Can you be diagnosed with depression and bipolar
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.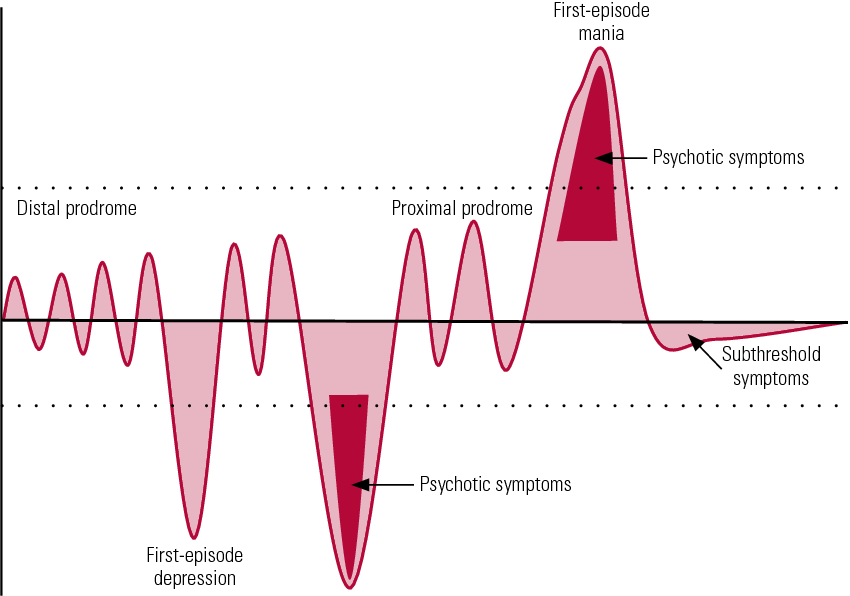
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. SAMHSA’s 2020 National Survey on Drug Use and Health reports that approximately 19.3 million people aged 18 or older had a substance use disorder in the past year.
Alcohol
Data:
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.
 6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- The 2019 National Survey on Drug Use and Health reports that 139.7 million Americans age 12 or older were past month alcohol users, 65.8 million people were binge drinkers in the past month, and 16 million were heavy drinkers in the past month
- About 2.3 million adolescents aged 12 to 17 in 2019 drank alcohol in the past month, and 1.2 million of these adolescents binge drank in that period (2019 NSDUH)
- Approximately 14.5 million people age 12 or older had an alcohol use disorder (2019 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired.
 The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.
 3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Data from the 2019 NSDUH reports that 58.1 million people were current (i.e., past month) tobacco users. Specifically, 45.9 million people aged 12 or older in 2019 were past month cigarette smokers (2019 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey.
 Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018 - E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year.
 Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH) - An estimated 745,000 people had used heroin in the past year, based on 2019 NSDUH data
- In 2019, there were 10.1 million people age 12 or older who misused opioids in the past year. The vast majority of people misused prescription pain relievers (2019 NSDUH)
- An estimated 1.6 million people aged 12 or older had an opioid use disorder based on 2019 NSDUH data
- Opioid use, specifically injection drug use, is a risk factor for contracting HIV, Hepatitis B, and Hepatitis C. The CDC reports that people who inject drugs accounted for 9 percent of HIV diagnoses in the United States in 2016
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.
 5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH) - 2019 NSDUH data indicates that 48.2 million Americans aged 12 or older, 17.5 percent of the population, used marijuana in the past year
- Approximately 4.8 million people aged 12 or older in 2019 had a marijuana use disorder in the past year (2019 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 04/27/2022
Bipolar Disorder | Symptoms, complications, diagnosis and treatment
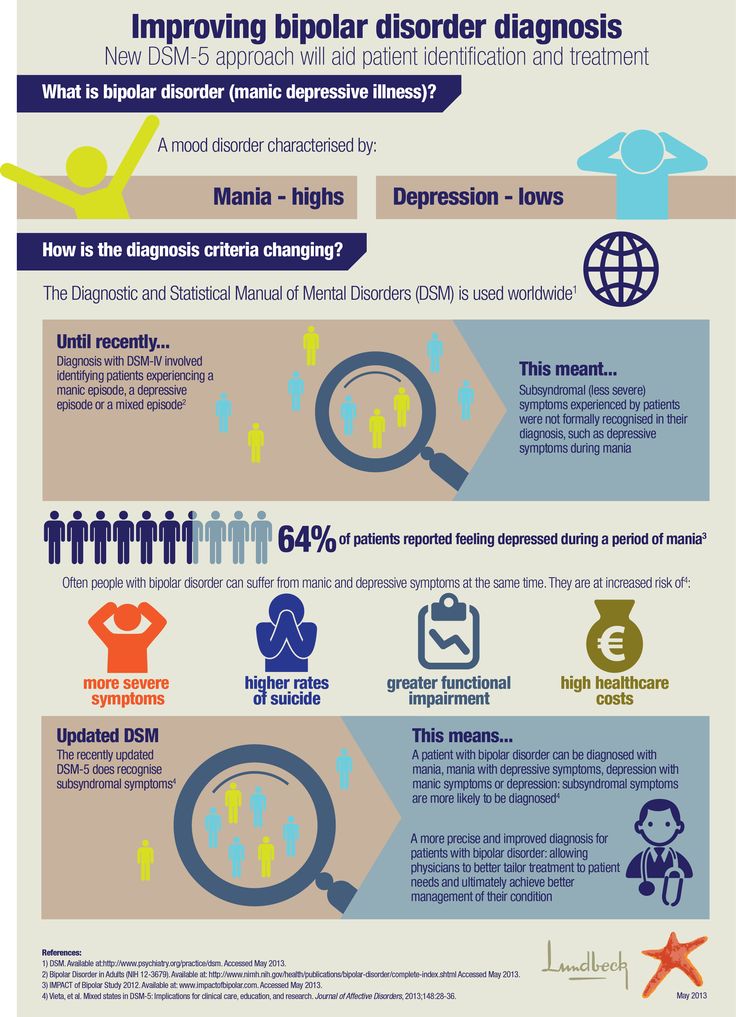
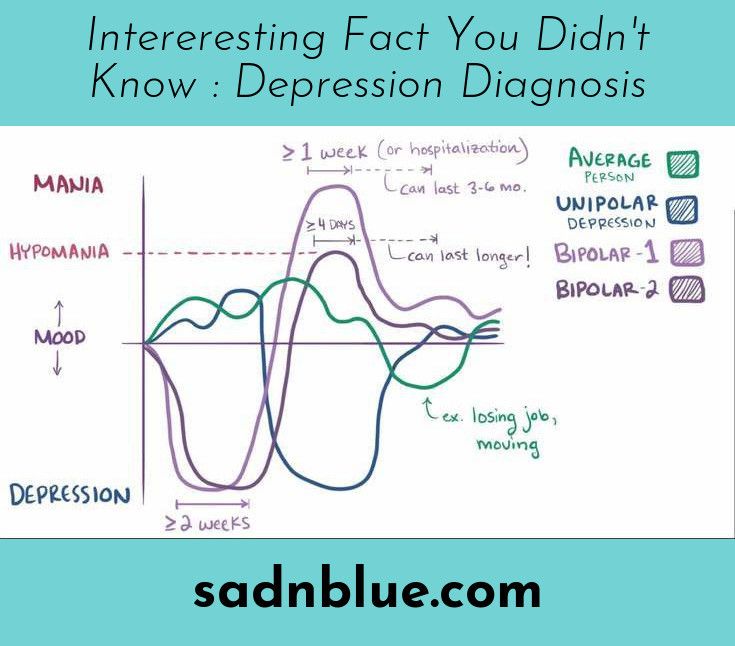
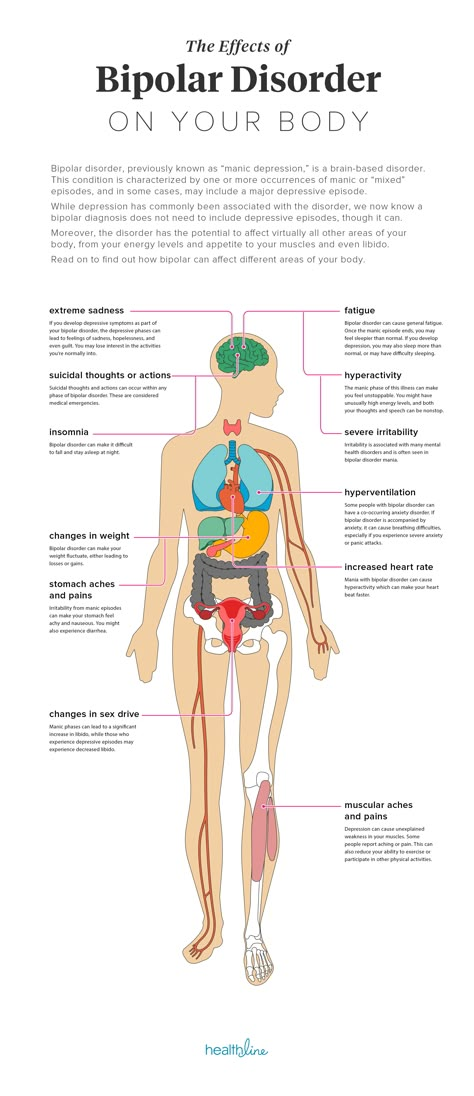
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). Episodes of mood swings may occur infrequently or several times a year.
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When the mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable.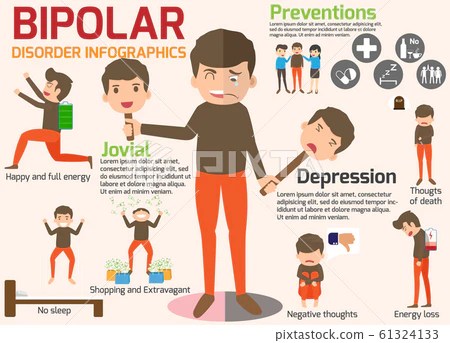 These mood swings can affect sleep, energy, alertness, judgment, behavior, and the ability to think clearly.
