Borderline personality splitting
Splitting in Borderline Personality Disorder
- Home
- Blog
- Understanding splitting in borderline personality disorder
Page medically reviewed by Dr Liam Parsonage (BA, MBBS, MRCPsych, PGCert) Consultant Psychiatrist at Priory Hospital North London
What is Splitting in Borderline Personality Disorder (BPD)?
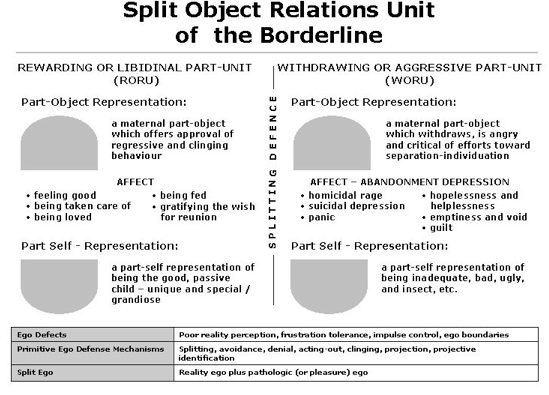
‘Splitting’ is common symptom for people with mental health issues like borderline personality disorder (BPD). Splitting means to divide something. It causes a person to view everything and everyone in black and white, ‘absolute’ terms. It stops them from being able to recognise or accept paradoxical qualities in someone or something and doesn’t allow for any ‘grey areas’ in their thinking. Splitting is a defence mechanism deployed by people with BPD and other personality disorders. Its development can be linked to experiences of early life traumas, such as abuse and abandonment.
Seeing and responding to the world in these extremes, through either a filter of positivity or negativity, can leave a person with BPD exhausted and emotionally drained. It can also lead to strains or fractures in their relationships as those close to the person become more and more affected by their behaviour. It's a commonly used defence mechanism that is done subconsciously in an attempt to protect against intense negative feelings such as loneliness, abandonment and isolation.
What Causes Splitting?
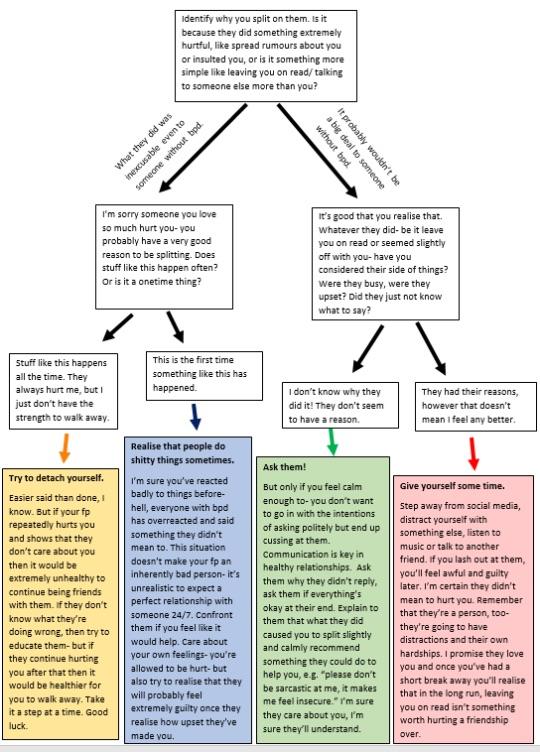
A split might often be caused by an event that triggers the extreme binary emotions that characterise BPD. Sometimes, these events might seem harmless or small to people without BPD, but they may in some way relate to previous trauma. This event might spark fears of abandonment, separation or severe anxiety.
The root cause is linked to how we develop as a child. When a baby enters the world, they experience the things within it as either good or bad, or as all or nothing.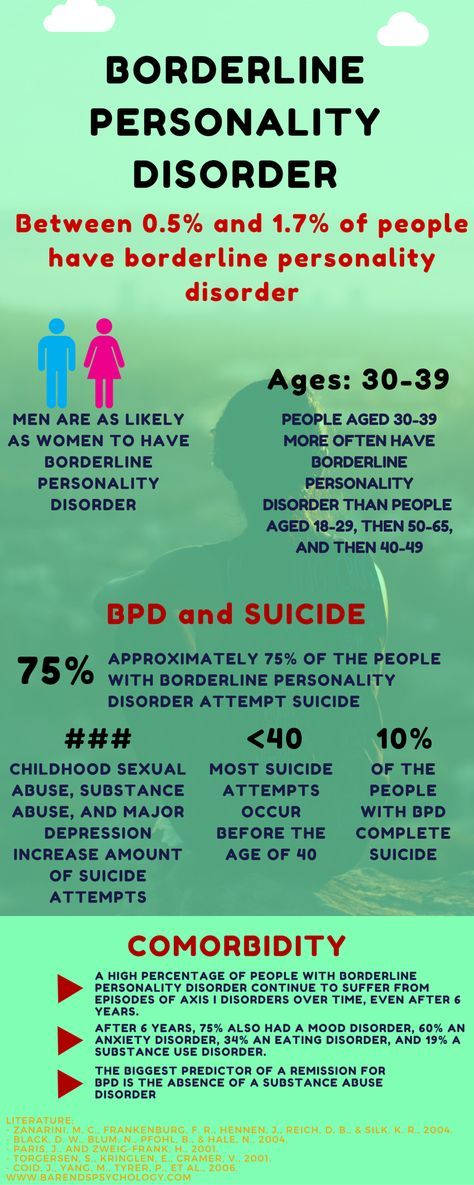 As the baby develops psychologically, they begin to understand that the world isn’t just good or bad. They become able to integrate the idea that good and bad can be held in the same object.
