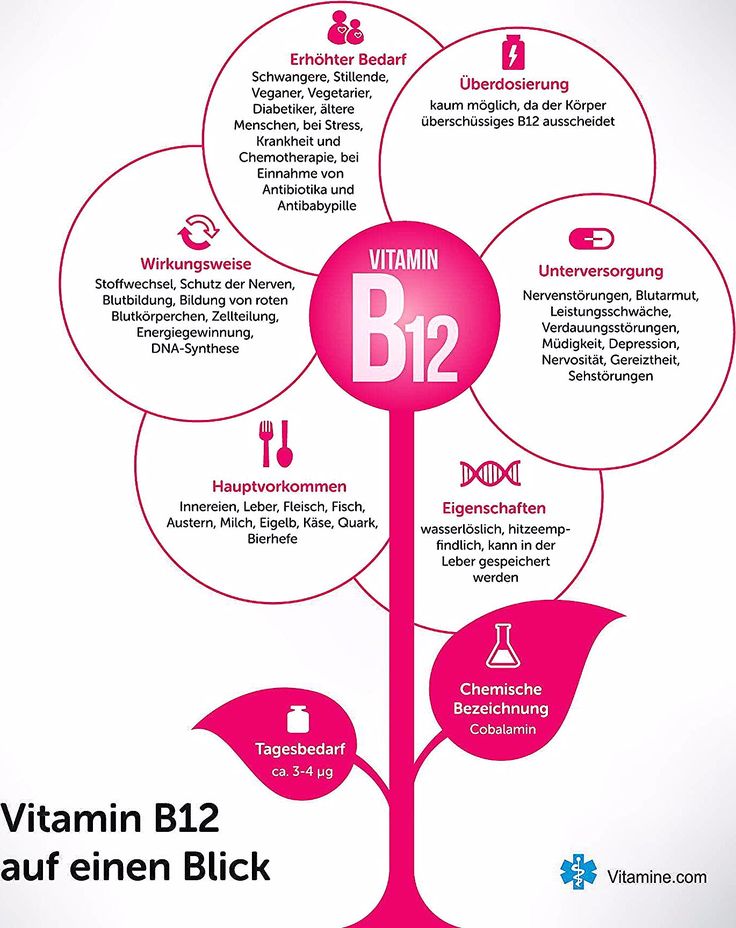 2005;29:1103–1112. [PubMed] [Google Scholar]
2005;29:1103–1112. [PubMed] [Google Scholar]
18. Vitamin B12 status and rate of brain volume loss in community-dwelling elderly. Vogiatzoglou A, Refsum H, Johnston C, et al. Neurology. 2008;71:826–832. [PubMed] [Google Scholar]
19. Pharmacological augmentation in unipolar depression: a guide to the guidelines [IN PRESS] Taylor RW, Marwood L, Oprea E, et al. Int J Neuropsychopharmacol. 2020 [PMC free article] [PubMed] [Google Scholar]
20. Efficacy of adding nutritional supplements in unipolar depression: a systematic review and meta-analysis. Schefft C, Kilarski LL, Bschor T, Köhler S. Eur Neuropsychopharmacol. 2017;27:1090–1109. [PubMed] [Google Scholar]
21. B-vitamins in relation to depression in older adults over 60 years of age: the Trinity Ulster Department of Agriculture (TUDA) Cohort Study. Moore K, Hughes CF, Hoey L, et al. J Am Med Dir Assoc. 2019;20:551–557. [PubMed] [Google Scholar]
22. Decreased brain levels of vitamin B12 in aging, autism and schizophrenia. Zhang Y, Hodgson NW, Trivedi MS, et al. PLoS One. 2016;11:146797. [PMC free article] [PubMed] [Google Scholar]
Zhang Y, Hodgson NW, Trivedi MS, et al. PLoS One. 2016;11:146797. [PMC free article] [PubMed] [Google Scholar]
23. Longitudinal association of vitamin B-6, folate, and vitamin B-12 with depressive symptoms among older adults over time. Skarupski KA, Tangney C, Li H, Ouyang B, Evans DA, Morris MC. Am J Clin Nutr. 2010;92:330–335. [PMC free article] [PubMed] [Google Scholar]
24. Folate and cobalamin in psychiatric illness. Hutto BR. Compr Psychiatry. 1997;38:305–314. [PubMed] [Google Scholar]
25. Status of vitamins B-12 and B-6 but not of folate, homocysteine, and the methylenetetrahydrofolate reductase C677T polymorphism are associated with impaired cognition and depression in adults. Moorthy D, Peter I, Scott TM, et al. J Nutr. 2012;142:1554–1560. [PMC free article] [PubMed] [Google Scholar]
26. Oral folic acid and vitamin B-12 supplementation to prevent cognitive decline in community-dwelling older adults with depressive symptoms--the Beyond Ageing Project: a randomized controlled trial.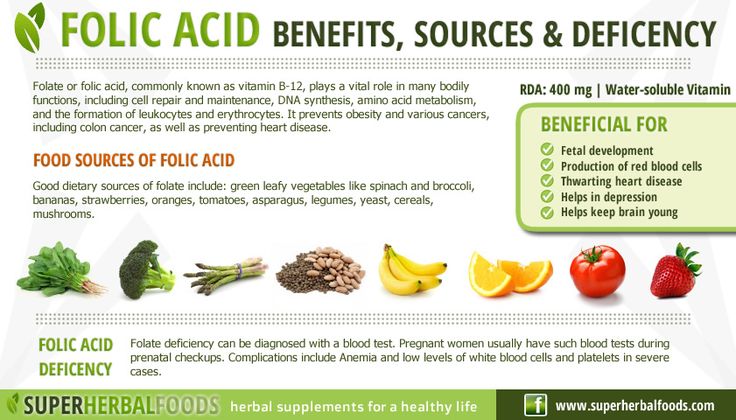 Walker JG, Batterham PJ, Mackinnon AJ, et al. Am J Clin Nutr. 2012;95:194–203. [PubMed] [Google Scholar]
Walker JG, Batterham PJ, Mackinnon AJ, et al. Am J Clin Nutr. 2012;95:194–203. [PubMed] [Google Scholar]
27. Nutritional status in patients with major depressive disorders: a pilot study in Tabriz, Iran. Gargari BP, Saboktakin M, Mahboob S, Pourafkari N. Health Promot Perspect. 2012;28:145–152. [PMC free article] [PubMed] [Google Scholar]
28. Association between vitamin b12 levels and melancholic depressive symptoms: a Finnish population-based study. Seppälä J, Koponen H, Kautiainen H, et al. BMC Psychiatry. 2013;13:145. [PMC free article] [PubMed] [Google Scholar]
29. Vitamin B12 supplementation in treating major depressive disorder: a randomized controlled trial. Syed EU, Wasay M, Awan S. Open Neurol J. 2013;7:44–48. [PMC free article] [PubMed] [Google Scholar]
30. The role of nutrients in protecting mitochondrial function and neurotransmitter signaling: implications for the treatment of depression, PTSD, and suicidal behaviors. Du J, Zhu M, Bao H, et al. Crit Rev Food Sci Nutr. 2016;56:2560–2578. [PMC free article] [PubMed] [Google Scholar]
2016;56:2560–2578. [PMC free article] [PubMed] [Google Scholar]
31. Neuropsychiatric and neurological problems among vitamin B12 deficient young vegetarians. Kapoor A, Baig M, Tunio SA, Memon AS, Karmani H. Neurosciences (Riyadh) 2017;22:228–232. [PMC free article] [PubMed] [Google Scholar]
32. Association between serum vitamin levels and depression in US adults 20 years or older based on national health and nutrition examination survey 2005-2006. Huang X, Fan Y, Han X, et al. Int J Environ Res Public Health. 2018;32:1215. [PMC free article] [PubMed] [Google Scholar]
33. Risk of depression in pregnant women with low-normal serum vitamin B12. Peppard L, Oh KM, Gallo S, Milligan R. Res Nurs Health. 2019;42:264–272. [PubMed] [Google Scholar]
34. The relationship of severity of depression with homocysteine, folate, vitamin B12, and vitamin D levels in children and adolescents [IN PRESS] Esnafoglu E, Ozturan DD. Child Adolesc Ment Health. 2020 [PubMed] [Google Scholar]
35. The relationship between dietary patterns and depression mediated by serum levels of folate and vitamin B12. Khosravi M, Sotoudeh G, Amini M, Raisi F, Mansoori A, Hosseinzadeh M. BMC Psychiatry. 2020;20:63. [PMC free article] [PubMed] [Google Scholar]
The relationship between dietary patterns and depression mediated by serum levels of folate and vitamin B12. Khosravi M, Sotoudeh G, Amini M, Raisi F, Mansoori A, Hosseinzadeh M. BMC Psychiatry. 2020;20:63. [PMC free article] [PubMed] [Google Scholar]
Vitamin B12 Supplementation in Treating Major Depressive Disorder: A Randomized Controlled Trial
Open Neurol J. 2013; 7: 44–48.
