Depersonalization derealization disorder symptoms
Depersonalization-derealization disorder | Sparrow
Overview
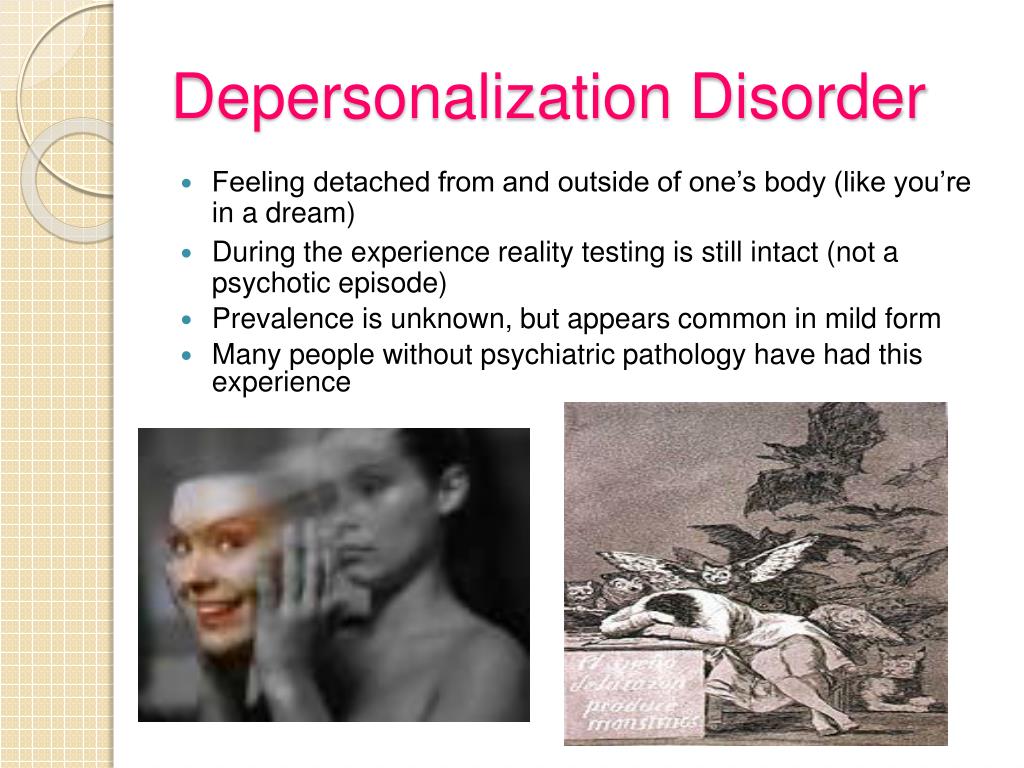
Depersonalization-derealization disorder occurs when you persistently or repeatedly have the feeling that you're observing yourself from outside your body or you have a sense that things around you aren't real, or both. Feelings of depersonalization and derealization can be very disturbing and may feel like you're living in a dream.
Many people have a passing experience of depersonalization or derealization at some point. But when these feelings keep occurring or never completely go away and interfere with your ability to function, it's considered depersonalization-derealization disorder. This disorder is more common in people who've had traumatic experiences.
Depersonalization-derealization disorder can be severe and may interfere with relationships, work and other daily activities. The main treatment for depersonalization-derealization disorder is talk therapy (psychotherapy), although sometimes medications also are used.
Symptoms
Persistent and recurrent episodes of depersonalization or derealization or both cause distress and problems functioning at work or school or in other important areas of your life. During these episodes, you are aware that your sense of detachment is only a feeling and not reality.
The experience and feelings of the disorder can be difficult to describe. Worry about "going crazy" can cause you to become preoccupied with checking that you exist and determining what's actually real.
Symptoms usually begin in the mid- to late teens or early adulthood. Depersonalization-derealization disorder is rare in children and older adults.
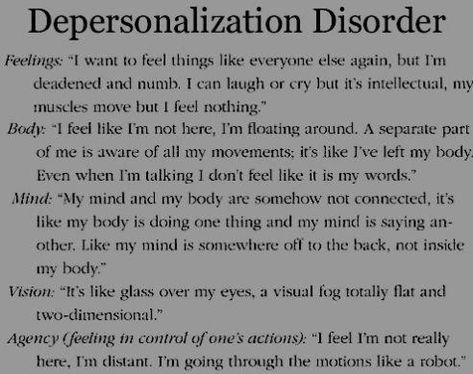
Depersonalization symptoms
Symptoms of depersonalization include:
- Feelings that you're an outside observer of your thoughts, feelings, your body or parts of your body — for example, as if you were floating in air above yourself
- Feeling like a robot or that you're not in control of your speech or movements
- The sense that your body, legs or arms appear distorted, enlarged or shrunken, or that your head is wrapped in cotton
- Emotional or physical numbness of your senses or responses to the world around you
- A sense that your memories lack emotion, and that they may or may not be your own memories
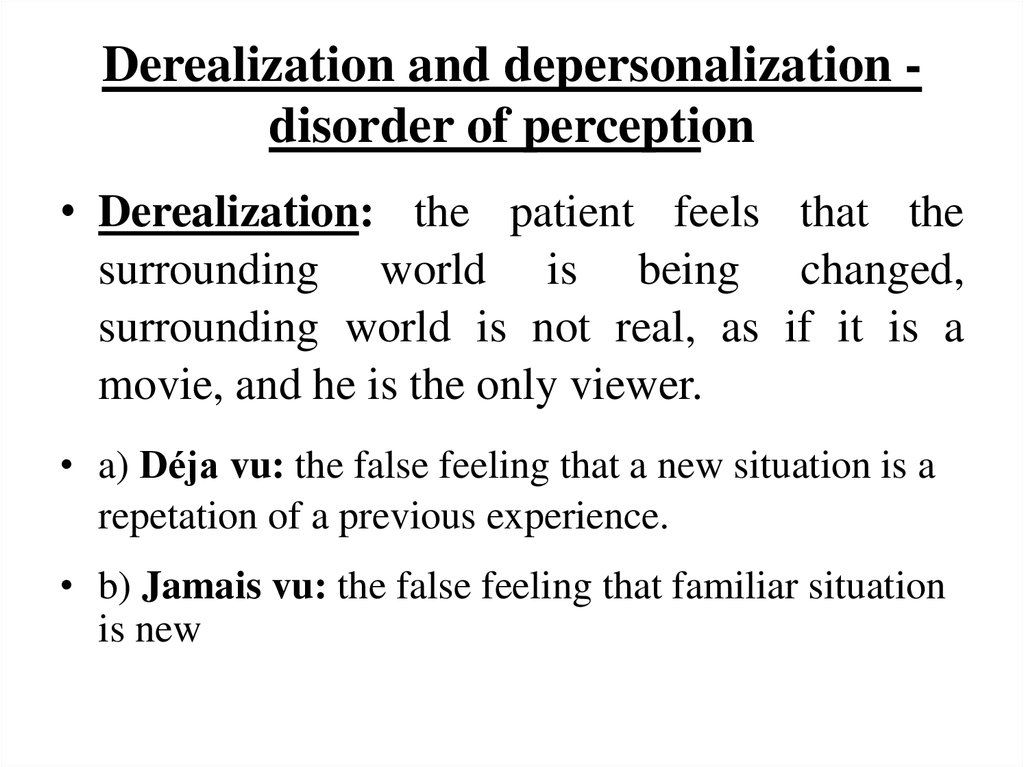
Derealization symptoms
Symptoms of derealization include:
- Feelings of being alienated from or unfamiliar with your surroundings — for example, like you're living in a movie or a dream
- Feeling emotionally disconnected from people you care about, as if you were separated by a glass wall
- Surroundings that appear distorted, blurry, colorless, two-dimensional or artificial, or a heightened awareness and clarity of your surroundings
- Distortions in perception of time, such as recent events feeling like distant past
- Distortions of distance and the size and shape of objects
Episodes of depersonalization-derealization disorder may last hours, days, weeks or even months at a time.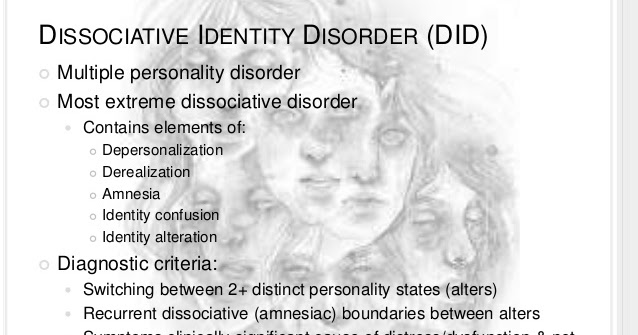 In some people, these episodes turn into ongoing feelings of depersonalization or derealization that may periodically get better or worse.
