Bipolar disorder vs schizophrenia
Bipolar Disorder vs. Schizophrenia: What’s the Difference?
Bipolar disorder and schizophrenia are two different chronic mental health disorders. People can sometimes mistake the symptoms of bipolar disorder for schizophrenia symptoms.
Read on to learn how these conditions are alike and how they differ.
Bipolar disorder and schizophrenia have some aspects in common, but here are the main differences:
Symptoms
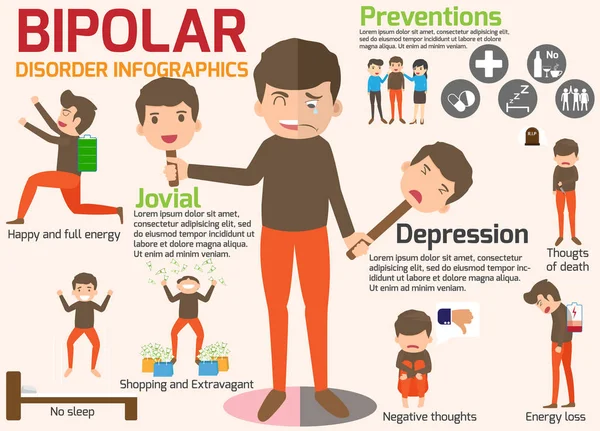
Bipolar disorder causes strong shifts in energy, mood, and activity levels. A person with bipolar disorder will switch between extreme excitement or mania and depression.
This may not happen continuously, meaning that you can experience spontaneous periods of a stable mood followed by periods of extreme mood shifts.
When they occur, these shifts can affect their ability to perform daily activities. In some cases, a person with bipolar disorder may also experience hallucinations and delusions (see below).
Schizophreniacauses symptoms that are more severe than the symptoms of bipolar disorder. People with schizophrenia experience hallucinations and delusions.
Hallucinations involve seeing, hearing, tasting, smelling, or feeling things that aren’t there. Delusions are false, irrational beliefs.
People with schizophrenia may also experience disorganized thinking, which can render them unable to care for themselves.
Frequency and ages affected
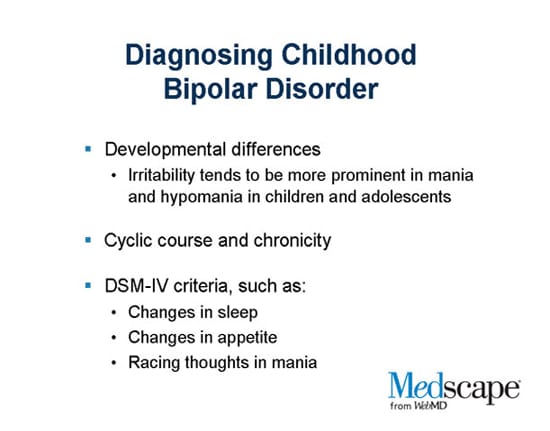
Bipolar disorder affects approximately 2.8 percent of people in the United States. Typically, it first appears between the late teen years and early adulthood. Children can also show signs of bipolar disorder.
Schizophrenia isn’t as common as bipolar disorder. It’s long been estimated to affect less than 1 percent of the U.S. population, although newer research suggests that it could range up to 1.6 percent or higher. People usually learn they have it between the ages of 16 and 30. Schizophrenia isn’t usually seen in children.
People living with bipolar disorder tend to undergo intense mood shifts that occur rapidly or over an extended time.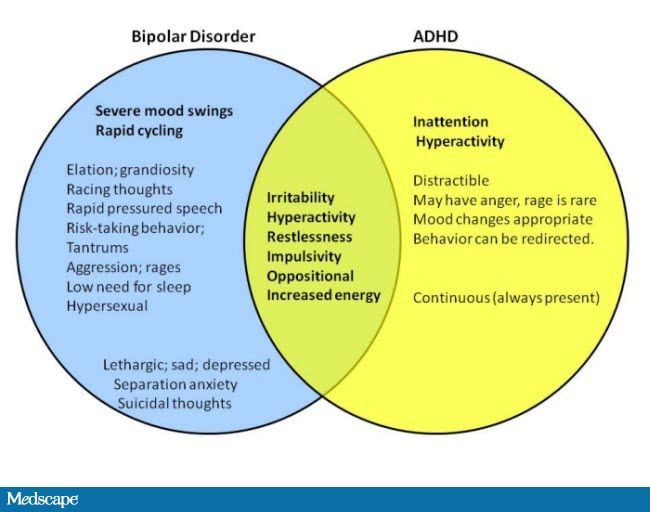 They can experience three types of episodes:
They can experience three types of episodes:
- Manic: Those having a manic episode may feel extremely elated, wired, jumpy, or irritable. They are highly energetic and active; their mood is expansive.
- Hypomanic: People undergoing hypomania will have less intense manic symptoms.
- Depressive: Those having a depressive episode may feel sad, hopeless, or anxious and lose interest in activities they used to enjoy. This mimics the symptoms of major depression.
People may be diagnosed with bipolar I disorder after having at least one episode of mania. They can be diagnosed with bipolar II disorder after undergoing a major depressive episode and hypomania.
These mood shifts may not occur continuously. Even if you experience periods of stable mood occasionally, you can be diagnosed with bipolar disorder as long as you fit the diagnostic criteria.
Cyclothymia, a less-intense condition, is diagnosed after someone exhibits alternating episodes of low-level depression and hypomania.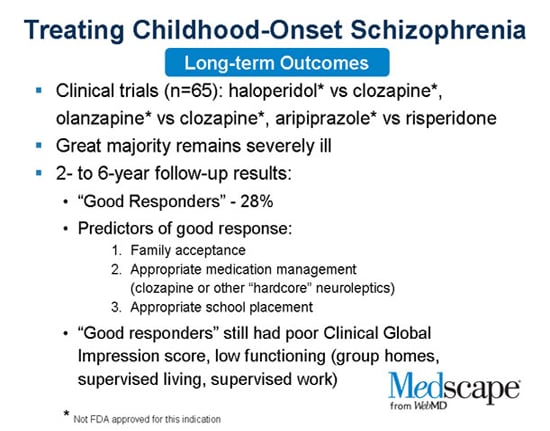
Other behavioral changes that may be symptoms of bipolar disorder include:
- restlessness
- hyperactivity
- reduced need for sleep or disordered sleep
- trouble staying focused
- irritability
- extreme self-confidence and impulsivity (manic episode)
- suicidal thoughts (depressive episode)
People with bipolar disorder may also experience psychotic symptoms during a severe manic or depressive episode. These can include hallucinations or delusions. Because of this, people may mistake symptoms of bipolar disorder for those of schizophrenia.
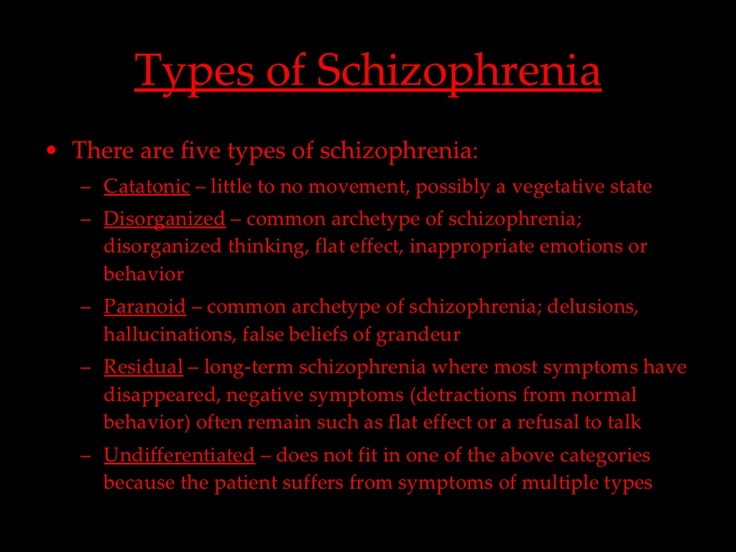
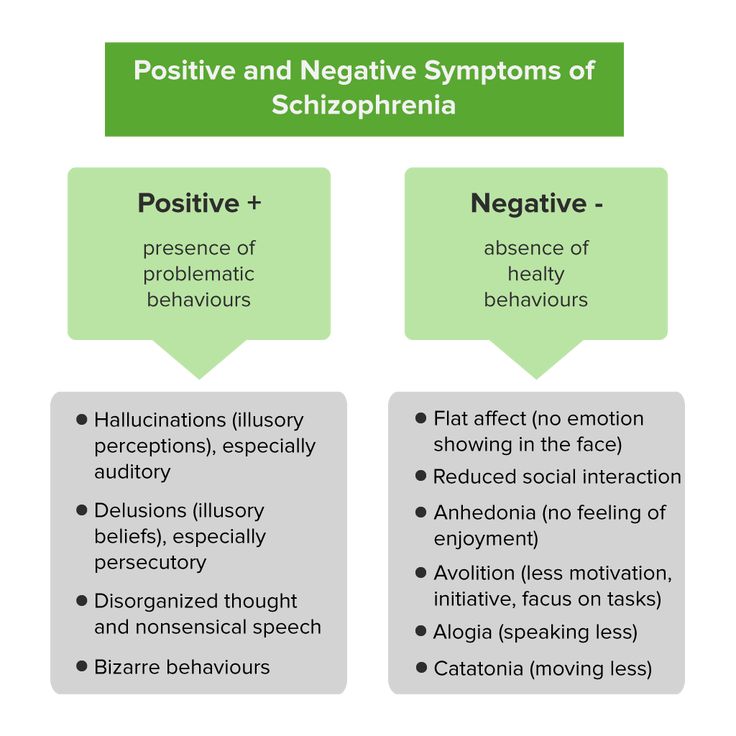
The symptoms of schizophrenia are divided into two groups, generally referred to as “positive symptoms” and “negative symptoms.” This isn’t based on whether a symptom is good or bad but on whether the symptoms add or remove a behavior.
