When does cymbalta start working
How Long Does It Take For Cymbalta To Work?
The world of mental health medications is a vast one. From SSRIs to stimulants and everything in-between, finding a drug that works well with your body and actually treats your condition can feel like a huge feat.
Cymbalta® is just one of these medications. And whether you’re considering taking Cymbalta or you’ve already started taking it, you’re probably wondering: when does this stuff start working?
Cymbalta can take six to eight weeks to start “working” fully, but it depends on a variety of factors.
In this piece, we’re going to cover what to expect when you start using Cymbalta® to treat your mental health, and how long you can expect it to take to work.
What Is Cymbalta?Cymbalta is a brand name for a drug known generically as duloxetine hydrochloride, or duloxetine for short.
Duloxetine is a serotonin and norepinephrine reuptake inhibitor (SNRI) that’s used to treat mental health conditions, generalized anxiety disorder and major depressive disorder.
It is also used to treat physical health conditions like diabetic peripheral neuropathy, fibromyalgia, chronic musculoskeletal pain, chemotherapy-induced peripheral neuropathy and urinary incontinence.
Today, we’re focusing on how duloxetine can be used to manage your mental health.
So, what exactly is a SNRI?
SNRIs are a class of drugs that are known as antidepressants, but can be used to treat a host of both mental and physical conditions.
They work by discouraging your brain’s reabsorption (or reuptake) of serotonin and norepinephrine, so that your body has a more readily available supply of these neurotransmitter-like hormones.
You can think of serotonin and norepinephrine as what you may have heard described as “happy hormones”,. Your brain uses these, along with others like dopamine, to regulate your mood, which is why SNRIs are effective for the treatment of depression and anxiety.
Duloxetine has the added benefit of increasing the production of dopamine in your brain. However, unlike its mechanism on serotonin and norepinephrine, it does not inhibit the reabsorption of this particular neurotransmitter hormone.
However, unlike its mechanism on serotonin and norepinephrine, it does not inhibit the reabsorption of this particular neurotransmitter hormone.
You can think of dopamine, serotonin and norepinephrine as messages that the nerve cells in your brain send to one another, allowing bits of information to pass between your nerve cells. The increased availability of them results in improvements in mood and anxiety.
What Is Cymbalta Used to Treat?In the world of mental health, Cymbalta is used for the treatment of generalized anxiety disorder, and major depressive disorder.
Generalized Anxiety DisorderAnxiety disorders are the most common type of mental disorder. According to the American Psychiatric Association, they affect nearly 30 percent of adults at some point in their lives.
Anxiety and fear themselves are normal parts of our emotional regulation, and are our natural reaction to stressors.
Anxiety is related to stress surrounding the future, while fear is related to stress in the immediate moment.
When anxiety or fear become out of proportion to a given situation, age inappropriate, or hinder a person’s ability to live a normal life, it can be an indication that the person is suffering from an anxiety disorder.
There are a variety of anxiety disorders, including generalized anxiety disorder, panic disorder and a variety of phobias, to name a few.
Cymbalta is effective in the treatment of generalized anxiety disorder, a condition in which a person experiences uncontrolled fear or anxiety more often than not for a period of six months or more, and exhibits at least three of the following symptoms,:
A sense of impending doom, panic or danger
Feelings of nervousness, irritability or being on the edge
Feeling weak, tired or having trouble sleeping or concentrating
Experiencing an increased heart rate, trembling, sweating or hyperventilation
Experiencing gastrointestinal issues, including weight loss
It is important to note that regardless of its severity, anxiety should be taken seriously. In cases of mild or moderate anxiety, some people find themselves able to go forward with their everyday lives.
In cases of mild or moderate anxiety, some people find themselves able to go forward with their everyday lives.
Individuals with severe anxiety may struggle to function and complete tasks like leaving the house.
The ability to keep functioning does not mean that anxiety is not valid. Over time, anxiety can have adverse effects on physical health, including complications like high blood pressure.
Options for treating anxiety include prescription medication, as well as therapy or online therapy with a mental healthcare provider.
These treatments can be effective for reducing feelings of anxiety and helping patients get back to living a more balanced life.
Major Depressive DisorderLike feelings of anxiety or fear, feelings of sadness every now and then are a normal part of our emotional regulation.
Major depressive disorder or clinical depression, however, is a medical condition that takes these feelings further to the point where they have a negative impact on quality of life.
It has the effect of putting the sufferer in a negative state of mind, eliciting feelings of extreme sadness, unhappiness and discontent, resulting in difficulties around going about daily life.
There exist a variety of depressive disorders, including psychotic depression, seasonal affective disorder and persistent depressive disorder.
In order to be diagnosed with depression, symptoms must persist for at least two weeks.
Symptoms of clinical depression include:
Feelings of anxiousness, sadness, hopelessness, emptiness, worthlessness, guilt, helplessness or pessimism
Difficulty with memory, making decisions or concentration
Thoughts of self harm or suicide
Decreased energy, loss of interest in activities that normally provide pleasure and increase in fatigue
Feelings or irritability or restlessness
Trouble with falling asleep or staying asleep
Changes in appetite or weight loss or gain
It is important to understand that depression can present differently in men than it does in women, with men being more likely to hide or ignore the emotional symptoms of depression.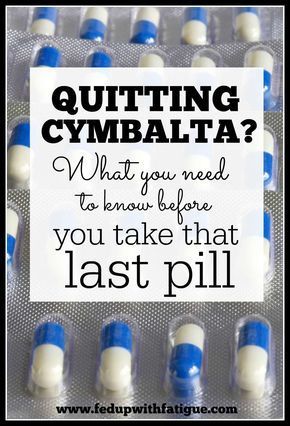 They’re more likely to seek treatment when the symptoms cross into the physical, like aches and pains, headaches, and digestive issues.
They’re more likely to seek treatment when the symptoms cross into the physical, like aches and pains, headaches, and digestive issues.
Similar to anxiety, options for treatment of major depressive disorder include medications like Cymbalta and therapy with your mental health provider.
It’s also worth noting specifically that in people with bipolar disorder, using Cymbalta to treat depressive episodes can put them at risk of switching from a depressive state into a manic episode, so make sure you speak to your healthcare provider specifically if you have a history of manic episodes.
online mental health assessment
your mental health journey starts here
How Long Does Cymbalta Take To Work?So, how long does it take for Cymbalta to work for depression or anxiety?
The answer is, it depends on your symptoms. Overall, it takes the drug several weeks of treatment to go into full effect.
However, for symptoms like lack of sleep, energy or appetite you may notice improvements within the first one to two weeks.
For other symptoms, like lack of interest in activities or depressed mood, you’ll need to wait closer to six to eight weeks to see full improvement.
You’ll also want to keep an eye out for common side effects of Cymbalta, and get in touch with your healthcare provider if you notice any of them.
Side effects that may occur but often go away within the first one to two weeks include:
Dry mouth
Decreased appetite
Feelings of nervousness, restlessness, fatigue or trouble sleeping
Nausea, headache and diarrhea
Other common side effects include increases in blood pressure, and sexual side effects like trouble reaching orgasm or ejaculating. These, unfortunately, do not often improve over time.
Rare and more serious possible side effects of Cymbalta include drops in blood pressure when moving from sitting to standing, serotonin syndrome, increased heart rate, glaucoma (a symptom of which can be eye pain) and others.
Cymbalta also comes with a Black Box Warning from the Food and Drug Administration (FDA), which means children, adolescents or young adults age 24 and younger are at increased risk for suicidal thoughts and behaviors.
If you start noticing this after taking Cymbalta, contact your healthcare provider immediately.
What to Do If You Don’t Notice ImprovementsFirst things first, do not, under any circumstances, stop taking your medication before getting medical advice from your mental healthcare provider.
