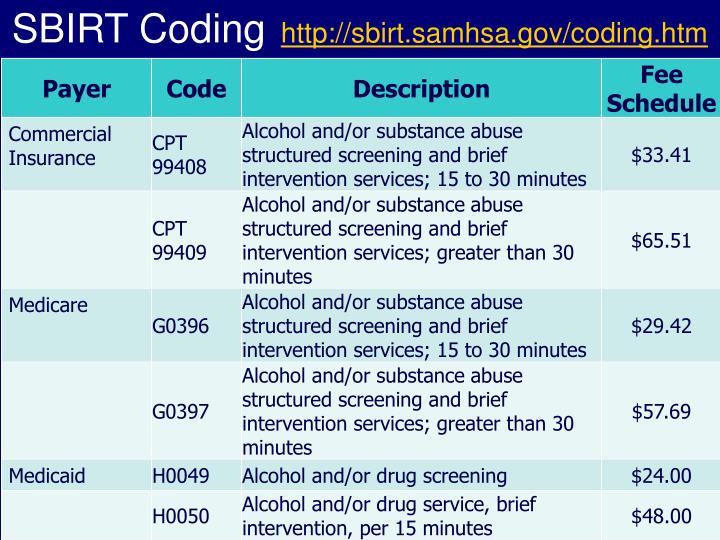
Billing codes for mental health services
Top CPT Codes for Mental Health Billing – My Clients Plus
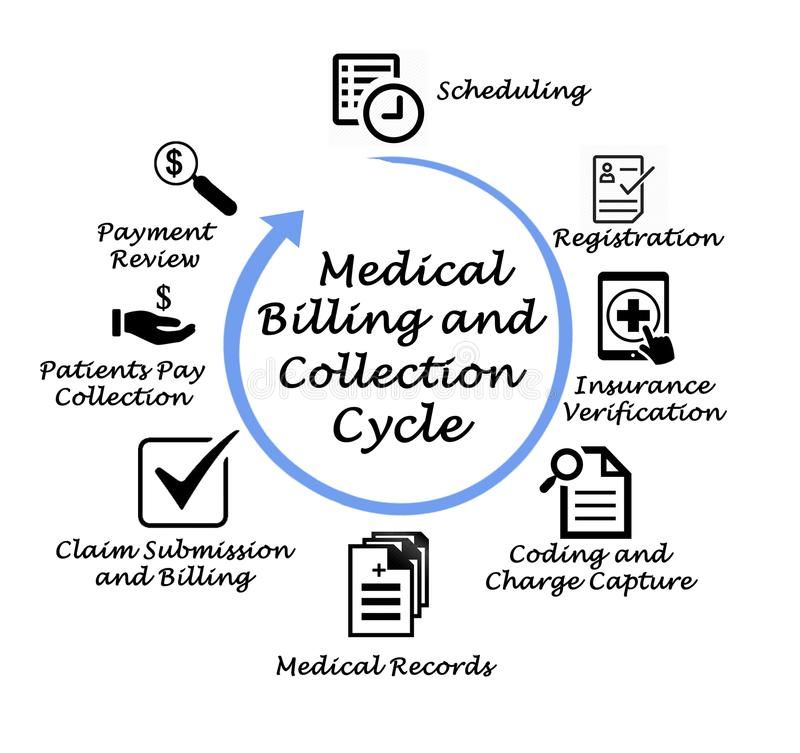
While precision in how you use CPT codes may not seem of utmost significance, in fact, using the correct CPT codes for the mental health services you provide is important for two major reasons. When your claims include the right codes, they’ll be accepted in a more timely manner, ensuring you have the necessary cash flow to operate your practice. Perhaps more urgently, coding mistakes could cause your practice to be audited, and errors could result in fines. In this post, we’ll cover what you need to know about using CPT codes and the most common codes you should become familiar with.
What are CPT Codes for Mental Health?
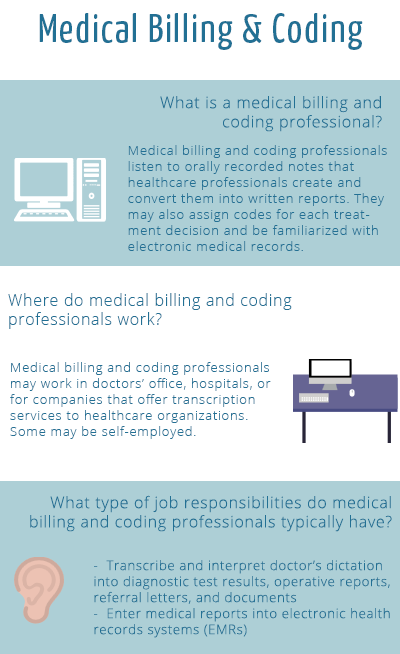
The Current Procedural Terminology (CPT) code set describes tests, evaluations, treatments, and other medical procedures used in the spectrum of healthcare. The set contains over 8,000 codes and is published and updated annually by the American Medical Association. It was created to track healthcare trends and issues as well to use in the claims submission process.
The codes communicate to payers what procedures you need to be reimbursed for as a provider.
The codes related to mental health (codes 90785-90899) are found in the Psychiatry section of the CPT code set and cover services provided by medical professionals, such as psychiatrists, as well as services that can be delivered by non-medical professionals such as licensed clinical psychologists, licensed professional counselors, licensed marriage and family therapists, and licensed clinical social workers.
Categories of Mental Health CPT Codes
The mental health CPT codes used by therapists are organized into four distinct categories. These categories make it easier to find the code you’re looking for.
Psychiatric Diagnostic Interview
- Code 90801: Psychiatric diagnostic interview examination
- Code 90802: Interactive psychiatric diagnostic interview examination
Psychiatric Therapeutic Services
- Codes 90804-90809: Insight-oriented, behavior modifying and/or supportive psychotherapy
- Codes 90810-90815: Interactive psychotherapy
Family Medical Psychotherapy
- 90846: Family psychotherapy (without the patient present)
- 90847: Family psychotherapy (with the patient present)
- 90849: Multiple-family group psychotherapy
Group Psychotherapy
- 90853: Group psychotherapy (other than a multiple-family group)
- 90857: Interactive group psychotherapy
Common Mental Health CPT Codes
While there are many codes that may be applicable to mental health services more broadly, in a therapy setting, you’ll probably find yourself using only a relatively small subset of these codes. Learning the most common CPT codes for mental health will help you choose the best code for each service you provide. Here are the most common codes that you’ll encounter as a therapist.
Learning the most common CPT codes for mental health will help you choose the best code for each service you provide. Here are the most common codes that you’ll encounter as a therapist.
90837 — Psychotherapy, 60 minutes
Description: Individual psychotherapy, 60 minutes, with client and/or family member.
Time: 60 minutes (functionally between 53 and 60 minutes)
90834 — Psychotherapy, 45 minutes
Description: Individual psychotherapy, 45 minutes, with client and/or family member.
Time: 45 minutes (functionally between 38 and 52 minutes)
90791 — Psychiatric diagnostic evaluation without medical services
Description: Initial diagnostic interview exam that does not include any medical services. Includes a chief complaint, history of present illness, family and psychosocial history, and complete mental status examination. (Use code 90792 for an initial evaluation with medical services.)
Time: Not time-based
90847 — Family psychotherapy (with client present), 50 minutes
Description: Family psychotherapy (conjoint psychotherapy) (with client present). (Can also be used for couples therapy.)
(Can also be used for couples therapy.)
Time: 50 minutes
90853 — Group psychotherapy (other than of a multiple-family group)
Description: Group psychotherapy (other than of a multiple-family group). Relies on the use of interactions of group members to examine the pathology of each individual within the group. The dynamics of the entire group are noted and used to modify behaviors and attitudes of the client members. (Used to report per-session services for each group member.)