As the baby develops psychologically, they begin to understand that the world isn’t just good or bad. They become able to integrate the idea that good and bad can be held in the same object.
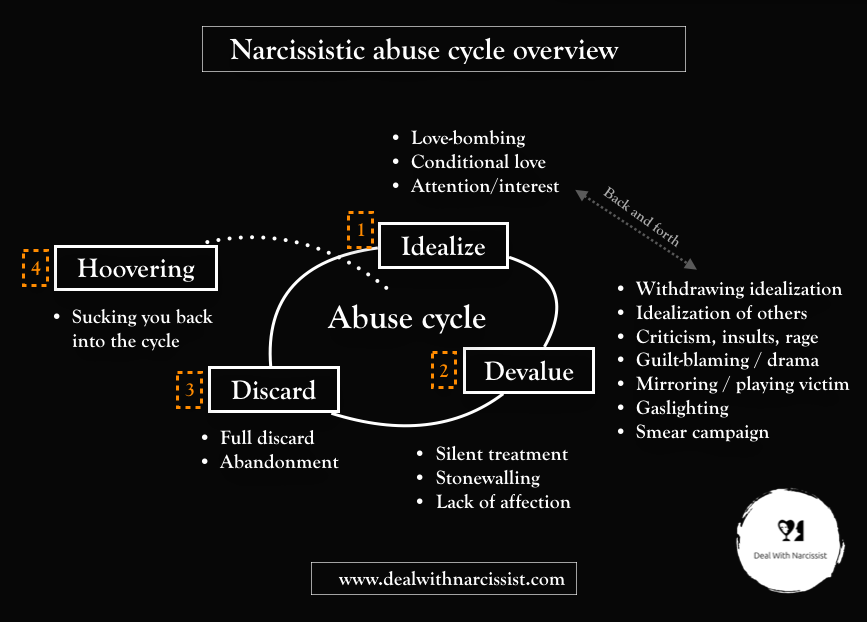
People with borderline personality disorder often experience overwhelming emotions and struggle to integrate the concept that good and bad can co-exist in another person. Splitting is a psychological mechanism which allows the person to tolerate difficult and overwhelming emotions by seeing someone as either good or bad, idealised or devalued. This makes it easier to manage the emotions that they are feeling, which on the surface seem to be contradictory.
The Effects of Splitting
Examples of splitting
A person with borderline personality disorder may use splitting in the following ways:
- People will be seen as ‘perfect’ or ‘evil’
- Something will ‘always’ or ‘never’ go right
- Someone will ‘always’ or ‘never’ be loving
A person may hold onto these black and white views permanently.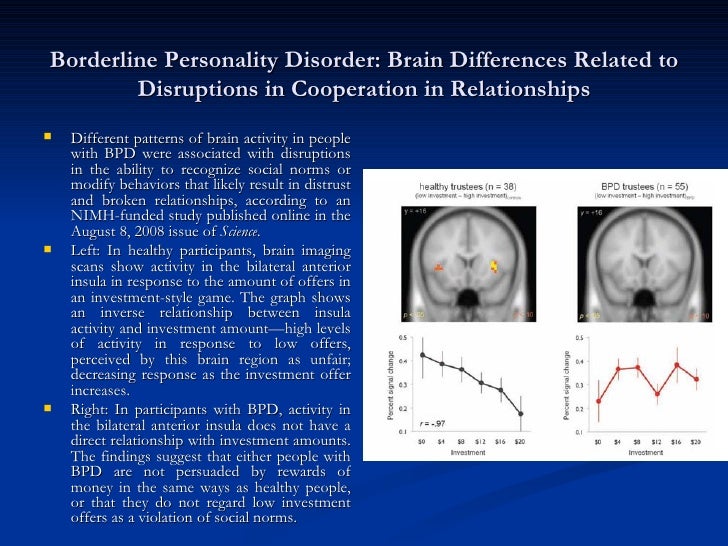 For others, their opposing views can fluctuate over time, where they switch from seeing someone or something as entirely good to entirely bad, or vice versa.
For others, their opposing views can fluctuate over time, where they switch from seeing someone or something as entirely good to entirely bad, or vice versa.
Symptoms of splitting
A common symptom of BPD is emotional dysregulation – this is where a person is less able to manage their emotional responses than individuals who don’t struggle with a personality disorder. Therefore, when a person with the disorder splits and perceives something or someone to be entirely good or bad, they are likely to respond in a way that falls outside what would be expected. These extreme emotions can be exhausting, both to the person with BPD and those who are closest to them.