Published online 2013 Nov 15. doi: 10.2174/1874205X01307010044
,2,1,* and 1,*
Author information Article notes Copyright and License information Disclaimer
Background/Objective:
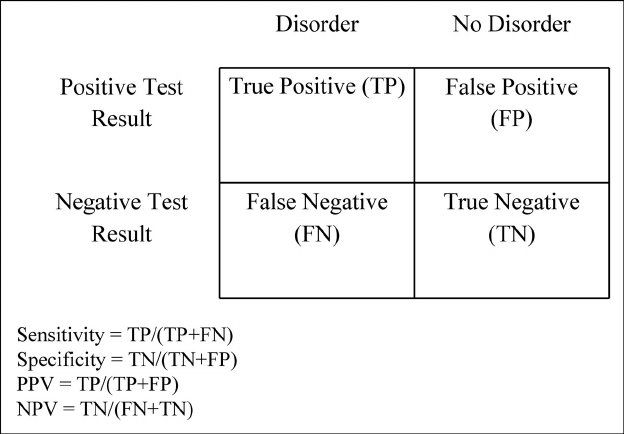
Recent literature has identified links between vitamin B12 deficiency and depression.We compared the clinical response of SSRI-monotherapy with that of B12-augmentation in a sample of depressed patients with low normal B12 levels who responded inadequately to the first trial with the SSRIs.
Methods:
Patients with depression and low normal B12 levels were randomized to a control arm (antidepressant only) or treatment arm (antidepressants and injectable vitamin B12 supplementation).
Results:
A total of 199 depressed patients were screened. Out of 73 patients with low normal B12 levels 34 (47%) were randomized to the treatment group while 39 (53%) were randomized to the control arm. At three months follow up 100% of the treatment group showed at least a 20% reduction in HAM-D score, while only 69% in the control arm showed at least a 20% reduction in HAM-D score (p<0.001). The findings remained significant after adjusting for baseline HAM-D score (p=0.001).
Conclusion:
Vitamin B12 supplementation with antidepressants significantly improved depressive symptoms in our cohort.
Keywords: Depression, vitamin B12, antidepressants, RCT.
Major Depressive Disorder is an important global public health problem associated with the significant burden and is projected to be the second leading cause of disability by 2020 [1]. Prevalence figures worldwide range between 4.2 – 17% and a systematic review of studies from Pakistan gave the estimates as high as 34% for anxiety and depressive disorders [2]. Clinical guidelines recommend the use of SSRIs as first-line treatment [3]. Remission rates in the acute phase of treatment are 30-40% and an overall 30% show poor response to anti-depressant monotherapy [4-6]. In such cases, addressing other co-morbid conditions is suggested in addition to upgrading or augmenting anti-depressant doses [3].
Clinical guidelines recommend the use of SSRIs as first-line treatment [3]. Remission rates in the acute phase of treatment are 30-40% and an overall 30% show poor response to anti-depressant monotherapy [4-6]. In such cases, addressing other co-morbid conditions is suggested in addition to upgrading or augmenting anti-depressant doses [3].
Pakistan, a developing country of 17 million people, is fraught with poverty, inadequate nutrition and underprivileged health systems. Several small-case studies from Pakistan show vitamin deficiencies to be common [7,8]. A small study from Islamabad on a clinical population of patients with megaloblastic anemia reported figures of 76% with vitamin B12 deficiency [9]. Although no large scale studies on general population are available here, studies from neighboring countries that share the culture and climate show vitamin deficiencies to be common [10-12]. A study on a healthy Indian population showed the prevalence of B12 deficiency to be 47% [13].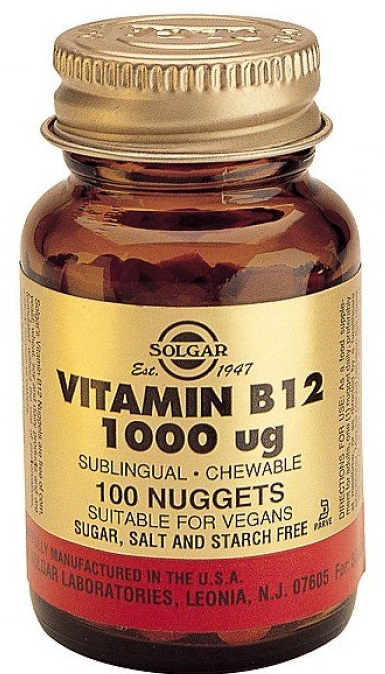
Vitamin B12 plays an important role in DNA synthesis and neurological function. Its deficiency is associated with hematological, neurological and psychiatric manifestations of which the latter includes irritability, personality change, depression, dementia and rarely, psychosis [14]. Recent literature has identified the links between this vitamin deficiency and depression. High B12 levels in serum are associated with good treatment response, high homocysteine levels which are common in folate / B12 deficiency and in those suffering from depression are associated with poor response to anti depressant treatment [15-17]. Hyperhomocysteinemia may have direct effects on neurotransmitters implicated in depression [18].