Positive symptoms might include the introduction of delusions or hallucinations. Negative symptoms might include social withdrawal or removing oneself from relationships or public events.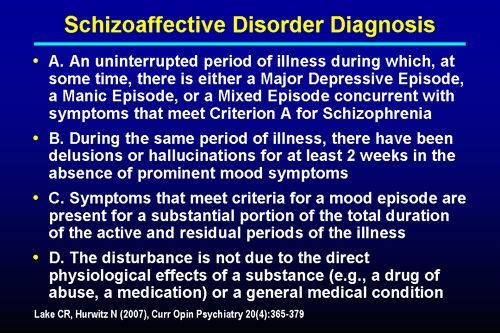
The early warning signs of schizophrenia can include:
- social isolation
- a loss of interest in activities
- moodiness
- a lack of any feelings
- making irrational statements
- surprising or unusual behavior
- an altered sleep schedule
- getting either too much or too little sleep
- an inability to express emotions
- inappropriate laughter
- violent outbursts
- acts of violence toward oneself
- hypersensitivity to touch, taste, and sound
- hallucinations (including auditory ones that appear as threatening, insulting or condemning voices)
- delusions
No one knows exactly what causes bipolar disorder or schizophrenia. But genetics is probably a risk factor, as both conditions can run in families.
This doesn’t mean someone will inherit the disorders if their parent or sibling has them. The risk increases, however, if multiple family members do. But just being aware of that risk increases the chance of early detection and treatment.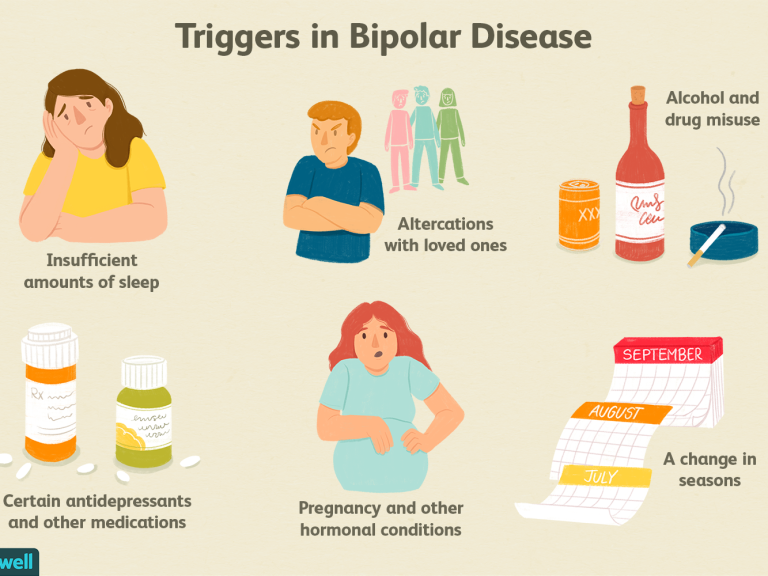
Environmental factors may also contribute to risk, but this connection isn’t entirely understood.
It is generally believed that both conditions occur equally across sex, race, and ethnicity, though historically, African American and Latino American/Hispanic individuals have been diagnosed with schizophrenia more often than other people, while Asian and Latino individuals have been more often diagnosed with bipolar I. Experts think these diagnoses could have been affected by bias or missed symptoms, making them unreliable.
Health professionals cannot use blood tests to diagnose bipolar disorder or schizophrenia. Instead, they will usually conduct a physical and psychological exam. During the exam, they’ll ask about their patient’s personal or family history of mental disorders and inquire into what symptoms they may have been experiencing.
On occasion, a blood test, MRI, or CT scan of the brain will be needed to help rule out other conditions. At times, a drug and alcohol screening may also be necessary.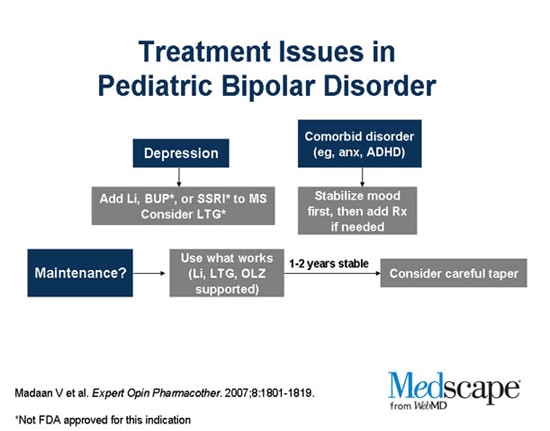
It may take several visits before the final determination is made. These visits are necessary and allow health professionals to get a full picture of a person’s symptoms. They may also ask patients to keep a daily record of mood and sleep patterns. This will help them spot patterns that point to manic and depressive episodes.
Treatment for bipolar disorder and schizophrenia can involve both therapy and medication.
For bipolar disorder, psychotherapy may include:
- learning about changes in mood and how to effectively manage them
- educating family members about the disorder so they can be supportive and help address episodes
- exploring how to improve relationships with friends and co-workers
- understanding how to avoid possible triggers, such as stress or a lack of sleep
A healthcare professional may prescribe medication that controls mood and helps with other symptoms. Examples include:
- mood stabilizers such as lithium
- atypical antipsychotics
- anticonvulsants
- anti-anxiety medications
People with bipolar disorder often have trouble sleeping.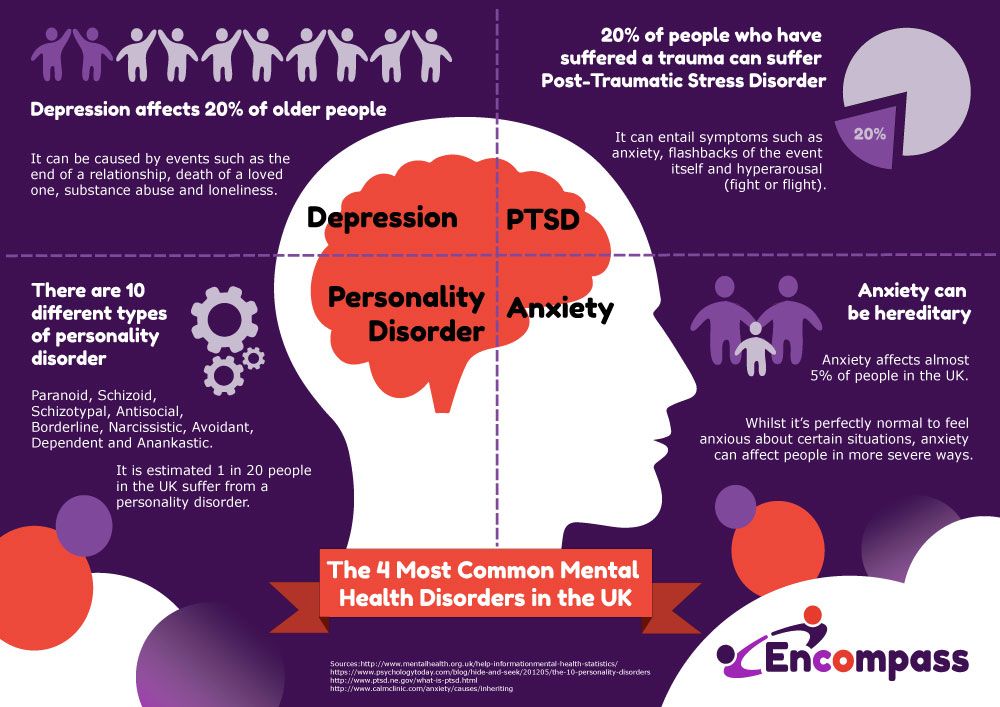 Sleep medication is sometimes prescribed.
Sleep medication is sometimes prescribed.
Treatment for schizophrenia includes antipsychotics and psychotherapy. Some of the more common antipsychotics used to treat schizophrenia include:
- risperidone (Risperdal)
- aripiprazole (Abilify)
- paliperidone (Invega)
- olanzapine (Zyprexa)
- ziprasidone (Geodon)
- haloperidol (Haldol)
Psychotherapy approaches may include cognitive behavioral therapy.
It’s possible to have an initial schizophrenic episode and never experience another one. People who have experienced just one episode may find a coordinated specialty care program called Recovery After an Initial Schizophrenia Episode especially helpful. The program offers:
- psychotherapy
- medication management
- family education and support
- work or education support
People living with bipolar disorder or schizophrenia have an increased risk of suicide. Anyone who has had suicidal thoughts should speak to a healthcare professional about treatment.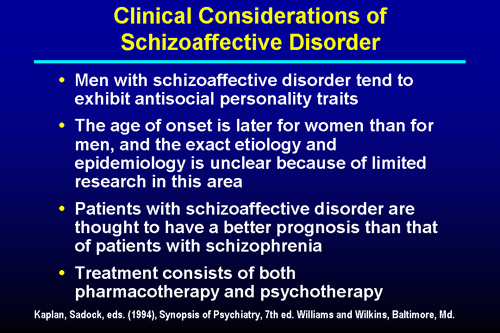 It is extremely important to continue taking all medications as your doctor prescribes, even if you’re feeling better.
It is extremely important to continue taking all medications as your doctor prescribes, even if you’re feeling better.
In addition, anyone living with bipolar disorder or schizophrenia may consider:
- joining a support group such as NAMI Connection
- Avoiding alcohol and substance use
- Following a relatively stable lifestyle.
- Getting an adequate amount of sleep.
- Maintaining a healthy diet.
- Using techniques to manage stress.
Bipolar disorder and schizophrenia can be confused, but they are different chronic mental health disorders. Some of the symptoms can overlap. However, bipolar disorder primarily causes extreme mood shifts, whereas schizophrenia causes delusions and hallucinations.
Both disorders can be serious and psychologically debilitating, though bipolar disorder is more common than schizophrenia. Both conditions may also be genetic, though it is thought that environmental factors may also be triggers.
