Anger after stopping antidepressants
I Had No Idea Going Off My SSRIs Would Make Me So Angry
According to Richard C. Shelton, M.D., a psychiatry professor at the University of Alabama School of Medicine, there's a name for what I was experiencing: rage attacks. They most likely result from decreased production of serotonin—the neurotransmitter that SSRIs increase in the brain—which can lead to aggression, says psychiatrist Steven P. Levine, M.D.
"Rage would be an uncommon, although not rare, experience after SSRI discontinuation," Dr. Shelton tells me. "Rage attacks are often accompanied by anxiety and can be similar to panic attacks."
It took around six months for these feelings to subside, and in the end, I was glad to be off the meds. The lethargic version of myself I'd become after starting SSRIs gave way to the intensely driven version I knew before going on them. I went from being complacent with a 9-to-5 I didn't really enjoy to wanting more out of my work, and I started building my own career on nights and weekends.
Another plus was that I could orgasm with relative ease again.
But the anger never totally went away. I'm not reliving every infuriating moment of my life every morning anymore, but I do get incredibly pissy at random times. Dr. Shelton and Dr. Levine both tell me this is pretty rare, since SSRI withdrawal symptoms usually go away after a few weeks or months. But for largely unknown reasons, a small percentage of people experience them for years. Often it's a sign that the SSRI was really covering up a preexisting emotional issue that got worse over time.
Some of the coping skills I learned during withdrawal still work for me now. I go on daily runs (in my exercise clothes this time!) to get out my aggression so I don't take it out on anyone else—though sometimes I do, usually by picking fights with my boyfriend. Having a good cry also helps get it out. I've noticed it's more likely to flare up when something else is wrong—like I didn't get enough sleep or I've been pressured into doing something I don't really feel like doing—so I treat it as a sign to take better care of myself.
But perhaps my best coping strategy has been to realize this anger and aggression aren't really me. A feeling has less power when you view it as a chemical imbalance, not your true personality. Whether my rage fits result purely from SSRI cessation or something more innate, I know my desire to form caring relationships is bigger than them.
So recently I apologized to my boyfriend for the fights I pick with him. "Sometimes I'm not even mad at you. I'm just already mad and then find something to be mad about," I explained.
"I already knew that," he laughed. "I can tell when you're just grumpy."
"But thanks for admitting it," he added. "You're a good girl."
"Yeah," I said, "I guess I still am." For a while, I'd really believed I wasn't. But at that moment, I saw my rage for what it was: just another battle I'm fighting—and beating.
Going Off Antidepressants - Harvard Health Publishing
Coming off your medication can cause antidepressant withdrawal – and could set you up for a relapse of depression.
Can going off your medication cause antidepressant withdrawal symptoms (antidepressant discontinuation syndrome)? About 10% of women ages 18 and over take antidepressants. As many of us know, these medications can be a godsend when depression has robbed life of its joy and made it hard to muster the energy and concentration to complete everyday tasks. But as you begin to feel better and want to move on, how long should you keep taking the pills?
If you're doing well on antidepressants and not complaining of too many side effects, many physicians will renew the prescription indefinitely — figuring that it offers a hedge against a relapse of depression. But side effects that you may have been willing to put up with initially — sexual side effects (decreased desire and difficulty having an orgasm), headache, insomnia, drowsiness, vivid dreaming, or just not feeling like yourself — can become less acceptable over time, especially if you think you no longer need the pills.
The decision to go off antidepressants should be considered thoughtfully and made with the support of your physician or therapist to make sure you're not stopping prematurely, risking a recurrence of depression. Once you decide to quit, you and your physician should take steps to minimize or avoid the discontinuation symptoms that can occur if such medications are withdrawn too quickly.
Why antidepressant withdrawal?
Antidepressants work by altering the levels of neurotransmitters — chemical messengers that attach to receptors on neurons (nerve cells) throughout the body and influence their activity. Neurons eventually adapt to the current level of neurotransmitters, and symptoms that range from mild to distressing may arise if the level changes too much too fast — for example, because you've suddenly stopped taking your antidepressant. They're generally not medically dangerous but may be uncomfortable.
Among the newer antidepressants, those that influence the serotonin system — selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) — are associated with a number of withdrawal symptoms, often called antidepressant or SSRI discontinuation syndrome. Stopping antidepressants such as bupropion (Wellbutrin) that do not affect serotonin systems — dopamine and norepinephrine reuptake inhibitors — seems less troublesome overall, although some patients develop extreme irritability.
