Antidepressant without side effects
Overview - SSRI antidepressants - NHS
Selective serotonin reuptake inhibitors (SSRIs) are a widely used type of antidepressant.
They're mainly prescribed to treat depression, particularly persistent or severe cases, and are often used in combination with a talking therapy such as cognitive behavioural therapy (CBT).
SSRIs are usually the first choice medicine for depression because they generally have fewer side effects than most other types of antidepressant.
As well as depression, SSRIs can be used to treat a number of other mental health conditions, including:
- generalised anxiety disorder (GAD)
- obsessive compulsive disorder (OCD)
- panic disorder
- severe phobias, such as agoraphobia and social phobia
- bulimia
- post-traumatic stress disorder (PTSD)
SSRIs can sometimes be used to treat other conditions, such as premenstrual syndrome (PMS), fibromyalgia and irritable bowel syndrome (IBS). Occasionally, they may also be prescribed to treat pain.
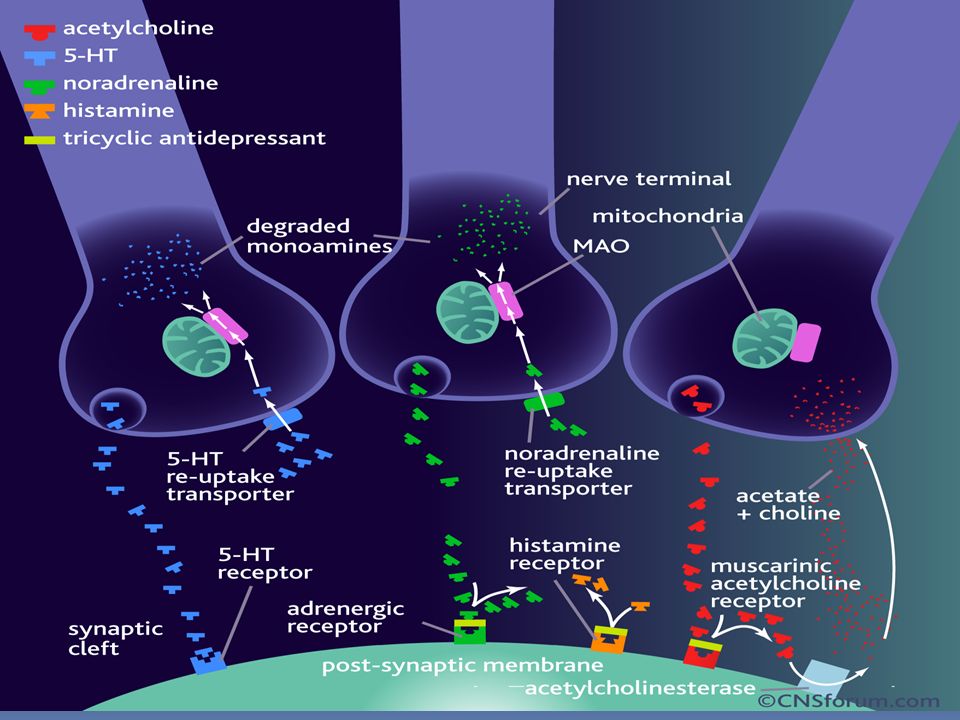
How SSRIs work
It's thought that SSRIs work by increasing serotonin levels in the brain.
Serotonin is a neurotransmitter (a messenger chemical that carries signals between nerve cells in the brain). It's thought to have a good influence on mood, emotion and sleep.
After carrying a message, serotonin is usually reabsorbed by the nerve cells (known as "reuptake"). SSRIs work by blocking ("inhibiting") reuptake, meaning more serotonin is available to pass further messages between nearby nerve cells.
It would be too simplistic to say that depression and related mental health conditions are caused by low serotonin levels, but a rise in serotonin levels can improve symptoms and make people more responsive to other types of treatment, such as CBT.
Doses and duration of treatment
SSRIs are usually taken in tablet form. When they're prescribed, you'll start on the lowest possible dose thought necessary to improve your symptoms.
When they're prescribed, you'll start on the lowest possible dose thought necessary to improve your symptoms.
SSRIs usually need to be taken for 2 to 4 weeks before the benefit is felt. You may experience mild side effects early on, but it's important that you don't stop taking the medicine. These effects will usually wear off quickly.
If you take an SSRI for 4 to 6 weeks without feeling any benefit, speak to your GP or mental health specialist. They may recommend increasing your dose or trying an alternative antidepressant.
A course of treatment usually continues for at least 6 months after you feel better, although longer courses are sometimes recommended and some people with recurrent problems may be advised to take them indefinitely.
Things to consider
SSRIs aren't suitable for everyone. They're not usually recommended if you're pregnant, breastfeeding or under 18, because there's an increased risk of serious side effects.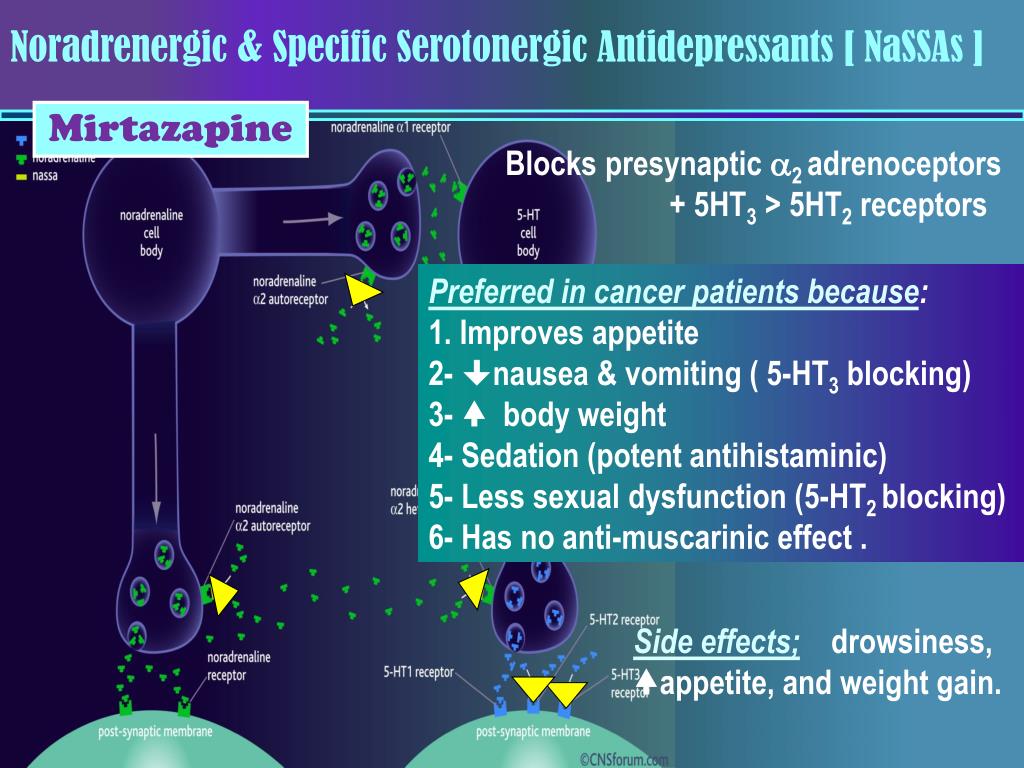 However, exceptions can be made if the benefits of treatment are thought to outweigh the risks.
However, exceptions can be made if the benefits of treatment are thought to outweigh the risks.
SSRIs also need to be used with caution if you have certain underlying health problems, including diabetes, epilepsy and kidney disease.
Some SSRIs can react unpredictably with other medicines, including some over-the-counter painkillers and herbal remedies, such as St John's wort. Always read the information leaflet that comes with your SSRI medicine to check if there are any medicines you need to avoid.
