Autism in pregnancy
How pregnancy may shape a child’s autism | Spectrum
Autism is predominantly genetic in origin, but a growing list of preterm exposures for mother and baby may sway the odds.
Photography by Ethan Hill
Even after her first child, Shane, was diagnosed with autism last year at the age of 2, Melissa Patao knew she wanted a bigger family. She was aware that any other children she had would have high odds of being diagnosed with the condition — estimates suggest that about 20 percent of siblings of autistic children also receive a diagnosis — but she was more than willing to take the chance. “I just adore Shane so much; he’s my world,” she says. In August, Patao gave birth to her second son, Zayden.
If it turns out that Zayden is also on the spectrum, “so be it,” Patao says. But all through her pregnancy, she wondered ‘what if?’ She found herself poring over research studies in an attempt to understand his odds of having autism and what might influence them.
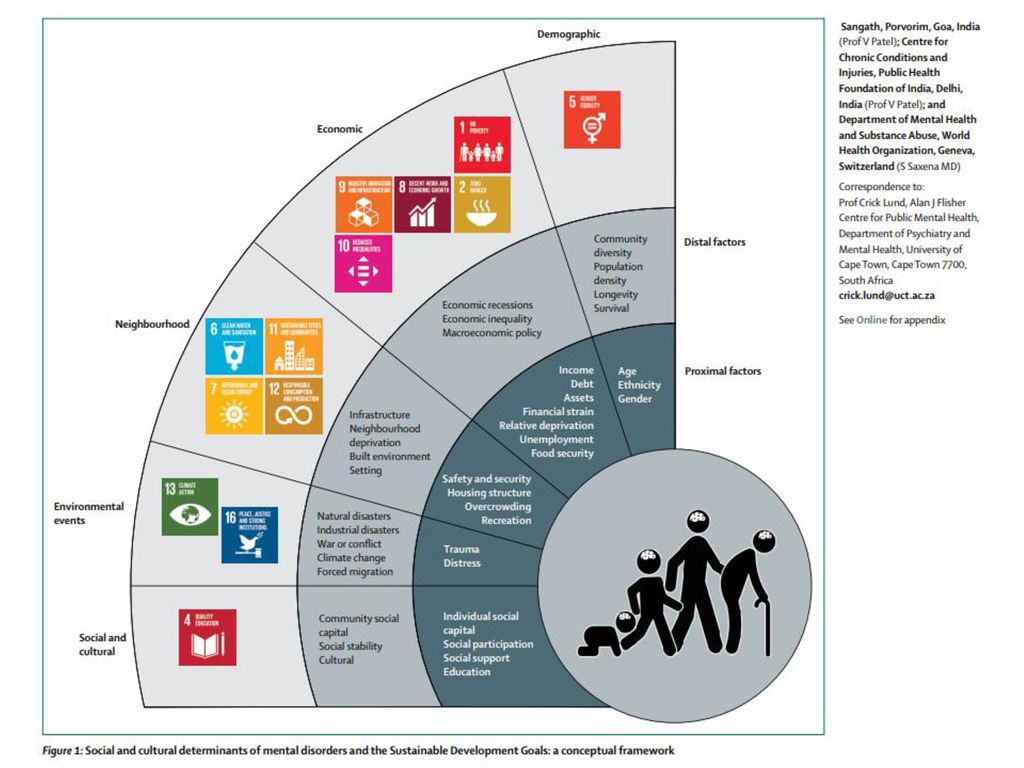
Patao, who is training to become a pediatric nurse practitioner, found no shortage of reading material: Last year alone, scientists published more than 100 papers on events during pregnancy that can influence a child’s odds of having autism. Genes determine about 50 to 95 percent of that risk. But that means that “there’s more to the story than just that genetic predisposition,” says Daniele Fallin, a genetic epidemiologist at Johns Hopkins University in Baltimore. Environmental contributions must also factor in.
The baby’s earliest environment — the womb — is critical: Because the fetal brain produces about 250,000 neurons every minute during pregnancy, experiences that interfere with that process can affect the developing brain in lasting ways. Studies have linked autism to a number of factors in pregnancy, among them the mother’s diet, the medicines she takes and her mental, immune and metabolic conditions, including preeclampsia (a form of high blood pressure) and gestational diabetes. Other preliminary work has implicated the quality of the air she breathes and the pesticides she is exposed to. And some research suggests that birth complications and birth timing may also play a role.
Other preliminary work has implicated the quality of the air she breathes and the pesticides she is exposed to. And some research suggests that birth complications and birth timing may also play a role.
The relationship between many of these factors and autism is still speculative. “That question of causality, it’s a burden that is very difficult to fulfill,” says Brian Lee, an epidemiologist at Drexel University in Philadelphia. This is generally true of research into environmental exposures, and particularly so for studies in pregnant women: Researchers cannot ethically expose pregnant women to possible risks; observational studies can only identify correlations, not causes; and the results of animal studies do not always extrapolate to people.
But researchers are starting to uncover biological threads that tie some of these prenatal exposures together. Many affect common biochemical pathways previously implicated in autism, such as those involving inflammation and aberrant immunity in both mother and baby. Each may only “contribute a little bit of risk here and there,” Lee says, but it is crucial to try to understand how all the pieces add up.
Each may only “contribute a little bit of risk here and there,” Lee says, but it is crucial to try to understand how all the pieces add up.
Uncertain outcome: Melissa Patao wonders whether her baby, Zayden, has autism like his brother Shane.
Inside the womb:Autism has been tied to events throughout pregnancy, including the first few days after conception. Even before a tiny human blastocyst attaches itself to the nutrient-rich lining of its mother’s uterus, factors that will shape its nervous system are already in play. In the days immediately following conception, genes that govern brain wiring are turned on and off in a process that requires folate, or vitamin B9. Folate may be important for the building of fundamental brain structures later on, too.
If a mother’s diet is deficient in folate, these processes can go awry, increasing the risk for neural defects, such as spina bifida and possibly autism. In a 2013 study, Norwegian researchers followed more than 85,000 women from 18 weeks into their pregnancies until an average of about six years after delivery, collecting information that included whether and when the women took supplements of folic acid, the synthetic form of folate, as well as the health of their children. Those who took supplements, especially between four weeks before and eight weeks after conception, were about 40 percent less likely to have children diagnosed with autism than those who did not take the supplements. Other studies have linked vitamin D deficiency in pregnant women with autism in their children, but the implications are unclear.
Those who took supplements, especially between four weeks before and eight weeks after conception, were about 40 percent less likely to have children diagnosed with autism than those who did not take the supplements. Other studies have linked vitamin D deficiency in pregnant women with autism in their children, but the implications are unclear.
How strongly a blastocyst attaches to the mother’s uterine wall after fertilization can affect its access to folic acid and other nutrients. A strong attachment ensures that the embryo connects with the mother’s blood vessels and remodels them to supply it with nutrients and oxygen throughout pregnancy, says Cheryl Walker, an obstetrician-gynecologist at the University of California, Davis. By contrast, a shallow implantation can lead to fetal growth restriction and low birth weight, both of which are linked to autism.
A shallow attachment can also lead to preeclampsia in the mother. Children with autism are twice as likely as typical children to have been exposed to preeclampsia, according to a 2015 study. In a woman with preeclampsia, blood vessels in the placenta “don’t dilate as well, and they don’t end up giving as many resources to that baby,” says Walker, who was involved in the study. As a result, the fetal brain may be starved of nutrients it needs to grow properly.
In a woman with preeclampsia, blood vessels in the placenta “don’t dilate as well, and they don’t end up giving as many resources to that baby,” says Walker, who was involved in the study. As a result, the fetal brain may be starved of nutrients it needs to grow properly.
The fetus’ immune system can also interfere with its brain development. Certain molecules, called cytokines, that control the migration of cells in the immune system are also crucial for neurons and immune cells to get to their correct locations in the nervous system. “The two systems talk to each other in ways that we didn’t realize they did,” says Judy Van de Water, a neuroimmunologist at the University of California, Davis.
