Adderall tension headache
All About Adderall and Migraine Headaches
Adderall can be an important part of ADHD management, but it’s not without its side effects. Adderall can cause headaches, but there’s limited evidence it causes or treats migraine.
Adderall is in a class of medications called central nervous system stimulants. People with attention deficit hyperactivity disorder (ADHD) often take Adderall to help improve symptoms.
And while this drug can be an effective ADHD treatment, it does come with potential side effects — like headaches.
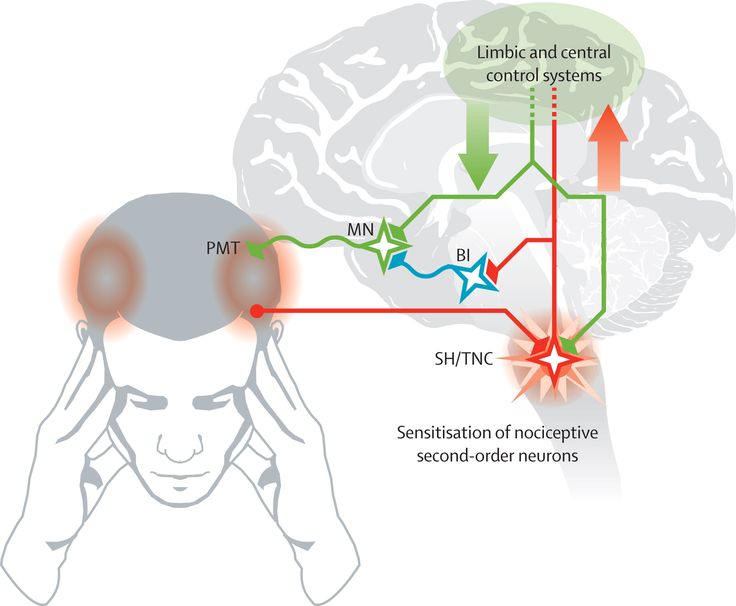
Migraine is a neurological condition known for its severe headaches. But migraine is more than that, with other symptoms like:
- debilitating pain
- nausea and vomiting
- auras (which come with their own symptoms like blurry vision)
The relationship between Adderall and migraine is currently quite complicated. It’s not clear if migraine attacks are a side effect of Adderall, although people who live with ADHD may be more likely to also have migraine.
Some people report, based on limited evidence, that Adderall may not necessarily cause migraine headaches but actually help treat them.
Headaches are one possible side effect of taking Adderall. But even if the headache is severe, it may not be a migraine headache.
According to the advocacy group Children and Adults with Attention-Deficit/Hyperactivity Disorder (CHADD), some people have headaches when they start ADHD medication. These typically stop once your body is used to the treatment.
CHADD also notes that there’s an apparent connection between ADHD and migraine.
People with ADHD often have migraine, possibly at a higher rate than people without ADHD. Therefore, someone who is taking Adderall for ADHD may have migraine headaches — but Adderall may not be the cause.
The generic name for Adderall is dextroamphetamine/amphetamine. It’s a central nervous system stimulant commonly prescribed for ADHD and narcolepsy.
Adderall has a number of common side effects, such as:
- high blood pressure
- insomnia
- weight loss
- headache
- dry mouth
- decreased appetite
- nausea
- abdominal pain
- diarrhea
- nervousness
- changes in mood
Headaches are one of the more common side effects of Adderall.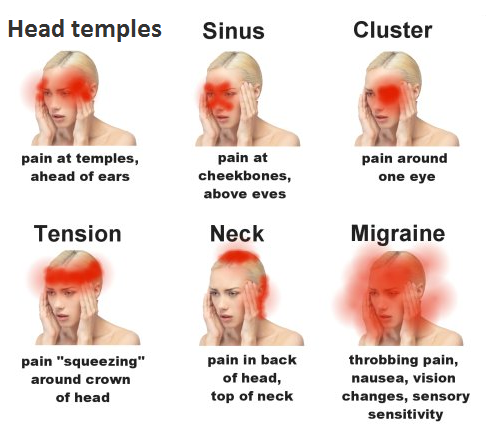
Like other medications, Adderall has a few less common but serious possible side effects, including:
- heart attack
- stroke
- seizure
- worsening psychiatric symptoms
These serious side effects are rare, but your doctor may discuss them with you if you are prescribed Adderall.
Adderall XR also comes with a boxed warning that it has a high potential for misuse and dependence.