Randomized trials have shown that folate and other nutritional supplementations have a significant effect in treating the treatment-resistant depression [19,20]. Folate deficiency has also been linked with the delay in treatment response as well as relapse [21,22].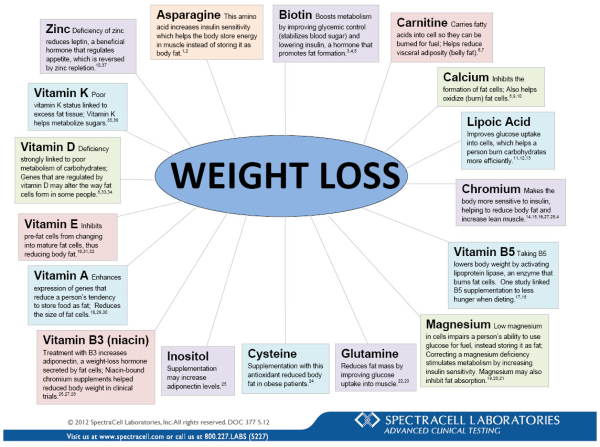
To date no adequately designed trial compares anti-depressant monotherapy with B12 augmentation. We aimed to compare the clinical response of antidepressants monotherapy with that of B12-augmentation in a sample of depressed patients with low normalB12 levels (190 pg/ml to 300 pg/ml).
The study was designed as an open label randomized controlled trial (clinical trials registration number (Clinical Trials.gov ID {"type":"clinical-trial","attrs":{"text":"NCT00939718","term_id":"NCT00939718"}}NCT00939718). Patients were enrolled from outpatient clinics of the department of Psychiatry at Aga Khan University Hospital, Karachi Pakistan from December 2009 - June 2010. Depression was defined as Patients scoring ≥ 16 on the 20-item Hamilton Rating Scale for Depression-Urdu version (HAM-D) [23,24].
Low normal B12 level was defined as B12 level ranging between 190 and 300 pg/ml. Patients with B12 deficiency (level below190 pg/ml) were not enrolled due to ethical reasons (patients with established B12 deficiency must be treated and not subjected to randomization).
Ethics Statement
A study protocol was approved by the Ethics Review Committee of Aga Khan University hospital. All patients signed an informed consent form.
Randomization and Masking
Patients with depression and low normal B12 levels were randomized by a computer program into the control arm (antidepressants only) or treatment arm (antidepressants and injectable vitamin B12 supplementation). The randomization was carried out using a Microsoft Excel spreadsheet using the function “RAND” to generate uniform random numbers.
The randomized assignment was determined by partitioning the range of the random number. Randomization was not concealed for investigators. Antidepressants that were prescribed included either a tricyclic antidepressant (TCA) with a dose equivalent of imipramine 100 mg to 250 mg/ day and the SSRIs dose equivalent of Fluoxetine 20 – 40 mg/day. Patients with concurrent unstable medical illness, history of manic episodes or psychotic illness, psychotic symptoms in a depressive episode, concurrent substance misuse and patients with suicidal ideation were excluded. Participants in the control arm only received the antidepressants. Those in the treatment arm received B12 intramuscular injectable as 1000 mcg every week during the 6 weeks in addition to the antidepressants.
Participants in the control arm only received the antidepressants. Those in the treatment arm received B12 intramuscular injectable as 1000 mcg every week during the 6 weeks in addition to the antidepressants.
Any adverse effects of oral medications and injections (B12) were monitored and documented on an adverse effects sheet in the patient folder.
A decline in HAM-D score of 20% or more from the baseline, indicating an improvement in depression, was defined as the primary outcome. The total change in HAM-D score from baseline to follow up was defined as a secondary outcome. Additional secondary outcomes included the follow up HAM-D score and a reduction in HAM-D score of 50% or more from the baseline. Follow up of the HAM-D score was recorded during 12 weeks by a research officer who was unaware of the patient’s randomization.
Statistical Considerations
A total of 248 patients equally allocated to the two groups provides at least 90 percent power, with a 5 percent type I error rate, using a two-sided hypothesis test. This calculation assumes an anticipated difference in the response rate of 20 percent between the two groups with a 30 percent response rate in the SSRI group and at least a 50 percent response rate in the combination treatment group. Considering a 15 percent dropout rate in each group, an additional sample of 44 patients equally divided into the two groups would be needed to yield a total required sample size of 292 patients. Therefore, the target sample size for each arm was 146.
This calculation assumes an anticipated difference in the response rate of 20 percent between the two groups with a 30 percent response rate in the SSRI group and at least a 50 percent response rate in the combination treatment group. Considering a 15 percent dropout rate in each group, an additional sample of 44 patients equally divided into the two groups would be needed to yield a total required sample size of 292 patients. Therefore, the target sample size for each arm was 146.
Descriptive statistics were prepared for all characteristics including means and standard deviations for continuous measures and frequencies and percentages for categorical measures. Chi-square or Fisher’s exact tests were used to compare categorical baseline characteristics. Two-sample t tests were used to compare continuous baseline characteristics. Chi-square tests were used to examine the association between treatment and the 20% and 50% reductions in HAM-D outcomes. These analyses were extended to logistic regression to adjust for the baseline HAM-D score.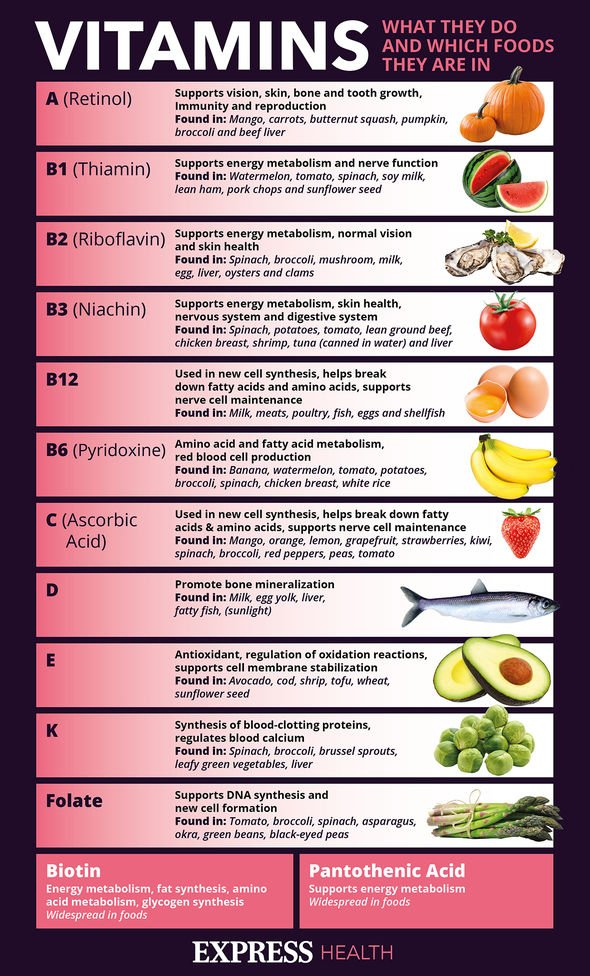 Two-sample t tests were used to examine the association between treatment and the follow up HAM-D score or change in HAM-D score from baseline to follow up. These analyses were extended to analysis of covariance to adjust for the baseline HAM-D score. All hypotheses tests were two-sided and p-values less than 0.05 were considered statistically significant. Analyses were conducted using SAS Version 9.2 (SAS Institute, Inc., Cary, NC, USA).
