Third wave cognitive behavioral therapy
What is Third Wave Cognitive Behavioral Therapy?
About
What is meant by “Third Wave?”
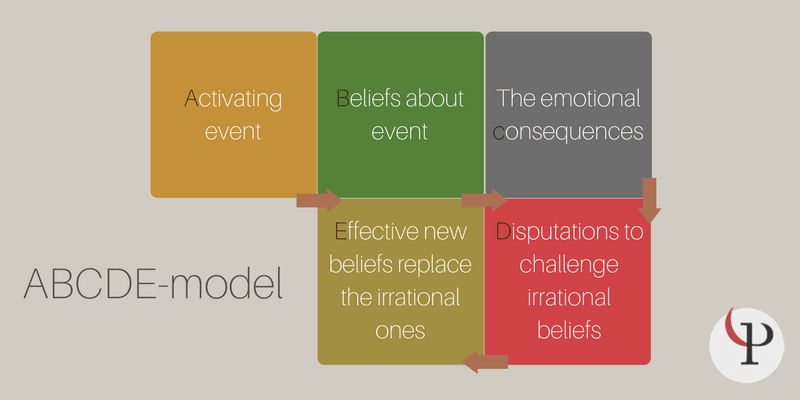
The “first wave” of behavioral therapies were characterized by behaviorism (i.e., operant conditioning, classical conditioning). Albert Ellis and Aaron Beck pioneered the “second wave” of behavioral therapies with cognitive behavioral therapy (CBT), which integrated a person’s thoughts and beliefs in understanding and changing behavior and emotional experiences such as depression.
“Third wave” cognitive behavioral therapies are a group of emerging approaches to psychotherapy that represent an evolution and extension of traditional cognitive behavioral treatment approaches. Third wave therapies prioritize the holistic promotion of psychological and behavioral
processes associated with health and well-being over the reduction or elimination of psychological and emotional symptoms, although that typically is a “side-benefit.” Concepts such as metacognition, acceptance, mindfulness, personal values, and spirituality are frequently incorporated into what might otherwise be considered traditional behavioral interventions. Rather than focusing on the content of a person’s thoughts and internal experiences, third wave behavioral therapists are instead more focused on the context, processes, and functions of how a person relates to internal experiences (i.e., thoughts, urges, sensations). Many of the strategies and interventions utilized in third wave cognitive behavioral therapies complement traditional cognitive behavioral interventions such as exposure therapy (e.g., systematic desensitization) and behavioral activation.
“Grounded in an empirical, principle-focused approach, the third wave of behavioral and cognitive therapy is particularly sensitive to the context and functions of psychological phenomena, not just their form, and thus tends to emphasize contextual and experiential change strategies in addition to more direct and didactic ones. These treatments tend to seek the construction of broad, flexible and effective repertoires over an eliminative approach to narrowly defined problems, and to emphasize the relevance of the issues they examine for clinicians as well as clients. The third wave reformulates and synthesizes previous generations of behavioral and cognitive therapy and carries them forward into questions, issues, and domains previously addressed primarily by other traditions, in hopes of improving both understanding and outcomes.” (from Hayes, 2004).”
The third wave reformulates and synthesizes previous generations of behavioral and cognitive therapy and carries them forward into questions, issues, and domains previously addressed primarily by other traditions, in hopes of improving both understanding and outcomes.” (from Hayes, 2004).”
ACCEPTANCE AND COMMITMENT THERAPY (ACT)
ACT is a behaviorally-oriented therapeutic approach that aims to modify how a person relates and responds to their internal experiences (i.e., thoughts, emotions, physical sensations, and urges) in order to more fully engage in values-based behaviors.
DIALECTICAL BEHAVIOR THERAPY (DBT)
DBT is a form of cognitive-behavioral therapy effective in treating intense emotional reactions and relationship difficulties.
MINDFULNESS-BASED COGNITIVE THERAPY (MBCT)
Through the practice and application of meditation people learn to cultivate a more mindful approach to experiencing difficult thoughts and emotions in order to develop healthier behavioral patterns.
METACOGNITIVE THERAPY (MCT)
Metacognitive therapy is shares similarities with the more traditional Cognitive Therapy, but rather than focusing on the content of thought the emphasis is on exploring a person’s thoughts and beliefs surrounding the content of their thoughts (i.e., metacognitions).
JOIN US!