These mood swings can affect sleep, energy, alertness, judgment, behavior, and the ability to think clearly.
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medication and psychological counseling (psychotherapy).
Symptoms
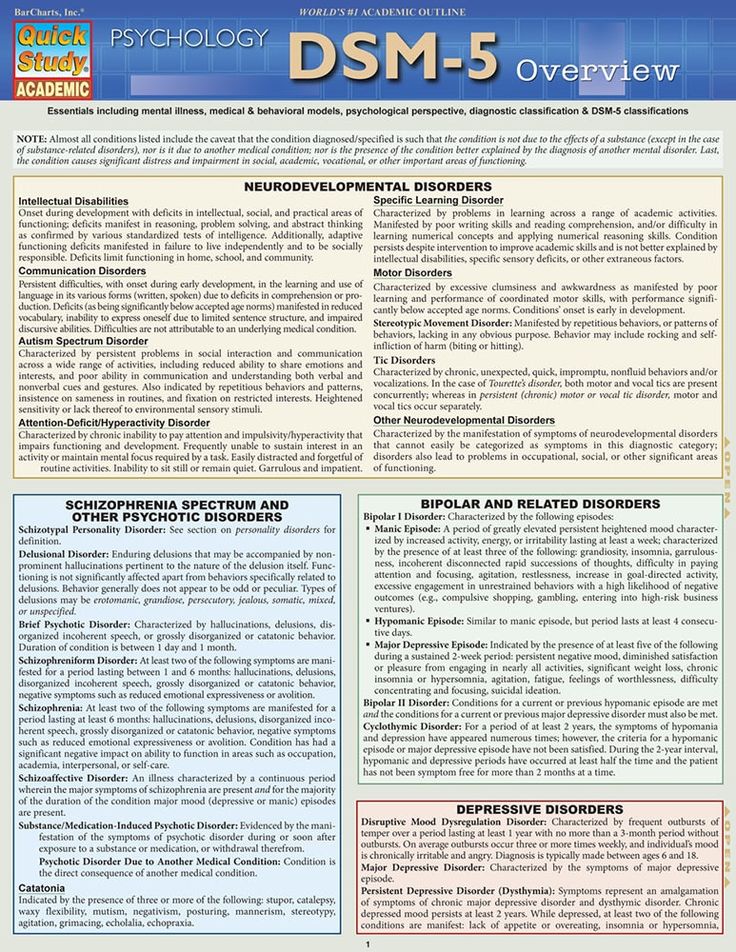
There are several types of bipolar and related disorders. They may include mania, hypomania, and depression. Symptoms can lead to unpredictable changes in mood and behavior, leading to significant stress and difficulty in life.
- Bipolar disorder I. You have had at least one manic episode, which may be preceded or accompanied by hypomanic or major depressive episodes. In some cases, mania can cause a break with reality (psychosis).
- Bipolar disorder II. You have had at least one major depressive episode and at least one hypomanic episode, but never had a manic episode.
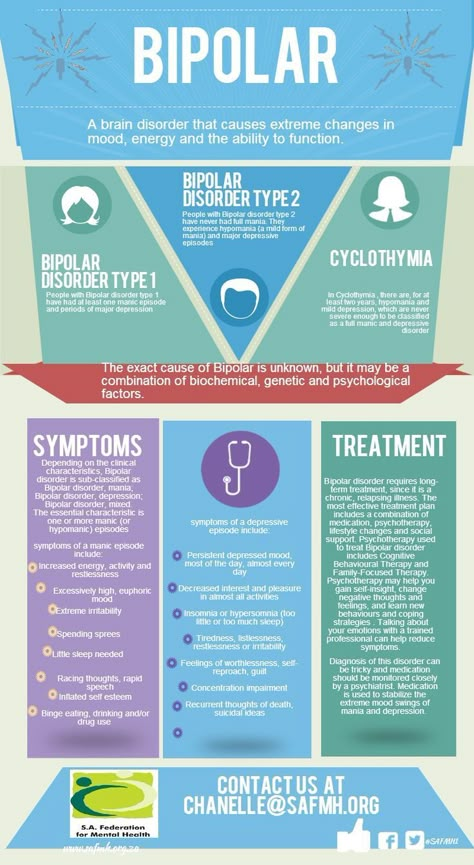
- Cyclothymic disorder. You have had at least two years - or one year in children and adolescents - many periods of hypomanic symptoms and periods of depressive symptoms (though less severe than major depression).
- Other types. These include, for example, bipolar and related disorders caused by certain drugs or alcohol, or due to health conditions such as Cushing's disease, multiple sclerosis, or stroke.
