Are chest pains a symptom of anxiety
Are They Linked?: Woodlands Heart and Vascular Institute: Cardiologists
Anxiety and Chest Pain: Are They Linked?: Woodlands Heart and Vascular Institute: CardiologistsChest pain is a frightening experience that sends many people to the emergency room. Nearly half of them learn they don’t have a heart problem. Of those, 30-40% discover that anxiety was the culprit.
In short, anxiety and chest pain share a close relationship, but that doesn’t mean you can assume anxiety is to blame. You can’t risk delaying medical attention when there’s a chance you have a heart condition or you’re having a heart attack.
If you suspect you’re having a heart attack, call 911. Otherwise, Laura Fernandes, MD, FACC, at Woodlands Heart and Vascular Institute can run diagnostics in the office to rapidly determine if you have cardiovascular disease.
Learn how anxiety causes chest pain and if it’s possible to tell the difference between anxiety and heart-related symptoms.
Anxiety defined
Anxiety is your body’s natural reaction to a threat, whether the threat is immediate or in the future. Any time you feel anxious, your brain automatically sends out hormones that activate the fight-or-flight response.
Whether you’re stuck in traffic, worried about a job interview, or face a threatening situation, your brain’s natural reaction energizes your body so you can deal with the threat or quickly react and escape the situation.
How anxiety causes chest pain
When you’re anxious, your brain sends a surge of adrenaline and cortisol through your body. These hormones immediately trigger a rapid rise in your heart rate and blood pressure. As a result, many people experience chest pain and sweating, or have a hard time breathing.
The sudden boost of adrenaline can narrow the arteries in your heart and attach to cells inside the heart. This condition, called stress cardiomyopathy, mimics a heart attack, from symptoms all the way down to changes in your heart’s electrical activity.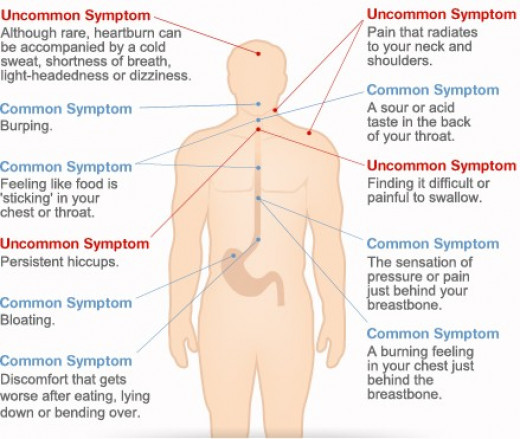
Though stress cardiomyopathy usually heals within a few days or weeks, it may lead to weak heart muscles, congestive heart failure, and abnormal heart rhythms.
Levels of adrenaline and cortisol don’t return to normal in people with anxiety disorders such as generalized anxiety disorder, panic disorder, and post-traumatic stress disorder. Chronically high hormone levels may trigger a panic attack (causing symptoms that feel like a heart attack) and increase your risk of cardiovascular disease.
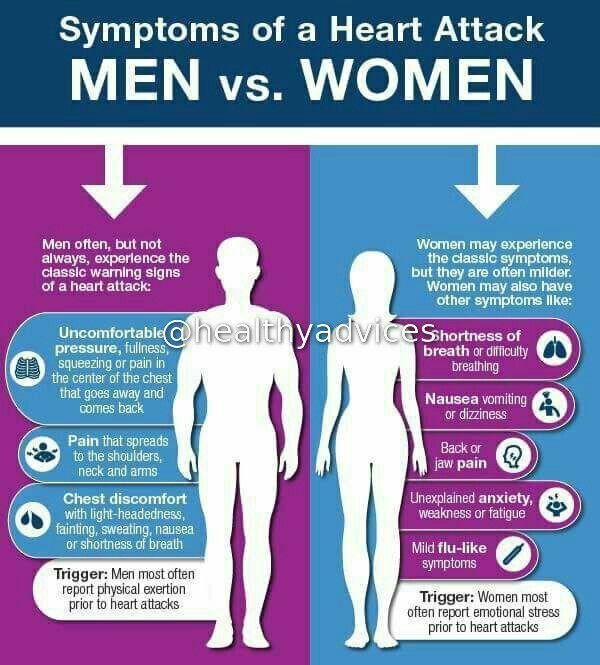
Symptoms of anxiety vs. cardiac chest pain
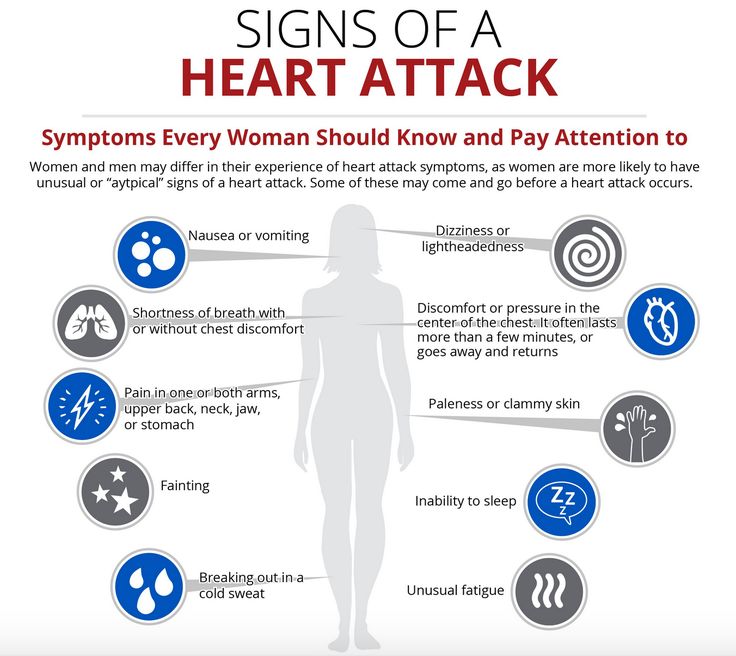