In some people, these episodes turn into ongoing feelings of depersonalization or derealization that may periodically get better or worse.
When to see a doctor
Passing feelings of depersonalization or derealization are common and aren't necessarily a cause for concern. But ongoing or severe feelings of detachment and distortion of your surroundings can be a sign of depersonalization-derealization disorder or another physical or mental health disorder.
See a doctor if you have feelings of depersonalization or derealization that:
- Are disturbing you or are emotionally disruptive
- Don't go away or keep coming back
- Interfere with work, relationships or daily activities
Causes
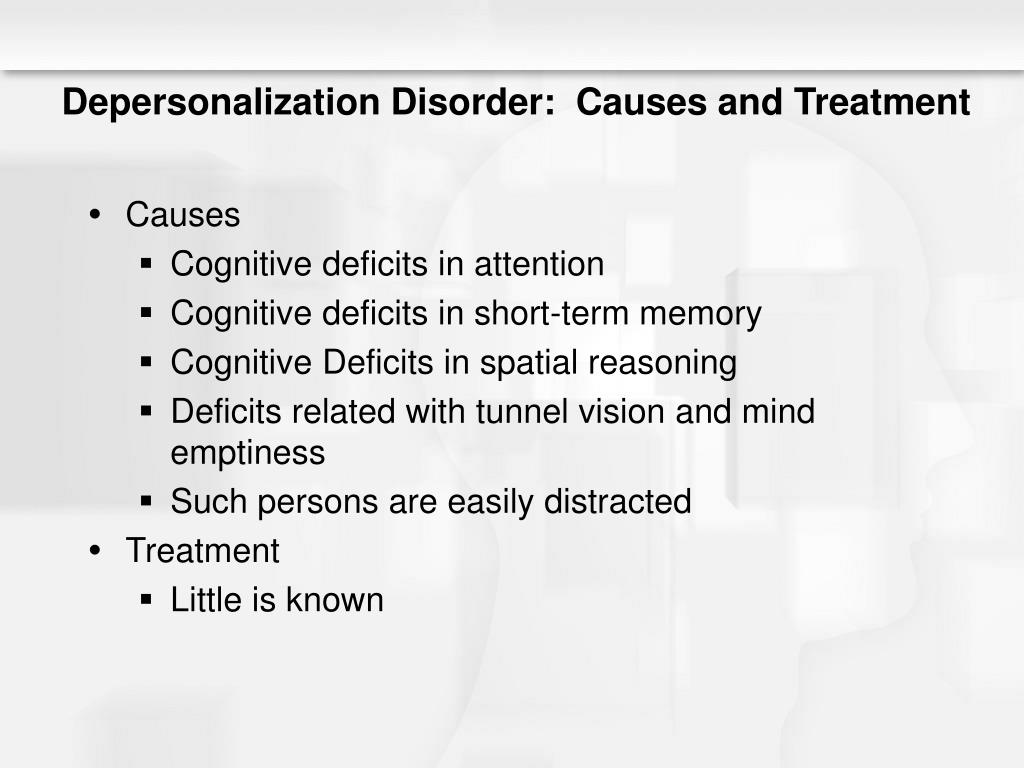
The exact cause of depersonalization-derealization disorder isn't well-understood. Some people may be more vulnerable to experiencing depersonalization and derealization than others, possibly due to genetic and environmental factors. Heightened states of stress and fear may trigger episodes.
Symptoms of depersonalization-derealization disorder may be related to childhood trauma or other experiences or events that cause severe emotional stress or trauma.
Risk factors
Factors that may increase the risk of depersonalization-derealization disorder include:
- Certain personality traits that make you want to avoid or deny difficult situations or make it hard to adapt to difficult situations
- Severe trauma, during childhood or as an adult, such as experiencing or witnessing a traumatic event or abuse
- Severe stress, such as major relationship, financial or work-related issues
- Depression or anxiety, especially severe or prolonged depression, or anxiety with panic attacks
- Using recreational drugs, which can trigger episodes of depersonalization or derealization
Complications
Episodes of depersonalization or derealization can be frightening and disabling.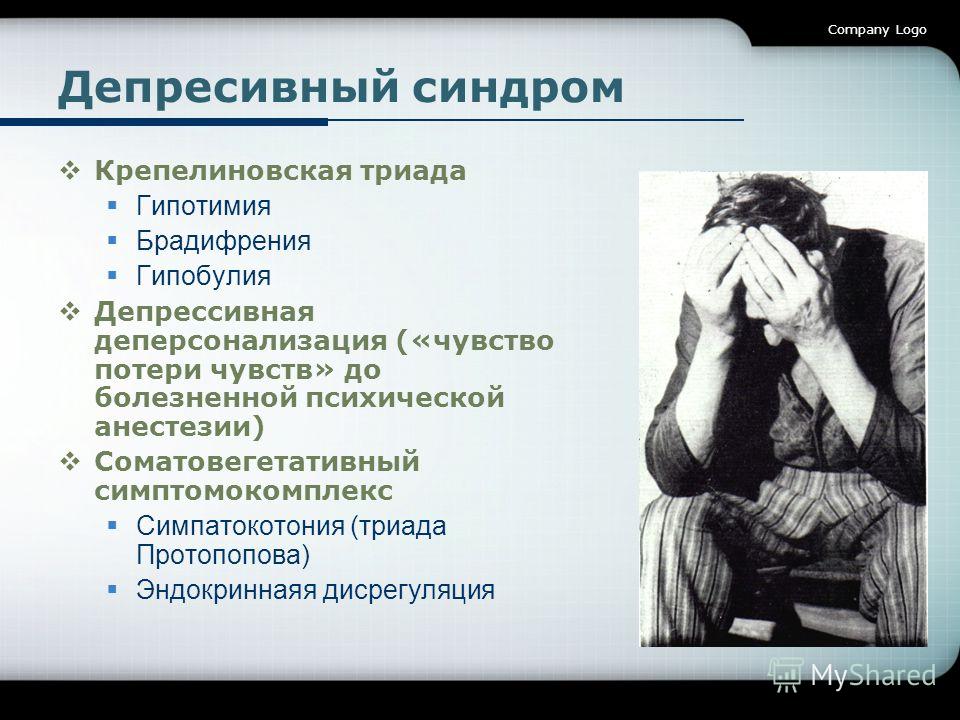 They can cause:
They can cause:
- Difficulty focusing on tasks or remembering things
- Interference with work and other routine activities
- Problems in relationships with your family and friends
- Anxiety or depression
- A sense of hopelessness
Diagnosis
Your doctor may determine or rule out a diagnosis of depersonalization-derealization disorder based on:
- Physical exam. In some cases, symptoms of depersonalization or derealization may be linked to an underlying physical health problem, medications, recreational drugs or alcohol.
