Blood tests for psychiatric disorders
Mental Health Screening: MedlinePlus Medical Test
What is a mental health screening?
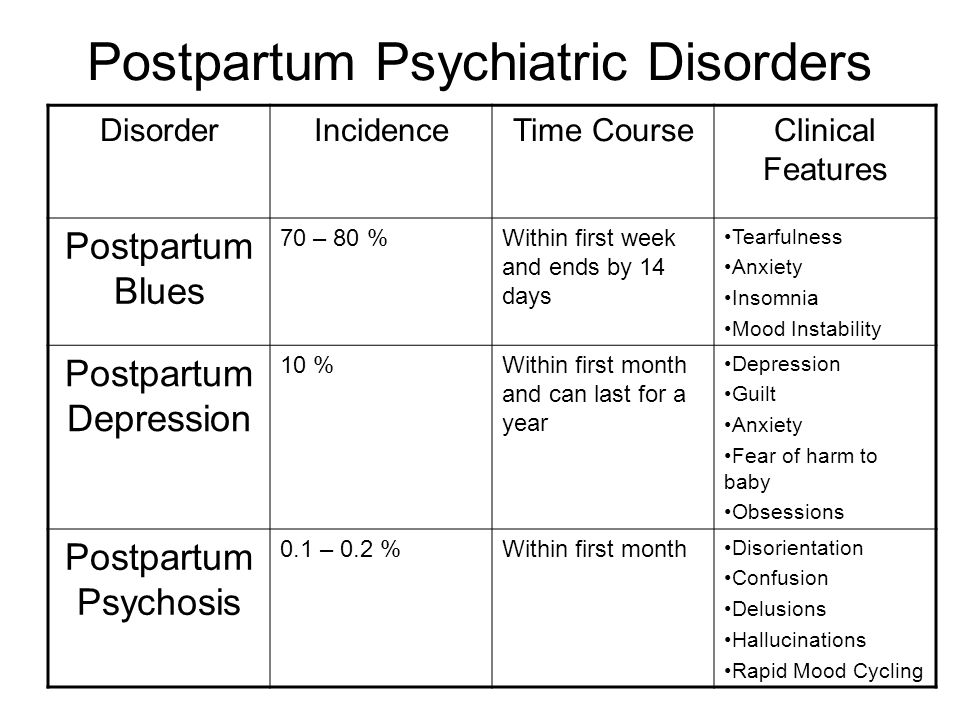
A mental health screening is an exam of your emotional health. It helps find out if you have a mental disorder. Mental disorders are common. They affect more than half of all Americans at some point in their lives. There are many types of mental disorders. Some of the most common disorders include:
- Depression and mood disorders. These mental disorders are different than normal sadness or grief. They can cause extreme sadness, anger, and/or frustration.
- Anxiety disorders. Anxiety can cause excessive worry or fear at real or imagined situations.
- Eating disorders. These disorders cause obsessive thoughts and behaviors related to food and body image. Eating disorders may cause people to severely limit the amount of food they eat, excessively overeat (binge), or do a combination of both.
- Attention deficit hyperactivity disorder (ADHD).
ADHD is one of the most common mental disorders in children. It can also continue into adulthood. People with ADHD have trouble paying attention and controlling impulsive behavior.
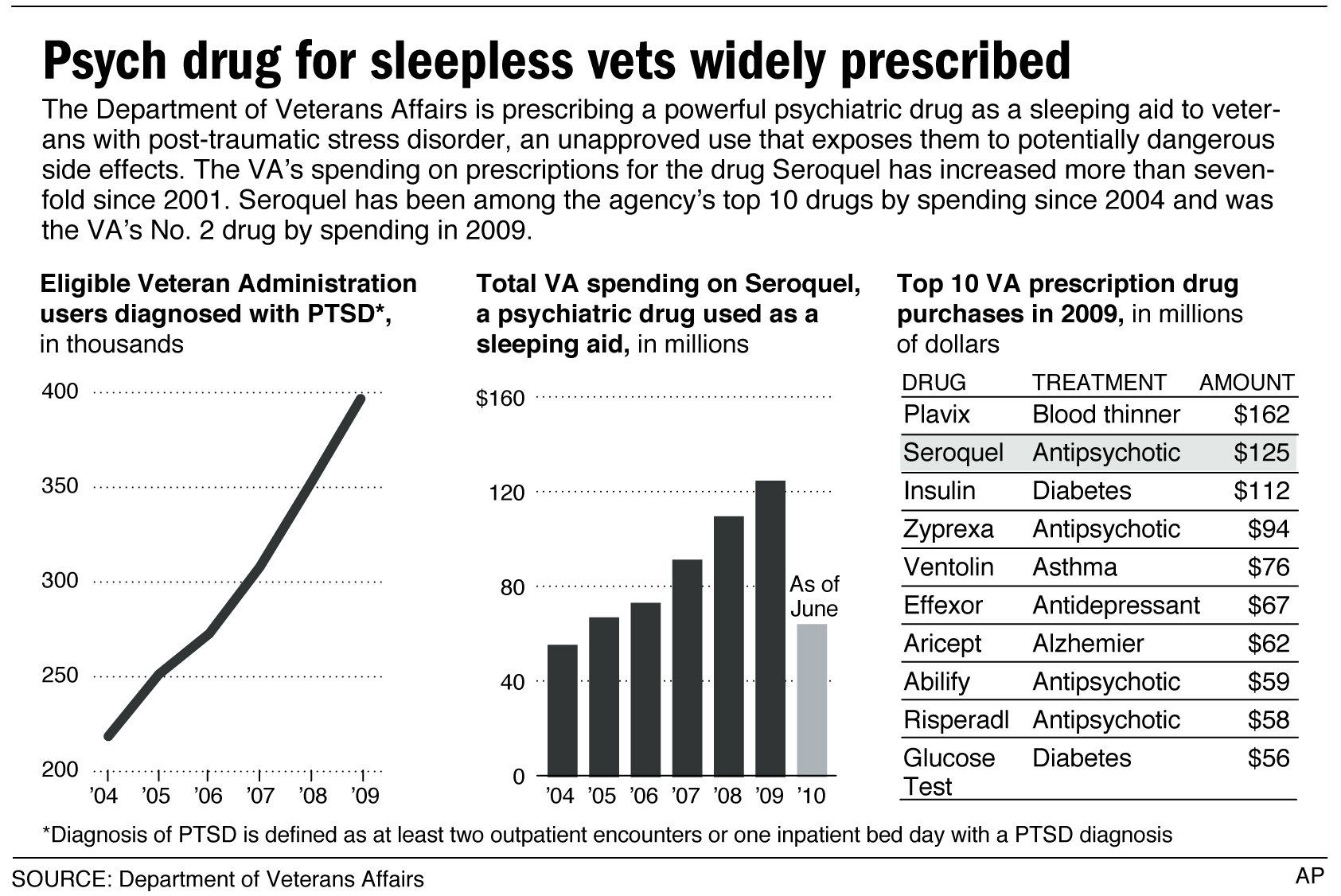
- Post-traumatic stress disorder (PTSD). This disorder can happen after you live through a traumatic life event, such as a war or serious accident. People with PTSD feel stressed and afraid, even long after the danger is over.
- Substance abuse and addictive disorders. These disorders involve excessive use of alcohol or drugs. People with substance abuse disorders are at risk for overdose and death.
- Bipolar disorder, formerly called manic depression. People with bipolar disorder have alternating episodes of mania (extreme highs) and depression.
- Schizophrenia and psychotic disorders. These are among the most serious psychiatric disorders. They can cause people to see, hear, and/or believe things that aren't real.
The effects of mental disorders range from mild to severe to life-threatening. Fortunately, many people with mental disorders can be successfully treated with medicine and/or talk therapy.
Other names: mental health assessment, mental illness test, psychological evaluation, psychology test, psychiatric evaluation
What is it used for?
A mental health screening is used to help diagnose mental disorders. Your primary care provider may use a mental health screening to see if you need to go to a mental health provider. A mental health provider is a health care professional that specializes in diagnosing and treating mental health problems. If you are already seeing a mental health provider, you may get a mental health screening to help guide your treatment.
Why do I need a mental health screening?
You may need a mental health screening if you have symptoms of a mental disorder. Symptoms vary depending on the type of disorder, but common signs may include:
- Excessive worrying or fear
- Extreme sadness
- Major changes in personality, eating habits, and/or sleeping patterns
- Dramatic mood swings
- Anger, frustration, or irritability
- Fatigue and lack of energy
- Confused thinking and trouble concentrating
- Feelings of guilt or worthlessness
- Avoidance of social activities
One of the most serious signs of a mental disorder is thinking about or attempting suicide. If you are thinking about hurting yourself or about suicide, seek help right away. There are many ways to get help. You can:
If you are thinking about hurting yourself or about suicide, seek help right away. There are many ways to get help. You can:
- Call 911 or your local emergency room
- Call your mental health provider or other health care provider
- Reach out to a loved one or close friend
- Call a suicide hotline. In the United States, you can call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255)
- If you are a veteran, call the Veterans Crisis Line at 1-800-273-8255 or send a text to 838255
What happens during a mental health screening?
