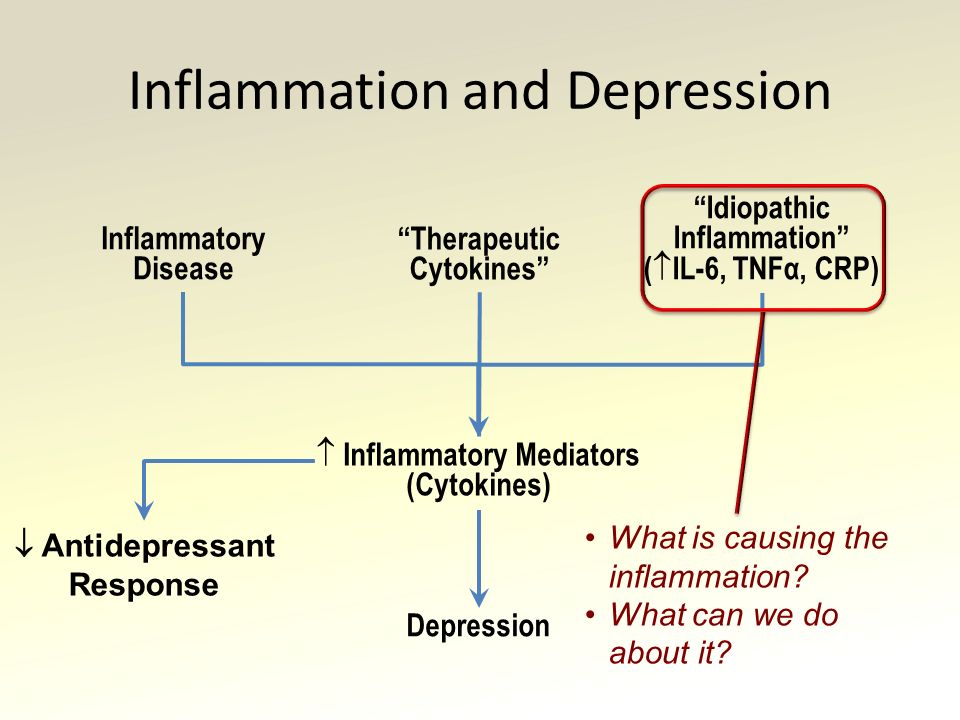
Conditions similar to depression
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers. The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.
2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
- Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
- The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.
 4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH) - Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
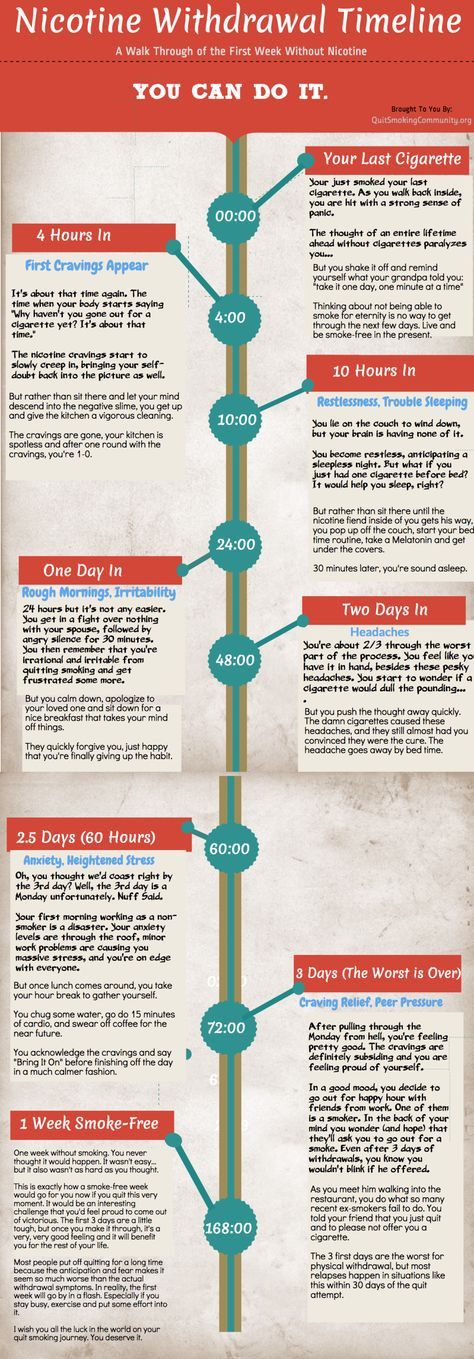
- In 2020, 20.
 7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month.
 The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people). - Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medications for Substance Use Disorders
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 03/22/2023
Evidence-Based Resources About Opioid Overdose
SAMHSA’s Evidence-Based Practice Resource Center (EBPRC) contains a wide variety of downloadable resources available from SAMHSA and other federal partners about opioid overdose and other substance use and mental health topics to help communities, clinicians, policy-makers and others with the information and tools to incorporate evidence-based practices into their communities or clinical settings.
Fact Sheet:
Using Naloxone to Reverse Opioid Overdose in the Workplace: Information for Employers and Workers | CDC (PDF | 785 KB) - This fact sheet helps employers understand the risk of opioid overdose and provides guidance about establishing a workplace naloxone program.
Tips for Teens: The Truth About Opioids | SAMHSA - This fact sheet for teens provides facts about opioids. It describes short- and long-term effects and lists signs of opioid use. The fact sheet helps to dispel common myths about opioids. Access sources cited in this fact sheet.
Toolkits:
Medication-Assisted Treatment (MAT) for Opioid Use Disorder in Jails and Prisons: A Planning and Implementation Toolkit | National Council of Behavioral Health - Developed by the National Council of Behavioral Health, this guide provides correctional administrators and healthcare providers tools for implementing MAT in correctional settings.
Opioid Overdose Prevention Toolkit | SAMHSA -This toolkit offers strategies to health care providers, communities, and local governments for developing practices and policies to help prevent opioid-related overdoses and deaths. Access reports for community members, prescribers, patients and families, and those recovering from opioid overdose.
