Icd 10 code neurocognitive disorder
Mild cognitive impairment of uncertain or unknown etiology
- ICD-10-CM Codes ›
- G00-G99 ›
- G30-G32 ›
- G31- ›
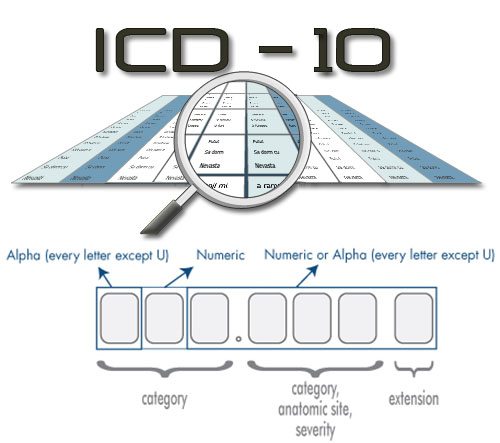
- 2023 ICD-10-CM Diagnosis Code G31.84
Mild cognitive impairment of uncertain or unknown etiology
- 2016 2017 2018 2019 2020 2021 2022 2023 - Revised Code Billable/Specific Code
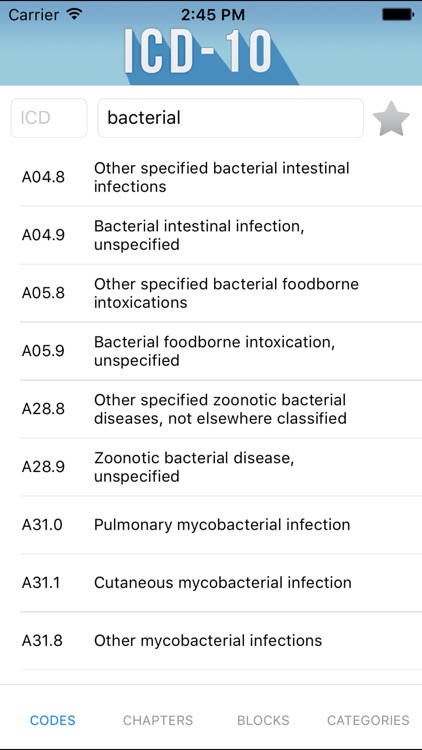
- G31.84 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- ICD-10-CM G31.84 is a revised 2023 ICD-10-CM code that became effective on October 1, 2022.
- This is the American ICD-10-CM version of G31.84 - other international versions of ICD-10 G31.84 may differ.
Applicable To
- Mild cognitive disorder NOS
- Mild neurocognitive disorder of uncertain or unknown etiology
Use Additional
Use Additional Help
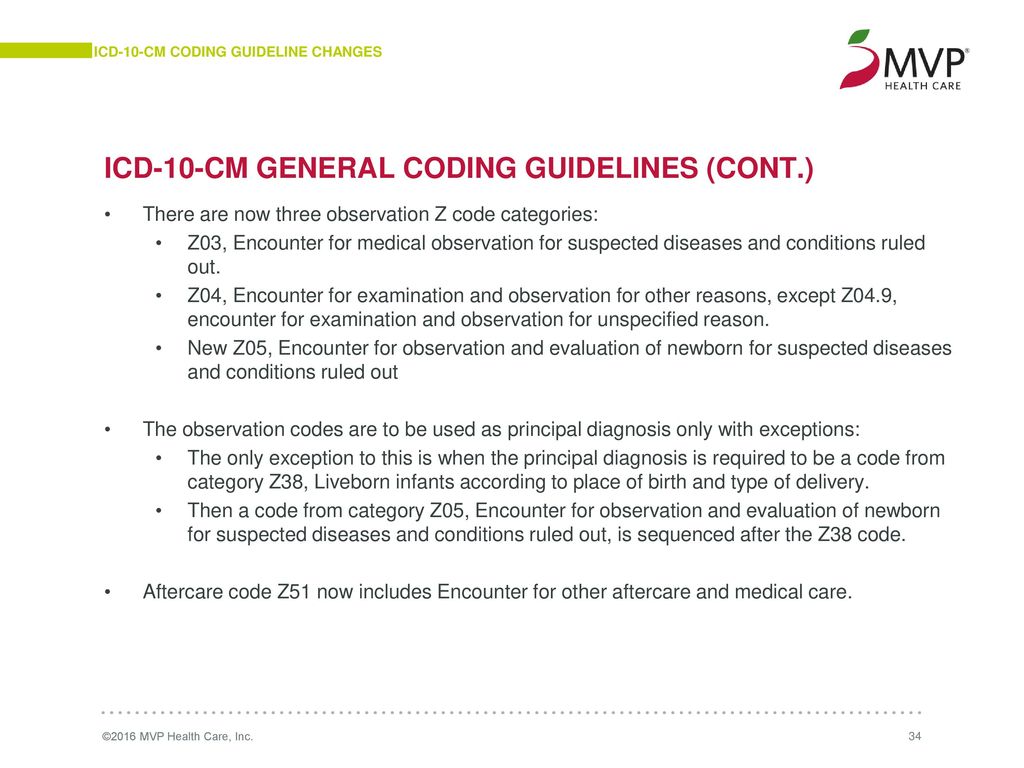
Certain conditions have both an underlying etiology and multiple body system manifestations due to the underlying etiology. For such conditions the ICD-10-CM has a coding convention that requires the underlying condition be sequenced first followed by the manifestation. Wherever such a combination exists there is a "use additional code" note at the etiology code, and a "code first" note at the manifestation code. These instructional notes indicate the proper sequencing order of the codes, etiology followed by manifestation. In most cases the manifestation codes will have in the code title, "in diseases classified elsewhere." Codes with this title are a component of the etiology/manifestation convention. The code title indicates that it is a manifestation code. "In diseases classified elsewhere" codes are never permitted to be used as first listed or principle diagnosis codes. They must be used in conjunction with an underlying condition code and they must be listed following the underlying condition.
- code to identify presence of:
- alcohol abuse and dependence (
ICD-10-CM Diagnosis Code F10
- F10 Alcohol related disorders
- F10.
 1 Alcohol abuse
1 Alcohol abuse- F10.10 …… uncomplicated
- F10.11 …… in remission
- F10.12 Alcohol abuse with intoxication
- F10.120 Alcohol abuse with intoxication, uncomplicate...
- F10.121 …… delirium
- F10.129 …… unspecified
- F10.13 Alcohol abuse, with withdrawal
- F10.130 Alcohol abuse with withdrawal, uncomplicated
- F10.131 Alcohol abuse with withdrawal delirium
- F10.132 Alcohol abuse with withdrawal with perceptual...
- F10.139 Alcohol abuse with withdrawal, unspecified
- F10.14 Alcohol abuse with alcohol-induced mood disor...
- F10.15 Alcohol abuse with alcohol-induced psychotic ...
- F10.150 Alcohol abuse with alcohol-induced psychotic ...
- F10.151 Alcohol abuse with alcohol-induced psychotic ...
- F10.159 Alcohol abuse with alcohol-induced psychotic ...
- F10.18 Alcohol abuse with other alcohol-induced diso...
- F10.180 Alcohol abuse with alcohol-induced anxiety di.
 ..
.. - F10.181 Alcohol abuse with alcohol-induced sexual dys...
- F10.182 Alcohol abuse with alcohol-induced sleep diso...
- F10.188 Alcohol abuse with other alcohol-induced diso...
- F10.180 Alcohol abuse with alcohol-induced anxiety di.
- F10.19 Alcohol abuse with unspecified alcohol-induce...
- F10.2 Alcohol dependence
- F10.20 …… uncomplicated
- F10.21 …… in remission
- F10.22 Alcohol dependence with intoxication
- F10.220 Alcohol dependence with intoxication, uncompl...
- F10.221 Alcohol dependence with intoxication delirium...
- F10.229 Alcohol dependence with intoxication, unspeci...
- F10.23 Alcohol dependence with withdrawal
- F10.230 Alcohol dependence with withdrawal, uncomplic...
- F10.231 …… delirium
- F10.232 Alcohol dependence with withdrawal with perce...
- F10.239 Alcohol dependence with withdrawal, unspecifi...
- F10.24 Alcohol dependence with alcohol-induced mood ...
- F10.
 25 Alcohol dependence with alcohol-induced psych...
25 Alcohol dependence with alcohol-induced psych...- F10.250 Alcohol dependence with alcohol-induced psych...
- F10.251 Alcohol dependence with alcohol-induced psych...
- F10.259 Alcohol dependence with alcohol-induced psych...
- F10.26 Alcohol dependence with alcohol-induced persi...
- F10.27 Alcohol dependence with alcohol-induced persi...
- F10.28 Alcohol dependence with other alcohol-induced...
- F10.280 Alcohol dependence with alcohol-induced anxie...
- F10.281 Alcohol dependence with alcohol-induced sexua...
- F10.282 Alcohol dependence with alcohol-induced sleep...
- F10.288 Alcohol dependence with other alcohol-induced...
- F10.29 Alcohol dependence with unspecified alcohol-i...
- F10.9 Alcohol use, unspecified
- F10.90 …… uncomplicated
- F10.91 …… in remission
- F10.92 Alcohol use, unspecified with intoxication
- F10.920 Alcohol use, unspecified with intoxication, u.
 ..
.. - F10.921 Alcohol use, unspecified with intoxication de...
- F10.929 Alcohol use, unspecified with intoxication, u...
- F10.920 Alcohol use, unspecified with intoxication, u.
- F10.93 Alcohol use, unspecified with withdrawal
- F10.930 Alcohol use, unspecified with withdrawal, unc...
- F10.931 Alcohol use, unspecified with withdrawal deli...
- F10.932 Alcohol use, unspecified with withdrawal with...
- F10.939 Alcohol use, unspecified with withdrawal, uns...
- F10.94 Alcohol use, unspecified with alcohol-induced...
- F10.95 Alcohol use, unspecified with alcohol-induced...
- F10.950 Alcohol use, unspecified with alcohol-induced...
- F10.951 Alcohol use, unspecified with alcohol-induced...
- F10.959 Alcohol use, unspecified with alcohol-induced...
- F10.96 Alcohol use, unspecified with alcohol-induced...
- F10.97 Alcohol use, unspecified with alcohol-induced...
- F10.98 Alcohol use, unspecified with other alcohol-i.
 ..
..- F10.980 Alcohol use, unspecified with alcohol-induced...
- F10.981 Alcohol use, unspecified with alcohol-induced...
- F10.982 Alcohol use, unspecified with alcohol-induced...
- F10.988 Alcohol use, unspecified with other alcohol-i...
- F10.99 Alcohol use, unspecified with unspecified alc...
- F10.
- F10 Alcohol related disorders
- exposure to environmental tobacco smoke (
ICD-10-CM Diagnosis Code Z77.22
Contact with and (suspected) exposure to environmental tobacco smoke (acute) (chronic)
- 2016 2017 2018 2019 2020 2021 2022 2023 Billable/Specific Code
Applicable To
- Exposure to second hand tobacco smoke (acute) (chronic)
- Passive smoking (acute) (chronic)
Type 1 Excludes
- nicotine dependence (F17.-)
- tobacco use (Z72.0)
Type 2 Excludes
- occupational exposure to environmental tobacco smoke (Z57.
 31)
31)
- history of tobacco dependence (
ICD-10-CM Diagnosis Code Z87.891
Personal history of nicotine dependence
- 2016 2017 2018 2019 2020 2021 2022 2023 Billable/Specific Code POA Exempt
Type 1 Excludes
- current nicotine dependence (F17.2-)
- hypertension (I10-I16
ICD-10-CM Range I10-I16
Hypertensive diseases
Type 1 Excludes
- neonatal hypertension (P29.2)
- primary pulmonary hypertension (I27.0)
Type 2 Excludes
- hypertensive disease complicating pregnancy, childbirth and the puerperium (O10-O11, O13-O16)
Use Additional
- code to identify:
- exposure to environmental tobacco smoke (Z77.22)
- history of tobacco dependence (Z87.891)
- occupational exposure to environmental tobacco smoke (Z57.31)
- tobacco dependence (F17.
 -)
-) - tobacco use (Z72.0)
- I10 Essential (primary) hypertension
- I11 Hypertensive heart disease
- I12 Hypertensive chronic kidney disease
- I13 Hypertensive heart and chronic kidney di...
- I15 Secondary hypertension
- I16 Hypertensive crisis
- occupational exposure to environmental tobacco smoke (
ICD-10-CM Diagnosis Code Z57.31
Occupational exposure to environmental tobacco smoke
- 2016 2017 2018 2019 2020 2021 2022 2023 Billable/Specific Code POA Exempt
Type 2 Excludes
- exposure to environmental tobacco smoke (Z77.22)
- tobacco dependence (
ICD-10-CM Diagnosis Code F17
- F17 Nicotine dependence
- F17.2 Nicotine dependence
- F17.20 Nicotine dependence, unspecified
- F17.200 Nicotine dependence, unspecified, uncomplicat...
- F17.201 Nicotine dependence, unspecified, in remissio...
- F17.
 203 Nicotine dependence unspecified, with withdra...
203 Nicotine dependence unspecified, with withdra... - F17.208 Nicotine dependence, unspecified, with other ...
- F17.209 Nicotine dependence, unspecified, with unspec...
- F17.21 Nicotine dependence, cigarettes
- F17.210 Nicotine dependence, cigarettes, uncomplicate...
- F17.211 Nicotine dependence, cigarettes, in remission...
- F17.213 Nicotine dependence, cigarettes, with withdra...
- F17.218 Nicotine dependence, cigarettes, with other n...
- F17.219 Nicotine dependence, cigarettes, with unspeci...
- F17.22 Nicotine dependence, chewing tobacco
- F17.220 Nicotine dependence, chewing tobacco, uncompl...
- F17.221 Nicotine dependence, chewing tobacco, in remi...
- F17.223 Nicotine dependence, chewing tobacco, with wi...
- F17.228 Nicotine dependence, chewing tobacco, with ot...
- F17.229 Nicotine dependence, chewing tobacco, with un...
- F17.29 Nicotine dependence, other tobacco product
- F17.
 290 Nicotine dependence, other tobacco product, u...
290 Nicotine dependence, other tobacco product, u... - F17.291 Nicotine dependence, other tobacco product, i...
- F17.293 Nicotine dependence, other tobacco product, w...
- F17.298 Nicotine dependence, other tobacco product, w...
- F17.299 Nicotine dependence, other tobacco product, w...
- F17.
- F17.20 Nicotine dependence, unspecified
- F17.2 Nicotine dependence
- F17 Nicotine dependence
- tobacco use (
ICD-10-CM Diagnosis Code Z72.0
Tobacco use
- 2016 2017 2018 2019 2020 2021 2022 2023 Billable/Specific Code POA Exempt
Applicable To
- Tobacco use NOS
Type 1 Excludes
- history of tobacco dependence (Z87.891)
- nicotine dependence (F17.2-)
- tobacco dependence (F17.2-)
- tobacco use during pregnancy (O99.33-)
Type 1 Excludes
Type 1 Excludes Help
A type 1 excludes note is a pure excludes. It means "not coded here". A type 1 excludes note indicates that the code excluded should never be used at the same time as G31.84. A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
A type 1 excludes note indicates that the code excluded should never be used at the same time as G31.84. A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
- age related cognitive decline (
ICD-10-CM Diagnosis Code R41.81
Age-related cognitive decline
- 2016 2017 2018 2019 2020 2021 2022 2023 Billable/Specific Code Adult Dx (15-124 years)
Applicable To
- Senility NOS
- altered mental status (
ICD-10-CM Diagnosis Code R41.82
Altered mental status, unspecified
- 2016 2017 2018 2019 2020 2021 2022 2023 Billable/Specific Code
Applicable To
- Change in mental status NOS
Type 1 Excludes
- altered level of consciousness (R40.-)
- altered mental status due to known condition - code to condition
- delirium NOS (R41.
