Bipolar with psychosis vs schizophrenia
How to tell the difference
Bipolar disorder and schizophrenia are mental health conditions that have some common traits and some key differences. Bipolar disorder causes shifts in mood, energy level, and thinking. Schizophrenia causes a person to appear to lose touch with reality.
People with bipolar disorder may experience episodes of mania and depression, often with periods of relative stability occurring in between.
Individuals with schizophrenia experience symptoms of psychosis, such as hallucinations or delusions. Some people with bipolar disorder also experience symptoms of psychosis.
Because of the overlap in symptoms, getting the right diagnosis can be challenging. Also, a person can have both schizophrenia and bipolar disorder, which can complicate diagnosis.
Some people have schizoaffective disorder, which involves a combination of schizophrenia symptoms and mood disorder symptoms.
In this article, we look at the similarities and differences between bipolar disorder and schizophrenia. We also discuss methods of diagnosis and options for treatment.
The symptoms of bipolar disorder and schizophrenia vary and can differ in type and severity.
They may get worse and then significantly improve or go into remission for a period of time.
People with bipolar disorder frequently experience extremes in mood. Healthcare professionals may classify “highs” as mania or, in less severe cases, hypomania. “Lows” involve a decrease in mood and, often, depression.
There are three main types of bipolar disorder, although some people have a different arrangement of symptoms:
- Bipolar I: The most intense type. It features episodes of mania and, often, depression that can last at least 1 or 2 weeks at a time. In some cases, a person can experience both states simultaneously.
- Bipolar II: This slightly less intense form involves major depression that can last for weeks, as well as bouts of hypomania that may last several days or more.
 The two may alternate rapidly or have stretches of time in between them.
The two may alternate rapidly or have stretches of time in between them. - Cyclothymia: This features alternating periods of lower grade depression and hypomania that can last weeks. It may also involve emotional dysregulation and anxious, impulsive, reactive behavior, according to a 2017 review. Mood changes are less dramatic but are never stable for more than 2 months.
All three conditions may include periods of stability.
Symptoms of mania
Mania can involve:
- irritability
- difficulty sleeping or less need for sleep
- excessive energy and restlessness
- high self-esteem
- expansive mood
- inability to concentrate or make decisions
- increased engagement in pleasurable activities, such as sexual activity or drug use
- intense excitement
- racing thoughts
- reckless behavior, such as overspending
In a person with bipolar I or II, depressive symptoms are the same as those in major depressive disorder.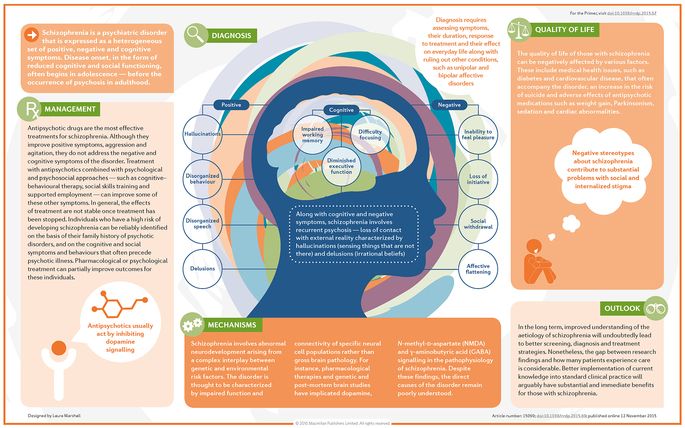
Symptoms of depression
The primary symptom of depression is a feeling of either sadness or hopelessness that persists for 2 weeks or longer. But depression can also cause a significant loss of interest or pleasure in most daily activities.
Other symptoms include:
- changes in appetite
- changes in sleep habits
- fatigue and low energy
- low self-esteem
- physical aches and pains without an apparent cause
- suicidal thoughts or behaviors
Bipolar disorder can also present with anxiety or episodes of psychosis, during which a person loses touch with reality.
When people display symptoms of psychosis, healthcare professionals may be unsure whether they have a type of bipolar disorder or schizophrenia.
Schizophrenia symptoms affect a person’s thoughts, emotions, and behaviors. They include:
Delusions
These are false beliefs, and most people with schizophrenia experience them.
For example, people may think that they are famous or special in a certain way, that they are being harassed or stalked, or that something terrible is about to happen.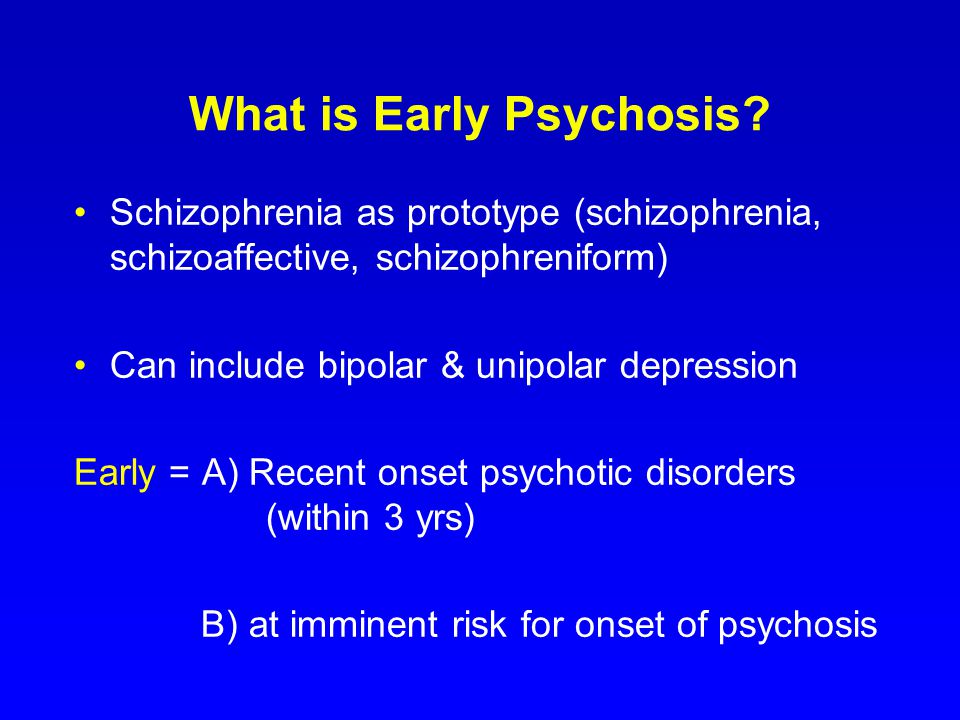
Hallucinations
During a hallucination, people see, hear, feel, taste, or smell things that are not there. The most common type of hallucination involves hearing voices.