Evidence Reviews/Guidebooks:
Evidence-Based Strategies for Preventing Opioid Overdose: What’s Working in the United States | CDC (PDF | 11.5 MB) - This CDC document reviews evidence-based strategies to reduce overdose. It explains why these strategies work, the research behind them, and examples of organizations that have put these strategies into practice.
Use of Medication-Assisted Treatment in Emergency Departments | SAMHSA - This guide examines emerging and best practices for initiating medication-assisted treatment (MAT) in emergency departments.
Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings | SAMHSA -This guide focuses on using medication-assisted treatment for opioid use disorder in jails and prisons and during the reentry process when justice-involved persons return to the community.
Telehealth for the Treatment of Serious Mental Illness and Substance Use Disorders | SAMHSA - This guide reviews ways that telehealth modalities can be used to provide treatment for serious mental illness and substance use disorders including opioid overdose among adults.
Treatment Improvement Protocols/Manuals:
TIP 63: Medications for Opioid Use Disorder | SAMHSA - This Treatment Improvement Protocol (TIP) reviews the use of the three Food and Drug Administration (FDA)-approved medications used to treat OUD—methadone, naltrexone, and buprenorphine.
Advisory: Opioid Therapy in Patients With Chronic Noncancer Pain Who Are in Recovery From Substance Use Disorders | SAMHSA - This advisory addresses screening and assessment tools, nonpharmacologic and nonopioid treatment for chronic pain, and the role of opioid therapy in people with chronic noncancer pain and SUDs.
Overdose Prevention & Naloxone Manual | HRC - This Harm Reduction Coalition (HRC) manual outlines the process of developing an Overdose Prevention and Education Program that may involve a take-home naloxone component.
Websites:
SAMHSA
- Medication-Assisted Treatment (MAT)
- MAT Medications, Counseling, and Related Conditions
- Opioid Overdose
- Know the Risks of Using Drugs
Other federal websites
- HHS.
 gov/opioids
gov/opioids - Opioids | NIDA
- Drug Overdose | CDC
- Rx Awareness | CDC
Visit the EBPRC for additional information, including Treatment Improvement Protocols, toolkits, resource guides, clinical practice guidelines, and other science-based resources.
Unpleasant Companions: What Mental Conditions Often Accompany Depression
Bombora publishing house publishes the book “So-so. Effective self-therapy for those who are tired of depression, anxiety and misunderstanding" by psychiatrist and psychotherapist Kirill Sychev. Sychev calls himself a punk and a cynic. Perhaps that is why his book on a serious topic, dedicated to a sad illness, makes you smile in places. Forbes Life publishes a chapter on diseases - private companions of depression.
We almost forgot about the conditions that resignedly sit next to depressive disorders. There are a lot of them, and very often these conditions are even confused with depression itself. Every day people come to me with such diagnoses. This happens for four main reasons (in my amateurish opinion).
There are a lot of them, and very often these conditions are even confused with depression itself. Every day people come to me with such diagnoses. This happens for four main reasons (in my amateurish opinion).
1. A psychiatrist has a very peculiar knowledge of mental illness. Such knowledge is very actively formed by the phrases “the professor knows better”, “it’s too early for you to think”, “what kind of public honey”, which steadily sound first inside the cathedral walls, and then in the heads of our doctors. And if you have a rough idea of what a particular disease looks like, they can still teach you how to distinguish it from another similar one or make two diagnoses at once, they rarely say.
2. For some reason, old-school Soviet psychiatrists believe that making two diagnoses at once is bad and merciless to patients. But their point of view is not supported by anyone in our mortal scientific world. Because because of this, the whole point of treatment is often lost. One sore provokes another - and vice versa.
Because because of this, the whole point of treatment is often lost. One sore provokes another - and vice versa.
3. In a serious condition, a person tends to describe only the most unbearable. Only the most distressing symptoms come from the lips of patients. And what is a little deeper often slips away and is lost. And that's okay. I can advise you to write down all the worrying symptoms for a week right at the moment when they bother you. Whatever it is. Though diarrhea, even tachycardia, even the fear of meeting riot police on the street.
4. Many of the symptoms are very similar and even the same.
But it is important for us not to be mistaken. Indeed, the size and color scheme of the handful of tablets that you will stuff into your mouth in the mornings (and evenings) often depends on this.
It is difficult to say one hundred percent why depression has these satellites. But, most likely, in most cases this is due to genetic and physiological anatomical tricks and to human behavior during the formation of all these conditions.
But, most likely, in most cases this is due to genetic and physiological anatomical tricks and to human behavior during the formation of all these conditions.
Dependencies
So. Let's start with dependencies. These are very interesting states in the context of depression. First, depression and addiction can coexist. And this happens quite often. Because depression is a condition in which it is very bad. And we don't like it when it's bad. We want it to be good. And more fun. And the first thing that comes to mind is an alcoholic. The man begins to wait for the weekend. It will be possible to relax (read “fuck up”) and forget about everything. Because depression is a constant mental chewing gum. Depression is constant stress. And both emotionally and physically.
Vinishko is an antidepressant, a tranquilizer and a stimulant at the same time. Plus, unlike other drugs, it is absolutely monopolized and legal. You don't have to go to the darknet for it. It's right here in Red and White. Right in the yard. How can you refuse?
Plus, unlike other drugs, it is absolutely monopolized and legal. You don't have to go to the darknet for it. It's right here in Red and White. Right in the yard. How can you refuse?
I think we will discuss the addiction formation system in the next book. But, if very briefly, the more and more often you drink, the more depressive thoughts in the morning. There you have a sense of guilt, and resentment, and sadness, and envy. And when dusk approaches, instead of a sexy vampire, you get a mad desire to close this circle as soon as possible. And you are better again.
I don't want to demonize alcohol. In general, my opinion on this issue is something like this: kill yourself only when you realize that you are killing yourself (and this is definitely not about suicide). When we drink every day, we must be aware of ourselves as drug addicts. And if we accept it in ourselves, then OK. We will just get sick a little more and die a little earlier. Who cares? Life is not the same for everyone. But when we try to drown out mental pain with an alcoholic, this is not a conscious choice. It is the desire to numb the pain. And we (psychiatrists) know much more effective methods of dealing with this. That's it.