It’s hard, if not impossible, to tell the difference between anxiety-induced chest pain and the pain caused by an underlying heart condition. In addition to your chest pain, both can cause:
- Dizziness
- Shortness of breath
- Sweating
- Heart palpitations
- Feeling of dread or being out of control
Everyone experiences slightly different symptoms, whether they have anxiety or a heart problem.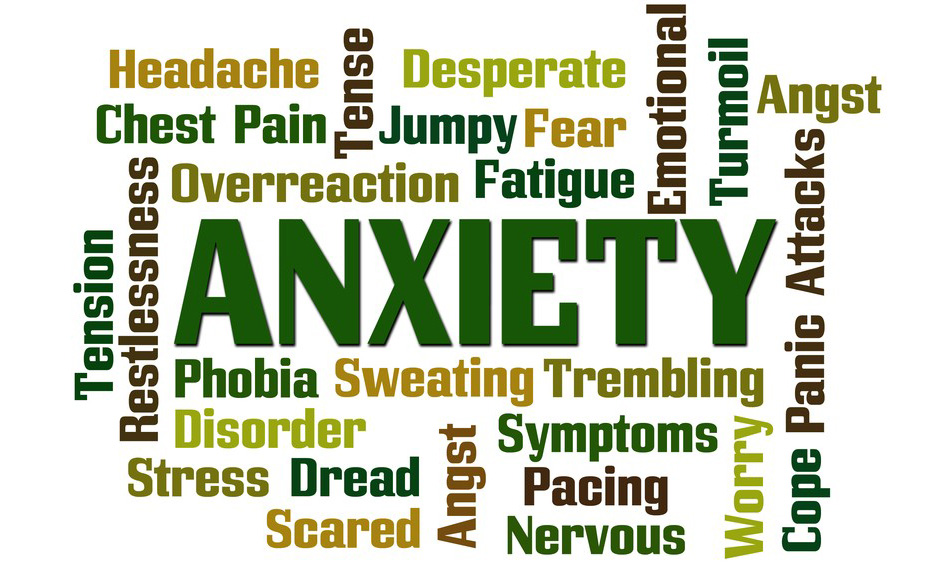 For this reason, the following two qualities aren’t written in stone. However, they’re generally true and may help you determine the cause of your chest pain:
For this reason, the following two qualities aren’t written in stone. However, they’re generally true and may help you determine the cause of your chest pain:
Pain location
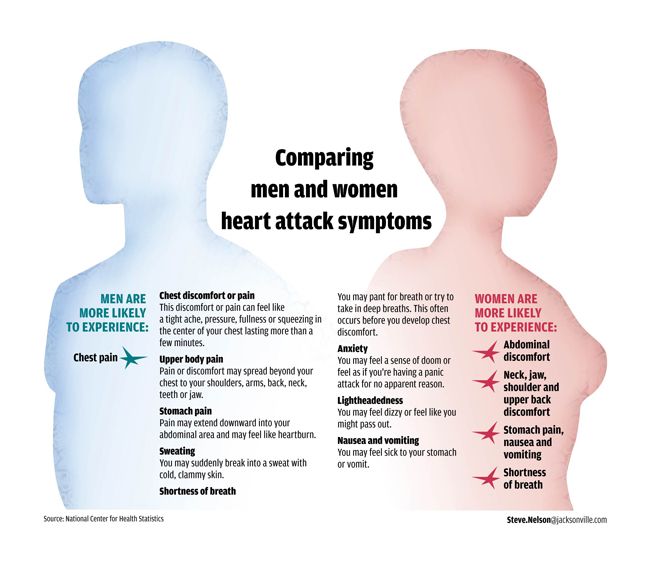
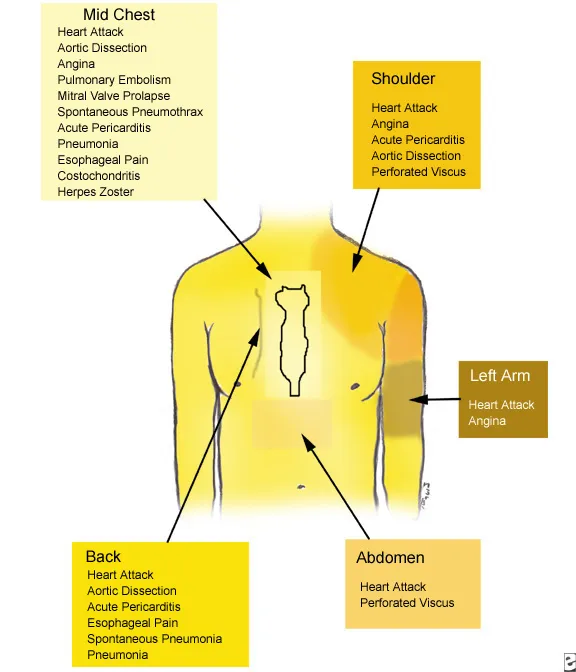
Chest pain from a heart attack often spreads throughout your chest and radiates to your jaw, shoulders, and arms. By comparison, chest pain from anxiety stays in your chest.
Pain patterns
Chest pain from a heart attack starts slowly and gradually gets worse, while an anxiety attack causes sudden chest pain that slowly improves. Many people find that anxiety-related chest pain goes away in about 10 minutes. However, other anxiety-related symptoms can last up to an hour after the pain improves.
If you have any questions about chest pain or other heart-related symptoms, call our office in The Woodlands, Texas,or schedule an appointment online today.
Five Foods That Promote Positive Heart Health
Your diet has the power to prevent heart disease and relieve the stress on your heart after you’re diagnosed with a cardiovascular condition.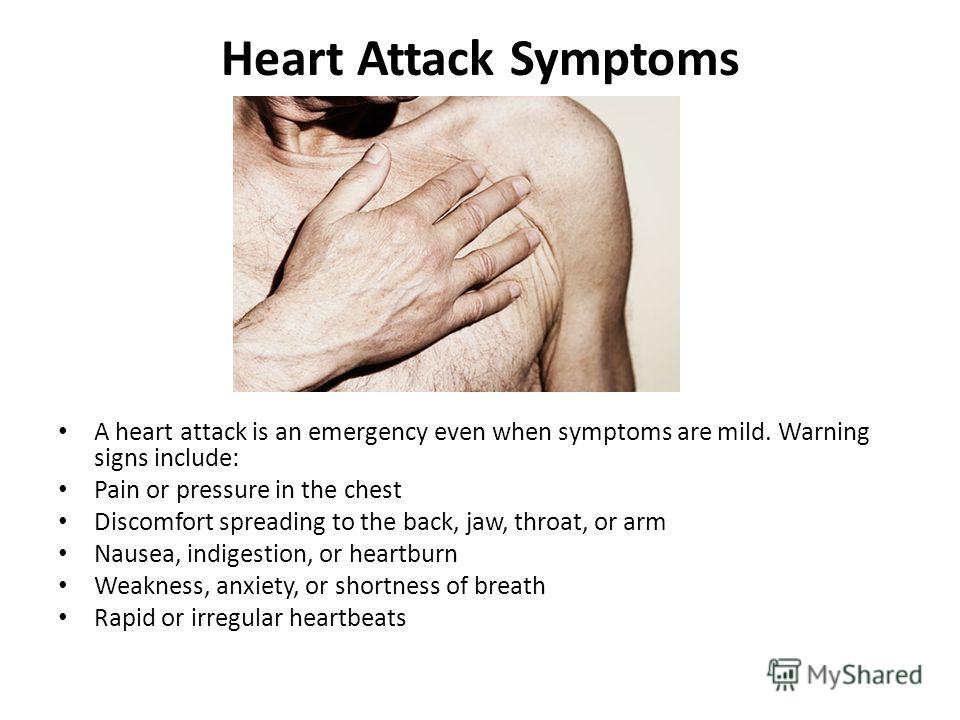 We share five exceptional foods and how they can help promote a healthy heart.
We share five exceptional foods and how they can help promote a healthy heart.
What Can You Learn From an Echocardiogram?
If you have symptoms of a heart problem, chances are you’ll need an echocardiogram. Echocardiograms are safe and fast, quickly providing exceptional images used to diagnose heart problems and make treatment decisions.
Understanding Your Treatment Options for Atrial Fibrillation
Atrial fibrillation is the most common type of heart arrhythmia, but there’s good news: Getting treatment can restore normal heart rhythm for most people. Here’s a rundown of the treatments used to control atrial fibrillation.
5 Habits That Raise Your Risk of Varicose Veins
Everyone hates the appearance of varicose veins, but many don’t realize they can take steps to prevent them.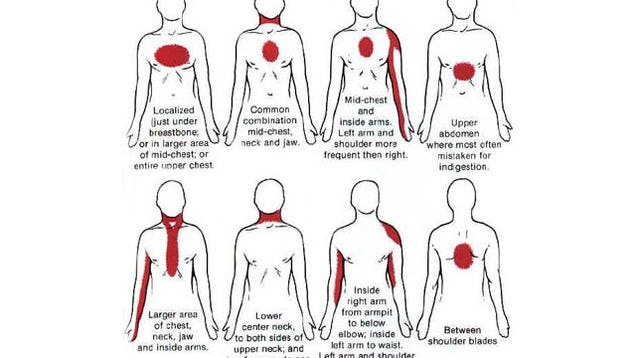 You can lower your risk by learning about and changing the lifestyle habits that contribute to varicose veins.
