Complications of ect
Electroconvulsive therapy (ECT) - Mayo Clinic
Overview
Electroconvulsive therapy (ECT) is a procedure, done under general anesthesia, in which small electric currents are passed through the brain, intentionally triggering a brief seizure. ECT seems to cause changes in brain chemistry that can quickly reverse symptoms of certain mental health conditions.
ECT often works when other treatments are unsuccessful and when the full course of treatment is completed, but it may not work for everyone.
Much of the stigma attached to ECT is based on early treatments in which high doses of electricity were administered without anesthesia, leading to memory loss, fractured bones and other serious side effects.
ECT is much safer today. Although ECT may still cause some side effects, it now uses electric currents given in a controlled setting to achieve the most benefit with the fewest possible risks.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Electroconvulsive therapy (ECT) can provide rapid, significant improvements in severe symptoms of several mental health conditions. ECT is used to treat:
- Severe depression, particularly when accompanied by detachment from reality (psychosis), a desire to commit suicide or refusal to eat.
- Treatment-resistant depression, a severe depression that doesn't improve with medications or other treatments.
- Severe mania, a state of intense euphoria, agitation or hyperactivity that occurs as part of bipolar disorder. Other signs of mania include impaired decision-making, impulsive or risky behavior, substance abuse, and psychosis.
- Catatonia, characterized by lack of movement, fast or strange movements, lack of speech, and other symptoms. It's associated with schizophrenia and certain other psychiatric disorders. In some cases, catatonia is caused by a medical illness.
- Agitation and aggression in people with dementia, which can be difficult to treat and negatively affect quality of life.
ECT may be a good treatment option when medications aren't tolerated or other forms of therapy haven't worked. In some cases ECT is used:
- During pregnancy, when medications can't be taken because they might harm the developing fetus
- In older adults who can't tolerate drug side effects
- In people who prefer ECT treatments over taking medications
- When ECT has been successful in the past
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Risks
Although ECT is generally safe, risks and side effects may include:
- Confusion. Immediately after treatment, you may experience confusion, which can last from a few minutes to several hours. You may not know where you are or why you're there. Rarely, confusion may last several days or longer. Confusion is generally more noticeable in older adults.
- Memory loss. Some people have trouble remembering events that occurred right before treatment or in the weeks or months before treatment or, rarely, from previous years. This condition is called retrograde amnesia. You may also have trouble recalling events that occurred during the weeks of your treatment. For most people, these memory problems usually improve within a couple of months after treatment ends.
- Physical side effects. On the days of an ECT treatment, some people experience nausea, headache, jaw pain or muscle ache. These generally can be treated with medications.
- Medical complications. As with any type of medical procedure, especially one that involves anesthesia, there are risks of medical complications. During ECT, heart rate and blood pressure increase, and in rare cases, that can lead to serious heart problems. If you have heart problems, ECT may be more risky.
How you prepare
Before having your first ECT treatment, you'll need a full evaluation, which usually includes:
- Medical history
- Complete physical exam
- Psychiatric assessment
- Basic blood tests
- Electrocardiogram (ECG) to check your heart health
- Discussion of the risks of anesthesia
These exams help make sure that ECT is safe for you.
What you can expect
The ECT procedure takes about five to 10 minutes, with added time for preparation and recovery. ECT can be done while you're hospitalized or as an outpatient procedure.
Before the procedure
To get ready for the ECT procedure:
- You'll have general anesthesia. So you can expect dietary restrictions before the procedure. Typically, this means no food or water after midnight and only a sip of water to take any morning medications. Your health care team will give you specific instructions before your procedure.
- You may have a brief physical exam.This is basically to check your heart and lungs.
- You'll have an intravenous (IV) line inserted. Your nurse or other team member inserts an IV tube into your arm or hand through which medications or fluids can be given.
- You'll have electrode pads placed on your head. Each pad is about the size of a silver dollar.
 ECT can be unilateral, in which electric currents focus on only one side of the brain, or bilateral, in which both sides of the brain receive focused electric currents.
ECT can be unilateral, in which electric currents focus on only one side of the brain, or bilateral, in which both sides of the brain receive focused electric currents.
Anesthesia and medications
At the start of the procedure, you'll receive these medications through your IV:
- An anesthetic to make you unconscious and unaware of the procedure
- A muscle relaxant to help minimize the seizure and prevent injury
You may receive other medications, depending on any health conditions you have or your previous reactions to ECT.