- Lab tests. Some lab tests may help determine whether your symptoms are related to medical or other issues.
- Psychiatric evaluation. Your mental health professional asks about your symptoms, thoughts, feelings and behavior patterns, which can help determine if you have depersonalization-derealization disorder or other mental health disorders.
- DSM-5. Your mental health professional may use the criteria for depersonalization-derealization disorder listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
Treatment
Treatment of depersonalization-derealization disorder is primarily psychotherapy. However, sometimes medications may be added to your treatment plan.
Psychotherapy
Psychotherapy, also called counseling or talk therapy, is the main treatment. The goal is to gain control over the symptoms so that they lessen or go away. Two such psychotherapies include cognitive behavioral therapy and psychodynamic therapy.
Psychotherapy can help you:
- Understand why depersonalization and derealization occur
- Learn techniques that distract from your symptoms and make you feel more connected to your world and feelings
- Learn coping strategies to deal with stressful situations and times of extreme stress
- Address the emotions related to past trauma you've experienced
- Address other mental health conditions such as anxiety or depression
Medications
There are no medications specifically approved to treat depersonalization-derealization disorder.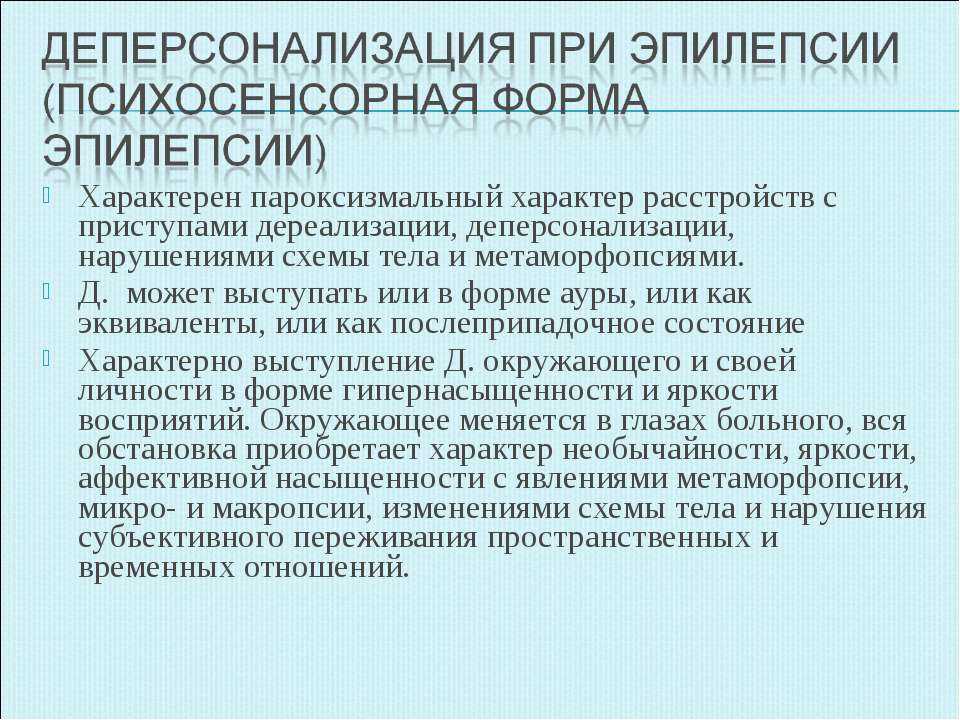 However, medications may be used to treat specific symptoms or to treat depression and anxiety that are often associated with the disorder.
However, medications may be used to treat specific symptoms or to treat depression and anxiety that are often associated with the disorder.
Coping and support
While depersonalization and derealization disorder can feel frightening, realizing that it's treatable may be reassuring. To help you cope with depersonalization-derealization disorder:
- Follow your treatment plan. Psychotherapy may involve practicing certain techniques on a daily basis to help resolve feelings of depersonalization and derealization. Seeking treatment early can improve your chances of successfully using these techniques.
- Learn about the condition. Books and internet resources are available that discuss why depersonalization and derealization occur and how to cope. Ask your mental health professional to suggest educational materials and resources.
- Connect with others. Stay connected with supportive and caring people — family, friends, faith leaders or others.

Preparing for an appointment
You're likely to start by first seeing your primary care doctor, but you may be referred to a doctor who specializes in brain and nervous system disorders (neurologist) or a doctor who specializes in diagnosing and treating mental health disorders (psychiatrist).
You may want to take a family member or friend along, if possible. Someone who accompanies you may remember something that you missed or forgot.
Here's some information to help you get ready for your appointment and what to expect from your doctor.
What you can do
Before your appointment, make a list of:
- Any symptoms you're experiencing, including any that may seem unrelated to the reason for your appointment
- Key personal information, including any major stresses or recent life changes
- All medications, vitamins, herbs and other supplements that you're taking, including dosages
- Questions to ask your doctor
Some basic questions to ask your doctor include:
- What's the most likely cause of my symptoms?
- Are there other possible causes?
- Do I need any tests to confirm the diagnosis?
- What treatments are available? Which do you recommend?
- Are there alternatives to the primary approach that you're suggesting?
- Do I need to see a specialist?
- Is there a generic alternative to the medicine you're prescribing?
- Are there any brochures or other printed material that I can have? What websites do you recommend?
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Be ready to answer them to reserve time to go over any points you want to spend more time on. Your doctor may ask:
Be ready to answer them to reserve time to go over any points you want to spend more time on. Your doctor may ask:
- When did you first begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What appears to worsen your symptoms?
- Do you have any long-term (chronic) health conditions?
- Do you have any mental health disorders, such as anxiety, depression or post-traumatic stress disorder (PTSD)?
- What medications or herbal supplements do you take?
- Do you drink alcohol or use recreational drugs?
