Cns depressant effect
Prescription CNS Depressants DrugFacts | National Institute on Drug Abuse (NIDA)
DrugFacts
What are prescription CNS depressants?
Image
Photo by ©iStock.com
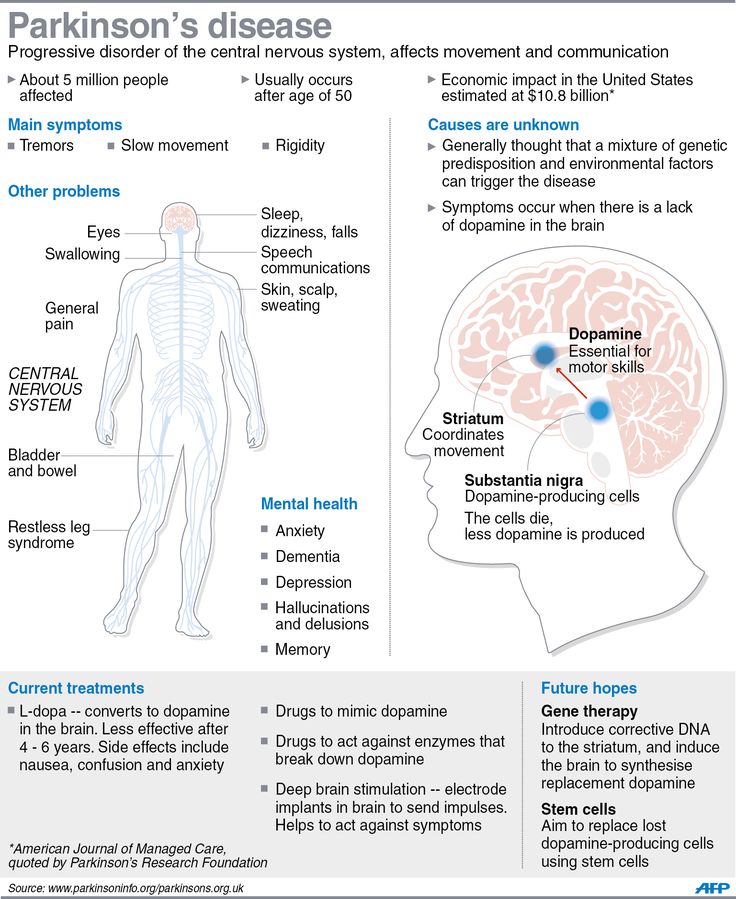
Central Nervous System (CNS) depressants are medicines that include sedatives, tranquilizers, and hypnotics. These drugs can slow brain activity, making them useful for treating anxiety, panic, acute stress reactions, and sleep disorders.
CNS depressants cause drowsiness; sedatives are often prescribed to treat sleep disorders like insomnia and hypnotics can induce sleep, whereas tranquilizers are prescribed to treat anxiety or to relieve muscle spasms.
Some examples of CNS depressants grouped by their respective drug class are:
| Benzodiazepines |
|---|
|
| Non-Benzodiazepine Sedative Hypnotics |
|
| Barbiturates |
|
How do people use and misuse prescription CNS depressants?
Most prescription CNS depressants come in pill, capsule, or liquid form, which a person takes by mouth. Misuse of prescription CNS depressants means:
- taking medicine in a way or dose other than prescribed
- taking someone else's medicine
- taking medicine for the effect it causes — to get high
When misusing a prescription CNS depressant, a person can swallow the medicine in its normal form or can crush pills or open capsules.
How do CNS depressants affect the brain?