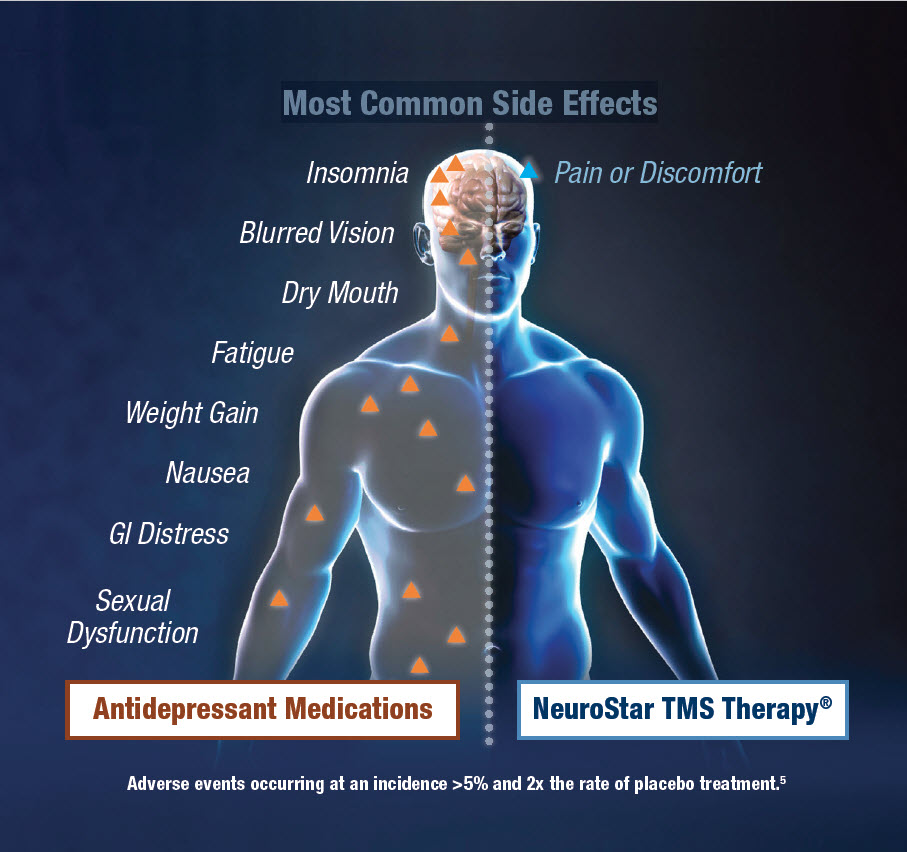
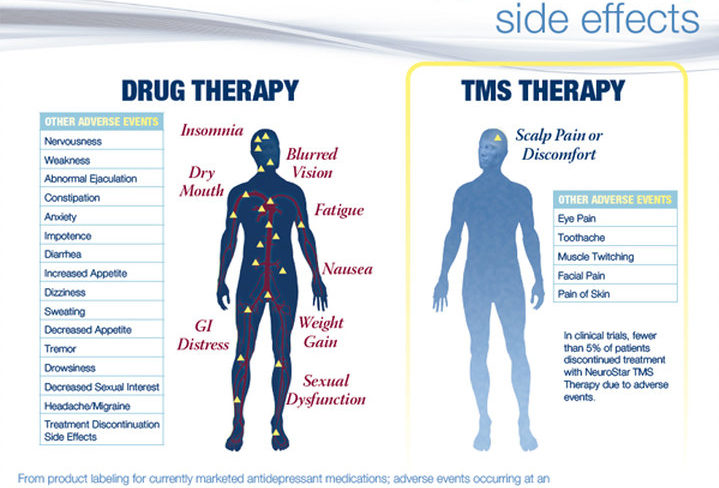
Side effects
Most people will only experience a few mild side effects when taking SSRIs. These can be troublesome at first, but they'll generally improve with time.
Common side effects of SSRIs can include:
- feeling agitated, shaky or anxious
- diarrhoea and feeling or being sick
- dizziness
- blurred vision
- loss of libido (reduced sex drive)
- difficulty achieving orgasm during sex or masturbation
- in men, difficulty obtaining or maintaining an erection (erectile dysfunction)
You'll usually need to see your doctor every few weeks when you first start taking SSRIs to discuss how well the medicine is working. You can also contact your doctor at any point if you experience any troublesome or persistent side effects.
You can also contact your doctor at any point if you experience any troublesome or persistent side effects.
Types of SSRIs
There are currently 8 SSRIs prescribed in the UK:
- citalopram (Cipramil)
- dapoxetine (Priligy)
- escitalopram (Cipralex)
- fluoxetine (Prozac or Oxactin)
- fluvoxamine (Faverin)
- paroxetine (Seroxat)
- sertraline (Lustral)
- vortioxetine (Brintellix)
Page last reviewed: 8 December 2021
Next review due: 8 December 2024
Initiating antidepressant therapy? Try these 2 drugs first
- Journal List
- J Fam Pract
- PMC3183928
J Fam Pract. 2009 Jul; 58(7): 365–369.
2009 Jul; 58(7): 365–369.
, MD, MPP,, MD, and , MD, MPH
John Hickner, MD, MSc, PURLS Editor
John Hickner, Department of Family Medicine, Cleveland Clinic ;
Author information Copyright and License information Disclaimer
For most patients, sertraline and escitalopram are more effective and better tolerated than other antidepressants.
Practice changer
When you initiate antidepressant therapy for patients who have not been treated for depression previously, select either sertraline or escitalopram. A large meta-analysis found these medications to be superior to other “new-generation” antidepressants.1
Strength of recommendation
A: Meta-analysis of 117 high-quality studies.
Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. 2009;373:746-758.
Lancet. 2009;373:746-758.
Mrs. D is a 45-year-old patient whom you’ve treated for type 2 diabetes for several years. On her latest visit, she reports a loss of energy and difficulty sleeping and wonders if they could be related to the diabetes. As you explore further and question Mrs. D about these symptoms, she becomes tearful—and tells you she has episodes of sadness and no longer enjoys things the way she used to. Although she has no past history of depression, when you suggest that her symptoms may be an indication of depression, she readily agrees.
You discuss treatment options, including antidepressants and therapy. Mrs. D decides to try medication. But with so many antidepressants on the market, how do you determine which to choose?
Major depression is the fourth leading cause of disease globally, according to the World Health Organization.2 Depression is common in the United States as well, and primary care physicians are often the ones who are diagnosing and treating it.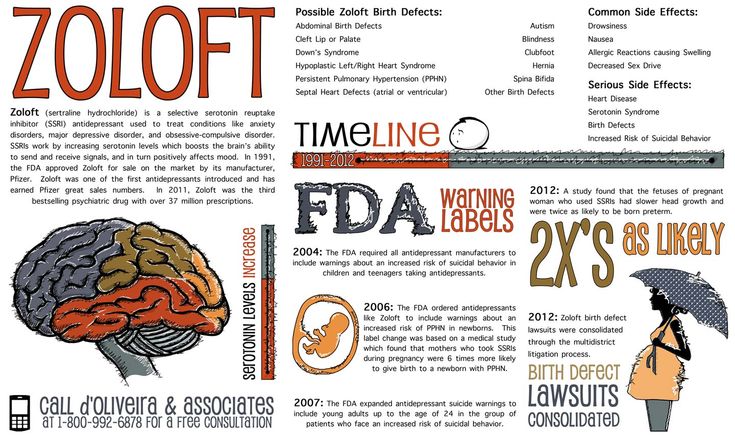 In fact, the US Preventive Services Task Force recently expanded its recommendation that primary care providers screen adults for depression, to include adolescents ages 12 to 18 years.3 When depression is diagnosed, physicians must help patients decide on an initial treatment plan.
In fact, the US Preventive Services Task Force recently expanded its recommendation that primary care providers screen adults for depression, to include adolescents ages 12 to 18 years.3 When depression is diagnosed, physicians must help patients decide on an initial treatment plan.
All antidepressants are
not equalOptions for initial treatment of unipolar major depression include psychotherapy and the use of an antidepressant. For mild and moderate depression, psychotherapy alone is as effective as medication. Combined psychotherapy and antidepressants are more effective than either treatment alone for all degrees of depression.4
The ideal medication for depression would be a drug with a high level of effectiveness and a low side-effect profile; until now, however, there has been little evidence to support 1 antidepressant over another. Previous meta-analyses have concluded that there are no significant differences in either efficacy or acceptability among the various second-generation antidepressants on the market. 5,6 Thus, physicians have historically made initial monotherapy treatment decisions based on side effects and cost.7,8 The meta-analysis we report on here tells a different story, providing strong evidence that some antidepressants are more effective and better tolerated than others.
5,6 Thus, physicians have historically made initial monotherapy treatment decisions based on side effects and cost.7,8 The meta-analysis we report on here tells a different story, providing strong evidence that some antidepressants are more effective and better tolerated than others.