Time: Not time-based
90846 – Family psychotherapy (without client present), 50 minutes
Description: Therapy session intended to aid the treatment of the client, where the family of a client is present without the client being present.
Time: 50 minutes
90875 – Under other psychiatric services or procedures
Description: Individual psychophysiological therapy incorporating biofeedback training by any modality (face-to-face with the client), with psychotherapy (e. g., insight-oriented, behavior modifying, or supportive psychotherapy).
g., insight-oriented, behavior modifying, or supportive psychotherapy).
Time: 20-30 minutes
90832 – Psychotherapy, 30 minutes
Description: Individual psychotherapy, 30 minutes
Time: 30 minutes (functionally between 16 – 37 mins)
90838 – Psychotherapy, 60 minutes, with E/M service
Description: Individual psychotherapy, 60 minutes with client and/or family member when performed with an evaluation and management (E/M) service.
Time: 60 minutes (functionally between 53 and 60 minutes)
99404 — Under preventive medicine, individual counseling services
Description: Preventive medicine counseling and/or risk factor reduction intervention(s) provided to an individual (separate procedure)
Time: 60 minutes (functionally between 53 and 60 minutes)
CPT Code Modifiers
Code modifiers provide additional information to a payer. Modifiers can describe the license level of provider, when services were provided, and how the services were provided, among other things.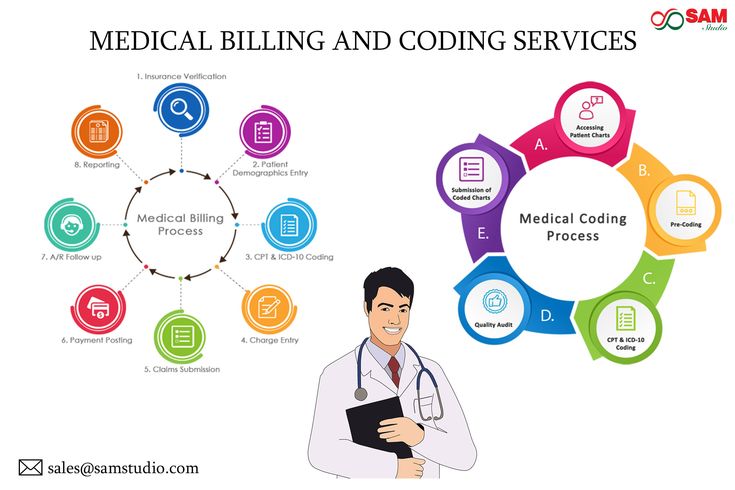 Here are four modifiers that you may encounter.
Here are four modifiers that you may encounter.
- Modifier 25 — Typically, a single code will accurately describe a session. But occasionally, you may find that a fully separate E/M service is needed (performed by the same provider) on the same day. Modifier 25 is used in these situations, as it calls out that service as separate and reimbursable. Note that you can only attach modifier 25 to codes 99201-99215, 99341-99350.
- Modifier 59 — Similar to modifier 25, this modifier is used to describe a distinct non-E/M procedural service done on the same day. Note that your documentation must support a separate session.
- Modifier GT — Used for telehealth sessions involving interactive audio and video.
- Modifier UT — Used when the provider sees a patient in crisis.
When you understand how CPT codes work and have a firm knowledge of the codes you’ll use most often in your therapy practice, you’ll increase your claims submission rate and reduce the likelihood of being flagged for inappropriate coding. Beyond the practicality of improving cash flow, accurate coding delivers peace of mind since you won’t have to worry about whether or not you’re using CPT codes correctly.
Beyond the practicality of improving cash flow, accurate coding delivers peace of mind since you won’t have to worry about whether or not you’re using CPT codes correctly.
Mental Health CPT Codes: The Definitive Guide [2022]
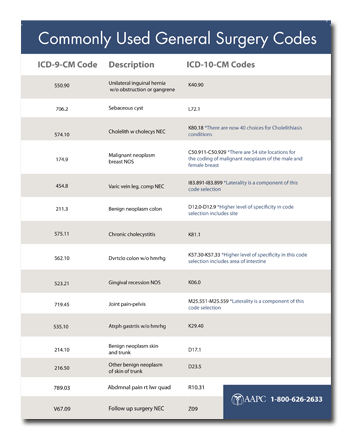
CPT (Current Procedural Terminology) is a standardized medical codeset maintained by the AMA. CPT codes are five digit numeric codes describing everything from surgery to radiology to psychotherapy.
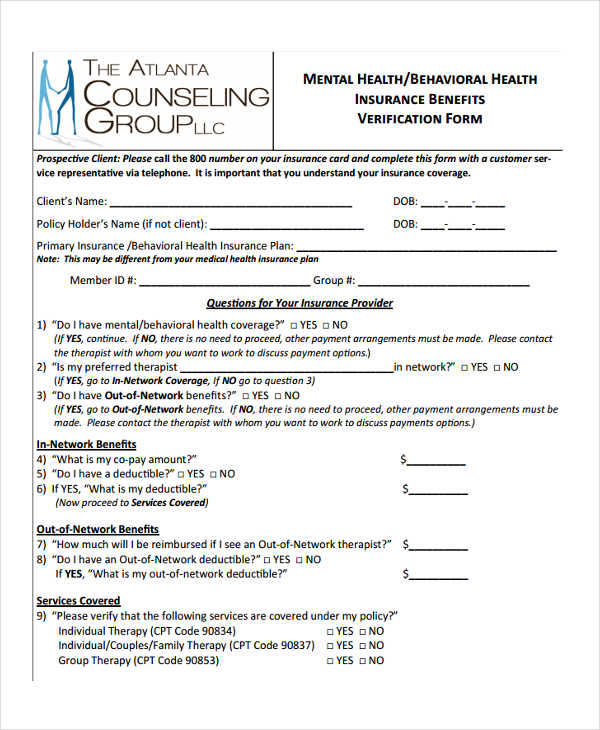
CPT Codes are different from Diagnosis Codes or ICD10 F-Codes for billing and coding your insurance claims. Here’s our mental health diagnosis code list if you need to look one up.
For therapists that are on managed care panels or provide superbills to their clients, knowing your CPT codes is paramount to getting paid in full and avoiding insurance audits.
The amount insurance companies will reimburse depends on a number of different factors (professional credentials, geographic location, etc.), but using the correct CPT Code and add-on code(s) to express the exact service is an important part to the whole process and in ultimately determining your payment!
Errors, accidental or otherwise, will directly impact insurance company’s payment of services. If you need help with making sure your billing and coding is error-free, our mental health billing service can help.
If you need help with making sure your billing and coding is error-free, our mental health billing service can help.
Think about reaching out if the rest of this article hurts your feelings.
Article Index:
- Most Common Mental Health CPT Codes
- Add-On CPT Codes for Mental Health Billing
- Mental Health CPT Code Cheat Sheet [PDF]
- Testing & Evaluation CPT Codes
- Psych and Evaluation and Management (E/M) Codes
- Sample Reimbursement Rates by License Type
- Sample Reimbursement Rates by CPT Code
The most common CPT Codes used by therapists and behavioral health professionals:
Outpatient Mental Health Therapist Diagnostics, Evaluation, Intake CPT Code:- 90791 – Psychiatric Diagnostic Evaluation (usually just one/client is covered)
- 90832 – Psychotherapy, 30 minutes (16-37 minutes).
- 90834 – Psychotherapy, 45 minutes (38-52 minutes).
- 90837 – Psychotherapy, 60 minutes (53 minutes and over).
- 90846 – Family or couples psychotherapy, without patient present.
- 90847 – Family or couples psychotherapy, with patient present.
- 90853 – Group Psychotherapy (not family).
- 98968 – Telephone therapy (non-psychiatrist) – limit 3 units/hours per application.
- 90839 – Psychotherapy for crisis, 60 minutes (30-74 minutes).