Infections during pregnancy may scramble this signaling. A successful pregnancy involves an intricate immune dance: A woman’s immunity has to tamp down so that it does not attack the fetus as a foreign invader but also remain vigilant enough to ward off harmful infections. Even when that goes to plan, though, serious infections can ramp up her immune response, to the detriment of her child. For example, a 1977 study found a surprisingly high prevalence of autism — 1 in 13 — among children born to mothers who were infected with rubella during pregnancy. And a 2015 study that followed more than 2.3 million children born in Sweden from 1984 to 2007 reported that women who are hospitalized for infections during pregnancy have about a 30 percent increase in the odds of having a child with autism compared with other pregnant women.
For example, a 1977 study found a surprisingly high prevalence of autism — 1 in 13 — among children born to mothers who were infected with rubella during pregnancy. And a 2015 study that followed more than 2.3 million children born in Sweden from 1984 to 2007 reported that women who are hospitalized for infections during pregnancy have about a 30 percent increase in the odds of having a child with autism compared with other pregnant women.
Predicting risk: Manish Arora studies chemical exposures that may affect a child’s odds of autism.
That risk may be mediated at least in part by inflammation and disrupted immune signaling in the mother. A 2013 study of 1.2 million Finnish births found that women with the highest levels of C-reactive protein, a common inflammation marker, in their blood are 80 percent more likely to have children diagnosed with autism than women with the lowest levels. Last year, Van de Water and her colleagues reported that women who went on to have autistic children with intellectual disability had elevated blood levels of certain cytokines halfway through gestation.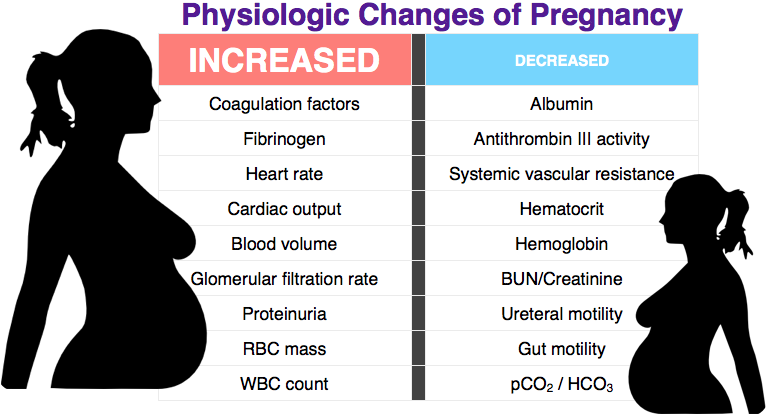
Some cytokines seem to be particularly important in mediating autism risk. In mice, immune activation contributes to autism only when a subset of immune cells, called T-helper 17 cells, release a cytokine called interleukin 17. In mice without these cells, inflammation during pregnancy does not seem to lead to autism. T-helper 17 cells are produced in response to specific gut bacteria, raising the possibility that pregnant women with these bacteria are especially susceptible to the kind of inflammation that contributes to autism. Eliminating those specific bacteria from pregnant women’s guts might lower the odds of autism in their children — a possibility researchers are investigating.
Obesity, diabetes before and during pregnancy, stress and autoimmune conditions in the mother have been associated with autism in her child, too: All either induce inflammation or impair immune signaling in other ways. These pieces of evidence, taken together, are called the ‘maternal immune activation hypothesis. ’ A meta-analysis of 32 papers published earlier this year found that women who are obese or overweight before pregnancy are 36 percent more likely than women at a healthy weight to have children later diagnosed with autism.
’ A meta-analysis of 32 papers published earlier this year found that women who are obese or overweight before pregnancy are 36 percent more likely than women at a healthy weight to have children later diagnosed with autism.
Van de Water’s work has shown that some autoimmune reactions can even directly damage the fetal brain. (During pregnancy, a woman’s antibodies can cross the placenta and even cross the fetal blood-brain barrier.) In 2013, Van de Water’s team reported that 23 percent of mothers of autistic children carry antibodies to fetal brain proteins, compared with 1 percent of mothers of typical children. No one knows why these women might have these antibodies — it’s “the $50 million question,” Van de Water says — but researchers posit they may be yet another byproduct of a maternal immune system gone haywire. Factors outside the mother’s body can also wield powerful effects.
“We’re starting to put things together that we never, ever thought to look at in combination.Outside the womb:” Judy Van de Water
Manish Arora’s desk at the Icahn School of Medicine at Mount Sinai in New York City is a chaotic jumble of half-empty coffee mugs, philosophy books and baby teeth. The tiny teeth were donated for a study unrelated to autism, but they may uncover secrets about the condition nonetheless, he says.
Arora is many things: a dentist, a scientist and a father to 6-year-old triplets. He is soft-spoken and often speaks in metaphors. In his professional life, he strives to understand how chemical exposures early in life affect brain development, a passion shaped by his childhood growing up on the border of Zambia and what is now Zimbabwe. He remembers trucks spraying pesticides such as DDT on the ground — and sometimes also on children playing outside — to control malaria, a practice that he continued to think about as he got older because of its potential harm.
As Arora knows from his dentistry work, baby teeth provide a record of a body’s chemical exposures.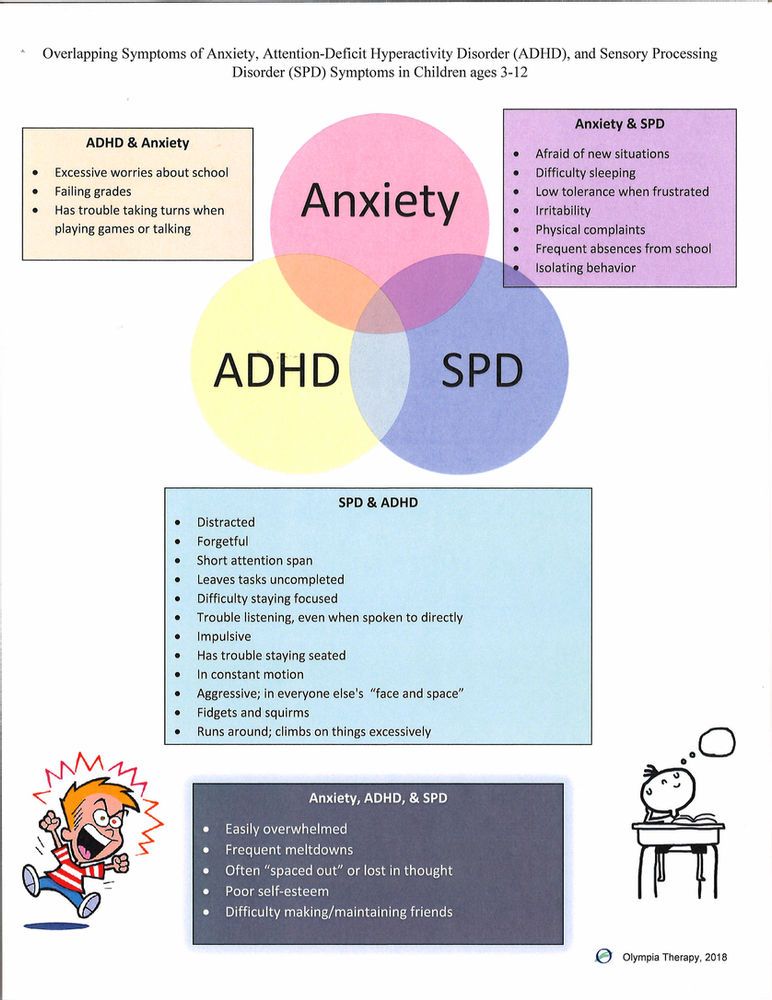 Teeth, he explains, are like trees: As they grow, they create rings — about one-tenth the diameter of a human hair — that record the chemicals and metals they encounter. These growth rings begin to form at the end of the first trimester of gestation and continue throughout life. “Today, you and me are forming a growth ring and it’s capturing everything that we’re exposed to,” he says. By studying the growth rings of discarded baby teeth, he and his colleagues can analyze what fetuses were exposed to in utero. The stress of birth creates a dark mark that can be used as a reference point.
