Definition of antisocial personality
Antisocial personality disorder - NHS
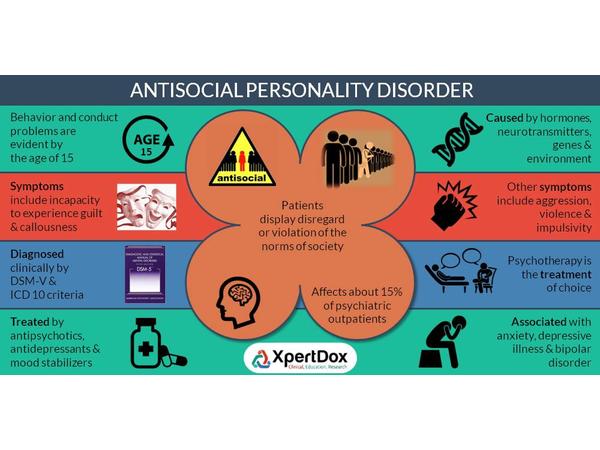
Personality disorders are mental health conditions that affect how someone thinks, perceives, feels or relates to others.
Antisocial personality disorder is a particularly challenging type of personality disorder characterised by impulsive, irresponsible and often criminal behaviour.
Someone with antisocial personality disorder will typically be manipulative, deceitful and reckless, and will not care for other people's feelings.
Like other types of personality disorder, antisocial personality disorder is on a spectrum, which means it can range in severity from occasional bad behaviour to repeatedly breaking the law and committing serious crimes.
Psychopaths are considered to have a severe form of antisocial personality disorder.
The Mind website has more information about signs of antisocial personality disorder
Find out more about personality disorders
Signs of antisocial personality disorder
A person with antisocial personality disorder may:
- exploit, manipulate or violate the rights of others
- lack concern, regret or remorse about other people's distress
- behave irresponsibly and show disregard for normal social behaviour
- have difficulty sustaining long-term relationships
- be unable to control their anger
- lack guilt, or not learn from their mistakes
- blame others for problems in their lives
- repeatedly break the law
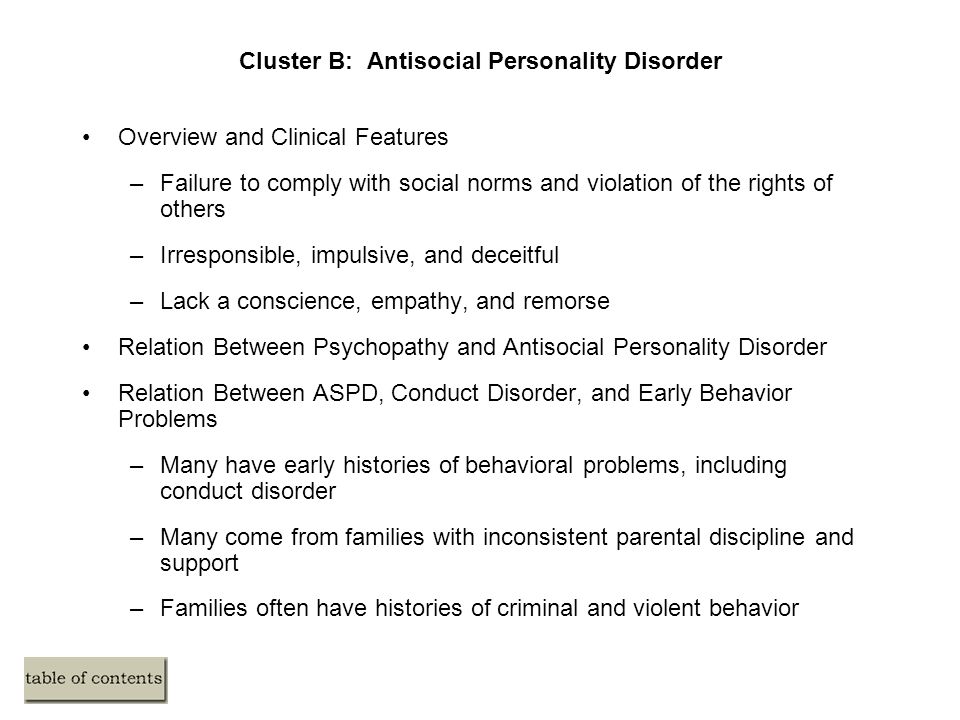
A person with antisocial personality disorder will have a history of conduct disorder during childhood, such as truancy (not going to school), delinquency (for example, committing crimes or substance misuse), and other disruptive and aggressive behaviours.
Who develops antisocial personality disorder?
Antisocial personality disorder affects more men than women.
It's not known why some people develop antisocial personality disorder, but both genetics and traumatic childhood experiences, such as child abuse or neglect, are thought to play a role.
A person with antisocial personality disorder will have often grown up in difficult family circumstances.
One or both parents may misuse alcohol, and parental conflict and harsh, inconsistent parenting are common.
As a result of these problems, social services may become involved with the child's care.
These types of difficulties in childhood will often lead to behavioural problems during adolescence and adulthood.
Effects of antisocial personality disorder
Criminal behaviour is a key feature of antisocial personality disorder, and there's a high risk that someone with the disorder will commit crimes and be imprisoned at some point in their life.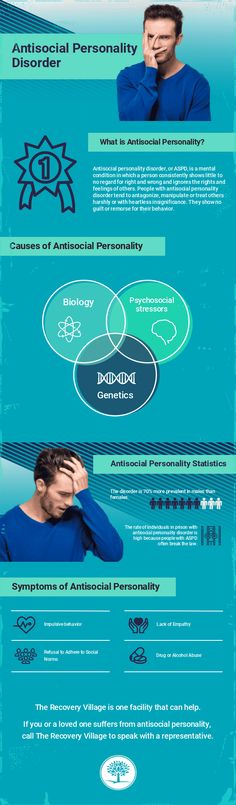
Men with antisocial personality disorder have been found to be 3 to 5 times more likely than women to misuse alcohol and drugs than those without the disorder. They also have an increased risk of dying prematurely as a result of reckless behaviour or attempting suicide.
People with antisocial personality disorder are also more likely to have relationship problems during adulthood and be unemployed and homeless.
Diagnosing antisocial personality disorder
To be diagnosed with antisocial personality disorder, a person will usually have a history of conduct personality disorder before the age of 15.
Antisocial personality disorder is diagnosed after rigorous detailed psychological assessment.
A diagnosis can only be made if the person is aged 18 years or older and at least 3 of the following criteria behaviours apply:
- repeatedly breaking the law
- repeatedly being deceitful
- being impulsive or incapable of planning ahead
- being irritable and aggressive
- having a reckless disregard for their safety or the safety of others
- being consistently irresponsible
- lack of remorse
These signs are not part of a schizophrenic or manic episode – they're part of a person's everyday personality and behaviour.
This behaviour usually becomes most extreme and challenging during the late teens and early 20s. It may improve by the time the person reaches their 40s.
Treating antisocial personality disorder
In the past, antisocial personality disorder was thought to be a lifelong disorder, but that's not always the case and it can sometimes be managed and treated.
Evidence suggests behaviour can improve over time with therapy, even if core characteristics such as lack of empathy remain.
But antisocial personality disorder is one of the most difficult types of personality disorders to treat.
A person with antisocial personality disorder may also be reluctant to seek treatment and may only start therapy when ordered to do so by a court.
The recommended treatment for someone with antisocial personality disorder will depend on their circumstances, taking into account factors such as age, offending history and whether there are any associated problems, such as alcohol or drug misuse.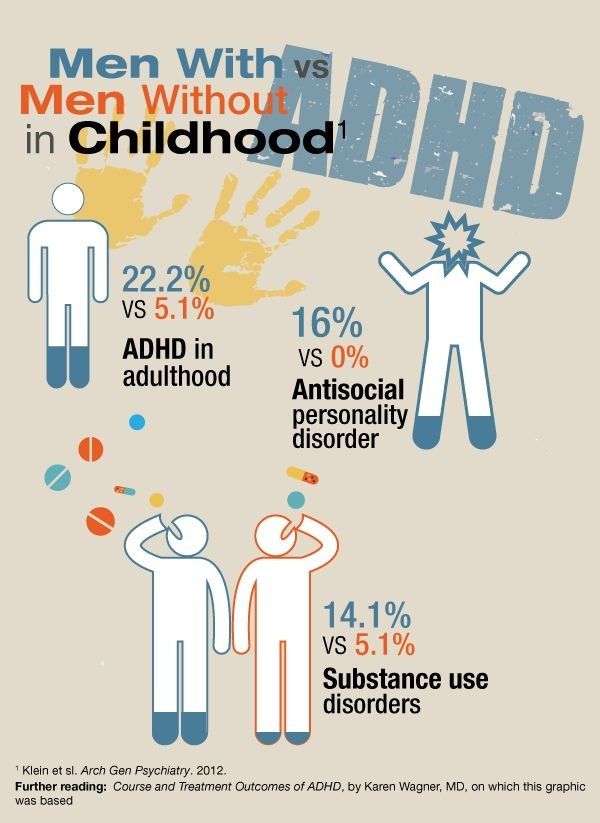
The person's family and friends will often play an active role in making decisions about their treatment and care.
Sometimes, substance misuse services and social care may also need to be involved.
National Institute for Health and Care Excellence (NICE): management and prevention of antisocial personality disorder
Talking therapies
Cognitive behavioural therapy (CBT) is sometimes used to treat antisocial personality disorder.
It's a talking therapy that aims to help a person manage their problems by changing the way they think and behave.
Mentalisation-based therapy (MBT) is another type of talking therapy that's becoming more popular in the treatment of antisocial personality disorder.
The therapist will encourage the person to consider the way they think and how their mental state affects their behaviour.
