Can your brain shut down
Neural circuits responsible for conscious self-control are highly vulnerable to even mild stress. When they shut down, primal impulses go unchecked and mental paralysis sets in
- Journal List
- HHS Author Manuscripts
- PMC4774859
Sci Am. Author manuscript; available in PMC 2016 Mar 2.
Published in final edited form as:
Sci Am. 2012 Apr; 306(4): 48–53.
doi: 10.1038/scientificamerican0412-48
PMCID: PMC4774859
NIHMSID: NIHMS761807
PMID: 22486116
Copyright and License information Disclaimer
The entrance exam to medical school consists of a five-hour fusillade of hundreds of questions that, even with the best preparation, often leaves the test taker discombobulated and anxious.
For some would-be physicians, the relentless pressure causes their reasoning abilities to slow and even shut down entirely. The experience—known variously as choking, brain freeze, nerves, jitters, folding, blanking out, the yips or a dozen other descriptive terms—is all too familiar to virtually anyone who has flubbed a speech, bumped up against writer’s block or struggled through a lengthy exam.
For decades scientists thought they understood what happens in the brain during testing or a battlefront firefight. In recent years a different line of research has put the physiology of stress in an entirely new perspective. The response to stress is not just a primal reaction affecting parts of the brain that are common to a wide array of species ranging from salamanders to humans. Stress, in fact, can cripple our most advanced mental faculties, the areas of the brain most developed in primates.
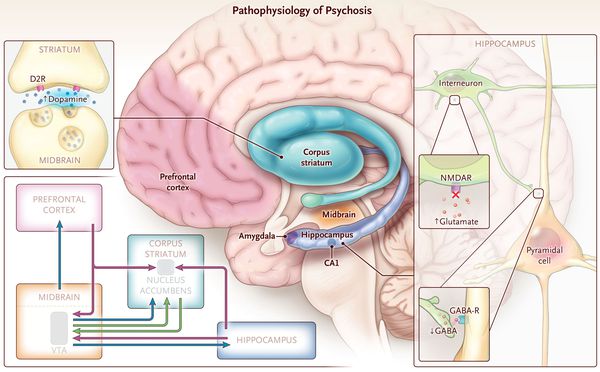
Older textbooks explained that the hypothalamus, an evolutionarily ancient structure lodged at the base of the brain, reacts to stress by triggering the secretion of a wave of hormones from the pituitary and adrenal glands, which makes the heart race, elevates blood pressure and diminishes appetite.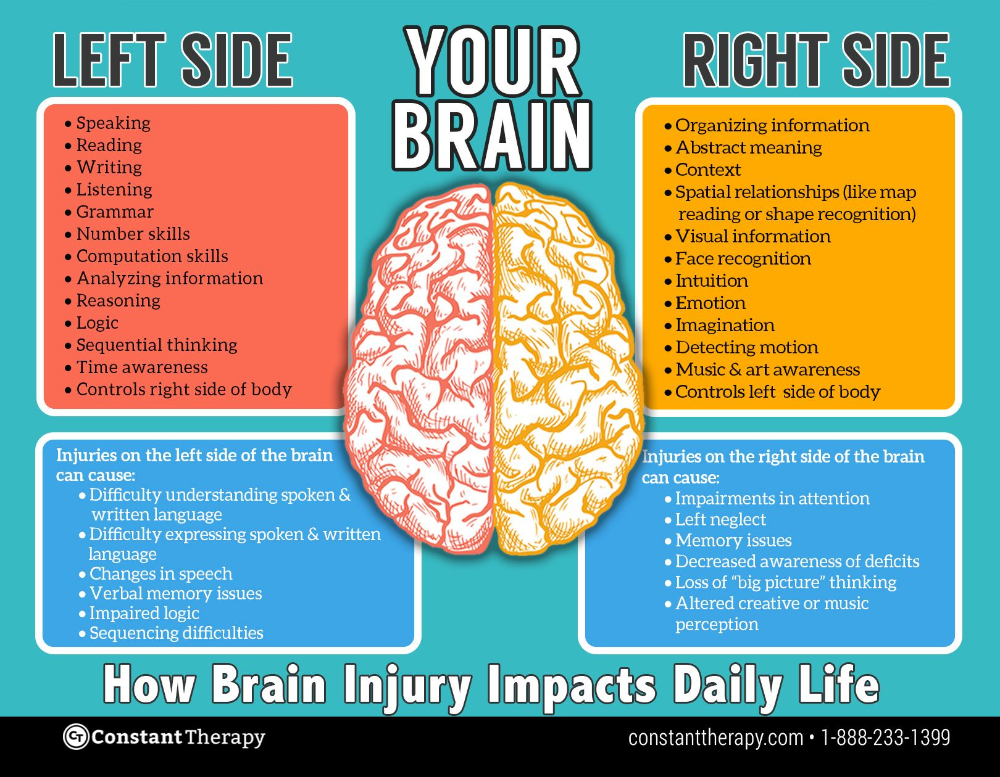 Now research reveals an unexpected role for the prefrontal cortex, the area immediately behind the forehead that serves as the control center that mediates our highest cognitive abilities—among them concentration, planning, decision making, insight, judgment and the ability to retrieve memories. The prefrontal cortex is the part of the brain that evolved most recently, and it can be exquisitely sensitive to even temporary everyday anxieties and worries.
Now research reveals an unexpected role for the prefrontal cortex, the area immediately behind the forehead that serves as the control center that mediates our highest cognitive abilities—among them concentration, planning, decision making, insight, judgment and the ability to retrieve memories. The prefrontal cortex is the part of the brain that evolved most recently, and it can be exquisitely sensitive to even temporary everyday anxieties and worries.
When things are going well, the prefrontal cortex acts as a control center that keeps our baser emotions and impulses in check. The new research demonstrates that acute, uncontrollable stress sets off a series of chemical events that weaken the influence of the prefrontal cortex while strengthening the dominance of older parts of the brain. In essence, it transfers high-level control over thought and emotion from the prefrontal cortex to the hypothalamus and other earlier evolved structures. As the older parts take over, we may find ourselves either consumed by paralyzing anxiety or else subject to impulses that we usually manage to keep in check: indulgence in excesses of food, drink, drugs or a spending spree at a local specialty store. Quite simply, we lose it.
Quite simply, we lose it.
The growing understanding that acute stress can severely compromise the function of higher “executive” areas in the human brain has drawn the interest of investigators. They are now not just trying to understand what happens in your head when you freeze but also developing behavioral and pharmaceutical interventions to help you keep your composure.
Why we lose it has fascinated scientists for decades. After World War II, investigators analyzed why pilots who were highly skilled in peacetime made simple but fatal mistakes in maneuvering their craft during the heat of battle. What actually happens behind the human skull’s frontal bone remained a mystery until the relatively recent arrival of neuroimaging techniques. In a brain scanner, the riot of activity in the prefrontal cortex gives a clue to just how vulnerable the brain’s master controller is.