When seeing someone or something as entirely good, this can leave the person with BPD vulnerable to harm and danger as they are unable to see associated risks. Also, when believing a person is completely perfect, this can also lead to co-dependency, where they rely on that individual for all their wants and needs. This can be harmful to both parties, and a draining responsibility.
This can be harmful to both parties, and a draining responsibility.
When a real or perceived slight is then experienced by the person with borderline personality disorder, this can cause them to feel disappointed, betrayed, unloved or abandoned, and view the other party as entirely bad. The individual may then become angry, or withdraw entirely. They may also become incredibly angry with themselves. There are techniques to manage anger during this time.
Care and Management of BPD Splitting
If you are close to a person with borderline personality disorder, there are a number of ways to support them so that they are able to better manage their splitting behaviour. These include the following:
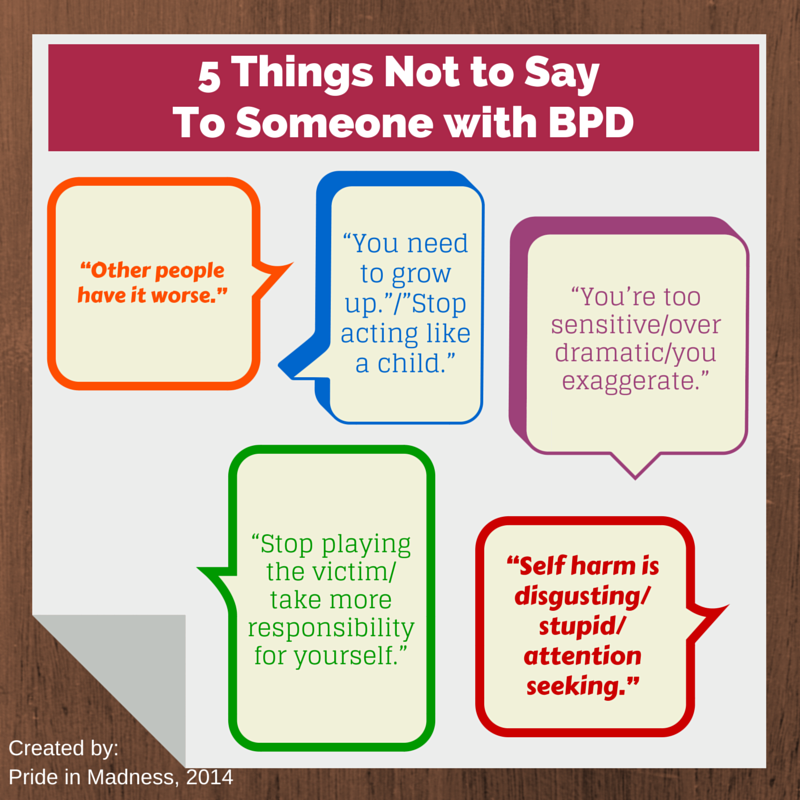
- Remember that splitting is a symptom of borderline personality disorder - while it can be difficult not to take their words and actions personally, remember that the person is not intentionally trying to hurt you.
 Splitting is something that they are doing unknowingly
Splitting is something that they are doing unknowingly - Think about how you respond to the person who is splitting - try to remain calm and if you find this difficult, give yourself an opportunity to cool down by postponing the conversation
- Show the person that you really do care - a person with BPD is likely to be dealing with feelings of abandonment, isolation and loneliness. Therefore, try to show the person that they are cared for and that they are heard
- Set healthy boundaries to help manage behaviours – work with the person with BPD to set limits so that they understand the behaviours that you won’t tolerate, such as throwing objects or violence. While these boundaries may be unintentionally challenged at times, make sure that you carry out the pre-determined consequence, which may include walking away from the situation
It is also important for you to encourage the person to receive the right treatment, and be an advocate of it when they do so.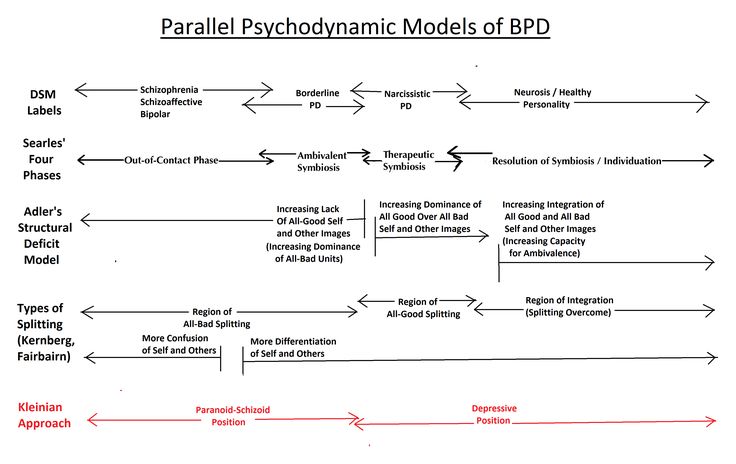
BPD Treatment
BPD is a very personal issue, so treatment is geared towards lessening the negative impact it might be having on your life. After you've received a diagnosis for BPD, you might undergo a course of talking therapy and take on a prescription of appropriate medication to help with the ongoing management of the symptoms.
