Bipolar disorder support
Bipolar Disorder - Depression and Bipolar Support Alliance
Bipolar disorder is a treatable mental health condition marked by extreme changes in mood, thought, energy, and behavior. It is not a character flaw or a sign of personal weakness. Bipolar disorder was previously known as manic depression because a person’s mood can alternate between the “poles” of mania (highs) and depression (lows). These changes in mood, or “mood swings,” can last for hours, days, weeks or months.
For statistics about bipolar disorder, click here.
On this page:
- Bipolar Disorder Diagnosis
- Symptoms of Bipolar Disorder
- Mania Screeners
- Risk Factors
- Types of Bipolar Disorder
- Bipolar Disorder in Children
- Bipolar Disorder in Young Adults
- Bipolar Disorder in Older Adults
- Bipolar Disorder Treatment Options
Bipolar Disorder Diagnosis
When people experience symptoms of both mania and depression at the same time, they’re said to be experiencing a mixed state (or mixed mania). They have all of the negative feelings that come with depression, but they also feel agitated, restless and activated, or “wired.” Those individuals who have had a mixed state often describe it as the very worst part of bipolar disorder.
The screeners provided below are confidential assessment tools to explore your mental health and determine whether you should contact a mental health professional.
Resource
5 steps to take after a bipolar disorder diagnosis
Symptoms of Bipolar Disorder
Mania: The “Highs” of Bipolar Disorder
Symptoms of mania include
- heightened mood, exaggerated optimism and self-confidence;
- excessive irritability, aggressive behavior;
- decreased need for sleep without experiencing fatigue;
- grandiose thoughts, inflated sense of self-importance;
- racing speech, racing thoughts, flight of ideas;
- impulsiveness, poor judgment, easily distracted;
- reckless behavior; and
- in the most severe cases, delusions and hallucinations.
Depression: The “Lows” of Bipolar Disorder
Symptoms of depression include
- prolonged sadness or unexplained crying spells;
- significant changes in appetite and sleep patterns;
- irritability, anger, worry, agitation, anxiety;
- pessimism, indifference;
- loss of energy, persistent lethargy;
- feelings of guilt, worthlessness;
- inability to concentrate, indecisiveness;
- inability to take pleasure in former interests, social withdrawal;
- unexplained aches and pains; and
- recurring thoughts of death or suicide.
Bipolar Depression
People with bipolar disorder experience bipolar depression (the lows) more often than mania or hypomania (the highs). Bipolar depression is also more likely to be accompanied by suicidal thinking and behavior.
It’s during periods of bipolar depression that most people seek professional help and receive a diagnosis. In fact, most people with bipolar disorder in the outpatient setting are initially seen for—and diagnosed with—unipolar depression.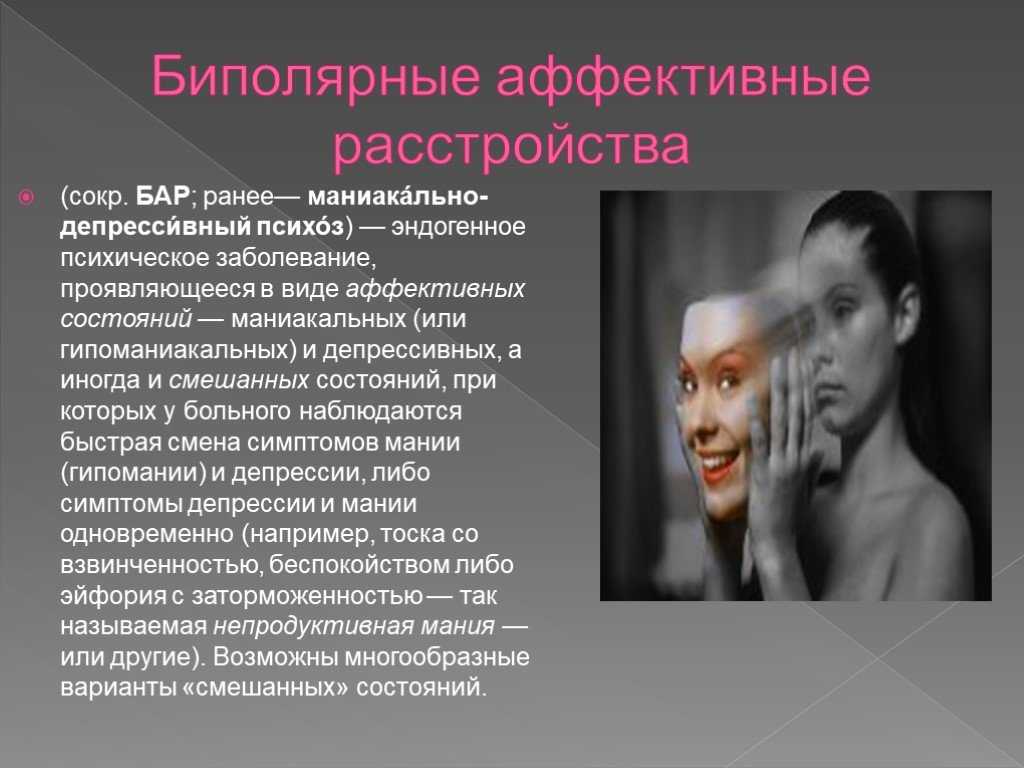 Unfortunately, incorrect treatment for bipolar disorder can actually lead to episodes of mania and other problems, so it’s important monitor your symptoms and follow up with your health care providers.