Disorganized thinking and speech
People exhibiting these symptoms may not make sense when communicating with others. They may give unrelated answers to questions, or their sentences may seem meaningless to the people around them.
Unusual behavior
People with schizophrenia can demonstrate unpredictable behavior. For example, they may act childlike, assume strange postures, or move constantly.
Inability to function as usual
Schizophrenia can affect a person’s ability to take care of their personal hygiene, engage with others in socially acceptable ways, or perform everyday activities.
The following symptoms may occur in either bipolar disorder or schizophrenia:
Episodes of psychosis
For some people with bipolar disorder, an episode of mania or depression can give rise to hallucinations or delusions.
Disorganized thinking
This is common among people living with schizophrenia, but people with bipolar disorder may also seem to have disorganized thoughts. During episodes of mania, a person may have difficulty concentrating on a single idea or task.
Symptoms of depression
During periods of depression, people with either condition may demonstrate a loss of interest in things they once enjoyed. Some people may feel like they cannot experience pleasure or may have trouble concentrating or making decisions.
Some researchers report high rates of drug and alcohol misuse among people with schizophrenia, bipolar disorder, or depression.
If a person has significant symptom overlap, they may receive a diagnosis of schizoaffective disorder, a related but separate mental health condition.
Bipolar disorder is more common than schizophrenia.
Bipolar disorder affected about 40 million people worldwide in 2019, while 24 million people — about 1 in 300 adults — were living with schizophrenia at that time.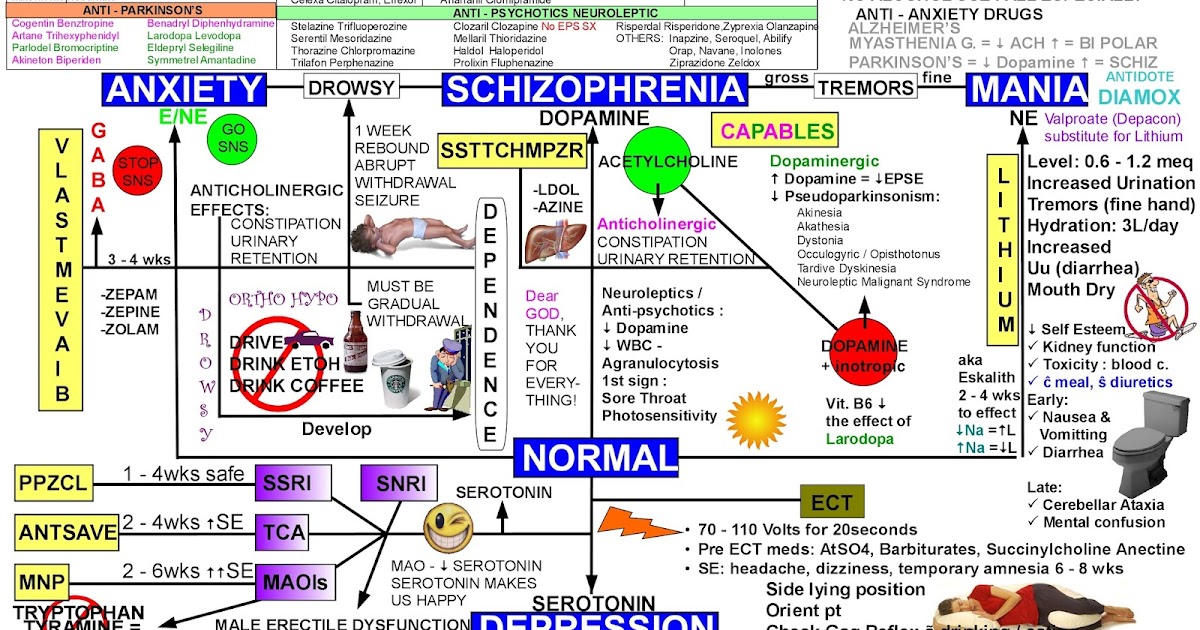
Statistics from the National Institute of Mental Health (NIMH) suggest that approximately 2.8% of U.S. adults experience bipolar disorder in a given year and 4.4% experience it at some point in their lives. Among those, 82.9% have serious impairment due to their symptoms and 17.1% have moderate impairment.
Symptoms of bipolar disorder usually start to appear around age 25, and the condition affects males and females equally.
The NIMH notes that it is difficult to know precisely how many people live with schizophrenia because the diagnosis is complex and symptoms overlap with those of other conditions. In addition, diagnostic criteria vary. Some figures suggest that schizophrenia affects less than 1% of the U.S. population, while advocacy groups say it could be 1.6% or more.
Symptoms typically appear from late adolescence to the early 20s in males and in the late 20s to mid-30s in females.
The experience and likelihood of having bipolar disorder or schizophrenia can vary depending on factors such as a person’s family history and race or ethnicity.
Family history
Having a family member with bipolar disorder or schizophrenia does not mean that someone will definitely have the same diagnosis.
Experts do not know precisely what causes these conditions, but researchers have pinpointed a number of genetic variants in people with these diagnoses. The odds of having either condition increase when a parent or sibling has it.
Brain structure, environment, lifestyle, trauma, and other stressors may further influence the development and intensity of these conditions.
Race and ethnicity
Research suggests that Black Americans receive diagnoses of schizophrenia at up to four or five times the rate that white Americans do. Among Latino American or Hispanic Americans, diagnosis rates are up to three times as high as those of white Americans.
One small 2010 study found that Asian and Latino individuals were more likely to receive a diagnosis of bipolar I disorder than white individuals.
