Borderline personality disorder webmd
How to Handle a Relationship With Someone Who Has It
Written by Kate Rope
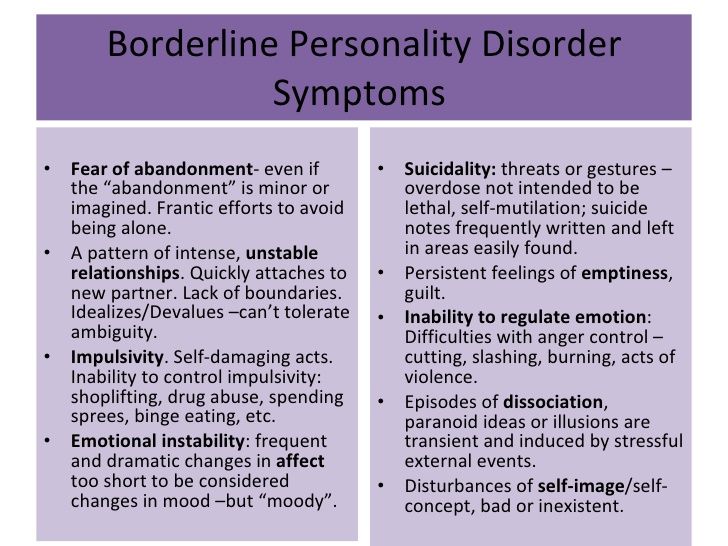
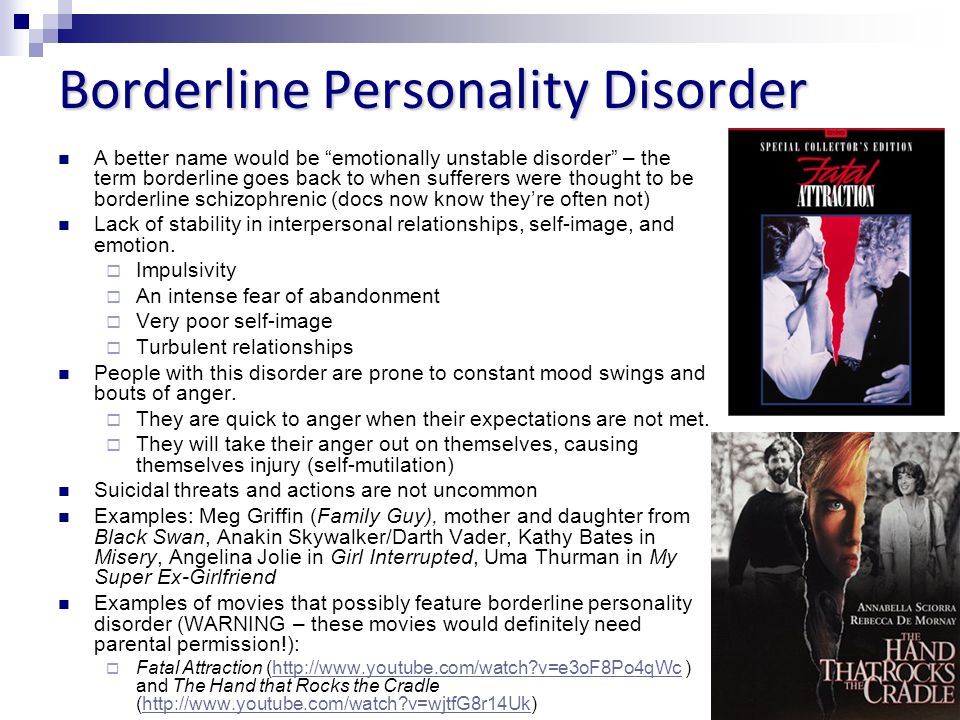
People who live with borderline personality disorder (BPD) have a hard time regulating their emotions, which can be very intense, and handling stress. This can lead them to lash out at the people in their lives. As a result, they often have turbulent relationships that are as hard for the other people in them as BPD is for the person living with it. If you live with someone who has BPD, this isn’t news to you, but you may feel be at a loss about how to do anything about it.
Daniel S. Lobel, PhD, a clinical psychologist who specializes in supporting the loved ones of people with BPD, has advice on how to help yourself, your partner, and your relationship get to a healthier place.
Learn About Borderline Personality Disorder
Living with borderline personality disorder -- or living with someone who has it -- can be isolating. People with BPD and the people who live with them often feel totally alone. Education is critical, especially when it comes to the behaviors that come with the condition.
People with BPD tend to lash out and attack the person who doesn’t have it, Lobel says. “So people who are with people who have BPD end up feeling bad about themselves.”
Learning about how BPD causes this helps people who don’t have it understand that it isn’t them. Lobel suggests these sites to learn more about borderline personality disorder and find support:
- BPDcentral.com
- Personality Disorder Awareness Network
- National Alliance on Mental Illness
Take Care of Yourself First
Before you do anything else, “you have to stop the person from hurting you in order to make progress in the relationship,” Lobel says. Trying to help them when you’re being treated poorly -- being yelled at, living with passive aggressive behavior -- isn’t safe for you and isn’t likely to help your partner.
Instead, he says, the first step is setting a boundary about your well-being.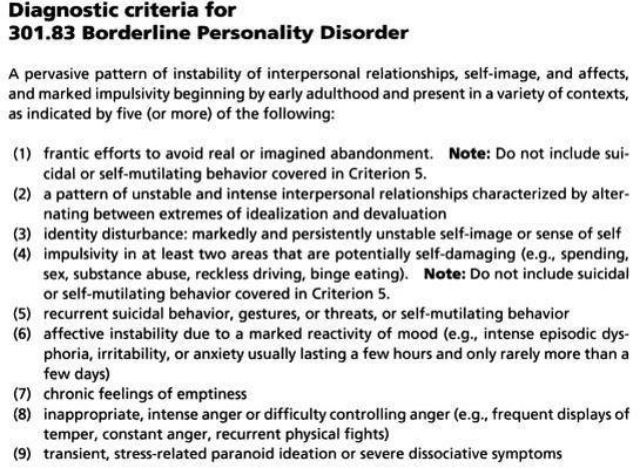 He suggests telling your partner, “I can’t be with you unless I am well, and in order for me to be well, I have to stop you from hurting me.”
He suggests telling your partner, “I can’t be with you unless I am well, and in order for me to be well, I have to stop you from hurting me.”
If your partner says they can’t stop, they’ll likely need professional help before you can make any progress. The goal in this step, Lobel says, is to let your partner know, “you have to stop abusing me or we have nowhere to go.”
Set -- and Stick With -- Boundaries
“People with BPD try to get other people to do for them what they should be doing for themselves,” Lobel says. And often they succeed, because the other person just wants to stop the yelling, so they give in.
Instead, tell your partner, “I will not participate in things that are unhealthy.” That might mean insisting they don’t use drugs or alcohol in the house, or not joining in if they do. It could mean leaving if your partner is yelling at you or belittling you.
Enforce Emotional Boundaries, Too
People with borderline personality disorder often bring the people near them into their emotions.
“They think, ‘If I’m angry, you need to be angry too,’ so they will create a circumstance that makes the other person angry,” Lobel says.
If you can spot these trends, it will go a long way toward stopping this co-dependent cycle.
Lobel suggests telling your partner, “You’re angry. I understand. I don’t need to be angry to understand that you’re angry. We can talk about your anger, but you can’t yell at me or be abusive.”
If they can’t stop the behavior, you can tell them “You have to handle this on your own.”