Stopping antidepressants such as bupropion (Wellbutrin) that do not affect serotonin systems — dopamine and norepinephrine reuptake inhibitors — seems less troublesome overall, although some patients develop extreme irritability.
Having discontinuation symptoms doesn't mean you're addicted to your antidepressant. A person who is addicted craves the drug and often needs increasingly higher doses. Few people who take antidepressants develop a craving or feel a need to increase the dose. (Sometimes an SSRI will stop working — a phenomenon called "Prozac poop-out" — which may necessitate increasing the dose or adding another drug.)
Antidepressant withdrawal can look like depressionDiscontinuation symptoms can include anxiety and depression. Since these may be the reason you were prescribed antidepressants in the first place, their reappearance may suggest that you're having a relapse and need ongoing treatment.
If symptoms last more than a month and are worsening, it's worth considering whether you're having a relapse of depression. |
Antidepressant withdrawal symptoms
Neurotransmitters act throughout the body, and you may experience physical as well as mental effects when you stop taking antidepressants or lower the dose too fast. Common complaints include the following:
Common complaints include the following:
- Digestive. You may have nausea, vomiting, cramps, diarrhea, or loss of appetite.
- Blood vessel control. You may sweat excessively, flush, or find hot weather difficult to tolerate.
- Sleep changes. You may have trouble sleeping and unusual dreams or nightmares.
- Balance. You may become dizzy or lightheaded or feel like you don't quite have your "sea legs" when walking.
- Control of movements. You may experience tremors, restless legs, uneven gait, and difficulty coordinating speech and chewing movements.
- Unwanted feelings. You may have mood swings or feel agitated, anxious, manic, depressed, irritable, or confused — even paranoid or suicidal.
- Strange sensations. You may have pain or numbness; you may become hypersensitive to sound or sense a ringing in your ears; you may experience "brain-zaps" — a feeling that resembles an electric shock to your head — or a sensation that some people describe as "brain shivers.
 "
"
As dire as some of these symptoms may sound, you shouldn't let them discourage you if you want to go off your antidepressant. Many of the symptoms of SSRI discontinuation syndrome can be minimized or prevented by gradually lowering, or tapering, the dose over weeks to months, sometimes substituting longer-acting drugs such as fluoxetine (Prozac) for shorter-acting medications. The antidepressants most likely to cause troublesome symptoms are those that have a short half-life — that is, they break down and leave the body quickly. (See the chart "Antidepressant drugs and their half-lives.") Examples include venlafaxine (Effexor), sertraline (Zoloft), paroxetine (Paxil), and citalopram (Celexa). Extended-release versions of these drugs enter the body more slowly but leave it just as fast. Antidepressants with a longer half-life, chiefly fluoxetine, cause fewer problems on discontinuation.
Besides easing the transition, tapering the dose decreases the risk that depression will recur. In a Harvard Medical School study, nearly 400 patients (two-thirds of them women) were followed for more than a year after they stopped taking antidepressants prescribed for mood and anxiety disorders. Participants who discontinued rapidly (over one to seven days) were more likely to relapse within a few months than those who reduced the dose gradually over two or more weeks.
In a Harvard Medical School study, nearly 400 patients (two-thirds of them women) were followed for more than a year after they stopped taking antidepressants prescribed for mood and anxiety disorders. Participants who discontinued rapidly (over one to seven days) were more likely to relapse within a few months than those who reduced the dose gradually over two or more weeks.
Antidepressant drugs and their half-lives* | ||
| Drug | Half out of body in | 99% out of body in |
| Serotonin reuptake inhibitors | ||
| paroxetine (Paxil) | 24 hours | 4. |
| sertraline (Zoloft) | 26 hours | 5.4 days |
| escitalopram (Lexapro) | 27 to 32 hours | 6.1 days |
| citalopram (Celexa) | 36 hours | 7.3 days |
| fluoxetine (Prozac) | Four to six days | 25 days |
| Serotonin and norepinephrine reuptake inhibitors | ||
| venlafaxine (Effexor) | 5 hours | 1 day |
| duloxetine (Cymbalta) | 12 hours | 2. |
| desvenlafaxine (Pristiq) | 12 hours | 2.5 days |
| Dopamine and norepinephrine reuptake inhibitor | ||
| bupropion (Wellbutrin) | 21 hours | 4.4 days |
| *Discontinuation symptoms typically start when 90% or more of the drug has left your system. Source: Adapted from Joseph Glenmullen, M.D., The Antidepressant Solution: A Step-by-Step Guide to Safely Overcoming Antidepressant Withdrawal, Dependence, and "Addiction" (Free Press, 2006). | ||
How to go off antidepressants
If you're thinking about stopping antidepressants, you should go step-by-step, and consider the following:
Take your time. You may be tempted to stop taking antidepressants as soon as your symptoms ease, but depression can return if you quit too soon. Clinicians generally recommend staying on the medication for six to nine months before considering going off antidepressants. If you've had three or more recurrences of depression, make that at least two years.
