Asd severity levels
Autism Diagnosis Criteria: DSM-5 | Autism Speaks
What are the DSM-5 diagnostic criteria for autism?
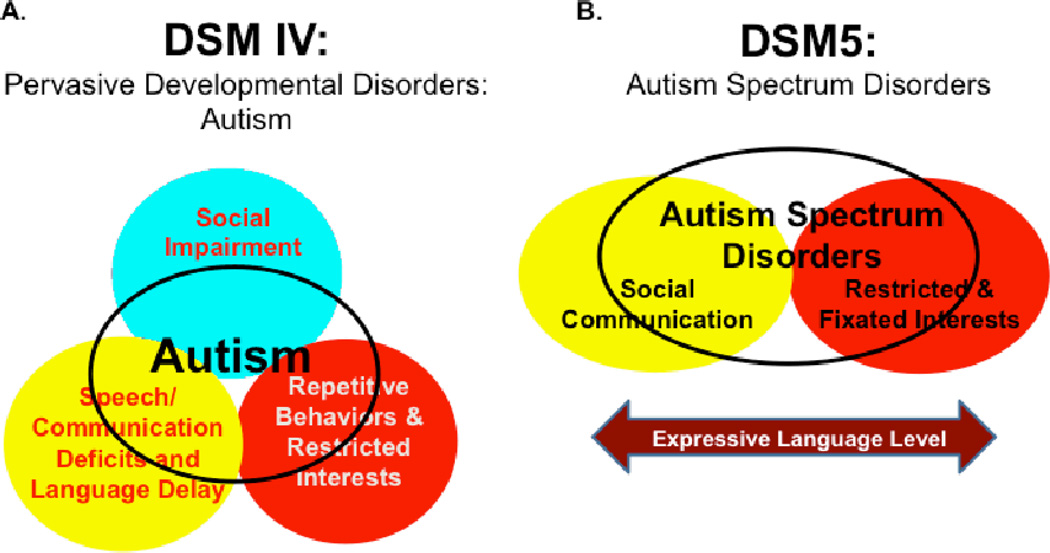
In 2013, the American Psychiatric Association released the fifth edition of its Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
The DSM-5 is now the standard reference that healthcare providers use to diagnose mental and behavioral conditions, including autism.
By special permission of the American Psychiatric Association, you can read the full-text of the new diagnostic criteria for autism spectrum disorder and the related diagnosis of social communication disorder below.
Also see: Answers to frequently asked questions about DSM-5 criteria for autism
DSM-5 Autism Diagnostic Criteria
A. Persistent deficits in social communication and social interaction across multiple contexts, as manifested by the following, currently or by history (examples are illustrative, not exhaustive, see text):
- Deficits in social-emotional reciprocity, ranging, for example, from abnormal social approach and failure of normal back-and-forth conversation; to reduced sharing of interests, emotions, or affect; to failure to initiate or respond to social interactions.
- Deficits in nonverbal communicative behaviors used for social interaction, ranging, for example, from poorly integrated verbal and nonverbal communication; to abnormalities in eye contact and body language or deficits in understanding and use of gestures; to a total lack of facial expressions and nonverbal communication.
- Deficits in developing, maintaining, and understanding relationships, ranging, for example, from difficulties adjusting behavior to suit various social contexts; to difficulties in sharing imaginative play or in making friends; to absence of interest in peers.
Specify current severity: Severity is based on social communication impairments and restricted repetitive patterns of behavior. (See table below.)
B. Restricted, repetitive patterns of behavior, interests, or activities, as manifested by at least two of the following, currently or by history (examples are illustrative, not exhaustive; see text):
- Stereotyped or repetitive motor movements, use of objects, or speech (e.
 g., simple motor stereotypies, lining up toys or flipping objects, echolalia, idiosyncratic phrases).
g., simple motor stereotypies, lining up toys or flipping objects, echolalia, idiosyncratic phrases). - Insistence on sameness, inflexible adherence to routines, or ritualized patterns or verbal nonverbal behavior (e.g., extreme distress at small changes, difficulties with transitions, rigid thinking patterns, greeting rituals, need to take same route or eat food every day).
- Highly restricted, fixated interests that are abnormal in intensity or focus (e.g, strong attachment to or preoccupation with unusual objects, excessively circumscribed or perseverative interest).
- Hyper- or hyporeactivity to sensory input or unusual interests in sensory aspects of the environment (e.g., apparent indifference to pain/temperature, adverse response to specific sounds or textures, excessive smelling or touching of objects, visual fascination with lights or movement).
Specify current severity: Severity is based on social communication impairments and restricted, repetitive patterns of behavior. (See table below.)
(See table below.)
C. Symptoms must be present in the early developmental period (but may not become fully manifest until social demands exceed limited capacities or may be masked by learned strategies in later life).
D. Symptoms cause clinically significant impairment in social, occupational, or other important areas of current functioning.