Early diagnosis is critical.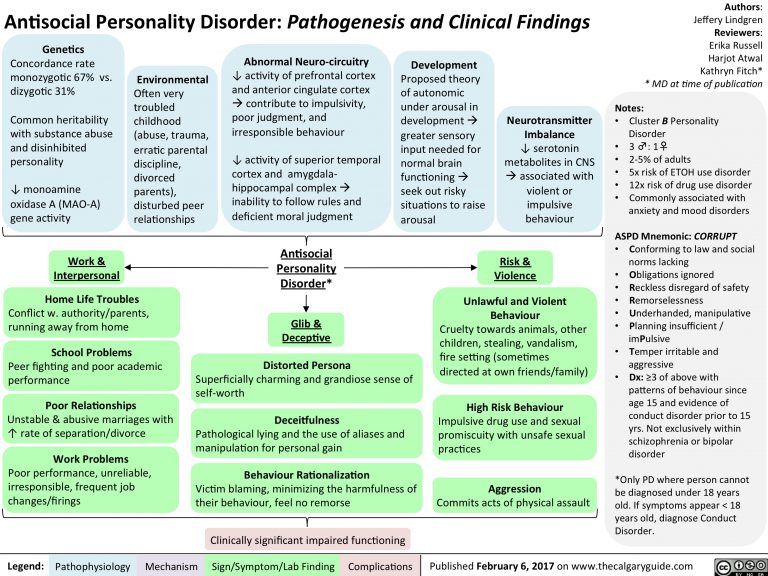 Be sure to speak with a healthcare professional if there is any concern about the emergence of bipolar disorder or schizophrenia. A well-thought-out treatment plan can go a long way toward managing these conditions and preventing future relapses. So will avoiding lifestyle and environmental factors that trigger episodes.
Be sure to speak with a healthcare professional if there is any concern about the emergence of bipolar disorder or schizophrenia. A well-thought-out treatment plan can go a long way toward managing these conditions and preventing future relapses. So will avoiding lifestyle and environmental factors that trigger episodes.
Can bipolar and schizophrenia occur together?
There is research indicating that similar genetic factors can predispose a person to develop either of the conditions. But you can be diagnosed with schizophrenia or bipolar disorder based only on criteria from the “Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5).”
This is because one diagnosis will usually exclude the other. But if a person exhibits symptoms of both conditions but does not fit either of these diagnoses, they could have schizoaffective disorder.
How can I help a person with schizophrenia or bipolar disorder?
It is difficult to watch a friend or a loved one with a mental health condition.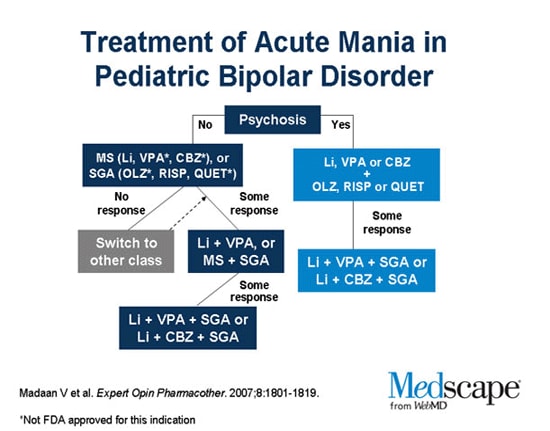 A good place to find advice on how to cope and how to help can be a support group. Consider joining the family support group of the National Alliance of Mental Illness (NAMI) or other support groups in your area.
A good place to find advice on how to cope and how to help can be a support group. Consider joining the family support group of the National Alliance of Mental Illness (NAMI) or other support groups in your area.
What should I do if I am diagnosed with schizophrenia or bipolar disorder?
You can manage the symptoms of bipolar disorder and schizophrenia with medication and therapy combined with a healthy lifestyle. Having a support system through support groups and family, friends, or co-workers can help you as you undergo treatment.
Bipolar Disorder vs. Schizophrenia: What’s the Difference?
Bipolar disorder and schizophrenia are two different chronic mental health disorders. People can sometimes mistake the symptoms of bipolar disorder for schizophrenia symptoms.
Read on to learn how these conditions are alike and how they differ.
Bipolar disorder and schizophrenia have some aspects in common, but here are the main differences:
Symptoms
Bipolar disorder causes strong shifts in energy, mood, and activity levels.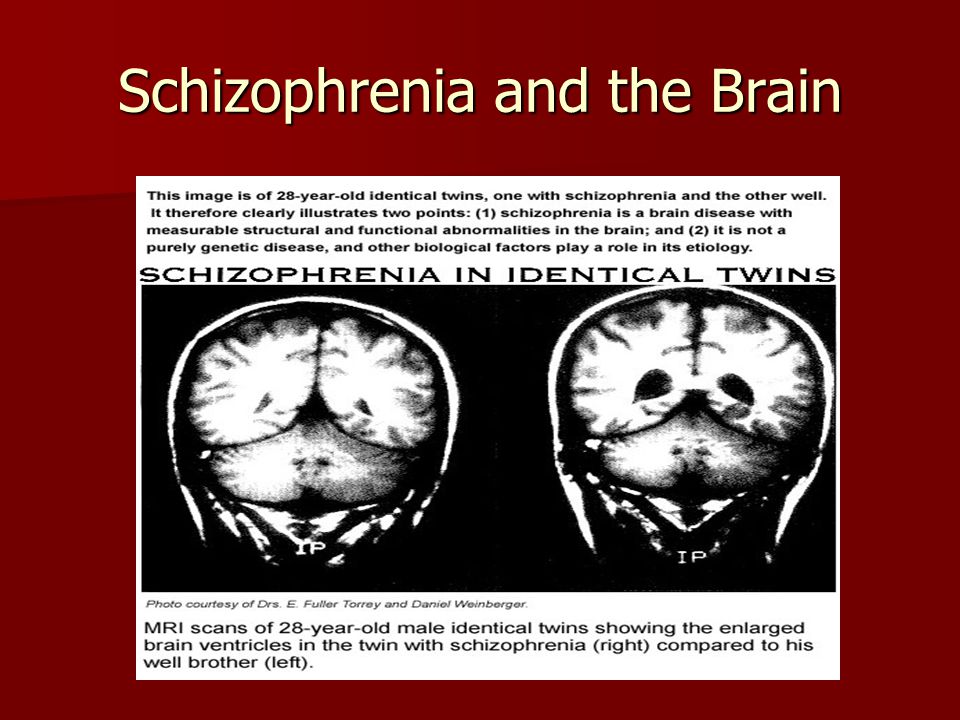 A person with bipolar disorder will switch between extreme excitement or mania and depression.
A person with bipolar disorder will switch between extreme excitement or mania and depression.
This may not happen continuously, meaning that you can experience spontaneous periods of a stable mood followed by periods of extreme mood shifts.
When they occur, these shifts can affect their ability to perform daily activities. In some cases, a person with bipolar disorder may also experience hallucinations and delusions (see below).
Schizophreniacauses symptoms that are more severe than the symptoms of bipolar disorder. People with schizophrenia experience hallucinations and delusions.
Hallucinations involve seeing, hearing, tasting, smelling, or feeling things that aren’t there. Delusions are false, irrational beliefs.
People with schizophrenia may also experience disorganized thinking, which can render them unable to care for themselves.
Frequency and ages affected
Bipolar disorder affects approximately 2.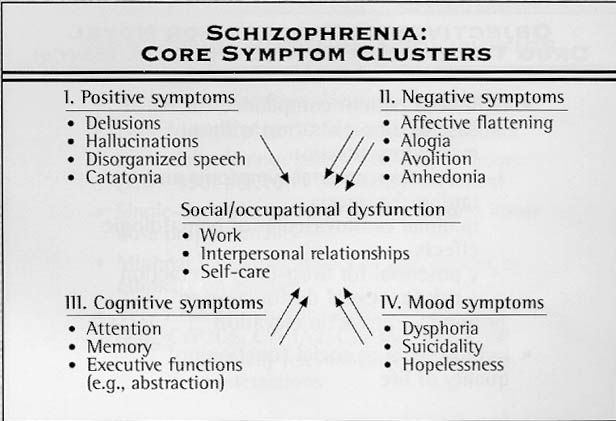 8 percent of people in the United States. Typically, it first appears between the late teen years and early adulthood. Children can also show signs of bipolar disorder.
8 percent of people in the United States. Typically, it first appears between the late teen years and early adulthood. Children can also show signs of bipolar disorder.
Schizophrenia isn’t as common as bipolar disorder. It’s long been estimated to affect less than 1 percent of the U.S. population, although newer research suggests that it could range up to 1.6 percent or higher. People usually learn they have it between the ages of 16 and 30. Schizophrenia isn’t usually seen in children.
People living with bipolar disorder tend to undergo intense mood shifts that occur rapidly or over an extended time. They can experience three types of episodes:
- Manic: Those having a manic episode may feel extremely elated, wired, jumpy, or irritable. They are highly energetic and active; their mood is expansive.
- Hypomanic: People undergoing hypomania will have less intense manic symptoms.
- Depressive: Those having a depressive episode may feel sad, hopeless, or anxious and lose interest in activities they used to enjoy.
 This mimics the symptoms of major depression.
This mimics the symptoms of major depression.
People may be diagnosed with bipolar I disorder after having at least one episode of mania. They can be diagnosed with bipolar II disorder after undergoing a major depressive episode and hypomania.
These mood shifts may not occur continuously. Even if you experience periods of stable mood occasionally, you can be diagnosed with bipolar disorder as long as you fit the diagnostic criteria.
Cyclothymia, a less-intense condition, is diagnosed after someone exhibits alternating episodes of low-level depression and hypomania.