Are you a mental health professional looking for your clinical home? Whether you are a new or a seasoned mental health professional, we are interested in hearing from you if you are interested in joining a group of passionate, competent clinicians excited about the therapeutic application of mindfulness practice and behavior change.
Today's the day to make a change.
The third wave of cognitive behavioral therapy and the rise of process‐based care
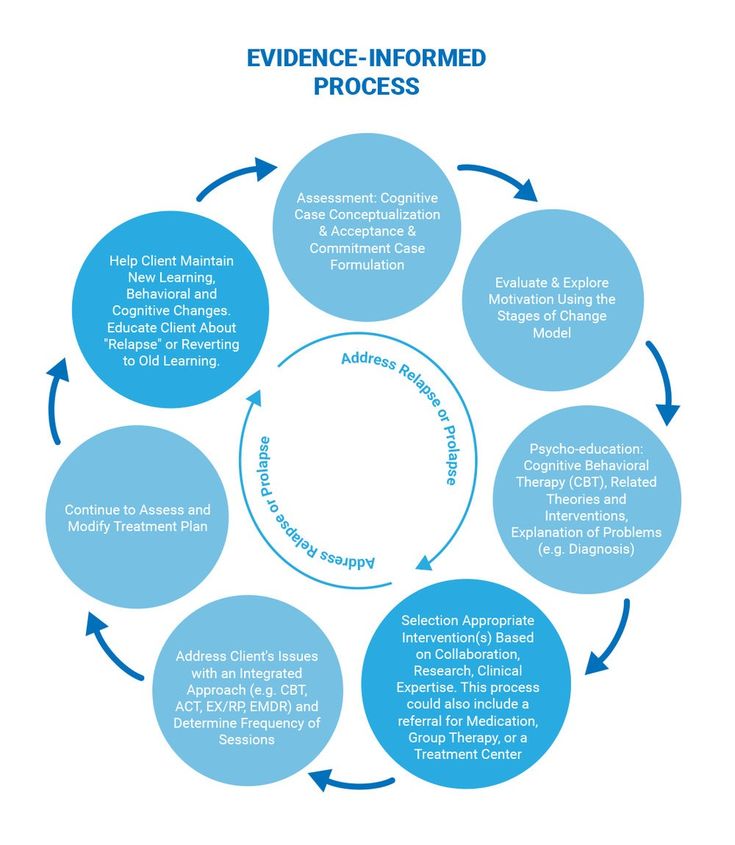
The term cognitive behavioral therapy (CBT) identifies a family of interventions that are widely recognized as the set of psychological treatments with the most extensive empirical support1.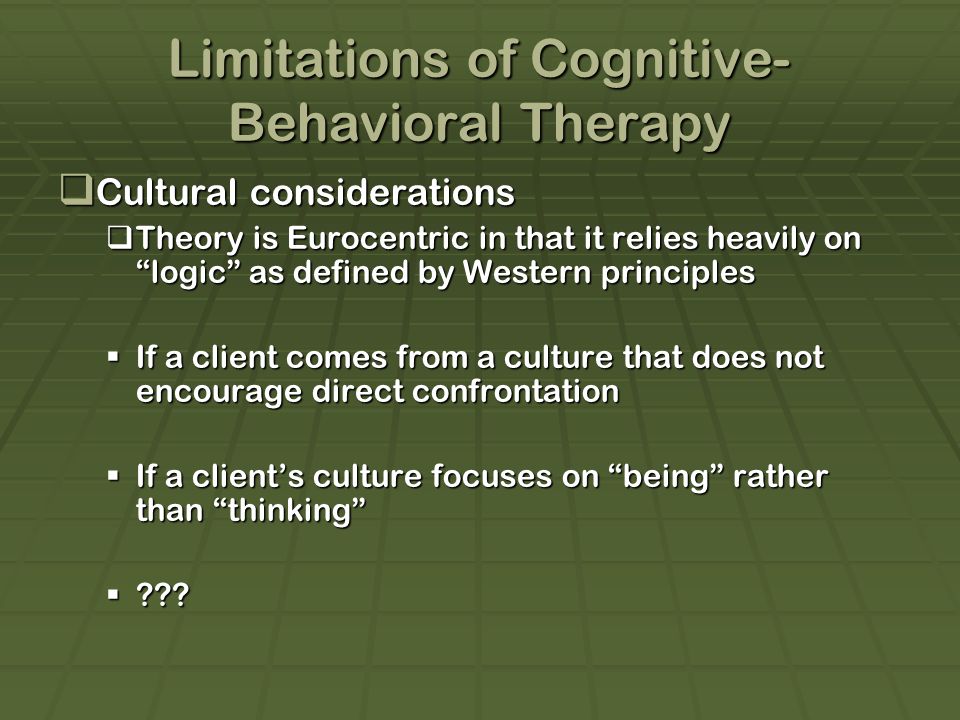 CBT is not monolithic, however, and it has been through several distinct eras, generations, or waves. The first generation of this tradition was behavior therapy: the application of learning principles to well‐evaluated methods designed to change overt behavior. By the late 1970s, behavior therapy had moved into the era of classic CBT: a new generation of methods and concepts focused on the role of maladaptive thinking patterns in emotion and behavior, and the use of methods to detect and change those patterns.
CBT is not monolithic, however, and it has been through several distinct eras, generations, or waves. The first generation of this tradition was behavior therapy: the application of learning principles to well‐evaluated methods designed to change overt behavior. By the late 1970s, behavior therapy had moved into the era of classic CBT: a new generation of methods and concepts focused on the role of maladaptive thinking patterns in emotion and behavior, and the use of methods to detect and change those patterns.
The arrival of a “third wave” of CBT was declared 13 years ago2. The claim was that a change was occurring in orienting assumptions within CBT, and that a set of new behavioral and cognitive approaches were emerging based on contextual concepts focused more on the persons’ relationship to thought and emotion than on their content. Third wave methods emphasized such issues as mindfulness, emotions, acceptance, the relationship, values, goals, and meta‐cognition. New models and intervention approaches included acceptance and commitment therapy, dialectical behavior therapy, mindfulness‐based cognitive therapy, functional analytic psychotherapy, meta‐cognitive therapy, and several others.
The idea that a “third wave” of CBT had arrived led to significant controversy3. The metaphor of a “wave” suggested to some that previous generations of work would be washed away, but that was not the intent and that was not the result. Waves hitting a shore assimilate and include previous waves – but they leave behind a changed shore. It seems to us that we are now in a position to begin to evaluate what will be left behind in a more permanent way from third wave CBT.
There is no doubt that several concepts and methods that have been central to third wave interventions (mindfulness methods; acceptance‐based procedures; decentering; cognitive defusion; values; psychological flexibility processes) are now permanently part of the CBT tradition and indeed of evidence‐based therapy more generally, in large part because evidence suggests that they are helpful4. These newer concepts and methods now largely co‐exist side by side with previously established ones, with the dialectic between them serving as a useful spur to theoretical and technological investigation.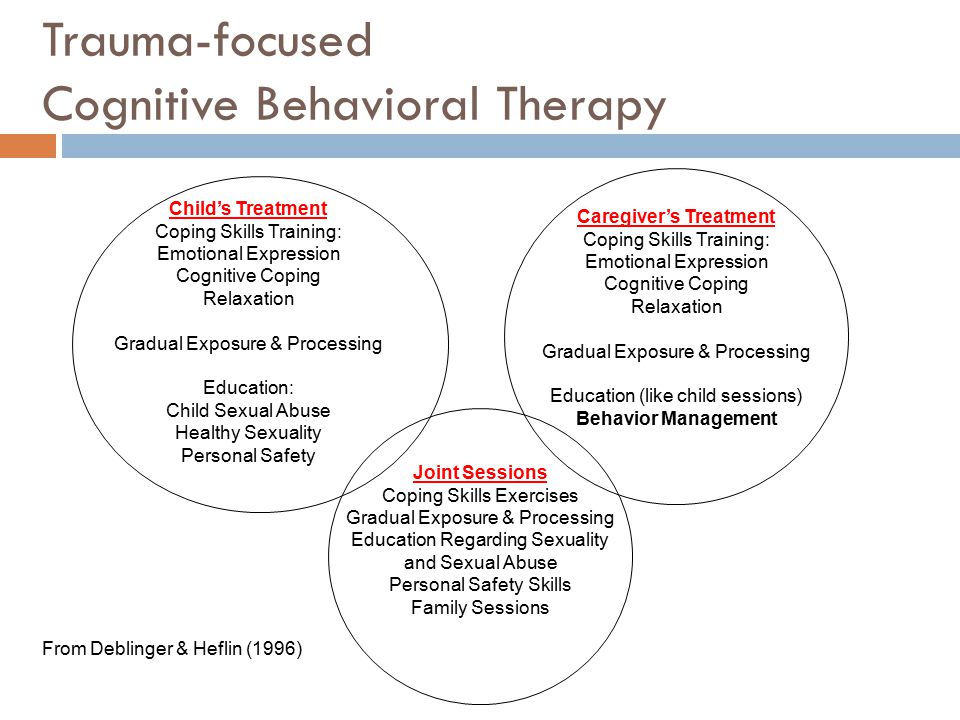 In some cases, we now know that traditional CBT methods work in part by changing processes that became central after the arrival of third wave methods5. Third wave methods have been added to packages that include traditional behavioral and cognitive methods, resulting in useful approaches6. Research has begun to identify moderators indicating when older and newer methods work best with different populations7, suggesting that evidence‐based practitioners can serve their clients by knowing methods from all of the CBT generations.
