Can depo shot cause depression
Depressive symptoms and Depo-Provera - PubMed
. 1998 Apr;57(4):237-40.
doi: 10.1016/s0010-7824(98)00024-9.
C Westhoff 1 , C Truman, D Kalmuss, L Cushman, A Davidson, M Rulin, S Heartwell
Affiliations
Affiliation
- 1 College of Physicians and Surgeons, Columbia University, New York, New York, USA.
- PMID: 9649914
- DOI: 10.1016/s0010-7824(98)00024-9
Free article
C Westhoff et al. Contraception. 1998 Apr.
Free article
. 1998 Apr;57(4):237-40.
doi: 10.1016/s0010-7824(98)00024-9.
Authors
C Westhoff 1 , C Truman, D Kalmuss, L Cushman, A Davidson, M Rulin, S Heartwell
Affiliation
- 1 College of Physicians and Surgeons, Columbia University, New York, New York, USA.
- PMID: 9649914
- DOI: 10.1016/s0010-7824(98)00024-9
Abstract
Women enrolled in a multicenter prospective study were evaluated to identify any possible relationship between depressive symptoms and the use of contraceptives. Women choosing Depo-Provera (n = 495) were evaluated before starting these contraceptives and were reinterviewed 1 year later. Women who continued the method had lower depressive symptom scores at baseline than did the women who discontinued the method or who were lost to follow-up. Among the continuing Depo-Provera users, the depressive symptom scores improved slightly at 1 year (7.4 vs 6.7). Those subjects with the highest (i.e., worst) scores at enrollment demonstrated improved scores at follow-up.
Women choosing Depo-Provera (n = 495) were evaluated before starting these contraceptives and were reinterviewed 1 year later. Women who continued the method had lower depressive symptom scores at baseline than did the women who discontinued the method or who were lost to follow-up. Among the continuing Depo-Provera users, the depressive symptom scores improved slightly at 1 year (7.4 vs 6.7). Those subjects with the highest (i.e., worst) scores at enrollment demonstrated improved scores at follow-up.
PIP: The product labeling for Depo-Provera cites depression as an infrequent side effect. Previous research on this topic has documented self-reported depression or mood changes in 1-5% of Depo-Provera users. These studies were limited, however, by a lack of measurement of baseline depression. In the present study, 495 new acceptors of Depo-Provera enrolled in a broader prospective cohort study conducted at three US hospitals (Texas, Pennsylvania, New York) were interviewed at enrollment and again after 12 months of use. Included in both the initial and follow-up questionnaires were six questions on depressive symptoms in the past month taken from the Mental Health Inventory. At 12 months, 172 women were still using Depo-Provera, 221 had discontinued the method, and 102 were lost to follow-up. Women who were still using Depo-Provera at 12 months had lower depressive symptom scores at baseline than women who discontinued use or were lost to follow-up. Between baseline and the 12-month follow-up, the mean depression score dropped from 7.4 to 6.7 among continuing users and remained steady at 8.0 among discontinuers. The mean depression score in the quintile of women with the highest depression scores at baseline also decreased after 12 months of use, from 15.4 to 9.5. These results suggest that Depo-Provera use is not likely to exacerbate symptoms in women with pre-existing depression.
Included in both the initial and follow-up questionnaires were six questions on depressive symptoms in the past month taken from the Mental Health Inventory. At 12 months, 172 women were still using Depo-Provera, 221 had discontinued the method, and 102 were lost to follow-up. Women who were still using Depo-Provera at 12 months had lower depressive symptom scores at baseline than women who discontinued use or were lost to follow-up. Between baseline and the 12-month follow-up, the mean depression score dropped from 7.4 to 6.7 among continuing users and remained steady at 8.0 among discontinuers. The mean depression score in the quintile of women with the highest depression scores at baseline also decreased after 12 months of use, from 15.4 to 9.5. These results suggest that Depo-Provera use is not likely to exacerbate symptoms in women with pre-existing depression.
Similar articles
-
Depressive symptoms and Norplant contraceptive implants.
Westhoff C, Truman C, Kalmuss D, Cushman L, Rulin M, Heartwell S, Davidson A. Westhoff C, et al. Contraception. 1998 Apr;57(4):241-5. doi: 10.1016/s0010-7824(98)00022-5. Contraception. 1998. PMID: 9649915
-
Long-term depot medroxyprogesterone acetate (Depo-Provera) use in inner-city adolescents.