Replace Unhealthy Connection With Healthy Connection
Fighting with or defending yourself from a partner who’s treating you badly saps your interest and ability to do enjoyable things with them. That makes it harder to connect.
Lobel says making a change, like walking away when they’re treating you badly, frees up time and emotional space for you to have positive interactions, like watching a movie or taking a walk together. These are more positive ways of showing love.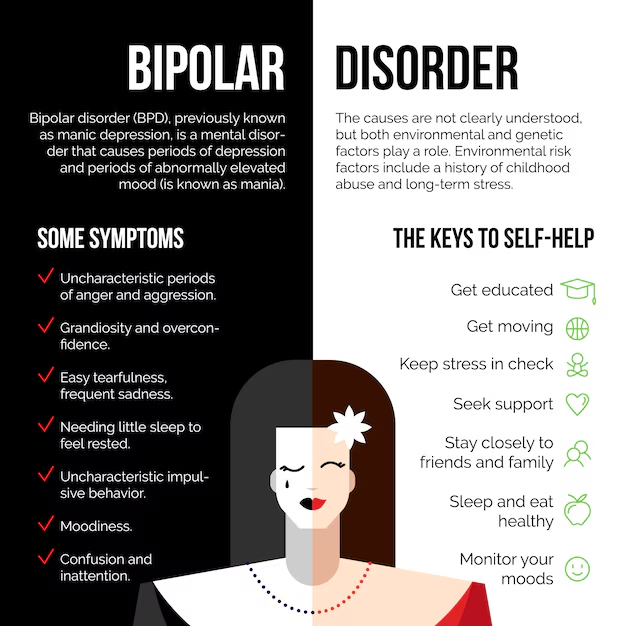
Be Consistent
“Consistency is so important,” Lobel says, “because people with BPD test boundaries. If you set a limit, they may see what ways they can push or encroach on the limit.” If the pattern between you has been to let boundaries be stretched or broken over a long time, it won’t change overnight.
“You can’t just change up the boundary one day and expect them to comply,” he says. “In the short-term they will test it more.” That means things are likely to get worse before they get better.
“But if you can get past that part, and if you are very consistent,” Lobel says, “they will start to accept your boundaries.” They won’t stop testing your limits, but they will do it less and less.
Support Your Partner’s Treatment
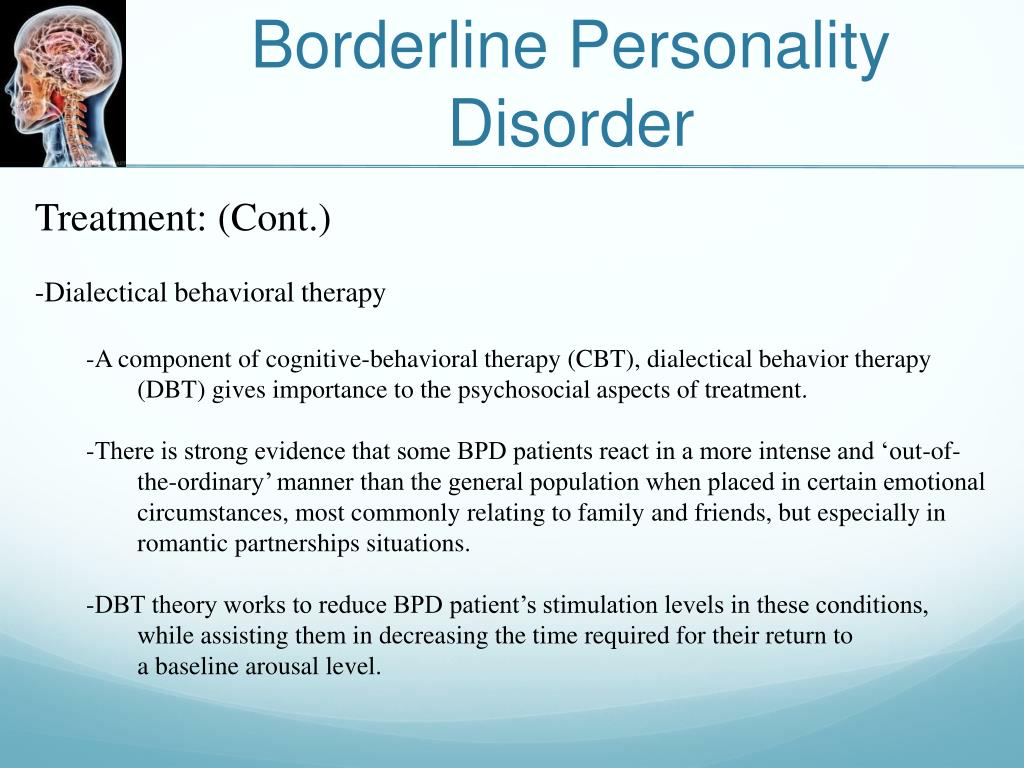
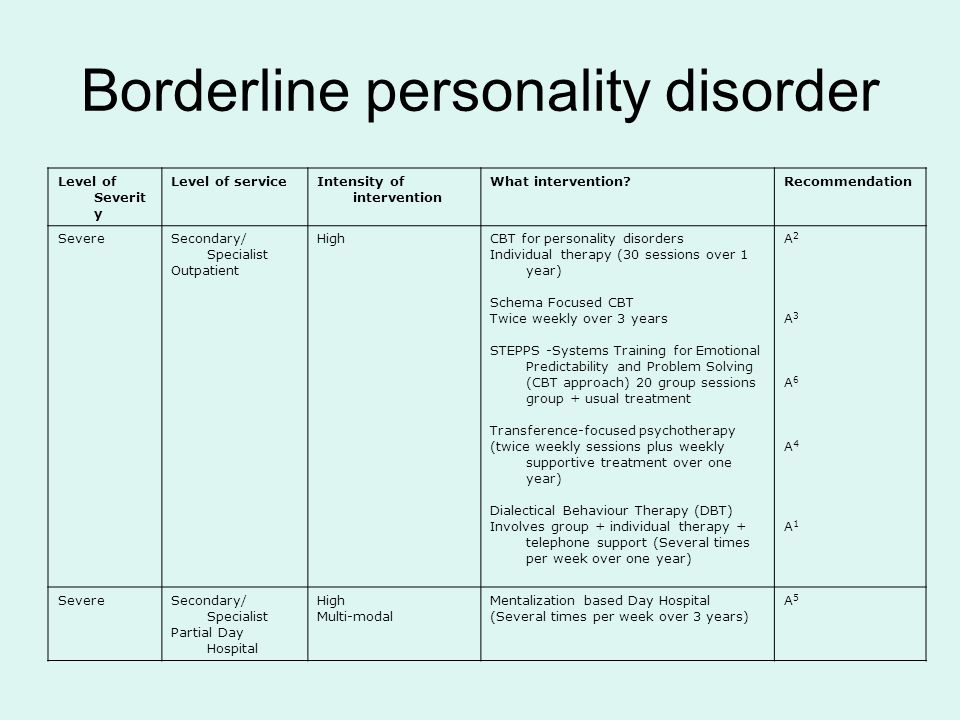
There’s no medication that specifically treats borderline personality disorder. But there are therapies, like dialectical behavior therapy (DBT), which is the go-to treatment. “Trying to get them into a DBT program is very helpful,” Lobel says, because it teaches people with BPD healthier ways to respond and interact.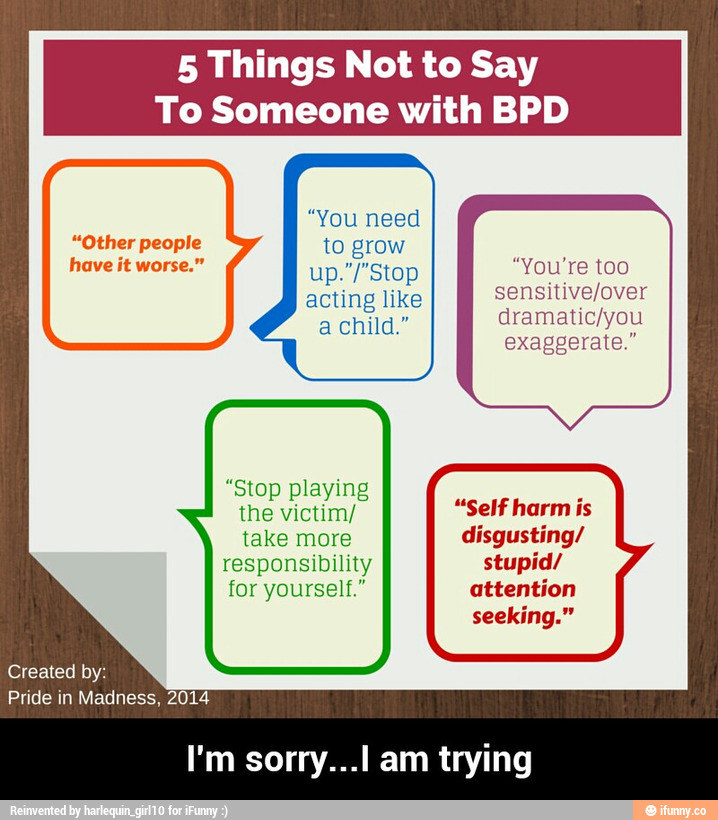 You’ll want to find a therapist who’s has experience working with DBT and with people who have borderline personality disorder.