Unfortunately, incorrect treatment for bipolar disorder can actually lead to episodes of mania and other problems, so it’s important monitor your symptoms and follow up with your health care providers.
Mania Screeners
- Screening for Adult Mania
- Screening for Child/Youth Mania
- Screening for Child/Youth Mania (Parent Version)
Risk Factors
While there is no single cause of mood disorders, researchers have identified a number of risk factors that may contribute to an individual experiencing a mood disorder.
These risk factors include:
- Having a family member who lives with a mood disorder or other mental health condition
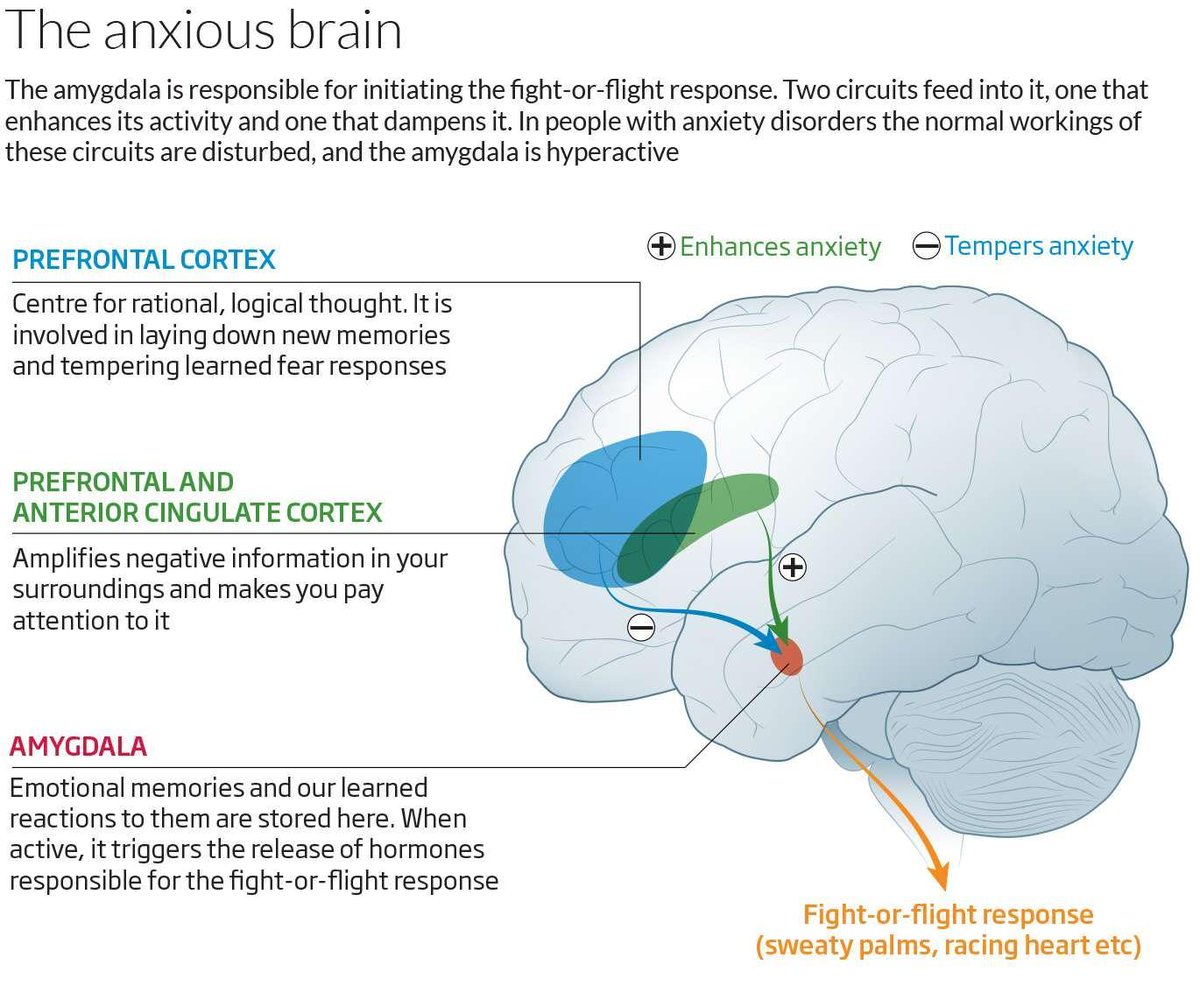
- Having specific genetics or brain structure
- Experiencing trauma or stressful life events
- Adverse Childhood Experiences (ACEs) such as poverty or abuse
- Excessive use of drugs or alcohol
Types of Bipolar Disorder
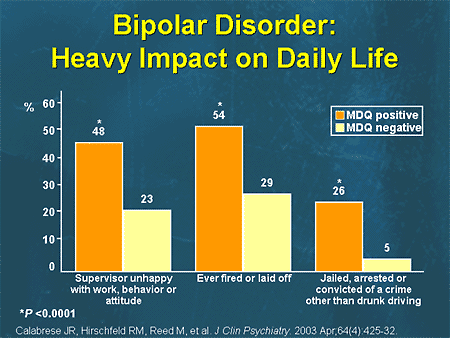
There are several types of bipolar disorder.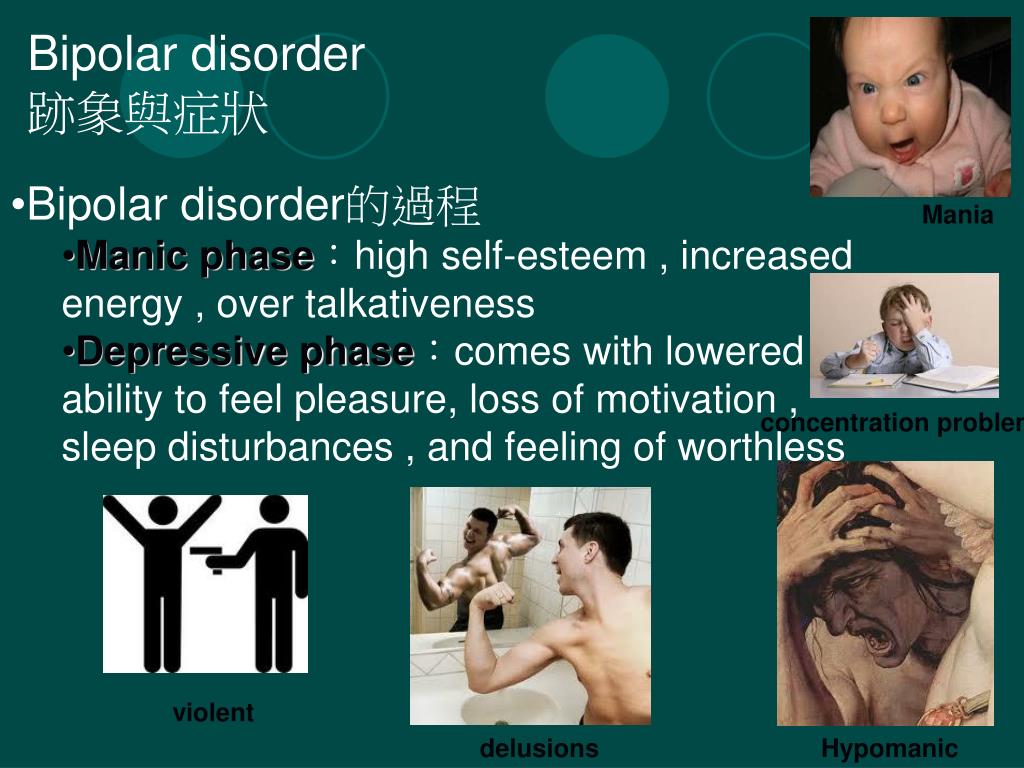 Each kind is defined by the length, frequency, and pattern of episodes of mania and depression. Mood swings that come with bipolar disorder are usually more severe than ordinary mood swings and symptoms can last weeks or months, severely disrupting a person’s life. For example, depression can make a person unable to get out of bed or go to work or mania can cause a person to go for days without sleep.
Each kind is defined by the length, frequency, and pattern of episodes of mania and depression. Mood swings that come with bipolar disorder are usually more severe than ordinary mood swings and symptoms can last weeks or months, severely disrupting a person’s life. For example, depression can make a person unable to get out of bed or go to work or mania can cause a person to go for days without sleep.
Bipolar I Disorder
Bipolar I is characterized by one or more episodes of mania or mixed episodes (which is when you experience symptoms of both mania and depression).
Bipolar II Disorder
Bipolar II disorder is diagnosed after one or more major depressive episodes and at least one episode of hypomania, with possible periods of level mood between episodes.
The highs in bipolar II, called hypomanias, are not as high as those in bipolar I (manias). Bipolar II disorder is sometimes misdiagnosed as major depression if episodes of hypomania go unrecognized or unreported. If you have recurring depressions that go away periodically and then return, ask yourself if you also have:
If you have recurring depressions that go away periodically and then return, ask yourself if you also have:
- Had periods (lasting four or more days) when your mood was especially energetic or irritable?
- Were you:
- Feeling abnormally self-confident or social?
- Needing less sleep or more energetic?
- Unusually talkative or hyper?
- Irritable or quick to anger?