Polaneczky M, Liblanc M. Polaneczky M, et al. J Adolesc Health. 1998 Aug;23(2):81-8. doi: 10.1016/s1054-139x(98)00014-7. J Adolesc Health. 1998. PMID: 9714170
-
Depot medroxyprogesterone acetate pioneers. A retrospective study at a North Carolina Health Department.
Potter LS, Dalberth BT, Cañamar R, Betz M. Potter LS, et al. Contraception. 1997 Nov;56(5):305-12. doi: 10.1016/s0010-7824(97)00160-1.
 Contraception. 1997. PMID: 9437559
Contraception. 1997. PMID: 9437559 -
Depo Provera. Position paper on clinical use, effectiveness and side effects.
Bigrigg A, Evans M, Gbolade B, Newton J, Pollard L, Szarewski A, Thomas C, Walling M. Bigrigg A, et al. Br J Fam Plann. 1999 Jul;25(2):69-76. Br J Fam Plann. 1999. PMID: 10454658 Review.
-
Vaginal bleeding patterns in women using once-a-month injectable contraceptives.
Fraser IS. Fraser IS. Contraception. 1994 Apr;49(4):399-420. doi: 10.1016/0010-7824(94)90035-3. Contraception. 1994. PMID: 8013222 Review.
See all similar articles
Cited by
-
The association between depression and contraceptive behaviors in a diverse sample of new prescription contraception users.

Shelef DQ, Raine-Bennett T, Chandra M, Adler N, Marshall CJ, Steinberg JR. Shelef DQ, et al. Contraception. 2022 Jan;105:61-66. doi: 10.1016/j.contraception.2021.08.015. Epub 2021 Sep 2. Contraception. 2022. PMID: 34481788
-
Progesterone, reproduction, and psychiatric illness.
Standeven LR, McEvoy KO, Osborne LM. Standeven LR, et al. Best Pract Res Clin Obstet Gynaecol. 2020 Nov;69:108-126. doi: 10.1016/j.bpobgyn.2020.06.001. Epub 2020 Jun 18. Best Pract Res Clin Obstet Gynaecol. 2020. PMID: 32723604 Free PMC article. Review.
-
Contraception and mental health: a commentary on the evidence and principles for practice.
Hall KS, Steinberg JR, Cwiak CA, Allen RH, Marcus SM. Hall KS, et al.
 Am J Obstet Gynecol. 2015 Jun;212(6):740-6. doi: 10.1016/j.ajog.2014.12.010. Epub 2014 Dec 12. Am J Obstet Gynecol. 2015. PMID: 25511241 Free PMC article. Review.
Am J Obstet Gynecol. 2015 Jun;212(6):740-6. doi: 10.1016/j.ajog.2014.12.010. Epub 2014 Dec 12. Am J Obstet Gynecol. 2015. PMID: 25511241 Free PMC article. Review. -
Psychological distress and post-abortion contraceptive method effectiveness level chosen at an urban clinic.
Steinberg JR, Tschann JM, Henderson JT, Drey EA, Steinauer JE, Harper CC. Steinberg JR, et al. Contraception. 2013 Dec;88(6):717-24. doi: 10.1016/j.contraception.2013.08.009. Epub 2013 Sep 9. Contraception. 2013. PMID: 24094755 Free PMC article.
-
Clinical Case Rounds in Child and Adolescent Psychiatry: De Novo Self-Mutilation and Depressive Symptoms in a 17-year-old Adolescent Girl Receiving Depot-Medroxyprogesterone Acetate.
St-André M, Stikarovska I, Gascon S.
 St-André M, et al. J Can Acad Child Adolesc Psychiatry. 2012 Feb;21(1):59-62. J Can Acad Child Adolesc Psychiatry. 2012. PMID: 22299016 Free PMC article.
St-André M, et al. J Can Acad Child Adolesc Psychiatry. 2012 Feb;21(1):59-62. J Can Acad Child Adolesc Psychiatry. 2012. PMID: 22299016 Free PMC article.
See all "Cited by" articles
Publication types
MeSH terms
Substances
Grant support
- R01 HD29638/HD/NICHD NIH HHS/United States
Does Depo-Provera Cause Mood Changes?