We will just get sick a little more and die a little earlier. Who cares? Life is not the same for everyone. But when we try to drown out mental pain with an alcoholic, this is not a conscious choice. It is the desire to numb the pain. And we (psychiatrists) know much more effective methods of dealing with this. That's it.
To summarize: depression with its mental pains (there is no soul, if it's just a figure of speech) exacerbates the desire to drink, sniff and smoke. And when we drink, sniff, and smoke, we tend to exacerbate depression.
But there is another variant that is downright differentiated. This is when a depressive state is formed against the background of constant drunkenness (mephedrone, heroinism). That is, a person causes a similar state of mood with the help of drugs. And there are enough such cases.
I have quite a number of patients who come to me with depressive symptoms. And then finished with drug addiction. And everything recovered on its own. After all, alcohol at least changes our sleep, physical activity and nutrition. And those who have read the book carefully up to this point should be aware of how important these three processes are. So be aware and be honest with yourself. Even in addictions.
And then finished with drug addiction. And everything recovered on its own. After all, alcohol at least changes our sleep, physical activity and nutrition. And those who have read the book carefully up to this point should be aware of how important these three processes are. So be aware and be honest with yourself. Even in addictions.
Related material
Anxiety disorders
But you don't know what anxiety is, do you? Or do you know? Usually in smart textbooks on psychophysiology they write something like this.
Fear is your body's response to a real threat. And not only that - real, also recognizable. That is, the one you really know. So, as a child will not be afraid of an electric kettle until a direct collision of his delicate skin with this hot asshole.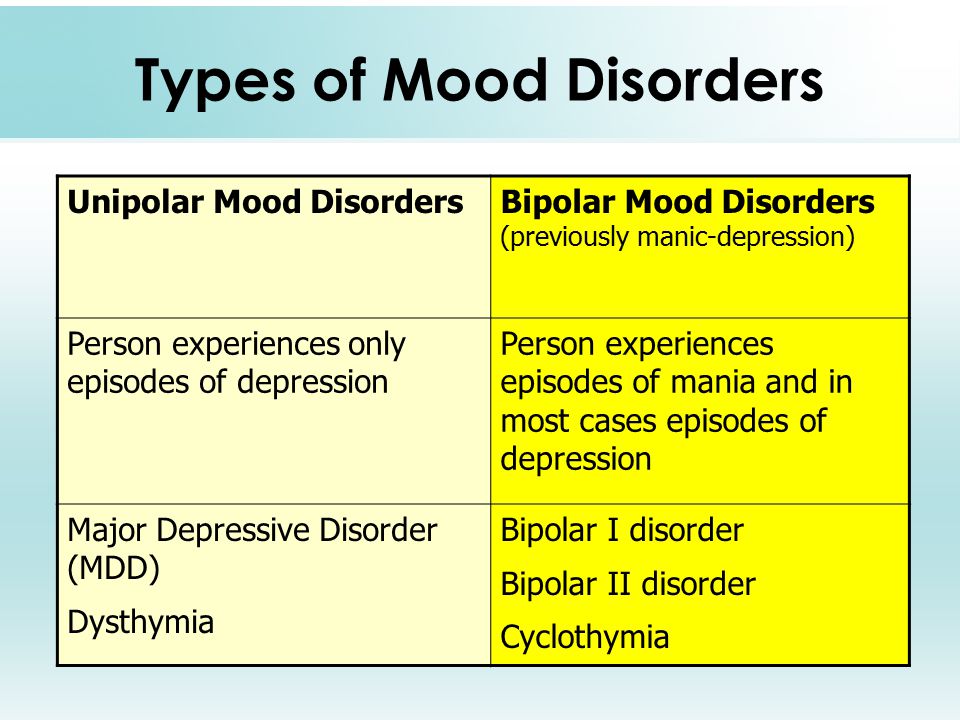 And then it will be. But then it won’t happen again, because he will understand that the kettle itself does not pose any threat. The thing is that you need to be careful around the kettle. And that's enough for your immunity.
And then it will be. But then it won’t happen again, because he will understand that the kettle itself does not pose any threat. The thing is that you need to be careful around the kettle. And that's enough for your immunity.
If we take a simpler linear situation, then we experience fear at the very moment when a servant of the people from the State Duma flies into the oncoming lane in a black Mercedes with a flashing light. And before that, we drove calmly, did not touch anyone and did not worry about anything. Our brain immediately orders to deign to stand out a large amount of adrenaline. Well, off we go according to our old scheme from the previous chapters.
But anxiety is a slightly different state. Although it seems like anxiety too, it seems like such vile nervousness too. And physically it feels about the same (and sometimes stronger). Yes, and we behave, to tell the truth, absolutely similarly.
First, it is variable in time. Maybe before the danger, when we cannot fall asleep for fear that tomorrow we will go to the proctologist. And he will poke his plump fingers right into our causal place. Or later, when everything was already stuffed into us, and the anxiety did not understand why it remained. Such is the proctological PTSD (you will soon understand what these letters are).
Or maybe even without any existing danger. Okay, stop scaring the proctologist. Let's return to the gopnik from the State Duma. You are driving along Sadovoye. And it begins to seem to you that these ghouls are having lunch right now. And according to the standard program, they are going to eat human flesh in a restaurant right here nearby. And they will go along this street. And they will go to the other side. And here you are. And the anxiety begins.
Alas, it turns out we need the alarm. Paradoxically, in order to experience fear less often. Well, more precisely, in order to get into life-threatening situations less often. After all, it is in them that we experience fear. That is, anxiety is our protector. But, as is often the case with defenders, she is also a part-time abuser. He says: “I’m so good, I’ll save you from evil dogs ... But it’s better not to go anywhere at all, then you won’t see dogs either.” And we are happy to fall for such nonsense, believe it and become dependent on anxiety. And then we can develop those same anxiety disorders.
