Bipolar disorder misdiagnosed
Misdiagnosis of Bipolar Disorder - PMC
1. Khouzam HR, Singh F. Bipolar disorder: Historic perspective, current pharmacologic treatment options, and review of quetiapine. Expert Rev Neurotherapeut. 2006;6(2):131–44. [PubMed] [Google Scholar]
2. Angst J, Sellaro R. Historical perspectives and natural history of bipolar disorder. Biol Psychiatry. 2000;48(6):445–57. [PubMed] [Google Scholar]
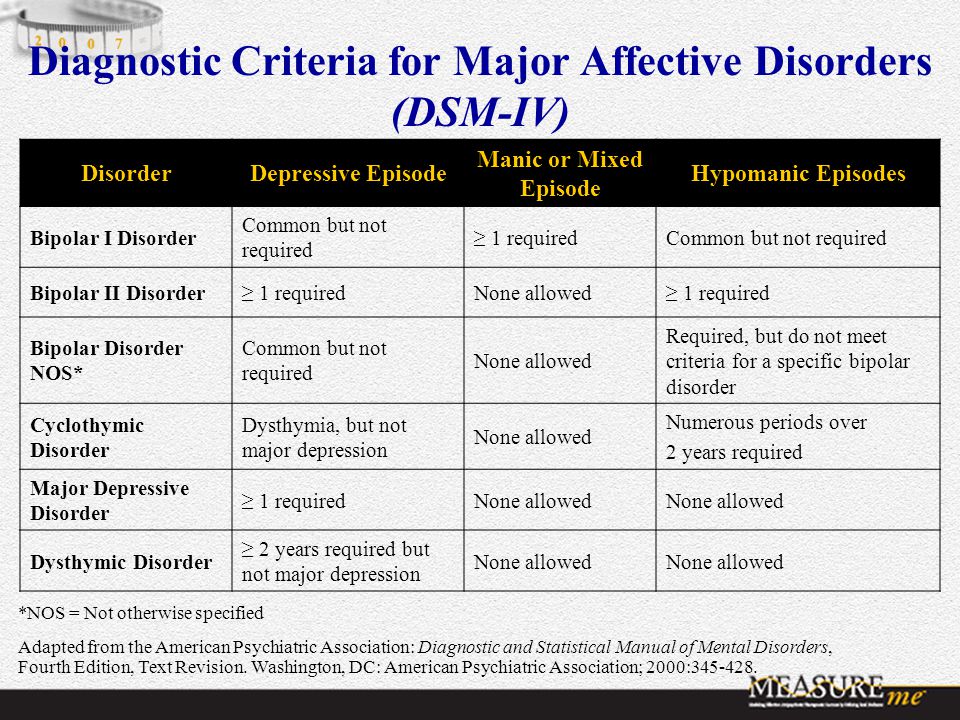
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Third Edition. Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
5. Angst J. The emerging epidemiology of hypomania and bipolar II disorder. J Affect Disord. 1998;50:143–51. [PubMed] [Google Scholar]
6. Akiskal HS, Bourgeois ML, Angst J, et al. Re-evaluating the prevalence of and diagnostic composition within the broad clinical spectrum of bipolar disorders. J Affect Disord. 2000;59:S5–S30. [PubMed] [Google Scholar]
7. Judd LL, Akiskal HS. The prevalence and disability of bipolar spectrum disorders in the US population: Re-analysis of the ECA database taking into account subthreshold cases. J Affect Disord. 2003;73:123–31. [PubMed] [Google Scholar]
8. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–27. [PMC free article] [PubMed] [Google Scholar]
9. Osby U, Brandt L, Correia N, et al. Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry. 2001;58:844–50. [PubMed] [Google Scholar]
10. Woods SW. The economic burden of bipolar disease. J Clin Psychiatry. 2001;61(suppl 13):38–41. [PubMed] [Google Scholar]
11. US Department of Health, Education, and Welfare. Medical Practice Project: A State-of-the-Science Report for the Office of the Science Secretary for the US Department of Health, Education, and Welfare. Baltimore, MD: Policy Research; 1979. [Google Scholar]
Baltimore, MD: Policy Research; 1979. [Google Scholar]
12. Hirschfeld RM, Lewis L, Vornik LA. Perceptions and impact of bipolar disorder: How far have we really come? Results of the National Depressive and Manic-Depressive Association 2000 survey of individuals with bipolar disorder. J Clin Psychiatry. 2003;64:161–74. [PubMed] [Google Scholar]
13. Lish JD, Dime-Meenan S, Whybrow PC, et al. The National Depressive and Manic-Depressive Association (DMDA) survey of bipolar members. J Affect Disord. 1994;31:281–94. [PubMed] [Google Scholar]
14. Morselli PL, Elgie R. GAMIAN Europe. GAMIANEurope/ BEAM survey I—global analysis of a patient questionnaire circulated to 3450 members of 12 European advocacy groups operating in the field of mood disorders. Bipolar Disord. 2003;5:265–78. [PubMed] [Google Scholar]
15. Ghaemi SN, Sachs GS, Chiou AM, et al. Is bipolar disorder still underdiagnosed? Are antidepressants overutilized? J Affect Disord. 1999;52:135–44. [PubMed] [Google Scholar]
16. Ghaemi SN, Boiman EE, Goodwin FK. Diagnosing bipolar disorder and the effect of antidepressants: a naturalistic study. J Clin Psychiatry. 2000;61:804–8. [PubMed] [Google Scholar]
Ghaemi SN, Boiman EE, Goodwin FK. Diagnosing bipolar disorder and the effect of antidepressants: a naturalistic study. J Clin Psychiatry. 2000;61:804–8. [PubMed] [Google Scholar]
17. Bowden CL. A different depression: Clinical distinctions between bipolar and unipolar depression. J Affect Disord. 2005;84:117–25. [PubMed] [Google Scholar]
18. Hirschfeld R, Vornik LA. Recognition and diagnosis of bipolar disorder. J Clin Psychiatry. 2004;65(suppl 15):5–9. [PubMed] [Google Scholar]
19. Perugi G, Micheli C, Akiskal HS, et al. 2000;41:13–18. Polarity of first episode, clinical characteristics, and course of manic depressive illness: A systemic retrospective investigation of 320 bipolar I patients. [PubMed] [Google Scholar]
20. Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv. 2001;52:51–5. [PubMed] [Google Scholar]
21. Akiskal HS. The prevalent clinical spectrum of bipolar disorders; beyond DSM IV. J Clin Psychopharmacol. 199;16:4S–14S. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
22. Angst J, Gamma A, Lewinsohn P. The evolving epidemiology of bipolar disorder. World Psychiatry. 2002;1:146–8. [PMC free article] [PubMed] [Google Scholar]
23. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse: Results from the Epidemiologic Catchment Area (ECA) study. JAMA. 1990;264:2511–8. [PubMed] [Google Scholar]
24. Chen YW, Dilsaver SC. Comorbidity of panic disorder in bipolar illness: Evidence from the epidemiological Catchment Area Survey. Am J Psych. 1995;152:280–2. [PubMed] [Google Scholar]
25. Chen YW, Dilsaver SC. Comorbidity for obsessive compulsive disorder in bipolar and unipolar disorders. Psychiatry Res. 1995;59:57–64. [PubMed] [Google Scholar]
26. Cassidy F, Ahearn EP, Carroll BJ. Substance abuse in bipolar disorder. Bipolar Disord. 2001;3:181–8. [PubMed] [Google Scholar]
27. McElroy SL, Altshuler LL, Suppes T, et al. Axis I psychiatric comorbidity and its relationship to historical illness variables in 288 patients with bipolar disorder.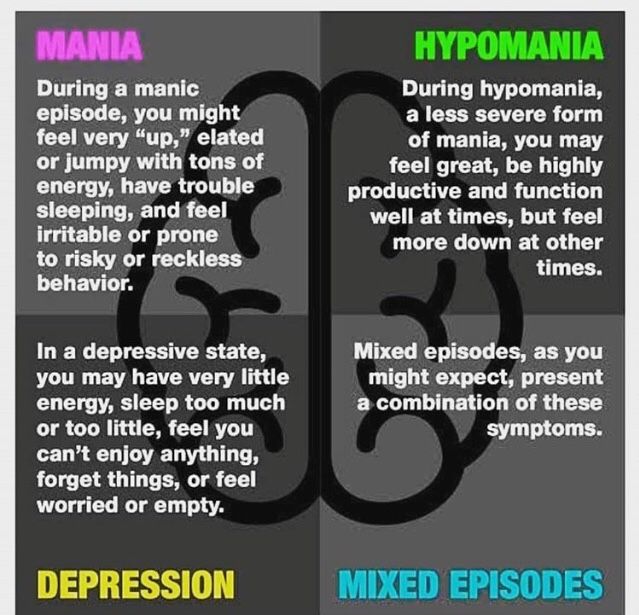 Am J Psychiatry. 2001;158:420–6. [PubMed] [Google Scholar]
Am J Psychiatry. 2001;158:420–6. [PubMed] [Google Scholar]
28. Freeman MP, Freeman SA, McElroy SL. The comorbidity of bipolar and anxiety disorders: Prevalence, psychobiology, and treatment issues. J Affect Disord. 2002;68:1–23. [PubMed] [Google Scholar]
29. Krishnan KR. Psychiatric and medical comorbidities of bipolar disorder. Psychosom Med. 2005;67:1–8. [PubMed] [Google Scholar]
30. McElroy SL. Diagnosing and treating comorbid (complicated) bipolar disorder. J Clin Psychiatry. 2004;65(suppl 15):35–44. [PubMed] [Google Scholar]
31. Lish JD, Dime-Meenan S, Whybrow PC, Price RA, Hirschfeld RM. The National Depressive and Manic-Depressive Association (DMDA) survey of bipolar members. J Affect Disord. 1994;31:281–94. [PubMed] [Google Scholar]
32. Geller B, Luby J. Child and adolescent bipolar disorder: A review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 1997;36:68–76. [PubMed] [Google Scholar]
33. Biederman J, Wozniak J, Kiely K, et al. CBCL clinical scales discriminate prepubertal children with structured interview-derived diagnosis of mania from those with ADHD. J Am Acad Child Adolesc Psychiatry. 1995;34:464–71. [PubMed] [Google Scholar]
J Am Acad Child Adolesc Psychiatry. 1995;34:464–71. [PubMed] [Google Scholar]
34. Biederman J, Faraone S, Mick E, et al. Attention-deficit hyperactivity disorder and juvenile mania: An overlooked comorbidity? J Am Acad Child Adolesc Psychiatry. 1996;35:997–1008. [PubMed] [Google Scholar]
35. Biederman J, Mick E, Bostic JQ, et al. The naturalistic course of pharmacological treatment of children with manic-like symptoms: A systematic chart review. J Clin Psychiatry. 1998;59:628–37. [PubMed] [Google Scholar]
36. Ghaemi SN, Lenox MS, Baldessarini RJ. Effectiveness and safety of long-term antidepressant treatment in bipolar disorder. J Clin Psychiatry. 2001;62:565–9. [PubMed] [Google Scholar]
37. Calabrese JR, Rapport DJ, Kimmel SE, Shelton MD. Controlled trials in bipolar I depression: Focus on switch rates and efficacy. Eur Neuropsychopharmacol. 1999;9:S109–S112. [PubMed] [Google Scholar]
38. Altshuler LL, Post RM, Leverich GS, et al. Antidepressant-induced mania and cycle acceleration: A controversy revisited.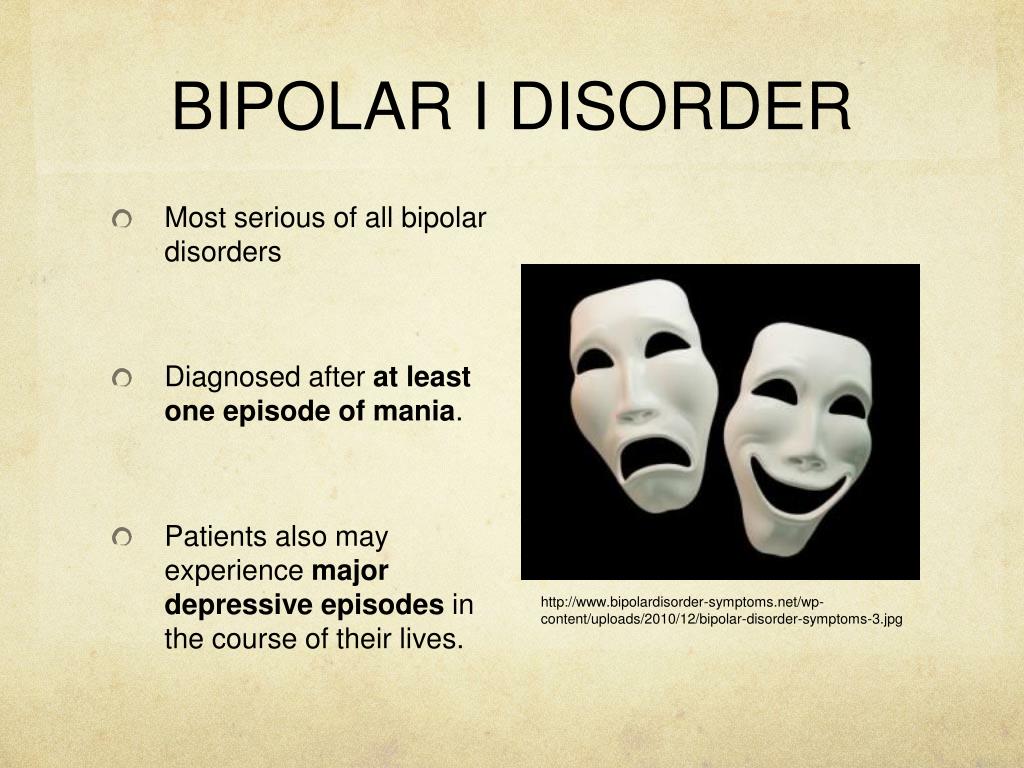 Am J Psychiatry. 1995;152:1130–8. [PubMed] [Google Scholar]