Teeth, he explains, are like trees: As they grow, they create rings — about one-tenth the diameter of a human hair — that record the chemicals and metals they encounter. These growth rings begin to form at the end of the first trimester of gestation and continue throughout life. “Today, you and me are forming a growth ring and it’s capturing everything that we’re exposed to,” he says. By studying the growth rings of discarded baby teeth, he and his colleagues can analyze what fetuses were exposed to in utero. The stress of birth creates a dark mark that can be used as a reference point.
In May, Arora and his colleagues reported an analysis of baby teeth collected from 193 children, including 32 sets of twins in which one twin is autistic and the other is not. The team analyzed the children’s tooth growth rings using a highly sensitive form of mass spectrometry. The levels of metals such as zinc and copper typically cycle together in a pattern — both metals help to regulate neuronal firing — but in autistic children, the cycles are shorter, less regular and less complex than in controls. Arora’s team created an algorithm based on these group differences that can predict a child’s autism with more than 90 percent accuracy.
Arora’s team created an algorithm based on these group differences that can predict a child’s autism with more than 90 percent accuracy.
Arora’s work is part of a growing field that is attempting to decipher what kinds of environmental exposures increase the odds of autism and how they interact with human biology and genetics. These are tough questions to answer. Researchers cannot easily collect blood or saliva samples from fetuses to see what’s circulating through them. Instead, they try to discern fetal exposures by using the mother’s environment as a proxy. If a pregnant woman takes a particular medication, for instance, researchers can extrapolate that the fetus, too, was exposed.
So far, though, results have been mixed. Studies suggest that autism is associated with thalidomide, a drug prescribed for morning sickness in the 1950s and 1960s and later found to cause serious birth defects. Valproate, a drug used to treat epilepsy, bipolar disorder and migraines, is also linked to autism when taken during pregnancy.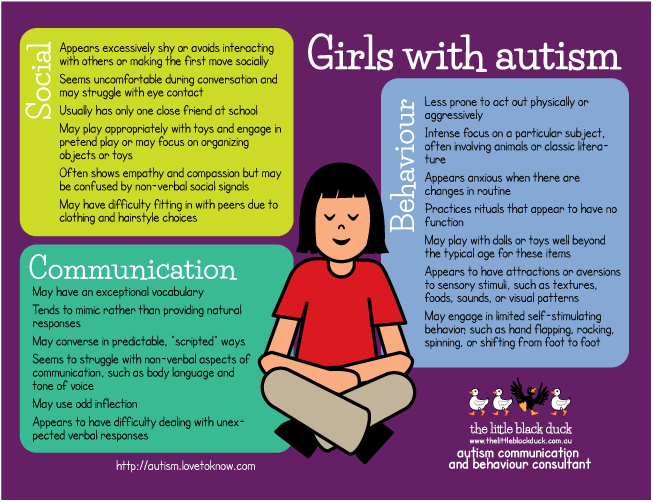 But for other common drugs, such as antidepressants, an association with autism is harder to discern.
But for other common drugs, such as antidepressants, an association with autism is harder to discern.
Chemical record: Growth rings in baby teeth reveal exposures before and after birth.
Part of the problem is that women take antidepressants for underlying mental-health conditions — so if an association is found, it is often unclear whether the root cause is her medication or her genetics. “It’s very difficult to disentangle,” says Hilary Brown, an epidemiologist at the University of Toronto Scarborough in Canada. Last year, through a clever study design, she and her colleagues inched a bit closer to the truth. They studied sibling pairs in which one sibling had been exposed to antidepressants in utero and the other had not, allowing them to control for the severity of the mother’s depression, among other factors. They reported that the siblings exposed to antidepressants were no more likely to have autism than their unexposed siblings. The results suggest that the medications themselves do not increase autism risk.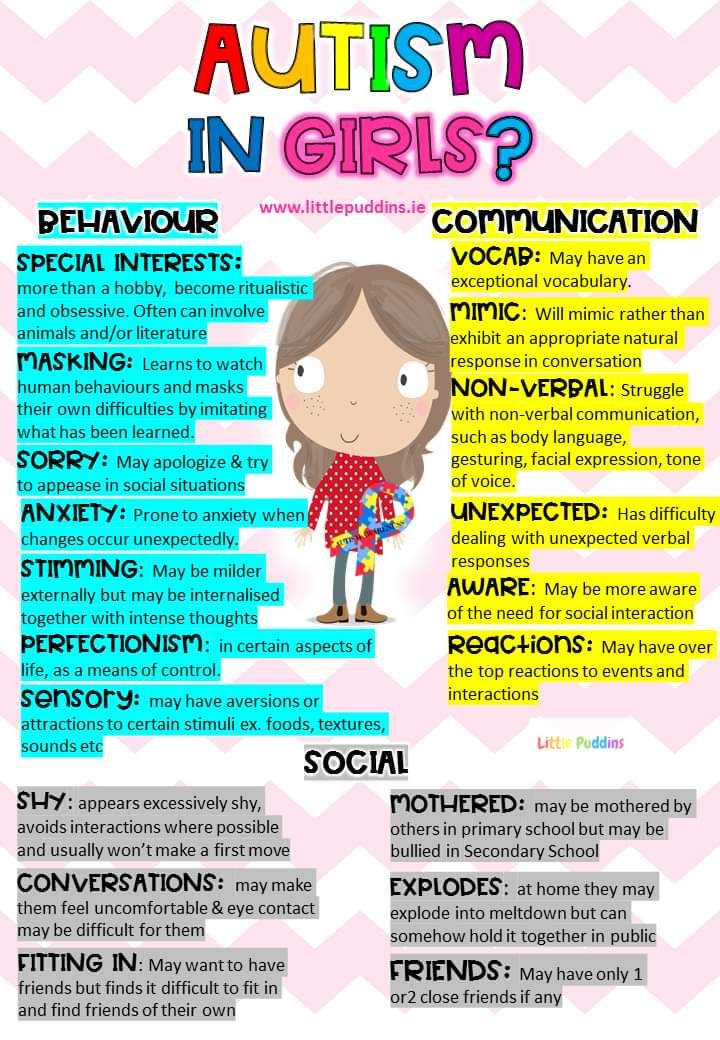
Some research has also linked the use of acetaminophen (commonly marketed as Tylenol) during pregnancy to autism. But again, it is unclear whether it is acetaminophen that is the problem, or the underlying reason for its use — pain or an infection, leading back to the maternal immune activation hypothesis.
Air pollution might also be linked to autism risk, but the details are hazy. At least 14 studies have suggested an association with autism, and air pollution is known to trigger inflammation, but analyses of individual airborne chemicals have been inconsistent. Researchers are also confused by the fact that cigarette smoking, which contains many of the same chemicals as air pollution, is not associated with the condition.
Certain pesticides, such as chlorpyrifos, can disrupt sex-hormone pathways implicated in animal models of autism. But again, studies linking pesticides to autism have been mixed, and questions about causation are unresolved. More answers may emerge, however, as researchers uncover new ways to study interactions between fetuses and the outside world. In addition to Arora’s work on baby teeth, researchers are investigating what kinds of chemical stories meconium, a newborn’s first feces, can tell.
In addition to Arora’s work on baby teeth, researchers are investigating what kinds of chemical stories meconium, a newborn’s first feces, can tell.
“If it’s a difficult birth … then that increases the risk of autism dramatically.” Sam WangBirth and beyond:
Princeton University neuroscientist Sam Wang has long been interested in autism’s potential environmental causes, but he says he finds the research intimidating. “It’s like the sands of the seas,” he says. “It’s this enormous literature, and people who work in it have all these different perspectives.”
