Depression treatment therapy
Depression (major depressive disorder) - Diagnosis and treatment
Diagnosis
Your doctor may determine a diagnosis of depression based on:
- Physical exam. Your doctor may do a physical exam and ask questions about your health. In some cases, depression may be linked to an underlying physical health problem.
- Lab tests. For example, your doctor may do a blood test called a complete blood count or test your thyroid to make sure it's functioning properly.
- Psychiatric evaluation. Your mental health professional asks about your symptoms, thoughts, feelings and behavior patterns. You may be asked to fill out a questionnaire to help answer these questions.
- DSM-5. Your mental health professional may use the criteria for depression listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
Types of depression
Symptoms caused by major depression can vary from person to person. To clarify the type of depression you have, your doctor may add one or more specifiers. A specifier means that you have depression with specific features, such as:
- Anxious distress — depression with unusual restlessness or worry about possible events or loss of control
- Mixed features — simultaneous depression and mania, which includes elevated self-esteem, talking too much and increased energy
- Melancholic features — severe depression with lack of response to something that used to bring pleasure and associated with early morning awakening, worsened mood in the morning, major changes in appetite, and feelings of guilt, agitation or sluggishness
- Atypical features — depression that includes the ability to temporarily be cheered by happy events, increased appetite, excessive need for sleep, sensitivity to rejection, and a heavy feeling in the arms or legs
- Psychotic features — depression accompanied by delusions or hallucinations, which may involve personal inadequacy or other negative themes
- Catatonia — depression that includes motor activity that involves either uncontrollable and purposeless movement or fixed and inflexible posture
- Peripartum onset — depression that occurs during pregnancy or in the weeks or months after delivery (postpartum)
- Seasonal pattern — depression related to changes in seasons and reduced exposure to sunlight
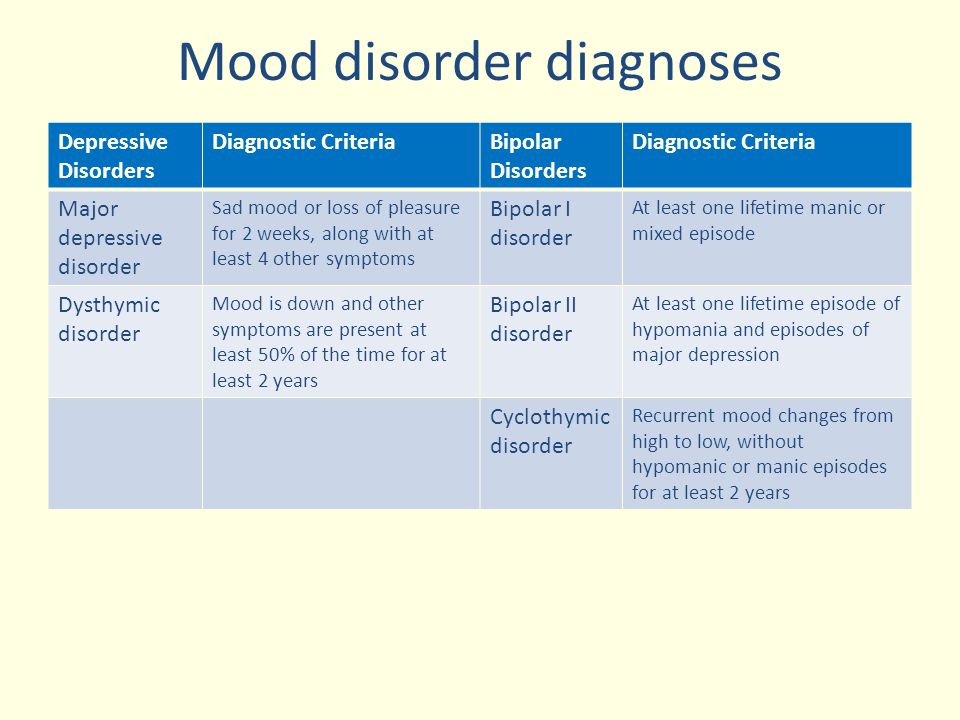
Other disorders that cause depression symptoms
Several other disorders, such as those below, include depression as a symptom. It's important to get an accurate diagnosis, so you can get appropriate treatment.
It's important to get an accurate diagnosis, so you can get appropriate treatment.
- Bipolar I and II disorders. These mood disorders include mood swings that range from highs (mania) to lows (depression). It's sometimes difficult to distinguish between bipolar disorder and depression.
- Cyclothymic disorder. Cyclothymic (sy-kloe-THIE-mik) disorder involves highs and lows that are milder than those of bipolar disorder.
- Disruptive mood dysregulation disorder. This mood disorder in children includes chronic and severe irritability and anger with frequent extreme temper outbursts. This disorder typically develops into depressive disorder or anxiety disorder during the teen years or adulthood.
- Persistent depressive disorder. Sometimes called dysthymia (dis-THIE-me-uh), this is a less severe but more chronic form of depression. While it's usually not disabling, persistent depressive disorder can prevent you from functioning normally in your daily routine and from living life to its fullest.

- Premenstrual dysphoric disorder. This involves depression symptoms associated with hormone changes that begin a week before and improve within a few days after the onset of your period, and are minimal or gone after completion of your period.
- Other depression disorders. This includes depression that's caused by the use of recreational drugs, some prescribed medications or another medical condition.
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your depression (major depressive disorder)-related health concerns Start Here
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Complete blood count (CBC)
Treatment
Medications and psychotherapy are effective for most people with depression. Your primary care doctor or psychiatrist can prescribe medications to relieve symptoms.![]() However, many people with depression also benefit from seeing a psychiatrist, psychologist or other mental health professional.
However, many people with depression also benefit from seeing a psychiatrist, psychologist or other mental health professional.
If you have severe depression, you may need a hospital stay, or you may need to participate in an outpatient treatment program until your symptoms improve.
Here's a closer look at depression treatment options.
Medications
Many types of antidepressants are available, including those below. Be sure to discuss possible major side effects with your doctor or pharmacist.
- Selective serotonin reuptake inhibitors (SSRIs). Doctors often start by prescribing an SSRI. These drugs are considered safer and generally cause fewer bothersome side effects than other types of antidepressants. SSRIs include citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac), paroxetine (Paxil, Pexeva), sertraline (Zoloft) and vilazodone (Viibryd).
- Serotonin-norepinephrine reuptake inhibitors (SNRIs). Examples of SNRIs include duloxetine (Cymbalta), venlafaxine (Effexor XR), desvenlafaxine (Pristiq, Khedezla) and levomilnacipran (Fetzima).

- Atypical antidepressants. These medications don't fit neatly into any of the other antidepressant categories. They include bupropion (Wellbutrin XL, Wellbutrin SR, Aplenzin, Forfivo XL), mirtazapine (Remeron), nefazodone, trazodone and vortioxetine (Trintellix).