Democratic therapeutic communities (DTC)
Evidence suggests community-based programmes can be an effective long-term treatment method for people with antisocial personality disorder, and is becoming increasingly popular in prisons.
DTC is a type of social therapy that aims to address the person's risk of offending, as well as their emotional and psychological needs.
It's based around large and small therapy groups and focuses on community issues, creating an environment where both staff and prisoners contribute to the decisions of the community.
There may also be opportunities for educational and vocational work.
The recommended length of treatment is 18 months, as there needs to be enough time for a person to make changes and put new skills into practice.
Self-motivation is another important factor for acceptance on to this type of scheme. For example, the person must be willing to work as part of a community, participate in groups, and be subject to the democratic process.
For example, the person must be willing to work as part of a community, participate in groups, and be subject to the democratic process.
Read more about DTC and working with offenders with personality disorder on GOV.UK
Medicine
There's little evidence to support the use of medicine for treating antisocial personality disorder, but certain antipsychotic and antidepressant medicines may be helpful in some instances.
Carbamazepine and lithium may help control symptoms such as aggression and impulsive behaviour, and a class of antidepressant called selective serotonin reuptake inhibitors (SSRIs) may improve anger and general personality disorder symptoms.
Further information
- Personality disorders
Antisocial Personality Disorder - StatPearls
Continuing Education Activity
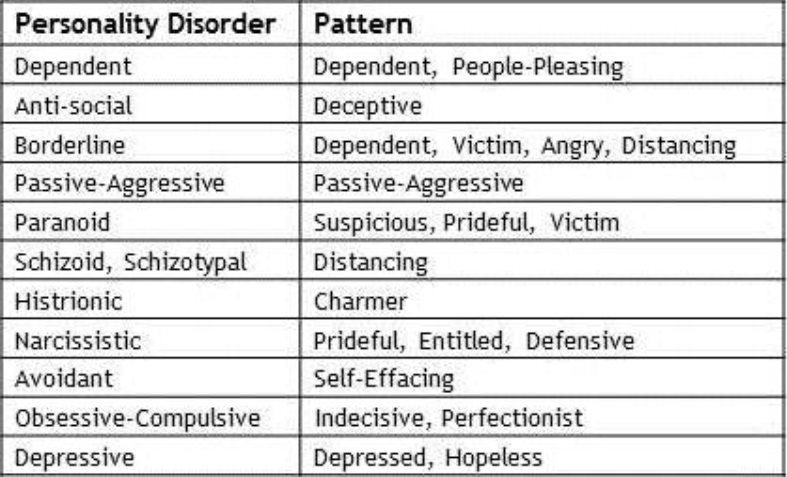
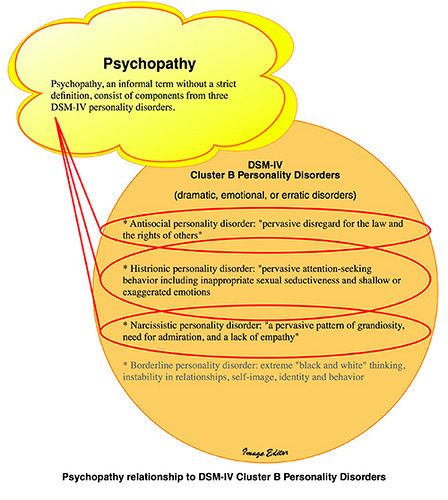
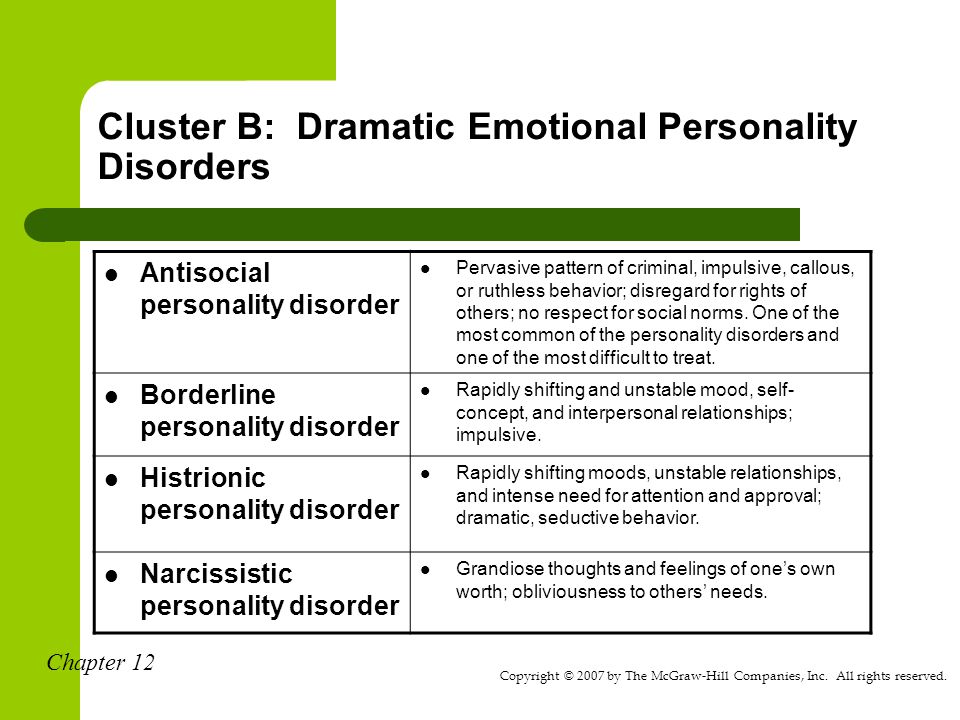
This activity reviews the evaluation and treatment of antisocial personality disorder (ASPD). ASPD is a deeply ingrained and dysfunctional thought process that focuses on social exploitive, delinquent, and criminal behavior most commonly known due to the affected individual's lack of remorse for these behaviors. ASPD falls into 1 of 4 cluster-B personality disorders within the DSM V, which also includes narcissistic, borderline, and histrionic personality disorders. This activity reviews the role of the an interprofessional team in evaluating, treating, and improving the care for patients with this condition.
ASPD is a deeply ingrained and dysfunctional thought process that focuses on social exploitive, delinquent, and criminal behavior most commonly known due to the affected individual's lack of remorse for these behaviors. ASPD falls into 1 of 4 cluster-B personality disorders within the DSM V, which also includes narcissistic, borderline, and histrionic personality disorders. This activity reviews the role of the an interprofessional team in evaluating, treating, and improving the care for patients with this condition.
Objectives:
Identify the psychopathology of antisocial personality disorder
Summarize the diagnostic criteria of Antisocial personality disorder.
Outline the treatment and management options available for Antisocial personality disorder.
Summarize interprofessional team strategies for improving care coordination and communication to advance the treatment of antisocial personality disorder and improve outcomes.
Access free multiple choice questions on this topic.
Introduction
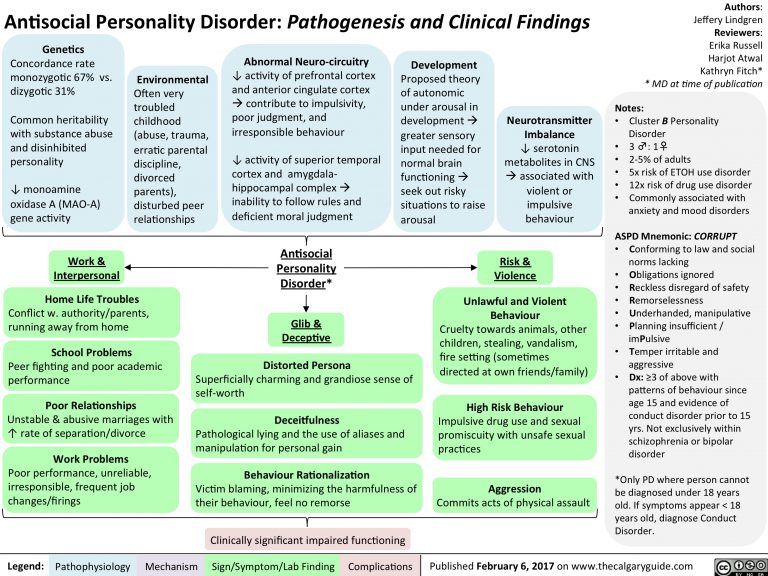
Antisocial personality disorder (ASPD) is a deeply ingrained and rigid dysfunctional thought process that focuses on social irresponsibility with exploitive, delinquent, and criminal behavior with no remorse. Disregard for and the violation of others' rights are common manifestations of this personality disorder, which displays symptoms that include failure to conform to the law, inability to sustain consistent employment, deception, manipulation for personal gain, and incapacity to form stable relationships.[1]
The Diagnostic and Statistical Manual of Mental Disorders (DSM 5) classifies all ten personality disorders into three clusters (A, B, and C). Antisocial personality disorder falls into 1 of 4 cluster-B disorders, which also includes borderline, narcissistic, and histrionic. All of these disorders characteristically present with dramatic, emotional, and unpredictable interactions with others. [2] Antisocial personality disorder is the only personality disorder that is not diagnosable in childhood. Before the age of 18, the patient must have been previously diagnosed with conduct disorder (CD) by the age of 15 years old to justify diagnostic criteria for ASPD.[1]
[2] Antisocial personality disorder is the only personality disorder that is not diagnosable in childhood. Before the age of 18, the patient must have been previously diagnosed with conduct disorder (CD) by the age of 15 years old to justify diagnostic criteria for ASPD.[1]