E. These disturbances are not better explained by intellectual disability (intellectual developmental disorder) or global developmental delay. Intellectual disability and autism spectrum disorder frequently co-occur; to make comorbid diagnoses of autism spectrum disorder and intellectual disability, social communication should be below that expected for general developmental level.
Note: Individuals with a well-established DSM-IV diagnosis of autistic disorder, Asperger’s disorder, or pervasive developmental disorder not otherwise specified should be given the diagnosis of autism spectrum disorder. Individuals who have marked deficits in social communication, but whose symptoms do not otherwise meet criteria for autism spectrum disorder, should be evaluated for social (pragmatic) communication disorder.
Individuals who have marked deficits in social communication, but whose symptoms do not otherwise meet criteria for autism spectrum disorder, should be evaluated for social (pragmatic) communication disorder.
Specify if:
- With or without accompanying intellectual impairment
- With or without accompanying language impairment
- (Coding note: Use additional code to identify the associated medical or genetic condition.)
- Associated with another neurodevelopmental, mental, or behavioral disorder
- (Coding note: Use additional code[s] to identify the associated neurodevelopmental, mental, or behavioral disorder[s].)
- With catatonia
- Associated with a known medical or genetic condition or environmental factor
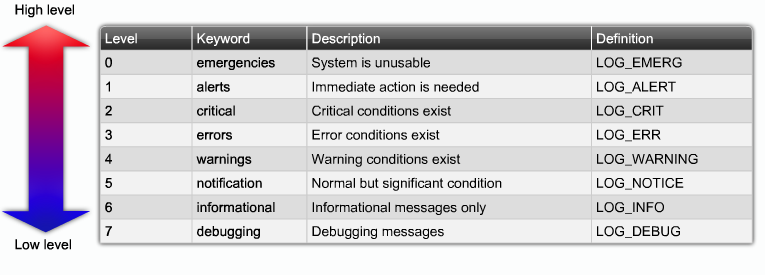
| Severity level | Social communication | Restricted, repetitive behaviors |
| Level 3 | Severe deficits in verbal and nonverbal social communication skills cause severe impairments in functioning, very limited initiation of social interactions, and minimal response to social overtures from others. | Inflexibility of behavior, extreme difficulty coping with change, or other restricted/repetitive behaviors markedly interfere with functioning in all spheres. Great distress/difficulty changing focus or action. |
| Level 2 | Marked deficits in verbal and nonverbal social communication skills; social impairments apparent even with supports in place; limited initiation of social interactions; and reduced or abnormal responses to social overtures from others. For example, a person who speaks simple sentences, whose interaction is limited to narrow special interests, and how has markedly odd nonverbal communication. | Inflexibility of behavior, difficulty coping with change, or other restricted/repetitive behaviors appear frequently enough to be obvious to the casual observer and interfere with functioning in a variety of contexts. |
| Level 1 | Without supports in place, deficits in social communication cause noticeable impairments. Difficulty initiating social interactions, and clear examples of atypical or unsuccessful response to social overtures of others. May appear to have decreased interest in social interactions. For example, a person who is able to speak in full sentences and engages in communication but whose to- and-fro conversation with others fails, and whose attempts to make friends are odd and typically unsuccessful. | Inflexibility of behavior causes significant interference with functioning in one or more contexts. Difficulty switching between activities. Problems of organization and planning hamper independence. |
Social (Pragmatic) Communication Disorder
Diagnostic Criteria
A. Persistent difficulties in the social use of verbal and nonverbal communication as manifested by all of the following:
- Deficits in using communication for social purposes, such as greeting and sharing information, in a manner that is appropriate for the social context.
- Impairment of the ability to change communication to match context or the needs of the listener, such as speaking differently in a classroom than on the playground, talking differently to a child than to an adult, and avoiding use of overly formal language.
- Difficulties following rules for conversation and storytelling, such as taking turns in conversation, rephrasing when misunderstood, and knowing how to use verbal and nonverbal signals to regulate interaction.
- Difficulties understanding what is not explicitly stated (e.g., making inferences) and nonliteral or ambiguous meanings of language (e.g., idioms, humor, metaphors, multiple meanings that depend on the context for interpretation).
B. The deficits result in functional limitations in effective communication, social participation, social relationships, academic achievement, or occupational performance, individually or in combination.