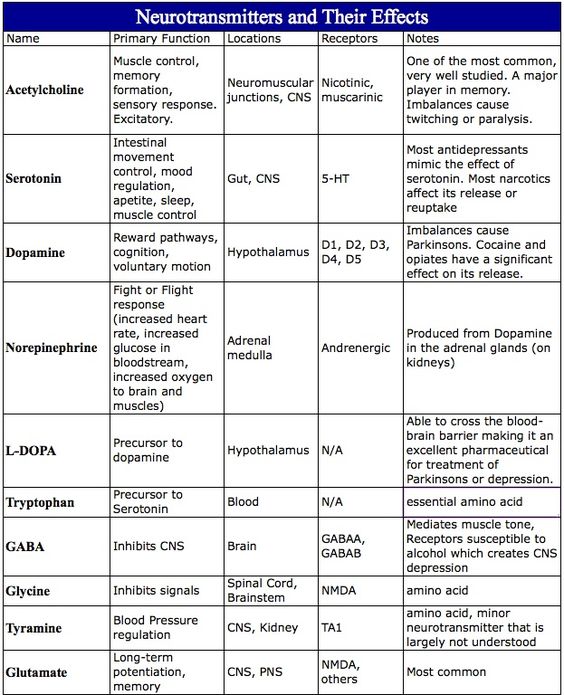
Most CNS depressants act on the brain by increasing activity of gamma-aminobutyric acid (GABA), a chemical that inhibits brain activity. This action causes the drowsy and calming effects that make the medicine effective for anxiety and sleep disorders. People who start taking CNS depressants usually feel sleepy and uncoordinated for the first few days until the body adjusts to these side effects. Other effects from use and misuse can include:
- slurred speech
- poor concentration
- confusion
- headache
- light-headedness
- dizziness
- dry mouth
- problems with movement and memory
- lowered blood pressure
- slowed breathing
If a person takes CNS depressants long term, he or she might need larger doses to achieve therapeutic effects.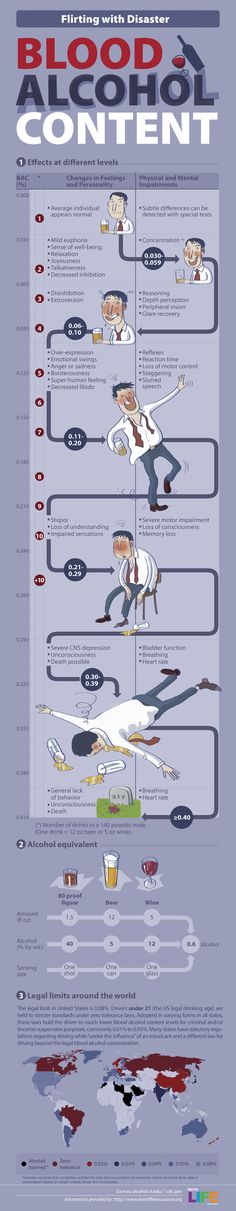 Continued use can also lead to dependence and withdrawal when use is abruptly reduced or stopped. Suddenly stopping can also lead to harmful consequences like seizures.
Continued use can also lead to dependence and withdrawal when use is abruptly reduced or stopped. Suddenly stopping can also lead to harmful consequences like seizures.
Can a person overdose on CNS depressants?
Yes, a person can overdose on CNS depressants. An overdose occurs when the person uses enough of a drug to produce life-threatening symptoms or death (read more on our Intentional vs. Unintentional Overdose Deaths webpage).
When people overdose on a CNS depressant, their breathing often slows or stops. This can decrease the amount of oxygen that reaches the brain, a condition called hypoxia. Hypoxia can have short- and long-term mental effects and effects on the nervous system, including coma and permanent brain damage.
How can a CNS depressant overdose be treated?
The most important step to take is to call 911 so a person who has overdosed can receive immediate medical attention. Flumazenil (Romazicon®) is a medication that medical personnel can use to treat benzodiazepine overdose and has also been shown effective in treating overdose from sleep medicines. The drug might not completely reverse slowed breathing and can lead to seizures in some patients who are taking certain antidepressants. Flumazenil is short acting, and the patient may need more of it every 20 minutes until he or she recovers. For barbiturates and nonbenzodiazepines, body temperature, pulse, breathing, and blood pressure should be monitored while waiting for the drug to be eliminated.
The drug might not completely reverse slowed breathing and can lead to seizures in some patients who are taking certain antidepressants. Flumazenil is short acting, and the patient may need more of it every 20 minutes until he or she recovers. For barbiturates and nonbenzodiazepines, body temperature, pulse, breathing, and blood pressure should be monitored while waiting for the drug to be eliminated.
Can prescription CNS depressant use lead to addiction and substance use disorder?
Yes, use or misuse of prescription CNS depressants can lead to problem use, known as a substance use disorder (SUD), which takes the form of addiction in severe cases. Long-term use of prescription CNS depressants, even as prescribed by a doctor, can cause some people to develop a tolerance, which means that they need higher and/or more frequent doses of the drug to get the desired effects. A SUD develops when continued use of the drug leads to negative consequences such as health problems or failure to meet responsibilities at work, school, or home, but despite all that the drug use continues.
Those who have become addicted to a prescription CNS depressant and stop using the drug abruptly may experience a withdrawal. Withdrawal symptoms-which can begin as early as a few hours after the drug was last taken—include:
- seizures
- shakiness
- anxiety
- agitation
- insomnia
- overactive reflexes
- increased heart rate, blood pressure, and temperature with sweating
- hallucinations
- severe cravings
People addicted to prescription CNS depressants should not attempt to stop taking them on their own. Withdrawal symptoms from these drugs can be severe and—in the case of certain medications-potentially life—threatening.
How can people get treatment for prescription CNS depressant addiction?