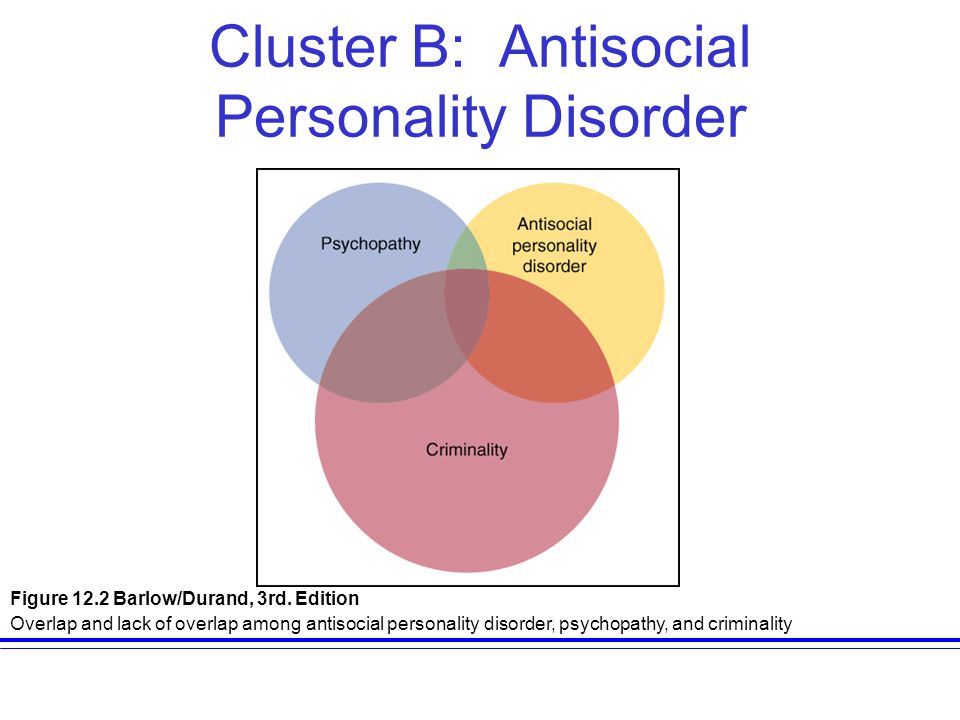
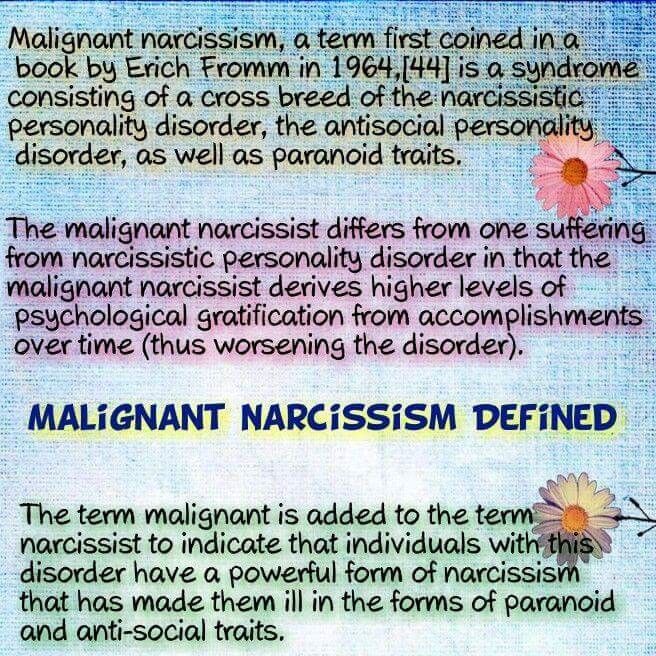
Many researchers and clinicians argue this diagnosis, with concerns of significant overlap with other disorders, including psychopathy. However, others counter that psychopathy is simply a subtype of antisocial personality disorder, with a more severe presentation. Recent literature states that although a heterogeneous construct that can subdivide into multiple subtypes that share many similarities and are often comorbid but not synonymous, individuals with ASPD must be characterized biologically and cognitively to ensure more accurate categorization and appropriate treatment.[3]
Etiology
Although the precise etiology is unknown, both genetic and environmental factors have been found to play a role in the development of ASPD. Various studies in the past have shown differing estimations of heritability, ranging from 38% to 69%. Environmental factors that correlate to the development of antisocial personality disorder include adverse childhood experiences (both physical and sexual abuse, as well as neglect) along with childhood psychopathology (CD and ADHD).[4]
Various studies in the past have shown differing estimations of heritability, ranging from 38% to 69%. Environmental factors that correlate to the development of antisocial personality disorder include adverse childhood experiences (both physical and sexual abuse, as well as neglect) along with childhood psychopathology (CD and ADHD).[4]
Other studies stress the importance of both shared and non-shared environmental factors, including both family dynamics and peer relations on the development of ASPD. Research has focused on establishing the exact gene contributing to ASPD, and much evidence is pointing toward the 2p12 region of chromosome 2 and variation within AVPR1A. Interactions of specific genes with the environment have been an area of study as well, with evidence of variation in the oxytocin receptor gene (OXTR) contributing to the broad ranges of behavior elicited in antisocial personality disorder due to its effect on the influence of deviant peer affiliation.[5]
Epidemiology
The estimated lifetime prevalence of ASPD amongst the general population falls within 1 to 4%.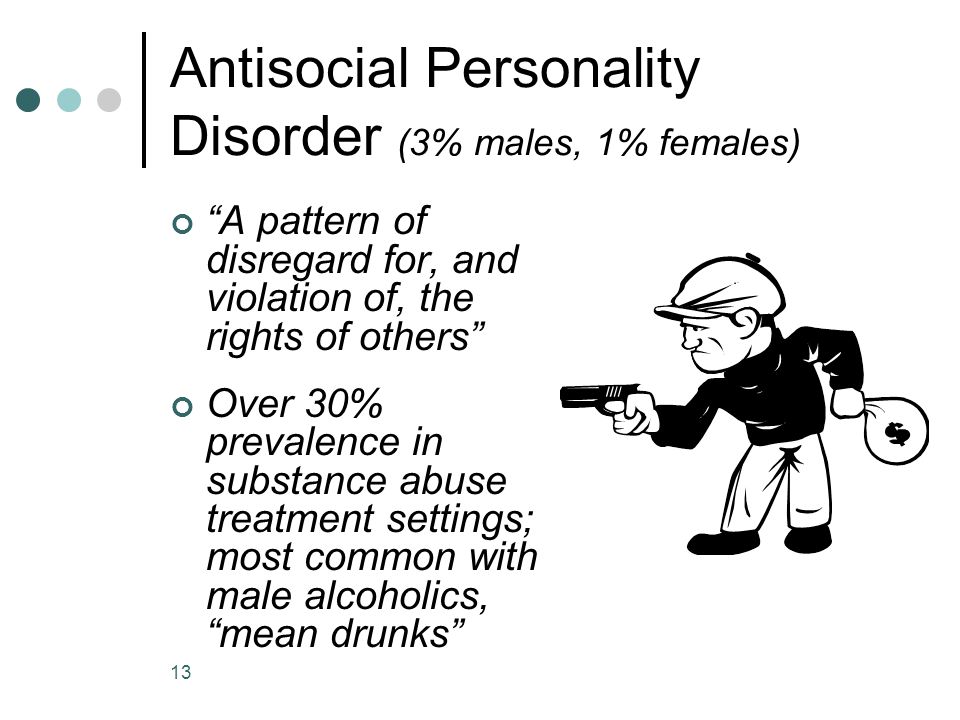 [6][7] Due to the predicting factor of the initial diagnosis of conduct disorder before the age of 15, this assumption can be quite broad as CD does not always get adequately evaluated.[8] Gender distribution tends to be skewed towards males, with 3 to 5 times more likelihood of being diagnosed with ASPD than females, with 6% men and 2% women within the general population.[9] Substance abuse has been found to show a significant correlation to the diagnosis of antisocial personality disorder,[10] while education and intelligence displays a negative correlation,[9][11] with a higher prevalence of ASPD amongst those with lower IQs and reading levels.[12] Research has shown reductions in the prevalence rate with increasing age in criminal populations,[13] as well as epidemiological samples.[9] Changes in personality traits with age and increased mortality with the behavior of antisocial personality disorder have been hypothesized to justify this age-dependent alteration.[14]
[6][7] Due to the predicting factor of the initial diagnosis of conduct disorder before the age of 15, this assumption can be quite broad as CD does not always get adequately evaluated.[8] Gender distribution tends to be skewed towards males, with 3 to 5 times more likelihood of being diagnosed with ASPD than females, with 6% men and 2% women within the general population.[9] Substance abuse has been found to show a significant correlation to the diagnosis of antisocial personality disorder,[10] while education and intelligence displays a negative correlation,[9][11] with a higher prevalence of ASPD amongst those with lower IQs and reading levels.[12] Research has shown reductions in the prevalence rate with increasing age in criminal populations,[13] as well as epidemiological samples.[9] Changes in personality traits with age and increased mortality with the behavior of antisocial personality disorder have been hypothesized to justify this age-dependent alteration.[14]
History and Physical
Before performing a comprehensive psychiatric assessment of the patient, a careful history and physical examination is necessary.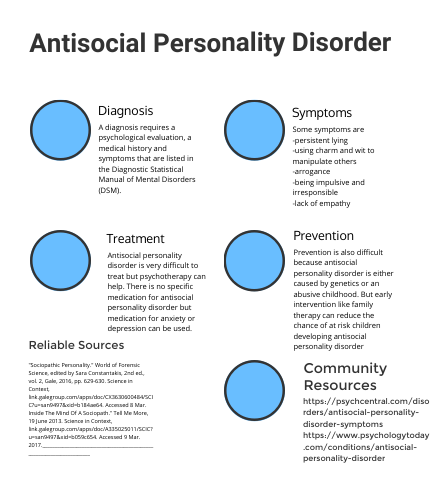 "The DSM-5 diagnostic criteria for Antisocial Personality Disorder
"The DSM-5 diagnostic criteria for Antisocial Personality Disorder
A pervasive pattern of disregard for and violation of the rights of others, since age 15 years, as indicated by three (or more) of the following:
Failure to conform to social norms concerning lawful behaviors, such as performing acts that are grounds for arrest.