Equipment
During the procedure:
- A blood pressure cuff placed around one ankle stops the muscle relaxant medication from entering your foot and affecting the muscles there. When the procedure begins, your doctor can monitor seizure activity by watching for movement in that foot.
- Monitors check your brain, heart, blood pressure and oxygen use.
- You may be given oxygen through an oxygen mask.
- You may also be given a mouth guard to help protect your teeth and tongue from injury.
Inducing a brief seizure
When you're asleep from the anesthetic and your muscles are relaxed, the doctor presses a button on the ECT machine. This causes a small amount of electric current to pass through the electrodes to your brain, producing a seizure that usually lasts less than 60 seconds.
- Because of the anesthetic and muscle relaxant, you remain relaxed and unaware of the seizure. The only outward indication that you're having a seizure may be a rhythmic movement of your foot if there's a blood pressure cuff around your ankle.
- Internally, activity in your brain increases dramatically. A test called an electroencephalogram (EEG) records the electrical activity in your brain. Sudden, increased activity on the EEG signals the beginning of a seizure, followed by a leveling off that shows the seizure is over.
A few minutes later, the effects of the short-acting anesthetic and muscle relaxant begin to wear off. You're taken to a recovery area, where you're monitored for any potential problems. When you wake up, you may experience a period of confusion lasting from a few minutes to a few hours or more.
You're taken to a recovery area, where you're monitored for any potential problems. When you wake up, you may experience a period of confusion lasting from a few minutes to a few hours or more.
Series of treatments
In the United States, ECT treatments are generally given two to three times weekly for three to four weeks — for a total of six to 12 treatments. Some doctors use a newer technique called right unilateral ultrabrief pulse electroconvulsive therapy that's done daily on weekdays.
The number and type of treatments you'll need depend on the severity of your symptoms and how rapidly they improve.
You can generally return to normal activities a few hours after the procedure. However, some people may be advised not to return to work, make important decisions, or drive until one to two weeks after the last ECT in a series, or for at least 24 hours after a single treatment during maintenance therapy. Resuming activities depends on when memory loss and confusion are resolved.
Results
Many people begin to notice an improvement in their symptoms after about six treatments with electroconvulsive therapy. Full improvement may take longer, though ECT may not work for everyone. Response to antidepressant medications, in comparison, can take several weeks or more.
No one knows for certain how ECT helps treat severe depression and other mental illnesses. What is known, though, is that many chemical aspects of brain function are changed during and after seizure activity. These chemical changes may build upon one another, somehow reducing symptoms of severe depression or other mental illnesses. That's why ECT is most effective in people who receive a full course of multiple treatments.
Even after your symptoms improve, you'll still need ongoing depression treatment to prevent a recurrence. Ongoing treatment may be ECT with less frequency, but more often, it includes antidepressants or other medications, or psychological counseling (psychotherapy).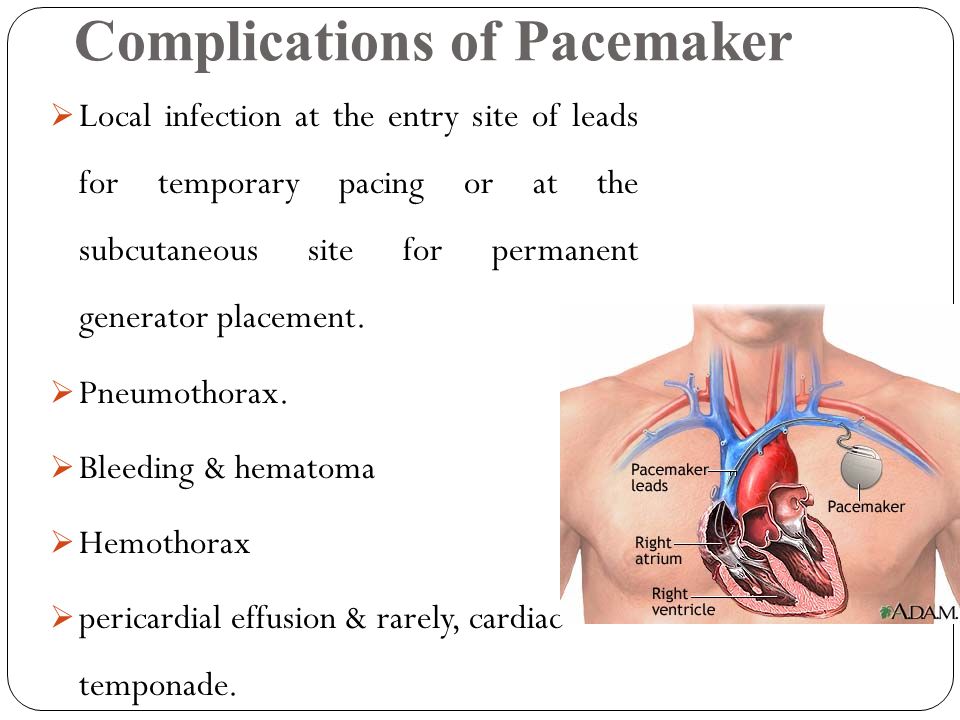
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
By Mayo Clinic Staff
Related
Products & Services
What It Is & Side Effects
Overview
What is electroconvulsive therapy (ECT)?