Researchers are not exactly sure why this occurs, but some have suggested that trauma, stress, or marginalization may contribute to the emergence of such conditions.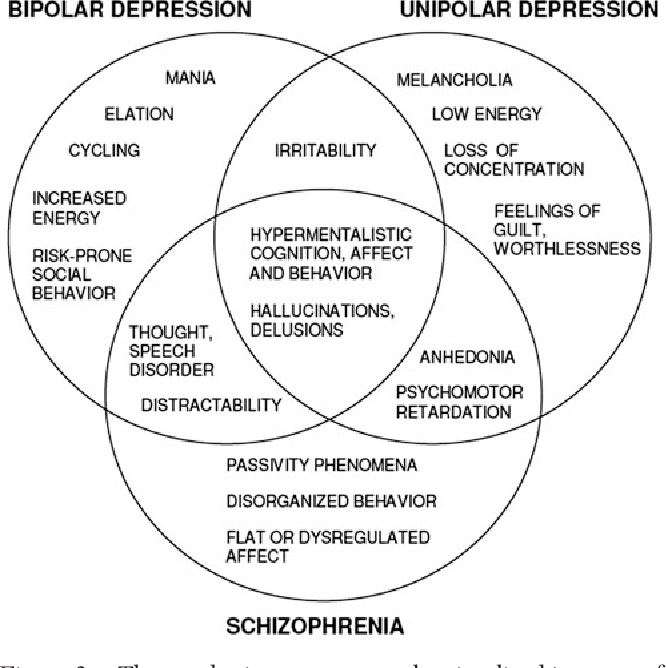
However, other experts say that there is no difference in the prevalence of bipolar disorder and schizophrenia among those of different racial or ethnic backgrounds. Instead, people may receive a misdiagnosis of a more severe condition when health professionals are biased or unable or unwilling to make an accurate diagnosis.
For example, a Black American may receive a diagnosis of schizophrenia when their symptoms more closely represent major depression or the mania associated with bipolar I disorder. Healthcare disparities among People of Color can amplify these issues and lead to insufficient diagnosis and treatment.
Following strict diagnostic criteria can help health professionals determine whether a person has a particular condition. Broader clinical training can help reduce ethnocentric bias.
Medical professionals use the same procedures to diagnose bipolar disorder and schizophrenia. The process typically involves:
A physical examination
This helps determine whether medical problems are causing psychological symptoms.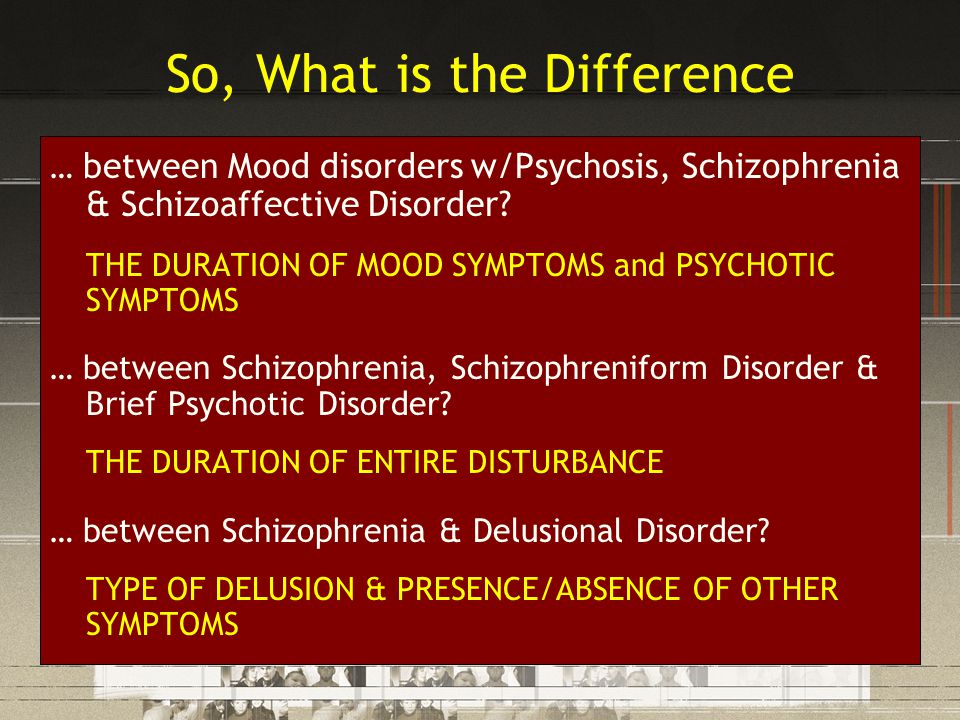 It can include:
It can include:
- blood tests
- MRI or CT scans of the brain
- drug and alcohol screenings
A psychological evaluation
Healthcare professionals — usually psychiatrists — look for signs and symptoms of bipolar disorder and schizophrenia, examining anything that affects a person’s thoughts, emotions, and behaviors.
They may ask a person about their personal and family mental health history and have them complete a psychological self-assessment form.
During this evaluation, healthcare professionals will closely observe the person’s appearance and actions.
They will then compare the person’s symptoms with the criteria in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, 5th edition, text revision (DSM-5-TR).
Diary of symptoms and moods
People who may be experiencing schizophrenia or bipolar disorder may wish to keep a daily diary of their thoughts, moods, and sleep habits.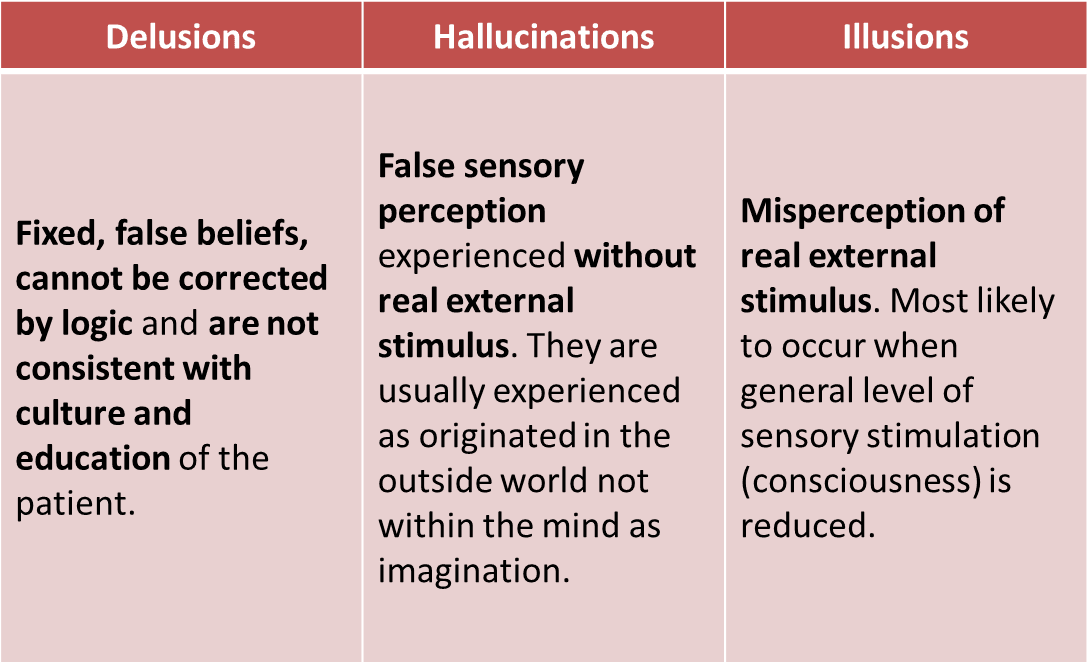 Healthcare professionals can use this to identify patterns in their behavior and to spot other clues that inform diagnosis and treatment.