Deceitfulness, repeated lying, use of aliases, or conning others for pleasure or personal profit.
Impulsivity or failure to plan.
Irritability and aggressiveness, often with physical fights or assaults.
Reckless disregard for the safety of self or others.
Consistent irresponsibility, failure to sustain consistent work behavior, or honor monetary obligations.
Lack of remorse, being indifferent to or rationalizing having hurt, mistreated, or stolen from another person.
The individual is at least age 18 years.
Evidence of conduct disorder typically with onset before age 15 years.
The occurrence of antisocial behavior is not exclusively during schizophrenia or bipolar disorder."
Evaluation
No current diagnostic modalities, such as tests including serology, are currently accepted standards in diagnosing antisocial personality disorder. However, genetic testing and neuroimaging have been used to evaluate potential causes and patterns, respectively, with ASPD (see Etiology section above). Patients with antisocial personality disorder are at a higher risk of contracting certain viral infections and sexually transmitted diseases associated with high-risk behavior, including hepatitis C and human immunodeficiency virus, as well as increased mortality rates due to accidents, traumatic injuries, suicides, and homicides.[15][16][17]
Treatment / Management
Although there has been a multitude of interventions tested in the past, an appropriate algorithm fails to exist today.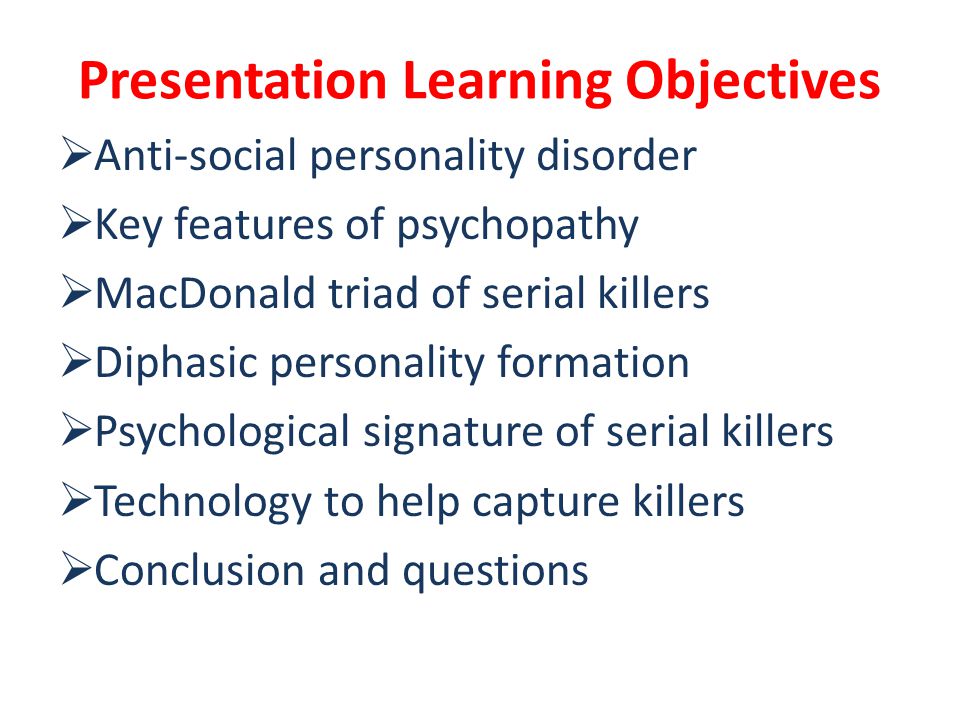 Literature suggests early treatment intervention with conduct disorder in children as the least costly and most effective with treating ASPD.[18] However, researchers have employed certain psychopharmacology and psychotherapy throughout literature, but due to the severity of potential harms in adulthood, intricate consideration are necessary when delineating a treatment course.[19]
Literature suggests early treatment intervention with conduct disorder in children as the least costly and most effective with treating ASPD.[18] However, researchers have employed certain psychopharmacology and psychotherapy throughout literature, but due to the severity of potential harms in adulthood, intricate consideration are necessary when delineating a treatment course.[19]
Most of the needs of antisocial personality disorder are addressable in the outpatient setting. Hospitalization is not cost-effective as it provides little to no benefit to those with ASPD, and it is very costly. Also, the presence of those with ASPD in a psychiatric hospital disrupts the environment, thus affecting the treatment of other patients in need of therapeutic care. Hospitalization is reserved for treating co-occurring conditions or possible complications, such as substance intoxication/withdrawal or recent suicidal behavior.
Insufficient evidence exists to support any psychological intervention in adults with ASPD.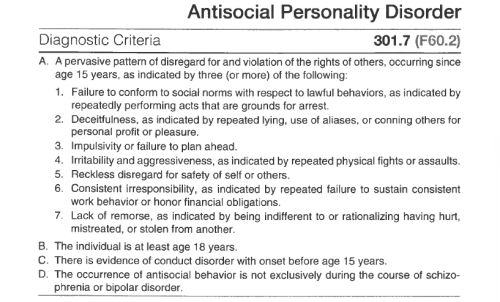 [20] No pharmacological intervention has been shown to treat ASPD, but medications are highly recommended to treat co-occurring conditions. Aggressive behavior is treatable with second-generation antipsychotics as first-line therapy, including risperidone (2 to 4mg/day), quetiapine (100 to 300mg/day). Second and third-line therapies for aggression include selective serotonin reuptake inhibitors (SSRI), sertraline (100 to 200mg/day) or fluoxetine (20mg/day), and mood stabilizers; lithium and carbamazepine (dosed at recommended levels for bipolar disorder), respectively. Anticonvulsants, such as oxcarbazepine and carbamazepine, can be used to aid with impulsivity. Bupropion and atomoxetine are often used to treat associated ADHD due to their non-addictive nature.
[20] No pharmacological intervention has been shown to treat ASPD, but medications are highly recommended to treat co-occurring conditions. Aggressive behavior is treatable with second-generation antipsychotics as first-line therapy, including risperidone (2 to 4mg/day), quetiapine (100 to 300mg/day). Second and third-line therapies for aggression include selective serotonin reuptake inhibitors (SSRI), sertraline (100 to 200mg/day) or fluoxetine (20mg/day), and mood stabilizers; lithium and carbamazepine (dosed at recommended levels for bipolar disorder), respectively. Anticonvulsants, such as oxcarbazepine and carbamazepine, can be used to aid with impulsivity. Bupropion and atomoxetine are often used to treat associated ADHD due to their non-addictive nature.
Differential Diagnosis
Narcissistic personality disorder (cluster B personality disorder with overlap; exploitive and uncompassionate, but not aggressive or deceitful)
Borderline personality disorder (cluster B personality disorder with overlap; manipulative, but for reassurance and nurture)
Substance use disorder (Impulsivity and irresponsibility due to substance influence must be ruled out before diagnosing ASPD.
 ASPD can be diagnosed if substance use is co-occurring)
ASPD can be diagnosed if substance use is co-occurring)
Prognosis
Of those children with conduct disorder, 25% of girls and 40% of boys will meet the diagnostic criteria for antisocial personality disorder. Boys exhibit symptoms earlier than girls, who often only elicit these symptoms in puberty. Children who do not develop conduct disorder and progress to the age of 15 without antisocial behaviors will not develop ASPD. Childhood conduct disorder is a reliable prognosticator of adulthood ASPD.[1] The small percentage of adults with antisocial personality disorder who never met the criteria or never received an assessment for conduct disorder, tend to have milder symptoms.[21]
Antisocial personality disorder, although a chronic condition with a lifelong presentation, has had moderations shown with advancing ages, with the mean remitted age of 35 years old. Those with less baseline symptomatology showed better-remitted rates. Studies in the past revealed remission rates of 12 to 27% and 27 to 31% rates of improvement, but not remitted. Crime rates and severity reflect this relation as well, with peak crime statistics in late teens and higher severity of crimes at younger ages. Those with later presentations of antisocial behavior showed less severe behavioral problems. Those who were either never imprisoned or imprisoned for longer periods displayed greater remission rates than those imprisoned for shorter periods. This finding indicated that short-term incarceration could be somewhat preventive for future antisocial behavior.[1]
Crime rates and severity reflect this relation as well, with peak crime statistics in late teens and higher severity of crimes at younger ages. Those with later presentations of antisocial behavior showed less severe behavioral problems. Those who were either never imprisoned or imprisoned for longer periods displayed greater remission rates than those imprisoned for shorter periods. This finding indicated that short-term incarceration could be somewhat preventive for future antisocial behavior.[1]
Complications
Many individuals diagnosed with antisocial personality disorder remain a burden to their families, coworkers, and closely associated peers, such as neighbors, despite becoming less troublesome with age. Mental health comorbidities and associated addictive disorders, as well as higher mortality rates due to suicides and homicides, only add to this burden. Most of those who improve with age remain unable to re-claim their lost prospects, including education, domestication, and employment.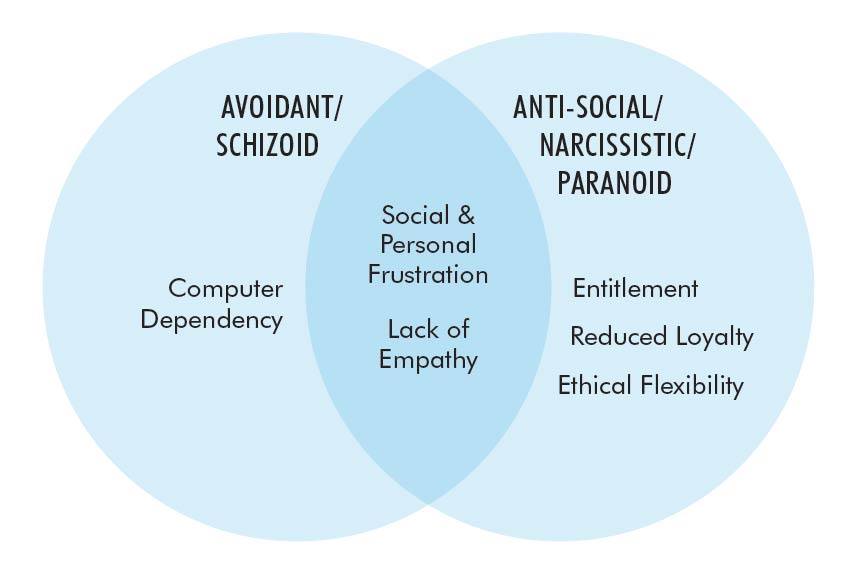 Those patients who did show remission were more likely to have spousal or family ties, with better social support.[1]
Those patients who did show remission were more likely to have spousal or family ties, with better social support.[1]
Deterrence and Patient Education
Antisocial personality disorder is one of the best-documented disorders in all of literature pertaining to psychiatry, including etiology, epidemiology, pathophysiology, neuroanatomy, heritability, and interventional treatment. However, an established treatment algorithm and specialized psychopharmacology currently fail to exist.