It’s important that any change in your dosage of Cymbalta be guided by your provider to mitigate any potential negative effects from the change, especially if you’ve ever experienced suicidal ideations or are using Cymbalta to treat depression that is a function of bipolar disorder.
You’ll want to get in touch with your healthcare provider and talk about options available to you like shifting your dosage or shifting medications altogether.
psych meds online
psychiatrist-backed care, all from your couch
Final Thoughts on CymbaltaCymbalta is used to treat a host of medical conditions, from mental disorders to chronic musculoskeletal pain.
When using to treat anxiety or depression, remember that it can take several weeks to reach its full effect.
You’ll want to be in close contact with your healthcare provider as you begin treatment with this medication to ensure as smooth an experience as possible.
Hims' online psychiatry includes generic Cymbalta, duloxetine, as a treatment option to aid you in getting back to your best self.
12 Sources
Hims & Hers has strict sourcing guidelines to ensure our content is accurate and current. We rely on peer-reviewed studies, academic research institutions, and medical associations. We strive to use primary sources and refrain from using tertiary references.
- Dhaliwal JS, Spurling BC, Molla M. (2021, June 11). Duloxetine. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK549806/
- Duloxetine (cymbalta). (2016, January). National alliance on mental illness. Retrieved from https://www.nami.org/About-Mental-Illness/Treatments/Mental-Health-Medications/Types-of-Medication/Duloxetine-(Cymbalta)
- What is serotonin? (2018, December).
 Hormone Health Network. Retrieved from https://www.hormone.org/your-health-and-hormones/glands-and-hormones-a-to-z/hormones/serotonin
Hormone Health Network. Retrieved from https://www.hormone.org/your-health-and-hormones/glands-and-hormones-a-to-z/hormones/serotonin - Norepinephrine. (2019, September). Hormone Health Network. Retrieved from https://www.hormone.org/your-health-and-hormones/glands-and-hormones-a-to-z/hormones/norepinephrine
- FAQ: Antidepressants. MIT Medical. Retrieved from https://medical.mit.edu/faqs/antidepressants
- What are anxiety disorders? (2021, June). American Psychiatric Association. Retrieved from https://www.psychiatry.org/patients-families/anxiety-disorders/what-are-anxiety-disorders
- Generalized anxiety disorder (GAD). (2021, July 28). Anxiety and depression association of america. Retrieved from https://adaa.org/understanding-anxiety/generalized-anxiety-disorder-gad
- Symptoms. (2021, September 21). Anxiety and depression association of america. Retrieved from https://adaa.org/understanding-anxiety/generalized-anxiety-disorder-gad/symptoms
- Scientists discover link in brain between anxiety and weight loss.
 (2019, January 17). Scripps research. Retrieved from https://www.scripps.edu/news-and-events/press-room/2019/20190117-xu-baoji-anxiety-and-weight-loss.html
(2019, January 17). Scripps research. Retrieved from https://www.scripps.edu/news-and-events/press-room/2019/20190117-xu-baoji-anxiety-and-weight-loss.html - Anxiety and heart disease. Johns hopkins medicine. Retrieved from https://www.hopkinsmedicine.org/health/conditions-and-diseases/anxiety-and-heart-disease
- Depression. (2018, February). National Institute of Mental Health. Retrieved from https://www.nimh.nih.gov/health/topics/depression#part_2257
- Men and depression. (2017, January). National Institute of Mental Health. Retrieved from https://www.nimh.nih.gov/sites/default/files/documents/health/publications/men-and-depression/mendepression-508.pdf
This article is for informational purposes only and does not constitute medical advice. The information contained herein is not a substitute for and should never be relied upon for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment. Learn more about our editorial standards here.
Learn more about our editorial standards here.
How Long Does it Take to Work?
If you are one of the millions of Americans who is affected by common mental and physical health conditions like major depressive disorder, generalized anxiety disorder, fibromyalgia, and diabetic neuropathy, you may be surprised to know that one medication, Cymbalta, can offer relief for all of your symptoms.
Cymbalta is a prescription medication that can be safely used to treat a number of physical and mental health conditions, but how long does Cymbalta take to work?
What is Cymbalta?Cymbalta, also sold under the generic name duloxetine hydrochloride, is a prescription medication that belongs to a class of drugs called selective serotonin norepinephrine reuptake inhibitor antidepressants (SSNRIs).
SSNRIs most commonly treat mental health conditions like depression and anxiety.
The U.S. Food and Drug Administration (FDA) first approved Cymbalta in August 2004 for the treatment of depression, and it quickly became one of the most commonly prescribed antidepressants in the United States.
An estimated 16.5 million prescriptions were written for Cymbalta in 2017, making it the 46th most popularly prescribed drug in the United States.
What is Cymbalta Used to Treat?
Cymbalta is approved for the treatment of major depressive disorder and other physical and mental health conditions, including general anxiety disorder (GAD) in adults and children who are at least seven years old, diabetic neuropathy, and fibromyalgia.
A brief explanation of each of these conditions and their associated symptoms is provided below.
Clinical Depression/Major Depressive DisorderMajor depressive disorder, also known as clinical depression, is a mental health condition characterized by intense, persistent feelings of sadness that last for at least two weeks or more.
The condition impacts all areas of a person’s life, including sleeping patterns, appetite, mood, and behaviors. It is common for people with major depressive disorder to lose interest in hobbies or activities that they once enjoyed, experience difficulty performing daily tasks, and experience suicidal thoughts or behaviors.
The following symptoms are commonly associated with major depressive disorder:
- Difficult concentrating and low energy
- Mood swings
- Nervous energy
- Feelings of moving or thinking in slow motion
- Sleeping and eating more or less than usual
- Feeling sad, empty, or tearful
- Lost of interest in activities you used to enjoy
- Suicidal thoughts or behaviors
- Feelings of worthlessness, guilt, hopelessness, or helplessness
Generalized anxiety disorder, or GAD, is one of the most common forms of anxiety disorder and often has no obvious cause or reason.
Symptoms commonly associated with generalized anxiety disorder may culminate in a panic attack and can include an increased heart rate, trouble concentrating, rapid breathing, restlessness, and difficulty falling asleep.
A more acute form of anxiety, called an anxiety attack or panic attack, has symptoms that include dry mouth, feeling faint or dizzy, shortness of breath, sweating, chills or hot flashes, apprehension and worry, restlessness, distress, fear, numbness or tingling.
Fibromyalgia is characterized by unexplainable chronic musculoskeletal pain that occurs all over the body.
Symptoms of the condition include chronic musculoskeletal pain, mood issues, fatigue, tension headaches, temporomandibular joint (TMJ) disorders, sleep issues, memory issues, irritable bowel syndrome (IBS), depression, and anxiety.
The cause of fibromyalgia is unclear, but it may be linked to improper processing of pain signals by the brain, which causes painful sensations to be amplified.
The FDA also now lets you take Cymbalta for other types of chronic pain such as diabetic peripheral neuropathic pain, back pain, and more.
Diabetic neuropathyDiabetic peripheral neuropathy is a complication of diabetes that can occur when patients are unable to control their high blood sugar.
Chronically high blood sugar levels cause damage to the nerves in the body, particularly in the legs and feet.
Symptoms of diabetic neuropathy can range from problems with the blood vessels and heart to pain and numbness in the legs and feet, as well as digestive issues or urinary tract problems.
Starting Cymbalta should be discussed with a healthcare provider especially in the case of breastfeeding (as it can pass into breast milk), narrow angle glaucoma, psychiatric disorders such as bipolar disorder that involve manic episodes, a history of liver damage, liver problems, or liver injury, or have a history of high blood pressure.
Like most SSNRIs and antidepressants, Cymbalta does not work immediately.