- +90840 – Add-on code for an additional 30 minutes (75 minutes and over). Used in conjunction with 90839.
- +90785 – Interactive Complexity add-on code. Covered below.
- 90404 – Cigna / MHN EAP CPT Code. These two companies use a unique CPT code for EAP sessions.
- 96101 – Psychological testing, interpretation and reporting by a psychologist (per Hour)
- 90880 – Hypnotherapy – limit 10 units/hours per application
- 90876 – Biofeedback
- 90849 – Multiple family group psychotherapy
- 90845 – Psychoanalysis
Mental Health Add-On CPT Codes
Here is a short list of the most common Add-On codes for routine outpatient mental health billing.
- Add-On CPT Code 90785 – Interactive complexity. Example: play therapy using dolls or other toys. This is an interactive complexity add-on code that is not a payable expense. This code only indicates that the treatment is complex in nature.
- Add-On CPT Code 90863 – Pharmacologic Management after therapy.
- Add-On CPT Code 99050 – Services provided in the office at times other than regularly scheduled office hours, or days when the office is normally closed.
- Add-On CPT Code 99051 – Services provided in the office during regularly scheduled evening, weekend, or holiday office hours.

- Add-On CPT Code 99354 – Additional time after the additional time of 74 minutes. Adding another 30 minutes. (Only use if the duration of your session is at least 90 minutes for 90837 or 80 minutes for 90847).
- Add-On CPT Code 99355 – Additional time after first 60 minutes. First additional 30 to 74 minutes.
- Add-On CPT Code 90840 – 30 additional minutes of psychotherapy for crisis. Used only in conjunction with CPT 90839.
- Add-On CPT Code 90833 – 30 minute psychotherapy add-on. Example: Psychiatrist evaluates medication response, then has 30 minute session.
- Add-On CPT Code 90836 – 45 minute psychotherapy add-on. Example: Clinical Nurse Specialist evaluates medication response, then has 45 minute session.
If you’re wondering how to handle billing add-on codes, we can help make this process simple and automatic. Learn how we can help by inquiring about our billing service.
- 90792 – Psychiatric Diagnostic Evaluation with medical services (usually just one/client is covered)
- 99201 – E/M – New Patient Office Visit – 10 Minutes
- 99202 – E/M – New Patient Office Visit – 20 Minutes
- 99203 – E/M – New Patient Office Visit – 30 Minutes
- 99204 – E/M – New Patient Office Visit – 45 Minutes
- 99205 – E/M – New Patient Office Visit – 60 Minutes
- 99211 – E/M – Established Patients – 5 Minutes
- 99212 – E/M – Established Patients – 10 Minutes
- 99213 – E/M – Established Patients – 15 Minutes
- 99214 – E/M – Established Patients – 25 Minutes
- 99215 – E/M – Established Patients – 40 Minutes
- 99443 – Telephone therapy (psychiatrist), – limit 3 units/hours per application
Mental Health CPT Code Cheat Sheet
Download a copy of our PDF Behavioral Health CPT Code Cheat Sheet!
CPT Coding for TherapyCPT coding for psychotherapy doesn’t have to be difficult! There are an overwhelming amount of total CPT Codes (~8,000), however only 24 are specifically designated for psychotherapy and other mental health services.
To make matters even simpler, nearly all therapists will regularly use an even smaller subset of these 24.
CPT is a large and dynamic code set that changes year to year, but the psychotherapy codes seldom change.
The most recent change for psychotherapy codes took place in 2019, then 2013, and previously 1998.
To ensure your coding is current and up to date, consider using a billing service instead of having to remember all the codes.
Behavioral Health CPT Add-On Codes
A CPT Add-on Code is a code describing a service performed in in conjunction with a primary service. Many of these add-on codes are associated with a specific CPT Code or a small set of CPT Codes and cannot be used otherwise.
For instance, the behavioral health CPT Code for interactive complexity (+90785) can be used for a diagnostic (90791, 90792) or a normal psychotherapy session (90832, 90834, 90837) but not a crisis psychotherapy session (90839).
Add-on Codes are identified by a + sign in front of the number, i. e. +90840 is an add-on code for extra time in the case of crisis psychotherapy.
e. +90840 is an add-on code for extra time in the case of crisis psychotherapy.
On CMS 1500 forms CPT Add-on codes are simply added on a new line.
Add-on codes are extremely important to use in order to most accurately describe the services being rendered and to ensure your services are maximized per session.
We help the mental health providers that work with us in our billing service do all of this for every appointment.
Mental Health Testing CPT Codes [2020]
These codes are only effective January 1st, 2019.
Assessment of Aphasia and Cognitive Performance Testing CPT Codes
CPT Code 96105
Assessment of aphasia (includes assessment of expressive and receptive speech and language function, language comprehension, speech production ability, reading, spelling, writing, e.g., by Boston Diagnostic Aphasia Examination) with interpretation and report, per hour
CPT Code 96125
Standardized cognitive performance testing (e. g., Ross Information Processing Assessment) per hour of a qualified health care professional’s time, both face-to-face time administering tests to the patient and time interpreting these test results and preparing the report
g., Ross Information Processing Assessment) per hour of a qualified health care professional’s time, both face-to-face time administering tests to the patient and time interpreting these test results and preparing the report
Developmental/Behavioral Screening and Testing
CPT Code 96110
Developmental screening (e.g., developmental milestone survey, speech and language delay screen), with scoring and documentation, per standardized instrument
CPT Code 96112
Developmental test administration (including assessment of fine and/or gross motor, language, cognitive level, social, memory, and/ or executive functions by standardized developmental instruments when performed), by physician or other qualified health care professional, with interpretation and report; first hour
Add-on CPT Code + 96113 – Each additional 30 minutes (List separately in addition to code for primary procedure)
CPT Code 96127
Brief emotional/behavioral assessment (e.g. , depression inventory, attention-deficit/hyperactivity disorder [ADHD] scale), with scoring and documentation, per standardized instrument
, depression inventory, attention-deficit/hyperactivity disorder [ADHD] scale), with scoring and documentation, per standardized instrument
Psychological/Neuropsychological Testing CPT Codes
These codes have changed in 2019.
Neurobehavioral Status Exam CPT Codes
CPT Code 96116
Neurobehavioral status exam (clinical assessment of thinking, reasoning and judgement, e.g., acquired knowledge, attention, language, memory, planning and problem solving, and visual spatial abilities), by physician or other qualified health care professional, both faceto-face time with the patient and time interpreting test results and preparing the report; first hour
Add-on CPT Code +96121 – Each additional hour (List separately in addition to code for primary procedure)
Test Evaluation Services CPT Codes
CPT Code 96130
Psychological testing evaluation services by physician or other qualified health care professional, including integration of patient data, interpretation of standardized test results and clinical data, clinical decision making, treatment planning and report and interactive feedback to the patient, family member(s) or caregiver(s), when performed; first hour
Add-on CPT Code +96131 – Each additional hour (List separately in addition to code for primary procedure)
CPT Code 96132
Neuropsychological testing evaluation services by physician or other qualified health care professional, including integration of patient data, interpretation of standardized test results and clinical data, clinical decision making, treatment planning and report and interactive feedback to the patient, family member(s) or caregiver(s), when performed; first hour
Add-on CPT Code +96133 – Each additional hour (List separately in addition to code for primary procedure)
Test Administration and Scoring CPT Codes
CPT Code 96136
Psychological or neuropsychological test administration and scoring by physician or other qualified health care professional, two or more tests, any method, first 30 minutes
Add-on CPT Code +96137 – Each additional 30 minutes (List separately in addition to code for primary procedure)
CPT Code 96138
Psychological or neuropsychological test administration and scoring by technician, two or more tests, any method; first 30 minutes
Add-on CPT Code +96139 – Each additional 30 minutes (List separately in addition to code for primary procedure)
Automated Testing and Result CPT Codes
96146 – Psychological or neuropsychological test administration, with single automated instrument via electronic platform, with automated result only
Mental Health Evaluation & Management (E/M) Codes
There are also E/M (evaluation & management) in conjunction with psychotherapy, used by authorized prescribers, psychiatrists, and MDs.