Bipolar II is not a milder form of Bipolar I but is a separate diagnosis. Although bipolar I manic episodes can be severe and dangerous, people with bipolar II can be depressed for longer periods of time, which can cause significant impairment.
Although bipolar disorder can occur at any age, it is usually diagnosed in adolescence or early twenties. Symptoms can vary from person to person, and symptoms can change over time.
Mania and hypomania
Mania and hypomania are two different types of episodes, but they share the same symptoms. Mania is more pronounced than hypomania and causes more noticeable problems at work, school, and social activities, as well as relationship difficulties. Mania can also cause a break with reality (psychosis) and require hospitalization.
Mania is more pronounced than hypomania and causes more noticeable problems at work, school, and social activities, as well as relationship difficulties. Mania can also cause a break with reality (psychosis) and require hospitalization.
Both a manic episode and a hypomanic episode include three or more of these symptoms:
- Abnormally optimistic or nervous
- Increased activity, energy or excitement
- Exaggerated sense of well-being and self-confidence (euphoria)
- Reduced need for sleep
- Unusual talkativeness
- Distractibility
- Poor decision-making - for example, in speculation, in sexual encounters, or in irrational investments
Major depressive episode
Major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in daily activities such as work, school, social activities, or relationships. Episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless, or tearful (in children and adolescents, depressed mood may manifest as irritability)
- Marked loss of interest or feeling of displeasure in all (or nearly all) activities
- Significant weight loss with no diet, weight gain, or decreased or increased appetite (in children, failure to gain weight as expected may be a sign of depression)
- Either insomnia or sleeping too much
- Either anxiety or slow behavior
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking, planning or attempting suicide
Other features of bipolar disorder
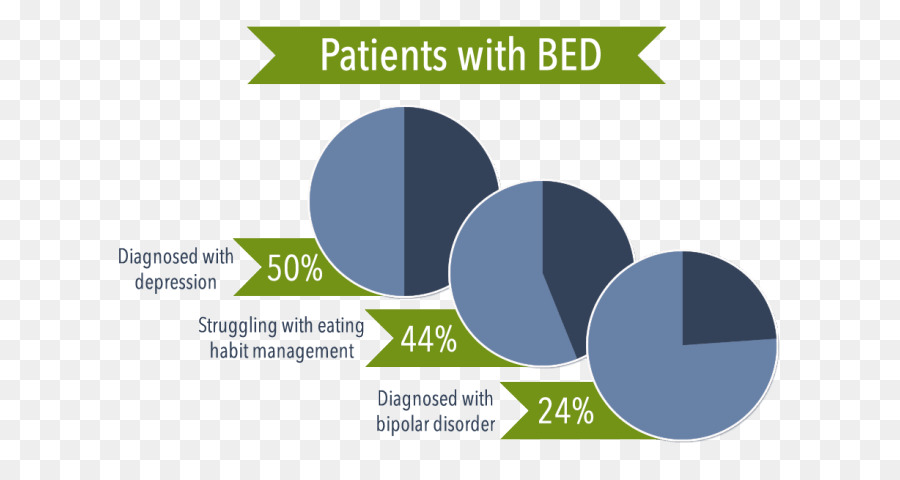
Signs and symptoms of bipolar I and bipolar II disorder may include other signs such as anxiety disorder, melancholia, psychosis, or others.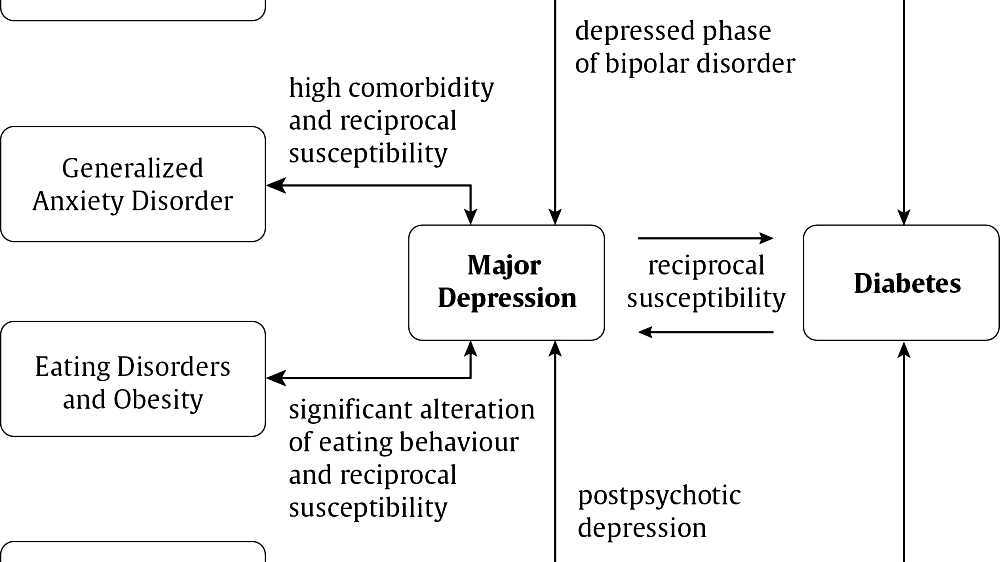 The timing of symptoms may include diagnostic markers such as mixed or fast cycling. In addition, bipolar symptoms may occur during pregnancy or with the change of seasons.