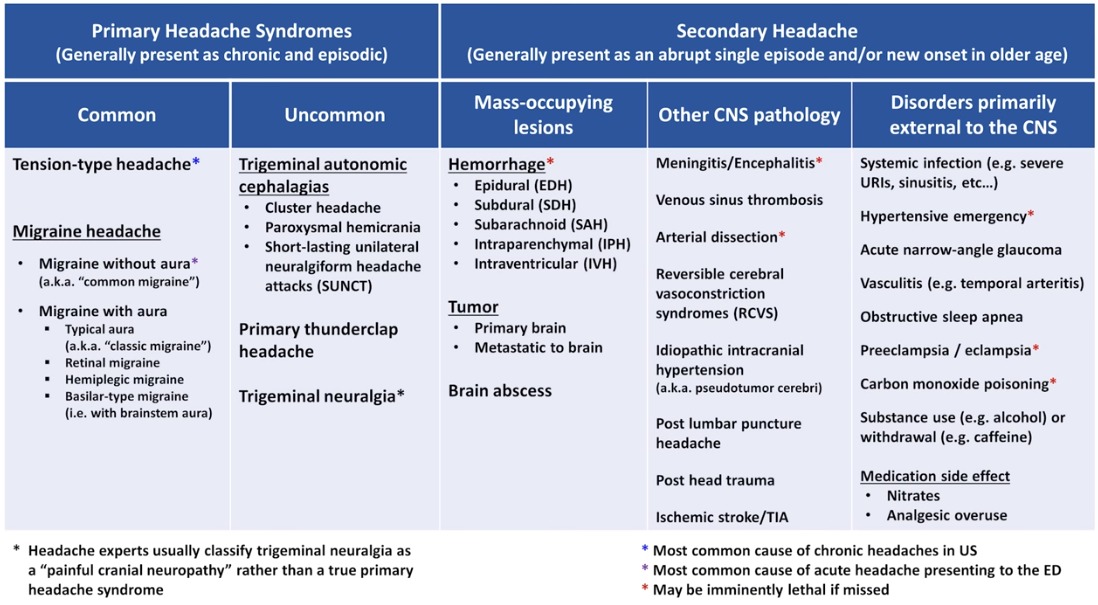
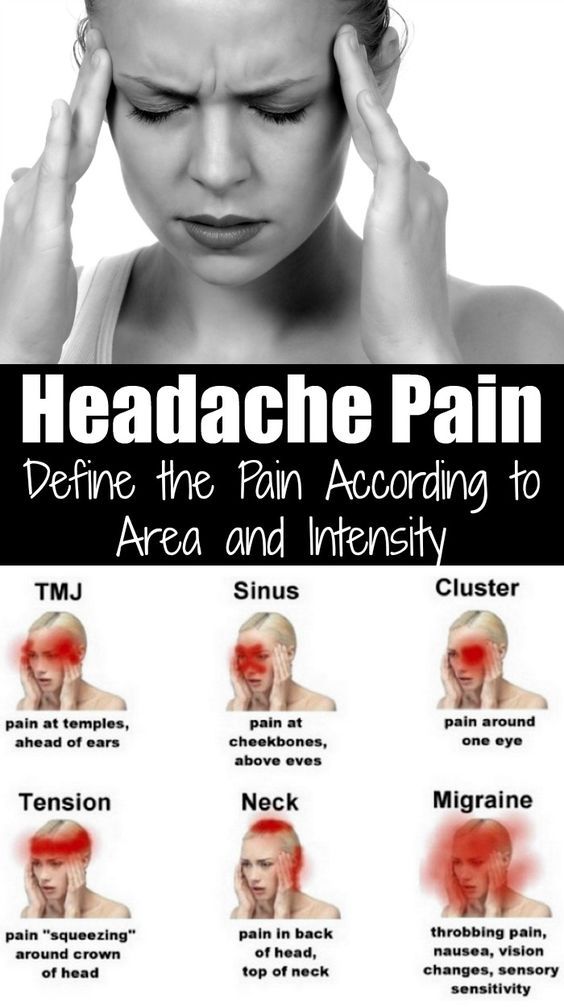
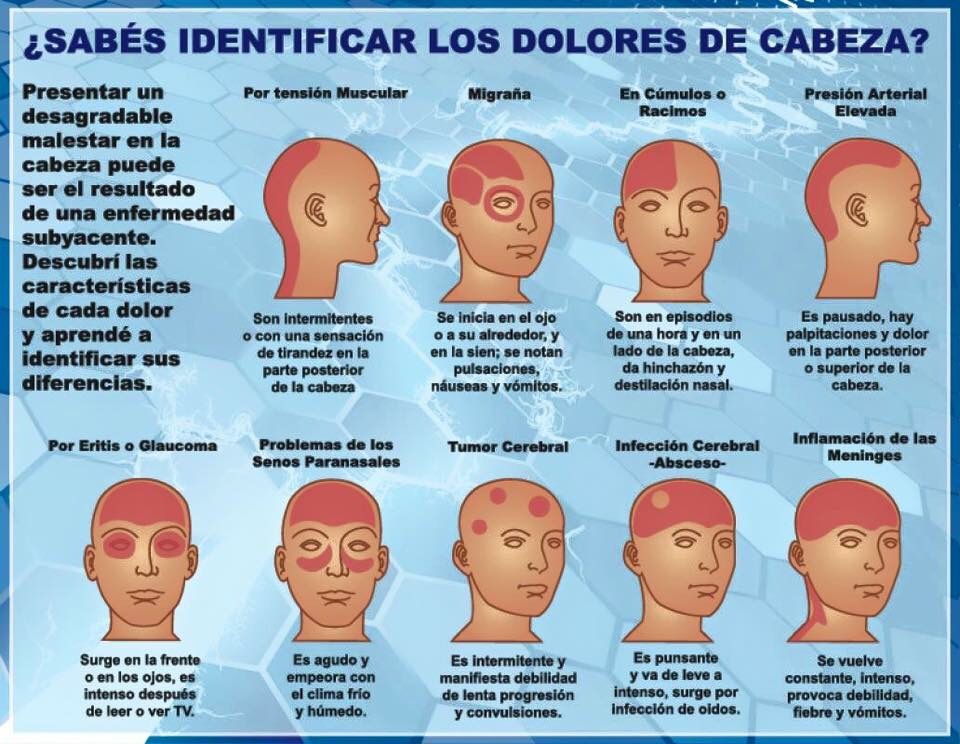
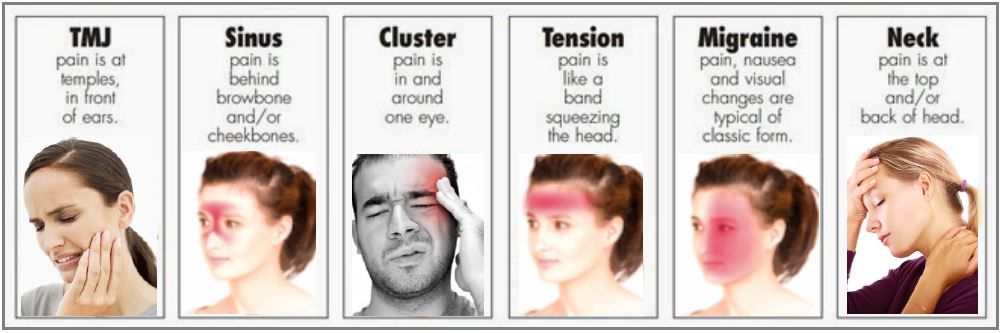
There are a few key differences between a migraine headache and other types of headaches.