Talk to your clinician about the benefits and risks of antidepressants in your particular situation, and work with her or him in deciding whether (and when) to stop using them. Before discontinuing, you should feel confident that you're functioning well, that your life circumstances are stable, and that you can cope with any negative thoughts that might emerge. Don't try to quit while you're under stress or undergoing a significant change in your life, such as a new job or an illness.
Make a plan. Going off an antidepressant usually involves reducing your dose in increments, allowing two to six weeks between dose reductions. Your clinician can instruct you in tapering your dose and prescribe the appropriate dosage pills for making the change. The schedule will depend on which antidepressant you're taking, how long you've been on it, your current dose, and any symptoms you had during previous medication changes. It's also a good idea to keep a "mood calendar" on which you record your mood (on a scale of one to 10) on a daily basis.
Consider psychotherapy. Fewer than 20% of people on antidepressants undergo psychotherapy, although it's often important in recovering from depression and avoiding recurrence. In a meta-analysis of controlled studies, investigators at Harvard Medical School and other universities found that people who undergo psychotherapy while discontinuing an antidepressant are less likely to have a relapse.
Stay active. Bolster your internal resources with good nutrition, stress-reduction techniques, regular sleep — and especially physical activity. Exercise has a powerful antidepressant effect. It's been shown that people are far less likely to relapse after recovering from depression if they exercise three times a week or more. Exercise makes serotonin more available for binding to receptor sites on nerve cells, so it can compensate for changes in serotonin levels as you taper off SSRIs and other medications that target the serotonin system.
Seek support. Stay in touch with your clinician as you go through the process. Let her or him know about any physical or emotional symptoms that could be related to discontinuation. If the symptoms are mild, you'll probably be reassured that they're just temporary, the result of the medication clearing your system. (A short course of a non-antidepressant medication such as an antihistamine, anti-anxiety medication, or sleeping aid can sometimes ease these symptoms. ) If symptoms are severe, you might need to go back to a previous dose and reduce the levels more slowly. If you're taking an SSRI with a short half-life, switching to a longer-acting drug, like fluoxetine, may help.
) If symptoms are severe, you might need to go back to a previous dose and reduce the levels more slowly. If you're taking an SSRI with a short half-life, switching to a longer-acting drug, like fluoxetine, may help.
You may want to involve a relative or close friend in your planning. If people around you realize that you're discontinuing antidepressants and may occasionally be irritable or tearful, they'll be less likely to take it personally. A close friend or family member may also be able to recognize signs of recurring depression that you might not perceive.
Complete the taper. By the time you stop taking the medication, your dose will be tiny. (You may already have been cutting your pills in half or using a liquid formula to achieve progressively smaller doses.) Some psychiatrists prescribe a single 20-milligram tablet of fluoxetine the day after the last dose of a shorter-acting antidepressant in order to ease its final washout from the body, although this approach hasn't been tested in a clinical trial.
Check in with your clinician one month after you've stopped the medication altogether. At this follow-up appointment, she or he will check to make sure discontinuation symptoms have eased and there are no signs of returning depression. Ongoing monthly check-ins may be advised.
Image: AlinaTraut/Getty Images
Antidepressant discontinuation syndrome: diagnosis, prevention and treatment
04/18/2017
UP TO ZMISTU NUMBER
Withdrawal symptoms may occur after discontinuation of any class of antidepressants. The largest number of publications is devoted to selective serotonin reuptake inhibitors (SSRIs), apparently due to the fact that drugs of this class are most often prescribed for the treatment of depressive disorders. Usually these symptoms are mild and disappear on their own after a while. However, some patients may need to resume pharmacotherapy. This review briefly discusses the main clinical aspects of the antidepressant discontinuation syndrome.
Usually these symptoms are mild and disappear on their own after a while. However, some patients may need to resume pharmacotherapy. This review briefly discusses the main clinical aspects of the antidepressant discontinuation syndrome.