Better preventative measures are necessary as many of those with ASPD may only have an evaluation upon incarceration after inflicting harm. One is not apt to seek help for ASPD symptomatology. Many only seek assistance for co-occurring mental disorders or only present for court-mandated assessments.
Even with the remission rates in advanced ages, antisocial personality disorder causes much turmoil to the patient and the patient’s surrounding community. The lives of those with ASPD remain negatively impacted even after remission.
Enhancing Healthcare Team Outcomes
The diagnosis, categorization, and management of ASPD is quite complex and multifaceted, often only presenting after harm has already taken place. Management of the disorder is best with an interprofessional team dedicated to the treatment of mental health disorders. People with antisocial personality disorder are at risk of incarceration due to the violent and deceitful nature of the behaviors elicited in ASPD. Hospitalization provides no benefit to a patient with ASPD and can actually create a disruptive hospital environment to others who truly need hospitalization for therapeutic purposes. The majority of these individuals are noncompliant with therapy and often fail to show up at clinics. Thus, management can be difficult.
The physician overseeing the case almost inevitably needs to be a psychological specialist; they can work collaboratively with the patient's family physician, but the complexity of this diagnosis requires specist-level care. Nursing staff should also have specialized psychological training, so they have received adequate training on ways to approach and cope with these individuals, as well as to be able to recognize therapeutically significant signs and behaviors that need to be brought to the treating physician's attention. They can also assess patient compliance as well as give their impressions of treatment effectiveness. A pharmacist should also provide consultation on the medications used, verifying dosing and checking carefully for drug interactions, and reporting to the nurse or physician if there are any concerns. Only with a collaborative interprofessional team approach patients with antisocial personality disorder receive optimal care leading to better outcomes. [Level 5]
Nursing staff should also have specialized psychological training, so they have received adequate training on ways to approach and cope with these individuals, as well as to be able to recognize therapeutically significant signs and behaviors that need to be brought to the treating physician's attention. They can also assess patient compliance as well as give their impressions of treatment effectiveness. A pharmacist should also provide consultation on the medications used, verifying dosing and checking carefully for drug interactions, and reporting to the nurse or physician if there are any concerns. Only with a collaborative interprofessional team approach patients with antisocial personality disorder receive optimal care leading to better outcomes. [Level 5]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Black DW. The Natural History of Antisocial Personality Disorder.
 Can J Psychiatry. 2015 Jul;60(7):309-14. [PMC free article: PMC4500180] [PubMed: 26175389]
Can J Psychiatry. 2015 Jul;60(7):309-14. [PMC free article: PMC4500180] [PubMed: 26175389]- 2.
Regier DA, Kuhl EA, Kupfer DJ. The DSM-5: Classification and criteria changes. World Psychiatry. 2013 Jun;12(2):92-8. [PMC free article: PMC3683251] [PubMed: 23737408]
- 3.
Brazil IA, van Dongen JDM, Maes JHR, Mars RB, Baskin-Sommers AR. Classification and treatment of antisocial individuals: From behavior to biocognition. Neurosci Biobehav Rev. 2018 Aug;91:259-277. [PubMed: 27760372]
- 4.
DeLisi M, Drury AJ, Elbert MJ. The etiology of antisocial personality disorder: The differential roles of adverse childhood experiences and childhood psychopathology. Compr Psychiatry. 2019 Jul;92:1-6. [PubMed: 31079021]
- 5.
Fragkaki I, Cima M, Verhagen M, Maciejewski DF, Boks MP, van Lier PAC, Koot HM, Branje SJT, Meeus WHJ. Oxytocin Receptor Gene (OXTR) and Deviant Peer Affiliation: A Gene-Environment Interaction in Adolescent Antisocial Behavior.
 J Youth Adolesc. 2019 Jan;48(1):86-101. [PubMed: 30315439]
J Youth Adolesc. 2019 Jan;48(1):86-101. [PubMed: 30315439]- 6.
Lenzenweger MF, Lane MC, Loranger AW, Kessler RC. DSM-IV personality disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007 Sep 15;62(6):553-64. [PMC free article: PMC2044500] [PubMed: 17217923]
- 7.
Trull TJ, Jahng S, Tomko RL, Wood PK, Sher KJ. Revised NESARC personality disorder diagnoses: gender, prevalence, and comorbidity with substance dependence disorders. J Pers Disord. 2010 Aug;24(4):412-26. [PMC free article: PMC3771514] [PubMed: 20695803]
- 8.
Werner KB, Few LR, Bucholz KK. Epidemiology, Comorbidity, and Behavioral Genetics of Antisocial Personality Disorder and Psychopathy. Psychiatr Ann. 2015 Apr;45(4):195-199. [PMC free article: PMC4649950] [PubMed: 26594067]
- 9.
Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions.
 J Clin Psychiatry. 2005 Jun;66(6):677-85. [PubMed: 15960559]
J Clin Psychiatry. 2005 Jun;66(6):677-85. [PubMed: 15960559]- 10.
Moran P. The epidemiology of antisocial personality disorder. Soc Psychiatry Psychiatr Epidemiol. 1999 May;34(5):231-42. [PubMed: 10396164]
- 11.
Neumann CS, Hare RD. Psychopathic traits in a large community sample: links to violence, alcohol use, and intelligence. J Consult Clin Psychol. 2008 Oct;76(5):893-9. [PubMed: 18837606]
- 12.
Simonoff E, Elander J, Holmshaw J, Pickles A, Murray R, Rutter M. Predictors of antisocial personality. Continuities from childhood to adult life. Br J Psychiatry. 2004 Feb;184:118-27. [PubMed: 14754823]
- 13.
Harpur TJ, Hare RD. Assessment of psychopathy as a function of age. J Abnorm Psychol. 1994 Nov;103(4):604-9. [PubMed: 7822561]
- 14.
Vachon DD, Lynam DR, Widiger TA, Miller JD, McCrae RR, Costa PT. Basic traits predict the prevalence of personality disorder across the life span: the example of psychopathy.
 Psychol Sci. 2013 May;24(5):698-705. [PubMed: 23528790]
Psychol Sci. 2013 May;24(5):698-705. [PubMed: 23528790]- 15.
Black DW, Gunter T, Loveless P, Allen J, Sieleni B. Antisocial personality disorder in incarcerated offenders: Psychiatric comorbidity and quality of life. Ann Clin Psychiatry. 2010 May;22(2):113-20. [PubMed: 20445838]
- 16.
Falcus C, Johnson D. The Violent Accounts of Men Diagnosed With Comorbid Antisocial and Borderline Personality Disorders. Int J Offender Ther Comp Criminol. 2018 Jul;62(9):2817-2830. [PubMed: 29039227]
- 17.
Instanes JT, Haavik J, Halmøy A. Personality Traits and Comorbidity in Adults With ADHD. J Atten Disord. 2016 Oct;20(10):845-54. [PubMed: 24271945]
- 18.
Frick PJ. Early Identification and Treatment of Antisocial Behavior. Pediatr Clin North Am. 2016 Oct;63(5):861-71. [PubMed: 27565364]
- 19.
Repo-Tiihonen E, Hallikainen T. [Antisocial personality disorder]. Duodecim. 2016;132(2):130-6. [PubMed: 26939485]
- 20.
Gibbon S, Duggan C, Stoffers J, Huband N, Völlm BA, Ferriter M, Lieb K. Psychological interventions for antisocial personality disorder. Cochrane Database Syst Rev. 2010 Jun 16;(6):CD007668. [PMC free article: PMC4167848] [PubMed: 20556783]
- 21.
Goldstein RB, Dawson DA, Saha TD, Ruan WJ, Compton WM, Grant BF. Antisocial behavioral syndromes and DSM-IV alcohol use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Clin Exp Res. 2007 May;31(5):814-28. [PubMed: 17391341]
Asocial personality
Asocial personality - A person with a poorly developed (or perverted) sense of responsibility, low moral values, and a lack of interest in others. Another name for an antisocial personality is a sociopath.