Am J Psychiatry. 1995;152:1130–8. [PubMed] [Google Scholar]
39. Wehr TA, Sack DA, Rosenthal NE, Cowdry RW. Rapid cycling affective disorder: Contributing factors and treatment response in 51 patients. Am J Psychiatry. 1988;145:179–84. [PubMed] [Google Scholar]
40. Li J, McCombs JS, Stimmel GL. Cost of treating bipolar disorder in the California Medicaid (Medi-Cal) program. J Affect Disord. 2002;71:131–9. [PubMed] [Google Scholar]
41. McCombs JS, Thiebaud P, Shi L. Impact of unrecognized bipolar disorders in patients treated with antidepressant medications(abstract) Value Health. 2003;6:352. [Google Scholar]
42. Cooke RG, Robb JC, Young LT, Joffe RT. Well-being and functioning in patients with bipolar disorder assessed using the MOS 20-ITEM short form (SF-20) J Affect Disord. 1996;39:93–7. [PubMed] [Google Scholar]
43. Jamison KR. Suicide and bipolar disorder. J Clin Psychiatry. 2000;61:47–51. [PubMed] [Google Scholar]
44. American Psychiatric Association.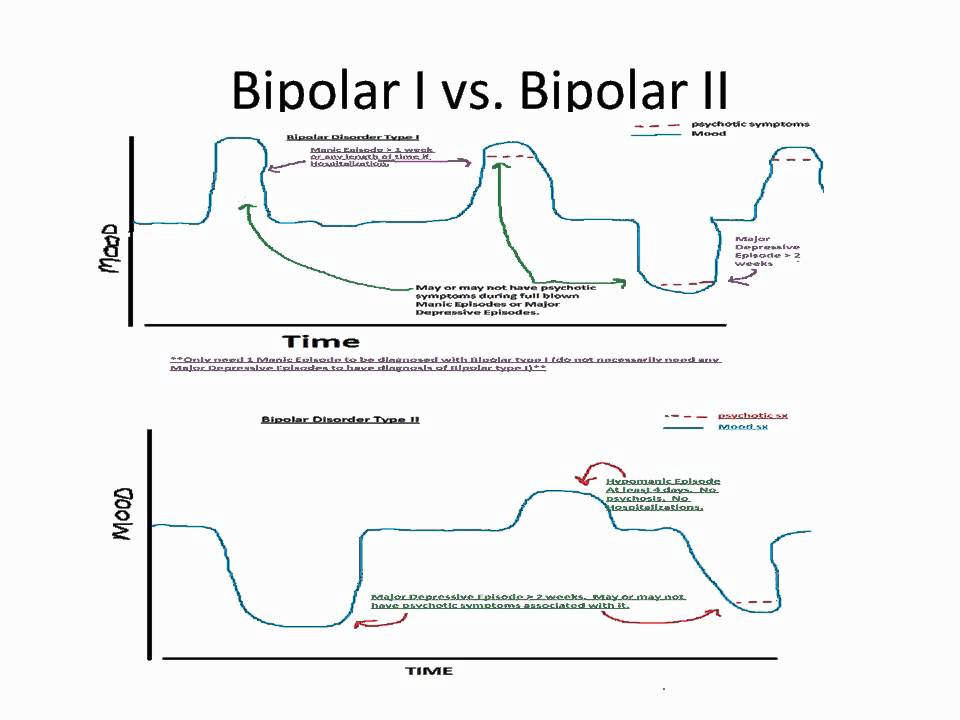 Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: American Psychiatric Press, Inc.; 1994. pp. 317–63. [Google Scholar]
Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: American Psychiatric Press, Inc.; 1994. pp. 317–63. [Google Scholar]
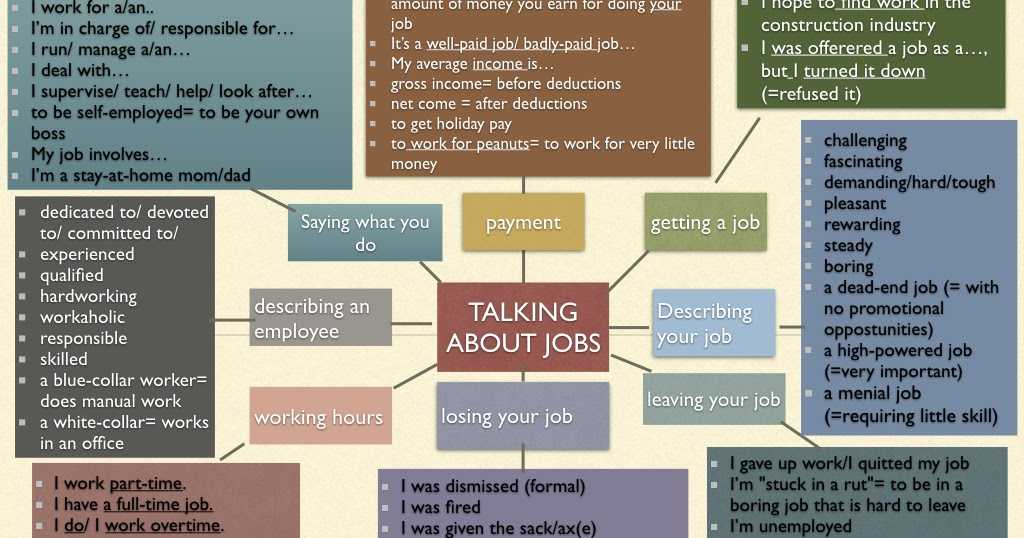
45. Matza LS, De Lissovoy G, Sasane R, et al. The impact of bipolar disorder on work loss. Drug Benefit Trends. 2004;16:476–81. [Google Scholar]
46. Begley CE, Annegers JF, Swann AC, et al. The lifetime cost of bipolar disorder in the US: An estimate for new cases in 1998. Pharmacoeconomics. 2001;19:483–95. [PubMed] [Google Scholar]
47. Rice DP, Miller LS. The economic burden of affective disorders. Br J Psychiatry. 1995;4(Suppl):34–42. [PubMed] [Google Scholar]
48. Perlis RH. Misdiagnosis of bipolar disorder. Am J Man Care. 2005;11:S271–4. [PubMed] [Google Scholar]
49. Manning JS, Haykal RF, Connor PD, et al. On the nature of depressive and anxious states in a family practice setting: The high prevalence of bipolar II and related disorders in a cohort followed longitudinally. Compr Psychiatry. 1997;38:102–8.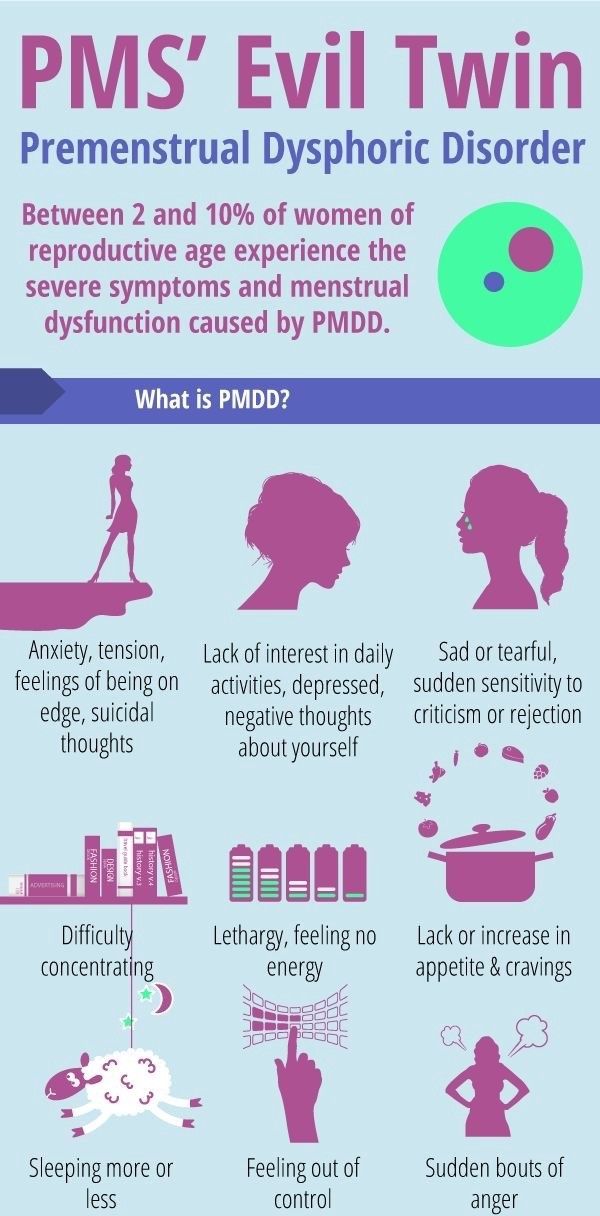 [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
50. Hilty DM, Brady KT, Hales RE. A review of bipolar disorders amongst adults. Psychiatr Serv. 1999;50:201–3. [PubMed] [Google Scholar]
51. Baldassano CF. Assessment tools for screening and monitoring bipolar disorder. Bipolar Disord. 2005;7(Suppl 1):8–15. [PubMed] [Google Scholar]
52. Hirschfeld RM, Calabrese JR, Weissman MM, et al. Screening for bipolar disorder in the community. J Clin Psychiatry. 2003;64:53–9. [PubMed] [Google Scholar]
53. Hirschfeld RM, Holzer C, Calabrese JR, et al. Validity of the mood disorder questionnaire: A general population study. Am J Psychiatry. 2003;160:178–80. [PubMed] [Google Scholar]
54. Hirschfeld RM, Williams JB, Spitzer RL, et al. Development and validation of a screening instrument for bipolar spectrum disorder: The Mood Disorder Questionnaire. Am J Psychiatry. 2000;157:1873–5. [PubMed] [Google Scholar]
55. Ghaemi SN, Miller CJ, Berv DA, et al. Sensitivity and specificity of a new bipolar spectrum diagnostic scale.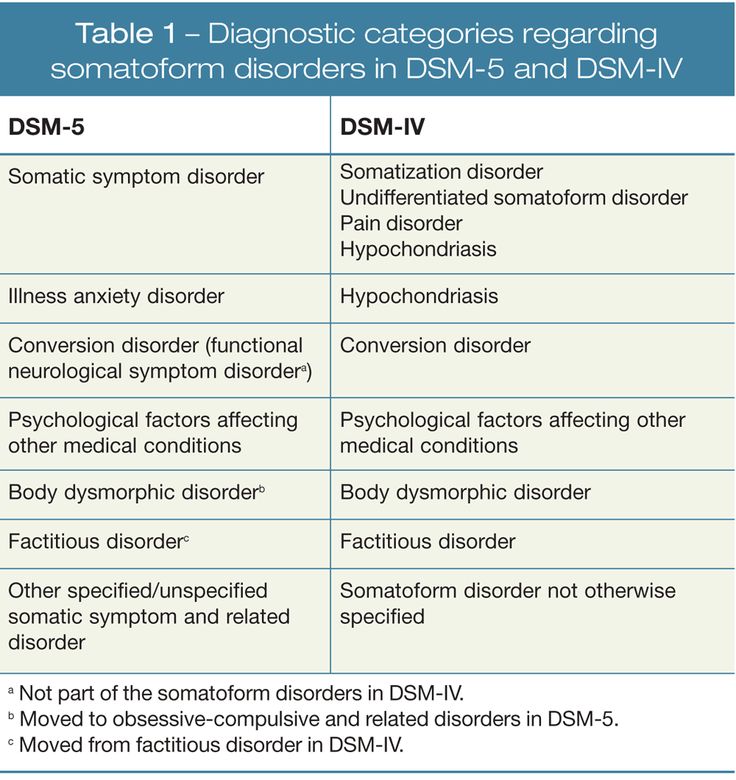 J Affective Disorders. 2005;84:273–7. [PubMed] [Google Scholar]
J Affective Disorders. 2005;84:273–7. [PubMed] [Google Scholar]
56. Meyer TD, Hautzinger M. Screening for bipolar disorders using the hypomanic personality scale. J Affect Disord. 2003;75:149–54. [PubMed] [Google Scholar]