Two-sample t tests were used to examine the association between treatment and the follow up HAM-D score or change in HAM-D score from baseline to follow up. These analyses were extended to analysis of covariance to adjust for the baseline HAM-D score. All hypotheses tests were two-sided and p-values less than 0.05 were considered statistically significant. Analyses were conducted using SAS Version 9.2 (SAS Institute, Inc., Cary, NC, USA).
Results
A total of 199 depressed patients were screened for the B12 levels. Vitamin B12 deficiency was present in 44 (22%) patients; 73 (36%) had low normal B12 levels and 82 (42%) had normal B12 levels. Patients with low B12 levels were given the prescriptions for B12 replacement therapy in addition to the antidepressants. These patients were not randomized. Out of 73 patients with low normal B12 levels 34 (47%) were randomized to the treatment group while 39 (53%) were randomized to the control arm. There were no significant differences between the two groups at baseline except for the higher depression scores in the treatment group (Table ). No adverse effects or complications were noted in either group. For the primary outcome of 20% reduction in HAM-D score, significantly more subjects from the treatment group showed a 20% reduction unadjusted for baseline HAM-D score (100% vs. 69%; p < 0.001). Examining a50% reduction from baseline, this effect remained significant (44% vs. 5%; p < 0.001). We also adjusted the analyses of reduction for the baseline HAM-D score and our findings remained significant (Table ). Additionally, the change in HAM-D score was significantly greater for the treatment group, unadjusted and adjusted for the baseline HAM-D score (Table ).
No adverse effects or complications were noted in either group. For the primary outcome of 20% reduction in HAM-D score, significantly more subjects from the treatment group showed a 20% reduction unadjusted for baseline HAM-D score (100% vs. 69%; p < 0.001). Examining a50% reduction from baseline, this effect remained significant (44% vs. 5%; p < 0.001). We also adjusted the analyses of reduction for the baseline HAM-D score and our findings remained significant (Table ). Additionally, the change in HAM-D score was significantly greater for the treatment group, unadjusted and adjusted for the baseline HAM-D score (Table ).
Table 1.
Baseline Characteristics Shown as Mean ± Standard Deviation or Frequency (Percent)
| Treatment (n=34) | Control (n=39) | p-value | |
|---|---|---|---|
| Age, in years | 37.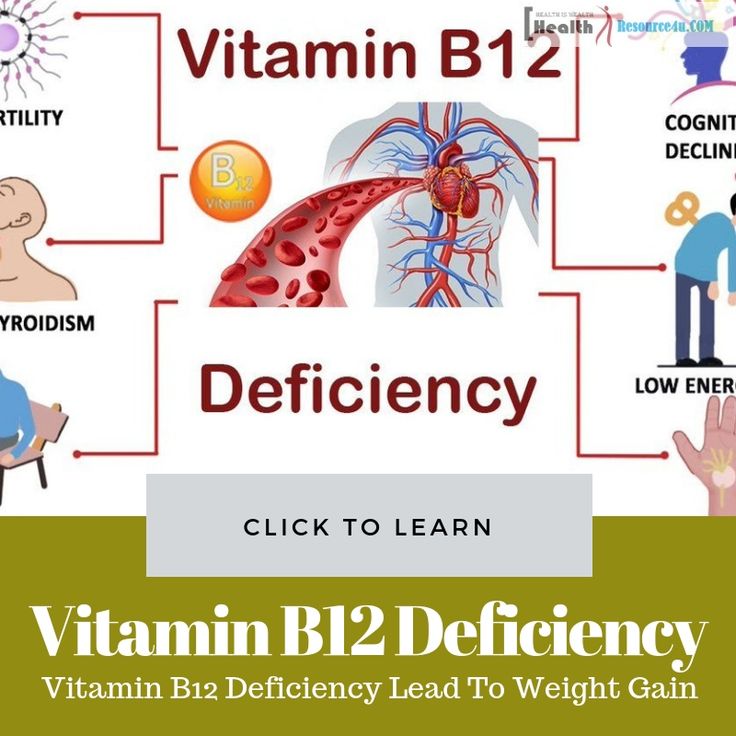 68 ± 13.38 68 ± 13.38 | 36.56 ± 12.28 | 0.71 |
| Total HAM-D | 23.21 ± 5.85 | 19.38 ± 5.70 | 0.006 |
| Vitamin B12 level | 238.49 ± 33.21 | 245.16 ± 27.82 | 0.36 |
| Gender | |||
| Male | 18 (52.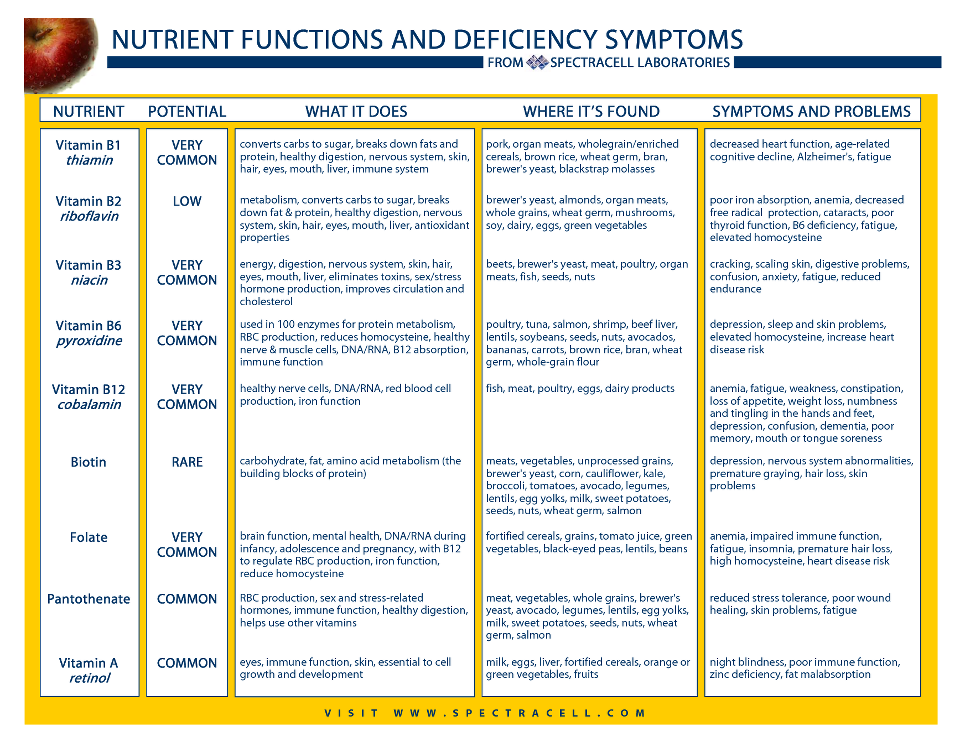 9) 9) | 20 (51.3) | 0.89 |
| Female | 16 (47.1) | 19 (48.7) | |
| Marital status | |||
| Single never married | 9 (26.5) | 13 (33.3) | 0.84 |
| Married | 21 (61. 8) 8) | 21 (53.9) | |
| Divorced/separated/widowed | 4 (11.8) | 5 (12.8) |
Open in a separate window
Table 2.