It takes time for the drug to begin to affect the imbalance of chemicals within the brain.
It is possible to notice improvement in sleep, energy levels, and appetite within the first one to two weeks of taking the medication.
Improvement in depressed mood and increases in interest in activities may take longer to occur, sometimes up to six to eight weeks to fully improve.
Treatment Options for Depression, Anxiety, and Other Mental Health Ailment
| Plan | Product | Features | Treatment Today |
|---|---|---|---|
| 70% off your 1st Month | Psychiatry evaluation + medication | Hims |
$85/month - Includes everything | Start Treatment Today |
| 70% off your 1st Month | Psychiatry evaluation + medication | Hers |
$85/month - Includes everything | Start Treatment Today |
| $349/month - Most Effective Treatment Plan | Medication + Therapy | Brightside Health |
$349/month - Coupon available. | Start Treatment Today |
| $33/Week for 1st Month - Proven most effective | Medication + Therapy | Cerebral |
Starting at $33/Week for 1st Month | Start Treatment Today |
Cymbalta, the brand name medication, is also available in a generic form as duloxetine, which is substantially less expensive than Cymbalta.
Cymbalta is covered by some commercial insurance plans and may be covered by Medicare and Medicaid, but the generic version of the medication is covered by nearly all plans.
Regardless of your insured status, it is possible to find both the generic and brand name versions of the drug at a lower price by using a pharmacy discount card.
The following table compares the costs of a 30 day supply of Cymbalta and duloxetine.
Costs of a 30-Day Supply of Cymbalta and Duloxetine
Cymbalta
Duloxetine
20 mg oral capsules
$243.72
$46.18
30 mg oral capsules
$277.60
$18.22
60 mg oral capsules
$277.60
$22.94
How Do I Know What Dose of Cymbalta to Take?Your healthcare provider will determine the right dose of Cymbalta for each patient based on their age, the form of the medication they take, and the condition being treated.
SSNRIs like Cymbalta often need to be adjusted several times before the right dose is found, so expect your doctor to make changes to your medication as needed.
Adults with clinical depression generally take an initial dose of 40 mg per day, taken as one 20 mg release capsule twice per day.
Your doctor may choose to gradually increase your dose over time to a maintenance dose of 60 mg per day, taken either as one 30 mg capsule twice per day or one 60 mg capsule per day.
The maximum daily dosage for treatment of clinical depression should not exceed 120 mg per day, even if you are off schedule and need to miss your next dose.
Adults with generalized anxiety disorder typically take one 60 mg capsule of Cymbalta per day with a maximum dosage that should not exceed 120 mg per day.
Elderly patients are more likely to experience side effects when taking Cymbalta, so they are typically treated at an initial dose of 30 mg.
Children taking Cymbalta typically begin treatment at a dose of 30 mg per day before increasing to 60 mg per day, with a maximum of 120 mg per day.
Patients taking Cymbalta for treatment of fibromyalgia or diabetic peripheral neuropathy typically take a dose of 60 mg once per day.
Current studies do not support taking a dose higher than 60 mg per day for additional benefit.
When use of the medication is stopped abruptly or the dosage is suddenly changed, Cymbalta can cause withdrawal symptoms in the central nervous system and increased risk of suicidal thoughts, particularly in patients who have been taking the medication for more than six weeks.
It’s important that patients do not change their dose of Cymbalta or stop taking their prescription without consulting with their doctor. Due to the high incidence of serious side effect withdrawal symptoms associated with Cymbalta, the term “Cymbalta Withdrawal Syndrome” has been coined to refer to the collection of symptoms that may occur after stopping the medication.
Although Cymbalta Withdrawal Syndrome has a high likelihood of occurrence and can be experienced even when discontinuing the medication under the guidance of your doctor, withdrawing from Cymbalta under a doctor’s medical can help to minimize your symptoms and will help you to manage symptoms appropriately.
You should seek medical advice if you experience symptoms of Cymbalta withdrawal, which include:
- Irritability
- Drowsiness or fatigue
- Nausea
- Vomiting
- Vivid nightmares
- Increased sweating
- Insomnia (trouble sleeping)
- Dizziness
- Muscle spasms or tremors
- Headache
- Paresthesias
- Seizures
- Electrical shock sensations
- Feelings of anxiety
- Malaise
- Depressive symptoms
Possible side effects of Cymbalta generally fall into two categories: common and less common. Common side effects associated with Cymbalta include:
Common side effects associated with Cymbalta include:
- Muscle weakness
- Low blood pressure
- Weight loss
- Tiredness or sleepiness
- Skin rash
- Dark urine
- Eye pain
- Skin reactions
- Lightheadedness
- Tremor
- Dry mouth
- Weight gain
- Unusual changes in appetite
- Nausea
- Orthostatic hypotension
- Constipation
- Abdominal Pain or Stomach Pain
- Excessive sweating
- Vomiting
- Loss of appetite
- Bruising Easily
Less common adverse effects that may occur in long-term users of Cymbalta include:
- Sexual dysfunction
- Colitis
- Liver disease or damage in individuals who mix the medication with alcohol
- Frequent urination
Some potential drug interactions between the use of Cymbalta and the following over the counter and prescription drugs may exist: other SNRIs including venlafaxine, selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine, fluvoxamine, and paroxetine due to increased risk of serotonin syndrome, non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen, tricyclic antidepressants, antipsychotics including thioridazine, monoamine oxidase inhibitors (MAO inhibitors/MAOIs) including methylene blue, phenelzine, tranylcypromine, and isocarboxazid, antibiotics such as linezolid, tramadol, ciprofloxacin, triptans, tryptophan, amphetamines, blood thinners, flecainide, propafenone, quinidine, buspirone, and St. John's Wort.
John's Wort.
https://clincalc.com/DrugStats/Drugs/Cymbalta
https://www.webmd.com/drugs/2/drug-91490-2114/Cymbalta-oral/Cymbalta-sprinkle-capsule-oral/details
https://www.drugs.com/Cymbalta.html
https://medlineplus.gov/druginfo/meds/a604030.html
https://www.mayoclinic.org/drugs-supplements/Cymbalta-oral-route/description/drg-20067247
https://www.health.harvard.edu/a_to_z/major-depression-a-to-z
https://www.nami.org/About-Mental-Illness/Treatments/Mental-Health-Medications/Types-of-Medication/Duloxetine-(Cymbalta)
Duloxetine for the treatment of painful neuropathy, chronic pain or fibromyalgia
Review question
Does duloxetine work to treat pain generated by nerves when damaged by disease or pain caused by fibromyalgia?
Relevance
Duloxetine is a medicine used to treat depression and urinary incontinence (urinary leakage), and may also be useful for certain types of pain. Pain can occur spontaneously when there is damage to the nerves that carry pain information to the brain (neuropathic pain). When nerve damage occurs outside of the spinal cord, it is called peripheral neuropathy. Another type of pain, nociceptive pain, occurs when nerves sense damage to another tissue (such as a prick in the skin). Some types of pain of unknown origin occur without visible nerve or tissue damage. This type of pain occurs, for example, with fibromyalgia. The purpose of this review was to evaluate the benefits and harms of duloxetine for the treatment of neuropathic pain and chronic pain of all types.
Pain can occur spontaneously when there is damage to the nerves that carry pain information to the brain (neuropathic pain). When nerve damage occurs outside of the spinal cord, it is called peripheral neuropathy. Another type of pain, nociceptive pain, occurs when nerves sense damage to another tissue (such as a prick in the skin). Some types of pain of unknown origin occur without visible nerve or tissue damage. This type of pain occurs, for example, with fibromyalgia. The purpose of this review was to evaluate the benefits and harms of duloxetine for the treatment of neuropathic pain and chronic pain of all types.