Image
Photo by © NIDA
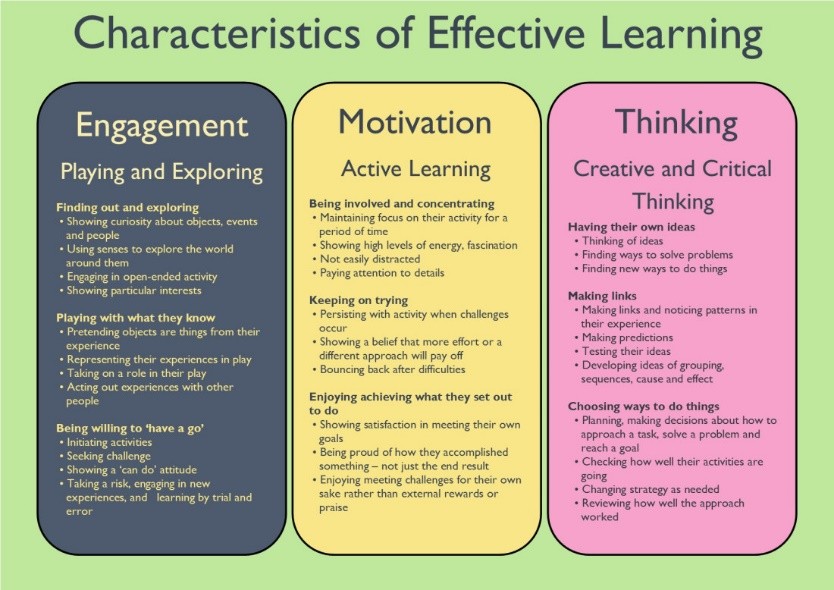
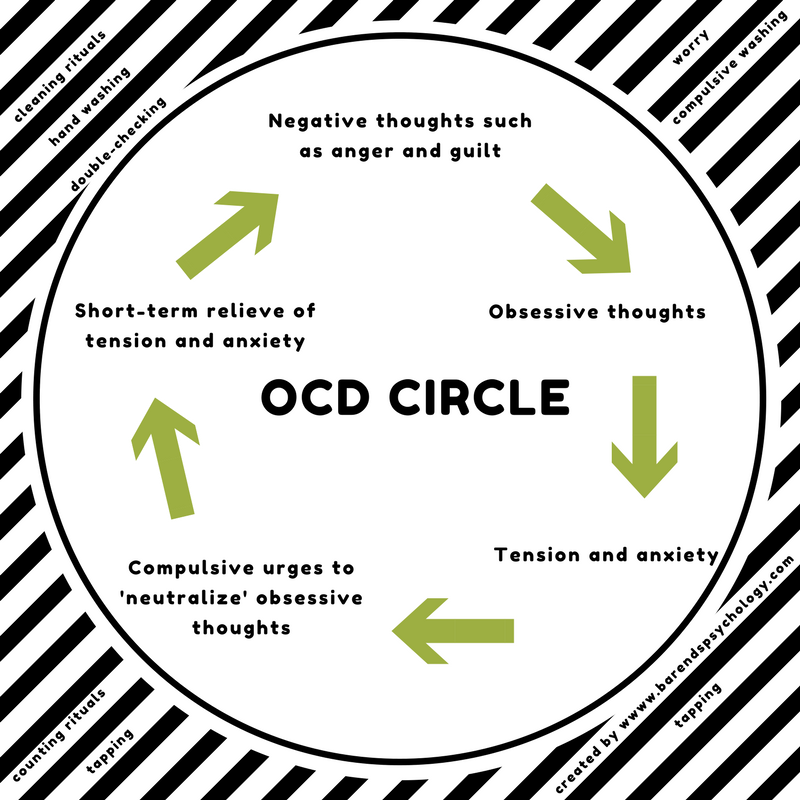
There isn't a lot of research on treating people for addiction to prescription CNS depressants. However, people addicted to these medications should undergo medically supervised detoxification because the dosage they take should be tapered gradually. Counseling, either in an outpatient or inpatient program, can help people through this process. One type of counseling, cognitive-behavioral therapy, focuses on modifying the person's thinking, expectations, and behaviors while improving ways to cope with life's stresses. Cognitive-behavioral therapy has helped people successfully adapt to stop using benzodiazepines.
Counseling, either in an outpatient or inpatient program, can help people through this process. One type of counseling, cognitive-behavioral therapy, focuses on modifying the person's thinking, expectations, and behaviors while improving ways to cope with life's stresses. Cognitive-behavioral therapy has helped people successfully adapt to stop using benzodiazepines.
Often prescription CNS depressant misuse occurs along with the use of other drugs, such as alcohol or opioids. In those cases, the person should seek treatment that addresses the multiple addictions.
Points to Remember
- Prescription CNS depressants are medicines that can slow brain activity to treat anxiety and sleep disorders.
- Prescription CNS depressants act on the brain by increasing activity of GABA, a chemical that slows brain activity.
- People who start taking prescription CNS depressants usually feel sleepy and uncoordinated at first. They can also have poor concentration, confusion, lowered blood pressure, and slowed breathing.
- A person can overdose on prescription CNS depressants. Flumazenil (Romazicon®) can be used to treat benzodiazepine and sleep medicine overdoses. Body temperature, pulse, breathing, and blood pressure should be monitored while waiting for the drug to be eliminated.
- Prescription CNS depressant use or misuse can lead to a substance use disorder, which takes the form of addiction in severe cases, even when used as prescribed by a doctor.
- Withdrawal symptoms include: seizures; shakiness; anxiety; agitation; insomnia; overactive reflexes; increased heart rate, blood pressure, and temperature; hallucinations; and severe cravings.
