Body numb after drinking
Alcoholic Neuropathy: Causes, Symptoms and Diagnosis
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
What is Alcoholic Neuropathy?
Alcohol can be toxic to nerve tissue. People who drink too much may start to feel pain and tingling in their limbs. This is known as alcoholic neuropathy. In people with alcoholic neuropathy, the peripheral nerves have been damaged by too much alcohol use. The peripheral nerves transmit signals between the body, the spinal cord, and the brain.
Thiamine, folate, niacin, vitamins B6 and B12, and vitamin E are all needed for proper nerve function. Drinking too much can alter levels of these nutrients and affect the spread of alcoholic neuropathy. Fortunately, abstaining from alcohol can help restore your nutritional health. This may improve your symptoms and help prevent further nerve damage. However, some alcohol-induced nerve damage is permanent.
9 Celebrity Alcoholics You May Not Know About
Alcoholic neuropathy can affect both movement and sensation. Symptoms range from slight discomfort to major disability. Although the condition is not life threatening, it can decrease your quality of life. Some areas of the body affected by alcoholic neuropathy include:
Arms and Legs
- numbness
- tingling and burning
- prickly sensations
- muscle spasms and cramps
- muscle weakness and atrophy
- loss of muscle functioning
- movement disorders
Urinary and Bowel
- incontinence
- constipation
- diarrhea
- problems starting urination
- feeling that the bladder hasn’t been emptied fully
Other
- sexual dysfunction
- impotence
- impaired speech
- difficulty swallowing
- heat intolerance, particularly following exercise
- vomiting and nausea
- dizziness or lightheadedness
Call your doctor if you have neuropathy symptoms. Early diagnosis and treatment make it more likely that you will be able to recover.
Early diagnosis and treatment make it more likely that you will be able to recover.
Your peripheral nerves help your body manage important sensory and motor functions including:
- bowel and urinary elimination
- walking
- sexual arousal
- arm and leg movement
- speech
Alcoholic neuropathy is the result of damage to these nerves. The damage may be the direct result of long periods where you drank too much alcohol. Nutritional problems linked to alcohol use, such as vitamin deficiency, can also cause nerve damage.
Your doctor will need to examine you to diagnose this condition. It is important to share any history of alcohol use with your doctor to get an accurate diagnosis. Your doctor will need to rule out other potential causes for your symptoms.
Tests, which may identify other potential causes of neuropathy, include:
- nerve biopsy
- nerve conduction tests
- upper GI and small bowel series
- neurological examination
- electromyography
- esophagogastroduodenoscopy (EGD)
- kidney, thyroid, and liver function tests
- complete blood count (CBC)
Blood tests can also look for vitamin deficiencies that are linked to both nerve health and alcohol use. Nutrients your doctor might test for include:
Nutrients your doctor might test for include:
- niacin
- thiamine
- folate
- vitamins B6 and B12
- biotin and pantothenic acid
- vitamins E and A
The most important thing you can do to treat this condition is to stop drinking. Treatment may first focus on problems with alcohol use. For some people, this may require inpatient rehab. Others may be able to stop drinking with outpatient therapy or social support.
Once alcohol use has been addressed, your doctor can focus on the neuropathy itself. Symptom management is important. Nerve damage can also make it difficult for you to carry out the functions of daily life. Nerve damage may even make injuries more likely.
Every person’s needs are different. Treatment for neuropathy may involve one, or many, different types of care. These include:
- vitamin supplements to improve nerve health (folate, thiamine, niacin, and vitamins B6, B12, and E)
- prescription pain relievers (tricyclic antidepressants and anticonvulsants)
- medication for people with problems urinating
- physical therapy to help with muscle atrophy
- orthopedic appliances to stabilize extremities
- safety gear, such as stabilizing footwear, to prevent injuries
- special stockings for your legs to prevent dizziness
Nerve damage from this condition is usually permanent. Your symptoms are likely to get worse if you don’t stop drinking. This could lead to disability, chronic pain, and damage to your arms and legs. However, if caught early enough, you can minimize the damage from alcoholic neuropathy. Avoiding alcohol and improving your diet can sometimes lead to a moderate to full recovery.
Your symptoms are likely to get worse if you don’t stop drinking. This could lead to disability, chronic pain, and damage to your arms and legs. However, if caught early enough, you can minimize the damage from alcoholic neuropathy. Avoiding alcohol and improving your diet can sometimes lead to a moderate to full recovery.
You can avoid alcoholic neuropathy by:
- avoiding excessive drinking of alcohol
- not drinking alcohol if you have symptoms of alcoholic neuropathy
- seeking help if you are having trouble avoiding alcohol
- eating a healthy and balanced diet
- taking vitamin supplements if you have deficiencies (always talk to your doctor before taking supplements)
The 19 Best Apps for Recovering Alcoholics of 2013
Alcohol-Related Neurologic Disease: Types, Signs, Treatment
Alcohol-related neurologic disease refers to a range of conditions caused by alcohol intake that affect the nerves and nervous system. Neurologic disorders can include fetal alcohol syndrome, dementia, and alcoholic neuropathy.
Alcohol is often consumed as a social beverage, but there are risks associated with it. Drinking alcohol can have a negative effect on the body, particularly on the nerves and muscle cells.
Alcohol is also considered an addictive substance. Consuming too much, especially over months or years, can result in severe symptoms.
Keep reading to learn about the different types of alcohol-related neurologic disease and its signs and symptoms.