A core therapy type that's developed specifically for BPD is dialectical behaviour therapy (DBT). DBT comes from the idea that two different beliefs or thoughts, that seem to be the opposite of each other, can both be simultaneously true. In DBT, these opposing ideas are acceptance (accepting yourself) and change (changing your behaviour). Over time, you will work out alternative and healthier ways of dealing with extreme emotions, helping to cultivate a worldview that is less self-destructive to you and those around you.
World Class BPD Treatment at Priory
At Priory, our mental health experts are experienced in providing treatment for people with borderline personality disorder.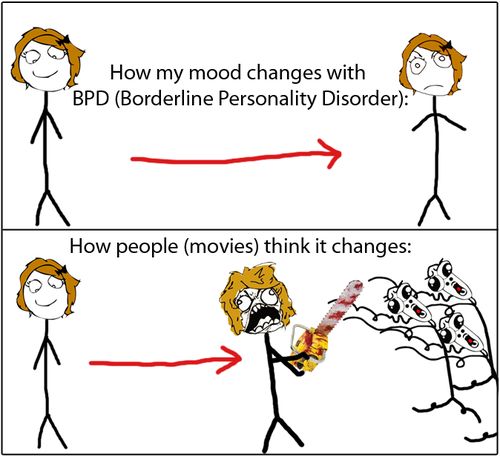 Depending on the severity of an individual’s personality disorder and the type of treatment that is recommended, support at Priory can be provided on a residential, day care or outpatient basis.
Depending on the severity of an individual’s personality disorder and the type of treatment that is recommended, support at Priory can be provided on a residential, day care or outpatient basis.
Our residential treatment programmes provide people with 24-hour care and support, which can include psychotherapy sessions, rehabilitative workshops and creative classes. Day care and outpatient care can also be provided when a borderline personality disorder isn’t as severe, providing a person with the opportunity to take part in therapy sessions in a flexible and supportive environment.
Whatever treatment plan helps you to lessen the negative impact BPD and splitting can have on your life, you'll find the world class team at Priory can help you regain control of your life. Use the information below to get in touch with us for a compassionate discussion about your symptoms and how we can support you today.
Get in Touch Today
For details of how Priory can provide you with assistance regarding mental health and wellbeing, please call 0800 840 3219 or click here to submit an enquiry form.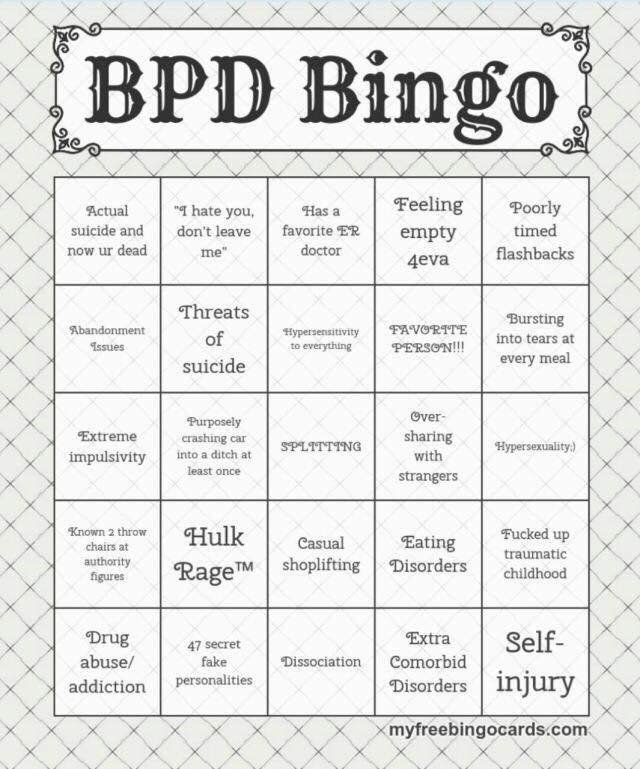 For professionals looking to make a referral, please click here
For professionals looking to make a referral, please click here
Meaning, duration, causes, and more
In borderline personality disorder (BPD), splitting means a person has difficulty accurately assessing another individual or situation. It can lead to intensely polarizing views of others, for instance, as either very good or very bad.
Instead, they see something as completely good or completely bad, and their assessment may switch back and forth rapidly. A person typically splits unconsciously or without realizing it.
Rather than seeing people in their lives as complex human beings with good, bad, and in-between characteristics, they may apply intensely polarizing or exaggerated labels. To them, their partner may be the “worst partner in the world” one day and the “greatest partner ever” the next.
Read on to learn more about what splitting looks like in BPD, its symptoms, duration, management strategies, and more.