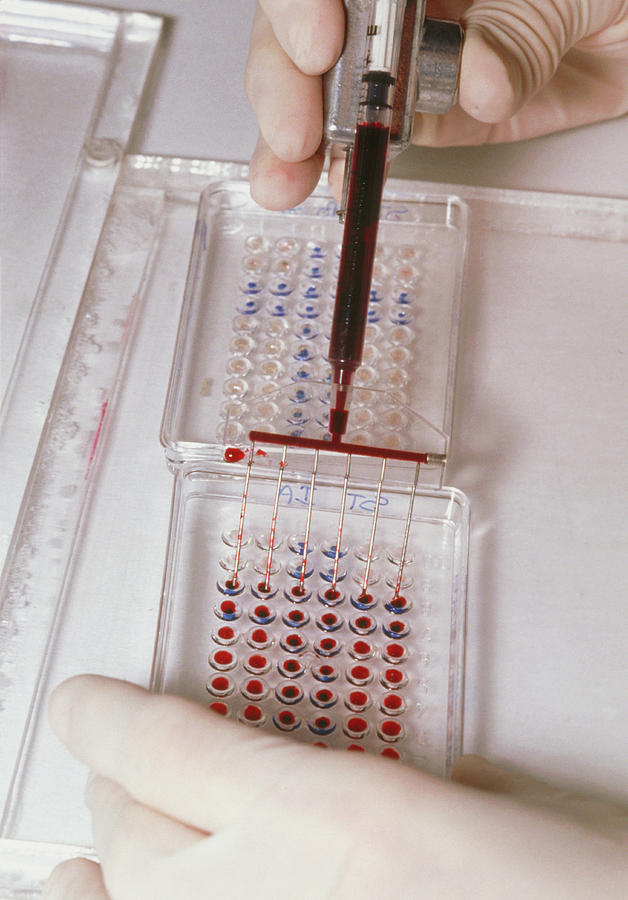
Your primary care provider may give you a physical exam and ask you about your feelings, mood, behavior patterns, and other symptoms. Your provider may also order a blood test to find out if a physical disorder, such as thyroid disease, may be causing mental health symptoms.
During a blood test, a health care professional will take a blood sample from a vein in your arm, using a small needle.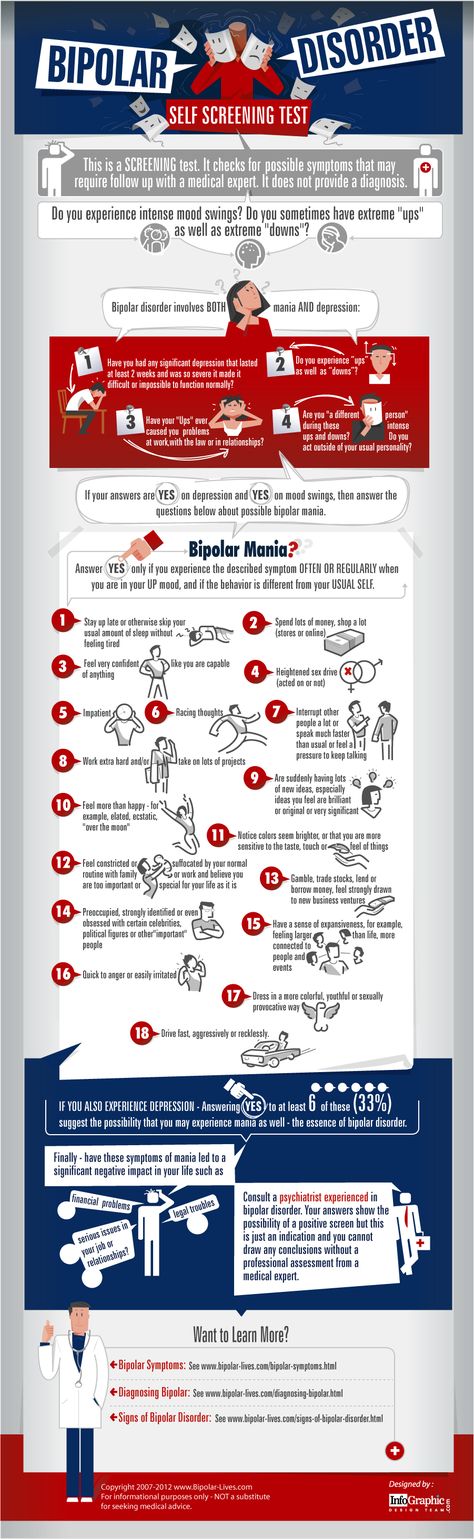 After the needle is inserted, a small amount of blood will be collected into a test tube or vial. You may feel a little sting when the needle goes in or out. This usually takes less than five minutes.
After the needle is inserted, a small amount of blood will be collected into a test tube or vial. You may feel a little sting when the needle goes in or out. This usually takes less than five minutes.
If you are being tested by a mental health provider, he or she may ask you more detailed questions about your feelings and behaviors. You may also be asked to fill out a questionnaire about these issues.
Will I need to do anything to prepare for a mental health screening?
You don't need any special preparations for a mental health screening.
Are there any risks to screening?
There is no risk to having a physical exam or taking a questionnaire.
There is very little risk to having a blood test. You may have slight pain or bruising at the spot where the needle was put in, but most symptoms go away quickly.
What do the results mean?
If you are diagnosed with a mental disorder, it's important to get treatment as soon as possible. Treatment may help prevent long-term suffering and disability.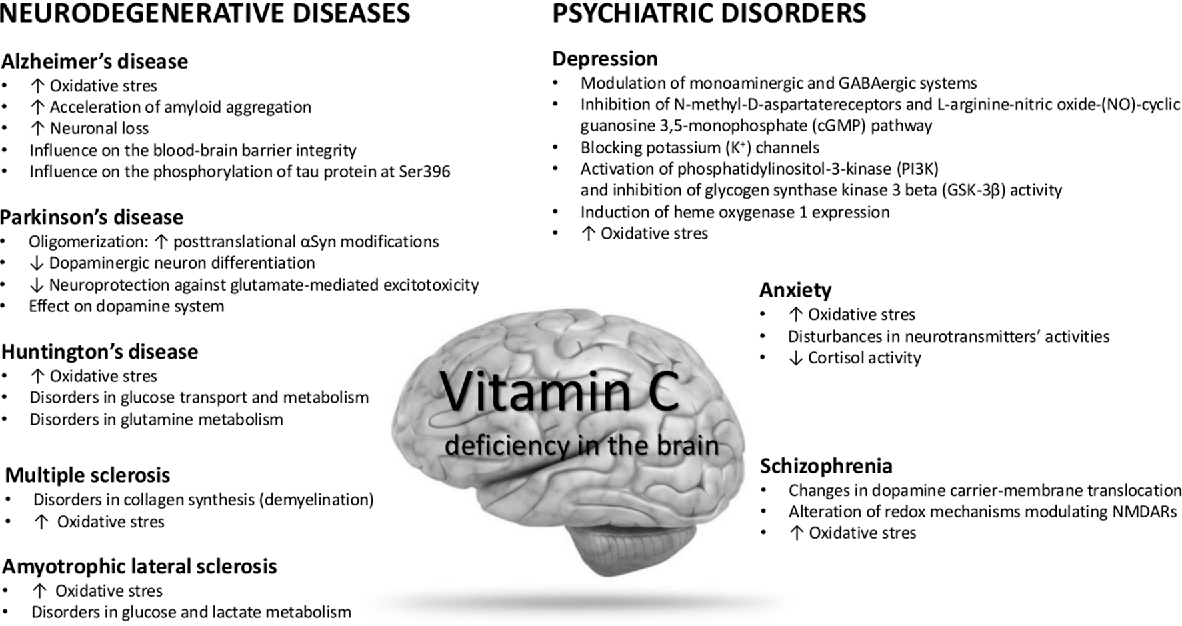 Your specific treatment plan will depend on the type of disorder you have and how serious it is.
Your specific treatment plan will depend on the type of disorder you have and how serious it is.
Is there anything else I need to know about a mental health screening?
There are many types of providers who treat mental disorders. The most common types of mental health providers include:
- Psychiatrist, a medical doctor who specializes in mental health. Psychiatrists diagnose and treat mental health disorders. They can also prescribe medicine.