57. Roy PH. Misdiagnosis of bipolar disorder. Am J Manag Care. 2005;11:S271–S274. [PubMed] [Google Scholar]
58. Kupfer DJ, Himmelhoch JM, Swartzburg M, Anderson C, Byck R, Detre TP. Hypersomnia in manic depressive disease. Dis Nerv Syst. 1972;33:720–4. [PubMed] [Google Scholar]
59. Hartmann E. Longitudinal studies of sleep and dream pattern in manic depressive patients. Arch Gen Psychiatry. 1968;19:312–29. [PubMed] [Google Scholar]
60. Brockington IF, Altman E, Hillier V, et al. The clinical picture of bipolar affective disorder in its depressed phase. Br J Psychiatry. 1982;141:558–62. [PubMed] [Google Scholar]
61. Perugi G, Akiskal HS, Latanzi L, et al. The high prevalence of soft bipolar II features in atypical depression. Compr Psychiatry.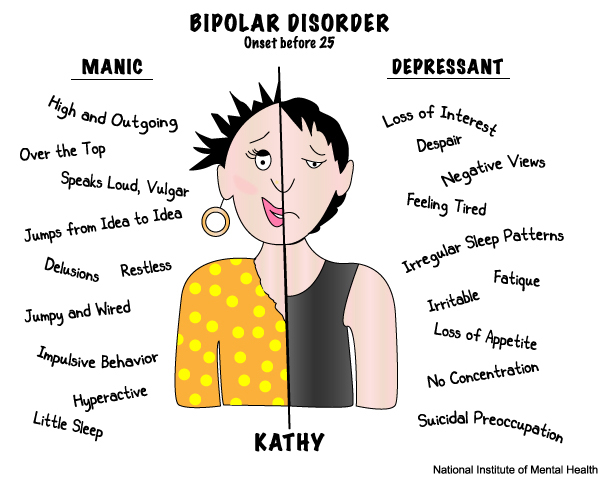 1997;38:102–8. [PubMed] [Google Scholar]
1997;38:102–8. [PubMed] [Google Scholar]
62. Wehr TA, Goodwin FK. Rapid cycling in manic depressives induced by tricyclic antidepressants. Arch Gen Psych. 1979;36:555–9. [PubMed] [Google Scholar]
63. Goodwin FK, Fireman B, Simon GE, et al. Suicide risk in bipolar disorder during treatment with lithium and divalproex. JAMA. 2003;290:1467–73. [PubMed] [Google Scholar]
64. Simon NM, Otto MW, Wisniewski SR, et al. Anxiety disorder comorbidity in bipolar disorder patients: Data from the first 500 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder(STEP-BD) Am J Psychiatry. 2004;161:2222–9. [PubMed] [Google Scholar]
65. Baethge C, Baldessarini RJ, Khalsa HM, et al. Substance abuse in first episode bipolar I disorder: Indications for early intervention. Am J Psychiatry. 2005;162:1008–10. [PubMed] [Google Scholar]
66. Manning JS, Connor PD, Sahai A. The bipolar spectrum: A review of current concepts and implications for the management of depression in primary care.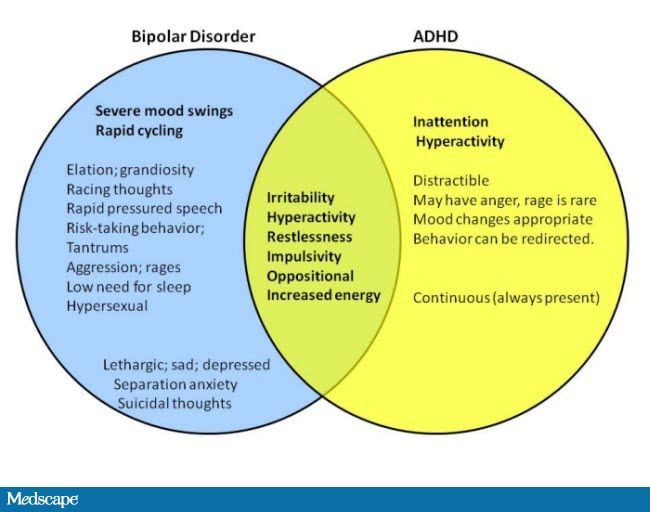 Arch Fam Med. 1998;6:63–71. [PubMed] [Google Scholar]
Arch Fam Med. 1998;6:63–71. [PubMed] [Google Scholar]
67. Janowski DS, Morter S, Hong L, Howe L. Myers Briggs Type Indicator and Tridementional Personality Questionnaire differences between bipolar patients and unipolar depressed patients. Bipolar Disord. 1999;2:98–108. [PubMed] [Google Scholar]
68. Katz MM, Robins E, Croughan J, et al. Behavioural measurement and drug response characteristics of unipolar and bipolar depression. Psychol Med. 1982;12:25–36. [PubMed] [Google Scholar]
69. Reich T, Winokur G. Postpartum psychosis in patients with manic depressive disease. J Nerv Ment Dis. 1970;151:60–8. [PubMed] [Google Scholar]
70. Berk M, Berk L, Moss K, et al. Diagnosing bipolar disorder: How can we do it better? Med J Australia. 2006;189(9):459–62. [PubMed] [Google Scholar]
71. Benazzi F. Unipolar depression with racing thoughts: A bipolar spectrum disorder? Psychiatry Clin Neurosci. 2005;59:570–5. [PubMed] [Google Scholar]
72. American Psychiatric Association. Practice guidelines for the treatment of patients with bipolar disorder. Am J Psychiatry. 1994;151(Suppl):36. [PubMed] [Google Scholar]
Practice guidelines for the treatment of patients with bipolar disorder. Am J Psychiatry. 1994;151(Suppl):36. [PubMed] [Google Scholar]
73. Amsterdam JD, Brunswick DJ. Antidepressant monotherapy for bipolar type II major depression. Bipolar Disord. 2003;5:388–95. [PubMed] [Google Scholar]
74. Amsterdam JD, Shults J, Brunswick DJ, Hundert M. Short term fluoxetine monotherapy for bipolar type II or bipolar NOS major depression-low manic switch rate. Bipolar disord. 2004;6:75–81. [PubMed] [Google Scholar]
75. Benazzi F. Symptoms of depression as possible markers of bipolar II disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2006;3:471–7. [PubMed] [Google Scholar]