Healthcare professionals can use this to identify patterns in their behavior and to spot other clues that inform diagnosis and treatment.
What are the criteria?
Here are some features that can help distinguish the different types of bipolar disorder:
- Bipolar I: at least one episode of mania
- Bipolar II: hypomania with a major depressive episode
- Cyclothymia: episodes of low level depression and hypomania that occur at least half the time over 2 years or longer
The criteria for schizophrenia vary, but according to the DSM-5-TR, a person may receive a diagnosis of schizophrenia if they have two or more of the following for a significant amount of time during a single month:
- delusions
- hallucinations
- disorganized speech
- grossly disorganized or catatonic behavior
- negative symptoms, such as reduced speech or lack of motivation
- social or occupational dysfunction lasting at least 6 months, including at least 1 month of symptoms
A doctor also needs to ensure that a person’s symptoms are not due to any other condition.
Both conditions require lifelong treatment.
Treatment for bipolar disorder
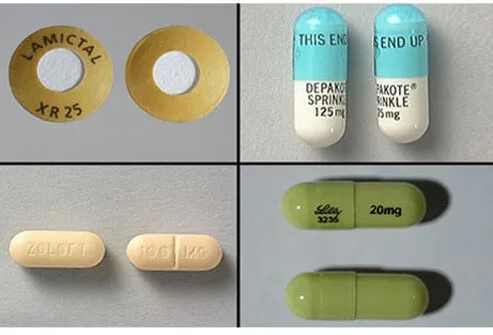
Many people with bipolar disorder require medication to stabilize their moods.
This can include:
- lithium, a mood stabilizer that may help prevent relapse and manage symptoms
- atypical antipsychotics
- anticonvulsants
Psychotherapy is an important part of bipolar disorder management. It may take place individually or in a group or family setting.
Therapy can help people manage their thoughts and emotions, establish routines, and identify triggers.
Those whose condition does not respond to medications or psychotherapy may benefit from electroconvulsive therapy (ECT). The goal of this treatment is to change the brain’s chemistry by sending electrical currents through it, causing a seizure.
Other strategies that can help people with bipolar disorder include:
- avoiding alcohol and drugs
- eating a balanced diet
- exercising regularly
- getting enough sleep
- managing stress
- seeking help and support from family, friends, and others
Bipolar disorder can vary widely, and the symptoms can change over time. A doctor will tailor treatment to suit the individual and may change the approach over time.
Treatment for schizophrenia
Antipsychotic medications are a vital part of treatment for most people with schizophrenia. Healthcare professionals believe that these medications change the brain’s chemistry and reduce symptoms such as hallucinations and delusions.
Some individuals require other medicines, such as antidepressants or antianxiety drugs. Some doctors may also use ECT to improve symptoms of psychosis.
When the person is able to manage the symptoms of psychosis, they can often benefit from psychological and social interventions, which may include:
- psychotherapy in both individual and family settings
- social or behavioral skills training to improve interactions with others
- employment support to help them secure or perform a job more easily
- daily living support to help them find housing and manage daily responsibilities
Other coping strategies include:
- avoiding alcohol and drug use
- joining a support group
- learning about schizophrenia
- maintaining certain lifestyle habits, such as eating a balanced diet, exercising, and following a sleep schedule
- managing stress through strategies such as meditation, exercise, and yoga
- seeking help from family and friends
Although bipolar disorder and schizophrenia have similarities, they also have key differences, especially when it comes to symptom severity and treatment.
People with bipolar disorder generally alternate between periods of high and low moods, while people with schizophrenia typically lose touch with reality as they experience hallucinations and delusions.
With treatment, a person who has either condition can manage their symptoms and reduce the condition’s impact on their life.
Bipolar disorder is typically more manageable after a person receives appropriate treatment. Schizophrenia is more challenging to treat, and people who have it tend to need greater support.
How to tell the difference
Bipolar disorder and schizophrenia are mental health conditions that have some common traits and some key differences. Bipolar disorder causes shifts in mood, energy level, and thinking. Schizophrenia causes a person to appear to lose touch with reality.
People with bipolar disorder may experience episodes of mania and depression, often with periods of relative stability occurring in between.
Individuals with schizophrenia experience symptoms of psychosis, such as hallucinations or delusions. Some people with bipolar disorder also experience symptoms of psychosis.
Because of the overlap in symptoms, getting the right diagnosis can be challenging. Also, a person can have both schizophrenia and bipolar disorder, which can complicate diagnosis.
Some people have schizoaffective disorder, which involves a combination of schizophrenia symptoms and mood disorder symptoms.
In this article, we look at the similarities and differences between bipolar disorder and schizophrenia. We also discuss methods of diagnosis and options for treatment.
The symptoms of bipolar disorder and schizophrenia vary and can differ in type and severity.
They may get worse and then significantly improve or go into remission for a period of time.
People with bipolar disorder frequently experience extremes in mood. Healthcare professionals may classify “highs” as mania or, in less severe cases, hypomania. “Lows” involve a decrease in mood and, often, depression.
There are three main types of bipolar disorder, although some people have a different arrangement of symptoms:
- Bipolar I: The most intense type.
It features episodes of mania and, often, depression that can last at least 1 or 2 weeks at a time. In some cases, a person can experience both states simultaneously.
- Bipolar II: This slightly less intense form involves major depression that can last for weeks, as well as bouts of hypomania that may last several days or more. The two may alternate rapidly or have stretches of time in between them.
- Cyclothymia: This features alternating periods of lower grade depression and hypomania that can last weeks. It may also involve emotional dysregulation and anxious, impulsive, reactive behavior, according to a 2017 review. Mood changes are less dramatic but are never stable for more than 2 months.
All three conditions may include periods of stability.