You can lower your risk by learning about and changing the lifestyle habits that contribute to varicose veins.
How To Manage Your Mental Health After a Heart Attack
Heart attacks do more than affect your physical health. They also take a toll on your mental health. Depression is such a common problem after a heart attack that the American Heart Association recommends routine screening.
Five Foods That Can Help Lower Your Blood Pressure
The foods you eat have such a dramatic impact on your cardiovascular health that dietary changes can help lower your blood pressure. Learn about five foods and the nutrients they contain that may help reduce blood pressure.
What It Feels Like, Causes, and Remedies
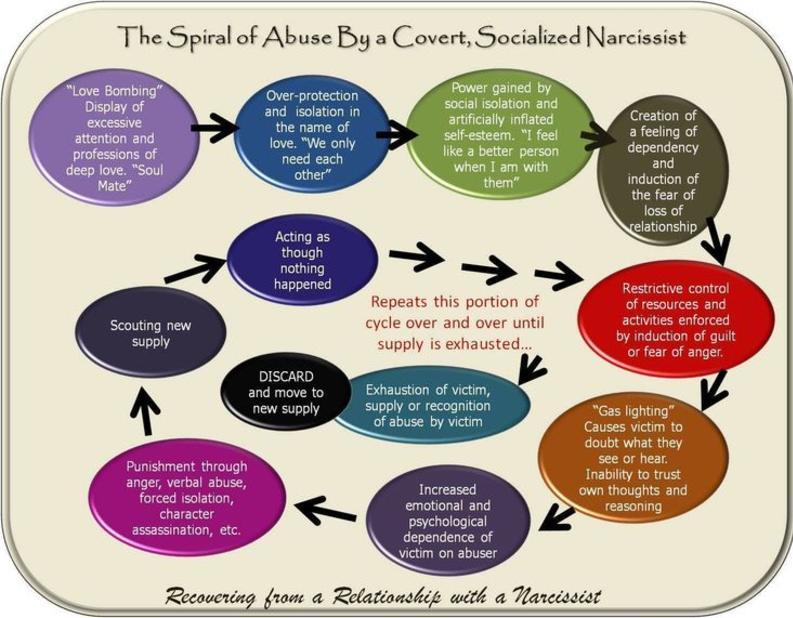
Feeling worried, fearful, or nervous from time to time is quite normal for most people. These are typical reactions to atypical moments in everyday life.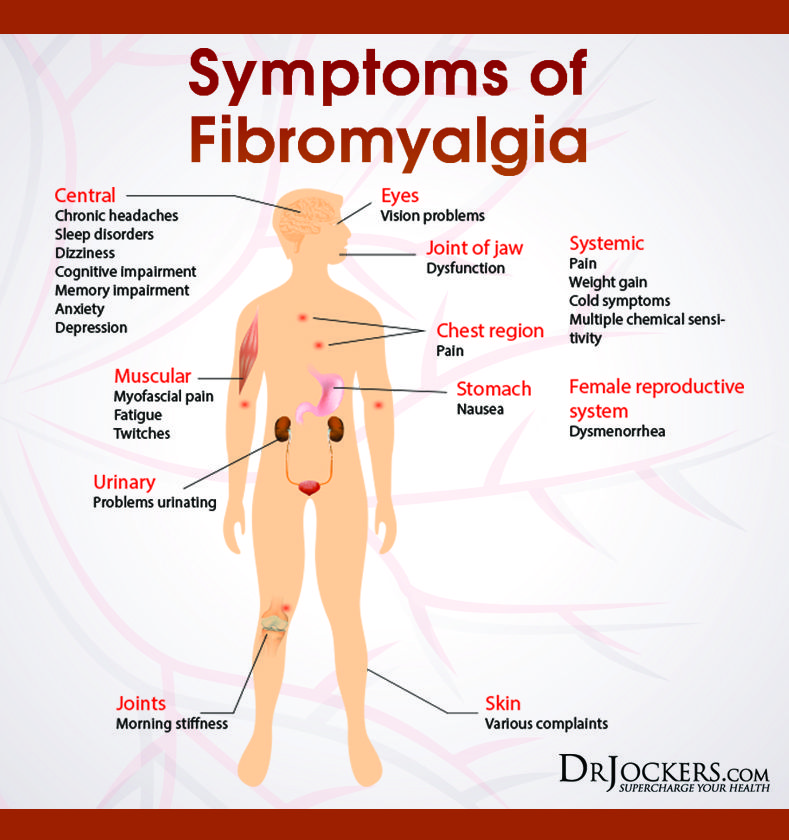
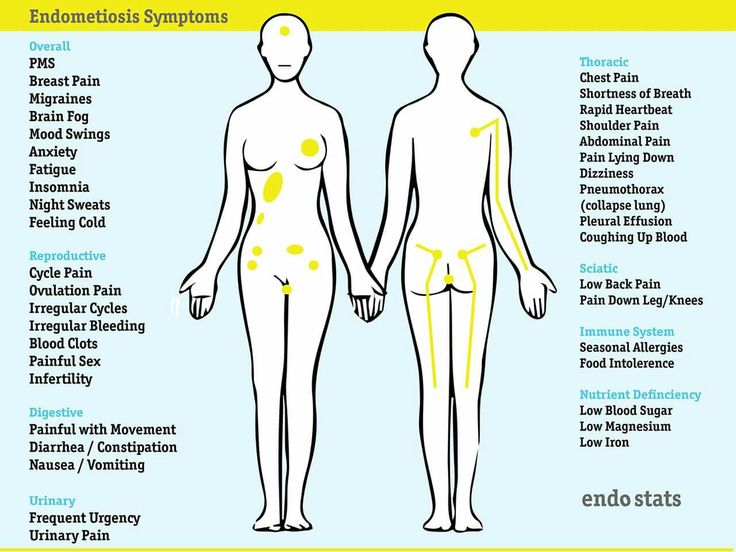
Some people experience anxiety frequently. Symptoms can move beyond feelings of concern or worry to other physical reactions. Occasionally, these symptoms are mistakenly associated with other conditions.
As an example, chest pain is sometimes a symptom of anxiety. Often the result of a panic attack or heightened reaction, chest pain is a concern because of the possible connection to heart attacks and other heart conditions.
If you experience frequent anxiety, learning to understand your chest pain can help you find symptom relief and identify when you need additional medical help.
Anxiety symptoms are rarely the same from person to person. Some days, symptoms aren’t even the same for the same person. Anxiety presents itself in a variety of ways, and that makes detecting or understanding symptoms difficult.