This condition is also called antidepressant withdrawal syndrome, although this is not entirely correct. The appearance of symptoms after stopping therapy does not mean that the drug is addictive. Antidepressants do not have addictive potential and do not cause addiction. This is an important positive point that should be communicated to patients, since most people will stop taking the prescribed treatment as soon as possible in case of fear of becoming dependent on the drug.
Why is it important to recognize antidepressant withdrawal syndrome?
There are three reasons: discomfort for the patient, diagnostic problem and possible compliance problems. Although withdrawal symptoms are rarely life-threatening, they are always associated with discomfort and some degree of psychosocial maladjustment. Hence the second problem: having experienced a withdrawal syndrome, the patient hardly agrees to any psychopharmacotherapy in the future. And finally, symptoms that occur in connection with the cessation of the action of an antidepressant can be mistaken for an exacerbation of a depressive disorder, another mental disorder, or a physical illness.
Although withdrawal symptoms are rarely life-threatening, they are always associated with discomfort and some degree of psychosocial maladjustment. Hence the second problem: having experienced a withdrawal syndrome, the patient hardly agrees to any psychopharmacotherapy in the future. And finally, symptoms that occur in connection with the cessation of the action of an antidepressant can be mistaken for an exacerbation of a depressive disorder, another mental disorder, or a physical illness.
For example, consider two typical scenarios. Convinced of achieving remission of major depressive disorder, the doctor hurries to please the patient that the antidepressant can be stopped, but forgets to tell how to do it correctly. The patient takes everything literally and the next day forgets about the medicine. A week later, he develops withdrawal symptoms, and he addresses his complaints to a) the same psychiatrist who forgets to ask how the antidepressant was withdrawn and perceives the symptoms as a relapse of depression; b) to another specialist, for example, a neurologist, to whom he prefers not to report about treatment with a psychiatrist. And the neurologist interprets these non-specific symptoms according to his competence. As a result, unnecessary examinations and possibly even treatment.
And the neurologist interprets these non-specific symptoms according to his competence. As a result, unnecessary examinations and possibly even treatment.
In addition, symptoms can be confused with side effects of a newly prescribed drug after discontinuation of an antidepressant, especially when switching between antidepressants with different mechanisms of action, for example, from paroxetine (SSRI) to bupropion (a dopamine and norepinephrine reuptake inhibitor). This can lead to the erroneous conclusion that the patient does not tolerate the new drug well. Symptoms of discontinuation of therapy may also be perceived as failure of therapy, especially irritability and anxiety.
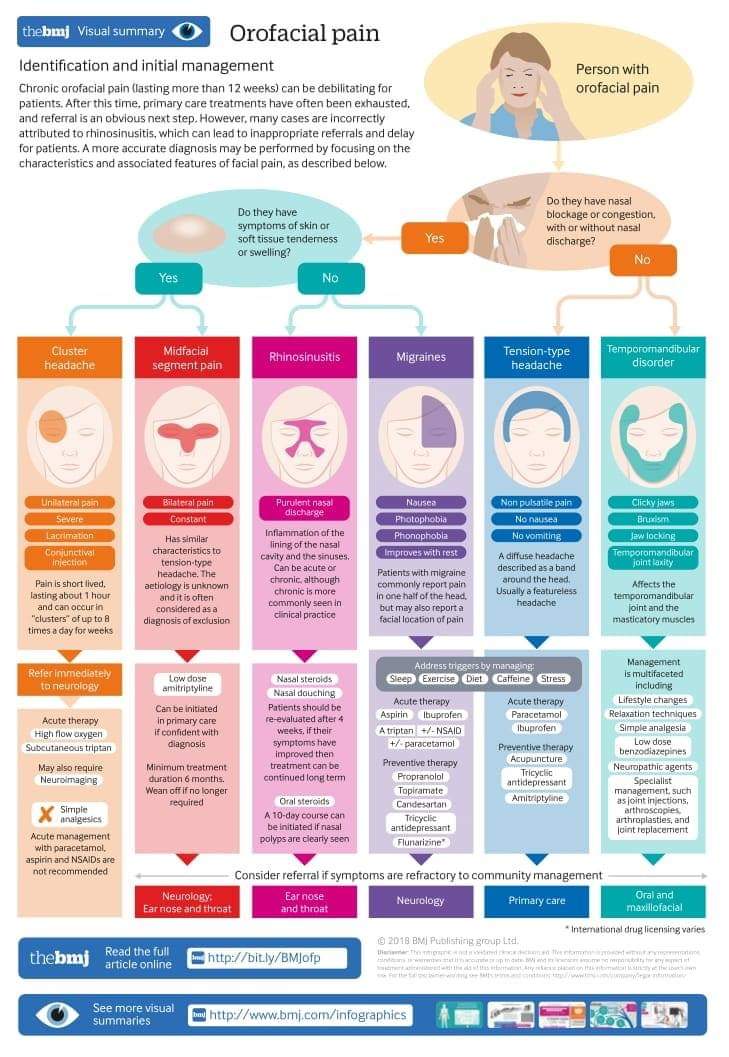
Symptoms of discontinuation of antidepressant therapy can be divided into six categories: sensory symptoms, balance disorders, general somatic, affective, gastrointestinal symptoms, and sleep disorders (Fig.).