In some cases, we now know that traditional CBT methods work in part by changing processes that became central after the arrival of third wave methods5. Third wave methods have been added to packages that include traditional behavioral and cognitive methods, resulting in useful approaches6. Research has begun to identify moderators indicating when older and newer methods work best with different populations7, suggesting that evidence‐based practitioners can serve their clients by knowing methods from all of the CBT generations.
While new concepts and methods are important, in our opinion, there is a more profound set of changes that has been introduced by the third wave. A subtle but important change is that there is now greater recognition of the central importance of philosophical assumptions to methods of intervention and their analysis. Science requires pre‐analytic assumptions about the nature of data, truth, and the questions of importance, and some of the differences between the waves and generations of CBT work were philosophical, not empirical. Recognizing this, the Inter‐Organizational Task Force on Cognitive and Behavioral Psychology Doctoral Education8 recently concluded that all CBT training should place more emphasis on philosophy of science training, in the hope of increasing the coherence and progressivity of research programs.
Recognizing this, the Inter‐Organizational Task Force on Cognitive and Behavioral Psychology Doctoral Education8 recently concluded that all CBT training should place more emphasis on philosophy of science training, in the hope of increasing the coherence and progressivity of research programs.
An examination of assumptions leads naturally to a concern for theories, models, and processes. The third wave has been far less focused on protocols for syndromes, and more focused on evidence‐based processes linked to evidence‐based procedures8, 9. Increased emphasis on processes of change and their biobehavioral impact has meanwhile been strengthened by Research Domain Criteria10 and transdiagnostic models, among other trends. A notable result is that there is now much more focus on moderators and mediators of change, and the construction of intervention models that emphasize the role of changeable transdiagnostic processes (i.e., functionally important pathways of change that cut across various diagnostic categories).
In part because of its greater process focus, modern CBT and evidence‐based therapy is more open to the investigation of a wider range of approaches from humanistic, existential, analytic, and spiritual traditions. This promises over time to reduce the dominance within intervention science of walled off schools of thought, or trademarked intervention protocols, and to bring different wings of the field together in an evidence‐based search for coherent and powerful sets of change processes.
As a purely syndromal focus weakens and a process focus strengthens, human psychological prosperity and the thriving of whole persons, not merely psychopathology, is also becoming more central. Behavioral and mental health is ultimately about health, not solely the absence of disorders.
This set of changes is accelerating a transition in evidence‐based care toward a process‐based field that seeks to integrate the full range of psychosocial and contextual biological processes. Such a field is so broad that it stretches the very term CBT almost to a breaking point and we would not be surprised if that term soon wanes in importance.
Such a field is so broad that it stretches the very term CBT almost to a breaking point and we would not be surprised if that term soon wanes in importance.
Researchers and practitioners alike seem ready for a turn toward process‐based therapy (PBT), in which processes, procedures and their linkage are evidence‐based, and are used to alleviate the problems and promote the prosperity of people. Similar to the trend toward personalized and precision medicine, focusing on changeable processes that can make a difference in the behavioral and mental health of individuals provides a way for evidence‐based care and person‐centered care to merge under a single umbrella of process‐based care. Orienting the field in that direction may ultimately be the most important “changed shore” produced by the third wave of CBT.
Steven C. Hayes1, Stefan G. Hofmann21Department of Psychology, University of Nevada, Reno, NV, USA; 2Department of Psychological and Brain Sciences, Boston University, Boston, MA, USA
1. Hofmann SG, Asnaani A, Vonk IJ et al. Cogn Ther Res 2012;36:427‐40. [PMC free article] [PubMed] [Google Scholar]
Hofmann SG, Asnaani A, Vonk IJ et al. Cogn Ther Res 2012;36:427‐40. [PMC free article] [PubMed] [Google Scholar]
2. Hayes SC. Behav Ther 2004;35:639‐65. [Google Scholar]
3. Hofmann SG, Asmundson GJ. Clin Psychol Rev 2008;28:1‐16. [PubMed] [Google Scholar]
4. Khoury B, Lecomte T, Fortin G et al. Clin Psychol Rev 2013;33:763‐71. [PubMed] [Google Scholar]
5. Arch JJ, Wolitzky‐Taylor KB, Eifert GH et al. Behav Res Ther 2012;50:469‐78. [PubMed] [Google Scholar]
6. Arch JJ, Eifert GH, Davies C et al. J Consult Clin Psychol 2012;80:750‐65. [PMC free article] [PubMed] [Google Scholar]
7. Wolitzky‐Taylor KB, Arch JJ, Rosenfield D et al. J Consult Clin Psychol 2012;80:786‐99. [PubMed] [Google Scholar]
8. Klepac RK, Ronan GF, Andrasik F et al. Behav Ther 2012;43:687‐97. [PubMed] [Google Scholar]
9. Hayes SC, Hofmann SG. (eds). Process‐based CBT: the science and core clinical competencies of cognitive behavioral therapy.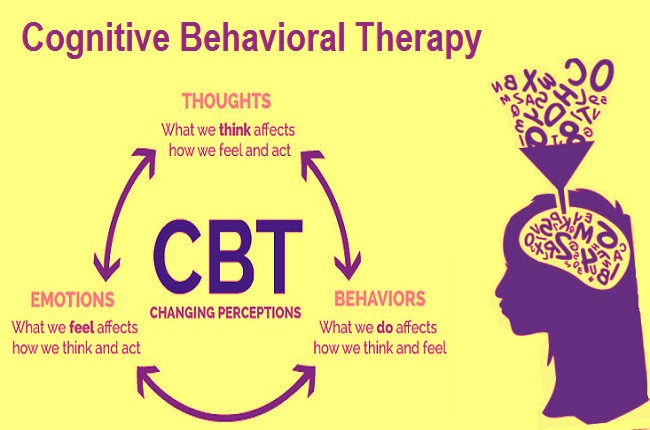 Oakland: New Harbinger, 2017. [Google Scholar]
Oakland: New Harbinger, 2017. [Google Scholar]
10. Insel T, Cuthbert B, Carvey M et al. Am J Psychiatry 2010;167:748‐51. [PubMed] [Google Scholar]
CBT Third Wave
Schema Therapy
Schema Therapy is a method developed by Jeffrey Young in the 1990s. J. Young was a practicing cognitive-behavioral therapist (a student of A. Beck) and sought to find an effective way to help clients for whom solving particular problems led to only a short-term result, after which a new round of suffering began.