Chest pain associated with anxiety feels different for each person. Some people may experience chest pain on a gradual basis. For others, the pain may be sudden and unexpected.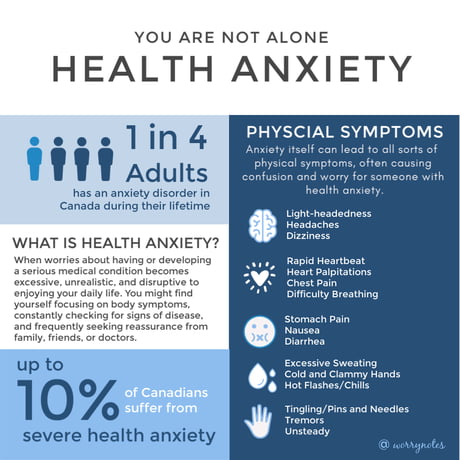 Anxiety chest pain can be described as:
Anxiety chest pain can be described as:
- sharp, shooting pain
- persistent chest aching
- an unusual muscle twitch or spasm in your chest
- burning, numbness, or a dull ache
- stabbing pressure
- chest tension or tightness
If you don’t have a history of chest pain with anxiety, you may be alarmed. Many people assume they’re having a heart attack and go to the hospital’s emergency department for treatment.
An estimated 25 to 50 percent of patients who come to the emergency department with low risk chest pain (chest pain not related to a heart attack) experience moderate to severe anxiety, according to 2018 research.
If you visit a hospital emergency room and the doctors don’t find a specific cause for your chest pain, consider consulting with your doctor about other possible causes, including anxiety.
Chest pain is a concerning symptom, and it’s usually best to seek emergency medical attention if you’re experiencing it.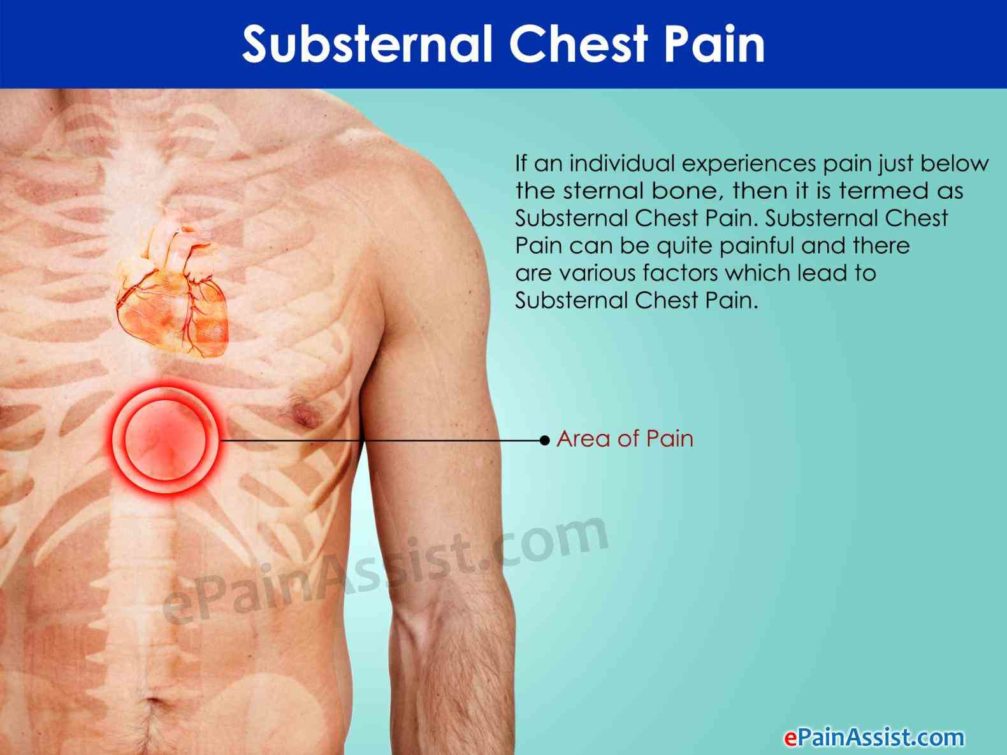 Even if the chest pain cause is anxiety, it’s better to know than to risk missing valuable time if you’re having a heart attack.
Even if the chest pain cause is anxiety, it’s better to know than to risk missing valuable time if you’re having a heart attack.
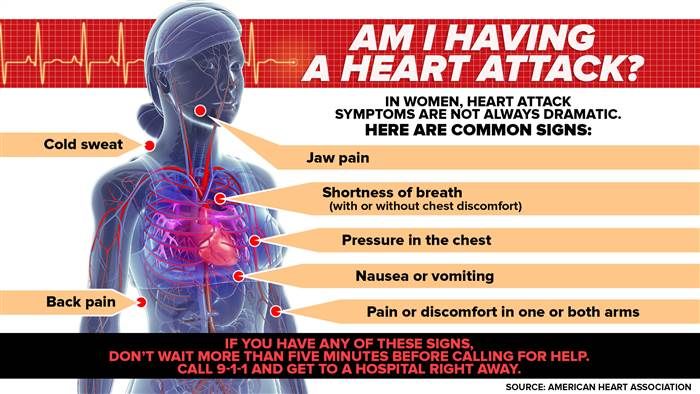
People describe chest pain in a number of ways when they’re having a heart attack. Some examples include:
- chest pain that radiates to other parts of your body, such as down your arms or up to your jaw
- chest pain that worsens with exertion
- nausea along with chest pain
- pressure in the chest, as if someone has put something heavy on your chest
- rapid heart rate
- shortness of breath
- squeezing sensation in the chest
An estimated 30 percent of patients who are having a heart attack don’t have chest pain, according to 2020 research. Some people report symptoms like back pain and fatigue as part of their heart attack symptoms.
While doctors know there is a connection between anxiety and chest pain, you still shouldn’t ignore your symptoms and seek medical attention.
Call your local emergency services if you’re having chest pain. Don’t attempt to drive yourself to the hospital. Emergency personnel can evaluate you and determine whether you’re having a cardiac event or if there’s another reason for your chest pain.
Don’t attempt to drive yourself to the hospital. Emergency personnel can evaluate you and determine whether you’re having a cardiac event or if there’s another reason for your chest pain.
When you’re anxious, your body can and often does produce physical reactions like sweating or shortness of breath.
When you become anxious, your brain and body set off an immediate stress response. This includes a physiological change. Your body may tighten up or grow tense.
A stress response can also include a psychological or emotional response. You may become aggressive or upset more easily. These responses are referred to as the fight-or-flight response. When you become stressed or anxious, your body prepares to fight back or run away.
If you experience this fight-or-flight stress reaction infrequently, your body should fully recover within 30 minutes. But if you experience it frequently, your body can’t recover as quickly. This can lead to increased muscle tension, and this tension may become painful in your chest.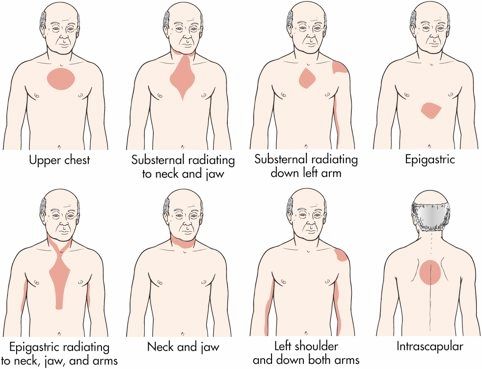
Likewise, in an even more stressful moment, your heart rate may increase, and the force of your heartbeats can grow stronger. That combined with tight chest muscles can make you feel unusual pain.
If you feel anxious, there are some simple techniques you can try. These techniques may not work every time, but they’re a great starting point when you need help managing your anxiety.
Practice deep breathing
Focused, deep breaths can calm both your mind and your body. Find a quiet room or area, and inhale for a count of 10. Hold for a second, and then exhale for a count of 10. Repeat this several times as you feel your heart rate fall.