Several years ago, in an attempt to bring clarity to the issue, Wang perused about 100 studies and then ranked dozens of associations between autism and both genetic and environmental factors by their relative risk ratios. He described his findings in a 2014 op-ed in The New York Times.
What came out on top in Wang’s analysis of environmental factors was birth — in particular, rare birth injuries to the cerebellum, a brain region that coordinates muscle movements, among other functions. “If it’s a difficult birth, or there’s a bleed on the cerebellum, then that increases the risk of autism dramatically,” by a whopping 3,800 percent, he says. “It’s bigger than any other risk factor, other than sharing your entire genome with a person with autism.” Wang’s research supports the link, too: He has shown that mice with early damage to the cerebellum later have serious cognitive and behavioral problems that mimic autism traits.
“If it’s a difficult birth, or there’s a bleed on the cerebellum, then that increases the risk of autism dramatically,” by a whopping 3,800 percent, he says. “It’s bigger than any other risk factor, other than sharing your entire genome with a person with autism.” Wang’s research supports the link, too: He has shown that mice with early damage to the cerebellum later have serious cognitive and behavioral problems that mimic autism traits.
The timing of birth also made Wang’s list: Babies born at least nine weeks premature seem to have higher odds of autism, he found.
When Noelle Mathias found out she was pregnant with her eldest daughter, Elena, in 2008, she took good care of herself. Mathias exercised, ate well and didn’t drink alcohol or smoke. “As far as I knew, it was a normal pregnancy,” she recalls. But her water broke early at 36 weeks and Elena was born less than 24 hours later. When Elena was 2, Mathias and her husband noticed she wasn’t responding to her name. They had Elena evaluated and, soon after, the girl was diagnosed with autism.
It’s impossible to know whether Elena’s preterm birth played a causal role in her diagnosis. Is being born early itself the issue, or might an underlying genetic susceptibility or environmental insult increase the odds of both preterm birth and autism?
Mathias’ second pregnancy was full term, and her daughter Elisa, now 8, is developmentally typical. But in Mathias’ third pregnancy, her water broke at only 25 weeks and she spent 53 days in the hospital on bed rest, hoping to delay birth as long as possible. Her son Emmanuel held out until 33 weeks and then spent time in the neonatal intensive care unit. He’s 2 now and seems to be developing typically.
Mathias has no idea why her first child has had a different outcome from the others. Parsing the risk for any one child is complicated by the fact that autism “isn’t just a ‘you have it or you don’t’ condition — it’s this wide phenotypic spectrum,” says Kristen Lyall, an epidemiologist at Drexel University’s A.J. Drexel Autism Institute. Perhaps some environmental factors preferentially influence social skills, whereas others primarily shape cognitive development, for instance.
Perhaps some environmental factors preferentially influence social skills, whereas others primarily shape cognitive development, for instance.
Keeping watch: The Patao family participates in a ‘baby sibling’ study, monitoring Zayden for signs of autism.
It may also be that certain combinations of factors — several environmental exposures in a row, perhaps, or a particular exposure along with a genetic susceptibility — are necessary to tilt a child’s brain development toward autism. A 2016 study, for example, found that in mice, maternal infection can modulate the effects of genes linked to autism, including CNTNAP2. “We’re starting to put things together that we never, ever thought to look at in combination,” Van de Water says. “You’ve got people working together that never would’ve necessarily crossed paths.” As part of those efforts, researchers are looking for fetal and infant biomarkers of autism, such as irregular cytokine profiles, anti-fetal antibodies and markers of oxidative stress, which might open the door to earlier and more effective interventions.
Because Zayden has an older brother with autism, Melissa Patao was able to enroll him in a ‘baby sibling’ study at the Yale Child Study Center. Researchers there followed Patao’s pregnancy with Zayden and plan to continue to track his development into toddlerhood. For now, Zayden is doing everything a 3-month-old usually does: He is smiling and interacting with his family, and he recently started laughing. His brother Shane is also doing well — he is engaging in pretend play and his language skills, which are only slightly delayed, are continually improving.
Patao welcomes the fact that Zayden will be monitored so closely. She and her husband will know if he shows autism traits early, and he will have access to recommended interventions at the youngest possible age, when they are known to have the largest impact. “Being part of this study was something so meaningful for me,” Patao says. “It totally took away the overwhelming anxiety of wondering, ‘what if?’”