Cipriani et al1 conducted a systematic review and multiple-treatments meta-analysis of 117 prospective randomized controlled trials (RCTs). Taken together, the RCTs evaluated the comparative efficacy and acceptability of 12 second-generation antidepressants: bupropion, citalopram, duloxetine, escitalopram, fluoxetine, fluvoxamine, milnacipran, mirtazapine, paroxetine, reboxetine, sertraline, and venlafaxine. The methodology of this meta-analysis differed from that of traditional meta-analyses by allowing the integration of data from both direct and indirect comparisons. (An indirect comparison is one in which drugs from different trials are assessed by combining the results of their effectiveness and comparing the combined finding with the effectiveness of a drug that all the trials have in common.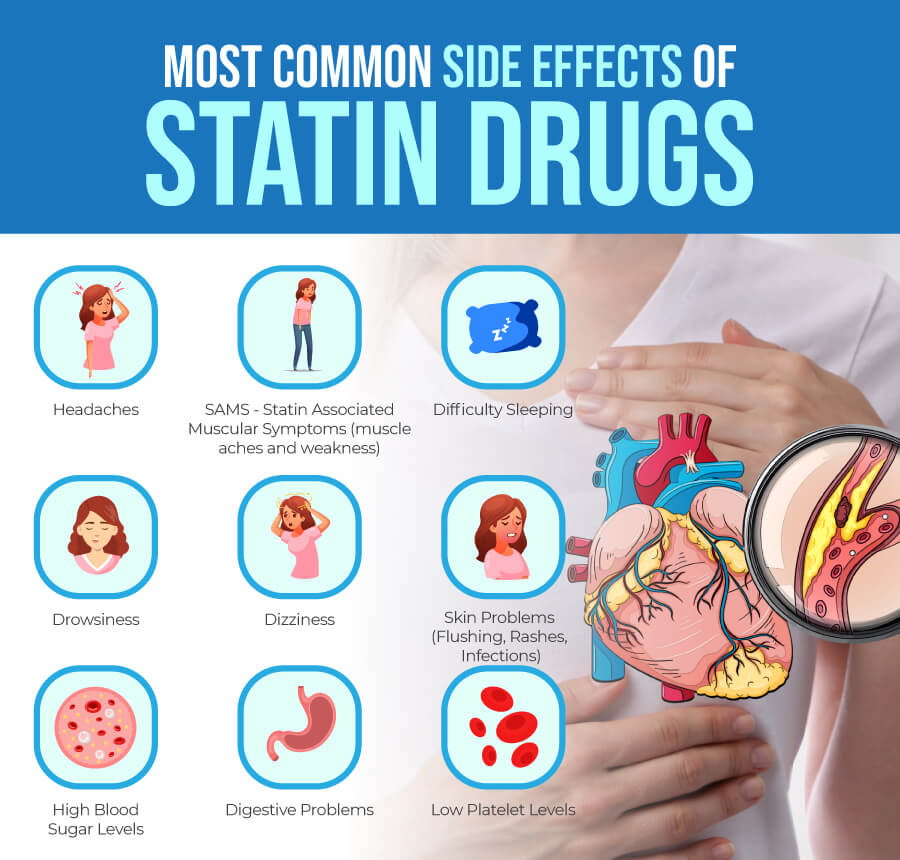 ) Previous studies, based only on direct comparisons, yielded inconsistent results.
) Previous studies, based only on direct comparisons, yielded inconsistent results.
The studies included in this meta-analysis were all RCTs in which 1 of these 12 antidepressants was tested against 1, or several, other second-generation antidepressants as monotherapy for the acute treatment phase of unipolar major depression. The authors excluded placebo-controlled trials in order to evaluate efficacy and acceptability of the study medications relative to other commonly used antidepressants. They defined acute treatment as 8 weeks of antidepressant therapy, with a range of 6 to 12 weeks. The primary outcomes studied were response to treatment and dropout rate.
Response to treatment (efficacy) was constructed as a Yes or No variable; a positive response was defined as a reduction of ≥50% in symptom score on either the Hamilton depression rating scale or the Montgomery-Asberg rating scale, or a rating of “improved” or “very much improved” on the clinical global impression at 8 weeks. Efficacy was calculated on an intention-to-treat basis; if data were missing for a participant, that person was classified as a nonresponder.
Efficacy was calculated on an intention-to-treat basis; if data were missing for a participant, that person was classified as a nonresponder.
Dropout rate was used to represent acceptability, as the authors believed it to be a more clinically meaningful measure than either side effects or symptom scores. Comparative efficacy and acceptability were analyzed. Fluoxetine—the first of the second-generation antidepressants—was used as the reference medication. The shows the outcomes for 9 of the antidepressants, compared with those of fluoxetine. The other 2 antidepressants, milnacipran and reboxetine, are omitted because they are not available in the United States.
Open in a separate window
Sertraline and escitalopram come out on top
Using fluoxetine as the reference medication, the researchers analyzed various second-generation antidepressants. Sertraline and escitalopram had the best combination of efficacy and acceptability.
OR, odds ratio.
Source: Cipriani A et al. Lancet. 2009.1
The overall meta-analysis included 25,928 individuals, with 24,595 in the efficacy analysis and 24,693 in the acceptability analysis. Nearly two-thirds (64%) of the participants were women. The mean duration of follow-up was 8.1 weeks, and mean sample size per study was 110. Studies of women with postpartum depression were excluded.
Escitalopram and sertraline stand out. Overall, escitalopram, mirtazapine, sertraline, and venlafaxine were significantly more efficacious than fluoxetine or the other medications. Bupropion, citalopram, escitalopram, and sertraline were better tolerated than the other antidepressants. Escitalopram and sertraline were found to have the best combination of efficacy and acceptability.
Efficacy results. Fifty-nine percent of participants responded to sertraline, vs a 52% response rate for fluoxetine (number needed to treat [NNT]=14). Similarly, 52% of participants responded to escitalopram, compared with 47% of those taking fluoxetine (NNT=20).
Similarly, 52% of participants responded to escitalopram, compared with 47% of those taking fluoxetine (NNT=20).
Acceptability results. In terms of dropout rate, 28% of participants discontinued fluoxetine, vs 24% of patients taking sertraline. This means that 25 patients would need to be treated with sertraline, rather than fluoxetine, to avoid 1 discontinuation. In the comparison of fluoxetine vs escitalopram, 25% discontinued fluoxetine, compared with 24% who discontinued escitalopram.
The efficacy and acceptability of sertraline and escitalopram compared with other second-generation antidepressant medications show similar trends.
The generic advantage. The investigators recommend sertraline as the best choice for an initial antidepressant because it is available in generic form and is therefore lower in cost. They further recommend that sertraline, instead of fluoxetine or placebo, be the new standard against which other antidepressants are compared.
We now have solid evidence for choosing sertraline or escitalopram as the first medication to use when treating a patient with newly diagnosed depression. This represents a practice change because antidepressants that are less effective and less acceptable have been chosen more frequently than either of these medications. That conclusion is based on our analysis of the National Ambulatory Medical Care Survey database for outpatient and ambulatory clinic visits in 2005-2006 (the most recent data available). We conducted this analysis to determine which of the second-generation antidepressants were prescribed most for initial monotherapy of major depression.
FAST TRACK
Antidepressants that are less effective and less acceptable than sertraline or escitalopram have been prescribed with greater frequency.
Our finding: An estimated 4 million patients ages 18 years and older diagnosed with depression in the course of the study year received new prescriptions for a single antidepressant. Six medications accounted for 90% of the prescriptions, in the following order:
Six medications accounted for 90% of the prescriptions, in the following order:
fluoxetine (Prozac)
duloxetine (Cymbalta)
escitalopram (Lexapro)
paroxetine (Paxil)
venlafaxine (Effexor)
sertraline (Zoloft).
Sertraline and escitalopram, the drugs shown to be most effective and acceptable in the Cipriani meta-analysis, accounted for 11.8% and 14.5% of the prescriptions, respectively.
The results of this study are limited to initial therapy as measured at 8 weeks. Little long-term outcome data are available; response to initial therapy may not be a predictor of full remission or long-term success. Current guidelines suggest maintenance of the initial successful therapy, often with increasing intervals between visits, to prevent relapse.9
FAST TRACK
Response in the acute phase of treatment for major depression may not be predictive of long-term outcomes.
This study does not add new insight into long-term response rates. Nor does it deal with choice of a replacement or second antidepressant for nonresponders or those who cannot tolerate the initial drug.
What’s more, the study covers drug treatment alone, which may not be the best initial treatment for depression. Psychotherapy, in the form of cognitive behavioral therapy or interpersonal therapy, when available, is equally effective, has fewer potential physiologic side effects, and may produce longer-lasting results.10,11
Little is known about study design
The authors of this study had access only to limited information about inclusion criteria and the composition of initial study populations or settings. There is a difference between a trial designed to evaluate the “efficacy” of an intervention (“the beneficial and harmful effects of an intervention under controlled circumstances”) and the “effectiveness” of an intervention (the “beneficial and harmful effects of the intervention under usual circumstances”). 12 It is not clear which of the 117 studies were efficacy studies and which were effectiveness studies. This may limit the overall generalizability of the study results to a primary care population.
12 It is not clear which of the 117 studies were efficacy studies and which were effectiveness studies. This may limit the overall generalizability of the study results to a primary care population.
Studies included in this meta-analysis were selected exclusively from published literature. There is some evidence that there is a bias toward the publication of studies with positive results, which may have the effect of overstating the effectiveness of a given antidepressant.13 However, we have no reason to believe that this bias would favor any particular drug.
Most of the included studies were sponsored by drug companies. Notably, pharmaceutical companies have the option of continuing to conduct trials of medications until a study results in a positive finding for their medication, with no penalty for the suppression of equivocal or negative results (negative publication bias). Under current FDA guidelines, there is little transparency to the consumer as to how many trials have been undertaken and the direction of the results, published or unpublished. 14
14
We doubt that either publication bias or the design and sponsorship of the studies included in this meta-analysis present significant threats to the validity of these findings over other sources upon which guidelines rely, given that these issues are common to much of the research on pharmacologic therapy. We also doubt that the compensation of the authors by pharmaceutical companies would bias the outcome of the study in this instance. One of the authors (TAF) received compensation from Pfizer, the maker of Zoloft, which is also available as generic sertraline. None of the authors received compensation from Forest Pharmaceuticals, the makers of Lexapro (escitalopram).