 0)
0)
- cerebral degeneration (
ICD-10-CM Diagnosis Code G31.9
Degenerative disease of nervous system, unspecified
- 2016 2017 2018 2019 2020 2021 2022 2023 Billable/Specific Code
- cerebrovascular diseases (I60-I69
ICD-10-CM Range I60-I69
Cerebrovascular diseases
Type 1 Excludes
- traumatic intracranial hemorrhage (S06.-)
Use Additional
- code to identify presence of:
- alcohol abuse and dependence (F10.-)
- exposure to environmental tobacco smoke (Z77.22)
- history of tobacco dependence (Z87.891)
- hypertension (I10-I16)
- occupational exposure to environmental tobacco smoke (Z57.31)
- tobacco dependence (F17.-)
- tobacco use (Z72.0)
- I60 Nontraumatic subarachnoid hemorrhage
- I61 Nontraumatic intracerebral hemorrhage
- I62 Other and unspecified nontraumatic intra.
 ..
.. - I63 Cerebral infarction
- I65 Occlusion and stenosis of precerebral ar...
- I66 Occlusion and stenosis of cerebral arter...
- I67 Other cerebrovascular diseases
- I68 Cerebrovascular disorders in diseases cl...
- I69 Sequelae of cerebrovascular disease
- change in mental status (
ICD-10-CM Diagnosis Code R41.82
Altered mental status, unspecified
- 2016 2017 2018 2019 2020 2021 2022 2023 Billable/Specific Code
Applicable To
- Change in mental status NOS
Type 1 Excludes
- altered level of consciousness (R40.-)
- altered mental status due to known condition - code to condition
- delirium NOS (R41.0)
- cognitive deficits following (sequelae of) cerebral hemorrhage or infarction (
ICD-10-CM Diagnosis Code I69.01
Cognitive deficits following nontraumatic subarachnoid hemorrhage
- 2016 2017 - Converted to Parent Code 2018 2019 2020 2021 2022 2023 Non-Billable/Non-Specific Code
 01-,
01-, ICD-10-CM Diagnosis Code I69.11
Cognitive deficits following nontraumatic intracerebral hemorrhage
- 2016 2017 - Converted to Parent Code 2018 2019 2020 2021 2022 2023 Non-Billable/Non-Specific Code
ICD-10-CM Diagnosis Code I69.21
Cognitive deficits following other nontraumatic intracranial hemorrhage
- 2016 2017 - Converted to Parent Code 2018 2019 2020 2021 2022 2023 Non-Billable/Non-Specific Code
ICD-10-CM Diagnosis Code I69.31
Cognitive deficits following cerebral infarction
- 2016 2017 - Converted to Parent Code 2018 2019 2020 2021 2022 2023 Non-Billable/Non-Specific Code
ICD-10-CM Diagnosis Code I69.81
Cognitive deficits following other cerebrovascular disease
- 2016 2017 - Converted to Parent Code 2018 2019 2020 2021 2022 2023 Non-Billable/Non-Specific Code
ICD-10-CM Diagnosis Code I69.91
Cognitive deficits following unspecified cerebrovascular disease
- 2016 2017 - Converted to Parent Code 2018 2019 2020 2021 2022 2023 Non-Billable/Non-Specific Code
 91-)
91-) - cognitive impairment due to intracranial or head injury (
ICD-10-CM Diagnosis Code S06
- S06.0 Concussion
- S06.1 Traumatic cerebral edema
- S06.2 Diffuse traumatic brain injury
- S06.3 Focal traumatic brain injury
- S06.4 Epidural hemorrhage
- S06.5 Traumatic subdural hemorrhage
- S06.6 Traumatic subarachnoid hemorrhage
- S06.8 Other specified intracranial injuries
- S06.9 Unspecified intracranial injury
- S06.A Traumatic brain compression and herniation
- dementia (
ICD-10-CM Diagnosis Code F01
- F01 Vascular dementia
- F01.5 Vascular dementia, unspecified severity
- F01.50 Vascular dementia, unspecified severity, with...
- F01.51 Vascular dementia, unspecified severity, with...
- F01.511 Vascular dementia, unspecified severity, with...
- F01.518 Vascular dementia, unspecified severity, with...
- F01.52 Vascular dementia, unspecified severity, with.
 ..
.. - F01.53 Vascular dementia, unspecified severity, with...
- F01.54 Vascular dementia, unspecified severity, with...
- F01.A Vascular dementia, mild
- F01.A0 Vascular dementia, mild, without behavioral d...
- F01.A1 Vascular dementia, mild, with behavioral dist...
- F01.A11 Vascular dementia, mild, with agitation
- F01.A18 Vascular dementia, mild, with other behaviora...
- F01.A2 Vascular dementia, mild, with psychotic distu...
- F01.A3 Vascular dementia, mild, with mood disturbanc...
- F01.A4 …… with anxiety
- F01.B Vascular dementia, moderate
- F01.B0 Vascular dementia, moderate, without behavior...
- F01.B1 Vascular dementia, moderate, with behavioral ...
- F01.B11 Vascular dementia, moderate, with agitation
- F01.B18 Vascular dementia, moderate, with other behav...
- F01.B2 Vascular dementia, moderate, with psychotic d...
- F01.
 B3 Vascular dementia, moderate, with mood distur...
B3 Vascular dementia, moderate, with mood distur... - F01.B4 …… with anxiety
- F01.C Vascular dementia, severe
- F01.C0 Vascular dementia, severe, without behavioral...
- F01.C1 Vascular dementia, severe, with behavioral di...
- F01.C11 Vascular dementia, severe, with agitation
- F01.C18 Vascular dementia, severe, with other behavio...
- F01.C2 Vascular dementia, severe, with psychotic dis...
- F01.C3 Vascular dementia, severe, with mood disturba...
- F01.C4 …… with anxiety
- F01.5 Vascular dementia, unspecified severity
ICD-10-CM Diagnosis Code F02
- F02 Dementia in other diseases classified elsewhe...
- F02.8 Dementia in other diseases classified elsewhe...
- F02.80 Dementia in other diseases classified elsewhe...
- F02.81 Dementia in other diseases classified elsewhe...
- F02.811 Dementia in other diseases classified elsewhe...
- F02.818 Dementia in other diseases classified elsewhe.
 ..
..
- F02.82 Dementia in other diseases classified elsewhe...
- F02.83 Dementia in other diseases classified elsewhe...
- F02.84 Dementia in other diseases classified elsewhe...
- F02.A Dementia in other diseases classified elsewhe...
- F02.A0 Dementia in other diseases classified elsewhe...
- F02.A1 Dementia in other diseases classified elsewhe...
- F02.A11 Dementia in other diseases classified elsewhe...
- F02.A18 Dementia in other diseases classified elsewhe...
- F02.A2 Dementia in other diseases classified elsewhe...
- F02.A3 Dementia in other diseases classified elsewhe...
- F02.A4 Dementia in other diseases classified elsewhe...
- F02.B Dementia in other diseases classified elsewhe...
- F02.B0 Dementia in other diseases classified elsewhe...
- F02.B1 Dementia in other diseases classified elsewhe...
- F02.B11 Dementia in other diseases classified elsewhe.
 ..
.. - F02.B18 Dementia in other diseases classified elsewhe...
- F02.B11 Dementia in other diseases classified elsewhe.
- F02.B2 Dementia in other diseases classified elsewhe...
- F02.B3 Dementia in other diseases classified elsewhe...
- F02.B4 Dementia in other diseases classified elsewhe...
- F02.C Dementia in other diseases classified elsewhe...
- F02.C0 Dementia in other diseases classified elsewhe...
- F02.C1 Dementia in other diseases classified elsewhe...
- F02.C11 Dementia in other diseases classified elsewhe...
- F02.C18 Dementia in other diseases classified elsewhe...
- F02.C2 Dementia in other diseases classified elsewhe...
- F02.C3 Dementia in other diseases classified elsewhe...
- F02.C4 Dementia in other diseases classified elsewhe...
- F02.8 Dementia in other diseases classified elsewhe...
ICD-10-CM Diagnosis Code F03
Unspecified dementia
- 2016 2017 2018 2019 2020 2021 2022 2023 Non-Billable/Non-Specific Code
Applicable To
- Major neurocognitive disorder NOS
- Presenile dementia NOS
- Presenile psychosis NOS
- Primary degenerative dementia NOS
- Senile dementia NOS
- Senile dementia depressed or paranoid type
- Senile psychosis NOS
Type 1 Excludes
- senility NOS (R41.
 81)
81)
Type 2 Excludes
- mild memory disturbance due to known physiological condition (F06.8)
- senile dementia with delirium or acute confusional state (F05)
- F01 Vascular dementia
- mild neurocognitive disorder due to a known physiological condition (
ICD-10-CM Diagnosis Code F06.7
Mild neurocognitive disorder due to known physiological condition
- 2023 - New Code Non-Billable/Non-Specific Code
Applicable To
- Mild neurocognitive impairment due to a known physiological condition
Code First
- the underlying physiological condition, such as:
- Alzheimer's disease (G30.-)
- frontotemporal neurocognitive disorder (G31.09)
- human immunodeficiency virus [HIV] disease (B20)
- Huntington's disease (G10)
- Neurocognitive disorder with Lewy bodies (G31.83)
- Parkinson's disease (G20)
- systemic lupus erythematosus (M32.
 -)
-) - traumatic brain injury (S06.-)
- vitamin B deficiency (E53-)
Type 1 Excludes
- age related cognitive decline (R41.81)
- altered mental status (R41.82)
- cerebral degeneration (G31.9)
- change in mental status (R41.82)
- cognitive deficits following (sequelae of) cerebral hemorrhage or infarction (I69.01-I69.11-, I69.21-I69.31-, I69.81- I69.91-)
- dementia (F01.-, F02.-, F03)
- mild cognitive impairment due to unknown or unspecified etiology (G31.84)
- neurologic neglect syndrome (R41.4)
- personality change, nonpsychotic (F68.8)
- neurologic neglect syndrome (
ICD-10-CM Diagnosis Code R41.4
Neurologic neglect syndrome
- 2016 2017 2018 2019 2020 2021 2022 2023 Billable/Specific Code
Applicable To
- Asomatognosia
- Hemi-akinesia
- Hemi-inattention
- Hemispatial neglect
- Left-sided neglect
- Sensory neglect
- Visuospatial neglect
Type 1 Excludes
- visuospatial deficit (R41.
 842)
842)
- personality change, nonpsychotic (
ICD-10-CM Diagnosis Code F68.8
Other specified disorders of adult personality and behavior
- 2016 2017 2018 2019 2020 2021 2022 2023 Billable/Specific Code
The following code(s) above G31.84 contain annotation back-references
Annotation Back-References
In this context, annotation back-references refer to codes that contain:
- Applicable To annotations, or
- Code Also annotations, or
- Code First annotations, or
- Excludes1 annotations, or
- Excludes2 annotations, or
- Includes annotations, or
- Note annotations, or
- Use Additional annotations
that may be applicable to G31.84:
- G00-G99
2023 ICD-10-CM Range G00-G99
Diseases of the nervous system
Type 2 Excludes
- certain conditions originating in the perinatal period (P04-P96)
- certain infectious and parasitic diseases (A00-B99)
- complications of pregnancy, childbirth and the puerperium (O00-O9A)
- congenital malformations, deformations, and chromosomal abnormalities (Q00-Q99)
- endocrine, nutritional and metabolic diseases (E00-E88)
- injury, poisoning and certain other consequences of external causes (S00-T88)
- neoplasms (C00-D49)
- symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (R00-R94)
- G31
ICD-10-CM Diagnosis Code G31
Other degenerative diseases of nervous system, not elsewhere classified
- 2016 2017 2018 2019 2020 2021 2022 2023 Non-Billable/Non-Specific Code
Type 2 Excludes
- Reye's syndrome (G93.
 7)
7)
Use Additional
- For codes G31.0-G31.83, G31.85-G31.9, use additional code, if applicable, to identify:
- dementia with anxiety (F02.84, F02.A4, F02.B4, F02.C4)
- dementia with behavioral disturbance (F02.81-, F02.A1-, F02.B1-, F02.C1-)
- dementia with mood disturbance (F02.83, F02.A3, F02.B3, F02.C3)
- dementia with psychotic disturbance (F02.82, F02.A2, F02.B2, F02.C2)
- dementia without behavioral disturbance (F02.80, F02.A0, F02.B0, F02.C0)
- mild neurocognitive disorder due to known physiological condition (F06.7-)
- Reye's syndrome (G93.