- Thinking faster than usual?
- More easily distracted/having trouble concentrating?
- More goal-directed or productive at work, school or home?
- More involved in pleasurable activities, such as spending or sex?
- Did you feel or did others say that you were doing or saying things that were unusual, abnormal or not like your usual self?
If so, talk to your health care provider about these energetic episodes, and find out if they might be hypomania. Getting a correct diagnosis of bipolar II disorder can help you find treatment that may also help lift your depression.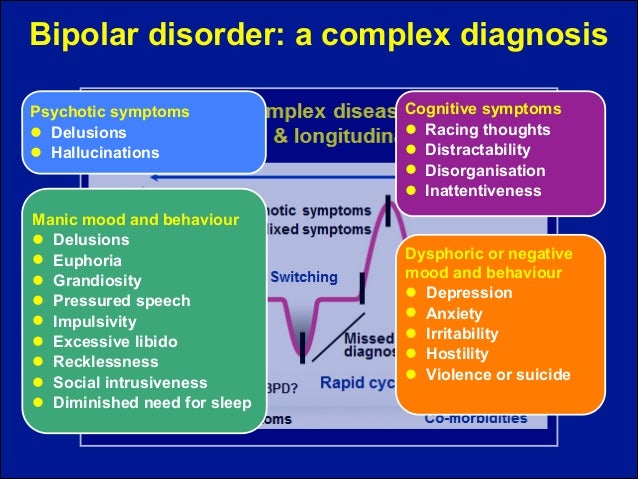
Other Specified Bipolar and Related Disorder (OSBARD)
Previously referred to as Bipolar Disorder-Not Otherwise Specified (BP-NOS), this diagnosis is used when individuals have clear manic and depressive symptoms that wax and wane but do not fit bipolar I, bipolar II, or cyclothymia.
Cyclothymia
Cyclothymia is a milder form of bipolar disorder characterized by several episodes of hypomania and less severe episodes of depression that alternate for at least two years. The severity of this illness may change over time.
Rapid Cycling
Bipolar disorder with rapid cycling is diagnosed when a person experiences four or more episodes of mania, hypomania, or depressive episodes in any 12-month period. Rapid cycling can occur with any type of bipolar disorder and may be a temporary condition for some people.
Learn More
Bipolar Disorder in Children and Adolescents
Mania in children often appears as extreme irritability or rage. Children and teens are more likely to have destructive outbursts than to be excited or euphoric.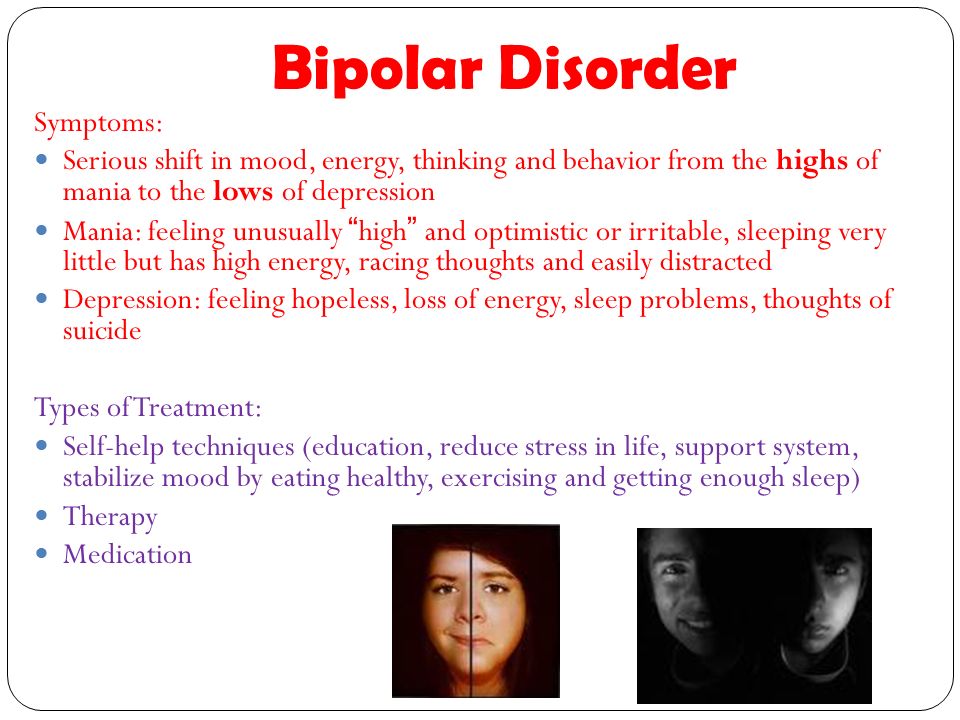 Depression in early life may have symptoms such as headaches, muscle aches, stomachaches or tiredness, frequent absences from school or poor performance in school, talk of or efforts to run away from home, irritability, complaining, unexplained crying, isolation, poor communication and extreme sensitivity to rejection or failure. Other signs of a possible mood disorder are alcohol or substance use and difficulty making or keeping friends.