Paradoxically, in order to experience fear less often. Well, more precisely, in order to get into life-threatening situations less often. After all, it is in them that we experience fear. That is, anxiety is our protector. But, as is often the case with defenders, she is also a part-time abuser. He says: “I’m so good, I’ll save you from evil dogs ... But it’s better not to go anywhere at all, then you won’t see dogs either.” And we are happy to fall for such nonsense, believe it and become dependent on anxiety. And then we can develop those same anxiety disorders.
Anxiety disorders are the most common conditions not only in depression. These are generally the most frequent pathological conditions of all mental states.
Let's quickly go over the main ones.
Related material
Post-traumatic stress disorder
Post-traumatic stress disorder. It's just like PTSD. After reading this paragraph, you can reread the part about the proctologist and enjoy the joke. Here is such a multi-way, ha!
It's just like PTSD. After reading this paragraph, you can reread the part about the proctologist and enjoy the joke. Here is such a multi-way, ha!
This condition occurs after wars, catastrophes and other threats to life. In our country, most often it occurs in women after obstetric violence in childbirth. There are huge statistics: more than thirty percent of all women who give birth get PTSD. This is a gigantic problem of the insane treatment of the staff to the absolutely helpless patients at that moment. Screaming, swearing, manipulation and disrespect lead to just such sad consequences.
Rape is also worth mentioning here. According to most reputable psychologists, such a violation of the integrity of a woman's boundaries is perceived as a threat to life, even if the rapist (and this is most often a relative or acquaintance) does not perceive the situation in this way.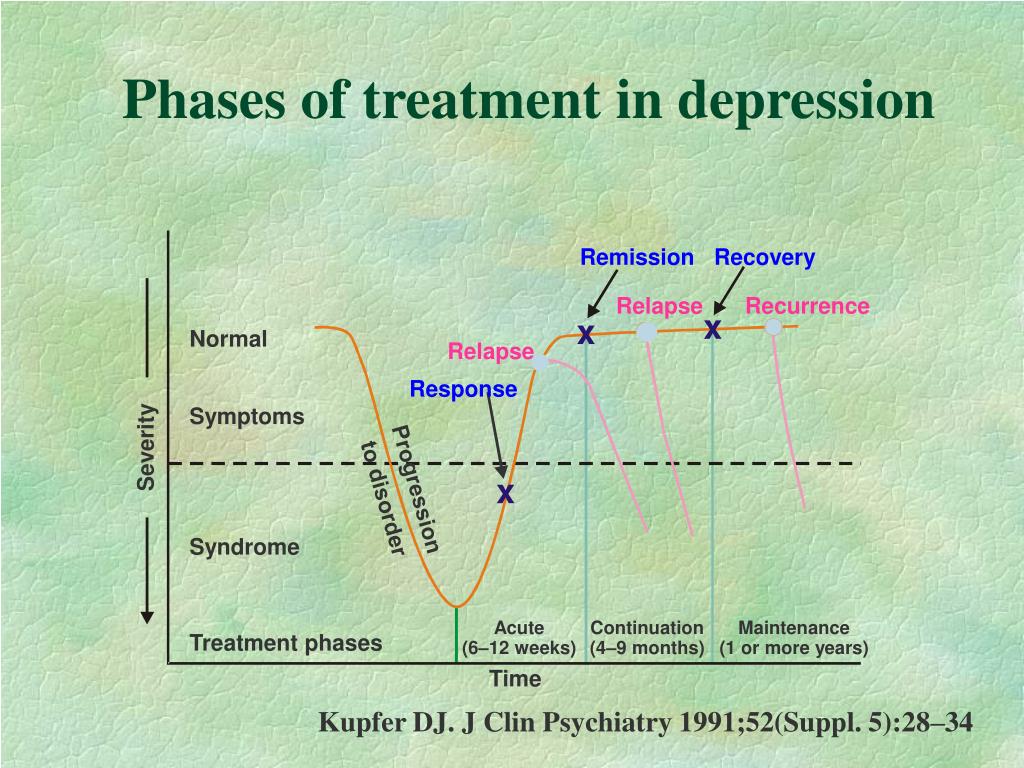
So what could be the symptoms here?
- Intrusive memories that repeat and repeat, mixed with the same disturbing and obsessive dreams. Sometimes it can even be a complete loss of orientation and awareness of the surrounding reality. The person seems to be back in the same place where the event took place. Often, terrible discomfort is brought by sounds similar to those from memories. Or partly reminiscent of landscapes. Or even time of day. Our brain is probably trying to protect us in this way.
So that we don't get into the same trouble again for anything in the world.
- And a person often forgets entire periods that make up a traumatic event.
- A person begins to avoid these thoughts, emotions, memories.
 He does not even want to talk about it or see people indirectly connected with the event. Does everything to forget it. But again, the brain does not want to do this at all. For him to forget is the same danger. And does he really need it? He's here so we don't die. Don't care about comfort.
He does not even want to talk about it or see people indirectly connected with the event. Does everything to forget it. But again, the brain does not want to do this at all. For him to forget is the same danger. And does he really need it? He's here so we don't die. Don't care about comfort.
Many times I have seen patients who could not describe anything at all, except for the emotions of rape. They couldn't even remember who it was or what it looked like. They began to feel shame and guilt. Absolutely absurd reasons for violence were expressed:
"I was to blame", "it was necessary with me, I'm bad." Women were alienated from friends, acquaintances, meetings. They ceased to be interested in what ignited them before. Some of them completely lost positive emotions.
I think you have already understood how difficult it can be to distinguish such a condition from ordinary major depression. Especially given the fact that many hide the events. I once had a patient who revealed the secret of rape after almost six months of therapy. Imagine what it cost her in terms of emotions. I have great admiration for these patients. You are cool. Not everyone can handle it. And can you.
Especially given the fact that many hide the events. I once had a patient who revealed the secret of rape after almost six months of therapy. Imagine what it cost her in terms of emotions. I have great admiration for these patients. You are cool. Not everyone can handle it. And can you.