Aside from intoxication, or drunkenness, drinking too much alcohol in a short time or over time can cause other conditions, including:
- memory loss
- seizures
- headaches
- memory blackouts
- coordination issues
- dehydration
- overdose
Long-term misuse can damage the nervous system, liver, and other organs. This damage may be irreversible. Drinking too much alcohol can also alter levels of certain nutrients in your body, including:
- thiamine (vitamin B1)
- folate (vitamin B9)
- vitamins B6 and B12
These vitamins are needed for proper nerve function.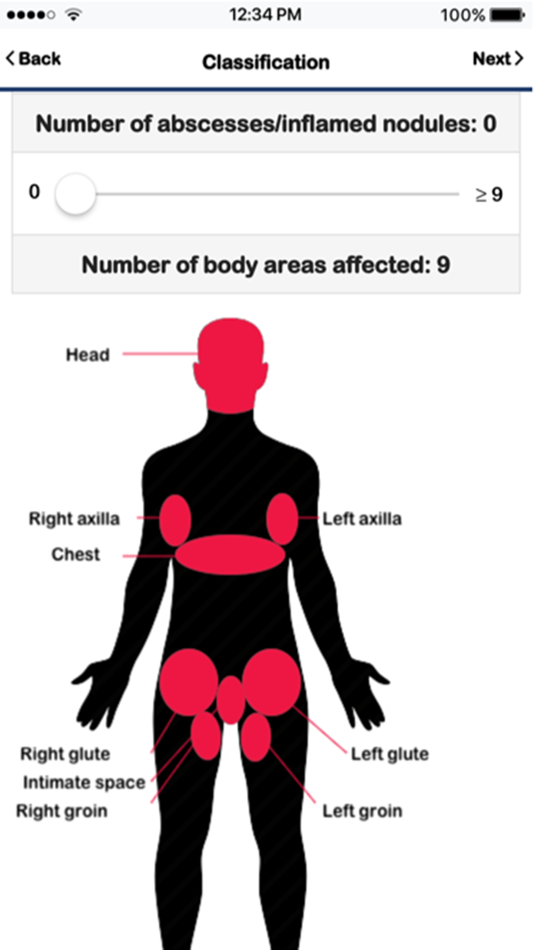 A diet poor in nutrients or avoiding eating can make nutritional deficiencies worse.
A diet poor in nutrients or avoiding eating can make nutritional deficiencies worse.
Alcohol-related neurologic disease can include the following conditions:
- Wernicke-Korsakoff syndrome, also called Wernicke’s encephalopathy and Korsakoff syndrome
- alcoholic neuropathy
- alcohol-induced cerebellar degeneration
- alcohol-related myopathy
- fetal alcohol syndrome
- alcohol withdrawal syndrome
- dementia, and other cognitive deficits
Females can be more susceptible than males to many of the negative consequences of alcohol use, such as nerve damage, as they may begin to see effects from a lower amount of alcohol consumption. This may be due to body weight and other biological differences.
Mild or moderate drinking may be safe for some people. But according to the Centers for Disease Control and Prevention (CDC), drinking less or not at all may help you avoid neurological harm.
Alcohol misuse can have many direct and indirect effects on the brain and nervous system. Examples of neurologic disease caused by alcohol can include:
Examples of neurologic disease caused by alcohol can include:
Wernicke-Korsakoff syndrome (WKS)
This condition is caused by brain damage due to a thiamine, or vitamin B1, deficiency. Thiamine deficiency is common in people who misuse alcohol. WKS is a combination of two different neurological diseases:
Wernicke’s encephalopathy
This is a severe and short-term neurologic disease that can be life threatening.
Symptoms can include:
- mental confusion
- muscle tremors
- poor muscle coordination
- paralysis of the nerves that move the eyes
- double vision
Korsakoff syndrome
This is a long lasting, or chronic, neurological disease. It usually develops as symptoms of Wernicke’s encephalopathy go away.
Symptoms may include:
- problems with learning and memory, including amnesia
- forgetfulness
- poor coordination
- difficulty walking
- hallucinations
Alcoholic neuropathy
Alcoholic neuropathy occurs when too much alcohol damages the peripheral nerves. This can be permanent, as alcohol can cause changes to the nerves themselves. Deficiencies in B6 and B12, thiamine, folate, niacin, and vitamin E can make it worse. These vitamins are all needed for proper nerve function.
This can be permanent, as alcohol can cause changes to the nerves themselves. Deficiencies in B6 and B12, thiamine, folate, niacin, and vitamin E can make it worse. These vitamins are all needed for proper nerve function.
Symptoms can include:
- numbness, tingling, and prickly sensations in the arms and legs
- muscle spasms and cramps
- muscle weakness
- movement disorders
- urinary and bowel problems like incontinence, constipation, and diarrhea
- sexual dysfunction, such as impotence
- difficulty swallowing
- impaired speech
- dizziness
- vomiting and nausea
Alcohol withdrawal syndrome
Alcohol withdrawal syndrome occurs when someone who has been drinking excessive amounts of alcohol for an extended period of time suddenly stops drinking or reduces their intake. Symptoms can develop just 5 hours after the last drink and persist for weeks.
Common symptoms of alcohol withdrawal can include:
- anxiety
- depression
- fatigue
- mood changes
- shakiness
- nightmares
- headache
- sweating
- nausea and vomiting
- insomnia
A more serious type of withdrawal is called delirium tremens. This can cause:
This can cause:
- confusion
- sudden mood changes
- hallucinations
- fever
- hyperthermia
- seizures
These symptoms can occur in addition to the symptoms of alcohol withdrawal.