Coding E/M is trickier, harder to document and more vulnerable to audit but usually results in greater reimbursement.
There’s also a series of E/M codes that are used without the psychotherapy component.
For more in-depth coverage on E/M coding for psychotherapy there are some good free webinars released by AACAP on E/M CPT Codes.
- Add-on CPT Code +90833 – E/M code for 30 minutes of psychiatry (used with 90832).
- Add-on CPT Code +90836 – E/M code for 45 minutes of psychiatry (used with 90834).
- Add-on CPT Code +90838 – E/M code for 60 minutes of psychotherapy (used with 90837).
- Psychotherapy must be at least 16 minutes.
- Time is very important and should be rounded to the nearest CPT Code.
- Outpatient vs. Inpatient is not important.
- E/M codes can only be used by prescribers (MD, DO, APN, PA).
Medicare 2022 Reimbursement Rates by CPT Code
| CPT Code | Description | Medicare Reimbursement Rate 2020 | Medicare Reimbursement Rate 2021 | Medicare Reimbursement Rate 2022 |
|---|---|---|---|---|
| 90791 | Psychological Diagnostic Evaluation | $140.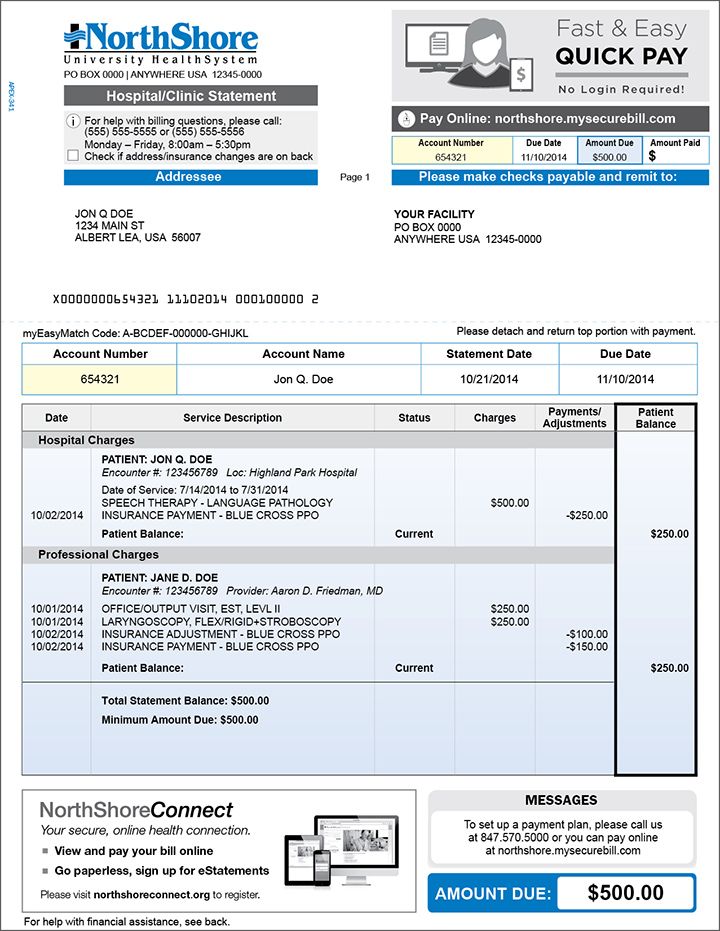 19 19 | $180.75 | $195.46 |
| 90792 | Psychological Diagnostic Evaluation with Medication Management | $157.49 | $201.68 | $218.90 |
| 90832 | Individual Psychotherapy, 30 Minutes | $68.47 | $77.81 | $85.07 |
| 90833 | Individual Psychotherapy with Evaluation and Management Services, 30 minutes | $71.00 | $71.18 | $77.88 |
| 90834 | Individual Psychotherapy, 45 Minutes | $91.18 | $103.28 | $112.29 |
| 90836 | Individual Psychotherapy with Evaluation and Management Services, 45 minutes | $89.74 | $90.02 | $98.30 |
| 90837 | Individual Psychotherapy, 60 Minutes | $136.95 | $152.48 | $164.84 |
| 90838 | Individual Psychotherapy with Evaluation and Management Services, 60 minutes | $118.57 | $119.33 | $129.30 |
| 90839 | Individual Crisis Psychotherapy initial 60 min | $157. 66 66 | ||
| 90840 | Individual Crisis Psychotherapy initial 60 min, each additional 30 min | $78.64 | ||
| 99201 | Evaluation and Management Services, Outpatient, New Patient | $46.49 | Not Covered | Not covered |
| 99202 | Evaluation and Management Services, Outpatient, New Patient | $77.48 | $73.97 | $80.91 |
| 99203 | Evaluation and Management Services, Outpatient, New Patient | $109.92 | $113.75 | $124.39 |
| 99204 | Evaluation and Management Services, Outpatient, New Patient | $166.86 | $169.93 | $185.26 |
| 99205 | Evaluation and Management Services, Outpatient, New Patient | $209.75 | $224.36 | $244.99 |
| 99211 | Evaluation and Management Services, Outpatient, Established Patient | $23.07 | $23.03 | $25.71 |
| 99212 | Evaluation and Management Services, Outpatient, Established Patient | $45. 77 77 | $56.88 | $62.76 |
| 99213 | Evaluation and Management Services, Outpatient, Established Patient | $75.32 | $92.47 | $100.57 |
| 99214 | Evaluation and Management Services, Outpatient, Established Patient | $110.28 | $131.20 | $141.78 |
| 99215 | Evaluation and Management Services, Outpatient, Established Patient | $147.76 | $183.19 | $200.00 |
| 99354 | Prolonged Services | $132.26 | $132.09 | $140.26 |
| 99355 | Prolong Services with E/M | $100.91 | $100.33 | $101.32 |
| 90846 | Family psychotherapy without patient, 50 minutes | $103.58 | $99.10 | $107.37 |
| 90847 | Family psychotherapy with patient, 50 minutes | $107.19 | $102.59 | $111.15 |
| 96105 | Assessment of aphasia and cognitive performance | $101. 54 54 | $109.26 | |
| 96112 | Developmental testing administration by a physician or qualified health care professional, 1st hr | $131.55 | $141.02 | |
| 96113 | Developmental testing administration by a physician or qualified health care professional, each additional hour | $58.62 | $66.54 | |
| 96116 | Neurobehavioral status exam performed by a physician or qualified health professional, first hour | $97.00 | $104.73 | |
| 96121 | Neurobehavioral status exam performed by a physician or qualified health professional, additional hour | $82.35 | $87.34 | |
| 96125 | Standardized cognitive performance test administered by health care professional | $107.12 | $115.69 | |
| 96127 | Brief emotional and behavioral assessment | $4.89 | $5.29 | |
| 96130 | Psychological testing and evaluation by a physician or qualified health care professional, first hour | $120. 73 73 | $132.70 | |
| 96131 | Psychological testing and evaluation by a physician or qualified health care professional, each additional hour | $91.42 | $98.68 | |
| 96132 | Neuropsychological testing and evaluation by a physician or qualified health care professional, first hour | $133.29 | $144.80 | |
| 96133 | Neuropsychological testing and evaluation by a physician or qualified health care professional, each additional hour | $103.98 | $112.29 | |
| 96136 | Neuropsychological or psychological test administration and scoring by a physician or qualified health care professional, first hour | $46.76 | $49.15 | |
| 96137 | Neuropsychological or psychological test administration and scoring by a physician or qualified health care professional, each additional hour | $41.87 | $44.24 | |
| 96138 | Neuropsychological or psychological test administration and scoring by a technician, first hour | $37. 34 34 | $38.56 | |
| 96139 | Neuropsychological or psychological test administration and scoring by a technician, each additional hour | $37.34 | $$39.32 |
(Source)
Interactive Complexity (+90785): Criteria and How to Bill+90785 is one of the new add-on codes in the most recent CPT update in 2013.