You’ll want to find a therapist who’s has experience working with DBT and with people who have borderline personality disorder.
Let your loved one know DBT can help anyone, not just folks with BPD, because it “helps people communicate and increase their tolerance for stress.”
Provide recognition when they make progress. “Compliment and comment on any positive changes and behaviors you notice,” Lobel says.
Know When You Need to Protect Yourself
“The ultimate boundary in a relationship with someone who has BPD, is telling them, ‘I just can’t stay,’” Lobel says. How do you know when it’s time to draw that line? Here are a few things to watch out for.
- Physical violence. Nobody should stay in a relationship where there’s continued physical violence, Lobel says. “Someone will get hurt, the police will be involved, nothing good can come from that."
- Too many boundaries. When there are so many topics or kinds of interactions you need to avoid to prevent your partner from lashing out, you’ve removed most of the sources of potential communication, intimacy, and connection.
- Your partner is unwilling to make changes. “If the person insists, ‘there is nothing wrong with me, it’s all you,’ that’s a red flag, and you probably have to pack your bags,” Lobel says.
- Your mood is consistently bad. “Are you walking around miserable all the time?” Lobel asks. “If you feel crappy about this relationship all day, every day, you gotta go.”
Know When to Protect Your Partner
One symptoms of BPD is self-harm, like cutting, or suicidal gestures such as overdose. If you see your partner injuring themselves, call 911.
Treatments for Borderline Personality Disorder (BPD)
Written by WebMD Editorial Contributors
In this Article
- Counseling
- Medication
- Other Tips
The main treatment for borderline personality disorder (BPD) is a combination of counseling and medication.
Counseling
The goal of counseling, also called psychotherapy or talk therapy, is to help you learn how to manage your emotions.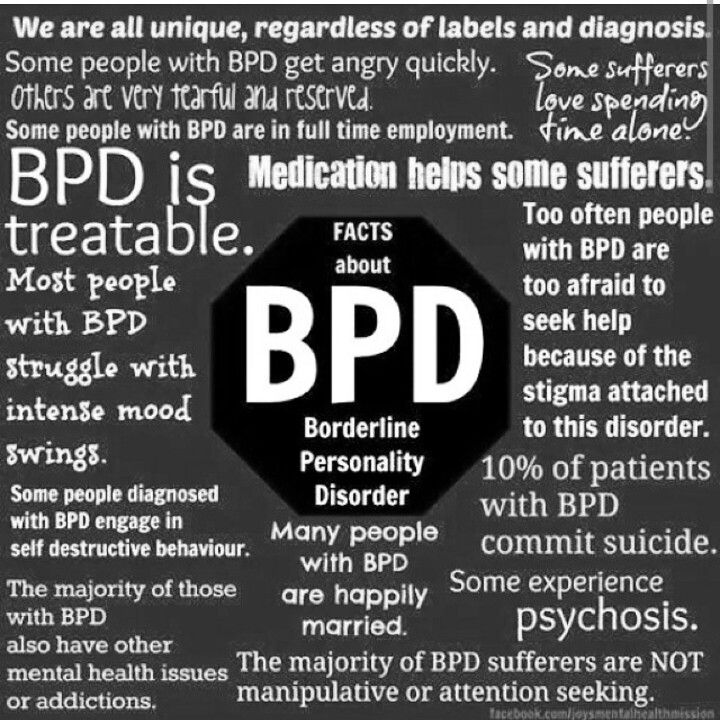 For example, you can observe your feelings ("I feel very angry right now") instead of acting on them. It helps you function in your daily life and relationships. Counseling can happen in a one-on-one setting with a therapist or in a group.
For example, you can observe your feelings ("I feel very angry right now") instead of acting on them. It helps you function in your daily life and relationships. Counseling can happen in a one-on-one setting with a therapist or in a group.
Depending on your symptoms and situation, your counselor may use one of these types of psychotherapy:
- Dialectical Behavior Therapy (DBT) began as a way to help manage crisis behavior, such as suicidal behavior or self-harm. It is the most commonly recommended therapy for BPD. It works with the concept of mindfulness, or being present in the moment. This helps you be aware of your emotions, moods, and behavior. You learn skills like how to tolerate negative emotions and how to communicate effectively.
- Cognitive Behavioral Therapy (CBT) focuses on changing the basics of what you believe about yourself and others.
- Schema-Focused Therapy is similar to CBT in how it reframes negative thoughts about yourself into positive ones.
Medication
Medication may also be used to treat your symptoms. Since depression and anxiety can be a big part of BPD, antidepressant and anti-anxiety medicines can be helpful. If you experience intense times of distorted thinking, your counselor may suggest an anti-psychotic medication.
Since behaviors of self-harm like cutting and suicide attempts are part of the symptoms of BPD, you may need to receive treatment in the hospital.
Other Tips
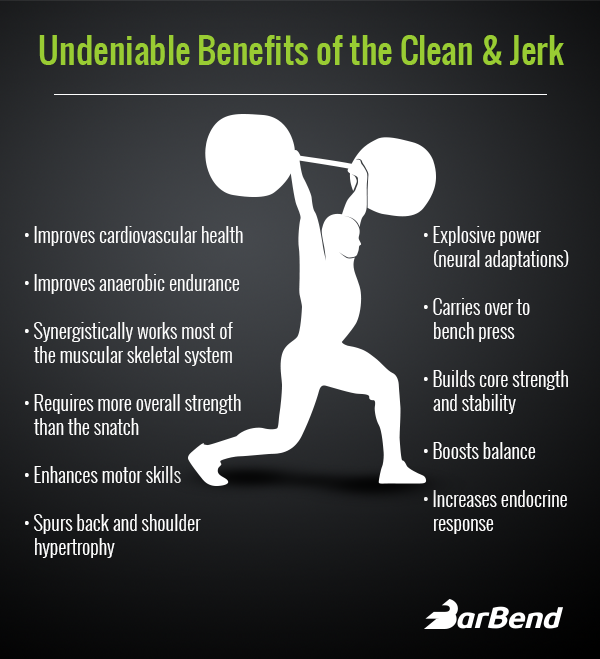
It’s possible to change the way you think, feel, and react to situations. It just takes time and effort. Being consistent with your treatment -- taking medications on schedule, keeping counseling appointments -- is the best way to start.