Alcohol-induced cerebellar degeneration
Cerebellar degeneration caused by alcohol occurs when neurons in the cerebellum deteriorate and die. The cerebellum is the part of the brain that controls coordination and balance.
Researchers have not determined if this is caused by the effects of alcohol on the brain or is the result of thiamine deficiency.
Symptoms can include:
- unsteady walk
- tremor in the trunk of the body
- jerky movements of the arms or legs
- slurred speech
- rapid movements of the eyes, called nystagmus
Alcohol-related myopathy
Alcohol affects muscle fibers causing alcoholic myopathy. Drinking too much alcohol over time can weaken the muscles. This condition can be acute, affecting people for a short period of time before resolving, or chronic, lasting for a longer period of time.
Up to 46 percent of people with alcohol-related myopathy showed noticeable reductions in strength compared with people without the condition.
Symptoms can include:
- muscle weakness
- atrophy (decrease in muscle mass, also called muscle wasting)
- muscle cramps
- stiffness
- spasms
Does alcohol cause muscle weakness?
Alcohol misuse can cause muscle weakness. According to a 2017 review, muscle myopathy is common in alcohol use disorder. In addition, about 40 to 60 percent of people who experience chronic alcohol misuse also experience alcohol-related myopathy.
Fetal alcohol syndrome
Fetal alcohol syndrome can occur when a person is exposed to alcohol before birth.
Risks for the baby can include brain damage and developmental, cognitive, and behavioral issues. These issues can appear at any time during childhood. No amount of alcohol is safe to drink while pregnant, according to the CDC.
Symptoms of fetal alcohol syndrome can include:
- low body weight
- poor muscle coordination
- hyperactive behavior
- difficulties with attention and memory
- learning disabilities, and speech and language delays
- issues with reasoning and judgment
- vision or hearing problems
- problems with the heart or kidneys
Excessive consumption of alcohol causes alcohol-related neurologic disease. When you consume alcohol, it’s absorbed into your bloodstream from the stomach and the small intestine. It’s then broken down by the liver and expelled from the body.
When you consume alcohol, it’s absorbed into your bloodstream from the stomach and the small intestine. It’s then broken down by the liver and expelled from the body.
The liver can only break down alcohol in small amounts at a time. The alcohol will continue to circulate in the bloodstream and eventually affect other organs.
Alcohol can have significant negative effects on the central nervoussystem (CNS). The CNS includes the brain and spinal cord. Drinking alcohol can also have negative effects on the peripheral nervous system (PNS). This includes the nerves that send signals to the muscles and organs.
How alcohol affects the brain and nervous system can depend on:
- how often a person drinks
- how much a person drinks
- the age at which a person starts to drink
- how long a person has been drinking
- sex
- genetic factors
- family history of alcoholism
- diet and general health
Early diagnosis can help prevent permanent neurological damage. A doctor will take a thorough health history and have you complete questionnaires related to alcohol intake to help diagnose these conditions.
A doctor will take a thorough health history and have you complete questionnaires related to alcohol intake to help diagnose these conditions.
It’s important to fill out questionnaires about alcohol intake and nutrition honestly. Diagnosis depends largely on noticing the signs of alcohol misuse. These may include:
- neglecting major responsibilities at work, school, or at home
- drinking while driving
- arrests for driving drunk or fighting while drunk
- inability to limit drinking
- continued use of alcohol despite negative consequences
- experiencing withdrawal symptoms
Some tests can be performed by a doctor to rule out other causes of neurologic symptoms.
Avoiding alcohol is the best way to treat these conditions and relieve symptoms. The earlier you stop intake, the more likely you are to recover.
You may need inpatient rehab or medical care, especially if you exhibit alcohol use disorder, alcohol dependence, or severe withdrawal symptoms. A good source of help is support from family and friends. Other support sources include:
A good source of help is support from family and friends. Other support sources include:
- local Alcoholics Anonymous (AA) support groups
- national agencies
- helplines
Once you stop alcohol intake, a doctor can address your specific symptoms. Every person’s needs are different. Doctors tailor specific treatments and alcohol abstinence programs to the individual.
Treatment may include:
- cognitive behavior therapy (CBT) and other therapies
- counseling
- prescription medications
- attending support groups
Intravenous thiamine may reverse the symptoms of WKS. But delirium tremens is a medical emergency and requires a hospital stay. You may need to be sedated for more than a week until the alcohol withdrawal symptoms go away. And a doctor may use brain-imaging techniques to monitor treatment over time.
Your condition can get worse if you continue to drink alcohol. Permanent damage to the nervous system and other parts of the body may occur. This may lead to:
This may lead to:
- disability
- chronic pain
- death
Completely avoiding alcohol and eating a balanced diet can help minimize damage. Your chances for recovery depend on how early the disease is diagnosed and how much damage has already occurred.
In a 2019 study, researchers showed that quitting alcohol had a positive effect on most people’s mental well-being. They noted the effect was particularly noticeable for women.
Doctors or family and friends can provide early intervention, which can help you avoid alcohol-related neurologic disease.