At first, information about the listed manifestations was accumulated from reports of clinical cases. Then this problem was studied in prospective double-blind clinical trials in which patients were specifically randomized to the abolition of antidepressant therapy.
Then this problem was studied in prospective double-blind clinical trials in which patients were specifically randomized to the abolition of antidepressant therapy.
In English literature, a mnemonic device is used to memorize the spectrum of antidepressant withdrawal syndrome: the main symptoms are encrypted in the word FINISH.
F - from "flu-like" - flu-like symptoms;
I - insomnia;
N - from "nausea" - nausea;
I - from "imbalance" - imbalance;
S - sensory symptoms;
H - from "hyperarousal" - increased excitability, which reflects affective disorders.
It should be noted that the symptoms presented in the figure are mainly associated with discontinuation of SSRIs and serotonin and norepinephrine reuptake inhibitors. The spectrum of symptoms during withdrawal of monoamine oxidase inhibitors (MAOIs) and tricyclic antidepressants has its own specifics. Thus, in the event of discontinuation of tricyclic antidepressants, sensory symptoms and balance disorders, as a rule, are not observed. With the abolition of MAO inhibitors, symptoms may be more pronounced than after the abolition of SSRIs. Patients may experience a worsening of depressive and anxiety symptoms, an acute impairment of consciousness up to catatonia.
With the abolition of MAO inhibitors, symptoms may be more pronounced than after the abolition of SSRIs. Patients may experience a worsening of depressive and anxiety symptoms, an acute impairment of consciousness up to catatonia.
When do withdrawal symptoms appear and how long do they last?
They usually appear within the first week after stopping the antidepressant; according to studies, on average on the second day. Spontaneous resolution occurs at different times - from 1 day to 3 weeks, on average, patients continue to experience symptoms for 10 days.
What causes withdrawal syndrome?
The syndrome occurs when all classes of antidepressants are discontinued. The largest number of reports was recorded for paroxetine. The half-life of the drug from blood plasma is the indicator that correlates more than others with the risk of developing a withdrawal syndrome. In other words, the shorter the residual effect of the drug after the last dose, the higher the likelihood of symptoms.
For example, fluoxetine has a half-life of 7 days, so this SSRI has the lowest risk of withdrawal. Paroxetine has an average half-life of 24 hours, hence the high risk of withdrawal syndrome, especially when the therapeutic dose is abruptly stopped.
Can antidepressant discontinuation syndrome be distinguished from depression relapse?
Common symptoms include dysphoria, decreased appetite, sleep disturbances and fatigue. But there are also distinctive features—symptoms that are rarely seen in depression, such as sensory phenomena (paresthesias) as well as dizziness, headache, and nausea. In addition, in the case of withdrawal syndrome, a rapid (within 1 day) improvement can be observed when the drug is resumed, while recurrent depression does not respond so quickly to therapy.
Who is at risk for developing antidepressant withdrawal syndrome?
Typically, these are patients who begin to feel better after a few weeks of taking an antidepressant and are not sufficiently informed about the need for long-term maintenance therapy. Women who find out they are pregnant during treatment may also abruptly stop taking the antidepressant for safety reasons.
Women who find out they are pregnant during treatment may also abruptly stop taking the antidepressant for safety reasons.
How to stop antidepressants to minimize the risk of withdrawal?