Both sertraline and escitalopram are covered by most health insurers. As noted above, sertraline is available in generic formulation, and is therefore much less expensive than escitalopram. In a check of online drug prices, we found a prescription for a 3-month supply of Lexapro (10 mg) to cost about $250; a 3-month supply of generic sertraline (100 mg) from the same sources would cost approximately $35 (www.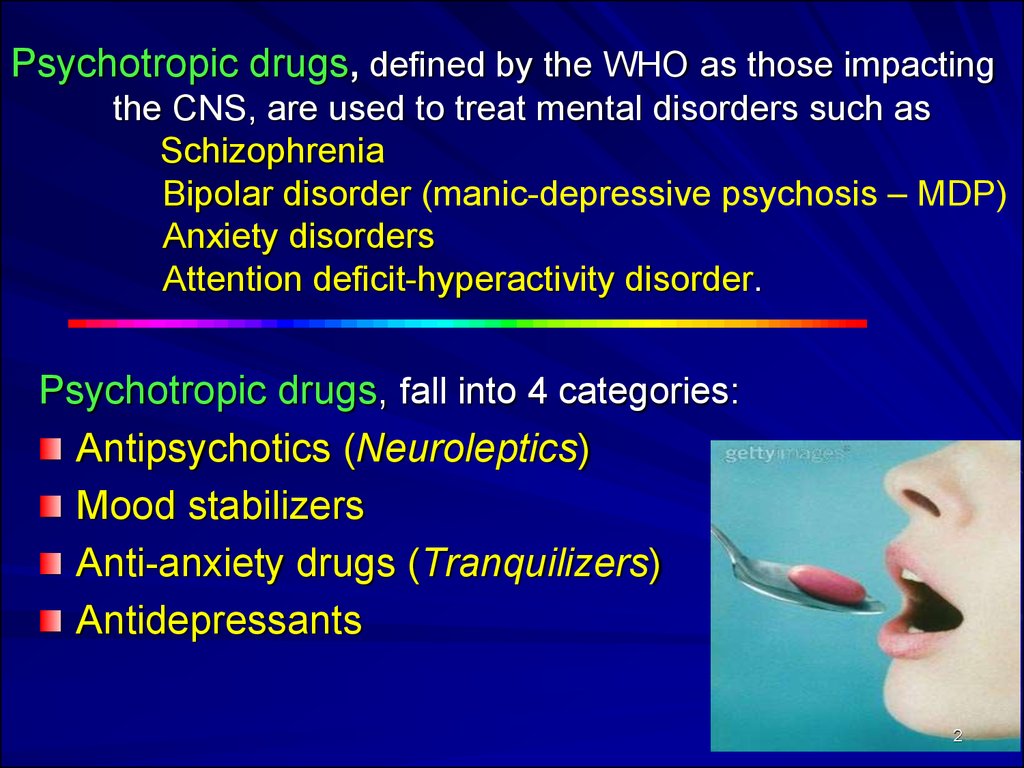 pharmcychecker.com). Both Pfizer, the maker of Zoloft, and Forest Pharmaceuticals, the maker of Lexapro, have patient assistance programs to make these medications available to low-income, uninsured patients.
pharmcychecker.com). Both Pfizer, the maker of Zoloft, and Forest Pharmaceuticals, the maker of Lexapro, have patient assistance programs to make these medications available to low-income, uninsured patients.
The PURLs Surveillance System is supported in part by Grant Number UL1RR02499 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
The authors wish to acknowledge Sofia Medvedev, PhD, of the University HealthSystem Consortium in Oak Brook, Ill, for analysis of the National Ambulatory Medical Care Survey data and the UHC Clinical Database.
PURLs methodology This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.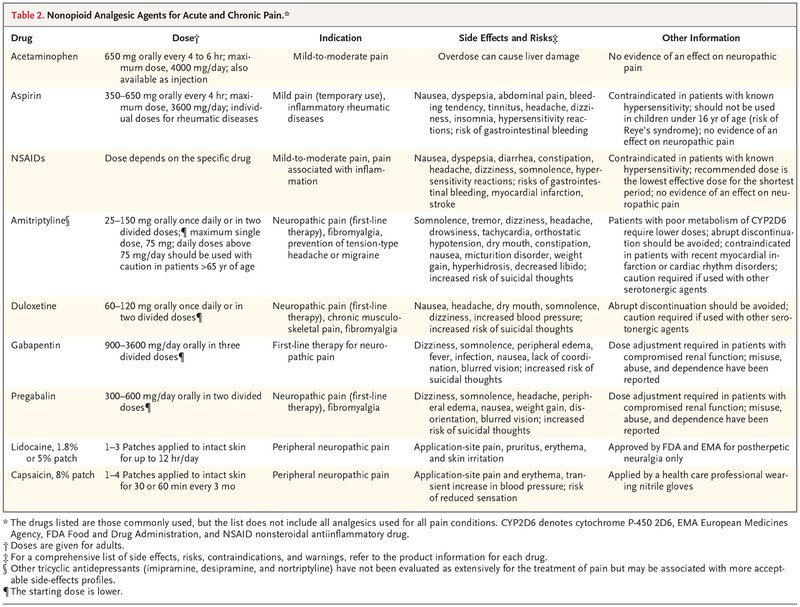 jfponline.com/purls.
jfponline.com/purls.
Gail Patrick, Department of Family Medicine, University of Chicago .
Gene Combs, Department of Family Medicine, University of Chicago .
Thomas Gavagan, Department of Family Medicine, University of Chicago .
1. Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. 2009;373:746–758.. [PubMed] [Google Scholar]
2. Murray CJ, Lopez AD. Global Burden of Disease. Cambridge, MA: Harvard University Press; 1996. [Google Scholar]
3. Williams SB, O’Connor EA, Eder M, et al. Screening for child and adolescent depression in primary care settings: a systematic evidence review for the U.S. Preventive Services Task Force. Pediatrics. 2009;123:e716–e735.. [PubMed] [Google Scholar]
4. Timonen M, Liukkonen T. Management of depression in adults. BMJ. 2008;336:435–439.. [PMC free article] [PubMed] [Google Scholar]
5. Gartlehner G, Hansen RA, Thieda P, et al. Comparative Effectiveness of Second-Generation Antidepressants in the Pharmacologic Treatment of Adult Depression. Comparative Effectiveness Review No. 7. (Prepared by RTI International-University of North Carolina Evidence Based Practice Center under Contract No. 290-02-0016.) Rockville, MD: Agency for Healthcare Research and Quality; January 2007. Available at: www.effectivehealthcare.ahrq.gov/reports/final.cfm. Accessed May 18, 2009. [Google Scholar]
Gartlehner G, Hansen RA, Thieda P, et al. Comparative Effectiveness of Second-Generation Antidepressants in the Pharmacologic Treatment of Adult Depression. Comparative Effectiveness Review No. 7. (Prepared by RTI International-University of North Carolina Evidence Based Practice Center under Contract No. 290-02-0016.) Rockville, MD: Agency for Healthcare Research and Quality; January 2007. Available at: www.effectivehealthcare.ahrq.gov/reports/final.cfm. Accessed May 18, 2009. [Google Scholar]
6. Hansen RA, Gartlehner G, Lohr KN, et al. Efficacy and safety of second-generation antidepressants in the treatment of major depressive disorder. Ann Intern Med. 2005;143:415–426.. [PubMed] [Google Scholar]
7. Adams SM, Miller KE, Zylstra RG. Pharmacologic management of adult depression. Am Fam Physician. 2008;77:785–792.. [PubMed] [Google Scholar]
8. Qaseem A, Snow V, Denberg TD, et al. Using second-generation antidepressants to treat depressive disorders: a clinical practice guideline from the American College of Physicians.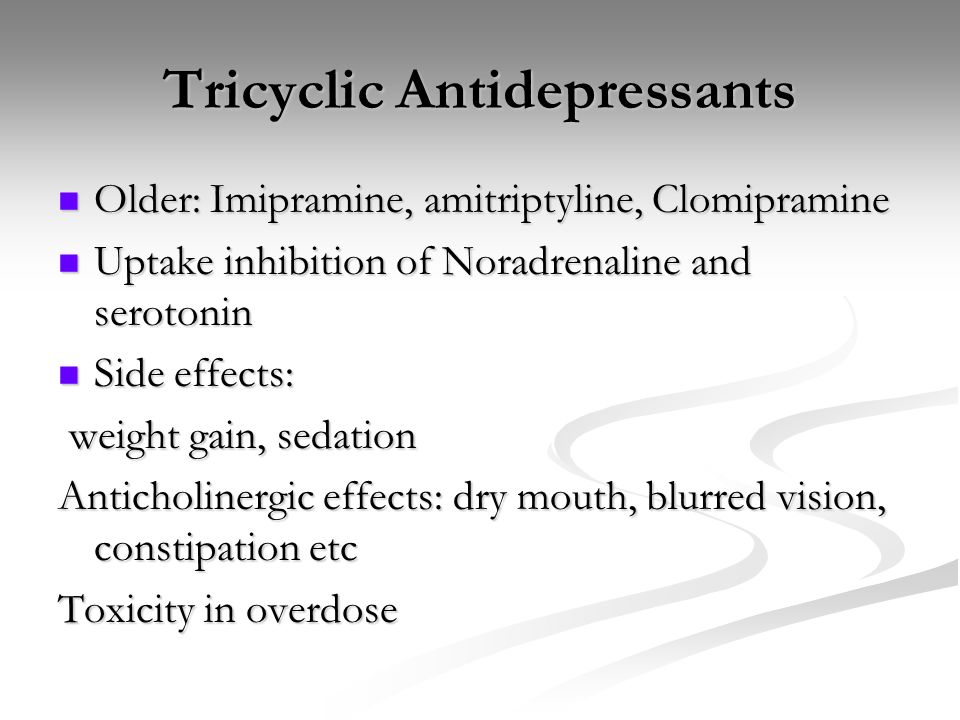 Ann Intern Med. 2008;149:725–733.. [PubMed] [Google Scholar]
Ann Intern Med. 2008;149:725–733.. [PubMed] [Google Scholar]
9. DeRubeis RJ, Hollon SD, Amsterdam JD, et al. Cognitive therapy vs medications in the treatment of moderate to severe depression. Arch Gen Psychiatry. 2005;62:409–416.. [PubMed] [Google Scholar]
10. deMello MF, de Jesus MJ, Bacaltchuk J, et al. A systematic review of research findings on the efficacy of interpersonal therapy for depressive disorders. Eur Arch Psychiatry Clin Neurosci. 2005;255:75–82.. [PubMed] [Google Scholar]
11. APA Practice Guidelines. Practice guideline for the treatment of patients with major depressive disorder, second edition. Available at: http://www.psychiatryonline.com/content.aspx?aID=48727. Accessed June 16, 2009. [Google Scholar]
12. Sackett D. An introduction to performing therapeutic trials. In: Haynes RB, Sackett DL, et al, eds. Clinical Epidemiology: How to Do Clinical Practice Research. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. [Google Scholar]
[Google Scholar]
13. Turner EH, Matthews AM, Linardatos E, et al. Selective publication of antidepressant trials and its influence on apparent efficacy. N Engl J Med. 2008;358:252–260.. [PubMed] [Google Scholar]
14. Mathew SJ, Charney DS. Publication bias and the efficacy of antidepressants. Am J Psychiatry. 2009;166:140–145.. [PubMed] [Google Scholar]
Articles from The Journal of Family Practice are provided here courtesy of Frontline Medical Communications Inc.