Electroconvulsive therapy (ECT) is a medical procedure that involves passing a mild electric current through your brain, causing a short seizure. This procedure is proven to have strong positive effects on severe, treatment-resistant mental health conditions. ECT’s history stretches back more than 80 years, and extensive research shows it’s an effective, safe technique. This treatment involves anesthesia so that you won't feel pain during the procedure.
ECT often has a negative connotation because of how it's been shown in movies, television shows and other media. These portrayals of ECT are usually inaccurate about how this procedure happens, whether or not it's painful or frightening and whether or not it's effective. These portrayals are not true-to-life, and they don’t show how healthcare providers do this procedure safely and humanely.
These portrayals are not true-to-life, and they don’t show how healthcare providers do this procedure safely and humanely.
Who needs to have this treatment?
ECT can treat people with severe mental health conditions and is an option for a wide range of ages. This procedure can help children (some states have specific restrictions), teenagers, and adults of all ages. The strongest benefits from ECT tend to happen in people over 60.
Why is ECT used?
The most common reasons for ECT are severe mental health conditions under the following circumstances:
- When medications aren’t working.
- When the person experiences an extreme shut down of function, called catatonia.
- In situations where a person is a danger to themselves or others, and medications will take days or weeks to become effective.
What conditions are treated with ECT?
ECT is a possible treatment for several conditions, including the following:
- Depression (especially in people who are over the age of 60).
- Schizophrenia (including other schizophrenia-spectrum conditions and psychotic disorders).
- Bipolar disorder and other conditions that involve mania.
How common is ECT?
Although it's effective and safe, ECT is not a common procedure. That’s likely the case for several reasons, a few of which include:
- ECT is rarely a first-line treatment for depression.
- There are several newer medications available to treat this condition.
- Fewer hospitals offer ECT (which affects people receiving inpatient and outpatient care).
Procedure Details
What happens before this procedure?
Before you start ECT, your healthcare provider will explain to you (or to someone who can make healthcare decisions for you) what ECT is and how it works. They’ll also make sure you don’t have any underlying health conditions or reasons that might mean you shouldn’t receive ECT.
Several tests are possible leading up to ECT, including (but not limited to) the following:
- Blood and urine tests.