C. The onset of the symptoms is in the early developmental period (but deficits may not become fully manifest until social communication demands exceed limited capacities).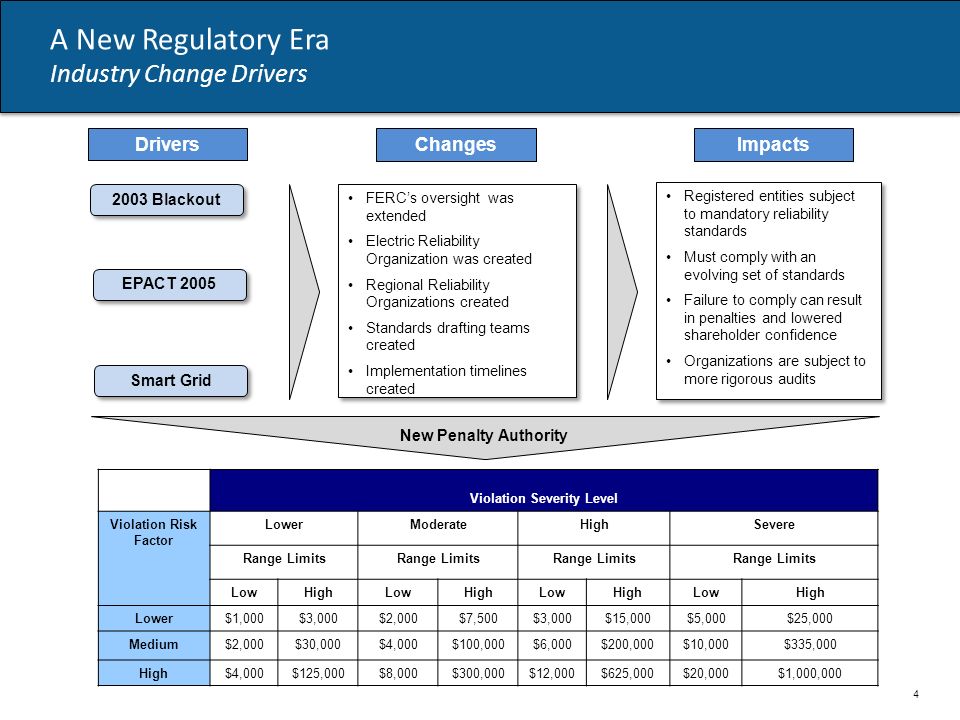
D. The symptoms are not attributable to another medical or neurological condition or to low abilities in the domains or word structure and grammar, and are not better explained by autism spectrum disorder, intellectual disability (intellectual developmental disorder), global developmental delay, or another mental disorder.
For more information
DSM-5 and Autism: Frequently Asked Questions
The 3 Levels of Autism Explained
Autism is a diagnosis that often carries a certain connotation. Those who are unfamiliar with the nuances of autism spectrum disorder (ASD) may assume that all children on the spectrum participate in repetitive behaviors, don’t make eye contact, and are largely non-verbal. While these signs can certainly be present, there are many children who fall within the spectrum whose symptoms are far milder and even those whose symptoms are more severe. It’s a wide and diverse range of possible complications, and despite what some may think, children within the spectrum do not all fall into neat little categories.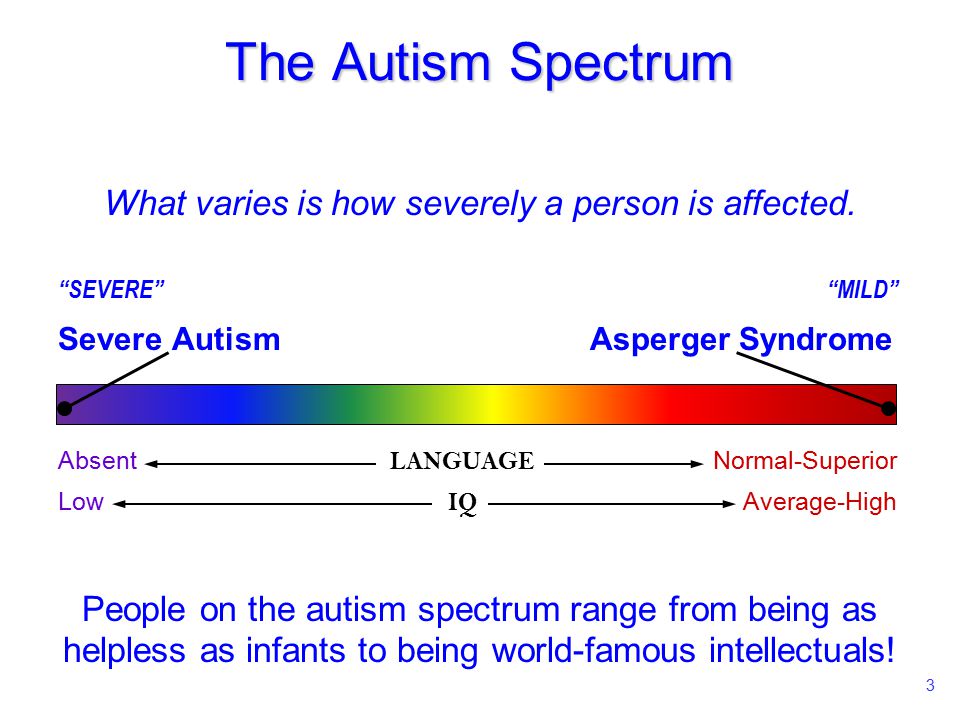 For that reason, the classifications of ASD have changed significantly over the years.
For that reason, the classifications of ASD have changed significantly over the years.
Much of the misconception surrounding ASD comes from terminology that was used prior to 2013. In this prior classification system, children fell into one of the following three categories:
- Autistic Disorder – More severe cases of ASD were previously classified as autistic disorder. The condition was often defined by communication troubles, repetitive behaviors, and social challenges among other symptoms.