Cite this article: https://doi. org/10.53053/EPQM9169
org/10.53053/EPQM9169
Syndication
This article was republished in The Atlantic.
TAGS: antidepressants, autism, baby sibs, biomarkers, CNTNAP2, environment, epigenetics, fever, immune system, maternal infection, obesity, pregnancy, valproic acid
Rethinking autism: the impact of maternal risk factors on autism development
1. Hyman SL, Levy SE, Myers SM. Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics. 2020;145:e20193447. [PubMed] [Google Scholar]
2. Baio J, Wiggins L, Christensen DL, Maenner MJ, Daniels J, Warren Z, Kurzius-Spencer M, Zahorodny W, Robinson Rosenberg C, White T, Durkin MS, Imm P, Nikolaou L, Yeargin-Allsopp M, Lee LC, Harrington R, Lopez M, Fitzgerald RT, Hewitt A, Pettygrove S, Constantino JN, Vehorn A, Shenouda J, Hall-Lande J, Van Naarden Braun K, Dowling NF. Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2014. MMWR Surveill Summ. 2018;67:1–23. [PMC free article] [PubMed] [Google Scholar]
MMWR Surveill Summ. 2018;67:1–23. [PMC free article] [PubMed] [Google Scholar]
3. Ramaswami G, Geschwind DH. Genetics of autism spectrum disorder. Handb Clin Neurol. 2018;147:321–329. [PubMed] [Google Scholar]
4. Wassink TH, Piven J. The molecular genetics of autism. Curr Psychiatry Rep. 2000;2:170–175. [PubMed] [Google Scholar]
5. Ladd-Acosta C, Hansen KD, Briem E, Fallin MD, Kaufmann WE, Feinberg AP. Common DNA methylation alterations in multiple brain regions in autism. Mol Psychiatry. 2014;19:862–871. [PMC free article] [PubMed] [Google Scholar]
6. Wan H, Zhang C, Li H, Luan S, Liu C. Association of maternal diabetes with autism spectrum disorders in offspring: a systemic review and meta-analysis. Medicine (Baltimore) 2018;97:e9438. [PMC free article] [PubMed] [Google Scholar]
7. International Diabetes Federation. IDF policy briefing: diabetes in pregnancy: protecting maternal health. 2013 [Google Scholar]
8. Xie W, Ge X, Li L, Yao A, Wang X, Li M, Gong X, Chu Z, Lu Z, Huang X, Jiao Y, Wang Y, Xiao M, Chen H, Xiang W, Yao P.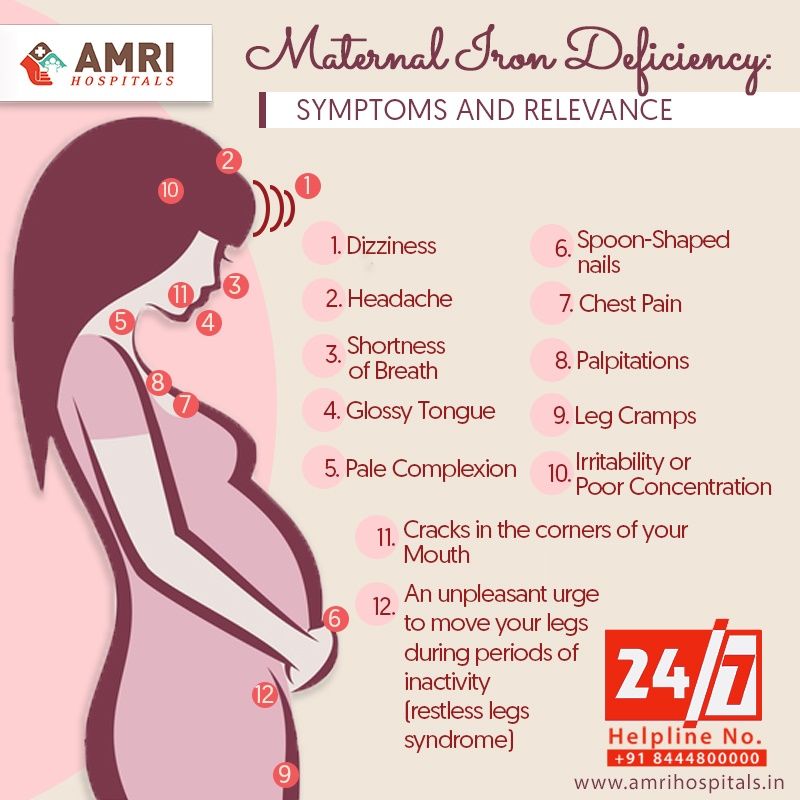 Resveratrol ameliorates prenatal progestin exposure-induced autism-like behavior through ERβ activation. Mol Autism. 2018;9:43. [PMC free article] [PubMed] [Google Scholar]
Resveratrol ameliorates prenatal progestin exposure-induced autism-like behavior through ERβ activation. Mol Autism. 2018;9:43. [PMC free article] [PubMed] [Google Scholar]
9. Xiang AH, Wang X, Martinez MP, Walthall JC, Curry ES, Page K, Buchanan TA, Coleman KJ, Getahun D. Association of maternal diabetes with autism in offspring. JAMA. 2015;313:1425–1434. [PubMed] [Google Scholar]
10. Li M, Fallin MD, Riley A, Landa R, Walker SO, Silverstein M, Caruso D, Pearson C, Kiang S, Dahm JL, Hong X, Wang G, Wang MC, Zuckerman B, Wang X. The association of maternal obesity and diabetes with autism and other developmental disabilities. Pediatrics. 2016;137:e20152206. [PMC free article] [PubMed] [Google Scholar]
11. Wang X, Lu J, Xie W, Lu X, Liang Y, Li M, Wang Z, Huang X, Tang M, Pfaff DW, Tang YP, Yao P. Maternal diabetes induces autism-like behavior by hyperglycemia-mediated persistent oxidative stress and suppression of superoxide dismutase 2. Proc Natl Acad Sci U S A. 2019;116:23743–23752.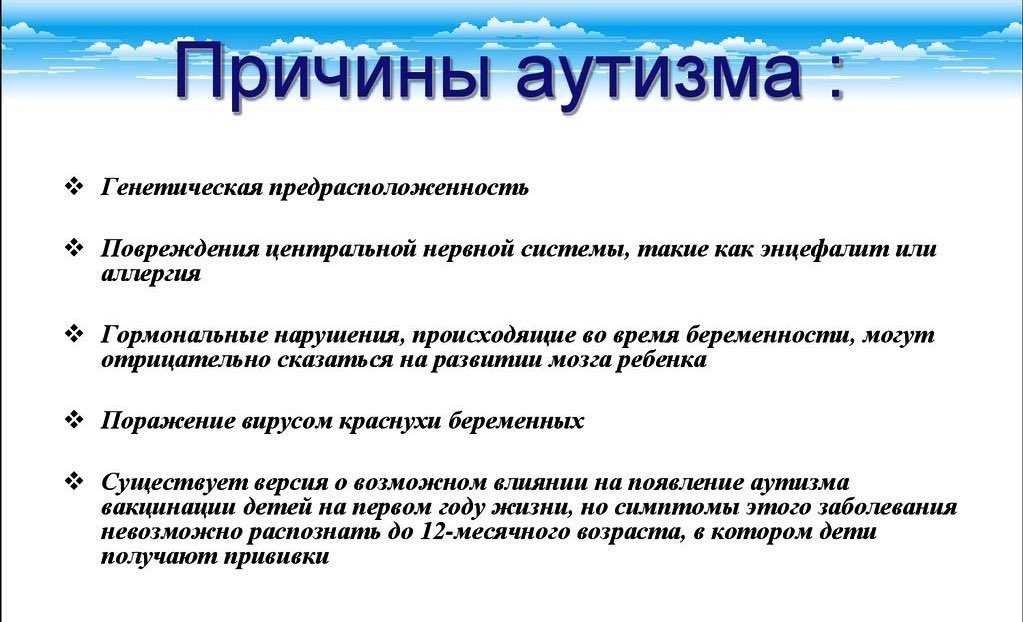 [PMC free article] [PubMed] [Google Scholar]
[PMC free article] [PubMed] [Google Scholar]
12. Lu J, Xiao M, Guo X, Liang Y, Wang M, Xu J, Liu L, Wang Z, Zeng G, Liu K, Li L, Yao P. Maternal diabetes induces immune dysfunction in autistic offspring through oxidative stress in hematopoietic stem cells. Front Psychiatry. 2020;11:576367. [PMC free article] [PubMed] [Google Scholar]
13. Menting MD, van de Beek C, Mintjens S, Wever KE, Korosi A, Ozanne SE, Limpens J, Roseboom TJ, Hooijmans C, Painter RC. The link between maternal obesity and offspring neurobehavior: a systematic review of animal experiments. Neurosci Biobehav Rev. 2019;98:107–121. [PubMed] [Google Scholar]
14. Liang Y, Yu H, Ke X, Eyles D, Sun R, Wang Z, Huang S, Lin L, McGrath JJ, Lu J, Guo X, Yao P. Vitamin D deficiency worsens maternal diabetes induced neurodevelopmental disorder by potentiating hyperglycemia-mediated epigenetic changes. Ann N Y Acad Sci. 2021;1491:74–88. [PubMed] [Google Scholar]
15. Liu J, Liang Y, Jiang X, Xu J, Sun Y, Wang Z, Lin L, Niu Y, Song S, Zhang H, Xue Z, Lu J, Yao P.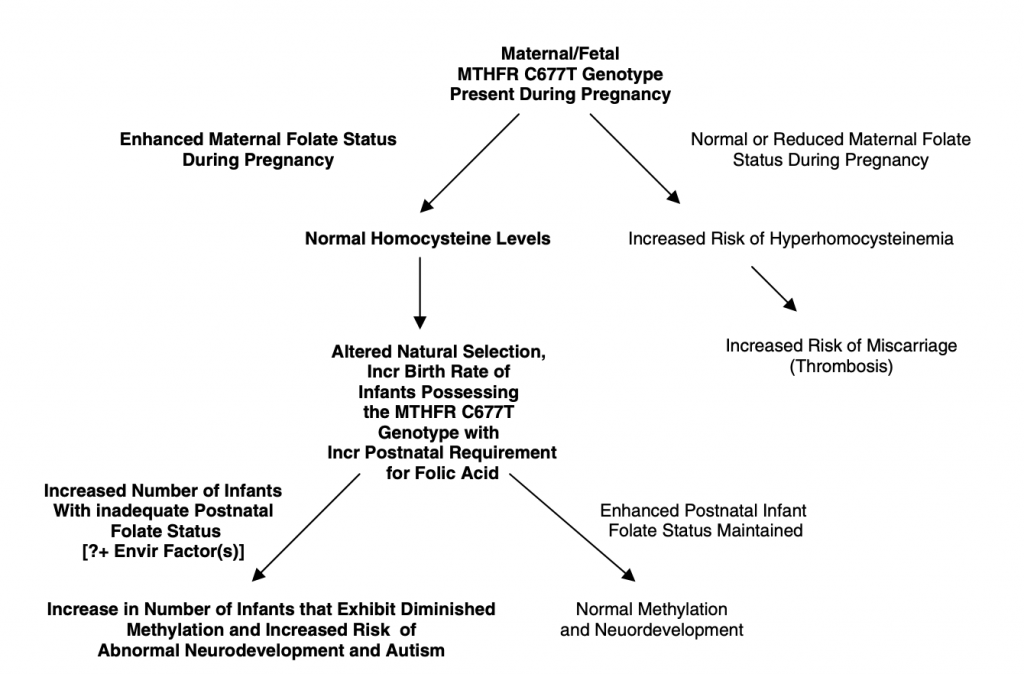 Maternal diabetes-induced suppression of oxytocin receptor contributes to social deficits in offspring. Front Neurosci. 2021;15:634781. [PMC free article] [PubMed] [Google Scholar]
Maternal diabetes-induced suppression of oxytocin receptor contributes to social deficits in offspring. Front Neurosci. 2021;15:634781. [PMC free article] [PubMed] [Google Scholar]
16. Sanchez CE, Barry C, Sabhlok A, Russell K, Majors A, Kollins SH, Fuemmeler BF. Maternal pre-pregnancy obesity and child neurodevelopmental outcomes: a meta-analysis. Obes Rev. 2018;19:464–484. [PMC free article] [PubMed] [Google Scholar]