- Tricyclic antidepressants. These drugs — such as imipramine (Tofranil), nortriptyline (Pamelor), amitriptyline, doxepin, trimipramine (Surmontil), desipramine (Norpramin) and protriptyline (Vivactil) — can be very effective, but tend to cause more-severe side effects than newer antidepressants. So tricyclics generally aren't prescribed unless you've tried an SSRI first without improvement.
- Monoamine oxidase inhibitors (MAOIs). MAOIs — such as tranylcypromine (Parnate), phenelzine (Nardil) and isocarboxazid (Marplan) — may be prescribed, typically when other drugs haven't worked, because they can have serious side effects. Using MAOIs requires a strict diet because of dangerous (or even deadly) interactions with foods ― such as certain cheeses, pickles and wines ― and some medications and herbal supplements.
 Selegiline (Emsam), a newer MAOI that sticks on the skin as a patch, may cause fewer side effects than other MAOIs do. These medications can't be combined with SSRIs.
Selegiline (Emsam), a newer MAOI that sticks on the skin as a patch, may cause fewer side effects than other MAOIs do. These medications can't be combined with SSRIs. - Other medications. Other medications may be added to an antidepressant to enhance antidepressant effects. Your doctor may recommend combining two antidepressants or adding medications such as mood stabilizers or antipsychotics. Anti-anxiety and stimulant medications also may be added for short-term use.
Finding the right medication
If a family member has responded well to an antidepressant, it may be one that could help you. Or you may need to try several medications or a combination of medications before you find one that works. This requires patience, as some medications need several weeks or longer to take full effect and for side effects to ease as your body adjusts.
Inherited traits play a role in how antidepressants affect you. In some cases, where available, results of genetic tests (done by a blood test or cheek swab) may offer clues about how your body may respond to a particular antidepressant. However, other variables besides genetics can affect your response to medication.
However, other variables besides genetics can affect your response to medication.
Risks of abruptly stopping medication
Don't stop taking an antidepressant without talking to your doctor first. Antidepressants aren't considered addictive, but sometimes physical dependence (which is different from addiction) can occur.
Stopping treatment abruptly or missing several doses can cause withdrawal-like symptoms, and quitting suddenly may cause a sudden worsening of depression. Work with your doctor to gradually and safely decrease your dose.
Antidepressants and pregnancy
If you're pregnant or breast-feeding, some antidepressants may pose an increased health risk to your unborn child or nursing child. Talk with your doctor if you become pregnant or you're planning to become pregnant.
Antidepressants and increased suicide risk
Most antidepressants are generally safe, but the Food and Drug Administration (FDA) requires all antidepressants to carry a black box warning, the strictest warning for prescriptions. In some cases, children, teenagers and young adults under age 25 may have an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed.
In some cases, children, teenagers and young adults under age 25 may have an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed.
Anyone taking an antidepressant should be watched closely for worsening depression or unusual behavior, especially when starting a new medication or with a change in dosage. If you or someone you know has suicidal thoughts when taking an antidepressant, immediately contact a doctor or get emergency help.
Keep in mind that antidepressants are more likely to reduce suicide risk in the long run by improving mood.
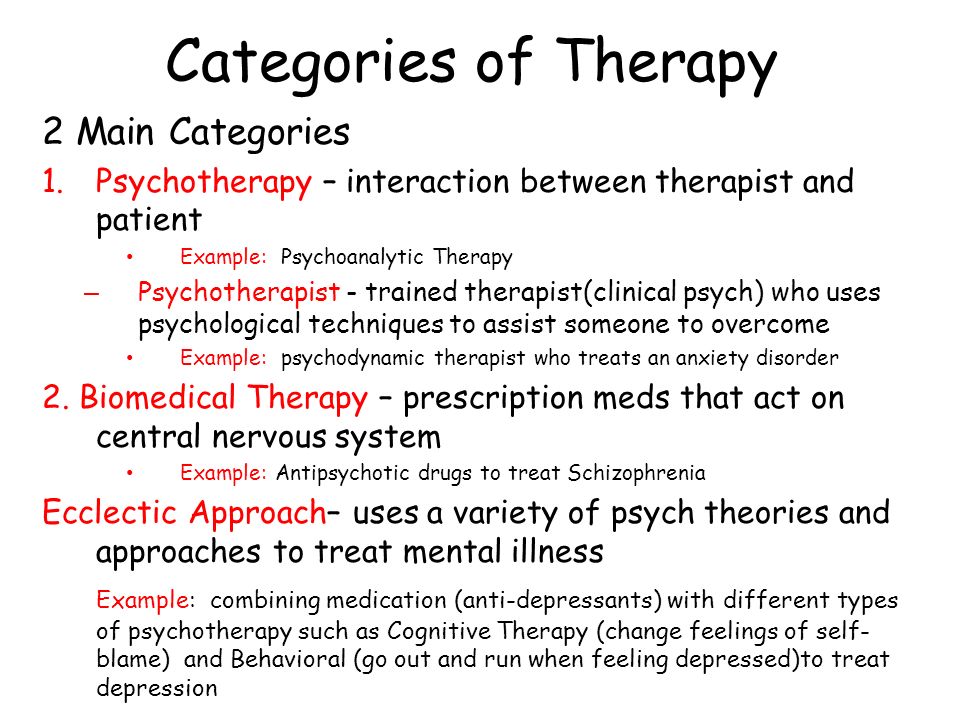
Psychotherapy
Psychotherapy is a general term for treating depression by talking about your condition and related issues with a mental health professional. Psychotherapy is also known as talk therapy or psychological therapy.