Fighting depression: 10 modern drugs
{{if type === 'partner-stocks'}}
{{/if}}
{{/if}} {{each list}}${this} {{if isGorzdrav}}
Delete
{{/if}}
{{/each}} {{/if}} Search by drug, disease, substance: DERMAKOSMETIKA, SOLGAR, NaturAge, Voltaren, KagocelHome
Articles
Fighting depression: 10 modern drugs
Depression is an urgent problem, the number of visits to doctors is growing every year. It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
What is meant by
depression Doctors have known it since ancient Greece and Egypt. Hippocrates described it as melancholy - a condition that is accompanied by anxiety, despondency, insomnia, refusal of food, irritability. Most often, the cause is childhood trauma or severe, frequent stress in adulthood. There are many provoking factors: the death of a loved one, deterioration of living conditions, alcoholism, brain diseases. Such cases are referred to as psychogenic depression.
Such cases are referred to as psychogenic depression.
The second type is endogenous. The problem appears not from large external shocks, but because of internal causes. A person is constantly dissatisfied with himself, subjecting himself to criticism. Many patients have panic attacks , haunted by a feeling of fear, anxiety.
How long the period of depression lasts
Many people mistake ordinary periods of low mood for depression. If they do not last long and are quickly replaced by periods of recovery, then we are not talking about a depressive state. The problem is obvious when the symptoms persist for months and dramatically change a person's life. Then you need to see a doctor.
What happens to the body
The most common theory is that there is a malfunction of neurotransmitters located in the brain. These substances transmit signals from neuron to neuron and are responsible for a person's mood.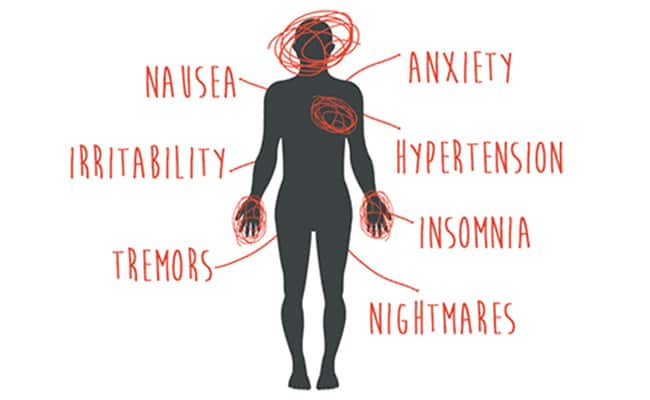 Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
How is
treated depressionDepression has been treated in different ways. In the ancient world - emetics and laxatives. In the Renaissance - wine and sunbathing. In the Age of Enlightenment - external stimuli, for example, insects. The 19th century brought new recipes - in particular, a solution of camphor in tartaric acid. The treatment also included the use of drugs, which are now no longer allowed for sale, and some are recognized as narcotic.
Obviously, all these drugs had no effect on increasing the amount of serotonin. And the treatment is precisely to normalize its production. This was done after creating modern antidepressants , which have a minimum of side effects, are safe for the body and are not addictive.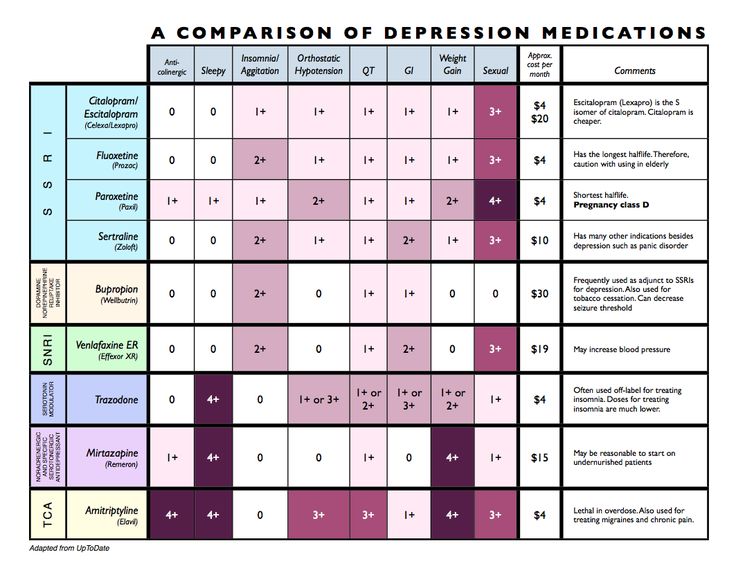 These are medicines, whose action is aimed specifically at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
These are medicines, whose action is aimed specifically at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
Prescription
If a healthy person takes antidepressants , there will be no effect . For a depressed patient, taking them will help:
- improve psychological state;
- get rid of irritability;
- panic fear;
- increase mental and physical activity;
- overcome the dreary mood.
Psychiatrists prescribe antidepressants for chronic back pain, headaches. And also with irritable bowel syndrome, incontinence and other cases when the body stops producing its own painkillers. Medication helps restore pain suppression mechanisms.
These drugs can only be taken with a doctor's prescription, as many of them are strong stimulants. Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Precautions
- Prescribed drug start drinking from a small dose - the first couple of days they take a quarter of a tablet. Gradually increase the dose to normal. So the body adapts better. Finish the course by reducing the dose.
- The first effect of appears only 2 weeks after the start of administration. Sustained action - after six months. All this time, you need to take remedy, without making passes, breaks.
-
Products are not combined with melatonin, St. John's wort, products and dietary supplements based on sibutramine, 5-HTP. Their combination can raise serotonin to dangerous levels.
 Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account.
Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account. - Drinking antidepressants is better in parallel with visits to a psychotherapist. If the drugs normalize the biochemical processes in the body, then this doctor will help normalize the psychological state after depression.
The best antidepressants
In medicine, they have long argued that some drugs give only a placebo effect. The purpose of the study was to find out which of them are the most effective and valid . The project involved 116 thousand patients, and its results were published by the authoritative edition of the Lancet. We offer a list of the best.