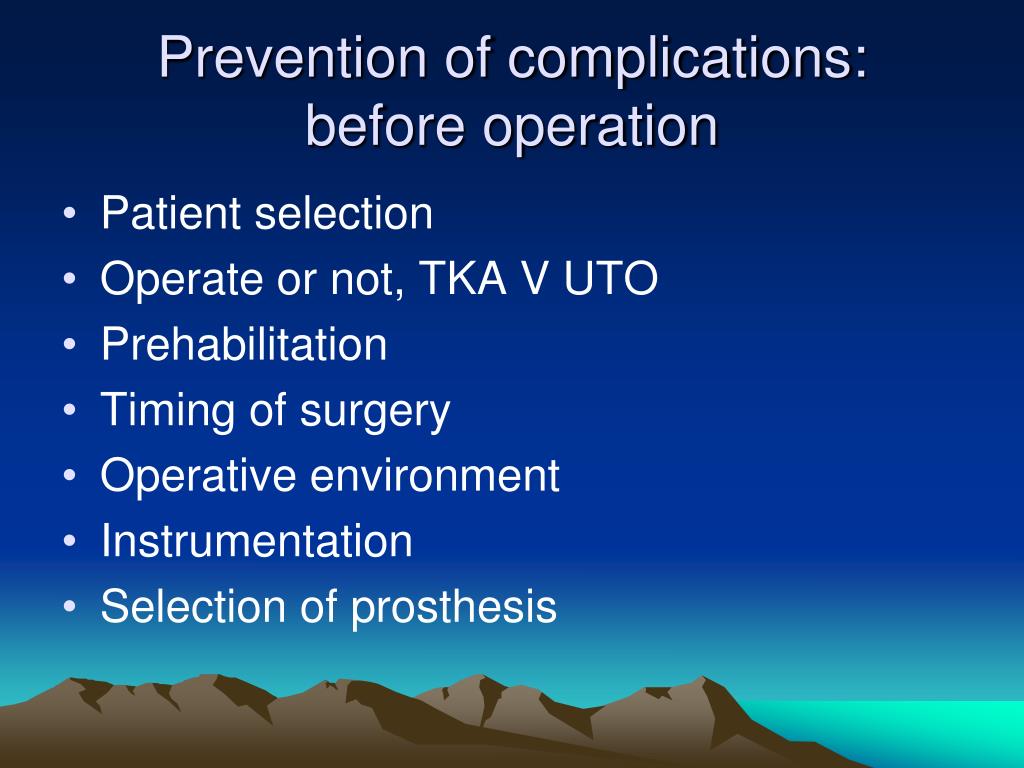 Some examples include complete blood count, a metabolic panel (basic or comprehensive), thyroid function, kidney function and more.
Some examples include complete blood count, a metabolic panel (basic or comprehensive), thyroid function, kidney function and more. - Imaging tests on your skull, brain and spine. These may include X-rays and computerized tomography (CT) scans.
- Electrocardiogram (ECG or EKG). This test looks at your heart function and can spot any unusual changes or problems with your heart’s electrical system.
Reasons why you shouldn’t receive ECT
There are some conditions and reasons why you shouldn’t receive ECT. Known as “contraindications,” these are all considered on a case-by-case basis. Even if you have a contraindication, providers can often adjust the treatment procedure to take these into account so you can still receive ECT. Contraindications include:
- A recent heart attack (myocardial infarction) or other unstable heart condition.
- Conditions that increase the pressure inside your skull (such as intracranial hypertension or brain tumors).
- A recent stroke, aneurysm or other cause of bleeding in your brain.
- Severe lung diseases like chronic obstructive pulmonary disease (COPD).
- Certain other life-threatening conditions or people who meet the level 4 or 5 requirements on the American Society of Anesthesiologists physical classification system.
Stoppage of food and liquids
Because general anesthesia is a part of ECT, your healthcare provider will have you fast before this procedure. That means stopping food eight hours before the procedure and stopping liquids two hours before.
What you should take off or remove
A healthcare provider may tell you to remove jewelry, medical devices, accessories or prosthetics before having this procedure. Common examples include taking off or removing your glasses, contact lenses, hearing aids, dentures or dental plates, etc. This helps avoid any risks of injury or choking because of these items.
Medication stoppage
Certain medications can affect how ECT affects you, including how effective this treatment is. Your healthcare provider may ask you to stop certain medications or reduce your dosage. However, you should only stop or change medications as directed by your provider.
Your healthcare provider may ask you to stop certain medications or reduce your dosage. However, you should only stop or change medications as directed by your provider.
What happens during this procedure?
ECT involves multiple healthcare providers, including a psychiatrist, anesthesiology specialist and other trained personnel.
Anesthesia and other preparations
ECT procedures start with general anesthesia, which puts you into a deep sleep and keeps you from feeling any pain, discomfort or anxiety during the procedure. Providers will also give you a muscle relaxant to avoid any injuries or strain that might happen during the seizure.
Providers will also insert a bite guard into your mouth to protect your teeth, and also insert an intravenous (IV) needle into one of your veins (usually one in your arm). The IV allows quick injection access for medications for anesthesia reasons or to counteract any side effects.
Electrode placement
A healthcare provider will then place electrodes, which are contact points for the electric current to travel through, against the skin of your head. The placement depends on your specific needs, and providers will choose a placement with the lowest chance of causing side effects. There are three different ways that providers can place the electrodes.