Steps you can take for prevention include:
- learning how much alcohol is considered too much
- limiting your daily alcohol intake to 1 drink or less for females, and 2 drinks or less for males, according to the CDC’s dietary guidelines for alcohol
- avoiding alcohol altogether
Ultimately, the best way to prevent alcohol-related neurologic disease is to not drink alcohol.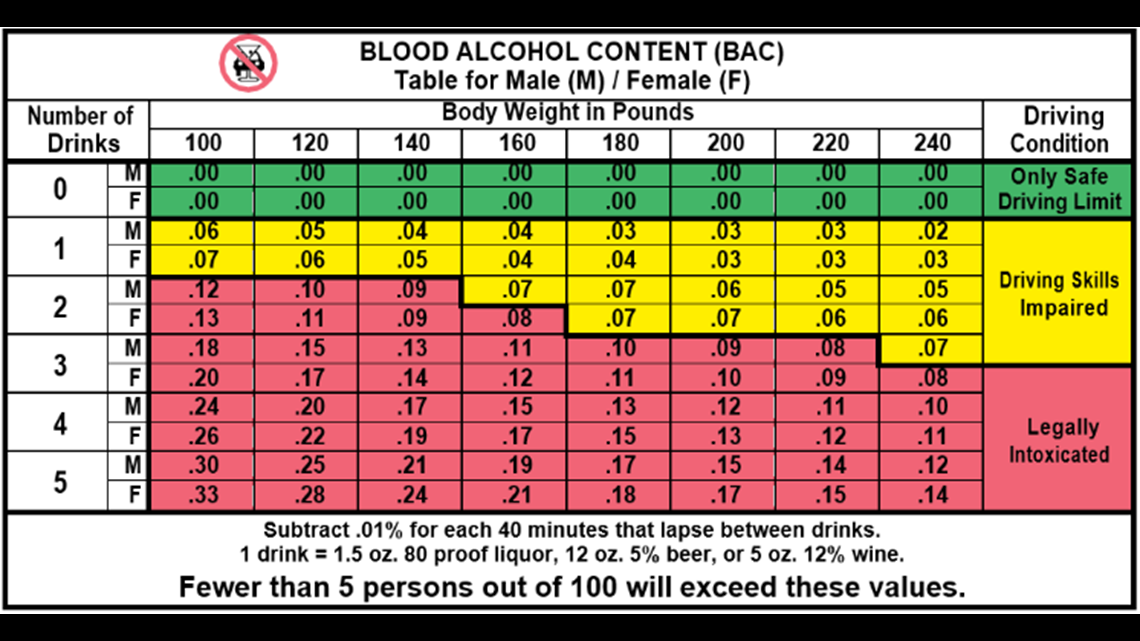
Alcohol misuse can lead to neurological damage that can affect multiple areas of a person’s health and well-being. The best way to avoid the issue is to limit alcoholic consumption to 2 or fewer drinks per day for males and 1 or fewer for females.
Several treatment options and interventions can help a person recover from alcohol dependence. Once a person stops using alcohol, they can often experience recovery from symptoms, though in some cases, some damage may be permanent.
why legs, arms, fingers fail and how to treat complications
The UK National Institute for Health and Clinical Excellence NICE has released information about new symptoms of complications after coronovirus: polyneuropathy and cardiovascular manifestations. These include:
- headache, migraine;
- cognitive impairment;
- muscle discomfort;
- numbness of limbs;
- convulsions at night;
- pain behind the sternum;
- insomnia;
- palpitations and shortness of breath.
If the deterioration does not go away within 6 months, there is chronic fatigue, decreased ability to work, limbs go numb after covid, it is necessary to undergo a comprehensive examination and rehabilitation course. Specialists of infectious diseases hospitals throughout Russia advise not to delay and contact neurologists. Complications can develop into a chronic form, up to disability. SARS-CoV-2 can cause brain damage, paralysis, encephalomyelitis, multiple sclerosis, stroke or psychosis.
Coronavirus rehabilitation programs
Read more
Why limbs go numb after COVID-19
The negative consequences of coronavirus are equally likely to develop in those who have had a severe infection, and those who have had mild or no symptoms at all. According to 40% of patients, they accidentally find out that they had been ill with SARS-CoV-2, turning to doctors with complaints of numbness and paresis of the limbs.
The main reason that hands become numb after coronavirus is damage to the myelin sheaths of nerves. This disrupts the process of passing impulses from receptors to the brain. This phenomenon is called paresthesia or hypesthesia, has the following symptoms:
- tingling in the limbs, which does not go away when changing positions;
- sensory impairment;
- Feeling cold in fingers and toes at normal room temperature.
Covid-19 patients may develop polyneuropathy, in which the sensitivity of the extremities is impaired. The cause of the pathology is a transferred infectious disease, accompanied by toxic shock syndrome due to poisoning of the body with the decay products of virus cells.
The same symptoms may indicate the development of vascular pathologies and be precursors of a stroke, in which:
- sudden onset of severe headache;
- any part of the body, arm, leg, cheek on the right or left side may fail or become numb;
- reduces the mouth, orientation and speech are disturbed.

If a person is not hospitalized in time, he may become completely or partially paralyzed.
One of the most dangerous complications after cavid is thrombosis, which can also cause numbness in the limbs. The virus infects the walls of blood vessels, and the formation of blood clots is a protective reaction of the body, in an attempt to prevent possible bleeding. A blood clot appears at the site of damage, which, like a patch, closes the weakened area.
Risk factors for thrombosis:
- Staying in a supine position for more than 3 days.
- Placement of venous catheters.
- Chronic heart failure.
- Severe lung injury.
- Ischemia.