1. Agomelatine
New generation drug. Agomelatine is used for severe depressive disorders, high levels of anxiety. Enhances the release of dopamine and norepinephrine, stimulates melatonin receptors.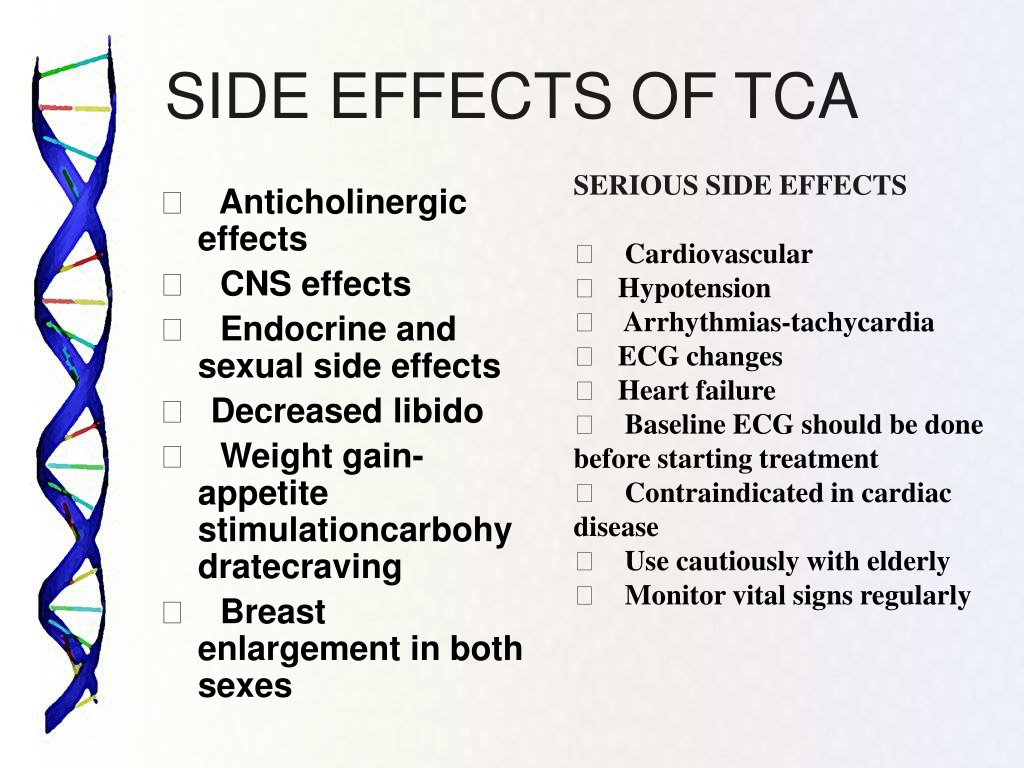 The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
Pros
+ Does not adversely affect attention and memory.
+ No lethargy during the day.
+ No sexual deviations.
+ No relation to blood pressure.
+ Do not reduce dosage upon discontinuation.
Cons
— In 1-10% of cases, increased sweating, diarrhea, constipation.
- Possible increased fatigue, drowsiness.
- There are no evidence-based safety studies in people with renal or hepatic insufficiency, therefore, such patients are advised to refrain from taking drugs with active ingredient agomelatine.
2. Amitriptyline
Tricyclic antidepressant. Moreover, the World Health Organization considers Amitriptyline the most reliable in this group. The standard dose is 200-250 mg / day. The action is to block the reuptake of neurotransmitters. A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
Pluses
+ Preparations with active ingredient amitriptyline are inexpensive.
+ High reliability, minimum side effects.
+ Relatively safe during breastfeeding.
Cons
- Possible side effect in the form of blurred vision, dry mouth.
- Lowering blood pressure.
- Some patients experience constipation.
- Drowsiness.
3. Escitalopram
It belongs to the group of modern serotonin reuptake inhibitors (SSRIs). Most often, it is recommended to take for anxiety, panic attacks. It is taken once, the standard dose is 10 mg per day. Escitalopram has a milder effect and is prescribed to patients for whom tricyclic drugs are contraindicated.
Pluses
+ Lasting effect comes after 3 months.
+ Indicated for patients with disorders of the cardiovascular system.
+ Soft action.
Cons
- In some patients, the functions of the gastrointestinal tract are disturbed, which is most often expressed in diarrhea.
- Anxiety may increase during the first 2 weeks, therefore it is recommended to start treatment with low doses and gradually increase them.
- Contraindicated in pregnancy and lactation.
4. Mirtazapine
A drug of the tetracyclic group. Mirtazapine - good stimulant for anxious depressions, has a moderate sedative effect. The average amount is 30 mg / day, it must be consumed once. Usually it is prescribed to patients who lose interest in life, cease to experience joy, pleasure. Effective in the correction of sleep, in particular, early awakenings.
Pros
+ Earlier onset of action than SSRIs (1 week).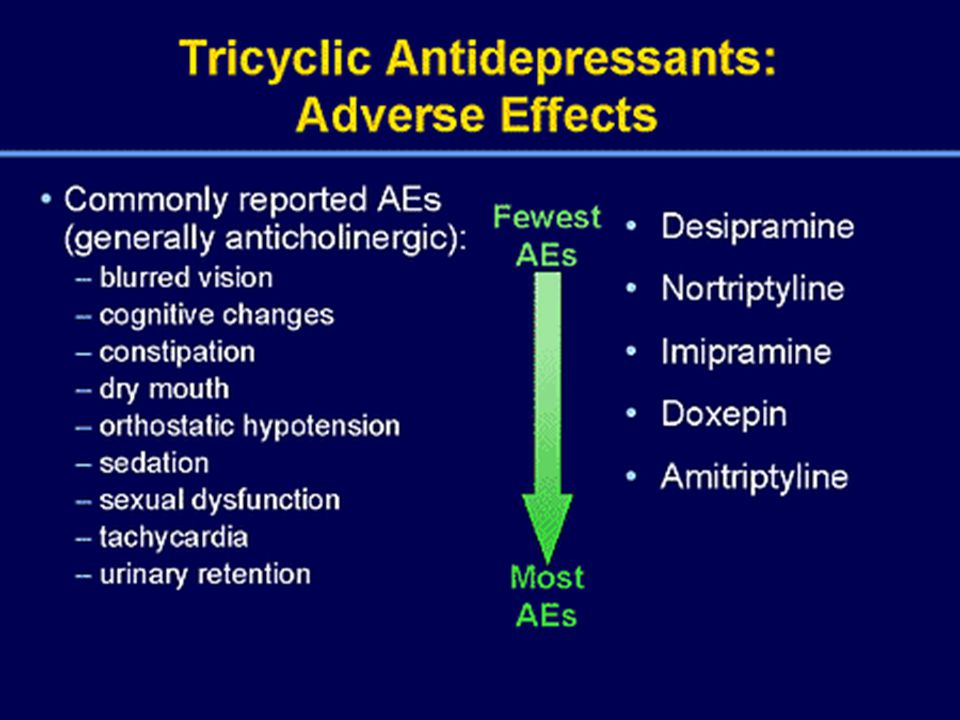
+ Works well with most general medicines.
+ Full effect in 4 weeks.
+ Does not affect sexual function.
Cons
- The active substance mirtazapine is contraindicated in diabetes mellitus, arterial hypotension, increased intraocular pressure.
— During the appointment, you must drive carefully and engage in potentially hazardous types of work.
- 18% of patients experience drowsiness, 15% dry mouth, 5% weight loss. Other side effects occur in 1-3% of cases.
5. Paroxetine
Belongs to the SSRI group, is used most often for severe anxiety, panic, social phobia, nightmares, stress after trauma. Paroxetine can resolve the problems of anxious depression, anxiety-phobic disorders. Take once a day at a dose of 20 mg.
Pros
+ The most powerful stimulant among SSRIs.
+ Anxiety and insomnia pass quickly.
+ Minimal side effects in the form of vomiting, diarrhea.
+ Suitable for patients with cardiovascular problems.
Cons
— Not suitable for patients with severe motor, mental inhibition.
- Reduces libido.
- Harmful to the fetus when taken during pregnancy.
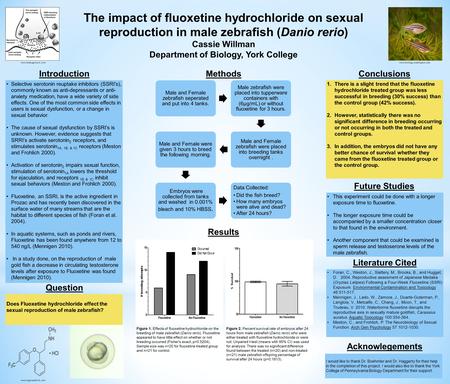
6. Fluoxetine
One of the most commonly used antidepressants in the SSRI group. Known as Prozac. Fluoxetine is also known as a good mood stimulant. Patients have a feeling of fear, tension, anxiety, gloomy dislike for others. Depending on the indications, the average daily dose is 20-60 mg.
Pluses
+ There is practically no effect on the work of the heart.
+ Does not cause sedation.
+ Effective for patients with motor retardation and excessive daytime sleepiness.
Cons
- May cause weight loss.
— Hypoglycemia is possible in diabetes mellitus.
- Contraindicated in severe renal impairment.
7. Fluvoxamine
Another SSRI drug.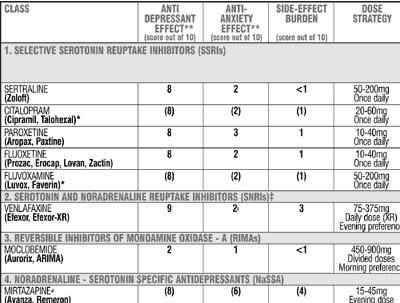 Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Pros
+ Lower price than traditional Prozac.
+ Faster action than him.