Characteristics of an antisocial personality
Behavior is almost entirely determined by a person's own needs.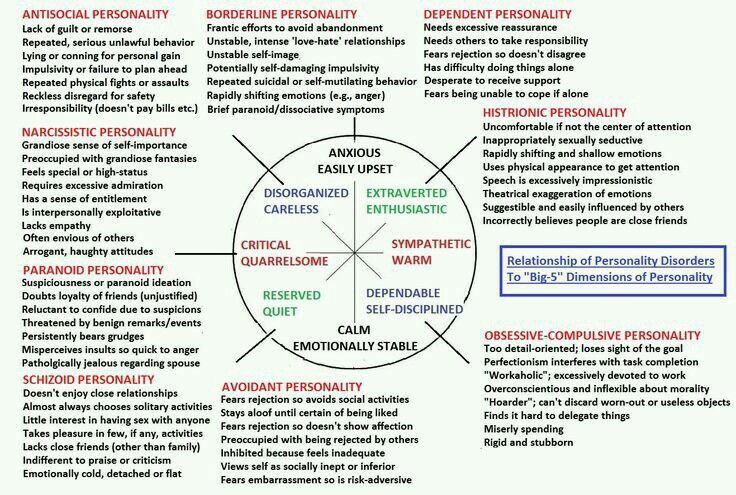
Painful reactions, frustrations to the state of one's own displeasure.
Desire for immediate relief (and relief at any cost) from unpleasant sensations.
Impulsivity, a tendency to live in the moment.
The extraordinary ease of lying.
Often play roles very skillfully.
Unstable self-esteem.
The need to excite oneself (to excite oneself).
Inability to change one's behavior as a result of punishment.
People around are often perceived as attractive, intelligent, charming people.
Easily get in touch, especially easy to converge on the basis of entertainment.
Lack of sincere sympathy for others.
No sense of shame or guilt for one's actions.
Three groups of factors contributing to the development of an antisocial personality are presented below: biological determinants, features of the relationship between parents and the child, style of thinking.
Biological factors
Research suggests genetic correlates of antisocial behavior.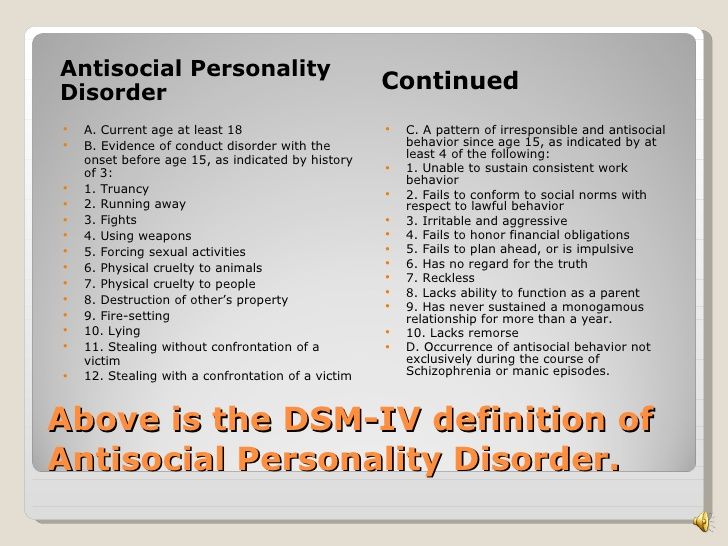 Identical twins have twice the concordance for criminal behavior than related twins, making it clear that this behavior is partly heritable.
Identical twins have twice the concordance for criminal behavior than related twins, making it clear that this behavior is partly heritable.
Adoption studies show that the crimes of adopted boys are similar to those of their biological fathers.
It is also noted that antisocial personalities have low excitability, which is why they seek to receive stimulation that causes appropriate sensations with the help of impulsive and dangerous actions.
Family factors
Research also shows that the quality of parental care received by a child with a history of hyperactivity and behavioral problems determines to a large extent whether or not the child develops an antisocial personality.
Children who are often left unattended or who are poorly cared for for long periods of time are much more likely to engage in criminal behavior patterns.
Also, children whose parents do not participate in their daily lives are more likely to become asocial.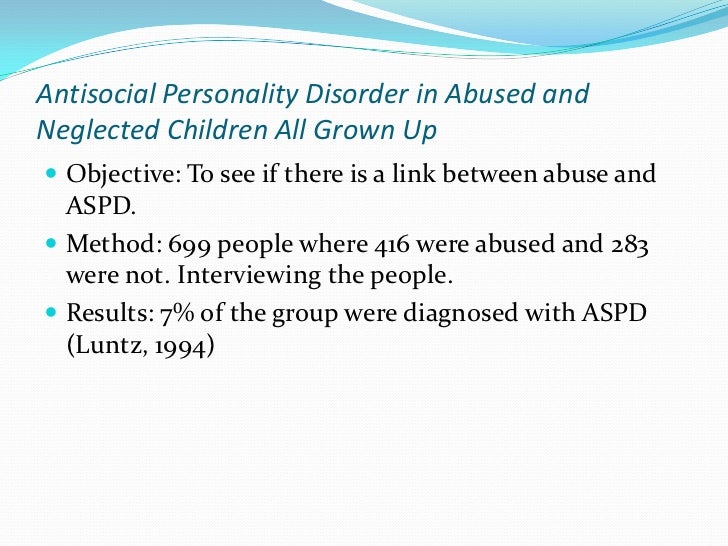
Biological and family factors often coincide, which enhances their effect. Children with behavioral problems often have neuropsychological problems resulting from maternal drug use, poor intrauterine nutrition, pre- and post-natal toxicity, abuse, birth complications, and low birth weight. Such children are more likely to be irritable, impulsive, awkward, hyperactive, inattentive. They slowly learn the material at school, which over time leaves a strong imprint on the child's self-esteem.
Thinking style
In children with behavioral disorders, an inadequate picture of the world, the processing of information about social interactions occurs in such a way that they develop aggressive reactions to these interactions. They expect aggression from other children and adults, interpret their actions based on the assumption of malevolence.
Children with behavioral disorders tend to consider any negative action of their peers directed at them not as accidental, but as deliberate.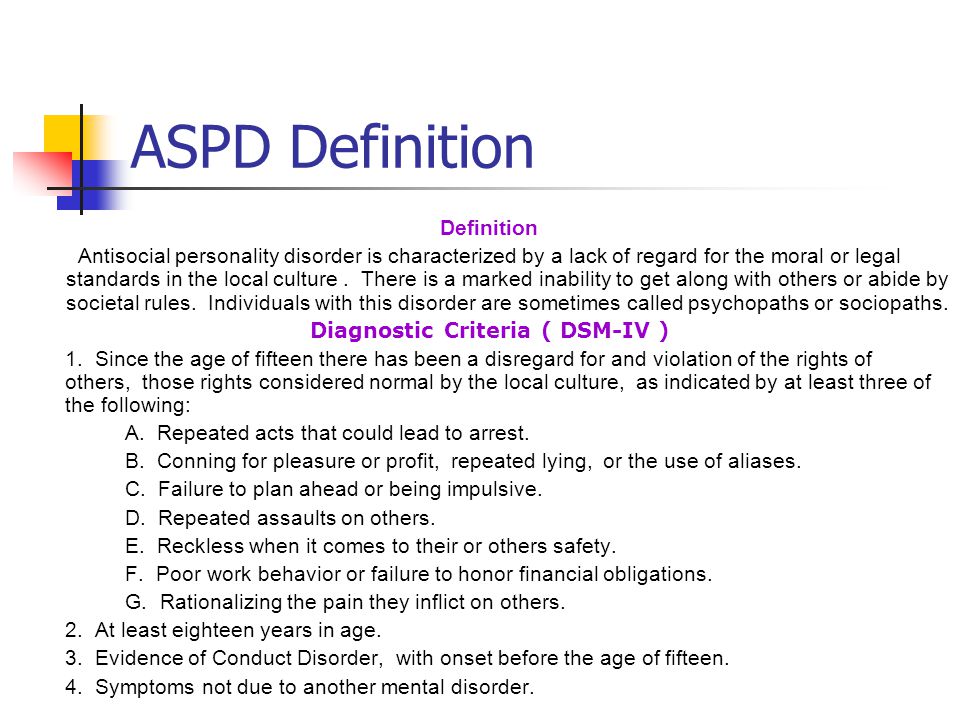 A low level of intellectual development encourages such a child to reduce everything to someone's "evil initiative."
A low level of intellectual development encourages such a child to reduce everything to someone's "evil initiative."
Not knowing how to behave assertively, the child eventually comes to the conclusion that aggression is the most reliable and effective tool.
The responses of others to the child's aggression usually only lead to the strengthening of the idea of the need for aggression.
In this way a vicious circle of interactions develops, supporting and inspiring the aggressive and antisocial behavior of the child.
Literature
Maklakov AG General psychology. St. Petersburg: Peter, 2001.
An asocial person - who is he, signs, characteristics of behavior
An asocial person is a person who chooses the basis of his behavior for actions that do not fit into the rules of social behavior of people, as well as moral prescriptions. At the same time, people leading an asocial lifestyle are not violators or criminals, rather they look like indifferent elements isolated from society with their own systems of values and priorities that do not support common rules and principles. An asocial person does not have a pronounced desire to interact, all social contacts occur only out of necessity or in the presence of rare emotional ties.
An asocial person does not have a pronounced desire to interact, all social contacts occur only out of necessity or in the presence of rare emotional ties.
Antisocial behavior of a person can be alarming by the constant choice of individual activities, the lack of full-fledged communication, the avoidance of joint activities. To extroverted people, such behavior may seem rude, dissatisfied, or even a direct insult, but in fact there is no open hostility or hatred behind this, it’s just that a person is better off alone and doing independent activities.