The prefrontal cortex is so sensitive to stress because of its special status within the hierarchy of brain structures. It is the most highly evolved brain region, bigger proportionally in humans than in other primates, and makes up a full third of the human cortex. It matures more slowly than any other brain area and reaches full maturity only after the teen years have passed. The prefrontal area houses the neural circuitry for abstract thought and allows us to concentrate and stay on task, while storing information in the mental sketch pad of working memory. This temporary memory storage area operates by allowing us to keep “in mind” such information as the sum of digits that need to be carried over to the next column when performing addition. As a mental-control unit, the prefrontal area also inhibits inappropriate thoughts and actions.
It is the most highly evolved brain region, bigger proportionally in humans than in other primates, and makes up a full third of the human cortex. It matures more slowly than any other brain area and reaches full maturity only after the teen years have passed. The prefrontal area houses the neural circuitry for abstract thought and allows us to concentrate and stay on task, while storing information in the mental sketch pad of working memory. This temporary memory storage area operates by allowing us to keep “in mind” such information as the sum of digits that need to be carried over to the next column when performing addition. As a mental-control unit, the prefrontal area also inhibits inappropriate thoughts and actions.
The neurological executive center functions through an extensive internal network of connections among the triangular-shaped neurons called pyramidal cells. These neurons also send out connections to more distant reaches of the brain that control our emotions, desires and habits. When unstressed, the circuits in this network hum along contentedly. Working memory reminds us to start that assignment due next week, and other circuitry sends a message to lower brain regions signaling that it is perhaps best to forgo a second glass of wine. Meanwhile a message to the amygdala, a deep-brain structure that controls fear reactions, provides assurance that the huge hulk approaching on the sidewalk is not about to smash you in the face.
When unstressed, the circuits in this network hum along contentedly. Working memory reminds us to start that assignment due next week, and other circuitry sends a message to lower brain regions signaling that it is perhaps best to forgo a second glass of wine. Meanwhile a message to the amygdala, a deep-brain structure that controls fear reactions, provides assurance that the huge hulk approaching on the sidewalk is not about to smash you in the face.
Keeping this network firing as it should can be a fragile process—and when stress hits, even small changes in the neurochemical environment can instantly weaken network connections. In response to stress, our brain floods with arousal chemicals such as norepinephrine and dopamine, which are released by neurons in the brain stem that send projections throughout the brain. Elevated levels of these signaling chemicals in the prefrontal cortex shut off neuron firing, in part by weakening the connection points, or synapses, between neurons temporarily. Network activity diminishes, as does the ability to regulate behavior. These effects only worsen as the adrenal glands near the kidneys, on command from the hypothalamus, spritz the stress hormone cortisol into the bloodstream, sending it to the brain. In this circumstance, self-control depends on a tricky balancing act.
Network activity diminishes, as does the ability to regulate behavior. These effects only worsen as the adrenal glands near the kidneys, on command from the hypothalamus, spritz the stress hormone cortisol into the bloodstream, sending it to the brain. In this circumstance, self-control depends on a tricky balancing act.
“Keeping one’s cool” is an expression that accurately represents a description of the underlying biological processes. The neural machinery of the prefrontal cortex—and its ability to muster working memory to stay focused on the task at hand—may keep the cascade of neurotransmitters generated deep within the brain from triggering a panicked tide of emotion.
Our research clarifying how easily the prefrontal cortex can be shut down started about 20 years ago. Studies in animals by one of us (Arnsten), along with the late Patricia Goldman-Rakic of Yale University, were among the first to illustrate how neurochemical changes during stress can rapidly switch off prefrontal function.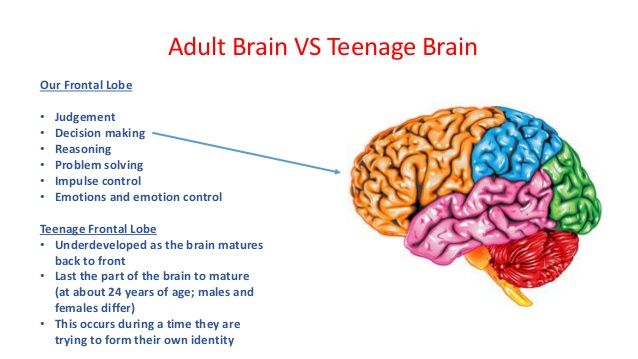 The work showed that neurons in the prefrontal cortex disconnect and stop firing after being exposed to a flood of neurotransmitters or stress hormones.
The work showed that neurons in the prefrontal cortex disconnect and stop firing after being exposed to a flood of neurotransmitters or stress hormones.
In contrast, areas deep within the brain take a stronger hold over our behavior. Dopamine arrives at a series of deep-brain structures, collectively called the basal ganglia, that regulate cravings and habitual emotional and motor responses. The basal ganglia hold sway not only when we ride a bicycle without falling but also when we indulge in addictive habits, such as those that make us long for that forbidden ice cream.
In 2001 Benno Roozendaal, now at the University of Groningen in the Netherlands, James McGaugh of the University of California, Irvine, and their colleagues found similar changes in the amygdala, another older brain region. In the presence of norepinephrine and cortisol, the amygdala alerts the rest of the nervous system to prepare for danger and also strengthens memories that are related to fear and other emotions.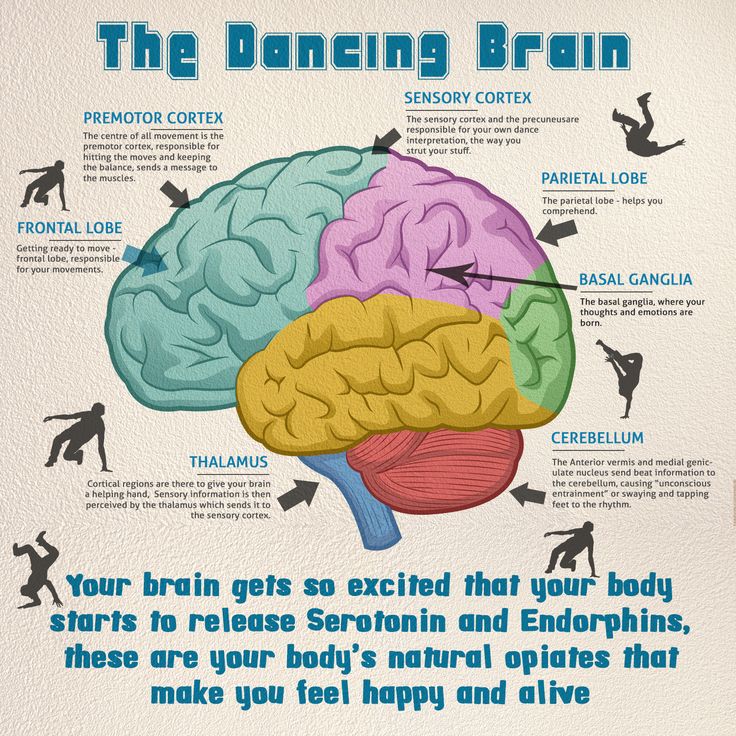
This research now extends to humans. These studies have begun to show that some people seem more vulnerable than others because of their genetic makeup or because of a previous history of stress exposure. After dopamine and norepinephrine switch off circuits in the prefrontal area required for higher cognition, enzymes normally chew up the neurotransmitters so that the shutdown does not persist. In this way, we can return to our baseline when stress abates. Certain forms of a gene can weaken these enzymes, making people more vulnerable to stress and, in some cases, mental illness. Similarly, environmental factors can increase vulnerability; for example, lead poisoning can mimic aspects of the stress response and erode cognition.