Content From Mayo Clinic Updated:
© 1998-2023 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use
Symptoms, Causes, Treatment & Support
Depersonalization disorder is a mental health condition that’s now formally known as depersonalization-derealization disorder (DDD).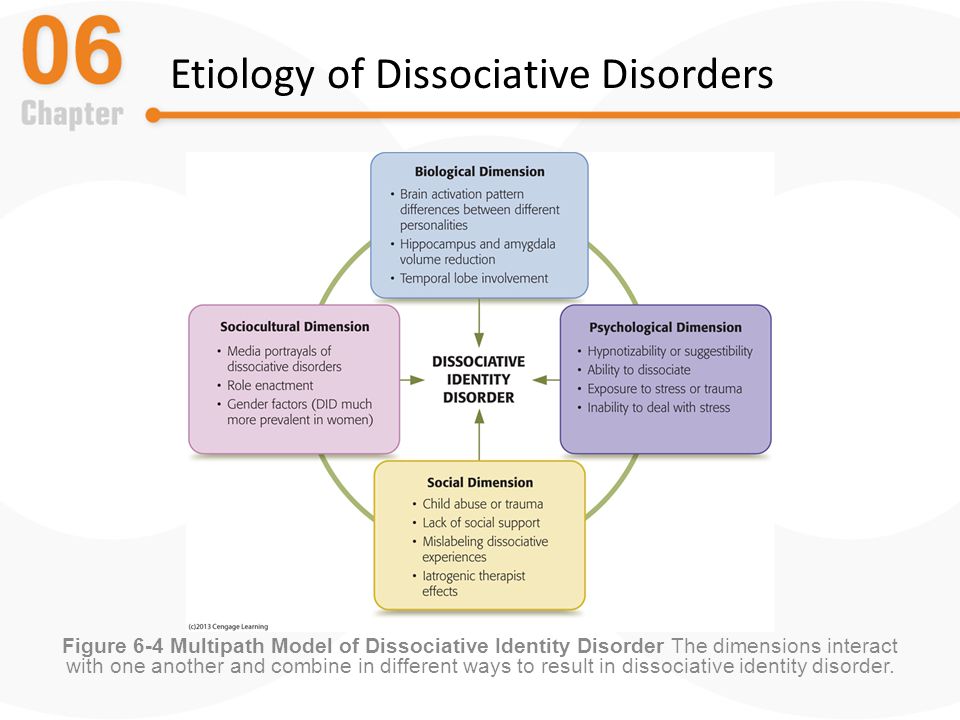
This updated name reflects the two major issues people with DDD experience:
- Depersonalization affects how you relate to yourself. It can make you feel as if you aren’t real.
- Derealization affects how you relate to other people and things. It can make you feel like your surroundings or other people aren’t real.
Together, these issues can leave you feeling distanced or disconnected from yourself and the world around you.
It’s not unusual to feel this way from time to time. But if you have DDD, these feelings can linger for long periods of time and get in the way of day-to-day activities.
Read on to learn more about DDD, including its symptoms and available treatment options.
DDD symptoms generally fall into two categories: symptoms of depersonalization and symptoms of derealization. People with DDD can experience symptoms of just one or the other or both.
Depersonalization symptoms include:
- feeling like you’re outside your body, sometimes as if you’re looking down on yourself from above
- feeling detached from yourself, as if you have no actual self
- numbness in your mind or body, as if your senses are turned off
- feeling as if you can’t control what you do or say
- feeling as if parts of your body are the wrong size
- difficulty attaching emotion to memories
Derealization symptoms include:
- having trouble recognizing surroundings or finding your surroundings hazy and almost dreamlike
- feeling like a glass wall separates you from the world — you can see what’s beyond but can’t connect
- feeling like your surroundings aren’t real or seem flat, blurry, too far, too close, too big, or too small
- experiencing a distorted sense of time — the past may feel very recent, while recent events feel as if they happened long ago
YOU’RE NOT ALONEFor many people, DDD symptoms are hard to put into words and communicate to others.
This can add to feeling like you don’t exist or are simply “going crazy.”
But these feelings are likely more common than you think. According to the most recent edition of the Diagnostic and Statistical Manual of Mental Disorders, close to 50 percent of adults in the United States will have an episode of depersonalization or derealization at some point in their lives, though only 2 percent meet criteria for a DDD diagnosis.
Read one person’s account of how it feels to experience depersonalization and derealization symptoms.
No one’s sure about the exact cause of DDD. But for some people, it seems to be linked to experiencing stress and trauma, especially at a young age.
For example, if you grew up around a lot of violence or yelling, you may have mentally removed yourself from those situations as a coping mechanism. As an adult, you might fall back on these disassociating tendencies in stressful situations.
Using certain drugs may also cause symptoms very similar to those of DDD in some people.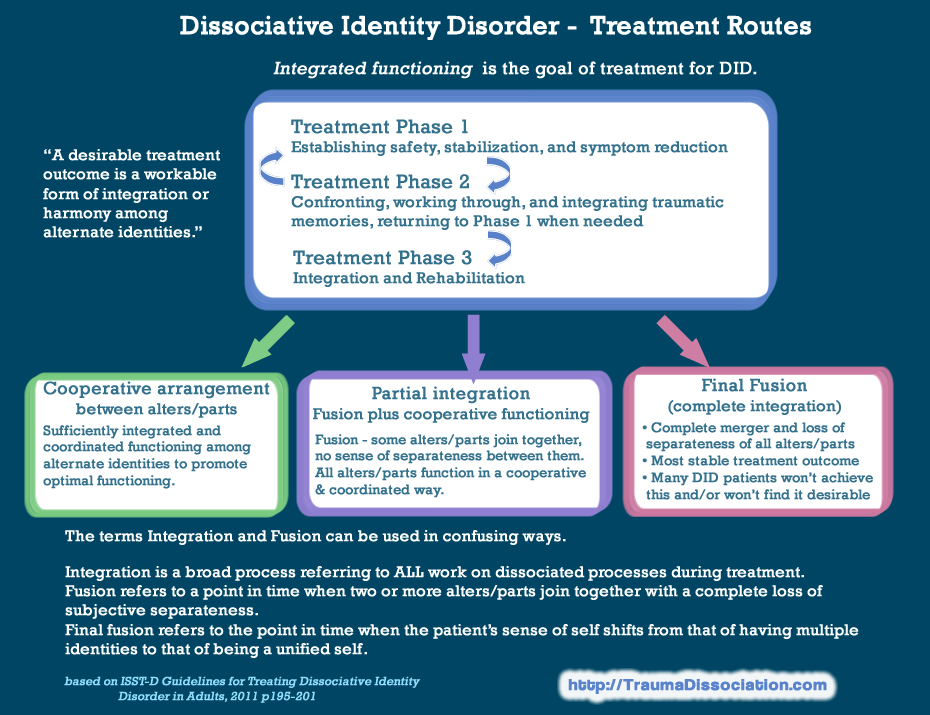 These drugs include:
These drugs include:
- hallucinogens
- MDMA
- ketamine
- salvia
- marijuana
A small 2015 study compared 68 people in recovery from substance use disorders who were abstinent for at least six months with 59 people who had never experienced a substance use disorder. More than 40 percent of those in recovery had at least mild symptoms of DDD.
Remember, it’s normal to feel a little “off” or removed from the world sometimes. But at what point do these feelings start to signal a mental health condition?
Generally, your symptoms may be a sign of DDD if they start to interfere with your daily life.