This code is used as an umbrella add-on code and can be used for four different criteria. The most common scenarios usually involve children, although this is not necessarily always the case.
Common Examples of Interactive Complexity:
- The use of play equipment with young children.
- Interpreters/translators.
- Involvement of parents with discordant views that complicate the treatment plan.
- Report of abuse/neglect.
Interactive complexity can be used in conjunction with the primary CPT Codes for diagnostics, psychotherapy, or group therapy and cannot be used for couple/family therapy or crisis codes.
+90785, can be used with: 90791, 90792, 90832, 90833, 90834, 90836, 90837, 90838, 90853.
Unsure when to use the interactive complexity code? Need help asking if it will be approved? Our billing service exclusively for mental health providers is here to help.
Am I Being Underpaid? Was I Paid the Right Amount?Here’s typical rates depending on the therapist’s credentials:
Typical Reimbursements by Type of Therapist| Type of Therapist | Reimbursement/Session |
| Social Workers | ~$55-60 |
| Marriage Family Therapists | ~$60-65 |
| Counselors | ~$60-65 |
| Psychologists | ~$70-80 |
These rates can vary significantly therapist to therapist but are good benchmarks for comparison.
How about CPT Codes? How do they affect the rate of reimbursement? This is a difficult and complex calculation, depending on the level of education, location, and license. The AMA has created a code search feature on their website that shows payment based off CPT Code and location.
The AMA has created a code search feature on their website that shows payment based off CPT Code and location.
This information is somewhat incomplete and is based off medicare payments and does not specify a number of other important factors. However, this tool is still very useful to compare the relative value CPT Codes against one another.
Private insurance will be correlated with some deviation from these numbers.
Reimbursement by CPT Code (Three Different Geographies)Reimbursement (Rest of CA)Reimbursement (Los Angeles)Reimbursement (WA)
| Code | California | Los Angeles | Washington |
| 90791 | $137.10 | $141.17 | $132.98 |
| 90792 | $147.84 | $152.16 | $143.39 |
| 90832 | $66.14 | $68.03 | $64.25 |
| +90833 | $67.69 | $69.69 | $65.70 |
| 90834 | $87.66 | $90.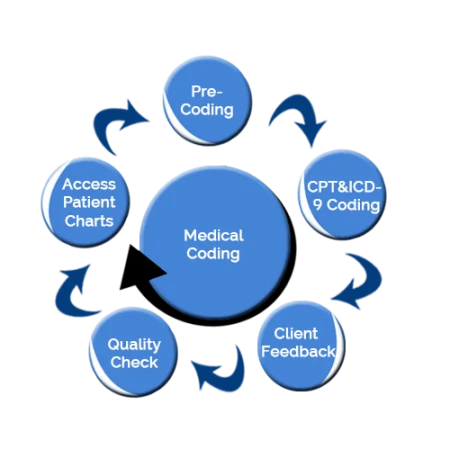 15 15 | $85.18 |
| +90836 | $85.71 | $88.21 | $83.18 |
| 90837 | $131.28 | $134.95 | $127.54 |
| +90838 | $113.07 | $116.42 | $109.75 |
| 90846 | $106.46 | $109.51 | $103.38 |
| 90847 | $109.75 | $112.82 | $106.60 |
| 90853 | $26.99 | $27.83 | $26.21 |
| 90839 | $137.22 | $141.04 | $133.28 |
| +90840 | $65.75 | $67.61 | $63.89 |
| +90785 | $14.67 | $15.08 | $14.24 |
Data from AMA Codemanager. These numbers are useful for relative comparison of individual CPT Codes and geography.
Therapist Reimbursement Rates for 2022
Read our definitive guide with 2022 reimbursement rates for mental health CPT codes.
Downcoding Claims
Downcoding (including less services on the claim than actually provided) will usually mean you get paid less, while upcoding (including more services on the claim than actually provided) can get you in trouble with your managed care panels.
It’s also important to note that it might be tempting to maximize your CPT codes to earn higher reimbursements.
This is highly recommended against and can get you flagged, audited and removed from insurance panels. Even if this is your biller’s error, the therapist is the one who ultimately bears the responsibility and will be the one penalized.
Here’s a video guide we did of this article!
Distilled Guide to Mental Health CPT Codes
If you are just starting out or just beginning to deal with managed care, keep it simple.
CPT Codes appear far more complex from the outside looking in. Make a quick cheatsheet.
Don’t worry about memorizing all the CPT Codes (there’s alot!) or even all of the mental health ones. You will likely just use just a few individual codes.
Memorize the relevant codes and use google or other references to find the correct CPT codes for more unique scenarios.
Call to verify eligibility and benefits and make sure those codes will be approved with that client’s coverage.
And if all of that sounds like too much trouble, offload the work to us. You won’t have to know one CPT code from another to get your billing paid in full.
Additional Resources- Medicare Reimbursement by CPT Code & Area
- CPT Reimbursement Lookup & RVU (Relative Value Unit) Overview
- Crosswalk of 2012 to 2013 CPT Codes
- CPT 2013 Standard Edition [Probably Unnecessary]
- Insurance Reimbursement Comparison Tool
Consider Outsourcing Your Billing
Don’t want to learn any of this stuff? We are your team of billing experts here to translate all of this gibberish into English! Reach out about our billing service if you are a licensed mental health provider (we only work with licensed mental health providers).
202020212022behavioral health cpt codesmental health billing guidemental health cpt codesmental health cpt codes guidemost common mental health cpt codes
Billing and Rendering Taxonomy Requirements - Washington State Local Health Insurance - CHPW
Billing and Rendering Taxonomy Requirements - Washington State Local Health Insurance - CHPW
Submitted August 29, 2022 in Bulletin board by James Eng
CHPW would like to remind all clinics and providers that claims must include valid and appropriate taxonomy codes for the billing provider and, if applicable, the imaging provider.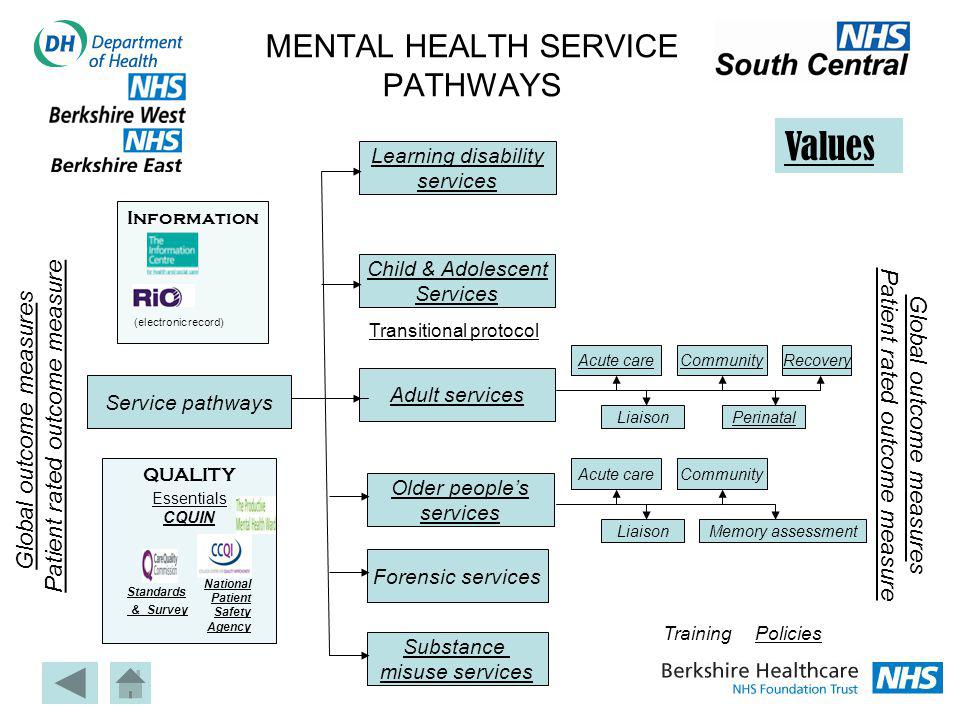
The CHPW Clearinghouse will reject any claims submitted without valid taxonomic billing and/or rendering codes and these claims will not be submitted to CHPW.