The placement depends on your specific needs, and providers will choose a placement with the lowest chance of causing side effects. There are three different ways that providers can place the electrodes.
- Right unilateral: This placement has both electrodes on the right side of your head. One electrode will be between your temple and the end of your eyebrow. The other electrode will be near the top of your head, directly above your right ear.
- Bifrontal: Electrodes placed using this configuration are on opposite sides of your forehead, just above the end of your eyebrow.
- Bitemporal: This placement involves one electrode aligned with the temple area on each side of your head.
A healthcare provider will coat the electrodes in a conductive gel that should prevent irritation and burns to your skin. While the electrical current involved is very low, skin irritation and burns are still possible.
Electricity requirements
ECT involves a very small electrical current, up to about 0. 4 amps. For comparison, a 9-volt alkaline battery can deliver about 0.6 amps of current for one hour before the battery is empty. Providers will also start the current at low levels and increase it until it has the desired effect.
4 amps. For comparison, a 9-volt alkaline battery can deliver about 0.6 amps of current for one hour before the battery is empty. Providers will also start the current at low levels and increase it until it has the desired effect.
The electrical current duration for ECT is also very brief. For most treatments, delivery of electrical current to your brain only lasts a few seconds.
Induced seizure
ECT uses an electrical current to cause a seizure, which is when a burst of electrical activity happens in your brain and causes affected brain cells to fire rapidly. This causes electrical and chemical changes in the way that area of your brain works, leading to improvements in how those areas of the brain work.
Seizures from ECT typically last between 30 and 90 seconds. In cases where they last longer, healthcare providers can stop the seizure using injectable medications.
What happens after this procedure?
After the seizure stops, healthcare providers will monitor you as you awaken from anesthesia. They'll also check your vital signs to look for any signs of side effects or other anesthesia-related problems that might happen.
They'll also check your vital signs to look for any signs of side effects or other anesthesia-related problems that might happen.
Most people are fully conscious within 10 to 15 minutes after this procedure and can be on their feet and walk around within 30 minutes.
Risks / Benefits
What are the advantages of ECT?
ECT has many advantages that make it a critical tool for treating mental health conditions.
- It is extremely effective. Experts agree that ECT is one of the most effective treatments for mood disorders like depression. It is also especially effective at helping people with depression that resist other forms of treatment like medication or therapy.
- It is very safe. The use of anesthesia and other modern care practices have greatly improved this procedure's overall safety. Even people who have heart problems can often receive ECT with adjustments to their medication or close monitoring of their vital signs.
- It is very safe in pregnancy.
- It works quickly. People who receive ECT typically see improvements in their symptoms, especially with conditions like major depressive disorder, after three to five treatments. That’s especially helpful when a person has a very severe mental health condition that puts their safety in jeopardy.
- It can help people when other treatments are unavailable. People who can’t take medications for mental health conditions for any reason can often still receive ECT. This can make a big difference for people with organ function problems or people who are pregnant (ECT is safe during all three trimesters of pregnancy).
- It’s especially effective in combination with medication. People receiving ECT often also receive medications for treatment, which can further improve the chances that their mental health condition will improve.
What are the disadvantages, risks or possible complications of this procedure?
Though it is extremely effective, ECT does have some disadvantages.
- There’s a risk of memory loss. Most people who undergo ECT have temporary memory loss and confusion. Most people's confusion clears up quickly, and memory loss usually goes away entirely within a few months. However, some people do have permanent memory problems. Using the right-unilateral electrode placement and shortening the electrical current duration can reduce the risk of this happening.
- It’s a medically intensive procedure. Each ECT procedure requires multiple providers with advanced training to be present. That means this treatment is often not available in smaller healthcare facilities and communities.
- This procedure might only have short-term effects. Some people who receive ECT need follow-up treatments. These “maintenance” procedures may need to happen for weeks or months. Usually, these follow-up treatments can happen once a week or even once every several months. The use of medication along with ECT can help with this.
Recovery and Outlook
What is the recovery time?
Most people who receive ECT recover quickly from the procedure. Most wake up within 15 minutes and can be on their feet within 30 minutes.
The overall course of treatment with ECT involves multiple treatments. These can happen multiple times per week for several weeks. Usually, people receive three ECT treatments per week.