Patients should be explained in an accessible form the features of the action of the prescribed antidepressant, the rules for increasing and gradually reducing the dose, and warn about a possible deterioration in well-being with an abrupt cessation of therapy. But at the same time, the words "withdrawal syndrome", "addiction", "addiction" should be avoided, since they can be perceived negatively and cause early termination of therapy. Sooner or later, that happy moment comes when it becomes clear that antidepressants can be abandoned. However, the withdrawal process, as a rule, takes several weeks, but in some cases even longer, especially if the patient's health worsens at the first steps of dose reduction. When prescribing fluoxetine, it is possible to cancel the drug without a gradual dose reduction, although it has not been specifically studied in studies.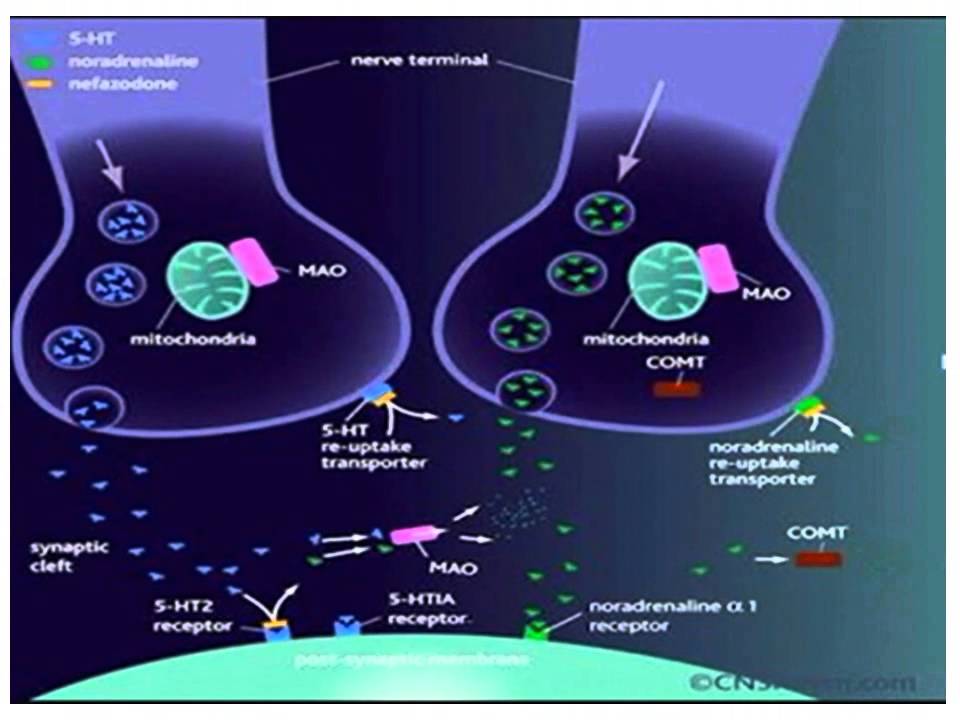
If possible, you should also discuss with the patient's relatives the creation of the most favorable conditions for the period of antidepressant withdrawal. Patients with major depressive disorder, as a rule, do not work and are at home, therefore they are not subjected to external psycho-emotional stress. It is optimal if the patient's close environment tries to create a positive atmosphere and tries to involve a family member in some kind of activity in order to distract from the perception of possible withdrawal symptoms.
How to help patients who complain of feeling worse after stopping antidepressants?
If this does happen, explain to the patient that the symptoms are not life-threatening and usually resolve within a few days. If the patient continues to experience symptoms and they reduce quality of life, it is common practice to restart the therapeutic dose of the antidepressant. In the future, you can again try to stop the drug through a very gradual dose reduction. If this does not help, then it is possible to transfer the patient to fluoxetine-SSRI with the lowest risk of withdrawal syndrome, and then cancel it.
If this does not help, then it is possible to transfer the patient to fluoxetine-SSRI with the lowest risk of withdrawal syndrome, and then cancel it.
Literature
1. Haddad P.M., AndersonI.M. (2007). Recognizing and managing antidepressant discontinuation symptoms. Advances in Psychiatric treatment, 13(6): 447-457.
2. Warner C.H., Bobo W., Warner C., Reid S., Rachal J. (2006). Antidepressant discontinuation syndrome. American Family Physician, 74(3): 449-456.
3. Renoir T. (2013). Selective serotonin reuptake inhibitor antidepressant treatment discontinuation syndrome: a review of the clinical evidence and the possible mechanisms involved. Frontiers in Pharmacology, 4.