Approximate Synonyms
- Cognitive impairment due to human immunodeficiency virus infection
- Hiv related cognitive impairment
- Mild cognitive impairment
- Mild cognitive impairment, so stated
- Mild neurocognitive disorder co-occurrent and due to alzheimer's disease
- Mild neurocognitive disorder co-occurrent and due to frontotemporal lobar degeneration
- Mild neurocognitive disorder co-occurrent and due to human immunodeficiency virus infection
- Mild neurocognitive disorder co-occurrent and due to huntington's disease
- Mild neurocognitive disorder co-occurrent and due to lewy body disease
- Mild neurocognitive disorder co-occurrent and due to multiple etiologies
- Mild neurocognitive disorder co-occurrent and due to parkinson's disease
- Mild neurocognitive disorder co-occurrent and due to prion disease
- Mild neurocognitive disorder co-occurrent and due to traumatic brain injury
- Mild neurocognitive disorder due to alzheimers disease
- Mild neurocognitive disorder due to frontotemporal lobar degeneration
- Mild neurocognitive disorder due to hiv infection
- Mild neurocognitive disorder due to huntingtons disease
- Mild neurocognitive disorder due to lewy body disease
- Mild neurocognitive disorder due to multiple etiologies
- Mild neurocognitive disorder due to parkinsons disease
- Mild neurocognitive disorder due to prion disease
- Mild neurocognitive disorder due to traumatic brain injury
- Minimal cognitive impairment
ICD-10-CM G31. 84 is grouped within Diagnostic Related Group(s) (MS-DRG v40.0):
84 is grouped within Diagnostic Related Group(s) (MS-DRG v40.0):
- 056 Degenerative nervous system disorders with mcc
- 057 Degenerative nervous system disorders without mcc
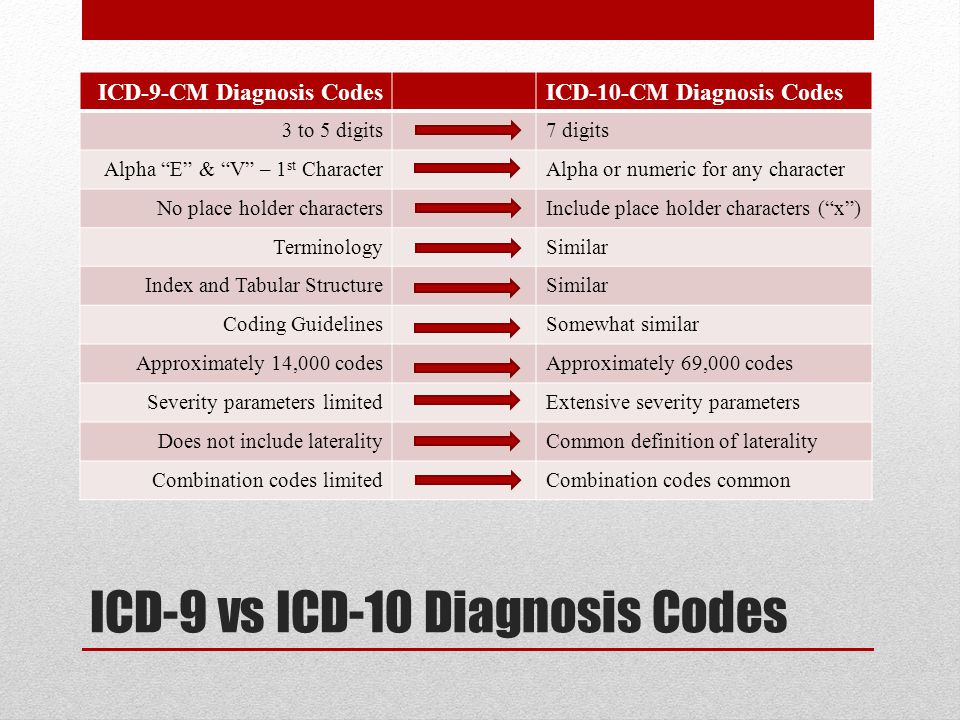
Convert G31.84 to ICD-9-CM
Code History
- 2016 (effective 10/1/2015): New code (first year of non-draft ICD-10-CM)
- 2017 (effective 10/1/2016): No change
- 2018 (effective 10/1/2017): No change
- 2019 (effective 10/1/2018): No change
- 2020 (effective 10/1/2019): No change
- 2021 (effective 10/1/2020): No change
- 2022 (effective 10/1/2021): No change
-
2023 (effective 10/1/2022): Revised code
- New description: Mild cognitive impairment of uncertain or unknown etiology
- 2022 description: Mild cognitive impairment, so stated
Code annotations containing back-references to G31.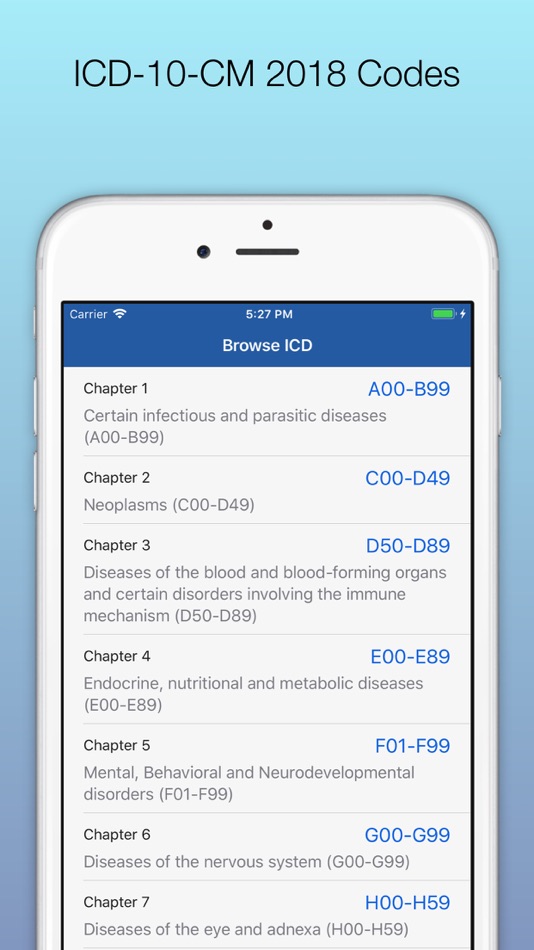 84:
84:
-
Type 1 Excludes: R41, F06.7, F07.0
ICD-10-CM Diagnosis Code R41
Other symptoms and signs involving cognitive functions and awareness
- 2016 2017 2018 2019 2020 2021 2022 2023 Non-Billable/Non-Specific Code
Type 1 Excludes
- dissociative [conversion] disorders (F44.-)
- mild cognitive impairment, so stated (G31.84)
ICD-10-CM Diagnosis Code F06.7
Mild neurocognitive disorder due to known physiological condition
- 2023 - New Code Non-Billable/Non-Specific Code
Applicable To
- Mild neurocognitive impairment due to a known physiological condition
Code First
- the underlying physiological condition, such as:
- Alzheimer's disease (G30.
 -)
-) - frontotemporal neurocognitive disorder (G31.09)
- human immunodeficiency virus [HIV] disease (B20)
- Huntington's disease (G10)
- Neurocognitive disorder with Lewy bodies (G31.83)
- Parkinson's disease (G20)
- systemic lupus erythematosus (M32.-)
- traumatic brain injury (S06.-)
- vitamin B deficiency (E53-)
Type 1 Excludes
- age related cognitive decline (R41.81)
- altered mental status (R41.82)
- cerebral degeneration (G31.9)
- change in mental status (R41.82)
- cognitive deficits following (sequelae of) cerebral hemorrhage or infarction (I69.01-I69.11-, I69.21-I69.31-, I69.81- I69.91-)
- dementia (F01.-, F02.-, F03)
- mild cognitive impairment due to unknown or unspecified etiology (G31.84)
- neurologic neglect syndrome (R41.4)
- personality change, nonpsychotic (F68.8)
ICD-10-CM Diagnosis Code F07.
 0
0
Personality change due to known physiological condition
- 2016 2017 2018 2019 2020 2021 2022 2023 Billable/Specific Code
Applicable To
- Frontal lobe syndrome
- Limbic epilepsy personality syndrome
- Lobotomy syndrome
- Organic personality disorder
- Organic pseudopsychopathic personality
- Organic pseudoretarded personality
- Postleucotomy syndrome
Type 1 Excludes
- mild cognitive impairment (G31.84)
- postconcussional syndrome (F07.81)
- postencephalitic syndrome (F07.89)
- signs and symptoms involving emotional state (R45.-)
Type 2 Excludes
- specific personality disorder (F60.-)
Diagnosis Index entries containing back-references to G31.84:
ICD-10-CM Codes Adjacent To G31.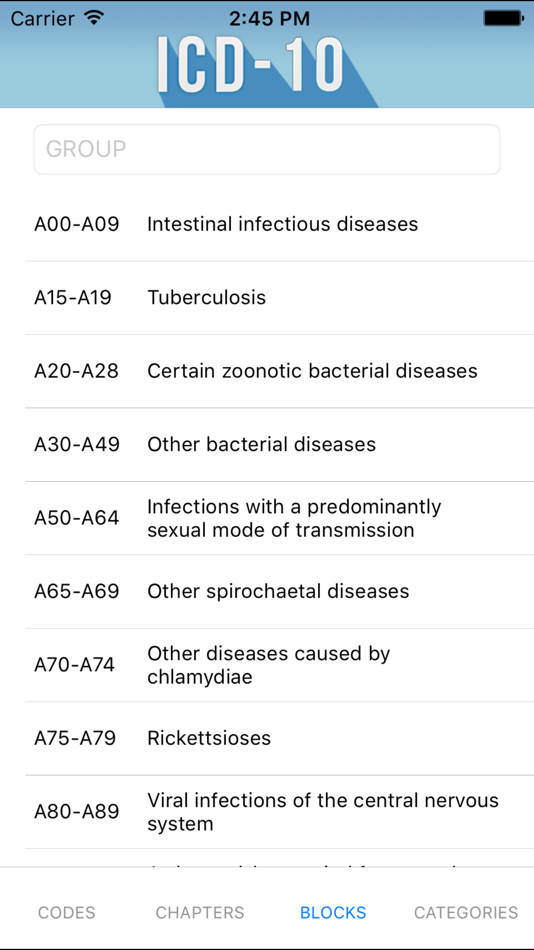 84
84
G31 Other degenerative diseases of nervous system, not elsewhere classified
G31.0 Frontotemporal dementia
G31.01 Pick's disease
G31.09 Other frontotemporal neurocognitive disorder
G31. 1 Senile degeneration of brain, not elsewhere classified
1 Senile degeneration of brain, not elsewhere classified
G31.2 Degeneration of nervous system due to alcohol
G31.8 Other specified degenerative diseases of nervous system
G31.81 Alpers disease
G31.82 Leigh's disease
G31.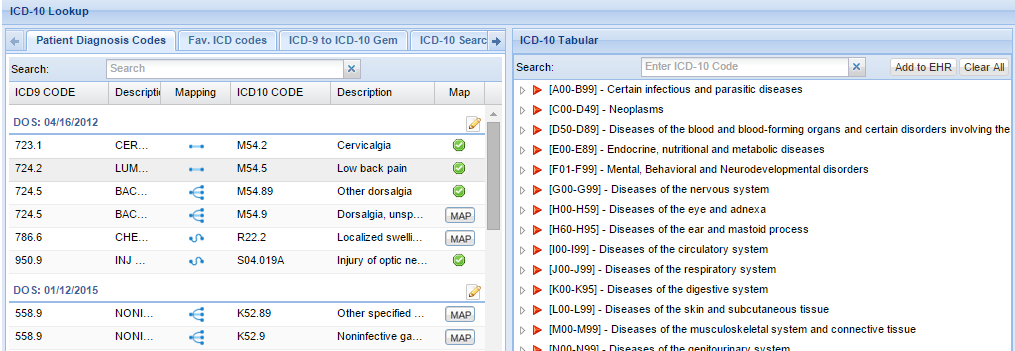 83 Neurocognitive disorder with Lewy bodies
83 Neurocognitive disorder with Lewy bodies
G31.84 Mild cognitive impairment of uncertain or unknown etiology
G31.85 Corticobasal degeneration
G31.89 Other specified degenerative diseases of nervous system
G31. 9 Degenerative disease of nervous system, unspecified
9 Degenerative disease of nervous system, unspecified
G32 Other degenerative disorders of nervous system in diseases classified elsewhere
G32.0 Subacute combined degeneration of spinal cord in diseases classified elsewhere
G32.8 Other specified degenerative disorders of nervous system in diseases classified elsewhere
G32.81 Cerebellar ataxia in diseases classified elsewhere
G32.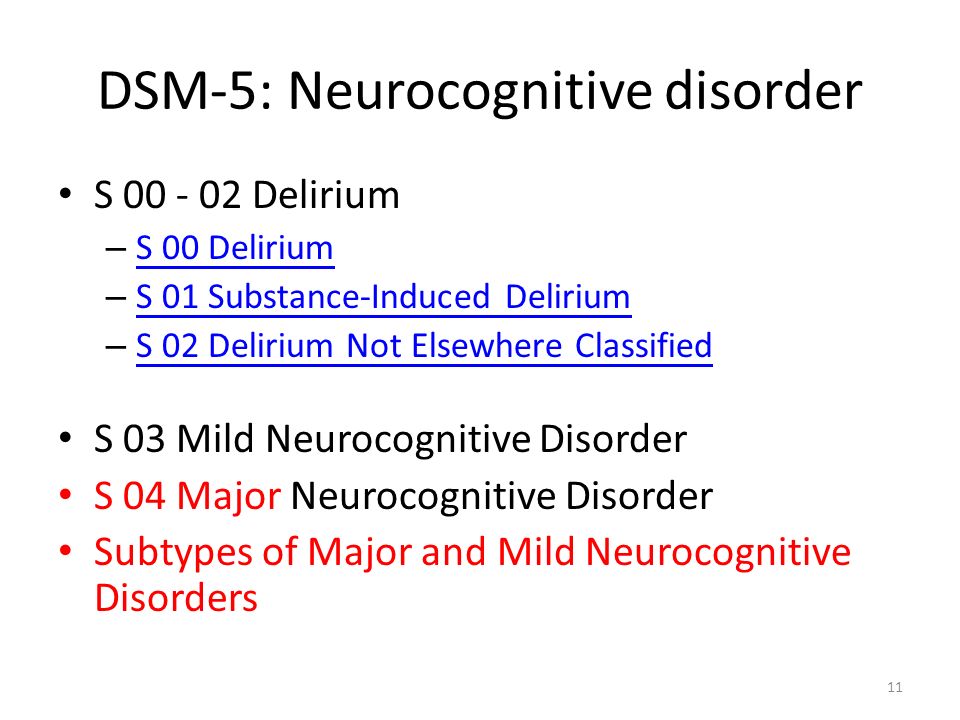 89 Other specified degenerative disorders of nervous system in diseases classified elsewhere
89 Other specified degenerative disorders of nervous system in diseases classified elsewhere
G35 Multiple sclerosis
G36 Other acute disseminated demyelination
Reimbursement claims with a date of service on or after October 1, 2015 require the use of ICD-10-CM codes.
Unspecified symptoms and signs involving cognitive functions and awareness
- ICD-10-CM Codes ›
- R00-R99 ›
- R40-R46 ›
- R41- ›
- 2023 ICD-10-CM Diagnosis Code R41.9
Unspecified symptoms and signs involving cognitive functions and awareness
- 2016 2017 2018 2019 2020 2021 2022 2023 Billable/Specific Code
- R41.
 9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. - Short description: Unsp symptoms and signs w cognitive functions and awareness
- The 2023 edition of ICD-10-CM R41.9 became effective on October 1, 2022.
- This is the American ICD-10-CM version of R41.9 - other international versions of ICD-10 R41.9 may differ.
Applicable To
- Unspecified neurocognitive disorder
The following code(s) above R41.9 contain annotation back-references
Annotation Back-References
In this context, annotation back-references refer to codes that contain:
- Applicable To annotations, or
- Code Also annotations, or
- Code First annotations, or
- Excludes1 annotations, or
- Excludes2 annotations, or
- Includes annotations, or
- Note annotations, or
- Use Additional annotations
that may be applicable to R41.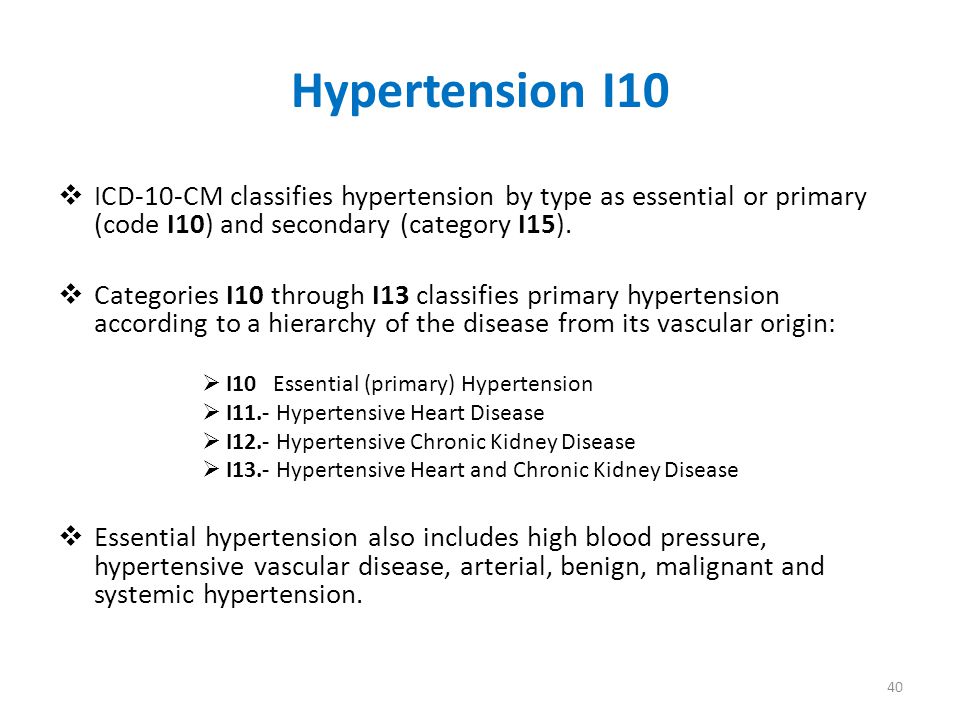 9:
9:
- R00-R99
2023 ICD-10-CM Range R00-R99
Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified
Note
- This chapter includes symptoms, signs, abnormal results of clinical or other investigative procedures, and ill-defined conditions regarding which no diagnosis classifiable elsewhere is recorded.