When to Call the Doctor
When should I see my healthcare provider?
Your healthcare provider can tell you more about the potential signs and symptoms to watch for that mean you need medical attention in the near future or immediately. If you notice the following, you should call your healthcare provider or go to the nearest emergency room:
- Severe headache.
- Fast heartbeat (tachycardia) or irregular heartbeat (arrhythmia).
- If you don’t feel better within two to three days, or if you feel worse.
- If you are worried about your mood or mental state.
When should I get emergency medical care?
You should get emergency care if you have disturbing thoughts about harming yourself, including thoughts of suicide or about harming others. If you have thoughts like this, you can call any of the following:
- National Suicide Prevention Lifeline (United States). To call this line, dial 1-800-273-TALK (1-800-273-8255).
- Local crisis lines. Mental health organizations and centers in your area may offer resources and help through crisis lines.
- Dial 911 (or your local emergency services number): You should call 911 (or the local emergency services number) if you feel like you’re in immediate danger of harming yourself. Operators and dispatchers for 911 lines can often help people in immediate danger because of a severe mental crisis and send first responders to assist.
Frequently Asked Questions
Is ECT painful?
No, the ECT procedure isn’t painful. ECT involves general anesthesia, which means you’re asleep while the procedure is happening. After the procedure, you may have some side effects, such as headache, nausea or sore muscles, but these are all normal. If you're worried about these, you can talk to your healthcare provider and ask them for guidance on what you can do to minimize these effects.
ECT involves general anesthesia, which means you’re asleep while the procedure is happening. After the procedure, you may have some side effects, such as headache, nausea or sore muscles, but these are all normal. If you're worried about these, you can talk to your healthcare provider and ask them for guidance on what you can do to minimize these effects.
Is ECT safe?
Yes, advances in modern medicine and ECT procedures make this treatment very safe. If you have healthcare conditions or concerns and you're worried about if these will be a problem, you can talk to your healthcare provider about these. Your provider can take other health conditions or circumstances into account, adjusting this procedure accordingly. They might also offer alternative options better suited for your needs.
Does ECT cause brain damage or memory loss?
Researchers and experts have looked at ECT using many different tools, imaging technologies and diagnostic tests. The available research shows that permanent negative effects from ECT like memory loss are rare. Memory loss does happen in some cases, but it’s usually temporary and goes away within a few months. Researchers also found that ECT stimulates certain types of brain function, which improves the symptoms that happen with many mental health conditions.
Memory loss does happen in some cases, but it’s usually temporary and goes away within a few months. Researchers also found that ECT stimulates certain types of brain function, which improves the symptoms that happen with many mental health conditions.
Does ECT work?
The available research shows that ECT is extremely effective, more so than any other available treatment for depression. No one entirely understands how ECT works for depression, but there are many theories. ECT may cause changes in brain chemistry or repair changes to the brain caused by severe, chronic depression.
A note from Cleveland Clinic
Electroconvulsive therapy is a procedure that can help people with severe mental health conditions. It's especially useful in cases where other treatments aren't an option or haven't worked. While this procedure often provokes a negative reaction because of portrayals in movies and television shows, this procedure is safe and effective. Healthcare providers will also go through several steps to make sure you are comfortable during this procedure and have minimal side effects. ECT can make a huge difference in relieving severe symptoms for many people, and it's often a life-saving procedure.
ECT can make a huge difference in relieving severe symptoms for many people, and it's often a life-saving procedure.
Electroconvulsive therapy (ECT) - procedure, indications, results
Electroconvulsive Therapy (alternatively called ECT, Electroconvulsive Therapy, ECT) is a medical procedure performed under general anesthesia in which small electrical currents are passed through the brain to deliberately induce a brief epileptic seizure.
Contents
Such manipulation seems to cause changes in brain chemistry and help to quickly reverse the symptoms of certain mental illnesses, for example:
- schizophrenia
- severe depression
- psychosis and thoughts of suicide
- bipolar disorder
- heavy mania
- A state of intense euphoria, arousal or hyperactivity that occurs as part of a bipolar disorder
- substance abuse
- catatonia characterized by lack of movement, rapid or strange movements, lack of speech
- aggression in people with dementia.