The timing of symptoms may include diagnostic markers such as mixed or fast cycling. In addition, bipolar symptoms may occur during pregnancy or with the change of seasons.
When to see a doctor
Despite extreme moods, people with bipolar disorder often do not realize how much their emotional instability disrupts their lives and the lives of their loved ones and do not receive the necessary treatment.
And if you are like people with bipolar disorder, you can enjoy feelings of euphoria and be more productive. However, this euphoria is always accompanied by an emotional disaster that can leave you depressed and possibly in financial, legal, or other bad relationships.
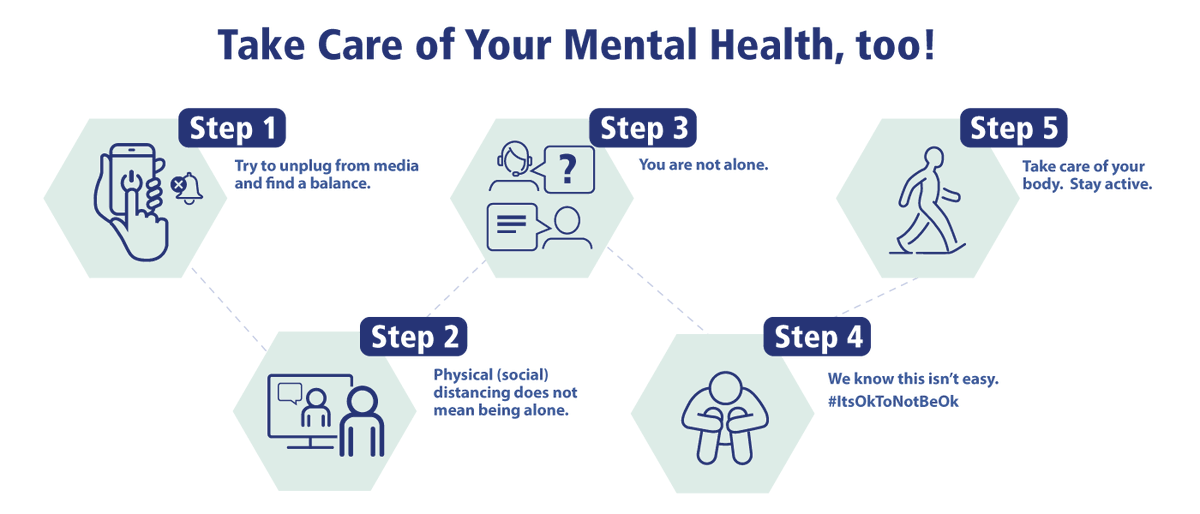
If you have symptoms of depression or mania, see your doctor or mental health professional. Bipolar disorder does not improve on its own. Getting mental health treatment with a history of bipolar disorder can help control your symptoms.
Bipolar affective disorder (BAD), its signs, types and methods of treatment
Manifestations of various emotions, a change in a person's mood, manifestations of both sadness and joy are normal and depend on many factors - from temperament and character to ongoing events that influence from the outside.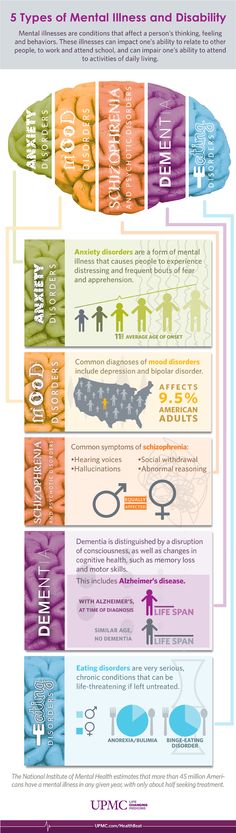 However, when these changes are excessive, often unexpected and for no apparent reason, emotions get out of control, or a person remains in a radically positive or negative mood for a long time, it is very likely that bipolar disorder can be diagnosed. This disease was first described at the end of 19century, the famous German psychiatrist Emil Kripelin, calling it manic-depressive psychosis. Many world famous personalities such as Vincent van Gogh, Isaac Newton, Ludwig van Beethoven, Abraham Lincoln suffered from this disease. A pronounced form of this disease, which is called bipolar affective disorder (BAD) in the international classification of diseases, is detected in 3% of the world's population.
However, when these changes are excessive, often unexpected and for no apparent reason, emotions get out of control, or a person remains in a radically positive or negative mood for a long time, it is very likely that bipolar disorder can be diagnosed. This disease was first described at the end of 19century, the famous German psychiatrist Emil Kripelin, calling it manic-depressive psychosis. Many world famous personalities such as Vincent van Gogh, Isaac Newton, Ludwig van Beethoven, Abraham Lincoln suffered from this disease. A pronounced form of this disease, which is called bipolar affective disorder (BAD) in the international classification of diseases, is detected in 3% of the world's population.