Different types of psychotherapy can be effective for depression, such as cognitive behavioral therapy or interpersonal therapy. Your mental health professional may also recommend other types of therapies. Psychotherapy can help you:
Your mental health professional may also recommend other types of therapies. Psychotherapy can help you:
- Adjust to a crisis or other current difficulty
- Identify negative beliefs and behaviors and replace them with healthy, positive ones
- Explore relationships and experiences, and develop positive interactions with others
- Find better ways to cope and solve problems
- Identify issues that contribute to your depression and change behaviors that make it worse
- Regain a sense of satisfaction and control in your life and help ease depression symptoms, such as hopelessness and anger
- Learn to set realistic goals for your life
- Develop the ability to tolerate and accept distress using healthier behaviors
Alternate formats for therapy
Formats for depression therapy as an alternative to face-to-face office sessions are available and may be an effective option for some people. Therapy can be provided, for example, as a computer program, by online sessions, or using videos or workbooks.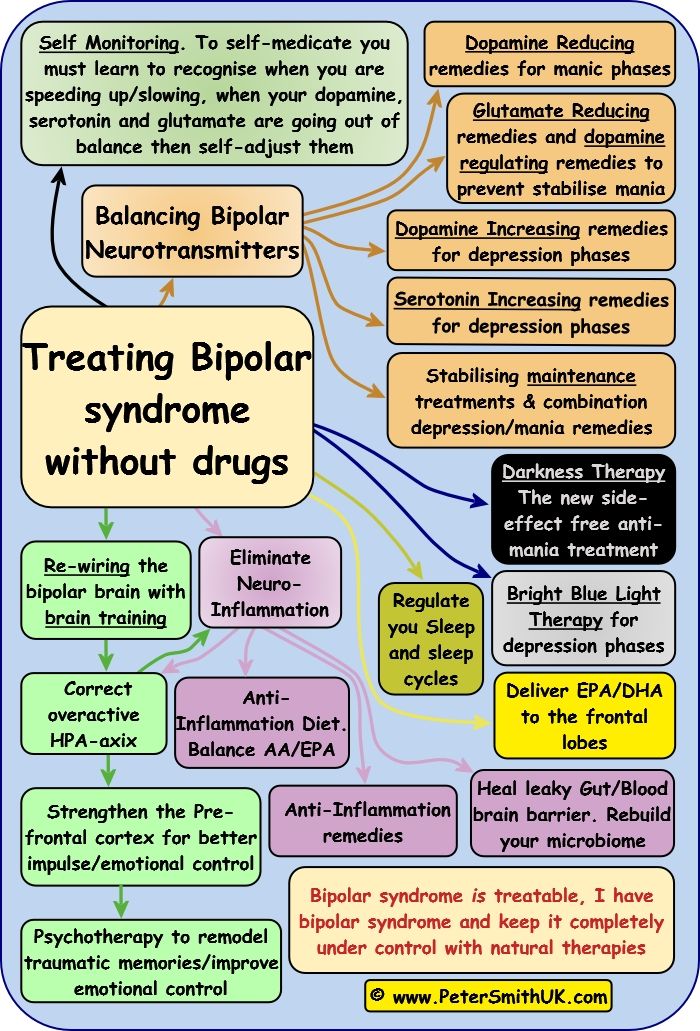 Programs can be guided by a therapist or be partially or totally independent.
Programs can be guided by a therapist or be partially or totally independent.
Before you choose one of these options, discuss these formats with your therapist to determine if they may be helpful for you. Also, ask your therapist if he or she can recommend a trusted source or program. Some may not be covered by your insurance and not all developers and online therapists have the proper credentials or training.
Smartphones and tablets that offer mobile health apps, such as support and general education about depression, are not a substitute for seeing your doctor or therapist.
Hospital and residential treatment
In some people, depression is so severe that a hospital stay is needed. This may be necessary if you can't care for yourself properly or when you're in immediate danger of harming yourself or someone else. Psychiatric treatment at a hospital can help keep you calm and safe until your mood improves.
Partial hospitalization or day treatment programs also may help some people. These programs provide the outpatient support and counseling needed to get symptoms under control.
These programs provide the outpatient support and counseling needed to get symptoms under control.
Other treatment options
For some people, other procedures, sometimes called brain stimulation therapies, may be suggested:
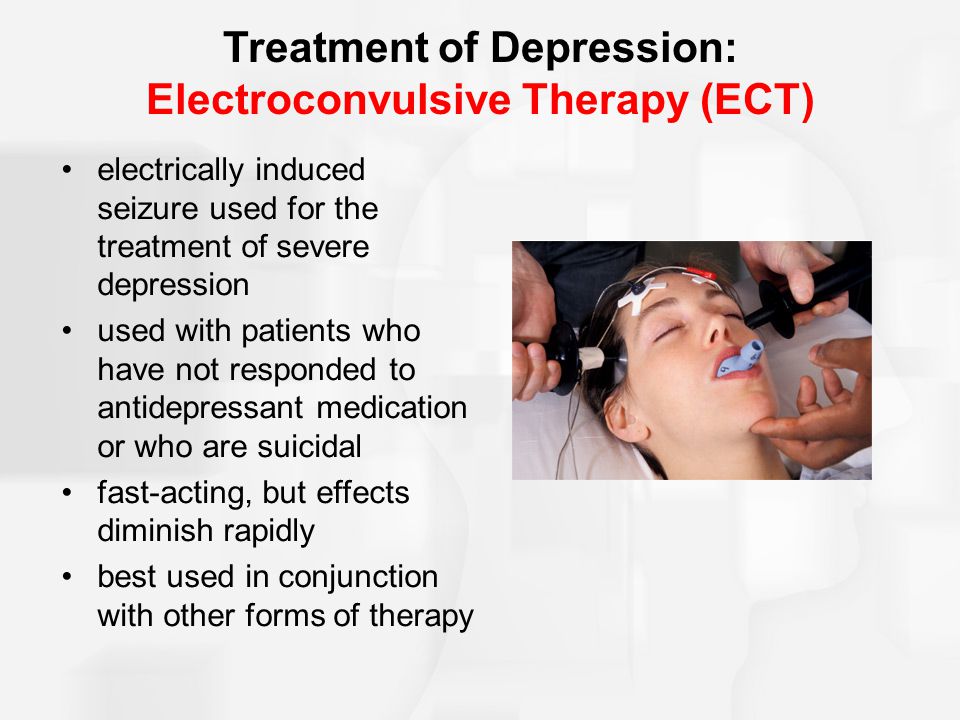
- Electroconvulsive therapy (ECT). In ECT, electrical currents are passed through the brain to impact the function and effect of neurotransmitters in your brain to relieve depression. ECT is usually used for people who don't get better with medications, can't take antidepressants for health reasons or are at high risk of suicide.
- Transcranial magnetic stimulation (TMS). TMS may be an option for those who haven't responded to antidepressants. During TMS, a treatment coil placed against your scalp sends brief magnetic pulses to stimulate nerve cells in your brain that are involved in mood regulation and depression.
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Antidepressants: Selecting one that's right for you
- Antidepressants: Side effects
- Atypical antidepressants
- Monoamine oxidase inhibitors (MAOIs)
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
- Treatment-resistant depression
- Tricyclic antidepressants and tetracyclic antidepressants
- Antidepressant withdrawal: Is there such a thing?
- Antidepressants and alcohol: What's the concern?
- Antidepressants and weight gain: What causes it?
- Antidepressants: Can they stop working?
- MAOIs and diet: Is it necessary to restrict tyramine?
- Electroconvulsive therapy (ECT)
- Psychotherapy
- Transcranial magnetic stimulation
- Vagus nerve stimulation
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Depression generally isn't a disorder that you can treat on your own. But in addition to professional treatment, these self-care steps can help:
- Stick to your treatment plan. Don't skip psychotherapy sessions or appointments. Even if you're feeling well, don't skip your medications. If you stop, depression symptoms may come back, and you could also experience withdrawal-like symptoms. Recognize that it will take time to feel better.