Requiring a custom service provider is only required for NPI/taxonomy billing at the billing level, because billing provider and rendering provider are the same. If your billing provider name is different from your rendering provider name, separate NPIs and taxonomies are required; in this case, billing and rendering cannot be the same taxonomy code.
Taxonomy Electronic Billing
- Billing taxonomy enters cycle 2000A, PRV*BI segment (paper claims: box 33b)
- NPI billing in cycle 2010AA segment NM1 * 85 (block 33a)
- Taxpayer Identification Number (TIN) included in cycle 2010AA, segment REF * EI (block 25)
- NPI rendering in cycle 2310B, segment NM1 * 82 (block 24j - bottom)
- For FQHC, if the render provider is different from the provider in loop 2310B, enter the taxonomy in loop 2420A.
- Render taxonomy included in loop 2310B, segment PRV * PE (box 24j - top)
See the Sample Electronic Claim and Sample Paper Claim sections at the end of this guide for a visual representation.
Continue reading for more information on taxonomy codes or visit https://taxonomy.nucc.org/ for other relevant taxonomies.
Tribal providers
Tribal providers must bill with the appropriate billing taxonomy. and the corresponding American Indian/Alaska Native (AI/AN) or non-AI/AN assigned tribe modifier.
Acceptable taxonomies for breeding providers
-
- Medical requirements: 208D00000X, 225100000X, 225X00000X, 235Z00000X, 152W00000X and 171M00000X
- Mental health claims: 2083P0901X
- Substance use disorder claims: 261QR0405X
- Residential wastewater treatment plant: 324500000x or 3245S0500x
Please refer to Tribal Health Billing Guidelines, https://www.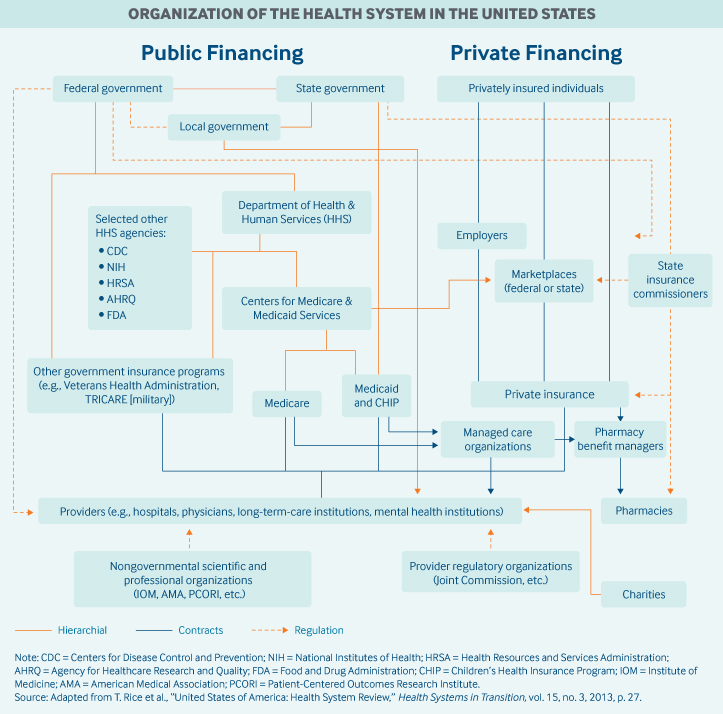 hca.wa.gov/billers-providers-partners/prior-authorization-claims-and-billing/provider-billing-guides-and- fee-schedules , more details.
hca.wa.gov/billers-providers-partners/prior-authorization-claims-and-billing/provider-billing-guides-and- fee-schedules , more details.
Behavioral Health Services
Change for CHPW plan/members for mental health services only (BHSO): For BHSO clients, the Washington State Health Authority (HCA) is responsible for paying for services that are considered lower level health care. Occupational mental health claims for these services must be made through ProviderOne. HCA will determine payment based on the following criteria:
- If the provider is a community mental health center, taxonomy 251S00000X or 261QM0801X, reimbursement is the responsibility of the managed care organization (MCO) and will be denied by the HCA by informing the provider of the MCO/BHSO billing.
- The following billing taxonomies indicate mental health services and are under the responsibility of the MCO/BHSO: 261QR0405X, 261QM2800X, 324500000X, 3245S0500X, 261QM3000X, 2083P0901X, 261QM0850X, 320800000X and 323PX00000.
- Taxonomy invoice 283Q00000X for psychiatric hospital must be billed to MCO/BHSO as changes in this update are for professional services only.
- Any other billing taxonomies HCA believes are intended to provide less acute services and will process and pay as medical claims rather than mental health claims, regardless of diagnosis. The HCA only considers the billing taxonomy.
- HCA will only pay for services that are billed as a fee-for-service; services that are not covered by service fees must be paid directly to the MCO, regardless of taxonomy.
- HCA updated mental health billing guidance regarding proper billing and use of taxonomies; please see https://www.hca.wa.gov/assets/billers-and-providers/mental-health-svcs-bg-20210901.pdf.
- HCA will escalate any future billing errors identified by vendors to HCA Program Integrity staff.
All mental health services must be billed under the appropriate billing taxonomy, including but not limited to those listed below.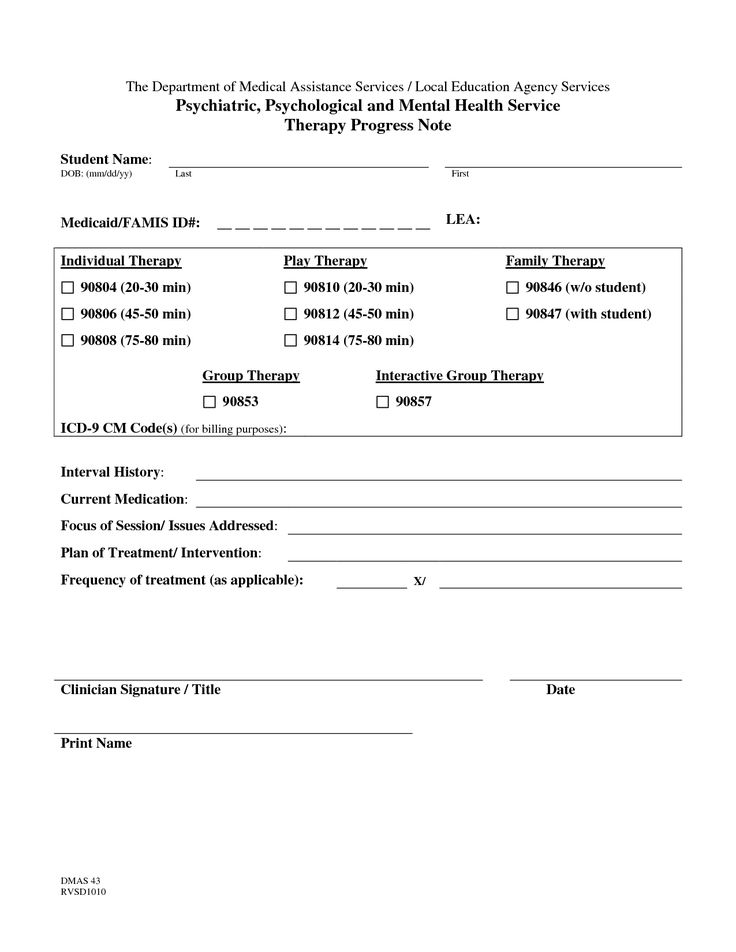
- Community Mental Health Centers: 251S00000X or 261QM0801X
- Mental Health Agencies (Billing Provider): 261QR0405X, 261QM2800X, 324500000X or 3245S0500X
- Rehabilitation (rehab) for substance use disorder (SUD): 261QR0405X
- Methadone Clinic / Centre: 261QM2800X
- Rehabilitation Center SUD: 324500000X
- Children's Rehabilitation Center SUD: 3245S0500X
Rural health clinics (RHC)
RHC services must be billed according to the RHC taxonomy in order to receive a service-based extension (SBE). As specified in HCA RHC Billing Guide :
How do I bill taxonomy codes for RHC?