Outcomes for Follow Up After 3 Months Shown as Mean ± Standard Deviation or Frequency (Percent)
| Treatment (n=34) | Control (n=39) | Unadjusted P-value | Adjusted* P-value | |
|---|---|---|---|---|
| 20% reduction in HAM-D score | 34 (100) | 27 (69. 2) 2) | <0.001 | 0.001 |
| 50% reduction in HAM-D score | 15 (44.1) | 2 (5.1) | <0.001 | <0.001 |
| Follow up HAM-D score | 12.12 ± 5.12 | 14.38 ± 4.73 | 0.053 | <0.001 |
| Change in HAM-D score | 11.09 ± 4.58 | 5.00 ± 3.38 | <0.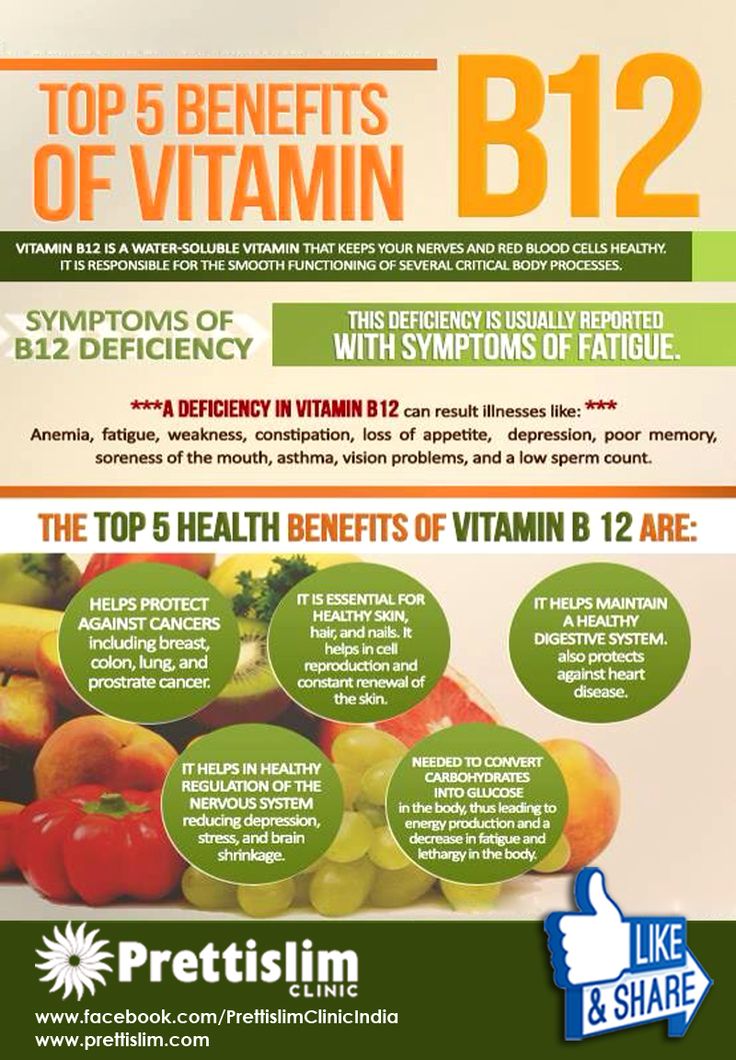 001 001 | <0.001 |
Open in a separate window
Coexistence of depression and vitamin B12 deficiency are not uncommon. These patients are routinely treated with SSRI and B12 supplementation, however it is not well established whether the people with low normal B12 and co-occurring depression should also receive B12 supplementation. Our study tried to address this issue. Despite not attaining the targeted sample size, the findings appear significant. Vitamin B12 deficiency was present in 22% of our depressed population. This frequency is high in a non-vegetarian, relatively young, middle to upper income population of our patients. A recent study of healthy adults from Karachi showed a population based prevalence of vitamin B12 deficiency (less than 200 pg/ml) in 9.74% people [25]. These findings indicate a substantial co-morbidity of B12 deficiency (22%) in our depressed patient population.
To our knowledge, this is the first randomized control trial in Pakistani population which has looked at clinically depressed patients with low B12 levels. We did not randomize B12 deficient patients due to ethical reasons. Low normal B12 levels were present in 36% of patients. These patients are often not treated with B12 supplementation. The findings of our study clearly indicate that these patients demonstrated significant improvement with B12 supplementation in addition to SSRI as compared to the control group even after adjustment for baseline HAM-D score. We think that these patients represent sub group within the clinically depressed population and a supplementation with B12 along with the conventional antidepressants may be a useful strategy in the treatment of depression in such cases.
We did not randomize B12 deficient patients due to ethical reasons. Low normal B12 levels were present in 36% of patients. These patients are often not treated with B12 supplementation. The findings of our study clearly indicate that these patients demonstrated significant improvement with B12 supplementation in addition to SSRI as compared to the control group even after adjustment for baseline HAM-D score. We think that these patients represent sub group within the clinically depressed population and a supplementation with B12 along with the conventional antidepressants may be a useful strategy in the treatment of depression in such cases.
We did not give sham injections to the control group. A placebo response due to injections may be responsible for the significant improvement in the treatment group. We also did not look at differences in response at specific doses of antidepressants nor did we stratify our groups on the basis of type of antidepressants prescribed. We also could not reach our sample size because we were not able to get another extension in our grant. Due to financial constraints we were not able to obtain final B12 levels. These are some of the limitations of our study. However, these findings have important clinical implications. B12 deficiency and low normal B12 levels are common and may be associated with depression and the inadequate response to antidepressant treatment in patients with depression. Vitamin B12 supplementation with antidepressants has significantly improved depressive symptoms in our group. Larger, multi-center studies are required to extend and replicate our findings.
Due to financial constraints we were not able to obtain final B12 levels. These are some of the limitations of our study. However, these findings have important clinical implications. B12 deficiency and low normal B12 levels are common and may be associated with depression and the inadequate response to antidepressant treatment in patients with depression. Vitamin B12 supplementation with antidepressants has significantly improved depressive symptoms in our group. Larger, multi-center studies are required to extend and replicate our findings.
Authors have no conflicts of interests to declare
Authors would like to acknowledge Michele Shaffer PhD from School of Public Health, Penn State University for her valuable input in statistical analysis and manuscript revision.