Depression in early life may have symptoms such as headaches, muscle aches, stomachaches or tiredness, frequent absences from school or poor performance in school, talk of or efforts to run away from home, irritability, complaining, unexplained crying, isolation, poor communication and extreme sensitivity to rejection or failure. Other signs of a possible mood disorder are alcohol or substance use and difficulty making or keeping friends.
Young people may also have a continuous, rapid-cycling, irritable and mixed symptom state that may co-occur with disruptive behavior disorders, particularly attention deficit hyperactivity disorder (ADHD) or conduct disorder (CD). Young people may have symptoms of ADHD and CD before having bipolar symptoms.
A child or adolescent who has symptoms of depression along with ADHD-like symptoms that are very severe, with excessive temper outbursts and mood changes, should be evaluated by a psychiatrist or psychologist with experience in bipolar disorder, particularly if there is a family history of the condition. This evaluation is especially important since medications prescribed for ADHD may worsen symptoms of mania.
This evaluation is especially important since medications prescribed for ADHD may worsen symptoms of mania.
The Parent and Caregiver Network (PCN), a program of the Depression and Bipolar Support Alliance (DBSA), guides families raising children with mood disorders to the answers, support, and stability they seek.
Learn more about bipolar disorder in children Learn more about bipolar disorder in teens
Bipolar Disorder in Young Adults
The transition to adulthood is challenging. Young adults (18-29 years of age) typically experience many changes such as moving out on their own, finding their first job, and building relationships with significant others. For those living with a mood disorder, this time of life can be particularly difficult. DBSA has specialized resources to help support young adults through these challenges as well as help them connect to other young adults.
Learn More
Bipolar Disorder in Older Adults
It is uncommon for bipolar disorder to appear for the first time in late life, but some people may have symptoms throughout adulthood and not be diagnosed until later in life. For older adults, it is important to have a complete medical examination, and to discuss all mental health history, family history, and current medications with health care providers. Other illnesses and the medications that treat them may trigger or mimic bipolar disorder symptoms. Older adults may tolerate or metabolize medications at different speeds than younger adults, so they may need different dosages. Talk therapy, group therapy and peer support, including DBSA support groups, can be valuable additions to older adults’ treatment.
Older adults are also encouraged to start support groups for older adults that meet earlier in the day, are accessible to people with disabilities, are closer to people’s homes or meet other special needs.
Find a Local Support Group Find an Online Support Group Get Wellness Resources
Bipolar Disorder Treatment Options
As with any treatment or medical procedure, different people will have different responses. DBSA does not endorse or recommend the use of any specific treatment or medication. For advice about specific treatments or medications, consult your healthcare provider.
Learn More
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems.Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse.Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
People with bipolar disorder tell how to properly support them
March 30 is celebrated as Bipolar Day around the world. With this disease, it is important to monitor mood changes, which can be difficult to do alone. The founder of the Bipolar Association, Masha Pushkina, has collected stories of people who are helped by treatment partners.
At the initiative of public organizations bringing together scientists, doctors and activists, every year on March 30, World Bipolar Day is celebrated. The date chosen was the birthday of Vincent van Gogh, an artist who, according to researchers, was the embodiment of a "bipolar genius."
With bipolar disorder, a person lives either in a state of high emotional uplift and excitement (mania), or in depression. According to world statistics, about 2% of people suffer from bipolar disorder in various forms. This means that in Russia there are at least three million bipolar people - this is about half of St. Petersburg.
In most cases, this condition responds well to medication. But, unfortunately, many do not seek help or do not know how to find it. Without treatment, the disease progresses and ultimately leads to sad consequences: loss of family, job, disability in general, and in almost every seventh case, suicide.
These consequences can be avoided. The peculiarity of bipolar disorder is that the onset of remission depends not only on the doctor and medications, but also on the behavior of the patient himself. Very often, bipolar people provoke seizures "with their own hands." The mood of people with BAD (bipolar affective disorder. - Note ed. ) is very unstable, the balance is fragile, and mania or depression can be “started” in dozens of ways: the psyche is easily shaken by psychoactive substances, alcohol, lack of sleep, too intense work, travel and even love. So, a short time after the next course of treatment with powerful drugs, the person again ends up in the hospital. And each new attack reduces the chances of a long remission, affects social status, and even more painfully - self-esteem.
The experience of people with mental disorders around the world has proven that you are much more likely to cope with difficulties when you are supported by people who understand your problems and condition, but do not look at you as a patient. As practice shows, such a person can be not only a partner or close relative. An old friend, and even a person with whom you have never met in person, can help you get through the darkest times. Masha Pushkina, especially for Afisha Daily, spoke with several bipolar people about those in whom they found their support. The result is a story not about illness, but about friendship and trust, which can defeat even madness.