Before making a diagnosis of DDD, your primary care provider (PCP) will first ask if you:
- have regular episodes of depersonalization, derealization, or both
- are distressed by your symptoms
They’ll also likely ask you whether you’re aware of reality when you experience symptoms. People with DDD are generally aware that what they’re feeling isn’t quite real.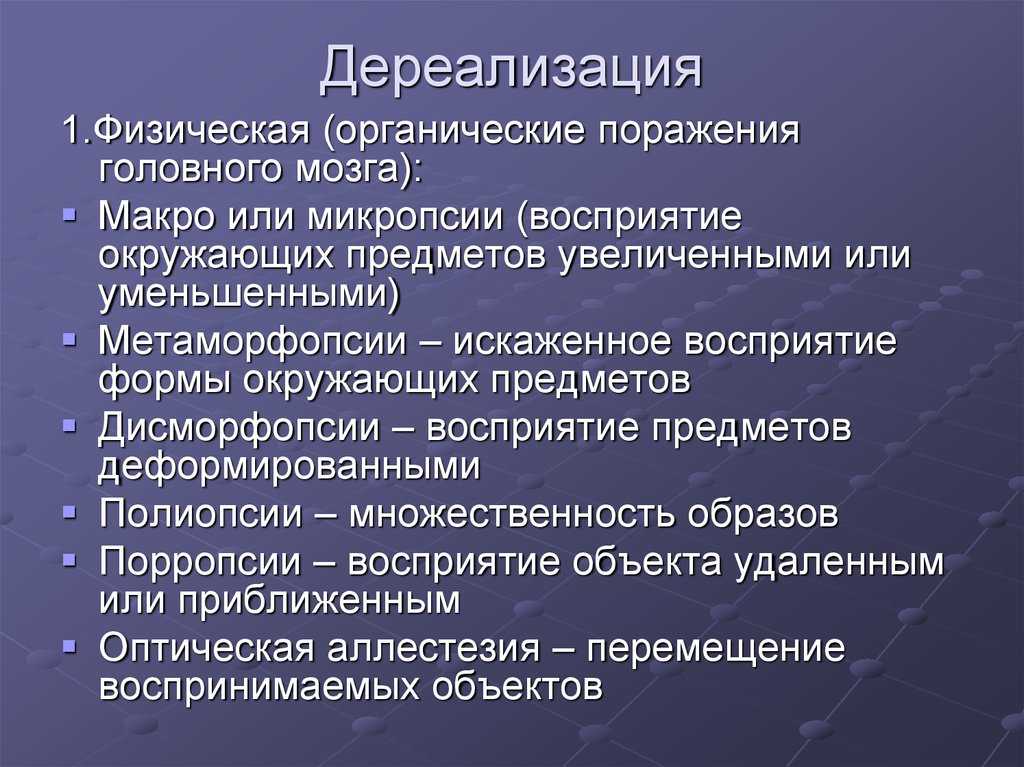 If you aren’t aware of reality in those moments, you may have another condition.
If you aren’t aware of reality in those moments, you may have another condition.
They’ll also want to confirm that your symptoms:
- can’t be explained by ingestion of prescribed or recreational drugs or a health condition
- aren’t caused by a different mental health condition, such as panic disorder, PTSD, schizophrenia, or another dissociative disorder
Keep in mind that mental health conditions can take some time to properly diagnose. To help the process along, make sure to tell your PCP about any other mental health conditions you have, especially depression or anxiety.
A 2003 study examining 117 cases of DDD found that people with DDD often also had depression, anxiety, or both.
The most effective treatment for DDD usually involves some type of therapy, especially psychodynamic therapy or cognitive behavioral therapy (CBT).
With the help of a therapist, you can learn about DDD, uncover and work through any past trauma or risk factors, and explore coping strategies to get through future episodes.
Concerned about the cost? Our guide to affordable therapy can help.
Finding a therapist can feel daunting, but it doesn’t have to be. Start by asking yourself a few basic questions:
- What issues do you want to address? These can be specific or vague.
- Are there any specific traits you’d like in a therapist? For example, are you more comfortable with someone who shares your gender?
- How much can you realistically afford to spend per session? Do you want someone who offers sliding-scale prices or payment plans?
- Where will therapy fit into your schedule? Do you need a therapist who can see you on a specific day of the week? Or someone who has nighttime sessions?
Once you’ve jotted down some notes about what you’re looking for, you can start to narrow in on your search. If you live in the United States, you can search for local therapists here.
quick tipIf you find yourself in a situation where you feel your symptoms starting to creep up on you, try engaging all of your senses.
This can help ground you in your body and surroundings.
Try:
- holding a few ice cubes
- smelling spices or an essential oil
- sucking on a hard candy
- listening to and singing along with a familiar song
For some, medication may also be helpful, but there isn’t a specific medication that’s known to treat DDD. Antidepressants may be helpful, especially if you also have underlying depression or anxiety.
But for some people, these can actually increase DDD symptoms, so it’s important to keep in close contact with your PCP or therapist about any changes in your symptoms.
Feeling disconnected from reality can be unsettling and overwhelming, especially if you experience it on a regular basis. You might start to think your symptoms will never go away.
In these situations, it can be helpful to connect with others facing similar issues. This is especially helpful between therapy appointments.
Consider joining an online support group, such as:
- DPSelfHelp.
 com, an online support group where people discuss depersonalization, including what’s worked for them and what hasn’t
com, an online support group where people discuss depersonalization, including what’s worked for them and what hasn’t - Facebook communities, including Depersonalization/Derealization Support Group and Depersonalization
If someone close to you is experiencing symptoms of DDD, there are several things you can do to offer support:
- Read up on the condition. If you’ve made it to this point in the article, you’re probably already doing this. There’s no need to become an expert on the subject, but having a little background info can help. This is especially true for DDD, as its symptoms are often hard for people experiencing them to put into words.
- Validate their experience. You can do this even if you don’t understand what they’re feeling. A simple “That must feel very uncomfortable, I’m sorry you’re dealing with this” can go a long way.
- Offer to go to a therapy session with them. During the session, you can learn more about the symptoms they experience or what triggers them.
 If they’re unsure about therapy, offering to join them for the first session may help.
If they’re unsure about therapy, offering to join them for the first session may help. - Understand it might be hard for them to reach out for help. It doesn’t hurt to make sure they know you’re available for support if they need you. Don’t assume silence means they don’t need or want help.
- Respect their boundaries. If they tell you they don’t want to talk about their symptoms or any past trauma, don’t push the subject or take it personally.
What are depersonalization and derealization and how to detect them
ContextAuthor: Polina Vernigor
Salvador Dali, Flesh on the Stones (1926) / Wikimedia
Perhaps at least once in your life you have felt that your body does not belong to you or that what is happening around you seems to be happening not to you and not really. These are quite common in society syndromes of depersonalization and derealization, which can manifest themselves both together and one by one. Due to similarities, the terms are often used together. Zaborona journalist Polina Vernigor figured out what are the signs of these symptoms, when to see a doctor, how to deal with it, and whether it is worth it.
Due to similarities, the terms are often used together. Zaborona journalist Polina Vernigor figured out what are the signs of these symptoms, when to see a doctor, how to deal with it, and whether it is worth it.
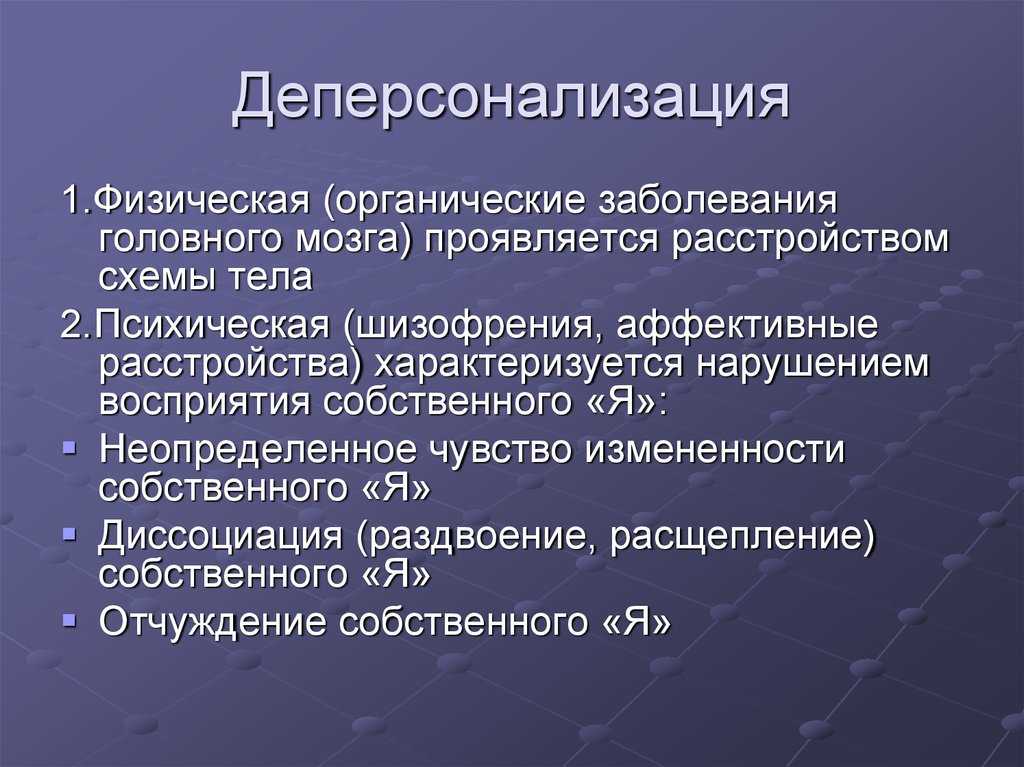
What is depersonalization and derealization?