CONTENT OF THE ARTICLE
- 1. Bipolar Personality Disorder - Overview
- 2. Symptoms and signs
- 3. Types of Bipolar Disorder
- 4. Phases of Bipolar Disorder
- 5. Bipolar disorder in women
- 6. Treatment of Bipolar Personality Disorder
It is not uncommon for women to use a combination of drug therapy and cognitive behavioral or interpersonal therapy with a psychotherapist.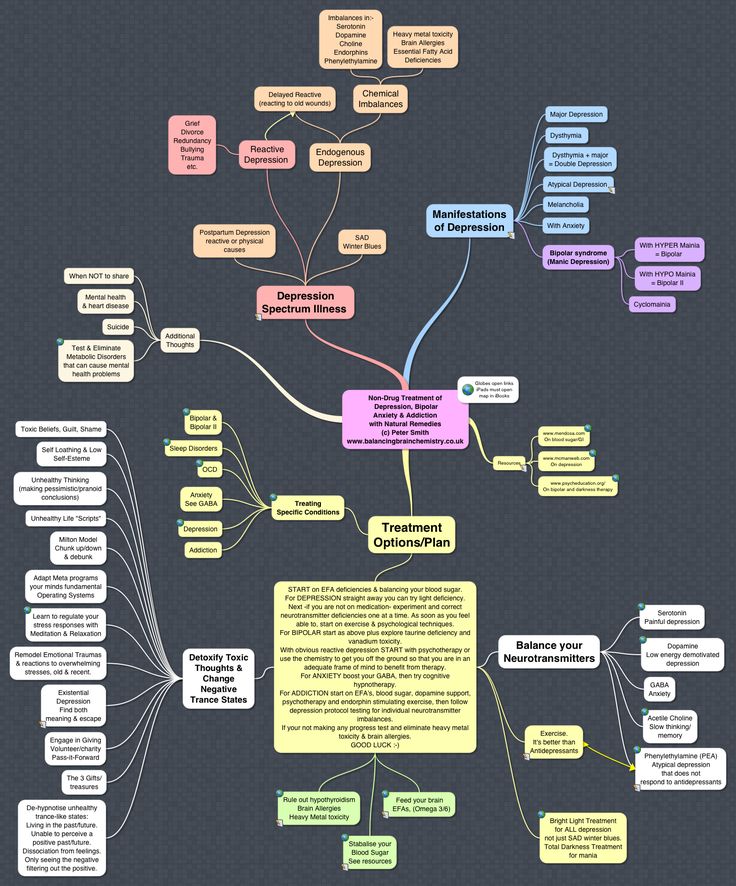
Bipolar personality disorder - general information
According to statistics, bipolar disorder affects people between the ages of 14 and 44. Unlike adults, children and adolescents experience more frequent mood swings from mania to depression, sometimes several times a day. 90% of young people make their debut precisely from the phase of depression or melancholy. Another feature of bipolar disorder is that, due to the low level of diagnosis, the patient can live with this disease for 5-10 years without knowing the cause of the painful symptoms.
Most often, bipolar disorder is diagnosed in people whose immediate family members have had a similar problem. The causes of this disease are unknown, but stress, overstrain, and various diseases can provoke the manifestation of its symptoms. However, having fenced off a person from the influence of these factors, it is impossible to get rid of the problem, you need to seek help from a psychotherapist.
Bipolar disorder is a disease that cannot be completely cured.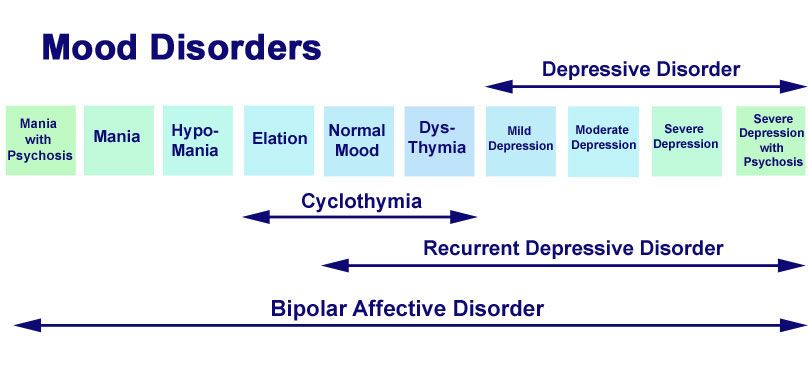 But with properly selected medication and psychotherapy, the quality of life is significantly improved and the periods between phases are lengthened. The person remains socialized and able to work.
But with properly selected medication and psychotherapy, the quality of life is significantly improved and the periods between phases are lengthened. The person remains socialized and able to work.