17. Cherskov A, Pohl A, Allison C, Zhang H, Payne RA, Baron-Cohen S. Polycystic ovary syndrome and autism: a test of the prenatal sex steroid theory. Transl Psychiatry. 2018;8:136. [PMC free article] [PubMed] [Google Scholar]
18. Kosidou K, Dalman C, Widman L, Arver S, Lee BK, Magnusson C, Gardner RM. Maternal polycystic ovary syndrome and the risk of autism spectrum disorders in the offspring: a population-based nationwide study in Sweden. Mol Psychiatry. 2016;21:1441–1448. [PMC free article] [PubMed] [Google Scholar]
19. Brown HK, Ray JG, Wilton AS, Lunsky Y, Gomes T, Vigod SN. Association between serotonergic antidepressant use during pregnancy and autism spectrum disorder in children. JAMA. 2017;317:1544–1552. [PubMed] [Google Scholar]
Association between serotonergic antidepressant use during pregnancy and autism spectrum disorder in children. JAMA. 2017;317:1544–1552. [PubMed] [Google Scholar]
20. Maher GM, O’Keeffe GW, Kearney PM, Kenny LC, Dinan TG, Mattsson M, Khashan AS. Association of hypertensive disorders of pregnancy with risk of neurodevelopmental disorders in offspring: a systematic review and meta-analysis. JAMA Psychiatry. 2018;75:809–819. [PMC free article] [PubMed] [Google Scholar]
21. Jiang HY, Xu LL, Shao L, Xia RM, Yu ZH, Ling ZX, Yang F, Deng M, Ruan B. Maternal infection during pregnancy and risk of autism spectrum disorders: a systematic review and meta-analysis. Brain Behav Immun. 2016;58:165–172. [PubMed] [Google Scholar]
22. Brown AS, Cheslack-Postava K, Rantakokko P, Kiviranta H, Hinkka-Yli-Salomäki S, McKeague IW, Surcel HM, Sourander A. Association of maternal insecticide levels with autism in offspring from a national birth cohort. Am J Psychiatry. 2018;175:1094–1101. [PMC free article] [PubMed] [Google Scholar]
23. Philippat C, Barkoski J, Tancredi DJ, Elms B, Barr DB, Ozonoff S, Bennett DH, Hertz-Picciotto I. Prenatal exposure to organophosphate pesticides and risk of autism spectrum disorders and other non-typical development at 3 years in a high-risk cohort. Int J Hyg Environ Health. 2018;221:548–555. [PMC free article] [PubMed] [Google Scholar]
Philippat C, Barkoski J, Tancredi DJ, Elms B, Barr DB, Ozonoff S, Bennett DH, Hertz-Picciotto I. Prenatal exposure to organophosphate pesticides and risk of autism spectrum disorders and other non-typical development at 3 years in a high-risk cohort. Int J Hyg Environ Health. 2018;221:548–555. [PMC free article] [PubMed] [Google Scholar]
24. Fountain C, Zhang Y, Kissin DM, Schieve LA, Jamieson DJ, Rice C, Bearman P. Association between assisted reproductive technology conception and autism in California, 1997-2007. Am J Public Health. 2015;105:963–971. [PMC free article] [PubMed] [Google Scholar]
25. Corsi DJ, Donelle J, Sucha E, Hawken S, Hsu H, El-Chaâr D, Bisnaire L, Fell D, Wen SW, Walker M. Maternal cannabis use in pregnancy and child neurodevelopmental outcomes. Nat Med. 2020;26:1536–1540. [PubMed] [Google Scholar]
26. Wood AG, Nadebaum C, Anderson V, Reutens D, Barton S, O’Brien TJ, Vajda F. Prospective assessment of autism traits in children exposed to antiepileptic drugs during pregnancy. Epilepsia. 2015;56:1047–1055. [PubMed] [Google Scholar]
Epilepsia. 2015;56:1047–1055. [PubMed] [Google Scholar]
27. von Ehrenstein OS, Ling C, Cui X, Cockburn M, Park AS, Yu F, Wu J, Ritz B. Prenatal and infant exposure to ambient pesticides and autism spectrum disorder in children: population based case-control study. BMJ. 2019;364:l962. [PMC free article] [PubMed] [Google Scholar]
28. Pu Y, Yang J, Chang L, Qu Y, Wang S, Zhang K, Xiong Z, Zhang J, Tan Y, Wang X, Fujita Y, Ishima T, Wang D, Hwang SH, Hammock BD. Maternal glyphosate exposure causes autism-like behaviors in offspring through increased expression of soluble epoxide hydrolase. Proc Natl Acad Sci U S A. 2020;117:11753–11759. [PMC free article] [PubMed] [Google Scholar]
29. Holmes AS, Blaxill MF, Haley BE. Reduced levels of mercury in first baby haircuts of autistic children. Int J Toxicol. 2003;22:277–285. [PubMed] [Google Scholar]
30. Majewska MD, Urbanowicz E, Rok-Bujko P, Namyslowska I, Mierzejewski P. Age-dependent lower or higher levels of hair mercury in autistic children than in healthy controls. Acta Neurobiol Exp (Wars) 2010;70:196–208. [PubMed] [Google Scholar]
Acta Neurobiol Exp (Wars) 2010;70:196–208. [PubMed] [Google Scholar]
31. Lakshmi Priya MD, Geetha A. Level of trace elements (copper, zinc, magnesium and selenium) and toxic elements (lead and mercury) in the hair and nail of children with autism. Biol Trace Elem Res. 2011;142:148–158. [PubMed] [Google Scholar]
32. Geier DA, Kern JK, King PG, Sykes LK, Geier MR. Hair toxic metal concentrations and autism spectrum disorder severity in young children. Int J Environ Res Public Health. 2012;9:4486–4497. [PMC free article] [PubMed] [Google Scholar]
33. Crider A, Thakkar R, Ahmed AO, Pillai A. Dysregulation of estrogen receptor beta (ERβ), aromatase (CYP19A1), and ER co-activators in the middle frontal gyrus of autism spectrum disorder subjects. Mol Autism. 2014;5:46. [PMC free article] [PubMed] [Google Scholar]