- Learn about depression. Education about your condition can empower you and motivate you to stick to your treatment plan. Encourage your family to learn about depression to help them understand and support you.
- Pay attention to warning signs. Work with your doctor or therapist to learn what might trigger your depression symptoms. Make a plan so that you know what to do if your symptoms get worse. Contact your doctor or therapist if you notice any changes in symptoms or how you feel.
 Ask relatives or friends to help watch for warning signs.
Ask relatives or friends to help watch for warning signs. - Avoid alcohol and recreational drugs. It may seem like alcohol or drugs lessen depression symptoms, but in the long run they generally worsen symptoms and make depression harder to treat. Talk with your doctor or therapist if you need help with alcohol or substance use.
- Take care of yourself. Eat healthy, be physically active and get plenty of sleep. Consider walking, jogging, swimming, gardening or another activity that you enjoy. Sleeping well is important for both your physical and mental well-being. If you're having trouble sleeping, talk to your doctor about what you can do.
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Depression, anxiety and exercise
Alternative medicine
Alternative medicine is the use of a nonconventional approach instead of conventional medicine. Complementary medicine is a nonconventional approach used along with conventional medicine — sometimes called integrative medicine.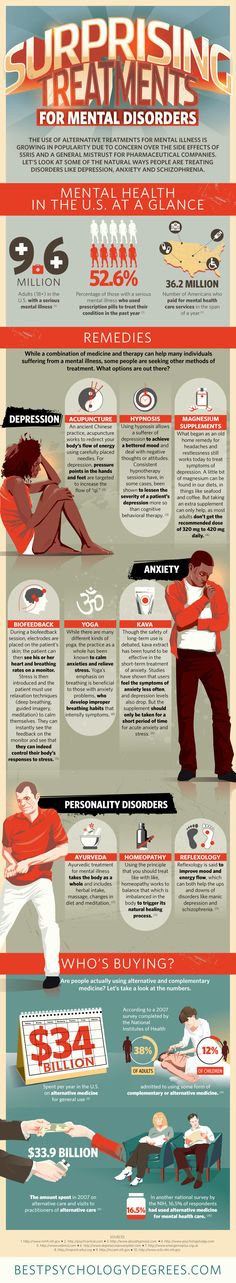
Make sure you understand the risks as well as possible benefits if you pursue alternative or complementary therapy. Don't replace conventional medical treatment or psychotherapy with alternative medicine. When it comes to depression, alternative treatments aren't a substitute for medical care.
Supplements
Examples of supplements that are sometimes used for depression include:
- St. John's wort. Although this herbal supplement isn't approved by the Food and Drug Administration (FDA) to treat depression in the U.S., it may be helpful for mild or moderate depression. But if you choose to use it, be careful — St. John's wort can interfere with a number of medications, such as heart drugs, blood-thinning drugs, birth control pills, chemotherapy, HIV/AIDS medications and drugs to prevent organ rejection after a transplant. Also, avoid taking St. John's wort while taking antidepressants because the combination can cause serious side effects.
- SAMe.
 Pronounced "sam-E," this dietary supplement is a synthetic form of a chemical that occurs naturally in the body. The name is short for S-adenosylmethionine (es-uh-den-o-sul-muh-THIE-o-neen). SAMe isn't approved by the FDA to treat depression in the U.S. It may be helpful, but more research is needed. SAMe may trigger mania in people with bipolar disorder.
Pronounced "sam-E," this dietary supplement is a synthetic form of a chemical that occurs naturally in the body. The name is short for S-adenosylmethionine (es-uh-den-o-sul-muh-THIE-o-neen). SAMe isn't approved by the FDA to treat depression in the U.S. It may be helpful, but more research is needed. SAMe may trigger mania in people with bipolar disorder. - Omega-3 fatty acids. These healthy fats are found in cold-water fish, flaxseed, flax oil, walnuts and some other foods. Omega-3 supplements are being studied as a possible treatment for depression. While considered generally safe, in high doses, omega-3 supplements may interact with other medications. More research is needed to determine if eating foods with omega-3 fatty acids can help relieve depression.
Nutritional and dietary products aren't monitored by the FDA the same way medications are. You can't always be certain of what you're getting and whether it's safe. Also, because some herbal and dietary supplements can interfere with prescription medications or cause dangerous interactions, talk to your doctor or pharmacist before taking any supplements.
Mind-body connections
Integrative medicine practitioners believe the mind and body must be in harmony for you to stay healthy. Examples of mind-body techniques that may be helpful for depression include:
- Acupuncture
- Relaxation techniques such as yoga or tai chi
- Meditation
- Guided imagery
- Massage therapy
- Music or art therapy
- Spirituality
- Aerobic exercise
Relying solely on these therapies is generally not enough to treat depression. They may be helpful when used in addition to medication and psychotherapy.
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Natural remedies for depression: Are they effective?
Coping and support
Talk with your doctor or therapist about improving your coping skills, and try these tips:
- Simplify your life. Cut back on obligations when possible, and set reasonable goals for yourself.
 Give yourself permission to do less when you feel down.
Give yourself permission to do less when you feel down. - Write in a journal. Journaling, as part of your treatment, may improve mood by allowing you to express pain, anger, fear or other emotions.
- Read reputable self-help books and websites. Your doctor or therapist may be able to recommend books or websites to read.
- Locate helpful groups. Many organizations, such as the National Alliance on Mental Illness (NAMI) and the Depression and Bipolar Support Alliance, offer education, support groups, counseling and other resources to help with depression. Employee assistance programs and religious groups also may offer help for mental health concerns.
- Don't become isolated. Try to participate in social activities, and get together with family or friends regularly. Support groups for people with depression can help you connect to others facing similar challenges and share experiences.

- Learn ways to relax and manage your stress. Examples include meditation, progressive muscle relaxation, yoga and tai chi.
- Structure your time. Plan your day. You may find it helps to make a list of daily tasks, use sticky notes as reminders or use a planner to stay organized.
- Don't make important decisions when you're down. Avoid decision-making when you're feeling depressed, since you may not be thinking clearly.
Preparing for your appointment
You may see your primary care doctor, or your doctor may refer you to a mental health professional. Here's some information to help you get ready for your appointment.
What you can do
Before your appointment, make a list of:
- Any symptoms you've had, including any that may seem unrelated to the reason for your appointment
- Key personal information, including any major stresses or recent life changes
- All medications, vitamins or other supplements that you're taking, including dosages
- Questions to ask your doctor or mental health professional
Take a family member or friend along, if possible, to help you remember all of the information provided during the appointment.
Some basic questions to ask your doctor include:
- Is depression the most likely cause of my symptoms?
- What are other possible causes for my symptoms?