Still other research focuses on what happens when the assault on the prefrontal cortex lasts for days or weeks. Chronic stress appears to expand the intricate web of connections among neurons in our lower emotional centers, whereas the areas engaged during flexible, sustained reasoning—anything from the philosophy of Immanuel Kant to calculus—start to shrivel.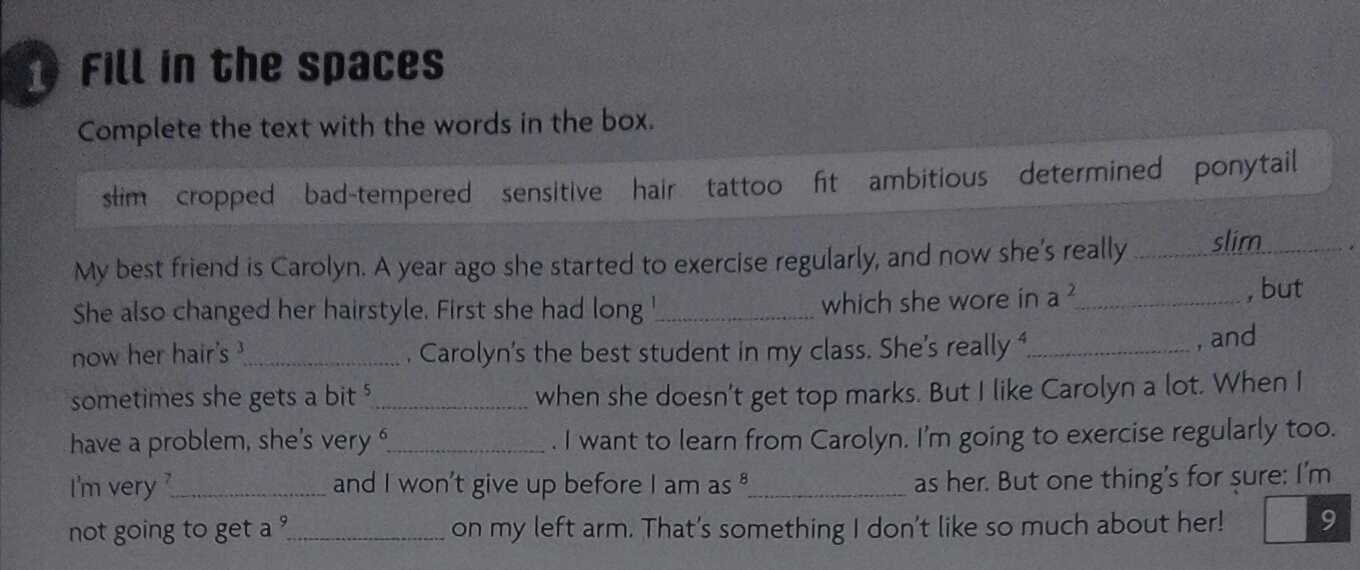 Under these conditions, the branching, signal-receiving dendrites in the primal amygdala enlarge, and those in the prefrontal cortex shrink. John Morrison of the Mount Sinai School of Medicine and his colleagues have shown that prefrontal dendrites can regrow if the stress disappears, but this ability to rebound may vanish if the stress is especially severe. One of us (Sinha) has found evidence of this in humans, where the shrinkage in prefrontal gray matter relates to history of stress exposure.
Under these conditions, the branching, signal-receiving dendrites in the primal amygdala enlarge, and those in the prefrontal cortex shrink. John Morrison of the Mount Sinai School of Medicine and his colleagues have shown that prefrontal dendrites can regrow if the stress disappears, but this ability to rebound may vanish if the stress is especially severe. One of us (Sinha) has found evidence of this in humans, where the shrinkage in prefrontal gray matter relates to history of stress exposure.
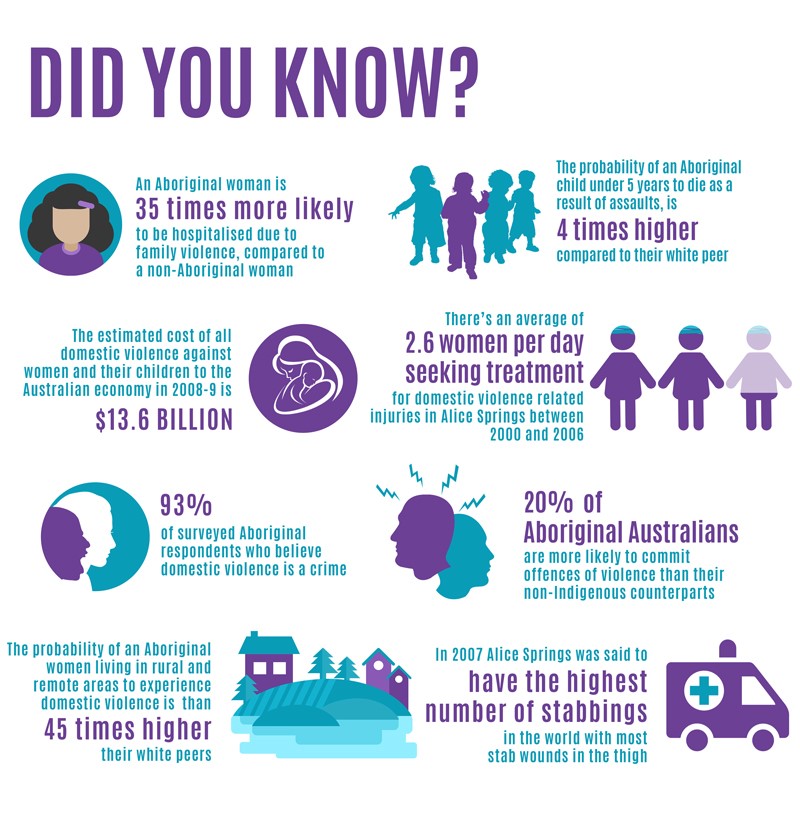
This chain of molecular events makes us more vulnerable to subsequent stress and most likely contributes to depression, addiction and anxiety disorders, including post-traumatic stress. Gender appears to be a factor in determining how we react to stress. In women, the hormone estrogen may amplify sensitivity. For example, as one of us (Mazure) and her colleagues have shown, life stress poses a greater risk for depression in women than men and is more likely to reduce abstinence from certain addictive behaviors, such as smoking, for women as compared with men. In men, stress may play a more prominent role in exacerbating cravings and eliciting habitual behaviors mediated by the basal ganglia.