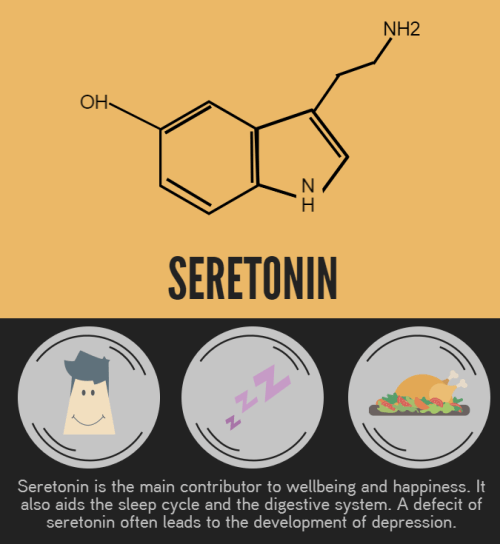
Routine is helpful in other ways, too. Regular meal and sleep times let your body know what to expect. Try to exercise daily too. It keeps stress levels low. Take a walk, don't sign up for a marathon -- it's important to set goals you know you can accomplish without getting overwhelmed.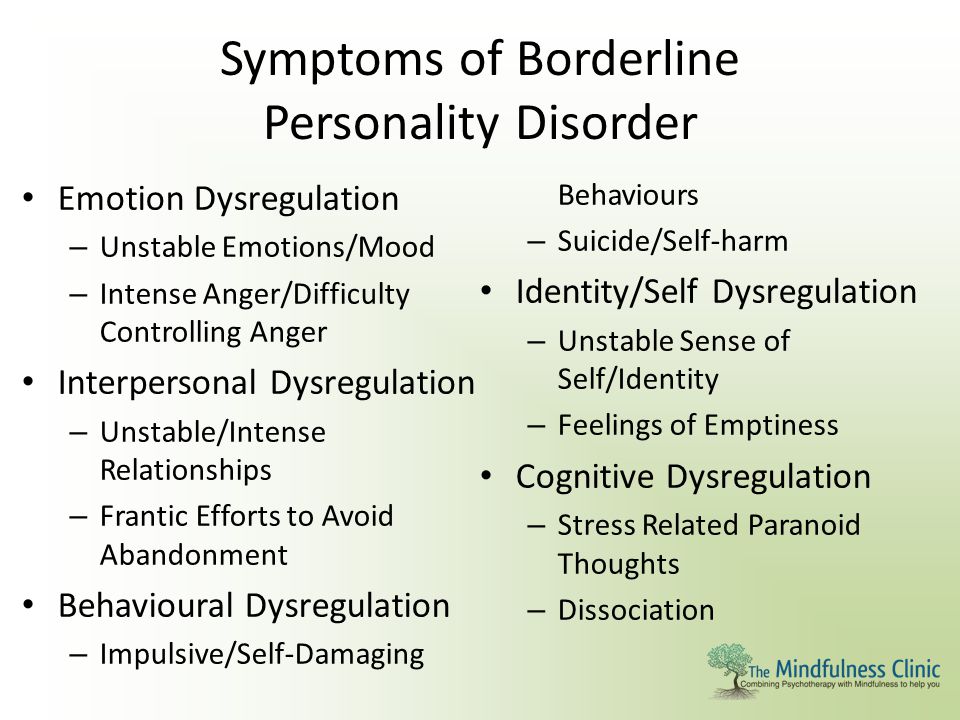
Eat more fruits and vegetables and less junk food. Steer clear of alcohol and drugs.
Surround yourself with people you can trust, including family, friends, and your treatment team. Talk with them about how you're feeling. It's better than keeping it all bottled up inside. If you notice a person or situation that triggers you, write it down and talk to your counselor about it.
The best medicine of all is being kind to yourself. Build support for yourself and use it. Having BPD isn't your fault, but you can change how it affects your life.
© 2021 WebMD, LLC. All rights reserved. View privacy policy and trust infoBorderline personality disorder
Borderline personality disorder is associated with unstable mood and behavior that has a significant impact on a person's daily life
Borderline personality disorder is a type of personality disorder in which a person experiences periods of tension, unstable moods and behaviors, and an altered "feeling of self".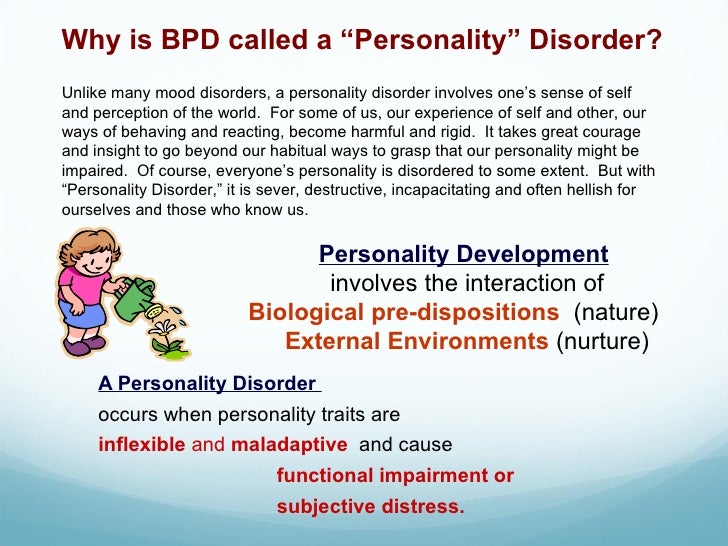 1 All of these can result in impulsive actions and relationship problems with friends and family members, impairing the person's ability to cope with everyday life. nine0005 1.2
1 All of these can result in impulsive actions and relationship problems with friends and family members, impairing the person's ability to cope with everyday life. nine0005 1.2
Borderline personality disorder is a serious illness associated with self-harm and suicidal attempts. One in ten patients complete suicide. 2
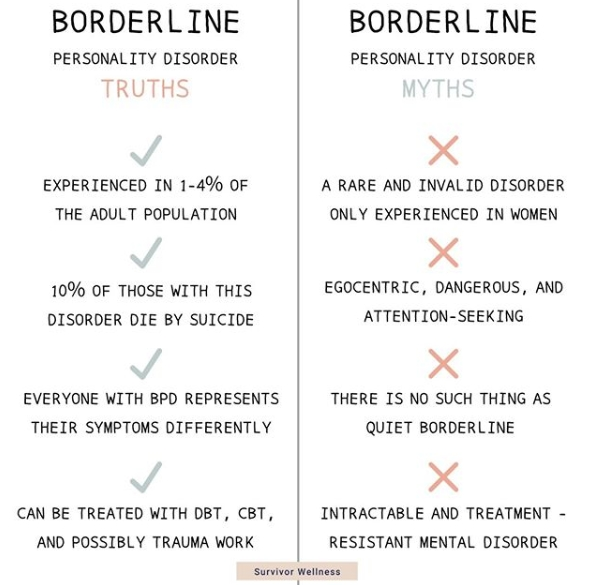
Facts About Borderline Personality Disorder
Borderline personality disorder is a type of personality disorder in which a person experiences periods of tension, unstable mood and behavior, and an altered sense of self. nine0005 1
One in ten patients complete suicide. 2
Patients with borderline personality disorder are very sensitive to changes in their environment, and may respond inappropriately and acutely to such changes. They may, for example, be afraid of being abandoned by a loved one. 2 If the person whom patient
2 If the person whom patient
is expecting arrives late, the patient easily changes the feeling of attachment to dislike or anger.1,2 This reflects the extreme perception of the world by the patient, who sees everything and everyone - including oneself – either good or bad.1,2
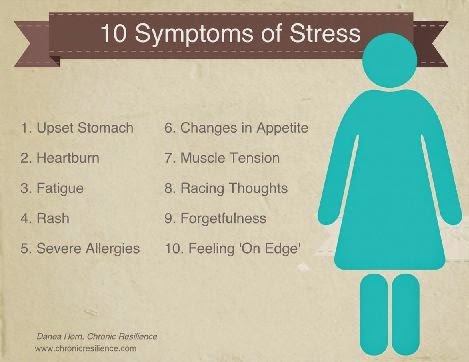
People with borderline personality disorder are often insecure, may suddenly change their life goals and views on career, life values and friends. .2 They may develop intense unwarranted anger or feelings of emptiness, and are prone to self-harm.2 Patients with borderline personality disorder may also experience depression and anxiety.1,2
Facts about Borderline Personality Disorder
Estimates of the proportion of people who have borderline personality disorder vary from less than 1% to around 6%. 2-4
Borderline personality disorder affects a roughly equal number of men and women, but appears to be more disabling in women the same frequency in men and women, but in women it is more severe.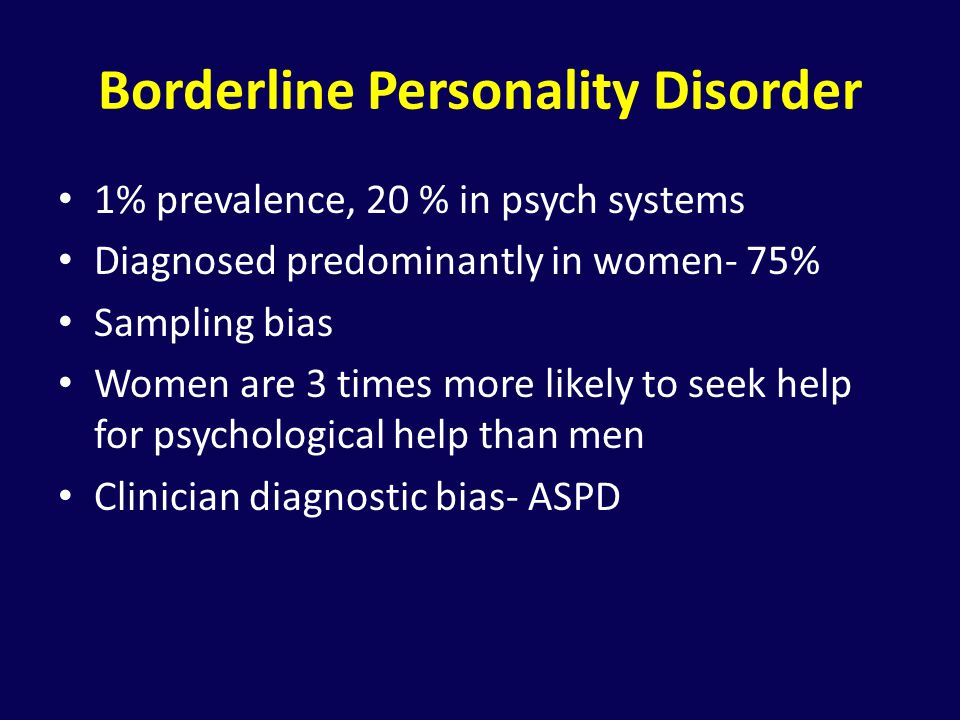 3
3