Take stock of the situation
Accept your feelings of anxiety, recognize them, and then work through putting them in perspective.
Are you worried about something you can’t control? Are you fearful of an outcome that’s unlikely? Are you dreading a situation you can’t control the outcome of? Talk your way through your feelings to find the source, and then work to put them into perspective.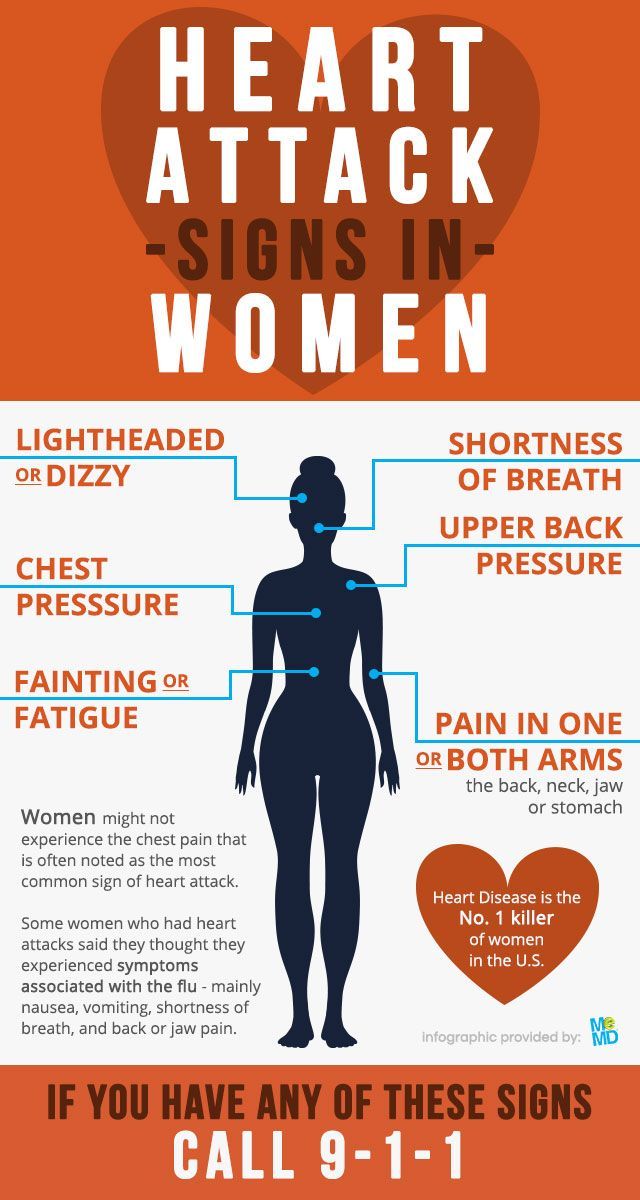
Picture a beautiful scene
If you’re feeling anxious, try visualizing a place that instantly calms you. This can be especially helpful if you’re feeling anxious while in a situation you can’t avoid, like a stressful meeting. Practice deep breathing while you envision this location.
Use a relaxation app
Smartphone apps for anxiety can walk you through stress reduction techniques and exercises. There are also meditation apps that may help you quiet your mind when you’re feeling anxious. Many of these apps are free, so you can try out several to find one that works for you.
Be proactive about your physical health
Are you taking good care of your body? Are you getting enough sleep? Are you eating well? Taking good care of your body is also taking good care of your mind. While this won’t help treat anxiety chest pain, it may help you reduce your risk for anxiety and subsequent chest pain in the future.
If your anxiety and chest pain are severe or chronic, you may need to consult with a therapist.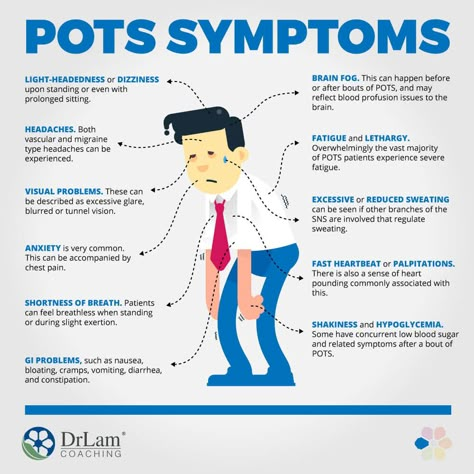 They can talk you through situations that cause anxiety and share coping techniques.
They can talk you through situations that cause anxiety and share coping techniques.
These techniques may not come naturally to you if you’re often anxious. This is where a healthcare professional can help.
A therapist or doctor may be able to teach you coping techniques that help you feel in control and secure. When you begin to regain a sense of calm, your symptoms, including chest pain, will subside.
If coaching techniques or mental exercises aren’t successful, you may need to consider a prescription. Anti-anxiety medications have side effects and risks. But using them as a stopgap while you learn how to cope with symptoms can be helpful.
Chest pain shouldn’t be ignored. If you’re experiencing it, seek medical attention to rule out a heart condition. If your chest pain is found to be related to anxiety, then you can work with a therapist or doctor to learn coping techniques or determine the best treatment for you.
Identifying anxiety as the cause of your chest pain is an important step in treating your condition.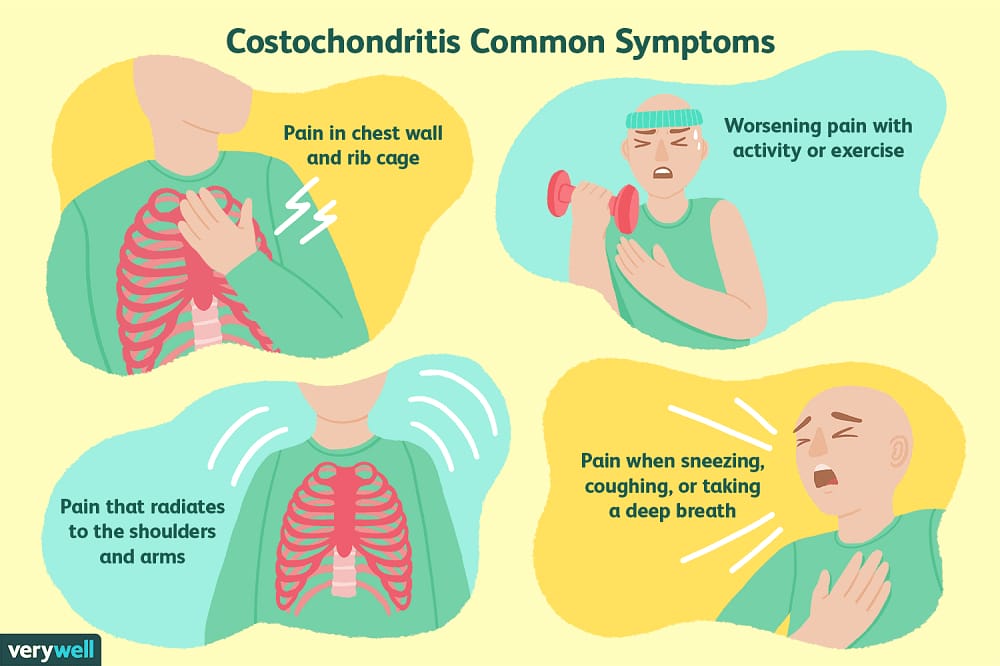 As you learn to manage the side effects of anxiety, you’ll also learn to manage unintended complications like chest pain.