Other behavioral changes that may be symptoms of bipolar disorder include:
- restlessness
- hyperactivity
- reduced need for sleep or disordered sleep
- trouble staying focused
- irritability
- extreme self-confidence and impulsivity (manic episode)
- suicidal thoughts (depressive episode)
People with bipolar disorder may also experience psychotic symptoms during a severe manic or depressive episode.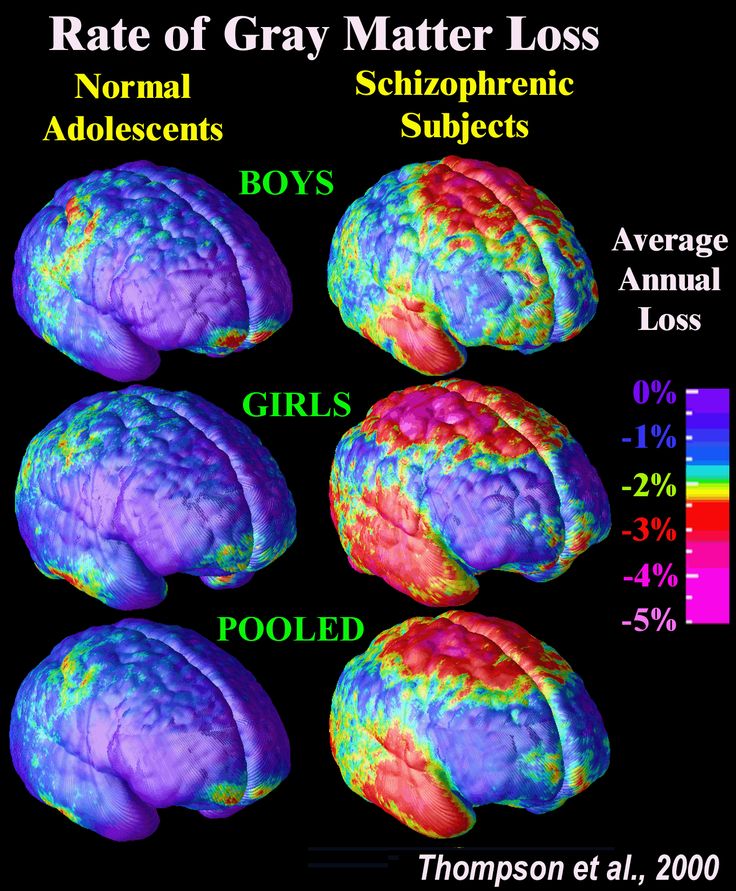 These can include hallucinations or delusions. Because of this, people may mistake symptoms of bipolar disorder for those of schizophrenia.
These can include hallucinations or delusions. Because of this, people may mistake symptoms of bipolar disorder for those of schizophrenia.
The symptoms of schizophrenia are divided into two groups, generally referred to as “positive symptoms” and “negative symptoms.” This isn’t based on whether a symptom is good or bad but on whether the symptoms add or remove a behavior.
Positive symptoms might include the introduction of delusions or hallucinations. Negative symptoms might include social withdrawal or removing oneself from relationships or public events.
The early warning signs of schizophrenia can include:
- social isolation
- a loss of interest in activities
- moodiness
- a lack of any feelings
- making irrational statements
- surprising or unusual behavior
- an altered sleep schedule
- getting either too much or too little sleep
- an inability to express emotions
- inappropriate laughter
- violent outbursts
- acts of violence toward oneself
- hypersensitivity to touch, taste, and sound
- hallucinations (including auditory ones that appear as threatening, insulting or condemning voices)
- delusions
No one knows exactly what causes bipolar disorder or schizophrenia. But genetics is probably a risk factor, as both conditions can run in families.
But genetics is probably a risk factor, as both conditions can run in families.
This doesn’t mean someone will inherit the disorders if their parent or sibling has them. The risk increases, however, if multiple family members do. But just being aware of that risk increases the chance of early detection and treatment.
Environmental factors may also contribute to risk, but this connection isn’t entirely understood.
It is generally believed that both conditions occur equally across sex, race, and ethnicity, though historically, African American and Latino American/Hispanic individuals have been diagnosed with schizophrenia more often than other people, while Asian and Latino individuals have been more often diagnosed with bipolar I. Experts think these diagnoses could have been affected by bias or missed symptoms, making them unreliable.
Health professionals cannot use blood tests to diagnose bipolar disorder or schizophrenia. Instead, they will usually conduct a physical and psychological exam.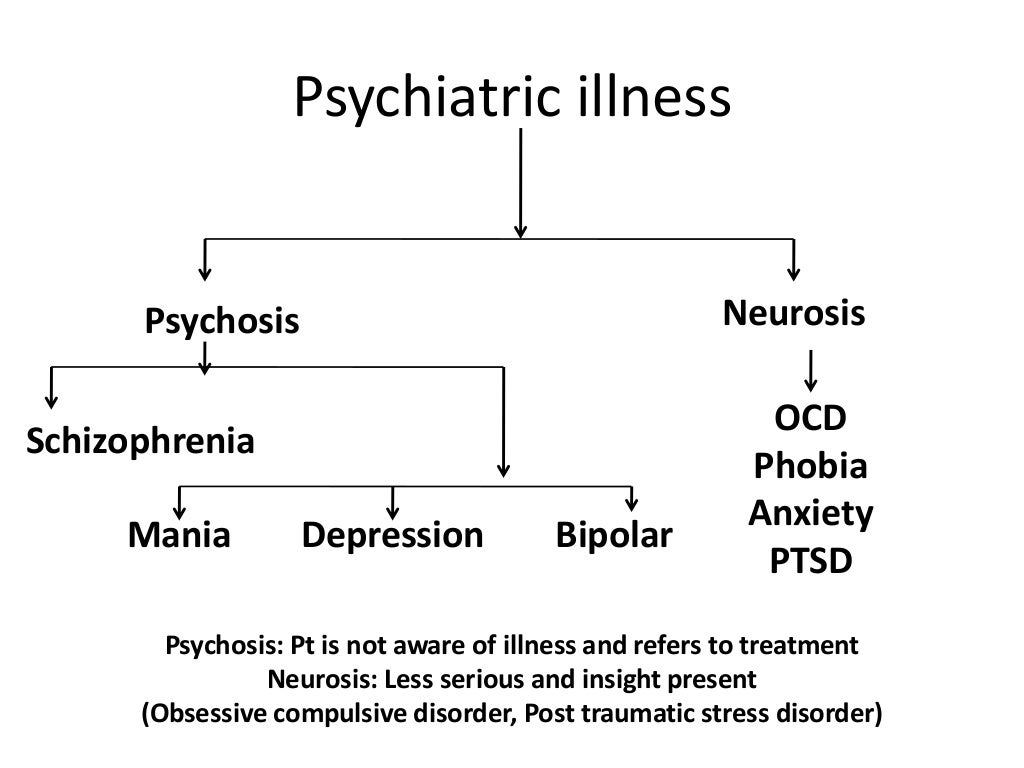 During the exam, they’ll ask about their patient’s personal or family history of mental disorders and inquire into what symptoms they may have been experiencing.
During the exam, they’ll ask about their patient’s personal or family history of mental disorders and inquire into what symptoms they may have been experiencing.
On occasion, a blood test, MRI, or CT scan of the brain will be needed to help rule out other conditions. At times, a drug and alcohol screening may also be necessary.
It may take several visits before the final determination is made. These visits are necessary and allow health professionals to get a full picture of a person’s symptoms. They may also ask patients to keep a daily record of mood and sleep patterns. This will help them spot patterns that point to manic and depressive episodes.
Treatment for bipolar disorder and schizophrenia can involve both therapy and medication.
For bipolar disorder, psychotherapy may include:
- learning about changes in mood and how to effectively manage them
- educating family members about the disorder so they can be supportive and help address episodes
- exploring how to improve relationships with friends and co-workers
- understanding how to avoid possible triggers, such as stress or a lack of sleep
A healthcare professional may prescribe medication that controls mood and helps with other symptoms. Examples include:
Examples include:
- mood stabilizers such as lithium
- atypical antipsychotics
- anticonvulsants
- anti-anxiety medications
People with bipolar disorder often have trouble sleeping. Sleep medication is sometimes prescribed.
Treatment for schizophrenia includes antipsychotics and psychotherapy. Some of the more common antipsychotics used to treat schizophrenia include:
- risperidone (Risperdal)
- aripiprazole (Abilify)
- paliperidone (Invega)
- olanzapine (Zyprexa)
- ziprasidone (Geodon)
- haloperidol (Haldol)
Psychotherapy approaches may include cognitive behavioral therapy.
It’s possible to have an initial schizophrenic episode and never experience another one. People who have experienced just one episode may find a coordinated specialty care program called Recovery After an Initial Schizophrenia Episode especially helpful. The program offers:
- psychotherapy
- medication management
- family education and support
- work or education support
People living with bipolar disorder or schizophrenia have an increased risk of suicide.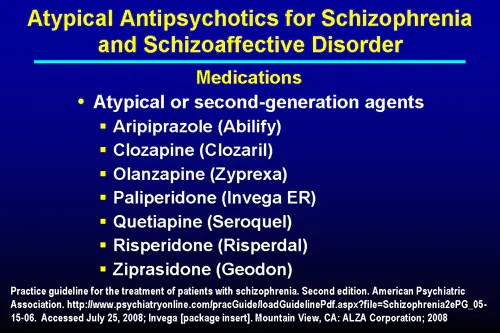 Anyone who has had suicidal thoughts should speak to a healthcare professional about treatment. It is extremely important to continue taking all medications as your doctor prescribes, even if you’re feeling better.
Anyone who has had suicidal thoughts should speak to a healthcare professional about treatment. It is extremely important to continue taking all medications as your doctor prescribes, even if you’re feeling better.
In addition, anyone living with bipolar disorder or schizophrenia may consider:
- joining a support group such as NAMI Connection
- Avoiding alcohol and substance use
- Following a relatively stable lifestyle.
- Getting an adequate amount of sleep.
- Maintaining a healthy diet.
- Using techniques to manage stress.
Bipolar disorder and schizophrenia can be confused, but they are different chronic mental health disorders. Some of the symptoms can overlap. However, bipolar disorder primarily causes extreme mood shifts, whereas schizophrenia causes delusions and hallucinations.
Both disorders can be serious and psychologically debilitating, though bipolar disorder is more common than schizophrenia. Both conditions may also be genetic, though it is thought that environmental factors may also be triggers.
Early diagnosis is critical. Be sure to speak with a healthcare professional if there is any concern about the emergence of bipolar disorder or schizophrenia. A well-thought-out treatment plan can go a long way toward managing these conditions and preventing future relapses. So will avoiding lifestyle and environmental factors that trigger episodes.
Can bipolar and schizophrenia occur together?
There is research indicating that similar genetic factors can predispose a person to develop either of the conditions. But you can be diagnosed with schizophrenia or bipolar disorder based only on criteria from the “Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5).”
This is because one diagnosis will usually exclude the other. But if a person exhibits symptoms of both conditions but does not fit either of these diagnoses, they could have schizoaffective disorder.
How can I help a person with schizophrenia or bipolar disorder?