Symptoms of borderline personality disorder most often first appear during adolescence.4 The disease is most severe and problematic in young adults and tends to improve with age.2 Symptoms may persist throughout life, but most patients with borderline personality disorder by the age of 30-40 have a stable job and a home.2
People with borderline personality disorder are emotionally and functionally unstable, which places a significant burden on their families.5 Mood swings are a source of stress for both the patient and his/her others, which can lead to the development of mental disorders in the latter.1,5
People who are concerned that they – or their loved ones – are experiencing symptoms of borderline personality disorder should see their doctor for help and advice.
Borderline personality disorder is diagnosed by a mental health professional using interviews and discussions about symptoms and medical history. 1
1
Psychotherapy can help people with borderline personality disorder by, for example, teaching them how to interact with others and to express their thoughts and feelings more clearly. nine0005 1 It may also be beneficial for caregivers and family members of those affected to receive therapy and guidance on how best to care for a person with borderline personality disorder. 1 There is currently no cure, but one study showed that, after 10 years, 50% of people with borderline personality disorder had recovered, being able to function at work and maintain personal relationships. 6
- National Institute of Mental Health. borderline personality disorder. NIH publication number QF 17-4928. Available from: https://www.nimh.nih.gov/health/publications/borderline-personality-disorder/index.shtml [accessed 30 September 2019].
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders.
 5th ed. Arlington, VA: American Psychiatric Association; 2013.
5th ed. Arlington, VA: American Psychiatric Association; 2013. - Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533–545.
- National Institute for Health and Clinical Excellence. Borderline personality disorder: recognition and management. 2009. Available from: https://www.nice.org.uk/guidance/cg78/resources/borderline-personality-disorder-recognition-and-management-pdf-975635141317 [accessed 30 September 2019].
- Bailey RC, Grenyer BFS. Burden and support needs of carers of persons with borderline personality disorder: a systematic review. Harv Rev Psychiatry. 2013;21(5):248–258. nine0097
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. Time to attainment of recovery from borderline personality disorder and stability of recovery: a 10-year prospective follow-up study.
 Am J Psychiatry. 2010;167(6):663–667.
Am J Psychiatry. 2010;167(6):663–667.
1. National Institute of Mental Health. borderline personality disorder. NIH publication number QF 17-4928. Available from: https://www.nimh.nih.gov/health/publications/borderline-personality-disorder/index.shtml [accessed 30 September 2019].
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
3. Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533–545.
4. National Institute for Health and Clinical Excellence. Borderline personality disorder: recognition and management. 2009. Available from: https://www.nice.org.uk/guidance/cg78/resources/borderline-personality-disorder-recognition-and-management-pdf-975635141317 [accessed 30 September 2019].
Access to Brain Health
We are dedicated to improving access to brain health in accordance with WHO.
Our Science
Lundbeck has developed some of the world’s most widely prescribed therapies.
This is Lundbeck nine0018
A specialized pharmaceutical company focused exclusively on brain diseases.