- Asperger’s Syndrome – On the opposite end of the spectrum was Asperger’s syndrome which was characterized by milder symptoms which may impact an individual’s communication or social skills.
- Pervasive Development Disorder, Not Otherwise Specified (PDD-NOS)
– For children who fell in the middle and didn’t fully meet the requirements for either autistic disorder or Asperger’s, a diagnosis of PDD-NOS was often given.
While the old system of classification may seem a little more cut-and-dried, the subtle differences that often distinguished one from the other left room for a lot of confusion and much was open to interpretation. To address this, ASD is now categorized into three different levels, indicating what level of support a patient may need.
- ASD Level 1 – Level 1 ASD is currently the lowest classification. Those on this level will require some support to help with issues like inhibited social interaction and lack of organization and planning skills.
- ASD Level 2 – In the mid-range of ASD is Level 2. In this level, individuals require substantial support and have problems that are more readily obvious to others. These issues may be trouble with verbal communication, having very restricted interests, and exhibiting frequent, repetitive behaviors.
- ASD Level 3 – On the most severe end of the spectrum is Level 3 which requires very substantial support.
 Signs associated with both Level 1 and Level 2 are still present but are far more severe and accompanied by other complications as well. Individuals at this level will have limited ability to communicate and interact socially with others.
Signs associated with both Level 1 and Level 2 are still present but are far more severe and accompanied by other complications as well. Individuals at this level will have limited ability to communicate and interact socially with others.
Parents of a child with suspected or diagnosed ASD need the support of a knowledgeable and understanding pediatrician. At Lane Pediatrics, our physicians fit the bill with experienced, compassionate, and comprehensive care. Learn more about them and our pediatric services by clicking below.
Autism Spectrum Disorder: Levels, Symptoms, Risk Factors and Treatment
Autism Spectrum Disorder (ASD) is a spectrum neurodevelopmental disorder that affects about 1.7% of the population in the United States.
ASD is characterized by deficits in social and emotional reciprocity, language development, problem solving, or cognitive skills, as well as restrictive and repetitive behavior patterns, but the level of impairment may vary from patient to patient.
Levels of Autism
The new Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5) standardizes terms previously used to describe patients with different levels of need such as Asperger's syndrome etc. for a single diagnosis of ASD . .
As the new term implies, this is a spectrum of disorders that includes different manifestations and severity.
Once a child has been diagnosed with an autism spectrum disorder, the condition is graded by severity from level one to level three. Each level determines the severity of the symptoms and the degree of assistance the child needs to remain effective in the general social environment.
- Level 1 usually means a mild illness requiring minimal care and treatment.
- Level 2 is mild autism in terms of symptom severity and need for support.
- Level 3 means that the child will need more intensive assistance in daily life.
Causes and risk factors for autism spectrum disorder
The causes of ASD are multifactorial, from genetic predisposition to influences.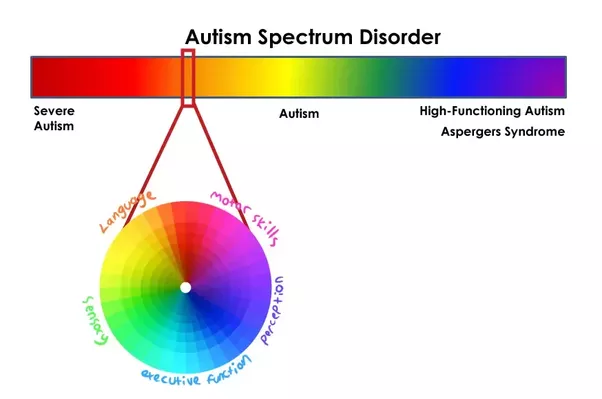 Food / Environment for vital illnesses.
Food / Environment for vital illnesses.
Several studies have attempted to link various acquired diseases, genes, diet and environmental factors to autism. While each study result has its merits, no study has been proven to be absolute.
Some working hypotheses for an increased risk of developing autism spectrum disorder include:
- Gender - Boys are four times more likely to develop the disorder than girls.
- Advanced paternal age at birth
- Folic acid deficiency during pregnancy
- Certain genetic disorders, including Down syndrome, Rett syndrome, and fragile X syndrome.
General symptoms of autism spectrum disorder
ASD is a disease with a genetic and neurological basis that manifests itself as behavioral problems. Behavioral fears are often rooted in a child's inherent disability caused by the illness itself.