+ Relatively minor side effects (diarrhea, dry mouth, drowsiness).
Cons
- Contraindicated in diabetes.
- Pregnant women - with caution, lactation - prohibited.
- Causes nausea in some patients.
8. Sertraline
One of the widely used and universal drugs of the SSRI group. They treat almost any depressive condition, panic disorder, social phobia. However, in severe clinical cases, sertraline may not be effective enough. The standard dose is 50 mg/day.
Pros
+ No cardiotoxicity.
+ The patient's psychomotor activity does not change.
+ Does not increase body weight.
+ Combines well with other groups of antidepressants.
Cons
— In the first 2 weeks there may be problems with sleep, diarrhea.
- Side effects of a sexual nature.
- Contraindicated in pregnant women.
9. Escitalopram
The drug is classified as an SSRI. Its difference is in its effectiveness in depression, which is accompanied by involuntary movements (tic, tremor, chewing, smacking). Escitalopram is prescribed to patients with panic, anxiety, phobias, obsessive thoughts or actions. The daily dose is 20 mg.
Pluses
+ Effective in tardive dyskinesia.
+ One of the most powerful SSRIs.
+ More pronounced thymoleptic effect (improvement of mood) compared to many antidepressants of the same group.
Cons
- In some patients, anxiety increases within 2 weeks after starting treatment.
— Gastrointestinal disorders, insomnia, agitation are possible.
— Use during pregnancy only in extreme cases, incompatible with feeding.
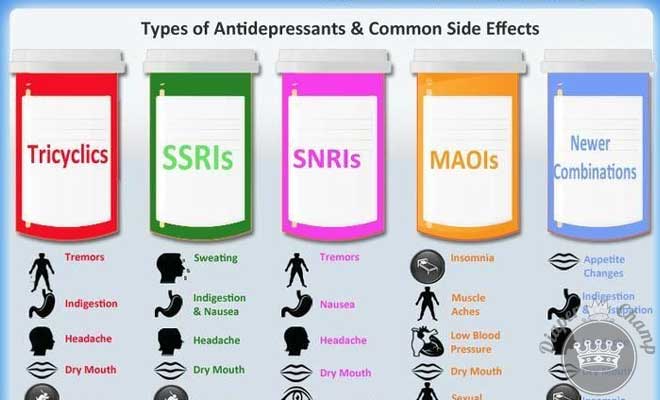
10. Venlafaxine
Belongs to the SNRI group. In addition to blocking the reuptake of serotonin, venlafaxine has a similar effect on another neurotransmitter, norepinephrine. The medicine is prescribed for depressive conditions of various origins, social phobias, anxiety, panic. Usually take 150 mg per day.
Pros
+ Better tolerated by patients than most tricyclics.
+ More pronounced effect than classic SSRIs.
+ Fewer contraindications.
Cons
- Traditional side effects of most antidepressants: nausea, drowsiness, dry mouth, diarrhea or constipation.
- May increase eye pressure.
- The most severe withdrawal syndrome among antidepressant drugs.
This list is not to be used as a recommendation. In any case, consult your doctor before purchasing. Be healthy!
list of the best drugs without prescriptions
Can I buy antidepressants without prescriptions? What mood improvers are most effective, when will lighter drugs help, and when powerful ones are needed, how do they affect the body, and can they be taken on their own? The main thing when choosing a medicine is not to harm your health.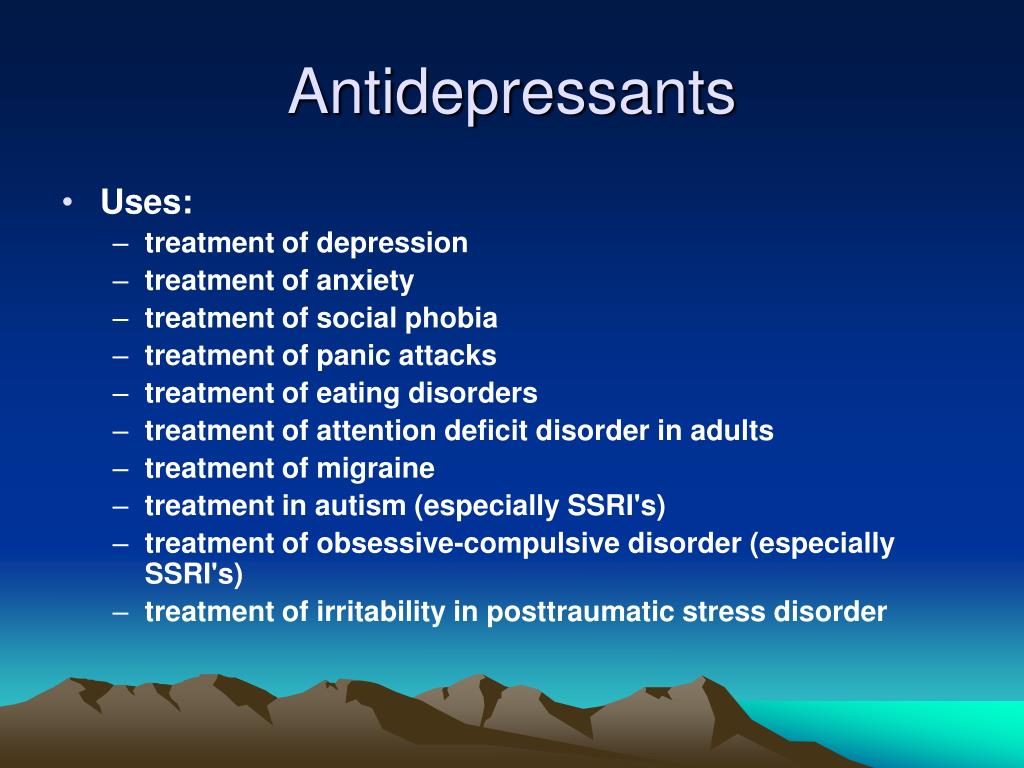
I'm depressed!
This can often be heard from friends or read on the forum. But, as a rule, the person making such statements is mistaken. After all, what is meant by "depression" in a colloquial environment? Usually it means just a short-term deterioration in mood, irritability, fatigue under the influence of circumstances. Sometimes a person just has a "bad day" or "gets up on the wrong foot" and calls it depression.
Nowadays, people are constantly faced with stress: overload at work, a frantic pace of life, excessive demands on themselves, a huge amount of information that flows from all sources. Not surprisingly, many people cannot cope with so many stressors, and this can manifest itself in various symptoms:
- anxiety;
- irritability;
- fatigue;
- sleep disorders;
- obsessive thoughts;
- panic attacks.
If these symptoms are short-lived and go away on their own, don't get too upset.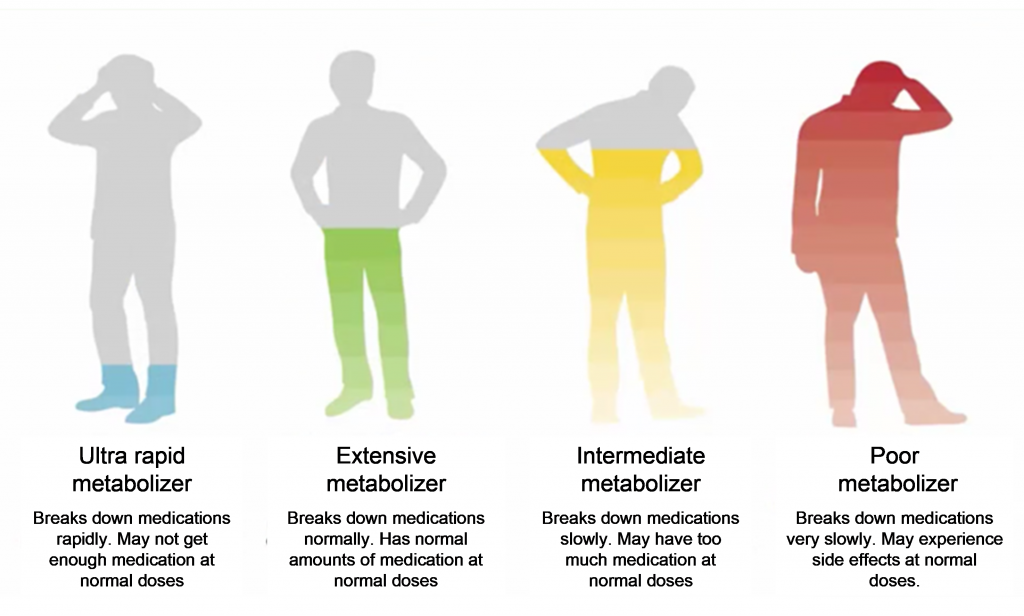 In most cases, they will be defeated by just a good rest. But sometimes vacation is not enough, and the body needs a little help. It is very important to choose the right medicines for this.
In most cases, they will be defeated by just a good rest. But sometimes vacation is not enough, and the body needs a little help. It is very important to choose the right medicines for this.