Treatment of borderline personality disorder in St. Petersburg
- Main
- Psychiatry
- Treatment of borderline disorder
Interest in borderline personality disorder (F60.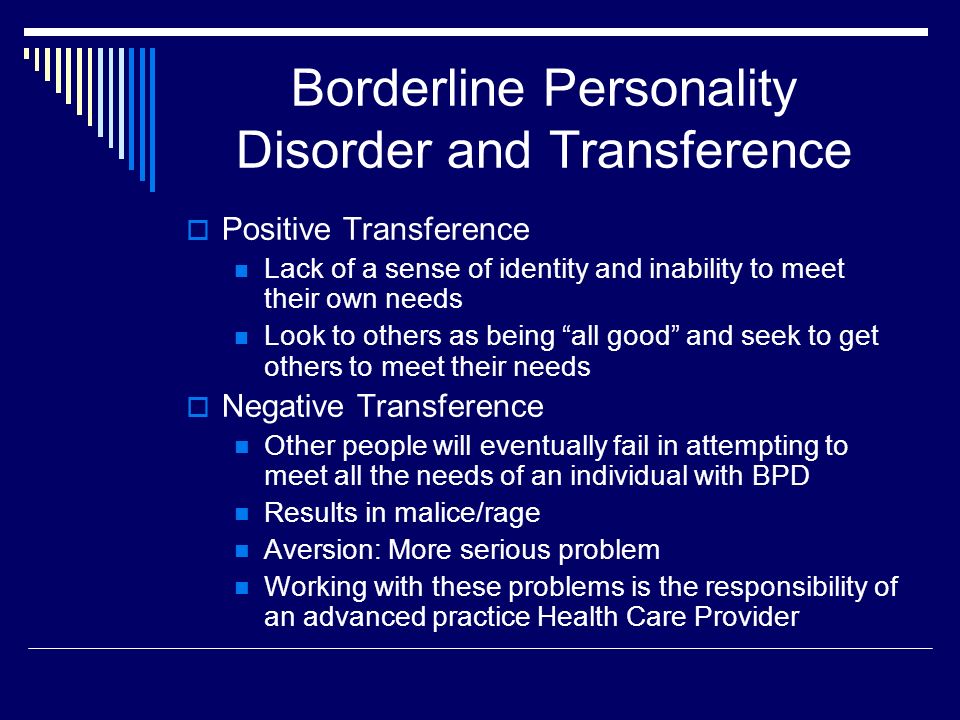 3 according to ICD-10) in our country is not so pronounced, in contrast to the interest of Western psychiatrists and psychotherapists, who consider this disease poorly understood. This is partly due to the increased focus on bipolar affective disorder, whose symptoms are similar to those of borderline personality disorder. nine0003
3 according to ICD-10) in our country is not so pronounced, in contrast to the interest of Western psychiatrists and psychotherapists, who consider this disease poorly understood. This is partly due to the increased focus on bipolar affective disorder, whose symptoms are similar to those of borderline personality disorder. nine0003
Unfortunately, the symptoms of borderline personality disorder are perceived by loved ones as personality traits. However, over time, they lead to deeper problems and often lead to the development of serious mental disorders.
Diagnosis of borderline personality disorder today is difficult due to the lack of a single description of the disease. However, the main symptoms of borderline personality disorder are commonly referred to as:
- fear of loneliness;
- depression;
- instability of personal relationships;
- excessive impulsiveness;
- suicidal behavior.
In our clinic, the treatment of borderline personality disorder is carried out by psychotherapists, and in the presence of associated complications (eg chronic depression) by psychiatrists. Depending on the case, treatment may be outpatient or inpatient (for example, for severe suicidal behavior). The prognosis for treatment of borderline personality disorder is favorable. nine0003
Depending on the case, treatment may be outpatient or inpatient (for example, for severe suicidal behavior). The prognosis for treatment of borderline personality disorder is favorable. nine0003
Borderline Disorder Doctor's Consultation:
+7 (812) 407-18-00
Thank you for your trust!
- Expert pharmacotherapy
- Psychotherapists with clinical experience
- Assistance in resocialization
| Service | Price | |
|---|---|---|
| Outpatient treatment | ||
| Psychiatric consultation | 5 000 ₽ | |
| Psychotherapist appointment | 5 000 ₽ | |
Reception of the chief physician Bocharov A.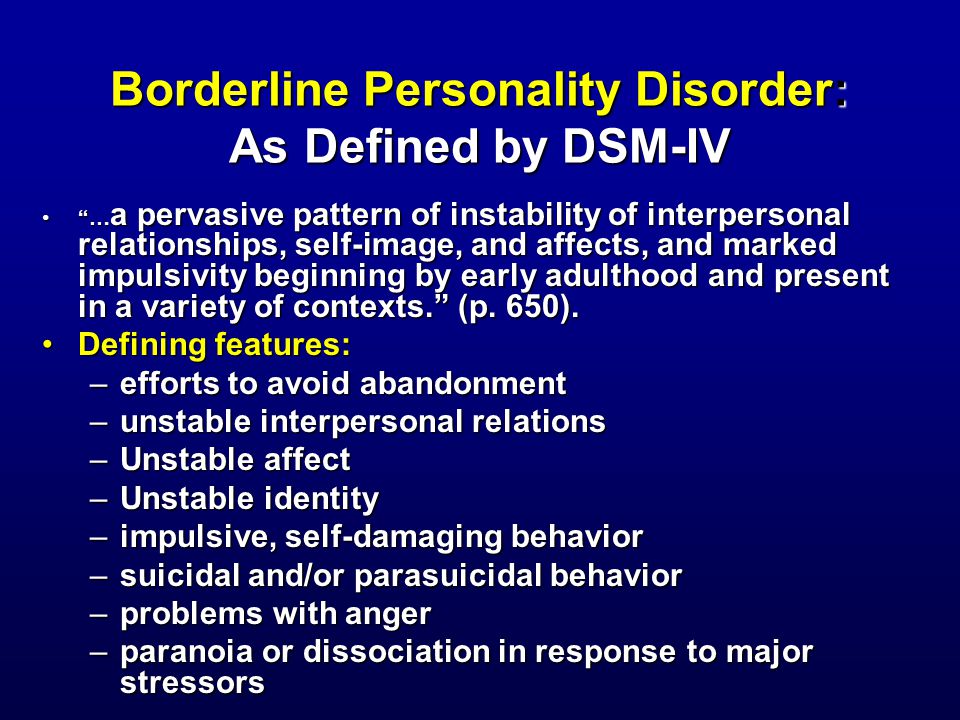 V. (Associate Professor, PhD) V. (Associate Professor, PhD) | 6 000 ₽ | |
| Psychiatric consultation at home | 6 000 ₽ | |
| Inpatient treatment | ||
| Delivery to hospital | Is free nine0193 | |
| Standard chamber | 8 900 ₽ | |
| 3-bed superior room | nine0196 12 000 ₽ | |
| 2-bed superior room | 15 000 ₽ | |
| 1 local VIP room | 19 500 ₽ | |
| Doctor's appointment 2 weeks after discharge | Is free | |
Differential diagnosis of PCR
The ICD-10 classification has a heading (F60) that describes specific personality disorders, including borderline mental disorders.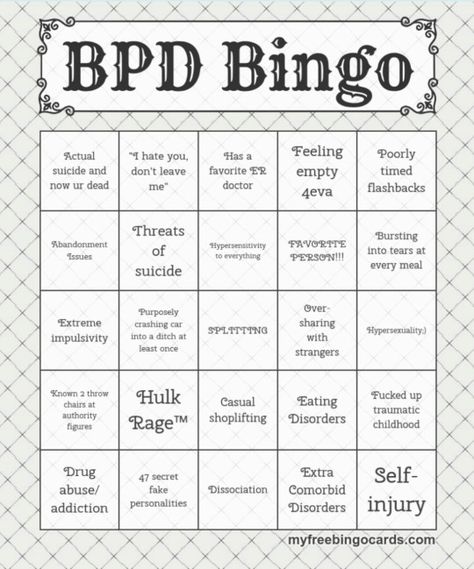 Rubric diseases are characterized by obvious personality disorders and deviations from normal behavior. nine0003
Rubric diseases are characterized by obvious personality disorders and deviations from normal behavior. nine0003
As a rule, diseases of this group develop during childhood and adolescence. Their peak is accompanied by social self-isolation and pathological inner experiences that affect relationships with loved ones and the quality of life in general.