And yes, PTSD can happen to men too. But I wanted to do a little for feminism. Too little is written about it. Even if you suddenly think that a lot.
Panic disorder
It is worth noting here that panic attacks occur in the majority of the population. 11 percent will have them at least once during the current year. And there is nothing especially terrible about them. It's just an intense fear. You go, for example, to the zoo. Approach the snake behind the glass. And there behind Harry Potter, bastard, dick - and threw you right at her. Well, an attack of suffocation immediately begins, you are shivering, pounding, your limbs go numb, sweat flows down your belly in the amount of half a liter in three minutes, you feel sick, your head is spinning. Also, there may be discomfort in the chest. And immediately thoughts, like cockroaches, ran: “stroke”, “heart attack”, “daeeeeeeeee”, “what if I go crazy with fear?”, “Or shit right on this python, and people will immediately point their fingers and laugh...". Everything around begins to seem strange and unreal.
Well, an attack of suffocation immediately begins, you are shivering, pounding, your limbs go numb, sweat flows down your belly in the amount of half a liter in three minutes, you feel sick, your head is spinning. Also, there may be discomfort in the chest. And immediately thoughts, like cockroaches, ran: “stroke”, “heart attack”, “daeeeeeeeee”, “what if I go crazy with fear?”, “Or shit right on this python, and people will immediately point their fingers and laugh...". Everything around begins to seem strange and unreal.
This state usually lasts up to ten minutes. And if you don’t do anything about it, then it will go away perfectly on its own. It's just that the body is so arranged that any changes should scare us very much. Our brains haven't changed much since the Stone Age. And we still expect (albeit subconsciously) danger from everything around.
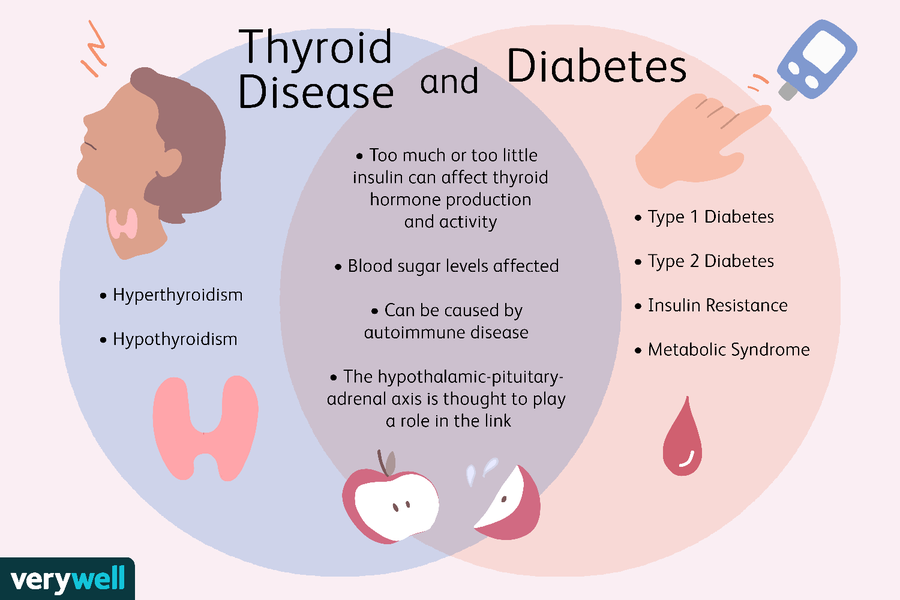
In general, panic attacks can also be the result of any changes in the body that you read about above.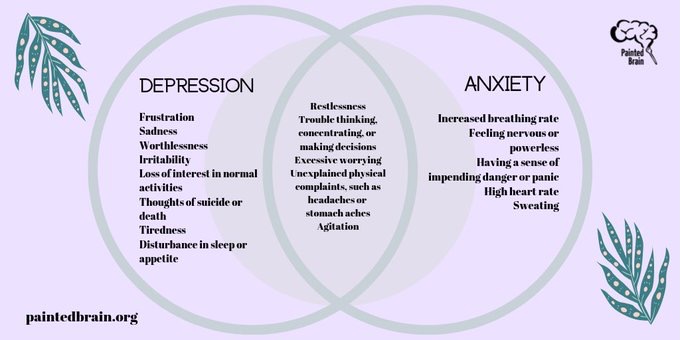 Iron deficiency and thyroiditis will easily invoke their diabolical symptoms. And you will probably be scared. At the very least, we never know 100 percent that this is happening. Usually in this case, panic attacks become a constant companion of a person. And it doesn't really depend on where or what you're doing. And also whether you are afraid of their repetition.
Iron deficiency and thyroiditis will easily invoke their diabolical symptoms. And you will probably be scared. At the very least, we never know 100 percent that this is happening. Usually in this case, panic attacks become a constant companion of a person. And it doesn't really depend on where or what you're doing. And also whether you are afraid of their repetition.
With panic disorder, opinions differ slightly on the diagnosis. I propose in this case to again refer to the American classification of diseases DSM-5. In order to make this diagnosis, your doctor will have to find out how long you have been suffering from this. And if panic attacks have been tormenting you for more than a month, then you will have to continue the diagnosis and ask two types of questions.
First: “Are you afraid of these attacks themselves? Do they cause persistent fear of their consequences? Do you think that you can go crazy because of them? Or die? Or lose control and throw yourself under a toy train at the mall while stripping naked?
Second: “Are you trying to avoid having these panic attacks? Less exercise to avoid tachycardia? Or do you strive to be in society less often so that at the time of the attack you don’t see laughter on the faces of colleagues in your tractor assembly shop?” Well, and the like.
And if at least one of the attacks was followed by at least one of these points, then hello - we have arrived! It's time to heal. Fortunately, such conditions are treated well. And most of the time, you don't even have to take pills. Everything will be removed after a full explanation of physiology and compliance with certain psychotherapeutic rules.
Phobias
I think everyone here has some idea of what it is. Depression is often (very often) accompanied by phobias.