Symptoms of mania
Mania can involve:
- irritability
- difficulty sleeping or less need for sleep
- excessive energy and restlessness
- high self-esteem
- expansive mood
- inability to concentrate or make decisions
- increased engagement in pleasurable activities, such as sexual activity or drug use
- intense excitement
- racing thoughts
- reckless behavior, such as overspending
In a person with bipolar I or II, depressive symptoms are the same as those in major depressive disorder.
Symptoms of depression
The primary symptom of depression is a feeling of either sadness or hopelessness that persists for 2 weeks or longer. But depression can also cause a significant loss of interest or pleasure in most daily activities.
Other symptoms include:
- changes in appetite
- changes in sleep habits
- fatigue and low energy
- low self-esteem
- physical aches and pains without an apparent cause
- suicidal thoughts or behaviors
Bipolar disorder can also present with anxiety or episodes of psychosis, during which a person loses touch with reality.
When people display symptoms of psychosis, healthcare professionals may be unsure whether they have a type of bipolar disorder or schizophrenia.
Schizophrenia symptoms affect a person’s thoughts, emotions, and behaviors. They include:
Delusions
These are false beliefs, and most people with schizophrenia experience them.
For example, people may think that they are famous or special in a certain way, that they are being harassed or stalked, or that something terrible is about to happen.
Hallucinations
During a hallucination, people see, hear, feel, taste, or smell things that are not there. The most common type of hallucination involves hearing voices.
Disorganized thinking and speech
People exhibiting these symptoms may not make sense when communicating with others. They may give unrelated answers to questions, or their sentences may seem meaningless to the people around them.
Unusual behavior
People with schizophrenia can demonstrate unpredictable behavior. For example, they may act childlike, assume strange postures, or move constantly.
Inability to function as usual
Schizophrenia can affect a person’s ability to take care of their personal hygiene, engage with others in socially acceptable ways, or perform everyday activities.
The following symptoms may occur in either bipolar disorder or schizophrenia:
Episodes of psychosis
For some people with bipolar disorder, an episode of mania or depression can give rise to hallucinations or delusions.
Disorganized thinking
This is common among people living with schizophrenia, but people with bipolar disorder may also seem to have disorganized thoughts. During episodes of mania, a person may have difficulty concentrating on a single idea or task.
Symptoms of depression
During periods of depression, people with either condition may demonstrate a loss of interest in things they once enjoyed. Some people may feel like they cannot experience pleasure or may have trouble concentrating or making decisions.
Some researchers report high rates of drug and alcohol misuse among people with schizophrenia, bipolar disorder, or depression.
If a person has significant symptom overlap, they may receive a diagnosis of schizoaffective disorder, a related but separate mental health condition.
Bipolar disorder is more common than schizophrenia.
Bipolar disorder affected about 40 million people worldwide in 2019, while 24 million people — about 1 in 300 adults — were living with schizophrenia at that time.
Statistics from the National Institute of Mental Health (NIMH) suggest that approximately 2.8% of U.S. adults experience bipolar disorder in a given year and 4.4% experience it at some point in their lives. Among those, 82.9% have serious impairment due to their symptoms and 17.1% have moderate impairment.
Symptoms of bipolar disorder usually start to appear around age 25, and the condition affects males and females equally.
The NIMH notes that it is difficult to know precisely how many people live with schizophrenia because the diagnosis is complex and symptoms overlap with those of other conditions. In addition, diagnostic criteria vary. Some figures suggest that schizophrenia affects less than 1% of the U.S. population, while advocacy groups say it could be 1.6% or more.
Symptoms typically appear from late adolescence to the early 20s in males and in the late 20s to mid-30s in females.
The experience and likelihood of having bipolar disorder or schizophrenia can vary depending on factors such as a person’s family history and race or ethnicity.
Family history
Having a family member with bipolar disorder or schizophrenia does not mean that someone will definitely have the same diagnosis.
Experts do not know precisely what causes these conditions, but researchers have pinpointed a number of genetic variants in people with these diagnoses. The odds of having either condition increase when a parent or sibling has it.
Brain structure, environment, lifestyle, trauma, and other stressors may further influence the development and intensity of these conditions.
Race and ethnicity
Research suggests that Black Americans receive diagnoses of schizophrenia at up to four or five times the rate that white Americans do. Among Latino American or Hispanic Americans, diagnosis rates are up to three times as high as those of white Americans.
One small 2010 study found that Asian and Latino individuals were more likely to receive a diagnosis of bipolar I disorder than white individuals.
Researchers are not exactly sure why this occurs, but some have suggested that trauma, stress, or marginalization may contribute to the emergence of such conditions.
However, other experts say that there is no difference in the prevalence of bipolar disorder and schizophrenia among those of different racial or ethnic backgrounds. Instead, people may receive a misdiagnosis of a more severe condition when health professionals are biased or unable or unwilling to make an accurate diagnosis.
For example, a Black American may receive a diagnosis of schizophrenia when their symptoms more closely represent major depression or the mania associated with bipolar I disorder. Healthcare disparities among People of Color can amplify these issues and lead to insufficient diagnosis and treatment.
Following strict diagnostic criteria can help health professionals determine whether a person has a particular condition. Broader clinical training can help reduce ethnocentric bias.
Medical professionals use the same procedures to diagnose bipolar disorder and schizophrenia. The process typically involves:
A physical examination
This helps determine whether medical problems are causing psychological symptoms. It can include:
- blood tests
- MRI or CT scans of the brain
- drug and alcohol screenings
A psychological evaluation
Healthcare professionals — usually psychiatrists — look for signs and symptoms of bipolar disorder and schizophrenia, examining anything that affects a person’s thoughts, emotions, and behaviors.
They may ask a person about their personal and family mental health history and have them complete a psychological self-assessment form.
During this evaluation, healthcare professionals will closely observe the person’s appearance and actions.
They will then compare the person’s symptoms with the criteria in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, 5th edition, text revision (DSM-5-TR).
Diary of symptoms and moods
People who may be experiencing schizophrenia or bipolar disorder may wish to keep a daily diary of their thoughts, moods, and sleep habits. Healthcare professionals can use this to identify patterns in their behavior and to spot other clues that inform diagnosis and treatment.
What are the criteria?