Previous Next
- View Larger Image
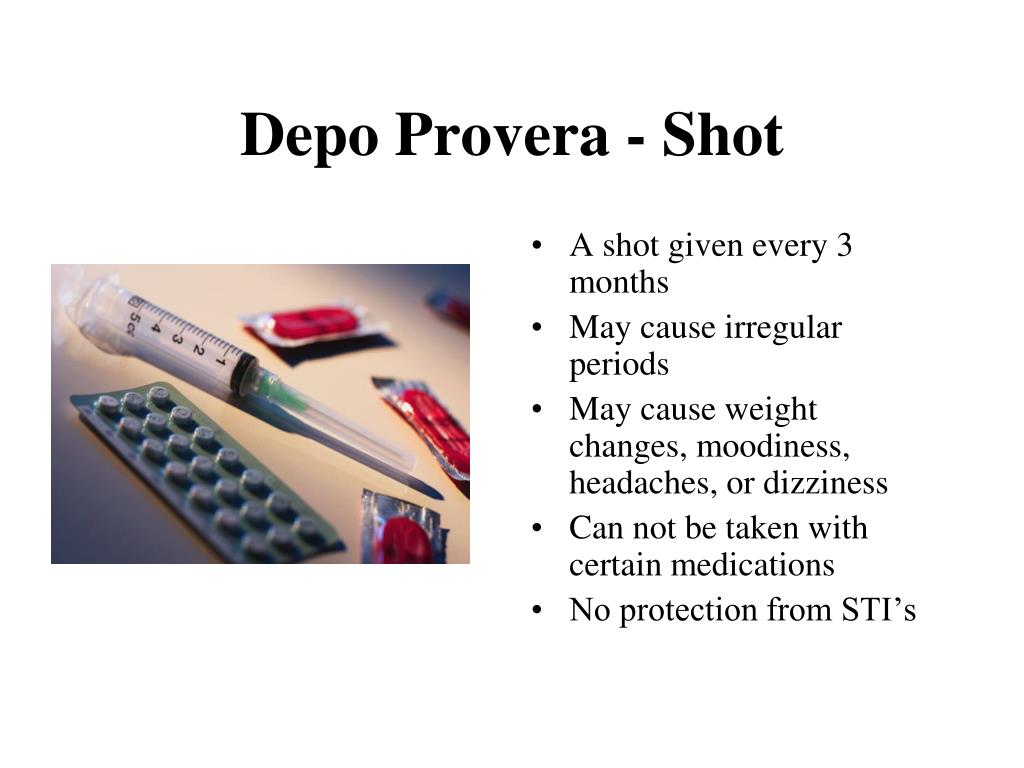
Depo-Provera (DMPA), also known as the birth control shot, is a highly effective form of contraception that lasts for 3 months, and thus requires only 4 injections per year. DMPA contains a long-lasting form of depot medroxyprogesterone acetate that works as a contraceptive agent by preventing the ovaries from releasing an egg each month. Potential side effects of DMPA include bone density loss, weight gain, and mood worsening. Although depression is listed in the packet insert as a side effect of the injection, available research addressing this side effect are limited and contradictory.
DMPA contains a long-lasting form of depot medroxyprogesterone acetate that works as a contraceptive agent by preventing the ovaries from releasing an egg each month. Potential side effects of DMPA include bone density loss, weight gain, and mood worsening. Although depression is listed in the packet insert as a side effect of the injection, available research addressing this side effect are limited and contradictory.
In two older studies, between 1% and 5% of DMPA users reported experiencing depression or mood changes on the treatment, but these studies used brief non-standardized interviews. Three more recent studies have used more structured assessments of mood to evaluate whether there are mood effects of DMPA use.
The 2006 Bulletin of the American College of Obstetricians and Gynecologists states that DMPA does not appear to be associated with mood worsening. This is based primarily on a one large study of 495 women who chose to use DMPA. After 12 months, 34% of participants were still using DMPA, 44% had discontinued use, and 20% were lost to follow-up. Over the 12 month period, depression levels improved slightly in the women who continued using DMPA, and depression levels were unchanged in those who discontinued it.
Over the 12 month period, depression levels improved slightly in the women who continued using DMPA, and depression levels were unchanged in those who discontinued it.