- Psychologist, a professional trained in psychology. Psychologists generally have doctoral degrees. But they do not have medical degrees. Psychologists diagnose and treat mental health disorders. They offer one-on-one counseling and/or group therapy sessions. They can't prescribe medicine, unless they have a special license. Some psychologists work with providers who are able to prescribe medicine.
- Licensed clinical social worker (L.C.S.W.) has a master's degree in social work with training in mental health.
 Some have additional degrees and training. L.C.S.W.s diagnose and provide counseling for a variety of mental health problems. They can't prescribe medicine, but can work with providers who are able to.
Some have additional degrees and training. L.C.S.W.s diagnose and provide counseling for a variety of mental health problems. They can't prescribe medicine, but can work with providers who are able to. - Licensed professional counselor. (L.P.C.). Most L.P.C.s have a master's degree. But training requirements vary by state. L.P.C.s diagnose and provide counseling for a variety of mental health problems. They can't prescribe medicine, but can work with providers who are able to.
- Advanced practice registered nurses (APRNs) are specially trained nurses who have a master’s or doctoral degree in psychiatric nursing. They assess, diagnose, and treat a variety of mental health disorders. Some ARPNs can prescribe medicines.
C.S.W.s and L.P.C.s may be known by other names, including therapist, clinician, or counselor.
If you don't know which type of mental health provider you should see, talk to your primary care provider.
References
- American Psychiatric Nurses Association [Internet].
 Falls Church (VA): American Psychiatric Nurses Association; Psychiatric Mental Health Nurses; [cited 2021 Aug 2]; [about 3 screens]. Available from: https://www.apna.org/i4a/pages/index.cfm?pageid=3292
Falls Church (VA): American Psychiatric Nurses Association; Psychiatric Mental Health Nurses; [cited 2021 Aug 2]; [about 3 screens]. Available from: https://www.apna.org/i4a/pages/index.cfm?pageid=3292 - Centers for Disease Control and Prevention [Internet]. Atlanta: U.S. Department of Health and Human Services; Learn About Mental Health; [updated 2018 Jan 26; cited 2018 Oct 19]; [about 3 screens]. Available from: https://www.cdc.gov/mentalhealth/learn
- Mayo Clinic [Internet]. Mayo Foundation for Medical Education and Research; c1998–2018. Mental health providers: Tips on finding one; 2017 May 16 [cited 2018 Oct 19]; [about 3 screens]. Available from: https://www.mayoclinic.org/diseases-conditions/mental-illness/in-depth/mental-health-providers/art-20045530
- Mayo Clinic [Internet]. Mayo Foundation for Medical Education and Research; c1998–2018. Mental illness: Diagnosis and treatment; 2015 Oct 13 [cited 2018 Oct 19]; [about 4 screens]. Available from: https://www.
 mayoclinic.org/diseases-conditions/mental-illness/diagnosis-treatment/drc-20374974
mayoclinic.org/diseases-conditions/mental-illness/diagnosis-treatment/drc-20374974 - Mayo Clinic [Internet]. Mayo Foundation for Medical Education and Research; c1998–2018. Mental illness: Symptoms and causes; 2015 Oct 13 [cited 2018 Oct 19]; [about 3 screens]. Available from: https://www.mayoclinic.org/diseases-conditions/mental-illness/symptoms-causes/syc-20374968
- Michigan Medicine: University of Michigan [Internet]. Ann Arbor (MI): Regents of the University of Michigan; c1995–2018. Mental Health Assessment: How It Is Done; [cited 2018 Oct 19]; [about 5 screens]. Available from: https://www.uofmhealth.org/health-library/aa79756#tp16780
- Michigan Medicine: University of Michigan [Internet]. Ann Arbor (MI): Regents of the University of Michigan; c1995–2018. Mental Health Assessment: Results; [cited 2018 Oct 19]; [about 8 screens]. Available from: https://www.uofmhealth.org/health-library/aa79756#tp16783
- Michigan Medicine: University of Michigan [Internet].
 Ann Arbor (MI): Regents of the University of Michigan; c1995–2018. Mental Health Assessment: Test Overview; [cited 2018 Oct 19]; [about 2 screens]. Available from: https://www.uofmhealth.org/health-library/aa79756
Ann Arbor (MI): Regents of the University of Michigan; c1995–2018. Mental Health Assessment: Test Overview; [cited 2018 Oct 19]; [about 2 screens]. Available from: https://www.uofmhealth.org/health-library/aa79756 - Michigan Medicine: University of Michigan [Internet]. Ann Arbor (MI): Regents of the University of Michigan; c1995–2018. Mental Health Assessment: Why It Is Done; [cited 2018 Oct 19]; [about 3 screens]. Available from: https://www.uofmhealth.org/health-library/aa79756#tp16778
- Merck Manual Consumer Version [Internet]. Kenilworth (NJ): Merck & Co. Inc.; c2018. Overview of Mental Illness; [cited 2018 Oct 19]; [about 2 screens]. Available from: https://www.merckmanuals.com/home/mental-health-disorders/overview-of-mental-health-care/overview-of-mental-illness
- National Alliance on Mental Illness [Internet]. Arlington (VA): NAMI; c2018. Know the Warning Signs [cited 2018 Oct 19]; [about 2 screens]. Available from: https://www.nami.org/Learn-More/Know-the-Warning-Signs
- National Alliance on Mental Illness [Internet].
 Arlington (VA): NAMI; c2018. Mental Health Screening; [cited 2018 Oct 19]; [about 3 screens]. Available from: https://www.nami.org/Learn-More/Mental-Health-Public-Policy/Mental-Health-Screening
Arlington (VA): NAMI; c2018. Mental Health Screening; [cited 2018 Oct 19]; [about 3 screens]. Available from: https://www.nami.org/Learn-More/Mental-Health-Public-Policy/Mental-Health-Screening - National Alliance on Mental Illness [Internet]. Arlington (VA): NAMI; c2018. Types of Mental Health Professionals; [cited 2018 Oct 19]; [about 3 screens]. Available from: https://www.nami.org/Learn-More/Treatment/Types-of-Mental-Health-Professionals
- National Heart, Lung, and Blood Institute [Internet]. Bethesda (MD): U.S. Department of Health and Human Services; Blood Tests; [cited 2018 Oct 19]; [about 3 screens]. Available from: https://www.nhlbi.nih.gov/health-topics/blood-tests
- National Institute of Mental Health [Internet]. Bethesda (MD): U.S. Department of Health and Human Services; Eating Disorders; [updated 2016 Feb; cited 2018 Oct 19]; [about 3 screens]. Available from: https://www.nimh.nih.gov/health/topics/eating-disorders/index.shtml
- National Institute of Mental Health [Internet].
 Bethesda (MD): U.S. Department of Health and Human Services; Mental Illness; [updated 2017 Nov; cited 2018 Oct 19]; [about 3 screens]. Available from: https://www.nimh.nih.gov/health/statistics/mental-illness.shtml
Bethesda (MD): U.S. Department of Health and Human Services; Mental Illness; [updated 2017 Nov; cited 2018 Oct 19]; [about 3 screens]. Available from: https://www.nimh.nih.gov/health/statistics/mental-illness.shtml - University of Rochester Medical Center [Internet]. Rochester (NY): University of Rochester Medical Center; c2018. Health Encyclopedia: Comprehensive Psychiatric Evaluation; [cited 2018 Oct 19]; [about 2 screens]. Available from: https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=85&contentid=P00752
Blood test offers new hope to people with depression | Mental Health News
A blood test using RNA markers is offering new hope to people with mood disorders such as depression in what could be a significant breakthrough in the diagnosis of mental health conditions.
A team from the US’s Indiana University School of Medicine launched the blood test in April, claiming it to be psychiatry’s first-ever biological answer to diagnosing a mood disorder.
“Our study shows that it is possible to have a blood test for depression and bipolar disorder, that have clinical utility, can distinguish between the two, and match people to the right medications,” said psychiatrist and geneticist Dr Alexander Niculescu, who led the research.
“This avoids years of trials and error, hospitalisations, and side-effects. As these are very common disorders, we think we can do a lot of good with this and other tests and apps we have developed.”
The study delved into the biological basis of mood disorders, developing a tool to distinguish which type of mood disorder a person has – depression or bipolar disorder.
To develop the test, Dr Niculescu’s team drew on its 15 years of previous research into how psychiatry relates to blood gene expression biomarkers – measurable indicators of a biological state in the form of RNA, DNA, proteins or other molecules.