Yana, 31 years old
Housewife, collects books and is fond of confectionery
Purposefully, I didn't find out about the ways of support anywhere, everything turned out quite naturally. I have been sick for 15 years. The first person who looked after me was my best friend, and now it's my husband.
When my hypomania (a mild degree of mania, which is characterized by a constantly high mood. - Approx. ed. ) accelerated into a full-fledged mania (this state is also characterized by a one-sided attraction to some topic, sometimes accompanied by delirium. - Note ed. ), it became clear that I needed to be looked after. A friend began to pay attention to repetitive patterns of behavior in one phase or another, and we decided together to find out what helps in such cases. I think my friend was afraid to take responsibility for my condition, but she turned out to be generous and selfless. When I got married, a friend passed this knowledge on to her husband, and he already supplemented it, based on his own experience. The husband initially knew with whom he connects his life. He says it didn't scare him.
I have obsessions during my manic episodes. My husband does not argue with me at this time, but he does not feed them either, trying to redirect my stormy energy in a different direction. You can’t argue, because the result will be the opposite: I will finally get stuck on the idea, I will consider that I must prove it at all costs, even if the whole world is against me, and there are enemies and conspiracies around. If this does not help, the husband agrees to discuss all these things, but at the same time tries to slow down their implementation by offering to draw up a specific and detailed plan. Sometimes it takes me a long time.
For example, I always want to move somewhere. Right now, and why aren't we packing our things yet? My husband is trying to make me sit down to describe what are the pros and cons of different cities, what attracts us to them. As a result, I sit for hours on different forums, make lists, think about how we will arrange our life, calculate the budget for different countries of the world. There is also a manic passion for travel, but after preparation, we usually implement these plans. And many years ago, in a fit of mania, I bought an apartment - with a mortgage, with hellish payments. Then it took a long time to resolve this situation, but, fortunately, everything worked out well.
My husband began to chart my mood. I also manage it, and we check the results so that they are objective. Quarrels due to the fact that the husband takes on the role of the elder often arise in the manic phase (never in depression). Then I become very suspicious, any attempts at control cause rage. But now the husband has learned from experience, so he does not react to attempts to unleash a conflict. With obvious attacks of rage and auto-aggression, he uses holding therapy (long strong hugs. - Note ed. ). We have seen this in autistic children, this is how their parents influence them.
When I'm depressed, he doesn't comfort me because it's pointless, but he tries to give reasonable arguments that this period has always ended and this time will also pass soon. We look at mood charts for the past months, discuss the duration of the attacks: two weeks have already passed and, judging by past experience, it should get better in a couple of weeks.
Such support from the husband helps in many ways. When I was being treated by two doctors, taking all the medicines, I didn’t have such support, everything was very bad. Over time, I stopped disappearing from home in a manic state and inflicting serious injuries on myself. All my super-ideas remain on paper in the form of graphs and tables, I don’t even have time to start putting them into practice, so that later I don’t have to deal with the consequences with the whole family.
Alice, 27 years old
Biologist
To be honest, I don't always find understanding from my healthy environment, I often faced condemnation, devaluation of problems. But from a person who has a similar experience, you won’t hear “don’t invent”, “you can’t feel so bad”, “take a walk and it will pass”.
It just so happens that my best friend also suffers from bipolar disorder. I did not look for support in specialized communities where patients communicate, we met by chance. My friend is much older, he has much more life experience, and he was able to become a real mentor for me. Not once did his actions worsen my condition - I hope that he can say the same about me.
When I'm on the rise, I feel uncomfortable when he tries to slow me down and reduce my passions. But as soon as this state passes and I again take a sober look at the situation, each time I thank him for trying to stop the revelry and disgrace. My friend himself is currently not being treated, but he never imposed his position on me, and when I turn to doctors, he supports me in this.
I told the doctor about this source of support - he is all for it. Before meeting a friend, I had suicidal attempts, but during the entire time of our communication I never tried to say goodbye to life. When you know that there is a person who will understand everything and share warmth (while even my own family repels me), that there is a place where you can come in any condition and where they will accept me without unnecessary questions and teachings, this is a source of great strength. and hope.
When I was expecting my second child, I was depressed. My husband did not yet fully understand the features of the disease and did not want to admit obvious things - this added problems, and my emotional state became extremely difficult. It seems that only thanks to the participation of my friend, I did not do anything to myself and successfully endured the pregnancy. The child was named after him.
Sergey, 49 years old
Freelancer
At the height of the depression, I was looking for any available support and ended up in an online group of anonymous debtors (people who have taken on large loans). One of the participants drew attention to my condition and said that I urgently need medical help. Despite the fact that she lives in the USA, we began to communicate regularly via Skype. Olga literally brought me to the hospital and helped me prepare for the treatment.