It is difficult to watch a friend or a loved one with a mental health condition.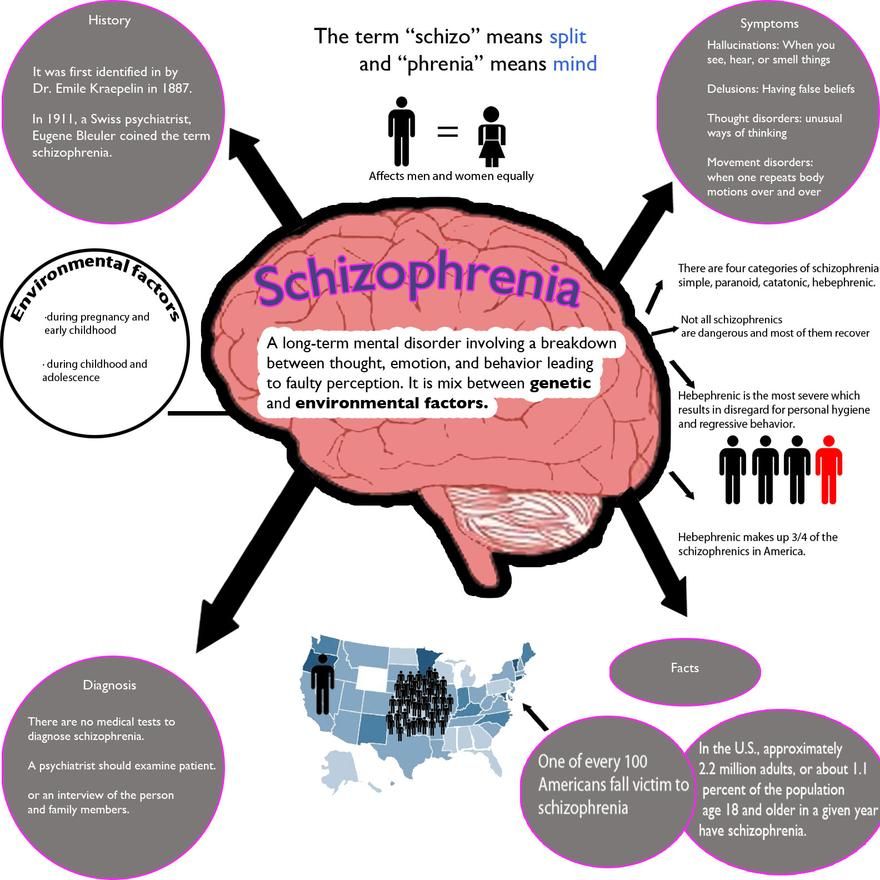 A good place to find advice on how to cope and how to help can be a support group. Consider joining the family support group of the National Alliance of Mental Illness (NAMI) or other support groups in your area.
A good place to find advice on how to cope and how to help can be a support group. Consider joining the family support group of the National Alliance of Mental Illness (NAMI) or other support groups in your area.
What should I do if I am diagnosed with schizophrenia or bipolar disorder?
You can manage the symptoms of bipolar disorder and schizophrenia with medication and therapy combined with a healthy lifestyle. Having a support system through support groups and family, friends, or co-workers can help you as you undergo treatment.
Schizophrenia and bipolar disorder: similarities and differences
There are a lot of mental disorders, syndromes and pathologies. At the same time, they have similar symptoms and signs in which the average person can get confused. Even an experienced doctor may need more than one month of observation of the patient in order to make an accurate diagnosis. In modern psychiatry, there are two main diseases - schizophrenia and bipolar disorder. Both are characterized by a state of psychosis, and sometimes hallucinations. But still, these are different pathologies that require two different approaches to treatment. Let's find out what is the difference between them.
Both are characterized by a state of psychosis, and sometimes hallucinations. But still, these are different pathologies that require two different approaches to treatment. Let's find out what is the difference between them.
In this article
- Bipolar disorder
- BAD manic
- BAD depressive phase
- Mixed States
- Main symptoms
- Main symptoms of schizophrenia
- Risk factors
- Main differences
- Treatment
- What is more dangerous
Bipolar disorder
Bipolar affective disorder (BAD), formerly known as manic-depressive psychosis, is an endogenous mental disorder with affective states - manic, depressive or mixed. It develops in phases that follow one another, as a result of which the patient's mood changes dramatically.
It should be understood that BAD is a fairly general concept for various disorders. Moreover, they usually develop in parallel with other disorders, such as anxiety.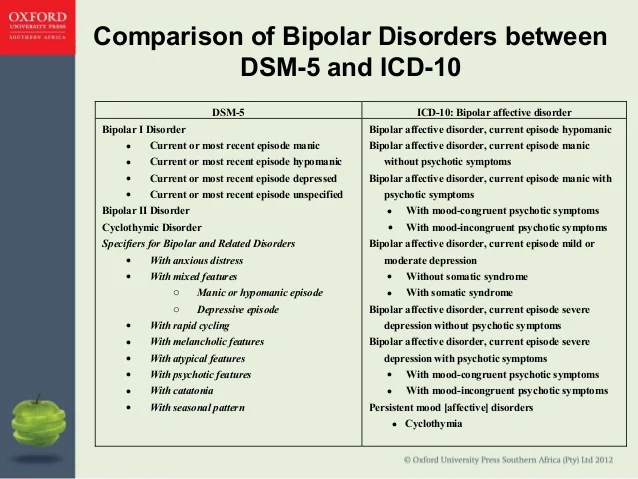 Its symptoms are so extensive that it requires careful diagnosis in each case. However, there are still general patterns. First of all, a phase flow is characteristic of a bipolar. There are two main stages of the disease:
Its symptoms are so extensive that it requires careful diagnosis in each case. However, there are still general patterns. First of all, a phase flow is characteristic of a bipolar. There are two main stages of the disease:
- manic;
- depressive.
Let's analyze each in more detail.
BAD manic
The initial phase is characterized by high spirits. The patient feels a surge of strength, both spiritual and physical. He talks a lot, and very quickly, but gradually the content of the speech becomes more and more meaningless. As a rule, one thought begins to replace another according to the principle of associations. There is hypermnesia, that is, an increased ability to remember details. A person begins to sleep less, but at the same time is quite active and eats a lot.
Further development of the phase leads to an increase in symptoms. The patient jokes and laughs a lot for no reason, but sometimes flares up and gets angry. Speech and motor overexcitation begins to be traced. At such moments, it is impossible to conduct a dialogue with a person, he jumps from one topic to another without discussing anything specific.
Speech and motor overexcitation begins to be traced. At such moments, it is impossible to conduct a dialogue with a person, he jumps from one topic to another without discussing anything specific.
People try to communicate less with such a person. He continues to be active, including at work, invests in new projects that everyone considers unpromising, makes bright plans and fantasizes a lot. Sleep duration is reduced to 3-4 hours a day.
Some episodes that occur to the patient during the manic phase are amnestic.
Then comes the stage of sharp motor excitation. The patient's actions are erratic, and speech becomes slurred. However, gradually the intensity of the symptoms decreases. First, motor excitation subsides while maintaining the speed of speech. But the latter also disappears over time. In a sense, the person returns to normal. Sometimes he is even more calm than he is in ordinary life.
Sometimes he is even more calm than he is in ordinary life.
BAD depressive phase
The depressive phase is the opposite of the manic phase and is characterized by a decrease in mood and activity. First, the general mental tone falls. Gradually, anxiety builds up. A person works less, because there is not enough physical and mental strength for a long activity. The patient's speech is slow, and the actions are inhibited.
Further progression of the disorder leads to the development of symptoms of severe depression. Anxiety, melancholy, loss of appetite, silence, delusional ideas are observed. A person does not answer questions or does it reluctantly and in monosyllables, eats little, engages in moral self-flagellation and self-abasement.
In this state, the patient often thinks about death and suicide. Moreover, suicidal attempts happen quite often, although they do not always lead to death. Illusions and hallucinations are rare, but some patients complain of voices ordering them to commit suicide.
The exit from the phase is accompanied by speech and motor activity. Gradually, the symptoms weaken and disappear. But it depends on the development of the depressive stage. It can be hypochondriacal, asthenic, delusional, etc. The name is due to the dominance of one or another feature.
Mixed states
In mixed states of bipolar disorder, manic and depressive symptoms are observed. They can occur both simultaneously and alternately with a difference of several hours. As a rule, this form of the disease occurs in young patients, especially in patients whose disorder manifested in adolescence.
This type of bipolar disorder is more difficult to diagnose due to the inconsistency of symptoms. A person can be both agitated and anxious-depressive at the same time. The course of the disease is also quite severe. 60% of these patients think about suicide. Moreover, about 50% of patients who committed suicide had precisely a mixed form of bipolar disorder.
Main symptoms
So, the main signs of bipolar disorder, which are observed in almost all cases, are the following symptoms:
- hyperactivity;
- fatigue;
- low concentration;
- irritability;
- impulsiveness;
- lethargy;
- sleep problems;
- suicidal ideation.
All this leads to problems in the family, relationships, at work or school. A person who previously studied well begins to get bad grades, and a responsible employee comes from work with a reprimand, etc. Such manifestations may be the reason for a visit to a psychologist or psychotherapist.
As for delusions and hallucinations, the hallmarks of most forms of schizophrenia, they are extremely rare in bipolar disorder. But the problem is that the presence of these symptoms does not always speak in favor of schizophrenic disorders. It is possible that BAD is still developing.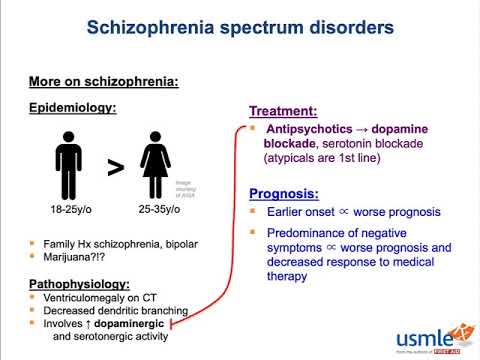
Main symptoms of schizophrenia
Schizophrenia is a complex and multifaceted disease with many symptoms. They are divided into two groups - positive and negative. The first testify to the activity of the psyche. This includes delusions and hallucinations. The latter are characterized by declines in mental tone. In this case, there are signs that are included in the symptoms of BAD:
- apathy and indifference;
- increased anxiety;
- outbursts of anger;
- motor or speech excitement;
- insomnia, nightmares;
- severe mood swings.