In men, stress may play a more prominent role in exacerbating cravings and eliciting habitual behaviors mediated by the basal ganglia.
More work on how stress alters the brain’s prefrontal self-control locus remains to be done. Some researchers are investigating how other neurochemicals affect the prefrontal cortex. Trevor W. Robbins and Angela Roberts of the University of Cambridge head one group looking at whether serotonin, which plays a key role in depression, may modulate stress and anxiety through its actions in the prefrontal cortex.
These studies remain challenging because modern ethical standards for experiments using humans require that subjects should not be exposed to situations of extreme psychological stress, and indeed human study participants are told they can stop at any time, giving them control over the experimental situation in a manner that does not mimic real-life stress. Several labs have succeeded in simulating the effects of uncontrolled stress by having study participants watch disturbing movies or, as done by the Sinha group, briefly imagine their own stressful experiences to tap into their reactions.
One question that still perplexes researchers is why the brain has built-in mechanisms to weaken its highest cognitive functions. We still do not know for sure, but the triggering of these primal reactions may perhaps have saved human lives when a predatory wild animal was lurking in the bushes. If we suddenly see a tiger burning bright in the forest, it is far more useful to freeze so that the animal cannot see us than to be remembering the words of William Blake’s poem.
Absent our slow, deliberate higher-brain networks, primitive brain pathways can stop us on a dime or ready us to flee. These mechanisms may serve a similar function when we face danger in the modern world—say, when a reckless driver cuts us off and we need to slam on the brakes. If we remain in this state, though, prefrontal function weakens, a devastating handicap in circumstances where we need to engage in complex decision making about a loved one’s serious medical condition or organize an important project on a tight deadline.
A logical response to our growing understanding of the jitters is to devise strategies to keep our neural-control center intact. Scientists hope that understanding the molecular events that cause the brain to degenerate from a “reflective” to a “reflexive” state may lead to better treatments for stress disorders. Some of these insights confirm what we already know. Training for emergencies or for military service is all about teaching the basal ganglia and other brain structures to learn the automatic reactions needed to survive. Animal research suggests that the sense of psychological control that becomes second nature to a soldier or emergency medical technician remains the deciding factor in whether we fall apart during stress. Public speaking exhilarates those who feel confident before an audience. For others, it induces nothing but terror, and their minds “go blank.”
The routines of the drill sergeant are mirrored by animal studies that show that juveniles grow up to be more capable in handling stress if they have had multiple, successful experiences confronting mild stress in their youth. Similarly, human studies indicate that success in managing challenging situations can build resilience. In contrast, if children stumble through these experiences, they can become more sensitive to and burdened by stress and depression when they grow up.
Similarly, human studies indicate that success in managing challenging situations can build resilience. In contrast, if children stumble through these experiences, they can become more sensitive to and burdened by stress and depression when they grow up.
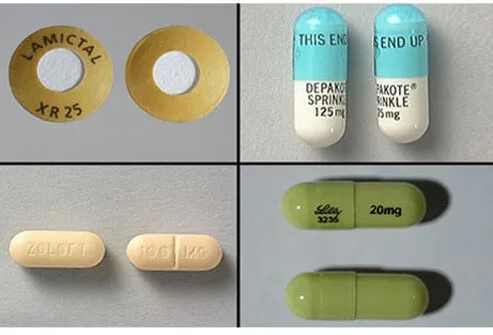
Clues to new treatments may be slowly emerging from the laboratory. The drug prazosin, a generic therapy for blood pressure that blocks some of norepinephrine’s detrimental actions, is being tested in veterans and civilians with post-traumatic stress disorder. Prazosin also appears to decrease both alcohol cravings and levels of consumption. A very recent study by Sherry McKee of Yale and her colleagues has found that another generic medication for blood pressure, called guanfacine, can inhibit some stress reactions and strengthen prefrontal cortical networks, helping people to resist smoking during stress exposure. (Arn-sten and Yale University receive royalties from Shire Pharmaceuticals for an extended-release form of guanfacine used for treatment of attention-deficit hyperactivity disorder for children and adolescents but do not receive royalties for the immediate-release form of the drug used in adults in this study. ) Further, many labs have shown that behavioral strategies such as relaxation, deep breathing and meditation can reduce the stress response.
) Further, many labs have shown that behavioral strategies such as relaxation, deep breathing and meditation can reduce the stress response.
And what about that sense of control? Perhaps by learning about how the brain reacts to stress, you may come away with an enhanced sense of control. So maybe the next time you are taking a test or speaking in public and your mind goes blank, you can say to yourself, “This is just my brain trying to save me from a tiger.” Maybe it will bring a comforting smile to your face even if it does not bring the correct answer or word to mind.
| Freezing under stress | a common experience for all of us at some point in our life, has its roots in a loss of control over “executive functions” that allow us to control our emotions. |
| Prefrontal cortical areas | which serve as the brain’s executive command centers, normally hold our emotions in check by sending signals to tone down activity in primitive brain systems. |
| Under even everyday stresses | the prefrontal cortex can shut down, allowing the amygdala, a locus for regulating emotional activity, to take over, inducing mental paralysis and panic. |
| Researchers are probing | further the physiology of acute stress and are considering behavioral and pharmaceutical interventions to help us retain composure when the going gets tough. |
Amy Arnsten is a professor of neurobiology at the Yale School of Medicine. Her research on molecular changes in the prefrontal cortex during stress and aging has led to treatments such as prazosin and guanfacine for post-traumatic stress disorder, attention-deficit hyperactivity disorder and other conditions.
Carolyn M. Mazure is a professor of psychiatry and psychology and associate dean for faculty affairs at the Yale School of Medicine. She created and directs Yale’s interdisciplinary women’s health research center.
Rajita Sinha directs the Yale Stress Center, which focuses on understanding the effects of stress on behavior. She is a professor of psychiatry at the Yale School of Medicine.
SCIENTIFIC AMERICAN ONLINE
Take a simple self-assessment to test the extent you are affected by acute stress at ScientificAmerican/apr2012/stress
- Amy FT. Stress Signalling Pathways That Impair Prefrontal Cortex Structure and Function. Arnsten in Nature Reviews Neuroscience. 2009 Jun;10:410–422. [PMC free article] [PubMed] [Google Scholar]
- Halpern Sue. Can’t Remember What I Forgot: Your Memory, Your Mind, Your Future. Three Rivers Press; 2009. [Google Scholar]
- Amy FT. Prefrontal Cortical Network Connections: Key Site of Vulnerability in Stress and Schizophrenia. Arnsten in International journal of Developmental Neuroscience. 2011;29(3):215–223. [PMC free article] [PubMed] [Google Scholar]
When Your Brain Crashes
Contrary to popular ideas about multitasking, when we attempt to do too many things at one time, especially if we are trying to do complex tasks, we end up being less effective and less productive. This can result in something called cognitive overload. Basically, just like a computer crashes, our brain shuts down, drastically limiting our ability to process all that is coming in. We often speak about this as being, or feeling overwhelmed or anxious. It’s kind of like trying to take a drink from a firehose, for example—it’s not very effective and we end up feeling more frustrated and stressed than when we started.