- Signs and symptoms that point rather definitely to a given diagnosis have been assigned to a category in other chapters of the classification. In general, categories in this chapter include the less well-defined conditions and symptoms that, without the necessary study of the case to establish a final diagnosis, point perhaps equally to two or more diseases or to two or more systems of the body. Practically all categories in the chapter could be designated 'not otherwise specified', 'unknown etiology' or 'transient'. The Alphabetical Index should be consulted to determine which symptoms and signs are to be allocated here and which to other chapters.
 The residual subcategories, numbered .8, are generally provided for other relevant symptoms that cannot be allocated elsewhere in the classification.
The residual subcategories, numbered .8, are generally provided for other relevant symptoms that cannot be allocated elsewhere in the classification. - The conditions and signs or symptoms included in categories R00-R94 consist of:
- (a) cases for which no more specific diagnosis can be made even after all the facts bearing on the case have been investigated;
- (b) signs or symptoms existing at the time of initial encounter that proved to be transient and whose causes could not be determined;
- (c) provisional diagnosis in a patient who failed to return for further investigation or care;
- (d) cases referred elsewhere for investigation or treatment before the diagnosis was made;
- (e) cases in which a more precise diagnosis was not available for any other reason;
- (f) certain symptoms, for which supplementary information is provided, that represent important problems in medical care in their own right.
Type 2 Excludes
- abnormal findings on antenatal screening of mother (O28.
 -)
-) - certain conditions originating in the perinatal period (P04-P96)
- signs and symptoms classified in the body system chapters
- signs and symptoms of breast (N63, N64.5)
- R40-R46
2023 ICD-10-CM Range R40-R46
Symptoms and signs involving cognition, perception, emotional state and behavior
Type 2 Excludes
- symptoms and signs constituting part of a pattern of mental disorder (F01-F99)
- R41
ICD-10-CM Diagnosis Code R41
Other symptoms and signs involving cognitive functions and awareness
- 2016 2017 2018 2019 2020 2021 2022 2023 Non-Billable/Non-Specific Code
Type 1 Excludes
- dissociative [conversion] disorders (F44.-)
- mild cognitive impairment, so stated (G31.
 84)
84)
ICD-10-CM R41.9 is grouped within Diagnostic Related Group(s) (MS-DRG v40.0):
- 947 Signs and symptoms with mcc
- 948 Signs and symptoms without mcc
Convert R41.9 to ICD-9-CM
Code History
- 2016 (effective 10/1/2015): New code (first year of non-draft ICD-10-CM)
- 2017 (effective 10/1/2016): No change
- 2018 (effective 10/1/2017): No change
- 2019 (effective 10/1/2018): No change
- 2020 (effective 10/1/2019): No change
- 2021 (effective 10/1/2020): No change
- 2022 (effective 10/1/2021): No change
- 2023 (effective 10/1/2022): No change
Diagnosis Index entries containing back-references to R41. 9:
9:
ICD-10-CM Codes Adjacent To R41.9
R41.81 Age-related cognitive decline
R41.82 Altered mental status, unspecified
R41.83 Borderline intellectual functioning
R41.84 Other specified cognitive deficit
R41. 840 Attention and concentration deficit
840 Attention and concentration deficit
R41.841 Cognitive communication deficit
R41.842 Visuospatial deficit
R41.843 Psychomotor deficit
R41. 844 Frontal lobe and executive function deficit
844 Frontal lobe and executive function deficit
R41.89 Other symptoms and signs involving cognitive functions and awareness
R41.9 Unspecified symptoms and signs involving cognitive functions and awareness
R42 Dizziness and giddiness
R43 Disturbances of smell and taste
R43. 0 Anosmia
0 Anosmia
R43.1 Parosmia
R43.2 Parageusia
R43.8 Other disturbances of smell and taste
R43.9 Unspecified disturbances of smell and taste
R44 Other symptoms and signs involving general sensations and perceptions
R44. 0 Auditory hallucinations
0 Auditory hallucinations
R44.1 Visual hallucinations
Reimbursement claims with a date of service on or after October 1, 2015 require the use of ICD-10-CM codes.
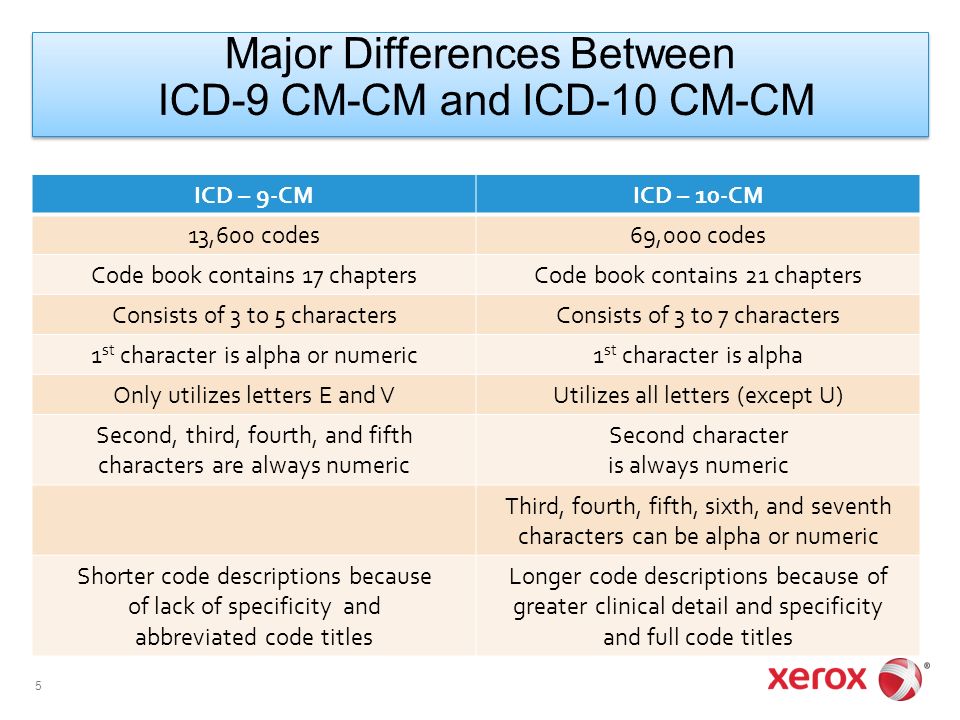
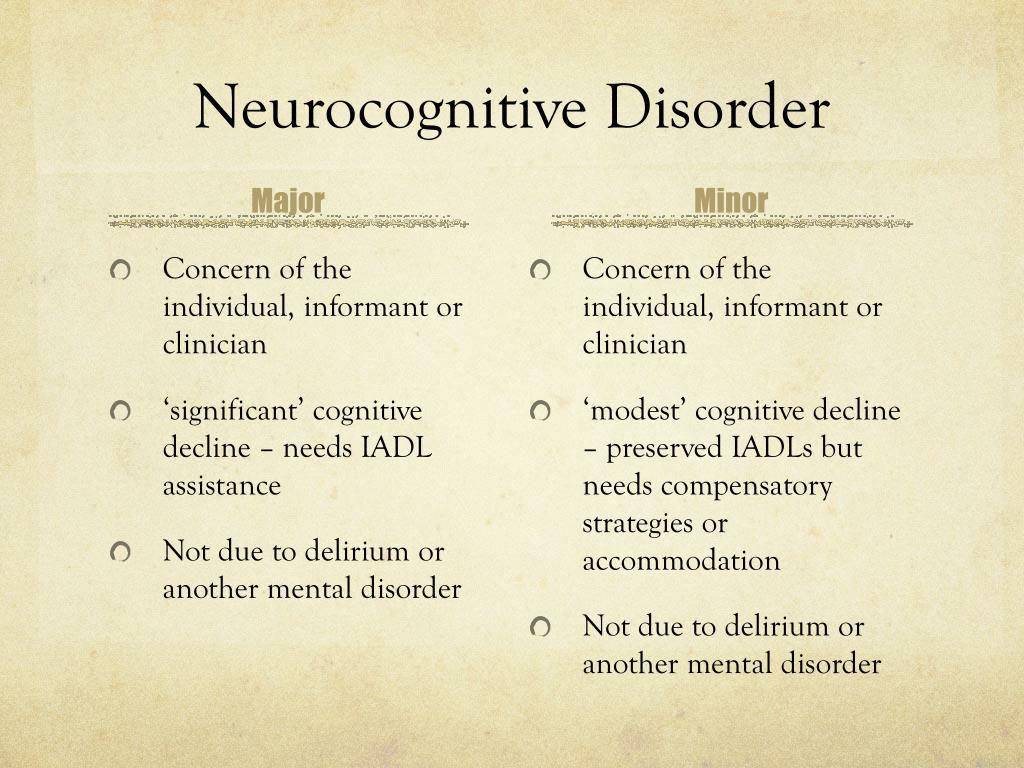
90,000 neurocognitive disorders in ICD -11: a new proposal and its result - World Psychiatry No. 02 2019
Subscribe to new numbers
Author:Wolfgang Gaebel1,2, Geoffrey M. Reed3,4, Robert Jakob5
1Department of Psychiatry and Psychotherapy, Medical Faculty, Heinrich-Heine University Düsseldorf, LVR-Klinikum Düsseldorf, Düsseldorf, Germany; 2WHO Collaborating Center on Quality Assurance and Empowerment in Mental Health, Düsseldorf, Germany; 3Department of Mental Health and Substance Abuse, World Health Organization, Geneva, Switzerland; 4Department of Psychiatry, Columbia University Medical Center, New York, NY, USA; 5Department of Health Statistics and Information Systems, World Health Organization, Geneva, Switzerlan
Issue page numbers: 239-240
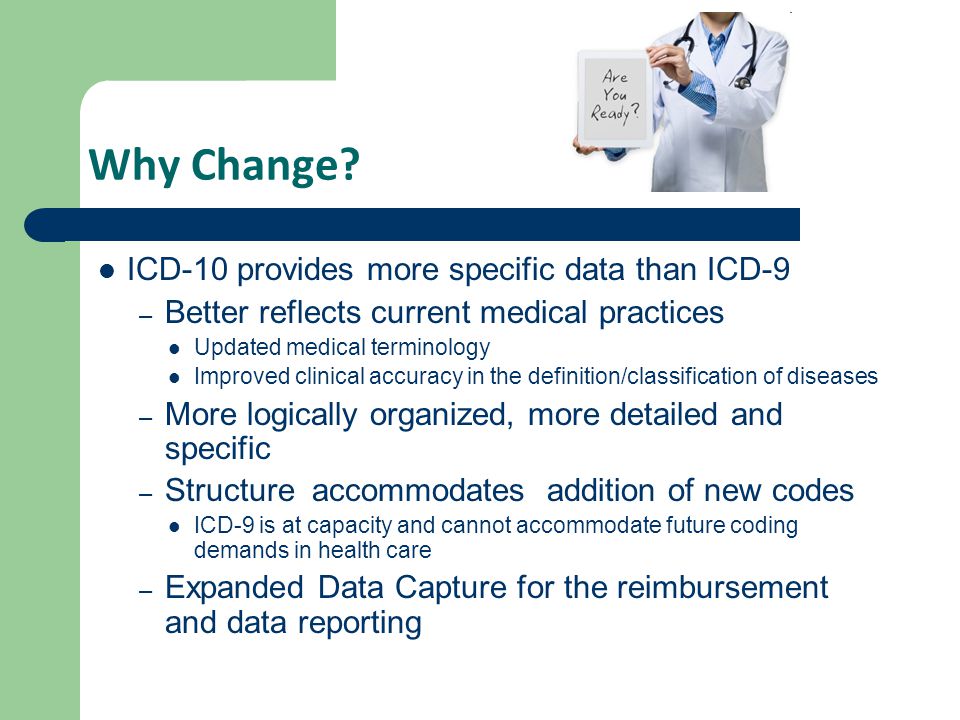
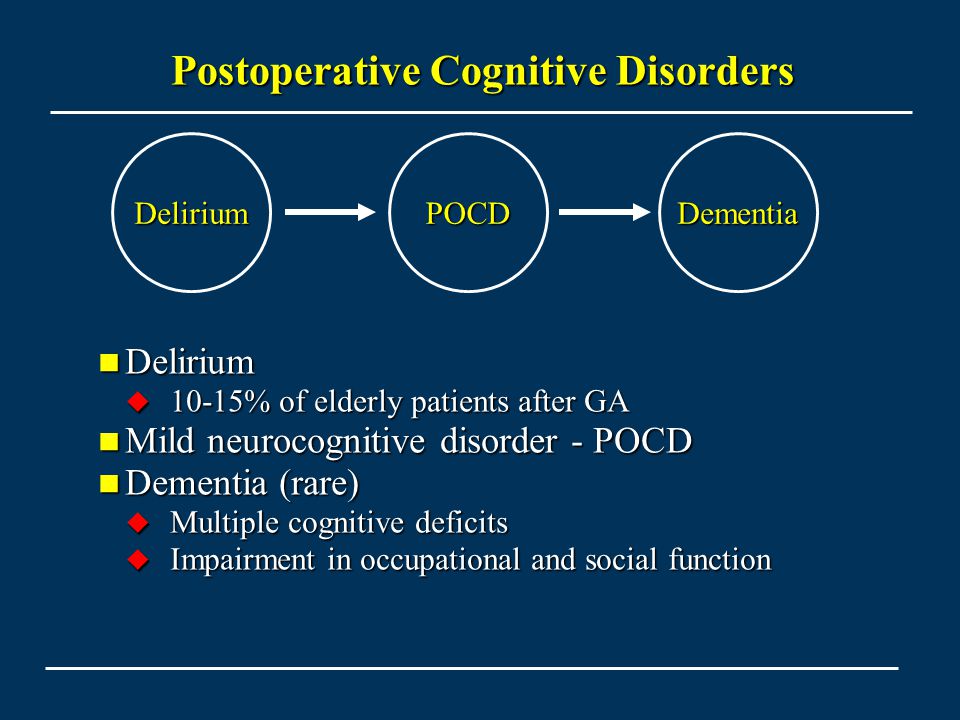
The optimal classification of diseases involving neurocognitive impairment has been an area of professional controversy between psychiatry and neurology over the past few years. This is reflected in the groupings of "neurocognitive disorders" in chapter 6 on mental disorders and "disorders with neurocognitive impairment as one of the main features" in chapter 8 on diseases of the nervous system in the preliminary version of the ICD-11.