- Increased platelet levels - blood clotting.
All of them are directly related to the coronavirus infection. Blood clots are dangerous. It leads to heart attacks, strokes, pulmonary embolism, gangrene. As a rule, development begins asymptomatically, but numbness of the legs after coronavirus, tingling and burning in the limbs can be observed. In this case, conventional blood thinners do not help.
In this case, conventional blood thinners do not help.
Swedish scientists have found that the level of the MBL protein, a lectin, rises sharply in those who are ill. There is no drug to stop this process, and tests for MBL activity are in the early stages of development.
Symptoms of complications
Depending on the type of complications, different symptoms may occur. Let's consider in more detail.
Symptoms of polyneuropathy
Pathology can be recognized by the following manifestations:
- muscle weakness, tremor;
- decreased reflexes;
- convulsions, involuntary twitches;
- "goosebumps" in the limbs, numbness;
- pain in the muscles, when touching the skin.
Signs of pulmonary thrombosis
This complication often occurs in the presence of pneumonia.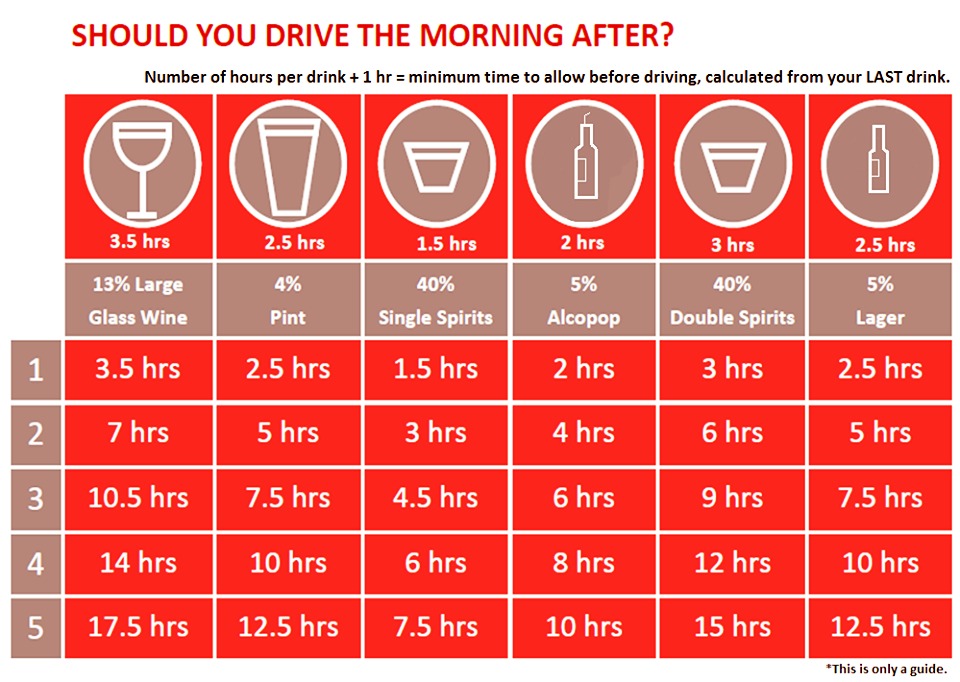 But sometimes the virus affects the respiratory organs and with a mild form of the disease. Signs of thrombosis:
But sometimes the virus affects the respiratory organs and with a mild form of the disease. Signs of thrombosis:
- rapid pulse;
- acute severe dyspnea, even at rest;
- fainting and persistent dizziness;
- chest pain, on inspiration;
- bloody clots in sputum when coughing.
Diagnosis, treatment, vaccination of COVID-19
More details
Symptoms of deep vein thrombosis
Many experts believe that the complication occurs more often in those people who already had problems with blood vessels and veins. Characteristic signs:
- pain and heaviness in the legs;
- redness in the form of stripes on the affected areas;
- development of cyanosis;
- sudden swelling;
- feelings of lack of air;
- fever, burning in hands, feet;
- hemoptysis.
Symptoms of arterial thrombosis
They also appear more often in patients who have pathologies leading to damage to blood vessels and veins. Signs:
- feeling of coldness in the extremities;
- spasms of feet and calves;
- sudden lameness;
- numbness of hands, feet, fingers;
- weakness, difficulty moving;
- nausea, vomiting, stool disorders due to blockage of intestinal vessels.
Which doctor to contact
You should start with a visit to a therapist. He collects an anamnesis, draws up a plan for the initial examination, gives direction for general blood and urine tests. This helps to determine the general somatic condition, the need for hospitalization. The patient then receives a referral to one or more subspecialists:
- Cardiologist.

- Phlebologist.
- Neurologist.
- Pulmonologist.
- Surgeon.
- Endocrinologist.
Paresthesia itself is not a disease. To make a diagnosis, it is necessary to pass a series of tests and undergo instrumental examinations. This can be done at the La Salute personal medicine clinic in the center of Moscow at a time convenient for you by appointment.
Seek medical attention if the following symptoms appear:
- frequent bouts of weakness in a short period of time;
- severe dizziness, fainting, double vision;
- impaired speech and vision;
- severe headache;
- urinary or stool incontinence;
- severe burning pain in the region of the heart for more than 3 minutes.
These symptoms may indicate the development of a stroke or cerebral edema. This condition is urgent, urgent hospitalization is necessary.
This condition is urgent, urgent hospitalization is necessary.