Learn More
For more information about prescription CNS depressants, see our:
- Commonly Used Drugs chart
- Misuse of Prescription Drugs Research Report
This publication is available for your use and may be reproduced in its entirety without permission from NIDA. Citation of the source is appreciated, using the following language: Source: National Institute on Drug Abuse; National Institutes of Health; U.S. Department of Health and Human Services.
Citation of the source is appreciated, using the following language: Source: National Institute on Drug Abuse; National Institutes of Health; U.S. Department of Health and Human Services.
Central Nervous System Depressants - Addiction Center
Central nervous system (CNS) depressants are drugs that slow down brain activity, making them effective for treating many conditions. These drugs operate by affecting the neurotransmitter gamma-aminobutyric acid (GABA), which leads to side effects such as drowsiness, relaxation, and decreased inhibition. Central nervous system depressants are used to treat a number of different disorders, including: insomnia, anxiety, panic attacks, stress, sleep disorders, pain, and seizures. There are three major types of CNS depressants: sedatives, hypnotics, and tranquilizers.
Drugs that are classified as CNS depressants include:
- Alcohol
- Barbiturates
- Benzodiazepines
- Many Sleeping Pills
- Opioids
Different classes of CNS depressants work in different ways, but all have the ability to reduce activity in the central nervous system and lower levels of awareness in the brain. While CNS depressants all share this ability, there are significant differences among substances within this drug class. In particular, some are generally considered to be safer and are prescribed more than others. However, it’s important to note that almost all depressants have the potential to be addictive and should only be used as prescribed. Central nervous system depressants are sometimes called sedatives or tranquilizers, although those terms are more properly applied to specific categories of CNS depressants.
While CNS depressants all share this ability, there are significant differences among substances within this drug class. In particular, some are generally considered to be safer and are prescribed more than others. However, it’s important to note that almost all depressants have the potential to be addictive and should only be used as prescribed. Central nervous system depressants are sometimes called sedatives or tranquilizers, although those terms are more properly applied to specific categories of CNS depressants.
Alcohol
Alcohol is one of the most widely used drugs in the world. The degree to which the brain is affected by this central nervous system depressant depends on how much, and how fast, a person drinks. Due to the initial positive behavioral effects of alcohol, many people don’t realize that the substance is a CNS depressant. For example, when someone first begins to drink, he or she may feel less reserved and more relaxed because of the chemical changes alcohol causes within the brain.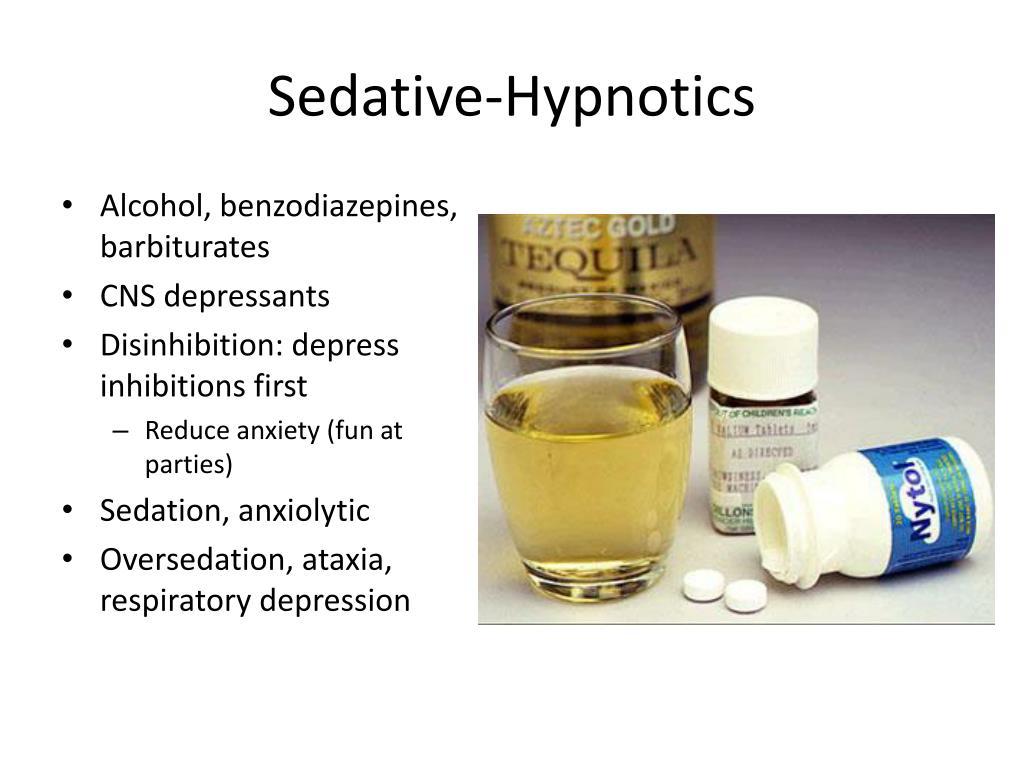 However, the more someone drinks, the more the brain is affected and the likelihood that a negative emotional response will take over. Alcohol can actually increase anxiety and stress rather than reduce it, and elicit other negative reactions such as anger, aggression, and depression. Chronic alcohol use can also lead to dependence, addiction, and withdrawal symptoms when attempting to stop usage of the drug.