1. Lack of social and emotional reciprocity.
The lack of social and emotional reciprocity makes the child very awkward in communication.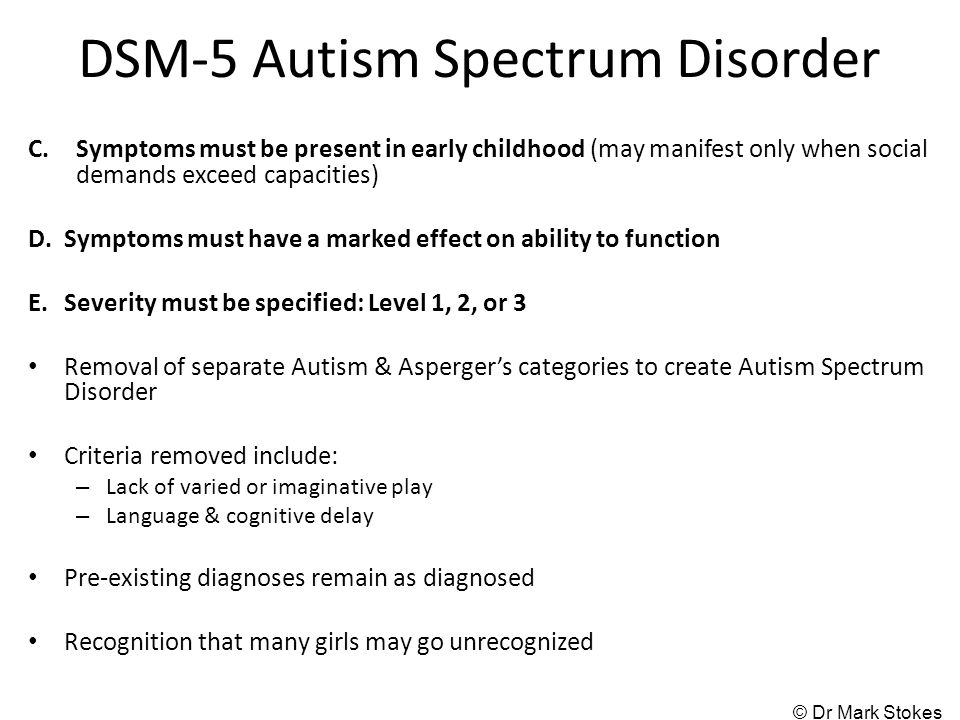 During infancy, they often find it difficult to bond with their parents. Young children are often more interested in things than other people.
During infancy, they often find it difficult to bond with their parents. Young children are often more interested in things than other people.
Most children with autism never develop proper eye contact or show no eye contact at all. At an early age, these children also do not have the ability to indicate demand or show interest.
As soon as a child grows up, at primary school age, his peers consider him clumsy. They tend to constantly miss social cues, such as an inability to detect sarcasm, and are often the target of bullying among their peers.
In pop culture, a mild case of ASD appears in the movie Mean Girls, where Rachel McAdams sarcastically says to Lindsay Lohan, "You're so beautiful." However, Lohan learned about the sarcasm later in the film.
Sheldon Cooper showed a more severe case of ASD in The Big Bang Theory, as he can never detect ridicule from his peers and is always the butt of ridicule on the show.
2. Violation of language development.
As most experts agree, language development is closely related to social development. Children with autism tend to have speech delays.
Some warning signs of early speech delay: inability to babble by 6 months, inability to say "mom" and "dad" at 15 months, and inability to say a single word other than "mom" and "dad" at 18 months.
Speech is extremely important for the development of any child, especially for children with autism. It is generally accepted that the better a child's ability to speak, the better the overall prognosis for autism spectrum disorder.
3. Restrictive and repetitive behaviors
Restrictive and repetitive behaviors are the most stereotypical manifestations of autism portrayed in the media. Most children with autism spectrum disorder have some limiting and repetitive patterns, but the manifestations can vary markedly depending on the severity of the disorder.
Some of the repetitive behaviors are headbutting and walking on tiptoe. Meanwhile, restrictive behavior can manifest itself in different areas of life, from people who are picky about food, to the need for a very strict daily routine, and much more.
Meanwhile, restrictive behavior can manifest itself in different areas of life, from people who are picky about food, to the need for a very strict daily routine, and much more.
Because of the need for a strict daily routine, a child with autism usually has difficulty transitioning or adapting to any change in daily routine. They often have excessive tantrums and become very irritable during an attack.
Treatment for autism spectrum disorder
Children with autism spectrum disorder are usually treated by a multidisciplinary team that typically includes but is not limited to the following:
- physiotherapy
- practice therapy
- psychology
- Speech therapy
- Behavior Analysis Applied Therapy (ABA)
- These interventions help children with their daily activities.
The treatment of autism spectrum disorders is perhaps the most important treatment and the backbone of ASD treatment. ABA therapy helps children cope with maladaptive behavior. Most importantly, ABA therapy can help children with transitions, often using interrupted verbs and objects.
Diagnosis of Autism Spectrum Disorder
Autism Spectrum Disorder is diagnosed by analyzing the child's behavior and developmental patterns. Standard screening for autism for all children at 18- and 24-month-old visits is done using a standard parent questionnaire known as the Modified Toddler Autism Checklist (MCHAT).
Although MCHAT is an excellent testing tool, it is not very sensitive or specific. One study found MCHAT to have a sensitivity of 40%. (5) Even if the child has a positive MCHAT test, further evaluation with more comprehensive developmental tests such as ADOS is needed to confirm the diagnosis.