Why Bipolar Disorder Is Often Misdiagnosed
About 4 percent of people in the United States experience bipolar disorder at some point in their lives, according to the National Institute of Mental Health (NIMH). And an estimated 2.8 percent of adults had the disorder in the past year.
But in recent years, some researchers have called some bipolar diagnoses into question, while others have maintained that the number of people with the disorder, which causes severe swings in energy levels and mood, is actually greater.
Bipolar disorder is often overdiagnosed, according to a review published in February 2016 in The Canadian Journal of Psychiatry that was authored by Mark Zimmerman, MD, a professor of psychiatry and human behavior at Brown University in Providence and principal investigator of the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) project — an ongoing clinical research study examining the diagnosis, assessment, and outcome of patients. The review, which examined more than 20 years of data from MIDAS as well as results from other studies of diagnosis in routine clinical practice in three other U.S. cities, noted that more complete and accurate diagnostic evaluations could reduce the number of misdiagnoses and improve the detection of conditions related to bipolar disorder.
This 2016 review looked at results from one of Dr. Zimmerman’s earlier studies, published in the Journal of Clinical Psychiatry, which suggested that bipolar disorder is often diagnosed in people who don’t have the condition.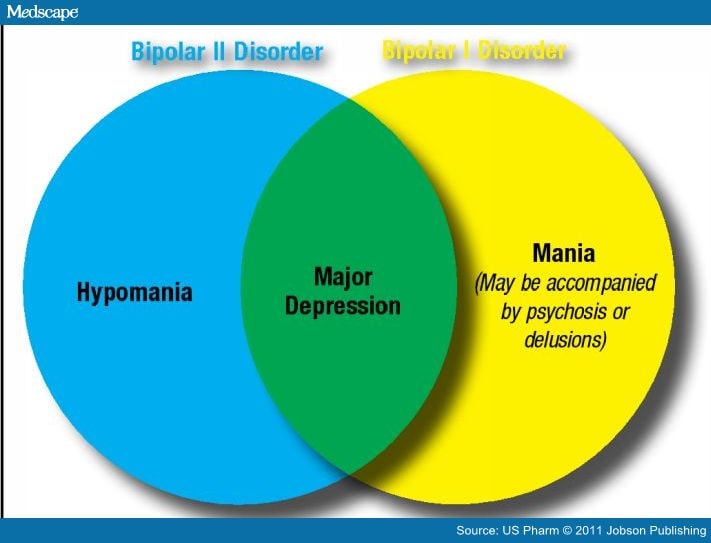 In that large study, his research team determined that fewer than half the people in the study who had been diagnosed with bipolar disorder met the clinical criteria for the illness.
In that large study, his research team determined that fewer than half the people in the study who had been diagnosed with bipolar disorder met the clinical criteria for the illness.
According to Zimmerman, the earlier study also revealed that some people who met the criteria for bipolar disorder had never been diagnosed with it, but in comparison, far more people had been mistakenly diagnosed as bipolar. He believes part of the reason is aggressive marketing to doctors by companies that produce the drugs used to treat bipolar disorder.
“When a pharmaceutical company repeatedly says, ‘Don’t miss bipolar disorder, don’t miss bipolar disorder… and when you diagnose it, here are some medications you can use to treat it,’ there’s a tendency to expand the concept,” Zimmerman says. According to the 2016 review, the limited amount of time that some clinicians spend with patients could also contribute to incorrect diagnoses.
Another factor has to do with bipolar disorder sharing some symptoms with other illnesses, such as borderline personality disorder, a condition marked by impulsive behavior and problems relating to other people.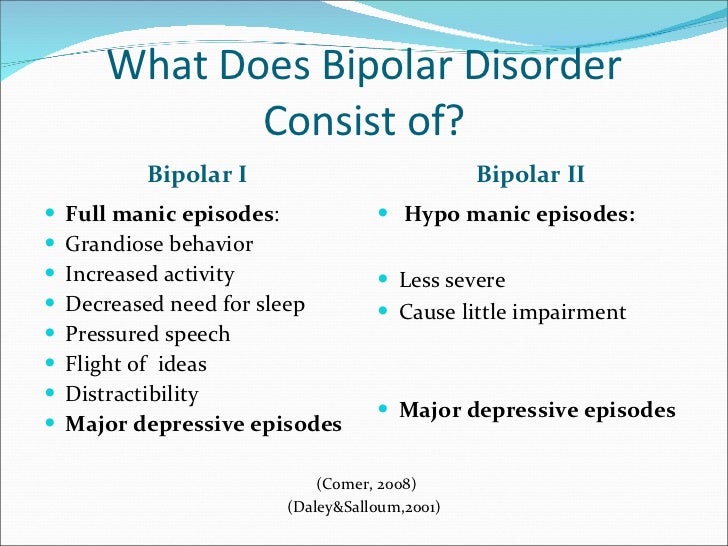 Because of this, Zimmerman says, people who have borderline personality disorder are often misdiagnosed as bipolar, as evidenced by a review published in The Scientific World Journal.
Because of this, Zimmerman says, people who have borderline personality disorder are often misdiagnosed as bipolar, as evidenced by a review published in The Scientific World Journal.
People with bipolar disorder frequently have another mental health issue or condition, such as anxiety disorder, an eating disorder, or a substance abuse problem, which can also contribute to difficulty getting the right diagnosis, according to the NIMH.