A migraine attack often involves a moderate to severe headache. Sometimes it can be hard to tell the difference between a bad headache and migraine.
Migraine symptoms can last from several hours to a few days.
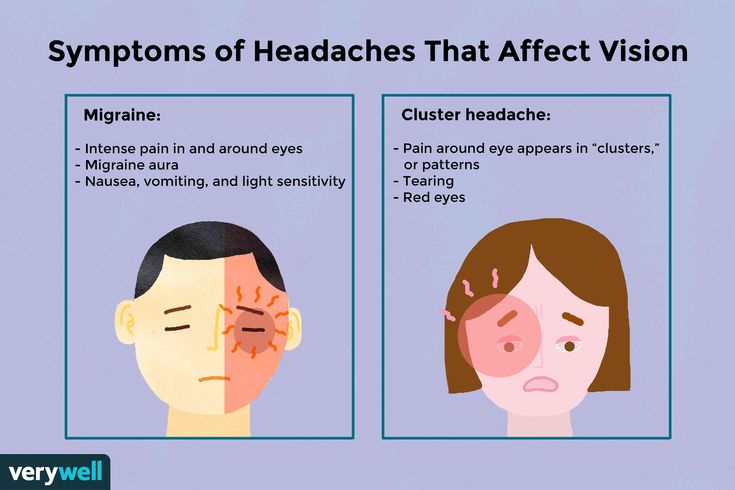
There are symptoms that are unique to migraine, though. These include:
- intense pain on only one side of the head
- throbbing pain that gets worse with movement
- nausea
- vomiting
- light and sound sensitivity
- auras
Auras and migraine
Some people have migraine with aura. Auras have their own set of visual, sensory, and speech or language symptoms.
Auras have their own set of visual, sensory, and speech or language symptoms.
Aura symptoms usually occur before and alongside migraine symptoms. Some characteristics of an aura include:
- seeing flashing lights and zig-zag patterns
- dizziness
- experiencing numbness or tingling in one hand that moves up to the arm
There is some evidence that Adderall may reduce the frequency of migraine attacks, although the data is far from conclusive and very limited.
One small 2004 trial study examined whether dextroamphetamine — a key ingredient in Adderall — might help with chronic tension-type and migraine headaches. The data suggests that dextroamphetamine may be effective for preventing migraine as well as tension headaches, though more research is needed.
Stimulants and pain management
Stimulants and amphetamines are sometimes part of pain treatment.
For example, cancer patients are sometimes prescribed stimulants to increase the effectiveness of opioids and to reduce the drowsiness opioids may cause.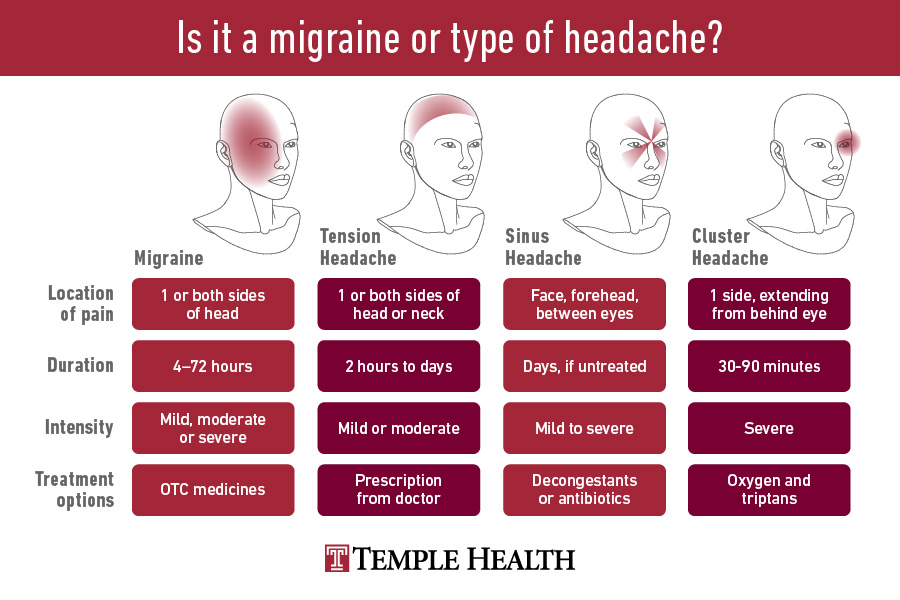 Stimulants may therefore have some pain-relieving properties that also work on migraine.