As you learn to manage the side effects of anxiety, you’ll also learn to manage unintended complications like chest pain.
While you can’t know for sure if or when you’ll experience anxiety chest pain again, preparing yourself with coping techniques and practices will help you feel more prepared and in control.
Read this article in Spanish.
Chest pain - causes, examination and treatment | Symptoms
Myocardial infarction or unstable angina
Signs: Represent an immediate danger to life. Sudden, pressing pain that spreads (radiates) to the jaw or arm, may be constant or transient. Sometimes shortness of breath or nausea. Pain that comes on with exertion and goes away with rest (angina pectoris). Abnormal heart sounds heard through a stethoscope. Frequent warning signs.
Thoracic aortic dissection (tear in the wall of the thoracic aorta)
Signs: Represent an immediate danger to life. Sudden, tearing pain that extends into or begins in the middle of the back.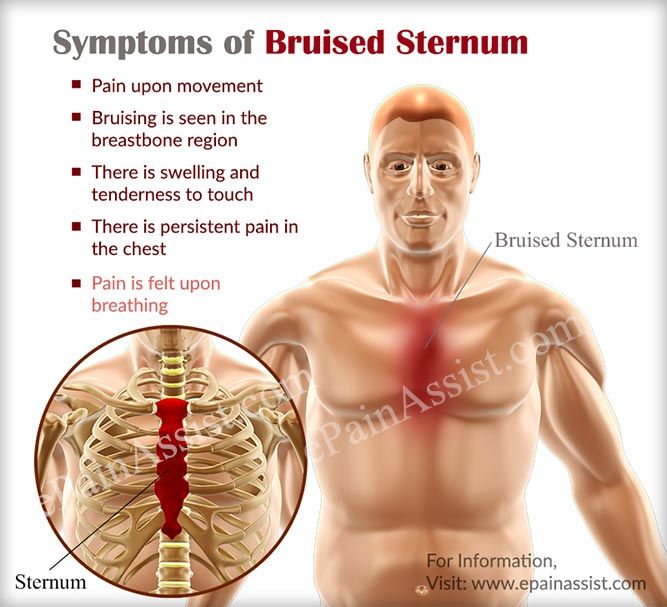 Sometimes dizziness, stroke, and pain, coldness, or numbness in the leg. Sometimes different pulse or blood pressure in the limbs. Usually in people over 55 with a history of high blood pressure. Warning signs.
Sometimes dizziness, stroke, and pain, coldness, or numbness in the leg. Sometimes different pulse or blood pressure in the limbs. Usually in people over 55 with a history of high blood pressure. Warning signs.
Pericarditis (inflammation of the lining around the heart)
Signs: Potentially life-threatening. Acute pain, constant or transient, aggravated by breathing, swallowing food, or lying on the back. Relaxes when leaning forward. Abnormal heart sounds heard through a stethoscope.
Spontaneous rupture of the esophagus
Signs: Represent an immediate danger to life. Sudden, sharp pain immediately after vomiting or after a medical procedure involving the esophagus (esophageal and gastric endoscopy or transesophageal echocardiography). Some warning signs.
Pancreatitis (inflammation of the pancreas)
Signs: Potentially life-threatening. Severe, persistent pain that: appears in the upper middle abdomen or lower chest. Often aggravated in the supine position, weakened by bending forward. Vomiting and soreness in the upper abdomen, sometimes shock. Often in people who abuse alcohol or have gallstones.
Often aggravated in the supine position, weakened by bending forward. Vomiting and soreness in the upper abdomen, sometimes shock. Often in people who abuse alcohol or have gallstones.
Peptic ulcers
Signs: Periodic vague discomfort that is felt in the upper middle of the abdomen or in the lower chest. Relief with antacids and sometimes after meals. Common in smokers and drinkers, or both. There are no warning signs.
Gastroesophageal reflux (GERD)
Signs: Periodic burning pain that spreads from the upper middle abdomen to the throat, worse when bending over or lying down. Relieves with antacids.
Diseases of the gallbladder and bile ducts (diseases of the biliary tract)
Signs: Intermittent discomfort, which is felt in the upper right side of the abdomen or in the lower middle of the chest, is observed after eating (but not after exercise).
Swallowing disorders (in which the peristalsis of food through the esophagus is impaired)
Signs: Pain that develops gradually over a long period of time may or may not appear during swallowing.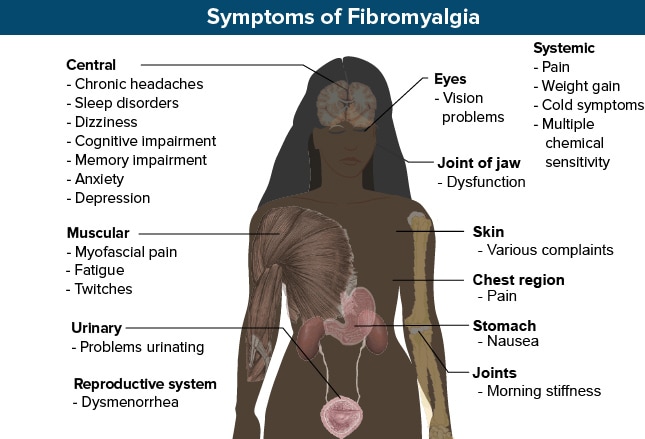 Usually difficulty swallowing.
Usually difficulty swallowing.
Pulmonary embolism (blockage of the pulmonary artery by a blood clot)
Signs: Represent an immediate danger to life. Often severe pain when breathing, shortness of breath, rapid breathing and rapid heartbeat. Sometimes a slight fever, coughing up blood, or shock. More likely in patients with risk factors for pulmonary embolism (history of blood clots, recent surgery, especially leg surgery, prolonged bed rest, leg cast or splint, older age, smoking, or cancer).
Tension pneumothorax (collapse of the lung with increased air pressure in the chest)
Signs: Represent an immediate danger to life. Significant shortness of breath. Low blood pressure, swollen neck veins, and decreased breath sounds heard through a stethoscope on one side. It usually occurs only after a severe chest injury.
Pneumonia
Signs: Potentially life-threatening. Fever, chills, cough, and usually yellow or green sputum. Often shortness of breath. Sometimes pain when breathing. Palpitations and congestion in the lungs revealed during the examination.
Often shortness of breath. Sometimes pain when breathing. Palpitations and congestion in the lungs revealed during the examination.
Pneumothorax (collapse of the lung)
Signs: Potentially life-threatening. Sudden sharp pain, usually in one side of the chest. Sometimes shortness of breath, weakening of breath sounds heard through a stethoscope on one side.
Pleurisy (inflammation of the lining around the lung)
Signs: Sharp pain when breathing. Usually in patients who have recently had pneumonia or a viral respiratory infection. Sometimes cough. There are no warning signs.
Musculoskeletal chest wall pain
Signs: Pain that is usually persistent (lasting a few days or more). Increases with movement and/or breathing. May have no apparent cause or result from coughing or physical exertion. Soreness at one point on the chest. There are no warning signs.
Fibromyalgia
Signs: Pain that is almost constant, spreads to large areas of the body, is usually accompanied by fatigue and impaired sleep quality.
Shingles
Signs: Acute girdle pain in the middle of the chest, but only on one side. Rash in the form of numerous small vesicles, sometimes filled with pus, in the area of localization of pain, sometimes arising after the onset of pain.