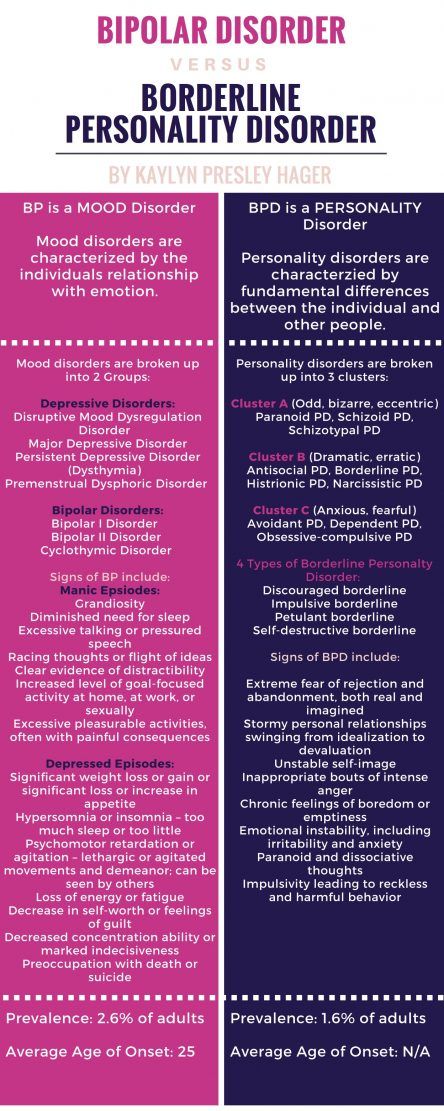
BPD is a type of personality disorder that causes people to experience intense emotions, self-image issues, and impulsive behaviors.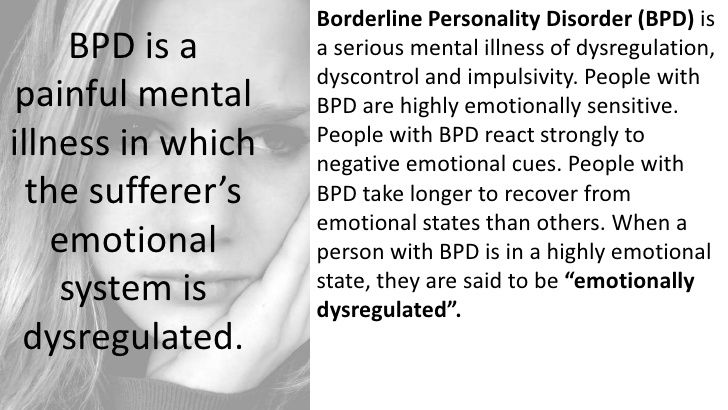 They often lack stability in personal relationships and behave irrationally.
They often lack stability in personal relationships and behave irrationally.
Splitting is a type of black-and-white thinking. It causes a person to perceive others — or even themselves — as all good or all bad. These perceptions may shift rapidly.
People engage in splitting because they have conflicting emotions about something or someone they find difficult to manage or intolerable. They may have unstable and intensive personal relationships that alternate between extreme highs and lows.
Often, individuals with BPD have difficulty maintaining a consistent sense of self. This also disrupts their perceptions of other people.
Splitting is a defense mechanism, and it is not unique to BPD. People with other mental health conditions, as well as those without any underlying mental illness, may also occasionally engage in splitting. However, in BPD, splitting is an ongoing pattern of relating to others that may often contribute to relationship instability.
There is no set period that a splitting behavior will last.
A person may alternate between conflicting perceptions of another several times a day, or their perception of someone as all good or all bad may last a very long time. They will continue to split until they find more effective ways to manage BPD symptoms.
Splitting is not always immediately apparent to people witnessing it. Individuals with BPD feel their emotions intensely and may believe that their perceptions reflect reality.
Some signs that a person is splitting include:
- idealizing someone one moment, then later calling them abusive or toxic
- not seeing nuance in the relationships or actions of others
- cutting people out of their life, then expressing feelings of abandonment
Some signs a person might detect in themselves include:
- many chaotic or unstable relationships
- rapidly changing feelings about other people
- feelings that seem more intense than the feelings of others
- alternating between pushing someone away and wanting them to stay
Some examples of splitting include:
- telling one’s romantic partner to leave, then begging them not to leave when they actually do
- attributing another person’s behavior to their fundamental goodness or badness instead of seeing them as a complex person with good, bad, and in-between attributes
- perceiving oneself or others as all good or all bad
- having very intense emotions about other people that shift rapidly according to a person’s feelings or circumstances
For people with BPD, splitting may be a way to manage conflicting emotions.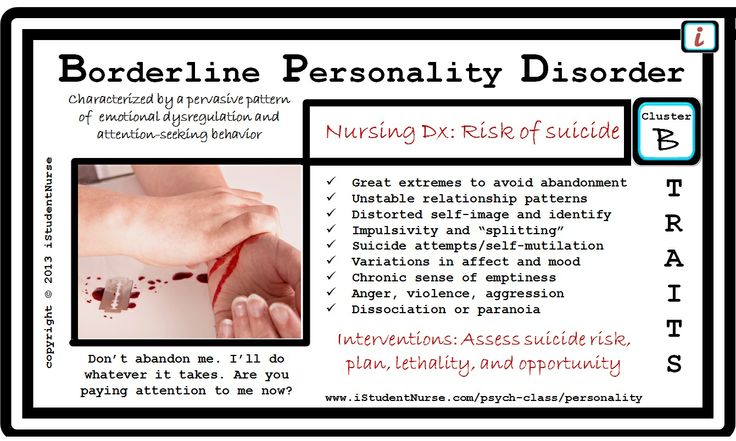
Experts do not fully understand the causes of BPD, but research points to several different potential causes, including:
- trauma or stress in childhood
- an invalidating environment in early childhood
- genetic factors
A person who thinks they may be splitting may wish to consider whether this is a pattern of behavior for them. If it is, treatment for BPD may be helpful.