Every system in the body – the brain, the nervous system, the immune system – has a common developmental route, says Dr Niculescu.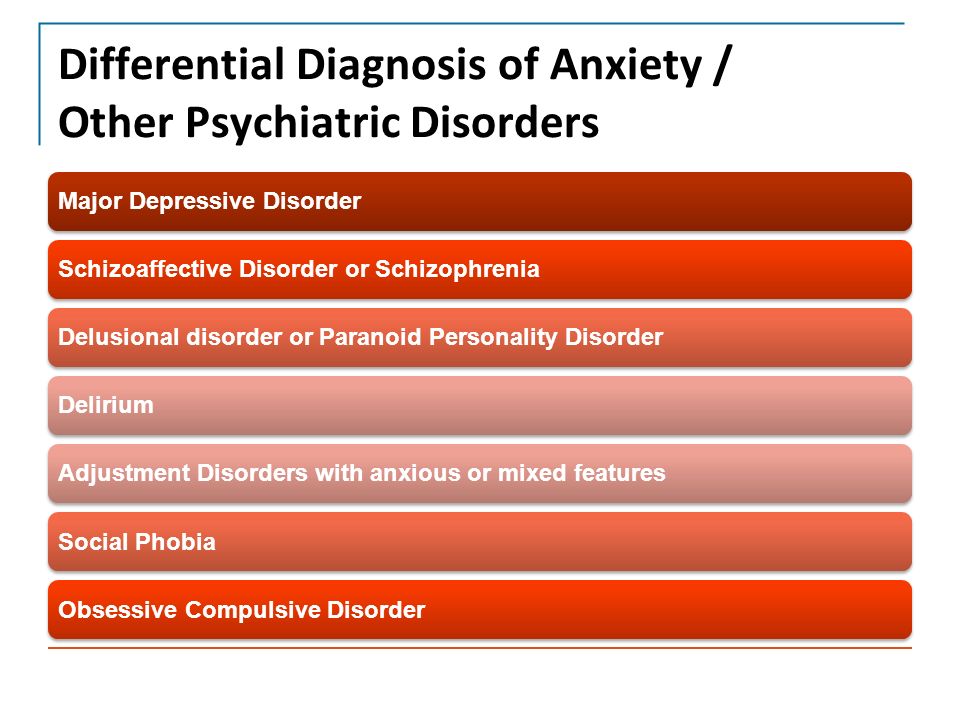
“For example, when you’re stressed or depressed, there are psycho-neurological mechanisms, hormones and other things that are released that affect your blood and your immune system,” he told Al Jazeera.
Conversely, an immune activation or inflammation would affect the brain.
Dr Alexander Niculescu and his team drew on 15 years of previous research to develop the test [Supplied]In the first stage of the study, the team identified a list of RNA biomarkers that could track mood states over a period of time. After validating them in an independent cohort of subjects with clinically severe depression and clinically severe mania, they finalised 26 biomarkers, which they whittled down to 12 through further testing.
With these findings, doctors would be able to send patients to a lab for bloodwork to indicate the causes of their symptoms, just as they would for a physical illness, says Dr Niculescu.
The biomarkers could also help with treatment because some of them were found to be affected by Selective Serotonin Reuptake Inhibitors (SSRIs), a class of antidepressants.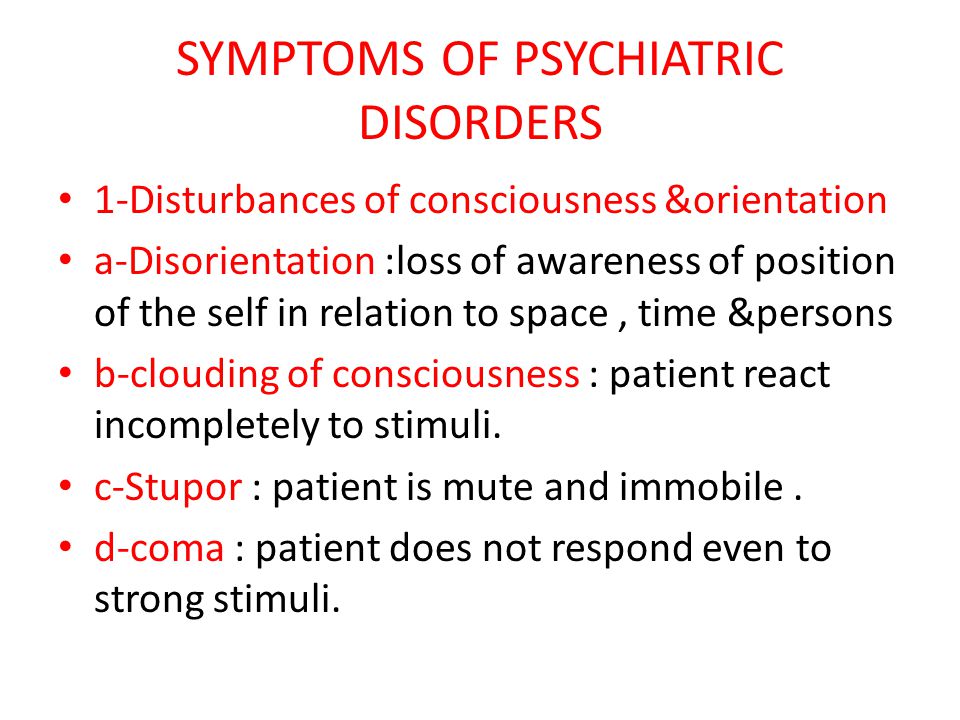 Three others were identified in previous work to be affected by lithium carbonate – a mood stabiliser used in the treatment of bipolar disorder.
Three others were identified in previous work to be affected by lithium carbonate – a mood stabiliser used in the treatment of bipolar disorder.
“Depending on which of those biomarkers are changed in [a patient], we have a list of medications … ranked by how tightly they match [the patient’s] biological profile,” Dr Niculescu said.
The blood tests developed by Dr Niculescu and his team are now available as CLIA tests for physicians to order, via a company set up by Niculescu and other experts in the field. CLIA are a set of US government standards for laboratories that test human specimens for health assessment or to diagnose, prevent, or treat disease
But according to Alexander Talkovsky, a programme officer in the Division of Translational Research at the National Institute of Mental Health (NIMH) in the United States, there is still research to be done. The key issue is whether the findings are replicated by independent researchers, he adds.
This process has been done to some extent within the study itself, says Dr Niculescu, through several steps of testing and validation in independent cohorts.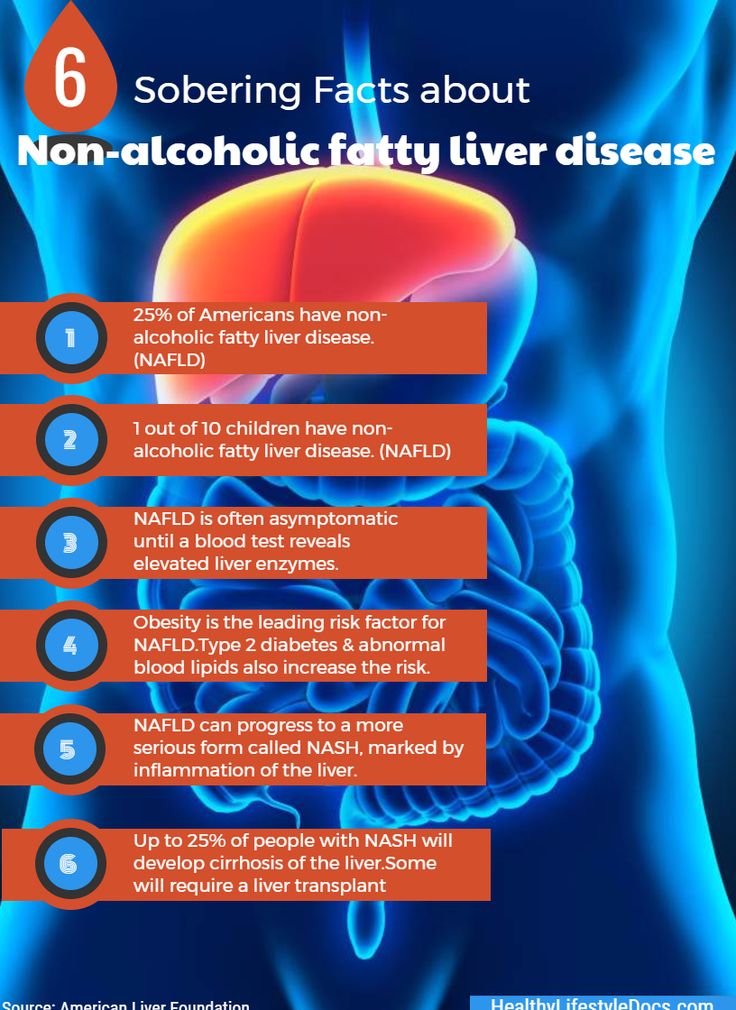 According to the study, promising findings were also generated by independent large scale genetic studies released after the study was complete.