34. Krezel W, Dupont S, Krust A, Chambon P, Chapman PF. Increased anxiety and synaptic plasticity in estrogen receptor beta-deficient mice. Proc Natl Acad Sci U S A. 2001;98:12278–12282. [PMC free article] [PubMed] [Google Scholar]
2001;98:12278–12282. [PMC free article] [PubMed] [Google Scholar]
35. Xu XJ, Zhang HF, Shou XJ, Li J, Jing WL, Zhou Y, Qian Y, Han SP, Zhang R, Han JS. Prenatal hyperandrogenic environment induced autistic-like behavior in rat offspring. Physiol Behav. 2015;138:13–20. [PubMed] [Google Scholar]
36. Xiang D, Lu J, Wei C, Cai X, Wang Y, Liang Y, Xu M, Wang Z, Liu M, Wang M, Liang X, Li L, Yao P. Berberine ameliorates prenatal dihydrotestosterone exposure-induced autism-like behavior by suppression of androgen receptor. Front Cell Neurosci. 2020;14:87. [PMC free article] [PubMed] [Google Scholar]
37. Zou Y, Lu Q, Zheng D, Chu Z, Liu Z, Chen H, Ruan Q, Ge X, Zhang Z, Wang X, Lou W, Huang Y, Wang Y, Huang X, Liu Z, Xie W, Zhou Y, Yao P. Prenatal levonorgestrel exposure induces autism-like behavior in offspring through ERβ suppression in the amygdala. Mol Autism. 2017;8:46. [PMC free article] [PubMed] [Google Scholar]
38. Halladay AK, Bishop S, Constantino JN, Daniels AM, Koenig K, Palmer K, Messinger D, Pelphrey K, Sanders SJ, Singer AT, Taylor JL, Szatmari P. Sex and gender differences in autism spectrum disorder: summarizing evidence gaps and identifying emerging areas of priority. Mol Autism. 2015;6:36. [PMC free article] [PubMed] [Google Scholar]
Sex and gender differences in autism spectrum disorder: summarizing evidence gaps and identifying emerging areas of priority. Mol Autism. 2015;6:36. [PMC free article] [PubMed] [Google Scholar]
39. Frazier TW, Georgiades S, Bishop SL, Hardan AY. Behavioral and cognitive characteristics of females and males with autism in the Simons Simplex Collection. J Am Acad Child Adolesc Psychiatry. 2014;53:329–340. e1–3. [PMC free article] [PubMed] [Google Scholar]
40. Schaafsma SM, Gagnidze K, Reyes A, Norstedt N, Månsson K, Francis K, Pfaff DW. Sex-specific gene-environment interactions underlying ASD-like behaviors. Proc Natl Acad Sci U S A. 2017;114:1383–1388. [PMC free article] [PubMed] [Google Scholar]
41. Hu VW, Sarachana T, Sherrard RM, Kocher KM. Investigation of sex differences in the expression of RORA and its transcriptional targets in the brain as a potential contributor to the sex bias in autism. Mol Autism. 2015;6:7. [PMC free article] [PubMed] [Google Scholar]
42. Hoffman EJ, Turner KJ, Fernandez JM, Cifuentes D, Ghosh M, Ijaz S, Jain RA, Kubo F, Bill BR, Baier H, Granato M, Barresi MJF, Wilson SW, Rihel J, State MW, Giraldez AJ. Estrogens suppress a behavioral phenotype in zebrafish mutants of the autism risk gene, CNTNAP2. Neuron. 2016;89:725–733. [PMC free article] [PubMed] [Google Scholar]
Hoffman EJ, Turner KJ, Fernandez JM, Cifuentes D, Ghosh M, Ijaz S, Jain RA, Kubo F, Bill BR, Baier H, Granato M, Barresi MJF, Wilson SW, Rihel J, State MW, Giraldez AJ. Estrogens suppress a behavioral phenotype in zebrafish mutants of the autism risk gene, CNTNAP2. Neuron. 2016;89:725–733. [PMC free article] [PubMed] [Google Scholar]
43. Turner TN, Wilfert AB, Bakken TE, Bernier RA, Pepper MR, Zhang Z, Torene RI, Retterer K, Eichler EE. Sex-based analysis of de novo variants in neurodevelopmental disorders. Am J Hum Genet. 2019;105:1274–1285. [PMC free article] [PubMed] [Google Scholar]
44. Robinson EB, Lichtenstein P, Anckarsäter H, Happé F, Ronald A. Examining and interpreting the female protective effect against autistic behavior. Proc Natl Acad Sci U S A. 2013;110:5258–5262. [PMC free article] [PubMed] [Google Scholar]
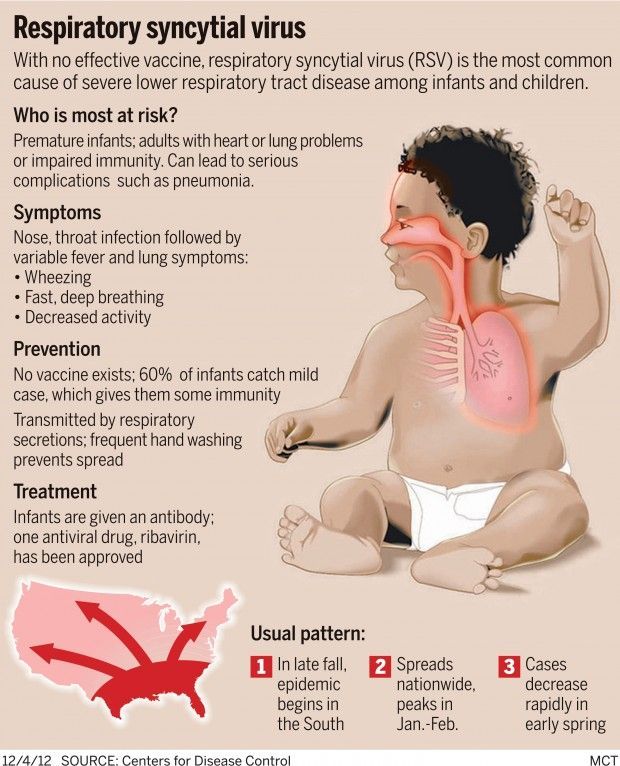
early signs of autism can be detected on prenatal ultrasound
Researchers at Ben-Gurion University in Israel have made a major announcement: the first signs of autism in a fetus can be detected as early as the second trimester of pregnancy.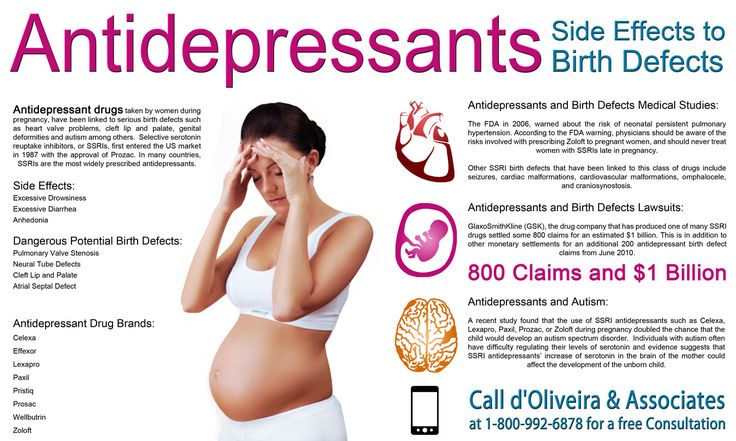 On ultrasound during prenatal screening, fetuses who developed autism after birth show abnormalities in the structure of the heart, kidneys, and head. The results of this study have already been published by the journal Brain.
On ultrasound during prenatal screening, fetuses who developed autism after birth show abnormalities in the structure of the heart, kidneys, and head. The results of this study have already been published by the journal Brain.
Scientists compared ultrasound findings of fetuses who later developed autism with those of their healthy siblings and their peers who did not have any developmental abnormalities. Approximately 30% of fetuses subsequently diagnosed with autism were found to have abnormal anatomical findings during screening during the second trimester of pregnancy. This indicator is three times higher than the rate of this kind of pathology in the general population and two times higher than in peers without developmental disabilities.