| Paranoid personality disorder (F60.0) | Sensitivity to failure, suspicion, perverted interpretation of the actions of others, hostility, disregard for other people, resentment, exaggerated self-esteem. nine0193 |
|---|---|
| Schizoid personality disorder (F60.1) | Insularity, inclination to solitude, fear of expressing feelings and emotions, lack of attachment to relatives and close people. |
| Antisocial personality disorder (F60.2) | Indifference to others, disregard for social obligations and norms, touchiness, aggressiveness, tendency to self-justify.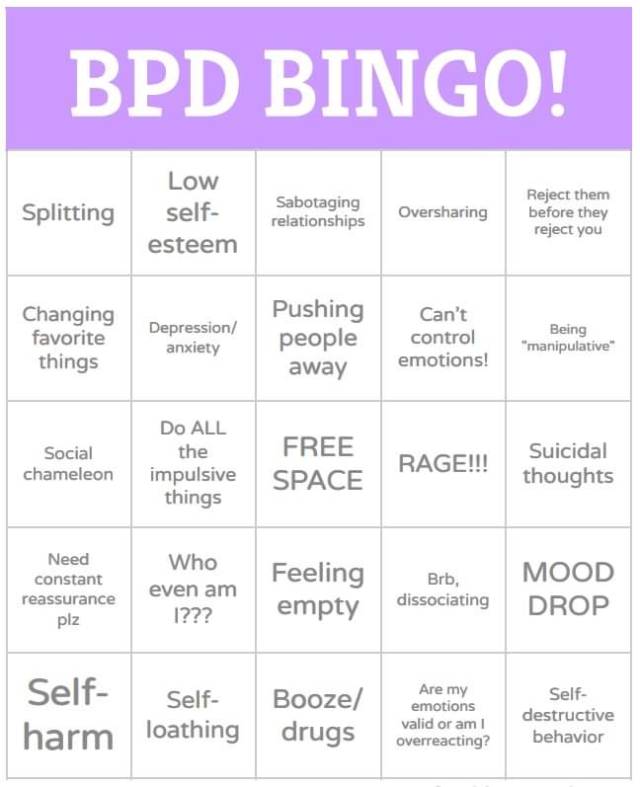 |
| Emotionally unstable personality disorder (F60.3) | Impulsiveness, emotional instability, lack of self-control, feeling of "inner emptiness", unstable interpersonal relationships, suicidal behavior, addiction to alcohol and psychoactive substances. |
| Histrionic personality disorder (F60.4) | Increased excitability, emotional instability, excessive "theatricality" of behavior and "dramatization", suggestibility, egocentrism, neglect of relatives and others. nine0193 |
| Anancaste personality disorder (F60.5) | Self-doubt, caution, preoccupation with trifles, inflexibility, isolation. |
| Anxious personality disorder (F60.6) | Tension, depression, feeling of inferiority, anxiety, acute reaction to criticism, tendency to exaggerate any danger, narrow social ties. |
| Dependent personality type disorder (F60.7) | Passivity, indecision, fear of loneliness, low self-esteem. |
Treatment of a borderline personality disorder
Assistance in resocialization
Information for specialists
There is no pharmacotherapy scheme that would have a positive effect on all symptoms of the border facility of the personality (PROL). The following are recommendations for the treatment of BPD, as well as data on the effectiveness of specific drugs or groups of drugs for specific symptom domains. nine0003
Specialists are advised to use psychotropic drugs only in the presence of comorbid pathology or the need to relieve emergency conditions. In addition, the minimum number of drugs should be chosen, avoiding non-specific polypharmacy [1]
Antidepressants . There is insufficient evidence for prescribing antidepressants to patients with BPD, except in cases of comorbidity with depression or anxiety disorders [1]. The SSRI group is one of the most commonly used in BPD, but new evidence suggests no positive effect of fluoxetine in preventing suicidal behavior [5]
Antipsychotics . Classical antipsychotics do not show any effect on BPD symptoms, except for the reduction of impulsive-aggressive manifestations during acute conditions, and side effects severely limit their use [1].
Classical antipsychotics do not show any effect on BPD symptoms, except for the reduction of impulsive-aggressive manifestations during acute conditions, and side effects severely limit their use [1].
Studies published in recent years provide limited evidence for the efficacy of some atypical antipsychotics. When used for six months or less, antipsychotics are effective for paranoia, dissociation, mood lability, and anger. Aripiprazole is effective in reducing anger, impulsivity, depression and anxiety. Olanzapine showed modest improvements in anger and anxiety [6]. nine0003
Mood stabilizers . Recommendations for the use of mood stabilizers are as follows: mood stabilizers (valproate, topiramate, and lamotrigine) are effective for symptoms such as impulsive-behavioral dyscontrol, affective instability, and cognitive-perceptual symptoms [1]. Topiramate was effective on impulsivity, anxiety and anger. Valproate caused improvements in anger and depression [6].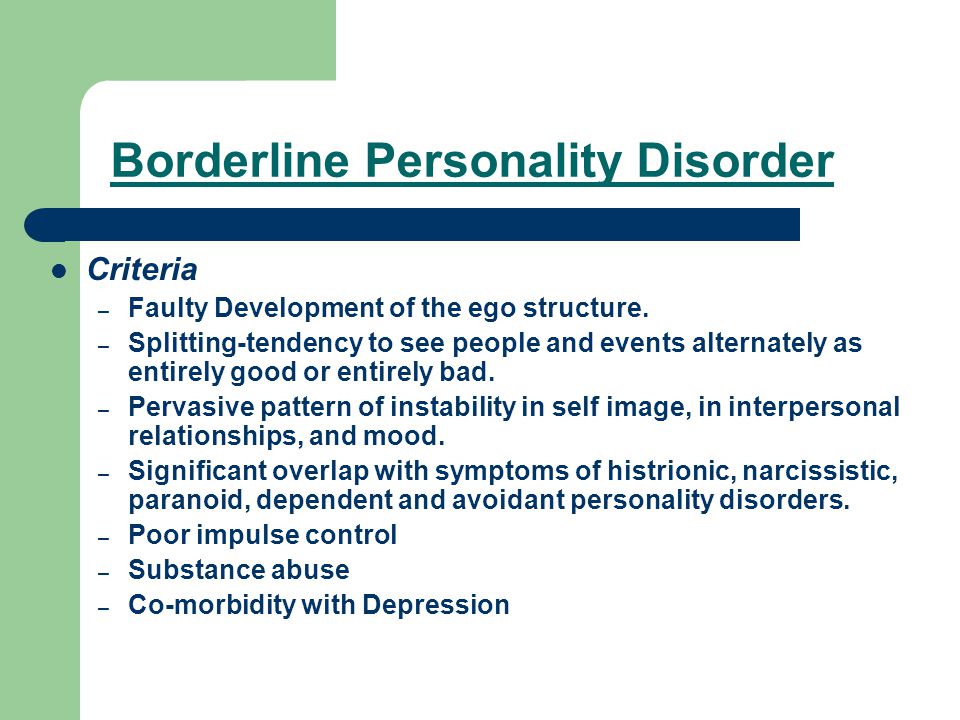 For lamotrigine, results are inconsistent. This drug has shown positive activity in relation to impulsivity and anger [6], but according to the results of randomized clinical trials, it is not a clinically effective treatment for patients with BPD [7]. nine0003
For lamotrigine, results are inconsistent. This drug has shown positive activity in relation to impulsivity and anger [6], but according to the results of randomized clinical trials, it is not a clinically effective treatment for patients with BPD [7]. nine0003
Other drugs . Omega-3 fatty acid preparations are effective against depressive symptoms in BPD [6]. Evidence suggests that omega-3 fatty acids have a positive effect on impulsive behavior and affective dysregulation. Omega-3 fatty acids, which have a high level of tolerance with minimal or no side effects, can be considered as an additional therapy [8].