Symptoms and signs
From the name it is clear that we are talking about two different poles of affective manifestations, that is, mood manifestations. One of these conditions is depression. Depression in bipolar disorder is pronounced, with vivid symptoms. It can last up to a year and is manifested not only by low mood, lack of ability to enjoy and interest in ongoing events, but also by psychosis, when ideas of self-accusation arise, the patient feels inferior, unnecessary, poisoning the life of others. There are also nihilistic thoughts about suffering from some kind of severe illness, despite medical evidence to the contrary. There may be delusional thoughts, as well as suicidal thoughts and even attempts.
The other pole of bipolar disorder is a hypomanic state or hypomania, the characteristic features of which are an increased euphoric emotional background, the patient is constantly on the move, hyperactive, and is distinguished by very fast, associative speech. The patient is constantly cheerful, often hypersexual, almost always awake or sleeping 2-3 hours a day.
The patient is constantly cheerful, often hypersexual, almost always awake or sleeping 2-3 hours a day.
Hypomania is often followed by a manic bipolar state with psychotic manifestations. The patient develops convictions in his own greatness, he believes that he is capable of anything, feels that he has a special calling in this world or that he is a descendant of great people. In extended manic episodes of mania with psychotic manifestations, anger, irritability, and direct aggression often occur. This condition leads the patient into extremely unpleasant and sometimes dangerous situations.
In addition to the typical symptoms of the disease, there are a large number of comorbid mental disorders. Comorbid mental disorders are those that accompany the underlying disease. The most common disorder of this kind is anxiety, which is manifested, among other things, by nonspecific autonomic symptoms, including sweating, palpitations, tremors of the limbs, various disorders of the gastrointestinal tract, dizziness, headaches, suffocation, and many others. In the case when these symptoms occur suddenly, mainly in public places, they are called panic attacks.
In the case when these symptoms occur suddenly, mainly in public places, they are called panic attacks.
Types of bipolar disorder
Bipolar disorder can be of Ι and ΙΙ types.
Bipolar I disorder is a condition in which the patient has persistent manias, i.e. overexcitation, enthusiastic inappropriate behavior, manic psychosis, as well as severe depressions. Symptoms of this type are more severe, so hospitalization is indicated in most cases.
Bipolar I disorder is characterized by short periods of hypomania followed by periods of deep depression. Hypomania is a pre-manic state with less active manifestations. Hypomania lasts a very short period of time - from several days to several hours, so sometimes patients do not even notice them and do not inform the doctor about it. Only careful, painstaking work with the patient makes it possible to identify hypomania, make the correct diagnosis and prescribe treatment.
Phases of bipolar disorder
There are several phases of bipolar personality disorder:
- Depressive (unipolar depression).
 People experience a depressed mood, despair and despondency, complain of a lack of energy and mental concentration, they can either eat too much or too little and sleep.
People experience a depressed mood, despair and despondency, complain of a lack of energy and mental concentration, they can either eat too much or too little and sleep.
Depersonalization and derealization may occur at the peak of bipolar depressive disorder. The boundaries of their own "I" and the world around them become blurred, patients experience difficulties in perceiving what is happening. Familiar places seem new, the colors of the surrounding world change, the patient constantly experiences a feeling of "déjà vu". Sounds become muffled, even if someone is talking very close, it seems to the patient that the voice is coming from afar.
- Manic (hypomanic). In this state, patients are full of energy, overly happy or optimistic, euphoric, and have extremely high self-esteem. At first glance, these are positive signs, but when a person experiences large-scale manic episodes, these symptoms and such an emotional state can reach dangerous extremes.
 A patient in this phase may indiscriminately spend huge amounts of money or behave carelessly, not realizing the full danger. In conversation, people may choke on words, speak at a high speed, or jump from one thought to another. These episodes may also be accompanied by delusions of grandeur or the adoption of serious decisions without thinking about the further consequences.
A patient in this phase may indiscriminately spend huge amounts of money or behave carelessly, not realizing the full danger. In conversation, people may choke on words, speak at a high speed, or jump from one thought to another. These episodes may also be accompanied by delusions of grandeur or the adoption of serious decisions without thinking about the further consequences.
In the development of the manic phase, the following stages of development can be distinguished:
- Hypomania - increased excitement, emotional upsurge.
- Mania - all signs are more pronounced, aggression, irritability, irascibility and rage are possible.
- Phase peak. The patient constantly experiences nervous excitement, he cannot relax. All his emotions are "heated" to the limit, coordination of movements is disturbed, thoughts are illogical and abrupt, in speech he constantly jumps from one sentence to another.
- Relief of symptoms. The patient gradually calms down.
 Movement disorders are on the decline. The speed of thinking and increased emotional mood remain unchanged.
Movement disorders are on the decline. The speed of thinking and increased emotional mood remain unchanged. - Return to normal.
- Mixed. Sometimes people have complaints that are characteristic of both depression and mania at the same time. They may also experience frequent phasing—4 or more episodes in one year.