- What kinds of tests will I need?
- What treatment is likely to work best for me?
- What are the alternatives to the primary approach that you're suggesting?
- I have these other health conditions. How can I best manage them together?
- Are there any restrictions that I need to follow?
- Should I see a psychiatrist or other mental health professional?
- What are the main side effects of the medications you're recommending?
- Is there a generic alternative to the medicine you're prescribing?
- Are there any brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your doctor will likely ask you a number of questions. Be ready to answer them to reserve time to go over any points you want to focus on. Your doctor may ask:
Be ready to answer them to reserve time to go over any points you want to focus on. Your doctor may ask:
- When did you or your loved ones first notice your symptoms of depression?
- How long have you felt depressed? Do you generally always feel down, or does your mood fluctuate?
- Does your mood ever swing from feeling down to feeling intensely happy (euphoric) and full of energy?
- Do you ever have suicidal thoughts when you're feeling down?
- Do your symptoms interfere with your daily life or relationships?
- Do you have any blood relatives with depression or another mood disorder?
- What other mental or physical health conditions do you have?
- Do you drink alcohol or use recreational drugs?
- How much do you sleep at night? Does it change over time?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
By Mayo Clinic Staff
What Types of Therapy Are Helpful For Depression?
by High Focus Centers
Depression is a potentially debilitating mental health disorder.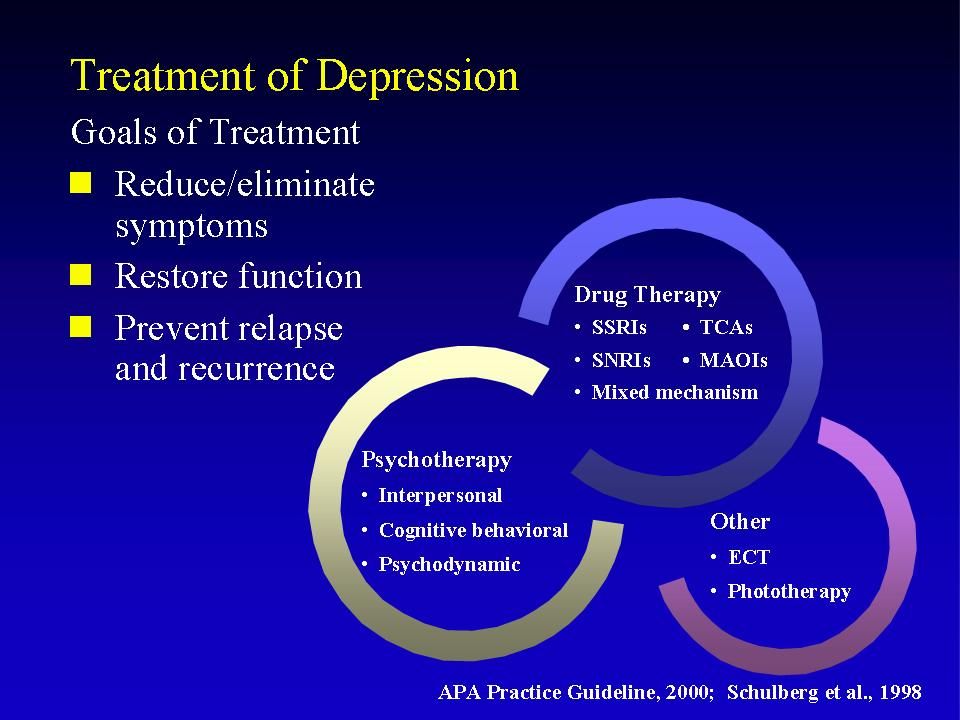 It’s also one of the most common. The CDC states almost 5% of adults report suffering from depression each year. However, cases may be underreported. Other sources place the actual number of individuals living with the disorder much higher.
It’s also one of the most common. The CDC states almost 5% of adults report suffering from depression each year. However, cases may be underreported. Other sources place the actual number of individuals living with the disorder much higher.
There is good news: depression is highly treatable. Each year we continue to learn more about mental health disorders and effective methods for treating them. Therapy is one such depression treatment.
Therapists use a range of therapeutic techniques to help their patients overcome depression.
Cognitive Behavioral Therapy (CBT)
Cognitive behavioral therapy, or CBT, helps an individual identify and change negative thoughts and associated behaviors.
People who suffer from depression often struggle with negative thought patterns. These thought patterns can influence our behavior. In turn, behavior reinforces the thought patterns. This creates a continual cycle of negative thoughts and depressed mood.
In many cases, our thought patterns are partly a result of our core beliefs. Therapists who use CBT help patients identify their core beliefs, address the negative thoughts that arise from them, and adjust their behavior accordingly.
Therapists who use CBT help patients identify their core beliefs, address the negative thoughts that arise from them, and adjust their behavior accordingly.
How Effective is CBT For Treating Depression?
There have been many studies that show CBT is an effective treatment for depression.
One study found that CBT was as effective as antidepressant medications in treating patients with depression. The same study also found that patients who completed the full course of CBT sessions were less likely to experience a relapse of their depression symptoms after treatment than those who received only medication.
Another recent study found that patients treated with CBT showed a marked improvement in their depression symptoms.
However, it’s important to note that some studies do find mixed results, and patients with the most severe symptoms also typically show the most improvement from therapy.
Dialectical Behavior Therapy (DBT)
Dialectical behavior therapy is very similar to CBT.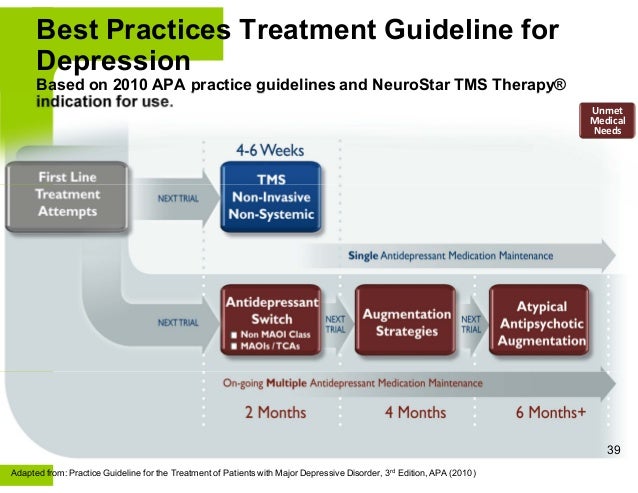 In fact, many of its techniques are based on it. However, DBT differs in that it teaches patients to identify, accept, and regulate their emotions.
In fact, many of its techniques are based on it. However, DBT differs in that it teaches patients to identify, accept, and regulate their emotions.
As the name implies, DBT helps patients engage in a “dialogue” with their emotions and behaviors. Patients are taught to challenge the contradictions in the attitudes and emotions that are preventing them from making positive changes in their life.