It is important to note, however, that in this study women who discontinued DMPA had slightly higher baseline depression scores than continuers. Furthermore, one of the limitations of this study is that it did not provide any information as to why such a large proportion of women discontinued DMPA use. If a significant proportion of those who discontinued did so because of mood worsening, we cannot conclude that DMPA use has no impact on mood.
Of two other studies that have examined the relationship between DMPA use and depression, one found a negative effect on mood and the other reported no relationship. The first was a 3- year study of 183 women which found that women using DMPA had an increase in depressive symptoms when compared with women not using DMPA. The women who stopped using DMPA during the study had higher levels of depression immediately before or immediately after they discontinued DMPA than they had before starting DMPA. Levels of depression in this group dropped to those observed in non-DMPA users within several months of the discontinuation of DMPA.
Levels of depression in this group dropped to those observed in non-DMPA users within several months of the discontinuation of DMPA.
The second study of 39 adolescents found that over 1 year of continued use, DMPA was not associated with any mood changes.
Although some women report mood worsening on DMPA, more research is needed to determine how common this side effect is and if women with a history of mood disorder are more susceptible to such a side effect. Women with a history of mood disorder should talk to their doctor about these risks and benefits before using DMPA.
One option for women considering DMPA who are concerned about side effects is to have a short trial of oral medroxyprogesterone acetate (Provera) – the same medication that is in the DMPA injection. The advantage of administering a short trial of oral medroxyprogesterone acetate is that, if there is an adverse reaction, the oral medication can be stopped immediately, whereas the side effects of the long acting DMPA injection may linger.
Adriann Kanarek-Farrell, BA
Hadine Joffe, MD, MSc
ACOG Practice Bulletin. No. 73: Use of hormonal contraception in women with coexisting medical conditions. Obstet Gynecol. 2006 Jun;107(6):1453-72.
Westhoff C, Truman C, Kalmuss D, Cushman L, Davidson A, Rulin M, Heartwell S. Depressive symptoms and Depo-Provera. Contraception 1998;57:237-40.
Civic D, Scholes D, Ichikawa L, LaCroix AZ, Yoshida CK, Ott SM, Barlow WE. Depressive symptoms in users and non-users of depot medroxyprogesterone acetate. Contraception 2000;61:385-90.
Gupta N, O’Brien R, Jacobsen LJ, Davis A, Zuckerman A, Supran S, Kulig J. Mood changes in adolescents using depot-medroxyprogesterone acetate for contraception: a prospective study. J Pediatr Adolesc Gynecol 2001;14:71-6.
Schwallie PC, Assenzo JR. Contraceptive use–efficacy study utilizing medroxyprogesterone acetate administered as an intramuscular injection once every 90 days. Fertil Steril 1973;24:331-9.
Fraser IS, Dennerstein GJ. Depo-Provera use in an Australian metropolitan practice. Med J Aust 1994;160:553-6.
Depo-Provera use in an Australian metropolitan practice. Med J Aust 1994;160:553-6.
Related Posts
Fighting depression: 10 modern drugs
{{if type === 'partner-stocks'}}
{{/if}}
{{/if}} {{each list}}${this} {{if isGorzdrav}}
Delete
{{/if}}
{{/each}} {{/if}} Search by drug, disease, substance: DERMAKOSMETIKA, SOLGAR, NaturAge, Voltaren, KagocelHome
Articles
Fighting depression: 10 modern drugs
Depression is an urgent problem, the number of visits to doctors is growing every year. It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
What is meant by
depression Doctors have known it since ancient Greece and Egypt. Hippocrates described it as melancholy - a condition that is accompanied by anxiety, despondency, insomnia, refusal of food, irritability. Most often, the cause is childhood trauma or severe, frequent stress in adulthood. There are many provoking factors: the death of a loved one, deterioration of living conditions, alcoholism, brain diseases.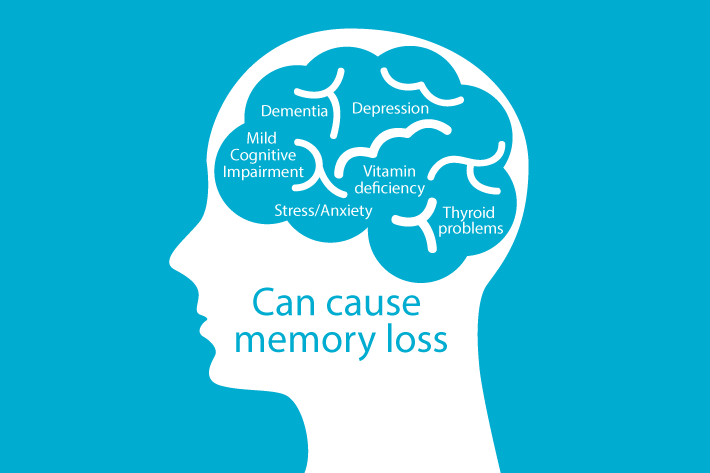 Such cases are referred to as psychogenic depression.