Okay, let's figure it out. A phobia is such a tremendous fear of something specific, and not just everything. In order for you to be diagnosed with such a fear, this fear must last at least six months. And you should do your best to avoid the object of this phobia. And it doesn't have to be anything really dangerous. That is, if you are afraid to inject curare poison into yourself, this is not a phobia. Well, and finally, you must get away from all these anxieties, discomforts and avoidance of problems. Someone will have them at work (“I’m afraid to go to the office, there are a lot of ficuses, they will devour me”). For some, phobias complicate social life (“I don’t go out because I’m afraid of lapdogs ... They are everywhere”).
And it doesn't have to be anything really dangerous. That is, if you are afraid to inject curare poison into yourself, this is not a phobia. Well, and finally, you must get away from all these anxieties, discomforts and avoidance of problems. Someone will have them at work (“I’m afraid to go to the office, there are a lot of ficuses, they will devour me”). For some, phobias complicate social life (“I don’t go out because I’m afraid of lapdogs ... They are everywhere”).
Social phobia deserves special mention. It is considered a separate disease. And it is very common in depression. These are states when we are afraid of the possibility of interacting with other people. Someone - any interaction. And someone only with people from his office (in which there are also ficuses ...).
There is a state in which a person is afraid of everything. More precisely, he does not even understand what exactly he is afraid of.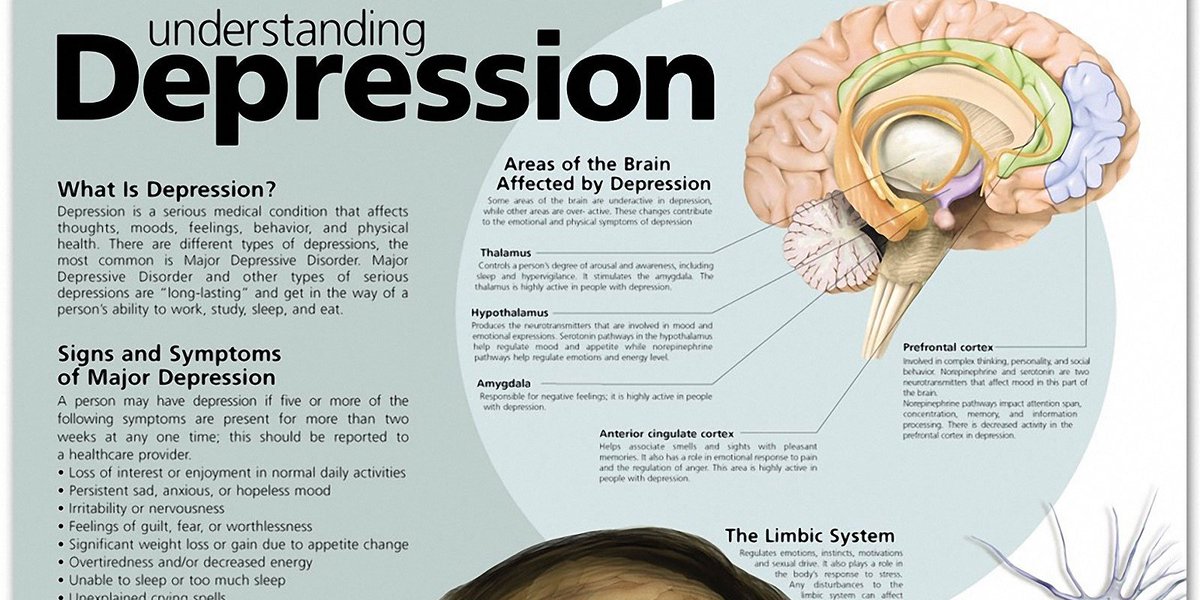 This is one of the most common diseases - friends of depression. It is easy to confuse this depression with him. And it's even easier to forget to make a second diagnosis.
This is one of the most common diseases - friends of depression. It is easy to confuse this depression with him. And it's even easier to forget to make a second diagnosis.
These guys are not very good at controlling anxiety, but they really want to and constantly try. Because of this, such a jerky state of constant excitement and irritability is formed. And in an excited and irritable state, we quickly use up our internal resources and get tired. It becomes difficult for us to concentrate. After all, we all the time think about what has strained us in the past and what will strain us in the future. We are not in the moment at all. Because of all of the above, sleep is disturbed, we find it difficult to fall asleep and easily wake up from any rustle of the iPhone on the nightstand. In addition, such patients complain of tension and pain in the muscles all the time.
Here I would like to put the fifth point and write about obsessive-compulsive disorder. But he was recently given a whole chapter in each of the classifications of diseases, so we cannot call him alarming. Naturally, this is a convention.
But he was recently given a whole chapter in each of the classifications of diseases, so we cannot call him alarming. Naturally, this is a convention.
Obsessive Compulsive Disorder
So. Obsessive-compulsive disorder is... but okay.
Obsessions are obsessive thoughts that tell us that if we do not wash our hands five hundred thousand million times, we will die from an attack of microbes. And that we didn't close the door, or turn off the stove, or take our medicine.
Compulsions are purposeful, but absolutely meaningless actions by which we try to eliminate these thoughts. For example, we wash our hands five hundred thousand million times or check the stove a couple of dozen times before leaving. They didn't even turn it on though. Sometimes compulsions are a compulsive counting in the head. Sometimes these are certain verification schemes (turn the handle to the right three times, then to the left two and again to the right four. Well, and then knock on the door with your right fist twice. But with your left - in no case. Otherwise, all over again). And if you think I'm joking here again, then no. This is an absolutely working scheme of one of my patients.
Sometimes compulsions are a compulsive counting in the head. Sometimes these are certain verification schemes (turn the handle to the right three times, then to the left two and again to the right four. Well, and then knock on the door with your right fist twice. But with your left - in no case. Otherwise, all over again). And if you think I'm joking here again, then no. This is an absolutely working scheme of one of my patients.