This can result in something called cognitive overload. Basically, just like a computer crashes, our brain shuts down, drastically limiting our ability to process all that is coming in. We often speak about this as being, or feeling overwhelmed or anxious. It’s kind of like trying to take a drink from a firehose, for example—it’s not very effective and we end up feeling more frustrated and stressed than when we started.
How stress can get in the way.
When we are problem solving, our brains are doing three very important activities: 1) taking in information from both our internal and external environment; 2) attempting to hold onto and remember information that is required for solving a particular problem; and 3) logically organizing that information by either combining, adding, and/or subtracting information, in order to make sense of how all that information is linked. However, all of these tasks that the mind undertakes cannot be effectively done at the same time.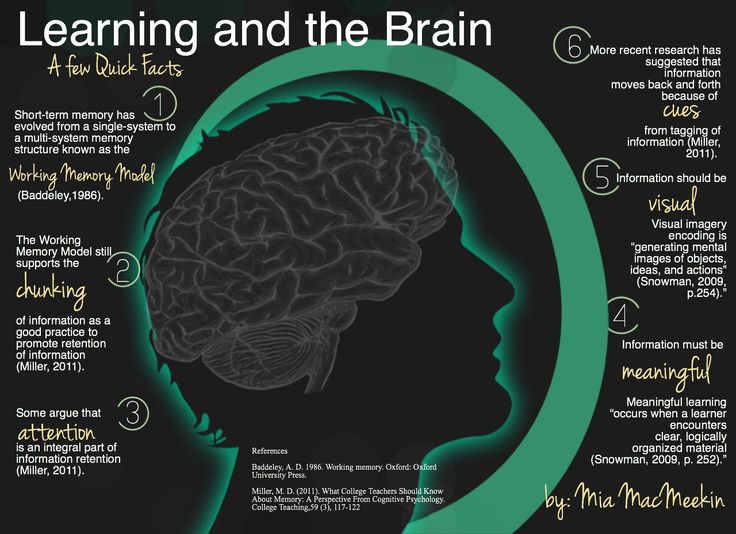 This is especially true when we are under stress, as it becomes even harder to be an effective problem solver. For example, trying to remember a bunch of info can interfere with understanding how all the pieces fit together. Another example, would be fighting with a spouse, being laid off from a job, dealing with a chronic disease, etc. all of these stressors can cloud our minds or distort our view of our problems.
This is especially true when we are under stress, as it becomes even harder to be an effective problem solver. For example, trying to remember a bunch of info can interfere with understanding how all the pieces fit together. Another example, would be fighting with a spouse, being laid off from a job, dealing with a chronic disease, etc. all of these stressors can cloud our minds or distort our view of our problems.
Dealing with cognitive overload: externalization
One tool we can use to combat cognitive overload is called externalization. Externalization involves putting to paper what is going on in our heads. This not only frees us from the difficult task of remembering all the different components of a problem, but more, allows us to begin the process of 1) better understanding and defining our problem and goal; 2) brainstorming possible solutions to solve our problem; 3) comparing each of the solutions in order to choose the one that has the highest probability of working; and 4) after testing out our solution, evaluating the outcome.
Dealing with cognitive overload: visualization
Another tool that proves useful in overcoming cognitive overload is Visualization. Visualization, as its name suggests, involves picturing a specific reality in our mind’s eye. This can help us better clarify a problem we are facing. That is, we can visualize each part of the problem we are facing and explore possible solutions. Eventually, this tool can help us identify the steps we need to get where we want to go.
For example, many professional athletes use this tool in order to enhance their success—from golfers visualizing their shot, to Olympic slalom skiers rehearsing each part of the course. Similarly, you can rehearse the steps you will take when deciding on how to solve a particular problem or issue you are facing.
Visualization is also a form of mindfulness which can help reduce our stress and anxiety. For example, some people during times of distress visualize a “safe place,” such as a favorite vacation spot, etc. to help calm themselves down. Other people use guided meditations as a way to change feeling states.
to help calm themselves down. Other people use guided meditations as a way to change feeling states.
Dealing with cognitive overload: simplification.
A final tool to help when we are feeling overloaded is called simplification. Simplification involves breaking complex problems down into a series of manageable steps. That is, it helps us take vague problems or goals and make them more specific, so that they are easier to work on, thereby reducing stress of large overwhelming goals or problems. For example, if we were working on a long-term goal of completing a four-year degree, simplification would involve focusing only on what we need to get done for that particular semester. Again, this is a way to practice mindfulness, as we are focusing only on what we need to do in the present to get to the next step.
About The Author
Isaac Smith, MAT, LCSW, FNTP is the founder of Whole Wellness Therapy, and serves as the Executive Director. Isaac gives presentations on topics including addiction, trauma, grief and loss, and anxiety, in addition to providing professional consultations. Prior to founding the practice, Isaac worked with UC Davis Health to help them build and launch their substance use disorder treatment program as well as their Collaborative Care program, which focuses on treating chronic depression and anxiety in older adults. Committed to life-long learning, Isaac holds a master's degree in Theology and has advanced training in nutritional therapy. Currently, he is pursuing a doctor of psychology degree at the Wright Institute in Berkeley, CA.
Isaac gives presentations on topics including addiction, trauma, grief and loss, and anxiety, in addition to providing professional consultations. Prior to founding the practice, Isaac worked with UC Davis Health to help them build and launch their substance use disorder treatment program as well as their Collaborative Care program, which focuses on treating chronic depression and anxiety in older adults. Committed to life-long learning, Isaac holds a master's degree in Theology and has advanced training in nutritional therapy. Currently, he is pursuing a doctor of psychology degree at the Wright Institute in Berkeley, CA.
How sleep deprivation affects the brain: the largest study ever
- Fergus Walsh
- BBC Medical Columnist
events.