J. Young introduced the term "scheme", by which he understood the system of ideas and strategies of behavior formed in childhood. The schema is created on the basis of early experience in satisfying needs and is a partially realized defense mechanism formed as a result of cognitive processing of many situations with a biased selection of the leading elements of the world structure, people, relationships. nine0005
The formed scheme determines the choice of significant people and unconscious expectations from them. Despite the fact that the implementation of the scheme leads to an unsatisfactory quality of life, the person follows it, since the uncertainty associated with abandoning the scheme seems to be a more threatening alternative. Unlike “beliefs”, with which a person, with proper training, is able to dissociate, the scheme largely replaces subjective reality for a person due to early formation and unconsciousness. nine0005
Despite the fact that the implementation of the scheme leads to an unsatisfactory quality of life, the person follows it, since the uncertainty associated with abandoning the scheme seems to be a more threatening alternative. Unlike “beliefs”, with which a person, with proper training, is able to dissociate, the scheme largely replaces subjective reality for a person due to early formation and unconsciousness. nine0005
18 maladaptive schemes according to J. Young indicating the leading need:
Secure attachment.
1. Abandonment.
2. Distrust.
3. Emotional deprivation.
4. Social isolation.
5.Defectiveness.
Sense of identity, autonomy and competence.
6. Addiction.
7. Vulnerability.
8. Merger.
9. Pessimism.
10. Doomed to failure, failure. nine0005
Freedom to express desires and feelings.
11. Submission.
12. Self-sacrifice.
13. Seeking approval/recognition.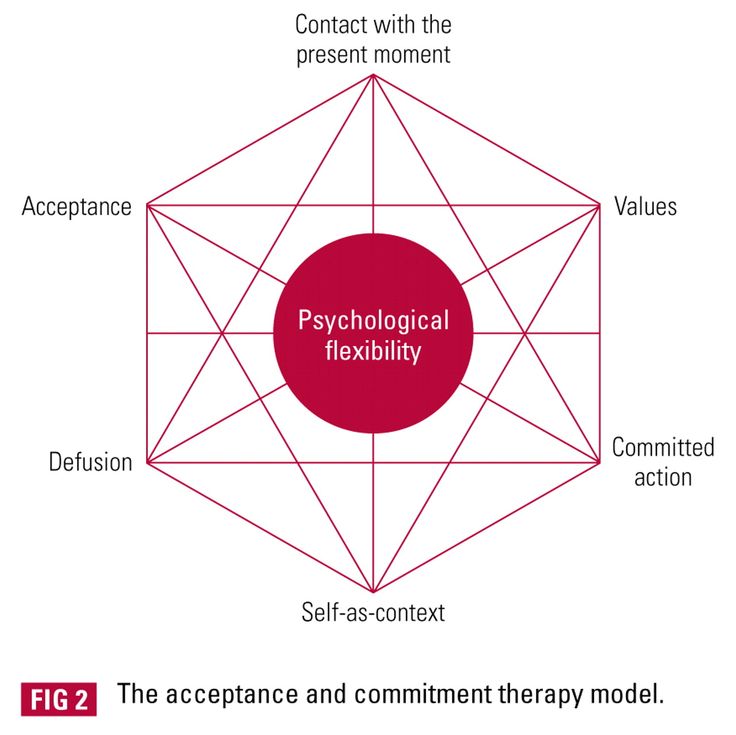
14. Suppression of emotions.
15. Rigid standards.
16. Punitiveness.
Understanding one's abilities and self-discipline:
17. Grandiosity.
18. Lack of self-control.
Because the schema is formed from early traumatic experiences, it causes distress and an urge to deal with it. J. Young singled out three main coping strategies. nine0005
1 The surrender of implies submission to the scheme and its obedient implementation up to the tragic end.
2 Avoidance implies restrictions in the realization of needs, which may imply a negative outcome. "If you don't have a dog, the neighbor won't poison it."
3 Overcompensation involves fighting the circuit in a clearly exaggerated manner. For example, instead of expecting trouble from other people, a person himself becomes a nuisance for everyone, but in the end he still remains alone. nine0005
The current combination of working circuits is called a mode. Each person has a set of modes for different roles and situations. Schema therapy assumes the client's responsibility for schema creation and operates with a range of tools to help change existing schemas.
Each person has a set of modes for different roles and situations. Schema therapy assumes the client's responsibility for schema creation and operates with a range of tools to help change existing schemas.
1. Classical CBT tools aimed at working with the cognitive sphere.
2. Tools of the humanistic direction of psychotherapy for the formation of high-quality therapeutic relationships and work with the emotional sphere. nine0005
3. Active imagination techniques (for example, rescripting) aimed at changing the emotional component of memories of the past.
Acceptance and Responsibility Cognitive Behavioral Therapy (ACT): Third Wave Therapy
SELECT A PSYCHOLOGIST
Cognitive Behavioral Therapy (CBT) is a direction that helps the client to get rid of irrational attitudes and develop more successful behavior patterns. Over time, CBT has evolved into a separate movement called Third Wave Cognitive Behavioral Therapy. nine0079
alter
DESTINATION GUIDE
Contents
1. First, second and third wave - what is the difference
First, second and third wave - what is the difference
2. Third Wave CBT Basic Principles
3. Acceptance and responsibility therapy: “truth is what works”
4. Dialectical Behavior Therapy: "a life worth living"
5. Mindfulness-based cognitive therapy
6. Schema Therapy
7. Case study
8. What to read?
The first, second and third wave - what is the difference
The first wave was directly behaviorism - a branch of psychology that dealt with human behavior. The second wave is CBT, which combined behavioral theory and cognitivism. In the third wave, CBT-based approaches began to emerge that focused more on awareness and acceptance. Third wave CBT includes techniques borrowed from other areas of psychotherapy, as well as some practices of Eastern philosophy, such as meditation. nine0005
While classical CBT focuses more on problems and negative patterns that need to be changed, Third Wave CBT helps the client to accept himself and his characteristics. This does not mean that there are no changes in therapy. The therapist helps the client to better understand himself and "work with what is."
This does not mean that there are no changes in therapy. The therapist helps the client to better understand himself and "work with what is."
Fundamentals of Third Wave CBT
Unlike traditional CBT, Third Wave CBT looks beyond the client's behavior and what happens to them. It focuses on the context and the person's inner attitude to what is happening. nine0003 Principles and tools on which Third Wave CBT is based:
Mindfulness
Mindfulness in Third Wave CBT is understood as focusing on the "here and now" moment. In a state of awareness, we notice everything that happens to us. We do not evaluate or try to control our own feelings and reactions. You can learn how to enter this state with the help of meditation practices.
Acceptance
Learning to accept things that you cannot control is what third wave CBT teaches. Negative thoughts, feelings and experiences are normal and should not be avoided or forced out of consciousness. nine0079
nine0079
Personal values
What is important to you personally in life? On the basis of what would you like to build your behavior and make choices? What do you value in other people? All of these are personal values. Knowing, understanding and accepting them is very important. A person who does not rely on them runs the risk of living an "empty" life - even if from the outside it seems good and full.