According to the study, promising findings were also generated by independent large scale genetic studies released after the study was complete.
But what if the study’s premise is in itself incorrect?
Professor Ian Hickie, co-director of health and policy at the University of Sydney’s Brain and Mind Centre, and a former national mental health commissioner in Australia, argues that finding one algorithm which applies to all mood disorder patients is unlikely because the disorders are so individual and are based on clinical presentation at different stages of life.
His team is instead connecting physiology and biology to individual peoples’ symptoms, not their category of illness.
“What systems are actually perturbed? How are they represented? What are the markers of that that you can detect?” he said. “And [then] what is the combination of biological, behavioural and other treatments that corrects the situation … and then keeps you well?”
Essentially, all of these findings can be used in conjunction with clinical assessment for more accurate and conclusive diagnosis and treatment, he says.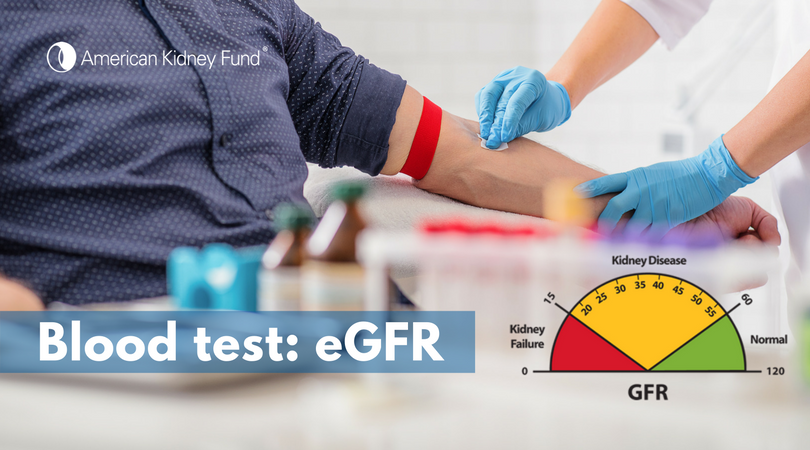
Objective testing could be of huge significance to patients going through what is currently an extremely slow process of diagnosis.
For bipolar disorder in particular, it can take years for the full array of symptoms to evolve.
Sydney psychiatrist, Dr Sonia Kumar, says that quite often bipolar disorder will first manifest itself as depression, with manic symptoms emerging later.
Other times, symptoms may be present but so low on the spectrum that diagnosis is unclear until they evolve.
If there were a biological test that could clarify these variables along with clinical assessment, says Kumar, clinicians could start accurate treatment earlier, which could mitigate a lot of suffering before it even happens.
Research associate Katrin Inci believes that an early diagnosis of her bipolar disorder could not only have saved her years of unresolved suffering, but also the severity to which her episodes escalated after diagnosis.
She was diagnosed with depression at age 13 and prescribed Zoloft, a type of antidepressant that is well known for inducing mania in bipolar patients.
“[It] spun me into a manic episode that lasted until I was 19, when I was hospitalised for the first time,” she said.
After her hospitalisation, when Inci finally received a correct diagnosis, she began what would be 10 years of trying new medications, navigating bipolar episodes and searching for wellness.
Dr Niculescu says objective tests for disorders like depression could help reduce the stigma associated with mental health conditions [Supplied]She believes that had she been diagnosed correctly at 13, her illness would not have become so severe.
Research shows that both bipolar and unipolar depression are degenerative diseases.
“If I was treated earlier … I would have had fewer episodes,” Inci told Al Jazeera. “I see it as [fewer] hospitalisations, which would have saved me tons of money and tons of time, and tons of anguish.”
An objective test for mood disorders like this blood test could also be key to reducing the stigma attached to mental health conditions, says Dr Niculescu.
“People will realise that it’s just a biological disorder … it’s not a moral weakness, you’re not lazy and so on,” he says.
Violet, a Russian model who prefers to share only her first name, has been living and working through depression for years.
She says she has internalised the stigma and often feels like a “liar”.
“Sometimes I feel like … I’m seeking attention or something,” she said. “These are things you get accused of a lot, even from people who are close to you … and then you start to wonder what if I’m actually just a selfish person who wants a lot of attention?”
Data goes a long way to dispelling this doubt, explains Kasia, a Sydney NGO worker who asked that only her first name be used.
She compares her diagnosis of depression as an adult with when she was diagnosed with Attention Deficit Hyperactivity Disorder (ADHD) as a child.
Because tests have been created for ADHD diagnosis, she was able to see objective results for her psychiatric assessment.
“They actually showed me all my brain scans and showed me how my brain was different. That was a huge day for me, it changed everything,” she said.
Kathmandu-based psychiatrist, Dr Pawan Sharma, says that such a test could break down even more barriers to care among his patients, particularly those from more rural, isolated communities where there is low cultural awareness of mental illness.
Many of these patients are not initially aware that sadness can be an illness, says the assistant professor in the department of psychiatry at the Patan Academy of Health Sciences.
“They come [to physicians] with physical symptoms – with headaches, insomnia, loss of energy, heart palpitations – and they [are then referred] to psychiatrists,” Dr Sharma said, noting that an objective test would give patients something tangible to help explain how they are feeling.
As it stands now, says NIMH’s Talkovsky, Dr Niculescu’s study goes a long way to achieving this and moving psychiatric research forward.
“What they’re doing represents a pretty important step in our ability to create objective markers [for] mental illness,” he said.
While it is still early days, with further research, the study’s blood test may yet become a significant part of the psychiatric diagnostic toolkit, bringing clarity to diagnosis and potentially changing millions of lives for the better.
Blood test for mental health: a discovery at the intersection of immunology and neurology
Photo from healththnowmedical.com
There are areas in medicine in which the accumulated body of knowledge does not yet allow effective prevention and treatment of diseases. These are psychiatry and neurology, closely related to each other, and immunology, which began to develop actively only from the middle of the last century. Interestingly, a number of recent studies by medical scientists have led to a stunning conclusion: the relationship between immune and nervous processes in the body is much more subtle and complex than was thought until recently.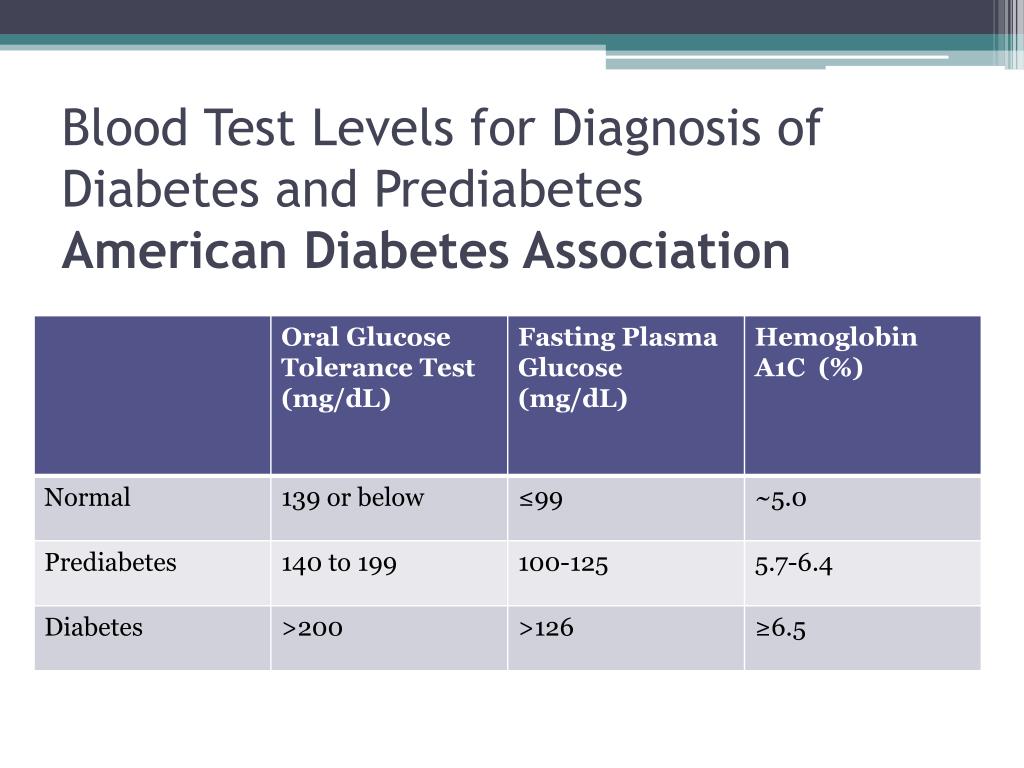
Suicide: recognize and prevent
Here, for example, is one of the extreme situations in psychiatry: a person is seized by suicidal thoughts, and he is one step away from committing suicide ... How to determine what is happening in the patient's head and prevent a fatal one in time step?