Malignant tumors of the chest or chest wall
Signs: Sometimes pain that worsens with inspiration. Sometimes chronic cough, history of smoking, weight loss, swollen lymph nodes in the neck.
Chest pain
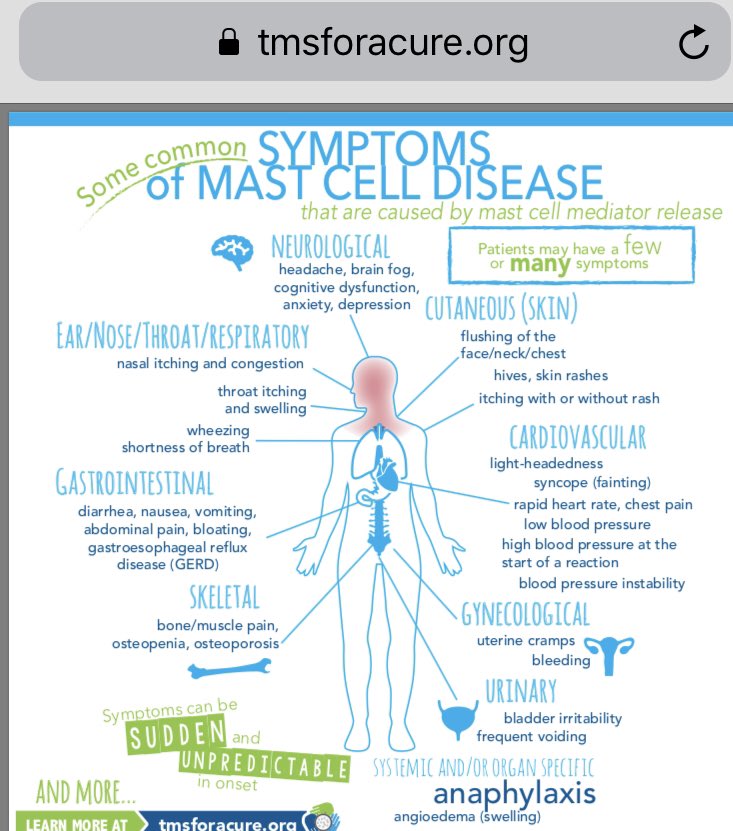
Chest pain is any pain or discomfort in the chest area. It can be caused by various diseases, including pathology of the heart, blood vessels, pericardium, lungs, pleura, trachea, esophagus, muscles, ribs, nerves. In some cases, chest pain is a sign of damage to organs outside the chest, such as the stomach, gallbladder, pancreas.
Thoracic pains are very varied: sharp, dull, aching, cutting, stitching, drawing, bursting, burning or pressure. Painful sensations differ in different diseases, but pain is not a specific symptom of a particular disease. Characteristics of pain may vary depending on the age, sex of the patient, concomitant diseases, psychological characteristics. Identifying the immediate cause of chest pain is often difficult and requires a series of diagnostic procedures.
Characteristics of pain may vary depending on the age, sex of the patient, concomitant diseases, psychological characteristics. Identifying the immediate cause of chest pain is often difficult and requires a series of diagnostic procedures.
It is one of the most alarming symptoms, as it can be a manifestation of severe, life-threatening conditions that require emergency medical attention, in particular myocardial infarction.
Russian synonyms
Thoracalgia, chest pain, chest pain
English synonyms
Chest pain, pain in the chest, thoracalgia.
Symptoms
Chest pain can be of different nature. Sometimes it is given in the arm, shoulder, shoulder blade, back, neck. The patient may complain not only of pain, but also of tightness, burning, discomfort in the chest area.
Unpleasant sensations may be aggravated by coughing, deep breathing, swallowing, pressure on the chest, changes in body position (permanent or intermittent).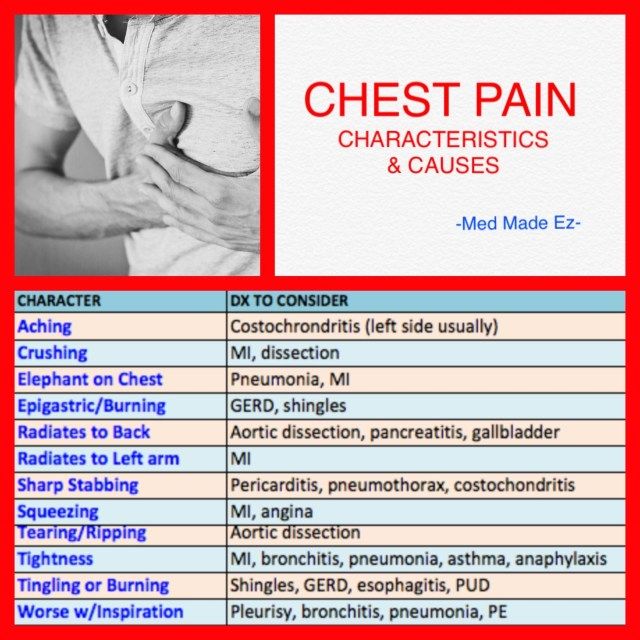 Pain and discomfort in the chest may be accompanied by a number of additional symptoms, depending on the underlying disease: belching or bitterness in the mouth, nausea, vomiting, difficulty swallowing.
Pain and discomfort in the chest may be accompanied by a number of additional symptoms, depending on the underlying disease: belching or bitterness in the mouth, nausea, vomiting, difficulty swallowing.
General information about the disease
Chest pain is a manifestation of various diseases, each of which requires a specific medical approach.
- Acute myocardial infarction (heart attack). Acute chest pain in people over 40 years of age is most often associated with this disease. Myocardial infarction occurs when damage and death of a portion of the myocardium as a result of impaired blood circulation in the coronary vessels. Most often, it is manifested by acute pain behind the sternum or to the left of the sternum, which is given to the back, neck, shoulder, arm and does not decrease when taking nitroglycerin or at rest. Symptoms vary from patient to patient. Elderly women are characterized by atypical symptoms: severe weakness, nausea and vomiting, rapid breathing, abdominal pain.

- Angina. A condition in which, as a result of atherosclerosis and narrowing of the coronary vessels, the blood supply to the heart muscle is disrupted. Pain in angina pectoris resembles that in myocardial infarction, but occurs during exercise, decreases at rest and is relieved by nitroglycerin.
- Dissecting aortic aneurysm. The aorta is a large vessel that carries blood from the left ventricle of the heart to organs and tissues. With a dissecting aneurysm, the intima (inner lining) of the aorta ruptures with blood penetrating into other layers of the aortic wall and subsequent dissection of the wall, which most often leads to complete rupture of the aorta and massive internal bleeding. The disease in most cases ends in death within a few hours or days, even with timely diagnosis and timely treatment.
Dissecting aortic aneurysm is most often the result of long-term arterial hypertension, and can also occur with Marfan syndrome, as a result of chest trauma, during pregnancy, or as a late complication of heart surgery.
The pain of a dissecting aortic aneurysm is similar to that of myocardial infarction and angina pectoris, may last for hours or days, and is not relieved by rest or nitroglycerin.
- Pulmonary embolism. Blockage by a thrombus of the pulmonary artery or its branches, through which venous blood flows from the right ventricle to the lungs for oxygenation. As a result, gas exchange is disturbed, hypoxia occurs, and pressure in the pulmonary arteries increases. Chest pain occurs suddenly, increases with deep inspiration, is accompanied by rapid breathing and, in some cases, hemoptysis. The risk of thromboembolism increases after surgery, prolonged immobility, during pregnancy, taking oral contraceptives, especially in combination with smoking, and with oncological diseases.