In themselves they are symptoms. Like headache, dizziness or restlessness. But there is a disorder of depersonalization-derealization, which is already a full-fledged psychiatric diagnosis. The disorder itself occurs in only about 2% of the population, but at least 50% of people experience symptoms at least once in their lives.
As symptoms, depersonalization and derealization may indicate mental disorders (panic attack, phobias, post-traumatic stress disorder, depression, schizophrenia, borderline personality disorder, etc.) or neurological (convulsions, brain tumor, post-concussion syndrome, metabolic disorders, migraines, Meniere's disease, etc.). They can also occur as a reaction to stress or trauma, and are also found in people with alcohol or drug addiction.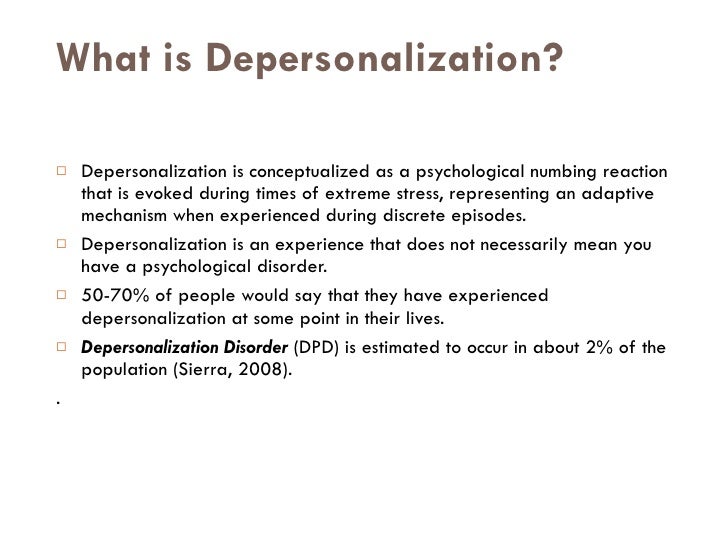
Almost always, these symptoms appear either in late childhood or early adulthood. On average, onset occurs at age 16, and 95% of cases are diagnosed before age 25. The first experience of depersonalization can be scary, as patients fear losing control and separating themselves from the rest of society. Most people with these symptoms misinterpret them as signs of severe psychosis or brain dysfunction. This usually leads to an increase in anxiety and obsessions, which contributes to the worsening of symptoms.
- Francisco Goya, Witches' Sabbat (1797-98) / Wikimedia
renamed Depersonalization/Derealization Disorder (DPDR). This diagnosis is classified as a dissociative disorder.
The latest International Classification of Diseases (ICD-11) reclassified DPDR as a disorder rather than a syndrome as before, and reclassified it as a dissociative disorder from the list of neurotic disorders.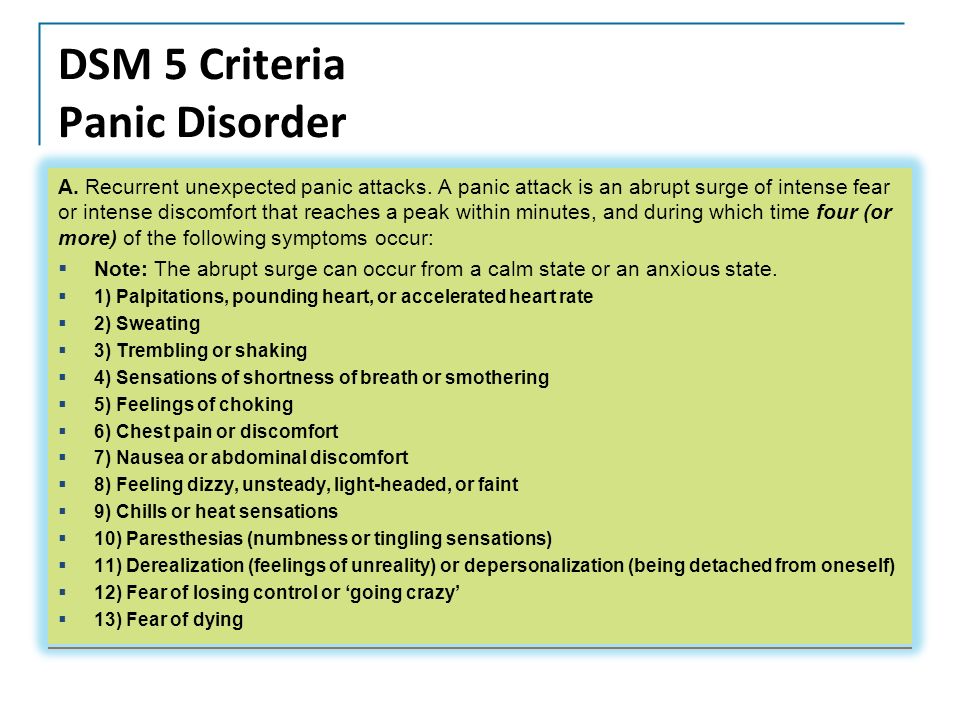 The description that is used in ICD-11 is similar to the criteria found in DSM-5.
The description that is used in ICD-11 is similar to the criteria found in DSM-5.
How do I know if I have depersonalization or derealization?
You can notice the symptoms yourself, but depersonalization-derealization disorder is a diagnosis that only a doctor can make. No laboratory tests reveal either the symptoms themselves or the disorder. To rule out the physical causes of these conditions, your doctor may order magnetic resonance imaging (MRI), electroencephalography (EEG), x-rays, or a urine test for toxic chemicals. If all these studies turn up nothing, then the cause is most likely mental states.