Psychological flexibility
Psychological flexibility is a kind of combination of all the other concepts of third wave CBT. It is the ability to live in the present moment, accept all your feelings and choose a life filled with personal values. A psychologically flexible person knows how to abandon irrational attitudes from the past in his favor. nine0079
There are several approaches to third wave CBT, and not all of them meet each of these principles. But the general idea - acceptance, values and awareness - is the same for everyone.
Acceptance and commitment therapy: “truth is what works”
Acceptance and commitment therapy (ACT) is an approach based on the principles of awareness and acceptance. It was developed by Stephen Hayes in 1982. Mindfulness helps us live in the moment without getting stuck in the past or worrying about the future. The practice of acceptance aims to stop avoiding negative scenarios and feelings. nine0079
Behavior must serve a purpose. For example, a man wants to meet a girl, but does not do it. What dictated his behavior? He is afraid to face rejection, embarrassment. This is an avoidance strategy. ACT focuses on motivation. Here, mindfulness skills are used to help the client track the purpose of their behavior and understand how it matches their values. The next step is to understand that the fear of rejection and emotional discomfort cannot harm the client. These sensations exist, but the client can act independently of them. nine0079
nine0079
Anton Rusakov, psychologist, works in third wave CBT:
ACT uses 6 basic techniques to work with a client:
Defusion
Suffering, loss, anger, sadness are natural parts of life. From the point of view of ACT, it is not these experiences that harm, but the cognitive "hitch" with them, identification. ACT helps the client understand that he is not his thoughts.
Self-context
This technique teaches the position of the observer. It is similar to "Disconnection" and, in fact, follows from it. In the position of an observer, a person understands that there are no such thoughts that could harm him. nine0079
Acceptance
The technique of acceptance aims to stop controlling everything that happens around and inside. Every event and experience has its place and time. We already know that we can "disconnect" with them - and then they will not be able to harm us. So, there is no need to avoid anything.
Present moment engagement
To be “here and now” means to treat life with interest and openness. It is the absence of anxiety about the past and the future. The ability to become involved in what is happening in the present moment is a key skill not only for ACT, but also for other areas of Third Wave CBT. nine0079
Values
In ACT sessions, the client defines his values and decides to live according to them. When making a life choice, a person should ask himself: “How does this relate to my values?”.
The difference between CBT and ACT is that CBT looks at the content of the mind. For example, a person wakes up in the morning and thinks: "I will die a homeless person." The cognitive therapist will ask me to present arguments for and against this idea. And the ACT therapist will ask, “Does this thought help you? Does it guide you to your values? We don't care if the thought is right or wrong. What matters is how it works.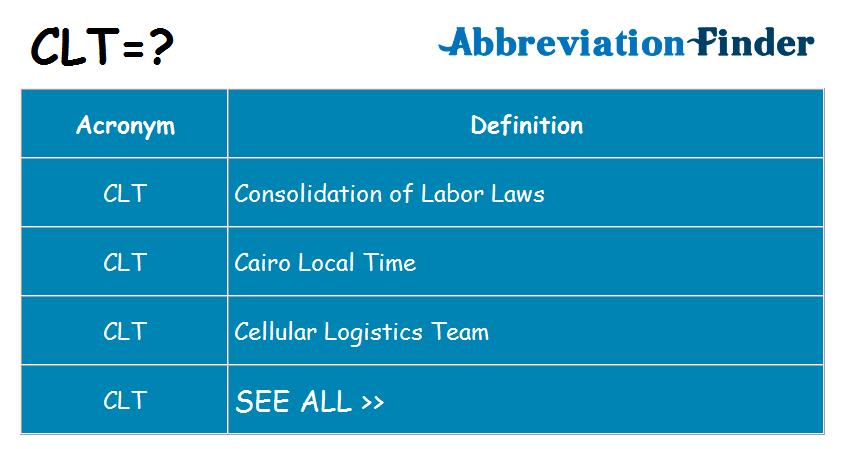 ACT's unspoken principle: "Truth is what works." nine0079
ACT's unspoken principle: "Truth is what works." nine0079
Anton Rusakov, psychologist, works in CBT of the third wave:
Committed Actions
It is not enough just to define values - in accordance with them, you need to set life goals and move towards them consistently. At the same time, negative thoughts and events do not interfere with a person and do not change his course. This is the final goal of ACT.
ACT teaches the client that discomfort is an integral part of life. It is impossible to avoid it all the time. But you can decide on your values and move towards your goals, regardless of it. nine0005
ACT sessions use many metaphors and thought experiments to achieve an effect. The effectiveness of ACT has been scientifically proven. It is especially recommended when working with anxiety disorders, depressive conditions and to support people who are faced with loss or an incurable illness.
ACT Metaphor: Imagine you want to swim in a pool. But there is a soccer ball floating there, which annoys you a lot. You enter the pool, forcefully push the ball under the water and hold it there. It turns out that the ball is under water, you can't see it. But now you can't swim - all your strength goes into holding the ball. So, maybe it's better to let him go, accept that he's swimming in the pool, and try to enjoy his vacation despite this? nine0079
But there is a soccer ball floating there, which annoys you a lot. You enter the pool, forcefully push the ball under the water and hold it there. It turns out that the ball is under water, you can't see it. But now you can't swim - all your strength goes into holding the ball. So, maybe it's better to let him go, accept that he's swimming in the pool, and try to enjoy his vacation despite this? nine0079
Anton Rusakov, psychologist, works in Third Wave CBT:
Dialectical Behavioral Therapy: “a life worth living”
Dialectical behavioral therapy (DBT) is designed to treat complex personality disorders, in particular borderline personality disorder (BPD). The founder of the approach, Marsha Linehan, herself suffered from BPD. She could not be diagnosed for a long time, not to mention the correct therapy. Marsha hurt herself, could not establish a social life, spent most of her time in the hospital and did not understand what was happening to her. "Life in hell," as Marsha herself comments, continued until one day she had an epiphany. She felt that she could accept herself for who she was. This sense of acceptance helped her cope with emotional instability. Marsha Linehan began to study psychology and psychotherapy. She immediately decided that she would work with severe cases and suicidal people. Marsha's method was based on the idea of total acceptance. She used cognitive behavioral therapy techniques, as well as elements of Zen Buddhism, breathing techniques and meditation. Subsequently, this approach became known as DBT - Dialectical Behavior Therapy. nine0005
"Life in hell," as Marsha herself comments, continued until one day she had an epiphany. She felt that she could accept herself for who she was. This sense of acceptance helped her cope with emotional instability. Marsha Linehan began to study psychology and psychotherapy. She immediately decided that she would work with severe cases and suicidal people. Marsha's method was based on the idea of total acceptance. She used cognitive behavioral therapy techniques, as well as elements of Zen Buddhism, breathing techniques and meditation. Subsequently, this approach became known as DBT - Dialectical Behavior Therapy. nine0005
DBT has a special strict format of work:
Group therapy 2-3 hours every week
In a group with the help of a therapist, the client trains the skills of coping with emotions. This is a key part of therapy, because it is the sphere of emotions and emotional responses that most often suffers from a personality disorder.