In the intervals between depressive and manic phases in bipolar disorder, there is a light period during which the general background of mood becomes relatively stable, the person continues to respond adequately to certain events, the emotional sphere is under his control. This is the main criterion for remission of bipolar disease.
Bipolar disorder in women
According to statistics, bipolar Ι disorder occurs with the same frequency in men and women, and type ΙΙ disease is more often diagnosed in women. It is also known that the female course of the disease is characterized by rapid cycles and mixed episodes.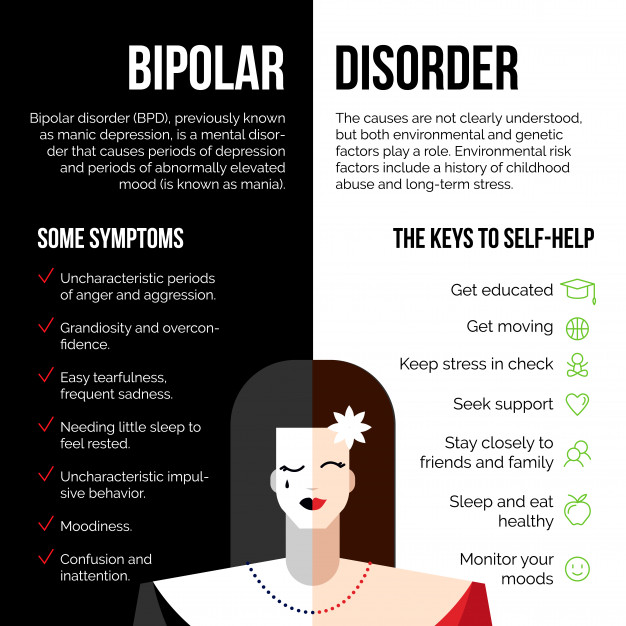 Comorbidities often include eating disorders, borderline personality disorder, alcohol or drug addiction, and psychotropic drug abuse. Women are more susceptible to such somatic diseases as migraine (intense headaches), thyroid pathologies, diabetes, and obesity.
Comorbidities often include eating disorders, borderline personality disorder, alcohol or drug addiction, and psychotropic drug abuse. Women are more susceptible to such somatic diseases as migraine (intense headaches), thyroid pathologies, diabetes, and obesity.
For women, a special technique is being developed to alleviate this disorder, since from adolescence to menopause there are specific changes in hormonal levels that must be taken into account. In addition, psychotropic substances, which are supposed to stabilize the condition, can adversely affect the intrauterine development of the fetus if the woman is in position. It is noted that in the first trimester of pregnancy this disorder is milder, but after childbirth they often have to deal with postpartum depression. Thus, at each stage of the development of the female body, a competent doctor must review and adjust the treatment regimen. Often in the treatment of women, a complex method is used that combines drug therapy and cognitive-behavioral or interpersonal therapy with a psychotherapist. This approach gives the fastest results.
This approach gives the fastest results.
Treatment for bipolar disorder
Attempts to get rid of bipolar disorder on your own do not bring the desired result and, ultimately, lead to an aggravation of the situation, including the development of drug or alcohol dependence. In the diagnosis of the disease, keeping a mood diary can help, where the patient records all his thoughts, emotions, feelings, changes in mood. Such records will help the doctor to assess the mental state in detail and make the correct diagnosis. If you suspect bipolar disorder, you should consult a doctor, and the sooner a person realizes that he has a disease and comes to the clinic for help, the sooner professional help will be provided to him and painful symptoms will be replaced by a stable condition. It is impossible to get rid of the disease on your own, since a person cannot fully adequately assess not only his actions, but also the alternation of the phases of the disease.
Bipolar disorder is one of the few mental disorders in which medication is indicated in 100% of cases, and psychotherapy is an auxiliary tool. This disease is incurable, but its diagnosis and treatment is extremely important. Treatment can reduce the number of episodes, their severity and intensity, as well as prevent negative life events, help prevent relationship breakups, job loss, and even suicidal attempts. Thus, the quality of life of a patient with bipolar disorder who is undergoing treatment will be several times higher than that of a person who neglects treatment. If the patient loses touch with reality and harms himself and others, he is subject to hospitalization, outpatient treatment in this case is not permissible.
This disease is incurable, but its diagnosis and treatment is extremely important. Treatment can reduce the number of episodes, their severity and intensity, as well as prevent negative life events, help prevent relationship breakups, job loss, and even suicidal attempts. Thus, the quality of life of a patient with bipolar disorder who is undergoing treatment will be several times higher than that of a person who neglects treatment. If the patient loses touch with reality and harms himself and others, he is subject to hospitalization, outpatient treatment in this case is not permissible.
If you have a disease, it is recommended to exclude coffee, strong tea, alcoholic and energy drinks from your diet in order not to provoke an overexcited state. If possible, you should stop smoking and in no case should you take even soft drugs. It is also very important to establish a sleep pattern, sleep at least 8 hours a day and try to go to bed at about the same time. You should learn to recognize mood swings and notice the early manifestations of new episodes.