The intensity of symptoms is determined by the type and form of schizophrenia. So, a sluggish one can develop for years, practically without manifesting itself, and a paranoid one usually has an acute and rapid development.
Risk factors
BAD can be distinguished from schizophrenia through differential diagnosis and long-term observation of symptoms.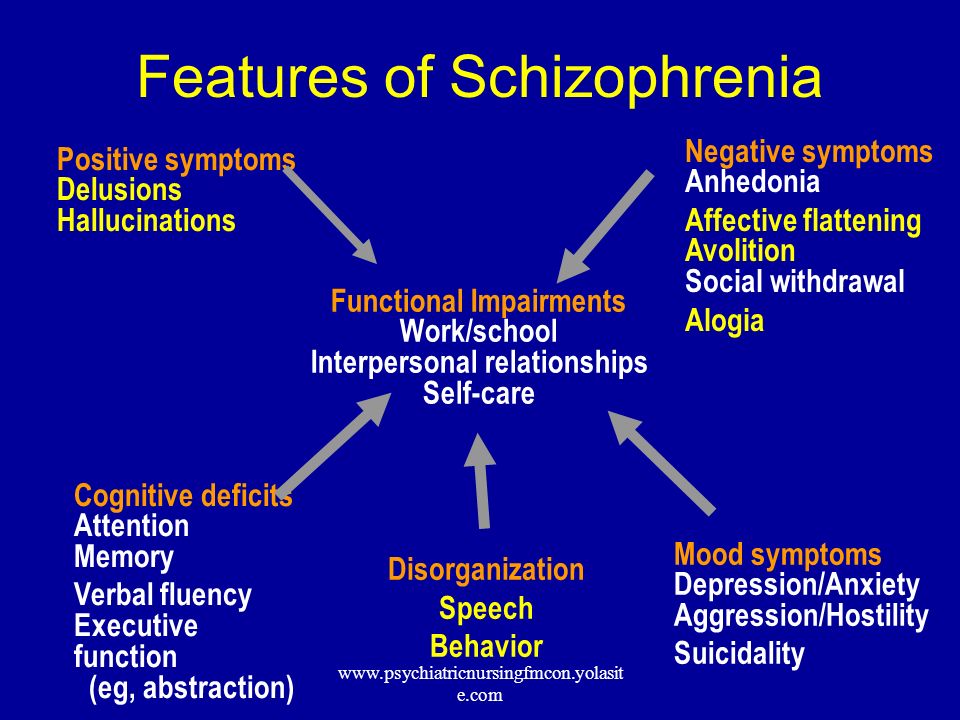 If we talk about the risk factors and causes of these psychopathologies, then they are largely similar. The fact is that the etiology of both disorders is unknown.
If we talk about the risk factors and causes of these psychopathologies, then they are largely similar. The fact is that the etiology of both disorders is unknown.
In most cases, we are talking about a genetic predisposition. First of all, doctors find out if there are people with mental disorders in the patient's family. The closer the degree of relationship, the higher the risk of the disease.
Main differences
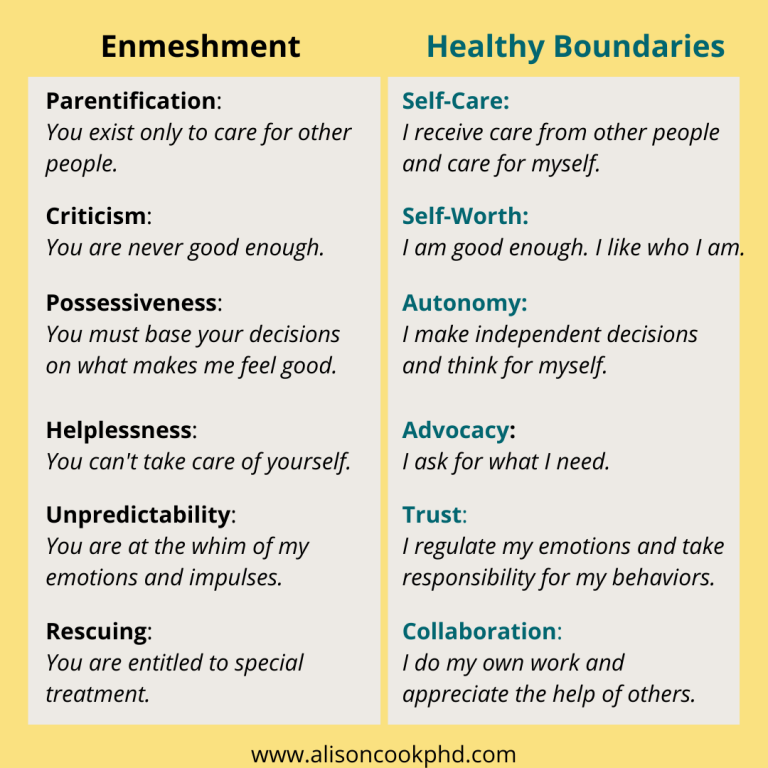
In bipolar disorder, psychosis leads to overexcitation of the nervous system. This also happens with schizophrenia. Also, a similar similarity is observed with negative symptoms. However, there are three main differences that allow differentiating diagnoses:
- In bipolar disorder, mania is accompanied by an extreme manifestation of feelings and emotions. However, in general, a person is adequate, and therefore rarely shows aggression. The schizophrenic is not always aware of his actions, therefore he is a danger to himself and others.
- With the development of bipolar disorder, the patient does not lose contacts and does not strive for complete loneliness even during a period of apathy. Withdrawal and alienation are the main symptoms of schizophrenia. They are especially noticeable in patients who are sociable in a healthy state.
- The main difference is in the consequences. Bipolar disorder does not damage the personality, while schizophrenia leaves its mark on the psyche. In a sense, after an attack, a person will never be the same as he was before. In bipolar disorder, even if the psychosis lasts for a long time, personality traits remain the same.
The similarity between bipolar disorder and schizophrenia is that both disorders are chronic. Treatment and prevention will take a lifetime.
Treatment
An accurate diagnosis of the patient can only be made after a few weeks or months after contacting the doctors. After that, the doctor will draw up a treatment card.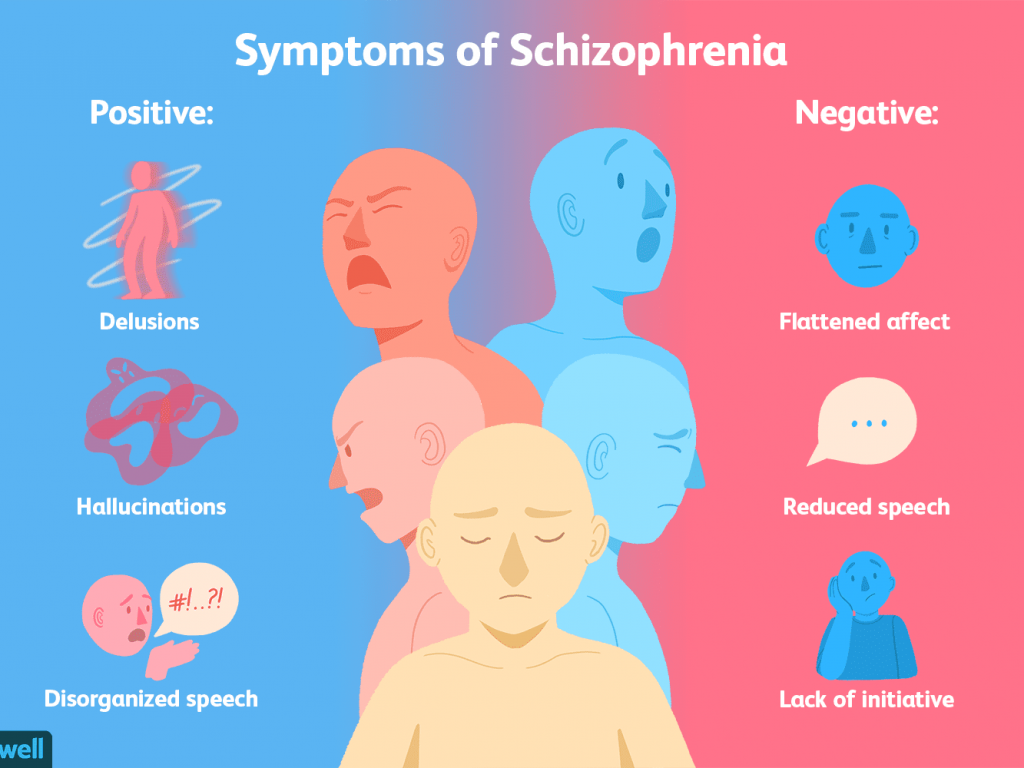
For bipolar disorder, it includes:
- psychotherapeutic sessions;
- mood stabilizers;
- antidepressants;
- sleeping pills.
Schizophrenia is treated much more difficult and longer. Sometimes it is necessary to use insulin-comatose therapy when the patient is artificially injected into a hypoglycemic coma. Antipsychotics and other antipsychotics are also prescribed. Psychotherapeutic methods include several areas - cognitive, behavioral, etc.
BAD cannot go into schizophrenia. These are two different diseases with different prognosis and outcomes.
BAD treatment can be done on an outpatient basis. Attacks in schizophrenia lead to hospitalization. The periods of remission in bipolar disorder are longer. However, serious consequences are possible in both cases.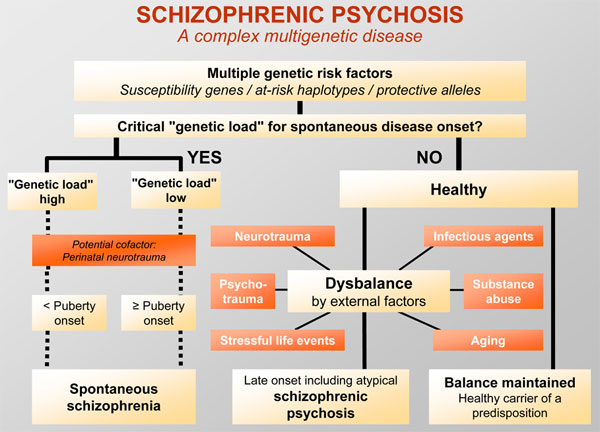 With complications, patients are assigned a disability. Sometimes they are considered insane. And this applies to patients with both bipolar disorder and schizophrenia.