Prepared by Dmitry Molchanov
- Number:
- Thematic issue "Neurology, Psychiatry, Psychotherapy" No. 1 (40), March 2017
21. 10.2022 PsychiatryFrequency and variability of non-negligible cases and associations with antidepressants: results of a systematic review, netting meta-analysis and economic modeling
10.2022 PsychiatryFrequency and variability of non-negligible cases and associations with antidepressants: results of a systematic review, netting meta-analysis and economic modeling
Great depressive discord affects approximately 350 million people in the whole world as the 13th cause of loss of health, followed by a global burden of illness [1, 2]. Antidepressants are the main means of treating the great depressive disorder. As previous studies have shown, drugs of the same class may have similar efficacy, but they may also vary significantly in the profile of side effects [3, 6-10]. Such manifestations as anxiety, sleeplessness, sexual dysfunction, changes in body mass, anhedonia (lack of satisfaction), are blamed practically on another patient's skin for depression, which can be overcome by the influx of antidepressants, which often become a cause [4]. Also, current recent data on side effects can help clinicians choose antidepressants to treat their patients.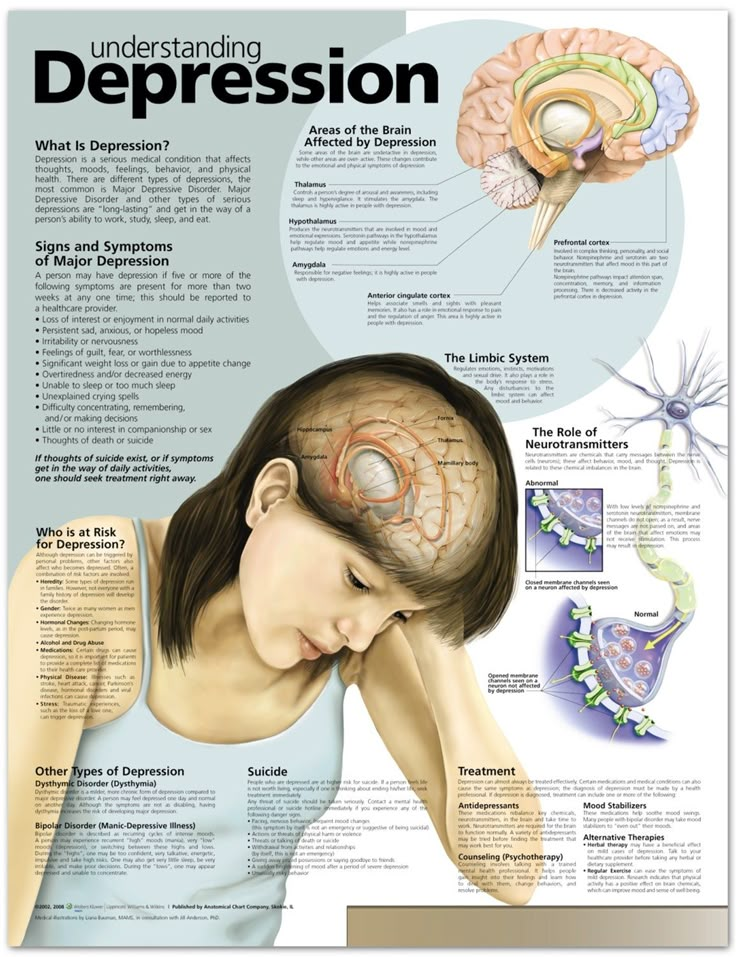 ...
...
10/17/2022 PsychiatryPost-traumatic stress disorder in the minds of the military camp: space and possibility of phytotherapy Our viiSkovі struggle in the minds of trival, the sobbing of the sovereign Zhitta Sustyatyv, and our civilian is the country of the same novin, about the no -reasoning of the hen of the hen of the tread, we are wounding the worship of the waist. It negatively affects the psycho-emotional state of people, so now not only psychiatrists, but representatives of other medical specializations and non-medical doctors can get stuck with post-traumatic stress disorder (PTSD) ....