Lifestyle interventions to help children with autism
Here are some ways to create a safe and caring environment for children with autism:
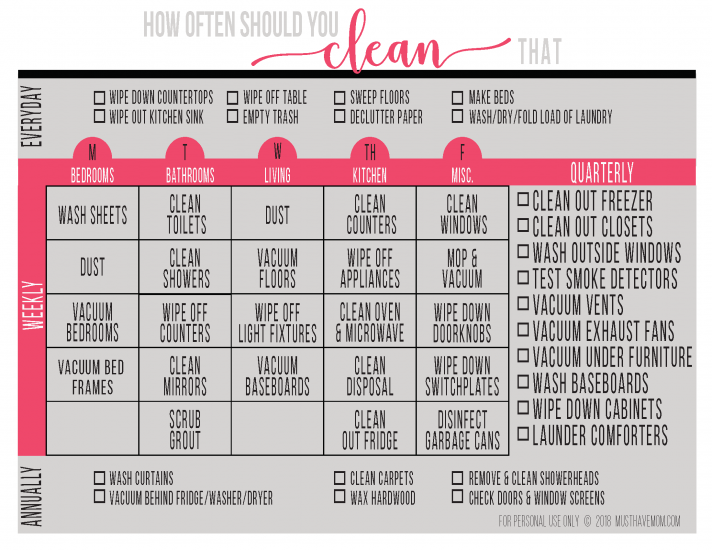
Establish a good daily routine and schedule for your child.
If your child has difficulty communicating or is prone to wandering, have them wear a health alert necklace or bracelet to keep an eye on them in case they get lost. You can also put an emergency form in your child's bag or pocket that contains your contact information and contact codes.
You can also put an emergency form in your child's bag or pocket that contains your contact information and contact codes.
Identify and develop your child's interests and hobbies. Getting your child involved in their favorite activities will help reduce repetitive behaviors and will also promote overall fitness. Some popular learning options include dance, yoga, jogging, horseback riding, and martial arts.
When will you see a doctor?
Your child's doctor should test for autism at 18 and 24 months of age. As mentioned above, the screening test is insensitive.
If your child develops any worrisome symptoms such as speech delay and severely inappropriate behavior, or if you have any suspicion of an autism spectrum disorder, bring your child to a medical office for immediate evaluation.
ASD Frequently Asked Questions
Can Diet Affect Autism Spectrum Disorder?
The basis of ASD treatment is an interdisciplinary treatment that includes physical therapy, occupational therapy, psychology, speech therapy and ABA.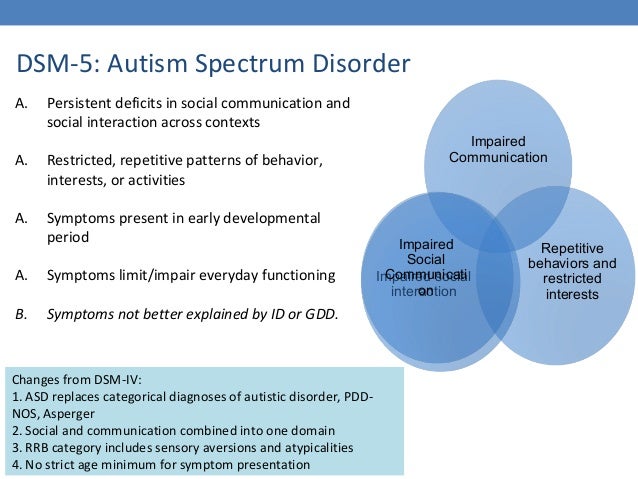
Although several studies have shown that various diets, such as the ketogenic diet, reduced sugar intake, and lower body mass index in general, have shown some interesting associations with ASD prevention, none have shown proven results for prevention. Thus, there are currently no specific diets that have been proven to prevent autism spectrum disorder.
Can autistic people live a normal life?
Yes, with the right treatment and social support, a person with autism can lead a normal life. With the right treatment, a child with autism can fulfill their potential and use their autism tendencies to their advantage in life and work.
Final word
There is no cure for autism spectrum disorder, but it can be managed with appropriate treatment and therapy to achieve an appropriate degree of functionality.
Children with autism have special needs, and caring for these needs is important around the clock for parents and caregivers, which can have negative consequences.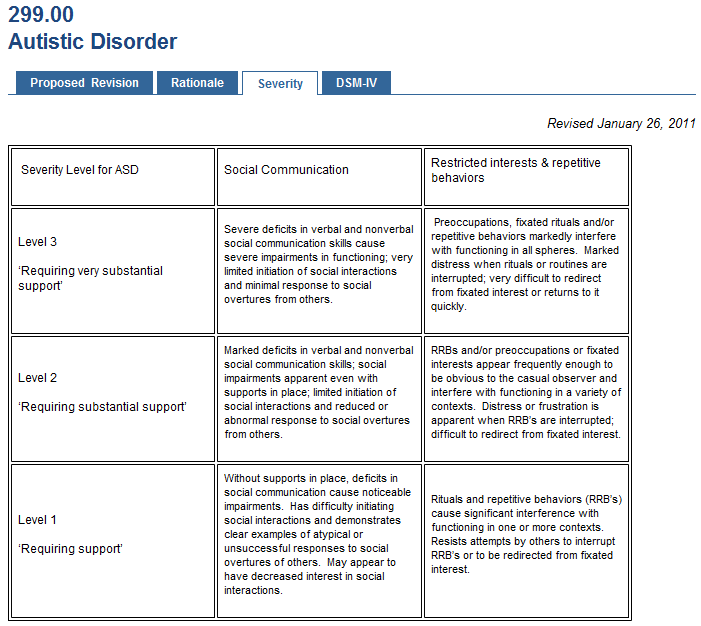 Therefore, as parents or guardians, it is important that you take care of your physical and emotional health without any guilt.