It was I who brought the classical variants from textbooks. But if you take something more interesting... For example, a girl thinks that she can kill her boyfriend with a knife. These thoughts are always with her. She is afraid of them and tries her best to get rid of them. And in order to do this, she takes these knives from the house to the trash. But for some reason, this fear only intensifies.
Let's not go deep into the origin mechanism.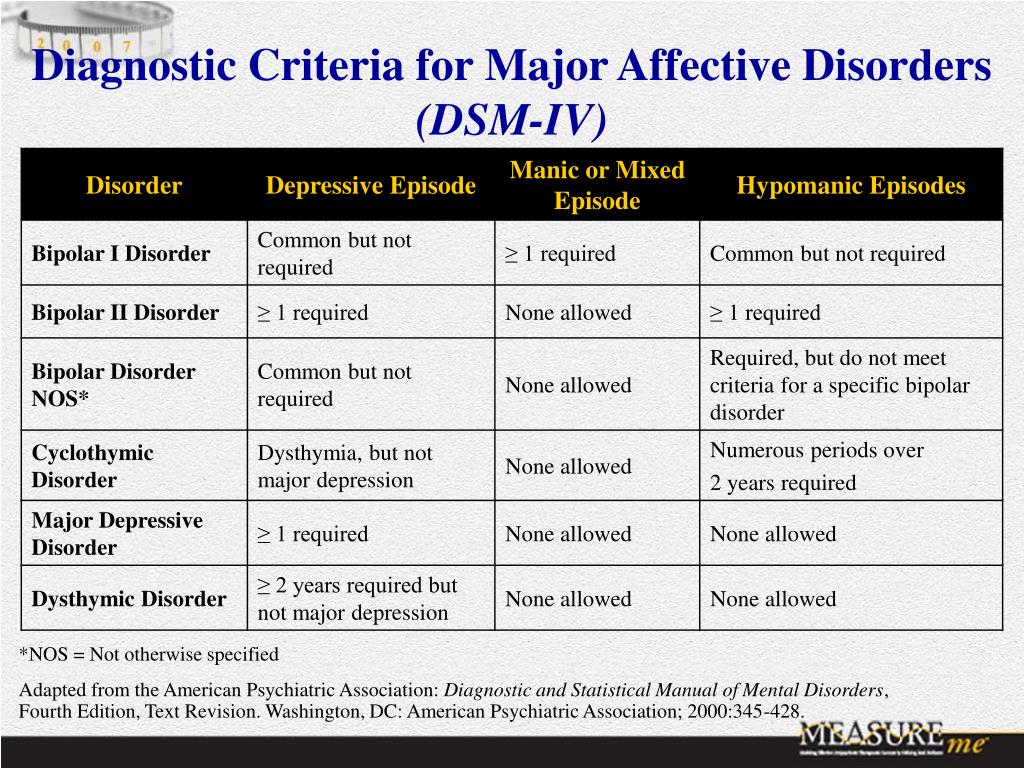 Scientists now agree that OCD develops due to malfunctioning of some parts of the brain responsible for memory. Well, and all the disturbing mechanisms, of course, exacerbate this.
Scientists now agree that OCD develops due to malfunctioning of some parts of the brain responsible for memory. Well, and all the disturbing mechanisms, of course, exacerbate this.
Depressive disorders in their various manifestations occur in OCD in 63 percent of cases. That's it.
The sore is treated hard and for a long time. These are some of the most difficult cases regarding psychotherapy. But therapy is becoming more effective, new schemes of drug care are emerging. So, most likely, soon everything will be better.
The last thing I'll mention in this chapter is eating disorders (EDDs). Since they are now found in more than half of women in one form or another. And men, too, suffer from them more and more often. And the treatment is complex, long and not always pleasant. At the same time, there are an extremely limited number of specialists in Mother Russia.
Do you remember, at the very beginning, we discussed the symptoms of depression? I said there that the appetite changes very often. And together with eating habits, everything is not limited to appetite. What does this group include? Actually a lot of things.
You can start with anorexia nervosa. This is when a person reads a group in contact with 40 kilograms (well, or there is 10 - 20 kilograms) And he forms a distorted image of an ideal body. And there is a constant fear of obesity. A person loses weight and still feels anxiety from every broccoli eaten. Often this leads to death, unfortunately. This is generally the most common mental state leading to death.
Add depression to that and I think you understand.
There is also compulsive overeating. Usually a person is on a diet. But on Wednesdays, he becomes so unbearable that he eats cake, meatballs, cheesecakes, bread and garlic. Then he drinks cola and adds boiled eggs with pasta seasoned with mayonnaise. Then he tortures himself with diets for another week and all over again. By the way, diets are evil. They almost always end up leading to further weight gain.
Usually a person is on a diet. But on Wednesdays, he becomes so unbearable that he eats cake, meatballs, cheesecakes, bread and garlic. Then he drinks cola and adds boiled eggs with pasta seasoned with mayonnaise. Then he tortures himself with diets for another week and all over again. By the way, diets are evil. They almost always end up leading to further weight gain.
And if, after gluttony, a person overeats on laxatives or vomits cheerfully in a tubzik, this is bulimia nervosa.
There are several other less common ailments on this spectrum. But more about them later.