Study profile
We reviewed all published scientific literature and found 18 trials with a total of 6407 participants that were of sufficient quality to include in this review. Eight clinical trials examined the effect of duloxetine in painful diabetic neuropathy and six in pain associated with fibromyalgia. Three trials looked at painful physical symptoms associated with depression, and one small study looked at duloxetine for stroke pain or spinal cord disease (central pain).
Main findings and quality of evidence
The usual dose of duloxetine is 60 mg. There was moderate-quality evidence that duloxetine at this dose reduced pain in painful diabetic peripheral neuropathy and fibromyalgia. In diabetic peripheral neuropathic pain, 50% or slightly more had an improvement on duloxetine 60 mg per day more than one and a half times more often than in the placebo group. In other words, five people with diabetic peripheral neuropathy must receive duloxetine in order for one of them to achieve an effect of 50% or more. The effect on fibromyalgia was similar, but the number of patients needed to be treated for improvement of 50% or more was eight. Based on only one study, it is not possible to determine whether the 20 mg dose is effective, and the 120 mg dose was no more effective than 60 mg.
We calculated that there were sufficient trials for diabetic neuropathy to draw these conclusions and no further trials are required. For fibromyalgia and the painful symptoms associated with depression, more trials are needed to make strong claims about the effectiveness of duloxetine.
For fibromyalgia and the painful symptoms associated with depression, more trials are needed to make strong claims about the effectiveness of duloxetine.
Most people who take duloxetine will have at least one side effect. They are mostly minor and the most common are feeling unwell, insomnia or drowsiness, headache, dry mouth, constipation or dizziness. About one in six people will stop taking duloxetine due to side effects. Serious problems associated with duloxetine are very rare.
Although duloxetine is useful in the treatment of neuropathic pain and fibromyalgia, there is little evidence from clinical trials comparing duloxetine with other antidepressants as to which is better.
We conclude that duloxetine can be used to treat pain associated with diabetic neuropathy and possibly fibromyalgia.
The information contained in this review is current up to November 2013, when the most recent literature search was made.
Translation notes:
Translation notes: Translation: Alexandrova Elvira Grigorievna. Editing: Gamirova Rimma Gabdulbarovna, Ziganshina Lilia Evgenievna. Russian translation project coordination: Kazan Federal University. For questions related to this transfer, please contact us at: [email protected]
Editing: Gamirova Rimma Gabdulbarovna, Ziganshina Lilia Evgenievna. Russian translation project coordination: Kazan Federal University. For questions related to this transfer, please contact us at: [email protected]
Depression
Russian Academy of Medical Sciences
SCIENTIFIC CENTER FOR MENTAL HEALTH
DEPRESSION (from hope to certainty).
(INFORMATION FOR PATIENTS AND THEIR FAMILIES)
MOSCOW
2008
Oleichik I.V. - Candidate of Medical Sciences, Leading Researcher of the Department for the Study of Endogenous Mental Disorders and Affective States
© 2008, Oleichik I.V.
© 2008, NTsPZ RAMS
The vast experience accumulated by mankind and reflected in many literary works convincingly shows that sadness (sadness, spleen) has always gone side by side with people, being one of the natural human emotions. None of us is immune from failures, illness, breakups, loss of loved ones, financial collapse. Each person can face something inevitable and inevitable, when it seems that life loses its meaning, and despair becomes boundless. However, normally, sadness, sadness and melancholy, as natural reactions to traumatic events, weaken over time and the person's condition returns to normal without special treatment. The situation is different with depressions, which are mental disorders that differ from natural physiological reactions in greater intensity, special severity of experiences and persistence of manifestations. True depression rarely goes away on its own, requiring persistent, sometimes long-term treatment.
None of us is immune from failures, illness, breakups, loss of loved ones, financial collapse. Each person can face something inevitable and inevitable, when it seems that life loses its meaning, and despair becomes boundless. However, normally, sadness, sadness and melancholy, as natural reactions to traumatic events, weaken over time and the person's condition returns to normal without special treatment. The situation is different with depressions, which are mental disorders that differ from natural physiological reactions in greater intensity, special severity of experiences and persistence of manifestations. True depression rarely goes away on its own, requiring persistent, sometimes long-term treatment.
A depressive state (from the Latin word depressio - suppression, oppression) is a disease that concerns not only an individual specific sick person, but is also a significant burden of modern society, since it is spreading more and more widely in the world, causing enormous damage to the health of the population and the state. economy. And this applies to all countries, regardless of their level of social development. Every year, at least 200 million people in the world fall ill with depression. Perhaps these figures are even higher, since most victims of depression do not seek help because they are not aware of the painfulness of their condition. Scientists have calculated that almost one in five people who have reached adulthood will experience at least one episode of depression during their lifetime.
economy. And this applies to all countries, regardless of their level of social development. Every year, at least 200 million people in the world fall ill with depression. Perhaps these figures are even higher, since most victims of depression do not seek help because they are not aware of the painfulness of their condition. Scientists have calculated that almost one in five people who have reached adulthood will experience at least one episode of depression during their lifetime.
In the most general sense, a depressive state is one of the possible forms of a person's response to the impact of stress factors. In some cases, depression can be triggered by external negative influences, for example, mental trauma, excessive educational or work overload, infection or other serious somatic disease, traumatic brain injury, changes in the hormonal background, which is especially important for the female body, regular certain medications, such as hormones, blood pressure medications, alcohol or other drug abuse. In other cases, depressive states develop as a manifestation of such mental illnesses, in which the main influence is heredity or characteristics of the nervous system (cyclothymia, dysthymia, manic-depressive psychosis, schizophrenia, etc.). If, based on the description of depressive symptoms set out later in our brochure, you realize that you have indeed developed a depressive state, do not fall into despair, do not “try to control yourself”, remember that depression is not a manifestation of weakness of will or character, on the contrary, weakening of volitional qualities is one of the main symptoms of depression. Depression is a disease like rheumatism, arthritis or hypertension, it responds well to treatment, resulting in almost always a full recovery. You should not blame yourself for the occurrence of depression, it does not indicate either your fault, or your weakness, or the possible development of a more severe mental pathology. Below we will tell you about the symptoms of depression, which can be extremely diverse.
In other cases, depressive states develop as a manifestation of such mental illnesses, in which the main influence is heredity or characteristics of the nervous system (cyclothymia, dysthymia, manic-depressive psychosis, schizophrenia, etc.). If, based on the description of depressive symptoms set out later in our brochure, you realize that you have indeed developed a depressive state, do not fall into despair, do not “try to control yourself”, remember that depression is not a manifestation of weakness of will or character, on the contrary, weakening of volitional qualities is one of the main symptoms of depression. Depression is a disease like rheumatism, arthritis or hypertension, it responds well to treatment, resulting in almost always a full recovery. You should not blame yourself for the occurrence of depression, it does not indicate either your fault, or your weakness, or the possible development of a more severe mental pathology. Below we will tell you about the symptoms of depression, which can be extremely diverse.
Manifestations of depression
Manifestations of depression can be very different. Depressive states can be manifested by a violation of almost all aspects of mental life: mood, memory, will, activity, which is expressed in the appearance of sadness, sadness, mental and muscle retardation, lasting at least 2 weeks. Depressed mood during depression can manifest itself as mild sadness, sadness, and boundless despair. Often it is accompanied by a feeling of melancholy, unbearable heaviness in the soul, with excruciating pain behind the sternum, a feeling of hopelessness, deep depression, hopelessness, helplessness, despair and uncertainty. At the same time, the patient is completely immersed in his gloomy experiences, and external events, even the most joyful ones, do not affect him, do not affect his mood, and sometimes even worsen the latter. A constant "companion" of a depressive mood is also anxiety of varying severity: from mild anxiety or tension to violent excitement, riot. Anxiety and bad mood arise at the mere thought of the need to make some kind of decision or change your plans due to suddenly changed circumstances. Anxiety can also manifest itself on the physical (bodily) level in the form of belching, intestinal cramps, loose stools, frequent urination, shortness of breath, palpitations, headaches, increased sweating, etc.