Study funding was supported by University research council grant of Aga Khan University (G&C code; 70210)
1. Murray C, Lopez A. The global burden of diseases a comprehensive assessment of Mortality and disability from diseases injuries and risk factors in 1990 and projected to 2020. Boston Harvard School of Public Health. WHO and World Bank. 1996 [Google Scholar]
Boston Harvard School of Public Health. WHO and World Bank. 1996 [Google Scholar]
2. Mirza I, Jenkins R. Risk factors prevalence and treatment of anxiety and depressive disorders in Pakistan systematic review. BMJ. 2004;328:794–8. [PMC free article] [PubMed] [Google Scholar]
3. Sohail Z, editor. Practice Guideline for the Treatment of Patients With Major Depressive Disorder DOI10.1176/appi.books.9780890423387.654001. 3rd ed. American Psychiatric Association. [Google Scholar]
4. Thase ME, Entsuah AR, Rudolph RL. Remission rates during treatment with Venlafaxine or selective serotonin reuptake inhibitors. Br J Psychiatry. 2001;178:234 –41. [PubMed] [Google Scholar]
5. Puech A, Montgomery SA, Prost JF, Solles A, Briley M. Milnacipran,a new serotonin and Noradrenaline reuptake inhibitor an overview of its antidepressant activity and clinical tolerability. Int Clin Psychopharmacol. 1997;12(2):99–108. [PubMed] [Google Scholar]
6. Antai-Otong D. Monotherapy Antidepressant.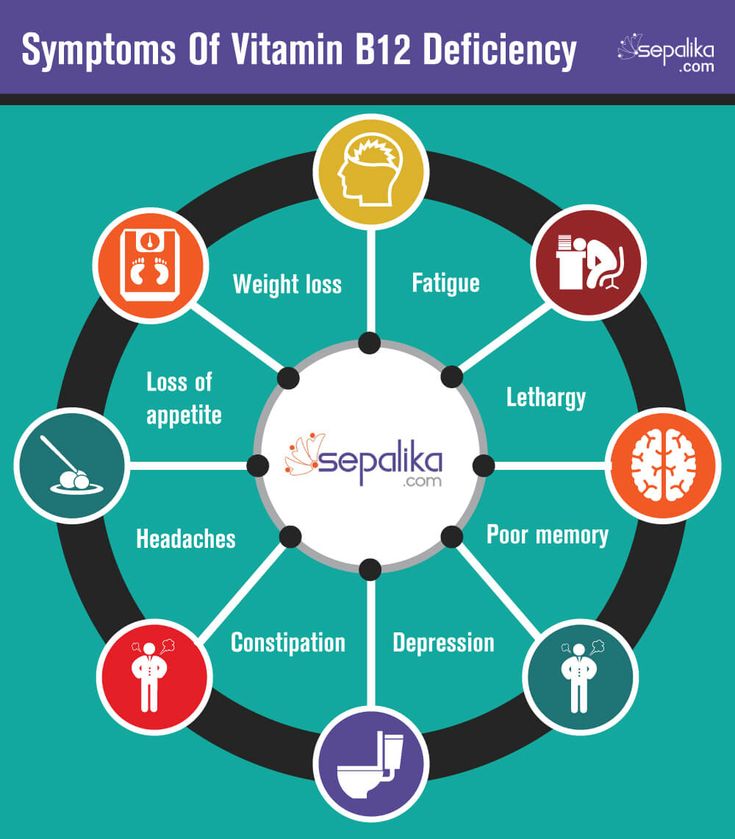 A Thing of the Past Implications for the Treatment of Major Depressive Disorder. Perspect Psych Care. 2007;43(3):142–5. [PubMed] [Google Scholar]
A Thing of the Past Implications for the Treatment of Major Depressive Disorder. Perspect Psych Care. 2007;43(3):142–5. [PubMed] [Google Scholar]
7. Shah RA, Qureshi MB, Khan AA. Magnitude of vitamin A deficiency in poor communities of the four selected districts of Punjab using (rapid assessment technique). Ann King Edward Med Coll. 2005;11(3):314–8. [Google Scholar]
8. Khan RM, Iqbal P. Deficiency of vitamin C in South Asia. Pak J Med Sci. 2006;22(3):347–55. [Google Scholar]
9. Hashim H, Tahir F. Frequency of vitamin B12 and folic acid deficiencies among patients with megaloblastic anemia. Ann Pak Inst Med Sci. 2006;2(3):192–4. [Google Scholar]
10. Yajnik CS, Deshpande SS, Lubree HG, et al. Vitamin B12 deficiency and hyperhomocysteinemia in rural and urban Indians. J Assoc Physicians India. 2006;54:775–82. [PubMed] [Google Scholar]
11. Fakhrzadeh H, Ghotbi S, Pourebrahim R, et al. Total plasma homocysteine folate and vitamin b12 status in healthy Iranian adults the Tehran homocysteine survey 2003–2004)/a cross sectional population based study. BMC Public Health. 2006;6:29. [PMC free article] [PubMed] [Google Scholar]
BMC Public Health. 2006;6:29. [PMC free article] [PubMed] [Google Scholar]
12. Lim HS, Heo YR. Plasma total homocysteine folate and vitamin B12 status in Korean adults. J Nutr Sci Vitaminol (Tokyo). 2002;48(4):290–7 . [PubMed] [Google Scholar]
13. Refsum H, Yajnik CS, Gadkari M, et al. Hyperhomocysteinemia and elevated methylmalonic acid indicate a high prevalence of cobalamin deficiency in Asian Indians. Am J Clin Nut. 2001;74(2):233–241. [PubMed] [Google Scholar]
14. Robert C, Brown DL. Vitamin B12 Deficiency. Am Fam Physician. 2003;67:979–86. [PubMed] [Google Scholar]
15. Hintikka J, Tolmunen T, Tanskanen A, Viinamäki H. High vitamin B12 level and good treatment outcome may be associated in major depressive disorder. BMC Psychiatry. 2003;3:17–22. [PMC free article] [PubMed] [Google Scholar]
16. Tiemeier H, vanTuijl HR, Hofman A, Meijer J, Kiliaan AJ, Breteler MM. Vitamin B12 folate and homocysteine in depression the Rotterdam Study. Am J Psychiatry. 2002;159(12):2099–01. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
17. Sachdev PS, Parslow RA, Lux O, et al. Relationship of homocysteine folic acid and vitamin B12 with depression in a middle aged community sample. Psychol Med. 2005;35(4):529–38. [PubMed] [Google Scholar]
18. Bottiglieri T, Laundy M, Crellin R, Toone BK, Carney MW, Reynolds EH. Homocysteine folate methylation and monoamine metabolism in depression. J Neurol Neurosurg Psychiatry. 2000;69:228–232. [PMC free article] [PubMed] [Google Scholar]
19. Alpert JE, Mischoulon D. Folinic acid (Leucovorin) as an adjunctive treatment for SSRI-refractory depression. Ann Clin Psychiatry. 2002;14(1):33–8. [PubMed] [Google Scholar]
20. Fava M, Borus JS. Folate vitamin B12 and homocysteine in major depressive disorder. Am J Psychiatry. 1997;154(3):426–8. [PubMed] [Google Scholar]
21. Papakostas GI, Peterson T. Serum folate vitamin B12 and homocysteine in major depressive disorder Part I.predictors of clinical response in fluoxetine-resistant depression. J Clin Psychiatry. 2004;65(8):1090–5. [PubMed] [Google Scholar]
J Clin Psychiatry. 2004;65(8):1090–5. [PubMed] [Google Scholar]
22. Papakostas GI, Peterson T. Serum folate vitamin B12 and homocysteine in major depressive disorder Part II predictors of clinical response in fluoxetine-resistant depression. J Clin Psychiatry. 2004;65(8):1096–8. [PubMed] [Google Scholar]
23. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. [PMC free article] [PubMed] [Google Scholar]
24. Chaudhry HR, Qureshi Z, Tareen IA, Yazdani I. Efficacy and tolerability of Paroxetine 20 mg daily in the treatment of depression and depression associated anxiety. J Pak Med Assoc. 2002;52(11):518–25. [PubMed] [Google Scholar]
25. Yakub M, Iqbal MP, Kakepoto GN, et al. High prevalence of mild hyperhomocystienemia and folate B12 and B6 deficiencies in an urban population in Karachi Pakistan. Pak J Med Sci. 2010;26(4):923–929. [Google Scholar]
Psychologists have found that loading doses of vitamin B6 help fight anxiety and depression - Gazeta.