Therefore, as parents or guardians, it is important that you take care of your physical and emotional health without any guilt.
Neglecting your health will only damage your ability to care for a child and push you to the brink of exhaustion. To this end, you can join support groups and seek professional advice. In addition to self-education about the disorder and its issues, and the best way to deal with it through the appropriate channels, is the way forward.
James McCracken. Anxiety disorders in children. Symptoms, diagnosis, treatment methods
The three most common disorders in children are anxiety disorder, obsessive-compulsive disorder, and tics and Tourette's syndrome. They often accompany each other, while quite well amenable to correction and therapy. They can be treated both medically and with the help of psychological methods of intervention. Anxiety disorders are much more common in children than depression and obsessive-compulsive disorder, but they are not always recognized by specialists in time.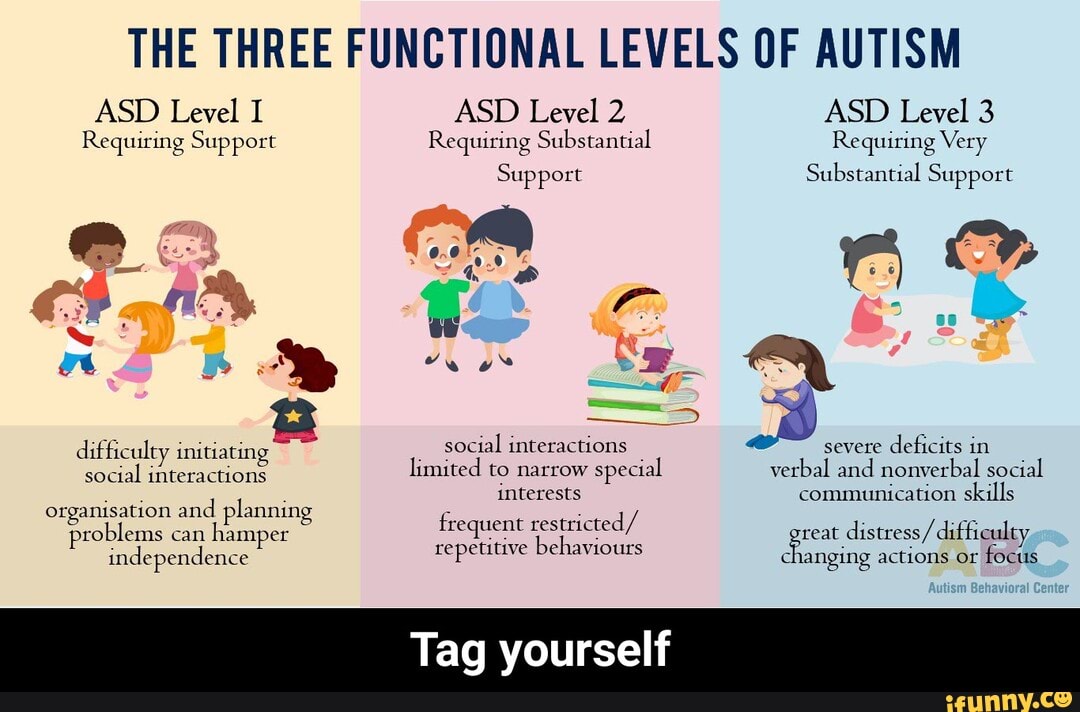 The reason for this is that children usually see a doctor already at school age, when the symptoms become more pronounced.
The reason for this is that children usually see a doctor already at school age, when the symptoms become more pronounced.