Each of these conditions requires complex treatment. Because the reasons can be completely different, and as a result, food absorption is disturbed, physical health in general worsens (we do not work on solar energy).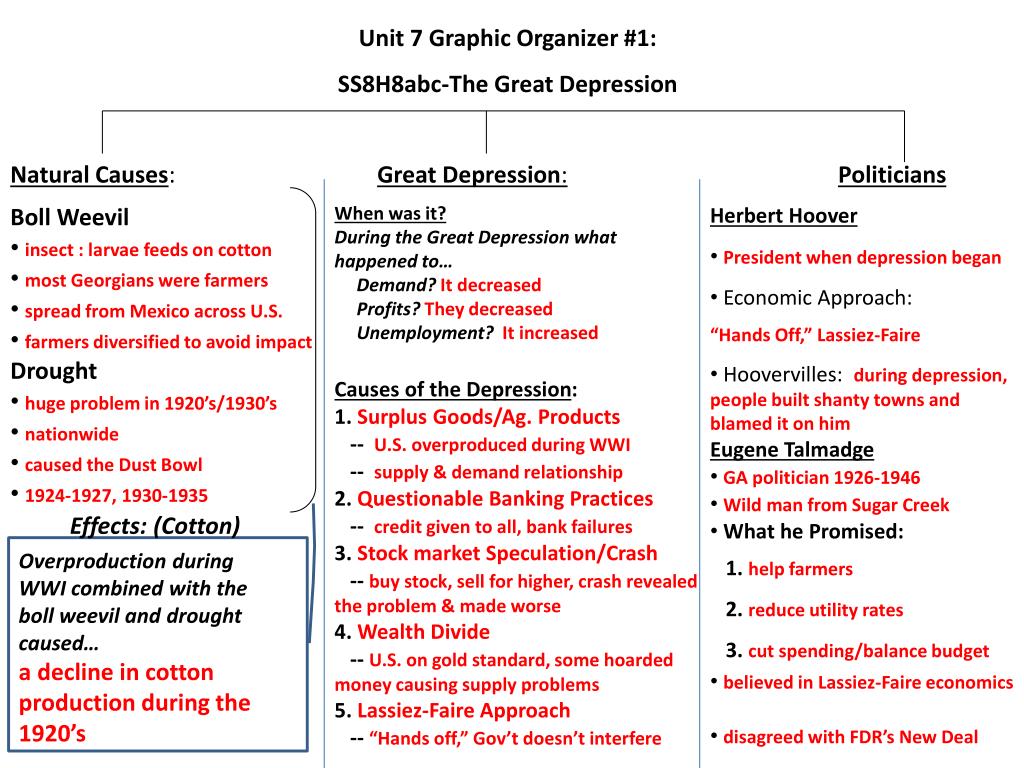 Well, other mental disorders are very fond of being activated against the background of all this goodness. So, if you notice something similar in yourself, it’s better to urgently rush to the doctor (not a nutritionist).
Well, other mental disorders are very fond of being activated against the background of all this goodness. So, if you notice something similar in yourself, it’s better to urgently rush to the doctor (not a nutritionist).
Types of depression - iFightDepression [EN]
There are different types of depression, which proceed in different ways.
Signs and symptoms vary in number, timing, severity and frequency, but are generally very similar. Because different types of depression are treated differently, it is important to pinpoint the type of depression. Depending on gender, age and cultural characteristics, people have different symptoms and severity of depression.
Neurotic, reactive (minor) depression is treated with psychotherapy.
Somatic and psychotic - medication. These terms are used by psychiatrists.
Studies have shown that depression has a phasic course. Periods of normal mood alternate with depressive episodes. Sometimes, instead of a depressive phase,
there may be a manic phase, which is manifested by irritability and high mood. If so, then it is not depression, but bipolar disorder (a more serious illness).
1. Depressive episode
The most common and typical form of depression is the depressive episode. An episode lasts from a few weeks to a year, but is always longer than 2 weeks. A single depressive episode is called a unipolar episode. Approximately one third of affected people experience only one episode, or "phase", during their lifetime. However, if a person does not receive appropriate treatment for depression, there is a risk of recurrent depressive episodes in the future. Depressive episodes always affect a person's performance to one degree or another.
2. Intermittent (recurrent) depressive disorder
When a depressive episode recurs, it is recurrent depressive disorder or major depressive disorder, which usually begins in adolescence or early adulthood. With this kind of depression, depressive phases, which can last from several months to several years, alternate with phases of normal mood. This type of depressive disorder can seriously affect performance and is unipolar in nature (no manic or hypomanic phase). This is the so-called "classic" or "clinical" depression.
3. Dysthymia
Dysthymia presents with milder and less severe symptoms than a depressive episode or recurrent depression. However, the disorder is permanent, with symptoms lasting much longer, at least 2 years, sometimes decades, which is why it is called "chronic depression". This disorder is unipolar and also affects performance. This type of depression sometimes develops into a more severe form (major depressive episode) and if this happens it is called double depression.
4. Bipolar depression, type I
This is the type of depression in bipolar disorder, formerly called manic-depressive illness, and is less common than unipolar depression. It consists of alternating depressive phases, phases of normal mood and so-called manic phases.
Manic phases are characterized by excessively high mood associated with hyperactivity, anxiety, and decreased need for sleep.
Mania affects thinking, judgment and social behavior causing serious problems and difficulties. When a person is in a manic phase, he makes frequent casual unsafe sex, makes unwise financial decisions. After a manic episode, such people often experience depression.
The best way to describe these "emotional upheavals" is "to be on top of the world and fall into the depths of despair".
Symptoms of the phases of depression in bipolar disorder are sometimes difficult to distinguish from unipolar depression.
5. Bipolar depression type II
More like recurrent depressive disorder than bipolar disorder. In this disorder, multiple depressive phases alternate with phases of mania, but with less pronounced euphoria. During these phases, family and loved ones may even mistakenly assume that the person is doing well.
6. Mixed anxiety-depressive disorder
In anxiety-depressive disorder, the clinical picture is very similar to depression, however, in depression, depressive syndromes always come first. In this case, both anxious and depressive symptoms are evenly combined.
7. Depressive psychotic episode
A special form of depressive episode is psychotic or delusional depression. Psychosis is a condition in which people see or hear things that do not exist (hallucinations) and/or have false ideas or beliefs (delusions). There are various types of delusions such as self-accusation for no reason (delusion of guilt), financial ruin (delusions of poverty), feeling of an incomprehensible illness (hypochondriac delusions). People with delusional depression almost always require inpatient psychiatric treatment. Psychotic episodes can be either unipolar or bipolar.
8. Atypical depression
This type of depression is characterized by hypersensitivity and mood swings, overeating and drowsiness, panic attacks. This type of depression is mild and can be bipolar.
9. Seasonal depressive disorder
This type of depression is similar to atypical depression and comes on seasonally with climate change, usually in autumn or winter.