Stimulants may therefore have some pain-relieving properties that also work on migraine.
Migraine is typically treated with pain-reducing medication. Physicians may recommend starting with an over-the-counter medication, like ibuprofen or acetaminophen.
If you think Adderall may be causing your migraine headaches, consider talking with your doctor. They may be able to work with you to find the right dose of your medication. They may also provide supplementary treatment or recommend an Adderall alternative.
Prescribed medications
The first-line prescription treatment for migraine is a class of drugs called triptans. They prevent the dilation of arteries in the head that happen during migraine. Triptans can also block pain signals to the brain.
Other medications to help treat migraine include:
- analgesics (acetaminophen): to help with pain management and inflammation
- antiemetics: to prevent nausea and vomiting
- dihydroergotamine: to narrow blood vessels
- NSAIDs (aspirin, diclofenac, ibuprofen, naproxen, ketorolac): nonsteroidal anti-inflammatory drugs
Alternative treatments
Alternative treatments for migraine might include:
- biofeedback, which monitors your body’s response to stress
- acupuncture
- vagus nerve stimulators
Adderall can be an effective treatment for ADHD and narcolepsy.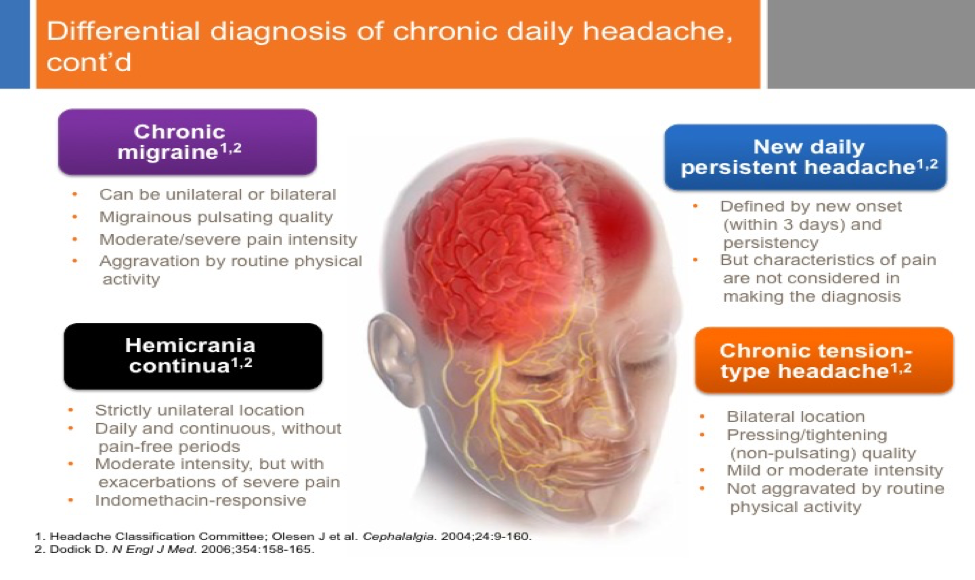 For people living with these conditions, Adderall can improve their quality of life.
For people living with these conditions, Adderall can improve their quality of life.
While headaches are a common side effect of Adderall, it’s not clear if Adderall causes migraine episodes. People who live with ADHD may also have migraine, whether or not they’re taking Adderall.
Treatment for migraine often involves over-the-counter and prescription pain medication. There is currently very limited evidence that Adderall may help treat migraine.
Pain management is an often complex process. A doctor can help you find the right treatment for severe migraine symptoms.
You may also find support and community with online groups dedicated to people living with migraine, like:
- Bezzy Migraine
- Miles for Migraine
- National Chronic Pain Support Groups
Speaking with a therapist about ADHD and migraine pain can also help you find behavioral strategies to manage daily living. You can get started finding a therapist by visiting PsychCentral’s resource guide for seeking mental health support today.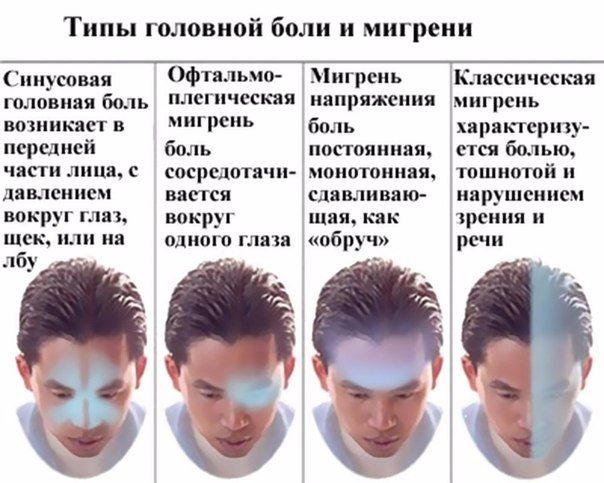
Adderall Headaches: How To Prevent Them
Adderall is a central nervous system (CNS) stimulant that increases alertness and energy by increasing neurotransmitter activity in the brain and boosting dopamine, norepinephrine, and serotonin levels.