Here are some features that can help distinguish the different types of bipolar disorder:
- Bipolar I: at least one episode of mania
- Bipolar II: hypomania with a major depressive episode
- Cyclothymia: episodes of low level depression and hypomania that occur at least half the time over 2 years or longer
The criteria for schizophrenia vary, but according to the DSM-5-TR, a person may receive a diagnosis of schizophrenia if they have two or more of the following for a significant amount of time during a single month:
- delusions
- hallucinations
- disorganized speech
- grossly disorganized or catatonic behavior
- negative symptoms, such as reduced speech or lack of motivation
- social or occupational dysfunction lasting at least 6 months, including at least 1 month of symptoms
A doctor also needs to ensure that a person’s symptoms are not due to any other condition.
Both conditions require lifelong treatment.
Treatment for bipolar disorder
Many people with bipolar disorder require medication to stabilize their moods.
This can include:
- lithium, a mood stabilizer that may help prevent relapse and manage symptoms
- atypical antipsychotics
- anticonvulsants
Psychotherapy is an important part of bipolar disorder management. It may take place individually or in a group or family setting.
Therapy can help people manage their thoughts and emotions, establish routines, and identify triggers.
Those whose condition does not respond to medications or psychotherapy may benefit from electroconvulsive therapy (ECT). The goal of this treatment is to change the brain’s chemistry by sending electrical currents through it, causing a seizure.
Other strategies that can help people with bipolar disorder include:
- avoiding alcohol and drugs
- eating a balanced diet
- exercising regularly
- getting enough sleep
- managing stress
- seeking help and support from family, friends, and others
Bipolar disorder can vary widely, and the symptoms can change over time. A doctor will tailor treatment to suit the individual and may change the approach over time.
Treatment for schizophrenia
Antipsychotic medications are a vital part of treatment for most people with schizophrenia. Healthcare professionals believe that these medications change the brain’s chemistry and reduce symptoms such as hallucinations and delusions.
Some individuals require other medicines, such as antidepressants or antianxiety drugs. Some doctors may also use ECT to improve symptoms of psychosis.
When the person is able to manage the symptoms of psychosis, they can often benefit from psychological and social interventions, which may include:
- psychotherapy in both individual and family settings
- social or behavioral skills training to improve interactions with others
- employment support to help them secure or perform a job more easily
- daily living support to help them find housing and manage daily responsibilities
Other coping strategies include:
- avoiding alcohol and drug use
- joining a support group
- learning about schizophrenia
- maintaining certain lifestyle habits, such as eating a balanced diet, exercising, and following a sleep schedule
- managing stress through strategies such as meditation, exercise, and yoga
- seeking help from family and friends
Although bipolar disorder and schizophrenia have similarities, they also have key differences, especially when it comes to symptom severity and treatment.
People with bipolar disorder generally alternate between periods of high and low moods, while people with schizophrenia typically lose touch with reality as they experience hallucinations and delusions.
With treatment, a person who has either condition can manage their symptoms and reduce the condition’s impact on their life.
Bipolar disorder is typically more manageable after a person receives appropriate treatment. Schizophrenia is more challenging to treat, and people who have it tend to need greater support.
“I need help” How do people with schizophrenia and bipolar disorder fight not only the disease, but also prejudice? . About how people with such serious diagnoses as schizophrenia and bipolar disorder cope with their problems and why society needs to change its attitude towards them - in the material "Lenta.ru".
Every tenth person on the planet suffers from various kinds of mental disorders, according to the World Health Organization (WHO). At the same time, mental disorders are among the top diseases leading to disability. The overall unfavorable statistics was exacerbated by the pandemic: self-isolation and quarantine measures, according to experts, often provoke exacerbations and relapses in such patients. In Russia, 5.6 million citizens need medical care due to mental disorders.
Each of them fights not only with the disease, but also with prejudices widespread in society. This is especially true for people with mental disorders such as schizophrenia and bipolar affective disorder (BAD). Most often, without proper attention, diseases of this type proceed chronically, with rare episodes of remission. Without professional medical care, life turns into existence: the disease leads to another reality, does not let go, cripples, deprives the future.
Photo: Shutterstock
Diagnosis is not a sentence
More than 21 million people worldwide have been diagnosed with schizophrenia, and 1.5-6.5 percent of the world's population suffers from bipolar disorder.
In Russia, every fifth person has friends with a diagnosis of schizophrenia in his environment, every tenth person personally knows a carrier of bipolar affective disorder (BAD): among acquaintances (5 percent), among relatives (3 percent). Such figures were shown by a survey of the All-Russian Public Opinion Research Center (VTsIOM) and the pharmaceutical company Gedeon Richter, which since 2019initiates social projects aimed at changing the attitude of society towards patients with mental illness.
At the same time, such diagnoses are a stigma that hinders social adaptation. It should be recognized that in the Russian Federation, public consciousness has been formed in such a way that it is customary to stay away from people with mental illness.
Research by VTsIOM and Gedeon Richter confirms the importance of overcoming the stereotypes that have developed in society. Mental health is just as important to maintain as physical health. Sensitivity to those who have lost it helps to ensure conditions for the acceptance of people with mental disorders in society. Attitudes toward people with illnesses such as schizophrenia and bipolar disorder are ultimately an indicator of the mental health of society as a whole
“Bipolar disorder is about me”
Maria from Moscow has been living with an official diagnosis of bipolar affective disorder for 4 of her 28 years. The most difficult thing for her was to explain to her relatives that bipolar disorder is the same disease as, for example, diabetes, and that its manifestations such as apathy, indifference to everything and everyone, or, conversely, bright flashes of violent activity, are not a consequence of a complex nature.
“I knew about my problems when I was in college, but I didn't attach any importance to them. However, the euphoria rolling in waves and the depression that followed it, up to thoughts of suicide, exhausted me more and more. I was sucked into a funnel of fear, I did not want to live, I could no longer cope. I needed help, and I ended up with a specialist. I found out that bipolar disorder is about me, I am sick, but it is being treated, ”says Maria.
People with bipolar disorder, which is a chronic illness, are characterized by alternating phases of ups and downs, explains the head of the psychological center, Viktoria Zhadenova. “During a manic episode, people with bipolar disorder are very productive, creative, ready to burn at work, gushing with ideas, forgetting to eat and sleep in a series of work tasks. However, such a rise is followed by a decline phase, and no one knows how long it will last, ”explains the expert. According to her, patients with bipolar disorder during a depressive episode, as a rule, are physically unable to do anything.
People who are aware of their diagnosis arrange the rhythm of life in such a way that their work does not suffer at the moment when they need a break. If colleagues do not know about such a feature of health, then it is difficult for them to understand the motivation of such a person. “Phases can last from a few days to several months. Living on a roller coaster is challenging for both the bipolar patient and those around them. At the moment of recession, a person becomes asocial,” comments V. Zhadenova.