How Getting the Wrong Diagnosis Can Be HarmfulFor individuals who are misdiagnosed with bipolar disorder, one potential pitfall may involve health problems that result from taking the prescription drugs used to treat the condition, according to Zimmerman. He notes that some medications, including atypical antipsychotics, can increase the risk for high cholesterol and diabetes, while others, such as lithium, have been linked to thyroid and kidney problems.
Conversely, up to 20 percent of people with bipolar disorder may be mistakenly diagnosed with depression by their primary care doctors, according to a study published in July 2011 in the British Journal of Psychiatry.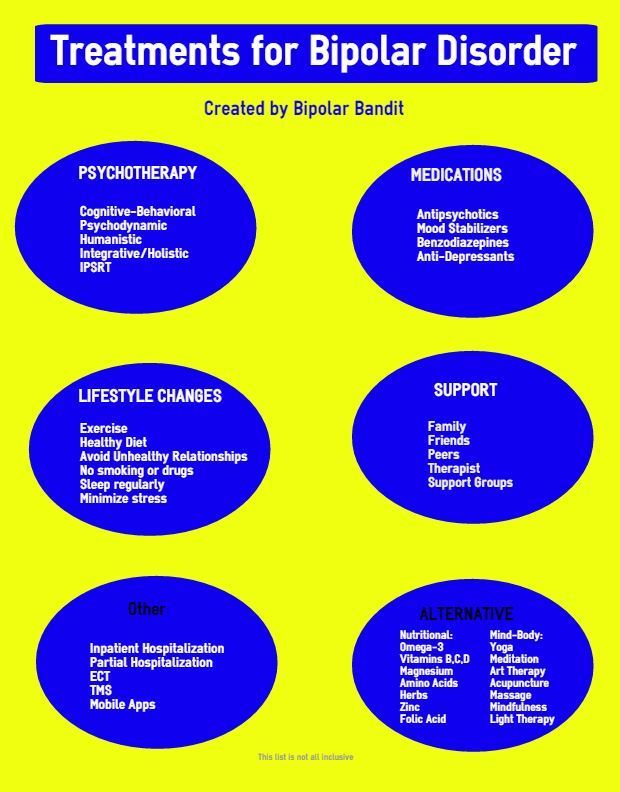 And another study, published in August 2017 in the journal Bipolar Disorders, analyzed the delay in diagnosis of 382 people with bipolar disorder and found that 90 of those individuals initially received a diagnosis of depression before being correctly diagnosed. According to the study, the lag between diagnoses was about nine years. The patients who were originally diagnosed with depression tended to be younger, have more manic symptoms, and have better coping skills, which perhaps helped them function throughout the day and contributed to the delay in getting the correct diagnosis.
And another study, published in August 2017 in the journal Bipolar Disorders, analyzed the delay in diagnosis of 382 people with bipolar disorder and found that 90 of those individuals initially received a diagnosis of depression before being correctly diagnosed. According to the study, the lag between diagnoses was about nine years. The patients who were originally diagnosed with depression tended to be younger, have more manic symptoms, and have better coping skills, which perhaps helped them function throughout the day and contributed to the delay in getting the correct diagnosis.
These findings aren’t surprising, says Jeremy Schwartz, a psychotherapist in Brooklyn, New York. Bipolar disorder can be hard to diagnose, he says, because people often seek professional help only during their down periods and neglect to mention their up, or manic, periods.
“The manic side of bipolar disorder isn’t always bothersome to people,” Schwartz says. “They have more energy and more motivation to do things. So the mental health professional doesn’t always hear about it.”
So the mental health professional doesn’t always hear about it.”
In addition, some younger people with bipolar disorder may have experienced depression but not yet had a manic episode, so a misdiagnosis of depression can sometimes occur simply because a person has not yet experienced mania. In some cases, the mania may not be entirely obvious, adding to the confusion for both the patient and the provider. As a clinical practice update published in October 2017 in the journal Mayo Clinic Proceedings points out, having depression and a hypomanic or manic episode at the same time (referred to as “mixed features”) can occur in as many as 40 percent of patients with major depressive disorder, which can make diagnosis even more complicated. A patient might then be diagnosed as having depression with “mixed features,” and while that symptom alone doesn’t necessarily indicate bipolar disorder, the author notes that the provider should consider bipolar disorder as a possibility in those cases.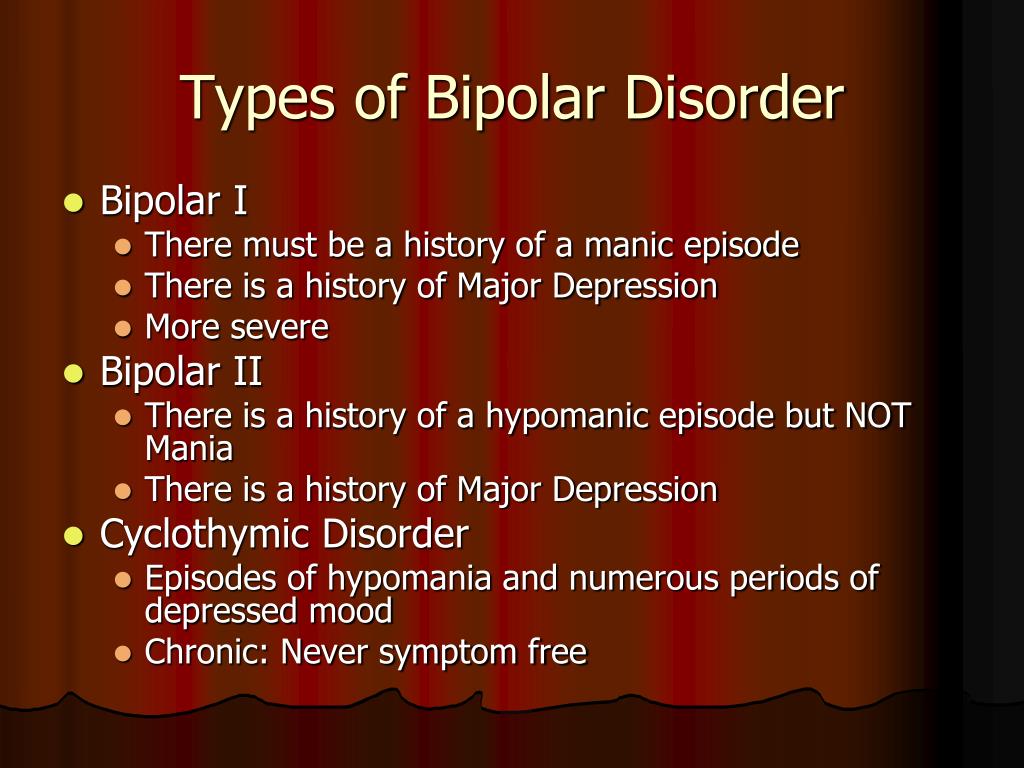
As a consequence, Schwartz says, those with bipolar disorder are often misdiagnosed as having depression and may be given inappropriate treatment. “When bipolar disorder is missed, people can be put on medication that actually worsens the manic symptoms,” Schwartz says. “So people end up waiting much longer to get the stability in their life that they’re looking for.”
In some cases, bipolar disorder may be mistaken for schizophrenia if the patient also has psychotic symptoms, according to NAMI, and someone with schizoaffective disorder can also be wrongfully diagnosed as bipolar. Attention deficit hyperactivity disorder (ADHD) and anxiety disorder can also be confused with bipolar disorder.