Americans are a pragmatic people, many young and healthy people have folders with wills and instructions in case of their death. They also approach mental difficulties calmly and thoroughly. It is common practice for the patient to draw up detailed instructions in advance. In the United States, there is a practice of issuing Treatment Agreements for people with mental illness (Treatment Contract). This document is needed so that family, friends and doctors recognize the symptoms of deterioration in time and take into account your experience and wishes in the treatment. Typically, such a document contains: a list of trusted people; signs of a normal state; signs of an approaching episode; symptoms of mania and depression; actions that trusted people should take to help a person get better and keep him from destructive acts; plan of action in case of an emergency (for example, a suicide attempt). who and what will be done in the event of his hospitalization so that he can be treated without anxiety for household chores.
In a period of severe depression, there is a struggle inside a person between the craving for death and the desire to live - and many external things can outweigh in one direction or another. Every clue is important to help you get out. It is very difficult for one to cope with all this.
I madly didn’t want to go to the hospital and wouldn’t have made up my mind myself, until the last I hoped that somehow everything would go away on its own. But under the supervision of a friend, I drew up a preparation plan: warn the customer at work, arrange to look after my cats. Reported to her about every step. But then he could no longer simply “escape” [from hospitalization], because he felt obliged to both her and the doctor. During depression, one's own life has no value, but the people dear to me, the promises made to them, do.
At the most difficult moment, Olga became my “outer brain”, which told me what to do when I didn’t understand anything myself. After I was discharged from the hospital, I turned to four friends for support. Usually we call each other once a week, I tell what my condition is. It is important not only to chat online, but also to hear the voice, you can understand a lot from it. Friends immediately pay attention, if I suddenly disappear and stop calling, then something is wrong.
I think it is possible to find such a person if you set yourself such a goal. Take a closer look at people in support groups, religious or other communities - those who understand what compassion and mutual assistance are. This must be an internally mature person, ready to take responsibility for you in a difficult situation. If this person has similar problems, then he will better understand your experiences. For this reason, relatives are far from always suitable: they themselves can panic, seeing how bad you feel, choke you with their anxiety, overprotection.
It is necessary to establish the frequency of communication and observe it. And of course, in no case should you parasitize on someone else's kindness. The support system works when you yourself take responsibility for your life, and do not outweigh it completely on another.
Anna and Valeriya, 21 years old
Students
Anna: After a major depressive episode four years ago that almost ended in a suicide attempt, I started looking for information on [support]. I managed to find a guide in English for relatives and friends on how to behave with such a person. I have sent this list to all my friends so that they have an idea of what is happening to me. For the past few years, Lera has been monitoring my emotional state on a daily basis, and if, in her opinion, it goes beyond the norm, she tells me about it. Lera just asks every day how I'm doing, and if she sees that I'm reacting strangely, she wonders if something happened. At first, it was very difficult, because, in principle, I did not like to regularly share personal experiences. But by regularly receiving feedback, I can imagine the dynamics: do the pills help, how long do the side effects last, does the depressive phase go into a moderate and severe degree, do I lose my critical thinking during hypomania.
Valeria: We gradually established a very trusting relationship. Anya studied the topic of bipolar disorder up and down, and I read the articles that she sent me. The diagnosis did not change anything for me, because it remained the same. After that, we already discussed some formalities (for example, who to call in case of an emergency).
Anna: I asked Lera to watch for hypomanic manifestations in which I lose an adequate assessment of my actions: impulsive night walks, alcohol begin.
Valeria: My friend is a very responsible and conscious girl who takes care of herself, her health and her wallet. Before buying something expensive, she asks for my advice - and then we are already sorting out the situation. We can entrust accounts to each other and not worry. I also know where and to whom to run in cases of exacerbation.
Anna: I react badly to prohibitions and reminders of illness. Yes, I periodically have to turn to relatives for help, change treatment or take long breaks, but I expect mutual respect so that they don’t look at me through the prism of the disease.
When the mood is unstable, harsh phrases like “the disease speaks in you”, “these are not your real emotions” cause persistent rejection, even when they are true. The line between accepting a loved one's illness and identifying him with a diagnosis for healthy people is extremely thin. Therefore, those who were able to grope it deserve great respect.
Anna: In the last year, I go to see the doctor with my parents. When the doctor notices that I may not be able to do it alone, she duplicates the instructions and advice for them. I, in turn, am a friend. The doctor has repeatedly emphasized that the change of episodes is more noticeable from the outside.
Valeria: We don't have any kind of hierarchy in relationships, so there is no pressure when one makes decisions for another. This is not eating each other's emotional resources, but complementing and supporting.
Anna: The main danger in a relationship with a person with a serious illness is to fall into codependency. This format is equally bad for both the "controller" and the "subordinate". Unfortunately, I have been in such relationships before. It is worth maintaining mutual respect and treating each other as equals. Illness should not dominate a relationship. In difficult episodes, it temporarily comes to the fore, but you should always remember that you are not a disease.
Anna: I have memory problems: I don't remember some episodes. In such cases, I can ask Lera for help. If you remember the last weeks, then these are regular reminders to call the doctor. In mixed episodes, this becomes an acute problem, because I can suddenly change my mind or forget. Against the backdrop of a severe episode, I may develop psychosis, and this is the most dangerous thing in the disease. Thanks to our format, I manage to avoid such exacerbations almost always.