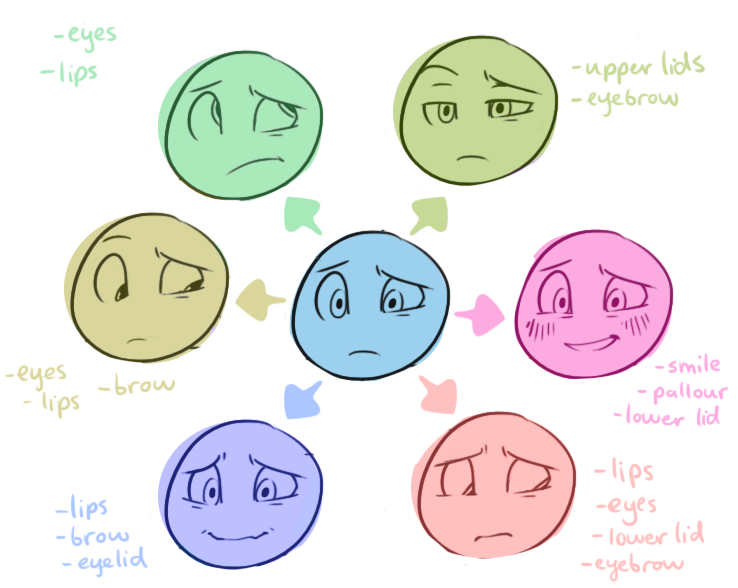
Signs of depersonalization:
- a feeling that you are watching your thoughts, feelings, body or parts of it from the outside - for example, as if you are floating in the air above you;
- feels like a robot and/or has no control over your speech and/or movements;
- your body or parts of it seem distorted, deformed, and your head seems to be wrapped in cotton wool;
- emotional or physical numbness of feelings or reactions to the environment;
- your memories lack emotion, and doubts arise whether they are really your memories.

- Henry Fuseli, Nightmare (1781) / Wikimedia
Signs of derealization:
- a feeling of alienation or ignorance of one's surroundings - for example, as if you are living in a movie or in a dream;
- emotional isolation from people close to you, as if you were separated by a glass wall;
- the environment appears distorted, blurry, colorless, two-dimensional or artificial;
- distortion in the perception of time, for example, recent events are perceived as the distant past;
- distortion of the distance, size and shape of objects.
Depersonalization-derealization disorder can be considered if these symptoms recur frequently and for a long time and are not the result of some other disease or disorder. In any case, if it drains you emotionally or interferes with your life, contact a specialist.
In any case, if it drains you emotionally or interferes with your life, contact a specialist.
What to do about it?
Very often, both the symptoms and the disorder do not require special treatment and go away on their own. But it depends on their nature and how much they bother you. For many patients, a full recovery is possible, especially if the symptoms are related to another disorder/disease that is being treated, or to stress that is being relieved. In other cases, depersonalization and derealization become more chronic and less noticeable. Even persistent or recurring symptoms can cause only minimal disturbance if you learn to perceive them correctly - for example, to focus on other thoughts or actions.
- Mikhail Vrubel, Demon Downcast (1901-02) / Wikimedia
If we still talk about the treatment of depersonalization-derealization disorder, then psychotherapy helps here. Treatment should take into account all the stresses associated with the onset of the disorder, as well as earlier traumas (eg, childhood abuse or neglect, physical, psychological or sexual abuse, etc.) that may cause patients to have a late onset of depersonalization and/or derealization. .
Treatment should take into account all the stresses associated with the onset of the disorder, as well as earlier traumas (eg, childhood abuse or neglect, physical, psychological or sexual abuse, etc.) that may cause patients to have a late onset of depersonalization and/or derealization. .
Different psychotherapeutic methods are successful for different patients. Cognitive techniques can help block intrusive thoughts about an unreal state of being. Behavioral techniques can help patients perform tasks that distract them from depersonalization and derealization. Grounding techniques use various senses (such as playing loud music or holding a block of ice) to help patients feel more real in the moment, and more connected to the body and surroundings. Psychodynamic Therapy helps patients cope with negative feelings, hidden conflicts or experiences that, due to accumulation, provoke symptoms.
Various preparations are also used, but none of them has been clearly proven to be effective. However, some patients benefit from selective serotonin reuptake inhibitors (SSRIs), opioid antagonists, anxiolytics, and stimulants. However, these drugs may work primarily by targeting other psychiatric disorders (eg, anxiety, depression) that cause depersonalization and/or derealization.
However, some patients benefit from selective serotonin reuptake inhibitors (SSRIs), opioid antagonists, anxiolytics, and stimulants. However, these drugs may work primarily by targeting other psychiatric disorders (eg, anxiety, depression) that cause depersonalization and/or derealization.
Polina Vernigor
Journalist
Polina VernigorWorthy of the material?
Support Zaborona on Patreon, so that we can publish more stories of the Church
Support Zaborona
Top
Depersonalization and derealization in Moscow
Depersonalization and derealization manifest themselves in the form of sensations when a person thinks that he is living in a dream or is watching himself from the outside.
Depersonalization and derealization are experienced by ordinary people, but usually these feelings are fleeting.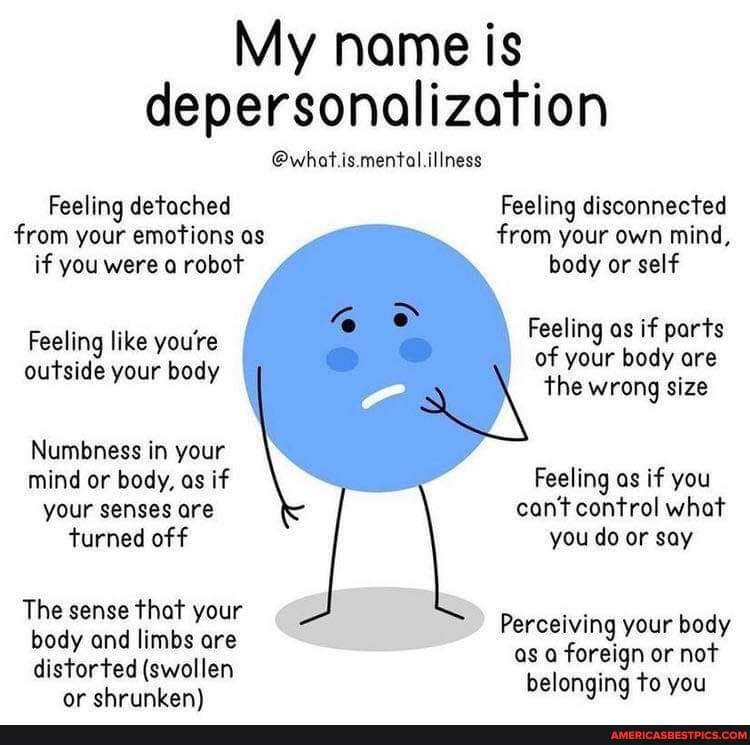 However, if they occur constantly or do not go to the end and affect the quality of life (they interfere with living a normal life), then it can be assumed that this is a disorder.
However, if they occur constantly or do not go to the end and affect the quality of life (they interfere with living a normal life), then it can be assumed that this is a disorder.
More common in people who have had a traumatic experience, or as a symptom of anxiety or depression.
Depersonalization-derealization disorder can be severe and interfere with relationships, work, and other daily activities. The main treatment for depersonalization-derealization disorder is talking therapy (psychotherapy), although drugs are sometimes used.
Symptoms of depersonalization
During derealization, a person feels like an outside observer of life:
-
Feeling that you are an outside observer of your thoughts, feelings, your body or parts of it - for example, as if you are floating in the air above you
-
Feeling like a robot or having no control over your speech or movements.

-
Sensation that your body, legs or arms seem distorted, enlarged or reduced, or that your head is wrapped in cotton.
-
Emotional or physical numbness of your senses or reactions to the world around you
-
The feeling that your memories are devoid of emotion and that they may or may not be your own memories.
Symptoms of derealization
The most common symptoms are "strange" sensations:
-
Feeling alienated from or "unfamiliar" with the outside world. It seems to a person that he lives in a movie or in a dream.