Without proper treatment to effectively even out the peaks and valleys of manic and depressive episodes, patients face an increased risk of turning to alcohol and drugs to cope with symptoms, according to a paper published in 2015 in The Journal of Clinical Psychiatry. The author notes that when symptoms such as mania or depression are compounded by substance abuse, patients can see their relationships or job or school performance deteriorate, causing a disabling ripple effect across all areas of their life.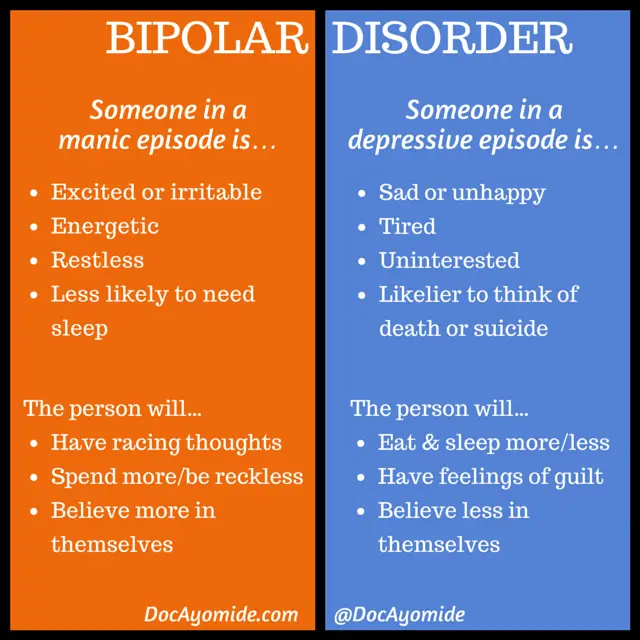 In addition, suicidal thoughts and behavior can also be consequences of a missed diagnosis.
In addition, suicidal thoughts and behavior can also be consequences of a missed diagnosis.
Being correctly diagnosed is an important step toward getting the right treatment for your bipolar disorder so you can manage your condition and live a healthy, active, and fulfilling life.
One of the most important things you can do to increase your chances of receiving an accurate diagnosis is to talk with your doctor about all of your symptoms and emotions — both the good and the bad — says Schwartz. “It helps to create a fuller picture of your experience,” he explains.
Once you receive your diagnosis, you can always ask your doctor about their reasoning, especially if you have any doubts or questions, notes Zimmerman. “Ask the doctor why they have made the diagnosis,” he says. “A good doctor should be willing to discuss the reasons and to explain if they’re uncertain about it.” If you don’t receive satisfactory answers, he adds, an opinion from another doctor may be in order.
Additional reporting by Deborah Shapiro and Jessica Migala
Is bipolar disorder overdiagnosed? Who is at risk of being misdiagnosed with this? | mental health articles | Emotional & Mental Health center
You may have heard that people who actually have bipolar disorder are at risk of being misdiagnosed with other conditions, especially (unipolar) depression, but did you know that the opposite can happen?
To get the right treatment, you need the right diagnosis - this is one of the most obvious foundations of modern medicine.
You've probably heard that bipolar disorder is incredibly difficult to diagnose - many patients take years and years of psychiatric visits and cries for help before they finally get a proper diagnosis. Many people who are actually bipolar are misdiagnosed with unipolar depression because they only have contact with psychiatrists during their depressive phases.
There is less talk about the fact that some people who should actually have different diagnoses are labeled bipolar instead, but it happens too. Like people who were diagnosed with bipolar disorder long ago, those who are misdiagnosed with it remain underdeveloped, unable to receive the kind of treatment or support they could actually benefit from.
Like people who were diagnosed with bipolar disorder long ago, those who are misdiagnosed with it remain underdeveloped, unable to receive the kind of treatment or support they could actually benefit from.
What conditions are most commonly misdiagnosed as bipolar disorder and why?
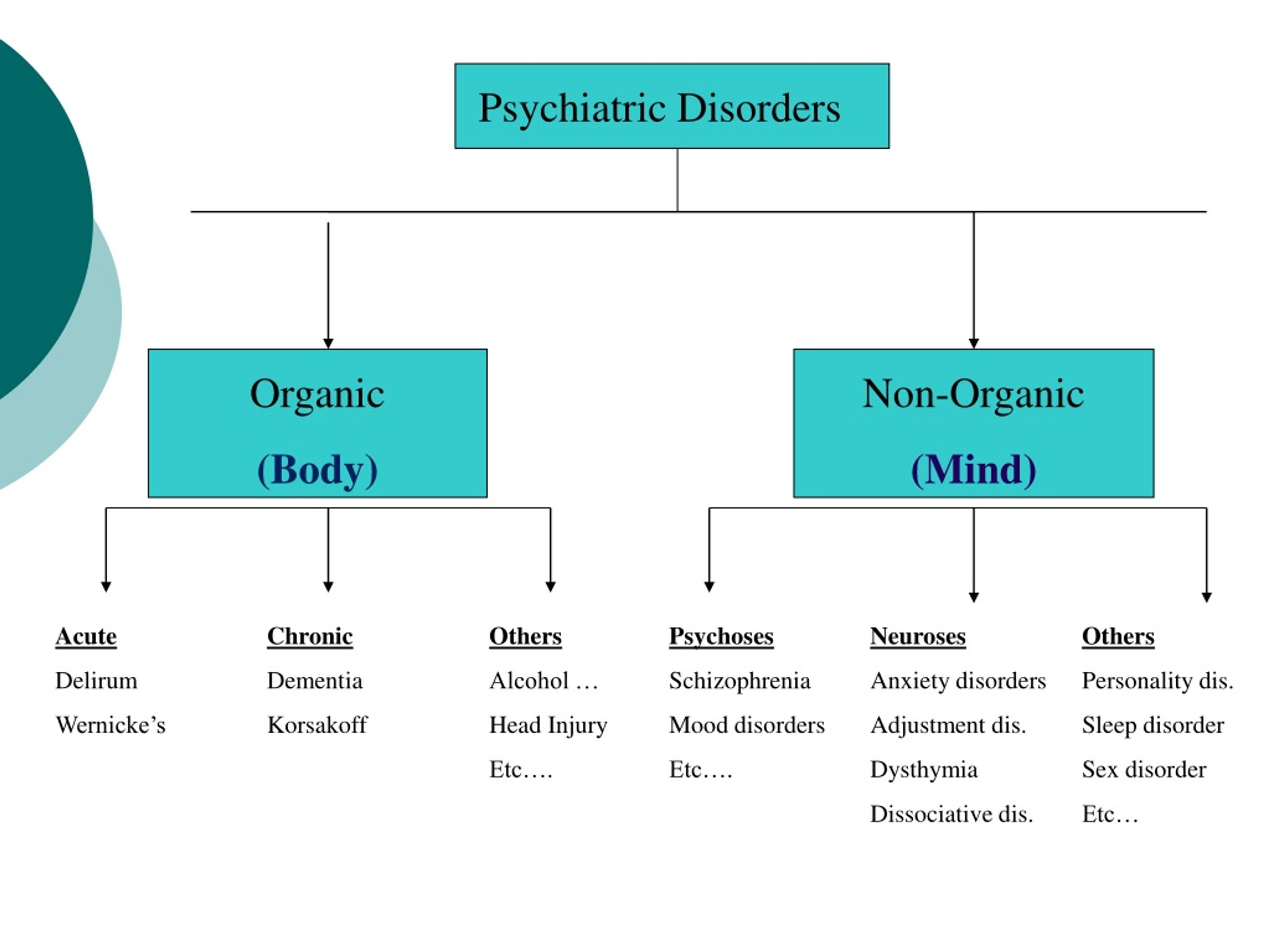
First, a refresher course: what is bipolar disorder?