Book your
COVID-19 test at La Salute Clinic
I consent to the processing personal data
Diagnosis of post-COVID complications
Numbness of the extremities is a sign that a serious pathological process is developing in the body: vascular, neurological, pulmonary. That is why research is needed comprehensive, to eliminate several problems at the same time. You may need:
- Clinical blood tests: general, ESR, biochemistry.
- Hormonal studies.
- Coagulogram.
- Blood test for deficiency of iron, calcium, vitamin B12.
- Angiography.
- CT of the lungs.
- Ultrasound of the thyroid gland.
- Vascular ultrasound with dopplerography.
- X-ray of the spine.
- Head MRI.
- Electromyography.
- Electroencephalogram.
This list does not mean that you will have to complete all the tests. The attending physician prescribes the method of instrumental diagnostics, depending on the indications, based on the anamnesis and clinical tests.
Treatment
When paresthesia or polyneuropathy occurs as a complication after covid, then in addition to the main treatment, rehabilitation may be needed to prevent new pathologies and the development of chronic diseases.
Medical and physiotherapy
Depending on the diagnosis, drugs are prescribed to correct the hormonal background, or to treat blood vessels:
- venotonics;
- anti-inflammatory injections;
- B vitamins;
- muscle relaxants;
- angioprotectors;
- chondroprotectors;
- painkillers;
- drugs to prevent thrombosis and dissolve clots.
Physiotherapeutic procedures are used in combination with drug treatment as rehabilitation support measures and to prevent aggravation of the condition:
- shock wave;
- electromyostimulation;
- reflexology;
- ozone therapy;
- magnetic resonance therapy;
- ultrasound;
- electrophoresis;
- exercise therapy;
- manual therapy;
- laser therapy.
Diet and drinking regimen
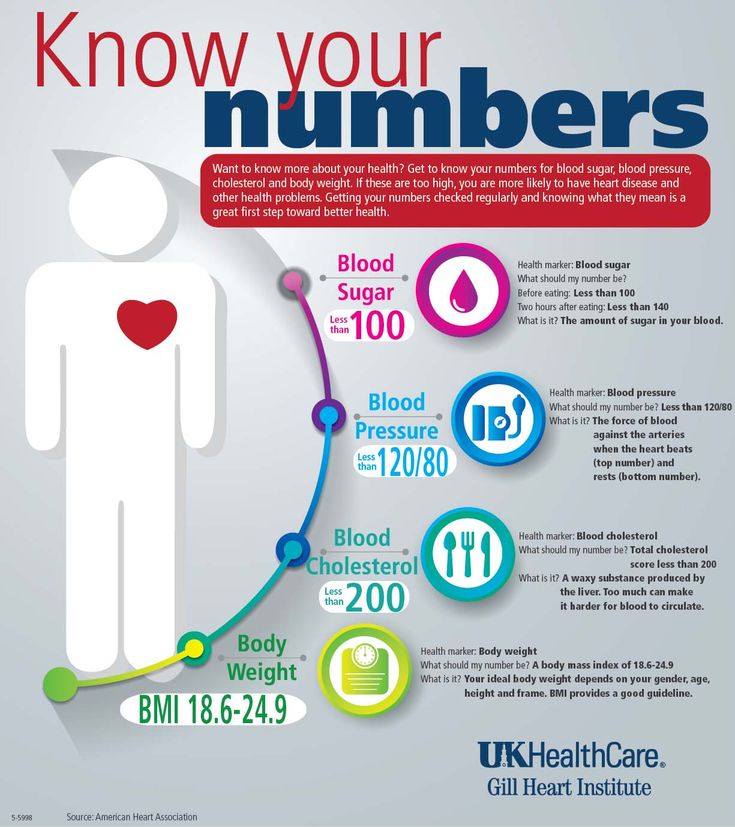
For any vascular problems and the risk of thrombosis, it is important during treatment to lower cholesterol levels, improve fluid metabolism, and prevent an increase in blood viscosity. Along with taking medications, you must follow a strict diet so as not to provoke the growth of blood clots. Everything that raises cholesterol will have to be excluded from the diet:
Everything that raises cholesterol will have to be excluded from the diet:
- sausages, semi-finished products;
- flour products;
- dairy products;
- fatty meats, broths;
- smoked products;
- products containing soya, beans, peas, lentils;
- any kind of cabbage;
- bananas, currants, citrus fruits;
- walnuts;
- alcohol and coffee;
- black and green tea;
- hot spices;
- canned food;
- fried foods.
Diagnosis, treatment, vaccination of COVID-19
More details
It is important to observe the drinking regimen for hematopoiesis and lymph renewal. The amount of clean water per day is calculated by the formula: 30 ml per 1 kg of weight.
Products recommended for vascular and neurological conditions:
- buckwheat, barley, oatmeal, millet;
- seaweed;
- watermelon, melon, red grapes;
- lean meat;
- fruit jelly;
- ginger and cinnamon;
- dark bitter chocolate;
- hard cheeses.
Raw garlic and onion have anticoagulant and antithrombotic effects. Their use helps to neutralize fatty foods, maintain vascular tone.
What can happen if complications are not treated
The danger of post-covid syndrome is that the complication often develops into an independent chronic disease that can lead to disability and even death. Doctors report covid-associated strokes and heart attacks among young people.