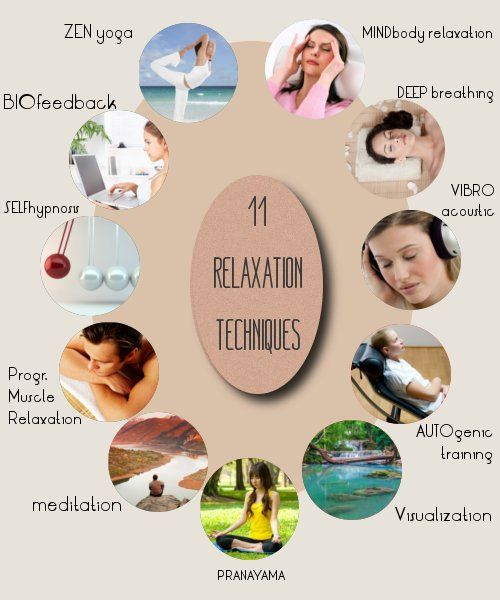
Some prevention strategies include:
- Gaining perspective: Considering whether a more moderate perspective might be helpful and reframing the situation. For example, perhaps a person did not destroy one’s life but disappointed or hurt them instead.
- Considering other traits: Practice thinking about naming other characteristics of the person and about the language contributing to splitting, such as “always” and “never.” Practice using more accurate language.
- Cultivating empathy: Consider why a person might behave as they do.

- Keeping a journal: A person can log emotions and better understand what experiences increase splitting behaviors, as well as one’s own feelings that come up during splitting.
The Food and Drug Administration (FDA) has not approved any medications to treat BPD. However, doctors may still prescribe medication to manage symptoms.
One of the most effective treatments is psychotherapy. Three different therapeutic approaches have proven especially helpful:
- Mentalizing-based therapy: This approach cultivates understanding and empathy to help people better manage intense emotions. The goal is to cultivate curiosity, so people make fewer assumptions about others’ behavior.
- Dialectical behavioral therapy: This approach offers mindfulness-based skills to help a person calm their emotions. It also includes social skills and emotion regulation training.
- Transference-focused psychotherapy: In this model, the therapist uses their relationship with the client as an avenue to explore and reframe problematic emotions and behaviors.
A doctor can refer a person to a psychotherapist and may also make recommendations about medications.
Individuals can contact a healthcare or mental health professional if:
- they often experience splitting
- they have a history of unstable, abusive, or chaotic relationships
- they frequently have intense emotions that feel difficult to control
- they have thoughts of self-harm or suicide
- they think they might have BPD or another mental health condition
Suicide prevention
If you know someone at immediate risk of self-harm, suicide, or hurting another person:
- Ask the tough question: “Are you considering suicide?”
- Listen to the person without judgment.
- Call 911 or the local emergency number, or text TALK to 741741 to communicate with a trained crisis counselor.
- Stay with the person until professional help arrives.
- Try to remove any weapons, medications, or other potentially harmful objects.

If you or someone you know is having thoughts of suicide, a prevention hotline can help. The 988 Suicide and Crisis Lifeline is available 24 hours a day at 988. During a crisis, people who are hard of hearing can use their preferred relay service or dial 711 then 988.
Click here for more links and local resources.
Splitting can undermine relationships, make it difficult to resolve conflict, leave a person feeling overwhelmed and confused, and cause them to feel disappointed in their relationships. However, the right treatment can ease BPD symptoms, including splitting.
It is important for a person to question their assessments of others, consider whether other explanations might be just as accurate, and cultivate empathy for the behaviors of others. A psychotherapist can help a person manage or decrease splitting behaviors and determine whether or not BPD causes it.