Adderall can be effective in treating ADHD, since it positively affects CNS receptors. However, one of the side effects of Adderall use or abuse is headaches.
Fortunately, these headaches are largely treatable and preventable.
Why Adderall Causes Headaches
There are a few different theories as to why Adderall, a brand name for amphetamine medication often misused by college students, may cause headaches.
One theory is that the medication can cause changes in blood pressure and blood flow, which can lead to headaches.
Another theory is that the stimulant effects of Adderall can lead to headaches in people who are sensitive to them.
Lactic acid buildup is also a side effect of using amphetamine-based prescriptions, which is a common trigger for migraines and headaches.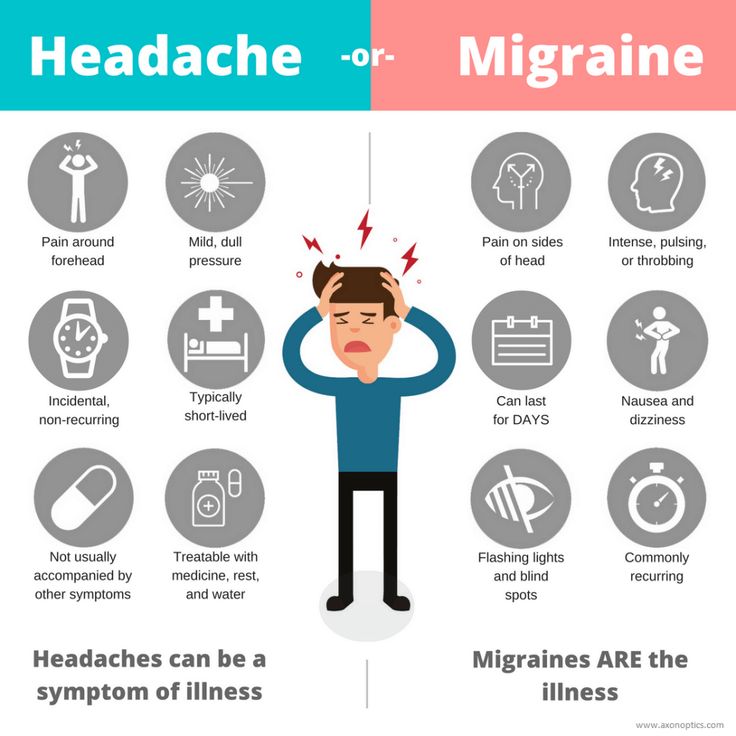
Some of the most common side effects of taking Adderall are fatigue, dry mouth, nausea, and headaches. The culprit for these side effects is likely the amphetamine in the drug.
This ADHD medication also raises your blood pressure and increases your heart rate, which can affect your sensitivity to headaches and make you more prone to experiencing them.
5 Tips For Preventing Adderall Headaches
There are a number of ways you can prevent Adderall-induced headaches.
1. Take The Medication As Prescribed
Taking too much Adderall, taking it more frequently than prescribed, or abusing it in another way can increase the risk of headaches.
2. Take Adderall With Food
Taking Adderall on an empty stomach can also lead to headaches.
While you can experience a loss of appetite with Adderall, taking dextroamphetamine or amphetamine medications without food can intensify their immediate effects.
3. Stay Hydrated When Taking Adderall
Making sure that you drink enough water is critical to keep some of the common side effects of Adderall use at bay.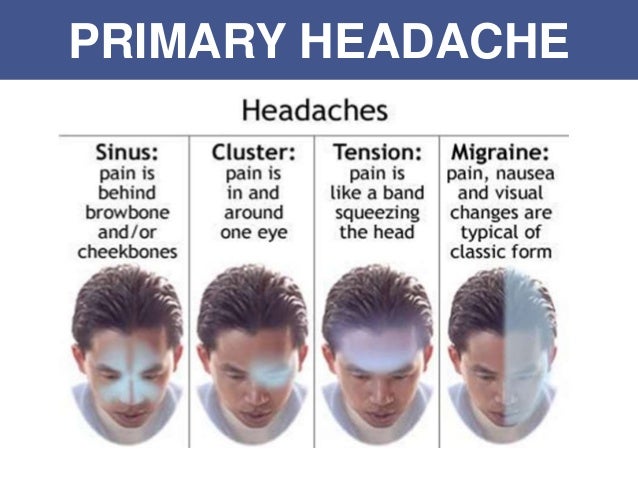
Drinking lots of water can lower your high blood pressure and decrease the pain by flushing out your body.
Also, taking over-the-counter pain relievers such as ibuprofen can limit the chances of developing a migraine headache, or mitigate the headache’s severity if you develop one.
4. Limit Caffeine And Alcohol Intake
Alcohol is a depressant, and caffeine is a stimulant.
Mixing a depressant with a stimulant, such as Adderall and alcohol, can confuse the CNS and upset the careful balance of hormones therein.
Combining stimulants can cause a number of possible side effects, such as agitation, excess excitability, and fidgeting, and can overstimulate the brain — leading to potential headaches.
Healthcare providers prescribing adolescents and adult ADHD patients Adderall in extended release forms (Adderall XR) recommend avoiding additional stimulants, such as coffee.