This is reflected in the groupings of "neurocognitive disorders" in chapter 6 on mental disorders and "disorders with neurocognitive impairment as one of the main features" in chapter 8 on diseases of the nervous system in the preliminary version of the ICD-11.
The optimal classification of diseases involving neurocognitive impairment has been an area of professional controversy between psychiatry and neurology over the past few years. This is reflected in the groupings of "neurocognitive disorders" in chapter 6 on mental disorders and "disorders with neurocognitive impairment as one of the main features" in chapter 8 on diseases of the nervous system in the preliminary version of the ICD-11.
The controversy over the placement of dementias in the ICD-11 was resolved by international consensus following the intervention of several mental health scientific associations1, with categories of dementias included in Chapter 6 and their underlying causes presented in Chapter 8, in line with the logic of
ICD-10.
In August 2018, a group of neurologists posted on the ICD-11 website a “complex hierarchical change proposal” proposing to replace “vascular dementia” with “vascular cognitive impairment” (VCI)2. Referring to the publication of a primer3, VCI was defined as “the contribution of vascular disease to cognitive impairment of any severity, from subjective cognitive decline and mild cognitive impairment to dementia”. In fact, the proposal argues that the term "vascular dementia" used in Chapter 6 has become "obsolete" and should be replaced by VCI in Chapter 8.
The stated rationale3 was that “vascular pathology is common in the elderly with and without cognitive decline... mainly caused by a combination of degenerative brain pathology in association with ischemia...; this requires a thorough neurological and imaging examination and will permanently rule out the diagnosis of 'vascular dementia' without proper investigations." The proposal ended with: “We also invite our colleagues in Chapter 6 on mental health to reconsider their definition of vascular dementia.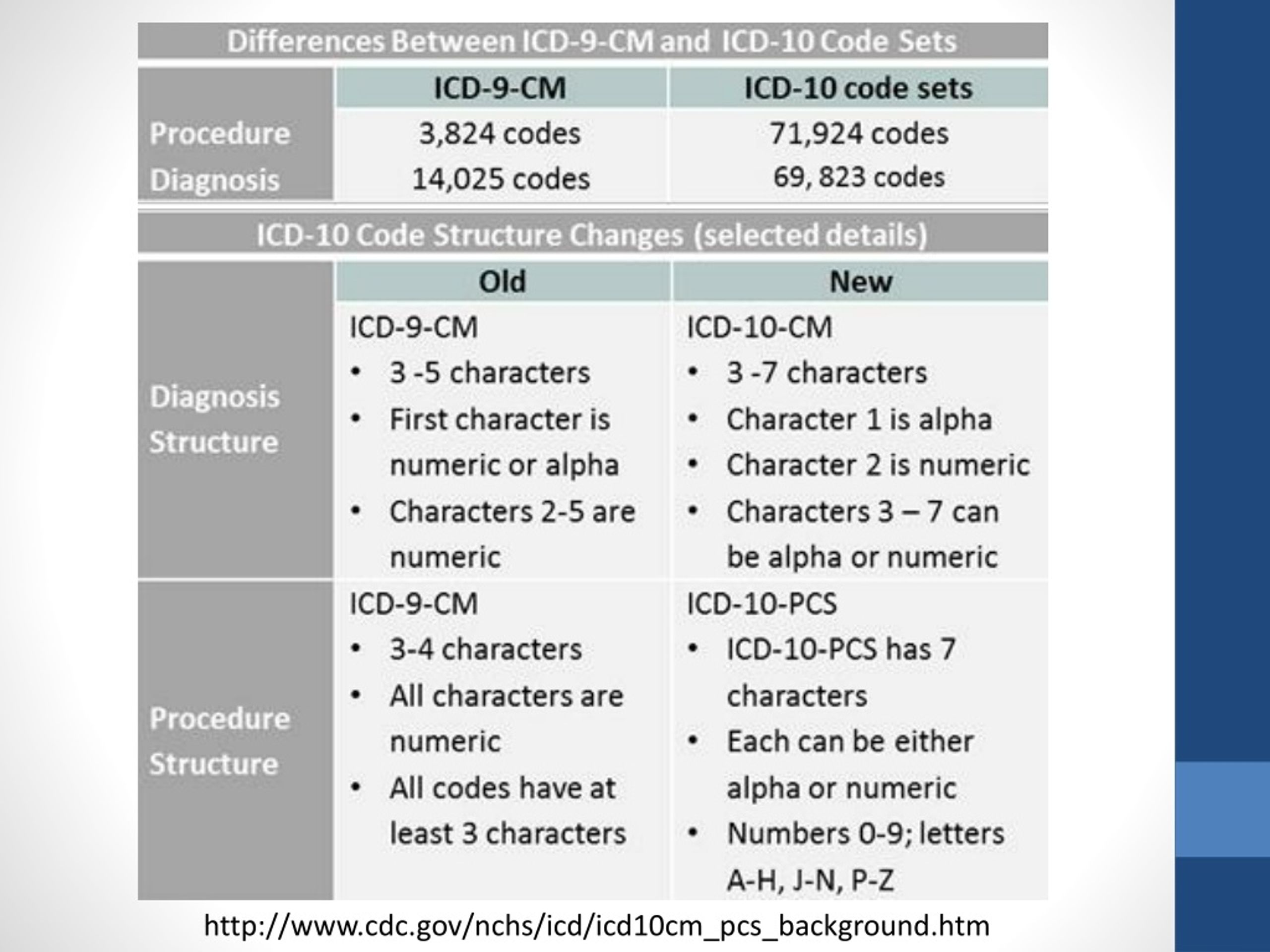 It is imperative that the ICD-11 truly reflects contemporary thinking and practice in the 21st century.”
It is imperative that the ICD-11 truly reflects contemporary thinking and practice in the 21st century.”
Following consultation with the World Health Organization (WHO), a round table was organized at the World Psychiatric Congress in Mexico City in September 2018 with invited psychiatric experts. A consensus was reached to publish the critical commentary after its endorsement by a broader group of experts representing various national and international scientific psychiatric associations4.
A comment posted on October 19, 2018 says:
• Even if it were appropriate to include "cognitive impairment" as a clinical manifestation of diseases or disorders, its proper place would be in the "Neurocognitive disorders" section of Chapter 6. In addition, it remains unclear why the term "vascular" should be added to cognitive impairment. , since the authors themselves rightly argue that vascular causes are almost never the exclusive etiology of this disorder.
• In addition, the VCI proposal refers to a pathoclinic continuum of cognitive impairment, drawn from current research on Alzheimer's disease models5.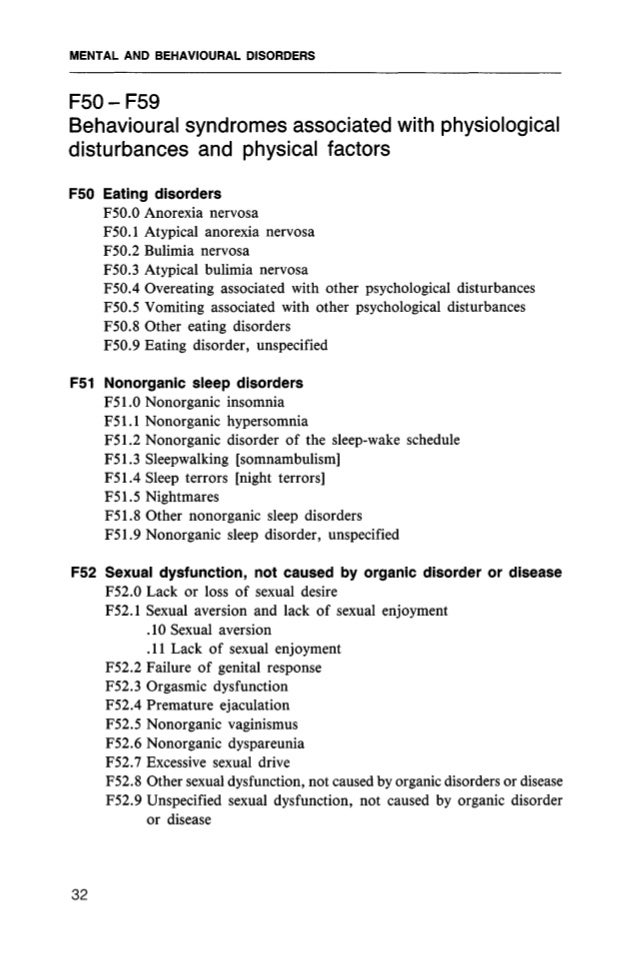 It lacks a clear classification concept, a convincing definition, an explicit operationalization of the "cognitive" profile, as well as a reasonable gradation of the severity of the "violation". Therefore, its diagnostic and classification relationship with subjective (preclinical), mild or severe forms (dementia) remains unclear and not consistently developed for use in the ICD-11.
It lacks a clear classification concept, a convincing definition, an explicit operationalization of the "cognitive" profile, as well as a reasonable gradation of the severity of the "violation". Therefore, its diagnostic and classification relationship with subjective (preclinical), mild or severe forms (dementia) remains unclear and not consistently developed for use in the ICD-11.
• With regard to predominantly vascular forms of neurocognitive disorders, the proposal does not reflect the close similarity between the terms 'vascular cognitive impairment' and 'vascular dementia', nor the option that they have of subsequent reconciliation with the detailed category 'cerebrovascular disease' in Chapter 8. Thus, the proposal to move, rename or replace vascular dementia with VCI does not comply with current classification principles6 and is not ready for implementation.
• Accordingly, the use of the term VCI and the suggestion of purely vascular cognitive "impairment" as a separate category is unconvincing. Moreover, "vascular" as a collective term refers to very different cerebrovascular diseases that may interact with other etiologies and whose role may change over the course of life. Therefore, "vascular" should not be used as a fixed combination in terms of a broad spectrum, such as VCI, covering multiple stages of diagnosis and etiology of cognitive impairment.
Moreover, "vascular" as a collective term refers to very different cerebrovascular diseases that may interact with other etiologies and whose role may change over the course of life. Therefore, "vascular" should not be used as a fixed combination in terms of a broad spectrum, such as VCI, covering multiple stages of diagnosis and etiology of cognitive impairment.
Taking into account modern scientific achievements3,5, the ICD-116 classification rules, the existing ICD-11 classification and the coding of neurocognitive disorders in chapters 6 and 81, the following changes were proposed:
• For 'vascular dementia', the coding note states that 'this category should never be used in primary tabulation'. Upon subsequent agreement, "6D81 vascular dementia" may already be associated with various "cerebrovascular diseases" from chapter 8, with "6D86 behavioral or psychological disorders in dementia" if necessary, and with an additional severity code. "6D80.2 dementia in Alzheimer's disease, mixed type with cerebrovascular disease" already makes it possible to code for mixed etiological forms of dementia, as recommended in the above proposal.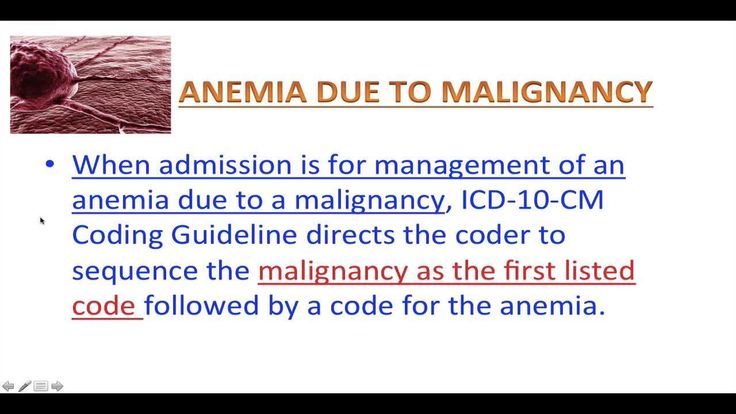 In the case of multiple etiologies, whatever is applicable can be coded.
In the case of multiple etiologies, whatever is applicable can be coded.
• However, for consistency in classification, vascular dementia should be reformulated as "dementia due to cerebrovascular disease" after the previously agreed wording ("dementia due to...") of the other categories of dementia in Chapter 6, and must necessarily be aligned with the corresponding category of cerebrovascular disease. in chapter 8.
• A related issue is the etiological rationale for "6D71 mild neurocognitive disorder". Subsequent reconciliation makes it possible to add as causal conditions a number of "diseases classified elsewhere" from Chapter 8 and others. However, there is no option to add "cerebrovascular disease" or multiple conditions. This needs to be corrected.
• Together with these proposed changes, the current version of ICD-11 regarding neurocognitive disorders of a vascular nature would already allow coding for mild and severe stages of neurocognitive disorders of a vascular or mixed etiology.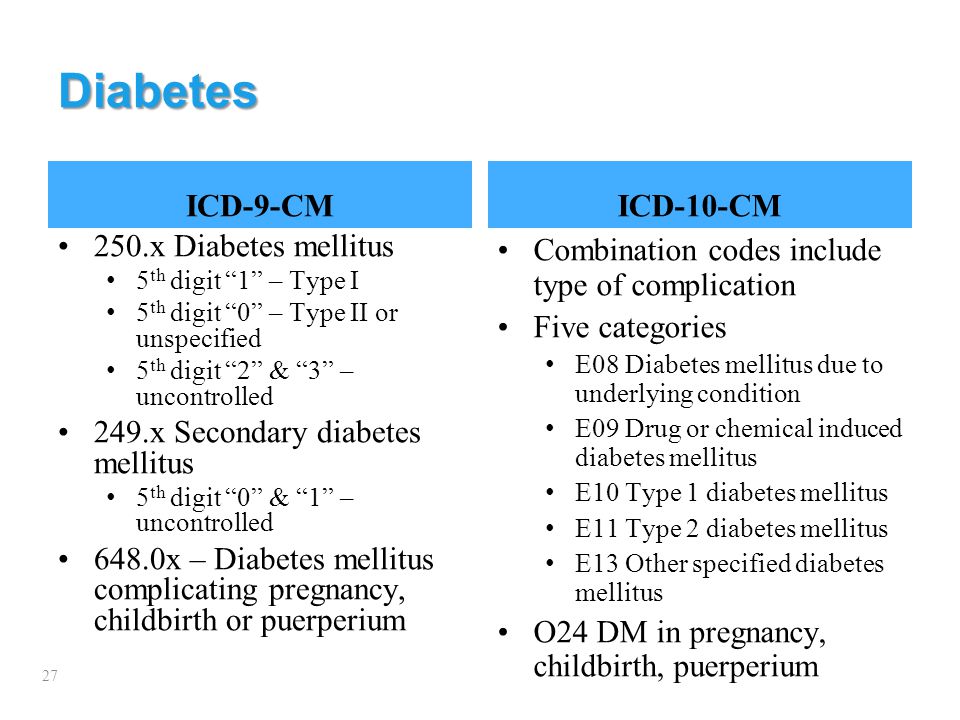
In conclusion, we note that the introduction of a new VCI category in Chapter 8 seems premature and unacceptable in terms of: a) the underdeveloped status of the classification concept of this object and b) its insufficient adaptation to the existing structure and coding options for neurocognitive disorders in ICD-11.