Borderline personality disorder
Borderline personality disorder is associated with unstable mood and behavior that has a significant impact on a person's daily life
Borderline personality disorder is a type of personality disorder in which a person experiences periods of tension, unstable moods and behaviors, and an altered "feeling of self". 1 All of these can result in impulsive actions and relationship problems with friends and family members, impairing the person's ability to cope with everyday life. 1.2
1 All of these can result in impulsive actions and relationship problems with friends and family members, impairing the person's ability to cope with everyday life. 1.2
Borderline personality disorder is a serious illness associated with self-harm and suicidal attempts. One in ten patients complete suicide. 2
Facts About Borderline Personality Disorder
Borderline personality disorder is a type of personality disorder in which a person experiences periods of tension, unstable mood and behavior, and an altered sense of self. 1
One in ten patients complete suicide. 2
Patients with borderline personality disorder are very sensitive to changes in their environment, and may respond inappropriately and acutely to such changes. They may, for example, be afraid of being abandoned by a loved one. 2 If the person whom patient
2 If the person whom patient
is expecting arrives late, the patient easily changes the feeling of attachment to dislike or anger.1,2 This reflects the extreme perception of the world by the patient, who sees everything and everyone - including oneself – either good or bad.1,2
People with borderline personality disorder are often insecure, may suddenly change their life goals and views on career, life values and friends. .2 They may develop intense unwarranted anger or feelings of emptiness, and are prone to self-harm.2 Patients with borderline personality disorder may also experience depression and anxiety.1,2
Facts about Borderline Personality Disorder
Estimates of the proportion of people who have borderline personality disorder vary from less than 1% to around 6%. 2-4
Borderline personality disorder affects a roughly equal number of men and women, but appears to be more disabling in women the same frequency in men and women, but in women it is more severe.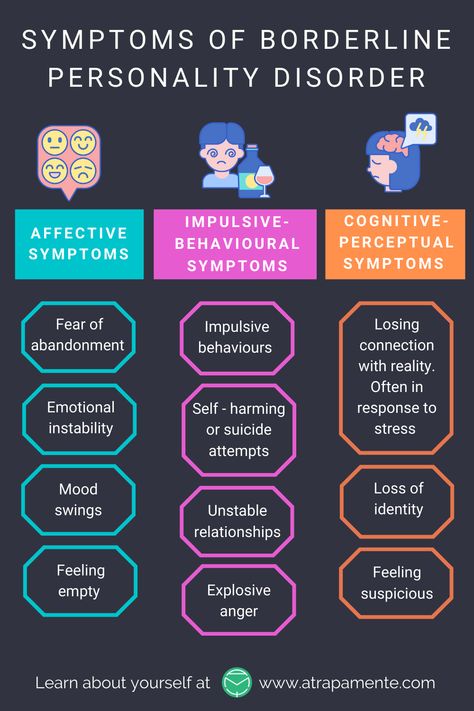 3
3
Symptoms of borderline personality disorder most often first appear during adolescence.4 The disease is most severe and problematic in young adults and tends to improve with age.2 Symptoms may persist throughout life, but most patients with borderline personality disorder by the age of 30-40 have a stable job and a home.2
People with borderline personality disorder are emotionally and functionally unstable, which places a significant burden on their families.5 Mood swings are a source of stress for both the patient and his/her others, which can lead to the development of mental disorders in the latter.1,5
People who are concerned that they – or their loved ones – are experiencing symptoms of borderline personality disorder should see their doctor for help and advice.
Borderline personality disorder is diagnosed by a mental health professional using interviews and discussions about symptoms and medical history. 1
1
Psychotherapy can help people with borderline personality disorder by, for example, teaching them how to interact with others and to express their thoughts and feelings more clearly. 1 It may also be beneficial for caregivers and family members of those affected to receive therapy and guidance on how best to care for a person with borderline personality disorder. 1 There is currently no cure, but one study showed that, after 10 years, 50% of people with borderline personality disorder had recovered, being able to function at work and maintain personal relationships. 6
- National Institute of Mental Health. borderline personality disorder. NIH publication number QF 17-4928. Available from: https://www.nimh.nih.gov/health/publications/borderline-personality-disorder/index.shtml [accessed 30 September 2019].
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders.
 5th ed. Arlington, VA: American Psychiatric Association; 2013.
5th ed. Arlington, VA: American Psychiatric Association; 2013. - Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533–545.
- National Institute for Health and Clinical Excellence. Borderline personality disorder: recognition and management. 2009. Available from: https://www.nice.org.uk/guidance/cg78/resources/borderline-personality-disorder-recognition-and-management-pdf-975635141317 [accessed 30 September 2019].
- Bailey RC, Grenyer BFS. Burden and support needs of carers of persons with borderline personality disorder: a systematic review. Harv Rev Psychiatry. 2013;21(5):248–258.
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. Time to attainment of recovery from borderline personality disorder and stability of recovery: a 10-year prospective follow-up study.
 Am J Psychiatry. 2010;167(6):663–667.
Am J Psychiatry. 2010;167(6):663–667.
1. National Institute of Mental Health. borderline personality disorder. NIH publication number QF 17-4928. Available from: https://www.nimh.nih.gov/health/publications/borderline-personality-disorder/index.shtml [accessed 30 September 2019].
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
3. Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533–545.
4. National Institute for Health and Clinical Excellence. Borderline personality disorder: recognition and management. 2009. Available from: https://www.nice.org.uk/guidance/cg78/resources/borderline-personality-disorder-recognition-and-management-pdf-975635141317 [accessed 30 September 2019].
Access to Brain Health
We are dedicated to improving access to brain health in accordance with WHO.
Our Science
Lundbeck has developed some of the world’s most widely prescribed therapies.
This is Lundbeck
A specialized pharmaceutical company focused exclusively on brain diseases.
Borderline personality disorder
Olga Vladimirovna Plotnikova
psychiatrist
Borderline personality disorder (hereinafter BPD) is characterized by increased anxiety, impulsive action. All these components greatly affect the quality of life. In addition, antisocial behavior, self-harm and an increased risk of suicide are common in borderline personality disorder.