Individual therapy 1 hour per week
Personal work with a therapist helps the client to integrate the acquired skills into his life, work with thoughts and behavior. nine0079
nine0079
Telephone consultation between sessions
If a client faces a difficult situation in everyday life, he can (by prior arrangement) call the therapist and receive the necessary support. The therapist will remind him of the strategies that the client has acquired in group and individual therapy, and negotiate with the client how he will apply them in the current situation.
Also, therapists who work in the DBT approach meet for group intervision and discuss their practice. Since they have to work with difficult, often suicidal clients, this stage is very important in order to avoid professional burnout. nine0005
As a rule, working with a client consists of 4 stages. Stage 1 begins after the preparatory work. Since such therapy is a long laborious process, as a preparation, the therapist works with the client's motivation.
Behavior control
The task of this stage is to stop destroying your life. In therapy, the client forms strategies that help him survive emotional distress.
In therapy, the client forms strategies that help him survive emotional distress.
For example, a client takes alcohol every time he feels sad. We think about how we could have acted differently in this situation. Can a client call a relative every time they feel sad? What is the advantage of this behavior over drinking alcohol? We agree that the next time the client experiences this emotion, he will engage in non-destructive behavior. Or he will call me and I will help him cope and remember the skills of self-regulation. nine0079
Anton Rusakov, psychologist, works in third wave CBT:
Effective emotion regulation
This stage follows naturally from the first. Those emotional regulation skills that all people normally have (listen to music, get distracted, talk with a friend, play sports) in people with a personality disorder may not be formed. In therapy, they are formed and worked out.
Finding "ordinary happiness and unhappiness"
At this stage, the therapist helps the client to build a normal life.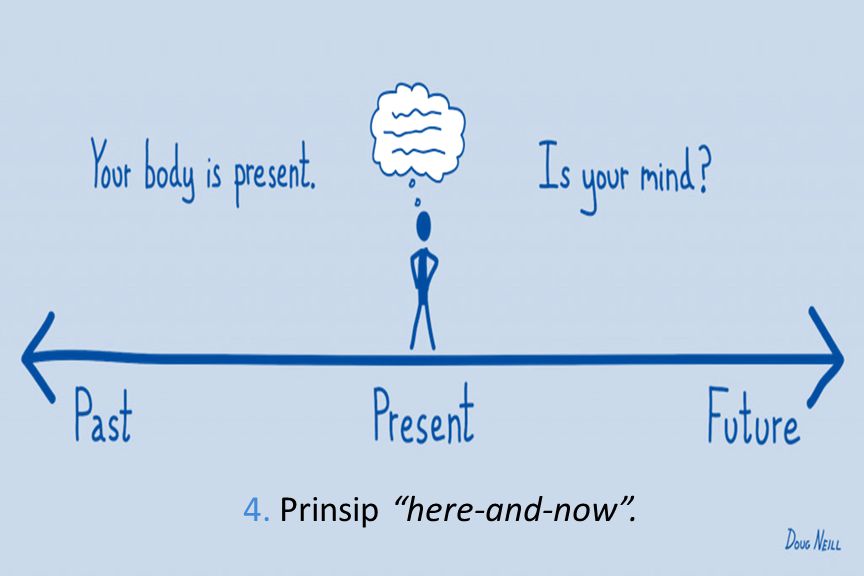 The client learns to solve problems with work, school and relationships. He gets used to the fact that in life there are always both positive and negative things - and you can interact with them.
The client learns to solve problems with work, school and relationships. He gets used to the fact that in life there are always both positive and negative things - and you can interact with them.
Finding a sense of joy, depth and freedom
This is the last stage of DBT, which is dedicated to building a happy and prosperous life. It is possible only after the client learns to solve everyday problems and effectively respond to different life situations. nine0079
The last two stages of DBT are similar in purpose and principles to ACT. The therapy lasts a long time - on average, it takes at least a year to achieve the effect. There are cases when the last stages of DBT last a lifetime - the client periodically visits a therapist, maintains the result and continues to improve his life.
Mindfulness-based Cognitive Therapy
Mindfulness-based Cognitive Therapy (MBCT) is an approach that grew out of the Mindfulness-based Stress Reduction (MBSR) program. This is a short term approach averaging 8 weeks. Work takes place in groups of up to 12 people. The creators of the approach are Zindel Segal, Mark Williams and John Tisdale. nine0005
This is a short term approach averaging 8 weeks. Work takes place in groups of up to 12 people. The creators of the approach are Zindel Segal, Mark Williams and John Tisdale. nine0005
MBCT aims to get rid of automatic thoughts and reactions. This is facilitated by the practice of meditation, which increases awareness. Impartial observation of the flow of one’s own thoughts, separation from them, studying the sensations in one’s own body reduces the level of anxiety and allows one not to “fall” into the usual negative scenario.
During therapy, the client learns 4 important skills:
Get out of the “thinking pattern”
Recognize situations and conditions that lead to the launch of a negative “thinking pattern”
Treat these situations more consciously and deal with them differently
Do not avoid the difficulties and negative aspects of life.