Image copyright Elenathewise
Image caption Chronic sleep deprivation is one of the problems of modern life.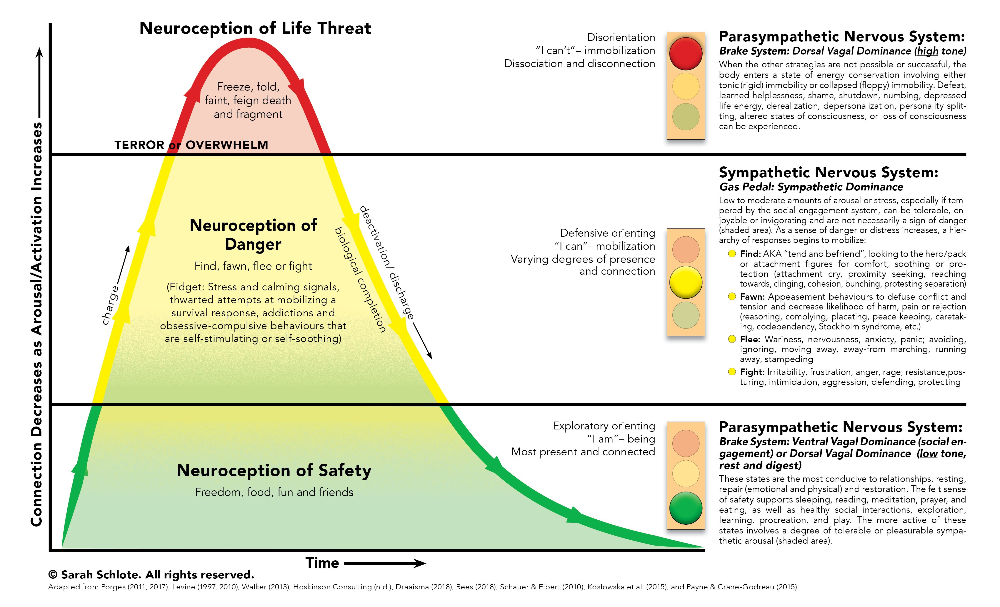
A team of researchers from the University of Western Ontario is calling on volunteers from around the world to complete a series of online cognitive tests.
With the help of specially designed computer programs, those who wish can evaluate their logic, language understanding and decision-making skills.
- Scientists: sleep is the key to beauty and success in communication
- Why we get sleepy after eating and what foods are to blame
- American company pays employees extra for sleep
I also decided to take these tests, agreeing that my brain would be scanned.
Pioneers
Leading the study is Adrian Owen, a British professor of neuroscience at the Institute of Brain and Consciousness at the University of Western Ontario.
"We're all familiar with the sensations of lack of sleep, but we don't know much about how sleep deprivation affects the brain," explains Professor Owen.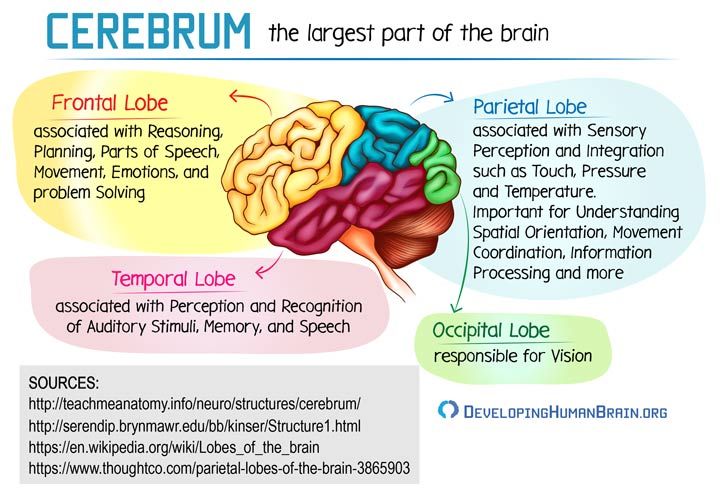 "We want to find out how it affects cognition, memory, and concentration." ".
"We want to find out how it affects cognition, memory, and concentration." ".
In the course of research, scientists intend to find out how people's cognitive performance will differ depending on how much they were assigned to sleep.
Of course, each person's sleep needs are different, but if researchers can recruit enough volunteers, they can determine the average number of hours of sleep needed for optimal brain function.
I joined a group of 4 volunteers who agreed to spend the night at the University of Western Ontario, where we experienced "brain games" that showed how the ability to perceive information depends on the amount of sleep.
Photo copyright, Alamy
Photo caption,Volunteers (clockwise from top left): Dr. Human Ganjavi, Sylvia Salewski, Evan Agnew, Cecilia Kramar
Volunteers
- Dr. Human Ganjavi, psychiatrist, 42 often working with patients on night shifts: "4-5 hours of sleep per night is normal for me.
 I know that lack of sleep leads to heart disease and can cause a stroke, but like many doctors, I do not consider this to myself."
I know that lack of sleep leads to heart disease and can cause a stroke, but like many doctors, I do not consider this to myself." - Silvia Salewski, 31 years old. Mother of two girls who are under 5 years old: “A good night is when they wake me up only two or three times. I don’t even remember what it’s like to sleep peacefully all night and I often feel scattered in the morning” .
- Evan Agnew, 75, retired, night shift clerk: "I've never needed 8 hours of sleep in a row, and at my age now I don't need more than 4 hours in a row. I get sleep during the day with a couple of naps."
- Cecilia Kramar, 31, neuroscientist, she studies the cognitive abilities of nocturnal mice, so she often stays up late in the lab: my brain can't function properly."
Tests
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
End of story Podcast
The tests offered by the authors of the study can be taken on regular computers, tablets and even smartphones.
Double Trouble: Seemingly simple, this test makes your gray matter move. You need to click on the word below that matches the color of the word above. If the word at the top is "blue" but it is red, you must click on the word at the bottom that is written in red, even if that word is "blue". Sounds crazy...
"Cut Out": The test starts out easy, but gets more difficult as you try to find a piece that is out of line.
Grammar logic: is the statement about the presented diagram true or false? At first glance, there is nothing difficult in this, until it comes to negative statements.
Spatial Planning: Like all games, these quizzes test your planning ability by measuring the cognitive skills you use in everyday life.
How did we manage?
We were awake until 4 am, after which we were allowed to sleep for 4 hours.
When we took the cognitive test again in the morning, Evan's, Cecilia's, and mine's scores were much worse than the night before.
The result of Human, who is used to working with patients in shifts, has not changed much, while it has even improved with Sylvia.
Image copyright, OWEN LAB, WESTERN
Image caption,The scan on the left shows brain activity after a full sleep, on the right - brain activity after a sleepless night
"Even though I'm feeling a bit scattered this morning, maybe it's because I'm used to not getting enough sleep," she explains. "I need to turn on as soon as the kids wake up, so that's okay for me."
I've always known that if I don't get enough sleep, I don't function well, so it wasn't surprising that my cognitive performance dropped dramatically in the morning.
To find out what was happening in my brain, I repeated the cognitive test already inside the MRI machine.
I was scanned twice: after a normal night's sleep and after a sleepless night.
MRI is able to detect blood flow in the brain: areas with increased activity are characterized by stronger flows, which look like orange clots on the graph.
The difference between the two scans was impressive: after a sleepless night, my brain activity was clearly inadequate, there were far fewer processes observed in it.
"Activity in the frontal and parietal lobes, which are known to be responsible for decision making, memory and problem solving, is markedly reduced," explains Professor Owen.
Photo copyright, FERGUS WALSH
Photo caption,Study led by Professor Adrian Owen of the University of Western Ontario
We all know how dangerous it is to drive when tired, as your reaction time slows down and you can fall asleep behind the wheel.