Causes:
Genetics BPD has an evident hereditary factor.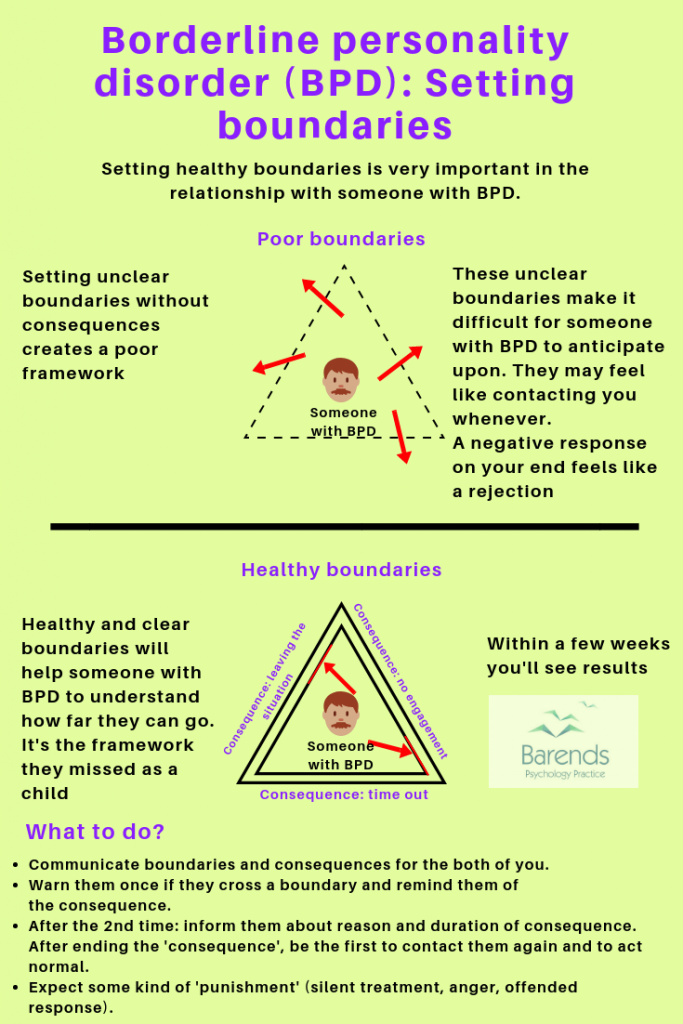 It would be more correct to say - predisposition. Like schizophrenia, BPD does not have a single gene that is responsible for the development of the disorder, but the influence of genetics is undeniable.
It would be more correct to say - predisposition. Like schizophrenia, BPD does not have a single gene that is responsible for the development of the disorder, but the influence of genetics is undeniable.
Neurophysiology or how does it work? Numerous neuroimaging studies (fMRI) have compared patients with BPD and healthy controls. Anomalies were found: a decrease in the level of serotonin, a decrease in the volume of the hippocampus, amygdala and other areas of the medial temporal lobe of the brain. The behavior of patients and their symptoms are a product of the special structure of their brain.
Environmental influences There are a lot of myths here. And, despite the appearance of neuroimaging data, for some reason they are still alive. The most common myth is the influence of childhood trauma on the occurrence of BPD. Indeed, studies of people with BPD show that they have a history of domestic violence, but again, not everyone is without exception. A case of childhood trauma can only provoke and awaken a hereditary predisposition to BPD, but this is not the cause of its development. It's all about the structure of the brain.
A case of childhood trauma can only provoke and awaken a hereditary predisposition to BPD, but this is not the cause of its development. It's all about the structure of the brain.
Why is this important? When we talk about diabetes, we don't think that willpower can change insulin levels. BPD is not a whim and cannot be cured by “education”, you need to learn to live with it.
Diagnostic criteria for borderline personality disorder:
- Tendency to make excessive efforts to avoid the real or imagined fate of being abandoned.
- Tendency to engage in intense, tense, and unstable relationships characterized by alternating extremes of idealization and devaluation.
- Identity disorder: marked and persistent instability of the image or feeling of the self.
- Impulsivity in at least two areas that involve self-harm (eg, spending money, substance abuse, traffic violations, habitual overeating).
- Recurrent suicidal behavior, hints or threats of suicide, acts of self-harm.
- Affective instability, very changeable mood (for example, periods of intense irritability or anxiety, usually lasting from several hours to several days).
- Constantly experienced feeling of emptiness.
- Inappropriate manifestations of intense anger or difficulty in controlling anger (eg, frequent irritability.
- Paranoid ideas.
How to treat?
The first line is the psycho-education of the patient and his relatives. This is very important, as it helps to understand what is happening with the patient and outline the tactics of further actions.
Schema therapy patients learn how to respond to their symptoms and then control them.
Medication helps to manage the severity of symptoms and gives strength to continue to fight BPD.
Special considerations to consider when choosing therapy
-Second generation antipsychotics should be used in patients with thought disorder, paranoia, identity disorder.