5. Eat Healthy Foods
Ensuring that you have a healthy, balanced diet can not only prevent Adderall-induced headaches, but can also mitigate many of the other side effects produced by the medication.
Can Adderall Headaches Be Permanent?
This central nervous system stimulant causes headaches, but they are not permanent.
Detoxification, hydration, and painkillers are often all that are necessary to erase a headache caused by Adderall.
There are other side effects of Adderall use that are caused by abuse of the drug, some of which can be long-lasting, such as mental health disorders and cardiovascular problems.
Some side effects of Adderall abuse are:
- weight loss
- sleep problems
- dry mouth
- decreased appetite
- nervousness
- psychosis
- mood swings
- anxiety
Can Adderall Withdrawal Cause Headaches?
Adderall is an effective medication for mitigating and treating ADHD symptoms and other hyperactive tics, but even when taken regularly you can experience withdrawal.
Headaches are also a symptom of Adderall withdrawal. If you regularly take or misuse Adderall and skip a dose, you may experience headaches.
It is important to understand that withdrawal symptoms are not the same as side effects, which happen while taking the drug, but that symptoms of withdrawal appear after its use is stopped.
Symptoms of Adderall withdrawal include:
- depression
- anxiety
- fatigue
- stomach aches or cramping
- vomiting
- nausea
Addiction Treatment Services For Adderall Abuse
Fortunately, there are many programs and services available to help people who abuse Adderall get off the drug and stay clean.
Some of these treatment options for Adderall drug abuse include:
- inpatient and outpatient programs
- behavioral therapy
- partial hospitalization programs (PHP)
- individual, group, and family counseling
- telehealth services
- detoxification
- vocational programs
- educational courses on drug and alcohol abuse
Find Substance Abuse Treatment At Bedrock Recovery Center
If you or a loved one is seeking treatment for a substance use disorder (SUD), call our free hotline today to learn about the accredited rehab programs available at Bedrock.
Tension-type headache - treatment, symptoms, causes, diagnosis
Tension-type headache is usually diffuse, mild to moderate in intensity, and is often described as a feeling of a "tight band" around the head. Tension-type headache (THT) is the most common type of headache, and yet the causes of this type of headache are still not well understood.
The treatment of tension headache is quite effective. Tension-type headache management is often a balance between a healthy lifestyle, the use of non-drug treatments, and the administration of adequate medication.
Symptoms
Symptoms of tension headache include:
- Dull, aching headache
- Feeling of "tightness" or pressure in the forehead or on the sides of the head and in the back of the head
- Soreness of the scalp, neck and shoulder muscles
Tension headaches fall into two main categories - episodic and chronic.
Episodic tension headaches
Episodic tension headaches can last from 30 minutes to a week. Episodic tension headaches occur on less than 15 days per month for at least three months. Frequent episodic tension headaches can become chronic.
Episodic tension headaches occur on less than 15 days per month for at least three months. Frequent episodic tension headaches can become chronic.
Chronic tension headaches
This type of tension headache lasts several hours and may be continuous. If headaches occur 15 days or more per month for at least three months, they are considered chronic.
Tension headaches and migraine
Tension headaches are sometimes difficult to distinguish from migraines. In addition, if a patient has frequent episodic tension-type headaches, they may also have migraines.
Unlike some forms of migraine, tension headaches are usually not accompanied by blurred vision, nausea, or vomiting. And if, with migraine, physical activity increases the intensity of the headache, then with a headache, stress loads do not have such an effect. Hypersensitivity to any light or sound can sometimes occur with tension headaches, but these symptoms are uncommon.
Causes
Causes of tension headache are not known. Medical experts believed that tension headaches are due to problems in the muscles of the face, neck and scalp, which in turn are due to strong emotions, excessive workload or stress. But studies show that muscle spasm is not the cause of this type of headache.
Medical experts believed that tension headaches are due to problems in the muscles of the face, neck and scalp, which in turn are due to strong emotions, excessive workload or stress. But studies show that muscle spasm is not the cause of this type of headache.
The most common theories are that people who have tension headaches and may have stress sensitivity are hypersensitive to pain. An increase in muscle soreness, which is a common symptom of tension-type headache, may be the result of an increase in general pain sensitivity.
Triggers
Stress is the most common trigger that causes tension headaches.
Risk factors
Risk factors for tension headache include:
- Gender. Women are more likely to get this type of headache. One study found that almost 90 percent of women and 70 percent of men experience tension headaches during their lifetime.
- Mean patient age. The frequency of tension-type headaches peaks at age 40, although this headache can develop at any age.
Complications
Due to the fact that headaches can be quite frequent, this can significantly affect productivity and quality of life in general, especially if they become chronic. Frequent pain can disrupt the usual way of life and overall performance.
Diagnosis
Diagnosis of tension-type headache is primarily based on clinical history and symptoms and neurological findings.
Physicians may be interested in answers to the following questions:
- When did the symptoms start?
- Did the patient notice any triggers such as stress or hunger?
- Were the symptoms continuous or episodic?
- How severe are the symptoms?
- How often do headaches occur?
- How long did you have a headache for the last time?
- What does the patient think reduces symptoms and what makes symptoms worse?
In addition, the doctor is also interested in the following details:
- Characteristics of pain.
 Does the pain throb? Is the pain dull, constant, or sharp?