On October 20/21, 2018, the authors of the VCI proposal published agreement7 with the above proposals and refused to introduce the VCI in chapter 8. After being brought to the attention of the responsible WHO authorities, the results of the discussion and subsequent actions were officially approved at the WHO Conference on the International Classification of ICD-11 in Seoul.
As of December 18, 2018, the proposed changes are being implemented in both the suspended and the current version of ICD-11 (https://icd.who.int/browse11/l-m/en).
Translation : Shunenkov D.A. (Ivanovo)
Editing : Ph.D. Boyko A.S. (Tomsk)
Gaebel W, Reed GM, Jakob R. Neurocognitive disorders in ICD-11: a new proposal and its outcome. World Psychiatry 2019;18(2):232-233.
Neurocognitive disorders in ICD-11: a new proposal and its outcome. World Psychiatry 2019;18(2):232-233.
DOI: 10.1002/wps.20634
List of used literature Hide list
1. Gaebel W, Jessen F, Kanba S. World Psychiatry 2018;17:229-30.
2. Shakir R, Scheltens P, Rossor M. Complex hierarchical changes proposal: Vascular dementia/vascular cognitive impairment (VCI). icd.who.int.
3. van der Flier WM, Skoog I, Schneider JA et al. Nat Rev Dis Primers 2018;4:18003.
4. Gaebel W. Comment: Vascular dementia/VCI. icd.who.int.
5. Jack CR, Bennett DA, Blennow K et al. Alzheimers Dement 2018;14:535-62.
6. World Health Organization. ICD-11 reference guide. icd.who.int.
7. Shakir R, Scheltens P, Rossor M. Comments: Vascular dementia/VCI. icd.who.int.
15 May 2019
Views: 645
0003
classification, main causes and treatment uMEDp
The article provides a definition, classification, diagnostic criteria, principles of pathogenetic and symptomatic therapy of non-dementia cognitive impairment. The possibilities of using the dopaminergic and noradrenergic drug piribedil (Pronoran) for the treatment of mild and moderate cognitive impairments that do not reach the severity of dementia are considered in detail.
The possibilities of using the dopaminergic and noradrenergic drug piribedil (Pronoran) for the treatment of mild and moderate cognitive impairments that do not reach the severity of dementia are considered in detail.
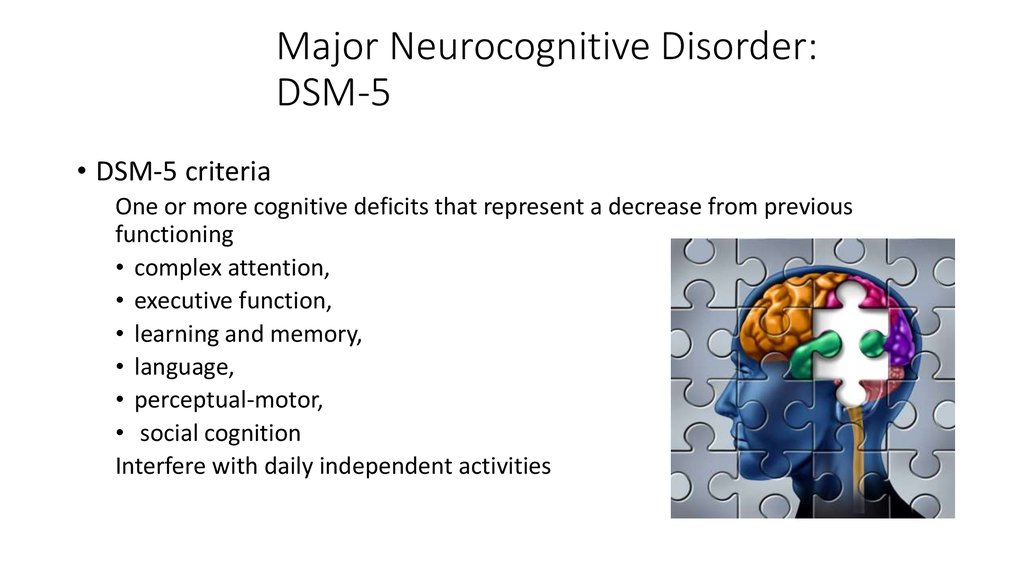
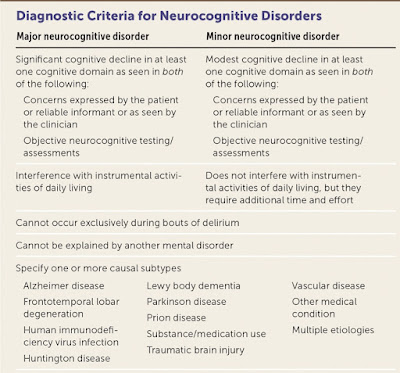
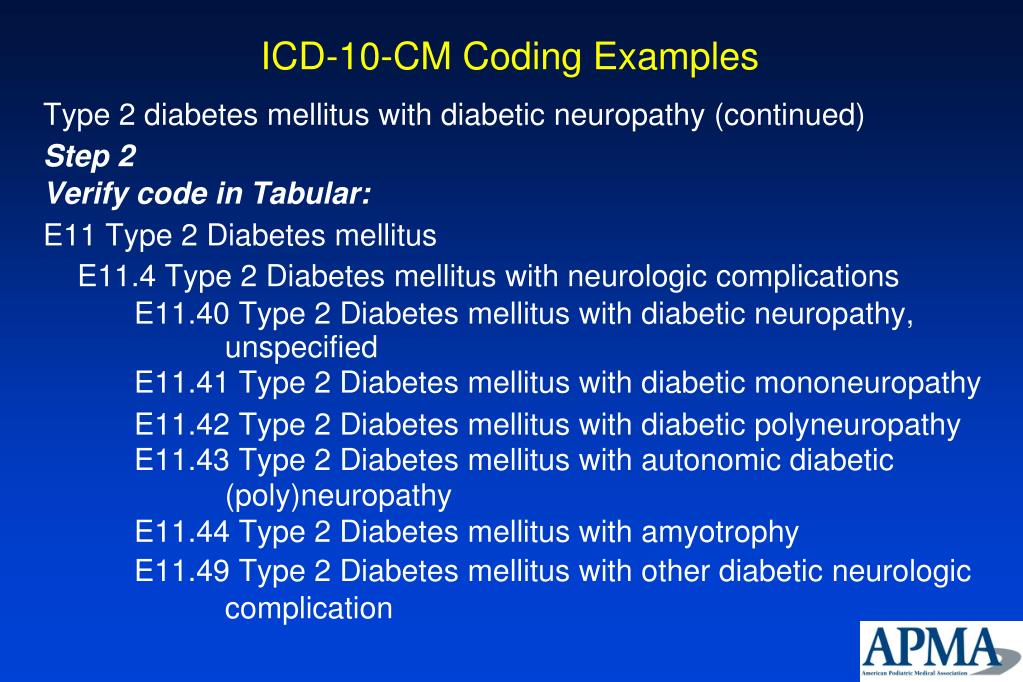
Table 1. Cognitive Functions (according to DSM-V)
Table 2. DSM-V
Diagnostic Criteria for Moderate and Severe Neurocognitive ImpairmentTable 3. Classification of cognitive impairment by severity [5]
Table 4. Diagnostic criteria for depression according to the International Classification of Diseases, 10th Revision
Fig. 1. The increase in the sum of points on the Montreal scale for assessing cognitive functions during therapy with Pronoran (group A), piracetam (group B), ginkgo biloba (group C) and vinpocetine (group D)
Fig. 2. Dynamics of subjective neurological symptoms during therapy with Pronoran (p < 0.05)
About 90% of the area of the human cerebral cortex is involved in cognitive activity. Therefore, most neurological diseases with an interest in the brain are accompanied by certain cognitive disorders. Usually they are combined with changes in the emotional-behavioral sphere, being united by a common pathomorphological and pathophysiological substrate. A practicing neurologist needs to assess the presence and characteristics of cognitive and other neuropsychiatric disorders and take this information into account when diagnosing syndromic, topical and nosological diseases of the nervous system.
Usually they are combined with changes in the emotional-behavioral sphere, being united by a common pathomorphological and pathophysiological substrate. A practicing neurologist needs to assess the presence and characteristics of cognitive and other neuropsychiatric disorders and take this information into account when diagnosing syndromic, topical and nosological diseases of the nervous system.
Cognitive impairment is of equal importance to clinicians in other medical specialties. The target organ of many somatic diseases, in particular, diseases of the cardiovascular system that are widespread in old age, is the brain. In this case, the assessment of the state of the brain is extremely important for assessing the effectiveness of controlling the underlying disease and choosing a therapeutic tactic.
The presence of cognitive impairments has an extremely negative impact on the quality of life of the patient and his immediate family, makes it difficult to treat concomitant diseases and carry out rehabilitation measures.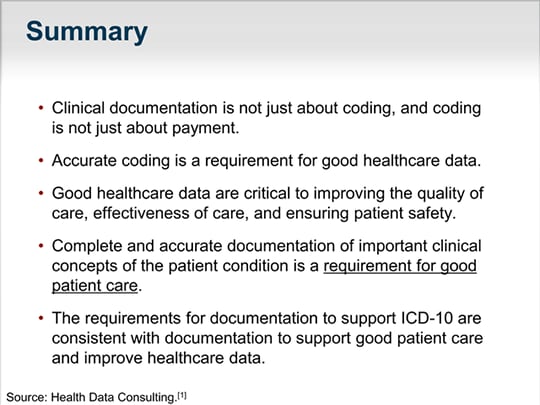 Therefore, timely diagnosis and the earliest possible start of therapy for existing cognitive disorders are very important.
Therefore, timely diagnosis and the earliest possible start of therapy for existing cognitive disorders are very important.
Definition and classification of cognitive impairments
According to the latest revision of the international recommendations for the diagnosis of mental disorders (Diagnostic and statistical manual of mental diseases - DSM-V), cognitive disorders include a decrease in comparison with the premorbid level of one or more higher brain functions that provide the processes of perception, storage, transformation and transmission of information (Table 1) [1].
It is important not only to establish cognitive decline and conduct its qualitative analysis, but also to quantify the severity of existing disorders. It is known that some drugs that are effective in severe cognitive impairment (dementia) have a much lesser effect on cognitive impairment that does not reach the degree of dementia. This is probably due to various neurochemical changes that are noted at the early and later stages of the pathological process [2–4].
Dementia (or, according to DSM-V, severe neurocognitive impairment) is characterized by significant impairment of higher brain functions that interfere with the normal functioning of the patient. With dementia, due to severe cognitive impairment, the patient is at least partially deprived of independence and needs outside help in the most common life situations (for example, when orienting in the area, shopping in a store) (Table 2) [1].
In the treatment of patients with severe cognitive disorders, priority should be given to drugs with a symptomatic effect, which can reduce the severity of disorders and thereby improve the quality of life of patients and their relatives.
The diagnosis of non-dementia cognitive impairment is established in cases where, despite the existing intellectual defect, the patient retains independence in everyday life. At the same time, the patient may feel some difficulties in mental work, which is reflected in complaints. However, the patient overcomes these difficulties without resorting to outside help (Table 2) [1]. In the treatment of patients with non-dementia cognitive disorders, one should not only use symptomatic therapy, but also take measures to prevent dementia.
In the treatment of patients with non-dementia cognitive disorders, one should not only use symptomatic therapy, but also take measures to prevent dementia.
According to the classification of Academician N.N. Yakhno, non-dementia cognitive disorders are divided into mild and moderate (Table 3) [5]. At the same time, patients with moderate impairments may experience difficulties in the most complex and unusual activities for the patient. At the same time, patients with mild disorders are completely independent and independent in all types of activity, including the most difficult one.
In recent years, the attention of neurologists, psychiatrists and representatives of other neurosciences has increased to an even earlier stage of cognitive deficiency - the so-called subjective cognitive impairment. The wording "subjective cognitive impairment" (subjective memory impairment, cognitive complaints) is currently widely used both in the scientific literature and in everyday clinical practice as an independent diagnosis.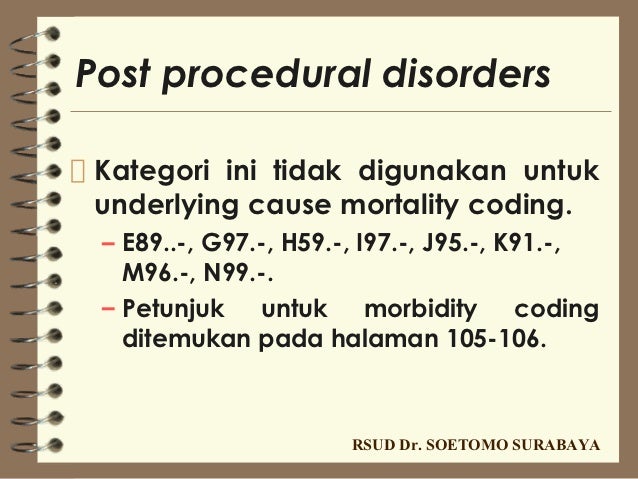 This diagnosis is made if there are cognitive complaints, while the results of objective cognitive tests remain within the age norm.
This diagnosis is made if there are cognitive complaints, while the results of objective cognitive tests remain within the age norm.
Patients may complain of increased forgetfulness, decreased concentration of attention, increased fatigue during mental work, and sometimes difficulty in finding the right word in a conversation. These complaints are a very urgent problem for the patient, which can serve as an independent or main reason for contacting a doctor. At the same time, the use of standard cognitive tests does not reveal any significant deviations from the accepted standards. Patients with subjective cognitive disorders fully maintain independence in everyday life. Cognitive difficulties are also invisible from the outside: relatives, colleagues and other persons always assess the patient's cognitive abilities as quite intact.
Currently, the following international diagnostic criteria (2014) for the syndrome of subjective cognitive impairment are known [6]:
-
patient complaints about a persistent deterioration in mental performance compared to the past, which arose for no apparent reason;
-
the absence of any deviations from the age norm according to the cognitive tests used to diagnose Alzheimer's disease and other dementing diseases;
-
cognitive complaints are not associated with any established diagnosis of a neurological, psychiatric disease or intoxication.

The dissociation between patient complaints, test results, and patients' day-to-day functioning raises legitimate questions about the true nature of the complaints. These issues are still far from being resolved and are being actively studied. At the present stage of scientific knowledge, it seems that patients with subjective cognitive impairments represent a very heterogeneous group, which includes both patients with the earliest stages of the dementing process, and patients with disorders of the anxiety-depressive and hypochondria spectrum.