Anxiety and bad mood arise at the mere thought of the need to make some kind of decision or change your plans due to suddenly changed circumstances. Anxiety can also manifest itself on the physical (bodily) level in the form of belching, intestinal cramps, loose stools, frequent urination, shortness of breath, palpitations, headaches, increased sweating, etc.
The picture of depression is complemented by the disappearance of desires, interests, a pessimistic assessment of everything around, ideas of one's own low value and self-blame. Deficiency of vital impulses is manifested in patients with a variety of symptoms - from lethargy, physical weakness to a state of weakness, loss of energy and complete impotence. Where an important decision is required, a choice between different options, human activity is sharply hampered. Depressed people are well aware of this: they complain that insignificant everyday tasks, small issues that used to be solved almost automatically, take on the significance of complex, painful, insoluble problems. At the same time, a person feels that he began to think, act and speak slowly, notes the suppression of instincts (including food and sexual instincts), the suppression or loss of the instinct of self-preservation and the lack of the ability to enjoy life up to complete indifference to what used to be liked evoked positive emotions.
At the same time, a person feels that he began to think, act and speak slowly, notes the suppression of instincts (including food and sexual instincts), the suppression or loss of the instinct of self-preservation and the lack of the ability to enjoy life up to complete indifference to what used to be liked evoked positive emotions.
People suffering from depression often feel "stupid", "mentally retarded", "feeble-minded". Thinking in depression becomes viscous, painful, requires special efforts, one mental image is hardly forced out by the next. The sick person is oppressed by the feeling of his own intellectual insolvency, professional collapse. Depressed patients can hardly describe their painful experiences to the doctor. Only after getting out of depression, many of them say that the mood at that moment was lowered, thinking was slow, all undertakings (including treatment) seemed in vain, and the years lived were empty and useless. However, at the time of the first visit to the doctor, they could not explain this because of the almost complete absence of thoughts in their heads, “para-lich of thinking”. With depression, there are also often complaints of memory loss, which is why those suffering from it assume that they have "Alzheimer's disease", "schizophrenia", "senile dementia", which is not true. Especially often these complaints are found in depressions that develop in adolescence.
With depression, there are also often complaints of memory loss, which is why those suffering from it assume that they have "Alzheimer's disease", "schizophrenia", "senile dementia", which is not true. Especially often these complaints are found in depressions that develop in adolescence.
Typical story
Aleksey, 18 years old, 1st year student of a technical university, describes his condition during depression as follows:
“From childhood, I was fond of technology and modeling, I could read special literature for hours, won school and regional olympiads in mathematics and physics. After graduating from school, my dream came true - I brilliantly passed the exams to a prestigious university. Then it seemed to me that the whole world was at my feet, I flew with happiness "as if on wings." In September, I happily began to study. At the beginning, everything worked out well, but after 2 months I began to notice that it was becoming increasingly difficult for me to absorb what I read, I did not remember the simplest text, I could not solve problems that I used to “click like nuts”. Trying to achieve success through many hours of brainstorming or drinking a few cups of coffee led to the fact that I completely stopped thinking about anything. It seemed to me that I was "finally and irreversibly stupid." At night I sobbed, wrapped in a blanket and thought about how best to commit suicide. Luckily, I met a senior in the library and shared my problems with him. My new acquaintance said that he experienced something similar and advised me to contact the psychiatrist of the student clinic. After the examination, I was diagnosed with juvenile depression and sent for treatment to a specialized medical center. After 2 months, I felt completely healthy, returned to my studies and caught up with my classmates.
Trying to achieve success through many hours of brainstorming or drinking a few cups of coffee led to the fact that I completely stopped thinking about anything. It seemed to me that I was "finally and irreversibly stupid." At night I sobbed, wrapped in a blanket and thought about how best to commit suicide. Luckily, I met a senior in the library and shared my problems with him. My new acquaintance said that he experienced something similar and advised me to contact the psychiatrist of the student clinic. After the examination, I was diagnosed with juvenile depression and sent for treatment to a specialized medical center. After 2 months, I felt completely healthy, returned to my studies and caught up with my classmates.
Depression can also be accompanied by real setbacks: for example, a decrease in academic performance, the quality of work, family conflicts, sexual disorders and their consequences for personal relationships. As a rule, the significance of these failures is exaggerated and as a result there is a false sense of the irreparability of what happened, "the collapse of all hopes. "
"
Another generally recognized danger of depression is the possibility of suicidal thoughts, which often lead to suicide attempts. The condition of a person suffering from depression can suddenly deteriorate sharply, which happens either without clear external causes, or under the influence of traumatic situations, unpleasant news. It is during these hours, and sometimes even minutes, that a fatal decision is made. Factors that increase the risk of suicide in depression are past suicide attempts, the severity and duration of the depressive state, the presence of anxiety in its structure, prolonged insomnia, loneliness or alienation in the family, alcohol and drug abuse, loss of work and a sharp change in lifestyle, as well as relatives commit suicide.
Typical story
Eugene E., 35 years old, leading manager of the company.
Almost all my life, my career went “on the ascending”, the goals set were clear, clear and achievable. The marriage was extremely harmonious, two beloved children grew up. He devoted almost all the time to the affairs of the company, occasionally, once every 1-2 months, he escaped with his family out of town, to the country. He often lacked sleep, stayed late at work, took home assignments, and was deeply worried about the affairs of the company. Gradually, irritability, fatigue, insomnia, difficulty concentrating appeared, more and more often he suffered a “fiasco” in intimate life. Thoughts appeared that life was lived in vain, that it is a "chain of tragic mistakes" that led to a dead end. He began to believe that the choice of work, friends, family was wrong, for which now "retribution has come." Analyzing the past years for a long time, he found more and more evidence and examples of his "duplicity, hypocrisy, insincerity, etc." I realized that the only way to solve all problems is to voluntarily leave this life. At the same time, he believed that by this act he would free the family from the “burden”, “loser”, “loser”. I decided, having locked myself in the garage, to get poisoned by the exhaust gases of the car.
He devoted almost all the time to the affairs of the company, occasionally, once every 1-2 months, he escaped with his family out of town, to the country. He often lacked sleep, stayed late at work, took home assignments, and was deeply worried about the affairs of the company. Gradually, irritability, fatigue, insomnia, difficulty concentrating appeared, more and more often he suffered a “fiasco” in intimate life. Thoughts appeared that life was lived in vain, that it is a "chain of tragic mistakes" that led to a dead end. He began to believe that the choice of work, friends, family was wrong, for which now "retribution has come." Analyzing the past years for a long time, he found more and more evidence and examples of his "duplicity, hypocrisy, insincerity, etc." I realized that the only way to solve all problems is to voluntarily leave this life. At the same time, he believed that by this act he would free the family from the “burden”, “loser”, “loser”. I decided, having locked myself in the garage, to get poisoned by the exhaust gases of the car. However, by chance, in a semi-conscious state, he was discovered by an employee of a garage cooperative. He explained what happened as an "accident". The thought of leaving life did not leave the patient. I decided to shoot myself with a gas pistol, which I had long ago acquired for self-defense. After a shot in the mouth, in a serious condition, he was taken to the Research Institute. Sklifasovsky, from where he was discharged a week later. The alarmed wife, suspecting something was wrong, decided to consult her husband with a psychiatrist. He was admitted to the clinic. He agreed to this only out of respect for family relations, he himself believed that treatment by psychiatrists was completely useless, because. his situation is hopeless and no medicines will help here, but will only "stupefy" his psyche. However, after two weeks of taking a modern antidepressant, the patient's point of view changed. Everything began to look not so bleak and hopeless, interest in work and life in general returned, I began to feel more cheerful, more energetic, interest in intimate life appeared.