Does the pain throb? Is the pain dull, constant, or sharp? - Pain intensity. A good indicator of headache severity is the amount of time a patient can work during a headache attack. Can the patient work? Are there episodes in which the headache led to awakening from sleep or sleep disturbance?
- Localization of pain. Does the patient feel pain in the whole head, only on one side of the head, or just in the forehead or eye sockets?
Instrumental methods of examination
If the patient has unusual or severe headaches, the doctor may order an additional examination to rule out more serious causes of headaches.
The two most commonly used diagnostic methods, such as CT (computed tomography) and MRI, allow visualization of organs and tissues and detect morphological changes.
Treatment
Some patients with tension-type headache do not go to the doctor and try to treat the pain themselves. Unfortunately, repeated self-use of painkillers can itself cause severe headaches.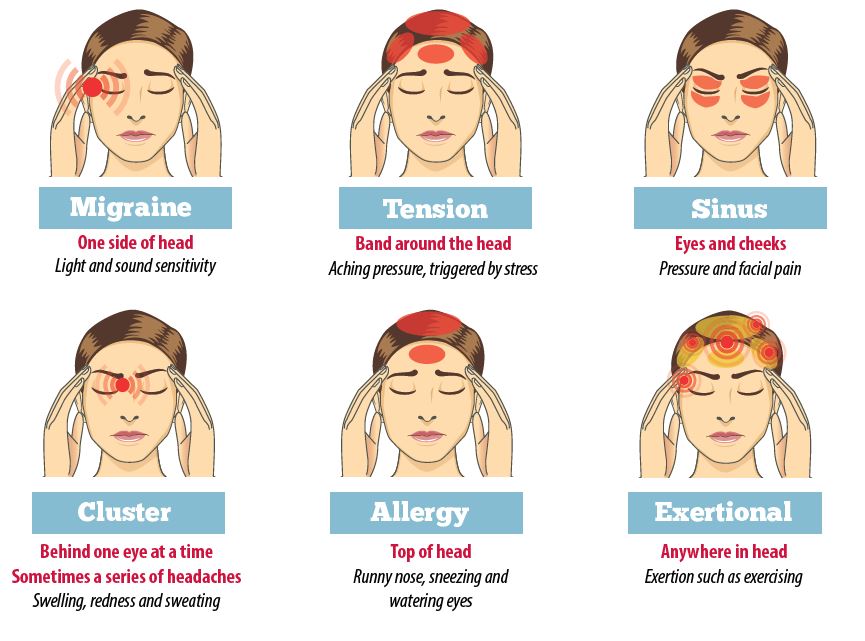
Medications
There is a wide variety of medicines, including over-the-counter medicines, to relieve pain, including:
- Painkillers. Simple over-the-counter pain relievers are usually the first line of treatment for headaches. These include aspirin, ibuprofen (Advil, Motrin IB, others), and naproxen (Aleve). Prescription drugs include naproxen (Naprosyn), indomethacin (Indocin), and ketorolac (ketorolac tromethamine).
- Combination preparations. Aspirin or acetaminophen, or both, often combined with caffeine or a sedative in the same medication. Combination preparations may be more effective than single-drug preparations.
- Triptans and drugs. For people who have both migraine and tension headaches, triptans can effectively relieve the headache. Opioids, or narcotics, are rarely used because of their side effects and the high risk of addiction.
Preventive drugs
Other drugs may be prescribed to reduce the frequency and severity of attacks, especially if the patient has frequent or chronic headaches that are not relieved by pain medication.
Prophylactic drugs may include:
- Tricyclic antidepressants. Tricyclic antidepressants, including amitriptyline and nortriptyline (Pamelor), are the most commonly used drugs for preventing tension-type headache. Side effects of these drugs may include weight gain, drowsiness, and dry mouth.
- Other antidepressants. There is evidence that antidepressants such as venlafaxine (Effexor XR) and mirtazapine (Remeron) are effective in patients who are also not depressed.
- Anticonvulsants and muscle relaxants. Other drugs that may prevent tension headaches from developing are anticonvulsants such as topiramate (Topamax) and muscle relaxants.
Lifestyle adjustments and home remedies
Rest, ice packs or long, hot showers can often relieve headaches.
Non-drug treatment
- Acupuncture. Acupuncture can provide temporary relief from chronic tension headache.
- Massage.
 Massage can help reduce stress and release tension. It is especially effective in relieving muscle spasm in the back of the head, neck, and shoulders.
Massage can help reduce stress and release tension. It is especially effective in relieving muscle spasm in the back of the head, neck, and shoulders. - Deep breathing, biofeedback and behavioral therapy. A variety of relaxation treatments are very helpful for tension headaches, including deep breathing and biofeedback.
Treatment of tension headache in Moscow in the Department of Neurology of the IAKI Clinic
Tension-type headache (THT) is one of the most common forms of primary headache, manifested by pain episodes lasting from 30 minutes to several days.
Attention!
Headache is an indicator of a range of different problems, from minor to serious (such as a brain tumor).
INSTITUTE OF ALLERGOLOGY AND CLINICAL IMMUNOLOGY has:
- range of services for accurate diagnosis of diseases
- special treatment programs
- courses of effective procedures conducted by specialists of our institute for more than 10 years
- consultations are carried out by doctors with academic degrees.