Initially targeted at depression, the approach has proven effective in anxiety disorders, chronic fatigue syndrome, and eating disorders.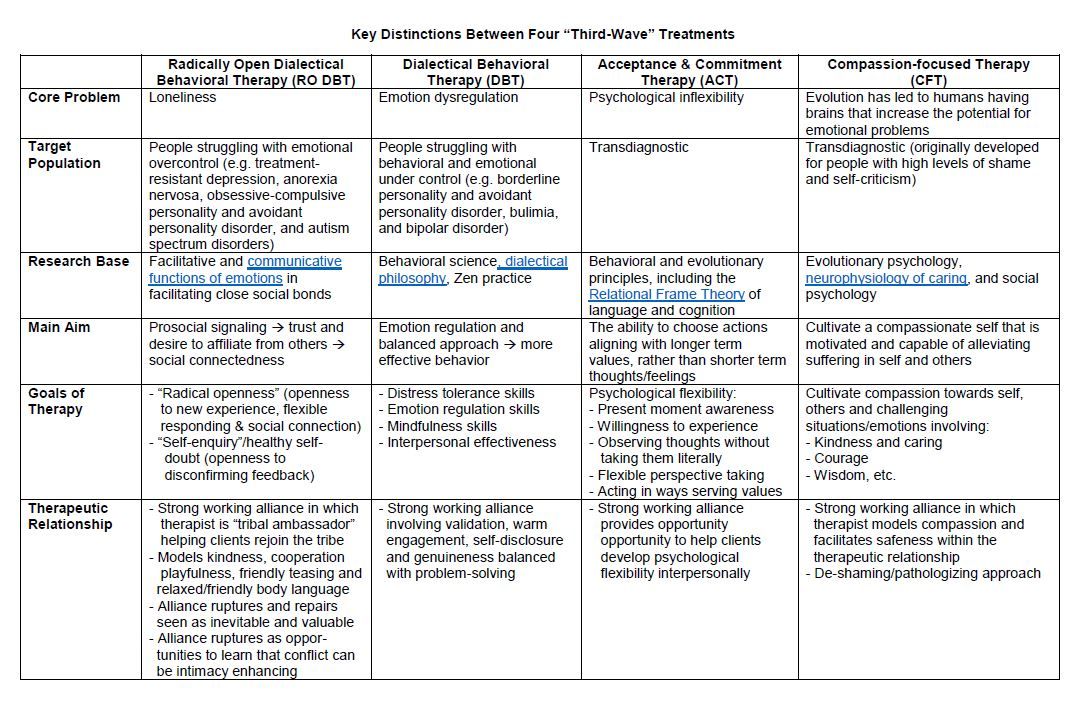
Schema therapy
Schema is a model of behavior and a system of ideas about the world learned in childhood. Even if the scheme is maladaptive, does not correspond to reality and prevents a person from being happy, he continues to "work out" it in adulthood. Schema therapy was developed in 19Jeffrey Yang, a student of CBT founder Aaron Beck, in the 1990s. He noticed that for some clients with lingering problems, CBT may not be enough. They achieve a short-term effect and improve a specific area of life - but after a while they "roll back" to the previous level.
Young came to the conclusion that some people form early maladaptive schemas that they cannot just give up. The scheme is formed in childhood, when 90,003 needs of 90,004 children were insufficiently or inadequately met. At that moment, the scheme served as a kind of protection. For example, a child feels insufficient care and support from their parents - and decides (because of their cognitive abilities) that all significant people will behave this way with them. He is ready for this in advance. As soon as someone important appears in his life, he will immediately prepare for alienation and coldness. In adulthood, such a person will unconsciously choose people who are not able to build healthy relationships. This will confirm his scheme and work on the principle of a "self-fulfilling prophecy". As long as the scheme works (even if it brings suffering), the world is stable, predictable and safe. That is why it is so difficult to abandon the scheme and standard CBT may not be enough. nine0079
He is ready for this in advance. As soon as someone important appears in his life, he will immediately prepare for alienation and coldness. In adulthood, such a person will unconsciously choose people who are not able to build healthy relationships. This will confirm his scheme and work on the principle of a "self-fulfilling prophecy". As long as the scheme works (even if it brings suffering), the world is stable, predictable and safe. That is why it is so difficult to abandon the scheme and standard CBT may not be enough. nine0079
Young identified 18 maladaptive schemes that develop in connection with the dissatisfaction of basic needs in childhood:
The need for reliable attachment
The need for autonomy, competence and a sense of identity
The need to freely express their feelings and needs of
consumption within boundaries
and self-control
The need for secure attachment
The need for autonomy, competence and a sense of identity
The need to freely express one's feelings and needs
The need for boundaries
and self-control
Abandonment
"Relationships with other people cannot be reliable: people will leave and leave me. "
"
Distrust
"Relationships are not safe - people ingratiate themselves and then use me for their own purposes."
Emotional deprivation
“There is a wall between me and those around me. I can't build close relationships." nine0079
Social isolation
“I am completely different from others, no one can understand me.”
Defectiveness
"Something is wrong with me."
Addiction
"I can't do anything on my own."
Vulnerability
"The world is a dangerous place and there is nothing I can do about it."
Merge
"I can't be on my own, without another person life has no meaning." nine0079
Pessimism
"The world is a very dark place where bad things happen to people."
Doomed to failure, failure
"I can't do it."
Submission
"I must act as others want."
Self-sacrifice
"I have no right to take care of myself, because others are more important.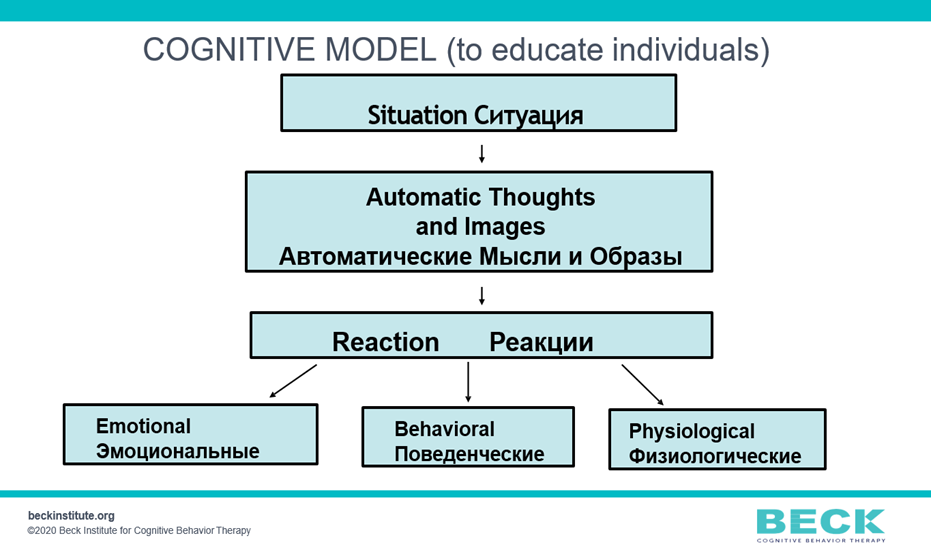 "
"
Seeking approval/recognition
“I don't know who I am. I rate myself the way you rate me." nine0079
Suppression of emotions
"Showing emotions is unacceptable."
Rigid standards
“I have to live up to the highest standards. You can always do a little better."
Punitiveness
"I must be punished for any mistake."
Grandiosity
"I am special and should always get what I want."