The ultrasound findings that showed the strongest association with autism were abnormalities in the development of the heart, kidneys, and head. These findings were more common in girls with autism and were also associated with the severity of autistic symptoms in children.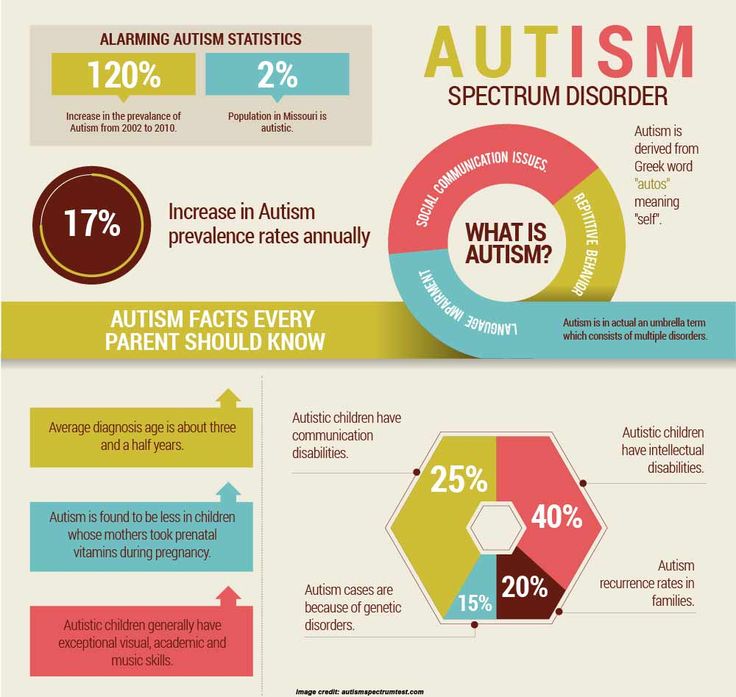
"The results of this study show that early signs of autism can be detected in the womb," says study leader Prof. Ben-Gurion - "Physicians will be able to use these signs, which can be found on conventional ultrasound, to assess the likelihood of having a child with autism."
These ultrasound results are not 100% positive for autism, but at least then doctors could use them to refer a woman for a genetic diagnosis, explained Prof. Reli Hershkovitz.
“Previous studies have shown that children born with congenital disorders, especially heart and kidney disorders, are more likely to develop autism.” Professor Menashe said.
Other related news:
- New discoveries in the study of autism
- Researchers at MC Chilov discovered the "Achilles' heel" of pancreatic cancer: a path to effective therapy
- Israeli study: Cancer can be prevented with peptide group
- Hope for patients with recurrent prostate cancer: Ichilov Medical Center confirmed the effectiveness of the "citrus" drug
Publication date: 02/10/2022
Author of article
Dr. Mikhail Zeigarnik
Mikhail Zeigarnik
We work seven days a week: 24/7
Service in three languages: Hebrew, Russian and English
Enter your details and the doctor of the clinic will call you back within an hour
I agree with the privacy policy. Please keep medical confidentiality.
Ultrasound during pregnancy and autism: what you need to know?
10/12/16
Some media have published the disturbing news about the connection between ultrasound and autism, but is there any real reason to avoid ultrasound? Explanations of a medical expert
Source: Autism Speaks
Translation: Elizaveta Morozova
I saw in the news that an ultrasound was associated with autism. My gynecologist ordered me this ultrasound. Do I have cause for concern?
Answered by Dr.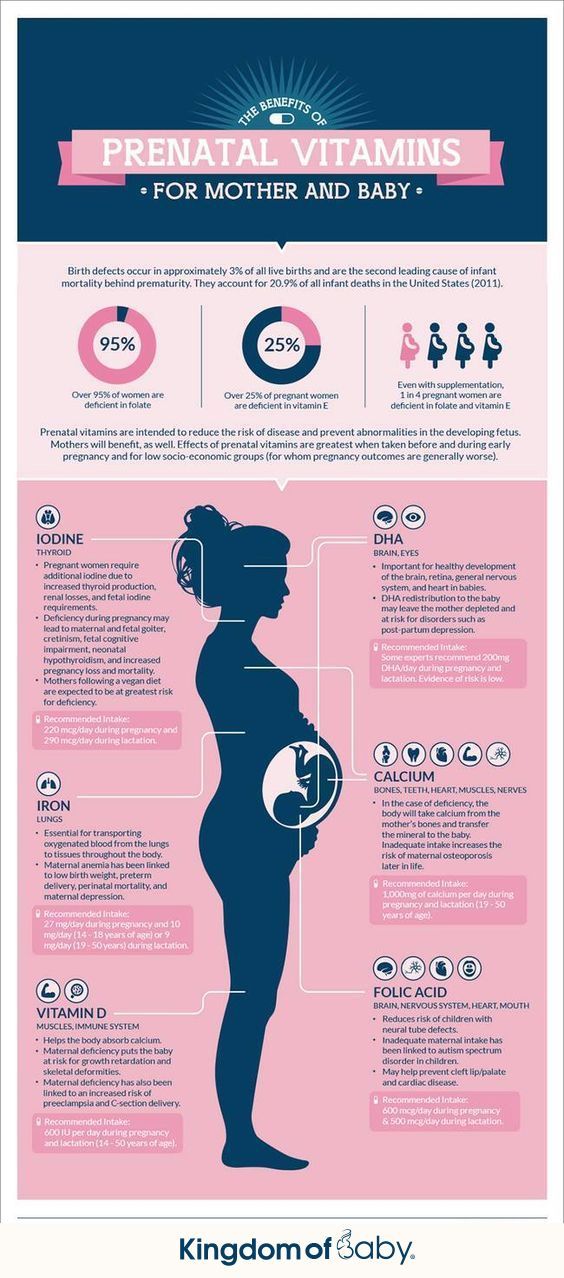 Daniel Coury, pediatrician, medical director of the Autism Speaks Autism Treatment Network, head of pediatric development and behavior at the National Children's Hospital in Columbus, USA.
Daniel Coury, pediatrician, medical director of the Autism Speaks Autism Treatment Network, head of pediatric development and behavior at the National Children's Hospital in Columbus, USA.
Thank you for your question. You are most likely referring to the recent headlines about the study on ultrasound and autism symptoms.
It is unfortunate that high-profile headlines in the media often lead to the fact that the context of scientific data is lost. A new study has found a link between ultrasound during the first trimester of pregnancy and the severity of autism symptoms in children with a genetic predisposition to the disorder. However, as I said, it is important to consider the context, and in this case it is "correlation or causation."
All this study has shown is that there is a tendency for the two phenomena, first trimester ultrasound and autism, to occur together (correlation). However, this does not mean that one phenomenon can be considered the cause of the second (causation).
In response to the high-profile headlines, many medical experts pointed out that if a doctor orders an ultrasound during the first trimester, then he is most likely worried about some medical condition that may affect the development of the child. So both ultrasound and autism may have a common cause - a medical problem, it is not necessary that ultrasound is the cause in itself.
More than 30 years of research into the effects of ultrasound on pregnancy. At the moment, there is no convincing evidence that this procedure has a negative impact on the health of the mother or child. On the other hand, it is true that doctors have begun to prescribe ultrasound more often than a few years ago. It worries me that they are now being done during normal pregnancies, and not just when there is a medical reason for doing so.
This study examined the association between first trimester ultrasound and the severity of autism symptoms. However, the study included only those children who had genetic abnormalities associated with a predisposition to autism. In other words, this study is not showed that ultrasound causes autism. It only suggests that ultrasound is somehow related to the severity of symptoms in a child who was initially predisposed to autism.
In other words, this study is not showed that ultrasound causes autism. It only suggests that ultrasound is somehow related to the severity of symptoms in a child who was initially predisposed to autism.
As I said earlier, both phenomena may have some common cause, for example, if the doctor is concerned about the course of pregnancy, then this increases the likelihood of prescribing an ultrasound, and subsequent developmental disorders in the child, including autism.
Given this context, you may need to discuss the following two questions with your gynecologist:
1. Why did the doctor order an ultrasound, is he worried about your pregnancy? If there is a rationale for ultrasound, then the benefits almost certainly outweigh any theoretical risk.
2. Do you have any reason to believe that your family may have a predisposition to autism? For example, do you already have a child on the autism spectrum? If this is the case, you may need to discuss with your doctor how dangerous it would be for you to refuse an ultrasound.