What depression really is
This is a long-term (2 weeks or more) marked decrease in mood, which is accompanied by several additional symptoms: decrease in activity, slowing down of mental activity, lack of joy from life. That is, if you are no longer touched by the usual joys - hobbies, family, gatherings with friends, then this is an occasion to think, observe your condition and, possibly, consult a doctor.
If you are no longer touched by the usual joys, then this is an occasion to think and, perhaps, consult a doctor.True depression is a serious and often serious illness that requires mandatory treatment by a psychiatrist with the appointment of special medications.
What drugs are used to treat depression?
They are collectively called antidepressants.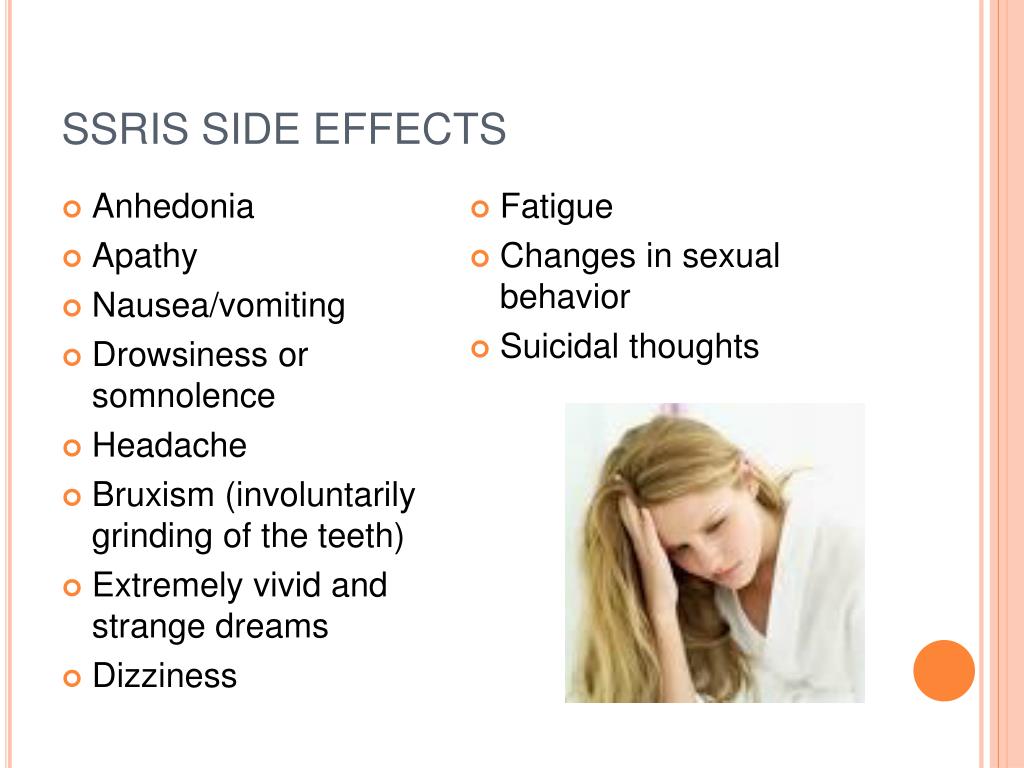 It is worth noting that in recent years, the indications for prescribing antidepressants have expanded significantly. Numerous studies have been conducted that have shown the effectiveness of antidepressants not only for depression, but also for anxiety, sleep disorders (insomnia), neurosis, and even neuropathic pain. Today, drugs from different groups of antidepressants are widely prescribed by psychiatrists, neurologists, and even therapists.
It is worth noting that in recent years, the indications for prescribing antidepressants have expanded significantly. Numerous studies have been conducted that have shown the effectiveness of antidepressants not only for depression, but also for anxiety, sleep disorders (insomnia), neurosis, and even neuropathic pain. Today, drugs from different groups of antidepressants are widely prescribed by psychiatrists, neurologists, and even therapists.
Two groups of drugs are most commonly used.
Tricyclic antidepressants
These are the oldest drugs that are considered the most powerful:
- Amitriptyline is a drug with a strong sedative and powerful antidepressant effect. Large doses are used to treat severe depression, and small doses are used for milder disorders. It relieves anxiety and has a hypnotic effect.
- Anafranil is a drug of balanced action, usually more easily tolerated than amitriptyline, and also relieves anxiety well.
 It is prescribed for the treatment of depression from mild to severe, various anxiety disorders.
It is prescribed for the treatment of depression from mild to severe, various anxiety disorders. - Melipramine - has a stimulating effect, they treat apathetic depression.
Selective serotonin reuptake inhibitors (SSRIs)
This is a more modern group of drugs. Their advantages are good tolerability and few or no side effects.
Often prescribed from this group:
- Fevarin — has anti-anxiety and good antidepressant effect. With prolonged use, it normalizes sleep, if it has been disturbed.
- Zoloft is a fairly strong daytime antidepressant. It relieves anxiety, obsessive thoughts, while not causing drowsiness.
- Paxil - relieves anxiety, often prescribed for the treatment of panic attacks.
There are many more modern antidepressants that have few side effects and are well tolerated:
- Ixel;
- Velaxin;
- Valdoxan;
- Trittiko;
- Simbalta and others.
But strong antidepressants are not sold without a prescription . They can only be prescribed by a doctor: a psychiatrist, a neurologist, sometimes a therapist.
Why can't I take antidepressants without a prescription?
- Only a doctor can assess the risk of side effects for a particular patient.
- Different antidepressants have different nuances of therapeutic action. If the medicine is chosen incorrectly, at best it will not help, at worst it will hurt.
- Dose selection is carried out individually. If you increase the dose too quickly on your own, you can experience a lot of unpleasant consequences.
- Cancellation should also be carried out gradually and under the supervision of a physician. Otherwise, you risk getting a withdrawal syndrome.
What to do?
There are a number of drugs available without a prescription. They are not effective for clinical depression, but they will help to cope with stress, short-term sleep disorders and irritability.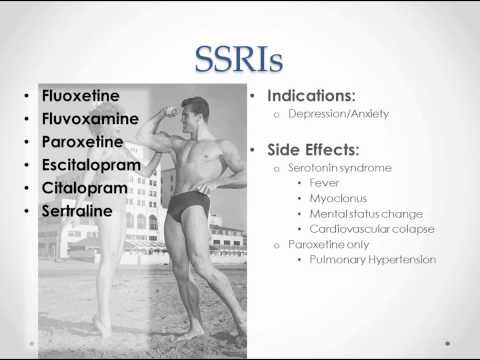 With their help, you can try to alleviate your psycho-emotional state a little:
With their help, you can try to alleviate your psycho-emotional state a little:
- Glycine is one of the most popular products. It is prescribed, starting from childhood, with stress, overwork, emotional overstrain. Sometimes effective for minor sleep disturbances.
- Afobazole . Has an anti-anxiety effect, eliminates the feeling of fear, tearfulness, irritability. It is used in the treatment of vegetative-vascular dystonia and even in alcoholism, to alleviate the symptoms of alcohol withdrawal. Not addictive. It should be borne in mind that children under 18 years of age are contraindicated.
- Novo-passit . Quite a strong sedative for nervousness and irritability. Effective in reducing concentration, memory, fatigue. Helps to restore the nervous system during periods of increased stress.
- Stressovit . Well calms, relieves irritability, anxiety, improves sleep. It is not recommended to drive a car and other activities that require increased concentration of attention during the period of treatment.
- Persen is a herbal medicine. Contains extracts of valerian, lemon balm and peppermint. It has a calming and anti-anxiety effect. It helps well with increased excitability, emotional lability, tearfulness. It can be used in the complex therapy of mild anxiety depressive disorders, facilitates the withdrawal of potent drugs.
- Magne B6 . Increases the body's resistance to stress. Magnesium deficiency can lead to an imbalance of the nervous system, irritability, sleep disturbances, so Magne B6 has a positive effect in these cases.
- Tenoten . It has an anti-anxiety, calming, anti-asthenic effect, helps to cope with stress and psycho-emotional stress.
 Relieves irritability and tension. Can be used in neurotic conditions.
Relieves irritability and tension. Can be used in neurotic conditions.
When should I see a doctor?
- If the decrease in mood persists for more than two weeks, and attempts at self-treatment have not been effective.
- If you have thoughts about unwillingness to live or suicidal thoughts.
- If depression significantly disrupts the usual course of life: you cannot work, fully communicate with your family, enjoy what used to bring joy.
You can consult a psychiatrist in confidence. Information about the very fact of treatment, not to mention the diagnosis and treatment, is a medical secret: they are not reported to work, they are not disclosed. It is better to diagnose depression early and start treatment than to bring it to advanced stages.
Literature
- Bauer M., Pfennig A., Severus E., Vaibrau P.S., Angst J., Muller H. Clinical recommendations of the World Federation of Biological Psychiatry on Biological Therapy of Unipolar Depressive Disorders Part 1: Acute and Acute and Acute CONTINUOUS TREATMENT OF UNIPOLAR DEPRESSIVE DISORDERS AS OF 2013//CURRENT THERAPY OF MENTAL DISORDERS Number: 4 Year: 2015 Pages: 33-40
- Antidepressant therapy and other treatments for depressive disorders.