The advantages of observation from a loved one are an early response and the fact that he knows the patient's usual behavior very well and can notice even small changes. The main disadvantage is that normal friendly communication risks turning into constant monitoring of symptoms. Not every mentally healthy person is able to remain within the boundaries of reason.
It is important to agree in advance, before an attack, what is an undoubted sign of a worsening condition (for example, persistent insomnia), and what you do not need to pay special attention to (for example, loud indignation at something that you do not like). In a difficult situation, often a loved one begins to behave not as an equal, but as a “healthy” and “knowledgeable”. Not all relationships stand this test.
There is also a variant of "buddy" (when two people with mental disorders look after each other. - Note ed. ) - it is good precisely because it is the true request of the patient and more equal relations without mixing roles. But I don't know the buddy support system.
To choose a person you can rely on in a critical situation, take a closer look at your surroundings. Above all, a high level of trust is needed. Your assistant should be open to nonjudgmental and open dialogue and at the same time emotionally stable and resistant to stress.
Support is essential for every person - very often we as mental health professionals need it. And with bipolar disorder, this problem is especially acute. At the initial stages, those closest to you often ignore the presence of the disease, and friends advise you to either "pull yourself together" or, conversely, "relax", sometimes with the help of alcohol. When it becomes obvious to everyone that the “condition” will not go away on its own, urgent hospitalization is already required. The saved patient receives the "stigma".
Psychiatrists then make it the responsibility of the uninitiated next of kin (parent or spouse) to monitor any changes in the patient, and they really try to do so. At the level of "laughing out loud - hypomania has begun, upset - depression." As a result, psychiatrists begin to treat quite normal human emotions based on complaints from relatives... and the circle closes.
For this to change, mental health literacy must play a major role. Relatives, in order to be able to help, need to understand well what is happening with a loved one. In many, including state clinics, groups for training relatives either already exist or are being created.
The support of loved ones in case of emergency is especially important. In deep depression or mania, a person is not able to independently control his behavior, this decision is made by relatives, sometimes without his consent. In the case of bipolar disorder, this should be the last option when all others have been exhausted.
Bipolar disorder | Symptoms, complications, diagnosis and treatment
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). Episodes of mood swings may occur infrequently or several times a year.
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When the mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, alertness, judgment, behavior, and the ability to think clearly.
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medication and psychological counseling (psychotherapy).
Symptoms
There are several types of bipolar and related disorders. These may include mania, hypomania, and depression. Symptoms can lead to unpredictable changes in mood and behavior, leading to significant stress and difficulty in life.
- Bipolar disorder I. You have had at least one manic episode, which may be preceded or accompanied by hypomanic or major depressive episodes. In some cases, mania can cause a break with reality (psychosis).
- Bipolar disorder II. You have had at least one major depressive episode and at least one hypomanic episode, but never had a manic episode.
- Cyclothymic disorder. You have had at least two years - or one year in children and adolescents - many periods of hypomanic symptoms and periods of depressive symptoms (though less severe than major depression).
- Other types. These include, for example, bipolar and related disorders caused by certain drugs or alcohol or due to health conditions such as Cushing's disease, multiple sclerosis or stroke.
Bipolar II is not a milder form of Bipolar I but is a separate diagnosis. Although bipolar I manic episodes can be severe and dangerous, people with bipolar II can be depressed for longer periods of time, which can cause significant impairment.
Although bipolar disorder can occur at any age, it is usually diagnosed in adolescence or early twenties. Symptoms can vary from person to person, and symptoms can change over time.
Mania and hypomania
Mania and hypomania are two different types of episodes, but they share the same symptoms. Mania is more pronounced than hypomania and causes more noticeable problems at work, school, and social activities, as well as relationship difficulties. Mania can also cause a break with reality (psychosis) and require hospitalization.
Both a manic and a hypomanic episode include three or more of these symptoms:
- Abnormally optimistic or nervous
- Increased activity, energy or excitement
- Exaggerated sense of well-being and self-confidence (euphoria)
- Reduced need for sleep
- Unusual talkativeness
- Distractibility
- Poor decision-making, such as in speculation, in sexual encounters, or in irrational investments
Major depressive episode
Major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in daily activities such as work, school, social activities, or relationships. Episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless, or tearful (in children and adolescents, depressed mood may present as irritability)
- Marked loss of interest or feeling of displeasure in all (or nearly all) activities
- Significant weight loss with no diet, weight gain, or decreased or increased appetite (in children, failure to gain weight as expected may be a sign of depression)
- Either insomnia or sleeping too much
- Either restlessness or slow behavior
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking, planning or attempting suicide
Other features of bipolar disorder
Signs and symptoms of bipolar I and bipolar II disorder may include other signs such as anxiety disorder, melancholia, psychosis, or others.