Three main types of anxiety disorders:
- Social anxiety disorder
- Separation anxiety disorder
- Specific phobias
These violations are quite serious, can lead to social exclusion and affect the life of children in all its aspects - from academic performance to family relationships. Children with anxiety disorders find it difficult to communicate with their peers at school, they avoid talking on the phone and are afraid of even a short separation from their parents (they ask mom and dad to always be in the same room with them, accompany them to the shower, etc.). They are also reluctant to enter into a conversation with strangers, feel awkward in a new environment, hide behind their parents when meeting people on the street or at a party, that is, in general, they are reluctant to make contact.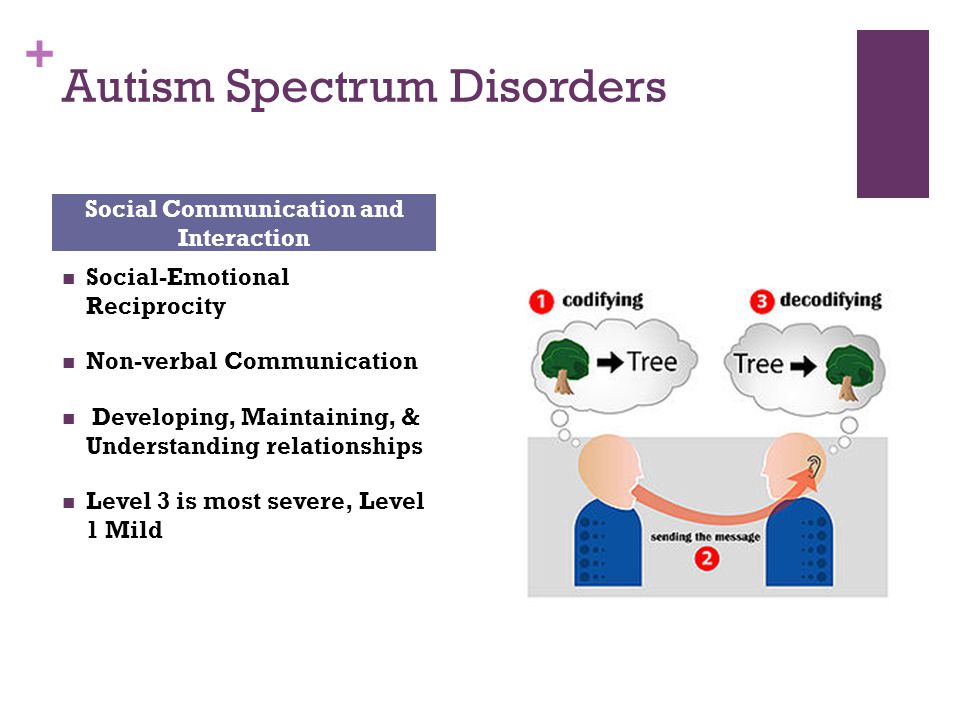
Early signs of anxiety in children:
- Extreme shyness and avoidance behavior at 2-4 years old (“behavioral depression”, Jerome Kagen)
- Selective mutism in the early school years
- Intolerance to separation from parents at kindergarten or schools
- Oppositional defiant behavior, irritability (these children are easily angered, annoyed, they often lose their temper)
- Heart palpitations, changes in the functioning of the autonomic nervous system, which lead to the release of stress hormones
-
The earlier anxiety disorders are diagnosed, the better the outcome of their treatment. It must also be remembered that the consequences of childhood anxiety can be very serious. In adulthood, such people are 3-4 times more at risk of depression and other mental illnesses. The average age of diagnosis is 10-13 years, but the first symptoms of disorders occur much earlier, at 2-3 years.
Diagnosis is complicated by the fact that anxiety disorders often coexist with other forms of anxiety (social phobia, generalized anxiety disorder, separation anxiety disorder, panic disorder, OCD, dysthymia, enuresis, ADHD, tic disorder, Tourette syndrome).
 For example, a person with few words of intelligible speech who rarely initiates interaction and, when he or she does, makes unusual approaches to meet needs only and responds to only very direct social approaches
For example, a person with few words of intelligible speech who rarely initiates interaction and, when he or she does, makes unusual approaches to meet needs only and responds to only very direct social approaches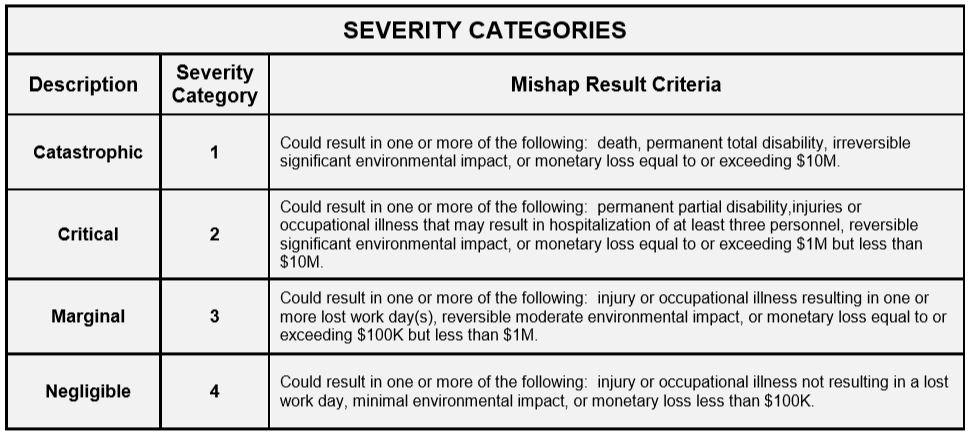 Distress and/or difficulty changing focus or action.
Distress and/or difficulty changing focus or action.