However, the more someone drinks, the more the brain is affected and the likelihood that a negative emotional response will take over. Alcohol can actually increase anxiety and stress rather than reduce it, and elicit other negative reactions such as anger, aggression, and depression. Chronic alcohol use can also lead to dependence, addiction, and withdrawal symptoms when attempting to stop usage of the drug.
Barbiturates
Barbiturates, or “downers,” are a type of CNS depressant that are prescribed to treat anxiety, tension, and sleep disorders. Common barbiturates include Amytal, Luminal (Phenobarbital), Mebaral, Nembutal, and Seconal. Barbiturates were previously regarded as a generally safe depressant, but problems with abuse, addiction, and overdose quickly became apparent after widespread prescription. These drugs can generate a sense of euphoria and relaxation even when taken in small doses, which encourages abuse in some. Barbiturates have also shown to have a dramatic impact on sleep patterns, resulting in suppressed REM sleep. In response to particularly high abuse rates from the 1950s to the 1970s, benzodiazepines, which are generally regarded as less addictive and less likely to cause overdose, were developed and popularized. Because the potential for addiction and overdose is so high, the drugs are no longer commonly used to treat anxiety and sleep problems.
In response to particularly high abuse rates from the 1950s to the 1970s, benzodiazepines, which are generally regarded as less addictive and less likely to cause overdose, were developed and popularized. Because the potential for addiction and overdose is so high, the drugs are no longer commonly used to treat anxiety and sleep problems.
Benzodiazepines
Sometimes called “benzos,” benzodiazepines are central nervous system depressants that are prescribed to treat anxiety, sleep disorders, convulsions, and other acute stress reactions. Common benzos include Valium, Xanax, and Ativan. Benzodiazepines are highly effective in treating anxiety and insomnia due to the sleep-inducing, sedative, and muscle-relaxing properties. While considered safe for short-term treatment, long-term or illicit use can lead to the development of a tolerance, addiction, and withdrawal symptoms upon cessation or rapid reduction in use.
Sleeping Pills
This category of CNS depressants includes non-benzodiazepine sleep aids, or “z-drugs,” such as Ambien, Sonata, and Lunesta.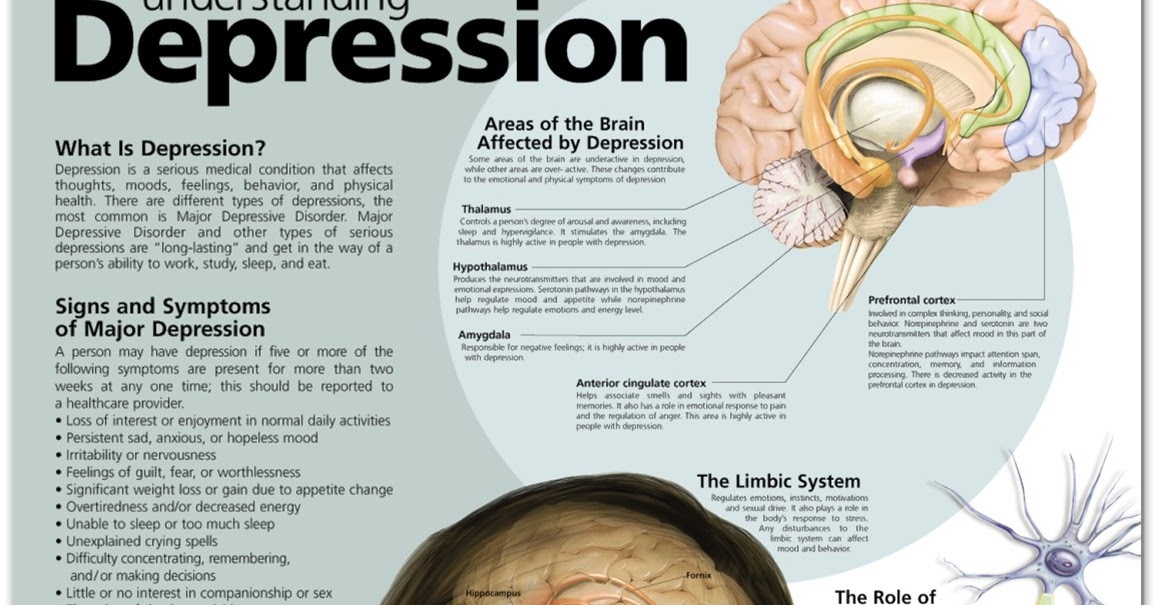 These drugs are designed to specifically treat insomnia and other sleep disorders. These sleeping pills are chemically different from other central nervous system depressants, and they work by stimulating the GABA neurotransmitter in a different way. Unlike benzodiazepines, Z-drugs do not reduce anxiety. The drugs are thought to have fewer side effects and risk of addiction compared to benzodiazepines; however, long-term use can still result in dependence and addiction.