However, we know much less about the subtle effects of daily lack of sleep.
"It's possible that lack of sleep can have a significant impact on decision making, and perhaps we should avoid making big decisions like buying a house or getting married without a good night's sleep," says Professor Owen.
Why is this important?
We spend almost a third of our lives sleeping, and sleep is as important as the food and air we breathe.
However, the modern pace of life means that there is less and less time for sleep.
Yet, as noted in an article published in Nature Reviews Neuroscience, we have surprisingly little understanding of the effects of chronic lack of sleep on our brains.
The article discussed the dramatic decline in sleep duration in developed countries and the urgent need for more research.
And those volunteers who took part in the sleep study were a great help in finding important answers that our society and scientists alike need.
What Happens to the Brain at Night and Why Getting Good Sleep Is Even More Important Than You Thought
Health
In fact, the worst thing you can do for your body and in particular the brain is not to take sleep seriously. We are publishing an excerpt from the book of neuroscientist Mithu Storoni “No Stress. A Scientific Approach to Combating Anxiety, Depression and Burnout” about how to set your biological clock to the desired mode, to easily fall asleep and wake up.
Each of us has a slightly different brain in the morning compared to what it was yesterday. The rational brain controls behavior with expert precision, second by second, but only when we are awake. This polished system of actions stimulates a flurry of activity: new neural networks and synapses are formed. The longer we are awake, the longer we are in a state of intense activity and growth. But sooner or later the brain gets tired and needs a break. After a long trip, we take the car to the workshop for maintenance, washing and replacement of parts. Sleep is the same workshop for the body and an absolutely necessary measure. During sleep, the brain makes a kind of inventory. Neural connections and synapses are refined and strengthened, and all unnecessary is removed. Some memories are strengthened, others are weakened. And by the time we wake up, the brain looks very different. In a dream, "cleansing" also occurs. The brain is surrounded by an irrigation system known as the glymphatic system. With its help, the redistribution of useful substances and the removal of "waste" occur. Animal experiments have shown that the glymphatic system is more active during sleep than during wakefulness. Astrocytes - large stellate cells that stimulate the growth of brain cells and synapses - are also involved in its work and, if the brain is awake and active for a long time, they are redistributed. This sometimes leads to a slight swelling of the brain, which disappears after a good night's sleep.
After a long trip, we take the car to the workshop for maintenance, washing and replacement of parts. Sleep is the same workshop for the body and an absolutely necessary measure. During sleep, the brain makes a kind of inventory. Neural connections and synapses are refined and strengthened, and all unnecessary is removed. Some memories are strengthened, others are weakened. And by the time we wake up, the brain looks very different. In a dream, "cleansing" also occurs. The brain is surrounded by an irrigation system known as the glymphatic system. With its help, the redistribution of useful substances and the removal of "waste" occur. Animal experiments have shown that the glymphatic system is more active during sleep than during wakefulness. Astrocytes - large stellate cells that stimulate the growth of brain cells and synapses - are also involved in its work and, if the brain is awake and active for a long time, they are redistributed. This sometimes leads to a slight swelling of the brain, which disappears after a good night's sleep.
At night, the brain goes through a kind of inventory. And by the time we wake up, he looks completely different.
When we sleep, the brain goes through several stages. In the first stage, the eyes move rapidly from side to side - this is the REM sleep phase. The other stage is called slow sleep. All night long we shuttle between these two stages and other states as well. And the more a person is awake, the more his brain needs slow sleep. If you go to bed after a day of being awake, the period of non-REM sleep will increase. In depressed patients, non-REM sleep is shorter than usual, which explains the fact that symptoms of depression are temporarily relieved by staying up all night and falling asleep the next night.
Falling asleep and waking up
To continue the analogy of sleep with a car repair shop for the brain: the longer and more difficult the journey, the more the brain needs routine maintenance repairs. The longer you are awake, the longer the brain stays in a state of mental activity and the higher its need for sleep.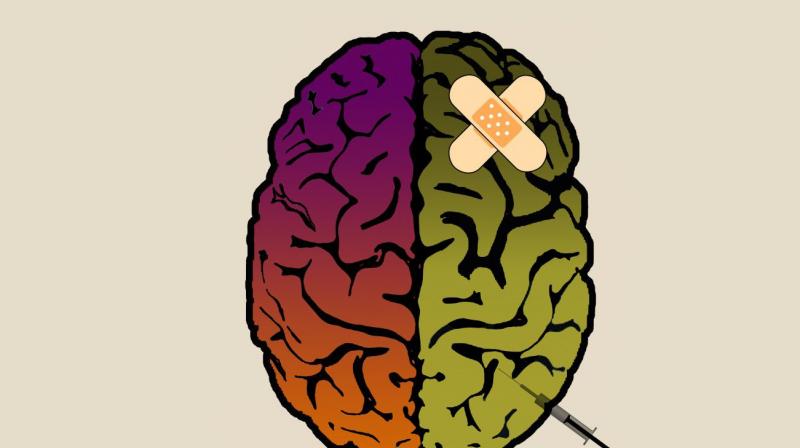 From the moment you wake up in the morning, your “sleep debt” begins to pile up. It is constantly increasing, and by the evening you can’t wait until you can pay. But there is one catch: the brain works in a 24-hour mode, and no matter how much "debt" you have accumulated, you will not be able to fall asleep at an unusual time for you. The biological clock is like a punctual guard who guards the gate to the country you are trying to enter - the world of wakefulness or the world of sleep. By the end of the evening, the “debt” accumulates and reminds of itself with poor health, but the inner guard will not let you into the land of sleep until the right time comes, from his “point of view”. And by about four in the morning you pay off your “debt”, but you are also not allowed to enter the country of wakefulness - the biological clock forces you to sleep for a few more hours.
From the moment you wake up in the morning, your “sleep debt” begins to pile up. It is constantly increasing, and by the evening you can’t wait until you can pay. But there is one catch: the brain works in a 24-hour mode, and no matter how much "debt" you have accumulated, you will not be able to fall asleep at an unusual time for you. The biological clock is like a punctual guard who guards the gate to the country you are trying to enter - the world of wakefulness or the world of sleep. By the end of the evening, the “debt” accumulates and reminds of itself with poor health, but the inner guard will not let you into the land of sleep until the right time comes, from his “point of view”. And by about four in the morning you pay off your “debt”, but you are also not allowed to enter the country of wakefulness - the biological clock forces you to sleep for a few more hours.
If you have accumulated a lot of "sleep debt" and your biological clock is out of balance, you will not fall asleep. If they work perfectly, but the “debt” has not yet accumulated (for example, you took a nap during the day), you will also not be able to sleep. To ensure a sound night's sleep, you need to take care of your biological clock.
If they work perfectly, but the “debt” has not yet accumulated (for example, you took a nap during the day), you will also not be able to sleep. To ensure a sound night's sleep, you need to take care of your biological clock.