10/17/2022 PsychiatryGamalate-V6 in the wake of the anxious states
The anxious state is an emotional discord, mindful of anxiety for the restlessness in front of the future podia or in a situation of innocence.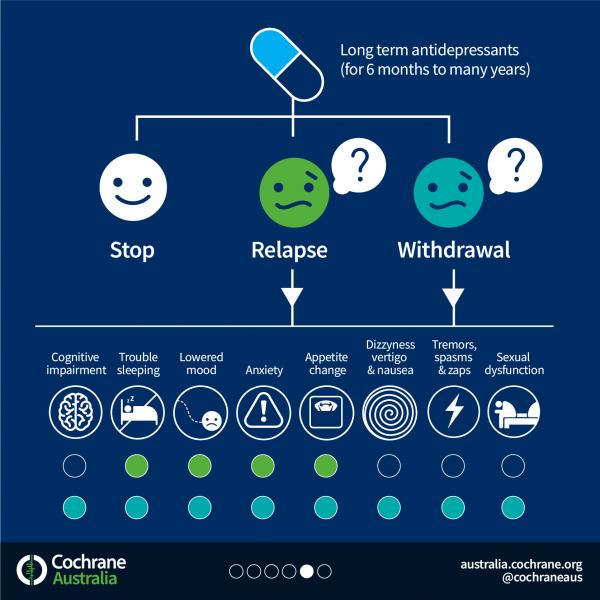 These physical changes are accompanied by organic symptoms (psychosomatic illnesses). On the other hand, organic illness can be troublesome, as if causing illness, pain, suffering of the patient, disrupted by the rhythm of that special social life, just work. Sedative drugs, especially benzodiazepines and sedatives, are most commonly seen in anxiety states. ...
These physical changes are accompanied by organic symptoms (psychosomatic illnesses). On the other hand, organic illness can be troublesome, as if causing illness, pain, suffering of the patient, disrupted by the rhythm of that special social life, just work. Sedative drugs, especially benzodiazepines and sedatives, are most commonly seen in anxiety states. ...
02.10.2022 Psychiatry Troubled discord in the practice of a family doctor: how can you safely repair it?
Scientific and practical conference “Until the Day of the Medical Practitioner (19.06.2022). International Conference on Advances in Health and Medical Science 2022 practitioners in various specialties for the development of topical nutrition and medical assistance to patients of a therapeutic profile. As part of the call, the professor of the Department of Internal Medicine of the Kharkiv National University named after I. V.N. Karazina, Doctor of Medical Sciences Marini Mykolaivna Kochueva "Anxious patient at the reception of a family doctor: how to recognize her safely repair?"....
As part of the call, the professor of the Department of Internal Medicine of the Kharkiv National University named after I. V.N. Karazina, Doctor of Medical Sciences Marini Mykolaivna Kochueva "Anxious patient at the reception of a family doctor: how to recognize her safely repair?"....
Antidepressant withdrawal syndrome. How to survive?
Do not stop your medications unless directed by your doctor. This is usually done gradually, the dosage is reduced every few days. But in the case of a phase inversion, when you switch from depression to hypomania or mania, withdrawal may occur more quickly.
If you're thinking of changing or stopping antidepressants, you need to know how your body might respond to chemical changes in your body, and it's even more important to know how you can ease withdrawal symptoms.
Best possible situation: you don't even need to read this article because there is no syndrome (hooray!).
Another option: you are experiencing withdrawal reactions, but you are ready for them and you know that they are temporary.
What to expect after stopping antidepressants
Many symptoms are associated with depression or anxiety, so it's worth keeping an eye on how you feel and how long it lasts. Often the withdrawal syndrome manifests itself as:
Don't stop antidepressants unless your psychiatrist tells you to.
It's easy to make the decision, "I don't want to burden the doctor" and start changing or stopping medication on your own. But please don't change anything unless your doctor tells you to, even if it's a small dose reduction. Antidepressants are helpful but potent, so it's important to consult a professional for the slightest change.
When you see a psychiatrist, ask how best to change your treatment. Usually, your doctor can make a plan to reduce your dosage instead of stopping abruptly. If you start a new medication, it is likely that it will be introduced gradually while lowering the level of the current medication. This will help alleviate withdrawal symptoms.
This will help alleviate withdrawal symptoms.
Get ready for panic attacks
You may feel panic during antidepressant withdrawal— either intermittently or continuously.
If you have already experienced panic attacks, use the techniques that are already suitable for you. If you haven't encountered them, place a paper bag next to your bed to breathe into during attacks. Practice deep breathing and count the objects in the room until your heartbeat stops.
Cry
Tears go hand in hand with panic attacks. In some cases, you can be very tearful. Our advice is to cry if you want to. You shouldn't be ashamed of it, and honestly, thanks to tears, you can feel quite refreshed. Do not be afraid.
Free up time in case of withdrawal
Especially if you stop treatment completely, free up a week or two of hard work to deal with it. Even a couple of days off can help. Give yourself time to adjust.
Of course, not everyone can take a day off at any time, but you can start “putting away” medication before the weekend, or at least clear your schedule.
 Here's how to distinguish discontinuation symptoms from relapse:
Here's how to distinguish discontinuation symptoms from relapse: 4 days
4 days 5 days
5 days