However, by chance, in a semi-conscious state, he was discovered by an employee of a garage cooperative. He explained what happened as an "accident". The thought of leaving life did not leave the patient. I decided to shoot myself with a gas pistol, which I had long ago acquired for self-defense. After a shot in the mouth, in a serious condition, he was taken to the Research Institute. Sklifasovsky, from where he was discharged a week later. The alarmed wife, suspecting something was wrong, decided to consult her husband with a psychiatrist. He was admitted to the clinic. He agreed to this only out of respect for family relations, he himself believed that treatment by psychiatrists was completely useless, because. his situation is hopeless and no medicines will help here, but will only "stupefy" his psyche. However, after two weeks of taking a modern antidepressant, the patient's point of view changed. Everything began to look not so bleak and hopeless, interest in work and life in general returned, I began to feel more cheerful, more energetic, interest in intimate life appeared. He took work to the clinic, called up colleagues. After two months of treatment, he fully returned to his usual life. With bewilderment, he recalled his thoughts about insolvency, the collapse of life, suicide. He took the drug prophylactically for about six months, then, on the recommendation of a doctor, he gradually reduced the dose and stopped taking it. Over the next two years, the condition remained stable, career growth continued, another child was born.
He took work to the clinic, called up colleagues. After two months of treatment, he fully returned to his usual life. With bewilderment, he recalled his thoughts about insolvency, the collapse of life, suicide. He took the drug prophylactically for about six months, then, on the recommendation of a doctor, he gradually reduced the dose and stopped taking it. Over the next two years, the condition remained stable, career growth continued, another child was born.
Depression is also characterized by sleep disturbances, which occur in approximately 80% of patients. As a rule, these are early awakenings with the inability to fall asleep, lack of a sense of sleep, difficulty falling asleep. These disorders, as well as restless sleep with unpleasant dreams, are often the very first symptoms of incipient depression.
If the depression is not deep, it is sometimes difficult to recognize it. This is due to the fact that people are ashamed to tell others about their problems, to admit to "weaknesses". Quite often, especially in Russia, depressive states are masked by alcohol abuse (“vodka heals”). In addition, often patients suffering from depression, in order to "shake themselves up", "throw into all serious", engage in casual sex, are fond of gambling or extreme sports, leave to serve on a contract in "hot spots", lead an idle lifestyle with constant attendance at entertainment events. Surrounding people, relatives who do not have psychiatric knowledge, often accuse them of debauchery, drunkenness, riotous lifestyle, parasitism. Meanwhile, this behavior is a kind of “cry for help”, an attempt to fill the spiritual emptiness brought by depression with new acquaintances and impressions.
Quite often, especially in Russia, depressive states are masked by alcohol abuse (“vodka heals”). In addition, often patients suffering from depression, in order to "shake themselves up", "throw into all serious", engage in casual sex, are fond of gambling or extreme sports, leave to serve on a contract in "hot spots", lead an idle lifestyle with constant attendance at entertainment events. Surrounding people, relatives who do not have psychiatric knowledge, often accuse them of debauchery, drunkenness, riotous lifestyle, parasitism. Meanwhile, this behavior is a kind of “cry for help”, an attempt to fill the spiritual emptiness brought by depression with new acquaintances and impressions.
Depressive conditions can occur in shallow forms that are easily treatable, but at least a third of depressions are more severe. Characteristics for such depressions are:
- ideas of guilt, sometimes reaching the degree of delirium, i.e. unshakable conviction in their sinfulness, low value (patients consider themselves great sinners, believe that because of them all relatives and Mankind will die, that they are “moral freaks” from birth, supposedly deprived of the foundations of morality and a sense of empathy for other people that they have no place on earth They find in their past numerous "confirmations" of what has been said above, they believe that the doctor and other patients are aware of these transgressions and express contempt and indignation with their facial expressions and gestures, but in the words “they hide, deny the obvious. ” Both the patients themselves and their relatives must remember this in order to prevent the impending threat in time: remove all firearms, piercing and cutting objects, ropes, potent drugs and poisonous close household fluids, close windows or shutters, do not let the patient go anywhere alone.If these ideas become persistent and cannot be dissuaded, it is urgent to seek advice from a psychiatrist. neurological institution or call a psychiatrist at home.
” Both the patients themselves and their relatives must remember this in order to prevent the impending threat in time: remove all firearms, piercing and cutting objects, ropes, potent drugs and poisonous close household fluids, close windows or shutters, do not let the patient go anywhere alone.If these ideas become persistent and cannot be dissuaded, it is urgent to seek advice from a psychiatrist. neurological institution or call a psychiatrist at home.
- mood swings during the day: in typical cases, the patient, waking up, immediately feels longing. Sometimes, even before full awakening, through a dream he experiences a painful premonition of a heavy coming morning. In the evening, the state of health improves somewhat.
- the patient may experience a feeling of unmotivated hostility towards relatives, friends, constant internal discontent and irritation, which makes him unbearable for the family.
- in a number of people suffering from depression, constant doubts, fear for the health and well-being of loved ones, obsessive ones, come to the fore. arising against the will, ideas about the misfortunes and troubles of family members.
arising against the will, ideas about the misfortunes and troubles of family members.
Typical story
Dmitry Petrovich, 58 years old, teacher.
“After minor troubles at work, I began to feel incomprehensible anxiety and agitation. Unpleasant thoughts came into my head that I did something wrong at work, because of which I double-checked everything many times and went home later than everyone else. But even at home, the anxiety did not let go: as soon as the daughter or wife lingered for at least half an hour, terrible pictures of traffic accidents or violence were drawn in the imagination. I fell asleep only in the morning, got up broken and felt sleepy all day. I took Valerian, Corvalol, but it practically did not help. At work, they hinted whether I should take a vacation. Friends advised me to consult a neuropathologist, but he did not find his pathology and sent me to a psychiatrist. I was diagnosed with anxiety depression. After a course of outpatient treatment, I completely recovered. ”
”
- in many cases, depression is characterized by unpleasant sensations in the body, disturbances in the activity of internal organs in the absence of objective signs of true somatic, i.e. non-mental illness. At the same time, many patients constantly report pain, internal discomfort. Some complain of headaches, pains in the stomach, joints, lower back, others - of disorders in the intestines: constipation, indigestion, irritation of the colon, others pay attention to a decrease in sexual desire and potency. In women, menstruation often becomes painful and irregular. Approximately 50% of depressed people at the doctor's office complain of such physical ailments, without mentioning the depressed mood or state of mind underlying the depression. Experiencing chronic pain or other unpleasant sensations in the body, patients may not realize that they are suffering from depression, even with severe melancholy, considering the latter a reaction to painful bodily discomfort.
- some patients are convinced that they have some rare and difficult to diagnose disease and insist on numerous examinations in general medical institutions. Doctors call this condition masked (hidden) depression, in which a person may experience pain in the head, in the limbs, behind the sternum, in the abdomen and in any other parts of the body, he may be haunted by anxious fears, he may suffer from insomnia or, on the contrary, too much sleep.
Doctors call this condition masked (hidden) depression, in which a person may experience pain in the head, in the limbs, behind the sternum, in the abdomen and in any other parts of the body, he may be haunted by anxious fears, he may suffer from insomnia or, on the contrary, too much sleep.
- Patients may experience disturbances in the cardiovascular system, skin itching or lack of appetite. All of these are manifestations of depression.