-
Feeling of emotional detachment from loved ones. It may seem to a person that a cold and impenetrable glass wall passes between him and his loved ones.
-
The world around you seems distorted, blurry, colorless, two-dimensional or artificial. Or, on the contrary, excessively clear.
-
Feeling that time goes "somehow wrong." Recent events may seem like events from a distant past.
-
Distortions in the perception of distance, size and shape of objects
These distortions can typically last for minutes, hours, days, weeks, or even months.
When to See a Doctor
Momentary feelings of depersonalization or derealization are common and not necessarily a cause for concern. However, persistent or strong feelings of detachment and distortion of the world around you, which impair the quality of life, may be a sign of an emotional disorder.
See a doctor if feelings of depersonalization or derealization:
-
disturbing
-
do not pass or constantly return
-
interfere with work, relationships, or daily activities.
Causes
The exact cause of depersonalization-derealization disorder has not been fully elucidated. Some people may be more prone to depersonalization and derealization than others, possibly due to genetic and environmental factors. An increased state of stress and fear, prolonged anxiety or depression can provoke seizures.
Symptoms of depersonalization-derealization disorder may be associated with childhood trauma or other experiences or events that caused severe emotional stress or trauma.
Causing factors
Factors that may increase the risk of developing depersonalization/derealization disorder include:
-
certain personality traits that cause you to avoid or deny difficult situations or make it difficult to adapt to difficult situations
-
Severe trauma in childhood or adulthood, such as a traumatic event or abuse.
-
Severe stress, such as serious relationship problems, financial problems, or work-related problems
-
Depression or anxiety, especially severe or prolonged depression, or anxiety with panic attacks
What are the risks?
Difficulty concentrating on tasks or remembering things
Interference in work and other daily activities
Relationship problems with family and friends
Anxiety or depression
Feeling of hopelessness
Diagnosis
Your doctor may diagnose or rule out depersonalization/derealization disorder based on:
-
physical examination.
 In some cases, symptoms of depersonalization or derealization may be related to an underlying physical health problem, medications, recreational drugs, or alcohol.
In some cases, symptoms of depersonalization or derealization may be related to an underlying physical health problem, medications, recreational drugs, or alcohol. -
Laboratory tests. Some lab tests can help determine if your symptoms are related to medical or other problems.
-
Specialized survey. A mental health professional will ask you about your symptoms, thoughts, feelings, and behaviors, which can help determine if you have depersonalization/derealization disorder or other mental disorders.
DSM-5. Your mental health professional may use the criteria for depersonalization-derealization disorder listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) published by the American Psychiatric Association.
Treatment
Treatment of depersonalization-derealization disorder is primarily psychotherapy.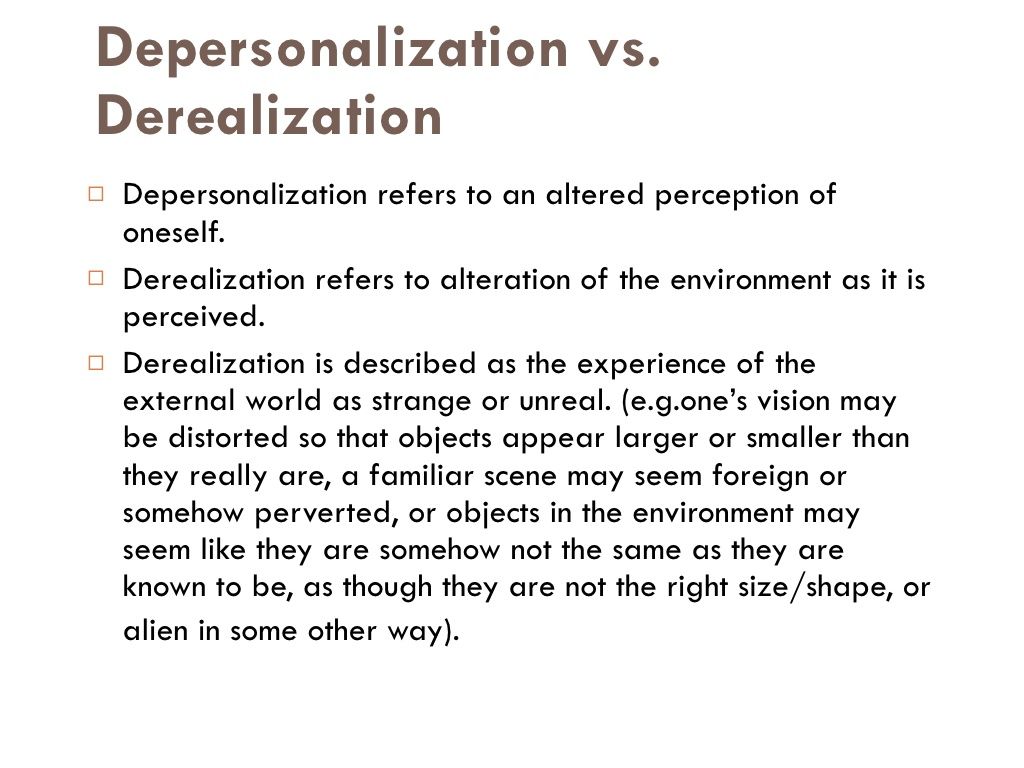 However, sometimes drugs may be added to the treatment plan.
However, sometimes drugs may be added to the treatment plan.
Psychotherapy
Psychotherapy is the main treatment for these symptoms. The goal of therapy is to control symptoms so that they decrease or disappear. Several types of evidence-based therapy are suitable for this - CBT (cognitive behavioral therapy) and ACT (acceptance and responsibility therapy).
How psychotherapy can help:
-
understand why depersonalization and derealization occur
-
learn techniques to help you take your mind off your symptoms and feel more connected to your world and feelings
-
learn coping strategies for stressful situations and times of high stress
-
Eliminate emotions associated with past traumas
-
Management of other mental disorders such as anxiety or depression.

Pharmacotherapy
There are no drugs specifically approved for the treatment of depersonalization/derealization disorder. However, medications may be used to reduce specific symptoms or to treat depression and anxiety, which often cause symptoms of derealization or depersonalization.
Request an appointment at Neuro-Psi Clinic
Treatment and support. Although depersonalization and derealization disorder can seem frightening, knowing that it is treatable can be reassuring. To help you deal with depersonalization/derealization disorder:
Follow your treatment plan . Psychotherapy may include daily practice of certain techniques to help deal with feelings of depersonalization and derealization. Seeking help early can increase your chances of successfully applying these techniques.
Check status.
In books and online resources you can find information about why depersonalization and derealization occur and how to deal with them. Ask your mental health professional for recommendations on educational materials and resources.
Connect with other people. Stay in touch with supportive and caring people - family, friends, religious leaders or others.
Preparing for your doctor's appointment
Make a list before you see your doctor:
-
Any symptoms you are experiencing, including any that may seem unrelated to the reason for your visit to the doctor
-
Key personal information, including any major stress or recent life changes
-
All medicines, vitamins, herbs and other supplements you take, including dosages.
Questions to ask your doctor
Key questions to ask your doctor include:
-
What is the most likely cause of my symptoms?
-
Are there other possible causes?
-
Do I need any tests to confirm the diagnosis?
-
What treatments are available? Which ones do you recommend?
-
Are there alternatives to the basic approach you propose?
-
Do I need to see another specialist?
-
Is there a generic alternative to the medicine you are prescribing?
What to expect from your consultation
Your doctor will likely ask you a number of questions.