In other words, an individual learns to “talk back to” negative and self-defeating thoughts. During this process, they can begin to replace these thoughts and behaviors with positive ones.
DBT And Depression Treatment
DBT offers many benefits in treating depression. Studies have supported these benefits.
One study, published in a 2016 issue of Child and Adolescent Mental Health, reported an “improvement in depressive symptoms for adolescents following a course of DBT.” Additional studies show similar improvements for adults and even for the elderly.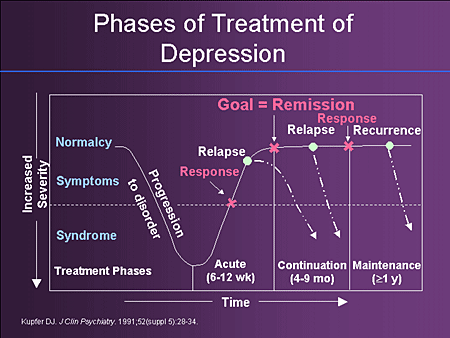
Behavioral Activation (BA)
Behavioral activation shares similarities with both CBT and DBT. Like these other types of therapy, BA focuses on a patient’s thoughts and behaviors.
Often, behavioral activation is used in conjunction with other therapeutic techniques to treat depression. BA helps patients adopt a long-term coping strategy by identifying specific goals and working toward meeting them.
When a person is depressed, they may try to avoid certain activities like social events. Therapists use behavioral activation to build positive reinforcement and help patients create an action plan to help them overcome avoidant behaviors.
The patient becomes increasingly confident and begins striving to meet realistic goals. As a result, a sense of positivity and accomplishment is reinforced. In turn, individuals begin to overcome depressive thoughts and behaviors.
Is Behavioral Activation Effective For Depression?
Behavioral activation is rarely used on its own. It’s more likely to be used alongside other therapeutic techniques as part of a holistic treatment plan.
It’s more likely to be used alongside other therapeutic techniques as part of a holistic treatment plan.
However, on its own, BA has been shown to help patients with mild to moderate levels of depression. Though, study authors note that the best results nonetheless come from a full-scale treatment.
It’s also important to note that behavioral activation is a relatively new therapy. This has led some studies to conclude more research must be done before the true efficacy of behavioral activation can be reported.
Problem-Solving Therapy (PST)
Problem-solving therapy is a therapeutic technique that helps individuals cope with life stressors that negatively impact their mental health.
We all experience stress, but major life stressors or chronic stress can take a heavy toll on our mental health. PST is designed to help people struggling with depression or anxiety identify and manage those stressors.
In practice, PST builds off of established techniques like adaptive problem-solving and mindfulness to help patients better understand and cope with stress.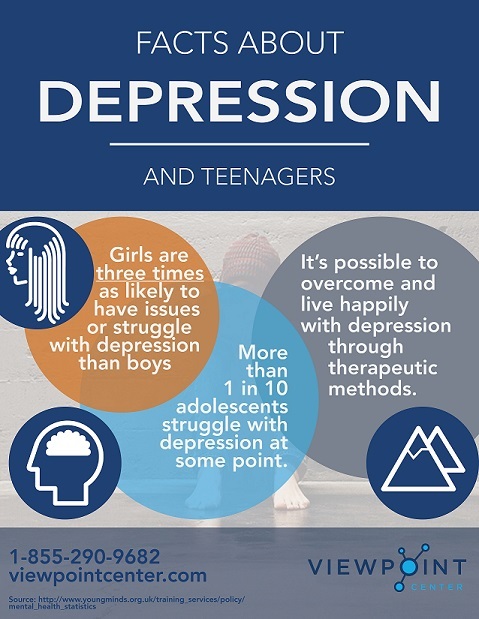 PST also helps patients to more effectively process negative emotions that can occur when we experience difficulties, like the loss of our job or the death of a loved one.
PST also helps patients to more effectively process negative emotions that can occur when we experience difficulties, like the loss of our job or the death of a loved one.
Interpersonal Therapy (IPT) For Depression
Interpersonal therapy was developed to help treat depression in adults. However, it has been increasingly used to treat other mental health disorders, as well.
IPT aims to help patients with mild to moderate depression address problems with interpersonal connections and improve relationships. Similar to problem-solving therapy, the focus of IPT is the patient’s actions and reactions.
Generally, IPT is time-limited, meaning treatment may only last for around 20 sessions. The length can vary based on the patient and their needs. During this time, the therapist and patient:
- Identify important interpersonal relationships in the patient’s life
- Address how these relationships affect their mental wellbeing
- Develop skills and strategies to improve these relationships
Studies have shown that IPT can have a positive impact for people suffering from depression. Although IPT may be more effective when incorporated into other forms of therapy, like CBT.
Although IPT may be more effective when incorporated into other forms of therapy, like CBT.
How Long Does Therapy Take For Treating Depression?
Each individual and their symptoms are different. Likewise, the treatment for their depression will vary based on their needs. In short, there’s no one-size-fits all approach to therapy or mental health treatment. However, the American Psychological Association states, “on average 15 to 20 sessions are required for 50 percent of patients to recover as indicated by self-reported symptom measures.”
The length of time a patient requires therapy to help treat their depression will depend on a number of factors:
- Severity of depression and symptoms
- Co-occurring disorders (such as anxiety, eating disorders, or substance abuse)
- Patient adherence to therapy and treatment
- Frequency of therapy sessions
These are only some of the factors that can impact the effectiveness of therapy.
Is Therapy or Medication Better For Depression?
Every patient is unique. As such, it’s important to tailor treatment to the individual. Antidepressant medications have proven to be effective for individuals with moderate to severe depression. Likewise, therapy has been shown to be as effective as medication for some patients.
However, the reality is many patients with severe or chronic depression will benefit most from a combination of therapy and an antidepressant medicine. The challenge is finding the right medication and the right balance between treatments.
For this reason, people with more severe depression should work with their doctor and a team of licensed mental health professionals to develop a complete treatment plan.
It’s important to understand that recovery from any mental health disorder takes time. Therapy can last for many months, while finding the right medication can take several attempts.
Get Help For Depression From An Experienced Team
If you or a loved one is struggling with depression, it’s important that you find the right level of care. At High Focus Centers, our team is composed of licensed mental healthcare professionals with experience treating a range of disorders.
At High Focus Centers, our team is composed of licensed mental healthcare professionals with experience treating a range of disorders.
If you’re searching for help with depression, contact our staff online or call us by phone at (877) 792-6430.