 Ru
Ru Psychologists have found that loading doses of vitamin B6 help fight anxiety and depression - Gazeta.Ru | News
close
100%
University of Reading researchers found that taking 50 daily doses of vitamin B6 reduced anxiety and symptoms of depression. At the same time, vitamin B12 did not cause a similar effect. The study was published in the journal Human Psychopharmacology Clinical and Experimental .
Psychopharmacologists divided more than 300 participants into three groups: some took 50 times the dose of vitamin B6 with meals, while others took the same amount of vitamin B12 or a placebo. All participants are young men and women over 18 years of age. The experiment lasted one month. At the end of the work, the participants passed tests that assessed their psycho-emotional state. It improved significantly in the vitamin B6 group, but did not change in the placebo group.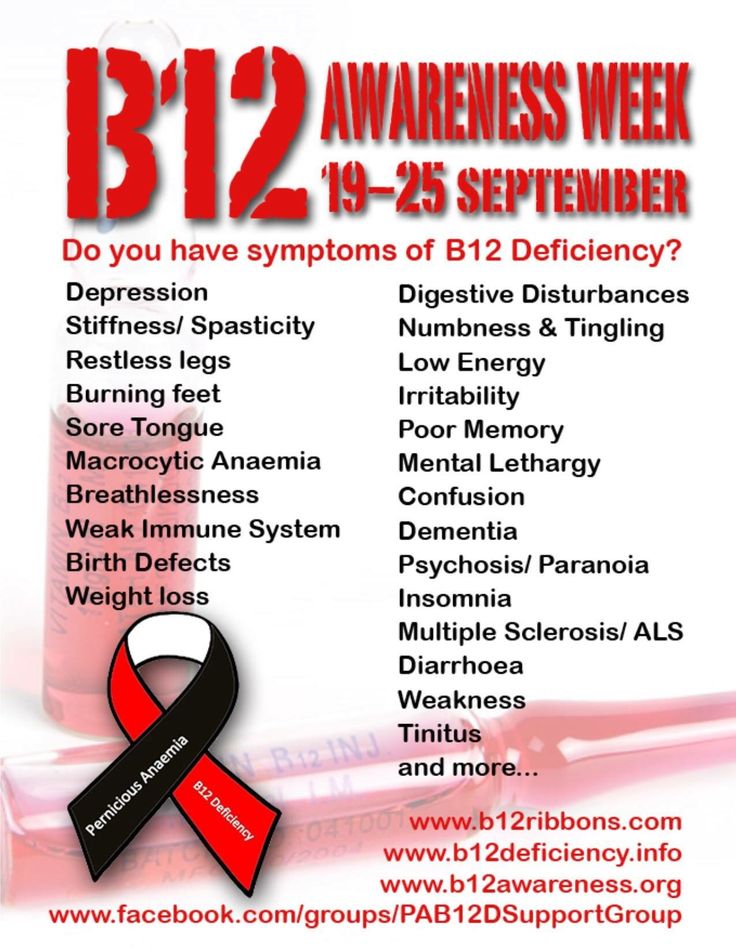 Vitamin B12 had little effect compared to B6. nine0003
Vitamin B12 had little effect compared to B6. nine0003
This effect may be associated with increased production of gamma-aminobutyric acid (GABA), a substance that inhibits the nervous system and has a sedative effect. Participants experienced mild side effects affecting vision. The authors of the study admit that it is too early to draw conclusions, and the antidepressant effect of vitamin B6 is much weaker than that of drugs. But if their results are confirmed, then patients with depression can count on one more therapy in addition to standard drugs. nine0003
Subscribe to Gazeta.Ru in News, Zen and Telegram.
To report a bug, select the text and press Ctrl+Enter
News
Zen
Telegram
Andrey Kolesnikov
A candle in the dark
About December, Hanukkah and Isaac Singer
Georgy Bovt
He is simply behind the times
Remembering the time of dear Leonid Ilyich
Alena Solntseva
The most important of the arts
About the New Year's film distribution and the prospect for cinemas
Dmitry Vodennikov
The golden trumpet of failure
About the plight of geeks
Maria Degtereva
Battle lost
Why Russian rock is dead and Russian rap is not
Error found?
Close
Thank you for your message, we will fix it soon.
Continue Reading
Depression Linked to Vitamin B12 Deficiency
Efthymia Kontela, Medical Specialist, Director of the City Hospital Emergency Department, confirms that people suffering from "monstrous" depression are deficient in Vitamin B12.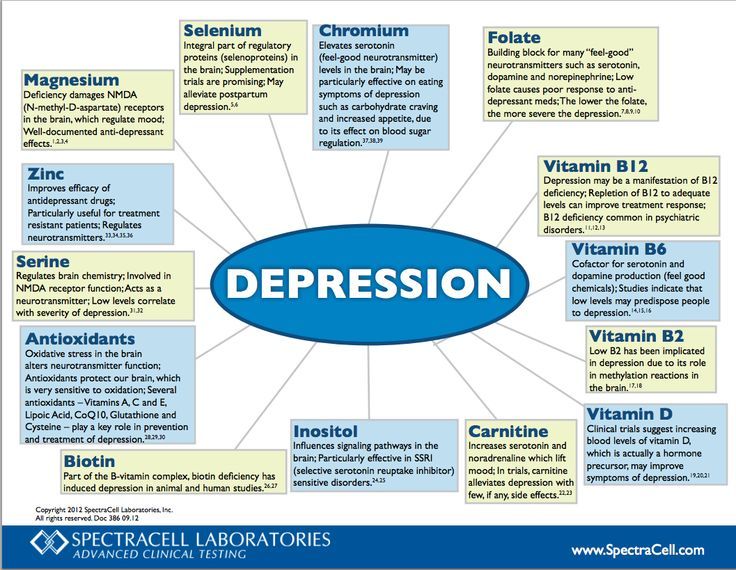
What is depression?
The term depression for most people is synonymous with sadness, hopelessness and dissatisfaction with life, when everything is seen in "gloomy colors." Depressive disorders were first described by Hippocrates and were considered among the most persistent, stable and well-diagnosed diseases.
The pathophysiology of depression is heterogeneous and includes biochemical changes in the brain, genetic predisposition, and environmental and individual factors.
Risk factors for depression include significant changes in a person's life, some mental or physical trauma, stressful situations, and abuse. However, when the desire for vigorous activity disappears (the inability to get out of bed: “why”?) And lasts for several months, it can be assumed that a person has depression.