- Pneumothorax. The accumulation of air or other gas in the pleural cavity - a slit-like space between the membranes lining the surface of the lungs and the inner surface of the chest.
 Accompanied by acute chest pain, rapid breathing, anxiety, loss of consciousness.
Accompanied by acute chest pain, rapid breathing, anxiety, loss of consciousness. - Pericarditis. Inflammation of the heart sac (pericardium), that is, the serous membrane of the heart. Pain occurs due to friction of the inflamed sheets of the pericardium. Pericarditis may be due to a viral infection, rheumatoid arthritis, systemic lupus erythematosus, renal failure. Often there is idiopathic pericarditis, that is, pericarditis of unknown etiology. The pain is acute, occurs only in the initial stages of the disease, may be accompanied by rapid breathing, fever, and malaise.
- Mitral valve prolapse. Pathology of the valve, which is located between the left atrium and the left ventricle of the heart. In some people, when the left ventricle contracts, the mitral valve flexes into the atrium and some of the blood from the left ventricle flows back into the left atrium. In most patients, this does not cause discomfort, however, in some, the heart rate increases and chest pains appear, which do not depend on physical exertion and do not radiate, unlike angina pectoris.
- Pneumonia. Inflammation of the lung tissue. Chest pain in pneumonia is usually unilateral, aggravated by coughing, accompanied by fever, malaise, cough.
- Esophagitis. Inflammation of the esophagus. Accompanied by chest pain, swallowing disorder. Symptoms do not improve with antacids.
- Gastroesophageal reflux disease. A chronic disease in which the acidic contents of the stomach reflux into the esophagus, resulting in damage to the lower esophagus. In this case, there may be an acute, cutting pain in the chest along the esophagus, heaviness, discomfort in the chest, belching, bitterness in the mouth, impaired swallowing, dry cough.
- Pleurisy. Inflammation of the pleura. The friction of the inflamed pleura causes pain. Pleurisy can be the result of a viral or bacterial infection, cancer, chemotherapy or radiation therapy, rheumatoid arthritis.
- Fractured ribs. In this case, the pain increases with deep breathing and movement.
- Other causes: pancreatitis, cholelithiasis, depression.

Who is at risk?
- People over 40.
- Obese.
- Patients with arterial hypertension.
- People with elevated blood cholesterol levels.
- Recent surgery.
- Suffering from alcoholism.
- Smokers.
- Pregnant.
- Suffering from cardiac arrhythmia.
- People with cancer.
- Taking certain drugs.
- People with chronic lung disease.
Diagnosis
Chest pain is not a specific symptom and may clearly indicate a particular disease. However, when this sign appears, the doctor must first of all exclude a number of life-threatening conditions that require immediate help. Sometimes only additional laboratory and instrumental studies can accurately determine the cause of chest pain.
Laboratory tests
- Complete blood count. Leukocytosis (with pleurisy, pneumonia), anemia (with dissecting aortic aneurysm), thrombocytosis and erythremia (with pulmonary embolism) can be detected.
- Erythrocyte sedimentation rate (ESR). Nonspecific indicator of inflammation. ESR can be increased with pleurisy, pericarditis, pneumonia and other diseases.
- C-reactive protein. Increased in inflammatory diseases, as well as in myocardial infarction. With angina pectoris, the level of C-reactive protein does not change.
- NT-proBNP (sodium uretic brain propeptide). Protein, the main part of which is found in myocardial cells. It is the precursor of the natriuretic peptide responsible for the excretion of sodium in the urine. This indicator is used to assess the risk of heart failure, identify the initial stages of heart failure, and evaluate ongoing therapy. Is highly specific. May be elevated in myocardial infarction.
- Troponin I. Troponin is a protein involved in muscle contraction. The cardiac form of troponin is found in the heart muscle and is released when the myocardium is damaged. It can be increased in myocardial infarction and other diseases accompanied by the destruction of cardiomyocytes.
- Myoglobin. A protein similar in structure to hemoglobin and responsible for the deposition of oxygen in muscle tissue, including the heart muscle. Increases with damage to muscle tissue, in the first hours after myocardial infarction.
- Alanine aminotransferase (ALT). An enzyme that is found mainly in the liver, as well as in skeletal muscles, kidneys and myocardium. An increase in ALT indicates liver damage, but may also indicate myocardial infarction and serves as an indicator of the extent of damage to the heart muscle.
- Aspartate aminotransferase (AST). This enzyme is found mainly in the myocardium, skeletal muscles, and liver. An increase in AST levels is a sign of myocardial infarction. The value of AST corresponds to the degree of damage to the heart muscle.
- Creatine kinase total. An enzyme involved in energy metabolism reactions. Its various isoforms are found in different tissues of the human body. An increase in the level of total creatine kinase is observed in myocardial infarction and myopathies.
- Creatine kinase MB. An isoform of creatine kinase found primarily in the myocardium and tissues of the nervous system. Its level corresponds to the extent of myocardial damage.
- Lactate dehydrogenase (LDH) total. An enzyme that is involved in energy metabolism and is found in almost all tissues of the body. Different types of LDH are present in different organs. Total lactate dehydrogenase may be elevated in myocardial infarction and liver disease.
- Lactate dehydrogenase 1, 2 (LDH 1, 2 fractions). These are types of lactate dehydrogenase, the increase of which is a more specific indicator of myocardial and renal damage.
- Lipase. Enzyme of the pancreas. Elevated lipase levels are specific to pancreatic diseases.
- Cholesterol, total. This is the main indicator of fat metabolism in the body. It is used to diagnose atherosclerosis and liver diseases.
- D-dimer. fibrin cleavage product. It is an indicator of fibrinolytic activity of the blood.
 The level of D-dimer can change with pulmonary embolism, dissecting aortic aneurysm.
The level of D-dimer can change with pulmonary embolism, dissecting aortic aneurysm. - The main blood electrolytes are potassium, sodium, chlorine, calcium. A change in the level of blood electrolytes may indicate pathology of the kidneys, adrenal glands, endocrine diseases, and malignant neoplasms.
- Urea, serum creatinine. These are the end products of nitrogen metabolism, which are excreted from the body by the kidneys. Their increase may indicate kidney pathology.
Instrumental research methods
- Electrocardiography (ECG). ECG changes are detected in myocardial infarction, angina pectoris, pericarditis. Helps to determine the localization and degree of myocardial damage.
- X-ray, computed tomography (CT), magnetic resonance imaging (MRI), ultrasound examination (ultrasound) of the chest. These are imaging methods that allow you to assess the condition of the chest organs, identify injuries, neoplasms, signs of internal bleeding and other pathological changes.
- Transesophageal echocardiography. An ultrasound scan in which a transducer is inserted into the esophagus. With its help, the state of the heart, its valves, and large vessels are assessed. It is of great diagnostic value in pulmonary embolism, aortic aneurysm.
- Angiography. X-ray examination of blood vessels using a non-toxic contrast agent, clearly visible on the pictures. Allows you to assess the condition and patency of blood vessels, including coronary ones.
Treatment
Treatment depends on the underlying disease, the symptom of which is chest pain. Therapy can consist of both the use of appropriate drugs and surgical procedures.
Prevention
There is no specific prophylaxis for most chest pain conditions. However, to reduce the risk of their development, quitting smoking and alcohol, sufficient physical activity, a healthy diet, and timely preventive medical examinations are useful.