Fighting depression: 10 modern drugs
{{if type === 'partner-stocks'}}
{{/if}}
{{/if}} {{each list}}${this} {{if isGorzdrav}}
Delete
{{/if}}
{{/each}} {{/if}} Search by drug, disease, substance: DERMAKOSMETIKA, SOLGAR, NaturAge, Voltaren, KagocelHome
Articles
Fighting depression: 10 modern drugs
Depression is an urgent problem, the number of visits to doctors is growing every year. It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
What is meant by
depression Doctors have known it since ancient Greece and Egypt. Hippocrates described it as melancholy - a condition that is accompanied by anxiety, despondency, insomnia, refusal of food, irritability. Most often, the cause is childhood trauma or severe, frequent stress in adulthood. There are many provoking factors: the death of a loved one, deterioration of living conditions, alcoholism, brain diseases. Such cases are referred to as psychogenic depression.
Such cases are referred to as psychogenic depression.
The second type is endogenous. The problem appears not from large external shocks, but because of internal causes. A person is constantly dissatisfied with himself, subjecting himself to criticism. Many patients have panic attacks , haunted by a feeling of fear, anxiety.
How long the period of depression lasts
Many people mistake ordinary periods of low mood for depression. If they do not last long and are quickly replaced by periods of recovery, then we are not talking about a depressive state. The problem is obvious when the symptoms persist for months and dramatically change a person's life. Then you need to see a doctor.
What happens to the body
The most common theory is that there is a malfunction of neurotransmitters located in the brain. These substances transmit signals from neuron to neuron and are responsible for a person's mood. Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
How is
treated depressionDepression has been treated in different ways. In the ancient world - emetics and laxatives. In the Renaissance - wine and sunbathing. In the Age of Enlightenment - external stimuli, for example, insects. The 19th century brought new recipes - in particular, a solution of camphor in tartaric acid. The treatment also included the use of drugs, which are now no longer allowed for sale, and some are recognized as narcotic.
Obviously, all these drugs had no effect on increasing the amount of serotonin. And the treatment is precisely to normalize its production. This was done after creating modern antidepressants , which have a minimum of side effects, are safe for the body and are not addictive. These are medicines, whose action is aimed specifically at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
These are medicines, whose action is aimed specifically at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
Prescription
If a healthy person takes antidepressants , there will be no effect . For a depressed patient, taking them will help:
- improve psychological state;
- get rid of irritability;
- panic fear;
- increase mental and physical activity;
- overcome the dreary mood.
Psychiatrists prescribe antidepressants for chronic back pain, headaches. And also with irritable bowel syndrome, incontinence and other cases when the body stops producing its own painkillers. Medication helps restore pain suppression mechanisms.
These drugs can only be taken with a doctor's prescription, as many of them are strong stimulants. Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Precautions
- Prescribed drug start drinking from a small dose - the first couple of days they take a quarter of a tablet. Gradually increase the dose to normal. So the body adapts better. Finish the course by reducing the dose.
- The first effect of appears only 2 weeks after the start of administration. Sustained action - after six months. All this time, you need to take remedy, without making passes, breaks.
-
Products are not combined with melatonin, St. John's wort, products and dietary supplements based on sibutramine, 5-HTP. Their combination can raise serotonin to dangerous levels.
 Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account.
Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account. - Drinking antidepressants is better in parallel with visits to a psychotherapist. If the drugs normalize the biochemical processes in the body, then this doctor will help normalize the psychological state after depression.
The best antidepressants
In medicine, they have long argued that some drugs give only a placebo effect. The purpose of the study was to find out which of them are the most effective and valid . The project involved 116 thousand patients, and its results were published by the authoritative edition of the Lancet. We offer a list of the best.
1. Agomelatine
New generation drug. Agomelatine is used for severe depressive disorders, high levels of anxiety. Enhances the release of dopamine and norepinephrine, stimulates melatonin receptors. The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
Pros
+ Does not adversely affect attention and memory.
+ No lethargy during the day.
+ No sexual deviations.
+ No relation to blood pressure.
+ Do not reduce dosage upon discontinuation.
Cons
— In 1-10% of cases, increased sweating, diarrhea, constipation.
- Possible increased fatigue, drowsiness.
- There are no evidence-based safety studies in people with renal or hepatic insufficiency, therefore, such patients are advised to refrain from taking drugs with active ingredient agomelatine.
2. Amitriptyline
Tricyclic antidepressant. Moreover, the World Health Organization considers Amitriptyline the most reliable in this group. The standard dose is 200-250 mg / day. The action is to block the reuptake of neurotransmitters. A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
Pluses
+ Preparations with active ingredient amitriptyline are inexpensive.
+ High reliability, minimum side effects.
+ Relatively safe during breastfeeding.
Cons
- Possible side effect in the form of blurred vision, dry mouth.
- Lowering blood pressure.
- Some patients experience constipation.
- Drowsiness.
3. Escitalopram
It belongs to the group of modern serotonin reuptake inhibitors (SSRIs). Most often, it is recommended to take for anxiety, panic attacks. It is taken once, the standard dose is 10 mg per day. Escitalopram has a milder effect and is prescribed to patients for whom tricyclic drugs are contraindicated.
Pluses
+ Lasting effect comes after 3 months.
+ Indicated for patients with disorders of the cardiovascular system.
+ Soft action.
Cons
- In some patients, the functions of the gastrointestinal tract are disturbed, which is most often expressed in diarrhea.
- Anxiety may increase during the first 2 weeks, therefore it is recommended to start treatment with low doses and gradually increase them.
- Contraindicated in pregnancy and lactation.
4. Mirtazapine
A drug of the tetracyclic group. Mirtazapine - good stimulant for anxious depressions, has a moderate sedative effect. The average amount is 30 mg / day, it must be consumed once. Usually it is prescribed to patients who lose interest in life, cease to experience joy, pleasure. Effective in the correction of sleep, in particular, early awakenings.
Pros
+ Earlier onset of action than SSRIs (1 week).
+ Works well with most general medicines.
+ Full effect in 4 weeks.
+ Does not affect sexual function.
Cons
- The active substance mirtazapine is contraindicated in diabetes mellitus, arterial hypotension, increased intraocular pressure.
— During the appointment, you must drive carefully and engage in potentially hazardous types of work.
- 18% of patients experience drowsiness, 15% dry mouth, 5% weight loss. Other side effects occur in 1-3% of cases.
5. Paroxetine
Belongs to the SSRI group, is used most often for severe anxiety, panic, social phobia, nightmares, stress after trauma. Paroxetine can resolve the problems of anxious depression, anxiety-phobic disorders. Take once a day at a dose of 20 mg.
Pros
+ The most powerful stimulant among SSRIs.
+ Anxiety and insomnia pass quickly.
+ Minimal side effects in the form of vomiting, diarrhea.
+ Suitable for patients with cardiovascular problems.
Cons
— Not suitable for patients with severe motor, mental inhibition.
- Reduces libido.
- Harmful to the fetus when taken during pregnancy.