These drugs are designed to specifically treat insomnia and other sleep disorders. These sleeping pills are chemically different from other central nervous system depressants, and they work by stimulating the GABA neurotransmitter in a different way. Unlike benzodiazepines, Z-drugs do not reduce anxiety. The drugs are thought to have fewer side effects and risk of addiction compared to benzodiazepines; however, long-term use can still result in dependence and addiction.
Opioids
Opioids are the most commonly prescribed pain medications in the United States and in much of the world. Some opioids, such as methadone, are also used for other purposes such as opioid addiction treatment. There are a number of different opioids, including legal prescription medications such as codeine and hydrocodone, and illegal street drugs, such as heroin.
While opioids vary tremendously in strength, addictive potential, and other aspects, they tend to be very chemically similar and typically have similar effects.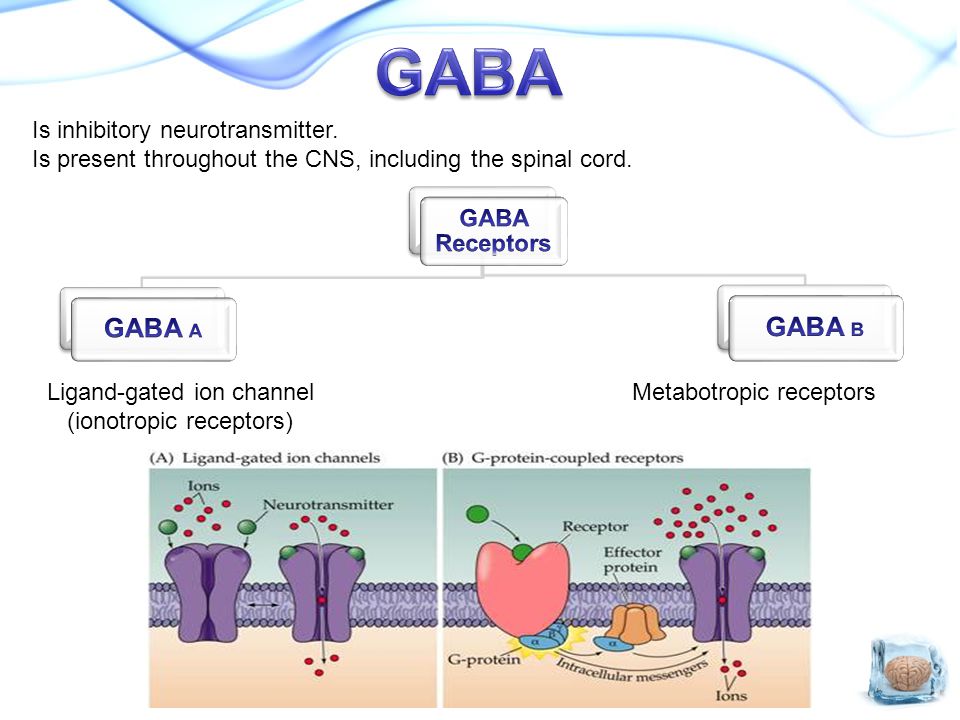 While opioids are considered extremely effective for treating pain, they are also some of the most addictive and dangerous drugs in the world. Every year, opioid overdose takes the lives of tens of thousands of Americans.
While opioids are considered extremely effective for treating pain, they are also some of the most addictive and dangerous drugs in the world. Every year, opioid overdose takes the lives of tens of thousands of Americans.