Such cases are referred to as psychogenic depression.
The second type is endogenous. The problem appears not from large external shocks, but because of internal causes. A person is constantly dissatisfied with himself, subjecting himself to criticism. Many patients have panic attacks , haunted by a feeling of fear, anxiety.
How long the period of depression lasts
Many people mistake ordinary periods of low mood for depression. If they do not last long and are quickly replaced by periods of recovery, then we are not talking about a depressive state. The problem is obvious when the symptoms persist for months and dramatically change a person's life. Then you need to see a doctor.
What happens to the body
The most common theory is that there is a malfunction of neurotransmitters located in the brain. These substances transmit signals from neuron to neuron and are responsible for a person's mood. Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
How is
treated depressionDepression has been treated in different ways. In the ancient world - emetics and laxatives. In the Renaissance - wine and sunbathing. In the Age of Enlightenment - external stimuli, for example, insects. The 19th century brought new recipes - in particular, a solution of camphor in tartaric acid. The treatment also included the use of drugs, which are now no longer allowed for sale, and some are recognized as narcotic.
Obviously, all these drugs had no effect on increasing the amount of serotonin. And the treatment is precisely to normalize its production. This was done after creating modern antidepressants , which have a minimum of side effects, are safe for the body and are not addictive. These are medicines, whose action is aimed specifically at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
These are medicines, whose action is aimed specifically at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
Prescription
If a healthy person takes antidepressants , there will be no effect . For a depressed patient, taking them will help:
- improve psychological state;
- get rid of irritability;
- panic fear;
- increase mental and physical activity;
- overcome the dreary mood.
Psychiatrists prescribe antidepressants for chronic back pain, headaches. And also with irritable bowel syndrome, incontinence and other cases when the body stops producing its own painkillers. Medication helps restore pain suppression mechanisms.
These drugs can only be taken with a doctor's prescription, as many of them are strong stimulants. Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Precautions
- Prescribed drug start drinking from a small dose - the first couple of days they take a quarter of a tablet. Gradually increase the dose to normal. So the body adapts better. Finish the course by reducing the dose.
- The first effect of appears only 2 weeks after the start of administration. Sustained action - after six months. All this time, you need to take remedy, without making passes, breaks.
-
Products are not combined with melatonin, St. John's wort, products and dietary supplements based on sibutramine, 5-HTP. Their combination can raise serotonin to dangerous levels.
 Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account.
Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account. - Drinking antidepressants is better in parallel with visits to a psychotherapist. If the drugs normalize the biochemical processes in the body, then this doctor will help normalize the psychological state after depression.
The best antidepressants
In medicine, they have long argued that some drugs give only a placebo effect. The purpose of the study was to find out which of them are the most effective and valid . The project involved 116 thousand patients, and its results were published by the authoritative edition of the Lancet. We offer a list of the best.
1. Agomelatine
New generation drug. Agomelatine is used for severe depressive disorders, high levels of anxiety. Enhances the release of dopamine and norepinephrine, stimulates melatonin receptors. The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
Pros
+ Does not adversely affect attention and memory.
+ No lethargy during the day.
+ No sexual deviations.
+ No relation to blood pressure.
+ Do not reduce dosage upon discontinuation.
Cons
— In 1-10% of cases, increased sweating, diarrhea, constipation.
- Possible increased fatigue, drowsiness.
- There are no evidence-based safety studies in people with renal or hepatic insufficiency, therefore, such patients are advised to refrain from taking drugs with active ingredient agomelatine.
2. Amitriptyline
Tricyclic antidepressant. Moreover, the World Health Organization considers Amitriptyline the most reliable in this group. The standard dose is 200-250 mg / day. The action is to block the reuptake of neurotransmitters. A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
Pluses
+ Preparations with active ingredient amitriptyline are inexpensive.