6. Fluoxetine
One of the most commonly used antidepressants in the SSRI group. Known as Prozac. Fluoxetine is also known as a good mood stimulant. Patients have a feeling of fear, tension, anxiety, gloomy dislike for others. Depending on the indications, the average daily dose is 20-60 mg.
Pluses
+ There is practically no effect on the work of the heart.
+ Does not cause sedation.
+ Effective for patients with motor retardation and excessive daytime sleepiness.
Cons
- May cause weight loss.
— Hypoglycemia is possible in diabetes mellitus.
- Contraindicated in severe renal impairment.
7. Fluvoxamine
Another SSRI drug. Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Pros
+ Lower price than traditional Prozac.
+ Faster action than him.
+ Relatively minor side effects (diarrhea, dry mouth, drowsiness).
Cons
- Contraindicated in diabetes.
- Pregnant women - with caution, lactation - prohibited.
- Causes nausea in some patients.
8. Sertraline
One of the widely used and universal drugs of the SSRI group. They treat almost any depressive condition, panic disorder, social phobia. However, in severe clinical cases, sertraline may not be effective enough. The standard dose is 50 mg/day.
Pros
+ No cardiotoxicity.
+ The patient's psychomotor activity does not change.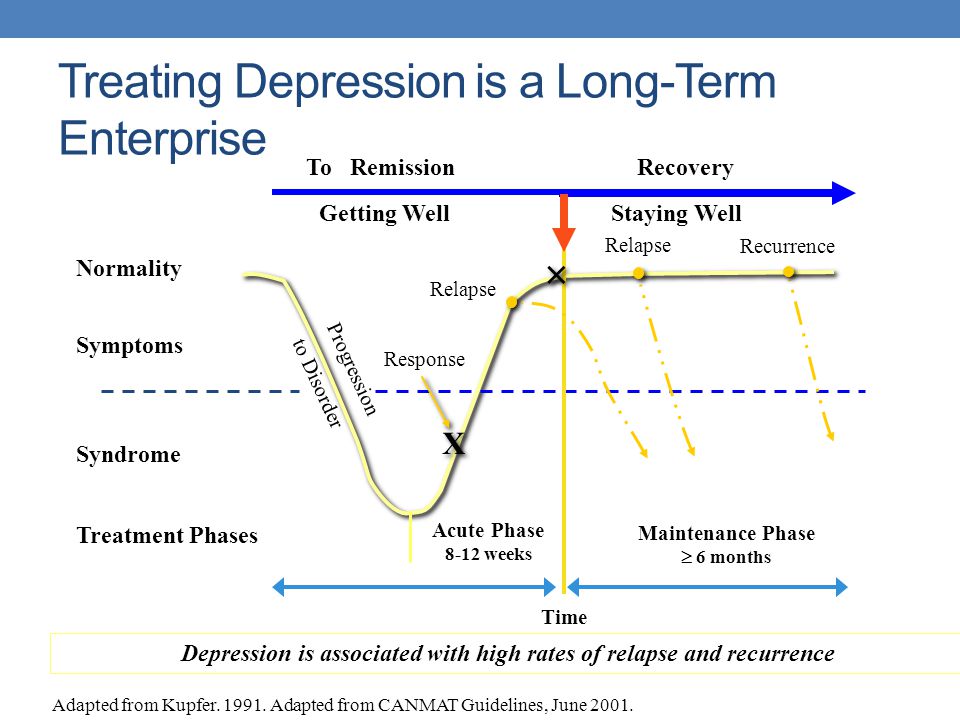
+ Does not increase body weight.
+ Combines well with other groups of antidepressants.
Cons
— In the first 2 weeks there may be problems with sleep, diarrhea.
- Side effects of a sexual nature.
- Contraindicated in pregnant women.
9. Escitalopram
The drug is classified as an SSRI. Its difference is in its effectiveness in depression, which is accompanied by involuntary movements (tic, tremor, chewing, smacking). Escitalopram is prescribed to patients with panic, anxiety, phobias, obsessive thoughts or actions. The daily dose is 20 mg.
Pluses
+ Effective in tardive dyskinesia.
+ One of the most powerful SSRIs.
+ More pronounced thymoleptic effect (improvement of mood) compared to many antidepressants of the same group.
Cons
- In some patients, anxiety increases within 2 weeks after starting treatment.
— Gastrointestinal disorders, insomnia, agitation are possible.
— Use during pregnancy only in extreme cases, incompatible with feeding.
10. Venlafaxine
Belongs to the SNRI group. In addition to blocking the reuptake of serotonin, venlafaxine has a similar effect on another neurotransmitter, norepinephrine. The medicine is prescribed for depressive conditions of various origins, social phobias, anxiety, panic. Usually take 150 mg per day.
Pros
+ Better tolerated by patients than most tricyclics.
+ More pronounced effect than classic SSRIs.
+ Fewer contraindications.
Cons
- Traditional side effects of most antidepressants: nausea, drowsiness, dry mouth, diarrhea or constipation.
- May increase eye pressure.
- The most severe withdrawal syndrome among antidepressant drugs.
This list is not to be used as a recommendation. In any case, consult your doctor before purchasing. Be healthy!
Depression Treatment in St.
 Petersburg | ICh RAS
Petersburg | ICh RAS Treatment of patients with depression at the Clinic of the Institute of Human Chemistry RAS
Complex forms of depression put a person to bed, blocking the sun's rays and the blue sky from him. All the colors of life fade, there is a desperate hopelessness and oppressive anxiety. The patient does not leave the house, refuses to eat, he has thoughts of suicide. According to statistics, depression affects about 20% of the population in developed countries of the world. Most people are not well aware of the characteristic manifestations and consequences of this disease. Therefore, many patients seek qualified help at a depression treatment clinic when the condition becomes severe.
Symptoms of depression
Depression is not temporary mood swings that every person experiences on a daily basis. This is a serious disorder that requires the mandatory intervention of a doctor. In a depressed state, a person has negative thoughts, a pessimistic outlook on life, a feeling of hopelessness arises, and joy disappears.
One should be on guard when depression does not go away and begins to affect all areas of life:
- psycho-emotional state affects working capacity;
- there are problems in communication;
- there are constant conflicts in the family;
- markedly reduced self-esteem;
- there are thoughts about leaving life.
An important condition for effective treatment of depression is timeliness. The sooner a person turns to a specialist, the faster he will overcome the disease. Today, psychiatry has a whole arsenal of methods to combat depression.
In addition to the main ones, there are other methods of treatment. These are phototherapy, homeopathy, sleep deprivation, electroconvulsive therapy, insulin therapy. The doctor can prescribe physiotherapy, massage, hirudotherapy, acupuncture, give recommendations on changing lifestyle and nutrition. It is believed that greater effectiveness of treatment is achieved by combining psychotherapy, pharmacotherapy and other methods.