What is actually a biological clock
In fact, there are many clocks in our body. There are thousands of them! The cells of the heart tissue have their own clock, the cells of the liver and intestines have their own. Each part of the brain has its own clock and rhythm. But the main, central clock is located in an area called the suprachiasmatic nucleus. Like the conductor of an orchestra, they control the rest of the peripheral clocks, synchronizing them, and then they show the same time.
Chronic stress disrupts the biological clock and circadian rhythms. In addition, disrupting the daily rhythms, we are more prone to stress. The central clock synchronizes the peripheral ones by sending neural and hormonal signals.
One of these signals is cortisol. If your cortisol levels go through the roof during chronic stress, your biological clock is disrupted. A healthy body produces this hormone in a natural rhythm, corresponding to daily rhythms. A small release of cortisol occurs in the morning, and at night its production stops. When circadian rhythms fail, the normal fluctuation of cortisol levels and the function of the HPA system are interrupted, which negatively affects our perception of stress.
If your cortisol levels go through the roof during chronic stress, your biological clock is disrupted. A healthy body produces this hormone in a natural rhythm, corresponding to daily rhythms. A small release of cortisol occurs in the morning, and at night its production stops. When circadian rhythms fail, the normal fluctuation of cortisol levels and the function of the HPA system are interrupted, which negatively affects our perception of stress.
There is a theory that chronic stress disrupts the body clock, causing depression and other mood disorders. Any activity that alters the normal rhythm of cortisol production disrupts the circadian rhythm. It can be physical activity (intense training), emotional manifestations (arousal, anger), food (coffee) - anything that leads to an increase in cortisol levels.
And here melatonin
Melatonin is sometimes called the hormone of darkness. It is produced by the pineal gland (pineal gland). In the absence of bright blue light, your master clock, the suprachiasmatic nucleus, tells the pineal gland to produce more melatonin. Figuratively speaking, the master clock communicates with the rest of the body through melatonin - it is distributed throughout the bloodstream and instructs the peripheral clock to work smoothly. According to recent research, melatonin also has anti-inflammatory and antioxidant properties.
Figuratively speaking, the master clock communicates with the rest of the body through melatonin - it is distributed throughout the bloodstream and instructs the peripheral clock to work smoothly. According to recent research, melatonin also has anti-inflammatory and antioxidant properties.
The production of melatonin at night dulls the stress response. The possibility of using this hormone to treat patients prone to high blood pressure at night is being studied: there is a theory that pressure fluctuations are associated with excessive activity. Melatonin reduces the sympathetic response to psychological stress. Early animal data suggest that melatonin protects the brain from the effects of chronic stress.
A study has shown that agomelatine (a melatonin receptor stimulant) reverses many of the effects of chronic, shock, and mild stress in male mice, including changes in behavior and the hippocampus. But not only the active production of melatonin at night is important. Scientists are working on a theory that its increased production in the morning causes manifestations of depression, despite the fact that at night it helps to cope with its symptoms.
Scientists are working on a theory that its increased production in the morning causes manifestations of depression, despite the fact that at night it helps to cope with its symptoms.
Melatonin and the internal clock must work together. Let's look at how to achieve this.
Adjusting the biological clock
Chronic stress destabilizes the normal functioning of the biological clock, and disturbed sleep patterns and circadian biorhythms increase chronic stress. It turns out a vicious circle. Do your best to adjust your biological clock and you will be able to mitigate the effects of chronic stress. Four aspects of lifestyle affect biorhythms: light, nutrition, physical activity, and temperature. Everything that excites and sharpens perception also affects the biological clock. Light, nutrition, physical activity, and increased body temperature are all related to the waking state.
Optimal daily routine
Morning
- Wake up and immediately open all the curtains, exposing yourself to the bright morning light.
- Have a hearty breakfast at the same time every day.
- After breakfast, stay in bright daylight for at least 30 minutes.
Day
- At least three times a day, try to be in bright daylight: after breakfast; at lunch; in the period from 16 to 18 hours.
- Do sports in the morning. If this is not possible, schedule a workout for 16-18 hours, no later.
Evening
- Eat dinner as early as possible. Dinner should be light.
- Wear blue-blocking glasses.
- Use a program that reduces blue light from a computer screen (for example, f.lux).
- Dim the lights.
- After dimming the light, stop eating!
- Avoid intense exercise and physical activity.
- Avoid noise. Do not turn on the TV at high volume.
- Avoid stimulating influences.
- Do not go to social networks and do not look at "posts" and channels that cause you anger and negative reactions.
- Avoid caffeine and alcohol.
Before going to bed
- Switch off all electronic devices.
- Read a paper book.
- Take a warm bath.
- Keep your bedroom cool, but keep your feet warm.
How to set the biological clock back to stay awake longer
— In the evening, turn on the bright light.
- Go in for sports. The optimal time is two to three hours before the estimated time of falling asleep.
- Don't get cold. Keep your body warm—everything but your feet!
- Have a cup of coffee in the evening.
Night shift advice
If you work the night shift and want to switch between day and night, put on blue-blocking glasses in the morning and try to wear them during the day. Remove in the evening.
The heaviest meal should be at the time when you have "morning" (this moment can be programmed). "Breakfast" should be preceded by an 8-10 hour fast.
How to set the biological clock forward to fall asleep earlier
- Dim the lights before going to bed and block out the blue spectrum.
- If you watch movies on an airplane or work at a computer all night, wear blue-blocking glasses.
- Wake up an hour or two earlier than usual and immediately open the curtains to see the sunlight, or turn on bright artificial lighting.
- Have breakfast earlier than usual.
- Actively play sports to get tired faster and accumulate "debt on sleep." Do not exercise later than three hours before the expected time of falling asleep.
- Go to bed in a cool, well-ventilated room to cool your body, but keep your feet warm by wearing warm socks or covering them with a blanket. Take a warm bath before bed.
- Do not abuse caffeine.
How to overcome afternoon sleepiness
After dinner, we often want to take a nap. However, afternoon naps can reduce mental efficiency and impair cognitive flexibility. Numerous studies have been devoted to the study of ways to get rid of afternoon sleepiness. Drowsiness is experienced even by those who have had a good night's sleep and generally do not lack sleep. Scientists have come to several important conclusions.
Scientists have come to several important conclusions.
Blue light or bright daylight
Just half an hour in bright daylight after dinner reduces sleepiness. In one experiment, participants were exposed to artificial lighting enriched with blue light in the afternoon. It turned out that in such conditions, perception remains sharp, and mental performance improves.
Short afternoon nap
If possible, indulge in a short afternoon nap. But keep in mind that its duration should be no more than 15 minutes. Forty-five minutes of sleep greatly activates the parasympathetic system. But after a 15-minute sleep, the participants in the experiments showed slightly higher results when passing a cognitive test. If the work involves the use of complex analytical skills, even after a short sleep, it will take a little time to restore a high level of concentration. But in general, a 15-minute afternoon nap will improve your performance and mood.