When concomitant diseases are identified, consultations are held with specialists from related fields (otorhinolaryngologists, endocrinologists, neurologists, gastroenterologists, dermatovenereologists), consultations from Doctors of Medicine.
Symptoms
Attention!
Self-medication and abuse of painkillers can lead to a chronic process!
- Headaches lasting from 30 minutes to 7 days.
- Pattern of pain in the form of a "hoop" or "helmet".
- At least two of the following:
- double-sided localization
- pressing/compressive/non-pulsating character
- light or moderate intensity
- pain is not aggravated by normal physical activity (walking, climbing stairs)
- Both of the following:
- no nausea or vomiting (anorexia may appear)
- only one of the symptoms: photo- or phonophobia (rarely develop simultaneously)
- Relief of pain with positive emotions and in a state of psychological relaxation; amplification against the background of emotional experiences.
- Soreness and tension in the muscles of the neck and occiput.
- Increased anxiety, labile mood background, poor night sleep quality, apathy or irritability.
Tension headache in ICD 10 headache classification
- G 44.0 Histamine headache syndrome
- Chronic paroxysmal hemicrania
- "Histamine" headache: chronic. episodic
- G 44.1 Vascular headache, not elsewhere classified
- Vascular headache NOS
- G 44.2 Tension headache
- Chronic tension headache
- Episodic tension headache
- Tension headache NOS
- G44.3 Chronic post-traumatic headache
- G44.4 Headache due to medication, not elsewhere classified
- G44.8 Other specified headache syndrome
Causes
Attention!
Self-medication and abuse of painkillers can lead to a chronic process!
The pathogenesis of tension-type headache is still unclear.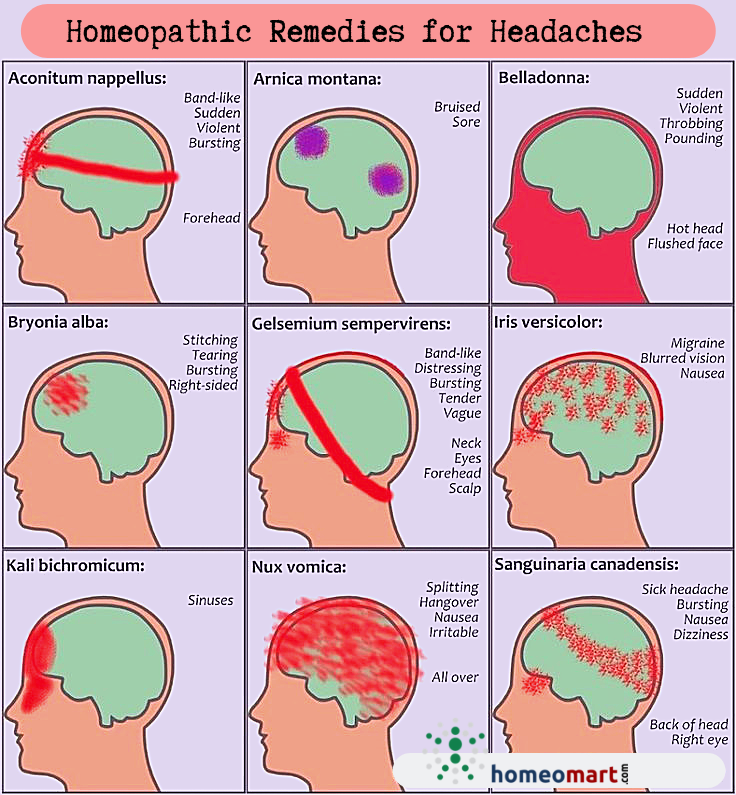 However, the factors that cause it are identified:
However, the factors that cause it are identified:
- Psychogenic factor (anxiety, stress).
- Misuse of painkillers.
- Muscle tension
- Emotional stress and psychiatric disorders (depression and anxiety that maintain muscle tension, leading to persistence (return) of pain).
Diagnostics
As a rule, establishing a diagnosis of tension-type headache is not difficult, but confirming the diagnosis is a time-consuming process. To do this, it is necessary to conduct a series of diagnostic studies that allow not only to confirm the disease, but also to find out the degree of its severity, as well as the main cause, which qualitatively improves the further treatment of the patient. Diagnostic measures are also necessary for differential diagnosis, exclusion of other diseases that have a similar picture of headache.
Treatment
In the treatment of tension headache, an integrated approach is used:
- Stabilization of the emotional state of the patient.
- Elimination of pericranial muscle dysfunction.
- Prevention of drug abuse (a form of chronic daily headache, usually occurring as a complication of a pre-existing primary headache (migraine or tension-type headache) as a result of regular or frequent use of analgesics, non-steroidal anti-inflammatory drugs, and other drugs)
The task of such treatment is to reduce pain and muscle-tonic syndrome, to prevent the transformation of episodic tension headache into a chronic headache.
For this, drug and non-drug methods of treating tension headaches are used, such as acupuncture, manual therapy, massage, etc.
Attention!
Selection of drug therapy should be made individually, taking into account the severity of the course of the disease, the presence of concomitant diseases, the age of the patient and the risk of possible side effects.
Please do not self-medicate on the basis of Internet data!
Department phone: +7 (495) 695-56-95
Patient information block
Preventive measures
It is also important for the patient to follow some recommendations:
- Get at least 7 hours of sleep per night.