Lack of self-control
"I can't control my desires and actions." nine0079
The scheme causes discomfort and pain because it is based on trauma. Therefore, people try to "cope" with it in different ways. Unfortunately, the methods are most often also maladaptive. There are 3 main coping strategies in schema therapy (from English coping - to cope) :
Surrender
The person passively follows the schema. For example, the “abandoned” chooses as partners only those people who are ready to leave him.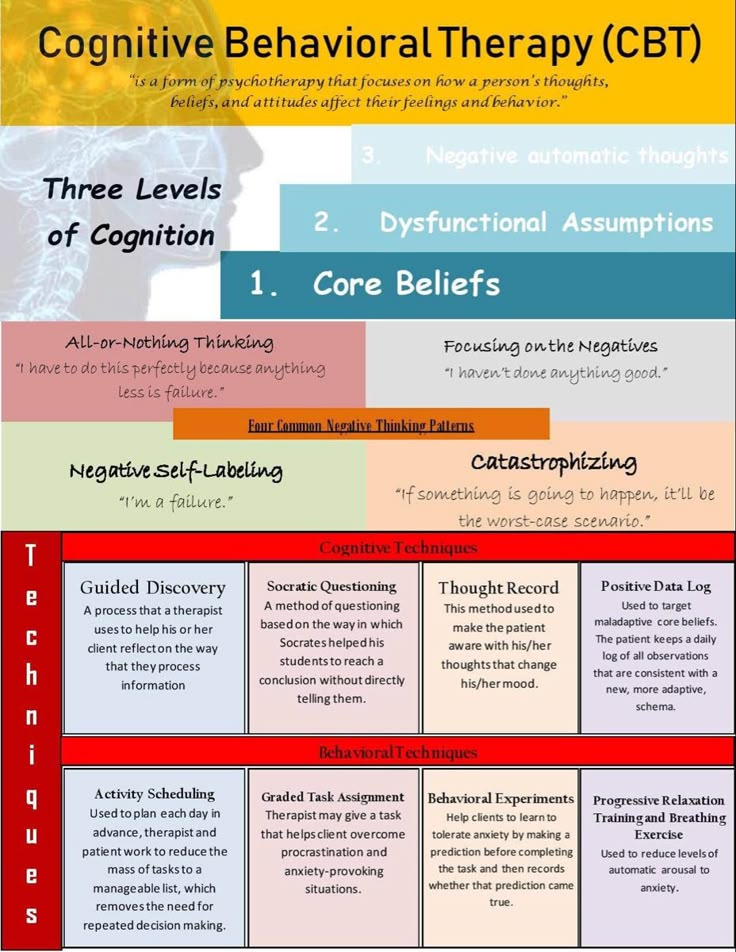
Avoidance
To avoid repeating the negative scenario, the person refuses to interact: does not build close relationships, does not tell anyone personal information, does not leave the house, etc.
Overcompensation , but does it in a deliberate or hypertrophied form. He leaves people first so that they do not leave him, he himself tries to manipulate or punish others in fear that they can do this to him. nine0079
Also in schema therapy there is the concept of mode . This is a certain set of schemes that “works” for a person at the moment. Each person has certain modes that he enters in different situations. It is very important for the therapist to understand what mode the client is in. This helps to "get through" to the part of the client that is responsible for the emergence of the schema.
The goal of schema therapy is to replace maladaptive schemas with healthier ones. To work with the thinking strategy, she uses techniques from CBT.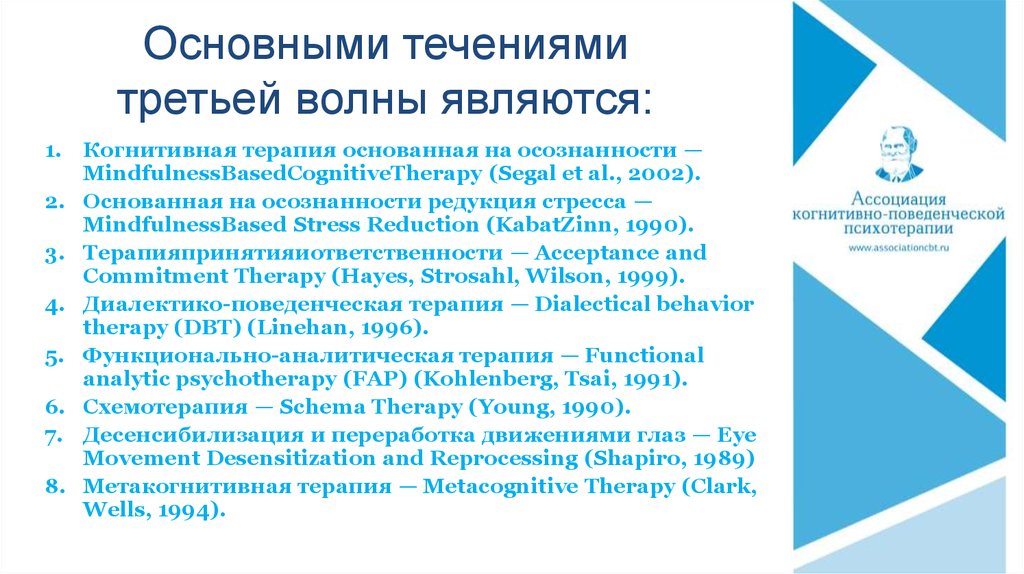 To work through the realm of feelings and emotional memory, the schema therapist uses Gestalt therapy techniques. Also in schema therapy is often used rescripting - "rewriting" of children's experience. The therapist gives special active imagination exercises in which the client helps the injured part of himself feel comfortable and safe.
To work through the realm of feelings and emotional memory, the schema therapist uses Gestalt therapy techniques. Also in schema therapy is often used rescripting - "rewriting" of children's experience. The therapist gives special active imagination exercises in which the client helps the injured part of himself feel comfortable and safe.
One of the important tools of schema therapy is the therapeutic relationship. The therapist "acts out" the role of a healthy parent. In this case, the client develops a trusting, secure relationship with the therapist. Often this is the first such experience that shows the client that such a relationship is possible. He can later transfer this experience to his life and to people outside the office. nine0079
Case study
“Several years ago a man approached me. He felt very bad, life consisted of the road to and from work. Spent a lot of time at home. I referred him to a psychiatrist, who diagnosed him with schizotypal personality disorder. The client had a problem with motivation: he wanted to change his life, to do something, but it was very difficult to organize it. For example, he wanted to get a promotion at work, but could not approach his superiors and ask for it. The idea that after that he would be treated badly interfered. We used a method from CBT - "cognitive reappraisal". They also worked with emotions and "crazy ideas". I used techniques from ACT and taught the client to disidentify from their thoughts and emotions. As a result, the client began to understand that he has fears and negative thoughts, but he knows how to act in spite of them. Now he successfully communicates at work, builds friendly relations, has received a good status. Psychotherapy is still going on, but the progress is clear.” nine0079
The client had a problem with motivation: he wanted to change his life, to do something, but it was very difficult to organize it. For example, he wanted to get a promotion at work, but could not approach his superiors and ask for it. The idea that after that he would be treated badly interfered. We used a method from CBT - "cognitive reappraisal". They also worked with emotions and "crazy ideas". I used techniques from ACT and taught the client to disidentify from their thoughts and emotions. As a result, the client began to understand that he has fears and negative thoughts, but he knows how to act in spite of them. Now he successfully communicates at work, builds friendly relations, has received a good status. Psychotherapy is still going on, but the progress is clear.” nine0079
Ekaterina Cherepkova, psychologist, combines Gestalt therapy and CBT of the third wave:
What to read?
The Happiness Trap.
Harris Russ
A set of specific strategies that will help you change your life, get rid of anxiety and negative attitudes.