-
- When billing for services that qualify for a match, HCA requires RHC to use billing taxonomy 261QR1300X at the claim level.
- A service taxonomy is also required.
- If the client or service is not eligible to meet with the RHC, the RHC may regularly bill as a non-RHC without HCPCS T1015 on the application.
Please refer to Rural Clinic Billing Guide for more information: https://www.hca.wa.gov/billers-providers-partners/prior-authorization-claims-and-billing/provider-billing-guides-and-fee-schedules.
Federally Certified Health Centers (FQHC)
It is recommended that CHPW comply with HCA billing requirements for FQHC. As stated in HCA Billing Guidelines for Federally Certified Health Centers (FQHC) :
How do I bill taxonomy codes for FQHC?
-
- When billing for services that qualify for a match, the HCA requires FQHCs to use billing taxonomy 261QF0400X at the claims level.
- A service taxonomy is also required.
See Taxonomy Electronic Bill above or see Billing Guide for Federally Certified Health Centers (FQHC) for more information: https://www.hca.wa.gov/billers-providers- partners/prior-authorization-claims-and-billing/provider-billing-guides-and-fee-schedules.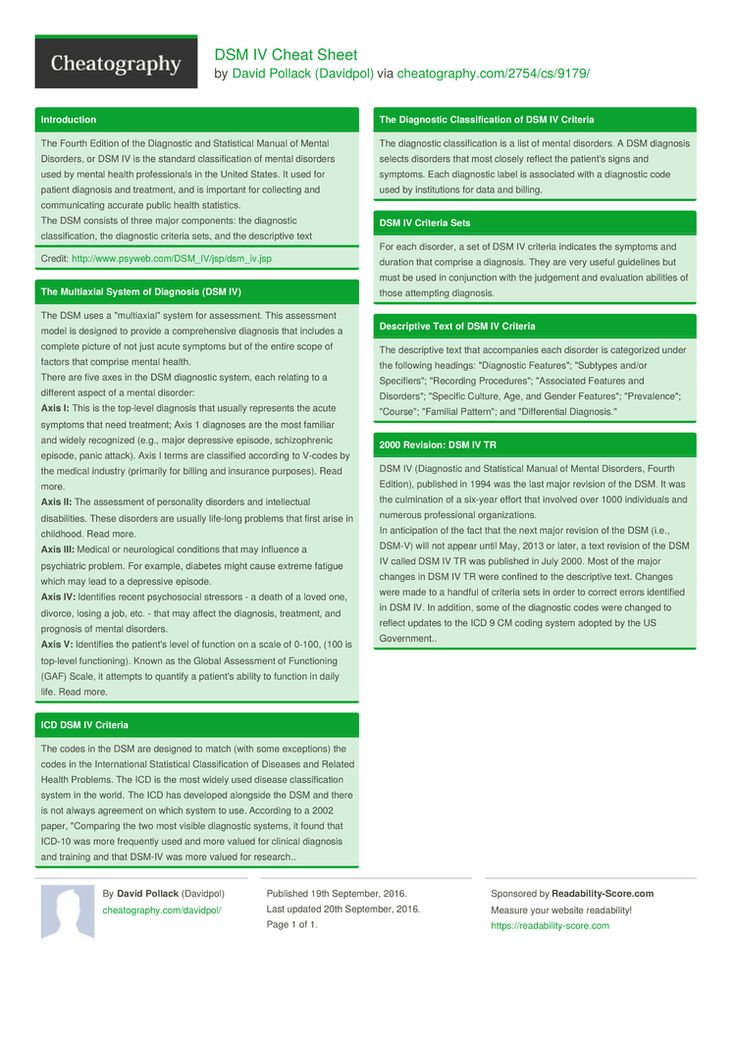
Taxonomy of Applied Behavior Analysis (ABA)
Applied Behavior Analysis (ABA) providers must use taxonomy number 103K00000X to bill for ABA therapy services to ensure that claims are properly paid. Providers must enter this taxonomy code in both the billing taxonomy fields and the service taxonomy fields on the CMS-1500 (HCFA) application form.
See NUCC Taxonomy Code Set Updates, https://taxonomy.nucc.org/ for more information.
E-Claim Example
In the e-Claim example below:
- PRV * BI segment is a billing provider taxonomy
- Segment NM1*85 - billing provider NPI
- REF * Segment EI is the tax identifier of the billing provider.
- NM1*82 segment - NPI rendering provider
- PRV * PE segment is a taxonomy of visualization service providers.
Sample paper claim
In the paper claim example below:
- Block 24j - at the top is the visualization provider taxonomy.

- Field 24j - Below is the NPI rendering provider.
- Field 25 is the taxpayer identification number of the payment system.
- Field 33a is the NPI billing provider.
- Box 33b is a billing provider taxonomy.
Billing Guides
See the HCA Billing Guides for precise organization and additional information. https://www.hca.wa.gov/billers-providers-partners/prior-authorization-claims-and-billing/provider-billing-guides-and-fee-schedules, including Tribal Health Billing Guide , Billing Guide for Federally Certified Health Centers (FQHC) , Billing Guide for Rural Clinics And more.
Questions?
If you have questions about the information in this bulletin, please contact EDI Support at [email protected]. Please include the claim number, member ID, date of service, and billing as this will assist in our investigation and clearinghouse opt-out resolution.
LEARN MORE ABOUT US
[random_content group_id = '25' num_posts = '1']- CUSTOMER SERVICE
- 1-800-440-1561
- (TTY relay: Dial 711)
- [email protected]
- NURSE CONSULTATION LINE
- (CHPW members)
- 1-866-418-2920
- (TTY relay: Dial 711)
- CASE MANAGEMENT
TECHNICAL SUPPORT - (CHPW members)
- 1-866-418-7004
- (TTY relay: Dial 711)
- ADDRESS
- 1111 Third Ave.
- Lux 400
- Seattle, Washington 98101
- WATCH
- 8:00 am to 5:00 pm
- Monday to Friday
- ADDRESS
- 1111 Third Ave.
- Lux 400
- Seattle, Washington 98101
QUICK LINKS
- Members
- Benefits +
- Print membership card
- myCHPW portal
- Plan and cover
- Find Doctor
- Behavioral Health Resources
- PLANS
- Apple Health (Medicaid)
- Medicare Benefits
- Double Right (SNP)
- Individual and family
- Plan Benefits
- Registration
- SUPPLIERS
- Previous resolution
- Provider Portals
- Molds and tools
- Bulletin Board
- Eligibility
- Mental health
- HealthMAPS Portal
- OTHERS
- Career
- Language assistance
- For Developers
- Contact us
☏ ANY QUESTIONS?