In some cases, the predominantly subjective nature of disorders is explained by methodological difficulties in objectifying cognitive status. Currently, there are no generally accepted recommendations on the use of specific methods for the diagnosis of dementia or non-dementia cognitive impairment. Therefore, in practice, tests of varying degrees of sensitivity, specificity and reproducibility are used. The use of tests with low sensitivity will lead to underdiagnosis of mild and moderate cognitive impairments and to overdiagnosis of so-called subjective impairments.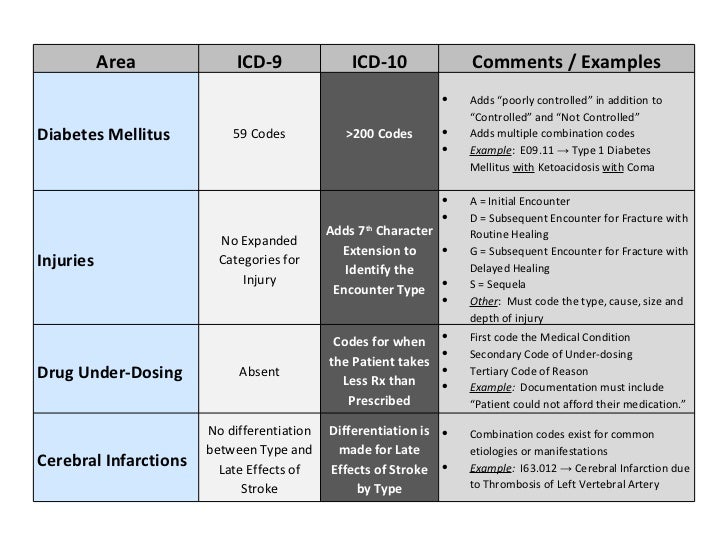
The diagnosis of "subjective cognitive impairment" is often received by patients with a high premorbid intellectual level. The cognitive functions reduced as a result of a cerebral disease in comparison with the individual norm will formally be within the average statistical standard for a long time. Consequently, cognitive decline can remain formally unconfirmed for a long time, in other words, “subjective”.
Complaints of a cognitive nature may be due to anxiety-depressive disorders in the absence of an organic cerebral disease. Thus, patients with a high level of anxiety will be overly concerned about minor situational forgetfulness. In this case, the reason for going to the doctor is such widespread complaints, including among healthy people, such as “I don’t remember why I came to the room”, “I don’t remember what I put where”, “I didn’t recognize a familiar person or didn’t remember him surname", etc.
However, the greatest research interest in a heterogeneous group of patients with subjective cognitive impairments is caused by patients with reduced tolerance to mental stress, since this pathological phenomenon may indeed be the earliest clinical manifestation of the dementing process. As is known, at the very initial stages of a neurodegenerative or cerebrovascular disease, clinical symptoms may be absent, despite the presence of organic brain damage, sometimes significant. This is due to the so-called cerebral reserve, that is, the compensatory capabilities of the brain. The presence of such opportunities will lead to a false negative test result. At the same time, in everyday life, the patient may experience difficulties in special conditions when the cerebral reserve is depleted and cannot overcome the difficulties that arise, for example, in a state of fatigue or emotional stress. At present, the development of the "intellectual treadmill" methodology is being carried out very actively in the world. It will allow assessing the degree of tolerance to increased mental stress, which may decrease to the development of clinically defined cognitive disorders.
As is known, at the very initial stages of a neurodegenerative or cerebrovascular disease, clinical symptoms may be absent, despite the presence of organic brain damage, sometimes significant. This is due to the so-called cerebral reserve, that is, the compensatory capabilities of the brain. The presence of such opportunities will lead to a false negative test result. At the same time, in everyday life, the patient may experience difficulties in special conditions when the cerebral reserve is depleted and cannot overcome the difficulties that arise, for example, in a state of fatigue or emotional stress. At present, the development of the "intellectual treadmill" methodology is being carried out very actively in the world. It will allow assessing the degree of tolerance to increased mental stress, which may decrease to the development of clinically defined cognitive disorders.
International studies show that the risk of developing dementia among patients with subjective cognitive impairment is significantly higher than the average in the population [6]. Therefore, even isolated complaints that are not confirmed by cognitive tests should not be ignored by the attending physicians. They cannot serve as a basis for any specific clinical diagnosis, but their presence is an indication for active prevention, primarily non-pharmacological (mental and physical activity, optimization of nutrition and lifestyle).
Therefore, even isolated complaints that are not confirmed by cognitive tests should not be ignored by the attending physicians. They cannot serve as a basis for any specific clinical diagnosis, but their presence is an indication for active prevention, primarily non-pharmacological (mental and physical activity, optimization of nutrition and lifestyle).
Diagnosis of moderate cognitive impairment
As follows from the above criteria (Table 2), the diagnosis of the syndrome of moderate neurocognitive impairment is based, firstly, on the complaints of patients and / or their relatives, and secondly, on objective test results. At the same time, it should be borne in mind that complaints of a cognitive nature are far from always straightforward. Usually, patients with the so-called amnestic type of the syndrome of moderate neurocognitive impairment complain of a decrease in memory or increased forgetfulness, in which progressive memory disorders predominate in their cognitive status.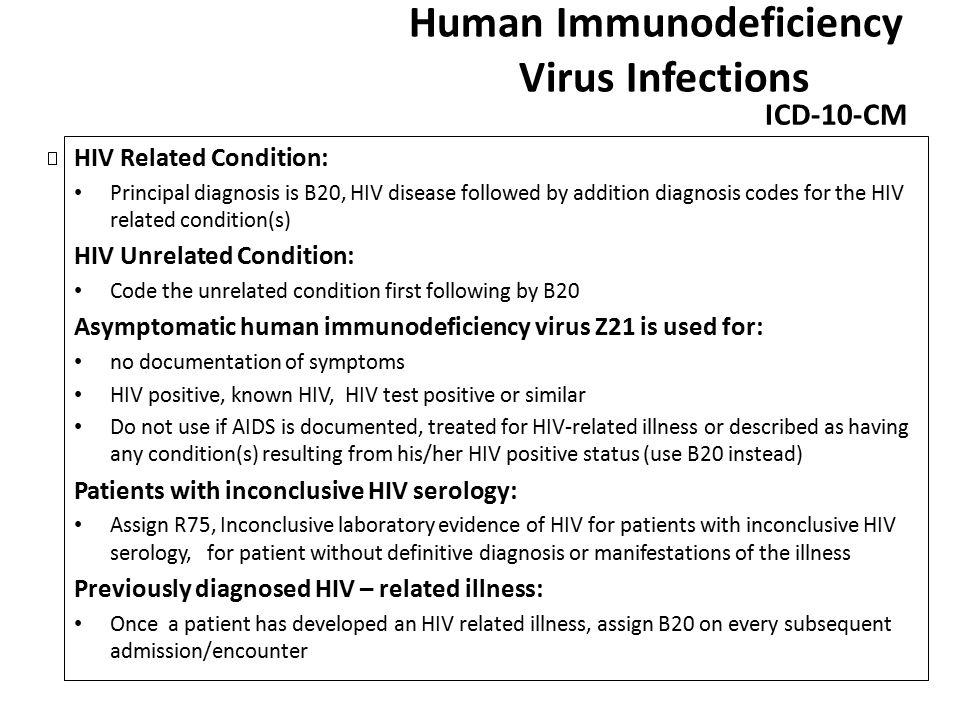 In such patients, Alzheimer's disease is most often established in the future. However, according to the analysis of specialized outpatient admission of patients with cognitive impairment, the most common cause of the syndrome of moderate cognitive impairment is cerebrovascular pathology. Thus, the experience of the first Russian clinic of memory disorders shows that dyscirculatory encephalopathy or the consequences of acute cerebrovascular accidents cause 68% of moderate cognitive impairments [7].
In such patients, Alzheimer's disease is most often established in the future. However, according to the analysis of specialized outpatient admission of patients with cognitive impairment, the most common cause of the syndrome of moderate cognitive impairment is cerebrovascular pathology. Thus, the experience of the first Russian clinic of memory disorders shows that dyscirculatory encephalopathy or the consequences of acute cerebrovascular accidents cause 68% of moderate cognitive impairments [7].
Vascular cognitive impairments in most cases are of the so-called subcortical-frontal type. At the same time, the memory for current events and life events practically does not suffer, and the cognitive status is dominated by a decrease in the concentration of attention and the pace of cognitive activity (bradyphrenia), a violation of frontal control functions (planning and control). A characteristic feature is also the frequent combination of cognitive and emotional-behavioral disorders: depression, apathy or affective lability. It should be emphasized that emotional and behavioral disorders in chronic cerebrovascular insufficiency are of an organic nature and are caused by the same brain damage (dysfunction of fronto-striatal connections) as cognitive impairment. The comorbidity of vascular depression and vascular cognitive impairment is at least 80% [8–11].
It should be emphasized that emotional and behavioral disorders in chronic cerebrovascular insufficiency are of an organic nature and are caused by the same brain damage (dysfunction of fronto-striatal connections) as cognitive impairment. The comorbidity of vascular depression and vascular cognitive impairment is at least 80% [8–11].
Patients with vascular cognitive disorders rarely complain of forgetfulness, since their memory is relatively intact. The structure of complaints is dominated by the so-called subjective neurological symptoms: headache, non-systemic dizziness, noise and heaviness in the head, increased fatigue, sleep disturbances. These symptoms are quite typical for the initial stages of dyscirculatory encephalopathy and in the recent past were considered as an important sign of chronic ischemic brain damage. It is now obvious that headache, dizziness and other unpleasant sensations in the head cannot be a direct result of cerebral ischemia. The pathogenesis of subjective neurological symptoms is more complex and is associated primarily with existing cognitive, emotional and motor disorders. So, headache most often has the character of a tension headache, which, as you know, is almost always caused by anxiety and / or depression. Sleep disturbances also have an emotional cause. Increased fatigue can either be a sign of depression (Table 4) or reflect a decrease in mental performance. In the latter case, this complaint is the subjective equivalent of cognitive disorders. Dizziness in chronic cerebrovascular insufficiency is usually non-systemic and is described as a feeling of unsteadiness when walking. Behind this sensation, as a rule, there are real imbalances due to damage to the fronto-striatal and fronto-cerebellar connections.
So, headache most often has the character of a tension headache, which, as you know, is almost always caused by anxiety and / or depression. Sleep disturbances also have an emotional cause. Increased fatigue can either be a sign of depression (Table 4) or reflect a decrease in mental performance. In the latter case, this complaint is the subjective equivalent of cognitive disorders. Dizziness in chronic cerebrovascular insufficiency is usually non-systemic and is described as a feeling of unsteadiness when walking. Behind this sensation, as a rule, there are real imbalances due to damage to the fronto-striatal and fronto-cerebellar connections.
Subjective neurological symptoms are almost always present in the initial stages of chronic cerebrovascular insufficiency. They cannot be the basis for a diagnosis, but should lead the doctor to suspect a chronic cerebrovascular disease. To confirm the diagnosis, a thorough assessment of the cognitive and emotional status using objective methods is required.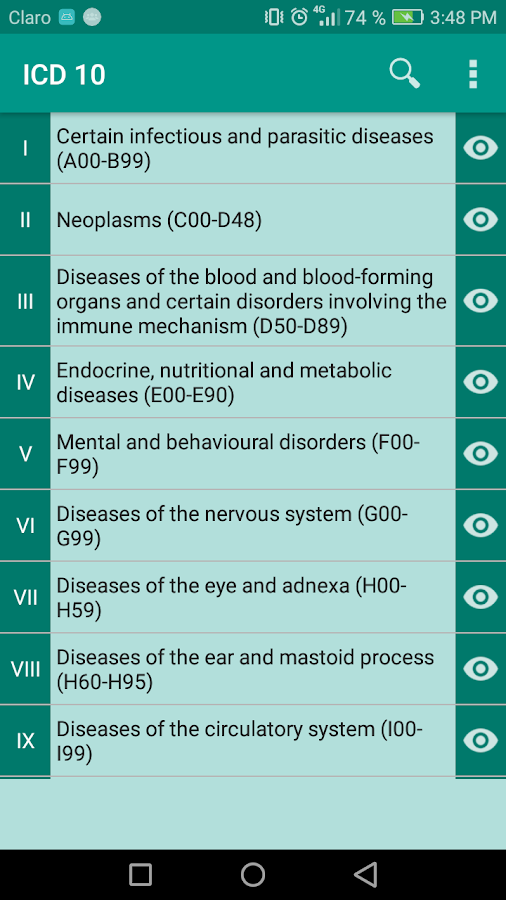 At the stage of moderate (non-dementic) cognitive disorders, the most sensitive methods should be used, for example, the Montreal Cognitive Assessment Scale [12].
At the stage of moderate (non-dementic) cognitive disorders, the most sensitive methods should be used, for example, the Montreal Cognitive Assessment Scale [12].
Pathogenetic and symptomatic therapy of non-dementia cognitive impairments
To date, a unified generally accepted protocol for the management of patients with cognitive impairments that do not reach the severity of dementia has not been finally developed. Many international studies have failed to demonstrate that pharmacotherapy with drugs such as acetylcholinesterase inhibitors, piracetam, non-steroidal anti-inflammatory drugs prevents or reduces the risk of dementia [2-4]. At the same time, the same studies showed the ability of some of the above drugs to reduce the severity of symptoms in patients with mild cognitive impairment syndrome.