"Bipolar disorder" is not one thing. The fifth (and current) edition of the Diagnostic and Statistical Manual of Mental Disorders, DSM-5, contains an entire chapter on "Bipolar and Related Disorders" that covers many diagnoses:
- Bipolar I
- Bipolar disorder II
- Cyclothymic disorder
- Bipolar and comorbid substance or drug induced disorder
- Bipolar and related disorder due to another disease
- Other specified bipolar and related disorders and unspecified bipolar and related disorders
The DSM-5 chapter on bipolar and related disorders is placed between the chapters on the spectrum of schizophrenia and other psychotic disorders and depressive disorders to acknowledge the fact that these disorders characterize aspects of both.
You are probably familiar with the fact that bipolar disorder is characterized by extreme mood changes or "mood episodes" and know that the two most extreme are mania and depression.
- When someone with bipolar disorder has a depressive episode, they will meet all of the diagnostic criteria for major depressive disorder - which includes symptoms such as feelings of sadness, emptiness, tears, and hopelessness, loss of interest in important tasks, and difficulty getting things done their daily duties, feelings of hopelessness and - in some cases - suicidal thoughts.
- Mania is an episode of "overwhelmed" mood during which one feels incredibly energetic and "nervous". Someone who experiences mania may feel euphoric or very irritated, but these mood episodes can be exhilarating either way, and people with mania may feel like they can do anything. They can lose touch with reality and behave quite risky.
Bipolar disorder - and the specifics will vary depending on the exact diagnosis - is also accompanied by periods of remission ("typical mood") and other mood episodes.
Hypomania is a less extreme form of mania where someone is energetic, has lots of racing ideas, is very talkative and doesn't need much sleep. Although the person suffering from hypomania will have an increased (even grandiose) self-esteem, there will be no psychotic features, no hospitalization is required, and the person can, with effort, cope with the responsibilities of his daily life.
Some people also have mixed episodes of depression and mania at the same time.
Bipolar II is the main diagnosis in which people experience (less intense) hypomanic and depressive episodes, and it is with this diagnosis that people are most likely to erroneously return. Other specified and unspecified bipolar and related disorders may also be diagnosed when a mental health professional is not entirely sure what is going on.
Conditions that may be misdiagnosed as bipolar disorder
Conditions that can be misdiagnosed as bipolar disorder are, of course, those that have symptoms that overlap. This certainly includes major depressive disorder (unipolar depression) (and we won't go into detail on this because it's obvious how such a misdiagnosis can come about), but goes far beyond it.
Borderline personality disorder, a condition characterized by erratic and intense interpersonal relationships, impulsive and reckless behavior, fears of abandonment by loved ones and efforts to prevent it, suicidal feelings and - note this - highly variable moods, may be misdiagnosed as bipolar disorder.
People with Attention Deficit/Hyperactivity Disorder (ADHD) tend to be visibly restless and restless and easily distracted unless they are focusing on something meaningful to them. Their high energy levels and impulsivity can give the impression of hypomania. It's not hard to see why ADHD can be misdiagnosed as bipolar disorder (and vice versa, especially in children), especially if someone with ADHD is already depressed and a gradual return to normal can be seen as signs of hypomania.
People on the autism spectrum can also be misdiagnosed with bipolar disorder. This is especially true for highly developed autistic people who would previously qualify for an Asperger's diagnosis. Social and behavioral differences in autistic people can be falsely attributed to depression (because the person is intimidated by new or overwhelming conditions) and mania or hypomania (because they are agitated and exhibit "jumping thoughts"). Women, who are more likely to overlook an autism diagnosis due to the misconception that men are more prone to autism, may be particularly vulnerable to this kind of misdiagnosis.
In addition, there is narcissistic personality disorder, grandiose self-esteem, a sense of entitlement, and a sense of "speciality," which can in many ways resemble a manic episode of bipolar disorder.
The Final Word
As research advances and we understand bipolar disorder and the brain in general, it is becoming clear that bipolar disorder is both underdiagnosed and overdiagnosed. That is, some people are given diagnoses that they should not have.
This can be far-reaching because although some conditions may have overlapping symptoms, this does not mean that they are managed or treated in the same way. For example, mood stabilizers would not be better served by someone with major depression or ADHD.
It is important to take into account the fact that people can have more than one diagnosis at the same time. Some people have not been misdiagnosed, but simply not fully diagnosed - they may indeed have bipolar disorder, but also, for example, ADHD.
Having said that, if you strongly suspect that you or someone you love has been misdiagnosed with bipolar disorder, it may well be time for further evaluation. Explain why you think the diagnosis was incorrect in as much detail as possible, and if you suspect another disorder, be sure to mention that as well.
In the end, correct diagnosis remains the key to better treatment.
Four diseases that doctors often misdiagnose - Blog
- Home
- >
- Blog
- >
- Four Diseases Doctors Often Misdiagnose
Physicians educate and hone their expertise, hoping to eventually get to the point where the diagnosis is obvious. But be that as it may, doctors are people, and people are not immune from mistakes. In medicine, such a mistake carries a risk and often a very high price.
You think that physical illness is easier to observe than, for example, mental illness. A stab wound, unlike depression, has clear evidence. But even physical conditions are not equal and, just like mental disorders and infectious diseases, may seem something completely different even to the most trained professional eye.
- Depression and stress associated with diabetes
People with diabetes have every reason to experience constant stress associated with constant check-ups, medications and diets.
More and more researchers are coming to the conclusion that this stress is similar to depression. But, in this case, treating depression can be unnecessary, or even dangerous, in the case of antidepressants - treating the symptoms of stress associated with diabetes often "cures" the depression that the doctor once saw.
"Because the diagnosis of depression is based on symptoms and is not tied to a cause, in many cases these symptoms actually reflect the stress that patients with diabetes are experiencing, rather than a clinical diagnosis of depression" , said Dr. Lawrence Fisher, lead author of a recent study presented at the 74th meeting of the American Diabetes Association.
Clinicians should treat stress symptoms as a manifestation of diabetes. Fisher says: "They should not be considered a form of psychopathy" .
- ADHD and OCD
Attention Deficit Hyperactivity Disorder and OCD are, in many ways, two sides of the same coin.
But a misdiagnosis can be disastrous for a child whose fragile brain is still developing. While both are attention-deficit disorders, ADHD manifests itself as great difficulty concentrating, while OCD manifests itself as hyperarousal and hyper-concentration.
A 2012 study found that ADHD patients are more impulsive than OCD patients. The danger comes from medications: people with ADHD are often prescribed Ritalin to reduce excitability. Prescribing this same focus-enhancing drug to people with OCD only worsens their condition.
"It's more likely that a young student will be diagnosed with ADHD instead of OCD because teachers are used to dealing with a lot of people with attention problems than with OCD" , said co-investigator Prof. Ruven Dar. "You can make a mistake if you don't look carefully enough" .
- HIV and influenza
It can take up to 3 months before the human immunodeficiency virus tests positive on routine tests.
Until then, there is a risky period of uncertainty. Common early signs of infection include weight loss, fever, nausea, vomiting, mouth ulcers, and swollen lymph nodes that are easily confused with flu symptoms.
A new study by the British Columbia Center for Excellence in HIV/AIDS Management provides clinicians with a set of guidelines for recognizing the difference between the two diseases and prescribing appropriate treatment. The authors claim that they are not criticizing physicians with their study. They just want to emphasize the importance of early testing and preventive work.
"A simple blood test combined with a clinical assessment allows us to detect this disease early and provide life-saving treatment" , - said the director of the Center, Dr. Julio Montaner.
- Bipolar Disorder and Personality Disorders
With all the advances in modern medicine, the best tool for diagnosing bipolar disorder is still the face-to-face interview with the patient.
Learn more