Scientists at the University of Georgia (USA) summarized data from 18 studies that included blood tests and post-mortem biopsy of the brain tissue of both psychiatric patients and healthy people. Among them were 583 patients with suicidal intentions, 315 without such, and 845 without deviations. Comparing the numbers, they found that the levels of two cytokines, interpleukin-1β and interleukin-6, were significantly elevated in the blood and brain of suicidal patients.
Cytokines are small informational molecules that the cells of the immune system use to communicate with each other. Pro-inflammatory cytokines provide the mobilization of the immune system's inflammatory response to infection or tissue damage - however, when the system fails, their work does not stop after the danger has passed. High levels of pro-inflammatory cytokines can lead to arthritis, atherosclerosis, asthma, and, as follows from the latest data, affect the mental state of a person.
High levels of pro-inflammatory cytokines can lead to arthritis, atherosclerosis, asthma, and, as follows from the latest data, affect the mental state of a person. Researchers hope that over time, a simple blood test will be enough to predict a patient's risk of dangerous self-injurious behavior, just as taking blood pressure readings today can prevent stroke risk.
Scientists are still in the initial stages of research. It is necessary to reproduce the results on a larger sample, as well as to evaluate the possibilities of preventing self-destructive actions of patients using anti-inflammatory therapies.
However, it is already clear that the literary image of an inflamed brain generating dangerous ideas is by no means a metaphor, although the Russian classics had no idea about cytokines.
Depression, psychosis and cytokines
Modern scientists from Cambridge are another matter. They analyzed data from a longitudinal (long-term) study of 4,500 parents and children.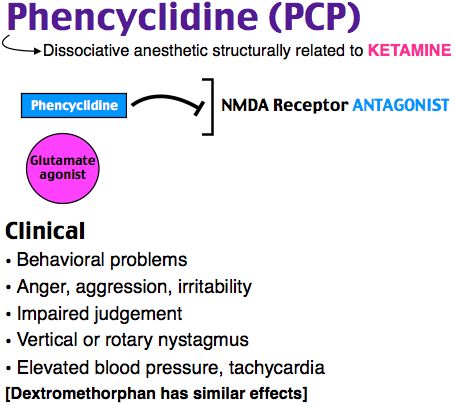 At the age of 9, blood samples were taken from the children, and at the age of 18, their mental health status was assessed.
At the age of 9, blood samples were taken from the children, and at the age of 18, their mental health status was assessed.
In accordance with the analysis data, all subjects were divided into three groups: with low, medium and high levels of the already familiar pro-inflammatory cytokine - interleukin-6 - in the blood. It turned out that in the third group, the risk of episodes of depression and psychosis was 2 times higher than in the first. Children who regularly had infectious diseases that led to the production of pro-inflammatory cytokines at the age of 18 were more prone to mental illness than their peers who experienced fewer flus and colds in childhood.
Scientists believe that inflammation may be a common factor that affects both physical and mental health. It is possible that both early childhood illness and stress lead to persistently high levels of interleukin-6 and other pro-inflammatory biomarkers, which in turn lead to chronic physical illness and mental impairment.
Patients with depression and schizophrenia are known to have a higher risk of heart disease and type 2 diabetes.
Findings by Cambridge scientists suggest that exercise and diet not only reduce the risk of heart disease, but also combat depression due to the common origin of these diseases.
Can anti-inflammatory drugs help treat psychotic disorders? This remains to be seen, but it is possible that antipsychotics will work best when combined with aspirin or another well-known and cheap remedy. There have already been similar studies in which aspirin has proven itself well as an additional drug in the treatment of schizophrenia spectrum diseases.
Multicentre clinical trials of the antibiotic minocycline, which can cross the blood-brain barrier and enter the brain, are currently underway to treat symptoms of schizophrenia such as apathy, withdrawal, and inability to enjoy. They can also be a consequence of the inflammatory process in the central nervous system.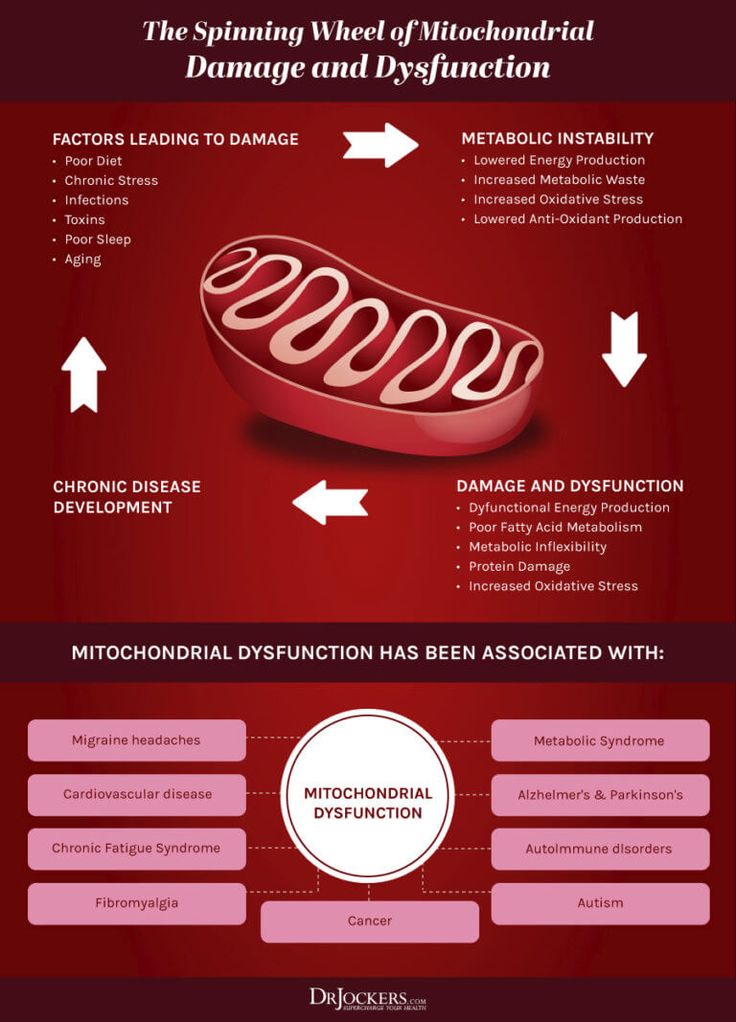
The immune system on the autism spectrum
The first assumptions about the role of immune system imbalance in autism were made 40 years ago, and now science has a lot of evidence for this theory. Research suggests that the levels of pro-inflammatory cytokines in the brains of autistic patients are also elevated and microglial cells are activated. Microglia are specialized immune cells of the nervous system that act as phagocytes that destroy infectious agents. Their activation leads to the destruction of nerve cells.
Evidence of impaired immune system function in autistic individuals has been obtained by scientists at the University of Kansas, researchers at the Department of Neurology at the Massachusetts General Hospital, and other research teams. And in April 2015, the journal Immunity published the work of scientists from the University of Virginia who discovered mutations in the MeCP2 gene in the microphages of patients with Rett syndrome.
Rett syndrome is a severe form of autism that affects almost exclusively girls. After an initial period of normal development of 12 to 18 months, the child begins to lose acquired skills and develop seizures and other physiological symptoms.
After an initial period of normal development of 12 to 18 months, the child begins to lose acquired skills and develop seizures and other physiological symptoms. Scientists have previously associated the disease with a mutation of the MeCP2 gene in brain cells, but the same mutation in immune cells is a completely unexpected and promising discovery. With Rett syndrome, the heart, muscles, gastrointestinal tract, and bone tissue are affected, and it is likely that therapy aimed at restoring the patient's immune function will help to significantly improve their condition.
The development of such a therapy is not a quick matter. It can be assumed, however, that transplantation of healthy donor bone marrow will be effective.