Indications for electroconvulsive therapy
ECT may be a good treatment option when medications are not tolerated or other forms of therapy do not work. In some cases it is used:
- during pregnancy, when drugs should not be taken because they may harm the fetus
- in the elderly who cannot tolerate the side effects of psychotropic drugs. nine0012
Consequences
Much of the stigma associated with electroshock therapy is based on early treatments in which high doses of electricity were administered without anesthesia, resulting in memory loss, broken bones, and other serious side effects. Modern electroconvulsive therapy is much safer. While ECT may still cause some side effects, it now uses electrical currents in a controlled environment to achieve the maximum benefit with the fewest possible risks. nine0005
Complications after treatment with electroconvulsive therapy may include:
- Confusion of consciousness.
 Immediately after treatment, you may experience confusion, which can last from a few minutes to several hours. Perhaps you don't know where you are. Rarely in older people, the confusion can last for several days.
Immediately after treatment, you may experience confusion, which can last from a few minutes to several hours. Perhaps you don't know where you are. Rarely in older people, the confusion can last for several days. - Memory loss. Some people have difficulty remembering events that happened just before treatment or weeks or months before treatment. This condition is called retrograde amnesia. You may also have trouble remembering events that happened in the weeks before your treatment. For most people, these memory problems usually improve within a few months of ending therapy. nine0012
- Physical side effects. On the days of ECT treatment, some people experience nausea, headache, jaw pain, or muscle pain.
- Medical complications. As with any type of medical procedure, especially anesthesia, there is a risk of medical complications. During ECT, heart rate and blood pressure increase, and in rare cases, this can lead to serious heart problems.
Electroconvulsive therapy
Preparation
Before the first electroconvulsive therapy treatment, you will need to undergo a comprehensive examination:
- Psychiatric assessment
- Basic blood tests
- X-ray of lungs
- Electrocardiogram
- Cardiac ultrasound
- MRI of the brain.

To prepare for electroconvulsive therapy, dietary restrictions should be followed prior to the procedure. This usually means no food or water for 12 hours before therapy. nine0005
Electroshock Therapy Procedure
The ECT procedure takes 5 to 10 minutes, with additional preparation and recovery time. It can be performed during hospitalization or as an outpatient procedure. At the beginning of therapy, the patient will be given anesthesia through an intravenous drip and a muscle relaxant to help minimize the seizure and prevent injury.
- The doctor then installs a series of sensors: nine0011 A blood pressure cuff around one ankle stops muscle relaxant from getting into the leg and affecting the muscles. Once the procedure begins, the doctor can monitor seizure activity by watching movement in the foot.
- Special sensors check the state of the brain, heart, blood pressure and oxygen supply to the lungs.
- A mouth guard will help protect your teeth and tongue from injury.
The next step is to put the patient to sleep. When he is asleep and his muscles are relaxed, the doctor presses a button on the ECT machine. This causes a small amount of electrical current to pass through the electrodes to the brain, causing an epileptic seizure that usually lasts less than 60 seconds. The only outward sign that a patient is having a mini-convulsive seizure may be the rhythmic movement of the foot. As a result of an electric shock, activity in the brain increases dramatically. This is recorded by an electroencephalogram. Sudden increased EEG activity signals the onset of seizures, followed by stabilization of brain activity. nine0005
Electroconvulsive therapy treatment is usually given 2-3 times a week for 3-4 weeks, and the course takes a total of 6 to 12 treatments. Some doctors use a newer form of therapy called one-sided ultra-rapid shock therapy, which is usually given daily, 5 days a week.
Typically, the patient can return to normal activities within a few hours after the procedure. However, some people may be advised not to return to work or make legal decisions for 1-3 weeks after their last ECT. nine0005
However, some people may be advised not to return to work or make legal decisions for 1-3 weeks after their last ECT. nine0005
Results
Scientists don't yet know exactly how ECT helps treat severe depression and other mental illnesses. However, many chemical aspects of brain function are known to change during and after seizures. These chemical changes may build on each other to reduce symptoms in some way. Many patients begin to notice an improvement in their symptoms after about 6 sessions of electroconvulsive therapy. Even after the symptoms improve, the patient will still need ongoing treatment to prevent the condition from recurring. Supportive care may include ECT less frequently, but most often includes antidepressants, psychotropic medications, or psychological counseling. nine0005
Share:
References:
- Banshchikov V.N., Rapoport A.M. "Electroconvulsive therapy in psychoneurological hospitals of the USSR" // Journal of Neurology and Psychiatry named after S.