What does an antisocial person mean
To understand what an antisocial person is and not to confuse this concept with antisocial, misanthropic and others, it is necessary to analyze the psychological root causes of this type of character, which does not relate to pathological disorders, but to the sociopathic spectrum. Initially, this is due to violations of the emotional spectrum, it is not only difficult for such people to actively and violently demonstrate their emotions, but even to express them verbally, some states remain closed for description, and only psychotechnics help to understand what is happening inside.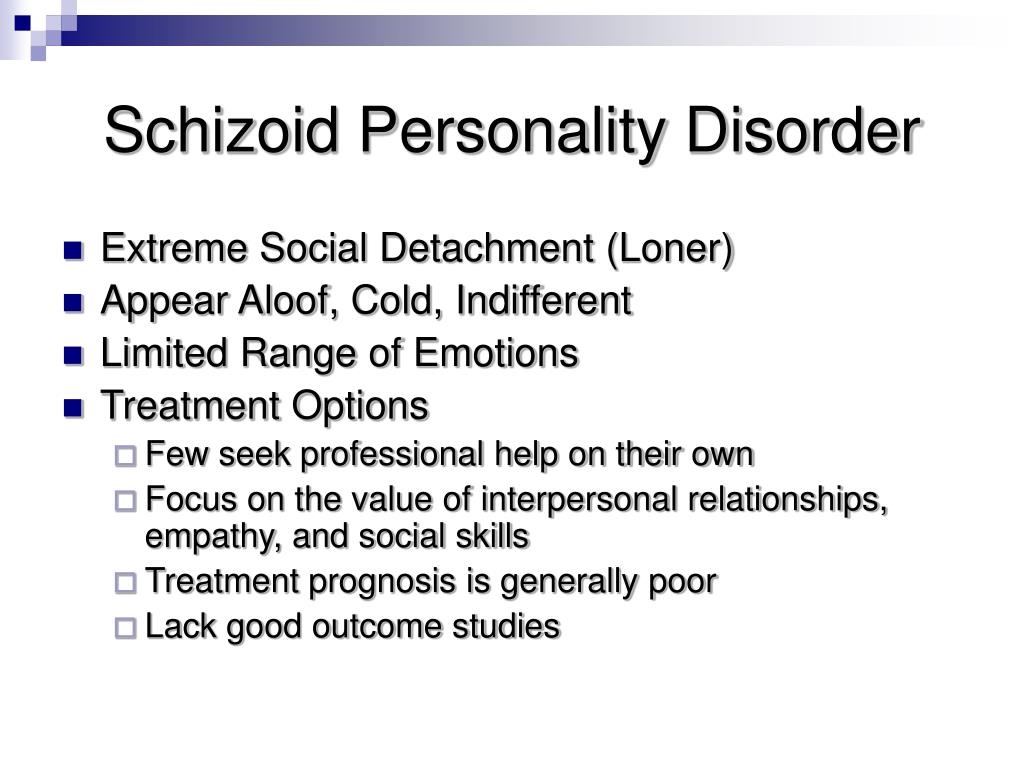 Since others demonstrate their feelings more vividly, talk about them more often, the antisocial type becomes uncomfortable and incomprehensible in their company.
Since others demonstrate their feelings more vividly, talk about them more often, the antisocial type becomes uncomfortable and incomprehensible in their company.
Values and importance are dominated by one's own views and priorities, so social rules and norms will be ignored. For example, if an antisocial person becomes bored, then he will not withstand a cultural pause, wait for goodbye, but simply leave (the performance, the guests - it doesn’t matter). He will also not smile at someone in order to make a good impression, a smile will appear only in a good mood, and polite communication only if there is respect for the interlocutor.
Due to desensitization in the emotional realm, a common reaction to any intrusion or attempt to impose social norms is aggression. It is the only way to respond to any stimuli, while in order to achieve what he wants from other people, an antisocial personality easily uses manipulation, lies, puts on any roles. It turns out that a person's antisocial behavior does not exclude adaptation, but uses it only in those situations when it is necessary for him, otherwise a cruel confrontation simply turns on.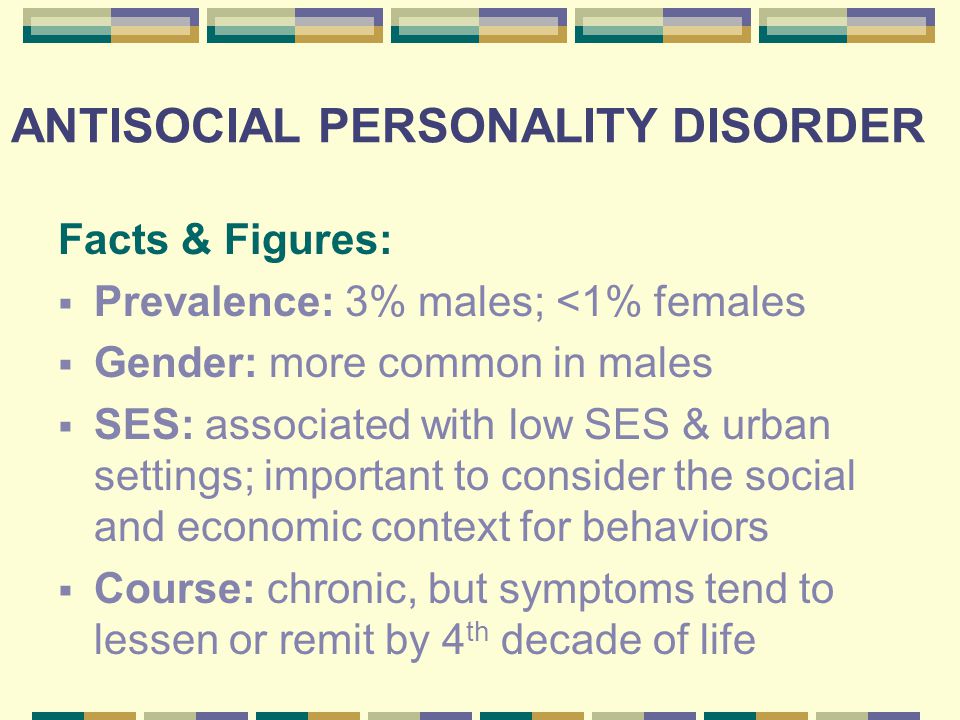
A high level of impulsivity makes it impossible for an asocial person to find adequate ways to satisfy his desires, but the need for their realization becomes extremely acute and requires fulfillment in the second of occurrence. This leads to the fact that people do not very good deeds just to get what they want faster, and it is difficult to explain to them the unworthiness of such a choice, because they are not able to understand the feelings of others and their suffering or pain, there is no shame and guilt, as the main regulators of social behavior.
Antisocial people are also in no hurry to correct unworthy deeds, because even at the sight of tears, pain and grief of others, they are completely sure that they are right, and they consider the undesirable behavior of others as manipulation and attempts to exert pressure. They do not analyze their negative actions and do not use them as an experience, i.e. once they apologize to someone, they can keep doing the same things.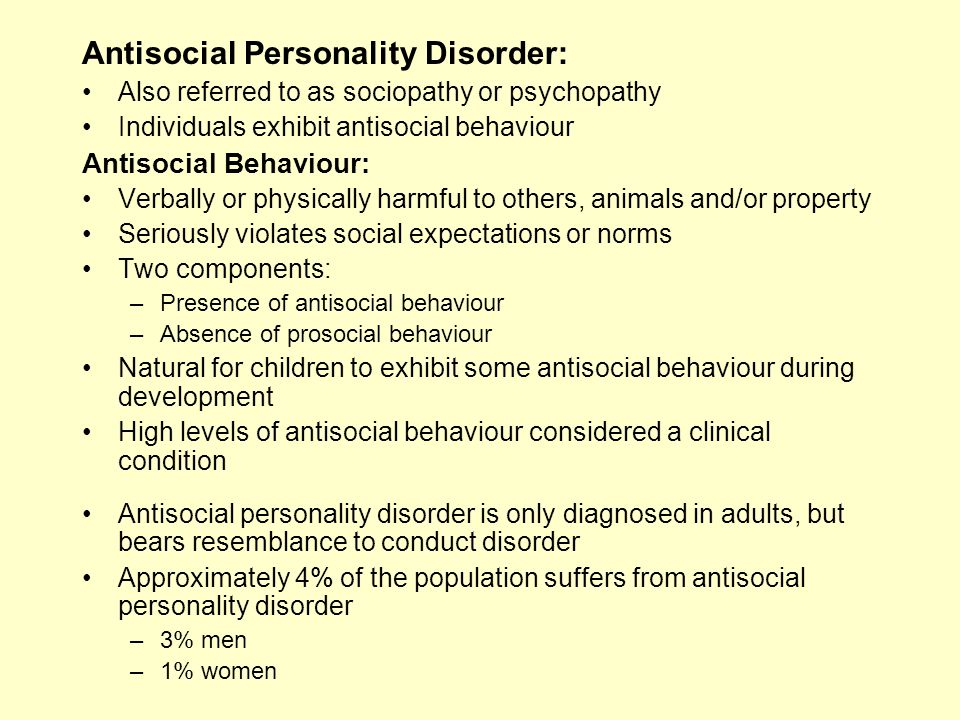
Many patterns of behavior can develop from such personality traits, so it is impossible to describe sociopathic or asocial as a manifestation of one thing in a limited set. There will be no instructions with quotes, but only an understanding of the internal motivation of a person and his social isolation. Even to their partners, who can be the center of the universe and really loved, an antisocial person will not show feelings, especially sensitivity. It is difficult to believe this for those who are not in close contact with them, because on the surface, asocial personalities are very charismatic and arouse the interest of almost everyone.