As for other parts of the autism spectrum, helminth therapy, which is being developed by several experimental teams in the USA, Great Britain, and Italy, seems to be very promising. A research team at Montefiori Medical Center and the Albert Einstein College of Medicine in New York, led by Dr.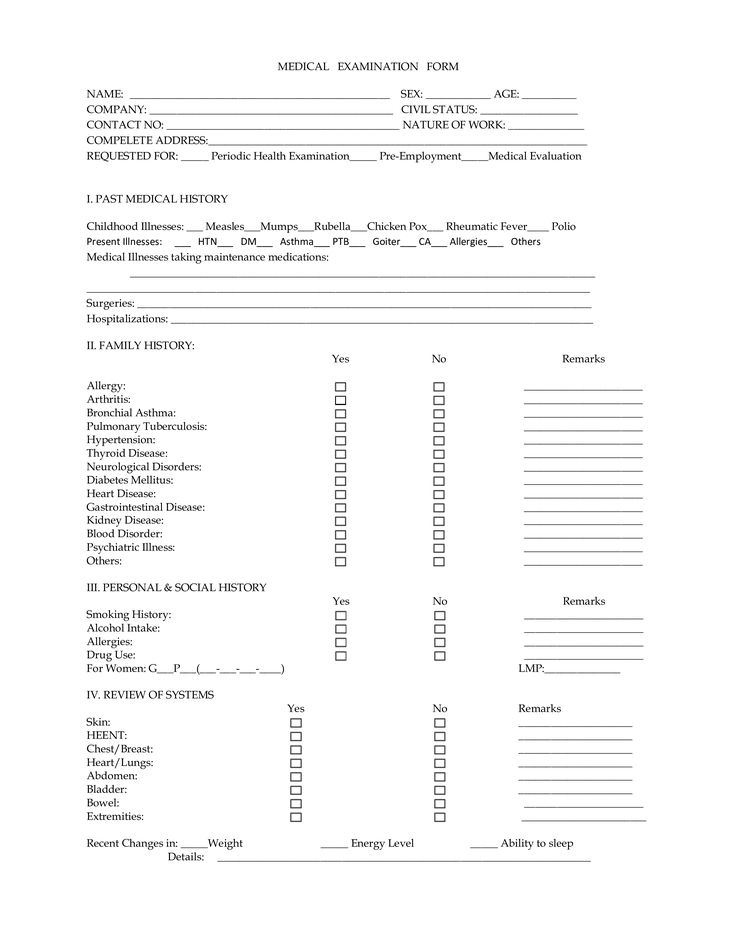 Eric Hollander, has tested the eggs of whipworm (Trichuris suis), a parasitic worm that lives in the intestines of pigs, as an immune therapy for autistic adults, with promising results. . This therapy is recognized as effective for the treatment of irritable bowel syndrome, but in the field of autism it has so far an experimental status.
Eric Hollander, has tested the eggs of whipworm (Trichuris suis), a parasitic worm that lives in the intestines of pigs, as an immune therapy for autistic adults, with promising results. . This therapy is recognized as effective for the treatment of irritable bowel syndrome, but in the field of autism it has so far an experimental status.
The aim of the Hollander group is to find out the effectiveness of this type of helminth in the treatment of symptoms of autism in children. The researchers hope that the use of Trichuris suis will overcome or alleviate irritability, rigidity, and a tendency to repetitive self-stimulating activities.
And most importantly:
More recently, it was discovered that the connection between the immune and nervous systems exists not only at the biochemical, but also at the anatomical level! Antoine Louveau, a laboratory professor at the University of Virginia Health System (UAV), made an amazing discovery: he found lymphatic vessels in the cerebral cortex.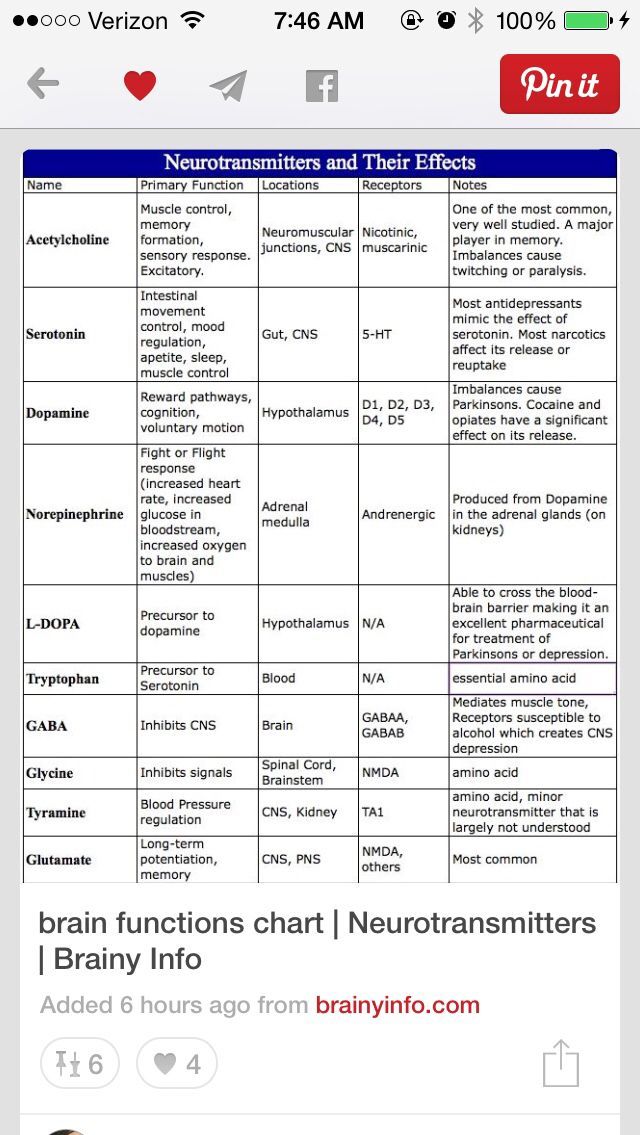
The lymphatic system complements the cardiovascular system and plays an important role in metabolism and the immune system. Until recently, scientists did not find lymphatic vessels in the cerebral cortex, as is now clear, due to the fact that they "hide", adjoining very close to the blood vessels. Since the study area is difficult to depict in a photograph, it was almost impossible to see the lymphatic vessels using standard methods.
One of the serious diseases associated with dysfunction of the immune and nervous systems is multiple sclerosis. The reasons for its occurrence remain unclear, and it is likely that it is the lymphatic vessels of the brain that are involved in the destructive process. According to the head of the scientific group, Professor Jonathan Kipnis, "in every neurological disease that has an immune component, these vessels can play an important role." Scientists hope that their further study will shed light on the cause of brain diseases and their treatment - from Alzheimer's disease and multiple sclerosis to autism.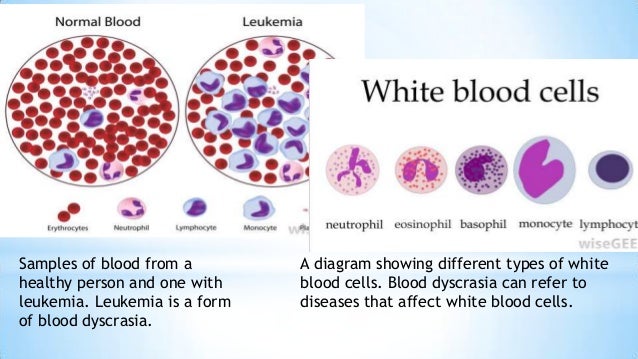
Establishing targeted and effective therapies for neurological and psychiatric diseases associated with the immune system is an ambitious and time-consuming task. However, even today there is every reason to raise the question of the study of the immune status of neurological and psychiatric patients as a necessary part of the examination of such patients.
Sources:
- Cytokines, Which Contribute To Inflammation, Found At High Levels In Brains Of Suicidal Patients
- Overactive Immune System May Be Linked to Mental Illness Risk
There is a genetic link between blood tests and mental disorders — Realnoe Vremya
Society
00:00, 04/19/2022
Is there a genetic link between blood biochemistry and mental disorders?
Biological markers of psychiatric disorders such as depression, schizophrenia and anorexia are found in routine blood tests.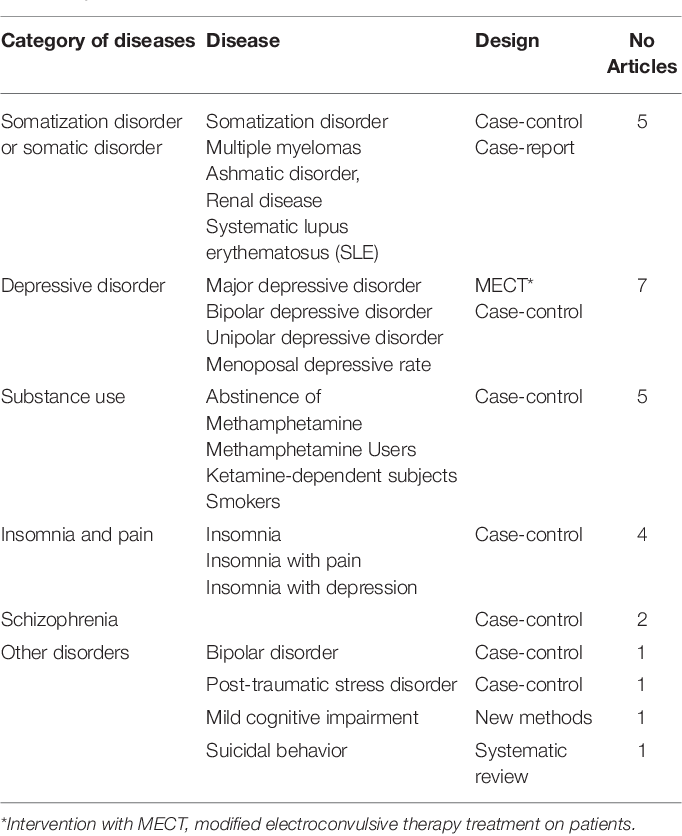 This is written for The Conversation by William Wray, a postdoctoral fellow at the School of Biomedical Sciences and Pharmacy at Newcastle University in Australia.