Psychotherapy and psychopharmacotherapy . Combining psychotropic drugs with psychotherapy has been shown to provide better results than single treatments for several of the main symptoms of BPD. Currently, psychotherapy is the recommended first line strategy in the treatment of BPD [2]. Systematic reviews and meta-analyses confirm the positive impact of psychotherapeutic interventions (primarily dialectical behavioral psychotherapy) on psychosocial functioning, severity, as well as self-injurious and suicidal behavior in BPD [2, 3].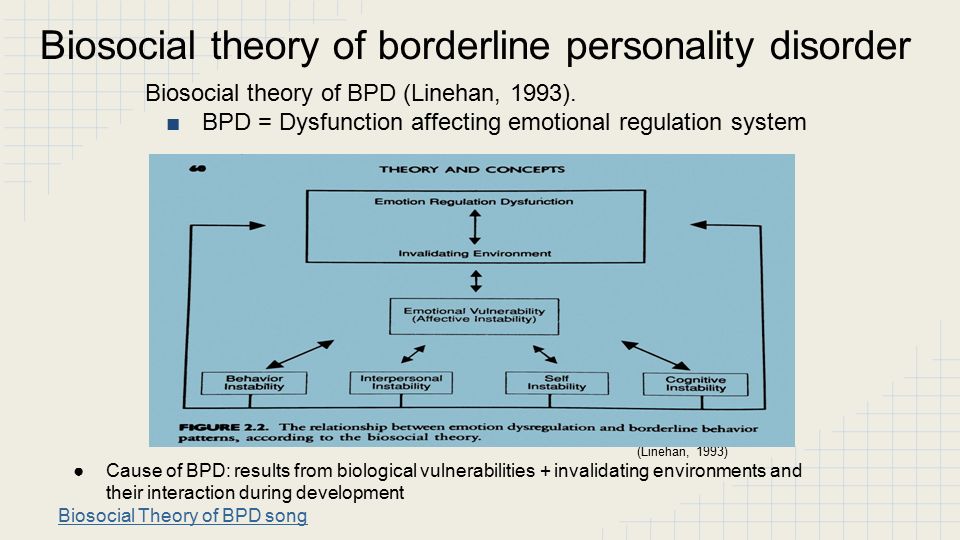 However, there is a low adherence of patients to psychotherapeutic methods [4]. nine0003
However, there is a low adherence of patients to psychotherapeutic methods [4]. nine0003
Based on the available evidence, psychotherapy targeting drug-resistant symptom domains such as fear of abandonment, feelings of emptiness, and identity disturbance, in conjunction with the use of mood stabilizers or atypical antipsychotics, appears to be the most promising therapeutic tool in the treatment of patients with BPD [1].
Author: Dolina A.A.
Edition: Kasyanov E.D.
Literature:
- Bozzatello P, Rocca P, De Rosa ML, Bellino S. Current and emerging medications for borderline personality disorder: is pharmacotherapy alone enough? Expert Opin Pharmacother. 2020 Jan;21(1):47-61. doi: 10.1080/14656566.2019.1686482. Epub 2019 Nov 6. PMID: 31693423.
- Bohus M, Stoffers-Winterling J, Sharp C, Krause-Utz A, Schmahl C, Lieb K. Borderline personality disorder. Lancet. 2021 Oct 23;398(10310):1528-1540.
 doi: 10.1016/S0140-6736(21)00476-1. PMID: 34688371
doi: 10.1016/S0140-6736(21)00476-1. PMID: 34688371 - Stoffers-Winterling J, Storebø OJ, Lieb K. Pharmacotherapy for Borderline Personality Disorder: an Update of Published, Unpublished and Ongoing Studies. Curr Psychiatry Rep. 2020 Jun 5;22(8):37. doi: 10.1007/s11920-020-01164-1. PMID: 32504127; PMCID: PMC7275094
- Chapman J, Jamil RT, Fleisher C. Borderline Personality Disorder. 2021 Aug 1. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 28613633
- Stoffers-Winterling J, Storebø OJ, Lieb K. Pharmacotherapy for Borderline Personality Disorder: an Update of Published, Unpublished and Ongoing Studies. Curr Psychiatry Rep. 2020 Jun 5;22(8):37. doi:10.1007/s11920-020-01164-1. PMID: 32504127; PMCID: PMC7275094.
- Justin D. Parker, Aimen Naeem. Pharmacologic Treatment of Borderline Personality Disorder. American Family Physician. 2019;99(5):333A-333B
- Stoffers-Winterling J, Storebø OJ, Lieb K. Pharmacotherapy for Borderline Personality Disorder: an Update of Published, Unpublished and Ongoing Studies.
 Curr Psychiatry Rep. 2020 Jun 5;22(8):37. doi: 10.1007/s11920-020-01164-1. PMID: 32504127; PMCID: PMC727509
Curr Psychiatry Rep. 2020 Jun 5;22(8):37. doi: 10.1007/s11920-020-01164-1. PMID: 32504127; PMCID: PMC727509 - Karaszewska DM, Ingenhoven T, Mocking RJT. Marine Omega-3 Fatty Acid Supplementation for Borderline Personality Disorder: A Meta-Analysis. J Clin Psychiatry. 2021 May 4;82(3):20r13613. doi: 10.4088/JCP.20r13613. PMID: 34004088 What are the treatments for borderline personality disorder? — https://www.webmd.com
- Depersonalization and derealization
- Suicidal behavior
- Anxiety disorder
Update date: 03/04/2022
Make an appointment
Date and time: (not set)
Make an appointment with a psychiatrist
Make an appointment with a psychiatrist
Select the date and time of your appointment
Today
January 02
Tomorrow
January 03
Wednesday
January 04
Thursday
05 January
Friday
January 06
Saturday
January 07
Sunday
January 08
Monday
January 09
Tuesday
January 10
Wednesday
January 11
Thursday
January 12
Friday
January 13
Saturday
January 14
Sunday
January 15
Monday
January 16
Tuesday
January 17
Wednesday
January 18
Thursday
January 19
Friday
January 20
Saturday
January 21
Sunday
January 22
Monday
January 23
Tuesday
January 24
Wednesday
January 25
Thursday
January 26
Friday
January 27
Saturday
January 28
Sunday
January 29
Monday
January 30
Tuesday
January 31
Treatment for borderline personality disorder
Bocharov Alexey
Viktorovich
Psychiatrist, psychotherapist
Head physician of clinic
Experience 41 years
Psychiatrist, psychotherapist, sexologist, child psychiatrist
Work experience 41 years
Sinenchenko Andrey
Georgievich
Psychiatrist, psychotherapist
PhD
Work experience 22 years
Psychiatrist, psychotherapist, narcologist
Work experience 22 years
Zun Sergey
Andreevich
Psychiatrist, narcologist
PhD
Experience 33 years
Psychiatrist, narcologist, psychotherapist
Work experience 33 years
Lisitsyna Elena
Alekseevna
Psychiatrist
Top category
Experience 33 years
Psychiatrist
Work experience 33 years
Buchelnikova Victoria
Viktorovna
Psychiatrist
Head of amb.