+ High reliability, minimum side effects.
+ Relatively safe during breastfeeding.
Cons
- Possible side effect in the form of blurred vision, dry mouth.
- Lowering blood pressure.
- Some patients experience constipation.
- Drowsiness.
3. Escitalopram
It belongs to the group of modern serotonin reuptake inhibitors (SSRIs). Most often, it is recommended to take for anxiety, panic attacks. It is taken once, the standard dose is 10 mg per day. Escitalopram has a milder effect and is prescribed to patients for whom tricyclic drugs are contraindicated.
Pluses
+ Lasting effect comes after 3 months.
+ Indicated for patients with disorders of the cardiovascular system.
+ Soft action.
Cons
- In some patients, the functions of the gastrointestinal tract are disturbed, which is most often expressed in diarrhea.
- Anxiety may increase during the first 2 weeks, therefore it is recommended to start treatment with low doses and gradually increase them.
- Contraindicated in pregnancy and lactation.
4. Mirtazapine
A drug of the tetracyclic group. Mirtazapine - good stimulant for anxious depressions, has a moderate sedative effect. The average amount is 30 mg / day, it must be consumed once. Usually it is prescribed to patients who lose interest in life, cease to experience joy, pleasure. Effective in the correction of sleep, in particular, early awakenings.
Pros
+ Earlier onset of action than SSRIs (1 week).
+ Works well with most general medicines.
+ Full effect in 4 weeks.
+ Does not affect sexual function.
Cons
- The active substance mirtazapine is contraindicated in diabetes mellitus, arterial hypotension, increased intraocular pressure.
— During the appointment, you must drive carefully and engage in potentially hazardous types of work.
- 18% of patients experience drowsiness, 15% dry mouth, 5% weight loss. Other side effects occur in 1-3% of cases.
5. Paroxetine
Belongs to the SSRI group, is used most often for severe anxiety, panic, social phobia, nightmares, stress after trauma. Paroxetine can resolve the problems of anxious depression, anxiety-phobic disorders. Take once a day at a dose of 20 mg.
Pros
+ The most powerful stimulant among SSRIs.
+ Anxiety and insomnia pass quickly.
+ Minimal side effects in the form of vomiting, diarrhea.
+ Suitable for patients with cardiovascular problems.
Cons
— Not suitable for patients with severe motor, mental inhibition.
- Reduces libido.
- Harmful to the fetus when taken during pregnancy.
6. Fluoxetine
One of the most commonly used antidepressants in the SSRI group. Known as Prozac. Fluoxetine is also known as a good mood stimulant. Patients have a feeling of fear, tension, anxiety, gloomy dislike for others. Depending on the indications, the average daily dose is 20-60 mg.
Pluses
+ There is practically no effect on the work of the heart.
+ Does not cause sedation.
+ Effective for patients with motor retardation and excessive daytime sleepiness.
Cons
- May cause weight loss.
— Hypoglycemia is possible in diabetes mellitus.
- Contraindicated in severe renal impairment.
7. Fluvoxamine
Another SSRI drug. Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Pros
+ Lower price than traditional Prozac.
+ Faster action than him.
+ Relatively minor side effects (diarrhea, dry mouth, drowsiness).
Cons
- Contraindicated in diabetes.
- Pregnant women - with caution, lactation - prohibited.
- Causes nausea in some patients.
8. Sertraline
One of the widely used and universal drugs of the SSRI group. They treat almost any depressive condition, panic disorder, social phobia. However, in severe clinical cases, sertraline may not be effective enough. The standard dose is 50 mg/day.
Pros
+ No cardiotoxicity.
+ The patient's psychomotor activity does not change.
+ Does not increase body weight.
+ Combines well with other groups of antidepressants.
Cons
— In the first 2 weeks there may be problems with sleep, diarrhea.
- Side effects of a sexual nature.
- Contraindicated in pregnant women.
9. Escitalopram
The drug is classified as an SSRI. Its difference is in its effectiveness in depression, which is accompanied by involuntary movements (tic, tremor, chewing, smacking). Escitalopram is prescribed to patients with panic, anxiety, phobias, obsessive thoughts or actions. The daily dose is 20 mg.
Pluses
+ Effective in tardive dyskinesia.
+ One of the most powerful SSRIs.
+ More pronounced thymoleptic effect (improvement of mood) compared to many antidepressants of the same group.