Psychosomatics also does not pass without a trace.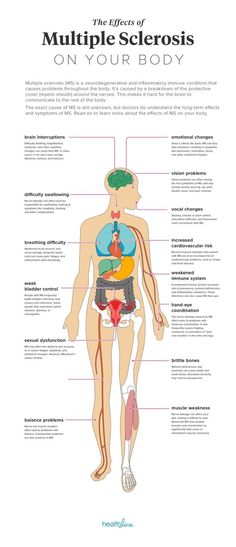 Against its background, neurosis, severe allergies, psychiatric disorders, gastrointestinal disorders, chronic migraines, and panic attacks may well develop.
Against its background, neurosis, severe allergies, psychiatric disorders, gastrointestinal disorders, chronic migraines, and panic attacks may well develop.
Complete blood count does not always help to determine the presence of pathologies in the body. More than 80% of patients turned to neurologists and cardiologists with complaints of feeling unwell, having normal indicators. Only in-depth research helped to identify various health disorders.
For example, during ischemia, a finger can go numb and the finger - the little finger on the left hand can be taken away. Localization of numbness in the feet and legs indicates the risk of thrombosis. Cramps, "cotton" legs and arms, thermoregulation failures occur with a stroke.
Cognitive impairment, against the background of numbness: disorders of memory, attention, visual impairment can lead to serious brain damage and paralysis.
If the cause of paresthesia is not determined in time, it will be very difficult to restore health, and in some situations it is simply impossible. According to statistics, every 200th patient under the age of 40 dies from a stroke or heart attack after covid. 1 out of 1000 people is forced to endure the amputation of limbs due to gangrene. Persistent disability is noted in every 30th patient who has been ill with covid.
According to statistics, every 200th patient under the age of 40 dies from a stroke or heart attack after covid. 1 out of 1000 people is forced to endure the amputation of limbs due to gangrene. Persistent disability is noted in every 30th patient who has been ill with covid.
Comprehensive examination and rehabilitation is necessary for everyone who has suffered from coronavirus in any form, if a full recovery has not yet occurred, there is constant fatigue, decreased ability to work, and symptoms that did not appear before. It is very dangerous to prescribe medications, anticoagulants, to self-medicate. Drug prevention and rehabilitation should take place under the strict supervision of a doctor and only according to indications.
Why rehabilitation is necessary after coronavirus
The main cause of complications from COVID-19 is severe intoxication caused by a large amount of decay products of viral microorganisms. It's not just the lungs that suffer.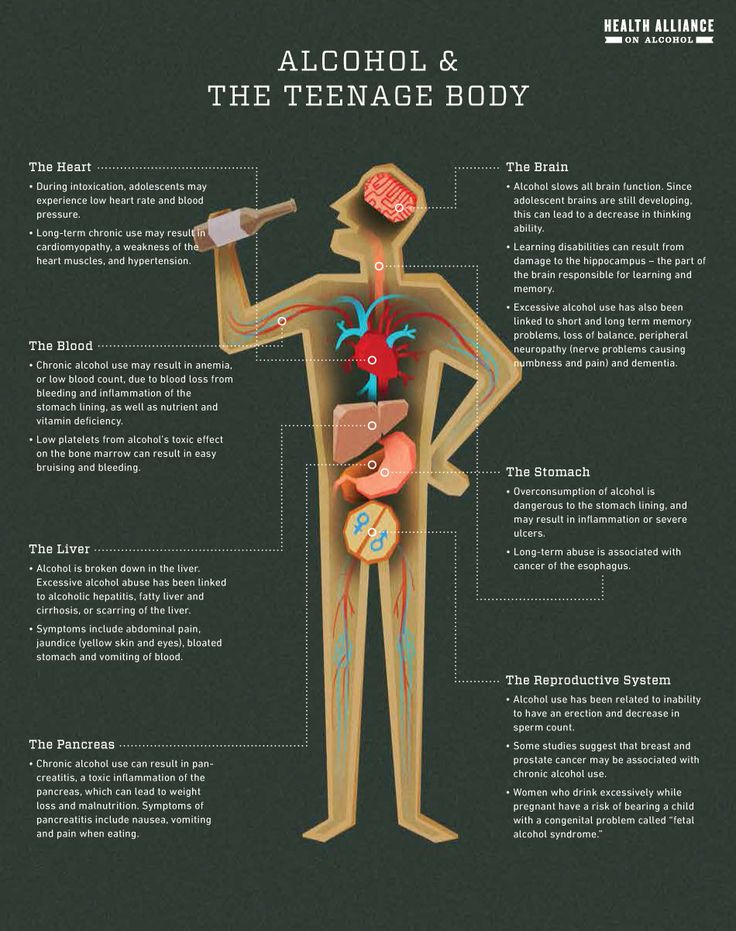 Coronavirus affects the walls of blood vessels, provokes the formation of blood clots, cholesterol plaques, blood sugar surges.
Coronavirus affects the walls of blood vessels, provokes the formation of blood clots, cholesterol plaques, blood sugar surges.
Violation of the musculoskeletal system caused by damage to the central and peripheral nervous systems, the formation of blood clots. The level of blood oxygen saturation decreases, this directly affects the work of the brain: headaches, constant weakness, disorientation, paresthesia begin.
People with heart and vascular pathologies, diabetes mellitus, chronic kidney and liver diseases are at risk for the development of irreversible complications. When the excretory system cannot cope with the removal of toxins, an overreaction of the immune system can develop, which will attack healthy cells. A complete examination after SARS-CoV-2 is mandatory if the state of health has not returned to normal.