Causes of antisocial behavior
People become antisocial, not born, despite the fact that biological factors also slightly predispose, but do not have a key influence on the formation of sociopathic qualities. Hereditary factors form a tendency to criminal behavior, but only due to high rates of impulsiveness and infantilism, which can be compensated for with proper education.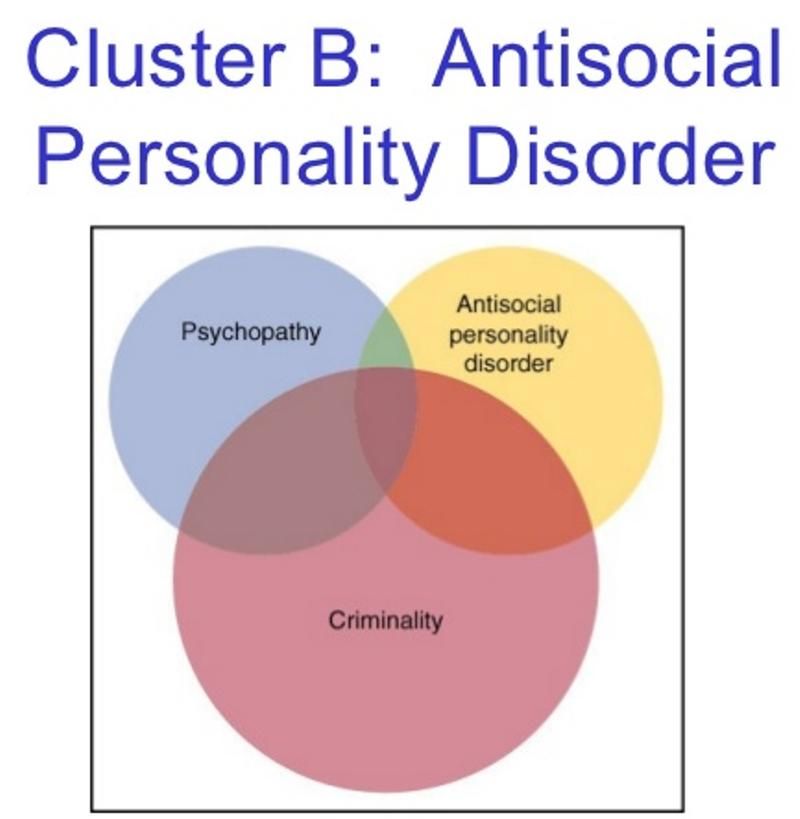 The negative impact of smoking, alcohol and drugs during pregnancy does not allow the nervous system to form normally, as a result of which not only emotional disruptions occur, but also self-control and the ability to understand others.
The negative impact of smoking, alcohol and drugs during pregnancy does not allow the nervous system to form normally, as a result of which not only emotional disruptions occur, but also self-control and the ability to understand others.
Even with a healthy formation of the nervous system and the development of the fetus without genetic abnormalities, asociality develops in the negative conditions of family life. When violence is applied to a child as a guiding factor in behavior, the general atmosphere is negative and aggressive, then the emotional sphere collapses and social distancing occurs.
Excessive coldness, indifference on the part of adults (especially characteristic when parents are not ready for the birth) forms a closed personality, with the understanding that indifference and the pursuit of only one's own interests is the only way of existence.
Children with hyperactivity owe much of their future to their parents and their attitude, since such an indirect feature of the nervous system can easily develop into asociality if left to chance or excessive cruelty.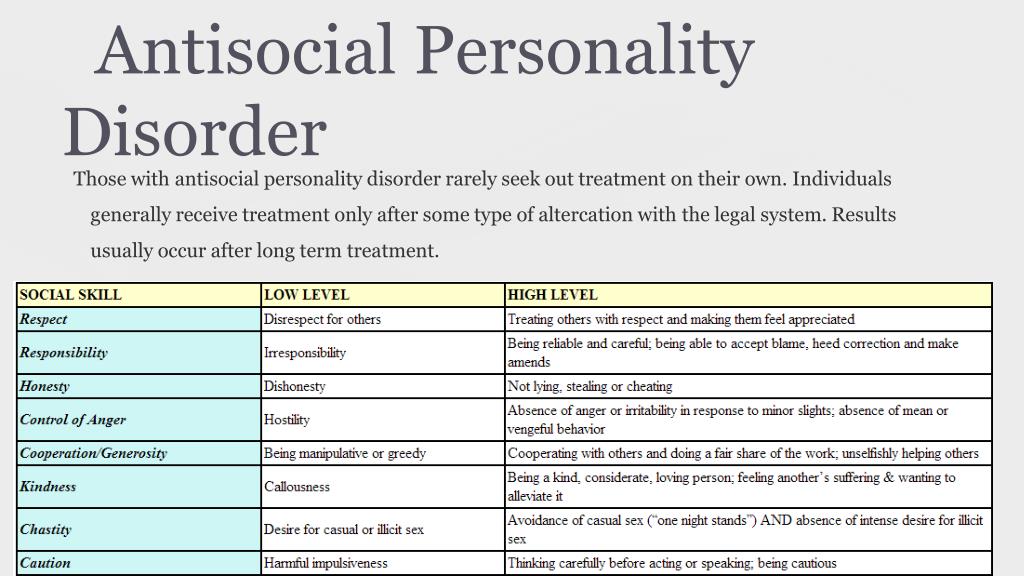
Leaving such children often unsupervised increases the risk of permissive criminal behavior patterns. And while this is happening within the walls of a house without adults, an imprint remains in the psyche that in the big world you can behave as you like, despite the knowledge of official prohibitions. The younger the child, the easier he obeys the rules of adults (parents or passers-by), so reducing the likelihood of contact with unstable elements is a prevention of asociality.
The environment also influences, for example, in countries where there is a high population density, and all possible work is connected with contacts, people rarely become asocial, only under serious biological factors. If a person has a choice regarding his activity and he is not satisfied with the situation around him, then asociality is a conscious choice. This happens in a situation of inconsistency between the individual and her level of culture to others - when a modest, intelligent girl lives in a village where they talk obscenities and drink regularly, then distancing themselves from such a society, going into Internet earnings and completely ignoring their norm and requirements can be the only salvation.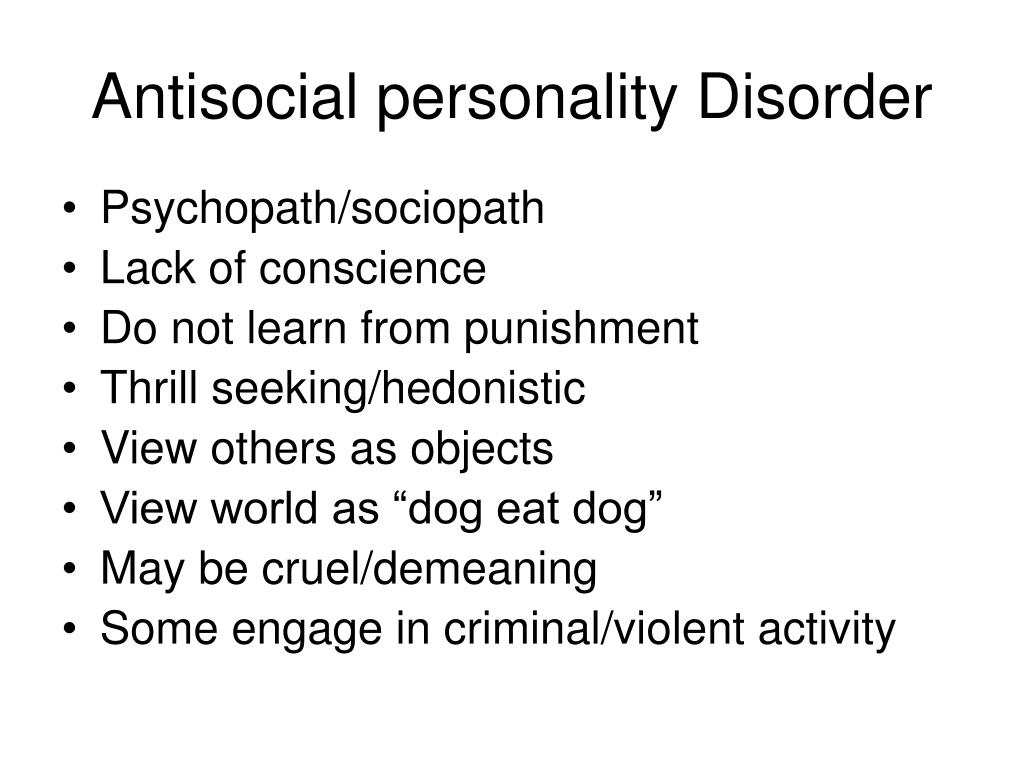
So it turns out that the causes of asociality can appear before birth and after the middle of life, depending on the mental structure and environment, but in any case, this quality cannot be attributed exclusively to negative or positive. In some situations, this leads to the development of deviant behavior, crimes and disruption of social ties, in others it helps to save one's own internal structure and psyche.
How to get rid of asociality
Prevention of asocial behavior of a person is the most effective method of total elimination of this phenomenon. To do this, on the part of the educational institution, those children who have detachment and other signs of an asocial person must be maximally involved in creative activities and sports, as ways of directing their activity and socialization. Any extra-curricular activities, additional circles and preparations are good - everything that will provide a surge of energy and systematization of free time, where the influence of negative elements will decrease.
Prevention also includes psychological conversations with both children and parents. This is important, because asociality begins to develop from an early age, and is most susceptible to family influence. No matter how social services and schools work, if there is no appropriate treatment and support in the family, then the development of social skills will go the wrong way, towards closing the personality or distorting emotional and behavioral patterns. Parents need to start monitoring their behavior, and not just scolding children, creating an atmosphere of trust instead of an authoritarian dictatorship.
If the question of changing antisocial behavior arises in adults, and the distancing itself does not have negative consequences (imprisonment, reduced academic performance, salary, etc.), then it is worth assessing where this desire comes from. Often society imposes stereotypes of communication, openness, full contact and continuous availability, but this may not suit you personally.