According to Maria, it took her years to accept herself, her illness, and the fact that her symptoms could return if she didn't follow the advice of a specialist. “At the initial stage of treatment, I seemed to be looking at myself from the outside: this is not about me, this is a strange dream. As soon as I got out of a difficult condition, with which I got to a specialist, I immediately forgot about all the recommendations. It was a mistake,” Maria admits. Now, according to her, she has learned to listen to herself: she does not deny her problems, but she was able to muffle her feelings of guilt. “I'm still in therapy. Medications and a strict regimen help me stop the symptoms, thanks to them I gained control over my life, ”says Maria.
“I heard other people's thoughts”
Victor M. realized that he was not like everyone else when he was 16. “I realized that I hear people's thoughts, it didn't bother me, it was even funny. I was the chosen one. I rode the tram to study, and there was a buzz of other people's thoughts around, ”says Viktor. But after a few years, he could not only go to the subway or a store, but was afraid to cross the threshold of the apartment: according to him, his superpowers were of interest to the special services, he was afraid of abduction and experiments that he could be subjected to because of "exclusivity and gift" . Victor was under the supervision of specialists after he went live on the social network and smashed the furniture in the apartment. He was diagnosed with paranoid schizophrenia. To recover, Victor needed several hospitalizations, the selection of an effective drug treatment regimen and control by his mother, who makes sure that he does not miss medication. The young man lives an active life: he returned from the sanatorium, where he restored his health, goes in for sports, meets friends.
“Schizophrenia is characterized by significant disturbances in the perception of reality and behavioral changes. Patients live in their own world: they are characterized by hallucinations, delusions, paranoia, disorganized thinking. The first alarm bells in men, as a rule, appear at the age of 18-25. In women, the disease is usually diagnosed at 25-30 years old, ”explains Victoria Zhadenova.
The diagnosis of schizophrenia is frightening and seems irreparable. However, as experts note, effective therapy, drug support and care from the environment allow such patients to live a full life, in which there is a place for social activity.
“I'm not happy with the restrictions that have come into my life since my diagnosis. For example, I won't be able to drive a car. However, after the last hospitalization, I realized how much I want to go home, I want to do my daily routine - go for a morning run or cook lunch. Now I am in a long-term remission, although I continue constant maintenance drug therapy, ”said Victor. Thanks to modern developments in the pharmaceutical industry for patients with schizophrenia, as in the case of Victor, it is possible to achieve a stable state of mind, prevent relapse and delay a possible attack of psychosis as much as possible.
On the way to remission
Patients like Anna and Victor do not pose a danger to others, but they make them want to keep their distance. People with mental disorders face many challenges every day. They do not have the opportunity to get an education and find a job, they experience difficulties in establishing social ties. Failure in the professional and personal spheres is further aggravated by the vulnerable condition of patients with bipolar disorder and schizophrenia.
The topics of socio-psychological adaptation of people with a mental diagnosis to the conditions of life in society are still surrounded by a large number of prejudices. However, the unhealthy bias that makes people with mental disorders reluctant to seek professional help until the very end is no longer ignored.
This is evidenced by the results of the latest survey conducted by Gedeon Richter in cooperation with VTsIOM. Thus, 38 percent of respondents are sure that a person with symptoms of schizophrenia is at risk of refusing to receive help in favor of self-treatment because of the fear that acquaintances will find out about the diagnosis in the event of a visit to a specialized specialist.
The fear that others will find out about a mental disorder and will be judged can also be attributed to significant barriers to refusing to receive specialized help for people with manifestations of bipolar disorder: 42 percent of respondents say so.
Photo: Shutterstock
Every patient with a mental disorder, sooner or later, will have to make a choice: not to be treated and let their condition take its course, take medication prescribed by a specialist, or end up in a treatment facility if their condition requires it. Most people with mental disorders, with the right approach and the right systematic drug treatment, have a chance to live a normal life, especially if the diagnosis is made in the early stages. In their case, the opportunity to be in stable remission and live a full life is great, therefore, for this category of patients, it is especially important to create a favorable psychological background both within the family and in a wider circle of their communication.
The condition of a patient with schizophrenia, as in the case of bipolar disorder, needs constant correction with medications. “Neither psychotherapy nor persuasion can help a person with bipolar disorder. Such conditions can only be corrected with medication. If this is not done, then the next time a person will go into an unregulated rise, and then again find himself at the peak of negativity, but even steeper. It is important for patients with bipolar disorder to learn to live in semitones, at half speeds, so that after euphoria they do not slide into a deep depression, ”says Viktoria Zhadenova.
She recommends not avoiding a visit to a specialist if there are warning signs. “Any mental state begins with sleep disturbance and anxiety. A person is changing before our eyes: he becomes wary, anxious, confused, distracted, begins to seem more irritable and sensitive than usual. He reacts to routine events too brightly, too negatively, or, on the contrary, too joyfully. The appearance of hypertrophied emotions against the background of sleep disturbance in any direction should alert the family and is a reason to seek professional help in order to exclude a mental illness or recognize it in time and get the necessary help, ”the expert warns.
Let us remind you that, according to the Ministry of Health of the Russian Federation, about 5.6 million people suffering from mental disorders are registered in the country. Ensuring the quality and accessibility of medical care and rehabilitation procedures for this category of citizens remains among the key tasks for healthcare. Schizophrenia and Bipolar Disorder0001
There are a lot of mental disorders, syndromes and pathologies. At the same time, they have similar symptoms and signs in which the average person can get confused. Even an experienced doctor may need more than one month of observation of the patient in order to make an accurate diagnosis. In modern psychiatry, there are two main diseases - schizophrenia and bipolar disorder. Both are characterized by a state of psychosis, and sometimes hallucinations. But still, these are different pathologies that require two different approaches to treatment. Let's find out what is the difference between them.
In this article
- Bipolar disorder
- BAD manic
- Depressive phase of bipolar disorder
- Mixed States
- Main symptoms
- Main symptoms of schizophrenia
- Risk factors
- Main differences
- Treatment
- What is more dangerous
Bipolar disorder
Bipolar affective disorder (BAD), formerly known as manic-depressive psychosis, is an endogenous mental disorder with affective states - manic, depressive or mixed. It develops in phases that follow one another, as a result of which the patient's mood changes dramatically.