Effects of Central Nervous System Depressants
Central nervous system depressants work by increasing the production of the neurotransmitter GABA, which in turn slows down brain activity and produces feelings of relaxation, drowsiness, and a number of other effects, including:
- Lowered blood pressure
- Dilated pupils
- Confusion or disorientation
- Slowed pulse and breathing
- Sleepiness or fatigue
- Difficulty urinating
- Dizziness
- Difficulty concentrating
- Memory loss
- Slowed reaction time
- Relaxation and euphoria
- Slurred speech
- Reduced inhibitions
- Loss of coordination
- Impaired judgement
- Blacking out
Long-term use can also produce a variety of negative effects, which depend on the type of depressant used and the severity of misuse.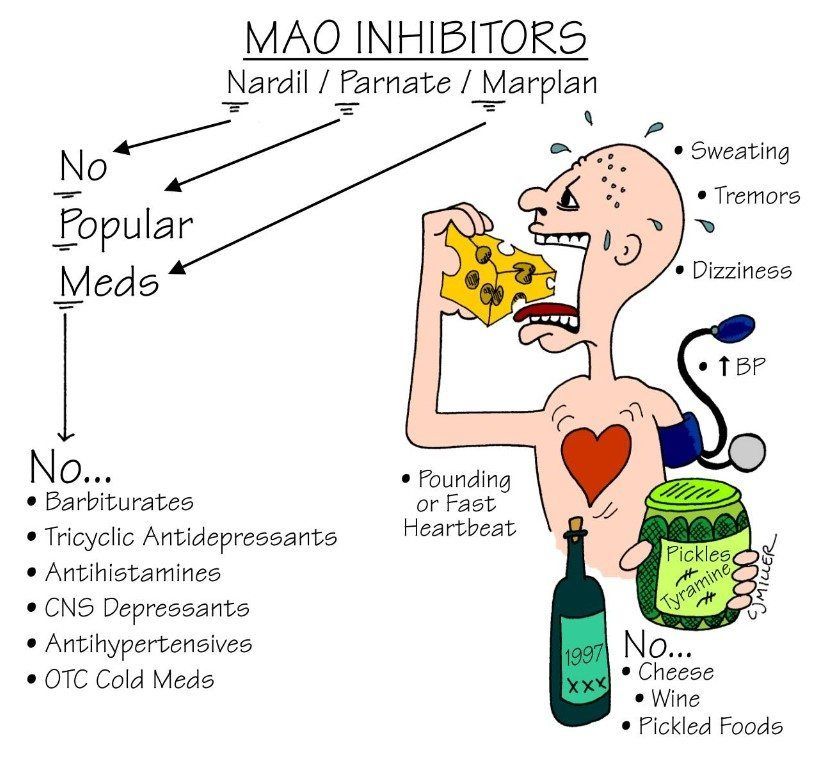 In particular, chronic abusers of depressants may develop a tolerance and require increasing doses to maintain the desired effects. Other potential long-term effects include:
In particular, chronic abusers of depressants may develop a tolerance and require increasing doses to maintain the desired effects. Other potential long-term effects include:
- Chronic fatigue
- Weight gain
- Hypersomnia
- Sexual dysfunction
- Breathing and sleep difficulties
- Depression
- Suicidal thoughts
- Physical dependence
- Addiction
Another possible side effect of central nervous system depressant use is overdose. Excessive consumption of depressants can lead to respiratory depression, seizures, and potentially even death. CNS depressants should not be combined with any medication or substance that causes sedation, including prescription pain medicines, certain over-the-counter allergy medications, and alcohol. If combined, they can slow breathing, or heart rate and respiration, which can be fatal. This risk is also compounded if CNS depressants are used to offset the effects of stimulant drugs, such as cocaine or Adderall. In particular, it is extremely dangerous to combine multiple CNS depressants, because the risk of serious complications such as overdose, respiratory failure, and death are greatly magnified.
In particular, it is extremely dangerous to combine multiple CNS depressants, because the risk of serious complications such as overdose, respiratory failure, and death are greatly magnified.
Looking for a place to start?
Join the thousands of people that have called a treatment provider for rehab information.
Free and confidential
Available 24/7
Access to professional treatment
Make a Call (870) 515-4356 (870) 515-4356
- OR -
Request a Call
Signs of CNS Depressant Abuse
The foremost sign of CNS depressant abuse is taking the drugs without medical direction, or outside a doctor’s prescribed guidelines. Examples of this include taking higher doses to intensify intoxication and taking someone else’s prescription. Other warning signs include:
- Secretive or abnormal behavior
- Decreased social activity or work productivity
- Mood swings
- Periods of depression or apathy
- Lack of energy or motivation
- Withdrawal symptoms when not using depressants
- Failing in attempts to stop using the drugs
Another telling sign of abuse is mixing CNS depressants with other drugs, including opioids and alcohol, to increase their effects.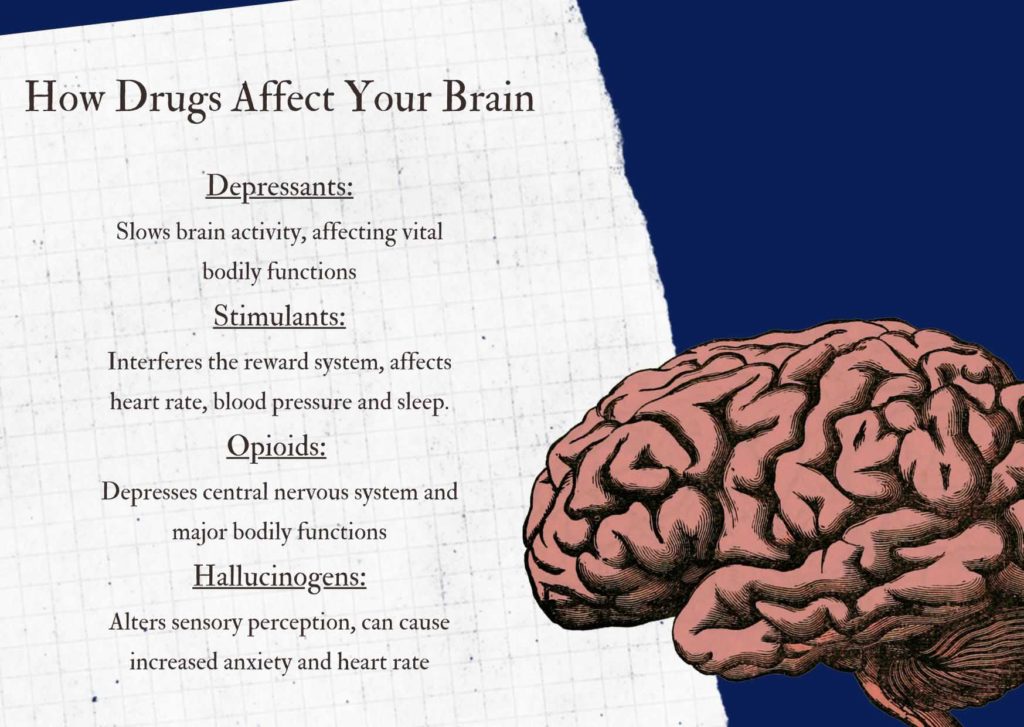 This may lead to severe adverse health reactions and possibly life-threatening consequences.