 S. Korsakov. 1952. - V.52. - No. 3. - p. 67-81.
S. Korsakov. 1952. - V.52. - No. 3. - p. 67-81. - Ventsovsky E.I. "Electroconvulsive therapy" // In the book. "Manual of Psychiatry. T.2. Ed. G.V. Morozov. Moscow, 1988. - p. 535-542.
- Grechko V.E., Puzin M.N., Avrutsky G.Ya. and others. "Electroconvulsive therapy in the treatment of patients with trigeminal neuralgia" // Journal of Neurology and Psychiatry. S.S.Korsakov. 1990. - T.90. - No. 2. - With. 109-114.
- Ilyina V.N. "Clinical and experimental data for the development of methods of facilitated electroconvulsive therapy" // Abstract of the thesis. diss.cand.med. Sciences. Yaroslavl, 1953. - 14 p.
- Komissarov A.G. "The effectiveness of electroconvulsive therapy in a patient with involutional psychosis" // Psychiatry. - 2003a. - T.4. No. 4. - p.69-71.
FGBNU NTsPZ. ‹‹General Psychiatry››
Feedback form
Question about the work of the siteQuestion to a specialistQuestion to the administration of the clinic
email address
Name
Message text
ELECTROSCONSCULAR THERAPY
Currently, ECT is practically the only widely used form of shock therapy. The mechanism of action of ECT is not fully known. It is assumed that electric shock causes an increase in the release of catecholamines: norepinephrine - in the frontal cortex, basal ganglia and hippocampus; dopamine - in the striatum, and also changes the sensitivity and increases the number of receptors for these neurotransmitters. nine0005
The mechanism of action of ECT is not fully known. It is assumed that electric shock causes an increase in the release of catecholamines: norepinephrine - in the frontal cortex, basal ganglia and hippocampus; dopamine - in the striatum, and also changes the sensitivity and increases the number of receptors for these neurotransmitters. nine0005
The main indication for the appointment of ECT is endogenous depression, resistant to antidepressant therapy. Patients with these conditions make up approximately 70% of the total number of patients who are prescribed this type of therapy. Positive results have been obtained with the use of ECT in patients with severe manic disorders. In schizophrenia, ECT is indicated when positive symptoms predominate, especially in cases where depression is detected in the clinical picture. Predictors of a good therapeutic response to ECT in schizophrenia, in addition to the presence of signs of depression, can be a short duration of the disease, the absence of premorbid features of schizoidness or paranoia. nine0005
nine0005
ECT is considered one of the most effective treatments for febrile catatonia, in which it is sometimes the only life-saving therapy. In rare cases, ECT is used to treat treatment-resistant obsessive-compulsive and anxiety-phobic disorders, as well as severe delirious conditions.
The dosage unit of ECT is the minimum seizure dose (the minimum voltage and exposure to electrical current at which a seizure is possible). The minimum convulsive dose is selected individually for each patient. Too low a convulsive dose causes a decrease in therapeutic effect, too high causes side effects, especially in the cognitive sphere. Before starting ECT, it is recommended to determine the patient's seizure threshold, which allows more accurate determination of the therapeutic seizure dose. In men, the threshold for convulsive readiness is higher than in women, so the minimum convulsive dose is also higher on average. The standard ECT technique uses alternating or direct current (voltage from 60 to 130 V for 0. 3–0.9With). The course of treatment usually includes 6 to 15 seizures.
3–0.9With). The course of treatment usually includes 6 to 15 seizures.
Apply bilateral and unilateral ECT technique. It is assumed that the effectiveness of both methods is approximately the same. Some researchers believe that the unilateral technique is somewhat safer, but this point of view has not received wide confirmation. Currently, ECT is carried out against the background of the use of muscle relaxants and intravenous anesthesia. This avoids complications such as fractures, dislocations, torn ligaments and muscles, as well as pain after the session. nine0005
ECT can lead to cognitive impairment, in particular to memory disorders. In some cases, the prevention of this kind of side effects is carried out by prescribing nootropics. Computed tomography studies have shown that ECT does not cause cortical atrophy, enlargement of the cerebral ventricles, or changes in the brain parenchyma.
ECT for the above conditions can lead to remission relatively quickly, but it is not always stable.