It should be understood that BAD is a fairly general concept for various disorders. Moreover, they usually develop in parallel with other disorders, such as anxiety. Its symptoms are so extensive that it requires careful diagnosis in each case. However, there are still general patterns. First of all, a phase flow is characteristic of a bipolar. There are two main stages of the disease:
- manic;
- depressive.
Let's analyze each in more detail.
BAD manic
The initial phase is characterized by high spirits. The patient feels a surge of strength, both spiritual and physical. He talks a lot, and very quickly, but gradually the content of the speech becomes more and more meaningless. As a rule, one thought begins to replace another according to the principle of associations. There is hypermnesia, that is, an increased ability to remember details. A person begins to sleep less, but at the same time is quite active and eats a lot.
Further development of the phase leads to an increase in symptoms. The patient jokes and laughs a lot for no reason, but sometimes flares up and gets angry. Speech and motor overexcitation begins to be traced. At such moments, it is impossible to conduct a dialogue with a person, he jumps from one topic to another without discussing anything specific.
People try to communicate less with such a person. He continues to be active, including at work, invests in new projects that everyone considers unpromising, makes bright plans and fantasizes a lot. Sleep duration is reduced to 3-4 hours a day.
Some episodes that occur to the patient during the manic phase are amnestic.
Then comes the stage of sharp motor excitation. The patient's actions are erratic, and speech becomes slurred. However, gradually the intensity of the symptoms decreases. First, motor excitation subsides while maintaining the speed of speech. But the latter also disappears over time. In a sense, the person returns to normal. Sometimes he is even more calm than he is in ordinary life.
BAD depressive phase
The depressive phase is the opposite of the manic phase and is characterized by a decrease in mood and activity. First, the general mental tone falls. Gradually, anxiety builds up. A person works less, because there is not enough physical and mental strength for a long activity. The patient's speech is slow, and the actions are inhibited.
Further progression of the disorder leads to the development of symptoms of severe depression. Anxiety, melancholy, loss of appetite, silence, delusional ideas are observed. A person does not answer questions or does it reluctantly and in monosyllables, eats little, engages in moral self-flagellation and self-abasement.
In this state, the patient often thinks about death and suicide. Moreover, suicidal attempts happen quite often, although they do not always lead to death. Illusions and hallucinations are rare, but some patients complain of voices ordering them to commit suicide.
The exit from the phase is accompanied by speech and motor activity. Gradually, the symptoms weaken and disappear. But it depends on the development of the depressive stage. It can be hypochondriacal, asthenic, delusional, etc. The name is due to the dominance of one or another feature.
Mixed states
In mixed states of bipolar disorder, manic and depressive symptoms are observed. They can occur both simultaneously and alternately with a difference of several hours. As a rule, this form of the disease occurs in young patients, especially in patients whose disorder manifested in adolescence.
This type of bipolar disorder is more difficult to diagnose due to the inconsistency of symptoms. A person can be both agitated and anxious-depressive at the same time. The course of the disease is also quite severe. 60% of these patients think about suicide. Moreover, about 50% of patients who committed suicide had precisely a mixed form of bipolar disorder.
Main symptoms
So, the main signs of bipolar disorder, which are observed in almost all cases, are the following symptoms:
- hyperactivity;
- fatigue;
- poor concentration;
- irritability;
- impulsiveness;
- lethargy;
- sleep problems;
- suicidal ideation.
All this leads to problems in the family, relationships, at work or school. A person who previously studied well begins to get bad grades, and a responsible employee comes from work with a reprimand, etc. Such manifestations may be the reason for a visit to a psychologist or psychotherapist.
As for delusions and hallucinations, the hallmarks of most forms of schizophrenia, they are extremely rare in bipolar disorder. But the problem is that the presence of these symptoms does not always speak in favor of schizophrenic disorders. It is possible that BAD is still developing.
Main symptoms of schizophrenia
Schizophrenia is a complex and multifaceted disease with many symptoms. They are divided into two groups - positive and negative. The first testify to the activity of the psyche. This includes delusions and hallucinations. The latter are characterized by declines in mental tone. In this case, there are signs that are included in the symptoms of BAD:
- apathy and indifference;
- increased anxiety;
- outbursts of anger;
- motor or speech excitement;
- insomnia, nightmares;
- severe mood swings.
The intensity of symptoms is determined by the type and form of schizophrenia. So, a sluggish one can develop for years, practically without manifesting itself, and a paranoid one usually has an acute and rapid development.
Risk factors
BAD can be distinguished from schizophrenia through differential diagnosis and long-term observation of symptoms. If we talk about the risk factors and causes of these psychopathologies, then they are largely similar. The fact is that the etiology of both disorders is unknown.
In most cases, we are talking about a genetic predisposition. First of all, doctors find out if there are people with mental disorders in the patient's family. The closer the degree of relationship, the higher the risk of the disease.
Key differences
In bipolar disorder, psychosis leads to overexcitation of the nervous system. This also happens with schizophrenia. Also, a similar similarity is observed with negative symptoms. However, there are three main differences that allow differentiating diagnoses:
- In bipolar disorder, mania is accompanied by an extreme manifestation of feelings and emotions.
However, in general, a person is adequate, and therefore rarely shows aggression. The schizophrenic is not always aware of his actions, therefore he is a danger to himself and others.
- With the development of bipolar disorder, the patient does not lose contacts and does not strive for complete loneliness even during a period of apathy. Withdrawal and alienation are the main symptoms of schizophrenia. They are especially noticeable in patients who are sociable in a healthy state.
- The main difference is in the consequences. Bipolar disorder does not damage the personality, while schizophrenia leaves its mark on the psyche. In a sense, after an attack, a person will never be the same as he was before. In bipolar disorder, even if the psychosis lasts for a long time, personality traits remain the same.
The similarity between bipolar disorder and schizophrenia is that both disorders are chronic. Treatment and prevention will take a lifetime.
Treatment
An accurate diagnosis of the patient can be made only after a few weeks or months after contacting the doctors. After that, the doctor will draw up a treatment card.
For bipolar disorder it includes:
- psychotherapeutic sessions;
- mood stabilizing drugs;
- antidepressants;
- sleeping pills.
Schizophrenia is treated much more difficult and longer. Sometimes it is necessary to use insulin-comatose therapy when the patient is artificially injected into a hypoglycemic coma. Antipsychotics and other antipsychotics are also prescribed. Psychotherapeutic methods include several areas - cognitive, behavioral, etc.
BAD cannot go into schizophrenia. These are two different diseases with different prognosis and outcomes.
BAD treatment can be done on an outpatient basis.