Unfortunately, state health programs do not yet provide for post-COVID rehabilitation. The necessary clinical and instrumental studies can be done in private laboratories in Moscow. The La Salute personal medicine clinic has its own diagnostic base and provides rehabilitation services after an illness, including the necessary tests and specialist consultations to determine the causes of limb numbness: a general practitioner, neurologist, cardiologist, endocrinologist.
The La Salute personal medicine clinic has its own diagnostic base and provides rehabilitation services after an illness, including the necessary tests and specialist consultations to determine the causes of limb numbness: a general practitioner, neurologist, cardiologist, endocrinologist.
Book your
COVID-19 test at La Salute Clinic
I consent to the processing personal data
Insurance partners
Other related articles
Enteric coronavirus in humans: symptoms and signs with diarrhea and vomiting
On what day does coronavirus appear after contact with an infected person and when to take a test for COVID-19
Mental disorders after coronavirus
Problems with the gastrointestinal tract after coronavirus
Intoxication of the body after coronavirus
How to restore the brain after coronavirus
Numbness
Skip to main content
Home
compressive neuropathy or nerve entrapment.
There are more than 20 types of neuropathy, the most common problem is carpal tunnel - the space between the bones of the palm and the ligament that contains the flexor tendons and the median nerve. If it is not elastic, as the pressure increases, the nerve is infringed. If the nerve is strongly and permanently restrained at any level (palm, elbow, shoulder), skin sensitivity and mobility disorders may occur, because part of the nerve fibers die. As the disease progresses, pain and numbness spread throughout the arm. This problem usually occurs in people with repetitive, strenuous work that overtaxes the palm and contributes to nerve entrapment. For example, people working at sawmills, on a conveyor, on a computer. The sensation of numbness and pain most often appears at night, depriving a person of sleep.
Working on a computer for a long time may result in pinching of the ulnar nerve , more often on the left arm. A characteristic sign is numbness of the little finger, sometimes a feeling of freezing, discomfort on the inner surface of the forearm. At first, there is usually no pain, so patients see a doctor belatedly.
At first, there is usually no pain, so patients see a doctor belatedly.
Hand numbness can be one of the symptoms not only of the carpal tunnel, but also of other serious diseases.
If both arms and/or both legs are numb, it may be polyneuropathy or some other pathology . Polyneuropathy means that many nerves are involved in the disease process, usually affecting the periphery - palms, fingers, feet, legs. Only fingers can go numb, maybe the whole palm and arm up to the shoulder. The same with the legs - only the foot or up to half of the lower leg can go numb. Polyneuropathy also manifests itself in the form of pain, a burning sensation, like the "restless legs" syndrome, in which a person cannot fall asleep at night because of the search for a comfortable place for the legs.
If the entire arm or leg is numb, it may not be peripheral neuropathy, but damage to nerves and nerve root plexuses .
If the numbness is short-lived at first, but becomes more frequent with time until it goes away, the cause is most likely in the central nervous system.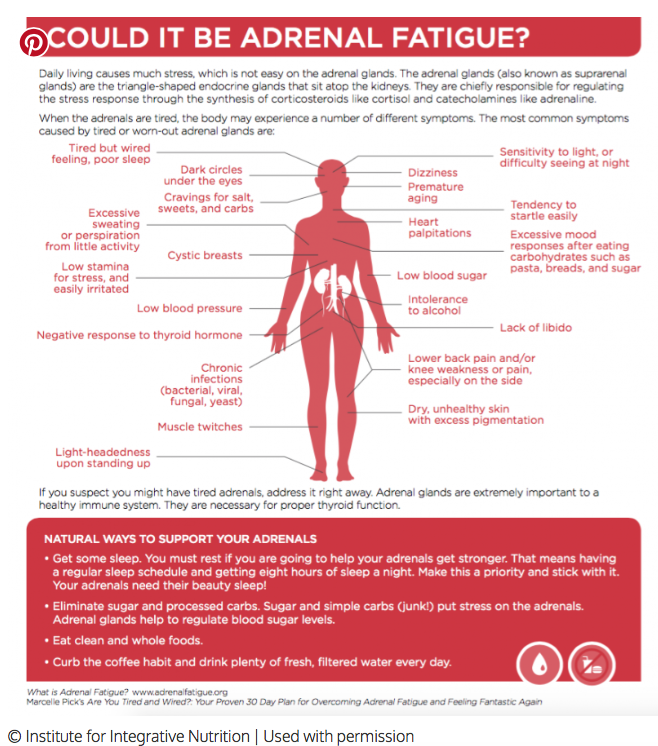 This may be a symptom of a brain tumor , cerebrovascular accident , a precursor of a stroke . Therefore, it is important for the doctor to know if the patient has numbness constant or undulating, associated with static or dynamic load, with a certain time of day , etc.
This may be a symptom of a brain tumor , cerebrovascular accident , a precursor of a stroke . Therefore, it is important for the doctor to know if the patient has numbness constant or undulating, associated with static or dynamic load, with a certain time of day , etc.
Feeling of numbness in the elderly is most often associated with transient circulatory disorders, so it is necessary to examine cerebral vessels .
This feeling can be a manifestation of a serious illness in young people - for example, multiple sclerosis . Numbness may indicate a tumor , aneurysm (expansion) of cerebral vessels. Depending on which part of the brain the vessels dilate, they press on the surrounding brain tissue, producing a throbbing sensation, headache, and other varying symptoms.
To determine the cause of numbness, a consultation with a neurologist
is required.