Currently, vasotropic and neurometabolic drugs, the dopaminergic and noradrenergic drug piribedil (Pronoran), and NMDA receptor blockers are widely used empirically in everyday clinical practice.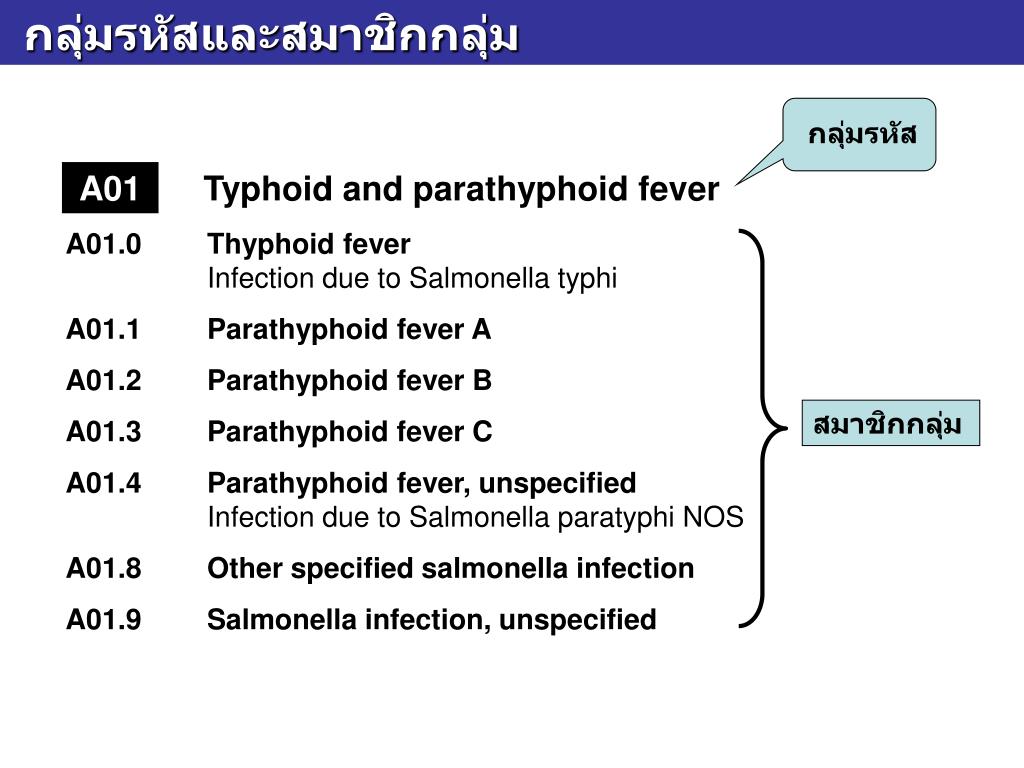
The results of a number of large studies and practical experience indicate the clinical effectiveness of the drug piribedil (Pronoran). Pronoran has a complex mechanism of action: it stimulates postsynaptic D 2 /D 3 - dopamine receptors and blocks presynaptic alpha-adrenergic receptors. At the same time, the blockade of presynaptic adrenergic receptors leads to an increase in cerebral noradrenergic activity. Thus, against the background of the use of this drug, the activity of two cerebral neurotransmitter systems increases: dopaminergic and noradrenergic. Both of these systems are directly involved in cognitive activity. At the same time, it is believed that dopaminergic stimulation of the prefrontal cortex, indirectly through the mesocortical dopaminergic pathway, plays an important role in attention processes and provides intellectual flexibility, that is, the ability to change the behavioral paradigm. Noradrenergic activation is important for the processes of memorization and reproduction of information, since it provides the optimal level of concentration and motivation for mnestic activity.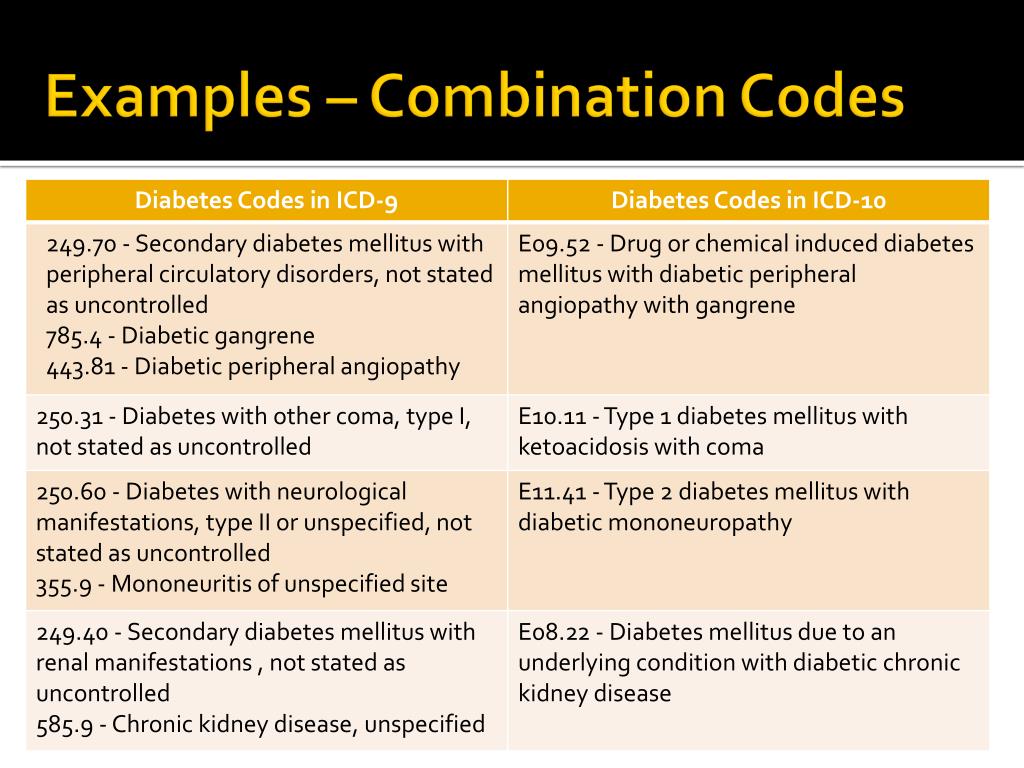 With age, the synthesis and activity of both dopamine and norepinephrine decrease. Therefore, the correction of these neurotransmitter disorders against the background of the use of Pronoran helps to reduce the severity of age-associated disorders of attention and memory. In addition, due to the adrenoblocking and dopaminergic action, Pronoran also has a favorable vasotropic effect, which creates additional benefits in case of cognitive impairment of vascular etiology [13-16].
With age, the synthesis and activity of both dopamine and norepinephrine decrease. Therefore, the correction of these neurotransmitter disorders against the background of the use of Pronoran helps to reduce the severity of age-associated disorders of attention and memory. In addition, due to the adrenoblocking and dopaminergic action, Pronoran also has a favorable vasotropic effect, which creates additional benefits in case of cognitive impairment of vascular etiology [13-16].
In clinical practice, Pronoran is used to treat mild and moderate cognitive impairment that does not reach the severity of dementia in patients over 50 years of age. The drug can be prescribed both for vascular cognitive impairment and at the initial stages of the neurodegenerative process. A large number of clinical studies have been performed for this indication, including those using a double-blind method. For example, in France in the 1980s. 14 clinical studies were conducted, in which more than 7 thousand patients with non-dementia cognitive impairments took part. It has been shown that Pronoran contributes to a significant improvement in memory, concentration and intellectual flexibility, that is, the ability to change the paradigm of behavior depending on external conditions [17, 18]. In 2001, the clinical efficacy of Pronoran was again demonstrated by D. Nagaradja and S. Jayashree. The authors used Pronoran in the syndrome of moderate cognitive impairment in accordance with modern diagnostic criteria. It was shown that against the background of the study drug, there was a more than two-fold increase in the frequency of cognitive improvement on the short mental status assessment scale compared with placebo, which was statistically and clinically significant [19].
It has been shown that Pronoran contributes to a significant improvement in memory, concentration and intellectual flexibility, that is, the ability to change the paradigm of behavior depending on external conditions [17, 18]. In 2001, the clinical efficacy of Pronoran was again demonstrated by D. Nagaradja and S. Jayashree. The authors used Pronoran in the syndrome of moderate cognitive impairment in accordance with modern diagnostic criteria. It was shown that against the background of the study drug, there was a more than two-fold increase in the frequency of cognitive improvement on the short mental status assessment scale compared with placebo, which was statistically and clinically significant [19].
Currently, Russian specialists also have significant experience in using Pronoran in patients with cognitive impairments that do not reach the severity of dementia. Thus, as part of the PROMETHEUS study, 574 patients from 33 cities in 30 regions of Russia, including 336 women and 207 men, aged 60 to 89 years (mean age 69.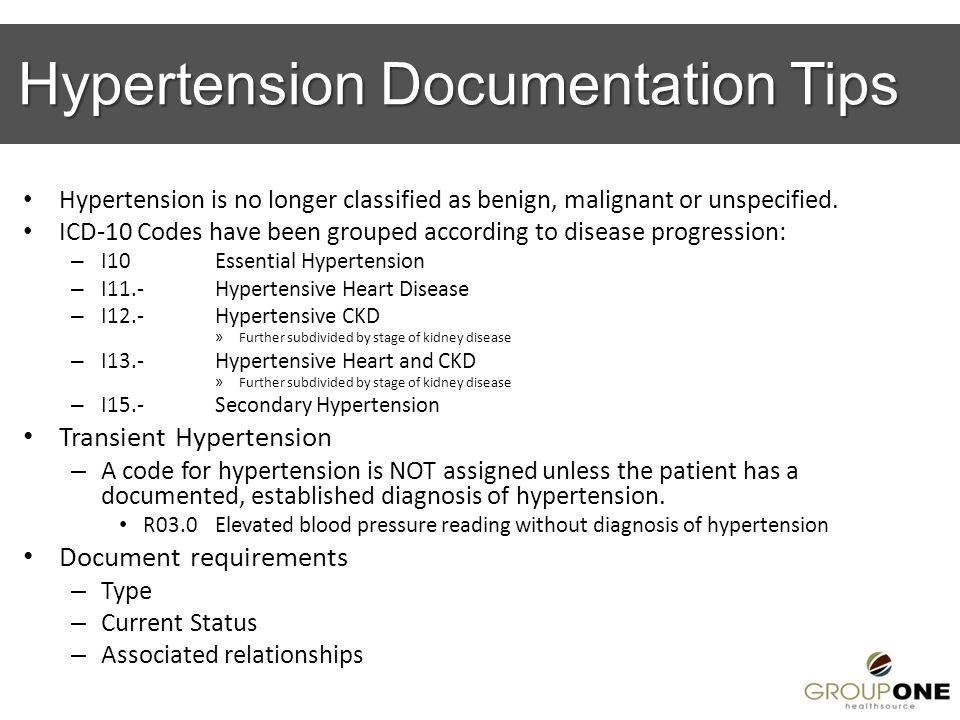 5 ± 5.5 years) received Pronoran with mild or moderate cognitive impairment. . Patients with cognitive complaints who scored 25–27 points on the Mini Mental Status Scale or who performed the clock drawing test with errors but did not meet the diagnostic criteria for dementia were selected for treatment. During therapy, a statistically significant improvement in cognitive functions was recorded, which was noted as early as the sixth week of treatment and further increased until the end of the 12-week follow-up. At the same time, one part of the patients received Pronoran monotherapy, and the other part received Pronoran in combination with vasotropic and / or neurometabolic drugs. No significant difference was shown between these groups of patients, that is, the combination of Pronoran with vasotropic and neurometabolic therapy had no advantages over monotherapy with the study drug [20, 21].
5 ± 5.5 years) received Pronoran with mild or moderate cognitive impairment. . Patients with cognitive complaints who scored 25–27 points on the Mini Mental Status Scale or who performed the clock drawing test with errors but did not meet the diagnostic criteria for dementia were selected for treatment. During therapy, a statistically significant improvement in cognitive functions was recorded, which was noted as early as the sixth week of treatment and further increased until the end of the 12-week follow-up. At the same time, one part of the patients received Pronoran monotherapy, and the other part received Pronoran in combination with vasotropic and / or neurometabolic drugs. No significant difference was shown between these groups of patients, that is, the combination of Pronoran with vasotropic and neurometabolic therapy had no advantages over monotherapy with the study drug [20, 21].
In the largest Russian non-comparative study, Pronoran was treated by more than 2,000 patients aged 50 to 94 years (mean age 64. 9 ± 8.3 years) with a diagnosis of stage 1 or 2 dyscirculatory encephalopathy and with mild or moderate cognitive impairment. violations. All patients took Pronoran for three months. According to the attending physicians, in 2/3 of cases there was a significant or moderate improvement in cognitive and other neurological functions [22].
9 ± 8.3 years) with a diagnosis of stage 1 or 2 dyscirculatory encephalopathy and with mild or moderate cognitive impairment. violations. All patients took Pronoran for three months. According to the attending physicians, in 2/3 of cases there was a significant or moderate improvement in cognitive and other neurological functions [22].
According to some data, the magnitude of the therapeutic effect of dopamine and noradrenergic therapy in relation to non-dementia cognitive disorders may be greater than that of other vasotropic and neurometabolic drugs actively used in clinical practice. In the FUETE study, 189 patients were observed, including 139 women and 57 men, aged 42 to 82 years (mean age 63.6 ± 8.5 years) with cognitive disorders that did not reach the severity of dementia, against the background of arterial hypertension and cerebral atherosclerosis . The patients were treated with various drugs, while the representatives of the therapeutic groups did not differ in age, level of education and clinical features of the underlying disease.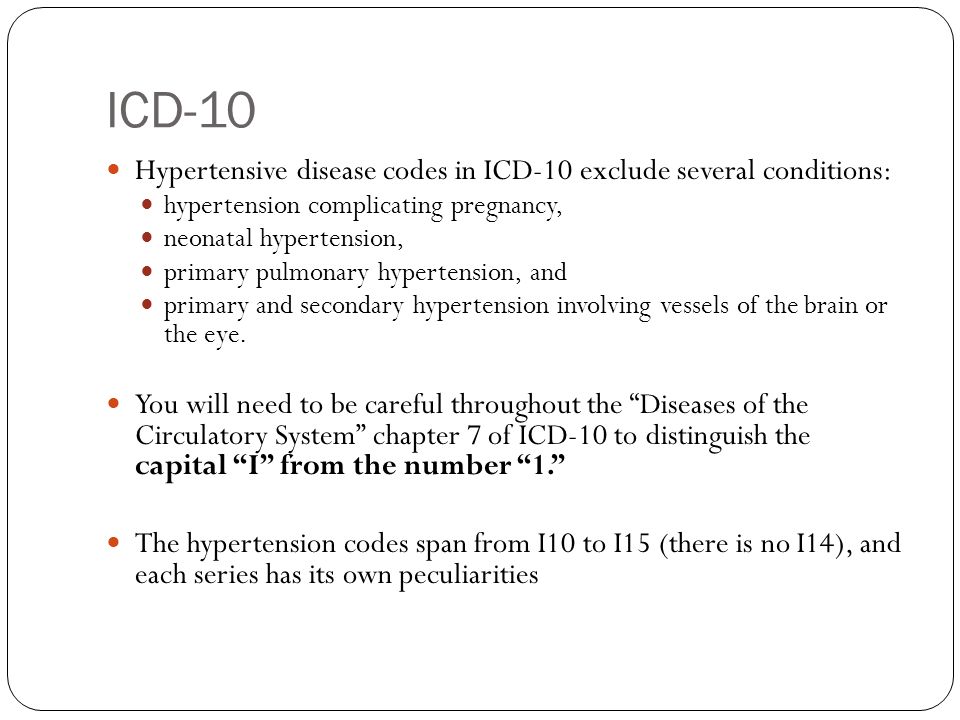 Against the background of the therapy, there was a regression of both subjective and objective cognitive disorders in all compared therapeutic groups. At the same time, the severity of subjective improvement and objective dynamics of cognitive tests against the background of the use of Pronoran after two months of therapy were significantly greater compared with vasotropic and neurometabolic therapy (Fig. 1) [23].
Against the background of the therapy, there was a regression of both subjective and objective cognitive disorders in all compared therapeutic groups. At the same time, the severity of subjective improvement and objective dynamics of cognitive tests against the background of the use of Pronoran after two months of therapy were significantly greater compared with vasotropic and neurometabolic therapy (Fig. 1) [23].
Regression of cognitive disorders, according to special tests, is the main criterion for the effectiveness of the therapy. However, as noted above, many patients with moderate cognitive impairment, primarily of a vascular nature, also complain of headache, non-systemic dizziness, noise, heaviness or other unpleasant sensations in the head, increased fatigue and sleep disturbances. These complaints are of the same nature and are associated with both cognitive impairment and changes in the emotional status of patients at the initial stage of chronic cerebrovascular insufficiency. They significantly reduce the quality of life of patients and are often the main reason for visiting a neurologist. Therefore, the dynamics of subjective neurological symptoms in patients with a syndrome of moderate neurocognitive disorders of vascular etiology during therapy is extremely important for assessing the significance of the clinical effect and the degree of influence of therapy on the daily life of patients. Regression of subjective neurological symptoms contributes most to adherence to therapy.
They significantly reduce the quality of life of patients and are often the main reason for visiting a neurologist. Therefore, the dynamics of subjective neurological symptoms in patients with a syndrome of moderate neurocognitive disorders of vascular etiology during therapy is extremely important for assessing the significance of the clinical effect and the degree of influence of therapy on the daily life of patients. Regression of subjective neurological symptoms contributes most to adherence to therapy.
In the study by N.N. Yakhno et al. (2006) 29 patients with a diagnosis of "moderate cognitive impairment" against the background of dyscirculatory encephalopathy of the first or second stage received Pronoran for three months [24]. At the same time, no other vasotropic or neurometabolic drugs were used. During treatment with Pronoran, the frequency and severity of headache, dizziness, fatigue and subjective feeling of forgetfulness significantly decreased (Fig. 2). Other authors also reported on the weakening of subjective neurological symptoms during the use of Pronoran [17, 18].