- the pathological sensations that patients experience during such depressions are quite real, painful, but they are the result of a special mental state, and not an internal disease. It must be remembered that the frequency of latent depressions exceeds the number of explicit ones many times over.
- with such depression, patients, as a rule, also have a changed attitude towards food: they can go without food for a long time and not feel hungry, and sitting down at the table, eat only 1-2 spoons - they have neither strength nor desire for more .
- a sign of depression can serve as a weight loss of more than 5 kg. within a month. In some people, especially women, the appetite for depression, on the contrary, increases, sometimes reaching the level of excruciating hunger, accompanied by severe weakness and pain in the epigastric region. In some cases, food is taken in excess due to an increased craving for sweets or attempts to distract oneself from painful thoughts by frequent eating.
Thus, we see that depression is a disease with many different manifestations that do not go away on their own, requiring special, sometimes long-term, medical intervention. Therefore, when the symptoms described above appear, it is necessary to seek help from a psychiatrist who will prescribe and monitor antidepressant treatment.
TREATMENT OF DEPRESSIVE DISORDERS
To date, it can be argued that the vast majority of cases of depression respond well to treatment. According to modern views, effective treatment of depression consists of a combination of pharmacotherapy, psychotherapy and, if necessary, other types of treatment. At the same time, the main role in therapy, of course, belongs to antidepressants - drugs specially designed for the treatment of various types of depression.
At the same time, the main role in therapy, of course, belongs to antidepressants - drugs specially designed for the treatment of various types of depression.
The creation of antidepressants is based on the discovery of scientists that depression develops as a result of a violation of the mechanism of biochemical transmission of nerve impulses in the brain regions responsible for mood, behavior, response to stress, sleep and wakefulness, appetite and some other functions. To ensure the coordination of the work of all these functional divisions, the brain sends special "commands" to them in the form of chemical impulses transmitted from the processes of one nerve cell (neuron) to the processes of another. This transmission is carried out with the help of chemical mediators (neurotransmitters), which, after transmitting a signal, partially return to the original neuron. This process is called neurotransmitter reuptake. Thanks to him, the number of mediators in the microscopic space between the processes of neurons (in the so-called synaptic cleft) decreases, which means that the necessary signals are transmitted worse. Numerous studies have shown that mediators of various structures, in particular, norepinephrine and serotonin, are involved in the transmission of signals that ensure the normal functioning of the nervous system. The first of them has a general activating effect, maintains the level of wakefulness of the body and takes part in the formation of adaptive reactions, and the second has the main antidepressant effect, controls impulsive actions, anxiety, aggressiveness, sexual behavior, falling asleep, feeling of pain, therefore serotonin is called sometimes a "good mood" regulator. A decrease in the number of mediators in the synaptic cleft causes symptoms of depression, while an increase, on the contrary, prevents their appearance. The ability of some drugs in one way or another to increase the concentration of mediators in the synaptic cleft allows them to be used as antidepressants.
Numerous studies have shown that mediators of various structures, in particular, norepinephrine and serotonin, are involved in the transmission of signals that ensure the normal functioning of the nervous system. The first of them has a general activating effect, maintains the level of wakefulness of the body and takes part in the formation of adaptive reactions, and the second has the main antidepressant effect, controls impulsive actions, anxiety, aggressiveness, sexual behavior, falling asleep, feeling of pain, therefore serotonin is called sometimes a "good mood" regulator. A decrease in the number of mediators in the synaptic cleft causes symptoms of depression, while an increase, on the contrary, prevents their appearance. The ability of some drugs in one way or another to increase the concentration of mediators in the synaptic cleft allows them to be used as antidepressants.
Now antidepressants are used in Russia, which can be conditionally divided into 4 generations according to the time of creation.
The first antidepressants to find wide clinical use were tricyclic drugs: amitriptyline and imipramine. They have a fairly powerful effect on most depressive states by blocking the reuptake of both norepinephrine and serotonin. However, the real clinical effect of these drugs is significantly offset by their undesirable side effects, which drastically reduce the quality of life of patients during treatment. Side effects of tricyclic antidepressants arise due to the nonspecificity of their effect on receptor structures. Acting in addition to the serotonin and norepinephrine system and other neurotransmitters (acetylcholine, histamine, dopamine), these antidepressants cause side effects such as urinary retention, dry mucous membranes, constipation, palpitations, fluctuations in blood pressure, confusion, tremor, sexual dysfunction. functions, weight gain. In such cases, it is necessary to prescribe other drugs to correct side effects or reduce the therapeutic dose of drugs, which naturally affects the effectiveness of the antidepressant action. It has been observed that up to 50% of patients refuse to take tricyclic antidepressants due to severe side effects. For the same reason, physicians are less likely to prescribe these drugs to patients on an outpatient basis.
It has been observed that up to 50% of patients refuse to take tricyclic antidepressants due to severe side effects. For the same reason, physicians are less likely to prescribe these drugs to patients on an outpatient basis.
The situation was somewhat improved by the introduction into practice of drugs of the second generation - tetracyclic antidepressants, which, along with the ability to block the reuptake of norepinephrine and serotonin, could also affect some other receptors. Being analogues of tricyclic compounds, these drugs have antidepressant activity comparable to them, but unlike their predecessors, they are safer, since they cause unwanted side effects much less often. In addition to the antidepressant, mianserin (lerivon) has a clear sedative, anti-anxiety and hypnotic effect. Maprotiline (Ludiamil) has a mild balanced antidepressant effect. In general, these drugs are able to cure mild to moderate depression, but are ineffective in patients with severe depression.
To date, antidepressants of the 3rd generation, such as fluoxetine (Prozac), fluvoxamine (Fevarin), paroxetine (Paxil), sertraline (Zoloft), citalopram (Cipralex) and some other drugs that selectively (selectively) affect the serotonin metabolism system, have received widespread recognition today.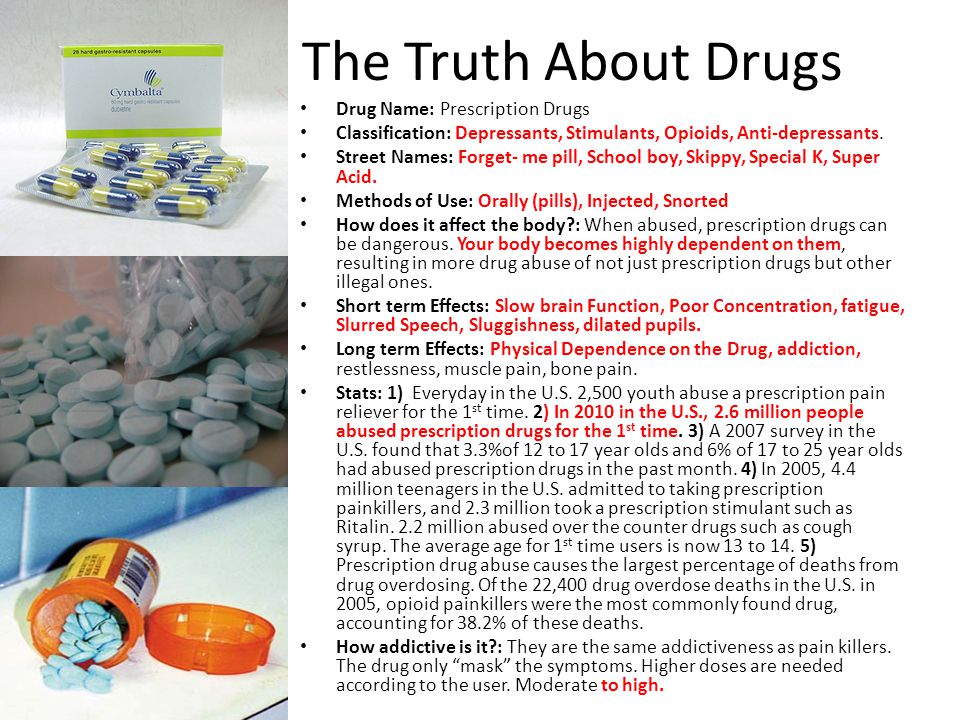 , preventing its reuptake in the synaptic cleft. Based on the mechanism of action, these antidepressants are combined into a group of selective serotonin reuptake inhibitors. In addition to treating depression, they are used to correct eating disorders, level panic disorders, so-called social phobias, various obsessive-compulsive disorders and chronic pain symptoms. These drugs have gained popularity due to the possibility of a once-daily intake, concomitant anti-anxiety effect, the presence of a psychostimulant component and a small number of side effects. In addition, they have low toxicity and are well tolerated by elderly patients. However, some researchers note their lack of effectiveness in the treatment of severe forms of depressive states, probably associated with selective activity in relation to only one neurotransmitter - serotonin. It should be noted that in recent years, some American scientists have associated the use of these drugs with an increased risk of suicide, which, however, is not proven.