With complications, patients are assigned a disability. Sometimes they are considered insane. And this applies to patients with both bipolar disorder and schizophrenia.
Which is more dangerous
Many people are interested in which is worse - BAD or schizophrenic psychopathology. The question is not very correct, however, in simple terms, bipolar disorder is not so dangerous. It does not lead to the disintegration of the personality. Schizophrenia can completely destroy it, as a result of which a person will forever remain in his inner world.
Sources:
- medalvian.ru
- allhealth.pro
- arbat25.ru
- psyandneuro.ru
Bipolar affective disorder and schizophrenia: what do they have in common?
In this section
Bipolar affective disorder (BAD) is a chronic, relapsing disorder in the category of mood disorders. BAD is characterized by recurrent (at least two) episodes in which mood and activity levels are significantly impaired. In some cases, there is mania or hypomania, in others - depression, not caused by a somatic disorder, the use of psychoactive substances (PSA), organic mental disorder. Symptoms of an acute episode are usually completely reduced during periods of remission 1 . Bipolar Disorder The condition was described as early as the fifth century BC 2 . However, to date, the underlying neuroscience is still largely unclear. There are suggestions about the multifactorial genesis of pathology with the participation of both biological-genetic and psychosocial factors. Significant progress has already been made in understanding the causes of bipolar disorder using modern molecular biology (eg, genetic and epigenetic studies) and imaging techniques (eg, positron emission tomography (PET) and functional magnetic resonance imaging (fMRI )2 . The hereditary burden of bipolar spectrum disorders is higher than in other mental disorders. Early onset and late diagnosis increase the risk of developing comorbid mental disorders and worsen the course of the disease 1 .
In some cases, there is mania or hypomania, in others - depression, not caused by a somatic disorder, the use of psychoactive substances (PSA), organic mental disorder. Symptoms of an acute episode are usually completely reduced during periods of remission 1 . Bipolar Disorder The condition was described as early as the fifth century BC 2 . However, to date, the underlying neuroscience is still largely unclear. There are suggestions about the multifactorial genesis of pathology with the participation of both biological-genetic and psychosocial factors. Significant progress has already been made in understanding the causes of bipolar disorder using modern molecular biology (eg, genetic and epigenetic studies) and imaging techniques (eg, positron emission tomography (PET) and functional magnetic resonance imaging (fMRI )2 . The hereditary burden of bipolar spectrum disorders is higher than in other mental disorders. Early onset and late diagnosis increase the risk of developing comorbid mental disorders and worsen the course of the disease 1 .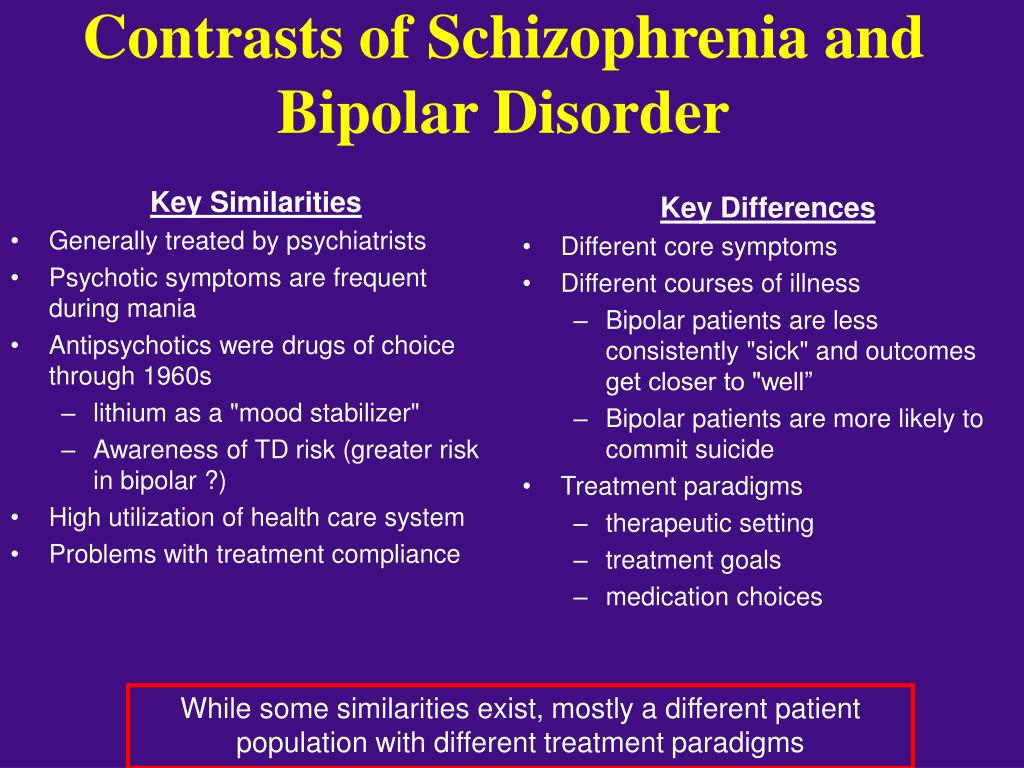
Epidemiology
The disease usually manifests at a young age or in late puberty (up to 20 years) 1 much earlier than the onset of recurrent depression 1 . The prevalence of bipolar disorder according to foreign data is from 0.5 to 2% (about 1% on average) 1 . The risk of development during life reaches 5%, and taking into account subsyndromal forms - up to 12% 1 . Significant geographic or ethnic differences in incidence rates have not been established.
The disorder is more common in women than in men, with a ratio of approximately 3:2 (2:1 in recurrent depression). BD is a disease with a high mortality rate, including associated with the risk of suicide - 20% of patients with BD 1 commit suicide. This is 20-30 times higher than in the general population and higher than in recurrent depression.
There is practically no information on the prevalence of BAD in Russia 1 .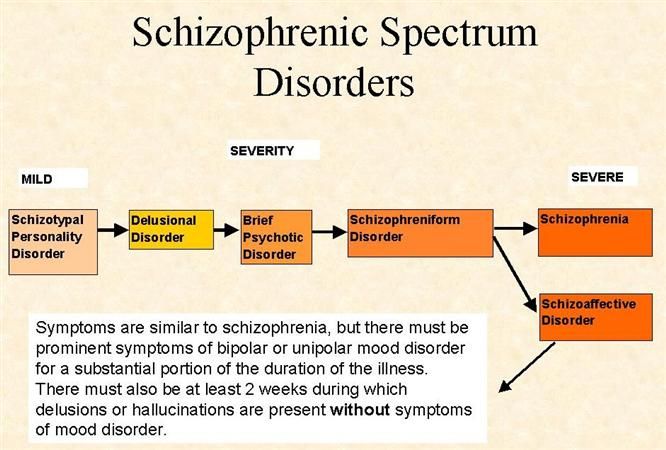
According to foreign data, 60-70% of patients with bipolar disorder are initially misdiagnosed, and in the future, the correct diagnosis is established only after, on average, 8-10 years after examination by three different doctors. In Russia, with a thorough diagnosis in accordance with the modern operational diagnostic criteria of the ICD-10 among patients diagnosed with recurrent depressive disorder (RDD), the proportion of patients with bipolar disorder is 40.8% 1 , and among patients diagnosed with "attack-like schizophrenia, or schizoaffective disorder" - 40.3% 1 .
Bipolar affective disorder and schizophrenia, what do they have in common?