The main complaints of patients with depression are associated with painful feelings of anxiety, constant sadness, frustration, loss of interest, fatigue, sleep problems, reduced ability to concentrate and poor memory. Several studies over the past decade show that regular exercise and physical activity reduce depression. nine0003
Several studies over the past decade show that regular exercise and physical activity reduce depression. nine0003
There also seems to be a connection between diet and depression. People with depression are deficient in many vitamins (due to the many stress hormones that destroy them) and especially eat a diet high in sugar, caffeine (mainly due to too much coffee), dairy products, and excessive alcohol consumption. .
With regard to vitamins that may be deficient in the body of people suffering from depression, it has been found that once their levels return to normal levels, depression "goes away". A person can also improve their "mood" thanks to several amino acids, minerals, as well as hormones (vitamin D3, cortisol, testosterone). nine0003
What is vitamin B12 and what are its benefits?
Vitamin B12 or cobalamin is a water-soluble vitamin that our body cannot produce, but which is involved in the metabolism of cells in the human body and belongs to the vitamin B complex.
The term vitamin B complex refers to the combination of 8 vitamins: B1, B2, B3, B5, B6, folic acid (B9), B12 and biotin. These vitamins cannot be stored in the body, so their availability depends entirely on the daily diet. nine0003
B vitamins are destroyed by alcohol, sugar, nicotine, caffeine, so it's no surprise that many people can be deficient so often. Vitamin B12 is found in animal products, red meat, beef liver, poultry, fish, shellfish, eggs and dairy products, as well as dietary supplements.
The main source of B12 in nature is bacteria, the only organisms that can produce this vitamin. In humans, these bacteria produce B12 in the large intestine. However, very little of it will be absorbed by the intestinal wall, so we must supplement with B12 to reach a satisfactory level. nine0003
What are the effects of vitamin B12?
Vitamin B12 is essential for many important hormonal and metabolic functions in the body. Including for the production of digestive enzymes and the transport of essential nutrients in and out of cells. A sufficient level of B12 is essential for normal hematopoiesis and neurological functionality. This vitamin contributes to the synthesis of many compounds in the body.
Including for the production of digestive enzymes and the transport of essential nutrients in and out of cells. A sufficient level of B12 is essential for normal hematopoiesis and neurological functionality. This vitamin contributes to the synthesis of many compounds in the body.
Vitamin B12 needed for:
- Energy supply - along with other B vitamins, it does not directly provide energy, but helps to maintain the normal metabolism of amino acids, fats and carbohydrates. Vitamin B12 is involved in a number of intracellular processes, ensuring the health of cells and the production of sufficient energy.
- Normal functioning of the nervous system. Vitamin B12 with folic acid is essential for myelin synthesis. This is a substance that surrounds nerve fibers, which protects them and ensures fast signal transmission between nerve cells. If myelin is damaged, the transmission of impulses is disrupted. Therefore, vitamin B12 is essential for the normal functioning of the nervous system.
 nine0135
nine0135 - Prevention of anemia. Good circulation is often associated with high iron levels, but folic acid and vitamin B12 actually play the same role. Therefore, they are called hematopoietic vitamins. B12 helps in the division of red blood cells, which are necessary to maintain a constant circulation of oxygen in the body. The constant circulation of oxygen ensures the functioning of all critical processes. Therefore, it is the deficiency of B12 and folic acid that, in fact, is often the cause of anemia. nine0021 Also, vitamin B12 helps the body get rid of excessive amounts of homocysteine, or waste products. They are formed as a result of metabolism and are toxic to cells. Therefore, it is essential that homocysteine is flushed out of the body. In this process, vitamin B12 helps protect the walls of blood vessels, preventing cardiovascular disease, Alzheimer's disease and dementia.
- DNA/RNA synthesis.
- Methylation. B12 is involved in the process in which the "methyl group" is donated to other molecules and thus maintains the chemical balance of the body and its various functions.
 This seemingly simple process happens billions of times per second. It is important for mood, brain function, energy production, body cleansing, the immune system, and many other functions. Methylation comes under attack when we are under stress. nine0135
This seemingly simple process happens billions of times per second. It is important for mood, brain function, energy production, body cleansing, the immune system, and many other functions. Methylation comes under attack when we are under stress. nine0135
There is a lot of talk these days about the consequences of reduced B12 intake due to the growing trend of people becoming vegetarians and vegans. However, there are other cases besides vegetarianism in which there is B12 deficiency. These include gastrointestinal upset and chronic drug use: for example, for stomach ulcers, metformin (known as glucophage), excessive liver stress (with the systematic use of alcoholic beverages), and certain drugs such as antibiotics, tranquilizers, and sleeping pills. nine0003
What happens when we lack vitamin B12?
Vitamin B12 deficiency can cause anemia, afternoon fatigue, inability to concentrate, lack of attention, poor memory, prolonged irritability and tearfulness, confusion, palpitations, diarrhea, and general malaise.
Since B12 plays a vital role in the nervous system, its absence can cause problems with nerve endings, especially in peripheral nerves. Over time, damage to the peripheral nerves can lead to difficulty moving, numbness, and muscle weakness. Symptoms of vitamin B12 deficiency often present as neurological symptoms long before the onset of typical hematological disorders. About one third of people with folic acid or vitamin B12 deficiency are anemic. A similar proportion applies to a number of neuropsychiatric symptoms. nine0003
More than a third of psychiatric patients have been found to be deficient in folic acid or vitamin B12. Vitamin B12 deficiency increases with age.
Anxiety and Depression Vitamins
5-hydroxytryptophan, or 5-HTP, is a derivative of the amino acid tryptophan, which is converted in our body to serotonin, a substance that promotes a sense of mental well-being by acting on our brain. nine0003
nine0003
Serotonin is a chemical that performs many functions in the human body. It seems to play a role in appetite, emotions, mood, movement, behavior, and autonomic nervous system function. It also seems to play a key role in maintaining mental balance. Low serotonin levels are associated with depression.
B-vitamins come into play to help our body maintain tryptophan levels and maximize its conversion to serotonin. Folic acid and vitamin B12 are considered particularly important B vitamins because studies have shown that they may play an important role in reducing the risk of developing or recurring clinical depression. nine0003
Many of the vitamins that increase serotonin levels in our body, as well as supplements that can improve the clinical picture in people with depression, can also reduce anxiety symptoms.
The recommended daily intake of B12 for adults is 2.4 mcg, with no restrictions established, since this vitamin is not considered to cause harmful effects, even when taken in large quantities, according to iefimerida. gr (however, before rather than listening to generalized data, consult your doctor.Do not self-medicate!). nine0003
Older people, because they are not good at absorbing B12, are advised to take it through fortified foods or multivitamins.
What types of vitamin B12 preparations are available?
Vitamin B12 is available in:
- capsules;
- tablets under the tongue;
- injectable;
- is a skin-acting gel.
In studies involving depressed patients treated with antidepressants for more than six months, their blood levels of vitamin B12 were measured at two different time intervals six months apart. Those who responded more fully to treatment were found to have higher body concentrations of vitamin B12 both at the beginning and at the end of the study period. nine0003
Researchers at the Max Planck Institute in Germany are working on developing a nutritional supplement that fights postpartum depression.