This is written for The Conversation by William Wray, a postdoctoral fellow at the School of Biomedical Sciences and Pharmacy at Newcastle University in Australia.
Psychiatric disorders, including depression, schizophrenia and anorexia, are directly related to biochemical parameters found in routine blood tests, according to our new study of genetic, biochemical and psychiatric data from nearly a million people.
This study may expand our understanding of what causes mental illness and may help identify new treatments.
A healthy mind in a healthy body
People often view mental health as separate from the health of the physical body. Far from it, there is clear evidence that many biochemical processes, such as those that cause diabetes and autoimmune diseases, directly affect our brain function.
Many studies have tried to solve this problem by focusing on substances called biomarkers that can be easily measured in the blood.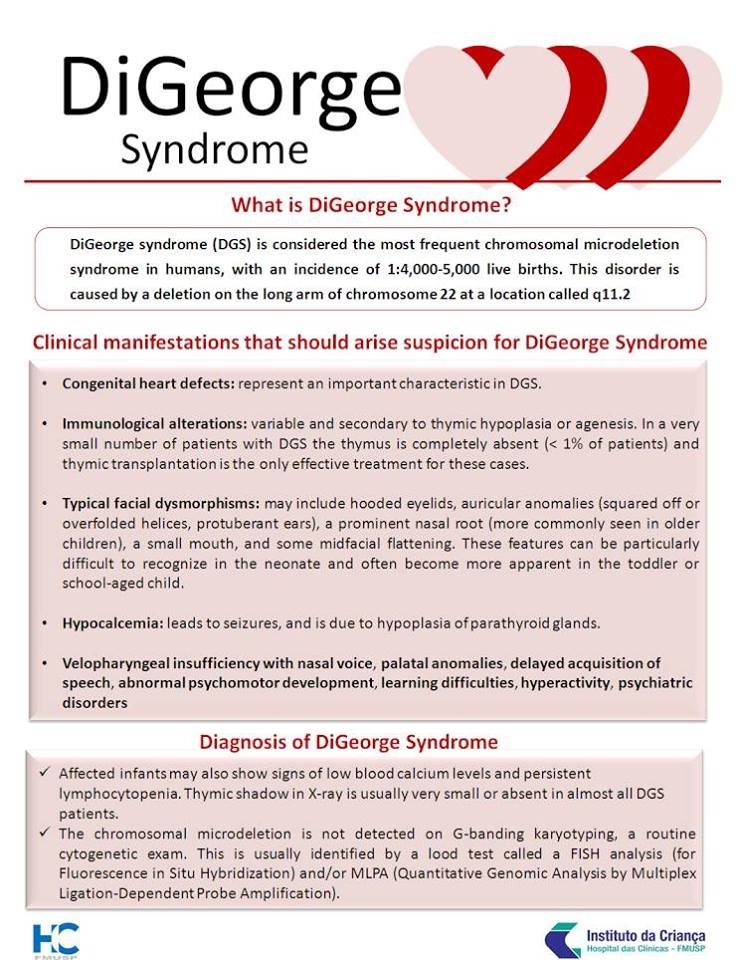
A biomarker is a kind of "mark" in the body, which is a sign of a certain disease or ongoing process. They are often related to the things your doctor tells you when reading your blood tests: cholesterol, blood sugar, liver enzymes, vitamins, or markers of inflammation.
Biomarkers found in routine blood tests are useful because they are often influenced by diet, lifestyle, and medication.
Photo: Maxim PlatonovThe complex role of genetics in mental health
It is often difficult to study the role of blood biomarkers in relation to mental health. Many studies in this area are often not large enough to draw firm conclusions.
One solution is to study the genetic influence on both mental illness and marker substances. Genetics are useful because we now have data from millions of people who have volunteered for research.
Both mental illness and blood biomarkers are what geneticists call "complex traits." Many genes are involved in complex traits, and environmental factors also contribute.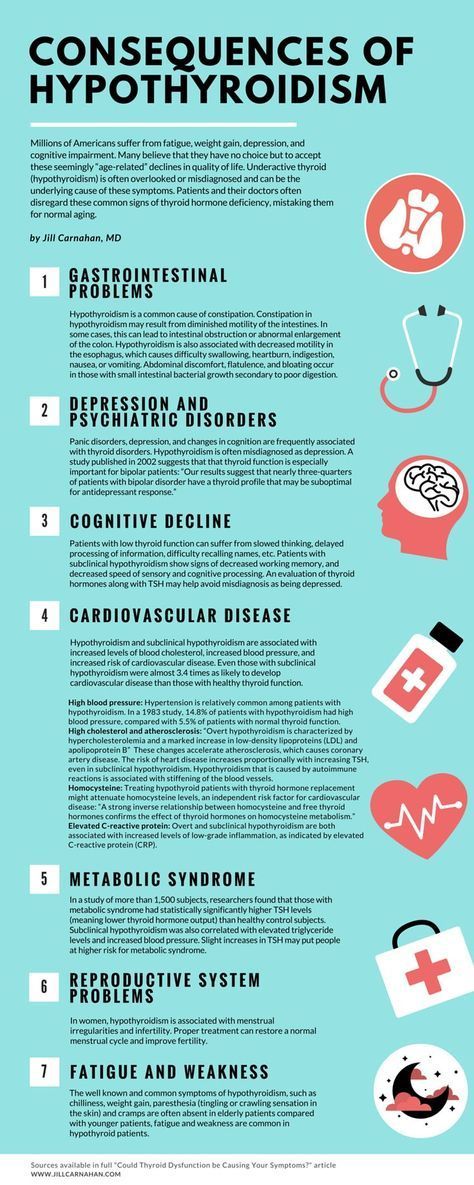
The wide availability of genetic data has allowed us to investigate how a huge number of tiny changes in the DNA sequence (or "variants") are associated with the risk of mental illness. These same variants can then be linked to measured blood levels of biomarkers.
For example, a variant of a certain gene may increase the risk of developing schizophrenia and may also be associated with a decrease in the level of a vitamin circulating in the blood. Most of these options individually are associated with very small changes in something, such as the risk of mental illness, but together they can cause more serious problems.
Photo: in-narofominsk.ruHow are blood biomarkers related to mental illness?
In our recent study, we sought to use genetics to explore the relationship between nine mental disorders and 50 factors measured in routine blood tests, such as cholesterol, vitamins, enzymes, and indicators of inflammation. We used data from very large studies, including nearly a million volunteers in total.
Our study confirms for the first time the existence of a so-called genetic correlation between blood biomarkers and mental illness. Genetic correlation means the effect of DNA sequence changes on the risk of mental illness, and the levels of this biomarker were more similar to each other than what could happen only by chance.
Take, for example, the positive genetic correlation between white blood cell count and depression. This may indicate that some process in our body affects both depression and white blood cells.
If we could define what this general process is, it could lead to a better understanding of what causes depression and it could be more accurately targeted for treatment.
Photo: Maxim PlatonovCorrelation or causation?
Our study showed that there is a correlation between the genetics of mental illness and factors in the blood, but it does not tell us whether blood biomarkers are involved in what causes mental illness.
To distinguish between correlation and causation in medicine, there are clinical trials in which patients are randomly given treatment or placebo. However, these tests are expensive and difficult to perform.
We did the best thing: we used DNA variants associated with changes in blood biomarkers to act like a natural clinical trial. This process exploits the fact that we randomly inherit DNA variants from our parents, in much the same way that clinical trial participants randomly receive a treatment or a placebo.
This is a complex method and the results require careful interpretation
We have found evidence that certain substances measured in the blood may indeed be the cause of some mental illnesses. For example, proteins associated with the immune system may be involved in depression, schizophrenia, and anorexia.
Further work is now needed to determine exactly how these blood counts are related to these disorders. The next step is to find out if they can be referred for treatment.