Get real answers
from real people
Phone: 1-800-440-1561
[email protected]
x
End of 50 minute hour? World of Psychology
On January 1, 2013, new coding procedures will go into effect for mental health services. Our Current Procedural Terminology (CPT) codes are used to bill insurers for services, and the psychiatry coding has not changed since 1998. Existing codes are self-explanatory. For example, psychiatrists are often discharged with the CPT code "90807", which is a 45-50 minute drug-managed outpatient psychotherapy session. Everyone knows what that means.
Our Current Procedural Terminology (CPT) codes are used to bill insurers for services, and the psychiatry coding has not changed since 1998. Existing codes are self-explanatory. For example, psychiatrists are often discharged with the CPT code "90807", which is a 45-50 minute drug-managed outpatient psychotherapy session. Everyone knows what that means.
Psychiatry has changed since 1998, and the current codes do not sense the complexity or variety of what psychiatrists do now. In addition to the basic CPT codes, there are more specific Evaluation and Management (E/M) codes that require certain elements of the exam and documentation, but many psychiatrists, myself included, have practiced without ever using these E/M codes.
New CPT codes include a level of sophistication that mental health clinicians and their support staff are only just now beginning to learn. The new codes were announced by the American Medical Association in mid-September and which new codes psychiatric professionals should use is not entirely clear; it requires training. A two-hour webinar was held at the National Council for Community Behavioral Health and demonstrated 99 slides to start the learning process. Their webinar reached maximum capacity and potential registrants were turned away. The American Psychiatric Association held a meeting in mid-November to train district leaders on how to do coding, and in my state the Maryland Psychiatric Society will begin offering workshops in December.
A two-hour webinar was held at the National Council for Community Behavioral Health and demonstrated 99 slides to start the learning process. Their webinar reached maximum capacity and potential registrants were turned away. The American Psychiatric Association held a meeting in mid-November to train district leaders on how to do coding, and in my state the Maryland Psychiatric Society will begin offering workshops in December.
New codes, like the old ones, allow you to pay for psychotherapy depending on the time, but in increments of 30, 45 and 60 minutes. Presumably longer sessions will result in higher reimbursement, but under the new rules, a 50-minute session - or any psychotherapy session that takes 38-52 minutes - will be coded as 45 minutes. The code for a 60 minute session will require the session to be at least 53 minutes long.
- Psychology of Torture
- Alternative Therapies Mental Health Improvement
- Therapy with a Real Trauma Doctor: Part One
- Sorry Wounded Healers
- Positive Psychology in Martial Arts
medications, E/M codes will be required for each appointment, and the code for pharmacological management will be cancelled. Time spent on medication and education should not be included in total psychotherapy time if the psychiatrist is doing both, so two codes would be used for the same visit and services offered in the same appointment should be different. You have it, right? The E/M codes will allow for five different levels of difficulty and will require the psychiatrist to provide specific documentation regarding history, expertise, and medical decision making. After analyzing all of this, I still haven't figured out the E/M codes and don't know what codes to use for my typical 50 minute psychotherapy session, which I think will now be 53 minutes, or maybe 38 minutes, which might be billed for 45 minutes – plus an added indefinite period of time required to complete the E/M medication related service once the level of difficulty has been determined. There will also be codes for crisis management and difficult family situations. Simply put, there will now be approximately 17 different ways to code a 50-minute drug management psychotherapy session, depending on what is said in the session, and each combination will give a different pay.
Time spent on medication and education should not be included in total psychotherapy time if the psychiatrist is doing both, so two codes would be used for the same visit and services offered in the same appointment should be different. You have it, right? The E/M codes will allow for five different levels of difficulty and will require the psychiatrist to provide specific documentation regarding history, expertise, and medical decision making. After analyzing all of this, I still haven't figured out the E/M codes and don't know what codes to use for my typical 50 minute psychotherapy session, which I think will now be 53 minutes, or maybe 38 minutes, which might be billed for 45 minutes – plus an added indefinite period of time required to complete the E/M medication related service once the level of difficulty has been determined. There will also be codes for crisis management and difficult family situations. Simply put, there will now be approximately 17 different ways to code a 50-minute drug management psychotherapy session, depending on what is said in the session, and each combination will give a different pay.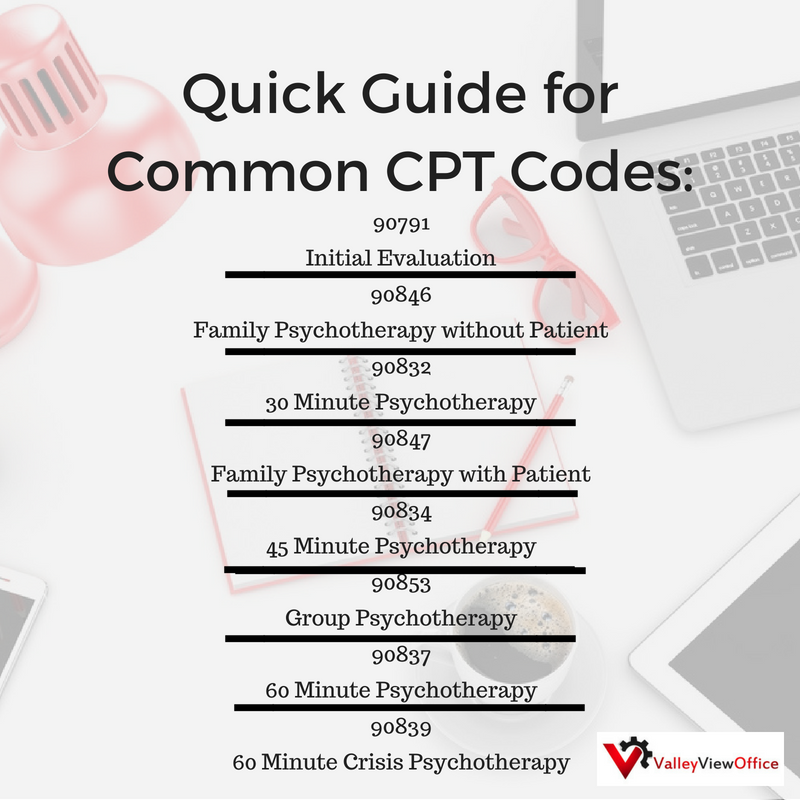 There doesn't seem to be a code for the time spent figuring out the correct code for each session, or any concern that these issues might distract physicians from the concerns of patient care.
There doesn't seem to be a code for the time spent figuring out the correct code for each session, or any concern that these issues might distract physicians from the concerns of patient care.
So what does this mean for mentally healthy practitioners and for patients who are receiving treatment? I think these changes will eventually become easy enough for those who offer only psychotherapy or only treatment. For psychiatrists, there is hope that coding will better understand what we are really doing and allow us to appreciate the complexity that distinguishes psychiatry from other mental health specialties. The fear is that these changes will create a lot of confusion, especially in the first place, and they promise to increase the paperwork burden and worry about inadvertently fraudulent claims.
Six weeks before implementation, tens of thousands of individual clinicians, administrators and institutions still need to be trained and then fine-tuned in the way they practice, document and pay.
I suspect we are in a transitional phase and that appointments will be sent with incorrect reject-only codes. Eventually, kinks will be developed, but the new system promises to be more cumbersome.
For a physician who participates in health insurance networks, payments may increase, and for those who do not participate, these changes may allow their patients to receive better reimbursement for out-of-network services. So far, though, that doesn't look good, at least not for Medicare providers and recipients. The 2013 Medicare fee schedule, released last week, shows that reimbursement for psychiatric assessments through medical services - those done by psychiatrists - will be lower than reimbursement for psychiatric assessments by social workers and psychologists. And timed psychotherapy provided by psychiatrists who also provide E/M services will be reimbursed at a lower rate than psychotherapy provided by those who do not deal with medical issues. This does not make sense and seems to contradict the premise that the creation of a comprehensive service coding system would promote understanding of the complexity of the medical aspects of treating mental disorders, parity of treatment, and reducing the stigma to see a psychiatrist.