This may lead to severe adverse health reactions and possibly life-threatening consequences.
Central Nervous System Depressant Withdrawal
Discontinuing use of CNS depressants can lead to withdrawal. Because of the way that depressants affect brain chemistry and slow activity, withdrawal can be severe and sudden when an individual stops taking them. Withdrawal symptoms typically begin 12 to 24 hours after the last dose of the drug and are most severe between 24 and 72 hours after this dose. Withdrawal symptoms generally begin to fade after this initial period, known as acute withdrawal; however, some symptoms, known as post-acute withdrawal symptoms (PAWS) may last for up to 24 months.
Additionally, many people going through benzodiazepine or barbiturate withdrawal will also experience a rebound effect in which the condition that they were originally taking the sedative for will come back stronger than before. For example, someone that was taking Xanax for anxiety will often experience worse anxiety upon cessation of the drug. Someone thinking about ending their use of a CNS depressant, or who has stopped and is suffering from withdrawal, should immediately seek medical treatment.
Someone thinking about ending their use of a CNS depressant, or who has stopped and is suffering from withdrawal, should immediately seek medical treatment.
Common central nervous system depressant withdrawal symptoms include:
- Insomnia
- Restlessness
- Nausea
- Vomiting
- Shaking
- Weakness
- Excessive sweating
- Irritability
- Hallucinations
- Anxiety
- Panic attacks
- Body tremors
- Seizures
- Depression
- Muscular stiffness or pain
- Changes in perception
- Heart palpitations
- Tension
- Memory issues
- Increased blood pressure and pulse
- Hypersensitivity to light and sound
- Aches and pains
Withdrawal from depressants can have potentially-life threatening complications. These risks are amplified when someone quits use of these drugs on their own or tries to stop taking them “cold turkey.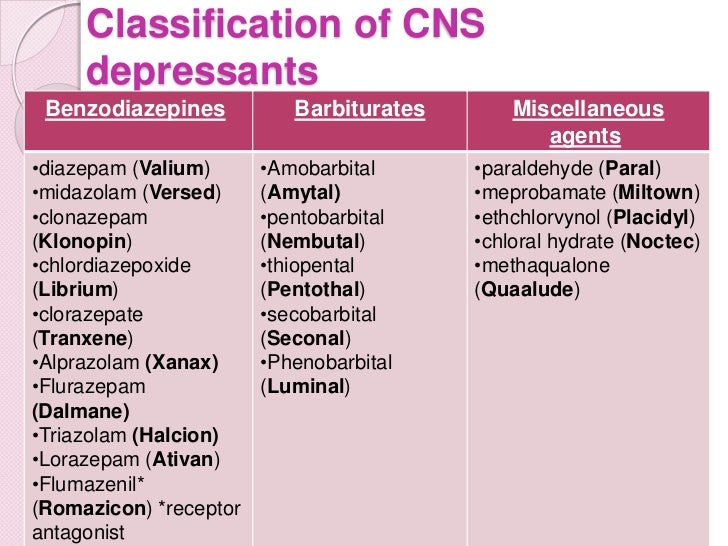 ” Medically-assisted detox is the safest way to withdraw from CNS depressants, as physicians can gradually decrease use and prescribe any medications to assist with debilitating withdrawal symptoms.
” Medically-assisted detox is the safest way to withdraw from CNS depressants, as physicians can gradually decrease use and prescribe any medications to assist with debilitating withdrawal symptoms.
Check if my insurance covers rehab
Addiction Center is not affiliated with any insurance.
Treatment and Therapies for CNS Depressant Addiction
Treatment for addiction to a central nervous system depressant begins with detox to allow the drugs to exit the system, preferably in rehab or medical facility. After detoxification, a patient will typically move onto a residential inpatient or outpatient treatment program. Drug abuse often co-occurs with other psychological issues, such as depression, and rehab affords individuals struggling with addiction the opportunity for these issues to be addressed with licensed professionals.
Treatment facilities will tailor treatment plans to the individual and include different types of therapies to help the patient replace negative behaviors with healthier ones.