Cons
- In some patients, anxiety increases within 2 weeks after starting treatment.
— Gastrointestinal disorders, insomnia, agitation are possible.
— Use during pregnancy only in extreme cases, incompatible with feeding.
10. Venlafaxine
Belongs to the SNRI group. In addition to blocking the reuptake of serotonin, venlafaxine has a similar effect on another neurotransmitter, norepinephrine. The medicine is prescribed for depressive conditions of various origins, social phobias, anxiety, panic. Usually take 150 mg per day.
Pros
+ Better tolerated by patients than most tricyclics.
+ More pronounced effect than classic SSRIs.
+ Fewer contraindications.
Cons
- Traditional side effects of most antidepressants: nausea, drowsiness, dry mouth, diarrhea or constipation.
- May increase eye pressure.
- The most severe withdrawal syndrome among antidepressant drugs.
This list is not to be used as a recommendation. In any case, consult your doctor before purchasing. Be healthy!
Can medications cause depression?
- Alex Therrien
- BBC health reporter
Photo credit, Getty Images
Photo caption,Experts say doctors must provide full information about which drugs you are taking
When we hear about the side effects of drugs, most often the first thing that comes to mind is the physical reaction of our body, such as a headache or a rash.
However, US scientists have provided new evidence that many prescription drugs can cause depression.
These include heart medications, oral contraceptives, and even some painkillers.
The study involved 26,000 people - and more than a third of the drugs they took provoked depression.
What does the study say?
In a study published in the Journal of the American Medical Association, researchers analyzed medical data from people who used at least one prescription drug between 2005 and 2014.
In 37% of the drugs taken by the subjects, depression was among the side effects.
- Is fast food a sure way to depression?
- If you are a woman, will you get quality health care?
Moreover, those who took only one drug with such a possible side reaction, the risk of developing depression increased by 7%. For those who took two drugs - by 9%, and for those who took three drugs - by 15%.
For those who took two drugs - by 9%, and for those who took three drugs - by 15%.
"It will surprise many that their medications, despite the fact that they may have nothing to do with mood changes or any other condition that is commonly associated with depression, can increase the risk of depressive symptoms and even lead to a diagnosis of depression" - notes Dima Kato of the University of Illinois, who led the research.
At the same time, it should be noted that any illness can negatively affect mood. In addition, some participants in the study may have experienced depression before.
What do other experts say?
British experts note that a study by their American colleagues indicates a link between drugs and an increased risk of depression, but not that drugs can be the cause of this condition.
"It is not surprising that the use of drugs to treat physical ailments, such as heart problems or lung disease, may be associated with depressive symptoms, since these physical ailments are already associated with an increased risk of depression," explains Professor David Baldwin of the British Royal college of psychiatrists.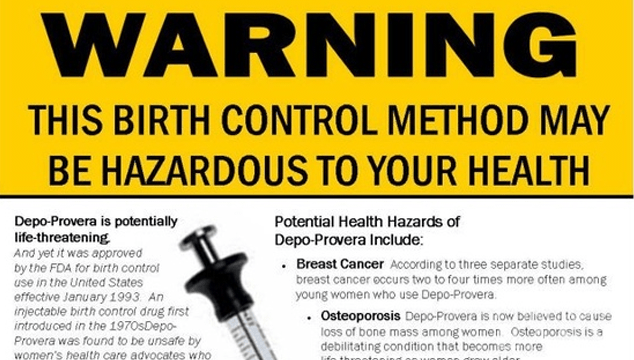
At the same time, Professor Helen Stokes-Lampard, chairman of the Royal College of Physicians, notes that the study indicates "how important it is for patients to tell their doctors or pharmacists about all the drugs they take."
Is there a risk?
Side effects depend on the pharmacological properties of the drug. For example, depression can be a common side effect of some oral contraceptives, meaning it affects up to 1 in 10 patients.
In turn, rare side effects may occur in 1 patient in 10 thousand.
Professor David Taylor of the British Royal Society of Pharmacy says that what's important here is whether there is a "reliable explanation" for why a particular drug causes depression.
- How bacteria affect our mood
- How hormones, immunity, microbes and pulse affect our character mood.
In other cases, it may be difficult to determine whether a drug is causing depression - or whether it is the illness for which it is prescribed.

Learn more