, preventing its reuptake in the synaptic cleft. Based on the mechanism of action, these antidepressants are combined into a group of selective serotonin reuptake inhibitors. In addition to treating depression, they are used to correct eating disorders, level panic disorders, so-called social phobias, various obsessive-compulsive disorders and chronic pain symptoms. These drugs have gained popularity due to the possibility of a once-daily intake, concomitant anti-anxiety effect, the presence of a psychostimulant component and a small number of side effects. In addition, they have low toxicity and are well tolerated by elderly patients. However, some researchers note their lack of effectiveness in the treatment of severe forms of depressive states, probably associated with selective activity in relation to only one neurotransmitter - serotonin. It should be noted that in recent years, some American scientists have associated the use of these drugs with an increased risk of suicide, which, however, is not proven.
Considering the high frequency of side effects in some of the above drugs and the insufficient antidepressant activity in others, psychopharmacologists have taken the path of developing more effective antidepressants - IV generation drugs that selectively block the reuptake of both serotonin and noradrenaline, without affecting other mediators. system and with minor side effects. Currently, 3 drugs meet these requirements: milnacipran (Ixel), duloxetine (Cymbalta) and venlafaxine (Effexor). Their antidepressant activity in the treatment of patients with severe and moderate depression has been confirmed in a number of specially conducted studies, which at the same time showed that these drugs are well tolerated.
It should be noted that antidepressants of plant origin (negrustin, gelarium hypericum, deprim, etc.) can be effective in mild depressive states, but there are no reliable data guaranteeing their effectiveness. The opinion of a number of doctors that all depression can be treated with herbs or, say, acupuncture, should be recognized as unfounded.
For extremely severe depressions that do not improve despite the use of the most powerful antidepressants, electroconvulsive therapy (ECT) can be effective, but this situation is extremely rare and requires careful justification by the commission of doctors and the consent of the patient.
An important additional role in antidepressant therapy, especially with concomitant anxiety, is played by tranquilizers - anti-anxiety drugs, such as Xanax, phenazepam, diazepam, nitrazepam, atarax, etc. Drugs that can, when taken systematically, prevent mood swings in various depressive disorders include so-called mood stabilizers or mood stabilizers - lithium preparations, carbamazepine, valproic acid salts, lamotrigine, topiramate. With their systematic intake in most patients, the clinical manifestations of depression either completely disappear or become rare and mild, requiring no hospitalization and not significantly affecting the ability to work.
Antipsychotics play a significant role in the treatment of certain forms of depression. These include both traditional drugs - fluanxol, triftazin, eglonil, teralen, neuleptil, sonapax, and atypical antipsychotics that are gaining more and more recognition among doctors: seroquel, solian, zeldox, rispolept, abilify, serdolect and others.
These include both traditional drugs - fluanxol, triftazin, eglonil, teralen, neuleptil, sonapax, and atypical antipsychotics that are gaining more and more recognition among doctors: seroquel, solian, zeldox, rispolept, abilify, serdolect and others.
In drug therapy of depressive conditions, an unconventional, strictly individual approach is used, with the obligatory provision of fruitful cooperation between the patient and the doctor. Otherwise, there may be a violation of medical recommendations regarding doses and regimens for taking medications. The patient's faith in the possibility of recovery, the absence of prejudice against the "harm" caused by psychotropic drugs, the systematic observance of the prescriptions prescribed by the doctor largely contribute to the achievement of therapeutic success.
Drug treatment of depression takes time. You should not expect a complete cure already in the first days of taking the drug. It must be remembered that all modern antidepressants begin to act on depressive symptoms no earlier than 1-2 weeks after the start of treatment.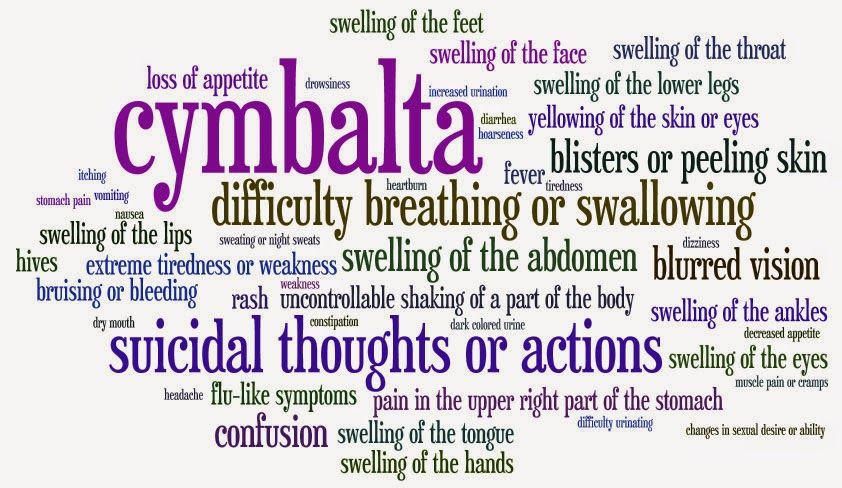 Cancellation of an antidepressant, as well as its appointment, should be carried out only by a doctor. Cancellation is usually made no earlier than 6 months from the normalization of the mental state. Even after the complete disappearance of all symptoms of depression, do not rush to stop taking the drug yourself, as there is a risk of an exacerbation of the disease. Therefore, doctors recommend continuing to take the antidepressant for a certain period of time. A common mistake is the premature withdrawal of drugs soon after a significant improvement in the condition or due to "forgetfulness". To avoid this, try to include the drug in the list of daily urgent matters - for example, store it in the bathroom and take it after hygiene procedures. When planning a trip, calculate exactly how many tablets you need for the entire period of absence from home. Breaking therapy is fraught with serious troubles.
Cancellation of an antidepressant, as well as its appointment, should be carried out only by a doctor. Cancellation is usually made no earlier than 6 months from the normalization of the mental state. Even after the complete disappearance of all symptoms of depression, do not rush to stop taking the drug yourself, as there is a risk of an exacerbation of the disease. Therefore, doctors recommend continuing to take the antidepressant for a certain period of time. A common mistake is the premature withdrawal of drugs soon after a significant improvement in the condition or due to "forgetfulness". To avoid this, try to include the drug in the list of daily urgent matters - for example, store it in the bathroom and take it after hygiene procedures. When planning a trip, calculate exactly how many tablets you need for the entire period of absence from home. Breaking therapy is fraught with serious troubles.
Conducted along with drug treatment, psychotherapy of patients with depressive states implies various systems of influence, including individual conversations, family and group therapy, etc.