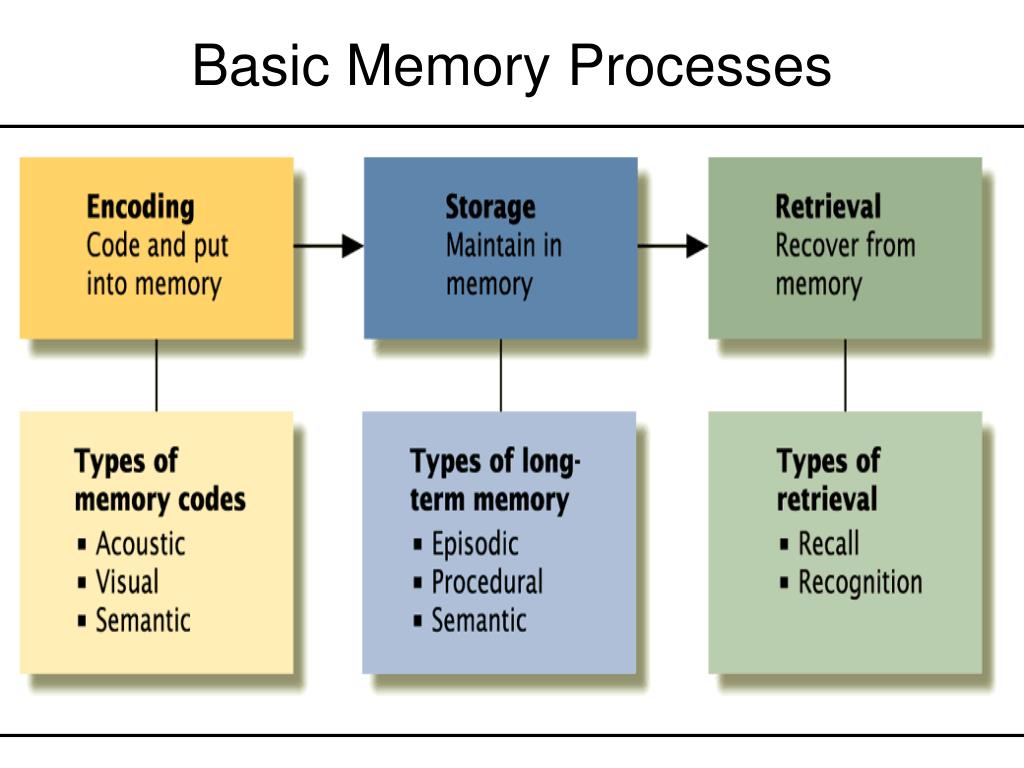
The study of neurocognitive impairment, its causes and consequences, and the development of new therapeutic strategies to manage or even prevent such impairment is currently one of the hottest areas of research in bipolar disorder (BD) (Martinez-Aran and Vieta, 2015).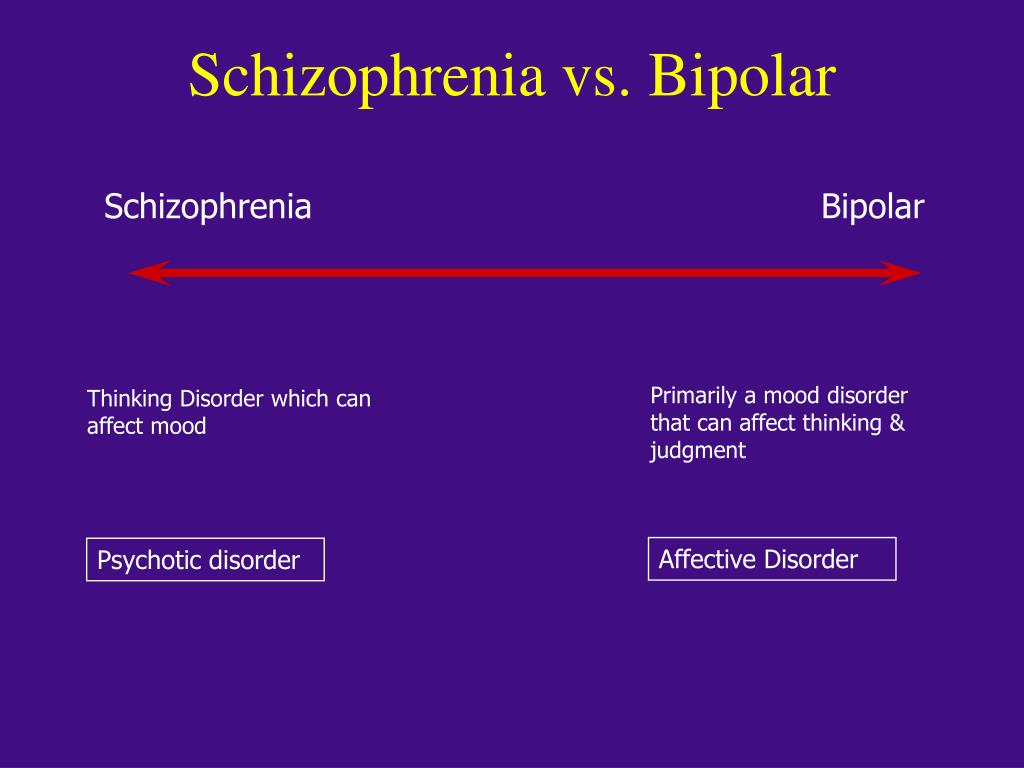 Data from various meta-analyses confirm that most patients with bipolar disorder have neurocognitive dysfunction even during euthymia (Robinson et al., 2006; Bourne et al., 2013; Bortolato et al., 2015). Some of these neurocognitive impairments seem to be present not only in the early stages of the disease (Torres et al., 2010; Lee et al., 2014; Bora and Pantelis, 2015), but also in the premorbid stages before the onset of the disease (Martino et al., 2015). According to the most recent meta-analyses, the most affected areas with moderate to high effect sizes are attention, verbal learning and memory, and executive functions, while premorbid intelligence appears to be preserved (Kurtz and Gerraty, 2009; Bourne et al., 2013) 3 .
Data from various meta-analyses confirm that most patients with bipolar disorder have neurocognitive dysfunction even during euthymia (Robinson et al., 2006; Bourne et al., 2013; Bortolato et al., 2015). Some of these neurocognitive impairments seem to be present not only in the early stages of the disease (Torres et al., 2010; Lee et al., 2014; Bora and Pantelis, 2015), but also in the premorbid stages before the onset of the disease (Martino et al., 2015). According to the most recent meta-analyses, the most affected areas with moderate to high effect sizes are attention, verbal learning and memory, and executive functions, while premorbid intelligence appears to be preserved (Kurtz and Gerraty, 2009; Bourne et al., 2013) 3 .
Because bipolar disorder is highly heritable, healthy first-degree relatives and children of patients with bipolar disorder may experience mild cognitive dysfunction (De la Serna et al., 2016). In this sense, some authors have suggested that neurocognitive deficit can be considered as a putative BD endophenotype (Arts et al.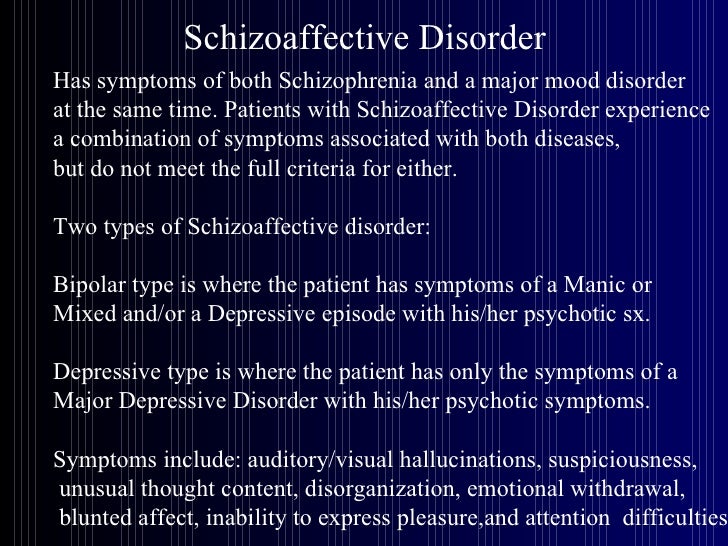 , 2008; Balanzá-Martínez et al., 2008; Bora et al., 2009) 3 .
, 2008; Balanzá-Martínez et al., 2008; Bora et al., 2009) 3 .
Available data indicate that the profile of neurocognitive impairment observed in patients with bipolar disorder is similar to that in patients with schizophrenia, although to a lesser extent; therefore, the differences between the two disorders seem to be predominantly quantitative rather than qualitative (Daban et al., 2006) 3 .
Overall, approximately 40% to 60% of patients with bipolar disorder have neurocognitive impairment, and there is great heterogeneity among these. In addition to the percentage of neurocognitive impairment in patients with bipolar disorder, similar data from several recent studies suggest that there are several neurocognitive subtypes among patients with bipolar disorder, which may also explain, at least in part, the existing variability in psychosocial functioning among patients. The use of cluster analysis approaches allowed different authors to detect different neurocognitive profiles in patients with both bipolar I disorder and bipolar II disorder: one with normal values (Burdick et al.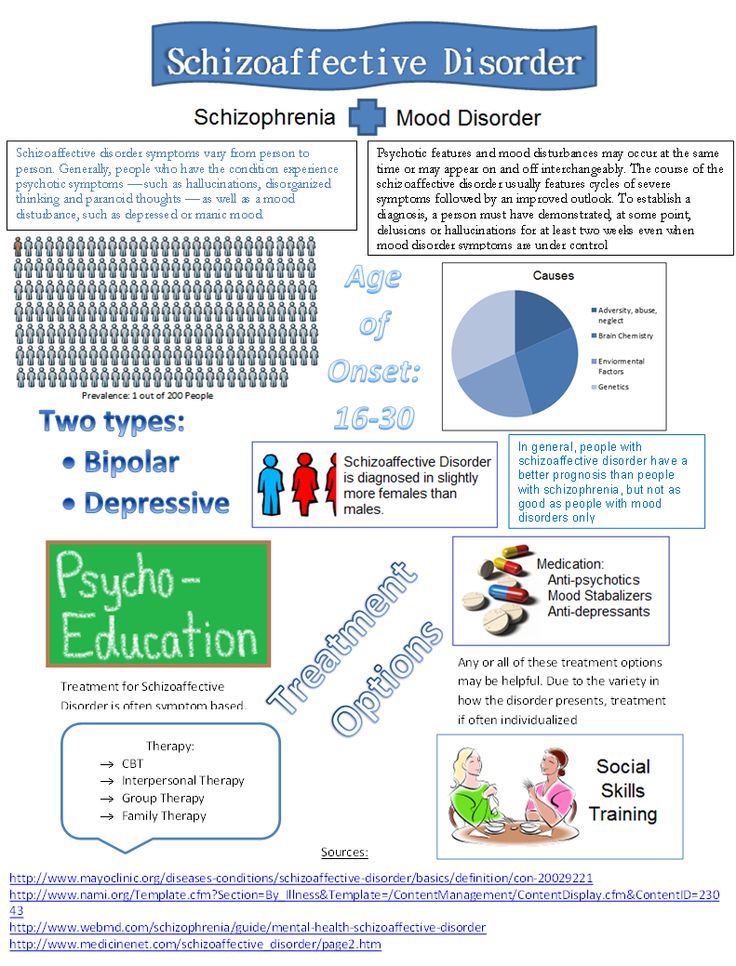 , 2014; Bora et al., 2016; Jensen et al. , 2016; Solé et al., 2016) 3 .
, 2014; Bora et al., 2016; Jensen et al. , 2016; Solé et al., 2016) 3 .
There is evidence that the use of antipsychotics in the treatment of bipolar disorder symptoms, including cognitive symptoms, has worked well 3 .
Sources:
- Clinical guidelines. Bipolar affective disorder. Ministry of Health of Russia. 2021.
- Freund N, Juckel G. Bipolar Disorder: Its Etiology and How to Model in Rodents. Methods Mol Biol. 2019;2011:61-77. doi: 10.1007/978-1-4939-9554-7_4. PMID: 31273693.
- Solé B, Jiménez E, Torrent C, Reinares M, Bonnin CDM, Torres I, Varo C, Grande I, Valls E, Salagre E, Sanchez-Moreno J, Martinez-Aran A, Carvalho AF, Vieta E. Cognitive Impairment in Bipolar Disorder: Treatment and Prevention Strategies. Int J Neuropsychopharmacol. 2017 Aug 1;20(8):670-680. doi: 10.1093/ijnp/pyx032. PMID: 28498954; PMCID: PMC5570032.
Login to Unlock
EPA 2021: Cognitive Recovery EPA 2021: Cognitive Recovery
(EPA) 2021 a scientific symposium was held on the different treatment options for
More…
Login to Unlock
Cognitive deficits and schizophreniaCognitive deficits and schizophrenia
Cognitive disorders are significantly associated with the hereditary risk of developing schizophrenia.